Abstract
Acute pancreatitis (AP) is a digestive emergency and can develop into a systematic illness. The role of the gut in the progression and deterioration of AP has drawn much attention from researchers, and areas of interest include dysbiosis of the intestinal flora, weakened intestinal barrier function, and bacterial and endotoxin translocation. Short-chain fatty acids (SCFAs), as one of the metabolites of gut microbiota, have been proven to be depleted in AP patients. SCFAs help restore gut homeostasis by rebuilding gut flora, stabilizing the intestinal epithelial barrier, and regulating inflammation. SCFAs can also suppress systematic inflammatory responses, improve the injured pancreas, and prevent and protect other organ dysfunctions. Based on multiple beneficial effects, increasing SCFAs is an essential idea of gut protective treatment in AP. Specific strategies include the direct use of butyrate or indirect supplementation through fiber, pre/pro/synbiotics, or fecal microbiota transplantation as a promising adjective therapy to enteral nutrition.
Keywords: acute pancreatitis, gut microbiota, short-chain fatty acids
1. Introduction
Acute pancreatitis (AP) is a common digestive emergency and can develop into a systematic illness with a higher risk of death. According to the complications present, AP can be classified as mild (MAP), moderately severe (MSAP), or severe (SAP). About one-fifth of the cases will develop into SAP, which makes individuals prone to combined multi-organ failure (MOF) [1]. Organ dysfunction usually occurs in the early stage, and infection of pancreatic or peripancreatic necrotic tissue is the leading cause of death in the late stage. Furthermore, gut dysfunction plays a vital role in the deterioration of AP, which is associated with infectious complications and is described as the “motor of MOF” [2]. Recent studies have found that the progression of SAP is associated with early systemic inflammatory response syndrome (SIRS), dysbiosis of the intestinal flora, weakened intestinal barrier function, and bacterial and endotoxin translocation.
In AP patients, there are changes in intestinal flora diversity and composition. The increase of pathogenic bacteria and the reduction of probiotics have been detected, as well as decreased levels of short-chain fatty acids (SCFAs). SCFAs, mainly including acetate, propionate, and butyrate, are produced by microbial fermentation of undigested dietary carbohydrates in the intestine. There is a biological gradient for SCFAs from the gut lumen to the periphery [3]. As one of the intestinal flora’s metabolites, SCFAs directly provide energy for intestinal mucosal epithelial cells. The remaining part can be absorbed into the bloodstream to provide energy to other cells in the body [4,5]. SCFAs participate in glucose and lipid metabolism as substrates after transporting to hepatocytes and adipocytes and regulate appetite by interplaying with neurons [6,7]. SCFAs are also important signaling molecules involved in stabilizing the intestinal barrier and promoting intestinal immunity. Specifically, SCFAs protect the intestinal barrier by regulating the expression and distribution of tight junction proteins and promoting the secretion of mucin on the intestinal surface [8,9]. Moreover, SCFAs suppress the production of pro-inflammatory cytokines and promote immune cell recruitment, thus being regarded as a potential bioactive molecule for treating intestinal diseases [10,11]. There are two major functional pathways of SCFAs: the inhibition of histone deacetylase (HDAC) to exert epigenetic effects and the activation of G protein-coupled receptors (GPRs) to transfer signals [12]. Microbiota alterations and the decreased production of SCFAs are involved in the increase of intestinal permeability, leading to intestinal bacterial translocation, pancreatic tissue necrosis and infection, and even sepsis and MODS [13].
However, there is still a lack of specific evaluation and treatment methods for gut dysfunction [14]. No quantitative method exists to detect it clinically except for doctors’ observations. For example, the loss of intestinal peristalsis indicates impaired intestinal function. One of the most well-studied interventions is early enteral nutrition. It can mitigate mortality, organ failure, sepsis, and necrosis infection by replenishing caloric losses, increasing blood flow to preserve the bowel mucosa, and stimulating intestinal motility [15,16]. Other gut protection strategies include restoring intestinal dynamics, selective decontamination of the digestive tract, and regulating intestinal flora by probiotics. SCFAs will be another important intervention target for AP in the future. Here, we review the changes in microbiota and SCFAs in AP, their possible mechanisms, and the potential therapeutic value of SCFAs, collectively aiming to provide a new theoretical basis for intestinal protective therapy of AP.
2. Alteration of Gut Microecology in AP
The role of dysbiosis in pancreatic diseases has attracted much attention with the rapid evolvement of microbiota research. Compared with healthy controls, AP is accompanied by intestinal microecological dysbiosis, although in the early stages of the disease course. Multiple studies found that the diversity of intestinal flora decreased either in AP patients or mice models (Table 1). The increased pathogenic bacteria and decreased probiotics are prominent features. At the phylum level, increased Bacteroidetes and Proteobacteria were found in AP patients with fewer Firmicutes and Actinobacteria. At the genus level, the main characteristic alterations were increased Enterobacteriaceae, Enterococcus, and Escherichia-Shigella, with decreased Bifidobacterium [17,18]. The main secretory products of Bifidobacterium are acetic acid and lactic acid, which can lower the intestinal pH and inhibit the growth of harmful intestinal bacteria. Reduced Bifidobacterium are also recognized cellulose degraders that promote the fermentation of dietary fiber and produce SCFAs. Stratified analysis of AP patients found that the microbiota alteration differed with the disease severity. Among these alterations, the decrease of SCFA-producing bacteria affected the integrity of the intestinal barrier and worsened the severity of AP. Zhu et al. reported that SAP was characterized by reduced commensal bacteria, such as Bacteroides, Alloprevotella, and Blautia. Their linear discrimination analysis coupled with effect size (LEfSe) analysis revealed a significant increase of Acinetobacter, Stenotrophomonas, and Geobacillus and a substantial reduction of Bacteroides, Alloprevotella, Blautia, and Gemella in SAP than mild acute pancreatitis (MAP) and moderately severe acute pancreatitis (MSAP) [18]. Previous studies have shown that these reduced organisms could facilitate fermentation and produce SCFAs [19,20,21,22]. Yu et al. found more Bacteroides, Escherichis-Shigella, and Enterococcus in MAP, MSAP, and SAP, respectively. Moreover, Eubacterium hallii, one of the butyrate-producing bacteria, was the most decreased strain in MASP and SAP patients [23].
Recently, investigations of microbial composition have extended to the pancreas, which was once thought to be a sterile organ. Several studies supported the fact that microorganisms inhabit the pancreas in a nonpathological state, namely inherent pancreatic microbiota [24,25]. However, there has not been a specific definition of normal pancreatic microbiota based on the limited research. Potential sources and routes of pancreatic bacteria include the esophagus, stomach, duodenum, or biliary tract microbiota via the pancreatic duct or translocation from the lower gastrointestinal tract through the portal circulation or mesenteric lymph nodes [14]. Pancreatic infection is a significant cause of complications and death in patients with acute necrotizing pancreatitis (ANP). About one-third of the patients with pancreatic necrosis will develop infectious necrosis [1], but it is more common later in the clinical course. Most infections are single intestinal microbial infections, such as Escherichia coli, Pseudomonas, Klebsiella, and Enterococcus, indicating the translocation of gut bacteria [26,27]. An ANP mice model study evaluated the spatial (lumen versus mucosa) and regional composition and function of the microbiota from the duodenum, ileum, caecum, colon, pancreas, and blood using 16S rRNA gene amplicon sequencing. Results showed that the distal gut microbiota was significantly impacted, and the duodenal microbiota might also play a role in bacterial translation and secondary infections [28].
Table 1.
Gut microbiota dysbiosis in acute pancreatitis compared with healthy controls.
| Studies | Subjects | Sample | Phylum | Genus | Species |
|---|---|---|---|---|---|
| Tian 2015 [29] | 76 AP and 32 HC | Fecal |
Enterobacteriaceae ↑ Enterococcus ↑ Bifidobacterium ↓ |
||
| Zhang 2018 [17] | 45 AP and 44 HC | Fecal | Bacteroidetes ↑ Proteobacteria ↑ Firmicutes ↓ Actinobacteria ↓ |
||
| Zhu 2019 [18] | 130 AP and 35 HC | Fecal | Proteobacteria ↑ Bacteroidetes ↓ |
Escherichia/Shigella ↑ Enterococcus ↑ An unknown genus in family of Enterobacteriaceae ↑ Prevotella_9 ↓ Faecalibacterium ↓ Blautia ↓ Lachnospiraceae ↓ Bifidobacterium ↓ |
|
| Yu 2020 [23] | 60 AP and 20 HC | Rectal swab |
Finegoldia ↑ Anaerococcus ↑ Enterococcus ↑ Eubacterium hallii ↓ |
Blautia ↓ Finegoldia ↑ |
|
| van den Berg 2021 [30] | 35 AP and 15 HC | Fecal | Proteobacteria ↑ |
Escherichia/Shigella ↑ Streptococcus ↑ Butyrate producers ↓ 1 |
AP, acute pancreatitis; HC, health controls. The arrows indicate the alteration of gut microbiota in AP compared with healthy controls. 1 A panel of butyrate producers based on genus taxonomy was constructed based on butyrate-producing taxa (Alistipes, Anaerostipes, Butyricicoccus, Butyricimonas, Butyrivibrio-010, Coprococcus_1, Coprococcus_2, Coprococcus_3, Eubacterium, Faecalibacterium, Flavonifractor, Odoribacter, Oscillibacter, Pseudoflavonifractor, Roseburia, Ruminococcus_2, Subdoligranulum).
3. Function of SCFAs in AP
3.1. Mitigation of Intestinal Injury
Gut barrier dysfunction is present in three of five patients with AP, which is associated with poor clinical outcomes [31]. Considering the site of SCFAs production, most studies on the mechanism of SCFAs focused on intestinal homeostasis [32]. Intestinal homeostasis is an organic and dynamic balancing state involving the gut microbiota, the intestinal epithelial barrier, and the mucosal immune barrier. The protective role of SCFAs can also be summarized in these three aspects. SCFAs can rebuild the disordered intestinal flora. After butyrate supplementation, the abundance of SCFA-producing Alloprevotella and Muribaculaceae increased [33,34]. SCFAs also act directly on the intestinal epithelium to protect the integrity of the intestinal barrier, which can be observed at the histological level. Moreover, SCFAs are a critical carbon source for colonic enterocytes [35]. SAP rats in the butyrate treatment group showed mitigated mucosa lesions and decreased epithelial apoptosis. Butyrate protected the intestinal barrier by upregulating tight junction proteins, such as zonula occludens-1 (ZO-1), claudin, and occludin [33,34]. In addition to the epithelial barrier repairment, butyrate also well-restored mucin-secreting goblet cells, thus protecting the damaged mucous membrane [33]. For the immunity barrier, pre-treatment with sodium butyrate ameliorated intestinal inflammation and injury by reducing intestinal pro-inflammatory cytokines, including tumor necrosis factor (TNF)-α and interleukin (IL)-6. Butyrate also increased the expression of Foxp3 at both mRNA and protein levels, detected in immunofluorescence staining and flow cytometry analysis. These results supported the elevated percentage of regulatory T cells (CD4+, CD25+, Foxp3+), which could maintain intestinal homeostasis by preventing inappropriate innate and adaptive immune responses [36,37,38].
SAP patients can develop intraabdominal hypertension (IAH), which can progress to abdominal compartment syndrome (ACS) with a high mortality rate of 66.7%. These severe abdominal complications may correlate with pancreatic necrosis and intra-abdominal infection, likely resulting from bacterial translocation [39,40,41]. Clostridium butyricum is an anaerobic bacterium that can ferment dietary fibers to produce SCFAs. SAP + IAH rats who received oral C. butyricum or butyrate had reduced pathological severity scores of intestinal injury and plasma levels of inflammatory markers. Compared with the nontreated group, the expression of ZO-1, claudin-1, and occludin increased, and claudin-2, matrix metallopeptidases 9 (MMP9), and TNF-a lowered in the treatment group, indicating repairment of the intestinal mucosal barrier. The treatment also rebuilt the intestinal flora, significantly increasing richness and diversity, growing probiotics (Lactobacillus, Coprococcus, and Allobaculum), and decreasing pathogenic species (Bacteroides, Escherichia, Helicobacter, and Desulfovibrio) [42]. These multiple reversed pathological responses suggested butyrate supplementation as a promising therapeutic strategy to restore intestinal function. Another study further confirmed the protective effect of C. butyricum or butyrate via downregulating MMP9 expression [43]. MMP9 was upregulated in intestinal tissues of the SAP model according to existing studies [44,45], and is one of the members of MMPs that can degrade and remodel extracellular matrix. MMPs are also involved in the inflammation process and intestinal barrier injury. For example, MMPs can increase endothelial cell permeability by disrupting tight junction proteins [46]. Additionally, Kocael et al. reported that MMP9 overexpression also facilitated the loss of intestinal villous in the mesenteric ischemia-reperfusion injury model [44]. Therefore, MMP9 is a vital molecule mediating intestinal injury and a potential target of SCFA supplementation.
3.2. Reduction of Pancreas Injury
There has been evidence for the direct interaction between the pancreas and SCFAs and the existence of the gut–pancreatic axis [47]. Cathelicidin-related antimicrobial peptide (CRAMP) production by insulin-secreting beta-cells is controlled by SCFAs produced by the gut microbiota. However, local functions of SCFAs in the pancreatic tissue of AP are limitedly studied. In the AP mice model, butyrate mitigated the severity of AP in multiple ways, reflected in both the pancreas and the gut. A study provided new insights into tissue-specific mechanisms of butyrate. Pre-treatment with sodium butyrate decreased the infiltration of macrophages and neutrophils in the pancreas and reduced levels of intestinal pro-inflammation cytokines. Sodium butyrate acted as an HDAC1 inhibitor in the pancreas or as a GPR109A agonist in the colon to suppress the activation of NLRP3 inflammasome [48]. Lei et al. also reported that, in the heparanase-exacerbated AP model, the supplementation of Parabacteroides or sodium acetate could reduce neutrophils in blood and infiltration in the pancreas [49]. Similarly, in another study, sodium butyrate supplementation significantly reduced the proportion of neutrophils, macrophages, and M2-type macrophages in the pancreatic tissue from AP mice and inhibited IL-1b, CXCL1, and TNF-a levels [34].
3.3. Prevention and Protection of Other Organ Dysfunctions
In the early phase of AP, inflammation of the pancreas activates cytokine cascades, which are clinically manifested as SIRS [50]. Avoidance of SIRS or timely termination of SIRS is the key to early control of AP. Fecal concentrations of butyrate, propionate, and acetate in patients with severe SIRS on admission decreased significantly compared with those in healthy volunteers. They remained low throughout the six weeks of intensive care unit (ICU) stay. In patients with gastrointestinal complications, including enteritis and dysmotility, the level of SCFAs was even lower [51]. Zhang et al. found that sodium butyrate treatment could inhibit the nuclear factor-κB (NF-κB) signaling pathway and lower the expression of High-mobility group box-1 (HMGB1), which is a late cytokine mediator stimulating the release of pro-inflammatory cytokines. The SAP model had reduced pathological lesions; reduced serum levels of HMGB1, TNF-a, and IL-6; as well as diminished HMGB1 mRNA levels and NF-κB activity [52]. Another study that used the SAP model also evaluated the plasma levels of several markers. The administration of Clostridium butyricum or butyrate reduced pro-inflammatory cytokines, including TNF-a, IL-6, IL-1β, and IL-12 [42]. What is more, SCFAs mitigated the inflammation in the lipopolysaccharide (LPS)-induced septic shock model by upregulating the anti-inflammatory cytokine IL-10 [53].
Patients with persistent SIRS are at risk for one or more organ failures, the leading cause of early death. Three organ systems should be assessed to define organ failure, including respiratory, cardiovascular, and renal systems. Organ failure may be transient with remission within 48 h in MSAP or persistent for more than 48 h in SAP [50]. SCFAs prevent or protect against organ failures by restoring the intestinal barrier and suppressing systematic inflammatory responses. Some changes mediated by SCFAs in specifically targeted organs, such as the lung and kidney, are also observed.
One-third of patients presenting with severe AP develop acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). The primary manifestation is hypoxemia, which can even develop into acute respiratory distress syndrome (ARDS). The lung injury is characterized by increased pulmonary microvasculature permeability and subsequent protein-rich exudate leakage into the alveolar spaces, forming the hyaline membrane [54,55]. The concept of the gut–lung axis has been proposed based on the bidirectional crosstalk between these two organs [56]. SCFAs provide one of these crosstalk pathways. Human lung tissue contained variable acetate and propionate levels, likely originating from the gut and transiting to the lung. SCFA receptors, namely free fatty acid receptor (FFAR) 2 and FFAR3, were expressed in vitro in alveolar macrophages (AM) and alveolar type 2 epithelial (AT2) cells, and exposure to LPS regulated this expression. This finding supported the direct effects of SCFAs on the lung [57]. Specifically, gut microbiota-produced LPS and SCFAs could strongly influence the course of lung injury and infections [58,59]. SCFAs significantly protected animals from LPS-induced ALI, as evidenced by suppressed HMGB1 release and NF-κB activation, decreased production of pro-inflammatory cytokines and reactive oxygen species, declined immune cell counting, and alleviated LPS-induced microvascular permeability and lung histological damage [60,61,62]. In the hypoxic model, butyrate treatment decreased the accumulation of alveolar and interstitial lung macrophages, prevented hypoxia-induced pulmonary vascular edema and vascular leakage, and upregulated the expression of tight junctions in lung microvascular endothelial cells [63]. Tian et al. similarly found that enrichment of propionate-producing gut bacteria (especially Lachnospiraceae) was related to reduced lung inflammation following lung ischemia-reperfusion injury in vivo [58]. Compared with AP patients without ARDS, AP with ARDS had higher abundances of the Proteobacteria phylum, the Enterobacteriaceae family, Escherichia-Shigella, and the Klebsiella pneumoniae genus but lower abundances of the Bifidobacterium genus [64]. Thus, gut microbiota and SCFAs may play essential roles in pancreatitis-associated lung injury through the above mechanisms, although no studies used the AP model.
Acute kidney injury (AKI) is another frequent complication of SAP. A comprehensive, retrospective, observational study reported an overall AKI prevalence of 7.9% among hospitalized patients with AP [65]. The pathogenesis may include increased vascular permeability, hypovolemia, inflammation, vasoconstriction, intravascular coagulation, and direct nephrotoxic effects [66]. Predictors for a higher likelihood of AKI include higher age, exhibiting biological male sex, a more significant number of co-morbidities, and electrolyte imbalance [65]. Andrade-Oliveira et al. observed that therapy with the three main SCFAs (acetate, propionate, and butyrate) improved renal dysfunction. In specific, SCFAs treatment reduced pro-inflammatory cytokines and chemokines in kidney tissue and serum, with low levels of toll-like receptor 4 (TLR4) mRNA and lesser activation of the NF-κB pathway. SCFA treatment also diminished apoptotic cells in kidney tissue, but increased the proliferation of kidney epithelial cells, thus promoting the restoration of injured tissue. Mice treated with acetate-producing bacteria also achieved better outcomes after AKI, having increased acetate levels in feces and plasma, low serum levels of creatinine and urea, and low serum levels of cytokines and chemokines [67]. Another study showed that a high-fiber diet had similar protective effects for AKI [68]. Zhang et al. evaluated other organs in the SAP model after sodium butyrate treatment and found alleviated liver and renal tissue histological injuries and improved hepatic and renal function reflected in decreased alanine aminotransferase and creatine levels [52].
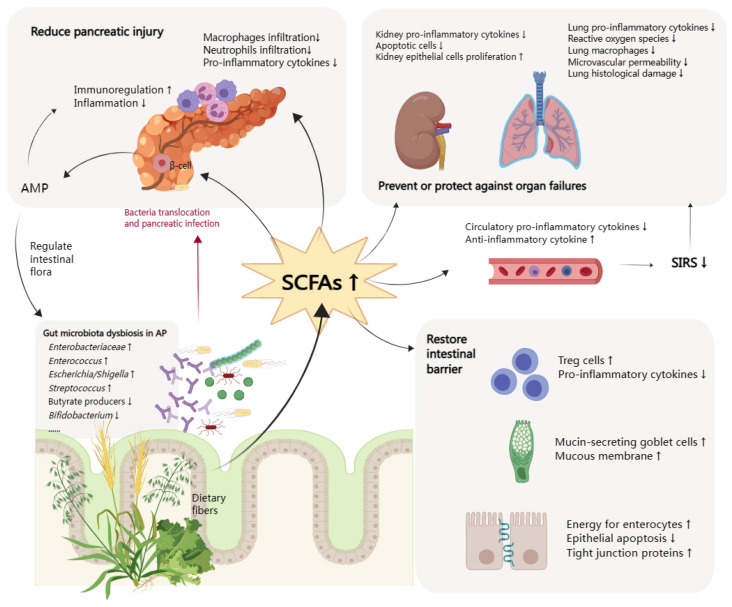
The late phase of AP is characterized by the persistence of systematic signs of inflammation or local complications, with an increased risk of infection. Up to 20% of AP patients develop extra-pancreatic infections, such as bloodstream infections, pneumonia, and urinary tract infections [69]. In a meta-analysis of studies performed in the ICU, there was a significantly lower risk of infection in the patients who received early enteral nutrition. Infectious complications occurred in 19% of the early nutritional group compared to 41% in the delayed group [70]. Considering that SCFAs can protect the intestinal barrier and prevent bacteria translocation, SCFAs are a good choice to reduce the incidence of systemic infectious complications of AP as a supplement to early enteral nutrition. The above-mentioned possible mechanisms of SCFAs in AP are summarized in Figure 1.
Figure 1.
Function of short chain fatty acids in acute pancreatitis. SCFAs, short chain fatty acids; AMP, antimicrobial peptide; SIRS, systemic inflammatory response syndrome; AP, acute pancreatitis; Treg cells, regulatory T cells. The arrows (↑ and ↓) indicate the alternation of gut microbiota in AP or histopathological changes after increasing SCFAs.
4. Treatment Potential of SCFAs in AP
4.1. Dietary Fiber Supplementation
Critically ill SAP patients treated with enteral nutrition and broad-spectrum antibiotics often present with diarrhea, indicating intestinal dysfunction. Compared with healthy volunteers, fecal microbiota mass and SCFAs were significantly lower in critically ill SAP patients, indicating gut dysbiosis and suppression of colonic fermentation. After 2–5 week fiber supplementation, there was a six-fold increase in fecal SCFAs and microbial counts of specific butyrate producers, with the resolution of diarrhea [71,72]. In a prospective double-blind randomized controlled trial (RCT) conducted by Karakan et al., nasojejunal enteral nutrition with prebiotic fiber supplementation in SAP improved hospital stay, duration of nutrition therapy, acute phase response, and overall complications compared to standard enteral nutrition therapy [73]. Therefore, fiber supplementation may preserve gut function in critically ill patients through increased SCFAs. It is an easy and safe improvement of standard enteral nutrition. However, the efficacy of fiber supplementation may be related to the abundance of SCFA-producing bacteria and intestinal motility.
4.2. Probiotics, Prebiotics, and Synbiotics
Due to the controversial evidence from clinical trials, pre/pro/synbiotics for AP have not been positively accepted and recommended in guidelines. The main conclusions of research on probiotics have undergone several changes in the last 20 years (Table 2). An early small-scale RCT reported that specific lactobacillus and fiber supplements effectively reduced pancreatic sepsis and the number of surgical interventions in AP [74]. Another RCT suggested that early nasojejunal feeding with synbiotics (Lactobacilli preparations and bioactive fibers) may prevent organ dysfunctions in the late phase of SAP [75]. However, a Dutch study showed that for patients with predicted SAP, probiotic prophylaxis with a combination of probiotic strains (Lactobacillus acidophilus, Lactobacillus casei, Lactobacillus salivarius, Lactococcus lactis, Bifidobacterium bifidum, and Bifidobacterium lactis) did not reduce the risk of infectious complications and was associated with an increased risk of mortality [76]. This study provided unexpected and exactly opposite results compared to previous RCTs. This unfavorable result might be related to a high prevalence of bowel ischemia in the treatment group. The authors provided a proposed mechanism that a high dose of bacteria combined with enteral nutrition increased oxygen demand and/or local mucosal effect. What is more, the higher AP severity, more types, higher dose and longer duration of probiotic organisms, and more aggressive hypercaloric enteral feeding compared with previous studies might also be influencing factors [77,78,79,80]. These conflicting results remind us that the optimized selection, dose, timing, delivery, and patient population of probiotics use are still pending further investigation. Subsequent trials demonstrated no increase in mortality or morbidity, with fewer infectious complications, multi-organ dysfunction, and decreased pro-inflammatory markers [81,82]. According to the pooled results of a systematic review including nine RCTs, pre/pro/synbiotics reduced the risk of organ failure and length of hospital stay in patients with SAP. Still, no difference was observed for SIRS, infected pancreatic necrosis, surgical intervention, septic morbidity, and mortality [83].
Prebiotic lactulose is a potent choice in treating AP patients suffering from gut failure. A recent prospective randomized trial compared the efficacy of lactulose and rhubarb in MSAP patients with intestinal dysfunction [84]. Lactulose had better performance in decreasing the serum levels of cytokines and gut permeability index, enriching the potential beneficial genus Bifidobacterium and inhibiting Escherichia-Shigella. Of note, the level of SCFAs remarkably increased after treatment, with a higher amount in the lactulose group than in the rhubarb group. In another study, Rohith et al. evaluated the efficacy of synbiotics (containing Streptococcus faecalis T-110, Clostridium butyricum TO-A, Bacillus mesentricus TO-A, and Lactobacillus sporogenes) in MSAP and SAP [85]. The results indicated that the value of synbiotics was limited, which only lowered bacteremia and length of hospitalization, but septic complications and mortality were not significantly different. Further studies must address some crucial questions, including the selection of potential beneficiary patient populations, the formulation of pre/pro/synbiotics, the optimal administration timing, and the treatment duration. Safety in particular requires attention when using live bacteria.
Table 2.
Use of probiotics, prebiotics, and synbiotics in AP.
| Studies | Subjects | Pre/Pro/Synbiotics | Main Effect of Treatment Group |
|---|---|---|---|
| Oláh 2002 [74] | 45 AP | Live L. plantarum 299, together with a substrate of oat fiber | Pancreatic sepsis ↓ Number of surgical interventions ↓ |
| Oláh 2007 [75] | 62 SAP | Four different lactobacilli preparations and prebiotics containing four bioactive fibers (inulin, beta-glucan, resistant starch, and pectin) | Incidence SIRS and MOF ↓ Rate of late (over 48 h) organ failure ↓ |
| Karakan 2007 [73] | 30 SAP | Standard enteral nutrition with soluble and insoluble fibers | Hospital stay ↓ APACHE II, CRP, and CT store normalization duration ↓ Overall complications ↓ |
| Besselink 2008 [76] | 298 predicted SAP | Lactobacillus acidophilus, Lactobacillus casei, Lactobacillus salivarius, Lactococcus lactis, Bifidobacterium bifidum, and Bifidobacterium lactis | Risk of mortality ↑ |
| Lata 2010 [86] | 22 AP | B. bifidum, B. infantis, L. acidophilus, L. casei, L. salivarius, L. lactis | Endotoxin levels ↓ |
| Sharma 2011 [82] | 50 AP | Lactobacillus acidophilus, Bifidobacterium longus, Bifidobacterium bifidum, and Bifidobacterium infantalis with fructo-oligosaccharide | CRP and immunoglobulins ↓ |
| Plaudis 2012 [87] | 90 SAP | Synbiotic 2000 Forte | Infection rate (pancreatic and peripancreatic necrosis) ↓ Rate of surgical interventions ↓ ICU and hospital stay ↓ Mortality rate ↓ |
| Cui 2013 [81] | 70 SAP | Bifidobacterium | Pro-inflammatory cytokines ↓ Earlier restoration of gastrointestinal function Complications ↓ Hospital day ↓ |
| Wang 2013 [88] | 183 SAP | Live Bacillus subtilis and Enterococcus faecium | Percentage of pancreatic sepsis and MODS ↓ Mortality rate ↓ Pro-inflammatory cytokines and APACHE II scores ↓ Plasma concentration of IL-10 ↑ |
| Zhu 2014 [89] | 39 SAP | C. Butyricum | Rate of intestinal ischemia and necrosis ↑ |
| Li 2014 [90] | 80 SAP | Bifidobacterium | Pro-inflammatory cytokines levels ↓ CRP and LDH levels ↓ Mortality and incidence of complications ↓ Duration of hospitalization ↓ |
| Wu 2017 [91] | 120 SAP | Live B. bifidus, B. acidophilus, E. faecalis, and B. cereus | Incidence of infection MODS ↓ Duration of abdomen pain and hospitalization ↓ |
| Fang 2018 [92] | 68 SAP | Live Bifidobacterium, Lactobacillus, and Enterococcus | Relieved clinical symptoms Hospitalization time ↓ Serum inflammatory cytokine levels ↓ |
| Wang 2023 [84] | 73 MSAP | Lactulose | Serum levels of cytokines ↓ Gut permeability index ↓ Bifidobacterium ↑ Level of SCFAs ↑ |
| Rohith 2023 [85] | 86 MSAP or SAP | Synbiotics containing Streptococcus faecalis T-110, Clostridium butyricum TO-A, Bacillus mesentricus TO-A, and Lactobacillus sporogenes | Total leucocyte and neutrophil counts ↓ Length of hospitalization ↓ |
AP, acute pancreatitis; MSAP, moderately severe acute pancreatitis; SAP, severe acute pancreatitis; SIRS, systemic inflammatory response syndrome; MOF, multi-organ failure; MODS, multiple organ dysfunction syndrome; APACHE II, Acute Physiology and Chronic Health Evaluation II; IL, interleukin; CRP, C-reactive protein; ICU, intensive care unit; CT, computed tomography; LDH, lactate dehydrogenase; SCFAs, short chain fatty acids. The arrows indicate the changes of main outcomes after the treatment of probiotics, prebiotics, or synbiotics.
4.3. Direct Supplementation of SCFAs
In 2019, the International Scientific Association for Probiotics and Prebiotics (ISAPP) proposed that a postbiotic is a “preparation of inanimate microorganisms and/or their components that confers a health benefit on the host”. Postbiotics are deliberately inactivated microbial cells with or without metabolites or cell components contributing to demonstrated health benefits [93]. SCFAs are one group of these beneficial metabolites. According to the mechanisms discussed above, SCFAs benefit AP on different levels, including regulating local and systematic inflammation, restoring intestinal barrier function, and reversing other organ dysfunctions. A research team from the University of Amsterdam used a mouse model of ANP fed with the Western diet, which contained 60% polyunsaturated fatty acids and no soluble fibers. The Western diet caused a bloom of Escherichia/Shigella and increased mortality and systemic infection in ANP mice. There was also a significant decrease in butyrate, amino acids, and carbohydrates. Collectively, these results confirmed that the Western diet is involved in AP pathogenesis. For therapeutic strategies, both oral and intraperitoneal butyrate reduced mortality and E. coli dissemination and reversed the microbiota alterations [30]. Although SCFAs have been subjected to clinical trials in humans with some encouraging results, including ulcerative colitis, radiation proctosigmoiditis, and visceral hypersensitivity, there have not been clinical trials about the administration of SCFAs in AP patients, and the current findings were all from animal models [94,95,96,97,98,99,100,101,102,103,104]. Direct SCFAs supplementation in enteral nutrition for AP treatment is essential for future clinical studies. It is expected to be safer than probiotics, which might cause bacteremia. However, SCFAs used as purified substances and not as a component of an inactivated microbial preparation would not be considered postbiotics.
4.4. Fecal Microbiota Transplantation
Fecal microbiota transplantation (FMT) is a direct approach to restoring the intestinal environment. It has been recommended to treat Clostridium difficile infection (CDI) [105]. The US Food and Drug Administration (FDA) issued a safety alert for using FMT after reports of serious adverse effects, including death due to infections with multidrug-resistant bacteria [106,107]. Yang et al. reported a case of MSAP complicated with severe CDI who suffered from diarrhea during his AP course. This 51-year-old man was treated by FMT as a first-line therapy. During the treatment, no adverse events were reported. Diarrhea resolved within five days after FMT. The patient remained asymptomatic, and the follow-up colonoscopy performed 40 days after discharge showed a complete recovery. However, the effect of FMT on AP was not evaluated and reported [108]. There are only some FMT-related studies conducted in AP mice. The bacteria translocation and mortality rate were significantly increased in pancreatitis mice that received FMT from healthy mice [30]. Another study reported that normobiotic FMT alleviated AP-induced gut microbiota dysbiosis and lessened the severity of AP, including mitochondrial dysfunction, oxidative damage, and inflammation. Gut microbiota-derived nicotinamide mononucleotide may play an essential role in this process [109]. According to these limited but controversial results from animal experiments, the effects and safety of FMT in AP treatment undoubtedly need further research.
5. Conclusions
Mucosal barrier protection is the common pathophysiological basis of almost all gastrointestinal diseases. Although the inflammation in AP starts in the pancreas, the gut plays an amplifier role in the disease course, leading to aggravated, even uncontrolled, inflammatory responses. Therefore, in treating AP, maintaining intact intestinal function is a significant part of controlling inflammation. SCFAs are a group of gut microbiota metabolites that could help rebuild the intestinal epithelial barrier and suppress inflammatory responses, thus maintaining a healthy intestinal environment. In addition to the intestine as the most important first step, SCFAs also reduce systematic inflammation and protect other organ functions, such as lung and kidney, which are frequently involved in AP. Therefore, supplementation of SCFAs directly or indirectly is a promising therapeutic approach, although existing research results are limited and controversial. More well designed clinical trials are needed for the comprehensive and individualized application of SCFAs, and safety is noteworthy, considering the complexity and aggressiveness of AP.
Author Contributions
Conceptualization, X.Y., J.L. and D.W.; writing—original draft preparation, X.Y. and J.L.; writing—review and editing, D.W.; project administration and funding acquisition, D.W. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the National Natural Science Foundation of China (grant number 32170788), the National High Level Hospital Clinical Research Funding (grant number 2022-PUMCH-B-023), the National Key Clinical Specialty Construction Project (grant number ZK108000), and the Beijing Natural Science Foundation (grant number 7232123).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Banks P.A., Freeman M.L. Practice guidelines in acute pancreatitis. Am. J. Gastroenterol. 2006;101:2379–2400. doi: 10.1111/j.1572-0241.2006.00856.x. [DOI] [PubMed] [Google Scholar]
- 2.Leaphart C.L., Tepas J.J., III The gut is a motor of organ system dysfunction. Surgery. 2007;141:563–569. doi: 10.1016/j.surg.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 3.Morrison D.J., Preston T. Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism. Gut Microbes. 2016;7:189–200. doi: 10.1080/19490976.2015.1134082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sakata T. Stimulatory effect of short-chain fatty acids on epithelial cell proliferation in the rat intestine: A possible explanation for trophic effects of fermentable fibre, gut microbes and luminal trophic factors. Br. J. Nutr. 1987;58:95–103. doi: 10.1079/BJN19870073. [DOI] [PubMed] [Google Scholar]
- 5.Pouteau E., Nguyen P., Ballèvre O., Krempf M. Production rates and metabolism of short-chain fatty acids in the colon and whole body using stable isotopes. Proc. Nutr. Soc. 2003;62:87–93. doi: 10.1079/PNS2003208. [DOI] [PubMed] [Google Scholar]
- 6.Reilly K.J., Rombeau J.L. Metabolism and potential clinical applications of short-chain fatty acids. Clin. Nutr. 1993;12:S97–S105. doi: 10.1016/S0261-5614(09)90016-4. [DOI] [Google Scholar]
- 7.Nøhr M.K., Egerod K.L., Christiansen S.H., Gille A., Offermanns S., Schwartz T.W., Møller M. Expression of the short chain fatty acid receptor GPR41/FFAR3 in autonomic and somatic sensory ganglia. Neuroscience. 2015;290:126–137. doi: 10.1016/j.neuroscience.2015.01.040. [DOI] [PubMed] [Google Scholar]
- 8.Wang H.B., Wang P.Y., Wang X., Wan Y.L., Liu Y.C. Butyrate enhances intestinal epithelial barrier function via up-regulation of tight junction protein Claudin-1 transcription. Dig. Dis. Sci. 2012;57:3126–3135. doi: 10.1007/s10620-012-2259-4. [DOI] [PubMed] [Google Scholar]
- 9.Willemsen L.E., Koetsier M.A., van Deventer S.J., van Tol E.A. Short chain fatty acids stimulate epithelial mucin 2 expression through differential effects on prostaglandin E(1) and E(2) production by intestinal myofibroblasts. Gut. 2003;52:1442–1447. doi: 10.1136/gut.52.10.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maslowski K.M., Vieira A.T., Ng A., Kranich J., Sierro F., Yu D., Schilter H.C., Rolph M.S., Mackay F., Artis D., et al. Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature. 2009;461:1282–1286. doi: 10.1038/nature08530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mowat A.M., Agace W.W. Regional specialization within the intestinal immune system. Nat. Rev. Immunol. 2014;14:667–685. doi: 10.1038/nri3738. [DOI] [PubMed] [Google Scholar]
- 12.He J., Zhang P., Shen L., Niu L., Tan Y., Chen L., Zhao Y., Bai L., Hao X., Li X., et al. Short-Chain Fatty Acids and Their Association with Signalling Pathways in Inflammation, Glucose and Lipid Metabolism. Int. J. Mol. Sci. 2020;21:6356. doi: 10.3390/ijms21176356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li X.Y., He C., Zhu Y., Lu N.H. Role of gut microbiota on intestinal barrier function in acute pancreatitis. World J. Gastroenterol. 2020;26:2187–2193. doi: 10.3748/wjg.v26.i18.2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas R.M., Jobin C. Microbiota in pancreatic health and disease: The next frontier in microbiome research. Nat. Rev. Gastroenterol. Hepatol. 2020;17:53–64. doi: 10.1038/s41575-019-0242-7. [DOI] [PubMed] [Google Scholar]
- 15.Al-Omran M., Albalawi Z.H., Tashkandi M.F., Al-Ansary L.A. Enteral versus parenteral nutrition for acute pancreatitis. Cochrane Database Syst. Rev. 2010;2010:Cd002837. doi: 10.1002/14651858.CD002837.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mederos M.A., Reber H.A., Girgis M.D. Acute Pancreatitis: A Review. JAMA. 2021;325:382–390. doi: 10.1001/jama.2020.20317. [DOI] [PubMed] [Google Scholar]
- 17.Zhang X.M., Zhang Z.Y., Zhang C.H., Wu J., Wang Y.X., Zhang G.X. Intestinal Microbial Community Differs between Acute Pancreatitis Patients and Healthy Volunteers. Biomed. Environ. Sci. 2018;31:81–86. doi: 10.3967/bes2018.010. [DOI] [PubMed] [Google Scholar]
- 18.Zhu Y., He C., Li X., Cai Y., Hu J., Liao Y., Zhao J., Xia L., He W., Liu L., et al. Gut microbiota dysbiosis worsens the severity of acute pancreatitis in patients and mice. J. Gastroenterol. 2019;54:347–358. doi: 10.1007/s00535-018-1529-0. [DOI] [PubMed] [Google Scholar]
- 19.Chen J., Kang B., Jiang Q., Han M., Zhao Y., Long L., Fu C., Yao K. Alpha-Ketoglutarate in Low-Protein Diets for Growing Pigs: Effects on Cecal Microbial Communities and Parameters of Microbial Metabolism. Front. Microbiol. 2018;9:1057. doi: 10.3389/fmicb.2018.01057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ma N., Wu Y., Xie F., Du K., Wang Y., Shi L., Ji L., Liu T., Ma X. Dimethyl fumarate reduces the risk of mycotoxins via improving intestinal barrier and microbiota. Oncotarget. 2017;8:44625–44638. doi: 10.18632/oncotarget.17886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu J., Yue S., Yang Z., Feng W., Meng X., Wang A., Peng C., Wang C., Yan D. Oral hydroxysafflor yellow A reduces obesity in mice by modulating the gut microbiota and serum metabolism. Pharmacol. Res. 2018;134:40–50. doi: 10.1016/j.phrs.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 22.Kellingray L., Gall G.L., Defernez M., Beales I.L.P., Franslem-Elumogo N., Narbad A. Microbial taxonomic and metabolic alterations during faecal microbiota transplantation to treat Clostridium difficile infection. J. Infect. 2018;77:107–118. doi: 10.1016/j.jinf.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 23.Yu S., Xiong Y., Xu J., Liang X., Fu Y., Liu D., Yu X., Wu D. Identification of Dysfunctional Gut Microbiota Through Rectal Swab in Patients with Different Severity of Acute Pancreatitis. Dig. Dis. Sci. 2020;65:3223–3237. doi: 10.1007/s10620-020-06061-4. [DOI] [PubMed] [Google Scholar]
- 24.Thomas R.M., Gharaibeh R.Z., Gauthier J., Beveridge M., Pope J.L., Guijarro M.V., Yu Q., He Z., Ohland C., Newsome R., et al. Intestinal microbiota enhances pancreatic carcinogenesis in preclinical models. Carcinogenesis. 2018;39:1068–1078. doi: 10.1093/carcin/bgy073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pushalkar S., Hundeyin M., Daley D., Zambirinis C.P., Kurz E., Mishra A., Mohan N., Aykut B., Usyk M., Torres L.E., et al. The Pancreatic Cancer Microbiome Promotes Oncogenesis by Induction of Innate and Adaptive Immune Suppression. Cancer Discov. 2018;8:403–416. doi: 10.1158/2159-8290.CD-17-1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beger H.G., Bittner R., Block S., Büchler M. Bacterial contamination of pancreatic necrosis. A prospective clinical study. Gastroenterology. 1986;91:433–438. doi: 10.1016/0016-5085(86)90579-2. [DOI] [PubMed] [Google Scholar]
- 27.Bradley E.L., III, Allen K. A prospective longitudinal study of observation versus surgical intervention in the management of necrotizing pancreatitis. Am. J. Surg. 1991;161:19–25. doi: 10.1016/0002-9610(91)90355-H. [DOI] [PubMed] [Google Scholar]
- 28.van den Berg F.F., Hugenholtz F., Boermeester M.A., Zaborina O., Alverdy J.C. Spatioregional assessment of the gut microbiota in experimental necrotizing pancreatitis. BJS Open. 2021;5:zrab061. doi: 10.1093/bjsopen/zrab061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tan C., Ling Z., Huang Y., Cao Y., Liu Q., Cai T., Yuan H., Liu C., Li Y., Xu K. Dysbiosis of Intestinal Microbiota Associated With Inflammation Involved in the Progression of Acute Pancreatitis. Pancreas. 2015;44:868–875. doi: 10.1097/MPA.0000000000000355. [DOI] [PubMed] [Google Scholar]
- 30.van den Berg F.F., van Dalen D., Hyoju S.K., van Santvoort H.C., Besselink M.G., Wiersinga W.J., Zaborina O., Boermeester M.A., Alverdy J. Western-type diet influences mortality from necrotising pancreatitis and demonstrates a central role for butyrate. Gut. 2021;70:915–927. doi: 10.1136/gutjnl-2019-320430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu L.M., Sankaran S.J., Plank L.D., Windsor J.A., Petrov M.S. Meta-analysis of gut barrier dysfunction in patients with acute pancreatitis. Br. J. Surg. 2014;101:1644–1656. doi: 10.1002/bjs.9665. [DOI] [PubMed] [Google Scholar]
- 32.Ding L., Chen H.Y., Wang J.Y., Xiong H.F., He W.H., Xia L., Lu N.H., Zhu Y. Severity of acute gastrointestinal injury grade is a good predictor of mortality in critically ill patients with acute pancreatitis. World J. Gastroenterol. 2020;26:514–523. doi: 10.3748/wjg.v26.i5.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gao Y., Davis B., Zhu W., Zheng N., Meng D., Walker W.A. Short-chain fatty acid butyrate, a breast milk metabolite, enhances immature intestinal barrier function genes in response to inflammation in vitro and in vivo. Am. J. Physiol. Gastrointest. Liver Physiol. 2021;320:G521–G530. doi: 10.1152/ajpgi.00279.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xiong Y., Ji L., Zhao Y., Liu A., Wu D., Qian J. Sodium Butyrate Attenuates Taurocholate-Induced Acute Pancreatitis by Maintaining Colonic Barrier and Regulating Gut Microorganisms in Mice. Front. Physiol. 2022;13:813735. doi: 10.3389/fphys.2022.813735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wong J.M., de Souza R., Kendall C.W., Emam A., Jenkins D.J. Colonic health: Fermentation and short chain fatty acids. J. Clin. Gastroenterol. 2006;40:235–243. doi: 10.1097/00004836-200603000-00015. [DOI] [PubMed] [Google Scholar]
- 36.Xiao S., Jing S., Jiakui S., Lei Z., Ying L., Han L., Xinwei M., Weiqin L. Butyrate Ameliorates Intestinal Epithelial Barrier Injury Via Enhancing Foxp3+ Regulatory T-Cell Function in Severe Acute Pancreatitis Model. Turk. J. Gastroenterol. 2022;33:710–719. doi: 10.5152/tjg.2022.21307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harrison O.J., Powrie F.M. Regulatory T cells and immune tolerance in the intestine. Cold Spring Harb. Perspect. Biol. 2013;5 doi: 10.1101/cshperspect.a018341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barnes M.J., Powrie F. Regulatory T cells reinforce intestinal homeostasis. Immunity. 2009;31:401–411. doi: 10.1016/j.immuni.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 39.Ke L., Ni H.B., Sun J.K., Tong Z.H., Li W.Q., Li N., Li J.S. Risk factors and outcome of intra-abdominal hypertension in patients with severe acute pancreatitis. World J. Surg. 2012;36:171–178. doi: 10.1007/s00268-011-1295-0. [DOI] [PubMed] [Google Scholar]
- 40.Ke L., Tong Z.H., Ni H.B., Ding W.W., Sun J.K., Li W.Q., Li N., Li J.S. The effect of intra-abdominal hypertension incorporating severe acute pancreatitis in a porcine model. PLoS ONE. 2012;7:e33125. doi: 10.1371/journal.pone.0033125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gong G., Wang P., Ding W., Zhao Y., Li J. The role of oxygen-free radical in the apoptosis of enterocytes and bacterial translocation in abdominal compartment syndrome. Free Radic. Res. 2009;43:470–477. doi: 10.1080/10715760902846157. [DOI] [PubMed] [Google Scholar]
- 42.Zhao H.B., Jia L., Yan Q.Q., Deng Q., Wei B. Effect of Clostridium butyricum and Butyrate on Intestinal Barrier Functions: Study of a Rat Model of Severe Acute Pancreatitis With Intra-Abdominal Hypertension. Front. Physiol. 2020;11:561061. doi: 10.3389/fphys.2020.561061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yan Q., Jia L., Wen B., Wu Y., Zeng Y., Wang Q. Clostridium butyricum Protects Against Pancreatic and Intestinal Injury After Severe Acute Pancreatitis via Downregulation of MMP9. Front. Pharmacol. 2022;13:919010. doi: 10.3389/fphar.2022.919010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kocael A., Inal B.B., Guntas G., Kelten C., Inal H., Topac H.I., Kocael P., Simsek O., Karaca G., Salihoglu Z., et al. Evaluation of matrix metalloproteinase, myeloperoxidase, and oxidative damage in mesenteric ischemia-reperfusion injury. Hum. Exp. Toxicol. 2016;35:851–860. doi: 10.1177/0960327115607946. [DOI] [PubMed] [Google Scholar]
- 45.Zhang H., Liu L., Jiang C., Pan K., Deng J., Wan C. MMP9 protects against LPS-induced inflammation in osteoblasts. Innate Immun. 2020;26:259–269. doi: 10.1177/1753425919887236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Apostolidou E., Paraskeva E., Gourgoulianis K., Molyvdas P.A., Hatzoglou C. Matrix metalloproteinases 2 and 9 increase permeability of sheep pleura in vitro. BMC Physiol. 2012;12:2. doi: 10.1186/1472-6793-12-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sun J., Furio L., Mecheri R., van der Does A.M., Lundeberg E., Saveanu L., Chen Y., van Endert P., Agerberth B., Diana J. Pancreatic β-Cells Limit Autoimmune Diabetes via an Immunoregulatory Antimicrobial Peptide Expressed under the Influence of the Gut Microbiota. Immunity. 2015;43:304–317. doi: 10.1016/j.immuni.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 48.Pan X., Fang X., Wang F., Li H., Niu W., Liang W., Wu C., Li J., Tu X., Pan L.L., et al. Butyrate ameliorates caerulein-induced acute pancreatitis and associated intestinal injury by tissue-specific mechanisms. Br. J. Pharmacol. 2019;176:4446–4461. doi: 10.1111/bph.14806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lei Y., Tang L., Liu S., Hu S., Wu L., Liu Y., Yang M., Huang S., Tang X., Tang T., et al. Parabacteroides produces acetate to alleviate heparanase-exacerbated acute pancreatitis through reducing neutrophil infiltration. Microbiome. 2021;9:115. doi: 10.1186/s40168-021-01065-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Banks P.A., Bollen T.L., Dervenis C., Gooszen H.G., Johnson C.D., Sarr M.G., Tsiotos G.G., Vege S.S. Classification of acute pancreatitis—2012: Revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111. doi: 10.1136/gutjnl-2012-302779. [DOI] [PubMed] [Google Scholar]
- 51.Yamada T., Shimizu K., Ogura H., Asahara T., Nomoto K., Yamakawa K., Hamasaki T., Nakahori Y., Ohnishi M., Kuwagata Y., et al. Rapid and Sustained Long-Term Decrease of Fecal Short-Chain Fatty Acids in Critically Ill Patients With Systemic Inflammatory Response Syndrome. JPEN J. Parenter. Enteral Nutr. 2015;39:569–577. doi: 10.1177/0148607114529596. [DOI] [PubMed] [Google Scholar]
- 52.Zhang T., Xia M., Zhan Q., Zhou Q., Lu G., An F. Sodium Butyrate Reduces Organ Injuries in Mice with Severe Acute Pancreatitis Through Inhibiting HMGB1 Expression. Dig. Dis. Sci. 2015;60:1991–1999. doi: 10.1007/s10620-015-3586-z. [DOI] [PubMed] [Google Scholar]
- 53.Wang F., Liu J., Weng T., Shen K., Chen Z., Yu Y., Huang Q., Wang G., Liu Z., Jin S. The Inflammation Induced by Lipopolysaccharide can be Mitigated by Short-chain Fatty Acid, Butyrate, through Upregulation of IL-10 in Septic Shock. Scand. J. Immunol. 2017;85:258–263. doi: 10.1111/sji.12515. [DOI] [PubMed] [Google Scholar]
- 54.Jacobs M.L., Daggett W.M., Civette J.M., Vasu M.A., Lawson D.W., Warshaw A.L., Nardi G.L., Bartlett M.K. Acute pancreatitis: Analysis of factors influencing survival. Ann. Surg. 1977;185:43–51. doi: 10.1097/00000658-197701000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shields C.J., Winter D.C., Redmond H.P. Lung injury in acute pancreatitis: Mechanisms, prevention, and therapy. Curr. Opin. Crit. Care. 2002;8:158–163. doi: 10.1097/00075198-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 56.Wang Z., Liu J., Li F., Luo Y., Ge P., Zhang Y., Wen H., Yang Q., Ma S., Chen H. The gut-lung axis in severe acute Pancreatitis-associated lung injury: The protection by the gut microbiota through short-chain fatty acids. Pharmacol. Res. 2022;182:106321. doi: 10.1016/j.phrs.2022.106321. [DOI] [PubMed] [Google Scholar]
- 57.Liu Q., Tian X., Maruyama D., Arjomandi M., Prakash A. Lung immune tone via gut-lung axis: Gut-derived LPS and short-chain fatty acids’ immunometabolic regulation of lung IL-1β, FFAR2, and FFAR3 expression. Am. J. Physiol. Lung Cell. Mol. Physiol. 2021;321:L65–L78. doi: 10.1152/ajplung.00421.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tian X., Hellman J., Horswill A.R., Crosby H.A., Francis K.P., Prakash A. Elevated Gut Microbiome-Derived Propionate Levels Are Associated With Reduced Sterile Lung Inflammation and Bacterial Immunity in Mice. Front. Microbiol. 2019;10:159. doi: 10.3389/fmicb.2019.00159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Prakash A., Sundar S.V., Zhu Y.G., Tran A., Lee J.W., Lowell C., Hellman J. Lung Ischemia-Reperfusion is a Sterile Inflammatory Process Influenced by Commensal Microbiota in Mice. Shock. 2015;44:272–279. doi: 10.1097/SHK.0000000000000415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li N., Liu X.X., Hong M., Huang X.Z., Chen H., Xu J.H., Wang C., Zhang Y.X., Zhong J.X., Nie H., et al. Sodium butyrate alleviates LPS-induced acute lung injury in mice via inhibiting HMGB1 release. Int. Immunopharmacol. 2018;56:242–248. doi: 10.1016/j.intimp.2018.01.017. [DOI] [PubMed] [Google Scholar]
- 61.Liu J., Chang G., Huang J., Wang Y., Ma N., Roy A.C., Shen X. Sodium Butyrate Inhibits the Inflammation of Lipopolysaccharide-Induced Acute Lung Injury in Mice by Regulating the Toll-Like Receptor 4/Nuclear Factor κB Signaling Pathway. J. Agric. Food Chem. 2019;67:1674–1682. doi: 10.1021/acs.jafc.8b06359. [DOI] [PubMed] [Google Scholar]
- 62.Xu M., Wang C., Li N., Wang J., Zhang Y., Deng X. Intraperitoneal Injection of Acetate Protects Mice Against Lipopolysaccharide (LPS)-Induced Acute Lung Injury Through Its Anti-Inflammatory and Anti-Oxidative Ability. Med. Sci. Monit. 2019;25:2278–2288. doi: 10.12659/MSM.911444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Karoor V., Strassheim D., Sullivan T., Verin A., Umapathy N.S., Dempsey E.C., Frank D.N., Stenmark K.R., Gerasimovskaya E. The Short-Chain Fatty Acid Butyrate Attenuates Pulmonary Vascular Remodeling and Inflammation in Hypoxia-Induced Pulmonary Hypertension. Int. J. Mol. Sci. 2021;22:9916. doi: 10.3390/ijms22189916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hu X., Han Z., Zhou R., Su W., Gong L., Yang Z., Song X., Zhang S., Shu H., Wu D. Altered gut microbiota in the early stage of acute pancreatitis were related to the occurrence of acute respiratory distress syndrome. Front. Cell. Infect. Microbiol. 2023;13:1127369. doi: 10.3389/fcimb.2023.1127369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Devani K., Charilaou P., Radadiya D., Brahmbhatt B., Young M., Reddy C. Acute pancreatitis: Trends in outcomes and the role of acute kidney injury in mortality- A propensity-matched analysis. Pancreatology. 2018;18:870–877. doi: 10.1016/j.pan.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 66.Nassar T.I., Qunibi W.Y. AKI Associated with Acute Pancreatitis. Clin. J. Am. Soc. Nephrol. 2019;14:1106–1115. doi: 10.2215/CJN.13191118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Andrade-Oliveira V., Amano M.T., Correa-Costa M., Castoldi A., Felizardo R.J., de Almeida D.C., Bassi E.J., Moraes-Vieira P.M., Hiyane M.I., Rodas A.C., et al. Gut Bacteria Products Prevent AKI Induced by Ischemia-Reperfusion. J. Am. Soc. Nephrol. 2015;26:1877–1888. doi: 10.1681/ASN.2014030288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu Y., Li Y.J., Loh Y.W., Singer J., Zhu W., Macia L., Mackay C.R., Wang W., Chadban S.J., Wu H. Fiber Derived Microbial Metabolites Prevent Acute Kidney Injury Through G-Protein Coupled Receptors and HDAC Inhibition. Front. Cell Dev. Biol. 2021;9:648639. doi: 10.3389/fcell.2021.648639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Besselink M.G., van Santvoort H.C., Boermeester M.A., Nieuwenhuijs V.B., van Goor H., Dejong C.H., Schaapherder A.F., Gooszen H.G. Timing and impact of infections in acute pancreatitis. Br. J. Surg. 2009;96:267–273. doi: 10.1002/bjs.6447. [DOI] [PubMed] [Google Scholar]
- 70.Marik P.E., Zaloga G.P. Early enteral nutrition in acutely ill patients: A systematic review. Crit. Care Med. 2001;29:2264–2270. doi: 10.1097/00003246-200112000-00005. [DOI] [PubMed] [Google Scholar]
- 71.O’Keefe S.J., Ou J., Delany J.P., Curry S., Zoetendal E., Gaskins H.R., Gunn S. Effect of fiber supplementation on the microbiota in critically ill patients. World J. Gastrointest. Pathophysiol. 2011;2:138–145. doi: 10.4291/wjgp.v2.i6.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Petrov M.S., Whelan K. Comparison of complications attributable to enteral and parenteral nutrition in predicted severe acute pancreatitis: A systematic review and meta-analysis. Br. J. Nutr. 2010;103:1287–1295. doi: 10.1017/S0007114510000887. [DOI] [PubMed] [Google Scholar]
- 73.Karakan T., Ergun M., Dogan I., Cindoruk M., Unal S. Comparison of early enteral nutrition in severe acute pancreatitis with prebiotic fiber supplementation versus standard enteral solution: A prospective randomized double-blind study. World J. Gastroenterol. 2007;13:2733–2737. doi: 10.3748/wjg.v13.i19.2733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Oláh A., Belágyi T., Issekutz A., Gamal M.E., Bengmark S. Randomized clinical trial of specific lactobacillus and fibre supplement to early enteral nutrition in patients with acute pancreatitis. Br. J. Surg. 2002;89:1103–1107. doi: 10.1046/j.1365-2168.2002.02189.x. [DOI] [PubMed] [Google Scholar]
- 75.Oláh A., Belágyi T., Pótó L., Romics L., Jr., Bengmark S. Synbiotic control of inflammation and infection in severe acute pancreatitis: A prospective, randomized, double blind study. Hepatogastroenterology. 2007;54:590–594. [PubMed] [Google Scholar]
- 76.Besselink M.G., van Santvoort H.C., Buskens E., Boermeester M.A., van Goor H., Timmerman H.M., Nieuwenhuijs V.B., Bollen T.L., van Ramshorst B., Witteman B.J., et al. Probiotic prophylaxis in predicted severe acute pancreatitis: A randomised, double-blind, placebo-controlled trial. Lancet. 2008;371:651–659. doi: 10.1016/S0140-6736(08)60207-X. [DOI] [PubMed] [Google Scholar]
- 77.McClave S.A., Heyland D.K., Wischmeyer P.E. Comment on: Probiotic prophylaxis in predicted severe acute pancreatitis: A randomized, double-blind, placebo-controlled trial. JPEN J. Parenter. Enteral Nutr. 2009;33:444–446. doi: 10.1177/0148607108331176. [DOI] [PubMed] [Google Scholar]
- 78.Stapleton J.R., McClave S.A. Controversial results with use of probiotics in critical illness: Contradictory findings from large multicenter trial. Curr. Gastroenterol. Rep. 2009;11:259–262. doi: 10.1007/s11894-009-0052-0. [DOI] [PubMed] [Google Scholar]
- 79.Expression of concern—Probiotic prophylaxis in predicted severe acute pancreatitis: A randomised, double-blind, placebo-controlled trial. Lancet. 2010;375:875–876. doi: 10.1016/S0140-6736(10)60360-1. [DOI] [PubMed] [Google Scholar]
- 80.Reddy B.S., MacFie J. Probiotic prophylaxis in predicted severe acute pancreatitis. Lancet. 2008;372:113. doi: 10.1016/S0140-6736(08)61025-9. [DOI] [PubMed] [Google Scholar]
- 81.Cui L.H., Wang X.H., Peng L.H., Yu L., Yang Y.S. [The effects of early enteral nutrition with addition of probiotics on the prognosis of patients suffering from severe acute pancreatitis] Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2013;25:224–228. doi: 10.3760/cma.j.issn.2095-4352.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 82.Sharma B., Srivastava S., Singh N., Sachdev V., Kapur S., Saraya A. Role of probiotics on gut permeability and endotoxemia in patients with acute pancreatitis: A double-blind randomized controlled trial. J. Clin. Gastroenterol. 2011;45:442–448. doi: 10.1097/MCG.0b013e318201f9e2. [DOI] [PubMed] [Google Scholar]
- 83.Yu C., Zhang Y., Yang Q., Lee P., Windsor J.A., Wu D. An Updated Systematic Review With Meta-analysis: Efficacy of Prebiotic, Probiotic, and Synbiotic Treatment of Patients With Severe Acute Pancreatitis. Pancreas. 2021;50:160–166. doi: 10.1097/MPA.0000000000001734. [DOI] [PubMed] [Google Scholar]
- 84.Wang J., Jiang M., Hu Y., Lei Y., Zhu Y., Xiong H., He C. Lactulose regulates gut microbiota dysbiosis and promotes short-chain fatty acids production in acute pancreatitis patients with intestinal dysfunction. Biomed. Pharmacother. 2023;163:114769. doi: 10.1016/j.biopha.2023.114769. [DOI] [PubMed] [Google Scholar]
- 85.Rohith G., Sureshkumar S., Anandhi A., Kate V., Rajesh B.S., Abdulbasith K.M., Nanda N., Palanivel C., Vijayakumar C. Effect of Synbiotics in Reducing the Systemic Inflammatory Response and Septic Complications in Moderately Severe and Severe Acute Pancreatitis: A Prospective Parallel-Arm Double-Blind Randomized Trial. Dig. Dis. Sci. 2023;68:969–977. doi: 10.1007/s10620-022-07618-1. [DOI] [PubMed] [Google Scholar]
- 86.Lata J., Juránková J., Stibůrek O., Príbramská V., Senkyrík M., Vanásek T. [Probiotics in acute pancreatitis—A randomised, placebo-controlled, double-blind study] Vnitr. Lek. 2010;56:111–114. [PubMed] [Google Scholar]
- 87.Plaudis H., Pupelis G., Zeiza K., Boka V. Early low volume oral synbiotic/prebiotic supplemented enteral stimulation of the gut in patients with severe acute pancreatitis: A prospective feasibility study. Acta Chir. Belg. 2012;112:131–138. doi: 10.1080/00015458.2012.11680811. [DOI] [PubMed] [Google Scholar]
- 88.Wang G., Wen J., Xu L., Zhou S., Gong M., Wen P., Xiao X. Effect of enteral nutrition and ecoimmunonutrition on bacterial translocation and cytokine production in patients with severe acute pancreatitis. J. Surg. Res. 2013;183:592–597. doi: 10.1016/j.jss.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 89.Zhu Y.M. Effects of probiotics in treatment of severe acute pancreatitis. World Chin. J. Dig. 2014;22:5013. doi: 10.11569/wcjd.v22.i32.5013. [DOI] [Google Scholar]
- 90.Jin L. Effect of early enteral nutrition with Bifico on levels of inflammatory mediators in plasma of patients with severe acute pancreatitis. World Chin. J. Dig. 2014;22:5609. [Google Scholar]
- 91.Wu P., Yu Y., Li L., Sun W. Effect and safety of probiotics combined early enteral nutrition on severe acute pancreatitis patients. Biomed. Res. 2017;28:1403–1407. [Google Scholar]
- 92.Fang J.J., Qin H., Shi C.L., Jing T., Yan B.Q., Gai L., Li X.G., Unit I.C. Effect of probiotics plus antibiotics on inflammatory cytokines and quality of life in patients with non-biliary severe acute pancreatitis. World Chin. J. Dig. 2018;26:270–275. doi: 10.11569/wcjd.v26.i4.270. [DOI] [Google Scholar]
- 93.Salminen S., Collado M.C., Endo A., Hill C., Lebeer S., Quigley E.M.M., Sanders M.E., Shamir R., Swann J.R., Szajewska H., et al. The International Scientific Association of Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics. Nat. Rev. Gastroenterol. Hepatol. 2021;18:649–667. doi: 10.1038/s41575-021-00440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Scheppach W., Sommer H., Kirchner T., Paganelli G.M., Bartram P., Christl S., Richter F., Dusel G., Kasper H. Effect of butyrate enemas on the colonic mucosa in distal ulcerative colitis. Gastroenterology. 1992;103:51–56. doi: 10.1016/0016-5085(92)91094-K. [DOI] [PubMed] [Google Scholar]
- 95.Steinhart A.H., Brzezinski A., Baker J.P. Treatment of refractory ulcerative proctosigmoiditis with butyrate enemas. Am. J. Gastroenterol. 1994;89:179–183. [PubMed] [Google Scholar]
- 96.Scheppach W. Treatment of distal ulcerative colitis with short-chain fatty acid enemas. A placebo-controlled trial. German-Austrian SCFA Study Group. Dig. Dis. Sci. 1996;41:2254–2259. doi: 10.1007/BF02071409. [DOI] [PubMed] [Google Scholar]
- 97.Vernia P., Marcheggiano A., Caprilli R., Frieri G., Corrao G., Valpiani D., Di Paolo M.C., Paoluzi P., Torsoli A. Short-chain fatty acid topical treatment in distal ulcerative colitis. Aliment. Pharmacol. Ther. 1995;9:309–313. doi: 10.1111/j.1365-2036.1995.tb00386.x. [DOI] [PubMed] [Google Scholar]
- 98.Steinhart A.H., Hiruki T., Brzezinski A., Baker J.P. Treatment of left-sided ulcerative colitis with butyrate enemas: A controlled trial. Aliment. Pharmacol. Ther. 1996;10:729–736. doi: 10.1046/j.1365-2036.1996.d01-509.x. [DOI] [PubMed] [Google Scholar]
- 99.Patz J., Jacobsohn W.Z., Gottschalk-Sabag S., Zeides S., Braverman D.Z. Treatment of refractory distal ulcerative colitis with short chain fatty acid enemas. Am. J. Gastroenterol. 1996;91:731–734. [PubMed] [Google Scholar]
- 100.Talley N.A., Chen F., King D., Jones M., Talley N.J. Short-chain fatty acids in the treatment of radiation proctitis: A randomized, double-blind, placebo-controlled, cross-over pilot trial. Dis. Colon Rectum. 1997;40:1046–1050. doi: 10.1007/BF02050927. [DOI] [PubMed] [Google Scholar]
- 101.Pinto A., Fidalgo P., Cravo M., Midões J., Chaves P., Rosa J., dos Anjos Brito M., Leitão C.N. Short chain fatty acids are effective in short-term treatment of chronic radiation proctitis: Randomized, double-blind, controlled trial. Dis. Colon Rectum. 1999;42:788–795. doi: 10.1007/BF02236937. [DOI] [PubMed] [Google Scholar]
- 102.Vernia P., Fracasso P.L., Casale V., Villotti G., Marcheggiano A., Stigliano V., Pinnaro P., Bagnardi V., Caprilli R. Topical butyrate for acute radiation proctitis: Randomised, crossover trial. Lancet. 2000;356:1232–1235. doi: 10.1016/S0140-6736(00)02787-2. [DOI] [PubMed] [Google Scholar]
- 103.Maggio A., Magli A., Rancati T., Fiorino C., Valvo F., Fellin G., Ricardi U., Munoz F., Cosentino D., Cazzaniga L.F., et al. Daily sodium butyrate enema for the prevention of radiation proctitis in prostate cancer patients undergoing radical radiation therapy: Results of a multicenter randomized placebo-controlled dose-finding phase 2 study. Int. J. Radiat. Oncol. Biol. Phys. 2014;89:518–524. doi: 10.1016/j.ijrobp.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 104.Vanhoutvin S.A., Troost F.J., Kilkens T.O., Lindsey P.J., Hamer H.M., Jonkers D.M., Venema K., Brummer R.J. The effects of butyrate enemas on visceral perception in healthy volunteers. Neurogastroenterol. Motil. 2009;21:952-e76. doi: 10.1111/j.1365-2982.2009.01324.x. [DOI] [PubMed] [Google Scholar]
- 105.Cammarota G., Ianiro G., Tilg H., Rajilić-Stojanović M., Kump P., Satokari R., Sokol H., Arkkila P., Pintus C., Hart A., et al. European consensus conference on faecal microbiota transplantation in clinical practice. Gut. 2017;66:569–580. doi: 10.1136/gutjnl-2016-313017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.DeFilipp Z., Bloom P.P., Torres Soto M., Mansour M.K., Sater M.R.A., Huntley M.H., Turbett S., Chung R.T., Chen Y.B., Hohmann E.L. Drug-Resistant E. coli Bacteremia Transmitted by Fecal Microbiota Transplant. N. Engl. J. Med. 2019;381:2043–2050. doi: 10.1056/NEJMoa1910437. [DOI] [PubMed] [Google Scholar]
- 107.Nicholson M.R., Hourigan S.K., Conrad M., Goyal A., Jensen K., Kelsen J., Kennedy M., Weatherly M., Kahn S.A. Current Challenges in Fecal Microbiota Transplantation for Clostridioides difficile Infection in Children. Am. J. Gastroenterol. 2021;116:1954–1956. doi: 10.14309/ajg.0000000000001350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hu Y., Xiao H.Y., He C., Lv N.H., Zhu L. Fecal microbiota transplantation as an effective initial therapy for pancreatitis complicated with severe Clostridium difficile infection: A case report. World J. Clin. Cases. 2019;7:2597–2604. doi: 10.12998/wjcc.v7.i17.2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Liu L.W., Xie Y., Li G.Q., Zhang T., Sui Y.H., Zhao Z.J., Zhang Y.Y., Yang W.B., Geng X.L., Xue D.B., et al. Gut microbiota-derived nicotinamide mononucleotide alleviates acute pancreatitis by activating pancreatic SIRT3 signalling. Br. J. Pharmacol. 2023;180:647–666. doi: 10.1111/bph.15980. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.