Abstract
Stress exposure is associated with psychiatric conditions, such as depression, anxiety, and post-traumatic stress disorder (PTSD). It is also a vulnerability factor to developing or reinstating substance use disorder. Stress causes several changes in the neuro-immune-endocrine axis, potentially resulting in prolonged dysfunction and diseases. Changes in several transmitters, including serotonin, dopamine, glutamate, gamma-aminobutyric acid (GABA), glucocorticoids, and cytokines, are associated with psychiatric disorders or behavioral alterations in preclinical studies. Complex and interacting mechanisms make it very difficult to understand the physiopathology of psychiatry conditions; therefore, studying regulatory mechanisms that impact these alterations is a good approach. In the last decades, the impact of stress on biology through epigenetic markers, which directly impact gene expression, is under intense investigation; these mechanisms are associated with behavioral alterations in animal models after stress or drug exposure, for example. The endocannabinoid (eCB) system modulates stress response, reward circuits, and other physiological functions, including hypothalamus–pituitary–adrenal axis activation and immune response. eCBs, for example, act retrogradely at presynaptic neurons, limiting the release of neurotransmitters, a mechanism implicated in the antidepressant and anxiolytic effects after stress. Epigenetic mechanisms can impact the expression of eCB system molecules, which in turn can regulate epigenetic mechanisms. This review will present evidence of how the eCB system and epigenetic mechanisms interact and the consequences of this interaction in modulating behavioral changes after stress exposure in preclinical studies or psychiatric conditions. Moreover, evidence that correlates the involvement of the eCB system and epigenetic mechanisms in drug abuse contexts will be discussed.
Keywords: Drug abuse, Endocannabinoid System, Epigenetics, Stress
Overview of stress response and circuitry
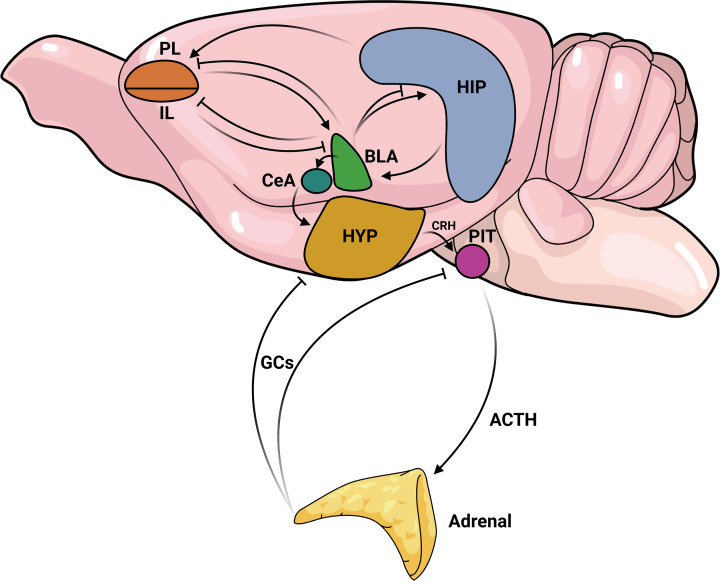
Stress is an important and evolutionarily conserved response that modulates several central nervous system (CNS) regions and the endocrine system to prepare the organism to face a challenging experience. The stressors, stimuli that trigger the stress response, can be chemical, physical, psychological, or combinations of these; and they can recruit different brain regions, which could overlap depending on the circumstances [1]. In general, stress exposure activates the hypothalamus–pituitary–adrenal (HPA) axis, leading to release of glucocorticoids (GCs) by the adrenal gland. GCs promote their stress effects mostly by activating glucocorticoid receptors (GR) in the periphery and in the brain, altering the expression of several genes to promote adaptation [2,3]. A simplified view of key brain regions involved in stress response is depicted in Figure 1. However, as reviewing this topic is beyond the scope of this study, the reader can find more comprehensive reviews about this topic, with figures summarizing the current knowledge, in several recent review studies [1,4–7]. Here, we will present some critical information about the central regions affected by stress, that influence behavioral response: the prefrontal cortex, amygdala, and hippocampus.
Figure 1. A simplified view of the key brain regions involved in the stress response.
The amygdala (basolateral-BLA and central-CeA nuclei) is a key region in initiating the stress response. It is an input region for projections sent by other regions, particularly by different subdivisions of the medial prefrontal cortex (mPFC). Specifically, the prelimbic region (PL) of the mPFC exerts excitatory influence on amygdala. In contrast, the infralimbic region (IL) inhibits the basolateral amygdala (BLA). The hippocampus (HIP) contributes to stress response by providing contextual information, with excitatory projections to the PL-mPFC and BLA. The BLA, in turn, inhibits the PL, IL, and has both inhibitory and excitatory projections to the HIP. The balance of these two projections controls the parallel HIP outputs. Integrating this information, the BLA activates the amygdala’s output region, the CeA, which sends excitatory projections to the hypothalamus (HYP), stimulating the production and release of corticotropin-releasing hormone (CRH). CRH acts on the pituitary gland triggering the synthesis and release of adrenocorticotropic hormone (ACTH). ACTH, in turn, is released in the blood and stimulates the synthesis of glucocorticoids (GCs) in the adrenal gland. Finally, released GCs establish a negative feedback loop within the hypothalamus and pituitary, modulating the peripheral and central nervous system areas to facilitate adaptive responses to stress. Depending on the duration and type of stressors, increased amygdala activity, cortical dysfunction and hippocampal atrophy can occur, impairing the ability of this adaptive response to occur, contributing to psychiatric disorders.
The prefrontal cortex (PFC) is responsible for complex functions such as integrating and processing different stimuli for decision-making, goal-directed behaviors, and working memory [8,9], in addition to emotional processing. The medial portion of the PFC (mPFC), the most studied in studies related to aversion and stress [10], is mainly divided into the prelimbic (PL) and the infralimbic (IL) portions, which can have distinct or opposite functions [11,12] due to their partially distinct connections and projections [13,14]. In general terms, the PFC is greatly activated during acute stress, and the excess of glutamate release and its impaired reuptake mediated by GCs may result in neurotoxicity [15], proinflammatory factors release, and neuronal death [16,17]. These changes can be related to the neuronal atrophy observed in the PFC of depressed and PTSD patients and animal models involving stress exposure [18,19] which could result in weakened PFC projections to the amygdala and hippocampus, impairing modulatory function exerted by PFC on these brain regions [20,21].
The amygdala is also an essential structure for emotional processing [5] and is divided into different nuclei. The basolateral nucleus (BLA) integrates and processes aversive/stressful stimuli received by several brain regions, being greatly activated during stressful events [5] and fear memory conditioning acquisition and consolidation [22,23]. BLA sends several outputs to the central nucleus (CeA) and the medial nucleus (MeA), which in turn project to other brain areas that will be responsible for triggering adaptative behaviors to facing stress [5]. As mentioned before, the amygdala receives inhibitory projections from the IL mPFC, which can be weakened after stressful situations, resulting in a lack of inhibition of BLA by the PFC and hyperactivation of the amygdala [24,25]. For instance, depressed and PTSD patients have bigger and more active amygdala than healthy volunteers [26–28].
Finally, the hippocampus, which is connected to the amygdala and PFC [29], comprises the dentate gyrus (DG) and Ammon’s horn/Cornus Ammonics (CA) subfields 1, 2, and 3. The CA1 region has outputs to several regions, including the PL and IL mPFC and BLA [30–32]. The hippocampus plays an important role in memory acquisition and discrimination of aversive contexts [33,34]. It also inhibits excessive activation of the HPA axis during stress response [35]. However, stress exposure can cause hippocampus atrophy and decreases neuronal plasticity, impairing its function and resulting, for example, in fear extinction learning deficits and fear generalization [33,36], anxiety-like and depressive-like behaviors [37]. Moreover, decreased hippocampal volume is reported in anxiety disorders, PTSD, and depression in humans [38–41]. Interestingly, based on a monozygotic twins study, it was suggested that a smaller hippocampal volume could be a risk factor for developing PTSD after traumatic events rather than a consequence of PTSD [42].
Although many other brain areas can be involved, it is well-known that a proper synchronization between the amygdala, mPFC, and hippocampus is necessary for adequate stress response and fear processing mechanisms. Therefore, impairment in this circuitry is frequently observed in psychiatric disorders. This poor connectivity can be associated with impaired molecular mechanisms in those brain regions, including dysfunctional neurotransmitter systems, such as endocannabinoids, and epigenetic modifications, which could control neuroplastic changes resulting in long-lasting consequences, such as impaired behavior.
The (endo)cannabinoid signaling in stress response
The endocannabinoid (eCB) system, activated by stress exposure, is considered a stress-buffer system and essential for several physiological conditions. The main eCBs are anandamide (AEA) and 2-arachidonoylglycerol (2-AG), which are produced on demand post-synaptically in response to an increase in neuronal activity, by actions of N-acyl phosphatidylethanolamine-specific phospholipase D (NAPE-PLD) and diacylglycerol lipase (DAGL) on membrane phospholipids, respectively. These eCBs are released in the synaptic cleft and act retrogradely in cannabinoid receptors (CB1/2) or post-synaptically in CB2, or in glial cells. CB1/2 are Gi-coupled receptors, then their activation result in the inhibition of adenylyl cyclase, the protein kinase A (PKA), and cellular Ca2+ influx, culminating in a blockade in neurotransmitter release that was increased before. Finally, AEA will be degraded by the fatty acid amide hydrolase (FAAH) enzyme mostly in the postsynaptic neuron, whereas 2-AG will be metabolized by the monoacylglycerol lipase (MAGL) enzyme in the presynaptic neuron [43].
Contrasting to CB1/2 receptors, the vanilloid receptor 1 (TRPV1) is expressed both pre- and post-synaptically. TRPV1 can be activated by AEA, increasing the Ca2+ influx and neurotransmitter release. Pieces of evidence suggest that AEA has its actions preferentially via CB1 receptors, whereas, at higher concentrations, the predominant effect could reflect its effects on TRPV1. This is one of the possible explanations for the bell-shaped dose-response curve often seen with AEA in behavioral responses [44]. It has been shown, for example, that by inhibiting CB1 receptors with an antagonist, the extinction learning process is impaired [45,46], and the treatment with a TRPV1 receptor agonist has a similar effect [47]. Moreover, the administration of a FAAH inhibitor facilitated the extinction learning process in wild-type mice [46]. Finally, the facilitation of CB1 signaling by a drug that blocks FAAH and antagonizes TRPV1 receptors is more potent in blocking the expression of fear conditioning than inhibiting these two targets individually, supporting the opposite role for CB1 and TRPV1 receptors in triggering fear behavior [48].
Overall, a very reductionist description of the eCB system is described here. In the past few years, several other targets of the eCB system were described, such as the G-protein-coupled receptor 55 (GPR55) and the peroxisome proliferator-activated receptor γ (PPARγ), which interact with eCBs and other substrates, promoting different effects. A more recent detailed review of this topic can be found in [43].
The eCB system is altered in several pathological conditions, such as cancer, gastrointestinal and cardiovascular diseases, eating disorders [49], and stress-related psychiatric conditions [39,40,50,51]. For instance, studies have shown that depressed women have decreased serum levels of AEA and 2-AG [52]. Moreover, depressed suicide victims have increased expression of CB1 receptors in the dorsolateral PFC [53]. Finally, genetic studies have shown that polymorphisms of the CB1 receptor have greater prevalence in depressed and anxious patients [54,55] and are correlated with treatment-resistant depression [56]. Interestingly, pharmacological studies indicate that the administration of rimonabant, a CB1 antagonist, increases symptoms of depression and anxiety in healthy individuals [57] and that the effects of conventional antidepressant drugs depend on the eCB signaling [58].
In PTSD patients, reduced peripheral AEA levels and higher expression of CB1 receptors in the brain are also reported [59]. Interestingly, non-PTSD individuals carrying the C385A allele of the rs324420 polymorphism, a mutation of the FAAH gene, had increased AEA levels, enhanced fear extinction [60], and lower amygdala reactivity during fear extinction recall [61]. Also, polymorphisms of the CB2 receptor and FAAH enzyme have been associated with greater susceptibility to childhood trauma and the development of psychiatry disorders later in life [62,63]. Other polymorphisms in the eCB system, including in the CB1 receptor, are associated with fear extinction and/or PTSD [64–66].
Altogether these data suggest a strong relationship between the eCB system and psychiatry conditions. Based on the existing evidence, impaired eCB signaling in the brain, induced by stress or as consequences of polymorphisms, could be involved in the neurobiology of stress-related disorders, including depression and PTSD. Therefore, targeting these changes in the eCB system is a potential tool to improve the outcome of those disorders, potentially achieving remission in treatment-resistant patients. However, this still need further investigation. More about these discussions can be found in excellent recently published reviews [64,67,68].
Animal model studies also corroborate the involvement of eCB signaling in the development of behavioral changes related to psychiatric symptoms. For instance, CB1 KO mice have elevated levels of depression- and anxiety-like behaviors after stress [69–72]. Moreover, these mice also have impaired fear extinction, a key feature of PTSD animal models [73]. Pharmacologically, these behavioral alterations are reproduced after chronic administration of CB1 antagonists [74,75]. CB1 agonists have also been shown to have antidepressant and anxiolytic effects after stress [76–78]. Furthermore, several papers reported the participation of the eCB system, particularly CB1 receptors, promoting fear extinction facilitation in different animal models [45,46,79,80]. CB2 participation in promoting behavioral responses seems to be more complex. The overexpression of this receptor promoted reduced levels of anxiety-like behaviors in the light-dark box and elevated plus maze in mice [81]. However, evidence shows that chronic administration of a CB2 antagonist produces an anxiolytic effect [82]. Another study from the same group observed that the overexpression of CB2 receptors reduced depressive-like behaviors in mice, whereas the administration of AM630, a CB2 antagonist, induced an antidepressant effect in wild-type mice. The drug had no effect in the transgenic line [83]. Moreover, CB2 KO mice have impaired contextual, but not cued, fear conditioning and enhanced spatial memory [84]. More studies using genetic and molecular techniques with specific cell types, such as microglia and astrocytes, are needed to investigate the interaction of CB2 expression and activity with other signaling systems involved in mood regulation and behavior.
Multiple mechanisms involved in the physiopathology of psychiatric conditions, like major depression, anxiety, and PTSD, can be regulated by the eCB system. Therefore, the resultant effects from eCB system manipulation have been related to several molecular alterations. For example, eCBs can counteract dysregulation in neurotransmitter systems [85–87], promote neuroplasticity [88,89], and attenuate inflammatory effects [90–93] induced by stress. In mice, both genetic deletion and the antagonism of CB1 receptors in the mPFC prolonged CORT release after stress. It has been proposed that the activation of CB1 in mPFC GABAergic interneurons disinhibits excitatory neuronal projections that are responsible for terminating stress response [94].
A more recent proposal regarding stress consequences implies the modulation of epigenetic mechanisms in the brain to promote behavioral changes. This review will focus on the crosstalk between the eCB system and epigenetics mechanisms to modulate the stress response. Considering a general knowledge about epigenetic mechanisms are necessary to understand how they can impact the eCB system, in the next section we will give an overview about this knowledge.
Key epigenetic mechanisms in stress response
Epigenetics focuses on the interaction between the environment and genome, whereby gene expression is modulated in response to new stimuli. In the short or long term after stress experiences, several epigenetic marks can be modified to adapt the organism to the environment; these marks can even be transmitted between generations. Because of a maladaptive response, these epigenetic changes can predispose the organism to diseases. There are three major epigenetic mechanisms for the regulation of gene expression: DNA modifications, histone modifications, and interference RNAs. Below, we will briefly describe each one of them, associating them with modifications in important stress-related systems.
DNA methylation
The DNA is passive to chemical modifications that do not change the nucleotide sequence but regulate gene transcription. Among many modifications described in the literature, cytosine methylation at the 5′ position (5mC) is the most investigated. The DNA-methyltransferases (DNMTs) family of enzymes in mammals, comprising DNMT1, DNMT3a, and DNMT3b, catalyzes the reaction of a methyl group addition to a cytosine [95]. The reaction occurs mainly in CpG dinucleotides, distributed throughout the genome but more concentrated in CpG islands in promoter regions of the genes. 5mC is recognized by methyl-CpG binding proteins (MBPs), such as methyl-CpG binding protein 2 (MeCP2), commonly related to psychiatry diseases [96,97]. 5mC is usually associated with the repression of gene expression, but it also can promote gene expression activation depending on the location of the CpG island in the gene body [98]. Despite some stability, DNA methylation is a dynamic process constantly subject to reversal (demethylation) by active and passive forms. The passive form occurs through DNA damage or replication, while the active form is a process based on methyl-cytosine modifications through the ten–eleven translocation (TET) enzyme family and the activation-induced cytidine deaminase/apolipoprotein B mRNA-editing enzyme complex (AID/APOBEC) [98].
Both DNA hyper- and hypomethylation of stress-related genes are found in various neuropsychiatric and neurological diseases [99–102]. Most clinical studies focus on genes related to glucocorticoid response and serotonin neurotransmission [100,103]. The promoter region of the glucocorticoid receptor gene (NR3C1) appears to be extremely sensitive to DNA methylation. Various stressor events, including child abuse, war and genocide-related trauma, maternal depression, or violence during pregnancy, correlate with increased [104–110] and decreased [105,111,112] methylation levels in NR3C1. Methylation of NR3C1 is also altered in the post-mortem brains of suicide victims and is associated with childhood traumatic experiences [113,114]. In these works, methylation levels frequently are inversely proportional to NR3C1 expression, and low levels of GR can directly impact the feedback of glucocorticoid release and HPA activity, contributing to altered responses to stress. Regarding the serotoninergic system, the serotonin transporter gene (SLC6A4) methylation levels are related to traumatic events, child abuse, work stress, and depression [115–121], and although it does not correlate with mRNA expression in the blood of patients, the hypomethylation of SLC6A4 is proposed to be a biomarker of diagnosis and drug response to major depression [118,122].
Histones modifications
Histones are proteins that, together with DNA, make the chromatin and organize its packaging state. There are four types of histones: H2A, H2B, H3, and H4. The addition of chemical groups to amino acid residues of the histones alters their binding to DNA modulating the access of transcription factors. The addition of group acetyl, or acetylation, is a modification primarily associated with gene expression. It occurs due to the action of histone acetyltransferases (HATs) and is erased by histone deacetylases (HDACs). Histone methylation is another modification related to gene expression or repression depending on the location of the methyl group. It is catalyzed by histone methyltransferases and reversed by histone demethylases, also occurring on lysine residues [123,124].
In humans, there are only a few works exploring histone mark changes in the context of stressful experiences and neuropsychiatric diseases. In these studies, they found differences in tri-methylation of H3 at lysine 27 (H3K27me3) and at lysine 4 (H3K4me3) levels in the brains of suicide victims when it was compared between control and depressive groups [125–127]. On the other hand, in animal models, several types of stressors, such as maternal separation, social stress, restraint stress, and chronic mild stress, induce alterations in HDACs and histone acetylation/methylation levels in a global or gene-specific manner [128–130]. Interestingly, antidepressant drugs with different mechanisms of action, such as ketamine, imipramine and fluoxetine, not only ameliorate behavior alterations after the stress but also alters HDACs activity and expression, or impact levels of acetylation at specific histone residues associated with important genes related to synaptic plasticity, such as Nr2b and Bdnf genes [131–138].
Non-coding RNAs
Micro RNAs (miRNAs), small interfering RNAs (siRNAs), long non-coding RNAs (lncRNAs), and piwi RNAs (piRNAs), along with others, are regulatory non-coding RNAs, which regulate transcription and translation processes most often through binding to mRNA [139]. Among these, miRNAs are the most characterized regarding their biogenesis and role in diseases. The binding of miRNA to complementary sequences of mRNAs induces their cleavage or, in the case of partial complementarity, induces the inhibition of translation in ribosomes [139].
miRNAs can either be regulated by stress signaling or act as a regulator of the stress response [140]. The capacity of a single miRNA to bind several mRNAs allows it to modulate entire cellular pathways, which in part explains altered levels of the same miRNA in different diseases. On stress-related diseases, it is possible to highlight some stress-regulated genes such as Nr3c1, Bdnf, Ntrk2, Slc6a4, and Crhr1 [141–144], which are also found to be regulated by histone modifications and DNA methylation [145–147]. Moreover, the miRNA network regulates and is regulated by proteins related to other epigenetic processes, such as HDACs, DNMTs, and MeCP2 [148]. Due to the stability and the facility to detect changes in easily accessible tissues, such as blood and saliva, miRNAs are indicated as excellent biomarker candidates for disease and treatment responsiveness [149].
Possible crosstalk between the eCB system and epigenetic mechanisms in stress response and psychiatric disorders
(Endo)cannabinoid control of epigenetic mechanisms
Cannabis use induces epigenetic alterations, supporting a relationship between the eCB system and epigenetic mechanisms. For instance, Cannabis-dependent patients have reduced methylation of the CB1 receptor gene promoter (Cnr1) and increased CB1 expression in the blood [150]. The same profile of methylation and CB1 expression was observed in peripheral blood lymphocytes of patients with schizophrenia reporting the use of Cannabis [151]. Moreover, prenatal Cannabis exposure decreased D2 receptors mRNA in Nucleus Accumbens (NAc) and amygdala of aborted fetuses, which was replicated in an animal model. In this model, there was increased di-methylation at lysine 9 of H3 (H3K9me2), a repressive mark, and decreased H3K4me3, mentioned earlier, an enhancer mark, and RNA polymerase II at the Drd2 gene locus [152,153], supporting the role of an epigenetic mechanism induced by Cannabis in decreasing D2 expression. These changes have implications for drug addiction, which will be discussed later, and other psychiatric conditions. For instance, the chronic administration of a CB1 agonist to adolescent male rats has been implicated in greater susceptibility to stress and anxiety-like behavior, in addition to increase DNMT and global methylation levels in the PFC of their adolescent offspring [154]. Also, paternal activation of CB2 receptors was implicated in impaired offspring growth via reduced expression of TET enzymes and altered DNA methylation in several genes [155].
Regarding treatment with CBD, it was demonstrated that acute CBD treatment decreased immobility in mice in the forced swimming test, similar to what was observed with DNMT inhibitors (5-AzaD and RG108). Interestingly, the combination of ineffective doses of CBD and DNMT inhibitors induced similar antidepressant effects, suggesting CBD effects could be directly modulating DNMTs. In fact, all drugs prevented the swimming stress-induced reduction of the DNA methylation in the PFC and the increase in the hippocampus. However, whereas the DNMT activity was decreased by swimming stress in the PFC and increased in the hippocampus, CBD could only counteract the first in this work [156]. In contrast, the hippocampal neurodegeneration induced by iron administration in neonatal rats, which induces mitochondrial DNA methylation alterations, was reverted by treatment with chronic CBD during adulthood [157]. Finally, subacute treatment with CBD induced hypomethylation of DNMT3a in the mouse hippocampus [158], a mechanism already shown to induce gene expression related to neurogenesis [159,160]. These pieces of evidence suggest a role for DNA methylation in CBD effects in animal stress models. As described before, many of these makers are also involved in stress-related disorders, and CBD has anxiolytic/antidepressant effects in psychiatric patients [161]. Therefore, it is possible to suggest that these CBD effects may involve DNA methylation; however, there are no studies in humans with this analysis, which would be very useful for better conclusions.
Histone modifications may also be involved in effects mediated by cannabinoids. Repeated co-administration of THC and CBD increased the acetylation in lysine 9 (H3K9ac) and 14 (H3K14ac) of H3 in the ventral tegmental area of adult mice [162]. In another study, acute CBD treatment increased levels of methylation and acetylation markers H3K4me3, H3K27me3, and H3K9ac in the cerebral cortex. In contrast, it decreased H3K9ac levels in the hypothalamus and H3K4me3 in the pons in rats, demonstrating that its effects are brain area-specific [163].
Chronic unpredictable stress (CUS) increased the nuclear expression and activity of HDAC2 and decreased the expression of CB1 levels, mainly in glutamatergic neurons, in the mouse cingulated cortex. Moreover, CUS reduced the expression of H3K9ac associated with CB1 and Neuropeptide Y (NpY) genes. They also showed that URB597, a FAAH inhibitor, which is expected to increase anandamide levels, reverted stress effects in the Npy gene, but not in Cnr1, and anxious behavior [164]. Like stress, a TRPV1 agonist (capsaicin), which increased immobility in the forced swimming test, increased HDAC2 expression in the mouse DG of the hippocampus [165] and enriched HDAC2 expression at Dlg4, Syp, Gria1, and Gria2 gene promoters, all related to neuroplasticity [166]. In contrast, genetic deletion of TRPV1 receptors, which induced an antidepressant-like phenotype, reduced HDAC2 levels in the same brain region and consequently increased levels of H3 and H4 global acetylation. In addition, TRPV1 knockout mice, contrary to what was observed with capsaicin injection, showed increased levels of plasticity and neurogenesis-related genes in the hippocampus, in addition to being resilient to stress [166]. Therefore, considering anandamide activates CB1 and TRPV1 receptors, we suggest that the bell-shaped profile of anandamide effect on behavior may be mediated by differential effects on CB1 and TRPV1 receptors, among other mechanisms, regulating the expression and activity of HDAC2, histone acetylation levels, gene expression, and neuroplasticity.
As described before, miRNAs play an essential role in gene expression regulation, being implied in several diseases. eCB system activity, in turn, seems to regulate miRNA expression and, therefore, could impact the pathogenesis and treatment of stress-related diseases. In mice, chronic mild stress (CMS) increased expression of some miRNAs in the PFC (miR-9-5p, miR-128-1-5p, and miR-382-5p) [167] that target Drd2, Clock, Map2k, Mapk1, and Bdnf genes [168–170], all related to the physiopathology of depression. Moreover, CMS induced decreased expression of others miRNAs (miR-16-5p, miR-129-5p, and miR-219a-5p) [167], which target Slc6a4, Htr2a, Bdnf, Grm7, Camk2a, and Camk2g genes, which are also related to depression physiopathology and antidepressant response [168,171–174]. In the same study, stressed animals treated with anandamide showed increased expression of all these miRNAs compared with the vehicle group; the depressive-like effect of stress in the forced swimming test was reverted [167]. Moreover, early life stress-induced depressive-like behavior in rats and downregulated miR-16 in males and miR-135a in females in the mPFC. These changes were reversed when rats received a FAAH inhibitor [175].
Additionally, lower expression levels of let-7d miRNA were observed in the cortex and hippocampus of CB1 knockout mice or after CB1 knockdown in zebrafish embryos. Conversely, the knockdown of let-7d in zebrafish embryos increased the expression of CB1 receptors, suggesting negative feedback in this regulation [176,177]. Moreover, let-7d overexpression in adult mouse hippocampus induced anxiolytic- and antidepressant-like effects [178]. Thus, it is arguable that anxiolytic and antidepressant effects induced by CB1 activation are promoted by let-7d expression and that this mechanism may be impaired in psychiatric conditions, such as depression. Furthermore, the anxiolytic and antidepressant effects induced by let-7d increased expression may occur, between other mechanisms, by the negative regulation of dopamine D3 receptors, mu-opioid receptors, TLX, an orphan nuclear receptor, and upregulation of miR-9, regulating neuroplasticity, cellular proliferation, neuronal differentiation, and migration [178–180].
In summary, the eCB system activity regulates the expression and activity of epigenetic enzymes, such as TETs, DNMTs, and HDACs, which result in differential global and specific-site levels of DNA and histone modifications. Moreover, the eCB system is also involved in miRNA expression regulation. All these alterations change gene expression related to neurotransmission, neurogenesis, and neuroplasticity. These mechanisms, also altered by stress, may be involved in the development of psychiatric conditions; therefore, more studies are needed to better understand how they work in physiological and pathological conditions to determine if they could be targets for treating these conditions.
So far, only a few studies combine stress protocols, modulation of the eCB system, and evaluation of epigenetic output, highlighting the need for more studies addressing that combination. These studies are summarized in Table 1. How eCB system molecules modulate epigenetic factors in stress-related contexts are outlined in Figure 1A.
Table 1. Studies combining stress protocol, eCB system modulation and epigenetic output in animal models.
| Pharmacological intervention | Sex, strain, age | Stress | Behavioral outputs | Molecular outputs | Reference |
|---|---|---|---|---|---|
| Prenatal CB1 agonist (WIN55212-2; 1.2 mg/Kg/day); from PND30 to PND49 | ♂ Rats, adolescent and adult | Offspring (PND60) exposed to Unpredictable stress during one week | Anxiogenic effect in the OFT induced by WIN in stressed offspring (PND68) | WIN ↑ global methylation and DNMT3a levels in the PFC of stressed offspring WIN ↑ DNMT1 levels in the PFC only in non-stressed offspring |
[154] |
| FAAH inhibitor (URB-597; 1.0 mg/Kg/day); from the 5th to the 11th week of stress protocol |
♂ mouse, 6 weeks old | CUS for eleven weeks | Not evaluated | CUS ↑ expression and activity of HDAC2 in the cingulate cortex CUS ↓ expression of H3K9ac associated with npy and cnr1 genes in the cingulate cortex URB reverted the effect of stress in the npy gene |
[164] |
| TRPV1 KO TRPV1 KD in DG |
♂ mouse, 4-5 weeks old | CUS for 14 days | CUS induced learned helplessness (LHT) in WT, but not in TRPV1 KO. Antidepressant- and anxiolytic effect of TRPV1 KO in the FST and NSFT, independent of stress exposure. TRPV1 KD in the DG mimics the TRPV1 KO phenotype in the FST |
↓ HDAC2 levels in the hippocampus of TRPV1 KO ↑ H3 and H4 global acetylation levels in TRPV1 KO hippocampus ↑ expression of neuroplasticity and neurogenesis genes in TRPV1 KO hippocampus TRPV1 KD in the DG mimics the TRPV1 KO phenotype |
[166] |
| AEA; 5 mg/Kg/day; After forced swimming pretest, 5 hours before and 1 hour after FST | ♂ mouse, 3 months old | CMS for 7 weeks | CMS induced depressive-like behavior in the FST and SPT AEA ↓ the stress effect in the FST |
CMS ↑ miR-9-5p, miR-128-1-5p, and miR-382-5p, and ↓ miR-16-5p, miR-129-5p, and miR-219a-5p expression in the PFC AEA ↑ expression of miR-9-5p, miR-128-1-5p, miR-382-5p, miR-16-5p, miR-129-5p, miR-219a-5p in the PFC of stressed mice |
[167] |
| FAAH inhibitor (URB-597; 0.4 mg/Kg/day); From PND45 to PND60) | ♂ and ♀ rats | ELS (from PND7 to PND 14) | ELS: ♂: ↓ distance traveled and ↑ freezing time in the OFT; ♀: ↑ freezing time in the OFT; URB treatment: ↑ SP in stressed ♂ and ♀; ↓SP in non-stressed ♀; ↑ the SR discrimination index in stressed ♂ and ♀; ↓ SR in non-stressed ♂; ↓ immobility in the FST in stressed ♂ and ♀; ↑ immobility in FST in non-stressed ♂; |
URB treatment: ↑ expression of miR-135a in the mPFC and ↓ it in the LHa and DR of non-stressed ♂ and ♀; Normalized the expression of miR-135a in the mPFC of stressed ♀; ↓ expression of miR-135a in the CA1 region of non-stressed ♂; ↑ the expression of miR-135a in the CA1 region of non-stressed ♀; ↓ miR-135a expression in the DR of stressed ♀; Normalized the expression of miR-16 in the mPFC of stressed ♂; ↑ expression of miR-16 in the mPFC of non-stressed ♂ ↑ expression of miR-16 in CA1 region of non-stressed ♀ ↑ expression of miR-16 in the LHa of stressed ♂ ↓ expression of miR-16 in the LHa of non-stressed ♀; ↑ expression of miR-16 in the DR of stressed ♀; |
[175] |
↑: increased; ↓: decreased; ♀: female animals; ♂: male animals; AEA, anandamide; CA1, Cornus Ammonics subfield 1 of hippocampus; CB1 and CB2, cannabinoid type 1 and 2 receptors; CMS, chronic mild stress; CUS, chronic unpredictable stress; DG, dentate gyrus; DNMT, DNA-methyltransferase; DR, dorsal raphe; ELS, early life stress; FAAH, fatty acid amide hydrolase; FST, forced swimming test; HDAC, histone deacetylase; KD, knockdown; KO, knockout; LHa, lateral habenula; LHT, learned helplessness test; mPFC, medial prefrontal cortex; NSFT, novelty suppressed feeding test; OFT, open field test; PFC, prefrontal cortex; PND, postnatal day; SP, sucrose preference; SPT, sucrose preference test; SR, social recognition; TRPV1, transient receptor potential vanilloid type 1.
Epigenetic control of the endocannabinoid system
Although the relevance of the epigenetic mechanisms to the activity of the endocannabinoid system is well known [181–184], this regulation in the context of stress is less explored. The investigation of epigenetic control of the eCB system relies mainly on the regulation of Cnr1 and Faah genes. This specificity can be explained by the attention these two genes receive due to their pharmacological importance in physiology and disease and their susceptibility to being regulated by epigenetic marks.
DNA methylation levels of Cnr1, for example, is reported to be inversely proportional to mRNA and protein expression of the gene [185–191]. Cnr1 methylation pattern is recurrently found altered in a variety of situations, such as diet [190,192,193], patients with schizophrenia [189], and THC consumption [150]; Cnr1 is also susceptible to demethylation by the agent 5-aza-2-deoxycytidine [194]. On the other hand, Faah hypermethylation is associated with alcohol consumption [195], while hypomethylation, along with an increase in mRNA and protein expression, is related to Alzheimer’s disease patients [196]. Nonetheless, the methylation of Cnr1 and Faah in stressful conditions are less explored. Chronic stress induces depressive-like behavior and results in hypermethylation in Cnr1 [188], including in several CpG islands of Cnr1 gene in sperm of the stressed rats and in their offspring’s brains [197]. In PTSD patients, the Cnr1 gene was one of several uniquely methylated genes found in patient’s PBMC [198], suggesting variations in CB1 expression could be involved in the pathology of this disease, as well as other psychiatric diseases, as discussed in previous reviews [67,199].
Histone modifications are also found in Cnr1 and Faah genes. Ethanol treatment in mice is correlated with an increase in histone acetylation marker H4K8a and Cnr1 expression and a decrease in histone methylation marker H3K9me2 in the neocortex and hippocampus [200,201]. On the other hand, histone methylation marker H3K9me2 and mRNA expression of the Cnr1 gene are induced at dorsal root ganglion in a model of nerve injury in mice [202]. Although no change in DNA methylation was observed in a model of binge-eating behavior, histone acetylation H3K9ac associated with the Faah gene and its mRNA expression decreased after frustration stress [203]. Moreover, after exposure to CUMS, histone acetylation H3K9ac decreased in the Cnr1 gene, although its mRNA expression remained unchanged [164].
Several miRNAS are reported as modulators of genes of the eCB system, including genes of Cnr1, Cnr2, and Faah (Table 2). Except for the miR-let-7d, which inhibits but does not have Cnr1 as a direct target [176], all described miRNAs have predicted pairing to their targets so far [176,192,204,205,206,207,208,209,210,211]. All these miRNAs directly bind to the transcript, inhibiting eCB-related gene expression.
Table 2. miRNAs related to the eCB system in animal models involving stress exposure or in psychiatric patients.
| Gene | miRNA | Population/Model | Sample | Results | Reference |
|---|---|---|---|---|---|
| Cnr1 | MiR23a [192] | CSD susceptible mice | Hippocampus | ↑ | [212] |
| miR-29a [204] | MS-ARS rats | mPFC | ↑ | [213] | |
| Treatment-resistant depression | Serum | ↓ | [214] | ||
| Chronic academic stress students | Total blood | ↑ | [215] | ||
| ARS mice | Basolateral amygdala | ↑ | [216] | ||
| miR-29b [205] | MDD patients | Cerebral spinal fluid | ↑ | [217] | |
| CUMS mice | PFC | ↓ | [218] | ||
| ARS mice | FC | ↑ | [219] | ||
| Fear conditioning mice | Hippocampus | ↓ | [220] | ||
| miR-30b [206] | MDD suicide subjects | PFC | ↑ | [221] | |
| ARS mice | FC | ↑ | [219] | ||
| CSD rats | Ventral hippocampus | ↑ | [222] | ||
| CUMS resilient mice | Amygdala | ↓ | [223] | ||
| Fear conditioning mice | Hippocampus | ↓ | [220] | ||
| miR-128 [207] | PTSD patients | Total blood | ↓ | [224] | |
| Tail shocks rats | Amygdala | ↑ | [225] | ||
| Fear conditioning mice | PFC | ↑ | [226] | ||
| Fear conditioning mice | Hippocampus | ↑ | [220] | ||
| MDD patients after escitalopram treatment | Total blood | ↑ | [146] | ||
| Depressed suicide subjects | Amygdala | ↑ | [225] | ||
| miR-301ª [192] | Depressed suicide subjects | PFC | ↓ | [227] | |
| CUMS mice | Ventral tegmental area | ↓ | [228] | ||
| miR-338-5p [208] | Psychological stress susceptible mice | PFC | ↑ | [229] | |
| CUMS resilient mice | Amygdala | ↓ | [223] | ||
| miR-494 [209] | Depressed suicide subjects | PFC | ↓ | [227] | |
| MDD patients | Plasma | ↑ | [230] | ||
| Ethanol exposed rat overexpressing antagomiR-494 | Amygdala | Anxiolytic | [231] | ||
| MDD patients after escitalopram treatment | Total blood | ↑ | [146] | ||
| MDE patients | Peripheral blood mononuclear cells | ↑ | [232] | ||
| PTSD Rat model | Serum | ↑ | [233] | ||
| ARS mice | FC | ↓ | [219] | ||
| miRNA let-7d [176] | ARS mice | PFC | ↓ | [234] | |
| MDD patients | Total blood | ↓ | [235] | ||
| MDD patients after escitalopram treatment | Total blood | ↓ | [146] | ||
| PTSD mice model | PFC | ↓ | [236] | ||
| Hypothalamus | ↑ | [236] | |||
| Mice overexpressing miRNA let-7d | Hippocampus | Anxiolytic | [178] | ||
| Antidepressant | [178] | ||||
| CUMS resilient mice | Amygdala | ↑ | [223] | ||
| Fear conditioning mice | Hippocampus | ↓ | [220] | ||
| Cnr2 | miR-187-3p [210] | ARS mice | Basolateral amygdala | ↓ | [216] |
| Contextual fear conditioning mice | Dorsal hippocampus | ↓ | [237] | ||
| Extinction of contextual fear conditioning mice | Basolateral amygdala | ↑ | [238] | ||
| Psychological stress susceptible mice | mPFC | ↓ | [229] | ||
| CUMS susceptible mice | Amygdala | ↓ | [223] | ||
| miR-665 [209] | CUMS resilient mice | Amygdala | ↑ | [223] | |
| Faah | mir-411 [211] | MS rats | Hypothalamus | ↑ | [239] |
| MS rats | PFC | Inversely proportional to sucrose preference | [240] | ||
| CUMS rats | Hippocampal Dentate Gyrus | ↑ | [241] |
↑: miRNA up-regulation; ↓: miRNA down-regulation; ARS, acute restraint stress; CRS, chronic restraint stress; CSD, chronic social defeat; CUMS, chronic unpredictable mild stress; MDD, major depressive disease; mPFC, medial prefrontal cortex; MS, maternal separation; PFC, prefrontal cortex, PTSD, post-traumatic stress disorder.
Similar to what is seen in studies evaluating DNA methylation and histone modifications related to the eCB system, most works describe miRNAs regulating Cnr1 expression in the context of stressful or psychiatric conditions. For instance, miR-128 is down-regulated in the blood of PTSD patients [224] but is up-regulated in the brain of depressed subjects [225]; however, it is also reported to increase in blood after 12 weeks of antidepressant treatment [146]. Overall, these data could suggest that miR-128 participates in disease and treatment response, but this pattern can be different depending on the psychiatric condition and the evaluated tissue. In animal models, miR-128 up-regulation is found in the amygdala, PFC, and hippocampus of stressed mice [220,225,226], which indicates it can participate in brain functions. Another miRNA, miR-301a, is also up-regulated in the brain of depressed suicide victims [227] and chronically stressed rats [228]. miR-494 findings in the blood and brain are contrasting: it was upregulated in blood of major depression patients [235] and after antidepressant treatment [146], in depression episodes [232], in a PTSD rat model [233]; however, it was downregulated in the brain of depressed suicide victims [227] or in the brain of acutely stressed rats [219]. miR-494 also had an anxiolytic effect in ethanol-exposed rats [231]. Moreover, miR-29a is up-regulated in the blood of stressed students but down-regulated in treatment-resistant depression patients [214,215]. After restraint stress, rats subjected or not to maternal separation have up-regulation of miR-29a in the amygdala and PFC [216], which is increased in the cerebral spinal fluid of MDD patients [217]; it is also increased in the frontal cortex of mice exposed to acute restraint stress [219] but decreased in the frontal cortex after chronic stress [218] and in the hippocampus 1 h after footshock stress in a fear conditioning paradigm [220]. Similarly, 1 h after fear conditioning, there was also a reduction in the miR-30b expression in the hippocampus [220], as seen after acute restraint stress [219], whereas chronic stress increases the same miR-30b in the hippocampus [223]. Another miRNA, miR-let-7d, appears to be important in various stress processes. It was reduced in the blood of MDD patients, and increased after antidepressant treatment [146,235]; its levels changed in the PFC, hypothalamus, hippocampus, and amygdala of animal models after different types of stressors [220,223,234,236]. Meanwhile, overexpression of miR-let-7d in the hippocampus has anxiolytic and antidepressant effects in mice, corroborating its function in behavior and potential impact in neuropsychiatry diseases [178]. Although there is no evidence of alterations in humans, miR-338-5p and miR-23a are altered after protocols of social stress and chronic unpredictable stress [212,223,229]. These works evidence a complex control by different miRNAs, including similarities or differences among patients with different psychiatric conditions and differences in animal models involving stress exposure.
There are two miRNAs reported to modulate Cnr2 in animal models of stress: miR-187-3p and miR-665. miR-187-3p is regulated in several stress protocols, including chronic mild stress, acute restraint stress, psychological stress, and after fear conditioning, indicating that miRNA as having an important role in stress responses in general [216,223,229,237,238]. Both acute and chronic stressors can decrease miR-187-3p expression in the amygdala, while it was up-regulated after the evaluation of extinction of conditioned fear memory [238]. Additionally, miR-665 is altered in the amygdala, being up-regulated after chronic mild stress [223]. miR-411, for the best of our knowledge, is the only FAAH miRNA regulated by stress, and it is only found regulated in animal models; it was increased in the hypothalamus, PFC, and hippocampus after maternal separation or chronic unpredictable mild stress [239–241].
eCB system genes are considerably sensitive to epigenetic control, particularly under stressful experiences, although the mechanisms are not completely elucidated. The discussed evidence highlights the importance of epigenetic mechanisms in the eCB system response to stress and in its dysfunction. For instance, histone modifications are fundamental to memory consolidation and extinction [242,243], and intervention in these processes could be key to treating trauma-related disorders. In fact, some stressors can induce histone modifications in the Faah and Cnr1 genes, which can reverberate or not in mRNA expression; moreover, the histone modifications, as acetylation, is one of the proposed mechanisms for the action of antidepressant drugs [244]. Even when the gene or the protein expression is not altered, epigenetic markers can influence the gene expression pattern in response to the environment. DNA methylation and miRNA expression are already suggested as biomarkers of disorders, prognosis, treatment prediction, and response. Considering the findings with the CB1 receptor in human and animal models, epigenetic modifications in the Cnr1 gene are promising biomarkers in neuropsychiatry conditions [67].
Possible cross-talk between eCB system and epigenetics in drug abuse and stress
The eCB system is critical to the reward-related effects of dopamine, which is involved in the neurobiological mechanism underlying drug addiction [245]. Indeed, the modulation of the eCB system regulates molecular and behavioral responses promoted by distinct addictive drugs, including psychostimulants and alcohol [246,247]. Stress is an important risk factor in the neurobiology of drug addiction [248,249]. Previous stress exposure is correlated to the vulnerability to developing the disorder and the reinstatement of drug seeking. Interestingly, behavioral and molecular evidence indicates that the eCB system is a required element in the ability of stress to modulate drug responses [250,251]. This convergence is consistent with the fact that exposure to addiction drugs promotes changes in important brain structures also involved in stress biology, such as the PFC, nucleus accumbens, hippocampus, and amygdala, which are also important targets for cannabinoids [252]. In this way, similarly to what was described for stress events, exposure to addiction drugs also modulated the eCB system, which involves epigenetic mechanisms.
For instance, cocaine self-administration (SA) promotes histone modifications and chromatin looping in the eCB system-associated genes [253]. Animals exposed to cocaine demonstrated increased H3K4me3 enrichment on the hippocampus’s promotor regions of FAAH and DAGLα coding genes. Moreover, using a 4C-seq approach targeting the Cnr1 promoter, authors also demonstrated that cocaine SA induces remodeling of chromatin loops in the hippocampus and the NAc, suggesting that 3D chromatin architecture at the Cnr1 locus was substantially changed following cocaine exposure [253]. Pieces of evidence also have demonstrated that the eCB system undergoes epigenetic modulation by alcohol, as briefly mentioned before. A blind epigenome-wide analysis of datasets that explored hazardous drinkers and binge drinkers versus controls evidenced that Faah hypermethylation is associated with alcohol consumption [195]. Accordingly, an elevation in the expression of CB1 associated with increased H4K8ac at the Cnr1 promoter was observed in adult mice exposed to alcohol on postnatal day 7 (PD7) [254]. These results provide evidence that epigenetic mechanisms contribute to altered regulation of the eCB system in response to specific abuse drugs.
Interestingly, epigenetic changes promoted by exposure to alcohol also appear to be modulated by the eCB system. Nagre and colleagues observed that treatment with ethanol in PD7 mice impaired DNA methylation through reduced DNA methyltransferases (DNMT1 and DNMT3A) levels; these effects were reversed by the blockade of CB1 before ethanol treatment [255]. Similarly, alcohol exposure at the PD7 was associated with enhanced HDAC1, HDAC2, and HDAC3 expression, which was also prevented by administering a CB1 receptor antagonist before alcohol exposure [256]. Moreover, using a similar protocol, another study demonstrated that exposure to ethanol activates the apoptotic caspase-3 enzyme via CB1 in neonatal mice and causes a reduction in MeCP2 levels [257]. Regarding miRNA processes, a reduction in the expression of brain CB1 was coupled with an increased complementary miR-26b in a mouse model of fetal alcohol spectrum disorders [258].
Corroborating the role of the eCB system in the regulation of drug response during development, converging pieces of evidence support that treatment with THC in early phases of development promotes epigenetic changes [259]. For instance, prenatal THC exposure significantly modifies the histone methylation profile in the NAc. Subjects exposed to THC during prenatal stage showed a decreased level of the H3K4me3 [152]. Similarly, persistent changes in H3K9, increased dimethylation and reduced trimethylation, were observed in the NAc of adult rats following adolescent THC exposure [260]. Another study observed a significant increase of H3K9me2 in the hippocampus and the amygdala of female rats exposed to THC during adolescence [261]. Moreover, using the same adolescent THC exposure, there was an enhancement in H3K9me3 in the nucleus accumbens, hippocampus, and PFC [261,262]. Preconception THC exposure also disrupts DNA methylation in the NAc, with cross-generational effects. In a study comparing rats with or without parental THC exposure, 1027 differentially methylated regions (406 hypermethylated and 621 hypomethylated) associated with parental THC exposure were found in the subsequent generation, even though they were not directly exposed to the drug [263].
Confirming the correlation between the inheritance of paternal epigenetic changes and cannabinoid exposure, developmental changes in the offspring were associated with premating paternal THC exposure [264]. Exposure to cannabinoids has also been associated with changes in sperm DNA methylation. The analysis of sperm DNA from adult rats exposed to 2 mg/kg of THC for 12 days identified 627 genes whose methylation status was altered [265]. Similarly, significant differential methylation of genes related to neurodevelopment was observed in the sperm of rats exposed to THC via oral gavage [266]. Similarly to the preclinical reports, substantial changes in both hypo- and hyper-DNA methylation, with the latter predominating, were determined in the sperm methylome of marijuana smokers [265]. The impact of cannabis exposure on DNA methylation status also was investigated directly in human spermatogenesis in vitro. The results revealed alterations in DNA methylation levels of genes related to autism, HCN1, and NR4A2 [267]. These studies provide compelling evidence that preconception exposure to cannabinoids can impact reproduction and paternal epigenetic inheritance, potentially leading to altered DNA methylation patterns that have an impact on gene expression and developmental outcomes in offspring.
Altogether these findings support the idea that the eCB system is involved in regulating epigenetic mechanisms and has an essential role in the effects of addictive drugs. Since this response profile also was observed with stress exposure and considering the role of stress in the neurobiology of the substance use disorder, future studies might evaluate the involvement of the eCB system in the modulation of drug addiction by stress.
Final remarks
In the last two decades, much attention was directed toward understanding how exposure to different stressors could result in long-term changes in the organism that could result in psychiatric disorders. In this context, a boom of studies evaluating epigenetic changes in animal models and a run to find epigenetic markers related to psychiatric conditions arose, bringing many new understandings in the neurobiology of psychiatric conditions.
Among several physiological systems affected by epigenetic modulation, one has, in particular, been in the spotlight of scientists for more than 20 years: the endocannabinoid system. As overviewed in this review, the eCB system has a fundamental role in controlling many functions, including the fine control of stress response and circuits involved in drug abuse. Although not fully explored, eCB system genes are sensitive to epigenetic control [183,184,268,269]. The discussed evidence highlights the importance of epigenetic mechanisms in the eCB system response to stress, drugs of abuse, and the dysfunctions caused by them. As epigenetic marks can persist, the long-term alteration in the expression of cannabinoid-related proteins may be part of triggering diseases, particularly after stressors or substance use disorder. More recently, as discussed, many studies have investigated if the behavioral consequences of exposure to stressors in animals’ models could result in epigenetic regulation of the eCB system. Changes in miRNAs that regulate eCB system molecules, for example, are observed after acute protocols of stress in animal models but also in postmortem brains of depressive subjects. Epigenetic changes can persist through generations, indicating how stress and drug exposure, for example, can modify the neurobiology along the generations.
As also discussed, in animal models, cannabinoids, including THC and CBD, promote several behavioral changes related to psychiatric disorders and induce epigenetic modifications, mainly related to DNA methylation and histone modifications. Besides, Cannabis use in humans appears to induce epigenetic changes not only in the eCB system but also in the dopaminergic system and others, indicating a potential mechanism by which it could lead to psychiatric disorders, including substance use disorder. Finally, exposure to cannabinoids during critical periods of brain development can induce persistent brain and behavioral changes in adulthood.
As summarized in this review, therefore, there appears to have a close relationship between modulation of the eCB system and evaluation of epigenetic changes (DNA methylation, histones modifications, and miRNAs) under stress conditions (Figure 2A) and how epigenetic markers under stress conditions, mainly miRNAs, influence the expression of eCB-related molecules (Figure 2B). Furthermore, common drugs of abuse, including alcohol, cocaine, and cannabis (THC), could promote their long-term effects by promoting epigenetic changes that impact the eCB system (Figure 2C). The elucidation of epigenetic mechanisms controlling, or being controlled by, the eCB system in stress-related disorders is essential to better understand the neurobiology of those disorders and to provide new treatment approaches. Finally, understanding the cross-talk between those systems can potentially lead to the identification of biomarkers, such as miRNAs, which could help to predict the course of the disease and treatment response.
Figure 2. Mechanisms involved in the cross-talk between the eCB system and epigenetic mechanisms in stress- and drug abuse-related contexts.
(A) In stressful contexts, interference with the eCB system can modulate a wide range of epigenetic factors. CB1 receptors, for example, modulate the expression of DNMTs and the microRNA let-7d. Moreover, the inhibition of FAAH and consequent increase in AEA levels, which may act at CB1 receptors, increases the expression of several miRNAs (miR-9-5p, miR-128-1-5p, miR-382-5p, miR-16-5p, miR-129-5p, miR-219a-5p, miR-16, and miR-135a) and H3K9ac levels at npy gene, and decreases the expression and activity of HDAC2. Moreover, TRPV1 receptors activation increases the expression of HDAC2 and reduces global H3/H4 acetylation levels. Finally, CB2 receptors have been shown to reduce TET enzyme levels. (B) Stress can regulate eCB genes through epigenetics tools. CB1 expression is reported to be sensitive to hypermethylation and increased levels of H3K9ac of the gene and affected by miRNAs (miR-23a, miR-29a, miR-29b-3, miR-30b, miR-128, miR-301a, miR-338-5p, miR-494, and miR-let-7d). FAAH expression may also be altered by H3K9ac and the miR-411. Furthermore, CB2 is one target of miR-187-3p and miR-665 expression. (C) The cross-talk between the systems in the context of drug abuse is very diversified since drugs with different mechanisms of action promote different alterations. For example, alcohol increases H4K8ac in the CB1 gene, and its protein expression is related to the down-regulation of MeCP2. Alcohol also down-regulates DNMT1 and DNMT3a and upregulates HDAC1, HDAC2, and HDAC3, and all these effects are blocked by CB1 antagonism. Moreover, DNA methylation of the FAAH gene is affected by alcohol exposure. Cocaine consumption is reported to increase H4K9me3 in FAAH and DAGLα genes. Regarding exposure to cannabinoids, THC induces global levels of H3K4me3 and H3K9me2 and can increase or decrease H3K9me3 depending on the exposure. More details about these mechanisms can be found in the main text. Dashed arrows indicate inhibition or reduction. Continuous arrow indicate induction or increase. Question mark indicates that the CB1 involvement after FAAH inhibition was not directed tested.
Abbreviations
- AID-APOBEC
activation-induced cytidine deaminase/apolipoprotein B mRNA-editing enzyme complex
- ARS
acute restraint stress
- AEA
anandamide
- BLA
basolateral amygdala
- CA
Ammon’s horn/Cornus Ammonics subfield
- CB
cannabinoid receptor
- CeA
central amygdala
- CNS
central nervous system
- CRS
chronic restraint stress
- CSD
chronic social defeat
- CUMS
chronic unpredictable mild stress
- D2
dopamine receptor D2
- DG
dentate gyrus
- DAGL
diacylglycerol lipase
- DNMT
DNA methyltransferase
- eCB
endocannabinoid
- FAAH
fatty acid amide hydrolase
- GABA
gamma-aminobutyric acid
- GC
glucocorticoid
- GPR55
G protein-coupled receptor 55
- GR
glucocorticoid receptor
- HAT
histone acetyltransferase
- HDAC
histone deacetylase
- HPA
hypothalamus-pituitary-adrenal
- IL
infralimbic
- MAGL
monoacylglycerol lipase
- MBP
methyl-CpG binding protein
- MDD
major depressive disease
- MeCP2
methyl CpG binding protein 2
- MeA
medial amygdala
- miRNA
micro RNA
- mPFC
medial prefrontal cortex
- MS
maternal separation
- NAc
nucleus accumbens
- NAPE-PLD
N-acyl phosphatidylethanolamine phospholipase D
- NpY
neuropeptide Y
- NR3C1
glucocorticoid receptor gene
- PBMC
peripheral blood mononuclear cell
- PD7
postnatal day 7
- PFC
prefrontal cortex
- PKA
protein kinase A
- PL
prelimbic
- PPARγ
peroxisome proliferator-activated receptor gamma
- PTSD
post-traumatic stress disorder
- SA
self-administration
- SLC6A4
solute carrier family 6 member 4
- TET
ten-eleven translocation enzyme
- TRPV1
vanilloid receptor 1
- 2-AG
2-arachidonoylglycerol
- 5mC
cytosine methylated at the 5′ position
Data Availability
Data sharing is not applicable.
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
A.A.C. and S.L.B. are receivers of FAPESP Master’s fellowship [grant numbers 2021/01656-3 and 2021/05406-1]; P.H.G. was supported by an Independent Research Fund Denmark fellowship (DFF-Forskningsprojekt 1 – Project Number 8020-00310B) provided by an Academic Cooperation Agreement between FCFRP/USP and Aarhus University; S.F.L. is supported by a FAPESP Young Research Grant [grant number 2017/19731-6].
Open Access
Open access for the present article was enabled after accepting the invitation to contribute with an article in the Neuronal Signaling journal, agreement with Portland Press and the Biochemical Society.
CRediT Author Contribution
Arthur A. Coelho: Conceptualization, Writing—original draft. Savio L. Bastos: Conceptualization, Writing—original draft. Pedro H. Gobira: Writing—original draft. Sabrina F. Lisboa: Conceptualization, Resources, Supervision, Funding acquisition, Writing—original draft, Writing—review & editing.
References
- 1.Godoy L.D., Rossignoli M.T., Delfino-Pereira P., Garcia-Cairasco N. and de Lima Umeoka E.H. (2018) A comprehensive overview on stress neurobiology: basic concepts and clinical implications. Front Behav. Neurosci. 121–23 10.3389/fnbeh.2018.00127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yamamoto K.R. (1985) Steroid receptor regulated transcription of specific genes and gene networks. Annu. Rev. Genet. 19, 209–252 10.1146/annurev.ge.19.120185.001233 [DOI] [PubMed] [Google Scholar]
- 3.Wang J.-C., Derynck M.K., Nonaka D.F., Khodabakhsh D.B., Haqq C. and Yamamoto K.R. (2004) Chromatin immunoprecipitation (ChIP) scanning identifies primary glucocorticoid receptor target genes. Proc. Natl. Acad. Sci. 101, 15603–15608 10.1073/pnas.0407008101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy M.D. and Heller E.A. (2022) Convergent actions of stress and stimulants via epigenetic regulation of neural circuitry. Trends Neurosci. 45, 955–967 10.1016/j.tins.2022.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang W.-H., Zhang J.-Y., Holmes A. and Pan B.-X. (2021) Amygdala circuit substrates for stress adaptation and adversity. Biol. Psychiatry 89, 847–856 10.1016/j.biopsych.2020.12.026 [DOI] [PubMed] [Google Scholar]
- 6.Alexandra Kredlow M., Fenster R.J., Laurent E.S., Ressler K.J. and Phelps E.A. (2022) Prefrontal cortex, amygdala, and threat processing: implications for PTSD. Neuropsychopharmacology 47, 247–259 10.1038/s41386-021-01155-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sousa N. (2016) The dynamics of the stress neuromatrix. Mol. Psychiatry 21, 302–312 10.1038/mp.2015.196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Le Merre P., Ährlund-Richter S. and Carlén M. (2021) The mouse prefrontal cortex: Unity in diversity. Neuron 109, 1925–1944 10.1016/j.neuron.2021.03.035 [DOI] [PubMed] [Google Scholar]
- 9.Friedman N.P. and Robbins T.W. (2022) The role of prefrontal cortex in cognitive control and executive function. Neuropsychopharmacology 47, 72–89 10.1038/s41386-021-01132-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McKlveen J.M., Myers B. and Herman J.P. (2015) The medial prefrontal cortex: coordinator of autonomic, neuroendocrine and behavioural responses to stress. J. Neuroendocrinol. 27, 446–456 10.1111/jne.12272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manoocheri K. and Carter A.G. (2022) Rostral and caudal basolateral amygdala engage distinct circuits in the prelimbic and infralimbic prefrontal cortex. eLife 11, e82688 10.7554/eLife.82688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Aerde K.I., Heistek T.S. and Mansvelder H.D. (2008) Prelimbic and infralimbic prefrontal cortex interact during fast network oscillations. PloS ONE 3, e2725 10.1371/journal.pone.0002725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gabbott P.L.A., Warner T.A., Jays P.R.L., Salway P. and Busby S.J. (2005) Prefrontal cortex in the rat: projections to subcortical autonomic, motor, and limbic centers. J. Comp. Neurol. 492, 145–177 10.1002/cne.20738 [DOI] [PubMed] [Google Scholar]
- 14.Vertes R.P. (2004) Differential projections of the infralimbic and prelimbic cortex in the rat. Synapse 51, 32–58 10.1002/syn.10279 [DOI] [PubMed] [Google Scholar]
- 15.Popoli M., Yan Z., McEwen B.S. and Sanacora G. (2012) The stressed synapse: the impact of stress and glucocorticoids on glutamate transmission. Nat. Rev. Neurosci. 13, 22–37 10.1038/nrn3138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gądek-Michalska A., Tadeusz J., Rachwalska P. and Bugajski J. (2013) Cytokines, prostaglandins and nitric oxide in the regulation of stress-response systems. Pharmacological Rep. 65, 1655–1662 10.1016/S1734-1140(13)71527-5 [DOI] [PubMed] [Google Scholar]
- 17.Pandey G.N., Rizavi H.S., Ren X., Fareed J., Hoppensteadt D.A., Roberts R.C.et al. (2012) Proinflammatory cytokines in the prefrontal cortex of teenage suicide victims. J. Psychiatr. Res. 46, 57–63 10.1016/j.jpsychires.2011.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Banasr M., Dwyer J.M. and Duman R.S. (2011) Cell atrophy and loss in depression: reversal by antidepressant treatment. Curr. Opin. Cell Biol. 23, 730–737 10.1016/j.ceb.2011.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rauch S.L., Shin L.M., Segal E., Pitman R.K., Carson M.A., McMullin K.et al. (2003) Selectively reduced regional cortical volumes in post-traumatic stress disorder. Neuroreport 14, 913–916 10.1097/01.wnr.0000071767.24455.10 [DOI] [PubMed] [Google Scholar]
- 20.Arnsten A.F.T. (2015) Stress weakens prefrontal networks: molecular insults to higher cognition. Nat. Neurosci. 18, 1376–1385 10.1038/nn.4087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Woo E., Sansing L.H., Arnsten A.F.T. and Datta D. (2021) Chronic stress weakens connectivity in the prefrontal cortex: architectural and molecular changes. Chronic Stress 5, 24705470211029254 10.1177/24705470211029254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sun Y., Gooch H. and Sah P. (2020) Fear conditioning and the basolateral amygdala. F1000Research 9, 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duvarci S., Popa D. and Pare D. (2011) Central amygdala activity during fear conditioning. J. Neurosci. 31, 289–294 10.1523/JNEUROSCI.4985-10.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hu F., Liang W., Zhang L., Wang H., Li Z. and Zhou Y. (2022) Hyperactivity of basolateral amygdala mediates behavioral deficits in mice following exposure to bisphenol A and its analogue alternative. Chemosphere 287, 132044 10.1016/j.chemosphere.2021.132044 [DOI] [PubMed] [Google Scholar]
- 25.Inagaki R., Moriguchi S. and Fukunaga K. (2018) Aberrant amygdala-dependent fear memory in corticosterone-treated mice. Neuroscience 388, 448–459 10.1016/j.neuroscience.2018.08.004 [DOI] [PubMed] [Google Scholar]
- 26.Siegle G.J., Steinhauer S.R., Thase M.E., Stenger V.A. and Carter C.S. (2002) Can't shake that feeling: event-related fMRI assessment of sustained amygdala activity in response to emotional information in depressed individuals. Biol. Psychiatry 51, 693–707 10.1016/S0006-3223(02)01314-8 [DOI] [PubMed] [Google Scholar]
- 27.Lupien S.J., Parent S., Evans A.C., Tremblay R.E., Zelazo P.D., Corbo V.et al. (2011) Larger amygdala but no change in hippocampal volume in 10-year-old children exposed to maternal depressive symptomatology since birth. Proc. Natl. Acad. Sci. 108, 14324–14329 10.1073/pnas.1105371108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Frodl T., Meisenzahl E., Zetzsche T., Bottlender R., Born C., Groll C.et al. (2002) Enlargement of the amygdala in patients with a first episode of major depression. Biol. Psychiatry 51, 708–714 10.1016/S0006-3223(01)01359-2 [DOI] [PubMed] [Google Scholar]
- 29.Dejean C., Courtin J., Rozeske R.R., Bonnet M.C., Dousset V., Michelet T.et al. (2015) Neuronal circuits for fear expression and recovery: recent advances and potential therapeutic strategies. Biol. Psychiatr. 78, 298–306 10.1016/j.biopsych.2015.03.017 [DOI] [PubMed] [Google Scholar]
- 30.Thierry A.-M., Gioanni Y., Dégénétais E. and Glowinski J. (2000) Hippocampo-prefrontal cortex pathway: Anatomical and electrophysiological characteristics. Hippocampus 10, 411–419 [DOI] [PubMed] [Google Scholar]
- 31.Ishikawa A. and Nakamura S. (2003) Convergence and interaction of hippocampal and amygdalar projections within the prefrontal cortex in the rat. J. Neurosci. 23, 9987–9995 10.1523/JNEUROSCI.23-31-09987.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim W.B. and Cho J.-H. (2017) Synaptic targeting of double-projecting ventral CA1 hippocampal neurons to the medial prefrontal cortex and basal amygdala. J. Neurosci. 37, 4868–4882 10.1523/JNEUROSCI.3579-16.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Çalışkan G. and Stork O. (2019) Hippocampal network oscillations at the interplay between innate anxiety and learned fear. Psychopharmacology (Berl.) 236, 321–338 10.1007/s00213-018-5109-z [DOI] [PubMed] [Google Scholar]
- 34.Asok A., Kandel E.R. and Rayman J.B. (2019) The neurobiology of fear generalization. Front Behav Neurosci. 12, 1–15 10.3389/fnbeh.2018.00329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim E.J., Pellman B. and Kim J.J. (2015) Stress effects on the hippocampus: a critical review. Learn. Memory 22, 411–416 10.1101/lm.037291.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Webler R.D., Berg H., Fhong K., Tuominen L., Holt D.J., Morey R.A.et al. (2021) The neurobiology of human fear generalization: meta-analysis and working neural model. Neurosci. Biobehavioral Rev. 128, 421–436 10.1016/j.neubiorev.2021.06.035 [DOI] [PubMed] [Google Scholar]
- 37.Murray F., Smith D.W. and Hutson P.H. (2008) Chronic low dose corticosterone exposure decreased hippocampal cell proliferation, volume and induced anxiety and depression like behaviours in mice. Eur. J. Pharmacol. 583, 115–127 10.1016/j.ejphar.2008.01.014 [DOI] [PubMed] [Google Scholar]
- 38.Gurvits T.V., Shenton M.E., Hokama H., Ohta H., Lasko N.B., Gilbertson M.W.et al. (1996) Magnetic resonance imaging study of hippocampal volume in chronic, combat-related posttraumatic stress disorder. Biol. Psychiatry 40, 1091–1099 10.1016/S0006-3223(96)00229-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nolan M., Roman E., Nasa A., Levins K.J., O'Hanlon E., O'Keane V.et al. (2020) Hippocampal and amygdalar volume changes in major depressive disorder: a targeted review and focus on stress. Chronic Stress 4, 2470547020944553 10.1177/2470547020944553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Karl A., Schaefer M., Malta L.S., Dörfel D., Rohleder N. and Werner A. (2006) A meta-analysis of structural brain abnormalities in PTSD. Neurosci. Biobehav. Rev. 30, 1004–1031 10.1016/j.neubiorev.2006.03.004 [DOI] [PubMed] [Google Scholar]
- 41.Bremner J.D., Randall P., Scott T.M., Bronen R.A., Seibyl J.P., Southwick S.M.et al. (1995) MRI-based measurement of hippocampal volume in patients with combat-related posttraumatic stress disorder. Am. J. Psychiatry 152, 973–981 10.1176/ajp.152.7.973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gilbertson M.W., Shenton M.E., Ciszewski A., Kasai K., Lasko N.B., Orr S.P.et al. (2002) Smaller hippocampal volume predicts pathologic vulnerability to psychological trauma. Nat. Neurosci. 5, 1242–1247 10.1038/nn958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cristino L., Bisogno T. and Di Marzo V. (2020) Cannabinoids and the expanded endocannabinoid system in neurological disorders. Nat. Rev. Neurol. 16, 9–29 10.1038/s41582-019-0284-z [DOI] [PubMed] [Google Scholar]
- 44.Witkin J.M., Tzavara E.T. and Nomikos G.G. (2005) A role for cannabinoid CB1 receptors in mood and anxiety disorders. Behav. Pharmacol. 16, 333–352 10.1097/00008877-200509000-00005 [DOI] [PubMed] [Google Scholar]
- 45.Marsicano G., Wotjak C.T., Azad S.C., Bisogno T., Rammes G., Cascio M.G.et al. (2002) The endogenous cannabinoid system controls extinction of aversive memories. Nature 418, 530–534 10.1038/nature00839 [DOI] [PubMed] [Google Scholar]
- 46.Lisboa S.F., Gomes F.V., Silva A.L., Uliana D.L., Camargo L.H.A., Guimarães F.S.et al. (2015) Increased contextual fear conditioning in iNOS knockout mice: additional evidence for the involvement of nitric oxide in stress-related disorders and contribution of the endocannabinoid system. Int. J. Neuropsychopharmacolog. 18, pyv005 10.1093/ijnp/pyv005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Terzian A.L.B., Dos Reis D.G., Guimarães F.S., Corrêa F.M.A. and Resstel L.B.M. (2014) Medial prefrontal cortex transient receptor potential vanilloid type 1 (TRPV1) in the expression of contextual fear conditioning in Wistar rats. Psychopharmacology (Berl.) 231, 149–157 10.1007/s00213-013-3211-9 [DOI] [PubMed] [Google Scholar]
- 48.Gobira P.H., Lima I.V., Batista L.A., de Oliveira A.C., Resstel L.B., Wotjak C.T.et al. (2017) N-arachidonoyl-serotonin, a dual FAAH and TRPV1 blocker, inhibits the retrieval of contextual fear memory: Role of the cannabinoid CB1 receptor in the dorsal hippocampus. J. Psychopharmacol. 31, 750–756 10.1177/0269881117691567 [DOI] [PubMed] [Google Scholar]
- 49.Marzo V.D., Bifulco M. and Petrocellis L.D. (2004) The endocannabinoid system and its therapeutic exploitation. Nat. Rev. Drug Discovery 3, 771–784 10.1038/nrd1495 [DOI] [PubMed] [Google Scholar]
- 50.Bassir Nia A., Bender R. and Harpaz-Rotem I. (2019) Endocannabinoid system alterations in posttraumatic stress disorder: a review of developmental and accumulative effects of trauma. Chronic Stress 3, 2470547019864096 10.1177/2470547019864096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Patel S., Hill M.N., Cheer J.F., Wotjak C.T. and Holmes A. (2017) The endocannabinoid system as a target for novel anxiolytic drugs. Neurosci. Biobehavioral Rev. 76, 56–66 10.1016/j.neubiorev.2016.12.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hill M.N., Miller G.E., Carrier E.J., Gorzalka B.B. and Hillard C.J. (2009) Circulating endocannabinoids and N-acyl ethanolamines are differentially regulated in major depression and following exposure to social stress. Psychoneuroendocrinology 34, 1257–1262 10.1016/j.psyneuen.2009.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hungund B.L., Vinod K.Y., Kassir S.A., Basavarajappa B.S., Yalamanchili R., Cooper T.B.et al. (2004) Upregulation of CB1 receptors and agonist-stimulated [35S]GTPγS binding in the prefrontal cortex of depressed suicide victims. Mol. Psychiatry 9, 184–190 10.1038/sj.mp.4001376 [DOI] [PubMed] [Google Scholar]
- 54.Gonda X., Petschner P., Eszlari N., Sutori S., Gal Z., Koncz S.et al. (2019) Effects of different stressors are modulated by different neurobiological systems: the role of GABA-A versus CB1 receptor gene variants in anxiety and depression. Front Cell Neurosci. 13, 1–12 10.3389/fncel.2019.00138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mitjans M., Serretti A., Fabbri C., Gastó C., Catalán R., Fañanás L.et al. (2013) Screening genetic variability at the CNR1 gene in both major depression etiology and clinical response to citalopram treatment. Psychopharmacology (Berl.) 227, 509–519 10.1007/s00213-013-2995-y [DOI] [PubMed] [Google Scholar]
- 56.Domschke K., Dannlowski U., Ohrmann P., Lawford B., Bauer J., Kugel H.et al. (2008) Cannabinoid receptor 1 (CNR1) gene: Impact on antidepressant treatment response and emotion processing in Major Depression. Eur. Neuropsychopharmacol. 18, 751–759 10.1016/j.euroneuro.2008.05.003 [DOI] [PubMed] [Google Scholar]
- 57.Christensen R., Kristensen P.K., Bartels E.M., Bliddal H. and Astrup A. (2007) Efficacy and safety of the weight-loss drug rimonabant: a meta-analysis of randomised trials. Lancet North Am. Ed. 370, 1706–1713 10.1016/S0140-6736(07)61721-8 [DOI] [PubMed] [Google Scholar]
- 58.Hill M.N., Ho W.-S.V., Hillard C.J. and Gorzalka B.B. (2008) Differential effects of the antidepressants tranylcypromine and fluoxetine on limbic cannabinoid receptor binding and endocannabinoid contents. J. Neural Transm. 115, 1673–1679 10.1007/s00702-008-0131-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Neumeister A., Normandin M.D., Pietrzak R.H., Piomelli D., Zheng M.Q., Gujarro-Anton A.et al. (2013) Elevated brain cannabinoid CB1 receptor availability in post-traumatic stress disorder: a positron emission tomography study. Mol. Psychiatry 18, 1034–1040 10.1038/mp.2013.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mayo L.M., Asratian A., Lindé J., Holm L., Nätt D., Augier G.et al. (2020) Protective effects of elevated anandamide on stress and fear-related behaviors: translational evidence from humans and mice. Mol. Psychiatry 25, 993–1005 10.1038/s41380-018-0215-1 [DOI] [PubMed] [Google Scholar]
- 61.Zabik N.L., Iadipaolo A.S., Marusak H.A., Peters C., Burghardt K. and Rabinak C.A. (2022) A common genetic variant in fatty acid amide hydrolase is linked to alterations in fear extinction neural circuitry in a racially diverse, nonclinical sample of adults. J. Neurosci. Res. 100, 744–761 10.1002/jnr.24860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lazary J., Eszlari N., Juhasz G. and Bagdy G. (2016) Genetically reduced FAAH activity may be a risk for the development of anxiety and depression in persons with repetitive childhood trauma. Eur. Neuropsychopharmacol. 26, 1020–1028 10.1016/j.euroneuro.2016.03.003 [DOI] [PubMed] [Google Scholar]
- 63.Lazary J., Eszlari N., Juhasz G. and Bagdy G. (2019) A functional variant of CB2 receptor gene interacts with childhood trauma and FAAH gene on anxious and depressive phenotypes. J. Affect. Disord. 257, 716–722 10.1016/j.jad.2019.07.083 [DOI] [PubMed] [Google Scholar]
- 64.Ney L.J., Crombie K.M., Mayo L.M., Felmingham K.L., Bowser T. and Matthews A. (2022) Translation of animal endocannabinoid models of PTSD mechanisms to humans: Where to next? Neurosci. Biobehavioral Rev. 132, 76–91 10.1016/j.neubiorev.2021.11.040 [DOI] [PubMed] [Google Scholar]
- 65.Lisboa S.F., Vila-Verde C., Rosa J., Uliana D.L., Stern C.A.J., Bertoglio L.J.et al. (2019) Tempering aversive/traumatic memories with cannabinoids: a review of evidence from animal and human studies. Psychopharmacology (Berl.) 236, 201–226 10.1007/s00213-018-5127-x [DOI] [PubMed] [Google Scholar]
- 66.Ney L.J., Matthews A., Hsu C.-M.K., Zuj D.V., Nicholson E., Steward T.et al. (2021) Cannabinoid polymorphisms interact with plasma endocannabinoid levels to predict fear extinction learning. Depress. Anxiety 38, 1087–1099 10.1002/da.23170 [DOI] [PubMed] [Google Scholar]
- 67.Navarrete F., García-Gutiérrez M.S., Jurado-Barba R., Rubio G., Gasparyan A., Austrich-Olivares A.et al. (2020) Endocannabinoid system components as potential biomarkers in psychiatry. Front Psychiatry 11, 1–30 10.3389/fpsyt.2020.00315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mayo L.M., Rabinak C.A., Hill M.N. and Heilig M. (2022) Targeting the endocannabinoid system in the treatment of posttraumatic stress disorder: a promising case of preclinical-clinical translation? Biol. Psychiatry 91, 262–272 10.1016/j.biopsych.2021.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Haller J., Bakos N., Szirmay M., Ledent C. and Freund T.F. (2002) The effects of genetic and pharmacological blockade of the CB1 cannabinoid receptor on anxiety. Eur. J. Neurosci. 16, 1395–1398 10.1046/j.1460-9568.2002.02192.x [DOI] [PubMed] [Google Scholar]
- 70.Aso E., Ozaita A., Serra M.-À. and Maldonado R. (2011) Genes differentially expressed in CB1 knockout mice: Involvement in the depressive-like phenotype. Eur. Neuropsychopharmacol. 21, 11–22 10.1016/j.euroneuro.2010.06.007 [DOI] [PubMed] [Google Scholar]
- 71.Valverde O. and Torrens M. (2012) CB1 receptor-deficient mice as a model for depression. Neuroscience 204, 193–206 10.1016/j.neuroscience.2011.09.031 [DOI] [PubMed] [Google Scholar]
- 72.Martin M., Ledent C., Parmentier M., Maldonado R. and Valverde O. (2002) Involvement of CB1 cannabinoid receptors in emotional behaviour. Psychopharmacology (Berl.) 159, 379–387 10.1007/s00213-001-0946-5 [DOI] [PubMed] [Google Scholar]
- 73.Mikics É., Dombi T., Barsvári B., Varga B., Ledent C., Freund T.F.et al. (2006) The effects of cannabinoids on contextual conditioned fear in CB1 knockout and CD1 mice. Behav. Pharmacol. 17, 10.1097/00008877-200605000-00003 [DOI] [PubMed] [Google Scholar]
- 74.Beyer C.E., Dwyer J.M., Piesla M.J., Platt B.J., Shen R., Rahman Z.et al. (2010) Depression-like phenotype following chronic CB1 receptor antagonism. Neurobiol. Dis. 39, 148–155 10.1016/j.nbd.2010.03.020 [DOI] [PubMed] [Google Scholar]
- 75.O'Brien L.D., Wills K.L., Segsworth B., Dashney B., Rock E.M., Limebeer C.L.et al. (2013) Effect of chronic exposure to rimonabant and phytocannabinoids on anxiety-like behavior and saccharin palatability. Pharmacol. Biochem. Behav. 103, 597–602 10.1016/j.pbb.2012.10.008 [DOI] [PubMed] [Google Scholar]
- 76.Rutkowska M. and Jachimczuk O. (2004) Antidepressant–like properties of ACEA (arachidonyl-2-chloroethylamide), the selective agonist of CB1 receptors. Acta Pol. Pharm. 61, 165–167 [PubMed] [Google Scholar]
- 77.Hill M.N. and Gorzalka B.B. (2005) Pharmacological enhancement of cannabinoid CB1 receptor activity elicits an antidepressant-like response in the rat forced swim test. Eur. Neuropsychopharmacol. 15, 593–599 10.1016/j.euroneuro.2005.03.003 [DOI] [PubMed] [Google Scholar]
- 78.Haller J., Varga B., Ledent C. and Freund T.F. (2004) CB1 cannabinoid receptors mediate anxiolytic effects: convergent genetic and pharmacological evidence with CB1-specific agents. Behav. Pharmacol. 15, 299–304 10.1097/01.fbp.0000135704.56422.40 [DOI] [PubMed] [Google Scholar]
- 79.Ganon-Elazar E. and Akirav I. (2013) Cannabinoids and traumatic stress modulation of contextual fear extinction and GR expression in the amygdala-hippocampal-prefrontal circuit. Psychoneuroendocrinology 38, 1675–1687 10.1016/j.psyneuen.2013.01.014 [DOI] [PubMed] [Google Scholar]
- 80.Laricchiuta D., Centonze D. and Petrosini L. (2013) Effects of endocannabinoid and endovanilloid systems on aversive memory extinction. Behav. Brain Res. 256, 101–107 10.1016/j.bbr.2013.08.010 [DOI] [PubMed] [Google Scholar]
- 81.García-Gutiérrez M.S. and Manzanares J. (2010) Overexpression of CB2 cannabinoid receptors decreased vulnerability to anxiety and impaired anxiolytic action of alprazolam in mice. J. Psychopharmacol. 25, 111–120 10.1177/0269881110379507 [DOI] [PubMed] [Google Scholar]
- 82.García-Gutiérrez M.S., García-Bueno B., Zoppi S., Leza J.C. and Manzanares J. (2012) Chronic blockade of cannabinoid CB2 receptors induces anxiolytic-like actions associated with alterations in GABA(A) receptors. Br. J. Pharmacol. 165, 951–964 10.1111/j.1476-5381.2011.01625.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.García-Gutiérrez M.S., Pérez-Ortiz J.M., Gutiérrez-Adán A. and Manzanares J. (2010) Depression-resistant endophenotype in mice overexpressing cannabinoid CB(2) receptors. Br. J. Pharmacol. 160, 1773–1784 10.1111/j.1476-5381.2010.00819.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Li Y. and Kim J. (2016) CB2 cannabinoid receptor knockout in mice impairs contextual long-term memory and enhances spatial working memory. Neural Plast. 2016, 9817089 10.1155/2016/9817089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gerdeman G. and Lovinger D.M. (2001) CB1 cannabinoid receptor inhibits synaptic release of glutamate in rat dorsolateral striatum. J. Neurophysiol. 85, 468–471 10.1152/jn.2001.85.1.468 [DOI] [PubMed] [Google Scholar]
- 86.Polissidis A., Galanopoulos A., Naxakis G., Papahatjis D., Papadopoulou-Daifoti Z. and Antoniou K. (2013) The cannabinoid CB1 receptor biphasically modulates motor activity and regulates dopamine and glutamate release region dependently. Int. J. Neuropsychopharmacolog. 16, 393–403 10.1017/S1461145712000156 [DOI] [PubMed] [Google Scholar]
- 87.Ferreira S.G., Teixeira F.M., Garção P., Agostinho P., Ledent C., Cortes L.et al. (2012) Presynaptic CB1 cannabinoid receptors control frontocortical serotonin and glutamate release – Species differences. Neurochem. Int. 61, 219–226 10.1016/j.neuint.2012.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Blázquez C., Chiarlone A., Bellocchio L., Resel E., Pruunsild P., García-Rincón D.et al. (2015) The CB1 cannabinoid receptor signals striatal neuroprotection via a PI3K/Akt/mTORC1/BDNF pathway. Cell Death Differentiation 22, 1618–1629 10.1038/cdd.2015.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Aso E., Ozaita A., Valdizán E.M., Ledent C., Pazos Á., Maldonado R.et al. (2008) BDNF impairment in the hippocampus is related to enhanced despair behavior in CB1 knockout mice. J. Neurochem. 105, 565–572 10.1111/j.1471-4159.2007.05149.x [DOI] [PubMed] [Google Scholar]
- 90.Zoppi S., Madrigal J.L., Caso J.R., García-Gutiérrez M.S., Manzanares J., Leza J.C.et al. (2014) Regulatory role of the cannabinoid CB2receptor in stress-induced neuroinflammation in mice. Br. J. Pharmacol. 171, 2814–2826 10.1111/bph.12607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lisboa S.F., Gomes F.V., Guimaraes F.S. and Campos A.C. (2016) Microglial cells as a link between cannabinoids and the immune hypothesis of psychiatric disorders. Front Neurol. 7, 10.3389/fneur.2016.00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lisboa S.F., Niraula A., Resstel L.B., Guimaraes F.S., Godbout J.P. and Sheridan J.F. (2018) Repeated social defeat-induced neuroinflammation, anxiety-like behavior and resistance to fear extinction were attenuated by the cannabinoid receptor agonist WIN55,212-2. Neuropsychopharmacology 43, 1924–1933 10.1038/s41386-018-0064-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Coelho A.A., Vila-Verde C., Sartim A.G., Uliana D.L., Braga L.A., Guimarães F.S.et al. (2022) Inducible nitric oxide synthase inhibition in the medial prefrontal cortex attenuates the anxiogenic-like effect of acute restraint stress via CB1 receptors. Front Psychiatry 13, 1–11 10.3389/fpsyt.2022.923177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hill M.N., McLaughlin R.J., Pan B., Fitzgerald M.L., Roberts C.J., Lee T.T.Y.et al. (2011) Recruitment of prefrontal cortical endocannabinoid signaling by glucocorticoids contributes to termination of the stress response. J. Neurosci. 31, 10506–10515 10.1523/JNEUROSCI.0496-11.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lyko F. (2018) The DNA methyltransferase family: a versatile toolkit for epigenetic regulation. Nat. Rev. Genet. 19, 81–92 10.1038/nrg.2017.80 [DOI] [PubMed] [Google Scholar]
- 96.Chin E.W.M. and Goh E.L.K. (2019) MeCP2 dysfunction in rett syndrome and neuropsychiatric disorders. Methods Mol. Biol. 2011, 573–591 10.1007/978-1-4939-9554-7_33 [DOI] [PubMed] [Google Scholar]
- 97.Du Q., Luu P.L., Stirzaker C. and Clark S.J. (2015) Methyl-CpG-binding domain proteins: readers of the epigenome. Epigenomics 7, 1051–1073 10.2217/epi.15.39 [DOI] [PubMed] [Google Scholar]
- 98.Ehrlich M. (2019) DNA hypermethylation in disease: mechanisms and clinical relevance. Epigenetics 14, 1141–1163 10.1080/15592294.2019.1638701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Vinkers C.H., Kalafateli A.L., Rutten B.P., Kas M.J., Kaminsky Z., Turner J.D.et al. (2015) Traumatic stress and human DNA methylation: a critical review. Epigenomics 7, 593–608 10.2217/epi.15.11 [DOI] [PubMed] [Google Scholar]
- 100.Klengel T., Pape J., Binder E.B. and Mehta D. (2014) The role of DNA methylation in stress-related psychiatric disorders. Neuropharmacology 80, 115–132 10.1016/j.neuropharm.2014.01.013 [DOI] [PubMed] [Google Scholar]
- 101.Zhang Y. and Liu C. (2022) Evaluating the challenges and reproducibility of studies investigating DNA methylation signatures of psychological stress. Epigenomics 14, 405–421 10.2217/epi-2021-0190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bakusic J., Schaufeli W., Claes S. and Godderis L. (2017) Stress, burnout and depression: A systematic review on DNA methylation mechanisms. J. Psychosom. Res. 92, 34–44 10.1016/j.jpsychores.2016.11.005 [DOI] [PubMed] [Google Scholar]
- 103.Argentieri M.A., Nagarajan S., Seddighzadeh B., Baccarelli A.A. and Shields A.E. (2017) Epigenetic pathways in human disease: the impact of DNA methylation on stress-related pathogenesis and current challenges in biomarker development. EBioMedicine 18, 327–350 10.1016/j.ebiom.2017.03.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Steiger H., Labonté B., Groleau P., Turecki G. and Israel M. (2013) Methylation of the glucocorticoid receptor gene promoter in bulimic women: Associations with borderline personality disorder, suicidality, and exposure to childhood abuse. Int. J. Eat. Disord. 46, 246–255 10.1002/eat.22113 [DOI] [PubMed] [Google Scholar]
- 105.Labonté B., Suderman M., Maussion G., Navaro L., Yerko V., Mahar I.et al. (2012) Genome-wide epigenetic regulation by early-life trauma. Arch. Gen. Psychiatry 69, 722–731 10.1001/archgenpsychiatry.2011.2287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Perroud N., Paoloni-Giacobino A., Prada P., Olié E., Salzmann A., Nicastro R.et al. (2011) Increased methylation of glucocorticoid receptor gene (NR3C1) in adults with a history of childhood maltreatment: a link with the severity and type of trauma. Transl. Psychiatry 1, e59 10.1038/tp.2011.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Radtke K.M., Ruf M., Gunter H.M., Dohrmann K., Schauer M., Meyer A.et al. (2011) Transgenerational impact of intimate partner violence on methylation in the promoter of the glucocorticoid receptor. Transl. Psychiatry 1, e21 10.1038/tp.2011.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tyrka A.R., Price L.H., Marsit C., Walters O.C. and Carpenter L.L. (2012) Childhood adversity and epigenetic modulation of the leukocyte glucocorticoid receptor: preliminary findings in healthy adults. PloS ONE 7, e30148 10.1371/journal.pone.0030148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Labonté B., Azoulay N., Yerko V., Turecki G. and Brunet A. (2014) Epigenetic modulation of glucocorticoid receptors in posttraumatic stress disorder. Transl. Psychiatry 4, e368 10.1038/tp.2014.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Vukojevic V., Kolassa I.T., Fastenrath M., Gschwind L., Spalek K., Milnik A.et al. (2014) Epigenetic modification of the glucocorticoid receptor gene is linked to traumatic memory and post-traumatic stress disorder risk in genocide survivors. J. Neurosci. 34, 10274–10284 10.1523/JNEUROSCI.1526-14.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Na K.-S., Chang H.S., Won E., Han K.-M., Choi S., Tae W.S.et al. (2014) Association between glucocorticoid receptor methylation and hippocampal subfields in major depressive disorder. PLoS ONE 9, e85425 10.1371/journal.pone.0085425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yehuda R., Flory J.D., Bierer L.M., Henn-Haase C., Lehrner A., Desarnaud F.et al. (2015) Lower methylation of glucocorticoid receptor gene promoter 1F in Peripheral blood of veterans with posttraumatic stress disorder. Biol. Psychiatry 77, 356–364 10.1016/j.biopsych.2014.02.006 [DOI] [PubMed] [Google Scholar]
- 113.McGowan P.O., Sasaki A., D'Alessio A.C., Dymov S., Labonté B., Szyf M.et al. (2009) Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat. Neurosci. 12, 342–348 10.1038/nn.2270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Suderman M., McGowan P.O., Sasaki A., Huang T.C.T., Hallett M.T., Meaney M.J.et al. (2012) Conserved epigenetic sensitivity to early life experience in the rat and human hippocampus. Proc. Natl. Acad. Sci. 109, 17266–17272 10.1073/pnas.1121260109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Beach S.R.H., Brody G.H., Todorov A.A., Gunter T.D. and Philibert R.A. (2010) Methylation at SLC6A4 is linked to family history of child abuse: An examination of the Iowa Adoptee sample. Am. J. Med. Genet. B Neuropsychiatr. Genet. 153B, 710–713 10.1002/ajmg.b.31028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Koenen K.C., Uddin M., Chang S.-C., Aiello A.E., Wildman D.E., Goldmann E.et al. (2011) SLC6A4 methylation modifies the effect of the number of traumatic events on risk for posttraumatic stress disorder. Depress. Anxiety 28, 639–647 10.1002/da.20825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Alasaari J.S., Lagus M., Ollila H.M., Toivola A., Kivimäki M., Vahtera J.et al. (2012) Environmental stress affects DNA methylation of a CpG rich promoter region of serotonin transporter gene in a nurse cohort. PLoS ONE 7, e45813 10.1371/journal.pone.0045813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kang H.-J., Kim J.-M., Stewart R., Kim S.-Y., Bae K.-Y., Kim S.-W.et al. (2013) Association of SLC6A4 methylation with early adversity, characteristics and outcomes in depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 44, 23–28 10.1016/j.pnpbp.2013.01.006 [DOI] [PubMed] [Google Scholar]
- 119.Zhao J., Goldberg J., Bremner J.D. and Vaccarino V. (2013) Association between promoter methylation of serotonin transporter gene and depressive symptoms: A monozygotic twin study. Psychosom. Med. 75, 523–529 10.1097/PSY.0b013e3182924cf4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang D., Szyf M., Benkelfat C., Provençal N., Turecki G., Caramaschi D.et al. (2012) Peripheral SLC6A4 DNA methylation is associated with in vivo measures of human brain serotonin synthesis and childhood physical aggression. PloS ONE 7, e39501 10.1371/journal.pone.0039501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kim J.M., Stewart R., Kang H.J., Kim S.W., Shin I.S., Kim H.R.et al. (2013) A longitudinal study of SLC6A4 DNA promoter methylation and poststroke depression. J. Psychiatr. Res. 47, 1222–1227 10.1016/j.jpsychires.2013.04.010 [DOI] [PubMed] [Google Scholar]
- 122.Okada S., Morinobu S., Fuchikami M., Segawa M., Yokomaku K., Kataoka T.et al. (2014) The potential of SLC6A4 gene methylation analysis for the diagnosis and treatment of major depression. J. Psychiatr. Res. 53, 47–53 10.1016/j.jpsychires.2014.02.002 [DOI] [PubMed] [Google Scholar]
- 123.Zhang Y., Sun Z., Jia J., Du T., Zhang N., Tang Y.et al. (2021) Overview of histone modification. In Histone Mutations and Cancer(Fang D. and Han J., eds), pp. 1–16, Springer Singapore, Singapore: 10.1007/978-981-15-8104-5_1 [DOI] [Google Scholar]
- 124.Lawrence M., Daujat S. and Schneider R. (2016) Lateral thinking: how histone modifications regulate gene expression. Trends Genet. 32, 42–56 10.1016/j.tig.2015.10.007 [DOI] [PubMed] [Google Scholar]
- 125.Fiori L.M., Gross J.A. and Turecki G. (2012) Effects of histone modifications on increased expression of polyamine biosynthetic genes in suicide. Int. J. Neuropsychopharmacol. 15, 1161–1166 10.1017/S1461145711001520 [DOI] [PubMed] [Google Scholar]
- 126.Golden S.A., Christoffel D.J., Heshmati M., Hodes G.E., Magida J., Davis K.et al. (2013) Epigenetic regulation of RAC1 induces synaptic remodeling in stress disorders and depression. Nat. Med. 19, 337–344 10.1038/nm.3090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cruceanu C., Alda M., Nagy C., Freemantle E., Rouleau G.A. and Turecki G. (2013) H3K4 tri-methylation in synapsin genes leads to different expression patterns in bipolar disorder and major depression. Int. J. Neuropsychopharmacol. 16, 289–299 10.1017/S1461145712000363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Nestler E.J., Peña C.J., Kundakovic M., Mitchell A. and Akbarian S. (2016) Epigenetic basis of mental illness. Neuroscientist: a Rev. J. Bringing Neurobiol. Neurol. Psychiatry 22, 447–463 10.1177/1073858415608147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Thumfart K.M., Jawaid A., Bright K., Flachsmann M. and Mansuy I.M. (2022) Epigenetics of childhood trauma: Long term sequelae and potential for treatment. Neurosci. Biobehav. Rev. 132, 1049–1066 10.1016/j.neubiorev.2021.10.042 [DOI] [PubMed] [Google Scholar]
- 130.Torres-Berrío A., Issler O., Parise E.M. and Nestler E.J. (2019) Unraveling the epigenetic landscape of depression: focus on early life stress. Dialogues Clin. Neurosci. 21, 341–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Tsankova N.M., Berton O., Renthal W., Kumar A., Neve R.L. and Nestler E.J. (2006) Sustained hippocampal chromatin regulation in a mouse model of depression and antidepressant action. Nat. Neurosci. 9, 519–525 10.1038/nn1659 [DOI] [PubMed] [Google Scholar]
- 132.Réus G.Z., Abelaira H.M., dos Santos M.A.B., Carlessi A.S., Tomaz D.B., Neotti M.V.et al. (2013) Ketamine and imipramine in the nucleus accumbens regulate histone deacetylation induced by maternal deprivation and are critical for associated behaviors. Behav. Brain Res. 256, 451–456 10.1016/j.bbr.2013.08.041 [DOI] [PubMed] [Google Scholar]
- 133.Nghia N.A., Hirasawa T., Kasai H., Obata C., Moriishi K., Mochizuki K.et al. (2015) Long-term imipramine treatment increases N-methyl-d-aspartate receptor activity and expression via epigenetic mechanisms. Eur. J. Pharmacol. 752, 69–77 10.1016/j.ejphar.2015.02.010 [DOI] [PubMed] [Google Scholar]
- 134.Schmauss C. (2015) An HDAC-dependent epigenetic mechanism that enhances the efficacy of the antidepressant drug fluoxetine. Sci. Rep. 5, 8171 10.1038/srep08171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Han A., Sung Y.B., Chung S.Y. and Kwon M.S. (2014) Possible additional antidepressant-like mechanism of sodium butyrate: targeting the hippocampus. Neuropharmacology 81, 292–302 10.1016/j.neuropharm.2014.02.017 [DOI] [PubMed] [Google Scholar]
- 136.Ershadi A.S.B., Amini-Khoei H., Hosseini M.J. and Dehpour A.R. (2021) SAHA improves depressive symptoms, cognitive impairment and oxidative stress: rise of a new antidepressant class. Neurochem. Res. 46, 1252–1263 10.1007/s11064-021-03263-8 [DOI] [PubMed] [Google Scholar]
- 137.Hsing C.H., Hung S.K., Chen Y.C., Wei T.S., Sun D.P., Wang J.J.et al. (2015) Histone deacetylase inhibitor trichostatin A ameliorated endotoxin-induced neuroinflammation and cognitive dysfunction. Mediators Inflamm. 2015, 163140 10.1155/2015/163140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Schroeder F.A., Lin C.L., Crusio W.E. and Akbarian S. (2007) Antidepressant-like effects of the histone deacetylase inhibitor, sodium butyrate, in the mouse. Biol. Psychiatry 62, 55–64 10.1016/j.biopsych.2006.06.036 [DOI] [PubMed] [Google Scholar]
- 139.Panni S., Lovering R.C., Porras P. and Orchard S. (2020) Non-coding RNA regulatory networks. Biochim. Biophys. Acta. 1863, 194417 10.1016/j.bbagrm.2019.194417 [DOI] [PubMed] [Google Scholar]
- 140.Lin R. and Turecki G. (2017) Noncoding RNAs in depression. In Neuroepigenomics in Aging and Disease(Delgado-Morales R., ed.), pp. 197–210, Springer International Publishing, Cham: 10.1007/978-3-319-53889-1_11 [DOI] [Google Scholar]
- 141.Snijders C., de Nijs L., Baker D.G., Hauger R.L., van den Hove D., Kenis G.et al. (2018) MicroRNAs in post-traumatic stress disorder. In Behavioral Neurobiology of PTSD(Vermetten E., Baker D.G. and Risbrough V.B., eds), pp. 23–46, Springer International Publishing, Cham: [DOI] [PubMed] [Google Scholar]
- 142.Murphy C.P. and Singewald N. (2019) Role of MicroRNAs in anxiety and anxiety-related disorders. In Behavioral Neurogenomics(Binder E.B. and Klengel T., eds), pp. 185–219, Springer International Publishing, Cham: [DOI] [PubMed] [Google Scholar]
- 143.O'Connor R.M., Gururajan A., Dinan T.G., Kenny P.J. and Cryan J.F. (2016) All roads lead to the miRNome: miRNAs have a central role in the molecular pathophysiology of psychiatric disorders. Trends Pharmacol. Sci. 37, 1029–1044 10.1016/j.tips.2016.10.004 [DOI] [PubMed] [Google Scholar]
- 144.Dwivedi Y. (2018) MicroRNAs in depression and suicide: recent insights and future perspectives. J. Affect. Disord. 240, 146–154 10.1016/j.jad.2018.07.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Hung Y.-Y., Wu M.-K., Tsai M.-C., Huang Y.-L. and Kang H.-Y. (2019) Aberrant expression of intracellular let-7e, miR-146a, and miR-155 correlates with severity of depression in patients with major depressive disorder and is ameliorated after antidepressant treatment. Cells 8, 1–12 10.3390/cells8070647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Bocchio-Chiavetto L., Maffioletti E., Bettinsoli P., Giovannini C., Bignotti S., Tardito D.et al. (2013) Blood microRNA changes in depressed patients during antidepressant treatment. Eur. Neuropsychopharmacol. 23, 602–611 10.1016/j.euroneuro.2012.06.013 [DOI] [PubMed] [Google Scholar]
- 147.Baudry A., Mouillet-Richard S., Schneider B., Launay J.M. and Kellermann O. (2010) miR-16 targets the serotonin transporter: a new facet for adaptive responses to antidepressants. Science 329, 1537–1541 10.1126/science.1193692 [DOI] [PubMed] [Google Scholar]
- 148.Wang S., Wu W. and Claret F.X. (2017) Mutual regulation of microRNAs and DNA methylation in human cancers. Epigenetics 12, 187–197 10.1080/15592294.2016.1273308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Pérez-Rodríguez D., López-Fernández H. and Agís-Balboa R.C. (2021) Application of miRNA-seq in neuropsychiatry: a methodological perspective. Comput. Biol. Med. 135, 104603 10.1016/j.compbiomed.2021.104603 [DOI] [PubMed] [Google Scholar]
- 150.Rotter A., Bayerlein K., Hansbauer M., Weiland J., Sperling W., Kornhuber J.et al. (2013) CB1 and CB2 receptor expression and promoter methylation in patients with cannabis dependence. Eur. Addict. Res. 19, 13–20 10.1159/000338642 [DOI] [PubMed] [Google Scholar]
- 151.Liu J., Chen J., Ehrlich S., Walton E., White T., Perrone-Bizzozero N.et al. (2014) Methylation patterns in whole blood correlate with symptoms in schizophrenia patients. Schizophr. Bull. 40, 769–776 10.1093/schbul/sbt080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.DiNieri J.A., Wang X., Szutorisz H., Spano S.M., Kaur J., Casaccia P.et al. (2011) Maternal cannabis use alters ventral striatal dopamine D2 gene regulation in the offspring. Biol. Psychiatry 70, 763–769 10.1016/j.biopsych.2011.06.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Wang X., Dow-Edwards D., Anderson V., Minkoff H. and Hurd Y.L. (2004) In utero marijuana exposure associated with abnormal amygdala dopamine D2 gene expression in the human fetus. Biol. Psychiatry 56, 909–915 10.1016/j.biopsych.2004.10.015 [DOI] [PubMed] [Google Scholar]
- 154.Ibn Lahmar Andaloussi Z., Taghzouti K. and Abboussi O. (2019) Behavioural and epigenetic effects of paternal exposure to cannabinoids during adolescence on offspring vulnerability to stress. Int. J. Dev. Neurosci. 72, 48–54 10.1016/j.ijdevneu.2018.11.007 [DOI] [PubMed] [Google Scholar]
- 155.Innocenzi E., De Domenico E., Ciccarone F., Zampieri M., Rossi G., Cicconi R.et al. (2019) Paternal activation of CB2 cannabinoid receptor impairs placental and embryonic growth via an epigenetic mechanism. Sci. Rep. 9, 17034 10.1038/s41598-019-53579-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Sales A.J., Guimarães F.S. and Joca S.R.L. (2020) CBD modulates DNA methylation in the prefrontal cortex and hippocampus of mice exposed to forced swim. Behav. Brain Res. 388, 112627 10.1016/j.bbr.2020.112627 [DOI] [PubMed] [Google Scholar]
- 157.da Silva V.K., de Freitas B.S., Dornelles V.C., Kist L.W., Bogo M.R., Silva M.C.et al. (2018) Novel insights into mitochondrial molecular targets of iron-induced neurodegeneration: Reversal by cannabidiol. Brain Res. Bull. 139, 1–8 10.1016/j.brainresbull.2018.01.014 [DOI] [PubMed] [Google Scholar]
- 158.Wanner N.M., Colwell M., Drown C. and Faulk C. (2020) Subacute cannabidiol alters genome-wide DNA methylation in adult mouse hippocampus. Environ. Mol. Mutagen. 61, 890–900 10.1002/em.22396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wu H., Coskun V., Tao J., Xie W., Ge W., Yoshikawa K.et al. (2010) Dnmt3a-dependent nonpromoter DNA methylation facilitates transcription of neurogenic genes. Science 329, 444–448 10.1126/science.1190485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wu Z., Huang K., Yu J., Le T., Namihira M., Liu Y.et al. (2012) Dnmt3a regulates both proliferation and differentiation of mouse neural stem cells. J. Neurosci. Res. 90, 1883–1891 10.1002/jnr.23077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.García-Gutiérrez M.S., Navarrete F., Gasparyan A., Austrich-Olivares A., Sala F. and Manzanares J. (2020) Cannabidiol: a potential new alternative for the treatment of anxiety, depression, and psychotic disorders. Biomolecules 10, 1–34 10.3390/biom10111575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Todd S.M., Zhou C., Clarke D.J., Chohan T.W., Bahceci D. and Arnold J.C. (2017) Interactions between cannabidiol and Δ9-THC following acute and repeated dosing: Rebound hyperactivity, sensorimotor gating and epigenetic and neuroadaptive changes in the mesolimbic pathway. Eur. Neuropsychopharmacol. 27, 132–145 10.1016/j.euroneuro.2016.12.004 [DOI] [PubMed] [Google Scholar]
- 163.Pastrana-Trejo J.C., Duarte-Aké F., Us-Camas R., De-la-Peña C., Parker L., Pertwee R.G.et al. (2021) Effects on the post-translational modification of H3K4Me3, H3K9ac, H3K9Me2, H3K27Me3, and H3K36Me2 levels in cerebral cortex, hypothalamus and pons of rats after a systemic administration of cannabidiol: a preliminary study. Cent. Nerv. Syst. Agents Med. Chem. 21, 142–147 10.2174/1871524920666200924114524 [DOI] [PubMed] [Google Scholar]
- 164.Lomazzo E., König F., Abassi L., Jelinek R. and Lutz B. (2017) Chronic stress leads to epigenetic dysregulation in the neuropeptide-Y and cannabinoid CB1 receptor genes in the mouse cingulate cortex. Neuropharmacology 113, 301–313 10.1016/j.neuropharm.2016.10.008 [DOI] [PubMed] [Google Scholar]
- 165.Wang S.E., Ko S.Y., Kim Y.-S., Jo S., Lee S.H., Jung S.J.et al. (2018) Capsaicin upregulates HDAC2 via TRPV1 and impairs neuronal maturation in mice. Exp. Mol. Med. 50, e455 10.1038/emm.2017.289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Wang S.E., Ko S.Y., Jo S., Choi M., Lee S.H., Jo H.-R.et al. (2017) TRPV1 Regulates Stress Responses through HDAC2. Cell Rep. 19, 401–412 10.1016/j.celrep.2017.03.050 [DOI] [PubMed] [Google Scholar]
- 167.Buran İ., Etem E.Ö., Tektemur A. and Elyas H. (2017) Treatment with TREK1 and TRPC3/6 ion channel inhibitors upregulates microRNA expression in a mouse model of chronic mild stress. Neurosci. Lett. 656, 51–57 10.1016/j.neulet.2017.07.017 [DOI] [PubMed] [Google Scholar]
- 168.Lee P.H., Perlis R.H., Jung J.Y., Byrne E.M., Rueckert E., Siburian R.et al. (2012) Multi-locus genome-wide association analysis supports the role of glutamatergic synaptic transmission in the etiology of major depressive disorder. Transl. Psychiatry 2, e184 10.1038/tp.2012.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Numakawa T., Nakajima S., Adachi N., Richards M. and Kunugi H. (2013) Neurotrophin Bdnf and novel molecular targets in depression pathogenesis. J. Neurol. Transl. Neurosci. 1, 1–8 [Google Scholar]
- 170.Dwivedi Y., Rizavi H.S., Roberts R.C., Conley R.C., Tamminga C.A. and Pandey G.N. (2001) Reduced activation and expression of ERK1/2 MAP kinase in the post-mortem brain of depressed suicide subjects. J. Neurochem. 77, 916–928 10.1046/j.1471-4159.2001.00300.x [DOI] [PubMed] [Google Scholar]
- 171.Launay J., Mouillet-Richard S., Baudry A., Pietri M. and Kellermann O. (2011) Raphe-mediated signals control the hippocampal response to SRI antidepressants via miR-16. Transl. Psychiatry 1, e56 10.1038/tp.2011.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Bai M., Zhu X., Zhang Y., Zhang S., Zhang L., Xue L.et al. (2012) Abnormal hippocampal BDNF and miR-16 expression is associated with depression-like behaviors induced by stress during early life. PLoS ONE 7, e46921 10.1371/journal.pone.0046921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Tochigi M., Iwamoto K., Bundo M., Sasaki T., Kato N. and Kato T. (2008) Gene expression profiling of major depression and suicide in the prefrontal cortex of postmortem brains. Neurosci. Res. 60, 184–191 10.1016/j.neures.2007.10.010 [DOI] [PubMed] [Google Scholar]
- 174.Shi Y., Yuan Y., Xu Z., Pu M., Wang C., Zhang Y.et al. (2012) Genetic variation in the calcium/calmodulin-dependent protein kinase (CaMK) pathway is associated with antidepressant response in females. J. Affect. Disord. 136, 558–566 10.1016/j.jad.2011.10.030 [DOI] [PubMed] [Google Scholar]
- 175.Portugalov A., Zaidan H., Gaisler-Salomon I., Hillard C.J. and Akirav I. (2022) FAAH Inhibition restores early life stress-induced alterations in PFC microRNAs associated with depressive-like behavior in male and female rats. Int. J. Mol. Sci. 23, 1–23 10.3390/ijms232416101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Chiarlone A., Börner C., Martín-Gómez L., Jiménez-González A., García-Concejo A., García-Bermejo M.L.et al. (2016) MicroRNA let-7d is a target of cannabinoid CB1 receptor and controls cannabinoid signaling. Neuropharmacology 108, 345–352 10.1016/j.neuropharm.2016.05.007 [DOI] [PubMed] [Google Scholar]
- 177.Wei Y.B., Liu J.J., Villaescusa J.C., Åberg E., Brené S., Wegener G.et al. (2016) Elevation of Il6 is associated with disturbed let-7 biogenesis in a genetic model of depression. Translational Psychiatry 6, e869 10.1038/tp.2016.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Bahi A. and Dreyer J.-L. (2018) Lentiviral-mediated let-7d microRNA overexpression induced anxiolytic- and anti-depressant-like behaviors and impaired dopamine D3 receptor expression. Eur. Neuropsychopharmacol. 28, 1394–1404 10.1016/j.euroneuro.2018.09.004 [DOI] [PubMed] [Google Scholar]
- 179.Zhao C., Sun G., Ye P., Li S. and Shi Y. (2013) MicroRNA let-7d regulates the TLX/microRNA-9 cascade to control neural cell fate and neurogenesis. Sci. Rep. 3, 1329 10.1038/srep01329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Chandrasekar V. and Dreyer J.-L. (2009) microRNAs miR-124, let-7d and miR-181a regulate Cocaine-induced Plasticity. Mol. Cell. Neurosci. 42, 350–362 10.1016/j.mcn.2009.08.009 [DOI] [PubMed] [Google Scholar]
- 181.Ferber S.G., Roth T.L. and Weller A. (2020) Epigenetic fragility of the endocannabinoid system under stress: risk for mood disorders and pharmacogenomic implications. Epigenomics 12, 657–660 10.2217/epi-2020-0037 [DOI] [PubMed] [Google Scholar]
- 182.Salamat J.M., Abbott K.L., Flannery P.C., Ledbetter E.L. and Pondugula S.R. (2022) Interplay between the cannabinoid system and microRNAs in cancer. ACS Omega 7, 9995–10000 10.1021/acsomega.2c00635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Meccariello R., Santoro A., Angelo S., Morrone R., Fasano S., Viggiano A.et al. (2020) The epigenetics of the endocannabinoid system. Int. J. Mol. Sci. 21, 10.3390/ijms21031113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Gomes T.M., Dias da Silva D., Carmo H., Carvalho F. and Silva J.P. (2020) Epigenetics and the endocannabinoid system signaling: An intricate interplay modulating neurodevelopment. Pharmacol. Res. 162, 105237 10.1016/j.phrs.2020.105237 [DOI] [PubMed] [Google Scholar]
- 185.Tao R., Li C., Jaffe A.E., Shin J.H., Deep-Soboslay A., Yamin Reet al. (2020) Cannabinoid receptor CNR1 expression and DNA methylation in human prefrontal cortex, hippocampus and caudate in brain development and schizophrenia. Transl. Psychiatry 10, 158 10.1038/s41398-020-0832-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Wang D., Wang H., Ning W., Backlund M.G., Dey S.K. and DuBois R.N. (2008) Loss of cannabinoid receptor 1 accelerates intestinal tumor growth. Cancer Res. 68, 6468–6476 10.1158/0008-5472.CAN-08-0896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Xia D., Wang D., Kim S.-H., Katoh H. and DuBois R.N. (2012) Prostaglandin E2 promotes intestinal tumor growth via DNA methylation. Nat. Med. 18, 224–226 10.1038/nm.2608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Hong S., Zheng G. and Wiley J.W. (2015) Epigenetic regulation of genes that modulate chronic stress-induced visceral pain in the peripheral nervous system. Gastroenterology 148, 148.e7–157.e7 10.1053/j.gastro.2014.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.D'Addario C., Micale V., Di Bartolomeo M., Stark T., Pucci M., Sulcova A.et al. (2017) A preliminary study of endocannabinoid system regulation in psychosis: Distinct alterations of CNR1 promoter DNA methylation in patients with schizophrenia. Schizophr. Res. 188, 132–140 10.1016/j.schres.2017.01.022 [DOI] [PubMed] [Google Scholar]
- 190.Pucci M., Micioni Di Bonaventura M.V., Vezzoli V., Zaplatic E., Massimini M., Mai S.et al. (2019) Preclinical and clinical evidence for a distinct regulation of Mu opioid and Type 1 cannabinoid receptor genes expression in obesity. Front. Genet. 10, 523 10.3389/fgene.2019.00523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Mancino S., Burokas A., Gutiérrez-Cuesta J., Gutiérrez-Martos M., Martín-García E., Pucci M.et al. (2015) Epigenetic and proteomic expression changes promoted by eating addictive-like behavior. Neuropsychopharmacology 40, 2788–2800 10.1038/npp.2015.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Di Francesco A., Falconi A., Di Germanio C., Micioni Di Bonaventura M.V., Costa A., Caramuta S.et al. (2015) Extravirgin olive oil up-regulates CB1 tumor suppressor gene in human colon cancer cells and in rat colon via epigenetic mechanisms. J. Nutr. Biochem. 26, 250–258 10.1016/j.jnutbio.2014.10.013 [DOI] [PubMed] [Google Scholar]
- 193.D'Addario C., Zaplatic E., Giunti E., Pucci M., Micioni Di Bonaventura M.V., Scherma M.et al. (2020) Epigenetic regulation of the cannabinoid receptor CB1 in an activity-based rat model of anorexia nervosa. Int. J. Eat. Disord. 53, 432–446 10.1002/eat.23271 [DOI] [PubMed] [Google Scholar]
- 194.Börner C., Martella E., Höllt V. and Kraus J. (2012) Regulation of opioid and cannabinoid receptor genes in human neuroblastoma and T cells by the epigenetic modifiers trichostatin A and 5-Aza-2′-deoxycytidine. NeuroImmunoModulation 19, 180–186 10.1159/000331474 [DOI] [PubMed] [Google Scholar]
- 195.Chen J., Hutchison K.E., Bryan A.D., Filbey F.M., Calhoun V.D., Claus E.D.et al. (2018) Opposite Epigenetic associations with alcohol use and exercise intervention. Front. Psychiatry 9, 594 10.3389/fpsyt.2018.00594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.D'Addario C., Di Francesco A., Arosio B., Gussago C., Dell'Osso B., Bari M.et al. (2012) Epigenetic regulation of fatty acid amide hydrolase in Alzheimer disease. PLoS ONE 7, e39186 10.1371/journal.pone.0039186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Franklin T.B., Russig H., Weiss I.C., Gräff J., Linder N., Michalon A.et al. (2010) Epigenetic transmission of the impact of early stress across generations. Biol. Psychiatry 68, 408–415 10.1016/j.biopsych.2010.05.036 [DOI] [PubMed] [Google Scholar]
- 198.Uddin M., Aiello A.E., Wildman D.E., Koenen K.C., Pawelec G., de los Santos R.et al. (2010) Epigenetic and immune function profiles associated with posttraumatic stress disorder. Proc. Natl. Acad. Sci. 107, 9470–9475 10.1073/pnas.0910794107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Hill M.N., Campolongo P., Yehuda R. and Patel S. (2018) Integrating endocannabinoid signaling and cannabinoids into the biology and treatment of posttraumatic stress disorder. Neuropsychopharmacology 43, 80–102 10.1038/npp.2017.162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Subbanna S., Nagre N.N., Umapathy N.S., Pace B.S. and Basavarajappa B.S. (2015) Ethanol exposure induces neonatal neurodegeneration by enhancing CB1R exon1 histone H4K8 acetylation and up-regulating CB1R function causing neurobehavioral abnormalities in adult mice. Int. J. Neuropsychopharmacolog. 18, pyu028 10.1093/ijnp/pyu028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Subbanna S., Shivakumar M., Psychoyos D., Xie S. and Basavarajappa B.S. (2013) Anandamide-CB1 receptor signaling contributes to postnatal ethanol-induced neonatal neurodegeneration, adult synaptic, and memory deficits. J. Neurosci.: Off. J. Soc. Neurosci. 33, 6350–6366 10.1523/JNEUROSCI.3786-12.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Luo Y., Zhang J., Chen L., Chen S.-R., Chen H., Zhang G.et al. (2020) Histone methyltransferase G9a diminishes expression of cannabinoid CB1 receptors in primary sensory neurons in neuropathic pain. J. Biol. Chem. 295, 3553–3562 10.1074/jbc.RA119.011053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Pucci M., Micioni Di Bonaventura M.V., Zaplatic E., Bellia F., Maccarrone M., Cifani C.et al. (2019) Transcriptional regulation of the endocannabinoid system in a rat model of binge-eating behavior reveals a selective modulation of the hypothalamic fatty acid amide hydrolase gene. Int. J. Eat. Disord. 52, 51–60 10.1002/eat.22989 [DOI] [PubMed] [Google Scholar]
- 204.Tung C.W., Ho C., Hsu Y.C., Huang S.C., Shih Y.H. and Lin C.L. (2019) MicroRNA-29a attenuates diabetic glomerular injury through modulating cannabinoid receptor 1 signaling. Molecules 24, 10.3390/molecules24020264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Sredni S.T., Huang C.C., Suzuki M., Pundy T., Chou P. and Tomita T. (2016) Spontaneous involution of pediatric low-grade gliomas: high expression of cannabinoid receptor 1 (CNR1) at the time of diagnosis may indicate involvement of the endocannabinoid system. Childs Nervous System 32, 2061–2067 10.1007/s00381-016-3243-7 [DOI] [PubMed] [Google Scholar]
- 206.Li L., Xu Y., Zhao M. and Gao Z. (2020) Neuro-protective roles of long non-coding RNA MALAT1 in Alzheimer's disease with the involvement of the microRNA-30b/CNR1 network and the following PI3K/AKT activation. Exp. Mol. Pathol. 117, 104545 10.1016/j.yexmp.2020.104545 [DOI] [PubMed] [Google Scholar]
- 207.Gou X., Wu J., Huang M., Weng Y., Yang T., Chen T.et al. (2020) microRNA-128 mediates CB1 expression and regulates NF-KB/p-JNK axis to influence the occurrence of diabetic bladder disease. J. Transl. Med. 18, 284 10.1186/s12967-020-02406-9 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 208.Zhang A., Bai Z., Yi W., Hu Z. and Hao J. (2021) Overexpression of miR-338-5p in exosomes derived from mesenchymal stromal cells provides neuroprotective effects by the Cnr1/Rap1/Akt pathway after spinal cord injury in rats. Neurosci. Lett. 761, 136124 10.1016/j.neulet.2021.136124 [DOI] [PubMed] [Google Scholar]
- 209.Möhnle P., Schütz S.V., Schmidt M., Hinske C., Hübner M., Heyn J.et al. (2014) MicroRNA-665 is involved in the regulation of the expression of the cardioprotective cannabinoid receptor CB2 in patients with severe heart failure. Biochem. Biophys. Res. Commun. 451, 516–521 10.1016/j.bbrc.2014.08.008 [DOI] [PubMed] [Google Scholar]
- 210.Xu A., Yang Y., Shao Y., Wu M. and Sun Y. (2019) Inhibiting effect of microRNA-187-3p on osteogenic differentiation of osteoblast precursor cells by suppressing cannabinoid receptor type 2. Differentiation 109, 9–15 10.1016/j.diff.2019.07.002 [DOI] [PubMed] [Google Scholar]
- 211.Most D., Salem N.A., Tiwari G.R., Blednov Y.A., Mayfield R.D. and Harris R.A. (2019) Silencing synaptic MicroRNA-411 reduces voluntary alcohol consumption in mice. Addict. Biol. 24, 604–616 10.1111/adb.12625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Huang C., Wang Y., Wu Z., Xu J., Zhou L., Wang D.et al. (2021) miR-98-5p plays a critical role in depression and antidepressant effect of ketamine. Transl. Psychiatry 11, 454 10.1038/s41398-021-01588-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Uchida S., Hara K., Kobayashi A., Funato H., Hobara T., Otsuki K.et al. (2010) Early life stress enhances behavioral vulnerability to stress through the activation of REST4-mediated gene transcription in the medial prefrontal cortex of rodents. J. Neurosci. 30, 15007–15018 10.1523/JNEUROSCI.1436-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Maffioletti E., Bocchio-Chiavetto L., Perusi G., Carvalho Silva R., Sacco C., Bazzanella R.et al. (2021) Inflammation-related microRNAs are involved in stressful life events exposure and in trauma-focused psychotherapy in treatment-resistant depressed patients. Eur. J. Psychotraumatol. 12, 1987655 10.1080/20008198.2021.1987655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Honda M., Kuwano Y., Katsuura-Kamano S., Kamezaki Y., Fujita K., Akaike Y.et al. (2013) Chronic academic stress increases a group of microRNAs in peripheral blood. PLoS ONE 8, e75960 10.1371/journal.pone.0075960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Sillivan S.E., Jones M.E., Jamieson S., Rumbaugh G. and Miller C.A. (2019) Bioinformatic analysis of long-lasting transcriptional and translational changes in the basolateral amygdala following acute stress. PLoS ONE 14, e0209846 10.1371/journal.pone.0209846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Wan Y., Liu Y., Wang X., Wu J., Liu K., Zhou J.et al. (2015) Identification of differential microRNAs in cerebrospinal fluid and serum of patients with major depressive disorder. PLoS ONE 10, e0121975 10.1371/journal.pone.0121975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Wan Y.-Q., Feng J.-G., Li M., Wang M.-Z., Liu L., Liu X.et al. (2018) Prefrontal cortex miR-29b-3p plays a key role in the antidepressant-like effect of ketamine in rats. Exp. Mol. Med. 50, 1–14 10.1038/s12276-018-0164-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Rinaldi A., Vincenti S., De Vito F., Bozzoni I., Oliverio A., Presutti C.et al. (2010) Stress induces region specific alterations in microRNAs expression in mice. Behav. Brain Res. 208, 265–269 10.1016/j.bbr.2009.11.012 [DOI] [PubMed] [Google Scholar]
- 220.Kye M.J., Neveu P., Lee Y.S., Zhou M., Steen J.A., Sahin M.et al. (2011) NMDA mediated contextual conditioning changes miRNA expression. PLoS ONE 6, e24682 10.1371/journal.pone.0024682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Gorinski N., Bijata M., Prasad S., Wirth A., Abdel Galil D., Zeug A.et al. (2019) Attenuated palmitoylation of serotonin receptor 5-HT1A affects receptor function and contributes to depression-like behaviors. Nat. Commun. 10, 3924 10.1038/s41467-019-11876-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Pearson-Leary J., Eacret D., Chen R., Takano H., Nicholas B. and Bhatnagar S. (2017) Inflammation and vascular remodeling in the ventral hippocampus contributes to vulnerability to stress. Transl. Psychiatry 7, e1160 10.1038/tp.2017.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Shen M., Song Z. and Wang J.H. (2019) microRNA and mRNA profiles in the amygdala are associated with stress-induced depression and resilience in juvenile mice. Psychopharmacology (Berl.) 236, 2119–2142 10.1007/s00213-019-05209-z [DOI] [PubMed] [Google Scholar]
- 224.Martin C.G., Kim H., Yun S., Livingston W., Fetta J., Mysliwiec V.et al. (2017) Circulating miRNA associated with posttraumatic stress disorder in a cohort of military combat veterans. Psychiatry Res. 251, 261–265 10.1016/j.psychres.2017.01.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Roy B., Dunbar M., Agrawal J., Allen L. and Dwivedi Y. (2020) Amygdala-based altered miRNome and epigenetic contribution of miR-128-3p in conferring susceptibility to depression-like behavior via Wnt signaling. Int. J. Neuropsychopharmacol. 23, 165–177 10.1093/ijnp/pyz071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Lin Q., Wei W., Coelho C.M., Li X., Baker-Andresen D., Dudley K.et al. (2011) The brain-specific microRNA miR-128b regulates the formation of fear-extinction memory. Nat. Neurosci. 14, 1115–1117 10.1038/nn.2891 [DOI] [PubMed] [Google Scholar]
- 227.Smalheiser N.R., Lugli G., Rizavi H.S., Torvik V.I., Turecki G. and Dwivedi Y. (2012) MicroRNA expression is down-regulated and reorganized in prefrontal cortex of depressed suicide subjects. PloS ONE 7, e33201 10.1371/journal.pone.0033201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Sun X., Song Z., Si Y. and Wang J.-H. (2018) microRNA and mRNA profiles in ventral tegmental area relevant to stress-induced depression and resilience. Prog. Neuropsychopharmacol. Biol. Psychiatry 86, 150–165 10.1016/j.pnpbp.2018.05.023 [DOI] [PubMed] [Google Scholar]
- 229.Yang J., Sun J., Lu Y., An T., Lu W. and Wang J.H. (2020) Revision to psychopharmacology mRNA and microRNA profiles are associated with stress susceptibility and resilience induced by psychological stress in the prefrontal cortex. Psychopharmacology (Berl.) 237, 3067–3093 10.1007/s00213-020-05593-x [DOI] [PubMed] [Google Scholar]
- 230.Homorogan C., Enatescu V.R., Nitusca D., Marcu A., Seclaman E. and Marian C. (2021) Distribution of microRNAs associated with major depressive disorder among blood compartments. J. Int. Med. Res. 49, 3000605211006633 10.1177/03000605211006633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Teppen T.L., Krishnan H.R., Zhang H., Sakharkar A.J. and Pandey S.C. (2016) The potential role of amygdaloid microRNA-494 in alcohol-induced anxiolysis. Biol. Psychiatry 80, 711–719 10.1016/j.biopsych.2015.10.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Belzeaux R., Bergon A., Jeanjean V., Loriod B., Formisano-Tréziny C., Verrier L.et al. (2012) Responder and nonresponder patients exhibit different peripheral transcriptional signatures during major depressive episode. Transl. Psychiatry 2, e185 10.1038/tp.2012.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Balakathiresan N.S., Chandran R., Bhomia M., Jia M., Li H. and Maheshwari R.K. (2014) Serum and amygdala microRNA signatures of posttraumatic stress: fear correlation and biomarker potential. J. Psychiatr. Res. 57, 65–73 10.1016/j.jpsychires.2014.05.020 [DOI] [PubMed] [Google Scholar]
- 234.Solich J., Kolasa M., Faron-Górecka A., Hajto J., Piechota M. and Dziedzicka-Wasylewska M. (2021) MicroRNA Let-7e in the mouse prefrontal cortex differentiates restraint-stress-resilient genotypes from susceptible genotype. Int. J. Mol. Sci. 22, 1–16 10.3390/ijms22179439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Maffioletti E., Cattaneo A., Rosso G., Maina G., Maj C., Gennarelli M.et al. (2016) Peripheral whole blood microRNA alterations in major depression and bipolar disorder. J. Affect. Disord. 200, 250–258 10.1016/j.jad.2016.04.021 [DOI] [PubMed] [Google Scholar]
- 236.Maurel O.M., Torrisi S.A., Barbagallo C., Purrello M., Salomone S., Drago F.et al. (2021) Dysregulation of miR-15a-5p, miR-497a-5p and miR-511-5p is associated with modulation of BDNF and FKBP5 in brain areas of PTSD-related susceptible and resilient mice. Int. J. Mol. Sci. 22, 10.3390/ijms22105157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Zhao C., Zhou B., Cao J., Zhang Y., Li W., Wang M.et al. (2020) miR-187-3p participates in contextual fear memory formation through modulating SATB2 expression in the hippocampus. Neuroreport 31, 909–917 10.1097/WNR.0000000000001484 [DOI] [PubMed] [Google Scholar]
- 238.Su J., Li P., Zhuang Q., Chen X., Zhang X., Li X.et al. (2021) Identification of the similarities and differences of molecular networks associated with fear memory formation, extinction, and updating in the amygdala. Front. Mol. Neurosci. 14, 778170 10.3389/fnmol.2021.778170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.McKibben L.A. and Dwivedi Y. (2021) Early life and adult stress promote sex dependent changes in hypothalamic miRNAs and environmental enrichment prevents stress-induced miRNA and gene expression changes in rats. BMC Genomics 22, 701 10.1186/s12864-021-08003-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.McKibben L.A. and Dwivedi Y. (2021) Early-life stress induces genome-wide sex-dependent miRNA expression and correlation across limbic brain areas in rats. Epigenomics 13, 1031–1056 10.2217/epi-2021-0037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Patrício P., Mateus-Pinheiro A., Irmler M., Alves N.D., Machado-Santos A.R., Morais M.et al. (2015) Differential and converging molecular mechanisms of antidepressants' action in the hippocampal dentate gyrus. Neuropsychopharmacology 40, 338–349 10.1038/npp.2014.176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Gupta S., Kim S.Y., Artis S., Molfese D.L., Schumacher A., Sweatt J.D.et al. (2010) Histone methylation regulates memory formation. J. Neurosci.:Off. J. Soc. Neurosci. 30, 3589–3599 10.1523/JNEUROSCI.3732-09.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Peixoto L. and Abel T. (2013) The role of histone acetylation in memory formation and cognitive impairments. Neuropsychopharmacology 38, 62–76 10.1038/npp.2012.86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Ookubo M., Kanai H., Aoki H. and Yamada N. (2013) Antidepressants and mood stabilizers effects on histone deacetylase expression in C57BL/6 mice: Brain region specific changes. J. Psychiatr. Res. 47, 1204–1214 10.1016/j.jpsychires.2013.05.028 [DOI] [PubMed] [Google Scholar]
- 245.Manzanares J., Cabañero D., Puente N., García-Gutiérrez M.S., Grandes P. and Maldonado R. (2018) Role of the endocannabinoid system in drug addiction. Biochem. Pharmacol. 157, 108–121 10.1016/j.bcp.2018.09.013 [DOI] [PubMed] [Google Scholar]
- 246.Wolfe S.A., Vozella V. and Roberto M. (2022) The synaptic interactions of alcohol and the endogenous cannabinoid system. Alcohol Res.: Curr. Rev. 42, 03 10.35946/arcr.v42.1.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Gobira P.H., Joca S.R. and Moreira F.A. (2022) Roles of cannabinoid CB1 and CB2 receptors in the modulation of psychostimulant responses. Acta Neuropsychiatrica 1–11 10.1017/neu.2022.23 [DOI] [PubMed] [Google Scholar]
- 248.Mantsch J.R., Baker D.A., Funk D., Le A.D. and Shaham Y. (2016) Stress-induced reinstatement of drug seeking: 20 years of progress. Neuropsychopharmacology 41, 335–356 10.1038/npp.2015.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Bardo M.T., Hammerslag L.R. and Malone S.G. (2021) Effect of early life social adversity on drug abuse vulnerability: focus on corticotropin-releasing factor and oxytocin. Neuropharmacology 191, 108567 10.1016/j.neuropharm.2021.108567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Tung L.W., Lu G.L., Lee Y.H., Yu L., Lee H.J., Leishman E.et al. (2016) Orexins contribute to restraint stress-induced cocaine relapse by endocannabinoid-mediated disinhibition of dopaminergic neurons. Nat. Commun. 7, 12199 10.1038/ncomms12199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.McReynolds J.R., Doncheck E.M., Li Y., Vranjkovic O., Graf E.N., Ogasawara D.et al. (2018) Stress promotes drug seeking through glucocorticoid-dependent endocannabinoid mobilization in the prelimbic cortex. Biol. Psychiatry 84, 85–94 10.1016/j.biopsych.2017.09.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Sinha R (2008) Chronic Stress, Drug Use, and Vulnerability to Addiction. Annals of the New York Academy of Sciences 1141, 1105–130 10.1196/annals.1441.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.De Sa Nogueira D., Bourdy R., Alcala-Vida R., Filliol D., Andry V., Goumon Y.et al. (2022) Hippocampal cannabinoid 1 receptors are modulated following cocaine self-administration in male rats. Mol. Neurobiol. 59, 1896–1911 10.1007/s12035-022-02722-9 [DOI] [PubMed] [Google Scholar]
- 254.Subbanna S., Nagre N.N., Umapathy N.S., Pace B.S. and Basavarajappa B.S. (2014) Ethanol exposure induces neonatal neurodegeneration by enhancing CB1R Exon1 histone H4K8 acetylation and up-regulating CB1R function causing neurobehavioral abnormalities in adult mice. Int. J. Neuropsychopharmacol. 18, 1–15 10.1093/ijnp/pyu028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Nagre N.N., Subbanna S., Shivakumar M., Psychoyos D. and Basavarajappa B.S. (2015) CB1-receptor knockout neonatal mice are protected against ethanol-induced impairments of DNMT1, DNMT3A, and DNA methylation. J. Neurochem. 132, 429–442 10.1111/jnc.13006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Shivakumar M., Subbanna S., Joshi V. and Basavarajappa B.S. (2020) Postnatal ethanol exposure activates HDAC-mediated histone deacetylation, impairs synaptic plasticity gene expression and behavior in mice. Int. J. Neuropsychopharmacol. 23, 324–338 10.1093/ijnp/pyaa017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Subbanna S., Nagre N.N., Shivakumar M., Joshi V., Psychoyos D., Kutlar A.et al. (2018) CB1R-mediated activation of caspase-3 causes epigenetic and neurobehavioral abnormalities in postnatal ethanol-exposed mice. Front Mol. Neurosci. 11, 45 10.3389/fnmol.2018.00045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Stringer R.L., Laufer B.I., Kleiber M.L. and Singh S.M. (2013) Reduced expression of brain cannabinoid receptor 1 (Cnr1) is coupled with an increased complementary micro-RNA (miR-26b) in a mouse model of fetal alcohol spectrum disorders. Clin. Epigenetics 5, 14 10.1186/1868-7083-5-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Szutorisz H. and Hurd Y.L. (2018) High times for cannabis: Epigenetic imprint and its legacy on brain and behavior. Neurosci. Biobehav. Rev. 85, 93–101 10.1016/j.neubiorev.2017.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Tomasiewicz H.C., Jacobs M.M., Wilkinson M.B., Wilson S.P., Nestler E.J. and Hurd Y.L. (2012) Proenkephalin mediates the enduring effects of adolescent cannabis exposure associated with adult opiate vulnerability. Biol. Psychiatry 72, 803–810 10.1016/j.biopsych.2012.04.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Prini P., Penna F., Sciuccati E., Alberio T. and Rubino T. (2017) Chronic Δ8-THC exposure differently affects histone modifications in the adolescent and adult rat brain. Int. J. Mol. Sci. 18, 10.3390/ijms18102094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Prini P., Rusconi F., Zamberletti E., Gabaglio M., Penna F., Fasano M.et al. (2018) Adolescent THC exposure in female rats leads to cognitive deficits through a mechanism involving chromatin modifications in the prefrontal cortex. J. Psychiatry Neurosci.:JPN 43, 87–101 10.1503/jpn.170082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Watson C.T., Szutorisz H., Garg P., Martin Q., Landry J.A., Sharp A.J.et al. (2015) Genome-wide DNA methylation profiling reveals epigenetic changes in the rat nucleus accumbens associated with cross-generational effects of adolescent THC exposure. Neuropsychopharmacology 40, 2993–3005 10.1038/npp.2015.155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Levin E.D., Hawkey A.B., Hall B.J., Cauley M., Slade S., Yazdani E.et al. (2019) Paternal THC exposure in rats causes long-lasting neurobehavioral effects in the offspring. Neurotoxicol. Teratol. 74, 106806 10.1016/j.ntt.2019.04.003 [DOI] [PubMed] [Google Scholar]
- 265.Murphy S.K., Itchon-Ramos N., Visco Z., Huang Z., Grenier C., Schrott R.et al. (2018) Cannabinoid exposure and altered DNA methylation in rat and human sperm. Epigenetics 13, 1208–1221 10.1080/15592294.2018.1554521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Schrott R., Rajavel M., Acharya K., Huang Z., Acharya C., Hawkey A.et al. (2020) Sperm DNA methylation altered by THC and nicotine: Vulnerability of neurodevelopmental genes with bivalent chromatin. Sci. Rep. 10, 16022 10.1038/s41598-020-72783-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Schrott R., Greeson K.W., King D., Symosko Crow K.M., Easley C.At. and Murphy S.K. (2022) Cannabis alters DNA methylation at maternally imprinted and autism candidate genes in spermatogenic cells. Systems Biol. Reproduct. Med. 68, 357–369 10.1080/19396368.2022.2073292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.D'Addario C., Di Francesco A., Pucci M., Finazzi Agrò A. and Maccarrone M. (2013) Epigenetic mechanisms and endocannabinoid signalling. FEBS J. 280, 1905–1917 10.1111/febs.12125 [DOI] [PubMed] [Google Scholar]
- 269.Rusconi F., Rubino T. and Battaglioli E. (2020) Endocannabinoid-epigenetic cross-talk: a bridge toward stress coping. Int. J. Mol. Sci. 21, 1–13 10.3390/ijms21176252 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable.