Abstract
Mitochondrial dysfunction is linked to age-associated inflammation or inflammaging, but underlying mechanisms are not understood. Analyses of 700 human blood transcriptomes revealed clear signs of age-associated low-grade inflammation. Among changes in mitochondrial components, we found that the expression of mitochondrial calcium uniporter (MCU) and its regulatory subunit MICU1, genes central to mitochondrial Ca2+ (mCa2+) signaling, correlated inversely with age. Indeed, mCa2+ uptake capacity of mouse macrophages decreased significantly with age. We show that in both human and mouse macrophages, reduced mCa2+ uptake amplifies cytosolic Ca2+ oscillations and potentiates downstream nuclear factor kappa B activation, which is central to inflammation. Our findings pinpoint the mitochondrial calcium uniporter complex as a keystone molecular apparatus that links age-related changes in mitochondrial physiology to systemic macrophage-mediated age-associated inflammation. The findings raise the exciting possibility that restoring mCa2+ uptake capacity in tissue-resident macrophages may decrease inflammaging of specific organs and alleviate age-associated conditions such as neurodegenerative and cardiometabolic diseases.
Subject terms: Inflammation, Mitochondria, Ageing, Ion channel signalling
Seegren et al. demonstrate that the mitochondrial calcium uptake complex is a key molecular apparatus that links age-related changes in mitochondrial physiology to systemic macrophage-mediated age-associated inflammation.
Main
Inflammation is widely recognized as a key driver of aging1,2. An age-associated low-grade, chronic inflammatory state promotes tissue damage and hence this process is referred to as inflammaging. The etiology of inflammaging is not understood but it is thought to involve an increase in the baseline inflammatory output by immune cells, as evident from higher cytokine levels and other inflammatory markers in the blood of aged humans3–6. Inflammatory stimuli can originate from multiple sources: pathogens, resident microbiomes, tissue damage-associated inflammatory signals, and even spontaneous production of inflammatory molecules by senescent cells7–9. Myeloid cells of the immune system, such as macrophages and neutrophils, are central players in inflammation and may contribute to inflammaging.
Macrophages reside in every organ system and act as sentinel cells monitoring their environment for infection or injury10–12. The inflammatory gene expression in macrophages is a highly regulated process with multiple checkpoints. The nuclear factor kappa B (NF-κB) family of dimeric transcription factors have an evolutionarily conserved and central role in inflammatory gene expression13,14. Many studies have pointed to the salience of NF-κB to inflammaging15–18. Analysis of age-related changes in gene expression in human and mouse tissues identified the NF-κB pathway as the most strongly associated transcriptional pathway to aging15. The secretion of high levels of pro-inflammatory cytokines in two different mouse models of accelerated aging was also found to be dependent on abnormal NF-κB activaton17. These studies suggest that a lowered threshold of NF-κB activation underlies inflammaging, but how this transpires is not understood. Many positive and negative signaling elements control the activation of NF-κB13. Among these regulatory checkpoints, the nuclear translocation and transcriptional activity of NF-κB is also controlled by cytosolic Ca2+ (cCa2+) signaling19–22.
Ca2+ is a ubiquitous and essential second messenger in cell biology23. Elevations in cCa2+ trigger an influx of Ca2+ into the mitochondrial matrix through the mitochondrial calcium uniporter (MCU), a Ca2+-selective ion channel that resides in the mitochondrial inner membrane24–30. The mitochondrial outer membrane is porous to ions, but the inner membrane has a resting membrane potential between −160 mV and −200 mV, relative to the cytosol24,31. MICU1 (refs. 32,33) and MICU2 (refs. 34), the EF-hand containing Ca2+-sensitive regulatory subunits of MCU interact directly with MCU in the intermembrane space. Structural studies support the view that MCU–MICU1–MICU2 interactions are configured to have a switch-like sensitivity to [Ca2+], enabling rapid mCa2+ uptake when cytosolic [Ca2+] increases beyond the resting range of ~10–100 nM35–38. Because the mitochondrial matrix contains many metabolic enzymes that are regulated by Ca2+, the mCa2+ signaling within the matrix has a profound effect on mitochondrial physiology and metabolism29,39,40. The cells of the vertebrate immune system use Ca2+ signaling for an immediate-early response to antigenic and inflammatory stimuli—cCa2+ elevations regulate the activation of both the innate and adaptive immune cells41. Recently, we revealed that mCa2+ signaling functions as an electrometabolic switch to fuel macrophage-mediated phagosomal killing42. The process involves a fast two-step Ca2+ relay to meet the bioenergetic demands of phagosomal killing. Additionally, recent reports have supported a role for the MCU and mCa2+ in macrophage polarization43,44, host defense42,45 and tissue homeostasis46–48. mCa2+ is thus emerging as a central node for innate immunity and inflammatory responses. Here we report a surprising discovery that mCa2+ uptake capacity of macrophages decreases progressively with age, and this is a major driver of inflammaging.
Results
Human blood transcriptomes reveal signs of age-associated low-grade inflammation
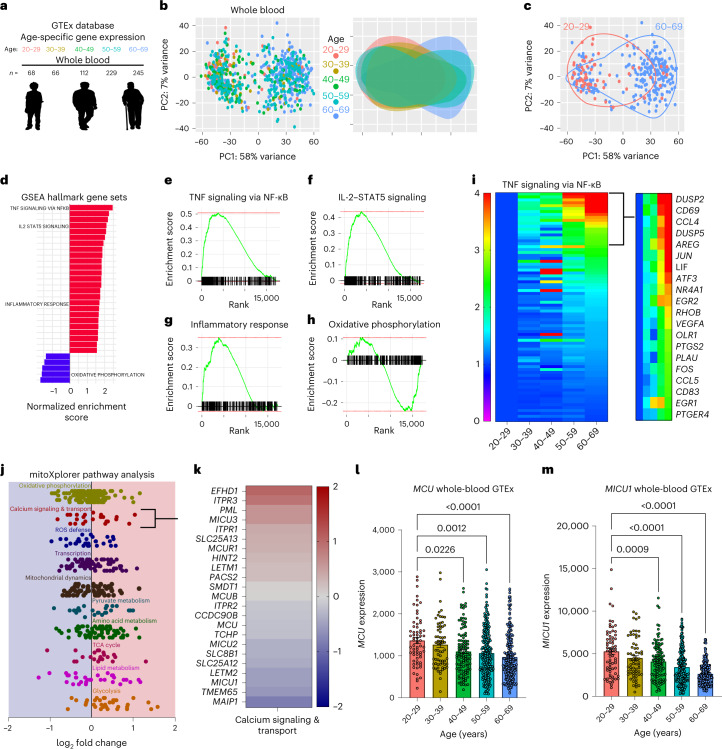
To gain insights into inflammaging, we mined the publicly available Genotype-Tissue Expression (GTEx) database (https://gtexportal.org/)49 for tissue-specific gene expression across five different human age groups (Fig. 1a). Because mature red blood cells are anucleated and do not contain any appreciable amounts of mRNA, RNA sequencing (RNA-seq) of whole blood is a reasonable surrogate of combined gene expression in the white blood cells and platelets. Expression profile data were obtained for different tissues, binned into age groups, and then subjected to differential gene expression analysis using DESeq2 R package. Principle-component analysis (PCA) plots, from the five different age groups, revealed clear age-associated clustering (Fig. 1b). The variance in overall gene expression was greatest when we compared the youngest population (age 20–29 years) with the oldest population (age 60–69 years; Fig. 1c), but the variance in overall gene expression was the least when we compared the second-oldest population (age 50–59 years) to the oldest population (age 60–69 years; Extended Data Fig. 1a). These data substantiate the view that gene expression in the blood changes significantly with age. To derive further insights and to distill testable hypotheses for the etiology of inflammaging, we focused our analysis on differences between the youngest (age 20–29 years) and oldest (age 60–69 years) samples. Gene-set enrichment analysis (GSEA) hallmark and GO pathway analyses of differentially expressed genes showed that the genes associated with inflammatory responses were upregulated in the older population (Fig. 1d and Extended Data Fig. 1b). Additionally, we observed a significant decrease in the gene expression related to oxidative phosphorylation, a mitochondrial process, in the older populations. Enrichment scores and gene ranks of inflammatory genes (Fig. 1e–g) and oxidative phosphorylation-associated genes (Fig. 1h) suggest a significant dysregulation in these pathways in the aged population. As shown in the heat map (Fig. 1i), genes associated with the NF-κB pathway were upregulated in the blood cells of older humans. Overall, these gene expression analyses show clear signs of age-associated chronic low-grade inflammation in the whole blood of human samples.
Fig. 1. Age-related changes in whole-blood gene expression are associated with increased inflammatory gene transcription and decreased expression of genes encoding mitochondrial Ca2+ transport.
a, GTEx database mined for tissue-specific gene expression across five indicated age groups; note the color coding for the age groups. b, Left, PCA of whole-blood gene expression from every sample, color coded according to the age groups. Right, the same data were used and color-coded clusters from each age group were overlaid. Note the variance in gene expression from different age groups. c, PCA plots from b were used to show only samples from the youngest and oldest age groups analyzed. d, Hallmark GSEA based on differential gene expression between the oldest (60–69 years) and youngest (20–29 years) datasets. Pathways were ranked by P value and plotted on the x axis by the normalized enrichment scores. e, GSEA of GSEA hallmark pathway, TNF signaling via NF-κB, based on differential gene expression of oldest (60–69 years) versus youngest (20–29 years) GTEx samples. Enrichment scores are plotted on the y axis and genes ranked in the ordered dataset are plotted on the x axis. f, GSEA of the IL-2–STAT5 GSEA hallmark pathway. g, GSEA of inflammatory response GSEA hallmark pathway. h, GSEA of the oxidative phosphorylation GSEA hallmark pathway. i, Heat map of expression levels of genes associated with the TNF–NF-κB pathway. Expression values were calculated as a fold change from the 20–29-year age group. j, mitoXplorer Pathway analysis based on DSeq2 analysis of oldest (60–69 years) versus youngest (20–29 years) GTEx samples. k, Individual genes in the calcium signaling and transport pathway were identified from mitoXplorer pathway analysis based on DSeq2 analysis of oldest (60–69 years) versus youngest (20–29 years) GTEx samples. Fold change was determined as a relative change in 60–69-year compared to 20–29-year GTEX samples. l, MCU gene counts for each sample in the GTEx database sorted by age. Error bars reflect the s.e.m.; P values were calculated using ordinary one-way analysis of variance (ANOVA). m, MICU1 gene counts for each sample in GTEx database sorted by age. Error bars reflect the s.e.m.; P values were calculated using ordinary one-way ANOVA.
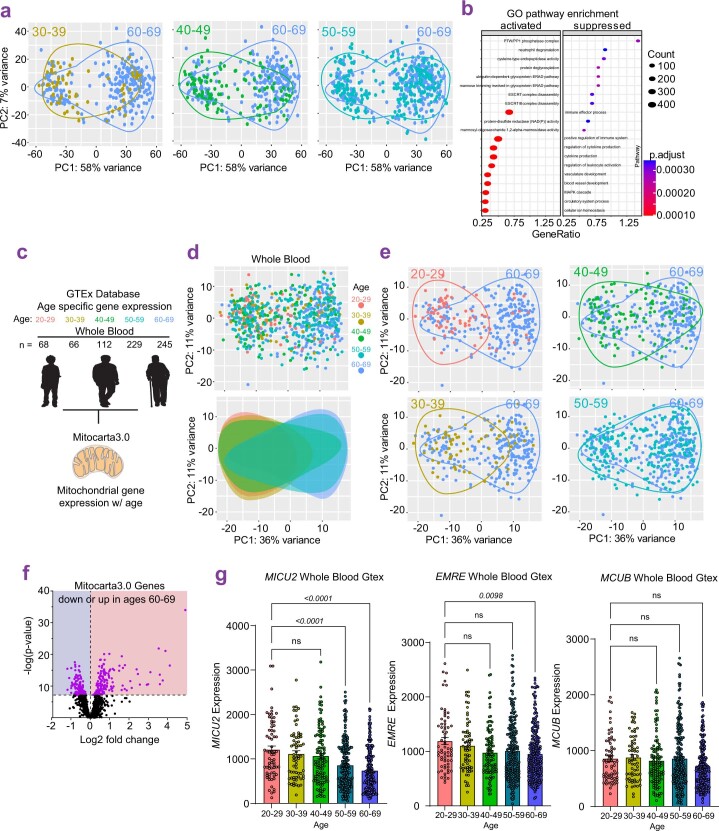
Extended Data Fig. 1. GTEx analysis of human whole blood transcriptomes.
a. Variance in gene expression in whole blood of different age groups based on Principal Component analysis on GTEx samples. b. GO pathway enrichment analysis based on DSeq2 from GTEx samples. Differential gene expression is plotted for ages 60–69 vs 20–29. Significance determined by Dotplot function (clusterProfiler R package1). c. Pipeline used for the analysis of genes encoding for mitochondria-localized proteins (mito-genes). d. Principal component analysis on mito-genes from GTEx samples. Variance in gene expression is shown for individual age groups. e. Variance in gene expression shown for age 20–29 vs 60–69, 30–39 vs 60–69, 40–49 vs 60–69, and 50–59 vs 60–69. f. Volcano plot of mito-genes expression levels in old (60–69y) vs young (20–29y) samples. Data normalization, dispersion estimates, and model fitting (negative binomial) were carried out with the DESeq function (DESeq2 R package). Wald statistics were used for the significance tests. g. MICU2, EMRE, and MCUB gene counts for each sample in GTEx database sorted by age. Error bars reflect SEM; p-values were calculated using one-way ANOVA.
Gene expression of mitochondrial Ca2+ uptake machinery correlates inversely with age
Both inflammation and mitochondrial dysfunction are hallmarks of aging1, and we wondered if there was a relationship pertinent to inflammaging. For the analysis of age-related changes in mitochondrial function, we used mitoXplorer, an analysis and visualization tool specialized for genes associated with mitochondrial functions (mito-genes)50. In accordance with previous observations, we observed significant age-related changes in the expression of mito-genes (Extended Data Fig. 1c–f). We noted a decrease in the mito-genes associated with oxidative phosphorylation, calcium signaling and reactive oxygen species defense (Fig. 1j). The mito-genes associated with mitochondrial transcription, mitochondrial dynamics, pyruvate metabolism and amino acid metabolism were expressed at similar levels. The lipid metabolism, tricarboxylic acid (TCA) cycle and glycolysis genes were expressed at higher levels in the aged population. Because Ca2+ signaling has a direct impact on inflammatory signaling in immune cells, we considered genes involved in mCa2+ signaling and found decreased expression of MCU, MICU1 and MICU2 (Fig. 1k). Moreover, the decrease in MCU and MICU1 expression was strongly associated with age, decreasing progressively as humans age (Fig. 1l,m). These observations suggested an age-associated dysregulation in mCa2+ uptake in the blood-borne immune cells. This transcriptional dysregulation was observed for MCU, MICU1 and MICU2 but the gene expression of EMRE (SMDT1) and the dominant-negative regulator MCUB showed no significant change with age (Fig. 1l,m and Extended Data Fig. 1g). We wondered if such an age-related decrease in MCU is found in all human tissues. We checked different tissues in the age-stratified GTEx data we had mined and found that the age-associated decrease in MCU gene expression was only seen in a few tissues—heart, whole blood and cerebellum (Extended Data Fig. 2a). The vast majority of tissues did not show decreased MCU expression, and some tissues, skeletal muscle, adipose tissue and thyroid showed the opposite trend—MCU expression in these tissues increased with age. The participant death parameters are reported in the GTEx database on a four-point Hardy Scale (Extended Data Fig. 2b). We assessed MCU expression across the reported Hardy Scale and found that the MCU expression was higher in the most abundant category (death 0), compared to other death categories (Extended Data Fig. 2b). The participants in death category 0 were on a ventilator before their death. When we analyzed the whole-blood samples of participants binned in this category (death 0), we still observed an age-dependent decrease in MCU (Extended Data Fig. 2c). Together, these results suggest that mCa2+ uptake capacity changes with age in some tissues, and likely contributes to age-related changes in the physiology of these tissues. From the standpoint of age-associated inflammation, the analyses put a spotlight on the key finding that in the blood, expression of MCU and MICU1 decrease progressively with age.
Extended Data Fig. 2. Age-associated changes in MCU expression in different human tissues.
a. Heat map for fold change gene reads of MCU across different tissues. b. MCU gene counts for each sample in GTEx database sorted by 4-point Hardy-Scale. Error bars reflect SEM; p-values were calculated using one-way ANOVA. c. MCU gene counts for each sample in GTEx database sorted by age for all death circumstance 0 on 4-point Hardy-Scale. Error bars reflect SEM; p-values were calculated using one-way ANOVA.
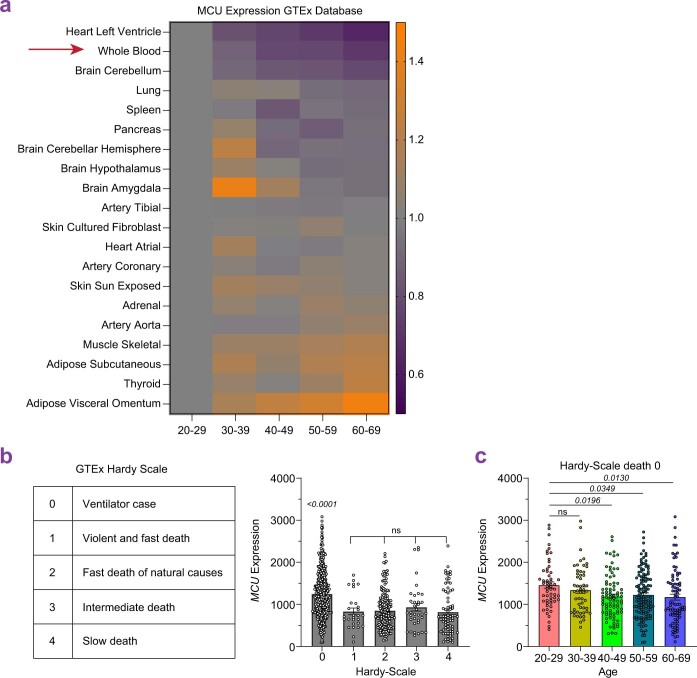
Reduced mitochondrial Ca2+ uptake in macrophages derived from old mice
The most abundant cell types in the human blood are myeloid cells, which are composed mainly of neutrophils and monocytes. Both of these cell types are short-lived in the blood but play a crucial role in inflammation. We reasoned that monocytes are more important for chronic low-grade inflammation because they can differentiate into macrophages and thereby sustain low-grade inflammation and inflammatory cascades over a relatively long period of time. Furthermore, all tissues and organs contain specialized resident macrophages, which are central to local inflammation and homeostasis. We also know that mCa2+ uptake plays an important role in macrophage-mediated fungal killing42. Considering these aspects, we focused our investigation on how mCa2+ signaling might affect macrophage-mediated inflammation. First, we confirmed that the age-associated decrease in Mcu expression was recapitulated in mouse bone marrow-derived macrophages from older mice (BMDMs-O) when compared to those from the young mice (BMDMs-Y; Fig. 2a). Importantly, the reduced gene expression resulted in decreased MCU protein levels (Extended Data Fig. 3a). MICU1 protein levels were unchanged (Extended Data Fig. 3a). We wondered if this transcriptional defect was a result of macrophage differentiation ex vivo or intrinsic to bone marrow progenitors. We measured the gene expression of Mcu and its regulatory subunits in undifferentiated bone marrow cells (BMCs) and bone marrow-derived macrophages (BMDMs) isolated from young (15–25 weeks) and old (80–90 weeks) mice (Extended Data Fig. 3b). In the old BMCs, we found a significant decrease in the expression of Mcu, Micu2 and Emre. In the BMDMs derived from old BMCs, we found a significant decrease in the gene expression of Mcu, Emre and Mcub. These results indicate that the bone marrow progenitors undergo substantial changes in the expression of MCU complex components, and especially in the expression of Mcu. Changes in regulatory subunit composition and expression can affect mCa2+ uptake capacity51. We reasoned that gross changes in the stoichiometry of the MCU complex would affect its protein mobility when resolved on a non-reducing gel. However, the mobility was identical in BMDMs-O and BMDMs-Y (Extended Data Fig. 3c). Stripping the membrane and immunoblotting for MICU1 showed comparable levels of MICU1 at the same mobility at MCU, although we found MICU1 in other complexes as well (Extended Data Fig. 3c). Next, we tested the most obvious hypothesis that macrophages exhibit an age-dependent decrease in their mCa2+ uptake. The basic technical design of this assay is to add Ca2+ to macrophages permeabilized with digitonin, and as the mitochondria take up the added Ca2+, its loss from the bath solution is reported by the reduction in the fluorescence of calcium green-5N, a small-molecule Ca2+ indicator in the bath solution. We show that BMDMs derived from the young mice exhibited robust mCa2+ uptake, but this process was significantly impaired in the BMDMs-O. The representative traces are shown in Fig. 2b and a quantification of the percentage of the added Ca2+ taken up by the mitochondria is shown in Fig. 2c. The addition of the mitochondrial uncoupler FCCP stops the Ca2+ uptake and even reverses it (Fig. 2b), indicating that the mCa2+ uptake is driven by the membrane potential of the mitochondrial inner membrane. Similarly, Ruthenium red (10 μM), a known blocker of MCU24,31, abrogates mCa2+ uptake, showing that the process is largely dependent on MCU. This age-associated reduction in mCa2+ uptake was found in both females and males (Fig. 2d). When we pulsed a much lower dose of Ca2+ (1 µM), the mCa2+ uptake in BMDMs-O was comparable for the first two pulses but started to lag behind BMDMs-Y after that (Extended Data Fig. 3d), consistent with impaired mCa2+ uptake. To determine if defects in mCa2+ uptake were a result of decreased mitochondrial membrane potential, we measured mitochondrial membrane potential in BMDMs-O and BMDMs-Y with TMRM, at baseline and after zymosan stimulation (Extended Data Fig. 4a). Surprisingly, BMDMs-O showed a modest hyperpolarization compared to BMDMs-Y suggesting the defect in mCa2+ uptake is independent of resting membrane potential (Extended Data Fig. 4a). We also measured ATP levels in BMDMs-Y and BMDMs-O but found no significant differences in ATP levels (Extended Data Fig. 4b). Besides an evaluation of mCa2+ uptake, we also quantified mitochondrial numbers and morphology. We immunostained for TOM20 and then applied an automated image processing software to quantify mitochondrial numbers and morphology of confocal images52. Comparing BMDMs-Y and BMDMs-O in this manner, we found a modest reduction in mitochondrial numbers but no significant differences in mitochondrial area, roundness and branches (Extended Data Fig. 4c–g). Overall, the results show conclusively that the macrophages in old mice have a significant defect in mCa2+ uptake, and this is attributable, at least in part, to a substantial decrease in MCU protein levels and to modest changes in mitochondrial numbers. Next, we focused on understanding the functional implications of this age-associated defect in mCa2+ uptake in macrophages.
Fig. 2. Macrophages generated from aged mice display decreased mitochondrial Ca2+ uptake.
a, Mcu expression in BMDMs. N = 12 biological replicates, from four mice. Error bars reflect the s.e.m.; P = 0.0016 according to Welch’s t-test, two-tailed. b, Representative traces of mCa2+ uptake. c, Quantification of b. N = 28 biological replicates. Error bars reflect the s.e.m.; P values were calculated using ordinary one-way ANOVA. RuR, Ruthenium red. d, mCa2+ uptake data shown in c—segregated by sex. Error bars reflect the s.e.m.; P values were calculated using Welch’s t-test, two-tailed. e, Representative cCa2+ oscillations. f, Maximum cCa2+. N = 88 cells, three independent experiments. Whiskers represent the minimum to maximum values for each dataset. The box represents the 75th and 25th percentiles. The line is the median; P < 0.0001 according to one-way ANOVA. g, CALIMA spatiotemporal Ca2+ dynamics. h, Number of oscillations in individual cells. N = 88 cells, three independent experiments. Whiskers represent the minimum to maximum values for each dataset. The box represents the 75th and 25th percentiles. Line is at the median; P < 0.0001 according to Welch’s t-test, two-tailed. i, Oscillation length in individual cells. N = 88 cells, three independent experiments. Whiskers represent the minimum to maximum values for each dataset. The box represents the 75th and 25th percentiles. Line is at the median; P < 0.0001 according to Welch’s t-test, two-tailed. NS, not significant.
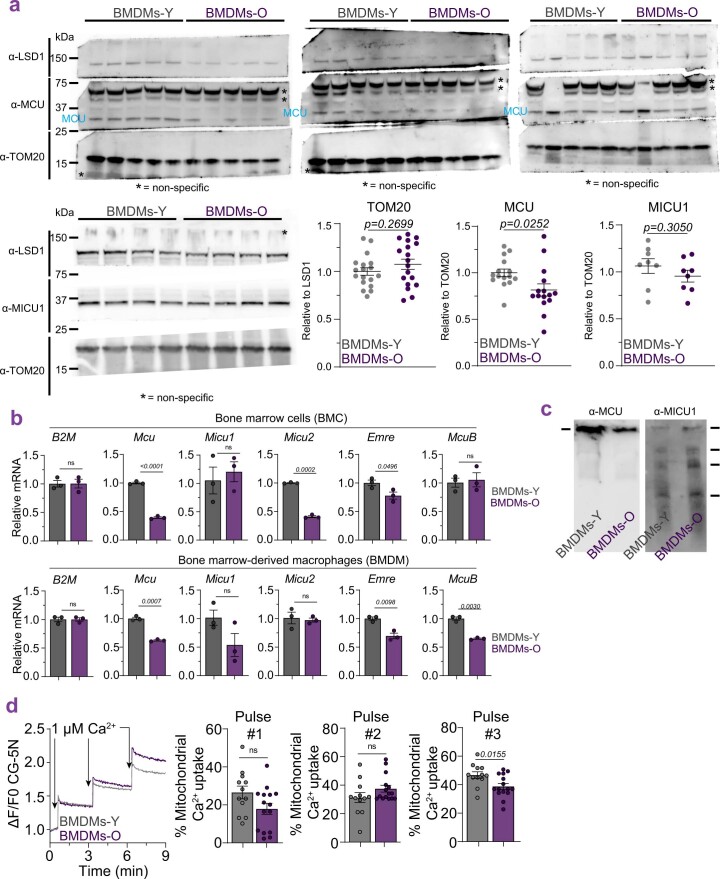
Extended Data Fig. 3. Expression of MCU components in BMDMs.
a. Western blot analysis of MCU, TOM20, and MICU1 protein. N = 5–15 mice, error bars reflect SEM; p-value determined by Welch’s t-test, two-tailed. b. Quantitative-PCR of Mcu and its regulatory subunits. N = 3 mice. Error bars reflect SEM; p-value determined by Welch’s t-test, two-tailed. c. Resolution of MCU complex in non-reducing conditions and immunoblotting for MCU and MICU1, N = 1 mouse. d. Pulsed mitochondrial Ca2+ uptake. N = 15 biological replicates.
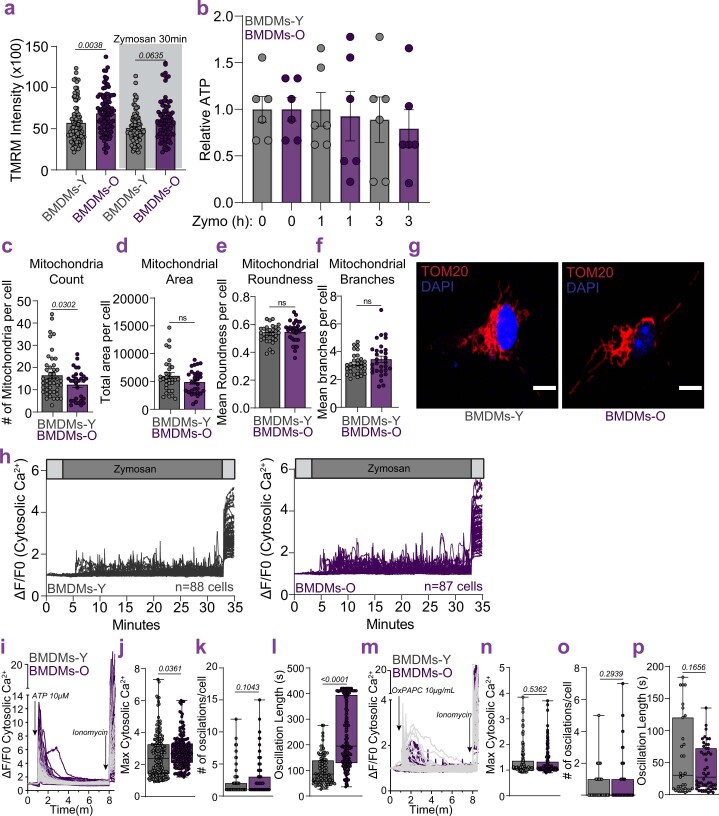
Extended Data Fig. 4. Analysis of mitochondria and Ca2+ responses in BMDMs.
a. Mitochondrial membrane potential. N = 90 cells, 3 independent experiments. Error bars reflect SEM; p-value determined by one-way ANOVA. b. Normalized luminescent measurements of ATP. N = 6 biological repeats. Error bars reflect SEM; p-value determined by one-way ANOVA. c. Mitochondrial counts. N = 30–45 cells, 3 independent experiments. Error bars reflect SEM; p-value significance according to Welch’s t-test, two-tailed. d. Mitochondrial area. N = 30–45 cells, 3 independent experiments. Error bars reflect SEM; not statistically significant according to Welch’s t-test, two-tailed. e. Mitochondrial roundness. N = 30–45 cells, 3 independent experiments. Error bars reflect SEM; not statistically significant according to Welch’s t-test, two-tailed. f. Mitochondrial branches. N = 30–45 cells, 3 independent experiments. Error bars reflect SEM; not statistically significant according to Welch’s t-test, two-tailed. g. Representative images of BMDMs-Y and BMDMs-O immunostained for TOM20. Scale bar at 10 µm. h. Cytosolic Ca2+ Oscillations in BMDMs-Y (n = 88 cells) and BMDMs-O (n = 87 cells). i. Cytosolic Ca2+ Oscillations with ATP. j. Maximum cytosolic Ca2+. N = 112 cells, 2 independent experiments. Whiskers represent the min to max values for each data set. Box represents 75th and 25th percentile. Line is at the median; p-value according to Welch’s t-test, two-tailed. k. Number of oscillations in individual cells. N = 112 cells, 2 independent experiments. Whiskers represent the min to max values for each data set. Box represents 75th and 25th percentile. Line is at the median; p<value according to Welch’s t-test, two-tailed. l. Oscillation length in individual cells. N = 112 cells, 2 independent experiments. Whiskers represent the min to max values for each data set. Box represents 75th and 25th percentile. Line is at the median; p<0.0001 according to Welch’s t-test, two-tailed. m. Cytosolic Ca2+ Oscillations with OxPAPC. n. Maximum cytosolic Ca2+. N = 104 cells, 2 independent experiments Whiskers represent the min to max values for each data set. Box represents 75th and 25th percentile. Line is at the median; p-value according to Welch’s t-test, two-tailed. o. Number of oscillations in individual cells. N = 104 cells, 2 independent experiments. Whiskers represent the min to max values for each data set. Box represents 75th and 25th percentile. Line is at the median; p<value according to Welch’s t-test, two-tailed. p. Oscillation length in individual cells. N = 104 cells, 2 independent experiments. Whiskers represent the min to max values for each data set. Line is at the median; p<0.0001 according to Welch’s t-test, two-tailed.
Amplified cytosolic Ca2+ oscillations in BMDMs-O responding to zymosan
We hypothesized that a reduction in mCa2+ uptake would disrupt cCa2+ signaling, which is crucial for inflammatory signaling. We challenged BMDMs derived from young and old mice with zymosan, a fungal glucan wherein the glucose monomers are polymerized through β-1,3 glycosidic bonds. Zymosan is a potent stimulator of both Toll-like receptor 2 (TLR2) and dectin-1 (CLEC7A) receptors on myeloid cells. The downstream activation of phospholipase C-gamma (PLC-γ) elicits a robust store-operated Ca2+ entry (SOCE), which involves an initial release of endoplasmic reticulum (ER)-resident Ca2+ stores, followed by more sustained entry of extracellular Ca2+ through the ORAI channels. Inflammatory gene expression mediated by multiple transcription factors, especially NF-κB, is highly sensitive to cCa2+ oscillations19,20. In response to zymosan, the amplitudes of the cCa2+ oscillations in BMDMs-O were significantly elevated compared to BMDMs-Y; typical and representative traces from cells are shown (Fig. 2e and Extended Data Fig. 4h). A statistical comparison of the maximum Ca2+ elevations achieved in each cell also shows that the BMDMs-O achieved significantly higher amplitudes (Fig. 2f). In these experiments, ionomycin, a Ca2+ ionophore, was used as a positive control demonstrating that both cell populations were loaded equivalently with the Ca2+ dye (FURA-2AM) and were thus capable of reporting higher and equivalent levels of Ca2+. The overlaid traces of cCa2+ from all cells are also shown (Extended Data Fig. 4h). The spatial distribution of these oscillations across the imaging field (containing many cells) is also informative but not captured by such a traditional display of Ca2+ oscillations. For a deeper analysis of this aspect of Ca2+ dynamics, we used CALIMA, an image analysis software specially designed to measure spatiotemporal aspects of Ca2+ oscillations53. The spatial distribution of Ca2+ oscillations in representative image fields is shown (Fig. 2g) with the origin of each circle at the cellular location and the diameter proportional to the number of spikes originating from that location. The color spectrum of the circles denotes the time at which that location first reported a spike. For instance, in each field, the location of the reddish-brown circle reported a Ca2+ spike earlier than the circles colored green and so on. These spatial maps clearly show that BMDMs-O exhibit a significantly higher number of Ca2+ oscillations for each cell and they also start spiking sooner than BMDMs-Y. These are quantified (Fig. 2h), and the differences in oscillatory lengths are also shown (Fig. 2i). These data establish that Ca2+ elevations are amplified in the BMDMs-O during inflammatory signaling. Our analysis on Ca2+ dynamics in response to fungal pathogens is highly relevant to chronic low-grade inflammation attributed to dysregulated microbiome and ‘leaky gut’ observed in older populations54. However, we were curious if this may also pertain to other mechanisms of chronic low-grade inflammation. Two additional sources of low-grade inflammation in older populations are ATP release from dying cells and oxidative stress. We subjected BMDMs-O to analyses of cCa2+ dynamics in response to ATP (Extended Data Fig. 4i–l) and oxidized PAPC (OxPAPC; Extended Data Fig. 4m–p). Although the nature of Ca2+ response to ATP is different from that to zymosan, the BMDMs-O showed dysregulated cCa2+ responses with an increase in maximum amplitudes (Extended Data Fig. 4j) and oscillation lengths (Extended Data Fig. 4l). This was not the case for OxPAPC-triggered Ca2+ responses—we did not find any significant differences between BMDMs-Y and BMDMs-O. This dichotomy suggests that mCa2+ uptake doesn’t play a major role in OxPAPC-triggered Ca2+ elevations.
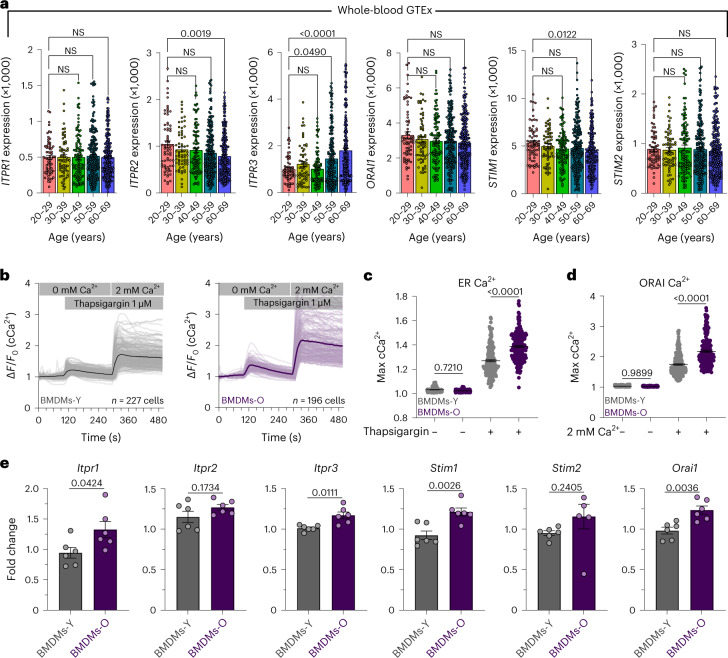
Inconsistent changes in gene expression of store-operated Ca2+ entry components
Recent reports in mice have suggested ER Ca2+ channels as important drivers of cellular aging and senescence55. Since mCa2+ uptake is thought to occur in close juxtaposition to ER Ca2+ release56, we analyzed the whole-blood GTEx transcriptome for age-associated changes in SOCE machinery. We observed inconsistent changes in the expression of SOCE components. There was an upregulation in ITPR3 but downregulation of ITPR1 (Fig. 3a). Additionally, we observed a modest decrease in STIM1 expression but no effect of age on ORAI1 or STIM2 expression (Fig. 3a). These observations do not support a clear role for changes in SOCE machinery. We also assessed composite SOCE responses in BMDMs-O and BMDMs-Y (Fig. 3b). In these experiments, macrophages were loaded with Fura-2-AM and placed in a 0 mM Ca2+ bath and stimulated with thapsigargin, a sarcoplasmic reticulum Ca2+ ATPase (SERCA) pump inhibitor, to visualize ER Ca2+ release (first elevation in cCa2+). This is followed by the addition of 2 mM extracellular Ca2+ to observe the ORAI-dependent Ca2+ influx (second elevation; Fig. 3b). Loss of mCa2+ uptake is predicted to increase both the first cCa2+ elevation caused by the release of Ca2+ from the ER and the second elevation caused by the entry of extracellular Ca2+ into the cytosol. Quantification of the ER Ca2+ release and ORAI Ca2+ entry revealed increased SOCE responses in BMDMs-O (Fig. 3c,d). Although reduced mCa2+ uptake is a major component of amplified SOCE, additional factors like increased release from the ER cannot be ruled out (Fig. 3e). Regardless of the mechanistic intricacies, amplified cCa2+ responses are a hallmark of BMDMs-O.
Fig. 3. Store-operated Ca2+ entry responses in macrophages generated from aged mice.
a, ITPR1, ITPR2, ITPR3, ORAI1, STIM1 and STIM2 gene counts for each sample in whole-blood GTEx database sorted by age. Error bars reflect the s.e.m.; P values were calculated using ordinary one-way ANOVA. b, Representative cCa2+ oscillations in BMDMs-Y and BMDMs-O. Bold lines indicated the mean of individual traces. c, Quantification of ER Ca2+. N = 150 cells, three independent experiments. Error bars represent the s.e.m.; P values were determined by one-way ANOVA. d, Quantification of ORAI Ca2+. N = 150 cells, three independent experiments. Error bars represent the s.e.m.; P value determined by one-way ANOVA. e, Fold change expression at baseline for SOCE genes. N = 6 biological replicates, two independent experiments. Error bars represent the s.e.m.; P value determined by Welch’s t-test, two-tailed.
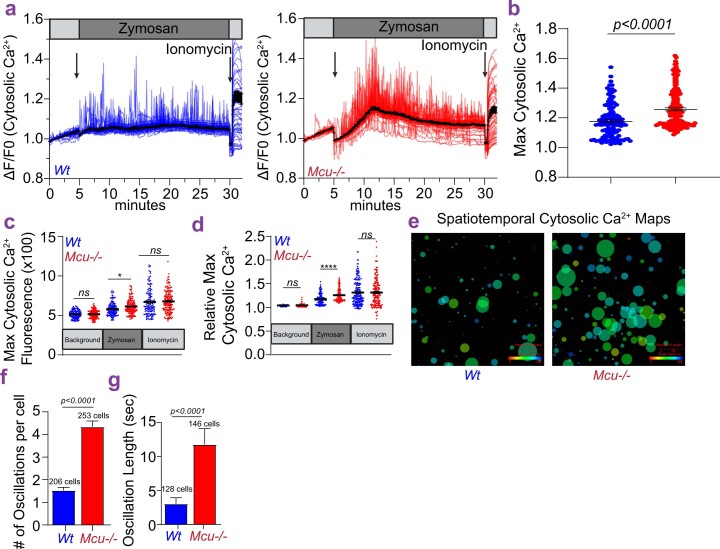
Mcu−/− BMDMs-Y recapitulate the amplified cytosolic Ca2+ signals seen in BMDMs-O
To establish that this effect on cCa2+ signaling is because of reduced mCa2+ uptake, we show that the effect can be robustly recapitulated in BMDMs derived from young mice (age range, 15–25 weeks) by simply deleting Mcu. As shown (Extended Data Fig. 5a), Mcu−/− BMDMs, derived from Mcufl(Cx3cr1-cre) mice42 show a robust amplification of cCa2+ oscillations in response to zymosan. The maximum Ca2+ levels achieved by individual cells are shown in Extended Data Fig. 5b. Appropriate controls for long-term Ca2+ imaging is shown in Extended Data Figs. 5c and 6d. The spatiotemporal analysis using CALIMA is shown in Extended Data Fig. 5e–g. This analysis shows that, as seen in old BMDMs, the Mcu−/− BMDMs exhibit many more oscillations for each cell, and the length of the oscillations is also increased. Together, these data establish that the increased cCa2+ signaling in the old BMDMs is a direct consequence of the reduced mCa2+ uptake.
Extended Data Fig. 5. cCa2+ dynamics in Mcu−/− BMDMs-Y.
a. Cytosolic Ca2+ Oscillations in wt and Mcu−/− BMDMs. b. Maximum cytosolic Ca2+. N = 83 cells, 2 independent experiments. Error bars represent SEM; p<0.0001 according to Welch’s t-test, two-tailed. c. Maximum cytosolic Ca2+. N = 83 cells, 2 independent experiments. Error bars represent SEM; p<0.0001(****), p≤0.001(***), p≤0.01(**), p≤0.05(*) determined by the Brown-Forsythe and Welch ANOVA test. d. Maximum cytosolic Ca2+. N = 83 cells, 2 independent experiments. Error bars represent SEM of two independent experiments; p<0.0001(****), p≤0.001(***), p≤0.01(**), p≤0.05(*) determined by the Brown-Forsythe and Welch ANOVA test. e. CALIMA maps depicting spatiotemporal aspects of cytosolic Ca2+ elevations. f. Average number of oscillations per cell, seen during zymosan stimulation. N = 83 cells, 2 independent experiments Error bars represent SEM; p<0.0001 according to Welch’s t-test, two-tailed. g. Mean of oscillation lengths during zymosan stimulation. N = 83 cells, 2 independent experiments Error bars represent SEM; p<0.0001 according to Welch’s t-test, two-tailed.
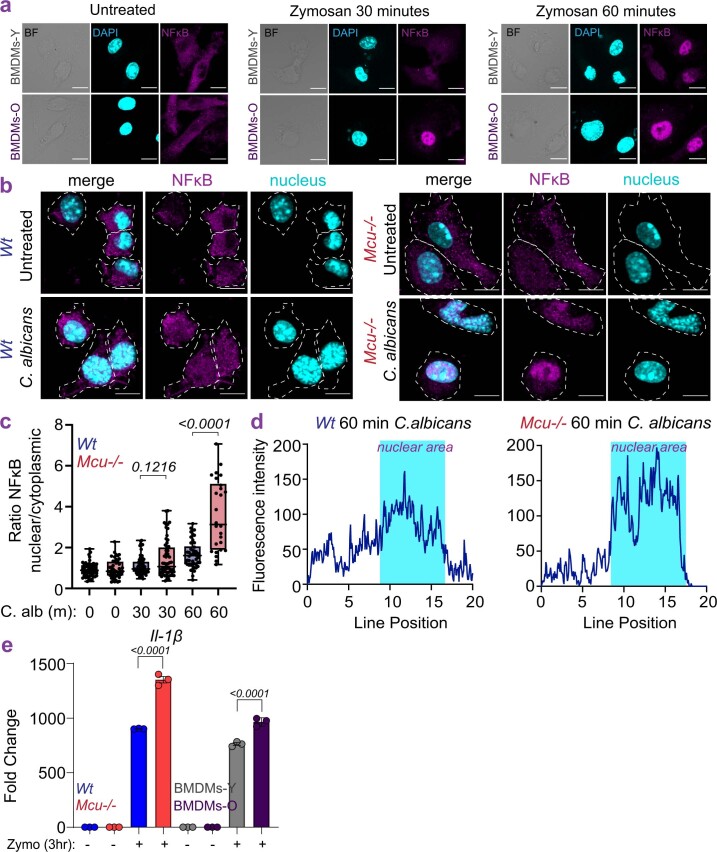
Extended Data Fig. 6. Analysis of NFkB translocation in response to C. albicans.
a. Representative images for data shown in Fig. 3g shown as single channels. b. Representative images from wt and Mcu−/− BMDMs, untreated or stimulated with C. albicans, for 30 or 60 minutes and immunostained for NFκB p65 subunit and nuclei (DAPI). The outline of cells was determined by bright field images. c. Nuclear to cytoplasmic ratios of the fluorescent intensity of NFκB for images shown in panel b. N = 30–72 cells, 2 independent experiments. Whiskers represent the min to max values for each data set. Box represents 75th and 25th percentile. Line is at the median; p-value according to one-way ANOVA. d. Representative analysis of fluorescent intensity of p65 staining along a line drawn across the cytoplasm and nucleus, as determined by DAPI staining (shaded blue). e. Zymosan-induced IL-1b expression (qPCR) in indicated BMDMs. N = 3 biological replicates. Error bars represent SEM, p-value calculated by one-way ANOVA.
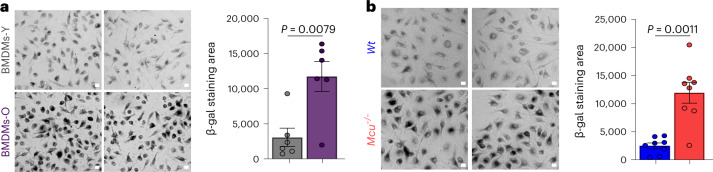
BMDMs-O and Mcu−/− BMDMs-Y show signatures of senescence
Aging is commonly associated with the presence of senescent cells and a long-standing hallmark of senescent cells is senescence-associated β-galactosidase (SA-β-gal) activity attributed to the lysosomal β-galactosidase in mammals57,58. To determine if BMDMs-O exhibited signs of cellular senescence, we compared SA-β-gal staining in BMDMs-O and BMDMs-Y (Fig. 4a). In this method, cells were stained with X-gal and imaged for the presence of blue precipitates formed by the activity of SA-β-gal. These precipitates can be observed under a bright-field light microscope and appear as dark aggregates. By measuring hundreds of cells, we found that BMDMs-O showed significantly increased SA-β-gal staining (Fig. 4a). We reasoned that if the loss of mCa2+ uptake contributes to this senescent signature, we would observe SA-β-gal activity in Mcu−/− macrophages from young mice. Indeed, Mcu−/− macrophages from young mice had robust SA-β-gal activity (Fig. 4b). These findings bolstered the hypothesis that loss of mCa2+ uptake in macrophages renders them hyper-inflammatory and as facilitators of inflammaging.
Fig. 4. BMDMs-O and young Mcu−/− macrophages show signatures of senescence.
a, SA-β-gal activity. Scale bar, 10 µm. N = 6 biological replicates. b, SA-β-gal activity. Scale bar, 10 µm. N = 8 biological replicates. In a and b, error bars reflect the s.e.m., and P values were calculated using Welch’s t-test, two-tailed.
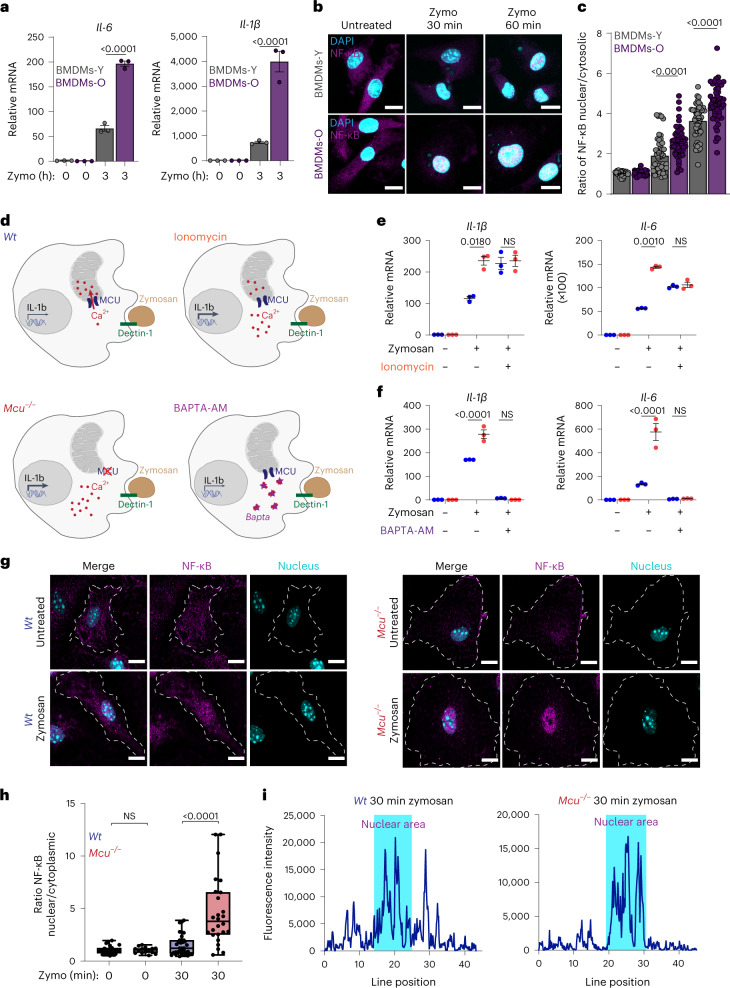
Hyper-inflammatory responses in both wild-type BMDMs-O and Mcu−/− BMDMs-Y
We hypothesized that the abnormally increased cCa2+ signaling in BMDMs-O would result in increased inflammatory output. Indeed, in response to zymosan, BMDMs-O expressed higher levels of pro-inflammatory cytokines interleukin (IL)-6 and IL-1β when compared to BMDMs-Y (Fig. 5a). NF-κB plays a crucial role in the transcription of these pro-inflammatory genes, and its activation is highly sensitive to Ca2+ signaling19,59. We measured NF-κB translocation (p65) in BMDMs-Y and BMDMs-O stimulated with zymosan and found that, in accordance with our model, the translocation of NF-κB was significantly enhanced in the BMDMs-O (Fig. 5b and Extended Data Fig. 6a). The quantification of the ratio of nuclear to cytoplasmic NF-κB shows that significantly more NF-κB translocated to the nuclei of BMDMs-O (Fig. 5c). These data show that macrophages from the older mice are hyper-inflammatory in response to zymosan. Consistently, we found that Mcu−/− macrophages from young mice also exhibit a hyper-inflammatory response to zymosan stimulation, establishing a model wherein reduction in mCa2+ uptake increases inflammatory output through amplified cCa2+ signaling (Fig. 5d). Predictably, the Mcu−/− BMDMs-Y showed significantly increased expression of both IL-1β and IL-6 (Fig. 5e). Note that when ionomycin was added to artificially increase cCa2+, even wild-type (WT) BMDMs-Y increased the expression of IL-1β, highlighting the sensitivity of the macrophage inflammatory response to cCa2+. A similar effect was observed for IL-6, but there was a key difference—while ionomycin increased the expression of IL-6 in WT cells, it also decreased the expression of IL-6 in Mcu−/− BMDMs. A possible reason for this is that unlike the oscillatory effects caused by reduced mCa2+ uptake, ionomycin causes a global and sustained elevation of Ca2+. In Mcu−/− BMDMs, this elevation is unbuffered by mCa2+ uptake, and this may inhibit other regulatory elements of IL-6 transcription. Nevertheless, the upregulation of both IL-1β and IL-6 is highly dependent on Ca2+ signaling. BAPTA-AM, a cell permeable, high-affinity Ca2+ chelator that prevents the elevation of cCa2+ during zymosan-triggered inflammatory signaling completely abrogated the expression of IL-1β and IL-6 (Fig. 5f). NF-κB translocation was also found to be enhanced in Mcu−/− BMDMs-Y (Fig. 5g). Quantification of the nuclear/cytoplasmic ratio revealed an increase in NF-κB activation in Mcu−/− BMDMs-Y (Fig. 5h). Representative line intensity plots across the nucleus and cytosol are shown (Fig. 5i). The increased activation of NF-κB in Mcu−/− macrophages was also seen when they were stimulated with the fungal pathogen Candida albicans (Extended Data Fig. 6b), but the translocation kinetics were slower in comparison to zymosan stimulation (Extended Data Fig. 6c). Representative line intensity plots are shown (Extended Data Fig. 6d). The inflammatory output, as measured by IL1B gene expression, of Mcu−/− BMDMs was higher than that of BMDMs-O because mCa2+ uptake was almost completely abrogated in Mcu−/− BMDMs, while it was reduced in BMDMs-O (Extended Data Fig. 6e). During the macrophage response to zymosan, the influx of extracellular Ca2+ into the cytosol depends predominantly on Orai channels. Predictably, treating the Mcu−/− BMDMs with an inhibitor of Orai, the main conduit of SOCE, greatly blunted the gene expression of both IL-1β and IL-6 (Extended Data Fig. 7a). BTP2 also blunted the nuclear translocation of NF-κB (Extended Data Fig. 7b). However, besides buffering cCa2+ elevations, mCa2+ uptake also regulates mitochondrial metabolism, primarily by regulating the activity of pyruvate dehydrogenase (PDH) complex and the TCA cycle60. In principle, the changes in mitochondrial metabolism in the Mcu−/− BMDMs could exert an added effect on macrophage inflammatory output. Although this possibility cannot be completely ruled out, the following evidence suggests that changes in mitochondrial metabolism play a minimal role in the immediate regulation of inflammatory outputs in Mcu−/− BMDMs. The influx of Ca2+ into the mitochondrial matrix regulates the TCA cycle through the activation of PDH complex. The PDH complex is activated through dephosphorylation by the Ca2+-activated PDH phosphatase (PDP)61 and abrogation of mCa2+ uptake prevents the dephosphorylation (and activation) of PDH. We reasoned that treating the cells with AZD7545, an inhibitor of the PDH kinase, would counter the lack of PDP activity and restore PDH activity in a Ca2+-independent manner. However, treating the Mcu−/− BMDMs with AZD7545 did not reduce the gene expression of IL-6 and only modestly reduced IL-1β (Extended Data Fig. 7c). These results support the model wherein amplified Ca2+ signaling in the cytosol is the main driver of the increased inflammatory output of Mcu−/− cells. Although the role of mitochondrial metabolism in regulating this process is not supported by the available data, it cannot be ruled out.
Fig. 5. Mitochondrial Ca2+ uptake buffers cytosolic Ca2+ to control inflammatory output in macrophages.
a, IL-6 and IL-1β mRNA expression from indicated BMDMs. Representative experiment, from two independent experiments. Error bars represent the s.e.m.; P < 0.0001 according to one-way ANOVA. b, Representative images from indicated BMDMs stimulated with zymosan for 30 and 60 min. Magenta shows immunostaining of NF-κB p65 subunit; cyan shows DAPI staining of nuclei. c, Nuclear to cytoplasmic ratios of the fluorescence intensity of NF-κB. N = 45 cells, three independent experiments. Bars reflect means of ratios; P values were determined by one-way ANOVA. d, Model depicting how mCa2+ uptake affects cCa2+ and inflammatory gene expression in response to zymosan. e, Effect of ionomycin on IL-1β and IL-6 mRNA expression in WT and Mcu−/− macrophages. Representative experiment, from two independent experiments. Error bars represent the s.e.m.; P values were determined by two-way ANOVA. f, Effect of BAPTA-AM on IL-1β and IL-6 expression in WT and Mcu−/− macrophages. Representative experiment, from two independent experiments. Error bars represent the s.e.m.; P value determined by two-way ANOVA. g, Representative images from WT and Mcu−/− macrophages, untreated or stimulated with zymosan for 30 min and immunostained for NF-κB p65 subunit and nuclei (DAPI). h, Nuclear to cytoplasmic ratios of the fluorescence intensity of NF-κB. N = 25 cells, from three independent experiments. Whiskers represent the minimum to maximum values for each dataset. The box represents the 75th and 25th percentiles. The line is the median; P < 0.0001 according to one-way ANOVA. i, Representative analysis of fluorescence intensity of p65 staining along a line drawn across the cytoplasm and nucleus (DAPI staining), which is shaded blue.
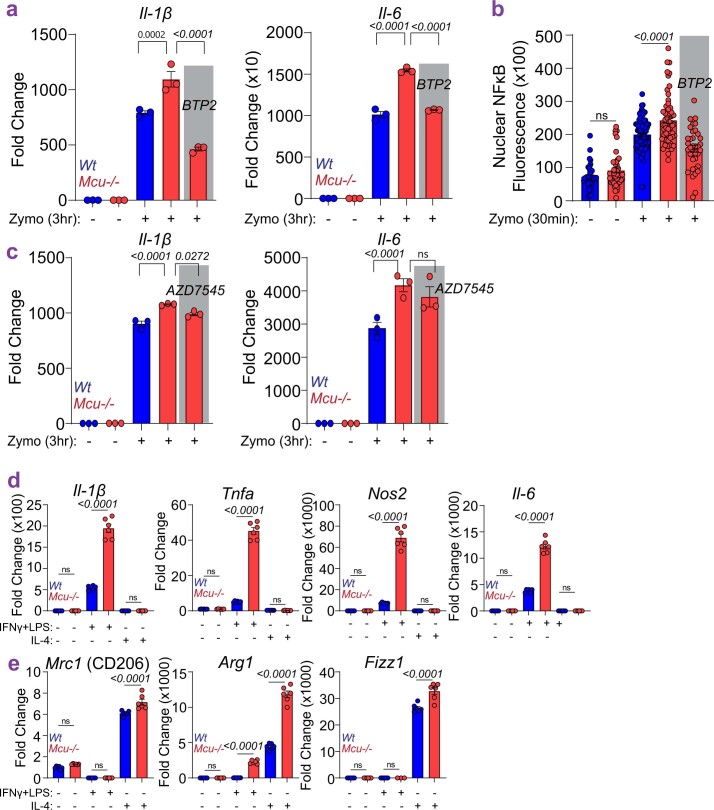
Extended Data Fig. 7. Effects of BTP2 and AZD7545 on inflammatory gene expression and analysis of macrophage activation.
a. Fold change expression of IL-1β and IL-6. N = 3 biological replicates. Error bars represent SEM; p-value determined by one-way ANOVA. b. Nuclear NFκB. N = 36–50 cells, 3 independent experiments. Error bars represent SEM; p-value determined by one-way ANOVA. c. Fold change expression of IL-1β and IL-6. N = 3 biological replicates. Error bars represent SEM; p-value determined by one-way ANOVA. d. Assessment of M1 polarization in wt and Mcu−/− BMDMs. N = 6 biological replicates. Error bars represent SEM; p-value determined by one-way ANOVA. e. Assessment of M2 polarization in wt and Mcu−/− BMDMs. N = 6 biological replicates. Error bars represent SEM; p-value determined by one-way ANOVA.
Abnormal functional polarization of Mcu−/− macrophages
Previous reports on the role of mCa2+ on macrophage polarization have shown links between mCa2+ and macrophage polarization. Mcu inhibition is linked to an impaired M2 polarization44,62, while deletion of Mcub is linked to enhanced M1 polarization and impaired M2 polarization43. The M1–M2 polarization is not universally accepted as being physiologically meaningful because macrophages achieve a spectrum of functional states in vivo. Nevertheless, we performed M1 and M2 polarization studies in Mcu−/− macrophages (Extended Data Fig. 7d,e). M1 polarized Mcu−/− macrophages showed enhanced expression of NF-κB target gene with unexpected expression of Arg1. Interestingly, M2 polarized Mcu−/− macrophages also showed enhanced expression of M2 markers. However, such polarization experiments are performed over 24 h and the outputs are an integrated result of many secondary and tertiary signaling cascades in macrophages.
Mcu−/− bone marrow-derived macrophages also show increased NLRP3 inflammasome activation
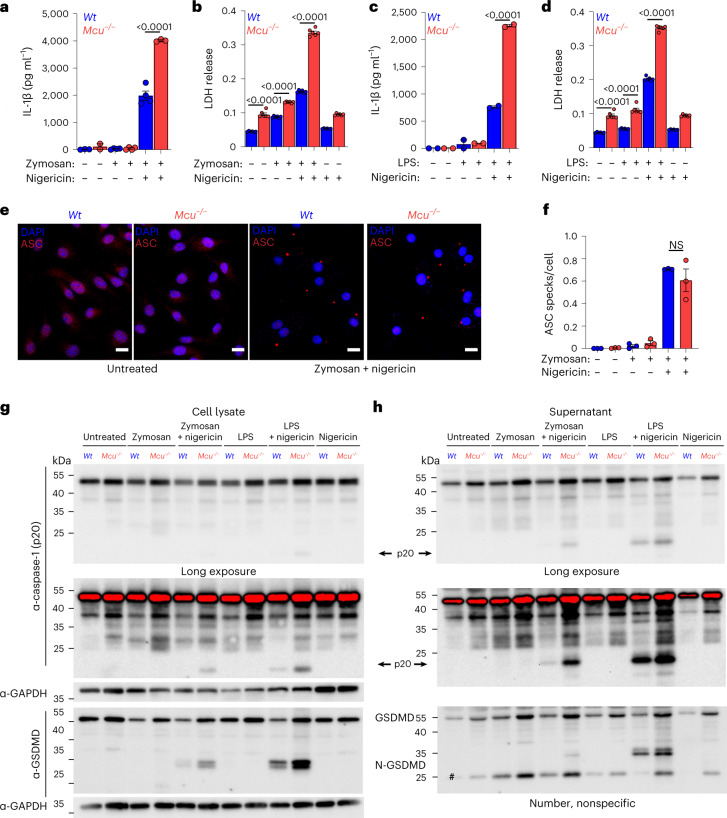
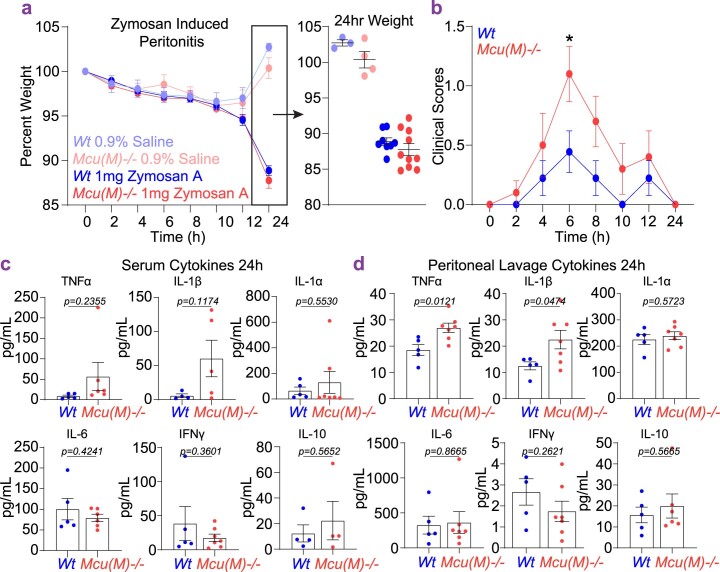
Next, we evaluated if the increased inflammatory gene expression caused by decreased mCa2+ uptake also increases inflammasome activation. WT and Mcu−/− macrophages from young mice were stimulated with zymosan for 3 h before the addition of nigericin (5 µM) for 1 h to activate the NLRP3 inflammasome. Mcu−/− macrophages released significantly more IL-1β (Fig. 6a) and lactate dehydrogenase (LDH; Fig. 6b), and this effect was also seen when the macrophages were first stimulated with lipopolysaccharide (LPS; Fig. 6c,d). We wondered if the assembly of the NLRP3 inflammasome is also accentuated in Mcu−/− macrophages. Assembly of NLRP3 inflammasome can be visualized through immunofluorescence microscopy of ASC speck formation63–67. We did not see any significant difference in ASC speck formation in Mcu−/− BMDMs (Fig. 6e,f) indicating that decreased mCa2+ uptake, and concomitantly increased cCa2+ signaling, does not have a major impact on the assembly of NLRP3 inflammasome. Activation of the NLRP3 inflammasome results in the proteolytic cleavage and activation of caspase-1 (CASP1). Activated CASP1 catalyzes the proteolytic processing of pro-IL-1β to its secreted form IL-1β. CASP1 also cleaves monomeric gasdermin D (GSDMD), thus catalyzing their oligomerization into a large multimeric gasdermin pore in the plasma membrane. The release of many potent pro-inflammatory mediators, including IL-1β and IL-18, is mediated through this large GSDMD pore. Overall, this process results in a highly inflammatory form of cell death called pyroptosis. We assessed the cleavage of CASP1 and GSDMD in NLRP3 activated macrophages. Notably, we found that the cleavage of both CASP1 and GSDMD was significantly increased in Mcu−/− macrophages—in both cell pellets (Fig. 6g) and in supernatants (Fig. 6h). These findings indicate that while decreased mCa2+ uptake does not affect NLRP3 assembly, it does have a significant impact on the downstream processing of CASP1 and GSDMD. Finally, we evaluated whether deletion of Mcu in the myeloid cells would manifest a hyper-inflammatory response in vivo. Previous reports have shown that long exposures to fungal beta-glucans can activate the NLRP3 inflammasome in macrophages68. In a model of zymosan-induced peritonitis, mice lacking Mcu in the myeloid cells, the Mcu(M)−/− mice, exhibited significantly worse clinical scores, and increased levels of IL-1β and tumor necrosis factor (TNF) in the peritoneal cavity (Extended Data Fig. 8a–d). However, we did not see increased levels of other pro-inflammatory cytokines (IL-1α, IL-6 and IFN-γ) that we measured in this model.
Fig. 6. Mcu−/− macrophages display increased inflammasome activation and output.
a, IL-1β enzyme-linked immunosorbent assay (ELISA) of cell supernatants collected from WT and Mcu−/− macrophages. Cells were stimulated with zymosan for 3 h followed by nigericin (5 µM) overnight. N = 3 biological replicates. Error bars represent the s.e.m.; P values were determined by one-way ANOVA. b, LDH levels in cell supernatants were collected from WT and Mcu−/− macrophages. N = 6 biological replicates. Error bars represent the s.e.m.; P < 0.0001 determined by one-way ANOVA. c, IL-1β ELISA of cell supernatants collected from WT and Mcu−/− macrophages. Cells were stimulated with LPS for 3 h followed by nigericin (5 µM) overnight. N = 2 biological replicates. Error bars represent the s.e.m.; P values were determined by one-way ANOVA. d, LDH levels in cell supernatants collected from WT and Mcu−/− macrophages. N = 6 biological replicates. Error bars represent the s.e.m.; P < 0.0001 determined by one-way ANOVA. e, Representative images of Mcu−/− and WT macrophages immunostained for ASC and nuclei (DAPI). Cells were stimulated with zymosan for 3 h followed by nigericin (5 µM) for 1 h. f, Quantification of ASC specks, average number of specks counted per cell, for WT and Mcu−/− macrophages. N = 3 biological replicates. Error bars represent the s.e.m.; no significance was determined by the one-way ANOVA. g, Western blot analysis of cell lysates from WT and Mcu−/− macrophages stimulated with zymosan for 3 h followed by nigericin (5 µM) for 1 h. Cell lysates were immunoblotted for caspase-1 (p20), GSDMD and GAPDH. h, Western blot analysis of supernatants corresponding to samples shown in g. N = 1 representative replicate, from two independent experiments. Cell supernatants were immunoblotted for caspase-1 (p20), GSDMD and GAPDH.
Extended Data Fig. 8. Zymosan induced peritonitis in mice wherein Mcu is deleted selectively in myeloid cells (Mcu(M)−/− mice).
a. Percent weight change for wt and Mcu(M)−/− mice in a model of Zymosan Induced Peritonitis. N = 9–10 mice. b. Clinical Scores for wt and Mcu(M)−/− mice in a model of Zymosan Induced Peritonitis. N = 9–10 mice. Error bars represent SEM; p≤0.05(*) determined by the one-way ANOVA. c. ELISA determined serum cytokines in wt and Mcu(M)−/− mice, at 24 hours, in a model of Zymosan Induced Peritonitis. N = 5 mice. Error bars represent SEM; p<0.0001 according to Welch’s t-test, two-tailed. d. Peritoneal lavage cytokines at 24 hours. N = 4–5 mice. Error bars represent SEM of two independent experiments: p-values according to Welch’s t-test, two-tailed.
Diminished mitochondrial Ca2+ uptake increases inflammatory output
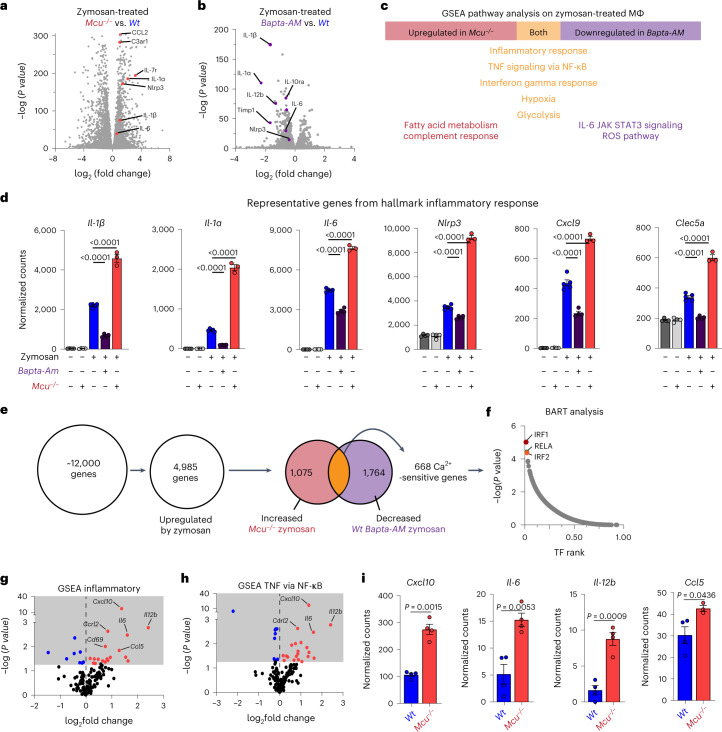
To develop a systems-level picture of how mCa2+ uptake affects the inflammatory response, we performed RNA-seq analysis on WT, Mcu−/− and BAPTA-AM loaded macrophages (all derived from young mice), before and after zymosan stimulation. In brief, the experiment was designed to reveal the Ca2+-sensitive genes that are dysregulated when mCa2+ uptake is diminished. Note that BAPTA-AM loading will affect all Ca2+-sensitive genes by ‘clamping’ intracellular Ca2+ elevations to near resting levels (<100 nM). We were especially interested in groups of genes that are relatively upregulated in Mcu−/− macrophages and downregulated in BAPTA-AM loaded cells. As expected, a volcano plot revealed that many inflammatory genes were significantly upregulated in zymosan-stimulated Mcu−/− macrophages when compared to their WT counterparts (Fig. 7a). Conversely, BAPTA-AM loading broadly decreased the expression of inflammatory gene transcription (Fig. 7b). GSEA pathway analysis revealed the key pathways that follow this pattern of regulation in macrophages, that is, upregulated when mCa2+ is diminished (cCa2+ signaling is enhanced) and downregulated when all Ca2+ signaling is prevented by BAPTA-AM (Fig. 7c). Genes involved in inflammatory responses and those involved in the overlapping TNF–NF-κB pathway showed this pattern most clearly. Using normalized counts, we showed significantly increased expression of Il1b, Il1a, Il6, Nlrp3, Cxcl9 and Clec5a when mCa2+ uptake was diminished during an inflammatory response to zymosan (Fig. 7d). In total, we identified 668 genes that are regulated by mCa2+ uptake in zymosan-stimulated macrophages (Fig. 7e). The analysis so far has focused on gene expression changes in response to a potent inflammatory stimulus (zymosan). We checked if abrogation of mCa2+ uptake in Mcu−/− macrophages upregulates inflammatory genes at baseline—without any overt exposure to an inflammatory stimulus. Surprisingly, although the expression levels were low in quiescent macrophages, we observed a clear upregulation of inflammatory response genes in unstimulated Mcu−/− macrophages (Fig. 7g,h). Similar to zymosan stimulation, GSEA pathway analysis revealed a significant enrichment of inflammatory pathways in Mcu−/− macrophages at baseline when compared to WT controls (Extended Data Fig. 9a,b). Within the inflammatory pathway genes, Cxcl10, Il6 and Il12b were significantly elevated (Fig. 7i). Together, these data show that diminished mCa2+ uptake drives low-grade inflammation in the absence of overt inflammatory stimuli and promotes a hyper-inflammatory response when the macrophages are exposed to inflammatory stimuli.
Fig. 7. RNA-seq analysis of Mcu−/− and BAPTA-AM-loaded BMDMs reveals transcripts sensitive to mCa2+ uptake.
a, Volcano plot showing increased expression of inflammatory genes in Mcu−/− BMDMs, compared to WT BMDMs, treated with zymosan for 3 h. Data normalization, dispersion estimates and model fitting (negative binomial) were carried out with the DESeq function (DESeq2 R package). Wald statistics were used for the significance tests. b, Volcano plot showing reduced expression of inflammatory genes in BAPTA-AM loaded BMDMs, when compared to unloaded BMDMs, treated with zymosan for 3 h. Data normalization, dispersion estimates and model fitting (negative binomial) were carried out with DESeq. Wald statistics were used for the significance tests. c, GSEA pathway analysis of Mcu−/−, BAPTA-AM loaded (WT) and unloaded WT BMDMs stimulated with zymosan for 3 h. MΦ, macrophage. d, Normalized counts for representative genes in the GSEA hallmark inflammatory response pathway. N = 3–5 biological replicates. Error bars represent the s.e.m.; P values were determined by one-way ANOVA. e, Schematic showing gene transcripts used for BART analysis. f, BART analysis of 668 mCa2+-sensitive genes identified in a. Transcription factor (TF) rank was plotted against the −log(P value) for each identified transcription factor. g, Volcano plot showing gene expression of the GSEA inflammatory response pathway in unstimulated Mcu−/− macrophages, compared to their WT counterparts. Data normalization, dispersion estimates and model fitting (negative binomial) were carried out with DESeq. Wald statistics were used for the significance tests. h, Volcano plot showing expression of genes of the GSEA TNF–NF-κB pathway in unstimulated Mcu−/− macrophages, compared to their WT counterparts. Data normalization, dispersion estimates and model fitting (negative binomial) were carried out with DESeq. Wald statistics were used for the significance tests. i, Normalized counts for representative genes in the GSEA hallmark inflammatory response pathway. N = 4 biological replicates. Error bars represent the s.e.m.; P value was determined by Welch’s t-test, two-tailed.
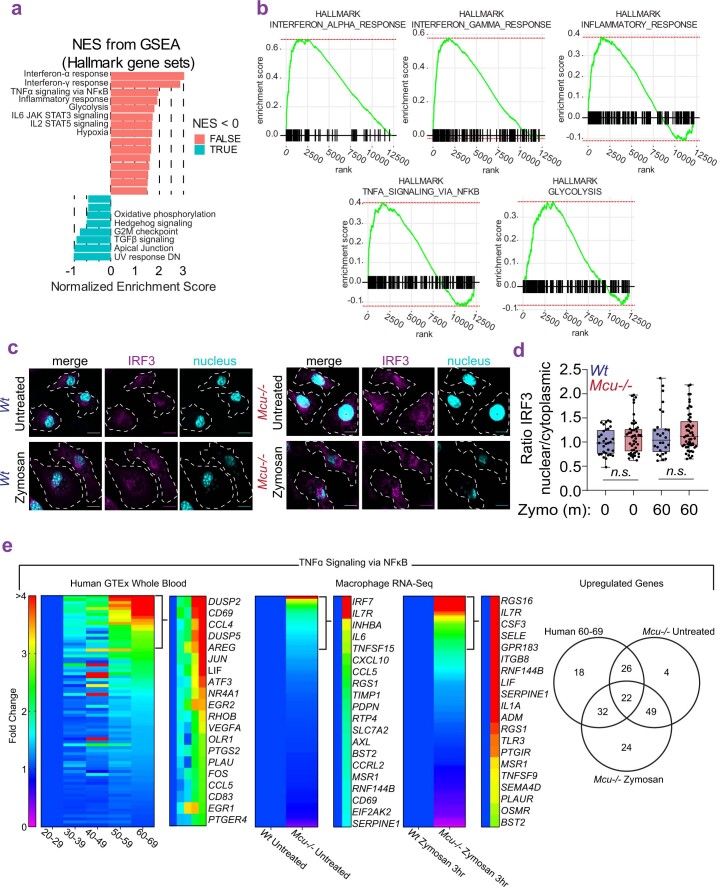
Extended Data Fig. 9. RNA-seq analysis of Mcu−/− macrophages and analysis of IRF3 translocation.
a. GSEA hallmark gene set enrichment analysis based on DSeq2 analysis of Mcu−/− versus wt BMDMs at baseline (untreated). b. Gene set enrichment analysis of GSEA pathways that are differentially expressed in Mcu−/− versus wt BMDMs at baseline (unstimulated). Enrichment scores (ES) are plotted on y-axis and genes ranked in ordered dataset are plotted in x-axis. c. Representative images from wt and Mcu−/− macrophages, untreated or stimulated with zymosan (30 min) and immunostained for IRF3 and nuclei (DAPI). Outline of cells was determined by bright field image. d. Quantified nuclear to cytoplasmic ratios of IRF3 fluorescence intensities in wt and Mcu−/− macrophages, unstimulated and zymosan-stimulated. N = 35–50 cells, 3 independent experiments. Box and whisker plot represents the min to max values for each data set. Line is at the median; p value calculated by one-way ANOVA test (found insignificant). e. Heatmaps show comparison of gene expression changes in the TNFα signaling via NFκB pathway from human and mice. Venn-diagram indicates similar genes upregulated in Human 60–69 compared to young Mcu−/− at baseline and following zymosan stimulation.
Analysis of Ca2+-sensitive inflammatory gene expression
We applied the binding analysis for regulation of transcription (BART) analysis69 to predict transcriptional regulators of the 668 mCa2+-sensitive genes we identified (Fig. 7e). This analysis complemented the ex vivo experiments by implicating the RelA family, which includes NF-κB, as being the responsible transcription factors (Fig. 7f). However, this analysis also suggested that transcription by interferon regulatory transcription factor (IRF) family proteins IRF1 and IRF3 is regulated by mCa2+ uptake; however, unlike NF-κB, we did not find any enhancement of IRF3 translocation in Mcu−/− cells (Extended Data Fig. 9c,d). It is, however, possible that Ca2+ signaling regulates an ancillary process of IRF3-mediated gene transcription. When we compare these datasets for similarities across species, we can identify 22 genes associated with inflammaging and reduced mCa2+ uptake in macrophages (Extended Data Fig. 9e).
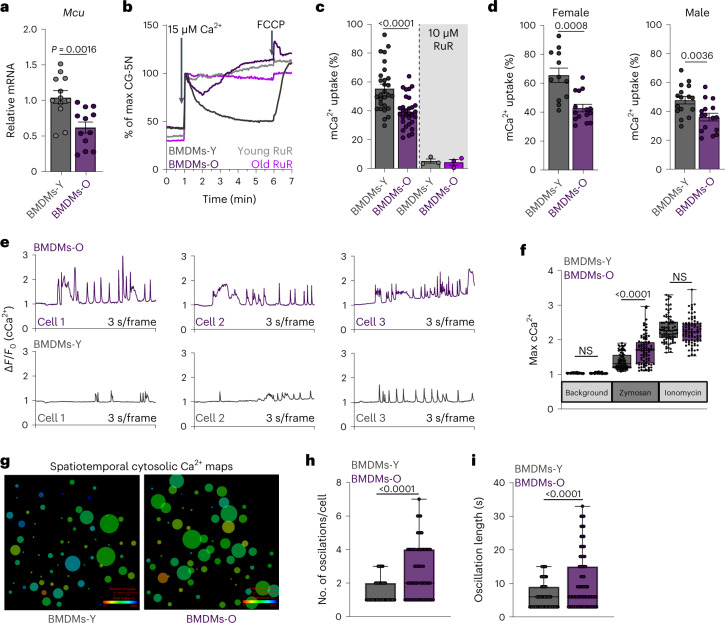
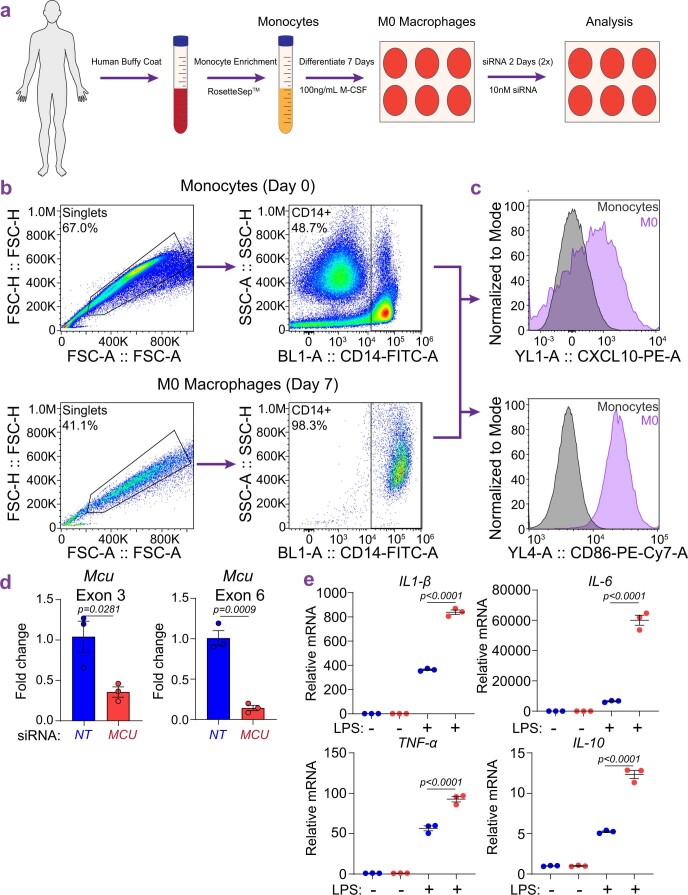
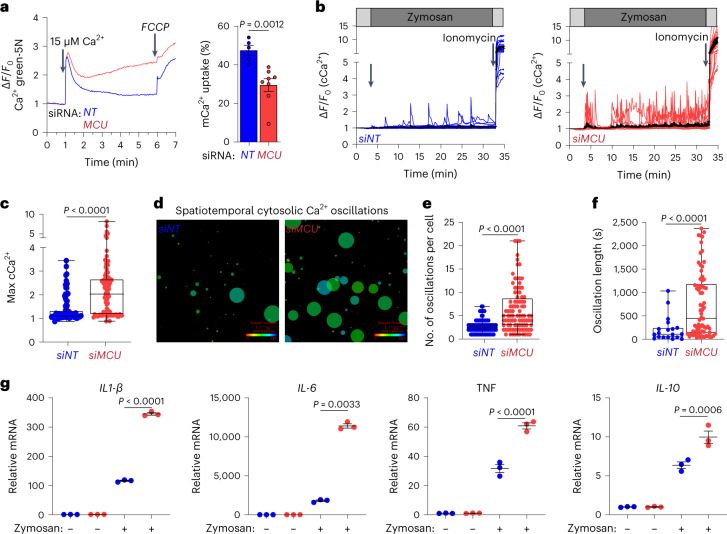
Mcu knockdown in human macrophages increases inflammatory output
As illustrated (Extended Data Fig. 10a), we differentiated human monocyte-derived macrophages (HMDMs) by first enriching the human monocytes from donor buffy coats and then culturing them for 7 d in growth medium supplemented with macrophage colony-stimulating factor. Flow cytometry analysis confirmed proper differentiation of the HMDMs. The HMDMs exhibited high-density staining of the macrophage markers CXCL10 and CD86, which were absent on undifferentiated monocytes on day 0 (Extended Data Fig. 10b,c). The short interfering RNA (siRNA)-mediated knockdown of MCU successfully reduced the mRNA levels of MCU, as measured by quantitative PCR with reverse transcription (RT–qPCR) analysis of MCU exon 3 and exon 6 (Extended Data Fig. 10d). Comparison of the mCa2+ uptake capacity clearly showed a robust uptake in HMDMs transfected with scrambled siRNA control (siNT-HMDMs) and a significantly diminished mCa2+ uptake in HMDMs transfected with MCU siRNA (siMCU-HMDMs; Fig. 8a). When stimulated with zymosan, the control siNT-HMDMs displayed Ca2+ oscillations throughout the 30 min of imaging. But similar to BMDMs-O and Mcu−/− BMDMs, the siMCU-HMDMs showed a significant increase in both the frequency and amplitude of the Ca2+ oscillations (Fig. 8b,c). The spatiotemporal analysis of the Ca2+ oscillations also revealed a similarity to mouse WT BMDMs-O and Mcu−/− BMDMs-Y. The siMCU-HMDMs exhibited significantly more Ca2+ spikes on an individual basis (Fig. 8d–f). Then, we checked the inflammatory response in siMCU-HMDMs and found that the expression levels of pro-inflammatory cytokines IL-1β, IL-6 and TNF were significantly higher when compared to siNT-HMDMs (Fig. 8g). Similar results were seen with LPS stimulation (Extended Data Fig. 10e). These results show that the sensitivity of the inflammatory response to mCa2+ uptake is conserved and can be demonstrated readily in human macrophages.
Extended Data Fig. 10. Validation of HMDMs and analysis of LPS response in HMDMs.
a. Schematic for isolation and differentiation of HMDMs from human buffy coats. b. Flow cytometry-based validation of enriched human monocytes and differentiated HMDMs. c. Upregulation of CXCL10 and CD86 in HMDMs after differentiation from monocytes. d. MCU mRNA levels in siNT and siMCU-transfected HMDMs. N = 3 biological replicates. Error bars represent SEM; p values determined by unpaired t-test. e. Fold changes in the gene expression of IL-1β, IL-6, TNFα, and IL-10 mRNA. N = 3 biological replicates. Error bars represent SEM; p-values determined by the one-way ANOVA.
Fig. 8. siRNA-mediated depletion of MCU in human monocyte-derived macrophages renders them hyper-sensitive to inflammatory stimuli.
a, Representative trace for a mCa2+ uptake in permeabilized siNT and siMCU-transfected HMDMs. Right, quantification of mCa2+ uptake. N = 5–8 biological replicates. Error bars represent the s.e.m.; P = 0.0012 determined by t-test. b, cCa2+ oscillations in siNT and siMCU-transfected HMDMs. ΔF/F0 values for Fura-2-AM loaded macrophages were plotted. Images were taken every 3 s. c, Maximum cCa2+. N = 88–98 cells, three independent experiments. Whiskers represent the minimum to maximum values for each dataset. The box represents the 75th and 25th percentiles. The line is the median; P < 0.0001 according to Welch’s t-test, two-tailed. d, CALIMA maps depicting spatiotemporal aspects of cCa2+ elevations. e, Oscillation frequency was determined for individual cells. N = 88–98 cells, three independent experiments. Whiskers represent the minimum to maximum values for each dataset. The box represents the 75th and 25th percentiles. The line is at the median; P < 0.0001 according to Welch’s t-test, two-tailed. f, Oscillation length was determined for individual cells. N = 88–98 cells, three independent experiments. Whiskers represent the minimum to maximum values for each dataset. The box represents the 75th and 25th percentiles. The line is the median; P < 0.0001 according to Welch’s t-test, two-tailed. g, Gene expression of IL-1β, IL-6, TNF and IL-10 mRNA. N = 3 biological replicates. Error bars represent the s.e.m.; P values were determined by one-way ANOVA.
Discussion
In this study, we report a surprising discovery that mCa2+ uptake capacity in macrophages drops significantly with age. This amplifies cCa2+ signaling and promotes NF-κB activation, rendering the macrophages prone to chronic low-grade inflammatory output at baseline and hyper-inflammatory when stimulated. Although mitochondrial dysfunction has long been a suspected driver of aging, our study pinpoints the MCU complex as a keystone molecular apparatus that links age-related changes in mitochondrial physiology to macrophage-mediated inflammation.
Gene expression analyses of human blood revealed clear signs of chronic age-associated inflammation, supporting the idea that blood transcriptomics can be used to monitor biomarkers of age-related low-grade inflammation. Both chronic low-grade inflammation and mitochondrial dysfunction are known hallmarks of aging, but mechanistic links between these two processes have not been defined with clear links to human biology70,71. For example, defective mitophagy in Prkn−/− mice may contribute to inflammaging by shedding mitochondrial DNA as an inflammatory stimulus in senescent cells71. Although a progressive age-associated decline in mitophagy is not evident in human myeloid cells, if one supposes that there is a steady age-associated shedding of inflammatory mediators from other senescent cells, our findings predict that the decreased mCa2+-uptake capacity will render the macrophages hyper-responsive to such inflammatory stimuli from senescent cells and thereby drive inflammaging. A recent study performed a comprehensive analysis of mitochondrial phenotypes in purified human cell types and mixtures but omitted mCa2+ uptake as a marker of mitochondrial fitness72. Interestingly, the authors found that their mitochondrial health index was most impaired in monocytes isolated from aged human donors. Although we chose to focus on macrophage-mediated inflammation, the broad outlines of the mechanistic model are likely applicable to other myeloid cells such as neutrophils and mast cells too, and that is an important line for our future investigations.
Whether macrophages deficient in mCa2+ uptake are hyper-inflammatory to all kinds of inflammatory stimuli is an outstanding question. For example, tissue-resident macrophages are constantly exposed to purinergic signals73 and our model predicts that in older mice and humans, the reduced Ca2+-buffering capacity of mitochondria will render the myeloid cells hyper-responsive to such purinergic signals. In addition to increased inflammation, a reduction in mCa2+ uptake also affects the ability of macrophages to phagocytose and kill pathogens, an immunological deficit known to be related to age. Analysis of genes that are especially sensitive to mCa2+ uptake points to the RelA family as the key transcription factors involved in this process. Consistently, we show that the nuclear translocation of NF-κB, which is central to the inflammatory response, is enhanced when mCa2+ uptake is diminished. Notably, the loss of mCa2+ uptake also results in hyperactivation of NFAT74, a transcription factor that is exquisitely sensitive to Ca2+ signaling. But in contrast to NFAT regulation, where Ca2+ is known to regulate NFAT nuclear translocation through the Ca2+-activated phosphatase calcineurin75,76, the precise mechanisms through which Ca2+ regulates NF-κB translocation are not entirely clear.
In a landmark study, Fieni et al. used direct patch-clamp recordings of mitoplasts to demonstrate that MCU current density varies greatly between tissues77. Remarkably, they found that MCU current densities in the cardiac mitoplasts from newborn mice were nearly five times larger than those found in the adult counterparts. In accordance with those findings, our analysis of the human gene expression data shows that expression of MCU in the heart reduces progressively with age. In addition to age-related changes in gene expression, other ancillary mechanisms, such as posttranslational modifications of the MCU complex, are likely to be very relevant to the overall regulation of mCa2+ uptake. Although we have clearly demonstrated that reduced mCa2+ uptake is an important component of this aging process, we cannot rule out other age-associated changes in the molecular machinery of Ca2+ signaling. For instance, we have evidence that ITPR3 expression increases with age. Interestingly, it was proposed recently that loss of Itpr2 leads to improved lifespan in mice55. Our future studies will focus on determining whether the ER–mitochondria contact sites in the macrophages are disrupted with age and on defining the regulatory mechanisms of the age-associated reduction in MCU transcription.
A major paradox in the field of mCa2+ signaling is that despite that its machinery is highly conserved in invertebrates and vertebrates78, and expressed ubiquitously in mammalian tissues, the deletion of Mcu, in the mixed background, yields smaller but viable mice79. These mice display moderate defects in skeletal muscle function79, but the overall phenotype is surprisingly mild for a process that is so well conserved and ubiquitous. The phenotype of global Mcu−/− mice is likely confounding in this respect because when a gene is deleted during embryogenesis, there is often a developmental compensation (not necessarily in the same molecular function). It is now becoming increasingly clear that a major role for mCa2+ signaling is tied to innate immune responses, the salience of which is largely masked in unchallenging conditions of a mouse vivarium. Recent studies establish that far from being a redundant Ca2+-buffering system, this molecular apparatus, centered on MCU and its regulatory subunits, has a profound role in host defense and inflammatory processes. Ironically, a steady age-associated erosion of its activities not only dampens the innate immune responses to fungal pathogens42, but also drives chronic low-grade inflammation. Interestingly, MCU-mutant flies show reduced lifespan80 but analyses of MCU-null hemocytes, the cells that constitute the Drosophila innate immune system, were not carried out. In mammals, tissue-resident macrophages occupy specialized niches in all organ systems. Age-associated decrease in the mCa2+-uptake capacity in these specialized tissue-resident macrophages may increase local inflammation and thereby have a major impact on organ physiology and homeostasis. An intriguing possibility is that resident macrophages of certain organ systems may be especially susceptible to such age-related changes. Our study sets the stage for many such research directions that may ultimately allow us to slow the onset and progression of many age-related diseases where chronic inflammation plays either a germinating or exacerbating role.
Methods
Mouse strains
Male and female mice aged 15 to 25 weeks (young) and 80–90 weeks (old) were used for all experiments. C57BL/6 mice we purchased from Jackson Laboratories (000664) within indicated age ranges. For WT and Mcu(M)−/− mouse experiments, mice aged 15–25 weeks were used. Mcu(M)−/− mice are reported previously42. The mouse experiments carried out in this study were reviewed and approved by the University of Virginia IACUC under the active protocol 3916.
Cell lines and cell culture
All cells were grown and maintained at 37 °C, 5% CO2. BMDMs were isolated and cultured as previously described81. In brief, bone marrow was extracted from mouse femur and tibia via centrifugation. The red blood cells were lysed with ACK lysis buffer and the remaining cells were counted and plated on petri dishes at a density of 2–4 × 106 cells per plate in BMDM Media (RPMI 1640 + 10% FBS + 20% L929-conditioned media). Cells were differentiated for 7 d and medium was replaced every 3 d. For experiments, BMDMs were used between days 9–14 after harvest.
GTEx and differential gene expression analysis
GTEx Analysis V8, gene counts and metadata were downloaded from the GTEx portal (https://gtexportal.org/)49 and analyzed using RStudio. Expression profile data were obtained for different tissues, binned into age groups and then subjected to differential gene expression analysis using DESeq2 (ref. 82) R package. PCA plots were generated using the plotPCA function. The differentially expressed genes were ranked based on the log2 fold change and FDR-corrected P values. The ranked list was then used to perform pathway analysis using GSEA software83. For the analysis of genes associated with mitochondrial functions, the differentially expressed genes were uploaded to mitoXplorer1.0 (ref. 50) for pathway analysis. Comparative plots were generated for specified pathways and the log2 fold change was plotted for individual genes.
Mitochondrial Ca2+ uptake in permeabilized macrophages
Ca2+ uptake assay was adapted for macrophages from Wettmarshausen et al.84 as reported in Seegren et al.42. In brief, cells were washed two times in D-PBS (without Ca2+ and Mg2+) and resuspended in ICM buffer containing 120 mM KCl, 5 mM NaCl, 1 mM MgCl2, 2 mM KH2PO4, 20 mM HEPES, 5 mM succinate, 5 mM malate, 5 mM glutamate, 500 nM thapsigargin and 0.1 µM calcium green-5N. Cells were immediately permeabilized with 35 µM digitonin for 5 min before recording on a FlexStation plate reader. Calcium green-5N fluorescence intensity was recorded every 2 s for the indicated time with injections of CaCl2 (concentration indicated in figure legend) and 10 µM FCCP at indicated times.
Cytosolic Ca2+ imaging using ratiometric Fura-2
Ratiometric imaging of macrophages using Fura-2-AM was as described previously by Seegren et al.42. In brief, macrophages were incubated for 30 min with gentle agitation at room temperature (RT) with 5 μM Fura-2-AM, 0.02% of pluronic acid and 500 μM probenecid in Ringer solution (155 mM NaCl, 4.5 mM KCl, 2 mM CaCl2, 1 mM MgCl2, 5 mM HEPES and 10 mM glucose, pH 7.4). Fura-2 emissions were collected at 510 nm and with 340/380 nm of excitation. Excitation was performed using a DG4 Illuminator (Sutter Instruments).
CALIMA analysis
Images acquired from cCa2+ imaging were uploaded into the CalciumImagingAnalyser from Radstake et al.53. Regions of interest were drawn manually over cells and processed for recorded cell activity. Spike detection parameters were set to the same values for each replicate and Excel sheets were exported for analysis in PRISM.
Bulk RNA-seq analysis
On average we received 30 million paired-end sequences for each of the replicates. RNA-seq libraries were checked for their quality using the fastqc program (http://www.bioinformatics.babraham.ac.uk/projects/fastqc/). The results from fastqc were aggregated using MultiQC software85. A program developed in-house was used for adaptor identification, and any contamination of adaptor sequence was removed with cutadapt (https://cutadapt.readthedocs.io/en/stable/). Reads were then mapped with the ‘splice aware’ aligner ‘STAR’86, to the transcriptome and genome of mm10 genome build. The HTseq software87 was used to count aligned reads that map onto each gene. The count table was imported to R to perform differential gene expression analysis using the DESeq2 package82. Lowly expressed genes (genes expressed only in a few replicates and had low counts) were excluded from the analysis before identifying differentially expressed genes. Data normalization, dispersion estimates and model fitting (negative binomial) were carried out with the DESeq function. The differentially expressed genes were ranked based on the log2fold change and FDR-corrected P values. The ranked file was used to perform pathway analysis using GSEA software83. The enriched pathways were selected based on enrichment scores as well as normalized enrichment scores.
Binding analysis for regulation of transcription
A gene list of 668 Ca2+-sensitive genes was uploaded into the BART web interface developed and maintained by the C. Zang laboratory at the University of Virginia69. The software identified the most likely transcription factors regulating the input genes. The area under the curve and P values were exported and plotted.
Immunoblotting
For analysis of caspase-1 and GSDMD
After treatment, the plates were centrifuged at 400g for 4 min and cell-free supernatants were collected. Cell lysates were prepared by directly adding 1× Laemmli sample buffer into the pellets and stored at −80 °C. At the day of electrophoresis, cell lysates were transferred into a 1.5-ml tube, sonicated and boiled at 95 °C for 5 min. Collected supernatants were cleared again by centrifugation at 400g for 5 min. Proteins in the supernatants were precipitated using 20% trichloroacetic acid, resuspended in 1× Laemmli sample buffer, and boiled at 95 °C for 5 min. Cell lysates and concentrated supernatants were run on a 12% homemade SDS–PAGE gel and transferred on to a 0.45-µm PVDF membrane (Millipore) using Towbin wet transfer buffer. After transfer, Ponceau S staining was performed to confirm equal loading of total proteins and the membrane was then blocked by 5% non-fat milk in TBST for 1 h at RT. Primary antibodies were diluted in TBST and incubated at 4 °C overnight. Horseradish peroxidase (HRP)-conjugated secondary antibodies were diluted in TBST at 1:10,000 and incubated for 1 h at RT. Membrane was developed by adding Luminata Forte Western HRP substrate (Millipore, WBLUF0100) and imaged on a Bio-Rad ChemiDoc Imager. Primary antibodies used were mouse anti-mCasp1(p20) (AdipoGen, Casper-1, 1:1,000 dilution) and rabbit anti-mGSDMD (Abcam, ab209845; 1:1,000 dilution). Secondary antibodies used were anti-mouse, HRP (Jackson, 115-035-003) and anti-rabbit, HRP (Jackson, 111-035-144).
Nuclear and cytoplasmic fractions
The Thermo Scientific NE-PER Nuclear Cytoplasmic Extraction Reagent kit was used to generate nuclear and cytosolic fractions from cells following zymosan stimulation. Briefly, cells underwent reagent-based lysis using cytoplasmic extraction reagents I & II followed by centrifugation for 5 min at 16,000g to separate nuclei from cytosolic fractions. The nuclei were then lysed using the nuclear extraction reagent and centrifuged for 5 min at 16,000g. The resulting supernatant contained the nuclear extract and was used for subsequent western blotting.
Native gel electrophoresis of MCU complex
The mitochondrial membrane proteins were extracted by incubating the isolated mitochondria with 1% digitonin on ice for 30 min. Samples were vortexed every few minutes. The mitochondrial extracts were then mixed at a 1:1 ratio with non-reducing sample loading buffer (62.5 mM Tris-HCl, pH 6.8, 40% (wt/vol) glycerol and 0.01% (wt/vol) bromophenol blue). Samples were resolved on 4–20% Mini-Protean TGX Stain-Free precast gels (Bio-Rad; 4568096) and run at 200 V for 5 h on ice. The gels were transferred onto a PVDF membrane using the Bio-Rad Turbo-blot system. Membranes were blocked with 5% milk for 30 min with gentle agitation before immunoblotting with primary antibody (α-MCU, clone D2Z3B, Cell Signaling 14997S and α-MICU1, clone D4P8Q, Cell Signaling 12524) in Signal Boost Immunoreaction Enhancer (Calbiochem, 407207-1KIT) at a 1:1,000 dilution. Staining with primary antibody was carried out overnight at 4 °C. Secondary anti-rabbit HRP was used in Signal Boost Immunoreaction enhancer for 2 h. The immunoblots were developed with SuperSignal West Pico PLUS Chemiluminescent Substrate (Thermo Fisher, 34580) 5 min before imaging.
qPCR
For all qPCR experiments, macrophages were plated at ~80% confluency into tissue culture-treated plates and rested overnight. For inflammatory gene expression, the following day, BMDMs were stimulated with Zymosan A BioParticles (Thermo Fisher, Z2849) at two particles per cell. For pharmacological pretreatments, on the day of experiment, BMDMs were treated with inhibitors for 30 min before the addition of zymosan, as described above. Inhibitor information and concentrations used were: BAPTA-AM (Thermo Fisher, B6769; 10 µM), ionomycin (Cayman Chemicals, 10004974; 1 µM), BTP2 (Sigma, 203890-M; 10 µM), zegocractin (MedChemExpress, HY-101942; 1 µM) and AZD7545 (MedChemExpress, HY-16082; 1 µM). For M1 versus M2 polarization, BMDMs were treated either with IFN-γ (R&D Systems, 485-MI-100/CF; 100 ng ml−1) and LPS (Invivogen, tlrl-eblps; 100 ng ml−1; to induce polarization toward a M1 phenotype) or with IL-4 (R&D Systems, 404-ML-010; 20 ng ml−1; to induce polarization toward a M2 phenotype). Total RNA was isolated from treated cells using RNeasy Plus Mini Kit. Following isolation, RNA concentration was determined using a NanoDrop 2000c spectrophotometer. RNA was converted to cDNA in a two-step reverse transcriptase process using the Promega Reverse Transcription Master Mix. Following cDNA synthesis, a Bio-Rad CFX Connect Real-Time system was used to perform qPCR reactions with SYBR Select Master Mix and 1 to 5 ng cDNA per well in a 96-well plate.
Immunofluorescence
Cells were plated overnight on coverslips before experiments. BMDMs were stimulated with Zymosan A BioParticles (Thermo Fisher, Z2849) at two particles per cell for indicated times. Following treatments, coverslips were washed 3× in PBS to remove loose/non-adherent cells. Coverslips were fixed in 4% paraformaldehyde and 4% sucrose (30 min, RT). Coverslips were washed 3× in wash buffer (PBS with 0.05% Tween-20), blocked and permeabilized at RT for 1 h in B/P buffer (1% BSA, 0.1% Triton X-100 and 0.05% Tween-20 in PBS), and then incubated with primary antibody diluted in B/P buffer overnight at 4 °C. Coverslips were washed 3× in wash buffer, and incubated at RT with the appropriate secondary antibody in B/P buffer for 2 h, followed by 3× washes in wash buffer. Coverslips were mounted on glass slides (ProLong Gold Antifade; Thermo Fisher, P36930), stored in a desiccation box at 4 °C until imaging. Confocal microscopy was performed on a Zeiss LSM 880. Data were acquired with Zen Black and analyzed using ImageJ. Antibodies used for immunofluorescence were: anti-ASC/TMS1/PYCARD antibody (F-9): sc-271054, Santa Cruz; anti-NF-κB p65 (D14E12) XP rabbit monoclonal antibody 8242, Cell Signaling; anti-IRF-3 (D83B9) rabbit monoclonal antibody 4302, Cell Signaling.
Mitogenie
To analyze mitochondrial morphology and other characteristics, images were cropped into individual cells and processed using a mitochondrial analysis workflow developed by the Kashatus laboratory52. Images were first input into the MitoCatcher application on the Mitogenie platform, generating binarized images of segmented mitochondrial networks. The MiA application on Mitogenie was used to analyze the images of the mitochondrial networks and produce quantitative measurements describing mitochondrial morphology.
LDH assay
BMDMs were incubated for 3 h with LPS (Invivogen, tlrl-eblps; 100 ng ml−1) or Zymosan A BioParticles (Thermo Fisher, Z2849; two particles per cell) at 37 °C and 5% CO2. After 3 h, cells were washed 3× with HBSS, resuspended in Ringer solution (155 mM NaCl, 4.5 mM KCl, 2 mM CaCl2, 1 mM MgCl2, 5 mM HEPES and 10 mM glucose, pH 7.4) with or without nigericin (Invivogen, tlrl-nig; 5 µM). After 24 h, LDH was measured in the supernatants using Pierce LDH Cytotoxicity Assay Kit (Thermo Fisher Scientific) according to the manufacturer’s instructions.
IL-1β ELISA
BMDMs were incubated for 3 h with LPS (Invivogen, tlrl-eblps; 100 ng ml−1) or Zymosan A BioParticles (Thermo Fisher, Z2849; two particles per cell) at 37 °C, 5% CO2. After 3 h, cells were washed 3× with HBSS, resuspended in Ringer solution (155 mM NaCl, 4.5 mM KCl, 2 mM CaCl2, 1 mM MgCl2, 5 mM HEPES, 10 mM glucose, pH 7.4) with or without nigericin (Invivogen, tlrl-nig; 5 µM). After 24 h, IL-1β was measured in the supernatants using ELISA MAX Standard Mouse IL-1β (BioLegend) according to the manufacturer’s instructions.
Zymosan-induced peritonitis
Mcu(M)−/− and WT mice were subjected to a model of zymosan-induced peritonitis88. In brief, mice were intraperitoneally injected with 55 mg per kg body weight Zymosan A and monitored for 24 h for clinical scores of conjunctivitis, lethargy, changes in hair coat and grimace pain to indicate symptoms of illness. Weight was monitored every 2 h and scoring was performed by a blinded member of the laboratory. Following 24 h, mice were euthanized. Blood and peritoneal lavage fluid were collected for Luminex analysis and cytokine detection.
Differentiation of human monocyte-derived macrophages
Human monocytes were isolated from healthy donor buffy coats procured from the American Red Cross Biomedical Services (ARCBS), with consent from the volunteer donors for whole-blood collection and its use for research (Leukpacks/Whole Blood Clinical Study Protocol LP-2). The distribution of buffy coats to the laboratory of B.N.D. at University of Virginia was also reviewed and approved by the ARCBS Institutional Review Board under the active protocol 2016-030. Differentiation of HMDMs was performed using PromoCell, Serum-free and Zeno-free cell culture method. In brief, buffy coats were enriched for monocytes using RosetteSep Human Monocyte Enrichment Cocktail. Enriched monocytes were plated on six-well plates in monocyte attachment medium for 1 h in a 5% CO2 and 37 °C incubator. Cells were washed three times with vigorous swirling in warm monocyte attachment medium to remove non-adherent cells. Cells were cultured for 7 d in Macrophage Generation Medium DXF with supplement mix to generate HMDMs. The siRNA knockdown of MCU was performed two times over 48 h using Lipofectamine 3000 with 10 nM siRNA. Antibodies used for flow cytometry were: FITC anti-human CD14 antibody, BioLegend 325603; PE/Cyanine7 anti-human CD86 Antibody, BioLegend 305421; and PE anti-human CXCL10 (IP-10) antibody, BioLegend 519503. Flow cytometry was performed on an Attune NxT with Attune NxT Software (v2.0+).
Statistics and reproducibility
All data were analyzed using Excel (Microsoft) and Prism 8 (GraphPad) software. All datasets were subjected to ROUT outlier test and the data points with Q < 1% were considered outliers and removed. In bar graphs, data are presented as means with error bars reflecting the s.e.m. or as indicated in figure legends. Statistical significance (P < 0.05) was computed using one-way ANOVA, two-way ANOVA and Welch’s t-test (two-tailed), as indicated in figure legends. The sample size and representation of ‘n’ (mice, experimental repeats or cells) is indicated in figure legends. Sample size was determined by using GPower3.l software. For all other experiments (ex vivo and in vivo), no power analysis was used for sample sizes and replicates, but they were determined based on experimental experience. In the box plots, the whiskers represent minimum and maximum values, the box represents the 75th and 25th percentiles and the horizontal line is the median. For zymosan-induced peritonitis, clinical scores were collected by laboratory personnel who were blinded to the genotype/condition of individual mice. All other experiments were not blinded but contained appropriate biological replication. The order of data collection was changed between experiments to avoid collection bias (for example, if the experiment was run as control, WT and then knockout for one experiment, the following experiment data was collected as knockout, WT and then control).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Unprocessed blots and primer information.
Acknowledgements
We thank the members of the laboratory of B.N.D. for their scientific insights and feedback. We thank the following core facilities for their technical resources and support: UVA Flow Cytometry Core, Carter Immunology Center Flow Cytometry Core, Advanced Microscopy Facility Core (UVA) and the UVA Research Histology Core. The work was funded with the following National Institutes of Health research grants: AI155808 (to B.N.D.), GM108989 (to B.N.D.), Owens Family Foundation (to B.N.D.), GM138381 (to S.E.E.), P30 CA044579 (to P.K.) and T32 GM007055-46 (to P.V.S.).
Extended data
Source data
Author contributions
Conception: P.V.S. and B.N.D.; Research design: P.V.S. and B.N.D.; Investigation: P.V.S., T.K.D., M.E.S., X.-Y.Z., S.B.V., L.H., R.J.O. and S.E.E.; Data analysis: P.V.S., M.E.S., S.B.V., L.H., X.-Y.Z. and P.K.; Resource assistance: G.W.B., J.K., P.K. and S.E.E.; Writing—draft and editing: P.V.S., T.K.D. and B.N.D.; Project administration: B.N.D.
Peer review
Peer review information
Nature Aging thanks Tito Calì and the other, anonymous, reviewer(s) for the contribution to the peer review of this work.
Data availability
The RNA-seq data are deposited in the publicly available Gene Expression Omnibus database under accession GSE228873. Source data are available with this paper. All other data are available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
is available for this paper at 10.1038/s43587-023-00436-8.
Supplementary information
The online version contains supplementary material available at 10.1038/s43587-023-00436-8.
References
- 1.Franceschi C, Garagnani P, Parini P, Giuliani C, Santoro A. Inflammaging: a new immune-metabolic viewpoint for age-related diseases. Nat. Rev. Endocrinol. 2018;14:576–590. doi: 10.1038/s41574-018-0059-4. [DOI] [PubMed] [Google Scholar]
- 2.Lopez-Otin C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153:1194–1217. doi: 10.1016/j.cell.2013.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leng S, Chaves P, Koenig K, Walston J. Serum interleukin-6 and hemoglobin as physiological correlates in the geriatric syndrome of frailty: a pilot study. J. Am. Geriatr. Soc. 2002;50:1268–1271. doi: 10.1046/j.1532-5415.2002.50315.x. [DOI] [PubMed] [Google Scholar]
- 4.Bruunsgaard H, Pedersen BK. Age-related inflammatory cytokines and disease. Immunol. Allergy Clin. North Am. 2003;23:15–39. doi: 10.1016/s0889-8561(02)00056-5. [DOI] [PubMed] [Google Scholar]
- 5.Ferrucci L, et al. The origins of age-related proinflammatory state. Blood. 2005;105:2294–2299. doi: 10.1182/blood-2004-07-2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dinarello CA. Interleukin 1 and interleukin 18 as mediators of inflammation and the aging process. Am. J. Clin. Nutr. 2006;83:447S–455S. doi: 10.1093/ajcn/83.2.447S. [DOI] [PubMed] [Google Scholar]
- 7.van Deursen JM. The role of senescent cells in ageing. Nature. 2014;509:439–446. doi: 10.1038/nature13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuilman T, et al. Oncogene-induced senescence relayed by an interleukin-dependent inflammatory network. Cell. 2008;133:1019–1031. doi: 10.1016/j.cell.2008.03.039. [DOI] [PubMed] [Google Scholar]
- 9.Kuilman T, Peeper DS. Senescence-messaging secretome: SMS-ing cellular stress. Nat. Rev. Cancer. 2009;9:81–94. doi: 10.1038/nrc2560. [DOI] [PubMed] [Google Scholar]
- 10.Okabe Y, Medzhitov R. Tissue biology perspective on macrophages. Nat. Immunol. 2016;17:9–17. doi: 10.1038/ni.3320. [DOI] [PubMed] [Google Scholar]
- 11.van Beek AA, Van den Bossche J, Mastroberardino PG, de Winther MPJ, Leenen PJM. Metabolic alterations in aging macrophages: ingredients for inflammaging? Trends Immunol. 2019;40:113–127. doi: 10.1016/j.it.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Nobs SP, Kopf M. Tissue-resident macrophages: guardians of organ homeostasis. Trends Immunol. 2021;42:495–507. doi: 10.1016/j.it.2021.04.007. [DOI] [PubMed] [Google Scholar]
- 13.Hayden MS, Ghosh S. Shared principles in NF-κB signaling. Cell. 2008;132:344–362. doi: 10.1016/j.cell.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 14.Zhang Q, Lenardo MJ, Baltimore D. 30 Years of NF-κB: a blossoming of relevance to human pathobiology. Cell. 2017;168:37–57. doi: 10.1016/j.cell.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adler AS, et al. Motif module map reveals enforcement of aging by continual NF-κB activity. Genes Dev. 2007;21:3244–3257. doi: 10.1101/gad.1588507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Donato AJ, Black AD, Jablonski KL, Gano LB, Seals DR. Aging is associated with greater nuclear NF kappa B, reduced I kappa B alpha, and increased expression of proinflammatory cytokines in vascular endothelial cells of healthy humans. Aging Cell. 2008;7:805–812. doi: 10.1111/j.1474-9726.2008.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Osorio FG, et al. Nuclear lamina defects cause ATM-dependent NF-κB activation and link accelerated aging to a systemic inflammatory response. Genes Dev. 2012;26:2311–2324. doi: 10.1101/gad.197954.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y, et al. NF-κB signaling in skin aging. Mech. Ageing Dev. 2019;184:111160. doi: 10.1016/j.mad.2019.111160. [DOI] [PubMed] [Google Scholar]
- 19.Dolmetsch RE, Lewis RS, Goodnow CC, Healy JI. Differential activation of transcription factors induced by Ca2+ response amplitude and duration. Nature. 1997;386:855–858. doi: 10.1038/386855a0. [DOI] [PubMed] [Google Scholar]
- 20.Dolmetsch RE, Xu K, Lewis RS. Calcium oscillations increase the efficiency and specificity of gene expression. Nature. 1998;392:933–936. doi: 10.1038/31960. [DOI] [PubMed] [Google Scholar]
- 21.Berry CT, et al. BCR-induced Ca2+ signals dynamically tune survival, metabolic reprogramming, and proliferation of naive B cells. Cell Rep. 2020;31:107474. doi: 10.1016/j.celrep.2020.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berry CT, May MJ, Freedman BD. Analysis of calcium control of canonical NF-κB signaling in B lymphocytes. Methods Mol. Biol. 2021;2366:145–164. doi: 10.1007/978-1-0716-1669-7_9. [DOI] [PubMed] [Google Scholar]
- 23.Clapham DE. Calcium signaling. Cell. 2007;131:1047–1058. doi: 10.1016/j.cell.2007.11.028. [DOI] [PubMed] [Google Scholar]
- 24.Kirichok Y, Krapivinsky G, Clapham DE. The mitochondrial calcium uniporter is a highly selective ion channel. Nature. 2004;427:360–364. doi: 10.1038/nature02246. [DOI] [PubMed] [Google Scholar]
- 25.Baughman JM, et al. Integrative genomics identifies MCU as an essential component of the mitochondrial calcium uniporter. Nature. 2011;476:341–345. doi: 10.1038/nature10234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Stefani D, Raffaello A, Teardo E, Szabo I, Rizzuto R. A forty-kilodalton protein of the inner membrane is the mitochondrial calcium uniporter. Nature. 2011;476:336–340. doi: 10.1038/nature10230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chaudhuri D, Sancak Y, Mootha VK, Clapham DE. MCU encodes the pore conducting mitochondrial calcium currents. Elife. 2013;2:e00704. doi: 10.7554/eLife.00704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sancak Y, et al. EMRE is an essential component of the mitochondrial calcium uniporter complex. Science. 2013;342:1379–1382. doi: 10.1126/science.1242993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kamer KJ, Mootha VK. The molecular era of the mitochondrial calcium uniporter. Nat. Rev. Mol. Cell Biol. 2015;16:545–553. doi: 10.1038/nrm4039. [DOI] [PubMed] [Google Scholar]
- 30.Oxenoid K, et al. Architecture of the mitochondrial calcium uniporter. Nature. 2016;533:269–273. doi: 10.1038/nature17656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garg V, Kirichok YY. Patch-clamp analysis of the mitochondrial calcium uniporter. Methods Mol. Biol. 2019;1925:75–86. doi: 10.1007/978-1-4939-9018-4_7. [DOI] [PubMed] [Google Scholar]
- 32.Perocchi F, et al. MICU1 encodes a mitochondrial EF hand protein required for Ca2+ uptake. Nature. 2010;467:291–296. doi: 10.1038/nature09358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Csordas G, et al. MICU1 controls both the threshold and cooperative activation of the mitochondrial Ca2+ uniporter. Cell Metab. 2013;17:976–987. doi: 10.1016/j.cmet.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Plovanich M, et al. MICU2, a paralog of MICU1, resides within the mitochondrial uniporter complex to regulate calcium handling. PLoS ONE. 2013;8:e55785. doi: 10.1371/journal.pone.0055785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fan M, et al. Structure and mechanism of the mitochondrial Ca2+ uniporter holocomplex. Nature. 2020;582:129–133. doi: 10.1038/s41586-020-2309-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang, C., Jacewicz, A., Delgado, B. D., Baradaran, R. & Long, S. B. Structures reveal gatekeeping of the mitochondrial Ca2+ uniporter by MICU1-MICU2. Elife10.7554/eLife.59991 (2020). [DOI] [PMC free article] [PubMed]
- 37.Wang, Y. et al. Structural insights into the Ca2+-dependent gating of the human mitochondrial calcium uniporter. Elife10.7554/eLife.60513 (2020). [DOI] [PMC free article] [PubMed]
- 38.Wu W, et al. The structure of the MICU1–MICU2 complex unveils the regulation of the mitochondrial calcium uniporter. EMBO J. 2020;39:e104285. doi: 10.15252/embj.2019104285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duchen MR. Mitochondria and calcium: from cell signalling to cell death. J. Physiol. 2000;529:57–68. doi: 10.1111/j.1469-7793.2000.00057.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rizzuto R, De Stefani D, Raffaello A, Mammucari C. Mitochondria as sensors and regulators of calcium signalling. Nat. Rev. Mol. Cell Biol. 2012;13:566–578. doi: 10.1038/nrm3412. [DOI] [PubMed] [Google Scholar]
- 41.Feske S, Wulff H, Skolnik EY. Ion channels in innate and adaptive immunity. Annu. Rev. Immunol. 2015;33:291–353. doi: 10.1146/annurev-immunol-032414-112212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Seegren PV, et al. Mitochondrial Ca2+ signaling is an electrometabolic switch to fuel phagosome killing. Cell Rep. 2020;33:108411. doi: 10.1016/j.celrep.2020.108411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Feno S, et al. The dominant-negative mitochondrial calcium uniporter subunit MCUb drives macrophage polarization during skeletal muscle regeneration. Sci. Signal. 2021;14:eabf3838. doi: 10.1126/scisignal.abf3838. [DOI] [PubMed] [Google Scholar]
- 44.Tedesco, S. et al. Mitochondrial calcium uptake is instrumental to alternative macrophage polarization and phagocytic activity. Int. J. Mol. Sci.10.3390/ijms20194966 (2019). [DOI] [PMC free article] [PubMed]
- 45.Li T, et al. Listeria monocytogenes upregulates mitochondrial calcium signalling to inhibit LC3-associated phagocytosis as a survival strategy. Nat. Microbiol. 2021;6:366–379. doi: 10.1038/s41564-020-00843-2. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 46.Sebag SC, et al. Inhibition of the mitochondrial calcium uniporter prevents IL-13 and allergen-mediated airway epithelial apoptosis and loss of barrier function. Exp. Cell. Res. 2018;362:400–411. doi: 10.1016/j.yexcr.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gu L, et al. Mitochondrial calcium uniporter regulates PGC-1α expression to mediate metabolic reprogramming in pulmonary fibrosis. Redox Biol. 2019;26:101307. doi: 10.1016/j.redox.2019.101307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rimessi A, et al. Pharmacological modulation of mitochondrial calcium uniporter controls lung inflammation in cystic fibrosis. Sci. Adv. 2020;6:eaax9093. doi: 10.1126/sciadv.aax9093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Consortium GT. The Genotype-Tissue Expression (GTEx) project. Nat. Genet. 2013;45:580–585. doi: 10.1038/ng.2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yim A, et al. mitoXplorer, a visual data mining platform to systematically analyze and visualize mitochondrial expression dynamics and mutations. Nucleic Acids Res. 2020;48:605–632. doi: 10.1093/nar/gkz1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Garg, V. et al. The mechanism of MICU-dependent gating of the mitochondrial Ca2+ uniporter. Elife10.7554/eLife.69312 (2021). [DOI] [PMC free article] [PubMed]
- 52.Rohani A, Kashatus JA, Sessions DT, Sharmin S, Kashatus DF. Mito Hacker: a set of tools to enable high-throughput analysis of mitochondrial network morphology. Sci. Rep. 2020;10:18941. doi: 10.1038/s41598-020-75899-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Radstake FDW, Raaijmakers EAL, Luttge R, Zinger S, Frimat JP. CALIMA: the semi-automated open-source calcium imaging analyzer. Comput. Methods Programs Biomed. 2019;179:104991. doi: 10.1016/j.cmpb.2019.104991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Spychala MS, et al. Age-related changes in the gut microbiota influence systemic inflammation and stroke outcome. Ann. Neurol. 2018;84:23–36. doi: 10.1002/ana.25250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ziegler DV, et al. Calcium channel ITPR2 and mitochondria-ER contacts promote cellular senescence and aging. Nat. Commun. 2021;12:720. doi: 10.1038/s41467-021-20993-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rizzuto R, Simpson AW, Brini M, Pozzan T. Rapid changes of mitochondrial Ca2+ revealed by specifically targeted recombinant aequorin. Nature. 1992;358:325–327. doi: 10.1038/358325a0. [DOI] [PubMed] [Google Scholar]
- 57.Lee BY, et al. Senescence-associated beta-galactosidase is lysosomal beta-galactosidase. Aging Cell. 2006;5:187–195. doi: 10.1111/j.1474-9726.2006.00199.x. [DOI] [PubMed] [Google Scholar]
- 58.Coppe JP, Desprez PY, Krtolica A, Campisi J. The senescence-associated secretory phenotype: the dark side of tumor suppression. Annu. Rev. Pathol. 2010;5:99–118. doi: 10.1146/annurev-pathol-121808-102144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brough D, et al. Ca2+ stores and Ca2+ entry differentially contribute to the release of IL-1 beta and IL-1 alpha from murine macrophages. J. Immunol. 2003;170:3029–3036. doi: 10.4049/jimmunol.170.6.3029. [DOI] [PubMed] [Google Scholar]
- 60.Denton RM. Regulation of mitochondrial dehydrogenases by calcium ions. Biochim. Biophys. Acta. 2009;1787:1309–1316. doi: 10.1016/j.bbabio.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 61.Turkan A, Hiromasa Y, Roche TE. Formation of a complex of the catalytic subunit of pyruvate dehydrogenase phosphatase isoform 1 (PDP1c) and the L2 domain forms a Ca2+ binding site and captures PDP1c as a monomer. Biochemistry. 2004;43:15073–15085. doi: 10.1021/bi048901y. [DOI] [PubMed] [Google Scholar]
- 62.Gherardi G, et al. Loss of mitochondrial calcium uniporter rewires skeletal muscle metabolism and substrate preference. Cell Death Differ. 2019;26:362–381. doi: 10.1038/s41418-018-0191-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Srimathi T, et al. Mapping of POP1-binding site on pyrin domain of ASC. J. Biol. Chem. 2008;283:15390–15398. doi: 10.1074/jbc.M801589200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hara H, et al. Phosphorylation of the adaptor ASC acts as a molecular switch that controls the formation of speck-like aggregates and inflammasome activity. Nat. Immunol. 2013;14:1247–1255. doi: 10.1038/ni.2749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shi J, et al. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature. 2015;526:660–665. doi: 10.1038/nature15514. [DOI] [PubMed] [Google Scholar]
- 66.Kofoed EM, Vance RE. Innate immune recognition of bacterial ligands by NAIPs determines inflammasome specificity. Nature. 2011;477:592–595. doi: 10.1038/nature10394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fink SL, Cookson BT. Caspase-1-dependent pore formation during pyroptosis leads to osmotic lysis of infected host macrophages. Cell Microbiol. 2006;8:1812–1825. doi: 10.1111/j.1462-5822.2006.00751.x. [DOI] [PubMed] [Google Scholar]
- 68.Kankkunen P, et al. (1,3)-beta-glucans activate both dectin-1 and NLRP3 inflammasome in human macrophages. J. Immunol. 2010;184:6335–6342. doi: 10.4049/jimmunol.0903019. [DOI] [PubMed] [Google Scholar]
- 69.Wang Z, et al. BART: a transcription factor prediction tool with query gene sets or epigenomic profiles. Bioinformatics. 2018;34:2867–2869. doi: 10.1093/bioinformatics/bty194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhang, H., Menzies, K. J. & Auwerx, J. The role of mitochondria in stem cell fate and aging. Development10.1242/dev.143420 (2018). [DOI] [PMC free article] [PubMed]
- 71.Sliter DA, et al. Parkin and PINK1 mitigate STING-induced inflammation. Nature. 2018;561:258–262. doi: 10.1038/s41586-018-0448-9. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 72.Rausser, S. et al. Mitochondrial phenotypes in purified human immune cell subtypes and cell mixtures. Elife10.7554/eLife.70899 (2021). [DOI] [PMC free article] [PubMed]
- 73.Desai BN, Leitinger N. Purinergic and calcium signaling in macrophage function and plasticity. Front. Immunol. 2014;5:580. doi: 10.3389/fimmu.2014.00580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yoast RE, et al. The mitochondrial Ca2+ uniporter is a central regulator of interorganellar Ca2+ transfer and NFAT activation. J. Biol. Chem. 2021;297:101174. doi: 10.1016/j.jbc.2021.101174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Muller MR, Rao A. NFAT, immunity and cancer: a transcription factor comes of age. Nat. Rev. Immunol. 2010;10:645–656. doi: 10.1038/nri2818. [DOI] [PubMed] [Google Scholar]
- 76.Li H, Rao A, Hogan PG. Interaction of calcineurin with substrates and targeting proteins. Trends Cell Biol. 2011;21:91–103. doi: 10.1016/j.tcb.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fieni F, Lee SB, Jan YN, Kirichok Y. Activity of the mitochondrial calcium uniporter varies greatly between tissues. Nat. Commun. 2012;3:1317. doi: 10.1038/ncomms2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bick AG, Calvo SE, Mootha VK. Evolutionary diversity of the mitochondrial calcium uniporter. Science. 2012;336:886. doi: 10.1126/science.1214977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pan X, et al. The physiological role of mitochondrial calcium revealed by mice lacking the mitochondrial calcium uniporter. Nat. Cell Biol. 2013;15:1464–1472. doi: 10.1038/ncb2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tufi R, et al. Comprehensive genetic characterization of mitochondrial Ca2+ uniporter components reveals their different physiological requirements in vivo. Cell Rep. 2019;27:1541–1550. doi: 10.1016/j.celrep.2019.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Schappe MS, et al. Chanzyme TRPM7 mediates the Ca2+ influx essential for lipopolysaccharide-induced Toll-like receptor 4 endocytosis and macrophage activation. Immunity. 2018;48:59–74. doi: 10.1016/j.immuni.2017.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15:550. doi: 10.1186/s13059-014-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Subramanian A, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA. 2005;102:15545–15550. doi: 10.1073/pnas.0506580102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wettmarshausen J, et al. MICU1 confers protection from MCU-dependent manganese toxicity. Cell Rep. 2018;25:1425–1435. doi: 10.1016/j.celrep.2018.10.037. [DOI] [PubMed] [Google Scholar]
- 85.Ewels P, Magnusson M, Lundin S, Kaller M. MultiQC: summarize analysis results for multiple tools and samples in a single report. Bioinformatics. 2016;32:3047–3048. doi: 10.1093/bioinformatics/btw354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dobin A, et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics. 2013;29:15–21. doi: 10.1093/bioinformatics/bts635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Anders S, Pyl PT, Huber W. HTSeq—a Python framework to work with high-throughput sequencing data. Bioinformatics. 2015;31:166–169. doi: 10.1093/bioinformatics/btu638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cash JL, White GE, Greaves DR. Zymosan-induced peritonitis as a simple experimental system for the study of inflammation. Methods Enzymol. 2009;461:379–396. doi: 10.1016/S0076-6879(09)05417-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Unprocessed blots and primer information.
Data Availability Statement
The RNA-seq data are deposited in the publicly available Gene Expression Omnibus database under accession GSE228873. Source data are available with this paper. All other data are available from the corresponding author upon reasonable request.