Abstract
Early life stress (ELS) significantly increases susceptibility to alcohol use disorder (AUD) by affecting the interplay between executive and salience networks (SN). The link between AUD and higher body-mass index (BMI) is known, but we lack understanding of how BMI impacts the relationship between ELS and brain connectivity in individuals with AUD. To bridge this gap, we investigated the effects of ELS on brain connectivity in AUD participants, taking into account differences in BMI. The cohort included 401 individuals with AUD, with approximately 60% having a BMI ≥ 25. Within the overall cohort, 123 participants underwent resting-state functional magnetic resonance imaging, revealing intriguing anticorrelations between SN seeds and brain regions involved in somatosensory processing, motor coordination, and executive control as an effect of ELS. Examining the relationship between ELS-driven brain connectivity and BMI, we observed negative correlations in connectivity among low BMI (≤ 24.9) vs. high BMI (≥ 25) individuals. For example, the left supramarginal gyrus (SMG) seed exhibited decreased connectivity with emotion regulation and decision-making regions, including the right occipital cortex, posterior cingulate cortex, and precuneus clusters (all |β| < −0.03, |p| < 0.05). Additionally, the right SMG seed showed reduced connectivity with impulse control and executive function regions, such as the left postcentral/middle frontal gyrus cluster (β = 0.04, p = 0.02). These findings highlight the role of ELS-induced alterations in SN seed connectivity, influenced by BMI, in the neurobiology of AUD. Understanding the neural mechanisms linking obesity, AUD, and ELS can guide targeted interventions for this population.
Keywords: Early life stress, Alcohol use disorder, Body mass index, Resting state functional MRI, Seed-based voxel connectivity, Salience network
Introduction
Early life stress (ELS), as determined by self-reported traumatic childhood events, such as emotional abuse, severe family conflict, domestic violence and bullying, has been linked to increased vulnerability to the development of alcohol use disorder (AUD) 1,2,3. Individuals with AUD and obesity exhibit poor decision-making abilities, which has been linked to disruptions in the salience network (SN) assessed in resting state functional MRI studies 4, 5. This maladaptive decision-making has been attributed to difficulties in switching between executive and salience networks 6. Accordingly, studies have extensively examined the relationship between heavy alcohol consumption and increased body weight over the past years 7.
It has been speculated that heavy alcohol consumption can lead to a higher body-mass index (BMI) via insulin resistance 8, 9. Although the evidence for a comorbidity between obesity and AUD is conflicting 10, the clinical relationship between these two disorders is complex and both are affected by common aspects of vulnerability to adverse events, as well as subsequent events whereby excess alcohol consumption can lead to both weight gain and to weight loss 7, 11, 12. Previous studies have shown that ELS is associated alterations in brain structure and function, including reduced centrality (defined as the impact of a particular region of the brain on the transmission and exchange of information within extensive networks of the brain) in SN regions, such as the anterior insula (AIns) and dorsal anterior cingulate cortex (ACC) 13–15.
Despite extensive research conducted on the topic, there is still insufficient evidence of any effects of ELS-related events on alterations of brain connectivity of salience, executive, somatosensory and impulse control networks in individuals with AUD, especially with varying BMI levels. In our earlier study using data from the human connectome project (HCP) we found notable associations between chronic alcohol consumption, BMI and the decision-making capabilities for monetary rewards in people with high-risk AUD and obesity symptoms 16. Expanding on these findings, our current objective is to examine how BMI modulates the impact of ELS on resting state seed-based functional connectivity among individuals with AUD. Our hypothesis is that ELS may influence the reduced connections of the salience network node with regions responsible for executive control and decision making in AUD, with patients with overweight or obesity (BMI ≥ 25 Kg/m2) and with AUD showing more pronounced effects then individuals with leanness (BMI ≤ 24.9 Kg/m2) and AUD.
Materials and methods
Participants
The study cohort, as presented in Table 1, was comprised of 401 treatment-seeking individuals with AUD (33% females) of which 123 individuals underwent resting state functional MRI scans. These were inpatients admitted in the NIAAA clinic for treatment and their resting state functional MRI scans were obtained following detoxification and withdrawal period from alcohol. Diagnosis of AUD was made via the Structured Clinical Interview for the Diagnostic Statistical Manual (DSM)-IV or DSM-5 (SCID)17–19. For the current analysis, individuals who were diagnosed with alcohol dependence or abuse via SCID-IV were considered to have an AUD. Daily alcohol consumption in the 90 days preceding the study was assessed using the timeline follow-back (TLFB) method 20. Individuals with substance use disorders other than AUD and nicotine dependence were excluded. Patients were allowed to smoke during their stay but were requested not to smoke or remove their nicotine patch two hours prior to their MRI scan. Of the individuals with AUD included in the present analysis, only 1% and 5% were found to experience alcohol-induced anxiety and mood disorders, respectively. The study was approved by the Institutional Review Board of the National Institutes of Health, and all participants provided written informed consent to participate.
Table 1.
Demographic and Clinical Characteristics of Participants
| AUD cohort (n = 401) | AUD sub-cohort (n = 123) | |||||
|---|---|---|---|---|---|---|
| High BMI (n = 240) | Low BMI (n = 161) | Test Statistics T-test or, Mann-Whitney for continuous/Chi-square for categorical variables |
High BMI (n = 71) | Low BMI (n = 52) | Test Statistics T-test or, Mann-Whitney for continuous/Chi-square for categorical variables |
|
| Age (years) (mean ± SD) | 47.9 ± 11.3 | 43.7 ± 11.3 | p < 0.001 | 45.4 ± 11.2 | 43.5 ± 10.6 | p = 0.33 |
| Sex | ||||||
| Males n (%) | 163 (67.9%) |
106 (65.8%) |
χ2 = 0.19; df = 1; p = 0.66 | 54 (76.1%) |
30 (56.6%) |
χ2 = 5.25; df = 1; p = 0.02 |
| Females n (%) | 77 (32.1%) |
55 (34.2%) |
17 (23.9%) |
23 (43.4%) |
||
| Years of Education | 13.7 ± 2.8 | 13.6 ± 3.1 | p = 0.78 | 13.4 ± 2.9 | 13.4 ± 2.5 | p = 0.94 |
| Household Income (Median) | 30K-39 999 |
30K-39 999 |
30K-39 999 |
30K-39 999 |
||
| Total drinks last 7 days | 92.42 ± 67.02 | 100.63 ± 88.27 | p = 0.29 | 91.83 ± 64.87 | 87.28 ± 68.50 | p = 0.74 |
| Alcohol Dependence Score | 21.22 ± 8.36 | 21.93 ± 8.58 | p = 0.41 | 21.52 ± 7.98 | 22.73 ± 8.43 | p = 0.41 |
| Age First Drink [years (mean ± SD)] | 14.76 ± 4.00 | 14.79 ± 5.24 | p = 0.94 | 14.64 ± 3.64 | 14.56 ± 4.64 | p = 0.91 |
| Age of AUD Onset [years (mean ± SD)] | 28.7 ± 10.59 | 27.3 ± 10.03 | p = 0.21 | 25.95 ± 9.10 | 27.64 ± 9.08 | p = 0.33 |
| Length of AUD history | 19.26 ± 11.95 | 16.38 ± 10.95 | p = 0.02 | 19.08 ± 11.84 | 15.79 ± 9.23 | p = 0.19 |
| (mean ± SD) | ||||||
| Smoking status | ||||||
| Yes, n (%) | 131 (54.6%) |
125 (77.6%) |
χ2 = 22.19; df = 1;p < 0.001 | 42 (59.2%) |
36 (67.9%) |
χ2 = 1.0; df = 1; p = 0.32 |
| No, n (%) | 109 (45.4%) |
36 (22.4%) |
29 (40.8%) |
17 (32.1%) |
||
| Ethnicity, n (%) | ||||||
| Non-Hispanic or Latino | 214 (89.2%) |
143 (88.8%) |
χ2 = 2.26; df = 2; p = 0.32 | 61 (85.9%) |
48 (90.6%) |
χ2 = 0.62; df = 2; p = 0.73 |
| Hispanic or Latino | 20 (8.3%) |
10 (6.2%) |
8 (11.3%) |
4 (7.5%) |
||
| Unknown/not reported | 6 (2.5%) |
8 (4.9%) |
2 (2.8%) |
1 (1.9%) |
||
| Race, n (%) | ||||||
| White | 127 (52.9%) |
78 (48.4%) |
χ2 = 5.31; df = 5; p = 0.38 | 37 (52.1%) |
30 (56.6%) |
χ2 = 2.89; df = 5; p = 0.71 |
| Black/African American | 83 (34.6%) |
63 (39.1%) |
21 (29.6%) |
15 (28.3%) |
||
| Asian | 3 (1.3%) |
5 (3.1%) |
1 (1.4%) |
0 | ||
| American Indian or Alaska Native | 4 (1.7%) |
0 | 1 (1.4%) |
0 | ||
| Multiracial | 7 (2.9%) |
5 (3.1%) |
4 (5.6%) |
5 (9.4%) |
||
| Unknown Race |
16 (6.7%) |
10 (6.2%) |
7 (9.9%) |
3 (5.7%) |
||
| ELS events (Median; IQR) |
3; 5 | 3; 5 | 2; 4 | 3; 5 | ||
Note: AUD cohort: NIAAA AUD inpatient treatment seekers; AUD sub-cohort: AUD inpatients who underwent resting state functional MRI;
NA: not available; Household Income: <$10,000 = 1, $10K–$19,999 = 2, $20K–$29,999 = 3, $30K–$39,999 = 4, $40K–$49,999 = 5, $50K–$74,999 = 6, $75K–$99,999 = 7, >=$100 000 = 8; length of AUD history (difference in age of AUD onset and current age). Here, * represents statistical significance with p value < 0.05; only white and black populations were included for chi-square analysis for racial differences.
Body-mass index (BMI)
BMI for all participants in the study was calculated by dividing their body weight by the square of their height (Kg/m2). Measurements of both body weight and height were recorded when participants enrolled in the NIAAA natural history study. The continuous BMI variable was utilized to categorize the AUD cohort into two groups: individuals with a low BMI (BMI ≤ 24.9) and those with a high BMI (BMI ≥ 25). Categorizing the AUD cohort into low BMI and high BMI groups allows for a more nuanced analysis of the relationship between BMI-, AUD- and ELS-influenced brain connectivity patterns.
Early life stress (ELS) events
ELS was operationalized using self-report questionnaire which consists of 19 standard life event items experienced in their early life as a child (up to age 18 years). The participants’ responses were recorded as yes/no for each life event including emotional, sexual and physical abuse, as well as violence, negligence, parental divorce, surgery, parental death, separation and so forth 21, 22. The sum of responses for all domains was used to create a complete ELS_events score (with a maximum score of 19; Mean = 3.58, SD = 3.2). Emotional abuse, severe family conflict, domestic violence and bullying were the most reported events.
Resting-state functional MRI (rsfMRI) data acquisition and preprocessing
Resting-state fMRI (rs-fMRI) scans were acquired from patients during the inpatient treatment phase when they were stabilized and not experiencing stress or acute withdrawal symptoms. Patients’ withdrawal scores were assessed using the Clinical Institute Withdrawal Assessment for Alcohol-revised (CIWA-Ar), a 10-item scale 23. To be eligible for rs-fMRI scans, patients had to have a average CIWA-Ar score below 8, which typically occurs at 1 week after admission, and the scans were done during weeks 2 or 3 of their inpatient stay. The scans were conducted at the NIH NMR Center, utilizing a Siemens 3T MRI Skyra scanner with a 20-channel head coil. Participants were instructed to keep their eyes open and remain alert during the ten-minute period of rs-fMRI data collection, with no additional stimuli presented. The functional scans, including the rs-fMRI, were acquired utilizing an echoplanar-imaging pulse sequence (TR: 2000 ms, TE: 30 ms, FA: 90°, FOV: 240 × 240 mm, 3.8 mm slice thickness, multi-slice mode: interleaved). A high-resolution T1-weighted MPRAGE (TR: 1900 ms, TE: 3.09 ms, FA: 10°, FOV: 240 × 240 mm, 1 mm slice thickness) was obtained for registration purposes. Preprocessing of the data was carried out using the CONN toolbox (version 18b), a Matlab-based toolbox for functional connectivity analysis (http://www.nitrc.org/projects/conn) 24, including realignment and unwarp, slice-timing correction, outlier identification, and normalization. Artifact detection was performed based on scan-to-scan differences in the global signal (z-value threshold 5) and subject motion parameters (threshold 0.9 mm) using the ‘art’ software for artifact rejection (www.nitrc.org/projects/artifact_detect/), with identified outlier scans included as first-level covariates.
Functional connectivity
To analyze rs-fMRI data, we used the CONN toolbox (18.b; https://www.nitrc.org/executedashboard/?group_id=279) with full width at half maximum spatial smoothing of 8 mm. To minimize effects of head motion, we regressed out principal components associated with segmented white matter and cerebrospinal fluid using CompCor 25, as well as twelve motion regressors (3 rotational, 3 translational, and their derivatives) calculated from CONN image preprocessing. The data were filtered using a band-pass filter of 0.008–0.09 Hz to eliminate very-low-frequency drift and high frequency noise, and linear trends were removed. We used a continuous squashing function (i.e., despiking) to further minimize the influence of potential outlier scans. Global BOLD signal was not regressed out to avoid the mathematical introduction of negative correlations 26.
We conducted a seed to voxel (whole brain) resting state connectivity analysis to investigate the influence of ELS on the connectivity of SN seed regions and the rest of the brain. The seeds were selected a priori based on our hypothesis of strong interaction of SN with executive function networks in addictive conditions 27–29. The seeds were defined based on the anatomical FSL Harvard-Oxford atlas, which is the default atlas utilized for segmentation during the CONN processing procedure. We included the anterior insula, anterior cingulate cortex and inferior parietal cortex supramarginal gyrus as seed regions associated with the SN. A separate model was created for the left and right structures for each seed. We extracted the mean time series of the seed region from their preprocessed functional data and calculated Pearson’s correlation coefficients for the connection between the seed and voxel for each participant. To enable further analyses, we transformed the resulting values into normally distributed Z-scores using the Fisher transformation. The identified correlations are presented in the results section.
Statistical analyses
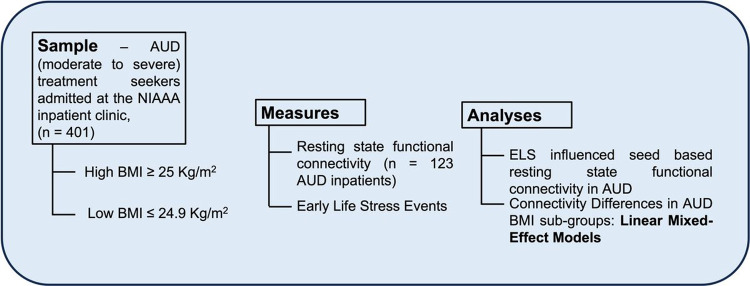
To compare the demographic and clinical characteristics of our study groups (AUD: low BMI vs. high BMI), we utilized Student’s t-tests and Mann-Whitney tests for continuous variables, and chi-squared tests for categorical variables. To identify group differences, ELS-associated connectivity coefficients between the seeds and significant clusters were extracted from CONN. We considered connection-level False Discovery Rate (FDR)-corrected P-values < 0.05 as significant 30. We then employed linear mixed effect models (LMEs) to investigate differences in correlations between the seed and significant clusters (interpreted as connectivity, the dependent variable) across our study groups and included AUDIT, BMI status, age, sex, and smoking status as fixed effects, and participants as random effect. We adjusted for multiple pairwise group comparisons using the Bonferroni correction. For all descriptives and regression models, we used SPSS 22 (IBM Corp., Armonk, NY) and addressed missing values in LMEs using the restricted maximum likelihood approach. Figure 1 provides an overview of the study flow, including participant grouping, measures and statistical approach used to investigate the study hypothesis.
Figure 1. The study flow listing the sample, measures and analytic techniques.
The alcohol use disorder (AUD) population was divided into two groups based on body-mass index (BMI) (High BMI and Low BMI). The measures included early life stress (ELS) events and resting-state functional connectivity (rs-fMRI). The main analyses consisted of seed-based rs-fMRI to identify early life stress-influenced connectivity patterns in individuals with AUD, as well as linear mixed-effects models to identify connectivity differences in the AUD BMI groups.
Results
Characteristics of the sample: demographic and clinical
Of a total of 401 participants with AUD (age mean SD: 46.21 ± 11.48; range: 21–74 yrs), n = 240 (60%) had a BMI ≥ 25 kg/m2 (AUD-high BMI), while n = 161 (40%) had a BMI between 18–24.9 Kg/m2 (AUD-low BMI). The resting state fMRI scans were acquired in 123 of the total participants [(age mean SD: 28.16 ± 6.28; range: 25–69 yrs), n = 71 AUD-high BMI; n = 52 AUD-low BMI]. The proportion of males was higher in the high BMI group (76.1%) compared to the low BMI group (56.6%; χ2 = 5.25; p = 0.02). The length of AUD history (difference in age of AUD onset and current age) was significantly higher among participants with a high BMI vs. those with a low BMI (p = 0.02). The full BMI distribution of the AUD cohort and sub-cohort (patients that underwent rs-fMRI) can be seen in Supplemental Figures S1 and S2. The data show a remarkable increase in rightward tail for BMI distribution in both the samples. However, there was no clear divergence in the occurrence of their ELS events between our BMI groups.
In the AUD cohort, the mean age of high BMI group (47.9 ± 11.3 years) was significantly higher than the low BMI counterpart (43.7 ± 11.3 years; p < 0.001). Furthermore, the percentage of smokers was higher in the low BMI (77.6%) category then the high BMI (54.6%; p < 0.001). No significant difference in sex, race, ethnicity, years of education and household income was identified between the BMI groups (refer to Table 1).
The BMI groups in the AUD sub-cohort exhibited no differences in age, sex, race, ethnicity, years of education, household income or smoking status. As expected, the two AUD BMI groups did not differ in their age of first alcohol drink (refer to Table 1).
Resting state fMRI
Influence of ELS events on seed-based voxel connectivity (SBVC)
The occurrence of ELS events predicted connectivity of multiple clusters to our seed regions; namely, left/right SMG, AIns and ACC after covarying for age and sex. For further information on the connected clusters, please refer to Table 2. Additionally, a visual representation of the extent of significance can be found in Fig. 2.
Table 2.
ELS_events Effect and Severe AUD - BMI Group Differences in the Seed-to-Voxel Analysis
| Seed | Connectivity Cluster | Adjusted Estimate (β), (95% CI), p value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Label | Lat. | Label | Lat. | x | y | z | k | P (peak, FWE) | Connectivity differences between AUD – BMI groups (AUD Low BMI vs. AUD High BMI) |
| Salience Network_SMG | L | Lateral Occipital Cortex |
R | +52 | −66 | +40 | 2584 | <0.001 | −0.06, (−0.12, −0.002), 0.03* |
| Cerebellum Crus 2 | R | +46 | −68 | −44 | −0.037, (−0.08, 0.015), 0.17 | ||||
| Cerebellum Crus 1 | R | +48 | −74 | −20 | −0.016, (−0.05, 0.019), 0.36 | ||||
| Intracalcarine cortex |
L | −08 | −76 | +12 | −0.022, (−0.06, 0.02), 0.31 | ||||
| Precuneus | +14 | −74 | +40 | 145 | 0.01 | −0.039, (−0.07, −0.005), 0.01* | |||
| Frontal Pole | L | −26 | +40 | −16 | 89 | <0.001 | −0.01, (−0.05, 0.029), 0.59 | ||
| Posterior Cingulate Gyrus |
−02 | −52 | +18 | 61 | 0.003 | −0.05, (−0.114, −0.002), 0.03* | |||
| R | Frontal Medial Cortex |
−02 | +32 | −24 | 726 | 0.02 | −0.033, (−0.07, 0.007), 0.105 | ||
| Insular Cortex | L | −52 | −32 | +22 | 8616 | <0.001 | 0.002, (−0.02, 0.02), 0.18 | ||
| Postcentral Gyrus |
L | −56 | +20 | +26 | 1011 | <0.001 | 0.04, (0.005, 0.089), 0.02* | ||
| Middle Frontal Gyrus | L | ||||||||
| Lateral Occipital Cortex |
L | −52 | −70 | +32 | 539 | <0.001 | 0.01, (−0.03, 0.06), 0.62 | ||
| Posterior Middle Temporal Gyrus |
L | −66 | −44 | +08 | 362 | <0.001 | 0.015, (−0.02, 0.05), 0.43 | ||
| Cerebellum8 | R | +36 | −48 | −54 | 206 | <0.01 | 0.004, (−0.02, 0.03), 0.77 | ||
| Cerebellum Crus2 |
R | +52 | −50 | −42 | 45 | <0.001 | 0.008, (−0.02, 0.04), 0.65 | ||
| Salience Network_ACC |
Anterior Temporal Fusiform Cortex |
L | −36 | −04 | −42 | 143 | 0.004 | −0.008, (−0.04, 0.02), 0.63 | |
| Salience Network_AIns |
L | Lateral Occipital Cortex |
R | +46 | −78 | −20 | 119 | <0.01 | 0.011, (−0.03, 0.06), 0.64 |
| Cerebellum Crusl |
R | +54 | −58 | −28 | 74 | 0.03 | 0.016, (−0.03, 0.06), 0.51 | ||
| R | Lateral Occipital Cortex |
L | −50 | −70 | +32 | 230 | <0.001 | 0.007, (−0.039, 0.054), 0.75 | |
| Hippocampus | R | +32 | −22 | −20 | 41 | 0.023 | −0.001, (−0.042, 0.039), 0.94 | ||
Notes: Statistics and descriptives for seed-to-voxel connectivity analyses. Abbreviations as follows: k: number of voxels in the cluster; Lat. (R/L): Laterality of brain region (Right/Left); FDR: false discovery rate correction; SD: standard deviation; SMG = Supramarginal Gyrus; AG = Angular Gyrus; ACC = Anterior Cingulate Cortex; AIns = Anterior Insula; AUD: Alcohol Use Disorder; BMI: Body-Mass Index. Group differences were adjusted for age, smoking status.
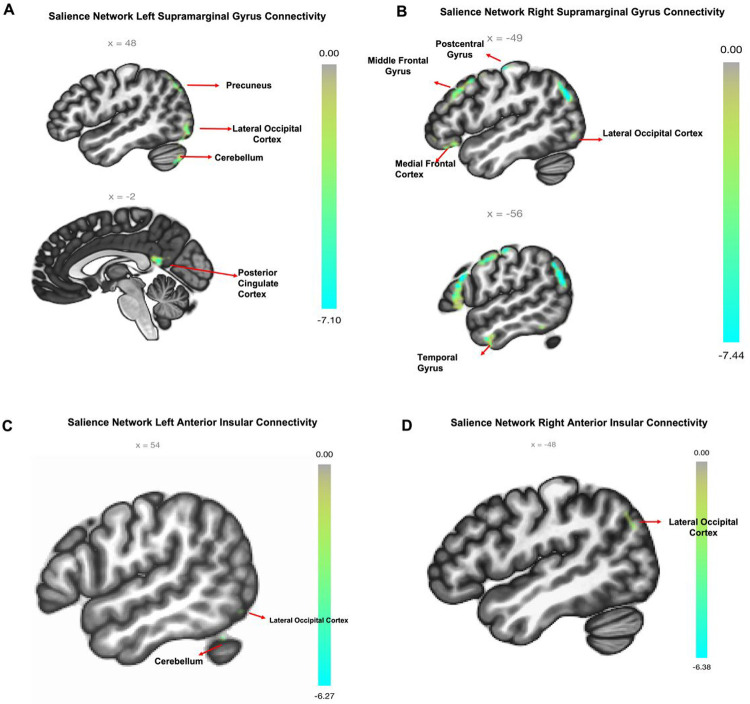
Figure 2. Early life stress-related connectivity pattern in AUD.
(A – D) Significant Seed-to-Voxel Connections Representing Salience Network Seed Regions (supramarginal gyrus left/right and anterior insula left/right). For anterior cingulate connectivity: plots of seed connectivity are not pictured as cluster size was small. Labels provided for perspective reference are as follows: LOC: Lateral Occipital Cortex, PCC: Posterior Cingulate Cortex, mFC: medial frontal cortex, PoG: Postcentral Gyrus, Ins: Insula, MFG: Middle Frontal Gyrus, MTG: Middle Temporal Gyrus; cluster of significant activation at the peak-wise PFWE < 0.001/cluster size P < 0.05 FDR corrected level. Directions of connectivity are noted in Table 2.
Left SMG showed negative connectivity driven by ELS with several clusters, including the right lateral occipital cortex (LOC), right cerebellum and left intracalcarine cortex, as well as the posterior cingulate cortex (PCC). However, left SMG had positive connectivity with clusters in the precuneus and left frontal pole. Conversely, driven by ELS the right SMG showed a positive connectivity with the left insular cortex and right cerebellum 8 clusters, but it was negatively connected to clusters in the frontal medial cortex, left postcentral gyrus, left middle frontal gyrus (MFG), left LOC, left middle temporal gyrus (MTG) and right cerebellum crus 2.
The ACC seed region exhibited positive connectivity with a cluster in the left anterior temporal fusiform cortex (ATFC). As for the left AIns seed, it showed negative connectivity with clusters in the right LOC and Cerebellum Crus 1. Meanwhile, the right AIns seed was negatively connected to the left LOC but positively connected to the right hippocampus.
Association of ELS predicts seed-based voxel connectivity with BMI levels in individuals with AUD
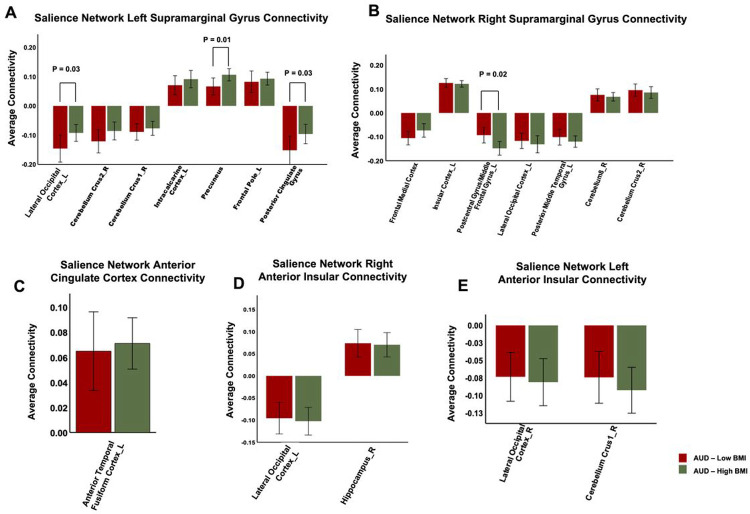
Our LME analysis, after adjustment for age, sex and smoking status, showed that individuals with AUD and low BMI (in comparison to those with high BMI) exhibited several negative correlations, such as in connectivity of the left SMG seed with the right LOC (β = −0.06; CI = −0.12, −0.002; p = 0.03) and PCC (β = −0.05; CI = −0.114, −0.002; p = 0.03) clusters. In addition, they also displayed a negative correlation with the connectivity of the left SMG with the precuneus (β = −0.03; CI = −0.07, −0.005; p = 0.01) cluster (refer to Table 3; Fig. 3A).
Figure 3. ELS-Driven Differential Seed-to-Voxel Connectivity Patterns: BMI Effects on AUD Groups.
The bar graphs illustrate the differential seed-to-voxel connectivity patterns driven by early life stress (ELS), focusing on the effects of BMI on AUD groups. Linear mixed effect models were utilized, adjusting for age, sex, and smoking status. The upper panel (A/B) displays the connectivity coefficients of the Supramarginal Gyrus (Left/Right) seeds for the respective groups. The lower left panel (C) represents the connectivity coefficient of the Anterior Cingulate Cortex seed by group. The lower middle panel (D) shows the connectivity coefficient of the Right Anterior Insula seed by group. Lastly, the lower right panel (E) exhibits the connectivity coefficient of the Left Anterior Insula seed by group. The provided labels serve as reference: AUD (Alcohol Use Disorder), BMI (Body-Mass Index), ELS (Early Life Stress), L (Left), R (Right). Multiple columns of bar graphs represent various significant clusters identified by name. Significance levels (p < 0.05) are indicated after Bonferroni correction.
***Further investigation showed that low BMI individuals revealed anticorrelation of right SMG seed connectivity with the left postcentral gyrus/MFG cluster (β = 0.04; CI = 0.005, 0.089; p = 0.02) compared to those with high BMI (Table 2; Fig. 3B). However, we did not observe any significant differences between BMI groups in the connectivity patterns of the ACC and AIns seeds with different brain clusters in the AUD BMI groups (refer to Table 2, Fig. 3C, D & E).
Discussion
In our population of individuals with moderate-to-severe AUD, we found a higher prevalence of individuals with overweight and obesity (approximately 60%). However, when examining the distribution of BMI, we did not observe a significant rightward skewing, indicating a relatively balanced distribution across the range. Surprisingly, we did not find a clear difference in the distribution of ELS events between patients with AUD and with a high or low BMI. Additionally, as we identified a significantly greater length of AUD history in participants with a high BMI as compared to a low BMI within our cohort, implying that those with a low BMI are still early in their history of AUD and have yet to gain weight. These findings suggest that the relationship between BMI and ELS in the context of AUD may not be straightforward, and there may be other factors that have a stronger impact on the association between ELS and BMI in individuals with AUD.
Therefore, on investigating the effect of ELS on functional brain connectivity in individuals with AUD who differ in BMI, we observed various connectivity patterns associated with ELS, indicating connections between the left and right SMG seed regions and whole brain. Also, these predicted connections were differentially associated with BMI levels within these individuals.
As predicted, we observed the main effect of ELS as anticorrelation of the SN seed regions, bilateral SMG and AIns, with several clusters in different regions of the brain, including the somatosensory and motor coordination areas (such as the bilateral LOC, right cerebellum, left posterior middle temporal gyrus (pMTG), left postcentral gyrus, and left intracalcarine cortex), frontal, or executive, control regions (e.g., the MFG). Exposure to stress during critical periods of brain development has been demonstrated to modify connectivity patterns and heighten the risk of developing AUD. Likewise, numerous studies provide evidence that experiencing ELS has harmful effects on individuals and enhances their susceptibility to alcohol use in adulthood 2, 31–35. Moreover, exposure to a series of ELS events leads to modifications in connectivity of brain regions associated with emotion, self-regulation and cognition, including nodes of the DMN, such as the PCC, mPFC and MTG, and within the fronto-limbic networks, such as the mPFC, ACC, amygdala and orbitofrontal cortex 36–38]. Children between the ages of 9 and 16 who were exposed to various stress events, such as conventional crimes, child maltreatment, peer/sibling victimization and sexual victimization, were found to have a reduced functional connection between their SMG and PCC 39. Studies have shown that in individuals with AUD, reduced connectivity within the SN is associated with decreased self-control and an inability to restrain cravings 5, as well as impaired inhibition for salient stimuli 40. Notably our analysis revealed lower functional connectivity between left/right SMG and clusters in motor [cerebellum (right Crus 1 & 2), occipital cortex, temporal (pMTG)] and somatosensory (postcentral gyrus), as well as frontal, or executive, control regions (e.g., the MFG) that reportedly are involved in processing of emotionally salient stimuli 41–44. As such, the lower connectivity of SN nodes with emotion and executive control regions are concordant with evidence in the literature that have shown the effect of ELS exposure in altering the connectivity of brain networks involved in emotion regulation and salience of rewards 45, 46. These previous findings suggest a disengagement of executive control functions when emotionally significant rewards are being processed in adults with AUD and a history of ELS. The negative association between left SMG activity and major default mode network (DMN) nodes (PCC, mPFC), which are normally inversely associated with goal-oriented actions 47, suggests that ELS can affect the decision-making ability of individuals with AUD. Such altered emotional processing and decision-making, resulting from ELS, may be interpreted as the underlying drivers for the development of stress-related AUD 48.
Moreover, we found that the functional connectivity of SN seeds was influenced by ELS, resulting in a positive correlation between the left SMG and ACC with DMN nodes (precuneus and left ATFC) in the AUD population. It is noteworthy that exposure to acute stress has been linked with elevated functional connectivity between the default mode and salience networks in healthy adults and adolescents 39, 49. Given that the participants in our study cohort were exposed to a variety of ELS events, spanning from one to nineteen stress events, it is probable that the direction of connectivity between different regions of the network was impacted by the overall degree of ELS they experienced. Our findings align with previous research suggesting that certain nodes within the DMN, such as the temporal fusiform cortex and precuneus, play a crucial role in social and self-related cognitive processes 50, 51, supporting the interpretation that increased SMG-ATFC/precuneus coupling, as a result of ELS events, may lead to heightened self-awareness and emotional response to negative social stimuli. This, in turn, could potentially increase impulsive decision-making and drinking behaviors as a way of regulating these emotions in individuals with AUD.
We further investigated the impact of BMI on ELS-influenced connectivity patterns of the SN with different brain regions in AUD. Contrary to our expectations, individuals with AUD and low BMI exhibited a stronger anticorrelation in the connectivity of the left SMG seed with the right LOC and PCC clusters, while exhibiting a weaker positive correlation with the precuneus cluster, compared to those with high BMI. This suggests that the SN left SMG connectivity with emotion regulation and decision-making regions is not always negatively impacted by AUD and may even be strengthened in these individuals with a low BMI. On the other hand, we observed that the ELS influenced anticorrelation of the right SMG seed with the somatosensory (left postcentral gyrus) and impulse control (left MFG) clusters was weaker in AUD-low BMI individuals compared to those with high BMI, which in light of previous findings 27, 28, 52–54, suggest elevated impulsivity and poor self-control behaviors in AUD with co-occurrence of high BMI. The findings suggest two potential scenarios: either ELS contributes to overeating in individuals with AUD, or ELS-induced overeating increases their susceptibility to excessive alcohol consumption.
Upon further examination, we found that the influence of ELS on connectivity patterns with the left and right hemispheric SN SMG seeds differed based on individuals’ BMI levels within our population with AUD. In particular, the magnitude of increase in BMI levels were observed to exert an impact on the connectivity of the left SMG with regions associated with the default mode network. On the other hand, a negative correlation was detected between the BMI levels of individuals with AUD and the connectivity of the right SMG with clusters in frontal regions that govern impulsive or self-control behaviors. Both pre-clinical and clinical studies have identified the contribution of ELS in increasing the risk for obesity 55–57 and AUD 32, 58, 59, which was attributed to persistent overactivation of the hypothalamic-pituitary-adrenal (HPA) axis 60, dysregulation of the mesolimbic dopamine functions 61, 62 and an imbalance in connectivity patterns of salience, emotion and somatosensory networks 63. Nonetheless, none of these studies demonstrated the relationship between ELS-influenced brain connectivity in adults with a comorbid occurrence of AUD and elevated BMI.
The present study offers intriguing insights into the intricate relationship between ELS, AUD, BMI and the connections of salience network seeds with the entire brain. These results are consistent with our hypothesis, which suggests that elevated BMI may alter the connectivity between the SN and brain regions that regulate executive and impulsive behaviors in individuals with AUD who have a history of ELS.
Limitations
There are several unanswered questions that need to be explored in future large cohort studies. One limitation of our study is the use of self-reported questionnaire to measure ELS events. This type of measure is prone to recall bias and may not provide a complete evaluation of ELS. Furthermore, our study did not disentangle the effect of each type of ELS experience, even though research shows that different adverse events may have different effects on brain structure and network connectivity. For example, deprivation and neglect are linked to changes in executive control network regions, such as the dorsolateral prefrontal cortex and parietal cortex, while threat and abuse-related exposures are linked to alterations in regions of the salience network 64. Additionally, adults who grew up in poverty exhibit reduced activation in the ventrolateral prefrontal cortex and have difficulty regulating emotions 65. In a recent study alterations in connectivity within the SN was found to mediate the effects of childhood abuse and neglect with problematic alcohol use 66. Although there are no studies that have directly compared the impact of ELS on connectivity differences based on BMI levels in the AUD population, the age at which the stress occurred 67 and the level or duration of stress exposure 68 are crucial factors that should be explored in future studies. Moreover, the correlations observed between ELS and brain connectivity in individuals with AUD at different BMI levels give rise to various conclusions. For instance, it is possible that ELS influences both alcohol abuse and excessive eating. Alternatively, it could be that ELS-driven AUD contributes to overeating, or that ELS-driven overeating increases vulnerability to alcohol overconsumption. The significance of these findings emphasizes the need for longitudinal studies instead of solely relying on cross-sectional research. It is also crucial to conduct longitudinal studies that follow individuals with AUD from an early stage, allowing the observation of potential changes in their brain patterns over time, particularly in relation to any fluctuations in BMI. Lastly, our study did not identify connectivity differences with salience network seeds in AIns and ACC, as reported in previous studies on the effects of ELS on salience network seed-based connectivity. This may be attributed to the relatively low severity of the stressors reported in our cohort, making direct comparisons with previous results difficult. In our forthcoming study, we aim to investigate potential sex effects that may be influencing the observed correlations and relationships. Furthermore, it is crucial to replicate our findings using large datasets to assess the consistency and reliability of the results, reinforcing the significance and validity of our study’s outcomes.
Conclusion
To conclude, we identified positive and negative correlations in the connectivity of our SN SMG seed with clusters associated with emotion, self-regulation, decision-making and impulsivity for salient stimuli in an AUD population with a history of ELS-related events. Further our results revealed the impact of BMI elevation on the observed brain connectivity patterns in study participants with AUD. These findings underscore the significance of ELS-induced SN seed connectivity in AUD with varying BMI levels and its role in the neurobiological mechanisms that drive AUD. The results from our study suggest potential directions for future large-scale research on the neural mechanisms for the comorbid occurrence of obesity in individuals with AUD with a history of ELS. This might facilitate the development of targeted interventions for such individuals.
Funding Sources
Dr. Joseph is receiving support from National Institute on Alcohol Abuse and Alcoholism (Z01AA000135) and Nursing Research (1ZIANR000035–01), the Office of Workforce Diversity, the National Institutes of Health Distinguished Scholar Award, and the Rockefeller University Heilbrunn Nurse Scholar Award. KA has received an Intramural Research Training Award from the National Institute on Alcohol Abuse and Alcoholism, as well as a Fellowship from the Center on Compulsive Behaviors, National Institutes of Health, Department of Health, and Human Services. Please note that the authors are solely responsible for the content of this study, and it does not necessarily reflect the official views of the NIH. This study was in part funded by NIAAA Intramural program (ZIAAA000123, PI: Reza Momenan).
The corresponding authors can provide the findings of this study upon receiving a reasonable request.
Footnotes
Competing Interests
The authors declare no competing interest.
Contributor Information
Khushbu Agarwal, National Institutes of Health.
Paule Joseph, National Institutes of Health.
Rui Zhang, National Institute on Alcohol Abuse and Alcoholism.
Melanie Schwandt, National Institute on Alcohol Abuse and Alcoholism / National Institutes of Health.
Vijay Ramchandani, National Institutes of Health.
Nancy Diazgranados, NIH.
David Goldman, National Institutes of Health.
Reza Momenan, National Institute On Alcohol Abuse and Alcoholism.
Data Availability
The information analyzed in this study from the NIAAA is bound by specific licenses and restrictions. The dataset is under the care and control of the NIAAA Office of the Clinical Director and is securely housed there. Dataset access requests are directed to Melanie Schwandt, melanies@mail.nih.gov.
References
- 1.Gondré-Lewis MC, Warnock KT, Wang H, June HL Jr., Bell KA, Rabe H et al. Early life stress is a risk factor for excessive alcohol drinking and impulsivity in adults and is mediated via a CRF/GABA(A) mechanism. Stress 2016; 19(2): 235–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramchandani VA, Stangl BL, Blaine SK, Plawecki MH, Schwandt ML, Kwako LE et al. Stress vulnerability and alcohol use and consequences: From human laboratory studies to clinical outcomes. Alcohol 2018; 72: 75–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwandt ML, Heilig M, Hommer DW, George DT, Ramchandani VA. Childhood trauma exposure and alcohol dependence severity in adulthood: mediation by emotional abuse severity and neuroticism. Alcohol Clin Exp Res 2013; 37(6): 984–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Canessa N, Basso G, Carne I, Poggi P, Gianelli C. Increased decision latency in alcohol use disorder reflects altered resting-state synchrony in the anterior salience network. Sci Rep 2021; 11(1): 19581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sullivan EV, Müller-Oehring E, Pitel AL, Chanraud S, Shankaranarayanan A, Alsop DC et al. A selective insular perfusion deficit contributes to compromised salience network connectivity in recovering alcoholic men. Biol Psychiatry 2013; 74(7): 547–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arcurio LR, Finn PR, James TW. Neural mechanisms of high-risk decisions-to-drink in alcohol-dependent women. Addict Biol 2015; 20(2): 390–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sayon-Orea C, Martinez-Gonzalez MA, Bes-Rastrollo M. Alcohol consumption and body weight: a systematic review. Nutr Rev 2011; 69(8): 419–431. [DOI] [PubMed] [Google Scholar]
- 8.Boden G, Chen X, DeSantis RA, Kendrick Z. Ethanol inhibits insulin action on lipolysis and on insulin release in elderly men. American Journal of Physiology-Endocrinology and Metabolism 1993; 265(2): E197–E202. [DOI] [PubMed] [Google Scholar]
- 9.de la Monte S, Derdak Z, Wands JR. Alcohol, insulin resistance and the liver-brain axis. J Gastroenterol Hepatol 2012; 27 Suppl 2(0 2): 33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Traversy G, Chaput J-P. Alcohol Consumption and Obesity: An Update. Current obesity reports 2015; 4(1): 122–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fazzino TL, Fleming K, Sher KJ, Sullivan DK, Befort C. Heavy Drinking in Young Adulthood Increases Risk of Transitioning to Obesity. Am J Prev Med 2017; 53(2): 169–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colditz GA, Giovannucci E, Rimm EB, Stampfer MJ, Rosner B, Speizer FE et al. Alcohol intake in relation to diet and obesity in women and men. Am J Clin Nutr 1991; 54(1): 49–55. [DOI] [PubMed] [Google Scholar]
- 13.He C, Fan D, Liu X, Wang Q, Zhang H, Zhang H et al. Insula network connectivity mediates the association between childhood maltreatment and depressive symptoms in major depressive disorder patients. Transl Psychiatry 2022; 12(1): 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta A, Mayer EA, Acosta JR, Hamadani K, Torgerson C, van Horn JD et al. Early adverse life events are associated with altered brain network architecture in a sex- dependent manner. Neurobiol Stress 2017; 7: 16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elton A, Tripathi SP, Mletzko T, Young J, Cisler JM, James GA et al. Childhood maltreatment is associated with a sex-dependent functional reorganization of a brain inhibitory control network. Hum Brain Mapp 2014; 35(4): 1654–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agarwal K, Demiral SB, Manza P, Volkow ND, Joseph PV. Relationship between BMI and alcohol consumption levels in decision making. International Journal of Obesity 2021; 45(11): 2455–2463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.First MB. Structured clinical interview for DSM-IV axis I disorders. Biometrics Research Department 1997. [Google Scholar]
- 18.First MB, Williams JB, Karg RS, Spitzer RL. Structured clinical interview for DSM-5—Research version (SCID-5 for DSM-5, research version; SCID-5-RV). Arlington, VA: American Psychiatric Association; 2015; 2015: 1–94. [Google Scholar]
- 19.Compton WM, Dawson DA, Goldstein RB, Grant BF. Crosswalk between DSM-IV dependence and DSM-5 substance use disorders for opioids, cannabis, cocaine and alcohol. Drug Alcohol Depend 2013; 132(1–2): 387–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Timeline followback: user’s guide. Addiction Research Foundation = Fondation de la recherche sur la toxicomanie … [Google Scholar]
- 21.Cohen RA, Hitsman BL, Paul RH, McCaffery J, Stroud L, Sweet L et al. Early life stress and adult emotional experience: an international perspective. Int J Psychiatry Med 2006; 36(1): 35–52. [DOI] [PubMed] [Google Scholar]
- 22.Sokołowski A, Dragan W. New Empirical Evidence on the Validity and the Reliability of the Early Life Stress Questionnaire in a Polish Sample. Front Psychol 2017; 8: 365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of Alcohol Withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). British Journal of Addiction 1989; 84(11): 1353–1357. [DOI] [PubMed] [Google Scholar]
- 24.Whitfield-Gabrieli S, Nieto-Castanon A. Conn: a functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connect 2012; 2(3): 125–141. [DOI] [PubMed] [Google Scholar]
- 25.Behzadi Y, Restom K, Liau J, Liu TT. A component based noise correction method (CompCor) for BOLD and perfusion based fMRI. Neuroimage 2007; 37(1): 90–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murphy K, Birn RM, Handwerker DA, Jones TB, Bandettini PA. The impact of global signal regression on resting state correlations: are anti-correlated networks introduced? Neuroimage 2009; 44(3): 893–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Galandra C, Basso G, Manera M, Crespi C, Giorgi I, Vittadini G et al. Salience network structural integrity predicts executive impairment in alcohol use disorders. Sci Rep 2018; 8(1): 14481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grodin EN, Cortes CR, Spagnolo PA, Momenan R. Structural deficits in salience network regions are associated with increased impulsivity and compulsivity in alcohol dependence. Drug Alcohol Depend 2017; 179: 100–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Padula CB, Tenekedjieva L-T, McCalley DM, Al-Dasouqi H, Hanlon CA, Williams LM et al. Targeting the Salience Network: A Mini-Review on a Novel Neuromodulation Approach for Treating Alcohol Use Disorder. Frontiers in Psychiatry 2022; 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society: Series B (Methodological) 1995; 57(1): 289–300. [Google Scholar]
- 31.Pilowsky DJ, Keyes KM, Hasin DS. Adverse childhood events and lifetime alcohol dependence. Am J Public Health 2009; 99(2): 258–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Enoch MA. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology (Berl) 2011; 214(1): 17–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moustafa AA, Parkes D, Fitzgerald L, Underhill D, Garami J, Levy-Gigi E et al. The relationship between childhood trauma, early-life stress, and alcohol and drug use, abuse, and addiction: An integrative review. Current Psychology 2021; 40(2): 579–584. [Google Scholar]
- 34.Robin RW, Chester B, Rasmussen JK, Jaranson JM, Goldman D. Prevalence, characteristics, and impact of childhood sexual abuse in a Southwestern American Indian tribe. Child Abuse Negl 1997; 21(8): 769–787. [DOI] [PubMed] [Google Scholar]
- 35.Koss MP, Yuan NP, Dightman D, Prince RJ, Polacca M, Sanderson B et al. Adverse childhood exposures and alcohol dependence among seven Native American tribes. Am J Prev Med 2003; 25(3): 238–244. [DOI] [PubMed] [Google Scholar]
- 36.Philip NS, Sweet LH, Tyrka AR, Price LH, Bloom RF, Carpenter LL. Decreased default network connectivity is associated with early life stress in medication-free healthy adults. Eur Neuropsychopharmacol 2013; 23(1): 24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cohodes EM, Kitt ER, Baskin-Sommers A, Gee DG. Influences of early-life stress on frontolimbic circuitry: Harnessing a dimensional approach to elucidate the effects of heterogeneity in stress exposure. Dev Psychobiol 2021; 63(2): 153–172. [DOI] [PubMed] [Google Scholar]
- 38.Ilomäki M, Lindblom J, Salmela V, Flykt M, Vänskä M, Salmi J et al. Early life stress is associated with the default mode and fronto-limbic network connectivity among young adults. Frontiers in Behavioral Neuroscience 2022; 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Corr R, Glier S, Bizzell J, Pelletier-Baldelli A, Campbell A, Killian-Farrell C et al. Triple Network Functional Connectivity During Acute Stress in Adolescents and the Influence of Polyvictimization. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging 2022; 7(9): 867–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zilverstand A, Huang AS, Alia-Klein N, Goldstein RZ. Neuroimaging Impaired Response Inhibition and Salience Attribution in Human Drug Addiction: A Systematic Review. Neuron 2018; 98(5): 886–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vuilleumier P, Armony JL, Clarke K, Husain M, Driver J, Dolan RJ. Neural response to emotional faces with and without awareness: event-related fMRI in a parietal patient with visual extinction and spatial neglect. Neuropsychologia 2002; 40(12): 2156–2166. [DOI] [PubMed] [Google Scholar]
- 42.Guell X, Schmahmann JD, Gabrieli J, Ghosh SS. Functional gradients of the cerebellum. Elife 2018; 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.E KH, Chen SH, Ho MH, Desmond JE. A meta-analysis of cerebellar contributions to higher cognition from PET and fMRI studies. Hum Brain Mapp 2014; 35(2): 593–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jenness JL, Peverill M, Miller AB, Heleniak C, Robertson MM, Sambrook KA et al. Alterations in neural circuits underlying emotion regulation following child maltreatment: a mechanism underlying trauma-related psychopathology. Psychological Medicine 2021; 51(11): 1880–1889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Evans GW. The Environment of Childhood Poverty. American Psychologist 2004; 59: 77–92. [DOI] [PubMed] [Google Scholar]
- 46.Herzberg MP, Gunnar MR. Early life stress and brain function: Activity and connectivity associated with processing emotion and reward. NeuroImage 2020; 209: 116493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Uddin LQ, Kelly AM, Biswal BB, Castellanos FX, Milham MP. Functional connectivity of default mode network components: correlation, anticorrelation, and causality. Hum Brain Mapp 2009; 30(2): 625–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Howell BR, Sanchez MM. Understanding behavioral effects of early life stress using the reactive scope and allostatic load models. Dev Psychopathol 2011; 23(4): 1001–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Oort J, Tendolkar I, Hermans EJ, Mulders PC, Beckmann CF, Schene AH et al. How the brain connects in response to acute stress: A review at the human brain systems level. Neuroscience & Biobehavioral Reviews 2017; 83: 281–297. [DOI] [PubMed] [Google Scholar]
- 50.Cavanna AE, Trimble MR. The precuneus: a review of its functional anatomy and behavioural correlates. Brain 2006; 129(Pt 3): 564–583. [DOI] [PubMed] [Google Scholar]
- 51.Frewen PA, Dozois DJ, Neufeld RW, Densmore M, Stevens TK, Lanius RA. Neuroimaging social emotional processing in women: fMRI study of script-driven imagery. Soc Cogn Affect Neurosci 2011; 6(3): 375–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Meyre D, Mohamed S, Gray JC, Weafer J, MacKillop J, de Wit H. Association between impulsivity traits and body mass index at the observational and genetic epidemiology level. Sci Rep 2019; 9(1): 17583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Han X-D, Zhang H-W, Xu T, Liu L, Cai H-T, Liu Z-Q et al. How Impulsiveness Influences Obesity: The Mediating Effect of Resting-State Brain Activity in the dlPFC. Frontiers in Psychiatry 2022; 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grodin E, Momenan R. Resting state connectivity and compulsivity: Association in alcohol use disorder. Neuropsychopharmacology 2017; 43: S452. [Google Scholar]
- 55.Colleluori G, Galli C, Severi I, Perugini J, Giordano A. Early Life Stress, Brain Development, and Obesity Risk: Is Oxytocin the Missing Link? Cells 2022; 11(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Entringer S, Buss C, Heim C. [Early-life stress and vulnerability for disease in later life]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2016; 59(10): 1255–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kaufman D, Banerji MA, Shorman I, Smith ELP, Coplan JD, Rosenblum LA et al. Early-Life Stress and the Development of Obesity and Insulin Resistance in Juvenile Bonnet Macaques. Diabetes 2007; 56(5): 1382–1386. [DOI] [PubMed] [Google Scholar]
- 58.Wang L, An C-X, Song M, Li N, Gao Y-Y, Zhao X-C et al. Evaluation of childhood traumatic experience as a risk factor for alcohol use disorder in adulthood. BMC Psychiatry 2020; 20(1): 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.al’Absi M. The influence of stress and early life adversity on addiction: Psychobiological mechanisms of risk and resilience. Int Rev Neurobiol 2020; 152: 71–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leng G, Adan RAH, Belot M, Brunstrom JM, de Graaf K, Dickson SL et al. The determinants of food choice. Proc Nutr Soc 2017; 76(3): 316–327. [DOI] [PubMed] [Google Scholar]
- 61.Koob GF, Bloom FE. Cellular and molecular mechanisms of drug dependence. Science 1988; 242(4879): 715–723. [DOI] [PubMed] [Google Scholar]
- 62.Sinha R. Chronic stress, drug use, and vulnerability to addiction. Annals of the New York Academy of Sciences 2008; 1141: 105–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Osadchiy V, Mayer EA, Bhatt R, Labus JS, Gao L, Kilpatrick LA et al. History of early life adversity is associated with increased food addiction and sex-specific alterations in reward network connectivity in obesity. Obesity Science & Practice 2019; 5(5): 416–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McLaughlin KA, Weissman D, Bitrán D. Childhood Adversity and Neural Development: A Systematic Review. Annu Rev Dev Psychol 2019; 1: 277–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kim P, Evans GW, Angstadt M, Ho SS, Sripada CS, Swain JE et al. Effects of childhood poverty and chronic stress on emotion regulatory brain function in adulthood. Proc Natl Acad Sci U S A 2013; 110(46): 18442–18447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rakesh D, Allen NB, Whittle S. Longitudinal changes in within-salience network functional connectivity mediate the relationship between childhood abuse and neglect, and mental health during adolescence. Psychological Medicine 2023; 53(4): 1552–1564. [DOI] [PubMed] [Google Scholar]
- 67.Herzog JI, Schmahl C. Adverse Childhood Experiences and the Consequences on Neurobiological, Psychosocial, and Somatic Conditions Across the Lifespan. Front Psychiatry 2018; 9: 420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Danese A, Widom CS. Objective and subjective experiences of child maltreatment and their relationships with psychopathology. Nature Human Behaviour 2020; 4(8): 811–818. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The information analyzed in this study from the NIAAA is bound by specific licenses and restrictions. The dataset is under the care and control of the NIAAA Office of the Clinical Director and is securely housed there. Dataset access requests are directed to Melanie Schwandt, melanies@mail.nih.gov.