Summary
Background
The ever-growing trend of abdominal obesity worldwide has garnered global attention over the past three decades. In India, BMI has conventionally been used to measure obesity. National Family Health Survey (NFHS) is the largest demographic and health survey (DHS) in India. For the first time, the NFHS conducted the fifth round in 2019–21 which assessed abdominal obesity through waist circumference. The objective of the current study was to determine the prevalence of abdominal obesity and explore the associated socioeconomic factors.
Methods
The prevalence of abdominal obesity in India was determined using the NFHS-5 dataset, where waist circumference was used as a measure. Multivariable binary logistic regression was then employed to examine the association of different socioeconomic factors with abdominal obesity.
Findings
The prevalence of abdominal obesity in the country was found to be 40% in women and 12% in men. The findings show that 5–6 out of 10 women between the ages of 30–49 are abdominally obese. The association of abdominal obesity in women is stronger with older age groups, urban residents, wealthier sections, and non-vegetarians. For those practising the Sikh religion, the prevalence is higher in both men and women. Abdominal obesity is also on the rise in rural areas and is penetrating lower and middle socioeconomic sections of society.
Interpretation
The findings of the current study highlight the need for the government and other stakeholders to proactively design targeted interventions for abdominal obesity, especially for women in their thirties and forties in India. Further research is recommended to understand the driving factors of abdominal obesity, their inter-operability, and the disease risk associated with this type of obesity.
Funding
None.
Keywords: Abdominal obesity, Central obesity, Waist circumference, India, Middle aged women
Research in context.
Evidence before this study
Obesity has emerged globally as a potential threat to public health, especially since the beginning of the 21st century. As of 2016, an estimated 44 percent of adults worldwide (more than 2 billion) are overweight or obese, and over 70 percent of them live in low-income or middle-income countries (LMICs). The ever-increasing proportion of overweight and obese adults categorised primarily on the BMI measure in LMICs, has established the fact that obesity is no more a problem of only high-income countries or urban settings. The prevalence of obesity is pertinent for LMICs, where under-nutrition is also persistent and that poses a threat of double burden of malnutrition. India has the third largest obese population in the world after USA and China, as per WHO estimates. Numerous studies have been conducted on abdominal obesity in different parts of India, but due to small sample sizes and region-specific focus, the studies were unable to provide an accurate overview of the situation in the country. Also, most studies on obesity have been done using the BMI indicator in India.
Added value of this study
In the fifth round of National Family Health Survey (NFHS, 2019–21), the biggest demographic and health survey (DHS) of India, abdominal obesity was assessed through waist circumference for the first time. This study was done on NFHS 5 data to estimate the prevalence of abdominal obesity in India, particularly amongst the women. The prevalence of abdominal obesity was found to be high in India. Overall, 40% of women and 12% of men are abdominally obese in the country, but 49.3% of women in the age group of 30–39 and 56.7% of women in the age group of 40–49 cross the cut-off mark. Measured on BMI, only 23% of the women cross the cut-off mark for obesity. Thus, some women who have healthy BMI also happen to have abdominal obesity. High prevalence is found in southern states of Kerala (65.4%) and Tamil Nadu (57.9%) and northern states of Punjab (62.5%) and Delhi (59%). Low prevalence is found in the states of Jharkhand (23.9%) and Madhya Pradesh (24.9%). Abdominal obesity is found to be associated with older age groups, urban residents, wealthier sections of the society, non-vegetarians, and the religious minority of Sikhs - for both men and women.
Implications of all the available evidence
High prevalence of abdominal obesity indicates an emerging health risk for Indian women. The findings of the study indicate a double burden of malnutrition in India. The government and other key stakeholders should take pro-active actions to design targeted interventions for the groups who have high abdominal obesity, particularly for the women in their thirties and forties.
Introduction
Obesity has emerged as a potential global public health threat, and its prevalence has been increasing since the beginning of the 21st century. As of 2016, more than 2 billion adults, representing 44 percent of the global adult population, were overweight or obese, with over 70 percent of them residing in low-income or middle-income countries (LMICs).1 This indicates that obesity is not limited to high-income countries or urban settings but is also prevalent in LMICs, where under-nutrition is persistent, posing a threat of double burden of malnutrition.2 It is crucial to address the growing prevalence of obesity in LMICs to prevent the adverse health consequences associated with it.
Obesity refers to the excessive accumulation of fat in the body, and the pattern of fat distribution plays a crucial role in determining metabolic risk. Based on the location of fat accumulation, there are two types of body forms which obese individuals generally exhibit: gynecoid or pear-shape (fat accumulation in lower body such as hips and thighs) and android or apple-shape (fat accumulation in the upper body such as the visceral or abdominal region).3 However, abdominal or visceral obesity, also known as central obesity, is considered the more serious form of fat distribution, as it predisposes individuals to various metabolic disorders and diseases. Asian Indians are more susceptible to abdominal obesity and accumulation of visceral fat, making them more vulnerable to associated health risks.4
Over the last three decades, multiple studies worldwide have raised awareness about abdominal obesity. In 1997, the WHO acknowledged the significance of abdominal obesity and proposed using indicators such as waist circumference to identify populations at a higher risk of abdominal obesity.5 Abdominal or central obesity is defined as having a waist circumference of more than 80 cm in women and more than 94 cm in men. It is a strong predictor of cardiovascular diseases, type-2 diabetes, and other metabolic disorders.6,7
Abdominal obesity has been on the rise globally since 1990,8 which calls for attention to be paid to this emerging characteristic to assess the potential risks of associated metabolic diseases in a community. There is ample evidence to suggest that abdominal obesity is a strong predictor of cardiovascular disease and type-2 diabetes. But BMI is the most widely used measure of determining obesity in clinical and research settings. BMI measures an individual's weight and height to classify them as normal, overweight, or obese. However, its diagnostic accuracy is debatable as it often leads to an inaccurate assessment of adiposity.9 Therefore, it is essential to incorporate additional indicators, such as waist circumference along with BMI to accurately assess the risk of obesity-related diseases.
Numerous studies have been conducted on abdominal obesity in different parts of India, but due to small sample sizes and region-specific focus, the studies were unable to provide an accurate overview of the situation in the country.10,11 National Family Health Survey is the largest demographic and health survey conducted in India. For the first time, the National Family Health Survey-5 (NFHS-5) conducted in 2019–21 measured abdominal obesity using waist circumference. The current study highlights the key findings of abdominal obesity prevalence and its distribution across various socio-economic segments in the country based on the NFHS-5 data. This study also sheds light on the socio-economic association of abdominal obesity in India and calls for evidence-based research on various aspects of abdominal obesity in the country. Policymakers are recommended to fund further research on abdominal obesity and associated factors to inform effective interventions.
Methods
NFHS-5 survey was conducted at a large scale and covered a representative sample of households throughout India. NFHS-5 survey was conducted from June 17, 2019, to April 30, 2021 in two phases owing to COVID-19 pandemic. The survey collected information from 636,699 households, 724,115 women and 101,839 men across all 36 states and union territories in India. The data on abdominal obesity obtained from this survey is crucial as it is the first time that waist circumference has been measured at the national level. NFHS-5 data was made available in the year 2022. First to fourth round of NFHS had measured general obesity through BMI measurement. In NFHS-5, abdominal or central obesity through waist circumference was measured for 6, 59,156 women and 85,976 men (aged between 15 and 49 years) across the country.
The definition of abdominal obesity used in the current study is based on waist circumference, which is considered a more accurate measure of abdominal obesity than the waist-to-hip ratio. In some people low waist-to-hip ratio could be a result of high hip circumference and vice-versa. Many studies have established the same too.12,13 The abdominal obesity has been defined as waist circumference of more than 80 cm in women and of more than 94 cm in men. The descriptive univariate analysis using the NFHS-5 dataset has been presented in the article. NFHS 5 data on the waist circumference of 659,156 women and 85,976 men, when treated for outliers at 3 SD has reduced to 655,328 women and 85,377 men respectively. The focus of the present study was on identifying the prevalence of abdominal obesity in different socioeconomic groups and examining the association between abdominal obesity and various demographic and economic factors, such as age, place of residence, level of education, religion, caste, wealth index, and type of diet.
Multivariable binary logistic regression was used to examine the relationship between the dependent variable (prevalence or non-prevalence of abdominal obesity) and the independent variables (socioeconomic factors such as age, place of residence, level of education, religion, caste, wealth index and type of diet). Multivariable binary logistic regression allowed the examination of the association between the dependent variable and multiple independent variables simultaneously. Overall, the study's findings are essential in highlighting the prevalence of abdominal obesity in India and its association with different socioeconomic factors.
Role of funding source
Not applicable.
Results
Abdominal obesity was found to be more prevalent amongst the women in India. For women, a waist circumference >80 cm, and for men, waist circumference >94 cm was considered as abdominal obesity. Individuals with BMI >25 were considered as overweight and those with BMI >30 were considered as obese.
The demographic segregation of data depicts that compared to women (39.6%), the prevalence of abdominal obesity was lower in men (11.9%).
As per the NFHS-5 data, 23% of women and 22.1% of men are overweight as per the BMI criterion. The preliminary finding on the status of abdominal obesity reveals that 40% of women and 12% of men are abdominally obese in the country. It is found that the 22.1% of men tend to have BMI above the cut-off range and 11.9% of them have a WC above the cut-off range. For women it is found that 23% of women have BMI above the cut-off range of 25 and 39.6% of women have WC above the cut-off range of 80 cm. Abdominal obesity is a significant health concern for women in India, as many women with a healthy BMI still have excess abdominal fat, which increases their risk of metabolic diseases and other health complications. The prevalence of abdominal obesity among women in India is quite high, with about 4 in 10 women having a waist circumference higher than the prescribed cut-off mark for abdominal obesity (Table 1), which puts them at an increased risk of metabolic complications and non-communicable diseases. Several other studies have reported the similar pattern of gender disparity in obesity where findings reveal that women tend to be more abdominally obese than man.14
Table 1.
Prevalence of BMI and WC - a comparison.
| Obesity parameter | Women (%) (95% CI) |
N | Men (%) (95% CI) |
N |
|---|---|---|---|---|
| Waist circumference >80 cm for women and >94 cm for men | 39.6 (39.5–39.7) | 655,328 | 11.9 (11.7–12.1) | 85,377 |
| BMI ≥ 25 | 23 (22.9–23.1) | 649,421 | 22.1 (21.8–22.3) | 84,925 |
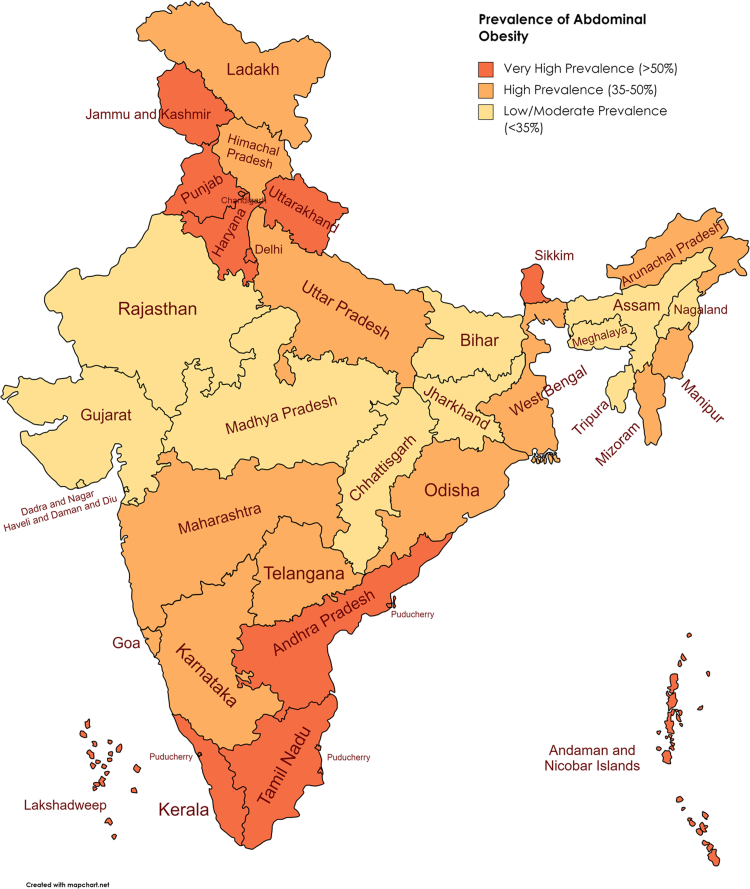
Regional segregation of data (Fig. 1) depicts that the range of the prevalence of abdominal obesity across states is 23.9%–65.4% in women and 1.8%–28.2% in men. More women are found to be obese in Southern states of Kerala (65.4%) and Tamil Nadu (57.9%) and northern states of Punjab (62.5%) and Delhi (59%). It is found to be less prevalent in the states of Jharkhand (23.9%) and Madhya Pradesh (24.9%). Kerala, Tamil Nadu, Punjab, and Delhi are generally considered to be more economically developed states in India compared to Jharkhand and Madhya Pradesh, which are relatively less developed. This is reflected in various socio-economic indicators such as per capita income, human development index, literacy rate, and access to basic amenities.15
Fig. 1.
Prevalence of abdominal obesity (waist circumference more than 80 cm) in women of age 15–49 years in Indian states.
Prevalence of abdominal obesity (as depicted by Table 2) for people residing in urban areas [women (W)-49.5% ± 0.2, men (M)-15.7% ± 0.4)] is higher than in those in rural areas (W-35% ± 14, M-10% ± 0.24). The prevalence of abdominal obesity is (W-56.7% ± 0.2, M-19.7% ± 0.5) in the adults belonging to the age group of 40–49, which is higher than those in the age group of 20–29 years (W-32.2% ± 0.2, M-7.4% ± 0.3). The older adults tend to be more obese than the younger ones. It is interesting to note that amongst the religious groups the prevalence was found to be less in the Buddhist (31.6% ± 1.4) and Jain women (43.1% ± 2.7) and was found to be more in the Sikh (61.8% ± 0.96) and the Christian women (48.1% ± 0.78). But the difference was not very pronounced in men.
Table 2.
Prevalence of abdominal obesity and general obesity in women and men, by background characteristics, India, 2019–21.
| S.No. | Background characteristics | Women |
Men |
||||||
|---|---|---|---|---|---|---|---|---|---|
| WC > 0.80 cm (95% CI) | N | BMI ≥ 25 (95% CI) | N | WC > 0.94 cm (95% CI) | N | BMI ≥ 25 (95% CI) | N | ||
| 1 | Age | ||||||||
| 15–19 | 12.7 (12.5–12.9) | 111,870 | 5.1 (5–5.3) | 111,720 | 2.5 (2.3–2.8) | 14,945 | 6.2 (5.8–6.6) | 14,942 | |
| 20–29 | 32.2 (32–32.4) | 200,810 | 16.3 (16.1–16.4) | 199,734 | 7.4 (7.1–7.8) | 25,979 | 17.2 (16.8–17.7) | 25,833 | |
| 30–39 | 49.3 (49–49.5) | 183,796 | 30.7 (30.5–30.9) | 181,526 | 16 (15.5–16.5) | 24,093 | 29.4 (28.9–30) | 23,892 | |
| 40–49 | 56.7 (56.5–57) | 158,852 | 35.5 (35.2–35.7) | 156,441 | 19.7 (19.2–20.3) | 20,360 | 31.3 (30.6–31.9) | 20,258 | |
| 2 | Place of residence | ||||||||
| Urban | 49.5 (49.3–49.7) | 208,886 | 31.7 (31.5–31.9) | 205,565 | 15.7 (15.3–16.1) | 28,901 | 28.6 (28–29.1) | 28,592 | |
| Rural | 35 (34.8–35.1) | 446,442 | 19 (18.9–19.1) | 443,857 | 10 (9.8–10.3) | 56,477 | 18.8 (18.4–19.1) | 56,333 | |
| 3 | Level of education | ||||||||
| No education | 39.5 (39.2–39.7) | 150,314 | 20.9 (20.6–21.1) | 149,411 | 8.4 (7.9–9) | 9074 | 17.3 (16.5–18) | 9050 | |
| Primary | 42.6 (42.3–43) | 78,242 | 25 (24.7–25.3) | 77,438 | 9.7 (9.1–10.3) | 9987 | 17.2 (16.5–17.9) | 9955 | |
| Secondary | 37.3 (37.1–37.5) | 328,074 | 22.4 (22.3–22.6) | 324,859 | 11.7 (11.4–12) | 49,945 | 21.4 (21.1–21.8) | 49,659 | |
| Higher | 45.1 (44.7–45.4) | 98,699 | 26.7 (26.4–27) | 97,714 | 15.9 (15.3–16.5) | 16,371 | 29.7 (29–30.4) | 16,261 | |
| 4 | Religion | ||||||||
| Hindu | 38.3 (38.2–38.5) | 536,425 | 22.3 (22.2–22.4) | 531,741 | 12 (11.8–12.2) | 67,900 | 22.1 (21.7–22.4) | 67,539 | |
| Muslim | 44.1 (43.8–44.5) | 85,730 | 24.9 (24.6–25.2) | 84,897 | 9.6 (9.1–10.1) | 13,115 | 20.2 (19.5–20.9) | 13,039 | |
| Christian | 48.1 (47.3–48.8) | 15,437 | 29.8 (29.1–30.6) | 15,222 | 16.9 (15.5–18.6) | 2250 | 27.8 (25.9–29.7) | 2234 | |
| Sikh | 61.8 (60.8–62.7) | 9864 | 37.5 (36.5–38.5) | 9732 | 21.1 (18.3–24.3) | 729 | 27.7 (24.6–31.1) | 725 | |
| Buddhist | 31.6 (30.2–33.1) | 4142 | 20.2 (19–21.5) | 4123 | 17.9 (15.6–20.5) | 929 | 27.2 (24.4–30.1) | 936 | |
| Jain | 43.1 (40.4–45.8) | 1263 | 29.8 (27.3–32.4) | 1247 | 17.6 (13.1–23.3) | 218 | 22.6 (17.5–28.6) | 217 | |
| Others | 25.6 (24–27.4) | 2468 | 13 (11.7–14.4) | 2460 | 15.2 (11.2–20.4) | 237 | 34.3 (28.6–40.6) | 236 | |
| 5 | Caste/Tribe | ||||||||
| Schedule Caste | 37.7 (37.5–38) | 143,968 | 20.7 (20.5–20.9) | 143,003 | 11.2 (10.7–11.6) | 17,554 | 19.9 (19.3–20.5) | 17,479 | |
| Schedule Tribe | 24.4 (24.1–24.8) | 61,555 | 12.2 (11.9–12.4) | 61,362 | 6.1 (5.6–6.7) | 7961 | 14.4 (13.6–15.1) | 7946 | |
| Other backward class | 39.5 (39.3–39.7) | 281,304 | 23.6 (23.4–23.7) | 278,579 | 12.6 (12.3–12.9) | 35,701 | 23.4 (23–23.9) | 35,563 | |
| Other | 48.2 (47.9–48.4) | 132,764 | 29.6 (29.3–29.8) | 131,075 | 15.4 (14.9–16) | 17,434 | 26.5 (25.9–27.2) | 17,248 | |
| 6 | Wealth Index | ||||||||
| Poorest | 23.7 (23.5–23.9) | 121,596 | 9.7 (9.5–9.9) | 121,271 | 4 (3.7–4.3) | 14,616 | 9.1 (8.6–9.6) | 14,574 | |
| Poorer | 31.8 (31.6–32.1) | 132,914 | 15.9 (15.7–16.1) | 132,383 | 6.7 (6.3–7) | 17,275 | 14.4 (13.9–14.9) | 17,237 | |
| Middle | 39.5 (39.3–39.8) | 136,570 | 22.9 (22.7–23.2) | 135,588 | 11.1 (10.6–11.5) | 18,423 | 21.2 (20.6–21.8) | 18,372 | |
| Richer | 46.7 (46.5–47) | 136,763 | 29.2 (29–29.5) | 135,112 | 16.6 (16.1–17.2) | 18,870 | 28.9 (28.3–29.6) | 18,765 | |
| Richest | 55.3 (55–55.6) | 127,485 | 36.8 (36.6–37.1) | 125,066 | 20.2 (19.6–20.8) | 16,194 | 35.1 (34.4–35.9) | 15,978 | |
| 7 | Type of diet | ||||||||
| Vegetarian/Occasionally non-vegetarian | 36.4 (36.2–36.6) | 304,945 | 20.9 (20.8–21.1) | 302,469 | 11.7 (11.4–12.1) | 28,707 | 20.6 (20.1–21) | 28,560 | |
| Non-vegetarian | 42.4 (42.2–42.5) | 350,383 | 24.8 (24.7–25) | 346,952 | 12 (11.8–12.3) | 56,670 | 22.8 (22.5–23.2) | 56,365 | |
| Total | 39.6 (39.5–39.7) | 655,328 | 23 (22.9–23.1) | 649,421 | 11.9 (11.7–12.1) | 85,377 | 22.1 (21.8–22.3) | 84,925 | |
Economic group data depicts that there is a higher prevalence of abdominal obesity amongst the wealthier sections of the Indian population. Of the total obese adults, more than half (W-51.8%, M-63%) fell in the top two richer quintiles. Abdominal obesity was less prominent in tribal population (W-24.4% ± 0.3, M-6.1% ± 0.5). The women who attained higher education (W-45.1% ± 0.3, M-15.9% ± 0.5) were more obese compared to men with the higher education. Women who consumed non-vegetarian diet (42.4% ± 0.16) had more of abdominal obesity than women who consumed vegetarian food or take an occasional non-vegetarian diet (36.4% ± 0.17). However, this difference in abdominal obesity for the diet type or level of education was not evident in men (Table 2).
We found that the abdominal obesity in women sets in during age 30–49 years. In the age group of 15–19, only 12.7% of the women were abdominally obese. When women reached the age of 20–29 years, 32.2% of the women were found to be abdominally obese. The prevalence of abdominal obesity increases to 49.3% of women during age 30–39 years and 56.7% of women are abdominally obese during age 40–49 years. As per the BMI measure, 16.3%, 30.7% and 35.5% of women are overweight during age 20–49 years. There is a tendency to acquire abdominal obesity much easier than the general obesity, as women age. This finding is consistent with the results of a longitudinal study conducted in the USA which showed that prevalence of abdominal obesity was almost double that of general obesity.9
One striking finding of the present study is that the prevalence of abdominal obesity was higher in older age groups and urban residents for both men and women, with twice as much prevalence among older adults compared to younger adults. Since the NFHS-5 survey only covered women aged 15–49 years, the study was unable to determine the status of obesity in women above 50 years. However, other studies conducted globally have reported a higher prevalence of abdominal obesity in older age groups compared to their younger counterparts.16 This trend is attributed to a decline in resting metabolic rate, hormonal changes, and reduced physical activity.17 Also, such a trend is likely to continue, as younger obese adults age into older adults. Therefore, there is a need for strong and strategic population-level interventions to reverse the trend of abdominal obesity increasing with age. It has been estimated that the number of overweight and obese individuals in India will increase considerably by 2040, particularly among rural residents and older Indians.18 India is currently undergoing demographic transition,19 and it is necessary to explore the factors affecting abdominal obesity separately among younger and older populations.
It is worth noting that the prevalence of obesity among women in India varies significantly across different states. However, there is not much variation in the prevalence of obesity among men across different states. The demographic profile, socioeconomic distribution, cultural and dietary practices, the status of physical activities in the population and the interplay of all these variables could possibly explain such high variation of abdominal obesity in Indian women across Indian states. Jharkhand state has highest proportion (65%) of poor households in the country in the NFHS-5 survey sample, while more than three-fourth of population in Kerala and Punjab belongs to the richer section in the survey sample.20 This indicates that economic prosperity differentials amongst Indian states, rather than the geography, is a marker for abdominal obesity. However, other factors like cultural diversity, food habits, and status of physical activity across states also need to be studied further.
Among the religious groups, the Sikh community emerged as abdominally obese (W-61.8%, M-21.1) group, followed by Christian women (48.1%) and Buddhist (17.9%) men. Upon further segregation of data, it was found that majority of the Sikh respondents (80%) belonged to the top two wealth quintiles of the society, further indicating economic prosperity as one of the markers.20 There is evidence to suggest that religious groups may reflect the combined effects of cultural practices, economic conditions, livelihoods, and dietary preferences on obesity. However, it is important to note that the relationship between religion and obesity is complex and multi-factorial. Factors such as genetics, age, gender, and socioeconomic status can also play a role in the development of obesity. To better understand the relationships between religious beliefs, lifestyle factors, and abdominal obesity, further research is needed across different religious groups in the country. This may involve examining dietary habits, physical activity levels, and other lifestyle factors in different religious communities, as well as exploring the cultural and social factors that contribute to these behaviours.
Socioeconomic factors and waist circumference - multivariable logistic regression
To understand the association of socioeconomic factor and waist circumference, multivariate logistic regression is applied. Those socio-economic groups which have higher prevalence of central obesity also reported a stronger association with higher values of waist circumference. The results of descriptive statistic and multivariate logistic regression are concurrent (Table 3).
Table 3.
Multivariable logistic regression of abdominal obesity among women 15–49 years on socio-economic determinants.
| Sbr | Background characteristics | Odds Ratio | 95% CI | SE | z-score | P > z |
|---|---|---|---|---|---|---|
| 1 | Age | |||||
| 15–19 years | 1.00 | |||||
| 20–29 years | 3.20 | (3.13–3.26) | 0.035 | 107.54 | 0 | |
| 30–39 years | 7.14 | (6.99–7.29) | 0.078 | 180.9 | 0.000 | |
| 40–49 years | 10.16 | (9.93–10.39) | 0.117 | 202.02 | 0.000 | |
| 2 | Place of residence | |||||
| Urban | 1.00 | |||||
| Rural | 0.88 | (0.87–0.9) | 0.006 | −17.66 | 0.000 | |
| 3 | Level of education | |||||
| No education | 1.00 | |||||
| Primary | 1.17 | (1.15–1.2) | 0.012 | 16.01 | 0.000 | |
| Secondary | 1.24 | (1.22–1.26) | 0.010 | 26.12 | 0.000 | |
| Higher | 1.21 | (1.18–1.23) | 0.013 | 16.85 | 0.000 | |
| 4 | Religion | |||||
| Hindu | 1.00 | |||||
| Muslim | 1.28 | (1.26–1.3) | 0.012 | 26.37 | 0.000 | |
| Christian | 1.38 | (1.33–1.43) | 0.026 | 17.02 | 0.000 | |
| Sikh | 2.03 | (1.94–2.12) | 0.047 | 30.73 | 0.000 | |
| Buddhist | 0.55 | (0.51–0.59) | 0.020 | −16.26 | 0.000 | |
| Jain | 0.70 | (0.61–0.8) | 0.047 | −5.3 | 0.000 | |
| Others | 0.99 | (0.89–1.09) | 0.052 | −0.26 | 0.793 | |
| 5 | Caste/Tribe | |||||
| Schedule Caste | 1.00 | |||||
| Schedule Tribe | 0.60 | (0.59–0.62) | 0.007 | −42.93 | 0.000 | |
| Other backward class | 0.93 | (0.92–0.95) | 0.007 | −9.21 | 0.000 | |
| Other | 1.10 | (1.09–1.12) | 0.010 | 11.19 | 0.000 | |
| 6 | Wealth Index | |||||
| Poorest | 1.00 | |||||
| Poorer | 1.41 | (1.39–1.44) | 0.014 | 34.99 | 0.000 | |
| Middle | 1.84 | (1.81–1.88) | 0.018 | 61.57 | 0.000 | |
| Richer | 2.34 | (2.29–2.39) | 0.025 | 81.09 | 0.000 | |
| Richest | 3.10 | (3.03–3.17) | 0.037 | 95.46 | 0.000 | |
| 7 | Diet | |||||
| Vegetarian/Occasionally Non-vegetarian | 1.00 | |||||
| Non-vegetarian | 1.27 | (1.26–1.29) | 0.007 | 40.78 | 0.000 |
The odds of high waist circumference in the age group of 40–49 years are ten times more than the adolescents. Female residents of rural areas are less likely to have abdominal obesity. Education is not a defining factor for abdominal obesity in women. The odds of Sikh women being abdominally obese are higher than that of the Hindu, Jain, or Buddhist women. As the households become wealthy, the women have greater odds of acquiring abdominal obesity. The women consuming non-vegetarian food have higher odds of being abdominally obese. Women belonging to scheduled tribes have lesser odds of acquiring abdominal obesity. The sample size of NFHS-5 is large, and the prevalence of abdominal obesity was found to be high in specific socio-economic groups. When examined for association of socio-economic groups with abdominal obesity, the results are concurrent with prevalence statistic.
Given the vast geography, heterogeneous habitat, and immense cultural diversity in India, conducting extensive research on the patterns and key drivers of abdominal obesity and their mutual interactions is essential. Such research can help identify effective interventions to prevent and treat abdominal obesity in different populations, considering the unique cultural, economic, and regional factors that contribute to this condition. The NFHS 5 data showing a diverse pattern of abdominal obesity across age, social and economic segregations highlights the need for further research on the underlying factors contributing to this trend. To better understand these factors, it is important to conduct studies that examine dietary practices, lifestyle variables, genetic structures, and their interactions among different age groups, urban and rural populations, wealthy and non-wealthy sections, and male and female populations in India. Moreover, regional, cultural, and economic dimensions also play a crucial role in determining the key drivers of abdominal obesity for various sections of society in India. Therefore, it is necessary to explore the unique cultural, economic, and regional factors that contribute to abdominal obesity among different groups in the country.
Discussion
Obesity is a result of energy imbalance in the body, where the energy intake from food exceeds the energy expenditure through physical activity. Maintaining a balance between energy intake and expenditure is essential to prevent the deposition of excess fat mass in the body. It is recommended to perform certain physical activities to expend excess amount of energy. A recent study on the pattern of physical activity in India revealed that a significant proportion of the Indian population (57%) is physically inactive or only mildly active, and females are less physically active than males.21 Physical inactivity is highest amongst the South Indian population (72%), making South zone more vulnerable to obesity and subsequently to chronic illnesses. The rural economy is undergoing an economic transition and has resulted in withdrawal of significant proportion of female workforce from economic activity. This also indicates the possibility of decreased physical activity in women, particularly, in rural areas.22 Few studies have established that transition from agricultural labour to wage labour, decreases the physical activity of women, rather than men.14 These findings underscore the importance of promoting physical activity, particularly among women. Encouraging regular physical activity can help individuals maintain a healthy weight and reduce the risk of chronic diseases associated with obesity. Policymakers and healthcare providers must prioritize initiatives that promote physical activity and encourage individuals to lead active lifestyles.
In India, scheduled castes and scheduled tribes are attributed to be the most disadvantaged socioeconomic groups. The findings of the present study suggest that the schedule tribes have a lesser prevalence of obesity, amongst the social groups. Abdominal obesity is not found to be strongly associated with the scheduled tribes in India, which comprise 8.08% of the Indian population. Many studies have indicated a high prevalence of malnutrition among adults and children of scheduled tribes. According to other studies, some key factors contributing to malnutrition among the scheduled tribes are low scores on wealth index, low access to health services and lack of education.23,24 As per NFHS-5 data, about 24% of the women from scheduled tribes have high waist circumference, and 12% of these women have high BMI. Amongst the men from scheduled tribes, the prevalence of abdominal obesity is 6.1%, which is low, but 14.4% have high BMIs. Indeed, as individuals move higher on the wealth index and secure better access to health services, they may become more vulnerable to abdominal obesity, particularly women in these social groups. The current study provides some indication of a possibility of scheduled tribe population also moving towards abdominal obesity in future. Further studies on specific social groups such as scheduled tribes, would provide a comprehensive analysis of unique health risks arising out of double burden of malnutrition. The policy research and action focus should be on preventing specific social groups as scheduled tribes to acquire abdominal obesity.
Amongst the religious ethic groups, Sikh women have a stronger association with obesity, in comparison to Hindu, Jain, or Buddhist women. Sikhs are a religious minority in India. Comprising of 1.72% of the population, most Sikhs are wealthy, and that is the reason why most of the Sikhs in the sample of NFHS-5 survey also make up to the higher wealth quintiles. As Sikhs make up a significant proportion of the population in Punjab, initiatives that specifically target this community can help address the issue of abdominal obesity. The Government of Punjab should take notice of the prevalence of high abdominal obesity amongst the women in the State of Punjab, and more specifically amongst the Sikh community. As for Jains and Buddhists, while they may follow an austere lifestyle, it is still important to monitor and address any potential health risks, including abdominal obesity. While they may be small religious and ethnic minorities, every community deserves access to healthcare and support for healthy lifestyle practices.
Obesity has conventionally been recognised as an issue pertaining to urban and wealthier sections of society. However, the NFHS-5 data highlights a considerable difference in obesity trends between urban and rural populations in India. This difference could be due to various factors, including changes in the rural economy and increased proximity to urban centres. As the share of agriculture in the overall occupational structure decreases and non-farm activities increase in the rural economy, there is a greater likelihood of rural residents being exposed to economic opportunities.22 This may lead to changes in food consumption habits and a shift towards processed foods, which are often high in calories and low in nutrients. About one-third of the women aged 15–49 years in rural areas are also found to be abdominally obese. The proximity to urban centres is also considered a determinant of rural obesity.25 Better accessibility to nearest town is likely to increase the exposure to economic opportunities. Changes in the food consumption habits happen when there is a better access to processed food supply chain, resulting in nutrition transition. Further enquiry into the factors determining abdominal obesity in rural women, and the interoperability aspect of nutrition transition, better access to food supply chain and lifestyle changes in rural areas is required. Understanding these factors is crucial for developing effective policies and initiatives to prevent and manage abdominal obesity in rural areas.
The wealth of the households emerged as a potential differentiator of abdominal obesity amongst the Indians. This is in concurrence with the findings of other studies which found higher prevalence of overweight/obesity among those having high standard of living (based on wealth score) in India.26 Reduced physical activity owing to organised work and mechanised transport, particularly for the wealthier sections of the society, has led to the adoption of a sedentary lifestyle. Consumption of fat-rich diet is one of the factors that explains the higher prevalence of abdominal obesity in the wealthier sections. As per a research study, higher-income groups consumed a diet where 32% of energy was derived from fat, while for the lower-income groups, only 17% of energy was derived from fat.27
Along with the economic development, the country is also undergoing nutrition transition, the replacement of brown rice with white rice, overconsumption of other refined/processed foods, carbohydrate rich diet, and increased consumption of vegetable oil, describes the nutrition transition in India. A study on dietary pattern in India, informs that the Indians consume 10% of the average total caloric intake from processed food. Urban households, in the highest income group, lead this nutrition transition with consumption of almost 30% of their total daily calories from processed food. Amongst the different regions of India, the calorie share of processed food is highest in South India.28
NFHS-5 report provides additional information on the diet pattern found in the country.20 The report reveals that majority of the Indians (W-71%, M-83%) are now non-vegetarians, who either regularly or occasionally consume egg or meat. About 45.2% of the women and 57.3% of the men consume egg or meat regularly, either daily or at least once in a week. Studies across the world have demonstrated that meat consumption is associated with abdominal obesity.29 Aerated drinks (sugar sweetened drinks), a potential contributor of obesity,30 is consumed regularly, at least once in a week by 15.5% of women and 24.6% of men in the country. The consumption is higher in urban areas (W-18.8%, M-29.4%) than it is in rural areas (W-13.9%, M-22.1%). Abdominal obesity was found to be more prevalent in the women who regularly (daily/weekly) consumed non-vegetarian food (42.4%) than those who were vegetarian or occasionally consumed non-vegetarian food (36.4%). But the same pattern was not found for men. Availability of rice and wheat as major staple crops, for the disadvantaged socio-economic groups through the public distribution system, has led to a better consumption of carbohydrates by them. The shift to unhealthy dietary practises, poor dietary diversity in food intake, physically inactive and sedentary lifestyle, predisposes a significant proportion of adults, particularly women to abdominal or central obesity. Indians are shifting to non-vegetarian diet, processed foods, aerated drinks, and carbohydrate and fat rich foods. Dietary transition is an important factor to be studied during economic transition. India has complex socio-economic-cultural heterogeneity. Family health surveys in India should cover in-depth information on dietary habits and physical activity in future. More data and research on these aspects will help the policy maker design better targeted public health interventions.
Men and women differ in the patterns of fat deposition and fat utilisation by the body.31 Women generally have a larger proportion of body fat mass as compared to men. Oestrogen has an effective role in distribution of fat deposition in women.32 It appears to be protective against abdominal fat deposition in women in reproductive age group but, the loss of oestrogens after menopause, independent of aging, makes women more vulnerable to abdominal obesity. The prevalence of lower sedentary metabolic rate in women compared to men,33 also explains prevalence of relatively higher abdominal obesity in women.
A comparison of BMI, waist circumference, and waist-to-hip ratio for the same population of women would be useful to identify those with a healthy BMI but high waist circumference. High BMI is an indicator of a metabolic risk.34 Many studies have examined whether middle-aged (30–49 years) weight gain in women is a function of aging or hormonal changes, and it has been found that the steady weight gain of half a kilogram annually during mid-life is due to age.32,34 Further research on Indian women with healthy BMI and high waist circumference will bring an inference on unique risks related to abdominal obesity in this segment of women. There is a need to conduct future research using all the three measures to enhance an understanding on the factors causing weight gain, be it hormonal changes during menopause, physical inactivity, or nutritional habits.35 A difference in estimates of BMI and waist circumference measures for women indicates that estimating BMI for a population is not enough; other measures should be included to understand their metabolic risk. Body mass index, waist circumference and waist-to-hip ratio are complementary measures and further exploration of the three measures will help the policy makers in designing better and targeted interventions, particularly for the women during age 30–49 years.
A literature review done for finding a relationship between overweight, obesity and related non-communicable diseases amongst Asian Indian girls and women concluded that abdominal obesity is higher in Asian Indians compared to white Caucasians and had an association with insulin resistance and multiple cardiovascular risk factors.8 Another review done on physical activity levels amongst South Asian women found that physical activity was particularly low amongst the South Asian women in the post pregnancy years, when caretaking duties were less.4
Obesity is a complex phenomenon, and its risk factors are numerous and mutually interactive.36 The increasing prevalence of abdominal obesity, particularly in middle-aged women, underscores the urgent need for further research to identify the driving factors of obesity and the contributing risk factors. Abdominal obesity is more prevalent among middle to older age groups, urban residents, wealthier sections of society, non-vegetarians, and those practising the Sikh religion. Moreover, the findings suggest that abdominal obesity is on the rise in rural areas and is penetrating lower and middle socioeconomic sections of society. Given that a significant proportion of the country's population lives in rural India, the burden of abdominal obesity and its associated risks could become overwhelming in no time. Therefore, a single strategy may not be effective given the socio-economic diversity of the country.37
Further research is needed to understand the health risks associated with abdominal obesity. Indians, particularly women, are more vulnerable to this type of obesity, putting them at significant risk of non-communicable diseases. The government and other key stakeholders should proactively consider designing targeted interventions to moderate the growing trend of abdominal obesity in India. The Health and Wellness Centres launched by the Government of India under Ayushman Bharat are a good start to introducing wellness programs in urban and rural areas. However, a major behaviour change program intervention for physical activity and nutritional patterns should be designed, aiming at the targeted sections of society.38
Contributors
MC - Study design, data interpretation, writing - final draft, writing - editing and reviewing. PS - Writing - original draft, data retrieval from NFHS-5, Preparation of figures and tables. MC, PS - Data analysis. Both authors approved the final version of the manuscript.
Data sharing statement
All data used in this analysis is available in the public domain (NFHS-5) downloaded from https://www.dhsprogram.com/.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
None.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2023.100208.
Appendix A. Supplementary data
References
- 1.Schneider P., Popkin B., Shekar M., et al. Health and economic impacts of overweight/obesity. 2020. Epub ahead of print 2020. [DOI]
- 2.Popkin B.M., Corvalan C., Grummer-Strawn L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395:65–74. doi: 10.1016/S0140-6736(19)32497-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gesta S., Tseng Y.H., Kahn C.R. Developmental origin of fat: tracking obesity to its source. Cell. 2007;131:242–256. doi: 10.1016/j.cell.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Joshi S.R. Metabolic syndrome - emerging clusters of the Indian phenotype. J Assoc Phys India. 2003 May;51:445–446. https://www.researchgate.net/publication/10568117 PMID: 12974423. [PubMed] [Google Scholar]
- 5.World Health Organisation (WHO) WHO; Geneva: 2008. Waist circumference and waist–hip ratio. Report of a WHO Expert Consultation. 8-11 December 2008. Archived from: https://www.who.int/publications/i/item/9789241501491. Accessed March 26, 2023. [Google Scholar]
- 6.Powell-Wiley T.M., Poirier P., Burke L.E., et al. Obesity and cardiovascular disease A scientific statement from the American heart association. Circulation. 2021;143:E984–E1010. doi: 10.1161/CIR.0000000000000973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Misra A., Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93:9–30. doi: 10.1210/jc.2008-1595. [DOI] [PubMed] [Google Scholar]
- 8.Wong M.C.S., Huang J., Wang J., et al. Global, regional and time-trend prevalence of central obesity: a systematic review and meta-analysis of 13.2 million subjects. Eur J Epidemiol. 2020;35(7):673–683. doi: 10.1007/s10654-020-00650-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Romero-Corral A., Somers V., Sierra-Johnson J., et al. Accuracy of body mass index to diagnose obesity in the US adult population. Int J Obes. 2008;32:959–966. doi: 10.1038/ijo.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahirwar R., Mondal P.R. Prevalence of obesity in India: a systematic review. Diabetes Metab Syndr. 2019;13(1):318–321. doi: 10.1016/j.dsx.2018.08.032. [DOI] [PubMed] [Google Scholar]
- 11.Pradeepa R., Anjana R.M., Joshi S.R., et al. Prevalence of generalized & abdominal obesity in urban & rural India- the ICMR-INDIAB study (Phase-I) [ICMR-INDIAB-3] Indian J Med Res. 2015;142:139–150. doi: 10.4103/0971-5916.164234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmad N., Adam S.I.M., Nawi A.M., et al. Abdominal obesity indicators: waist circumference or waist-to-hip ratio in Malaysian adults population. Int J Prev Med. 2016;7:82. doi: 10.4103/2008-7802.183654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kurpad S.S., Tandon H., Srinivasan K. Waist circumference correlates better with body mass index than waist-to-hip ratio in Asian Indians. Natl Med J India. 2003;16(4):189–192. https://pubmed.ncbi.nlm.nih.gov/14606765/ PMID: 14606765. [PubMed] [Google Scholar]
- 14.Kanter R., Caballero B. Global gender disparities in obesity: a review. Adv Nutr. 2012;3:491–498. doi: 10.3945/an.112.002063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ministry of Finance Economic survey of India 2022-23. 2023. https://www.indiabudget.gov.in/economicsurvey/ New Delhi.
- 16.Wong M.C.S., Huang J., Wang J., et al. Global, regional and time-trend prevalence of central obesity: a systematic review and meta-analysis of 13.2 million subjects. Eur J Epidemiol. 2020;35:673–683. doi: 10.1007/s10654-020-00650-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Villareal D.T., Apovian C.M., Kushner R.F., et al. Obesity in older adults: technical review and position statement of the American society for nutrition and NAASO, the obesity society. Obes Res. 2005;13:1849–1863. doi: 10.1093/ajcn/82.5.923. [DOI] [PubMed] [Google Scholar]
- 18.Luhar S., Timaeus I.M., Jones R., et al. Forecasting the prevalence of overweight and obesity in India to 2040. PLoS One. 2020;15:1–17. doi: 10.1371/journal.pone.0229438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saroha J. Demographic transition in India. Indian J Publ Health. 2017;4:193–198. http://ijrar.com/upload_issue/ijrar_issue_518.pdf [Google Scholar]
- 20.International Institute for Population Sciences (IIPS) and ICF . IIPS; Mumbai: 2021. National family health survey (NFHS-5), 2019-21: India. Archived from: http://rchiips.org/nfhs/NFHS-5Reports/NFHS-5_INDIA_REPORT.pdf. [Google Scholar]
- 21.Podder V., Nagarathna R., Anand A., et al. Physical activity patterns in India stratified by zones, age, region, BMI and implications for COVID-19: a nationwide study. Ann Neurosci. 2020;27:193–203. doi: 10.1177/0972753121998507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chand R., Srivastava S.K., Singh J. Changes in rural economy of India, 1971 to 2012: lessons for job-led growth. Econ Polit Wkly. 2017;52:64–71. https://www.niti.gov.in/sites/default/files/2021-08/5_EPW_Article_Changes_in_Rural_Economy_of_India_1971_to_2012.pdf [Google Scholar]
- 23.Mittal P.C., Srivastava S. Rural Remote Health; 2006. Diet, nutritional status and food related traditions of Oraon tribes of New Mal (West Bengal), India. Epub 2006 Apr 10. [DOI] [PubMed] [Google Scholar]
- 24.Van De Poel E., Speybroeck N. Decomposing malnutrition inequalities between Scheduled Castes and Tribes and the remaining Indian population. Ethn Health. 2009;14:271–287. doi: 10.1080/13557850802609931. [DOI] [PubMed] [Google Scholar]
- 25.Aiyar A., Rahman A., Pingali P. India's rural transformation and rising obesity burden. World Dev. 2021;138 doi: 10.1016/j.worlddev.2020.105258. [DOI] [Google Scholar]
- 26.Luhar S., Mallinson P.A.C., Clarke L., et al. Trends in the socioeconomic patterning of overweight/obesity in India: a repeated cross-sectional study using nationally representative data. BMJ Open. 2018;8:6–9. doi: 10.1136/bmjopen-2018-023935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shetty P.S. Nutrition transition in India. Publ Health Nutr. 2002;5:175–182. doi: 10.1079/phn2001291. [DOI] [PubMed] [Google Scholar]
- 28.Sharma M., Kishore A., Roy D., et al. A comparison of the Indian diet with the EAT-Lancet reference diet. BMC Publ Health. 2020;20:1–13. doi: 10.1186/s12889-020-08951-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang Y., Beydoun M.A. Meat consumption is associated with obesity and central obesity among US adults. Int J Obes. 2009;33:621–628. doi: 10.1038/ijo.2009.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luger M., Lafontan M., Bes-Rastrollo M., et al. Sugar-sweetened beverages and weight gain in children and adults: a systematic review from 2013 to 2015 and a comparison with previous studies. Obes Facts. 2018;10:674–693. doi: 10.1159/000484566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Power M.L., Schulkin J. Sex differences in fat storage, fat metabolism, and the health risks from obesity: possible evolutionary origins. Br J Nutr. 2008;99:931–940. doi: 10.1017/s0007114507853347. [DOI] [PubMed] [Google Scholar]
- 32.Leeners B., Geary N., Tobler P.N., et al. Ovarian hormones and obesity. Hum Reprod Update. 2017;23:300–321. doi: 10.1093/humupd/dmw045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ferraro R., Lillioja S., Fontvieille A.M., et al. Lower sedentary metabolic rate in women compared with men. J Clin Invest. 1992;90:780–784. doi: 10.1172/jci115951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Global BMI Mortality Collaboration. Di Angelantonio E., Bhupathiraju S., Wormser D., et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–786. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singh P.N., Arthur K.N., Orlich M.J., et al. Global epidemiology of obesity, vegetarian dietary patterns, and noncommunicable disease in Asian Indians. Am J Clin Nutr. 2014;100:359–364. doi: 10.3945/ajcn.113.071571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hruby A, Hu F.B. The epidemiology of obesity: a big picture. Pharmacoeconomics. 2015;33:673–689. doi: 10.1007/s40273-014-0243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khandelwal S., Reddy K.S. Eliciting a policy response for the rising epidemic of overweight-obesity in India. Obes Rev. 2013;14 Suppl 2:114–125. doi: 10.1111/obr.12097. [DOI] [PubMed] [Google Scholar]
- 38.NHSRC Ayushman BHARAT:Comprehensive primary health care through health and wellness centers. 2018. https://www.nhm.gov.in/ New Delhi.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.