Abstract
Objective
As personality changes and personality disorders are frequently observed in multiple sclerosis (MS), personality may be a prognostic factor for this disease. The present study investigated the influence of personality on disability, progression, and treatment adherence in MS.
Method
Personality was assessed in 41 patients with Relapsing–Remitting MS (30 females; mean age = 42.63 years) using the NEO Personality Inventory—3rd edition. Disability was measured with the Expanded Disability Status Scale, and treatment adherence information was collected from the Swiss MS Cohort. Correlation, multiple linear and partial least square regressions were performed to examine relations between personality, disability, and treatment adherence in MS.
Results
After accounting for age and time since disease onset, our analysis revealed that Neuroticism (β = 0.32, p = 0.01) and its Vulnerability facet (β = 0.28, p < 0.05) predicted greater disability, whereas Extraversion (β = −0.25, p = 0.04) and its Activity facet (β = −0.23, p < 0.05) predicted milder disability. Regarding disability progression, correlational analysis revealed that it was negatively correlated with Extraversion (r = −0.44, p = 0.02) and the Feelings facet of Openness (r = −0.41, p = 0.03), but regressions failed to highlight any predictive links. No significant results could be demonstrated for treatment adherence.
Conclusions
Overall, our study showed that some personality traits can impact disability in MS, indicating that these should be considered in clinical practice, as they could be used to adapt and improve patients’ clinical support.
Keywords: Multiple sclerosis, Personality and personality disorders, Disability/handicaps
Introduction
The influence of personality on clinical outcomes has been studied in several chronic pathologies, notably coronary heart disease, where some personality traits have been associated with a poor clinical prognosis (Kupper & Denollet, 2018; Williams et al., 2008). Given the frequent personality changes and personality disorders in multiple sclerosis (MS; Stathopoulou, Christopoulos, Soubasi, & Gourzis, 2010), it seems relevant to consider the role of personality in this disease. In their review, Stathopoulou and coworkers described the personality profiles of people with MS and highlighted changes characterized by increased irritability, agitation and apathy, as well as higher rates of psychiatric disorders, including personality disorders, owing to both brain damage and the psychosocial impact of chronic illness. The role of this variable is especially relevant as Personality, which refers to individual differences in tendencies to manifest coherent and systematic configurations of thoughts, emotions, and actions (McCrae & John, 1992), has been linked to several health variables (Strickhouser, Zell, & Krizan, 2017). In their meta-synthesis, Strickhouser and coworkers highlighted many associations between personality, as measured by the Five Factor Model (FFM; McCrae & John, 1992), and health, especially mental health in the general population. More specifically, they showed that the personality factors described by the FFM (i.e., Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness) are particularly relevant for predicting mental health. However, it appears relevant to investigate the role of personality in physical health and health-related behavior, as studies have shown that the Type D personality, which is associated with a high level of Neuroticism and a low level of Extraversion (De Fruyt & Denollet, 2002), is a risk factor for coronary heart disease, owing to less adaptive health-related behavior (Kupper & Denollet, 2018; Williams et al., 2008).
In MS, personality seems especially important, for in addition to frequent personality changes and disorders, patients have more dysfunctional personality profiles, characterized by low levels of Conscientiousness, Extraversion, and Agreeableness, and a high level of Neuroticism (Maggio et al., 2020). These profiles, especially those with a high level of Neuroticism, have been linked to several personality disorders (Widiger, Trull, Clarkin, Sanderson, & Costa, 2002). It has been suggested that these personality dysfunctions are influenced by other psychopathologies that are frequently observed in MS, notably anxiety and depression (Bruce & Lynch, 2011). Research on the impact of personality on quality of life has shown that Type D personality is associated with greater MS disability (Demirci, Demirci, & Demirci, 2017). Moreover, several studies in MS have highlighted links between personality and health-related behavior such as treatment adherence. For instance, one study showed that patients with MS who have Type D personality have poorer disease management and treatment adherence (Strober, 2017), whereas another found that high Neuroticism and Openness, as well as low Conscientiousness, were associated with poorer treatment adherence (Bruce, Hancock, Arnett, & Lynch, 2010). However, while there is some evidence that personality traits might influence MS disability (Demirci et al., 2017), their impact on disease progression has not yet been assessed. Furthermore, the previously mentioned role of personality in treatment adherence was assessed using questionnaires (i.e., subjectively), and to our knowledge, no study has so far highlighted links between personality and treatment adherence using objective measures. Finally, personality in MS is often studied via short questionnaires targeting Type D personality traits, neglecting the other personality traits described by the FFM. Similarly, most studies in the field of personality in MS have focused mainly on the five factors and have seldom investigated particular facets that represent more specific aspects of personality, which could serve as more precise prognostic indicators.
The aim of the present study was therefore to investigate the impact of the personality traits (factors and facets) identified in the FFM on the disability associated with MS, as well as on disability progression and treatment adherence, in patients drawn from the Swiss MS Cohort. We tested three hypotheses. First, based on previous reports of associations between personality and MS (Demirci et al., 2017), we expected some personality traits to be linked to higher scores on the Expanded Disability Status Scale (EDSS; Kurtzke, 1983), and some to be linked to milder symptoms (i.e., lower EDSS). Second, based on the literature showing associations between Type D personality and poorer clinical prognosis in patients with chronic heart disease (Kupper & Denollet, 2018), we expected to find similar associations between personality and another chronic disease, namely MS, with some personality traits being associated with a favorable progression. Third, in line with the literature on treatment adherence and Type D personality in MS (Strober, 2017), we expected to find associations between some personality traits and treatment adherence levels.
Materials and Methods
Participants
All individuals included in this study belonged to the Swiss MS Cohort, a prospective observational study involving seven Swiss MS centers that collect neurological, radiological, and biological samples from patients with MS every 6–12 months (Disanto et al., 2016) and had a confirmed MS diagnosis. We sent the French version of the NEO Personality Inventory—3rd edition (NEO-PI-3; McCrae, Costa, & Martin, 2005), along with a description of the study, to 125 patients, 47 of whom responded. Our final sample included 41 patients with Relapsing–Remitting MS (30 women and 11 men), as six patients had to be excluded on account of missing EDSS data, incomplete personality questionnaires, or because they had progressive forms of MS. Detailed sample characteristics are provided in Supplementary data (Supplementary Table 1).
Ethics
The study was conducted in accordance with the Declaration of Helsinki, and the study protocol was approved by the Cantonal Ethics Committee of Geneva (2018-00218).
Measures
Personality/NEO-PI-3
All participants responded to the NEO-PI-3 (McCrae et al., 2005), a validated questionnaire that measures the five major factors of personality: Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness. Each of these broad factors is composed of six specific facets (see Supplementary Tables 3–7, 9–13, and 15–19). Participants responded to 240 items on a scale ranging from 1 (strongly disagree) to 5 (strongly agree). Combinations of these five factors and 30 facets allowed to conduct an exhaustive assessment of personality.
Disability and progression/EDSS
We used the EDSS (Kurtzke, 1983) to assess disability and progression. This scale measures the level of disability caused by MS based on different functional systems that are independent of each other, but which together reflect neurological disorders in MS. Levels range from 0 (= no disability) to 10 (= death caused by MS). We extracted EDSS scores from the Swiss MS Cohort. To obtain a measure of disability progression, we subtracted patients’ most recent EDSS score from their oldest available one (i.e., 4 years earlier). We called this variable delta EDSS (for similar calculation see Iaffaldano et al., 2021; Malekzadeh et al., 2019).
Treatment adherence
Treatment adherence data were extracted from the Swiss MS Cohort, which provided information about treatment interruptions and their causes. This information was collected by the patient’s treating physician at each visit (for more details see Disanto et al., 2016). To create our variable, we summed the number of interruptions or changes in treatment for which no specific reasons (e.g., adverse event because of treatment or pregnancy) were given.
Analysis
Analyses were run with JASP 0.16.1.0 and XLSTAT 2022.
Association measures
As we wanted to highlight associations between personality and disability, progression, and treatment adherence in MS, we started our analysis with association measures. Some of our data were not normally distributed (Shapiro < 0.05), so we calculated Spearman’s correlation coefficient. We performed three independent analyses, one for each of our dependent variables (EDSS, delta EDSS, and treatment adherence). For each analysis, we also included the variables of age and time since disease onset (number of years since first symptoms), as these variables can influence MS disability (Manouchehrinia, Beiki, & Hillert, 2017).
Prediction measures
To test the predictive value of personality variables on our dependent variables, we performed two kinds of regression. Multiple linear regressions (MLRs) were performed to test the influence of the five personality factors on our dependent variables, controlling for the influence of age and time since disease onset. Classic MLRs were performed for the EDSS and delta EDSS variables. For treatment adherence, as there was rarely more than one treatment interruption, we coded treatment adherence as a categorical variable with two modalities (0 = no interruptions; 1 = one or more interruptions), and used a binary logistic MLR. For all MLRs, we used the stepwise method as the entry method. To highlight personality facets that might have an influence on our dependent variables, and because of our limited sample size, we performed partial least squares regressions (PLS-Rs), which can analyze data with numerous x variables (here, 30 facets) and multicollinearity (Wold, Sjöström, & Eriksson, 2001). To reduce the risk of overfitting (Andersen & Bro, 2010), for each PLS-R, we undertook variable selection using the PLS variable importance in the projection (VIP) method and the greater-than-one rule (see Chong & Jun, 2005). To identify relevant predictors in our final models, we used the regression coefficients. Again, for both the MLRs and PLS-Rs, we performed three independent analyses, one for each of our dependent variables, and in each analysis, we included age and time since disease onset as covariates.
Results
Correlations
EDSS
Spearman’s correlation coefficients showed that MS disability (EDSS) was positively correlated with age (r = 0.58, p < 0.01), time since disease onset (r = 0.54, p < 0.01), and the Anxiety (r = 0.33, p = 0.04) and Vulnerability (r = 0.34, p = 0.04) facets of Neuroticism. It was also negatively correlated with Extraversion (r = −0.40, p = 0.01) and its Activity facet (r = −0.34, p = 0.04).
Delta EDSS
Delta EDSS was negatively correlated with Extraversion (r = −0.44, p = 0.02) and with the Feelings facet of Openness (r = −0.41, p = 0.03).
Treatment adherence
Treatment adherence correlated positively with time since disease onset (r = 0.40, p = 0.01).
Multiple Linear Regressions
EDSS
The initial MLR model included the five factors of personality, age, and time since disease onset. To identify the most useful predictors, we conducted a stepwise regression. This showed that age (β = 0.38, p < 0.01), time since disease onset (β = 0.30, p = 0.03), Neuroticism (β = 0.32, p = 0.01), and Extraversion (β = −0.25, p = 0.04) yielded the lowest prediction error (RMSE = 1.07) and explained 55% (adjusted R2 = 0.54) of EDSS variance (see Fig. 1). Adding Openness, Agreeableness, and Conscientiousness did not improve the quality of the model, and they were therefore classified as nonsignificant predictors. The results of stepwise, forward, and backward regressions were all consistent.
Fig. 1.
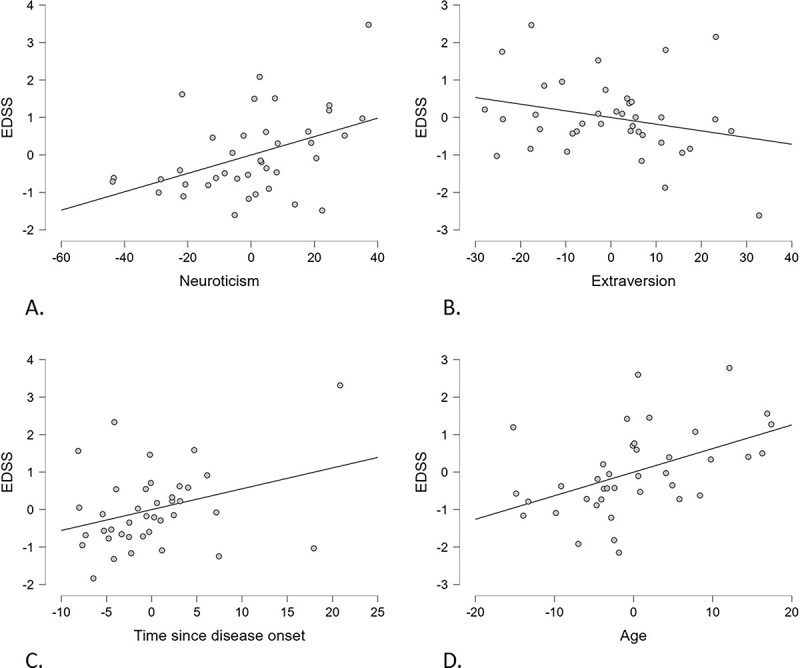
Regression lines and residuals for multiple linear regression (MLR), with Expanded Disability Status Scale (EDSS) score as a dependent variable. (A.) EDSS and Neuroticism: a higher Neuroticism score predicted a higher EDSS score. (B) EDSS and Extraversion: a higher Extraversion score predicted a lower EDSS score. (C) EDSS score and time since disease onset: a longer time since disease onset predicted a higher EDSS score. (D) EDSS and age: a greater age predicted a higher EDSS score.
Delta EDSS
The stepwise MLR with delta EDSS as the dependent variable showed that there was no meaningful predictor among our independent variables. The results of stepwise, forward, and backward regressions were all consistent.
Treatment adherence
The stepwise binary logistic MLR showed that the only meaningful predictor was age. However, it was not classified as a significant predictor (z = 1.42, p = 0.16). The results of stepwise, forward, and backward regressions were all consistent.
Partial Least Squares Regressions
EDSS
All 30 personality facets, as well as age, and time since disease onset, were initially included in the model. We used the PLS-VIP method with the greater-than-one rule to try to improve our model, and reran analysis including only the variables with a VIP > 1. Age and time since disease onset, together with the Activity and Vulnerability facets, were thus included in the final model (see Fig. 2). This allowed us to improve the model which, with one latent component, explained 53% of the variance in the EDSS score (R2 = 0.53) and had a predictive ability of 44% (Q2 = 0.44). Age, time since disease onset, Activity, and Vulnerability were classified as significant predictors (β = 0.29, p < 0.05; β = 0.32, p < 0.05; β = −0.23, p < 0.05; β = 0.28, p < 0.05).
Fig. 2.
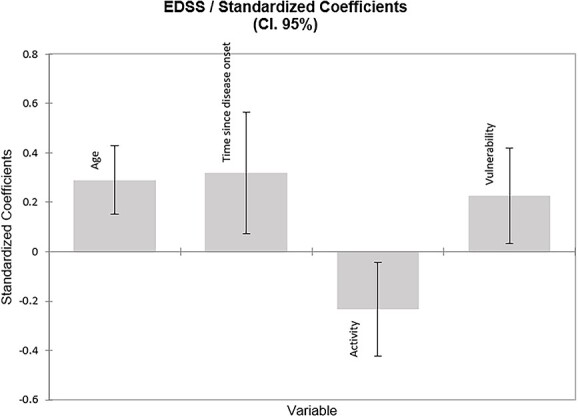
Regression coefficients of most useful variables selected by the partial least squares regression (PLS-R) for Expanded Disability Status Scale (EDSS) with all personality facets. Light gray = significant coefficient.
Delta EDSS
The final model included the age variable, the Openness facets Values, Fantasy, Feelings and Actions, the Extraversion facet Warmth, the Neuroticism facet Impulsiveness, the Agreeableness facets Compliance and Tender-Mindedness, and the Conscientiousness facet Competence (see Fig. 3). With one latent component, the model explained 42% of delta EDSS variance (R2 = 0.42) and had a predictive ability of 15% (Q2 = 0.15). Only age was classified as a significant predictor (β = 0.12, p < 0.05). The others had nonsignificant coefficients (β < −0.18, p > 0.05).
Fig. 3.
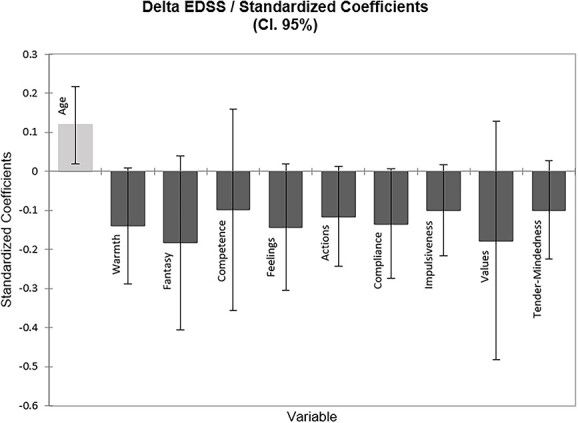
Regression coefficients of the most useful variables selected by the partial least squares regression (PLS-R) for delta Expanded Disability Status Scale (EDSS) with all personality facets. Light gray = significant coefficient.
Treatment adherence
The final model included the Extraversion facet Excitement-Seeking, the Agreeableness facet Modesty, the Conscientiousness facets Achievement-Striving, and the Neuroticism facet Self-Consciousness (see Fig. 4). With one latent component, the model explained 21% (R2 = 0.21) of treatment adherence variance, and had a predictive ability of 6% (Q2 = 0.06). None of the variables were classified as significant predictors (β < ± 0.23, p > 0.05).
Fig. 4.
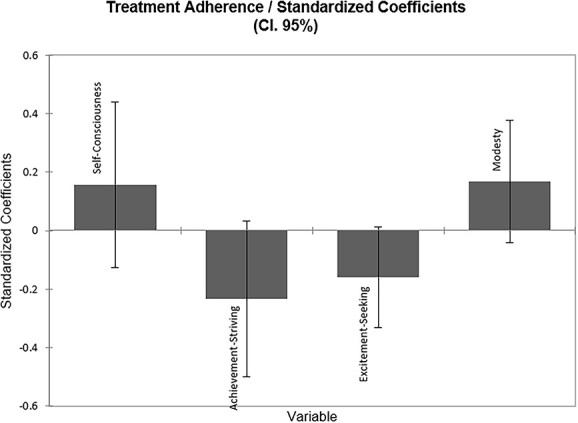
Regression coefficients of most useful variables selected by the partial least squares regression (PLS-R) for treatment rupture with all personality facets. Light gray = significant coefficient.
Discussion
The main objective of the present study was to highlight and specify the role of personality in the disability associated with MS, as well as in disability progression and treatment adherence. Results indicated that several personality variables were relevant predictors to consider, and the facets analysis allowed us to speculate on potential associations behind the role of personality in MS, with a discussion about the possible involvement of reserve and coping.
Regarding MS disability, Neuroticism and Extraversion were highlighted as significant predictors, the former being associated with higher disability and the latter with milder disability. These results are in line with studies assessing Type D personality, which have shown that Type D characteristics, namely, affective negativity and social inhibition, which are positively correlated with Neuroticism and negatively correlated with Extraversion (De Fruyt & Denollet, 2002), are associated with poorer clinical outcomes in MS, as well as in coronary heart disease (Demirci et al., 2017; Kupper & Denollet, 2018; Strober, 2017). While Neuroticism has already been associated with poorer disease management and greater psychological difficulties in MS (Strober, 2017), to our knowledge, the protective role of Extraversion regarding these aspects has only been highlighted through its negative correlation with Type D personality. Moreover, the PLS analysis revealed that of all the personality facets, only the Activity facet of Extraversion and the Vulnerability facet of Neuroticism were significant predictors of MS disability. One of the main objectives of the present study was to identify more precise personality variables (i.e., facets instead of factors) that would help us understand the role of personality in MS. Interestingly, the two facets highlighted by the PLS analysis belong to the personality factors that are most often cited in the MS literature, namely, Extraversion and Neuroticism. We can therefore surmise that the known role of these factors can in large part be explained by the facets highlighted in our study. In other words, the effects of Extraversion and Neuroticism would be strongly influenced by their Activity and Vulnerability facets. The involvement of Activity suggests that the protection afforded by Extraversion is mainly associated with the characteristics of this facet (i.e., need to stay occupied and live at an intense and lively pace). Interestingly, research has indicated that premorbid physical activity protects against disability progression, as measured by a self-reported scale (Motl, Dlugonski, Pilutti, Sandroff, & McAuley, 2012). Given the definition of this particular facet, it would be interesting to read these results in the light of another interesting concept that is often discussed in MS, namely, reserve (cognitive/brain reserve and brain maintenance). Reserve can be seen as a general protection against manifestations of brain damage (Stern, 2009; Stern et al., 2020), and as this protection is thought to be associated with life experiences, occupational exposure, and leisure activities (Stern, 2009), persons with higher Activity scores, who tend to engage in more sustained and vigorous activity in their everyday lives, may have greater reserve, thus protecting them from more severe disability. The concept of reserve is even more relevant in MS, as gray or white matter damage is not always associated with observable manifestations such as cognitive deficits (Sandroff, Schwartz, & DeLuca, 2016), and studying its potential association with personality could help to improve rehabilitation programs. Nevertheless, it is important to bear in mind that the association between Activity and disability may well be bidirectional, as Activity may lessen as physical and cognitive limitations increase.
The involvement of Vulnerability suggests that the negative impact of Neuroticism is especially associated with individuals’ perceived ability to cope with difficult or stressful situations. Interestingly, one study linked Neuroticism to resilience in a sample of college students, and suggested that the Vulnerability facet is, by definition, associated with less resilience (Campbell-Sills, Cohan, & Stein, 2006). These authors also highlighted an association between resilience and coping strategies. There is a vast literature regarding the impact of personality on coping, with various associations observed between the Big Five and different coping strategies (Watson & Hubbard, 1996). If we consider the definition of coping, the involvement of the Vulnerability facet could potentially be explained by coping abilities, as the individual’s perception of available resources is essential for managing external and/or internal demands in order to cope with stressful situations (Folkman, Lazarus, Dunkel-Schetter, DeLongis, & Gruen, 1986). The highlighting of the Vulnerability facet and its potential association with coping is particularly interesting, as it has been suggested that anxious and depressive disorders, which are frequent in MS (Magistrale & Nocentini, 2015; Théaudin & Feinstein, 2015), are related more to how individuals adjust to the adversity associated with disability than to the disability itself (Théaudin & Feinstein, 2015). Interestingly, our study indicated that the Vulnerability facet predicted disability itself, but it would be interesting to test the previously mentioned suggestion and see whether this association is mediated by adjustment to the disability (i.e., coping). A better understanding of the role of Vulnerability seems essential, if we are to properly support patients, as MS is a chronic and changing condition, meaning that patients constantly have to deal with the unpredictable course of the disease and its consequences.
We believe that highlighting the previously mentioned facets, as opposed to broad personality factors, is one of the strongpoints of our study. Although studying the five factors is useful for discerning patterns, it is also important to identify specific traits that might help to guide clinical management. Furthermore, given the frequent personality changes in MS, it is best not to assume that each factor structure will follow the one proposed by the model (i.e., strong correlation between each facet of a given factor). As highlighted by our correlation analysis, some factors have heterogeneous facets.
Regarding disability progression, no personality trait was classified as a significant predictor. Only correlational analysis yielded significant results, with a negative association between delta EDSS and Extraversion, as well as the Feelings facet of Openness (higher scores associated with milder progression). To our knowledge, although MS disability had already been associated with personality (Demirci et al., 2017), progression had never been assessed. Even if our study failed to highlight any significant predictors, we believe that personality should still be investigated when considering the progression of disability in MS, as the association with Extraversion highlighted by correlational analysis seems in line with the literature on Type D personality and our results regarding disability. As for the Feelings facet, even if Openness is mentioned less than Neuroticism and Extraversion, some studies have indicated that it is linked to better memory and lower risk of memory impairment in MS (Leavitt, Buyukturkoglu, Inglese, & Sumowski, 2017). This indicates the relevance of this personality factor and of its Feelings facet, which, as highlighted by our results, plays a potentially more specific role in the progression of disability.
Regarding treatment adherence, in contrast to previous studies assessing this variable (Bruce et al., 2010; Strober, 2017), no personality trait was classified as a significant predictor of the number of treatment interruptions. One possible explanation for this divergence is that previous studies of the association between personality and adherence relied on self-reported medication adherence (i.e., subjective measure), whereas we used an objective measure. Indeed, there has been some divergence between results yielded by objective versus subjective measures of adherence, with associations between personality and adherence being highlighted by adherence questionnaires and diaries, but not by objectives measures (Bruce et al., 2010).
Nevertheless, our results have to be interpreted with caution, as the present study had several limitations, beginning with its limited sample size. With a larger sample, other personality traits might have been highlighted, especially considering that some traits were close to significance in our study. Also, it is important to bear in mind that the characteristics of the respondents to the personality questionnaire and, more generally, of patients in the Swiss MS cohort may not be totally representative of the whole population of persons with MS. It is also important to consider that this study only included Relapsing–Remitting forms of MS, and the results may not be accurate for progressive forms. Moreover, we only had sufficient information on disability progression for a 4-year period. As MS is a disease that progresses over several decades, further studies are needed to explore the influence of personality on symptom progression over a longer period of time. Our short study period is a particular drawback, given that long-term worsening of disability, as measured by the EDSS, does not seem to be correlated with short-term worsening (Weinshenker, Issa, & Baskerville, 1996). Moreover, although the EDSS is widely used to estimate MS disability, it has often been criticized (Thompson & Hobart, 1998), notably because it is not a linear scale. Also, the score is essentially based on functional systems and walking, whereas cognitive and upper-limb deficits are given less consideration (Sharrack & Hughes, 1996). This represents a limitation, as cognitive deficits are frequently reported in MS and have a major impact on daily life (Chiaravalloti & DeLuca, 2008). Moreover, personality characteristics, such as a high level of Neuroticism and low levels of Agreeableness and Conscientiousness, have been associated with cognitive deficits, especially executive functions, as well as cortical atrophy (Benedict et al., 2008; Benedict, Priore, Miller, Munschauer, & Jacobs, 2001). It would therefore be useful to include such variables in future studies in order to fully understand the role of personality in MS.
Conclusion
The main objectives of this study were to investigate the influence of personality traits on disability, progression, and treatment adherence in MS. We showed that Neuroticism and Extraversion significantly affect MS disability. Interestingly, Activity and Vulnerability were also identified as predictive variables for MS disability, suggesting that these particular facets should be considered in clinical practice. Overall, our study highlights the potential of detailed personality assessments in MS, as these could guide the management of more vulnerable patients. Future studies should also consider cognitive deficits, imaging variables, and their relationship with personality, as this would also improve the clinical management of patients with MS.
Funding
The first author was funded by the University of Geneva (Clinical and Experimental Neuropsychology Laboratory, Faculty of Psychology; Prof. JAP). Data acquisition was performed as part of the Swiss Multiple Sclerosis Cohort Study. The funders had no role in data collection, discussion of content, preparation of the manuscript, or decision to publish. We would like to thank the patients for contributing their time to this study.
Conflict of interest
None declared.
Supplementary Material
Acknowledgements
The present study was conducted at the Psychology Faculty of the University of Geneva, Switzerland (Prof. Julie Anne Péron), in collaboration with the Neuroimmunology Unit of the Neurology Department of University Hospitals of Geneva, Switzerland (Prof. Patrice Henri Lalive and Prof. Andreas Kleinschmidt).
Contributor Information
Isabele Jacot de Alcântara, Clinical and Experimental Neuropsychology Laboratory, Faculty of Psychology, University of Geneva, Switzerland; Faculty of Medicine, University of Geneva, Switzerland.
Philippe Voruz, Clinical and Experimental Neuropsychology Laboratory, Faculty of Psychology, University of Geneva, Switzerland; Neurology Department, Geneva University Hospitals, Switzerland; Faculty of Medicine, University of Geneva, Switzerland.
Gilles Allali, Leenaards Memory Center, Lausanne University Hospital and University of Lausanne, Lausanne, Switzerland.
Chloé Fragnoli, Clinical and Experimental Neuropsychology Laboratory, Faculty of Psychology, University of Geneva, Switzerland.
Maria Paraskevi Antoniou, Clinical and Experimental Neuropsychology Laboratory, Faculty of Psychology, University of Geneva, Switzerland.
Patrice Henri Lalive, Neurology Department, Geneva University Hospitals, Switzerland; Faculty of Medicine, University of Geneva, Switzerland.
Julie Anne Péron, Clinical and Experimental Neuropsychology Laboratory, Faculty of Psychology, University of Geneva, Switzerland; Neurology Department, Geneva University Hospitals, Switzerland.
Data availability
The data used for the analysis are provided as Supplementary Materials.
References
- Andersen, C. M., & Bro, R. (2010). Variable selection in regression-a tutorial. Journal of Chemometrics, 24(11–12), 728–737. 10.1002/cem.1360. [DOI] [Google Scholar]
- Benedict, R. H., Hussein, S., Englert, J., Dwyer, M. G., Abdelrahman, N., Cox, J. L., et al. (2008). Cortical atrophy and personality in multiple sclerosis. Neuropsychology, 22(4), 432–441. 10.1037/0894-4105.22.4.432. [DOI] [PubMed] [Google Scholar]
- Benedict, R. H. B., Priore, R. L., Miller, C., Munschauer, F., & Jacobs, L. (2001). Personality disorder in multiple sclerosis correlates with cognitive impairment. Journal of Neuropsychiatry and Clinical Neurosciences, 13(1), 70–76. 10.1176/appi.neuropsych.13.1.70. [DOI] [PubMed] [Google Scholar]
- Bruce, J. M., Hancock, L. M., Arnett, P., & Lynch, S. (2010). Treatment adherence in multiple sclerosis: Association with emotional status, personality, and cognition. Journal of Behavioral Medicine, 33(3), 219–227. 10.1007/s10865-010-9247-y. [DOI] [PubMed] [Google Scholar]
- Bruce, J. M., & Lynch, S. G. (2011). Personality traits in multiple sclerosis: Association with mood and anxiety disorders. Journal of Psychosomatic Research, 70(5), 479–485. 10.1016/j.jpsychores.2010.12.010. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills, L., Cohan, S. L., & Stein, M. B. (2006). Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behaviour Research and Therapy, 44(4), 585–599. 10.1016/j.brat.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Chiaravalloti, N. D., & DeLuca, J. (2008). Cognitive impairment in multiple sclerosis. The Lancet Neurology, 7(12), 1139–1151. 10.1016/s1474-4422(08)70259-x. [DOI] [PubMed] [Google Scholar]
- Chong, I.-G., & Jun, C.-H. (2005). Performance of some variable selection methods when multicollinearity is present. Chemometrics and Intelligent Laboratory Systems, 78(1–2), 103–112. 10.1016/j.chemolab.2004.12.011. [DOI] [Google Scholar]
- De Fruyt, F., & Denollet, J. (2002). Type D personality: A five-factor model perspective. Psychology & Health, 17(5), 671–683. 10.1080/08870440290025858. [DOI] [Google Scholar]
- Demirci, S., Demirci, K., & Demirci, S. (2017). The effect of type D personality on quality of life in patients with multiple sclerosis. Noro Psikiyatri Arsivi, 54(3), 272–276. 10.5152/npa.2016.12764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Disanto, G., Benkert, P., Lorscheider, J., Mueller, S., Vehoff, J., Zecca, C., et al. (2016). The Swiss multiple sclerosis cohort-study (SMSC): A prospective Swiss wide investigation of key phases in disease evolution and new treatment options. PLoS One, 11(3), e0152347. 10.1371/journal.pone.0152347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman, S., Lazarus, R. S., Dunkel-Schetter, C., DeLongis, A., & Gruen, R. J. (1986). Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology, 50(5), 992–1003. 10.1037/0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- Iaffaldano, P., Lucisano, G., Caputo, F., Paolicelli, D., Patti, F., Zaffaroni, M., et al. (2021). Long-term disability trajectories in relapsing multiple sclerosis patients treated with early intensive or escalation treatment strategies. Therapeutic Advances in Neurological Disorders, 14, 17562864211019574. 10.1177/17562864211019574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kupper, N., & Denollet, J. (2018). Type D personality as a risk factor in coronary heart disease: A review of current evidence. Current Cardiology Reports, 20(11), 104. 10.1007/s11886-018-1048-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtzke, J. F. (1983). Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology, 33(11), 1444. 10.1212/WNL.33.11.1444. [DOI] [PubMed] [Google Scholar]
- Leavitt, V. M., Buyukturkoglu, K., Inglese, M., & Sumowski, J. F. (2017). Protective personality traits: High openness and low neuroticism linked to better memory in multiple sclerosis. Multiple Sclerosis Journal, 23(13), 1786–1790. 10.1177/1352458516685417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maggio, M. G., Cuzzola, M. F., Latella, D., Impellizzeri, F., Todaro, A., Rao, G., et al. (2020). How personality traits affect functional outcomes in patients with multiple sclerosis: A scoping review on a poorly understood topic. Multiple Sclerosis and Related Disorders, 46, 102560. 10.1016/j.msard.2020.102560. [DOI] [PubMed] [Google Scholar]
- Magistrale, G., & Nocentini, U. (2015). Anxiety and multiple sclerosis. In B. Brochet (Ed.), Neuropsychiatric symptoms of inflammatory demyelinating diseases (pp. 39–63), Springer, Lisbon. 10.1007/978-3-319-18464-7_4. [DOI] [Google Scholar]
- Malekzadeh, A., Leurs, C., van Wieringen, W., Steenwijk, M. D., Schoonheim, M. M., Amann, M., et al. (2019). Plasma proteome in multiple sclerosis disease progression. Annals of Clinical and Translational Neurology, 6(9), 1582–1594. 10.1002/acn3.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manouchehrinia, A., Beiki, O., & Hillert, J. (2017). Clinical course of multiple sclerosis: A nationwide cohort study. Multiple Sclerosis, 23(11), 1488–1495. 10.1177/1352458516681197. [DOI] [PubMed] [Google Scholar]
- McCrae, R. R., Costa, P. T., Jr., & Martin, T. A. (2005). The NEO-PI-3: A more readable revised NEO personality inventory. Journal of Personality Assessment, 84(3), 261–270. 10.1207/s15327752jpa8403_05. [DOI] [PubMed] [Google Scholar]
- McCrae, R. R., & John, O. P. (1992). An introduction to the five-factor model and its applications. Journal of Personality, 60(2), 175–215. 10.1111/j.1467-6494.1992.tb00970.x. [DOI] [PubMed] [Google Scholar]
- Motl, R. W., Dlugonski, D., Pilutti, L., Sandroff, B., & McAuley, E. (2012). Premorbid physical activity predicts disability progression in relapsing-remitting multiple sclerosis. Journal of the Neurological Sciences, 323(1–2), 123–127. 10.1016/j.jns.2012.08.033. [DOI] [PubMed] [Google Scholar]
- Sandroff, B. M., Schwartz, C. E., & DeLuca, J. (2016). Measurement and maintenance of reserve in multiple sclerosis. Journal of Neurology, 263(11), 2158–2169. 10.1007/s00415-016-8104-5. [DOI] [PubMed] [Google Scholar]
- Sharrack, B., & Hughes, R. A. C. (1996). Clinical scales for multiple sclerosis. Journal of the Neurological Sciences, 135(1), 1–9. 10.1016/0022-510x(95)00261-y. [DOI] [PubMed] [Google Scholar]
- Stathopoulou, A., Christopoulos, P., Soubasi, E., & Gourzis, P. (2010). Personality characteristics and disorders in multiple sclerosis patients: Assessment and treatment. International Review of Psychiatry, 22(1), 43–54. 10.3109/09540261003589349. [DOI] [PubMed] [Google Scholar]
- Stern, Y. (2009). Cognitive reserve. Neuropsychologia, 47(10), 2015–2028. 10.1016/j.neuropsychologia.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern, Y., Arenaza-Urquijo, E. M., Bartres-Faz, D., Belleville, S., Cantilon, M., Chetelat, G., et al. (2020). Whitepaper: Defining and investigating cognitive reserve, brain reserve, and brain maintenance. Alzheimer’s and Dementia, 16(9), 1305–1311. 10.1016/j.jalz.2018.07.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickhouser, J. E., Zell, E., & Krizan, Z. (2017). Does personality predict health and well-being? A metasynthesis. Health Psychology, 36(8), 797–810. 10.1037/hea0000475. [DOI] [PubMed] [Google Scholar]
- Strober, L. B. (2017). Personality in multiple sclerosis (MS): Impact on health, psychological well-being, coping, and overall quality of life. Psychology, Health & Medicine, 22(2), 152–161. 10.1080/13548506.2016.1164321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Théaudin, M., & Feinstein, A. (2015). Depression and Multiple Sclerosis: Clinical Aspects, Epidemiology, and Management. In Brochet, B. (Ed.), Neuropsychiatric symptoms of inflammatory demyelinating diseases (pp. 17–25). Springer, Lisbon. [Google Scholar]
- Thompson, A. J., & Hobart, J. C. (1998). Multiple sclerosis: Assessment of disability and disability scales. Journal of Neurology, 245(4), 189–196. 10.1007/s004150050204. [DOI] [PubMed] [Google Scholar]
- Watson, D., & Hubbard, B. (1996). Adaptational style and dispositional structure: Coping in the context of the five-factor model. Journal of Personality, 64(4), 737–774. 10.1111/j.1467-6494.1996.tb00943.x. [DOI] [Google Scholar]
- Weinshenker, B. G., Issa, M., & Baskerville, J. (1996). Long-term and short-term outcome of multiple sclerosis: A 3-year follow-up study. Archives of Neurology, 53(4), 353–358. 10.1001/archneur.1996.00550040093018. [DOI] [PubMed] [Google Scholar]
- Widiger, T. A., Trull, T. J., Clarkin, J. F., Sanderson, C., & Costa Jr, P. T. (2002). Personality disorders and the five-factor model of personality (2nd ed.). Washington, DC: American Psychological Association. 10.1037/10423-006. [DOI] [Google Scholar]
- Williams, L., O'Connor, R. C., Howard, S., Hughes, B. M., Johnston, D. W., Hay, J. L., et al. (2008). Type-D personality mechanisms of effect: The role of health-related behavior and social support. Journal of Psychosomatic Research, 64(1), 63–69. 10.1016/j.jpsychores.2007.06.008. [DOI] [PubMed] [Google Scholar]
- Wold, S., Sjöström, M., & Eriksson, L. (2001). PLS-regression: A basic tool of chemometrics. Chemometrics and Intelligent Laboratory Systems, 58(2), 109–130. 10.1016/s0169-7439(01)00155-1. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used for the analysis are provided as Supplementary Materials.


