Abstract
Evidence has not been established to support that combination chemotherapy with cyclophosphamide, vincristine, and dacarbazine (CVD) improves survival in patients with malignant pheochromocytoma and paraganglioma (M-PPGL). To investigate the efficacy of CVD for this disease, we retrospectively analyzed data of 23 patients with metastatic and unresectable M-PPGL (mean age, 41.7 ± 15.4 years) who received at least 2 cycles of this regimen. The follow-up period after initiation of CVD ranged from 0.3 to 13.7 years, with a median of 3.3 years. CVD therapy achieved a complete tumor response (CR) in 1 patient (4%), a partial response (PR) in 5 (22%), stable disease (SD) in 5 (22%), and progressive disease (PD) in 13 (52%), respectively. All of the responders (CR and PR) but 6% of the non-responders (SD and PD) showed substantial biochemical improvement. The progression-free survival period in the responders was significantly longer than in the non-responders (p < 0.01). Although the overall survival and survival after the diagnosis of M-PPGL were longer in the responders than the non-responders, the difference was not statistically significant (p = 0.08). The progression-free and overall survival period were significantly longer in the non-progression group (CR, PR, and SD) than in the progression group (PD) (1.7 ± 3.3 vs. 0.3 ± 0.3 years, p < 0.01, and 4.6 ± 3.6 vs. 2.0 ± 3.7 years, p = 0.01, respectively). It is therefore suggested that CVD chemotherapy could be useful in controlling tumor progression and improving survival in patients with metastatic and progressive M-PPGL.
Electronic supplementary material
The online version of this article (doi:10.1007/s12672-017-0284-7) contains supplementary material, which is available to authorized users.
Keywords: Antineoplastic combined chemotherapy, CVD therapy, Malignant pheochromocytoma, Paraganglioma, Survival time, Myelodysplastic syndromes
Introduction
Pheochromocytoma and paraganglioma are neuroendocrine tumors arising from chromaffin tissues. Approximately 5–10% of pheochromocytomas metastasize, as compared to 30–40% of non-head/neck paragangliomas [1], and the 5-year survival rate of malignant pheochromocytoma/paraganglioma (M-PPGL) has been reported as less than 50% [2].
There is currently no “gold standard” algorithm for the optimal management of M-PPGL. Surgical excision plus metastasectomy is the only curative option; however, curative resection is usually not possible. Further, although a recent meta-analysis on the effects of 131I-metaiodobenzylguanidine (MIBG) therapy on M-PPGL suggested that stable disease (SD) in terms of the tumor volume and a partial hormonal response were achieved in over 50 and 40% of patients, respectively [3], studies regarding the availability and appropriate administration dose of this therapy are limited in Japan.
Combination chemotherapy with cyclophosphamide, vincristine, and dacarbazine (CVD) for the treatment of metastatic M-PPGL was first introduced in 1985 [4]. CVD as first-line therapy is indicated for patients with rapidly progressive tumors and/or symptomatic disease and adequate performance status [5]. Since then, there have been several studies of CVD for patients with inoperable M-PPGL, most of which were retrospective [6–8]. These studies clearly showed that CVD chemotherapy ameliorated the surrogate outcomes such as tumor volume or hormone excess in some M-PPGL patients, whereas no apparent survival benefits from the therapy were found, probably due to the small number of patients available for analysis and the lack of systematic follow-up. In addition, the rarity of this tumor also makes it difficult to evaluate the exact prognosis of the patients.
With this in mind, the main purpose of the present study was to determine whether CVD could extend the survival time in a relatively large sample of patients with M-PPGL treated at two institutes.
Patients and Methods
Patients
The clinical records of 33 patients with M-PPGL, diagnosed based on the clinical and/or histopathological findings, treated at St. Marianna University School of Medicine Yokohama City Seibu Hospital or National Hospital Organization Kyoto Medical Center Hospital between 1999 and 2014 were retrospectively reviewed. All patients had metastatic lesions in non-chromaffin tissues, including the bone, liver, lungs, and lymph nodes. Among the total 33 patients with M-PPGL, 23 inoperable subjects who received at least 2 cycles of the CVD regimen were included in this study.
The effects of CVD on tumor volume and urinary catecholamine (CA) metabolites were analyzed. The prognosis and clinical features were compared between responders and non-responders to CVD, classified according to the tumor response.
The study protocol was approved by the Human Ethical Committees of St. Marianna University School of Medicine (No. 1780) and National Hospital Organization Kyoto Medical Center Hospital (No. 10-34) and was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013. All patients provided informed consent to participate in this study.
CVD Chemotherapy
CVD chemotherapy was administered basically following the original protocol described by Averbuch et al. [6], as follows: cyclophosphamide (750 mg/m2 body surface area) on day 1, vincristine (1.4 mg/m2 body surface area) on day 1, and dacarbazine (600 mg/m2 body surface area) on days 1 and 2 every 21 to 28 days. However, vincristine was capped at a maximum of 2 g/cycle according to the official instructions in Japan. The drug dose was reduced if necessary (e.g., in cases of inadequate biochemical profiles and toxicity). The treatment intervals were also modified to 60–90 days in some patients after the 4th cycle, owing to personal reasons (e.g., work schedule, economic problems). The patients were continuously monitored before and after each cycle. The CVD chemotherapy was discontinued based on the clinical judgment of the attending physicians in cases of tumor volume and/or CA increases and/or a lack of detected tumor response.
Tumor Response Assessment and Patient Classification
Before the introduction of CVD chemotherapy, initial radiological and nuclear medicine evaluations, including computed tomography scan and/or magnetic resonance imaging plus whole-body 131I-MIBG or 123I-MIBG scintigraphy, were performed. The imaging studies were repeated approximately every 3 months throughout the treatment. The tumor response to CVD was based on the sum of the maximum diameters of all measurable tumors. The response grade was determined by the response evaluation criteria in solid tumors version 1.1 [9], as follows: complete response (CR), disappearance of all target lesions; partial response (PR), at least a 30% tumor reduction; progressive disease (PD), development of a new lesion and/or an increase of 20% or more in the size of the target lesions; and SD, neither sufficient shrinkage to qualify for PR nor sufficient increase to qualify for PD.
Patients with CR or PR were defined as responders (n = 6, 26%) while those with SD or PD were defined as non-responders (n = 17, 74%). The clinical factors that contributed to the effectiveness of CVD were also analyzed.
Biochemical Response
The biochemical response was determined from 24-h urinary metanephrine, normetanephrine, and dopamine and classified as follows: CR, normalization of all biochemical tumor markers; PR, at least a 50% reduction; no change (NC), less than a 50% reduction or 25% increase; and PD, an increase of at least 25% in all three CA metabolites.
Survival Time
Four measures of survival were calculated, including progression-free survival (PFS), defined as the interval between the initiation of CVD treatment to the first documentation of PD or relapse; overall survival (OS), defined as the interval between the initiation of CVD treatment and the date of death or the last follow-up; the survival duration from the date of PPGL diagnosis to death or the last follow-up (survival duration from the diagnosis of PPGL); and the survival duration from the date of M-PPGL diagnosis to death or the last follow-up (survival duration from the diagnosis of M-PPGL).
Associations of Clinical Factors with Survival Time
We evaluated the clinical factors that predicted the survival time and response to chemotherapy by using Cox proportional hazards regression models. After analyzing the factors that influenced each survival time in the univariate analyses, factors with p < 0.1 were evaluated further using multivariate analyses. The results are reported as the hazard ratios with 95% confidence intervals (CIs).
Adverse Events
The adverse events and toxicity grades were assessed according to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE), version 4.0. (http://evs.nci.nih.gov/ftp1/CTCAE/Documentation/CTCAE_Governance_2010-03-11.pdf).
Statistical Analysis
Differences in continuous variables between the groups were compared using the Mann–Whitney test. χ 2 tests or Fischer’s exact test was performed where appropriate. The results are presented as the mean ± standard deviation, unless otherwise stated. The survival times were estimated by the Kaplan–Meier method, and the log-rank test was used for survival curve comparisons between the two groups. The predictive factors of survival were evaluated using univariate and multivariate Cox regression methods. Statistical significance was considered as p < 0.05. SAS 9.4 (SAS Institute Inc., Cary, NC) and StatView software (Abacus Concepts, Berkeley, CA) were used for all statistical calculations.
Results
Patient Characteristics
The demographic and clinical characteristics of the 23 M-PPGL patients (18 men and 5 women) enrolled in this study are shown in Tables 1 and 2. The mean ages at the first diagnosis of PPGL and at the diagnosis of M-PPGL were 41.7 ± 15.4 (range, 16∼65) and 46.6 ± 13.9 (range, 19∼68) years, respectively. The follow-up period after initiation of chemotherapy ranged from 1 to 13 years, with a median follow-up of 3.3 years. The primary tumor was located in the adrenal gland in 7 patients, was extra-adrenal in 14 patients, and was at multiple sites in 2 patients. The mean maximum tumor diameter at the start of chemotherapy was 6.5 ± 5.3 cm. Metastases to the lungs, liver, bone, and lymph nodes were observed in 53, 40, 61, and 48% of patients, respectively. The initial diagnosis was benign in nine patients, malignant in six patients, and unknown in eight patients. The mean interval between the diagnosis of PPGL and the detection of malignant disease was 5.2 ± 6.0 years (Table 2).
Table 1.
Characteristics of patients with malignant pheochromocytoma/paraganglioma treated with CVD chemotherapy
| Patient no. | Sex | Age at Dx of PPGL (years) | Age at Dx of M-PPGL (years) | Primary site(s) of disease | Metastatic site | Dx of PPGL∼Dx of M-PPGL (years) | Familial | Best tumor response | Best biochemical response | OS (years) | Survival status |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 44 | 46 | Retroperitoneal paraganglioma | Lung, bone, LN | 2.8 | NT | PR | CR | 8.2 | Dead |
| 2 | M | 16 | 41 | Lt adrenal | Lung, liver, LN | 25.3 | NT | PR | CR | 1.5 | Dead |
| 3 | F | 17 | 19 | Lt adrenal + paraaortic paraganglioma | Lung, bone, LN | 2.7 | VHL | PD | PD | 13.2 | Alive |
| 4 | F | 31 | 40 | Paraaortic paraganglioma | Lung, liver, LN | 9.0 | NT | CR | CR | 8.4 | Alive |
| 5 | M | 56 | 66 | Rt adrenal | Liver, bone | 11.0 | NT | PR | CR | 13.7 | Dead |
| 6 | M | 58 | 60 | Lt paraaortic paraganglioma | Bone | 2.2 | NT | PD | PD | 0.3 | Unknown |
| 7 | M | 55 | 58 | Lt paraaortic paraganglioma | Bone, LN | 3.8 | NT | SD | CR | 4.1 | Alive |
| 8 | M | 31 | 49 | Abdominal paraganglioma | Bone, LN | 18.9 | NT | PR | PR | 7.6 | Alive |
| 9 | M | 37 | 37 | Paraganglioma | Lung, liver, Bone, LN | 0 | NT | PD | PD | 0.7 | Dead |
| 10 | F | 17 | 24 | Rt adrenal | LN | 7.3 | NT | PR | CR | 2.5 | Alive |
| 11 | M | 55 | 60 | Rt adrenal | Lung, liver | 5.0 | NT | PD | NC | 3.8 | Dead |
| 12 | M | 46 | 46 | Intraperitoneal paraganglioma | Lung, liver, Bone | 1.0 | NT | PD | NC | 6.5 | Dead |
| 13 | M | 34 | 43 | Urinary bladder | Bone | 8.7 | NT | SD | NC | 4.6 | Alive |
| 14 | M | 23 | 27 | Rt adrenal | Bone | 4.3 | NF-1 | SD | PD | 2.3 | Alive |
| 15 | M | 56 | 57 | Rt adrenal | Liver | 0.9 | NT | PD | NC | 1.2 | Dead |
| 16 | M | 64 | 64 | Intraperitoneal paraganglioma | Lung, liver, Bone | 0.4 | NT | PD | NC | 0.4 | Dead |
| 17 | M | 52 | 57 | Retroperitoneal paraganglioma | Lung, bone | 5.0 | NT | PD | PD | 0.3 | Unknown |
| 18 | M | 33 | 33 | Rt adrenal | Liver, LN | 2.0 | NT | PD | PD | 3.9 | Alive |
| 19 | M | 36 | 36 | Intraperitoneal paraganglioma | Bone, LN | 0 | NT | PD | PD | 2.3 | Dead |
| 20 | M | 30 | 36 | Lt adrenal + intraperitoneal paraganglioma | LN | 6.0 | NT | SD | NC | 6.9 | Unknown |
| 21 | F | 47 | 47 | Paraaortic paraganglioma | Lung | 4.0 | NT | PD | NC | 2.8 | Alive |
| 22 | M | 65 | 68 | Rt adrenal | Lung | 4.3 | NT | SD | NC | 3.3 | Alive |
| 23 | M | 56 | 56 | Urinary bladder | Lung, bone | 2.6 | NT | PD | PD | 1.8 | Dead |
CVD cyclophosphamide, vincristine, and dacarbazine, M men, F female, LN lymph node, age at Dx of PPGL age at the first diagnosis of pheochromocytoma/paraganglioma, age at Dx of M-PPGL age at diagnosis of malignant pheochromocytoma/paraganglioma, Lt left, Rt right, NT not tested, VHL Von Hippel–Lindau disease, NF-1 neurofibromatosis type 1, CR complete response, PR partial response, SD stable disease, PD progression disease, NC no change, OS overall survival
Table 2.
Clinical profiles of the patients with malignant pheochromocytoma/paraganglioma treated with CVD chemotherapy
| All | Responders | Non-responders | p valuea | |
|---|---|---|---|---|
| Number of patientsNumber of deaths | 239 | 63 | 177 | – |
| Tumor response to CVD, n | – | CR 1/PR 5 | SD 5/PD 12 | – |
| Sex, n (M/F) | 18/5 | 3/3 | 15/2 | 0.09c |
| Primary tumor, n (adrenal/extra-adrenal/multiple) | 7/14/2 | 2/4/0 | 5/10/2 | 0.68d |
| Initial Dx, n (benign/malignant/unknown) | 9/6/8 | 5/0/1 | 4/6/7 | 0.03d |
| Age at Dx of PPGL, years (range) | 41.7 ± 15.4(16∼65) | 32.5 ± 15.5 | 44.9 ± 14.4 | 0.09b |
| Age at Dx of M-PPGL, years (range) | 46.5 ± 13.8(19∼68) | 44.3 ± 13.7 | 47.3 ± 14.2 | 0.70b |
| Maximum tumor diameter, cm (range) | 6.5 ± 5.3(1∼22) | 5.8 ± 4.8 | 6.9 ± 5.7 | 0.84b |
| Metastasis Lung, n (%) | 12 (52.2%) | 3 (50%) | 9 (53%) | 0.99c |
| Liver, n (%) | 9 (39.1%) | 3 (50%) | 6 (35%) | 0.64c |
| Bone, n (%) | 14 (60.9%) | 3 (50%) | 11 (65%) | 0.64c |
| Lymph nodes, n (%) | 11 (47.8%) | 5 (83%) | 6 (35%) | 0.06c |
| Number of metastatic organs | 2.0 ± 0.9 | 2.3 ± 0.8 | 1.9 ± 0.9 | 0.24b |
| Number of CVD cycles (range) | 11.6 ± 10.8(2∼41) | 24.5 ± 10.4 | 7.0 ± 6.5 | <0.01 |
| Biochemical response, n(CR/PR/NC/PD) | 6/1/8/8 | 5/1/0/0 | 1/0/8/8 | <0.01 |
| Dx of PPGL∼Dx of M-PPGL, years (median/range) | 5.2 ± 6.0(4.0/0∼25.3) | 12.4 ± 3.4(10.0/2.8∼25.3) | 3.1 ± 2.4(2.7/0∼8.7) | <0.01 |
The results are expressed as the mean ± standard deviation. Values of p < 0.05 were considered statistically significant (Mann–Whitney U test, Fisher’s exact test, or Pearson’s χ 2 test). Responders were defined as patients whose tumor responded to the CVD treatment (partial response or complete response). Non-responders were defined as patients whose tumors did not show a response to the treatment (stable disease or progressive disease)
CVD cyclophosphamide, vincristine, and dacarbazine, M men, F female, Dx diagnosis, age at Dx of PPGL age at the first diagnosis of pheochromocytoma/paraganglioma, age at Dx of M-PPGL age at diagnosis of malignant pheochromocytoma/paraganglioma, CR complete response, PR partial response, SD stable disease, PD progression disease, NC no change
aResponders vs. non-responders
bMann–Whitney U test
cFisher’s exact test
d χ 2 test
Genetic testing for genes that predispose to PPGL was performed in one young patient with multiple lesions and in one patient previously diagnosed with neurofibromatosis type 1 based on his clinical features. The former was diagnosed as having Von Hippel–Lindau disease with a proven VHL gene mutation, and the latter was genetically confirmed to suffer from neurofibromatosis type 1. Except for these two cases, there was no family history of PPGL and no past history of any disease suggestive of syndromic PPGL in our cohort.
Effectiveness of CVD Therapy
The mean number of cycles of CVD chemotherapy was 11.6 ± 10.8 (range, 2∼41); the number of cycles in responders was greater than that in non-responders. All patients were evaluated for the tumor and biochemical responses (Table 2). In terms of the tumor response, CVD therapy achieved CR in 1 patient (4%) and PR in 5 patients (22%), while 5 patients (22%) were unchanged (SD) and 12 patients (52%) had PD. In terms of the biochemical response, 6 patients (26%) showed a CR, 1 patient (4%) had a PR, 8 (35%) patients had no change (NC), and 8 patients (35%) had PD.
All responders showed a biochemical CR or PR, while only 6% of the non-responders fulfilled the criteria for biochemical CR or PR, suggesting that the antineoplastic effect of CVD chemotherapy results in decreased catecholamine excess.
There were more cases of metachronous metastases among patients in the responder group than in the non-responder group (Table 2). No difference was found between the two groups with regard to sex, age at first diagnosis, tumor size, and number of metastases. Furthermore, the time interval between the initial diagnosis of PPGL and the detection of malignant disease in the responders was longer than in the non-responders (Table 2).
Other Treatments in Addition to CVD
All surgical interventions, including a second operation in six patients, were performed before CVD initiation. Other chemotherapy regimens, including sunitinib performed after CVD, were deemed ineffective. Local radiation for bone metastasis and TAE for hepatic lesions were always performed during/after CVD treatment. 131I-MIBG treatments were administered in two cases (patients 10 and 17) before CVD and in four cases (patients 2, 5, 9, 12, and 15) after CVD. Therapies other than CVD are shown in Table 3. Before starting the CVD therapy, nearly all patients received α1-adrenergic and/or calcium channel blockers to achieve adequate blood pressure control. In cases where the heart rate remained elevated, β-blockers were additionally administered. No case was treated with α-methyl-para-tyrosine.
Table 3.
Other treatments in addition to CVD
| Responders | Non-responders | |||
|---|---|---|---|---|
| n | Pt no. | n | Pt no. | |
| 2nd OPE | 2 | 4, 8 | 1 | 21 |
| Local radiation | 0 | 2 | 13, 19 | |
| 131I-MIBG | 0 | 1 | 18 | |
| TAE | 0 | 1 | 15 | |
| 2nd OPE + 131I-MIBG | 1 | 10 | 3 | 3, 17, 22 |
| 2nd OPE + local radiation | 0 | 1 | 20 | |
| 2nd OPE + TAE + other neoplastic therapiesa | 1 | 2 | 0 | |
| TAE + local radiation + other neoplastic therapiesb | 1 | 5 | 0 | |
| 2nd OPE + 131I-MIBG + local radiation + other neoplastic therapiesc | 1 | 1 | 0 | |
| TAE + other neoplastic therapiesa | 0 | 1 | 9 | |
| 2nd OPE + TAE + local radiation + other neoplastic therapiesd | 0 | 1 | 12 |
All surgical interventions, including a second operation in six patients, were performed before CVD initiation. Other chemotherapy regimens, including sunitinib performed after CVD, were deemed ineffective. Local radiation for bone metastasis and TAE for hepatic lesions were always performed during/after CVD treatment. 131I-MIBG treatments were administered in two cases (patients 10 and 17) before CVD and in four cases (patients 2, 5, 9, 12, and 15) after CVD
CVD cyclophosphamide, vincristine, and dacarbazine, 2nd OPE second operation, local radiation local external beam radiation therapy, 131 I-MIBG 131I-labeled metaiodobenzylguanidine therapy, TAE transcatheter arterial embolization, Pt no. patient number
aCisplatin + 5-fluorouracil
bSunitinib
cCisplatin + VP-16
dS-1 (tegafur/gimeracil/oteracil potassium) + sunitinib
Survival
After commencing CVD therapy, 10 patients (3 in the responder group and 7 in the non-responder group) died. Eight of the 10 deceased patients died due to multiple organ failure secondary to disseminated metastasis while the causes of death in the remaining 2 patients were severe paralytic ileus resulting from CA excess and myelodysplastic syndrome related to the CVD regimen. Three patients in the non-responder group were lost to follow-up at 0.3, 0.3, and 6.9 years after the initiation of CVD treatment. In all patients, the 5-year PFS rate, OS rate, and survival rate from the time of diagnosis of PPGL and from the time of diagnosis of M-PPGL were 31.7, 64.9, 82.9, and 66.4%, respectively.
The PFS period in the non-responders was shorter than in the responders (median ± standard deviation; 0.33 ± 1.0 vs. 8.1 ± 3.4 years, p < 0.01), as determined by Kaplan–Meier analysis and the log-rank test (Supplementary Fig. S1a). Although not significant, the responders tended to have a better survival duration from the diagnosis of PPGL, compared to the non-responders (23.3 ± 5.9 vs. 7.0 ± 4.9 years, p = 0.08, Supplementary Fig. S2a). However, the OS time between the responders and non-responders (7.9 ± 4.5 vs. 2.8 ± 3.2 years, p = 0.27) as well as the survival duration from the diagnosis of M-PPGL (9.5 ± 4.2 vs. 3.7 ± 3.7 years, p = 0.34) did not differ between the two groups (Supplementary Figs. S1b and S2b). These results suggested that CVD therapy may not ameliorate the survival, despite tumor shrinkage and hormonal improvement being observed in some patients with M-PPGL.
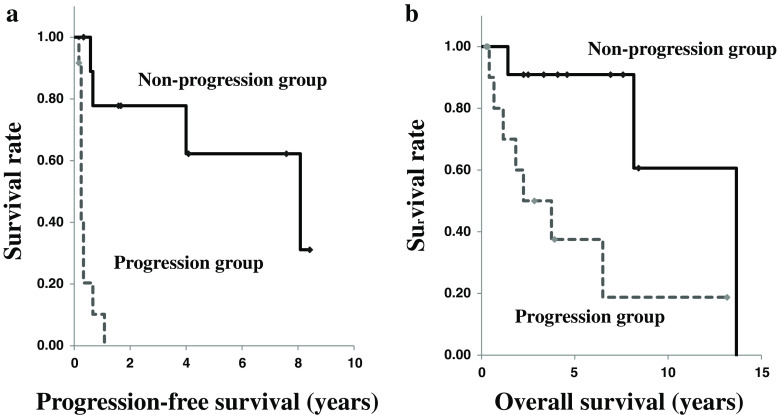
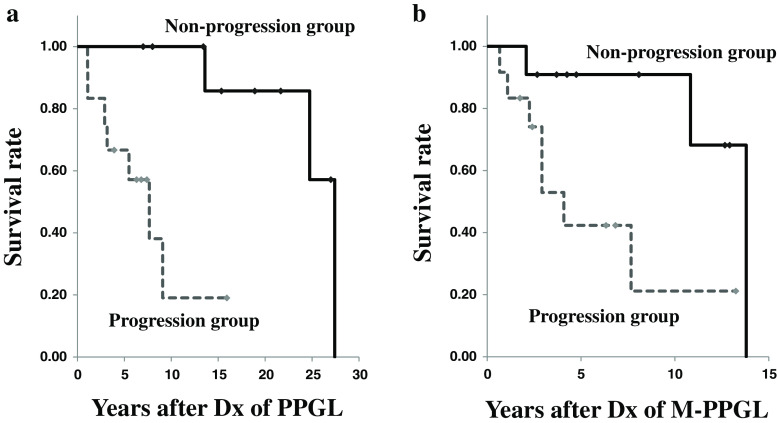
Based on these findings, we next reclassified the subjects into the progression (patients with a tumor response of “PD”) and non-progression groups (patients with a tumor response of “CR,” “PR,” or “SD”) and compared their survival rates. In the comparisons of PFS, OS, and the durations from the date of PPGL or M-PPGL diagnosis until the last follow-up, the non-progression group had significantly better survival rates than the progression group (Figs. 1a, b and 2a, b, at 62 vs. 0%, 91 vs. 38%, 100 vs. 67%, and 91 vs. 42%, respectively).
Fig. 1.
Kaplan–Meier survival curves in the non-progression and progression groups. a Progression-free survival (PFS). b Overall survival (OS). The PFS and OS in the non-progression group (solid lines; PFS, 1.7 ± 3.3 years; OS, 4.6 ± 3.6 years) were significantly longer than in the progression group (dashed lines; PFS, 0.3 ± 0.3 years; OS, 2.0 ± 3.7 years), as determined by Kaplan–Meier analysis with the log-rank test (χ 2 = 16.81; p < 0.001, and χ 2 = 6.16; p = 0.01, respectively)
Fig. 2.
Kaplan–Meier survival curves in the non-progression and progression groups for a the survival since the first diagnosis of pheochromocytoma/paraganglioma (time after Dx of PPGL) and b since the first diagnosis of metastases (time after Dx of M-PPGL). The durations from the first diagnoses of pheochromocytoma/paraganglioma and malignant disease until follow-up in the non-progression group (solid lines; time after Dx of PPGL, 15.3 ± 7.6 years; time after Dx of M-PPGL, 8.1 ± 4.4 years) were significantly longer than in the progression group (dashed line; time after Dx of PPGL, 5.9 ± 4.1 years; time after Dx of M-PPGL, 2.9 ± 3.6 years), as determined by Kaplan–Meier analysis with the log-rank test (χ 2 = 10.04; p < 0.01, and χ 2 = 5.49; p = 0.02, respectively)
Factors Associated with the Survival Time
We evaluated 15 clinical factors for their ability to predict survival. In the univariate analyses, survival was significantly related with or tended to be associated with the various investigated factors such as the number of CVD therapy cycles, benign or malignant status at the initial diagnosis, and tumor response (Table 4). For the multivariate analysis, Cox proportional hazards regression models were created to determine the factors independently associated with survival outcomes based on the univariate analysis results. Multivariate analysis revealed that the number of CVD therapy cycles was significantly associated with increased PFS (hazard ratio = 0.92, 95% CI = 0.86–0.99; p = 0.031) and that the duration from initial diagnosis to recurrence or metastasis was significantly related to the survival duration from the diagnosis of PPGL (hazard ratio = 0.34, 95% CI = 0.16–0.74; p = 0.007). Moreover, the presence of liver metastases tended to be associated with a reduced survival duration from the diagnosis of M-PPGL (hazard ratio = 3.61, 95% CI = 0.91–14.6, p = 0.068). However, OS was not significantly associated with any clinical factor (all p > 0.1).
Table 4.
Univariate analyses of the associations of prognostic factors with survival
| Clinical parameter | OS | PFS | Duration from Dx of PPGL | Duration from Dx of M-PPGL | ||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p value | HR (95% CI) | p value | HR (95% CI) | p value | HR (95% CI) | p value | |
| Sex (male vs. female) | 4.97 (0.56–44.09) | 0.150 | 1.73 (0.47–6.31) | 0.406 | 3.14 (0.38–26.18) | 0.291 | 4.50 (0.54–37.43) | 0.164 |
| Age at initial diagnosis | 1.04 (0.99–1.09) | 0.156 | 1.01 (0.97–1.04) | 0.655 | 1.06 (1.01–1.12) | 0.025 | 1.04 (0.98–1.09) | 0.183 |
| Age at malignant diagnosis | 1.03 (0.98–1.08) | 0.269 | 1.00 (0.96–1.04) | 0.867 | 1.04 (0.99–1.10) | 0.157 | 1.03 (0.98–1.08) | 0.289 |
| Initial diagnosis (malignant vs. benign) | 4.08 (0.72–23.13) | 0.112 | 3.59 (0.84–15.23) | 0.083 | 11.61 (1.42–95.03) | 0.022 | 3.29 (0.65–16.74) | 0.151 |
| (Unknown vs. benign) | 1.89 (0.26–13.93) | 0.532 | 1.92 (0.43–8.65) | 0.395 | 1.94 (0.27–14.16) | 0.514 | 1.23 (0.20–7.62) | 0.827 |
| Primary site (extra-adrenal vs. adrenal) | 1.05 (0.26–4.25) | 0.943 | 0.68 (0.23–2.07) | 0.502 | 1.31 (0.32–5.40) | 0.709 | 0.89 (0.22–3.59) | 0.867 |
| Tumor size at malignant diagnosis | 1.05 (0.92–1.19) | 0.468 | 1.05 (0.94–1.17) | 0.419 | 1.07 (0.93–1.23) | 0.333 | 1.05 (0.92–1.19) | 0.486 |
| Hypertension (yes vs. no) | 0.32 (0.06–1.64) | 0.172 | 0.75 (0.16–3.42) | 0.708 | 0.33 (0.06–1.71) | 0.187 | 0.30 (0.06–1.55) | 0.151 |
| Impaired glucose tolerance (yes vs. no) | 2.26 (0.56–9.10) | 0.253 | 2.02 (0.62–6.59) | 0.245 | 3.47 (0.81–14.81) | 0.093 | 2.29 (0.57–9.19) | 0.243 |
| Number of CVD therapy cycles | 0.94 (0.87–1.01) | 0.106 | 0.92 (0.86–0.99) | 0.031 | 0.96 (0.89–1.03) | 0.256 | 0.94 (0.87–1.02) | 0.137 |
| Duration from initial diagnosis to recurrence or metastasis | 0.90 (0.75–1.08) | 0.278 | 0.88 (0.75–1.04) | 0.124 | 0.34 (0.16–0.74) | 0.007 | 0.90 (0.75–1.09) | 0.298 |
| Lung metastasis (yes vs. no) | 3.32 (0.68–16.21) | 0.137 | 1.96 (0.65–5.91) | 0.230 | 2.07 (0.51–8.37) | 0.307 | 3.43 (0.71–16.56) | 0.125 |
| Liver metastasis (yes vs. no) | 3.18 (0.79–12.86) | 0.105 | 1.60 (0.54–4.76) | 0.401 | 3.07 (0.76–12.49) | 0.117 | 3.64 (0.91–14.60) | 0.068 |
| Bone metastasis (yes vs. no) | 1.31 (0.32–5.30) | 0.707 | 1.45 (0.48–4.39) | 0.513 | 2.70 (0.56–13.08) | 0.217 | 1.45 (0.36–5.82) | 0.599 |
| Lymph node metastasis (yes vs. no) | 0.54 (0.14–2.04) | 0.361 | 0.52 (0.18–1.53) | 0.237 | 0.32 (0.08–1.40) | 0.131 | 0.55 (0.14–2.15) | 0.394 |
| Tumor response (non-responders vs. responders) | 2.47 (0.47–12.93) | 0.285 | 4.74 (0.98–22.84) | 0.053 | 5.82 (0.65–51.76) | 0.114 | 2.18 (0.43–11.11) | 0.348 |
OS overall survival, PFS progression-free survival, HR hazard ratio, CI confidence interval, duration from Dx of PPGL duration from the first diagnosis of pheochromocytoma/paraganglioma, duration from Dx of M-PPGL duration from the diagnosis of malignant pheochromocytoma/paraganglioma, CVD cyclophosphamide, vincristine, and dacarbazine
Adverse Events
The most common toxicities encountered were grade <4 myelosuppression, peripheral neuropathy, and gastrointestinal disorders. Neutropenia, nausea, peripheral neuropathy, liver disorder, hemorrhagic cystitis, and cardiotoxicity occurred in 61, 61, 22, 13, 4, and 9% of patients, respectively. No subjects interrupted the CVD therapy due to severe adverse events, whereas one patient (patient no. 12) with neurotoxicity strongly wished to stop the treatment. These results indicate that by taking appropriate measures, this regimen was relatively well tolerated. Of note, at 8 years after the withdrawal of the antineoplastic agent, one patient with a partial tumor response to CVD developed therapy-related myelodysplastic syndrome (t-MDS).
Discussion
Systematic chemotherapy plays an important role in the treatment of metastatic PPGL. Several single agents and combination therapies have been used for this malignancy, with variable success. At present, CVD therapy is thought to be the most effective chemotherapy regimen, but its value has not yet been fully defined. The long-term clinical benefits of this regimen were reported in a 22-year prospective follow-up study of 18 patients [10]. In that study, CVD treatment produced a complete tumor response rate of 11% and a PR rate of 44%. However, no obvious benefits in OS were demonstrated. Similar results were demonstrated by a retrospective analysis from Japan, in which 47% of the 17 M-PPGL patients exhibited partial or minimal radiographic improvements [8]. Nevertheless, the median OS duration in the patients who experienced a tumor response was no longer than that in those who did not. Niemeijer et al. recently performed a meta-analysis in which they reported the rate of tumor shrinkage and CA reduction by CVD. However, they scarcely mentioned the impact of CVD on survival [11]. On the other hand, Ayala-Ramirez et al. found an association between longer survival and the response to chemotherapy [12]. Unfortunately, however, in their study, approximately 80% of the patients were treated with a regimen involving cyclophosphamide and dacarbazine, while only 10 (19.2%) patients underwent CVD treatment.
To the best of our knowledge, the present study is the largest series evaluating the effects of CVD on metastatic M-PPGL and the first research on the topic performed at two independent institutes. The best radiological responses to CVD in terms of the tumor volume were as follows: CR in one patient (4%), PR in 5 patients (22%), SD in 5 patients (22%), and PD in 11 patients (52%). Three previous, relatively large studies, including at least 15 patients, that investigated CVD for M-PPGL showed response rates of 25–55% [13], indicating that our outcome in terms of the tumor response was not superior to that of other studies. Nonetheless, we clearly demonstrated that the PFS and OS in the non-progression group were significantly longer than those in the progression group. To our knowledge, there has been no previous report comparing the effects of CVD on survival between the non-progression and progression groups. Our results indicate that tumor stability by CVD may produce a better survival in at least some M-PPGL patients. However, further researches to validate our findings are needed. Multivariate analysis revealed that a higher number of CVD therapy cycles were significantly associated with increased PFS; we posit that this is indicative of tumor progression being better controlled by longer CVD treatment. While it is possible that the greater number of cycles was a result of patients responding to treatment and thus opting to maintain it, we are unable to determine this owing to the study’s retrospective nature.
Haung et al. [10] reported that the median survival, calculated from 3 months after starting CVD, was 3.8 years for patients whose tumor showed a CR or PR to the chemotherapy, as compared to 1.8 years for the remaining cases. In our cohort, the median OSs in the responder and non-responder groups were 7.9 and 2.8 years, respectively. The proportion of responders in the present study was lower than in Huang’s study (26 vs. 55%), while the OS in our study seemed longer. Of note, some previous reports have suggested there are two subtypes of M-PPGL, with distinct clinical courses and outcomes [10, 14, 15]. Hence, it is uncertain whether the differences in the survival results among the different studies are due to beneficial impacts of CVD treatment or the natural history of the disease. Sixty percent of patients with SD showed no change in the biochemical response; therefore, CVD may have exhibited no effect in these patients. However, within the same SD group, the course of the disease varied from case to case. In this study, the grade of CVD response was unchanged, but some degree of tumor shrinkage and CA reduction after repeated chemotherapy was observed in one of five patients with SD (patient no. 11). The results suggest that continuing CVD treatment may contribute to the maintenance of stable disease state or prolonging OS in some, albeit few, patients with SD. It is well known that some patients with M-PPGL have long survival durations; therefore, demonstrating a proven survival benefit is difficult [13].
In order to determine the natural history of M-PPGL, Hescot et al. [16] investigated the PFS at 1 year in therapy-naïve patients to identify the related prognostic parameters. As approximately half of the patients achieved SD at 1 year, they advocated that a wait-and-see policy seemed appropriate at first-line therapy. In agreement with their result, the PFS at 1 year in our subjects was 45.2%. Furthermore, the 1-year OS rate was also similar between these two studies (94 vs. 91%), suggesting that the survival prognosis in some patients with aggressive M-PPGL may be unaffected by the current chemotherapy regimen. Therefore, it is important to extract which patients with unresectable M-PPGL are candidates for intensive pharmacological anti-neoplastic treatments and/or are expected to respond to the CVD regimen. Currently, the factors predicting the response to CVD chemotherapy in M-PPGL patients remain unknown. Tanabe et al. [8] reported that responders to CVD treatment had a longer survival from the time of the first diagnosis of PPGL to the detection of metastasis compared to non-responders. Similarly, we also found that the survival duration from the initial diagnosis of PPGL to recurrence or metastasis in the non-responders was shorter than in the responders, indicating that the impact of CVD may be greater in more slowly growing tumors.
The reported 5-year OS rates of metastatic M-PPGL vary between 34 and 60%, with a shorter survival associated with metastases to the liver and lungs, whereas longer survival is seen in patients with bone metastasis [17]. Choi et al. [18] indicated that poor survival in their 47 M-PPGL patients, including 33 cases treated with various combination modalities, was independently associated with older age and synchronous metastases in the multiple regression analysis. In the present analysis, the presence of liver metastases tended to associate with a reduced survival time from the diagnosis of M-PPGL. Thus, regulating liver metastasis may be one of the key factors determining the survival in these patients. In fact, among the five patients receiving transcatheter arterial embolization therapy for liver metastases, two cases whose growing hepatic lesions were suppressed to some extent survived for a relatively long period of time (patient nos. 2 and 5).
It should be pointed out that we consistently observed tumor progression during and after systemic chemotherapies other than CVD in the present cohort. In particular, the beneficial effect of sunitinib on tumor volume appeared transient, lasting only for a few weeks. Therefore, these other regimens were considered unlikely to affect the patient survival. On the other hand, we could not completely exclude the therapeutic benefit of 131I-MIBG on survival.
The tumor response was very similar to the biochemical response in our cohort, suggesting that the antineoplastic effect of CVD chemotherapy ameliorates catecholamine excess. However, 20 and 60% of SD patients exhibited biochemical CR and NC, respectively. This indicates that RECIST evaluation in the non-responder group is not necessarily concordant with the biochemical response. This aspect is worth paying attention to.
Similar to most prior studies, which indicated acceptable toxicity of the CVD regimen, there was no patient with severe adverse events (CTCAE grade ≥4) while continuing the CVD therapy in this study. However, we observed one case of t-MDS. This patient received 24 cycles of CVD therapy and external beam radiation for bone metastases during the 8 years after the diagnosis of metastatic M-PPGL. Subsequently, she developed progressive severe anemia with blast cells in the peripheral blood at 2 years after terminating CVD. t-MDS has been recognized as a devastating late complication of alkylating agent-based therapy, such as cyclophosphamide [19], and most commonly occurs 5 to 10 years after exposure to these drugs and/or irradiation. Moreover, t-MDS is usually associated with unbalanced losses of chromosomes 5 and/or 7. The present case possessed complex aberrations involving five chromosome deletions, including 46,XX,del(5)(q13q33) [1], 46,idem,-7,+mar [10], and 46,XX [9]. Accordingly, attention should be paid to the risk of t-MDS, especially following long-standing repeated alkylating agent-based chemotherapy with radiological intervention.
Our study has several limitations. We lost 3 of 23 patients during the follow-up period. Despite being the largest study to date, the present study was retrospective and lacked a control group and the number of the patients was still insufficient. Therefore, our results may be affected by selection bias. In addition, systematic molecular genetic testing, which may further clarify the clinical behavior and response to therapy, was not performed in the majority of patients. Succinate dehydrogenase B (SDHB) mutations are known to be strong predictors of prognosis [20]. Most of our patients did not consent to genetic testing and/or SDHB staining of their tumor tissues. Furthermore, 16 patients in this study had undergone surgery at other hospitals; therefore, it was very difficult to obtain their tumor specimens for staining. Although sunitinib and all systemic chemotherapies resulted in tumor regression and/or stability, we could not confirm the effects of interventions other than that of CVD on survival. Further large-scale cohort studies are needed to confirm the efficacy of CVD chemotherapy.
In conclusion, we are the first to demonstrate that the PFS and OS rates in the non-progression group are significantly longer than those in the progression group, suggesting that tumor stability by CVD treatment can improve survival in at least some M-PPGL patients. Tumor shrinkage, as well as decreased catecholamine secretion, can be expected in approximately one third of patients following CVD treatment and that the effect is maintained over time. Although CVD is not currently indicated for all patients with M-PPGL, controlling tumor progression by multimodal therapy including CVD is critical for improving survival in some patients with metastatic and unresectable M-PPGL.
Electronic supplementary material
Kaplan-Meier curves for survival in the responders and non-responders to cyclophosphamide, vincristine, and dacarbazine (CVD) therapy. (a) Progression-free survival (PFS; from the initiation of CVD until the date of relapse or significant tumor growth). The PFS in the responders (solid line; 8.1 ± 3.4 years [median ± standard deviation]) was significantly longer than in the non-responders (dashed line; 0.33 ± 0.9 years), as determined by Kaplan-Meier analysis with the log-rank test (χ2 = 4.882; p = 0.03). (b) Overall survival (OS; from the initiation of CVD until the date of death or the last follow-up). The responders (dashed line; 7.9 ± 4.5 years) and non-responders (solid line; 2.8 ± 3.2 years) had nearly identical OS curves (χ2 = 1.20; p = 0.273; log-rank test). (PPTX 52 kb)
Kaplan-Meier survival curves for survival since the first diagnosis of pheochromocytoma/paraganglioma (a) and the first diagnosis of metastases (b) in responders and non-responders to cyclophosphamide, vincristine, and dacarbazine (CVD). a, Patients whose tumor responded to the CVD treatment (responders, solid line) appeared to have slightly longer survival since the first diagnosis of pheochromocytoma/paraganglioma (23.3 ± 5.9 years) than those who did not (non-responders, dashed line; 7.0 ± 4.9 years), although this difference was not statistically significant (χ2 = 3.009; p = 0.08). b, There was no statistically significant difference in the mortality after the first diagnosis of metastases between the responders (solid line; 9.5 ± 4.2 years) and non-responders (dashed line; 3.7 ± 3.7 years) (χ2 = 0.929; p = 0.33). (PPTX 52 kb)
Compliance with Ethical Standards
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Research Involving Human Participants and/or Animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Chrisoulidou A, Kaltsas G, Ilias I, Grossman AB. The diagnosis and management of malignant phaeochromocytoma and paraganglioma. Endocr Relat Cancer. 2007;14:569–585. doi: 10.1677/ERC-07-0074. [DOI] [PubMed] [Google Scholar]
- 2.Eisenhofer G, Bornstein SR, Brouwers FM, Cheung NK, Dahia PL, de Krijger RR, Giordano TJ, Greene LA, Goldstein DS, Lehnert H, Manger WM, Maris JM, Neumann HP, Pacak K, Shulkin BL, Smith DI, Tischler AS, Young WF., Jr Malignant pheochromocytoma: current status and initiatives for future progress. Endocr Relat Cancer. 2004;11:423–436. doi: 10.1677/erc.1.00829. [DOI] [PubMed] [Google Scholar]
- 3.van Hulsteijn LT, Niemeijer ND, Dekkers OM, Corssmit EP. (131)I-MIBG therapy for malignant paraganglioma and phaeochromocytoma: systematic review and meta-analysis. Clin Endocrinol. 2014;80:487–501. doi: 10.1111/cen.12341. [DOI] [PubMed] [Google Scholar]
- 4.Keiser HR, Goldstein DS, Wade JL, Douglas FL, Averbuch SD. Treatment of malignant pheochromocytoma with combination chemotherapy. Hypertension. 1985;7:I18–I24. doi: 10.1161/01.HYP.7.3_Pt_2.I18. [DOI] [PubMed] [Google Scholar]
- 5.Plouin PF, Fitzgerald P, Rich T, Ayala-Ramirez M, Perrier ND, Baudin E, Jimenez C. Metastatic pheochromocytoma and paraganglioma: focus on therapeutics. Horm Metab Res. 2012;44:390–399. doi: 10.1055/s-0031-1299707. [DOI] [PubMed] [Google Scholar]
- 6.Averbuch SD, Steakley CS, Young RC, Gelmann EP, Goldstein DS, Stull R, Keiser HR. Malignant pheochromocytoma: effective treatment with a combination of cyclophosphamide, vincristine, and dacarbazine. Ann Intern Med. 1988;109:267–273. doi: 10.7326/0003-4819-109-4-267. [DOI] [PubMed] [Google Scholar]
- 7.Deutschbein T, Fassnacht M, Weismann D, Reincke M, Mann K, Petersenn S. Treatment of malignant phaeochromocytoma with a combination of cyclophosphamide, vincristine and dacarbazine: own experience and overview of the contemporary literature. Clin Endocrinol. 2015;82:84–90. doi: 10.1111/cen.12590. [DOI] [PubMed] [Google Scholar]
- 8.Tanabe A, Naruse M, Nomura K, Tsuiki M, Tsumagari A, Ichihara A. Combination chemotherapy with cyclophosphamide, vincristine, and dacarbazine in patients with malignant pheochromocytoma and paraganglioma. Horm Cancer. 2013;4:103–110. doi: 10.1007/s12672-013-0133-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45:228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 10.Huang H, Abraham J, Hung E, Averbuch S, Merino M, Steinberg SM, Pacak K, Fojo T. Treatment of malignant pheochromocytoma/paraganglioma with cyclophosphamide, vincristine, and dacarbazine: recommendation from a 22-year follow-up of 18 patients. Cancer. 2008;113:2020–2028. doi: 10.1002/cncr.23812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Niemeijer ND, Alblas G, van Hulsteijn LT, Dekkers OM, Corssmit EP. Chemotherapy with cyclophosphamide, vincristine and dacarbazine for malignant paraganglioma and pheochromocytoma: systematic review and meta-analysis. Clin Endocrinol. 2014;81:642–651. doi: 10.1111/cen.12542. [DOI] [PubMed] [Google Scholar]
- 12.Ayala-Ramirez M, Feng L, Habra MA, Rich T, Dickson PV, Perrier N, Phan A, Waguespack S, Patel S, Jimenez C. Clinical benefits of systemic chemotherapy for patients with metastatic pheochromocytomas or sympathetic extra-adrenal paragangliomas: insights from the largest single-institutional experience. Cancer. 2012;118:2804–2812. doi: 10.1002/cncr.26577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baudin E, Habra MA, Deschamps F, Cote G, Dumont F, Cabanillas M, Arfi-Roufe J, Berdelou A, Moon B, Al Ghuzlan A, Patel S, Leboulleux S, Jimenez C. Therapy of endocrine disease: treatment of malignant pheochromocytoma and paraganglioma. Eur J Endocrinol. 2014;171:R111–R122. doi: 10.1530/EJE-14-0113. [DOI] [PubMed] [Google Scholar]
- 14.Remine WH, Chong GC, Van Heerden JA, Sheps SG, Harrison EG., Jr Current management of pheochromocytoma. Ann Surg. 1974;179:740–748. doi: 10.1097/00000658-197405000-00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Heerden JA, Sheps SG, Hamberger B, Sheedy PF, 2nd, Poston JG, ReMine WH. Pheochromocytoma: current status and changing trends. Surgery. 1982;91:367–373. [PubMed] [Google Scholar]
- 16.Hescot S, Leboulleux S, Amar L, Vezzosi D, Borget I, Bournaud-Salinas C, de la Fouchardiere C, Libé R, Do Cao C, Niccoli P, Tabarin A, Raingeard I, Chougnet C, Giraud S, Gimenez-Roqueplo AP, Young J, Borson-Chazot F, Bertherat J, Wemeau JL, Bertagna X, Plouin PF, Schlumberger M, Baudin E. One-year progression-free survival of therapy-naive patients with malignant pheochromocytoma and paraganglioma. J Clin Endocrinol Metab. 2013;98:4006–4012. doi: 10.1210/jc.2013-1907. [DOI] [PubMed] [Google Scholar]
- 17.Pacak K, Eisenhofer G, Ahlman H, Bornstein SR, Gimenez-Roqueplo AP, Grossman AB, Kimura N, Mannelli M, McNicol AM, Tischler AS. Pheochromocytoma: recommendations for clinical practice from the First International Symposium. Nat Clin Pract Endocrinol Metab. 2007;3:92–102. doi: 10.1038/ncpendmet0396. [DOI] [PubMed] [Google Scholar]
- 18.Choi YM, Sung TY, Kim WG, Lee JJ, Ryu JS, Kim TY, Kim WB, Hong SJ, Song DE, Shong YK. Clinical course and prognostic factors in patients with malignant pheochromocytoma and paraganglioma: a single institution experience. J Surg Oncol. 2015;112:815–821. doi: 10.1002/jso.24063. [DOI] [PubMed] [Google Scholar]
- 19.Smith SM, Le Beau MM, Huo D, Karrison T, Sobecks RM, Anastasi J, Vardiman JW, Rowley JD, Larson RA. Clinical-cytogenetic associations in 306 patients with therapy-related myelodysplasia and myeloid leukemia: the University of Chicago series. Blood. 2003;102:43–52. doi: 10.1182/blood-2002-11-3343. [DOI] [PubMed] [Google Scholar]
- 20.Amar L, Baudin E, Burnichon N, Peyrard S, Silvera S, Bertherat J, Bertagna X, Schlumberger M, Jeunemaitre X, Gimenez-Roqueplo AP, Plouin PF. Succinate dehydrogenase B gene mutations predict survival in patients with malignant pheochromocytomas or paragangliomas. J Clin Endocrinol Metab. 2007;92:3822–3828. doi: 10.1210/jc.2007-0709. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Kaplan-Meier curves for survival in the responders and non-responders to cyclophosphamide, vincristine, and dacarbazine (CVD) therapy. (a) Progression-free survival (PFS; from the initiation of CVD until the date of relapse or significant tumor growth). The PFS in the responders (solid line; 8.1 ± 3.4 years [median ± standard deviation]) was significantly longer than in the non-responders (dashed line; 0.33 ± 0.9 years), as determined by Kaplan-Meier analysis with the log-rank test (χ2 = 4.882; p = 0.03). (b) Overall survival (OS; from the initiation of CVD until the date of death or the last follow-up). The responders (dashed line; 7.9 ± 4.5 years) and non-responders (solid line; 2.8 ± 3.2 years) had nearly identical OS curves (χ2 = 1.20; p = 0.273; log-rank test). (PPTX 52 kb)
Kaplan-Meier survival curves for survival since the first diagnosis of pheochromocytoma/paraganglioma (a) and the first diagnosis of metastases (b) in responders and non-responders to cyclophosphamide, vincristine, and dacarbazine (CVD). a, Patients whose tumor responded to the CVD treatment (responders, solid line) appeared to have slightly longer survival since the first diagnosis of pheochromocytoma/paraganglioma (23.3 ± 5.9 years) than those who did not (non-responders, dashed line; 7.0 ± 4.9 years), although this difference was not statistically significant (χ2 = 3.009; p = 0.08). b, There was no statistically significant difference in the mortality after the first diagnosis of metastases between the responders (solid line; 9.5 ± 4.2 years) and non-responders (dashed line; 3.7 ± 3.7 years) (χ2 = 0.929; p = 0.33). (PPTX 52 kb)