Abstract
Background and aims
Irrational antibiotic (AB) usage poses a serious concern to third‐world countries because of poor surveillance, lack of information, and patients' propensity for self‐medication. Additionally, the unpredictability of the coronavirus disease 2019 (COVID‐19) pandemic promoted the abuse of ABs, which accelerated the prevalence of antibiotic resistance (ABR). The primary aim of this study was to assess the pattern of AB usage and irrational use of ABs‐related potential factors associated with ABR among the students and teachers of a leading public university of Bangladesh.
Methods
A cross‐sectional web‐based survey was conducted among the students and teachers (n = 783) of the selected university, from January 1 to February 28, 2022. Descriptive statistics, χ 2 test, and logistic regression analysis were employed to analyze the collected data.
Results
The regression analysis supported that male participants had a 34% lower experience of acquiring ABR than female respondents (adjusted odds ratio [AOR] = 0.66, 95% confidence interval [CI] = 0.448, 0.973; p = 0.036). The 1st/2nd‐year level students had more than two times higher experience with ABR than the master's or higher‐class students (AOR = 2.149, 95% CI = 1.047, 4.412; p = 0.037). The participants who took ABs for 4–6 days showed more than two times ABR experience than those who took ABs for above 10 days (AOR = 2.016, 95% CI = 1.016, 4.003; p = 0.045). Respondents who finished their AB medication (dose completion) had a 57% less chance of acquiring ABR than the participants who did not complete their dose.
Conclusion
This study found that irrational use of ABs is more prevalent among the youth and female participants. At this stage, there is an urgent need for comprehensive statutory AB control rules, as well as measures for appropriate information, education, and surveillance throughout different groups of Bangladesh.
Keywords: antimicrobial resistance, Bangladesh, irrational use of drugs, regression analysis
1. INTRODUCTION
Antibiotics (AB) belong life‐saving drugs that help people fighting various noxious pathogens. 1 However, the effectiveness of ABs is jeopardized by the fast escalation of antibiotic resistance (ABR) and the scarcity of new ABs with novel mechanism(s) of action. 2 In 2015, the worldwide mortality toll from ABR was around 700,000 people. 3 Furthermore, it is anticipated that the ABR‐related mortality rate would have risen to 10 million per year by 2050. 4
ABR, is a discernable fact, where infectious bacteria get comparatively stronger than earlier due to incomplete and irrational use of ABs. Millions of people die due to AB resistance every year in today's world and gradually the situation is going out of control as the infectious bacteria are no longer vulnerable to ABs which worked effectively in previously. 5 The irrational use of ABs is a driving factor of ABR. According to the World Health Organization (WHO), medications are used rationally when patients receive the proper medicines, for the relevant indications, in dosages that fit their own specific requirements, for an acceptable amount of time, at the lowest cost to them and society, and with appropriate information. When one or more of these factors are not achieved, irrational or needless use of drugs occurs. 6
People in developing countries like Bangladesh lack even the most basic understanding of resistance, ABs, and diseases. They seek symptomatic relief, to which doctors respond by giving ABs in the hopes of a rapid recovery. It eventually leads to higher healthcare costs, longer hospital stays, and abrupt or protracted health consequences, including considerable increases in morbidity and eventual death. 7 A recent global study conducted in 76 countries reported that there is a 65% increase in AB consumption and a 35% increase in AB consumption rate driven mostly by low and middle‐income countries (LMICs). 8 In addition, during the COVID‐19 pandemic in Bangladesh, an unprecedented surge in consuming ABs has been experienced because people got infected with mild to moderate symptoms‐ cough, fever, and lung infiltrate resemble bacterial pneumonia, and the doctors had nothing to do but prescribe ABs since a gray line exist between bacterial pneumonia and COVID‐19. 9
Moreover, the precise incidence of COVID‐19 with bacterial coinfection is unclear, thereby exacerbating the need for the overuse of ABs. 10 , 11 According to preliminary statistics, subsequent bacterial infections claimed the lives of 50% of COVID‐19 patients. 12 Subsequent data revealed minimal rates of secondary bacterial infections in COVID‐19 sickness, with a meta‐analysis of hospitalized COVID‐19 patients showing just 8.02% bacterial coinfection, while other investigations showed none. 10 , 13 , 14 Again, the spread of rumors about taking ABs for a fake cure from SARS‐CoV‐2 has added an additional complexity. In this bleak backdrop, the worldwide pandemic of COVID‐19 affects AB usage and enhances the selection pressure of effective antimicrobials to mitigate the extra imminent load of antimicrobial resistance throughout this pandemic. 15 , 16 , 17 Several studies, however, have found that a large number of broad‐spectrum antimicrobials are given and used by COVID‐19 patients. 18 , 19 Furthermore, antimicrobials remain available without a prescription in many LMICs. Consequently, as compared to other contemporary world nations, ordinary people in LMICs acquire and consume antimicrobials without a prescription for many self‐limiting ailments. As a result of the dread of COVID‐19, it is projected that individuals all over the world will have ingested a large number of antimicrobials as self‐medication. 20 , 21
Antibacterial resistance is now a global catastrophe that demands collective and wide‐collaborative efforts despite having a Global Action Plan on Antimicrobial Resistance formulated by the WHO in 2015. 22 Several studies pointed at the attitude, knowledge, and perception of medical professionals regarding the use of AB for its irrational use and prescription that ultimately lead to ABR, while different studies highlighted the carelessness of the patients and their sweet‐will to continue the course of medicine. It is found in several studies that gender is a key determinant of AB prescribing, and a few recent studies found that women consume 36%–40% more ABs than men, particularly in developed countries. 18 In addition, age, education level, knowledge of AB usage, medication style, and reasons for taking ABs have significant associations with ABR.
Moreover, it is necessarily evident that inappropriate AB prescribing by physicians along with the failure of patients to comply with physician's instructions on how to use ABs are responsible for irrational use of ABs. It is not the failure of patient every time, rather, it can be the prescribers who write wrong prescriptions. So, it is imperative to find out how and to whom ABs are prescribed to effective and safe reduction of AB consumption in Bangladesh. However, since ABR has a positive correlation with high morbidity and mortality, this study aimed to investigate the patterns of irrational use of AB and factors potentially associated with ABR among the students and teachers of a public university in Bangladesh.
2. METHODS
2.1. Study design
An online‐based cross‐sectional survey was conceptualized to be conducted for data collection among the students and teachers of a leading public university in Bangladesh. A Google form questionnaire was generated, which contained three sections: Section A included demographic information, Section B held AB use‐related questions, and Section C was designed to explore parameters associated with ABR among AB users. The questionnaire was primarily drafted in the English version, and then it was translated into the Bangla version by a bilingual expert with medical knowledge for a better understanding of the respondents. A forward and backward translation procedure was adopted during the validation of the translated questionnaire. 23 According to the WHO global report 2014 on surveillance of antimicrobial resistance, 24 the complete questionnaire was designed, where several variables associated with the irrational use of ABs and its relation to resistance were subsequently validated and adjusted in the Bangladesh context through the recently published findings. 25 , 26 , 27 It is noted that the work has been reported in line with the STROBE checklist, 28 which is available in Supporting Information.
2.2. Participants and sampling
The study included students and teachers from the university, and the target respondents were recruited by applying a systematic random sampling strategy. 29 The following standard and simplified formula suggested by Yamane was used to enumerate the sample size from a known population 30 :
where n and N denote the estimated sample size, and population size of the study area, respectively. Noted that d signifies the 5% tolerated standard error or level of precision. Hence, the population size of the selected study area was around 39,000 (approximately, male:female = 60:40), 31 and finally, the calculated sample size was 396. In this study, we collected 783 responses that might lead to more reliable and representative data for a better understanding of the study results.
2.3. Independent variables
We considered several sociodemographic characteristics as independent variables in this current study. The sociodemographic factors included gender (male, female), study background (science, humanities/arts, and business studies/commerce), various age groups (18–25 years, 26–50 years, and above 50 years), highest education levels (1st/2nd years, 3rd/4th/5th year, master's or higher), and occupation (student and teacher). To differentiate the AB users from nonusers, at first, there was a straight‐cut simple question like: “Have you taken any antibiotics within the last one year”? The response of the respondents was collected as “Yes/No.”
2.4. Irrational use of ABs and outcome variable
There were several factors to be defined as controls for irrational use of ABs, such as the use of nonprescribed ABs (through self‐medication, pre‐experience/old prescription, suggestion from others, and so on), incompletion of dosage regimen, unconcerned to taking physicians/pharmacists' counseling before discontinuation of the therapy, random use of ABs for a short duration, and undiagnosed reasons behind the treatment. Besides, the lack of cautiousness toward ABR or enough knowledge for the appropriate use of ABs was also considered another factor behind the irrational use of ABs. Finally, the outcome variable was set by inquiring a simple question “whether the participants experienced the inefficacy of antibiotics or antibiotic was not working against the intended disease.” The answer of the participants was recorded as “Yes = 1” versus “No = 0.”
2.5. Ethics and approval
The students and teachers of the selected university, who were 18 years or more aged and understood the aim, were requested to participate in this survey. A short description of the background of the study, protocol, usefulness, announcing of anonymity, and privacy was stated at the beginning of the study. Besides, it was made clear to all the potential respondents that participation in the survey was utterly voluntary‐based, and no reward or monetary exchange will not be done. All the protocols, guidelines, and ethical considerations of the World Medical Declaration of Helsinki (2018) were followed while conducting the survey work. Furthermore, informed consent was taken electronically from each participant before responding to this web‐based survey, and the collected data sheet was preserved in private and confidential by the first author of the manuscript. Finally, after reviewing the research protocol and procedures, the Ethical Review Committee of the Faculty of Biological Sciences, University of Dhaka, Bangladesh, approved and provided an ethical clearance with an approval number (ref. no. 112/Biol./Scs.).
2.6. Data collection
During a predetermined timeframe from January 1 to February 28, 2022, the survey was conducted for data collection through several popular social media platforms (Facebook, Messenger, WhatsApp, IMO, Email, and so on) among the university teachers and students. A total of 783 participants participated to the survey with complete responses. Then we had to exclude around 13% (102 out of 783) responses because they did not take any AB within the last year. Finally, we cured 681 collected data from the participants who used ABs within the previous year for statistical analysis.
2.7. Data analysis
Data analysis and the interpretation of the findings from the study were made by following the established guidelines outlined by Assel et al. 32 First, descriptive statistics for univariate analysis were conducted to tabulate several sociodemographic factors with their frequency and percentage distributions. Then, to assess the association of various sociodemographic variables and several parameters of irrational use of ABs with ABR, a χ 2 test for bivariate analysis has been conducted. Finally, logistic regression for multivariate analysis was run to determine the significant association of the irrational use of AB‐related potential variables associated with ABR after adjusting other factors. All the analyses have been conducted using software IBM SPSS (version 20). The two‐sided statistical significance level was less than 5% (p < 0.05) during all the statistical enumerations.
3. RESULTS
3.1. Demographic characteristics
According to Table 1, the majority of the study participants (66.07%) were males, while the rest were females. More than half of the respondents (62.11%) were between the ages of 18 and 25. In terms of educational background, Science was represented by around 72.68% of the participants. Almost 56% of the study participants were in their 1st or 2nd year of bachelor's studies (22.17% in the 1st or 2nd year and 33.03% in the 3rd/4th/5th year of bachelor's studies). A total of 87.22% of those who took part in this study were students.
Table 1.
Demographic characteristics (distributions and percentages) and common trends of antibiotic use (rational or irrational) among antibiotic users of the study participants (N = 681).
| Variables | Options | Number (N) | Percentage (%) |
|---|---|---|---|
| Gender | Male | 450 | 66.07 |
| Female | 231 | 33.92 | |
| Age (years) | 18–25 | 423 | 62.11 |
| 26–50 | 246 | 36.12 | |
| 50+ | 12 | 1.76 | |
| Study background | Science | 495 | 72.68 |
| Arts | 138 | 20.26 | |
| Commerce | 48 | 7.04 | |
| Highest education | 1st/2nd year | 151 | 22.17 |
| 3rd/4th/5th year | 225 | 33.03 | |
| Master's or higher | 305 | 44.78 | |
| Occupation | Student | 594 | 87.22 |
| Teacher | 87 | 12.77 | |
| Medication style | Doctor's prescription | 510 | 74.88 |
| Other ways | 171 | 25.12 | |
| Main reason for AB use | Fever, common cold, and cough | 342 | 50.22 |
| Dysentery/diarrhea/food poisoning | 69 | 10.13 | |
| Infection | 126 | 18.50 | |
| Abdominal/other pain | 45 | 6.60 | |
| Other reasons | 99 | 14.53 | |
| Duration of AB use (days) | 1–3 | 216 | 31.71 |
| 4–6 | 285 | 41.85 | |
| 7–10 | 93 | 13.65 | |
| Above 10 | 87 | 12.77 | |
| Completion of the dosage regimen | Yes | 480 | 70.48 |
| No | 201 | 29.51 | |
| Experience regarding AB was not working on you | Yes | 246 | 36.12 |
| No | 435 | 63.87 | |
| Lack of cautiousness about ABR | Yes | 405 | 59.47 |
| No | 276 | 40.52 |
Abbreviations: AB, antibiotic, ABR, World Health Organization antibiotic resistance.
Table 1 also describes common patterns of AB use and factors associated with irrational use tendency among AB users within the last 1 year. According to the study, 25.12% of the participants took medications without consulting with a doctor; they either self‐medicated themselves or took others' suggestions, or took it from their old prescription or previous experience. For over 50% of the participants, the reason for using those prescribed and unprescribed medications was mostly because of having fever, common cold, or cough. Almost 32%–42% of them used ABs for 1–6 days. A total of 70.48% of them completed the doses regimen of the AB. Among those 29.51% who did not complete their therapy, 56.72% of them did not complete it because as they had their sense of well‐being. Among those who discontinued their AB dosage, only 38.19% of them consulted with a physician or pharmacist before doing it. Among the study participants, 63.87% of them experienced that the AB was not working on them. Almost 59.47% of them had no cautiousness about ABR.
Table 2 exhibits, among those on which AB is not working, 62.2% were males, 67.1% were aged between 18 and 25 years, 75.6% were from a science background, almost 59% were doing their bachelor's and almost 89% of them were students. Lack of cautiousness also varied across different socio‐demographic factors. Of those who had a lack of cautiousness about ABR, among them, 66.7% were males, 65.9% were aged between 18 and 25 years, 88.9% were from a science background, 59.5% were in their bachelor's studies, and 87.4% were students.
Table 2.
Demographic analysis of two critical parameters related to antibiotic resistance.
| Variables | Options | Lack of cautiousness (N = 405; 59.47%) | No counseling from doctor/pharmacist (N = 267; 61.80%) | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Gender | Male | 270 | 66.7 | 66 | 40.0 |
| Female | 135 | 33.3 | 99 | 60.0 | |
| Age (years) | 18–25 | 267 | 65.9 | 111 | 67.3 |
| 26–50 | 135 | 33.3 | 54 | 32.7 | |
| 50+ | 3 | 0.7 | ‐ | ‐ | |
| Study background | Science | 360 | 88.9 | 120 | 72.7 |
| Arts | 30 | 7.4 | 36 | 21.8 | |
| Commerce | 15 | 3.7 | 9 | 5.5 | |
| Highest education | 1st/2nd year | 91 | 22.5 | 33 | 20.0 |
| 3rd/4th/5th year | 150 | 37.0 | 69 | 41.8 | |
| Master's or higher | 164 | 40.5 | 63 | 38.2 | |
| Occupation | Students | 354 | 87.4 | 153 | 92.7 |
| Teachers | 51 | 12.6 | 12 | 7.3 | |
Moreover, over 61% of the respondents did not take any counseling from doctor or pharmacist during the discontinuation of AB with no completion of dosage (Table 2). Among them, 40% were males, 67.3% were young (18–25 years) respondents, 72.7% of respondents were from a science background, 62% of the bachelor's students, and 92.7% were students, who discontinued medication taking without consulting any physician or pharmacist. According to Figure 1, a total of 22% were Macrolide users, 15% were nitroimidazole users, 14% were quinolone users, 13% were cephalosporin users, 12% were penicillin users, 4% were tetracycline users and rest 20% were users of other types of ABs.
Figure 1.
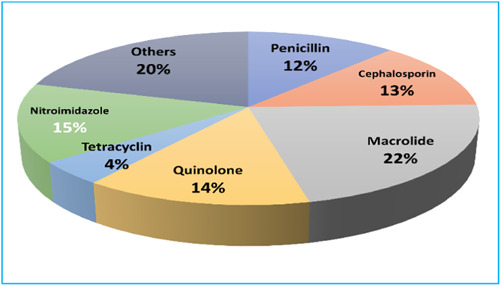
Frequency distributions of several most commonly used antibiotic groups among the study participants.
According to Figure 2, 74.88% of respondents took ABs according to doctor's prescription, but the rest were taking it based on self‐medication, suggestions or previous experience of taking ABs. The main reasons behind the discontinuation of ABs included sense of well‐being (56.72%), side effects (16.36%), high cost (14.9%), and carelessness (10.9%).
Figure 2.
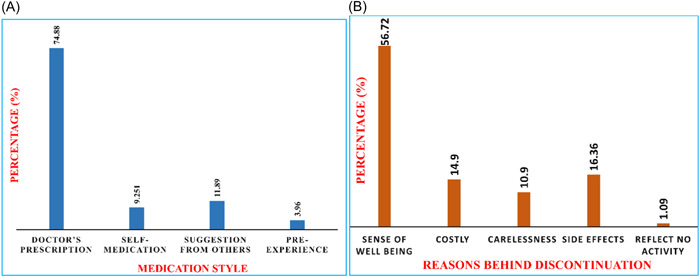
Frequency distributions of (A) medication style of antibiotic use, and (B) reasons behind the incompletion of the therapy among the study participants.
3.2. χ 2 analysis
In Table 3, the potential factors associated with ABR among the AB uses of the study area were analyzed. ABR was found in higher (39.0%) among 18–25 years old respondents than among the respondents beyond 25 years old, and the association between age and ABR was found to be significant (p < 0.05). ABR varied across education levels. The highest percentage (53.6%) was found among the 1st‐ and 2nd‐year students, and the association between education level and ABR was also significant (p < 0.001). Those who were using ABs upon doctor's prescription had the highest percentage (38.2%) resistance (Figure 3), and the medication style was found to be one of the significant (p < 0.048) factors of ABR.
Table 3.
χ 2 test for assessing several sociodemographic and irrational use of antibiotics related potential factors associated with antibiotic resistance among antibiotic users of the study participants (N = 681).
| Variables | Options | Experience on “antibiotics were not working” | ||||
|---|---|---|---|---|---|---|
| Yes | No | p‐value | ||||
| N | % | N | % | |||
| Gender | Male | 153 | 34.0 | 297 | 66.0 | 0.107 |
| Female | 93 | 40.3 | 138 | 59.7 | ||
| Study background | Science | 186 | 37.6 | 309 | 62.4 | 0.297 |
| Arts | 42 | 30.4 | 96 | 69.6 | ||
| Commerce | 18 | 37.5 | 30 | 62.5 | ||
| Age (years) | 18–25 | 165 | 39.0 | 258 | 61.0 | 0.045 |
| above 25 | 81 | 31.4 | 177 | 68.6 | ||
| Level of education | 1st/2nd | 81 | 53.6 | 70 | 46.4 | <0.001 |
| 3rd/4th/5th | 66 | 29.3 | 159 | 70.7 | ||
| Master's/higher | 99 | 32.5 | 206 | 67.5 | ||
| Occupation | Student | 219 | 36.9 | 375 | 63.1 | 0.290 |
| Teacher | 27 | 31.0 | 60 | 69.0 | ||
| Medication style | Doctor's prescription | 195 | 38.2 | 315 | 61.8 | 0.048 |
| Other ways | 51 | 29.8 | 120 | 70.2 | ||
| Main reason for AB use | Fever, common cold, and cough | 135 | 39.5 | 207 | 60.5 | <0.001 |
| Dysentery/diarrhea/food poisoning | 27 | 39.1 | 42 | 60.9 | ||
| Infection | 42 | 33.3 | 84 | 66.7 | ||
| Abdominal/other pain | 27 | 60.0 | 18 | 40.0 | ||
| Other purposes | 15 | 15.2 | 84 | 84.8 | ||
| Duration of AB use (days) | 1–3 | 75 | 34.7 | 141 | 65.3 | <0.001 |
| 4–6 | 126 | 44.2 | 159 | 55.8 | ||
| 7–10 | 27 | 29.0 | 66 | 71.0 | ||
| above 10 | 18 | 20.7 | 69 | 79.3 | ||
| Completion of the dosage regimen | Yes | 159 | 33.1 | 321 | 66.9 | 0.012 |
| No | 87 | 43.3 | 114 | 56.7 | ||
| Lack of cautiousness about ABR | Yes | 135 | 33.3 | 270 | 66.7 | 0.066 |
| No | 111 | 40.2 | 165 | 59.8 | ||
Note: Bold values are statistically significant.
Figure 3.
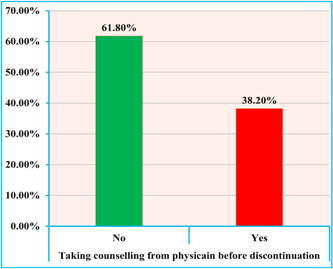
Percentage distributions of counseling (yes and no) received by the participants from physician.
A greater percentage (60.0%) of ABR was found who used AB for abdominal or other pain. The reason for using AB is also a potentially significant (p < 0.001) factor for its resistance. Duration of use was also significantly (p < 0.001) associated with resistance. The greatest percentage (44.2%) was found among those who used the AB for 4–6 days. The difference in dose completion was also significantly associated with ABR.
3.3. Logistic regression analysis
In an adjusted logistic regression model (Table 4), compared to females, the risk of developing ABR was 34% lower in males (adjusted odds ratio [AOR] = 0.66, 95% confidence interval [CI]: 0.448, 0.973). Age and educational/study background were not significantly associated with ABR. Compared to the respondents with master's and more highly educated respondents, 1st and 2nd‐year students were at significantly 2.15 times (AOR = 2.149, 95% CI: 1.047, 4.412) higher risk of developing ABR. In comparison to the reference group, respondents who followed the doctor's prescription were 1.973 times higher risk (AOR = 1.973, 95% CI: 1.191, 3.267) of developing ABR. Compared to those who had used AB for more than 10 days, 2.016 times higher (AOR = 2.016, 95% CI: 1.016, 4.003) chances of ABR were observed among those who took the dosage for 4–6 days. Respondents who used ABs for defined causes (i.e., fever, cold, cough, diarrhea, food poisoning, infection, abdominal) were at 2.09–5.5 times significantly higher risk of developing ABR than their reference group of people. Respondents who completed their AB dosage were significantly at 57% lower risk of developing ABR than the participants who did not finish their AB dosage.
Table 4.
Logistic regression analysis for finding several sociodemographic and irrational use of antibiotics related potential factors associated with ABR among antibiotic users of the study participants (N = 681).
| Variables | Categories | AOR | p‐value | 95% CI | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Gender | Male versus femaleR | 0.660 | 0.036 | 0.448 | 0.973 |
| Group/study background | Science versus commerceR | 1.226 | 0.558 | 0.620 | 2.423 |
| Arts versus commerceR | 0.856 | 0.678 | 0.411 | 1.783 | |
| Age | 18–25 versus above 25R | 1.023 | 0.950 | 0.508 | 2.060 |
| Level of education | 1st/2nd year versus MS and higherR | 2.149 | 0.037 | 1.047 | 4.412 |
| 3rd/4th/5th year versus MS and higherR | 0.673 | 0.276 | 0.331 | 1.371 | |
| Occupation | Student versus teacherR | 1.249 | 0.453 | 0.698 | 2.236 |
| Prescription practice | From doctor versus otherwaysR | 1.973 | 0.008 | 1.191 | 3.267 |
| Reason for administration of antibiotics | Fever, common cold, and cough versus othersR | 3.286 | 0.001 | 1.647 | 6.556 |
| Dysentery/diarrhea/food poisoning versus othersR | 4.209 | 0.001 | 1.859 | 9.530 | |
| Infection versus othersR | 2.095 | 0.044 | 1.020 | 4.301 | |
| Abdominal/other pain versus othersR | 5.580 | <0.001 | 2.247 | 13.856 | |
| Duration of antibiotics therapy (days) | 1–3 versus above 10R | 0.975 | 0.948 | 0.462 | 2.058 |
| 4–6 versus above 10R | 2.016 | 0.045 | 1.016 | 4.003 | |
| 7–10 versus above 10R | 1.656 | 0.193 | 0.775 | 3.538 | |
| Dose completion | Yes versus NoR | 0.426 | 0.001 | 0.259 | 0.703 |
| Having enough knowledge/cautiousness | Yes versus NoR | 0.712 | 0.113 | 0.468 | 1.084 |
| Constant | 0.164 | 0.004 | |||
Note: Bold values are statistically significant. Superscript R means reference group.
4. DISCUSSION
In this study, we evaluated different factors, including age, sex, education level, medication style, and causes of taking ABs and their relation to ABR. According to the study findings, gender, age, educational qualification, prescription pattern, and dosage duration were found to be significant predictors of ABR among the study population. According to the study findings, the primary reasons behind consuming ABs were cough, cold, dysentery, diarrhea, food poisoning, infection, abdominal and other pain.
In this study, this tendency of consuming unregulated ABs was found to be particularly more prevalent among young age people (18–25 years old). AB consumption also varied significantly across genders. According to the study, almost one‐third of the males and two‐fifth of the females had experienced ABR. We found females were more at risk of developing ABR. The study findings were also in line with other studies. 33 Infection patterns, frequent consultation with doctors for health issues, and social biases, might be the reasons behind their excessive use of ABs and, thereby development of ABR among women. 34
The educational qualification also affected ABR. More than half of the junior‐year students were found to be AB‐resistant. With respect to the MS student, 1st and 2nd year students were two times more likely to develop ABR. People with education are more cautious about taking medication, so, that might play a role in less development of ABR for the higher class respondents. 35 According to other studies with similar results, they defined that knowledge of ABR is often derived from higher education or experience and cannot be obtained through basic education even though the young community is not even interested to learn about disease‐related topics. 36
The duration of the dosage was also found to be the potential determiner of resistance development. About 35%–45% of those who used the AB regime for 1–6 days developed ABR. In comparison to those who used ABs for more than 10 days, those who used ABs for 4–6 days were two times more likely to develop resistance. The finding is in contrast with other findings, where shorter dosages were found to be protective of resistance. 37 These can be the underlying reasons for the misuse or overuse of ABs and, thereby, resistance occurs. According to the WHO, early termination of ABs consumption of insufficient quantum of drug favors the bacteria strain's general intrinsic resistance. 35 , 38 However, in another report, WHO said that shorter AB treatment increases the likelihood of being completed correctly, minimizes the side effects, and is more like to be cost‐effective. Additionally, shorter treatment reduces bacterial exposure to ABs, slowing down ABR. 39
Those who took medication for fever, common cold, and cough, dysentery/diarrhea/food poisoning, infection, abdominal/other pain were 2–5 times more likely to develop ABR. This can be because they lack a common understanding whether or not that condition can be treated with AB medications. For instance, even in viral flue people take AB therapy. These inappropriate uses of medications lead them to ABR. 35
Little research has been done on the factors underlying for AB use in the community, but this study can play a vital role in showing what drives people more to overuse ABs. It will help the policymakers to plan proper interventions to resist the uncontrolled use of ABs. There are several limitations of this study. As this is a cross‐sectional study, ABR was not properly analyzed. Which particular type of people were resistant was also not identified. As they self‐reported the resistance status, there is a possibility of social desirability bias. However, more attention urgently should be given to winning the battle against ABR. Further research on strain‐specific resistance is required. As the increased risk of ABs usage can lead to ABR, to control this, healthcare professionals should play a vital role. They can disseminate knowledge of how to prevent ABR, and what factors can contribute to ABR among the general masses. They can promote the necessity of sufficient adherence to AB dosage. 35
4.1. Practical implications
The research demonstrating that ABs should not be sold without a prescription reinforces the necessity for a rethinking in practice. It is critical for public health to change procedures around the irrational use as well as the non‐prescriptive sale of ABs. It is critical to understand pharmacists' and health professionals' attitudes and beliefs about practice, as well as the impediments to achieving best practice. Additionally, it is critical to understand the attitudes and ideas of consumers regarding self‐medication, particularly with ABs.
This study found that specific AB education for university students can increase their rational use of ABs; however, knowledge did often not relate to behavior. Moreover, this study recommends the implementation of patient education and awareness programs among the students and common people, using short videos, printed handouts, and other pedagogical tools, about AB usage and the adversity of self‐medication, indiscriminate use of medicines, or not completion of the course. Reminder devices and modification of medication packaging should be included in the intervention planning. Since resistant strains are barely confined to national borders, any region like Bangladesh with a high prevalence of resistance can serve as a reservoir. We propose that strong precautions must be taken against irrational AB usage, and the selling of ABs without a prescription be prohibited.
4.2. Future research
This study suggests that additional research should be conducted on the irrational use of ABs in a wider population, such as across many regions, or the entire country. Future research may focus on both rural and urban locations, and patients should be involved as much as possible to better understand this issue. Seasonal fluctuations in illness should also be considered, as they may have influenced disease patterns as well as AB usage. The reason for the changes in AB usage might also be studied to have a better understanding of the problem. This study also highlights the need for a comparative assessment of the ABR pandemics before and after COVID‐19, as well as the factors that contribute to them.
4.3. Limitations
The study's primary limitation was recall bias. Because many participants were unable to recall or omitted facts about their AB use histories, the study's accuracy was substantially impacted by their memories. Additionally, while the sample was selected using a method called systematic random sampling, there is a possibility that some selection bias occurred. This potential bias could restrict the applicability of the findings to the entire population. The sample size was small, and seasonal variations in disease was excluded due to the possibility that it influenced disease patterns as well as AB use. Despite such limitations, our findings have the potential to play a critical role in the regulation of AB distribution, prescription, and sale in Bangladesh by identifying existing prescription medicines and their consumption pattern.
5. CONCLUSIONS
In conclusion, this study found a significant percentage of improper AB usage with little or no awareness, as well as a high prevalence of self‐medication among Bangladeshis, particularly university students. This study establishes a significant relationship between age, education level, and resistance. Because irrational AB use is a growing serious issue of concern and it leads to ABR, several creative attempts and approaches are being introduced around the world to address this global health problem. As a result, there is an urgent need for effective statutory AB control regulations to limit the availability of ABs to the public, as well as measures for information, education, and surveillance throughout the country's diverse communities.
AUTHOR CONTRIBUTIONS
Md. Jamal Hossain: Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; software; supervision; validation; visualization; writing—original draft; writing—review and editing. Nasrin Jabin: Resources; software; validation; visualization; writing—original draft. Foyez Ahmmed: Data curation; formal analysis; investigation; methodology; software; validation; visualization. Arifa Sultana: Investigation; methodology; software; validation; visualization; writing—original draft. S. M. Abdur Rahman: Investigation; methodology; project administration; supervision; validation; visualization. Md. Rabiul Islam: Investigation; methodology; resources; validation; visualization; writing—review and editing.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
Ethical Review Committee of the Faculty of Biological Sciences, University of Dhaka, Bangladesh, approved the study protocol and provided an ethical approval number (ref. no. 112/Biol./Scs.).
INFORMED CONSENT
Informed consent from all the participants were taken.
TRANSPARENCY STATEMENT
The lead author Md. Jamal Hossain affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
The research was conducted by self‐funding.
Hossain MJ, Jabin N, Ahmmed F, Sultana A, Abdur Rahman SM, Islam MR. Irrational use of antibiotics and factors associated with antibiotic resistance: findings from a cross‐sectional study in Bangladesh. Health Sci Rep. 2023;6:e1465. 10.1002/hsr2.1465
DATA AVAILABILITY STATEMENT
All data involved to endorse the findings of this research were included in the manuscript. Further raw data is available from the corresponding author upon reasonable request. All authors have read and approved the final version of the manuscript and the corresponding author had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1. Sengupta S, Chattopadhyay MK, Grossart HP. The multifaceted roles of antibiotics and antibiotic resistance in nature. Front Microbiol. 2013;4:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Uddin TM, Chakraborty AJ, Khusro A, et al. Antibiotic resistance in microbes: history, mechanisms, therapeutic strategies and future prospects. J Infect Public Health. 2021;14(12):1750‐1766. [DOI] [PubMed] [Google Scholar]
- 3. Saha SK. Factors influencing clinician's antibiotic prescribing behaviors (APB) in Bangladesh: an in‐depth review using COMB model. Open Access J Transl Med Res. 2017;1(4):00019. [Google Scholar]
- 4. Dutta S, Haque M. COVID‐19: questions of antimicrobial resistance. Bangladesh Journal of Medical Science. 2021;20(2):221‐227. [Google Scholar]
- 5. Blair JMA, Webber MA, Baylay AJ, Ogbolu DO, Piddock LJV. Molecular mechanisms of antibiotic resistance. Nat Rev Microbiol. 2015;13(1):42‐51. 10.1038/nrmicro3380 [DOI] [PubMed] [Google Scholar]
- 6. WHO . The world medicines situation report 2011. Published online 2011.
- 7. Mannan A, Shohel M, Rajia S, Mahmud NU, Kabir S, Hasan I. A cross sectional study on antibiotic resistance pattern of Salmonella typhi clinical isolates from Bangladesh. Asian Pac J Trop Biomed. 2014;4(4):306‐311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Klein EY, Van Boeckel TP, Martinez EM, et al. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci USA . 2018;115(15):E3463‐E3470. 10.1073/pnas.1717295115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Parveen M, Molla MMA, Yeasmin M, Nafisa T, Barna AA, Ghosh AK. Evidences on irrational anti‐microbial prescribing and consumption among COVID‐19 positive patients and possible mitigation strategies: a descriptive cross sectional study. Bangladesh J Infect Dis. 2020;7(October):S3‐S7. 10.3329/bjid.v7i00.50155 [DOI] [Google Scholar]
- 10. Rawson TM, Moore LSP, Castro‐Sanchez E, et al. COVID‐19 and the potential long‐term impact on antimicrobial resistance. J Antimicrob Chemother. 2020;75(7):1681‐1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Morens DM, Taubenberger JK, Fauci AS. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis. 2008;198(7):962‐970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. The lancet. 2020;395(10229):1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Clancy CJ, Nguyen MH. Coronavirus disease 2019, superinfections, and antimicrobial development: what can we expect? Clin Infect Dis. 2020;71(10):2736‐2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bhargava B. Treatment guidelines for antimicrobial use in common syndromes. Published online 2019.
- 15. Dunachie SJ, Day NP, Dolecek C. The challenges of estimating the human global burden of disease of antimicrobial resistant bacteria. Curr Opin Microbiol. 2020;57:95‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guisado‐Gil A, Infante‐Domínguez C, Peñalva G, et al. Impact of the COVID‐19 pandemic on antimicrobial consumption and hospital‐acquired candidemia and multidrug‐resistant bloodstream infections. Antibiotics. 2020;9(11):816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Getahun H, Smith I, Trivedi K, Paulin S, Balkhy HH. Tackling antimicrobial resistance in the COVID‐19 pandemic. Bull World Health Organ. 2020;98(7):442‐442A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schröder W, Sommer H, Gladstone BP, et al. Gender differences in antibiotic prescribing in the community: a systematic review and meta‐analysis. J Antimicrob Chemother. 2016;71(7):1800‐1806. 10.1093/jac/dkw054 [DOI] [PubMed] [Google Scholar]
- 19. Clancy CJ, Buehrle DJ, Nguyen MH. PRO: the COVID‐19 pandemic will result in increased antimicrobial resistance rates. JAC‐Antimicrobial Resistance. 2020;2(3):dlaa049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sartelli M, C. Hardcastle T, Catena F, et al. Antibiotic use in low and middle‐income countries and the challenges of antimicrobial resistance in surgery. Antibiotics. 2020;9(8):497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jamil S, Bari QI, Akhter A, et al. Self‐medication practice and its potential determinants among Riverine‐Island's people in Sirajganj, Bangladesh: a cross‐sectional study. Bangladesh Pharm J. 2023;26(1):79‐88. [Google Scholar]
- 22. Nisabwe L, Brice H, Umuhire MC, et al. Knowledge and attitudes towards antibiotic use and resistance among undergraduate healthcare students at University of Rwanda. J Pharm Policy Pract. 2020;13(1):7. 10.1186/s40545-020-00207-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Koller M, Aaronson NK, Blazeby J, et al. Translation procedures for standardised quality of life questionnaires: the European Organisation for Research and Treatment of cancer (EORTC) approach. Eur J Cancer. 2007;43(12):1810‐1820. [DOI] [PubMed] [Google Scholar]
- 24. WHO . Antimicrobial Resistance. Global Report on Surveillance. World Health Organization. 2014:383‐394.
- 25. Biswas M, Roy MN, Manik MI, et al. Self medicated antibiotics in Bangladesh: a cross‐sectional health survey conducted in the Rajshahi city. BMC Public Health. 2014;14(1):847. 10.1186/1471-2458-14-847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Biswas M, Roy D, Tajmim A, et al. Prescription antibiotics for outpatients in Bangladesh: a cross‐sectional health survey conducted in three cities. Ann Clin Microbiol Antimicrob. 2014;13(1):15. 10.1186/1476-0711-13-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Islam MS, Sikdar KYK, Hossain AMA, Faroque A. Study on the pattern of antibiotic use including the resistance episodes in Bangladesh. Dhaka Univ J Pharmaceut Sci. 2019;18(2):135‐143. 10.3329/dujps.v18i2.43255 [DOI] [Google Scholar]
- 28. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. The Lancet. 2007;370(9596):1453‐1457. [DOI] [PubMed] [Google Scholar]
- 29. Hossain MJ, Kuddus MR, Rahman SMA. Knowledge, attitudes, and behavioral responses toward COVID‐19 during early phase in Bangladesh: a questionnaire‐based study. Asia Pacific J Public Health. 2020;33:141‐144. 10.1177/1010539520977328 [DOI] [PubMed] [Google Scholar]
- 30. Yamane Taro. Statistics, An Introductory Analysis. 2nd ed. Harper and Row; 1967. [Google Scholar]
- 31. D. Y. Patil University . University at a Glance. D. Y. Patil University. Published online 2015.
- 32. Assel M, Sjoberg D, Elders A, et al. Guidelines for reporting of statistics for clinical research in urology. BJU Int. 2019;123(3):401‐410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lee DS, Choe HS, Kim HY, et al. Role of age and sex in determining antibiotic resistance in febrile urinary tract infections. Int J Infect Dis. 2016;51:89‐96. 10.1016/j.ijid.2016.08.015 [DOI] [PubMed] [Google Scholar]
- 34. Smith DRM, Dolk FCK, Smieszek T, Robotham JV, Pouwels KB. Understanding the gender gap in antibiotic prescribing: a cross‐sectional analysis of English primary care. BMJ Open. 2018;8:e020203. 10.1136/bmjopen-2017-020203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Effah CY, Amoah AN, Liu H. A population‐based survey on knowledge, attitude and awareness of the general public on antibiotic use and resistance. Antimicrobial Resistance Infect Control. 2020;9:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Waaseth M, Adan A, Røen IL, et al. Knowledge of antibiotics and antibiotic resistance among Norwegian pharmacy customers—a cross‐sectional study. BMC Public Health. 2019;19(1):66. 10.1186/s12889-019-6409-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Canet JJ, Garau J. Importance of dose and duration of β‐lactam therapy in nasopharyngeal colonization with resistant pneumococci. J Antimicrob Chemother. 2002;50:39‐44. 10.1093/jac/dkf507 [DOI] [PubMed] [Google Scholar]
- 38. Kardas P, Devine S, Golembesky A, Roberts C. A systematic review and meta‐analysis of misuse of antibiotic therapies in the community. Int J Antimicrob Ag. 2005;26(2005):106‐113. 10.1016/j.ijantimicag.2005.04.017 [DOI] [PubMed] [Google Scholar]
- 39. WHO . 2020. Antimicrobial resistance: Does stopping a course of antibiotics early lead to antibiotic resistance ? Accessed January 1, 2023. Available from: https://www.who.int/news-room/questions-and-answers/item/antimicrobial-resistance-does-stopping-a-course-of-antibiotics-early-lead-to-antibiotic-resistance
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
All data involved to endorse the findings of this research were included in the manuscript. Further raw data is available from the corresponding author upon reasonable request. All authors have read and approved the final version of the manuscript and the corresponding author had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.


