Abstract
Background:
Among patients with cirrhosis, it remains unclear whether there are racial/ethnic differences in cirrhosis complications and mortality. We examined the associations between race/ethnicity and risk for hepatocellular carcinoma (HCC), cirrhosis decompensation, and all-cause mortality overall and by cirrhosis etiology.
Methods:
US Veterans diagnosed with cirrhosis from 2001 to 2014 (n = 120,992), due to hepatitis C virus (HCV; n = 55,814), alcohol-associated liver disease (ALD; n = 36,323), hepatitis B virus (HBV; n = 1,972), nonalcoholic fatty liver disease (NAFLD; n = 17,789), or other (n = 9,094), were followed through 2020 for incident HCC (n = 10,242), cirrhosis decompensation (n = 27,887), and mortality (n = 81,441). Multivariable Cox proportional hazards regression was used to estimate adjusted hazard ratios (aHR) and 95% confidence intervals (CI).
Results:
Compared with non-Hispanic White patients, Hispanic patients had higher risk for HCC overall (aHR, 1.32; 95% CI, 1.24–1.41) and by cirrhosis etiology, particularly for ALD- (aHR, 1.63; 95% CI, 1.42–1.87) and NAFLD-cirrhosis (aHR, 1.76; 95% CI, 1.41–2.20), whereas non-Hispanic Black patients had lower HCC risk in ALD- (aHR, 0.79; 95% CI, 0.63–0.98) and NAFLD-cirrhosis (aHR, 0.54; 95% CI, 0.33–0.89). Asian patients had higher HCC risk (aHR, 1.70; 95% CI, 1.29–2.23), driven by HCV- and HBV-cirrhosis. Non-Hispanic Black patients had lower risk for cirrhosis decompensation overall (aHR, 0.71; 95% CI, 0.68–0.74) and by cirrhosis etiology. There was lower risk for mortality among all other racial/ethnic groups compared with non-Hispanic White patients.
Conclusions:
Race/ethnicity is an important predictor for risk of developing HCC, decompensation, and mortality.
Impact:
Future research should examine factors underlying these racial/ethnic differences to inform prevention, screening, and treatment for patients with cirrhosis.
Introduction
Liver disease is a leading cause of morbidity and mortality worldwide and in the US (1–4). Mortality from cirrhosis and hepatocellular carcinoma (HCC) has increased over the past several decades (2, 5–7). The prevalence of common liver diseases substantially varies by race and ethnicity in the US. For example, hepatitis C virus (HCV) infection is more common among non-Hispanic Black (2.76%) compared with non-Hispanic White persons (1.20%; ref. 8). Chronic hepatitis B virus (HBV) infection is more prevalent among Asian persons (2.74%) compared with those who are not Asian or Black (0.15%; ref. 9). The prevalence of nonalcoholic fatty liver disease (NAFLD) is more common among Hispanic persons (22.9%) and less common among Black persons (12.0%) compared with White persons (14.4%; ref. 10).
Furthermore, marked racial/ethnic disparities in cirrhosis- and HCC-related prevalence, incidence, and mortality have been observed. The prevalence of cirrhosis is higher in non-Hispanic Black compared with non-Hispanic White persons regardless of HCV status (HCV-positive: 9% in Black persons vs. 7.7% in White persons; HCV-negative: 0.25% in Black persons vs. 0.09% in White persons; ref. 11). Higher HCC incidence rates have been observed in Asian (18.6 cases per 100,000 population), followed by Black (15.7 per 100,000), Hispanic (11.8 per 100,000), and non‐Hispanic White persons (7.0 per 100,000; ref. 12). Non-Hispanic White persons are at increased risk for cirrhosis-related mortality (24.61 per 100,000) compared with Hispanic (20.34 per 100,000), non-Hispanic Black (15.86 per 100,000), and non-Hispanic Asian persons (7.00 per 100,000; ref. 6). HCC-related mortality is higher in non-Hispanic Black persons (5.12 per 100,000) compared with non-Hispanic Asian (4.31 per 100,000), non-Hispanic White (3.87 per 100,000), and Hispanic persons (3.64 per 100,000; ref. 6).
However, among patients with established cirrhosis, it remains unclear whether the risk of HCC, cirrhosis decompensation (i.e., variceal bleeding, ascites, or hepatic encephalopathy), and mortality varies by race/ethnicity. Furthermore, it is important to consider underlying cirrhosis etiology, such as HCV, HBV, alcohol-associated liver disease (ALD), and NAFLD, which may confer differential risks for cirrhosis complications (13, 14). The objective of this study was to examine the associations between race/ethnicity and the risk of HCC, cirrhosis decompensation, and all-cause mortality in a cohort of US Veterans with cirrhosis, overall and according to cirrhosis etiology.
Materials and Methods
Study population
The Veterans Affairs (VA) health care system is the largest integrated health care system in the US, annually providing care to over 9 million enrolled Veterans through 170 VA Medical Centers and 1,074 outpatient clinics (15). We used data from the VA Corporate Data Warehouse (CDW), a national continually updated repository of electronic health records (EHR; ref. 16). Using the CDW, information on patient demographics, inpatient and outpatient visits, problem lists, procedures, vital signs, diagnostic tests, laboratory tests, and pharmacy prescriptions was extracted.
We created a cohort of all patients diagnosed with cirrhosis for the first time from January 1, 2001 to December 31, 2014 (n = 136,241) and retrospectively followed these patients from the date 90 days after cirrhosis diagnosis until March 31, 2020 for the development of HCC, cirrhosis decompensation, and/or death. Data extended backward to October 1999 to allow complete ascertainment of baseline characteristics. The following exclusions were applied: Death (n = 12,602) or liver transplantation (n = 353) within 90 days of cirrhosis diagnosis, <90 days of follow-up (n = 826), achieved sustained virologic response (SVR) to HCV within 90 days of cirrhosis diagnosis (n = 720), or follow-up began after liver transplantation (n = 748). Additional exclusions were separately applied for the analyses examining HCC [history of HCC before or within 90 days of cirrhosis diagnosis (n = 4,894)] and cirrhosis decompensation [history of decompensated cirrhosis before or within 90 days of cirrhosis diagnosis (n = 9,054)]. This study was approved by the Institutional Review Board of the VA Puget Sound Health Care System; the requirement to obtain informed consent was waived.
Definition of cirrhosis
Diagnosis of cirrhosis was defined as an associated International Classification of Diseases, Ninth Revision (ICD-9) code recorded at least twice in any inpatient or outpatient encounter, or a diagnosis of cirrhosis recorded once together with at least one complication of cirrhosis (varices without bleeding, varices with bleeding, ascites, encephalopathy, spontaneous bacterial peritonitis, hepatorenal syndrome, and hepatopulmonary syndrome; Supplementary Table S1). ICD-10 codes were adopted beginning in October, 2015. This case definition for cirrhosis has been validated and used in previous VA population-based studies (16, 17) and is associated with a 97% positive predictive value compared with chart review (16).
Among patients with cirrhosis, five mutually exclusive cirrhosis etiologies were defined (16, 17): (i) HCV: positive serum HCV RNA irrespective of any additional etiologies; (ii): HBV: ever positive for hepatitis B surface antigen (HBsAg) or viral load (HBV DNA; patients co-infected with HCV and HBV were categorized as HCV only; (iii): ALD: ICD-9 codes for alcohol use disorders in the absence of serological markers of HCV or HBV infection and without ICD-9 codes for hemochromatosis, primary biliary cirrhosis, primary sclerosing cholangitis, and autoimmune hepatitis (Supplementary Table S2; (iv): NAFLD: ICD-9 codes for diabetes (recorded at least twice) or a body mass index (BMI) ≥ 30 kg/m2 before cirrhosis diagnosis in the absence of HCV, HBV, ALD, and ICD-9 codes for hemochromatosis, primary biliary cirrhosis, primary sclerosing cholangitis, and autoimmune hepatitis (this definition reflects the diagnostic process used in clinical practice, incorporating known NAFLD risk factors, including diabetes and obesity, and exclusion of other etiologies, because NAFLD-related cirrhosis is not associated with unique histological, radiological, or serological features); (v) other: all other patients without HCV, HBV, ALD, and NAFLD.
Determination of race and ethnicity
Self-reported race and ethnicity documented in the EHR was used to categorize patients as non-Hispanic White, non-Hispanic Black, Hispanic, American Indian/Alaska Native (AI/AN), Asian, or Pacific Islander/Native Hawaiian (PI/NH). Race or ethnicity was missing in 11.7% of patients, which included those refusing to declare their race/ethnicity or had unknown/mixed race/ethnicity and did not identify a specific racial or ethnic group. Thus, we analyzed a separate race/ethnicity category for missing/unknown/declined to disclose.
Baseline characteristics
We ascertained baseline information on age, sex, and BMI (recorded within 6 months before cirrhosis diagnosis; ref. 16). Presence of type 2 diabetes mellitus, alcohol use disorders, substance use disorders, and human immunodeficiency virus (HIV) infection was based on ICD-9 codes recorded at least twice before cirrhosis diagnosis in any inpatient or outpatient encounter (Supplementary Table S2). We ascertained the following laboratory tests within 90 days of cirrhosis diagnosis: Albumin, aspartate aminotransferase to alanine aminotransferase ratio (AST/√ALT), bilirubin, creatinine, hemoglobin, platelet count, Model for End-Stage Liver Disease (MELD) score, Fibrosis-4 (FIB-4) score, and international normalized ratio (INR). Using ICD-9 codes, we determined the Charlson Comorbidity Index (CCI) as an estimate of overall comorbidity burden. Information on HCV genotype was also ascertained.
Low socioeconomic status (SES) was defined as having an ICD-9 code for low income or poverty developed by the VA Information Resource Center (ref. 18; Supplementary Table S2), assignment to Priority Group 5 (19, 20), or an Area Deprivation Index (ADI) score ≤ 15 (21, 22). For SES based on ICD codes, we used information at any time throughout follow-up; for SES based on Priority Group 5 and ADI, we used information in the year closest in time to cirrhosis diagnosis (and before cirrhosis diagnosis if available). Priority Groups were assigned to Veterans to determine enrollment eligibility for VA health care services based on level of service-connected disability and income (19). Priority Group 5, which has been used as an indicator of low SES (20), was defined as non-service-connected Veterans and non-compensable service-connected Veterans rated 0% disabled by the VA with an annual income and/or net worth below the VA national income threshold and the income threshold for their residential location, Veterans receiving VA pension benefits, or Veterans eligible for Medicaid programs (19, 20). The ADI is a measure of neighborhood-level SES disadvantage that includes factors for income, education, employment, and housing quality (22). Using geographic information on each patient's residential locations from the VA Planning Systems Support Group Enrollee Files, we linked each patient's census block group (or census tract or county if the census block group was unavailable) closest in time to cirrhosis diagnosis to determine the ADI score.
Outcome ascertainment
Patients were followed starting 90 days after cirrhosis diagnosis until March 31, 2020 to ascertain the following outcomes: HCC, cirrhosis decompensation, liver transplantation, and death. These outcomes were defined using ICD-9 or ICD-10 codes recorded at least twice during follow-up (Supplementary Table S1). This HCC case definition is associated with 84%–94% positive predictive values compared with chart review (23, 24). Cirrhosis decompensation was defined as the new development of at least one of the following conditions: Bleeding gastroesophageal varices, ascites, or hepatic encephalopathy (25). A single record was required for bleeding gastroesophageal varices (rather than at least two) as patients may only experience a single bleeding episode if it results in death.
Statistical analysis
Cox proportional hazards regression was used to estimate multivariable adjusted hazard ratios (aHR) and 95% confidence intervals (CI) for the associations between race/ethnicity and risk of HCC, cirrhosis decompensation, and death. Results for patients with missing/unknown/declined to disclose race/ethnicity were also presented. All models were stratified by VA medical center. All models were adjusted for the following potential confounders: age, sex, BMI, diabetes, cirrhosis etiology, history of HCC (for outcomes other than HCC), history of decompensated cirrhosis (for outcomes other than decompensated cirrhosis), CCI, alcohol use disorders, substance use disorders, albumin, bilirubin, creatinine, platelet count, AST/√ALT ratio, and SES. Results were presented for all patients with cirrhosis (overall) and separately by cirrhosis etiology (HCV, HBV, ALD, NAFLD, and other). Follow-up began 90 days after the date of cirrhosis diagnosis (to exclude prevalent outcomes) and extended until March 31, 2020. Patients with HCV who were cured as a result of antiviral treatment were censored at the date at which SVR was achieved.
Separate analyses were performed for HCC, cirrhosis decompensation, mortality, and liver transplantation, each with its own censoring. Patients with a history of HCC (active or previously treated) at inception into the cohort were excluded from the HCC analysis. Patients with a history of all three cirrhosis decompensations (bleeding gastroesophageal varices, ascites, and hepatic encephalopathy) at inception into the cohort were excluded from the cirrhosis decompensation analysis. Patients lacking at least one decompensation were included in this analysis and followed for the development of a new decompensation (e.g., a patient with ascites as their only decompensation would be followed for the development of bleeding gastroesophageal varices and/or hepatic encephalopathy, either of which would qualify as new cirrhosis decompensation). All patients were included in the analyses for mortality and liver transplantation.
Mortality is high in patients with cirrhosis and death can be a competing risk for HCC, where patients who are more likely to develop HCC may also be more likely to die beforehand, thus masking the development of HCC. Liver transplantation, although less common than death, can also be a competing risk for HCC. For this reason, we additionally performed competing risks proportional hazards regression to estimate sub-hazard ratios for HCC risk while simultaneously accounting for the competing risk of death or liver transplantation. All statistical tests were two-sided and P < 0.05 was considered statistically significant. All statistical analyses were conducted using Stata 15.1 (Stata Corp.).
Data availability
The data used in this research belong to the Veterans Health Administration. Although the data can be accessed by VA researchers with requisite approvals, they are not publicly available. However, the study methodology has been described to facilitate reproduction of the study results by VA researchers with access to the CDW.
Results
Population characteristics
Table 1 shows baseline characteristics for the 120,992 patients with cirrhosis included in this cohort. Patients were on average 60.3 years (±9.4) at cirrhosis diagnosis, predominantly male (97.5%), with an average BMI of 28.8 kg/m2 (±5.9) and/or an average CCI score of 4.5 (±2.1). The most common cirrhosis etiology was HCV (46.1%), followed by ALD (30.0%), NAFLD (14.7%), other (7.5%), and HBV (1.6%). Approximately 31.6% of patients had diabetes, 40.5% had a history of alcohol use disorders, 20.4% had a history of substance use disorders, and 56.2% were categorized as low SES. Most patients were non-Hispanic White (63.1%), followed by non-Hispanic Black (15.5%), Hispanic (7.6%), AI/AN (1.0%), Asian (0.3%), and PI/NH (0.9%). Patients with missing/unknown/declined to disclose race/ethnicity were similar to those with available race/ethnicity data.
Table 1.
Baseline characteristics of a cohort of 120,992 patients with cirrhosis at the time of cirrhosis diagnosis (2001–2014) overall and by race/ethnicity.
| Race/ethnicity | ||||||||
|---|---|---|---|---|---|---|---|---|
| Overall | Non-Hispanic White | Non-Hispanic Black | Hispanic | American Indian/Alaska Native (AI/AN) | Asian | Pacific Islander/Native Hawaiian (PI/NH) | Missing/unknown/declined to disclose | |
| Variable | n = 120,992 | n = 76,338 | n = 18,759 | n = 9,135 | n = 1,173 | n = 382 | n = 1,054 | n = 14,151 |
| Age (y; mean ± SD) | 60.3 ± 9.4 | 60.5 ± 9.4 | 58.7 ± 8.1 | 59.6 ± 9.7 | 57.8 ± 8.8 | 58.6 ± 12.1 | 59.5 ± 9.2 | 61.9 ± 10.4 |
| Male (%) | 97.5 | 97.6 | 97.0 | 98.2 | 95.7 | 94.0 | 97.5 | 97.7 |
| Cirrhosis etiology (%) | ||||||||
| HCV | 46.1 | 41.9 | 68.6 | 50.3 | 44.2 | 31.4 | 49.1 | 36.9 |
| HBV | 1.6 | 1.4 | 2.6 | 0.9 | 0.7 | 19.4 | 3.8 | 1.4 |
| ALD | 30.0 | 32.1 | 18.3 | 30.5 | 39.0 | 18.8 | 26.1 | 33.9 |
| NAFLD | 14.7 | 16.7 | 6.0 | 13.1 | 11.5 | 19.4 | 14.3 | 16.7 |
| Other | 7.5 | 7.9 | 4.4 | 5.3 | 4.5 | 11.0 | 6.7 | 11.1 |
| BMI (kg/m2; mean ± SD) | 28.8 ± 5.9 | 29.1 ± 6.0 | 27.5 ± 5.6 | 29.1 ± 5.6 | 29.5 ± 6.0 | 27.1 ± 5.0 | 29.2 ± 6.0 | 28.3 ± 5.9 |
| CCI (mean ± SD) | 4.5 ± 2.1 | 4.4 ± 2.0 | 4.6 ± 2.3 | 4.6 ± 2.2 | 4.2 ± 1.9 | 4.5 ± 2.0 | 4.6 ± 2.2 | 4.5 ± 2.1 |
| Diabetes (%) | 31.6 | 30.4 | 35.4 | 38.9 | 31.7 | 40.1 | 36.6 | 27.3 |
| Alcohol use disorders (%) | 40.5 | 39.4 | 49.9 | 42.0 | 48.6 | 22.3 | 37.8 | 33.2 |
| Substance use disorders (%) | 20.4 | 17.4 | 38.0 | 22.7 | 23.1 | 13.1 | 20.5 | 11.4 |
| HIV co-infection (%) | 1.5 | 0.8 | 4.4 | 2.2 | 0.9 | 1.0 | 0.8 | 1.1 |
| HCC (%) | 2.6 | 2.1 | 4.7 | 2.9 | 3.0 | 4.2 | 4.0 | 2.2 |
| Cirrhosis decompensation (%) | 21.2 | 21.7 | 18.1 | 19.3 | 22.3 | 17.0 | 17.6 | 24.7 |
| Ascites | 15.9 | 16.4 | 13.7 | 11.4 | 12.6 | 11.5 | 11.8 | 19.3 |
| Encephalopathy | 3.0 | 2.8 | 3.0 | 4.8 | 5.6 | 1.8 | 3.4 | 2.7 |
| Gastroesophageal varices (with bleeding) | 2.7 | 2.8 | 1.6 | 3.5 | 4.6 | 4.2 | 2.7 | 3.1 |
| Gastroesophageal varices (without bleeding) | 7.8 | 8.3 | 6.2 | 9.1 | 7.9 | 6.5 | 7.7 | 6.1 |
| HCV genotype (%) | ||||||||
| 1 | 59.7 | 55.5 | 77.8 | 57.5 | 57.6 | 56.7 | 57.1 | 42.6 |
| 2 | 6.3 | 7.9 | 1.7 | 8.6 | 8.3 | 6.7 | 6.2 | 5.1 |
| 3 | 7.3 | 9.8 | 0.7 | 8.6 | 8.7 | 7.5 | 8.3 | 7.1 |
| 4–6 | 0.6 | 0.6 | 0.6 | 0.9 | 0.6 | 5.0 | 0.4 | 0.6 |
| Missing | 26.1 | 26.1 | 19.3 | 24.4 | 24.9 | 24.2 | 28.0 | 44.6 |
| Low SES (%) | 56.2 | 55.3 | 60.1 | 60.1 | 60.5 | 56.0 | 53.3 | 53.8 |
| Laboratory results (mean ± SD) | ||||||||
| MELD score | 11.3 ± 4.9 | 11.1 ± 4.7 | 11.6 ± 5.1 | 11.1 ± 4.6 | 11.2 ± 4.8 | 10.5 ± 4.6 | 10.9 ± 4.9 | 12.2 ± 5.1 |
| FIB-4 score | 5.7 ± 15.8 | 5.6 ± 14.2 | 5.4 ± 16.8 | 6.5 ± 26.8 | 5.6 ± 15.9 | 6.0 ± 25.3 | 5.8 ± 18.8 | 6.0 ± 10.2 |
| Hemoglobin (g/dL) | 13.1 ± 2.3 | 13.2 ± 2.3 | 12.8 ± 2.2 | 13.1 ± 2.3 | 13.0 ± 2.4 | 13.5 ± 2.3 | 13.2 ± 2.3 | 12.9 ± 2.3 |
| Platelet Count (k/μL) | 155.3 ± 89.7 | 153.3 ± 89.0 | 169.8 ± 92.1 | 143.7 ± 81.8 | 153.0 ± 83.7 | 161.4 ± 86.1 | 146.6 ± 76.9 | 153.6 ± 93.9 |
| Creatinine (mg/dL) | 1.1 ± 0.8 | 1.0 ± 0.6 | 1.3 ± 1.3 | 1.0 ± 0.8 | 1.0 ± 0.8 | 1.3 ± 1.4 | 1.1 ± 0.8 | 1.1 ± 0.8 |
| Bilirubin (g/dL) | 1.5 ± 2.2 | 1.5 ± 2.3 | 1.4 ± 2.0 | 1.6 ± 2.2 | 1.7 ± 2.3 | 1.4 ± 1.7 | 1.4 ± 1.4 | 1.8 ± 2.4 |
| INR | 1.3 ± 0.5 | 1.3 ± 0.5 | 1.3 ± 0.4 | 1.3 ± 0.4 | 1.3 ± 0.4 | 1.2 ± 0.3 | 1.3 ± 0.4 | 1.4 ± 0.5 |
| Albumin (g/dL) | 3.4 ± 0.7 | 3.4 ± 0.7 | 3.3 ± 0.7 | 3.4 ± 0.7 | 3.4 ± 0.7 | 3.6 ± 0.7 | 3.4 ± 0.7 | 3.3 ± 0.7 |
HCV-cirrhosis was more prevalent among non-Hispanic Black patients (68.6%), whereas ALD-cirrhosis was more common among AI/AN patients (39.0%) and HBV-cirrhosis was more common among Asian patients (19.4%; Table 1). Diabetes was more common among Asian (40.1%), Hispanic (38.9%), and PI/NH patients (36.6%) compared with non-Hispanic White patients (30.4%). Alcohol use disorders occurred more frequently among non-Hispanic Black (49.9%) and AI/AN patients (48.6%) and less frequently in Asian patients (22.3%) compared with non-Hispanic White patients (39.4%). Substance use disorders were also elevated among non-Hispanic Black patients (38.0%) compared with other racial/ethnic groups. Laboratory results did not substantially differ by race/ethnicity.
Association between race/ethnicity and HCC risk
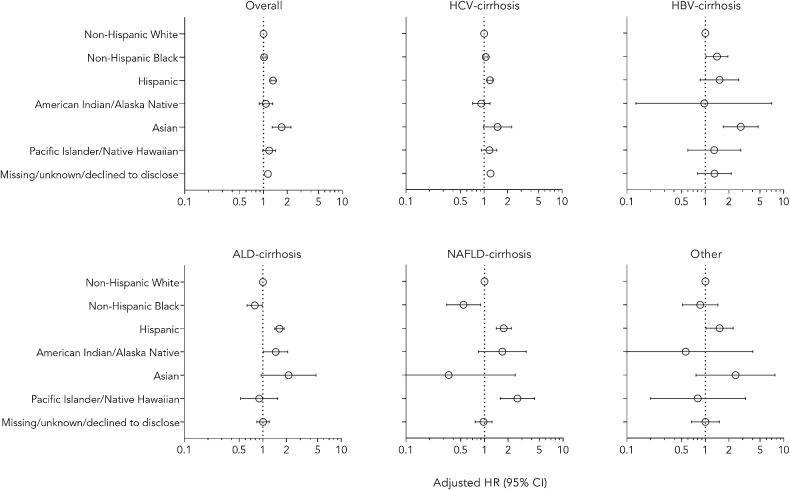
Among 116,098 patients with cirrhosis at risk for HCC, 10,242 developed HCC during a mean follow-up of 5.3 years (Supplementary Table S3). Overall, HCC incidence was 1.65 cases per 100 patient-years and was highest among Asian patients (2.40 per 100 patient-years), followed by Hispanic (2.29 per 100), non-Hispanic Black (2.29 per 100), PI/NH (1.65 per 100), AI/AN (1.61 per 100), and non-Hispanic White patients (1.51 per 100). Compared with non-Hispanic White patients, there was an increased risk for HCC among Asian (aHR, 1.70; 95% CI, 1.29–2.23) and Hispanic patients (aHR, 1.32; 95%, CI 1.24–1.41; Fig. 1). There was a suggestive positive association among PI/NH patients (aHR, 1.18; 95% CI, 0.98–1.42). No significant associations were observed among non-Hispanic Black or AI/AN patients.
Figure 1.
Adjusted associations for race/ethnicity and HCC risk. The reference group is non-Hispanic White patients and results are shown for all patients (overall) and for cirrhosis etiologies of HCV, HBV, ALD, NAFLD and other. Cox regression models are adjusted for age, sex, BMI, diabetes, cirrhosis etiology, history of cirrhosis decompensation, CCI, alcohol use disorders, substance use disorders, albumin, bilirubin, creatinine, platelet count, AST/√ALT ratio, and SES.
In analyses according to cirrhosis etiology, among patients with HCV-cirrhosis, Hispanic patients had a higher risk for HCC (aHR, 1.19; 95% CI, 1.10–1.29) compared with non-Hispanic White patients. A suggestive positive association was noted among Asian patients. Among patients with HBV-cirrhosis, non-Hispanic Black (aHR, 1.41; 95% CI, 1.02–1.94) and Asian patients (aHR, 2.84; 95% CI, 1.70–4.73) were at higher risk for HCC. Results were elevated, but not statistically significant, among Hispanic patients. Among patients with ALD-cirrhosis, there was a higher risk for HCC among Hispanic (aHR, 1.63; 95% CI, 1.42–1.87) and AI/AN patients (aHR, 1.46; 95% CI, 1.02–2.08), whereas non-Hispanic Black patients were at lower risk for HCC (aHR, 0.79; 95% CI, 0.63–0.98) compared with non-Hispanic White patients. For NAFLD-cirrhosis, Hispanic (aHR, 1.76; 95% CI, 1.41–2.20) and PI/NH patients (aHR, 2.62; 95% CI, 1.59–4.33) had a higher risk for HCC, and non-Hispanic Black patients had a lower risk for HCC (aHR, 0.54; 95% CI, 0.33–0.89) compared with non-Hispanic White patients. Among cirrhosis patients with other etiology, Hispanic patients had an increased risk for HCC (aHR, 1.52; 95% CI, 1.02–2.26). Competing risks proportional hazards analyses showed similar results (Supplementary Table S4).
Association between race/ethnicity and cirrhosis decompensation risk
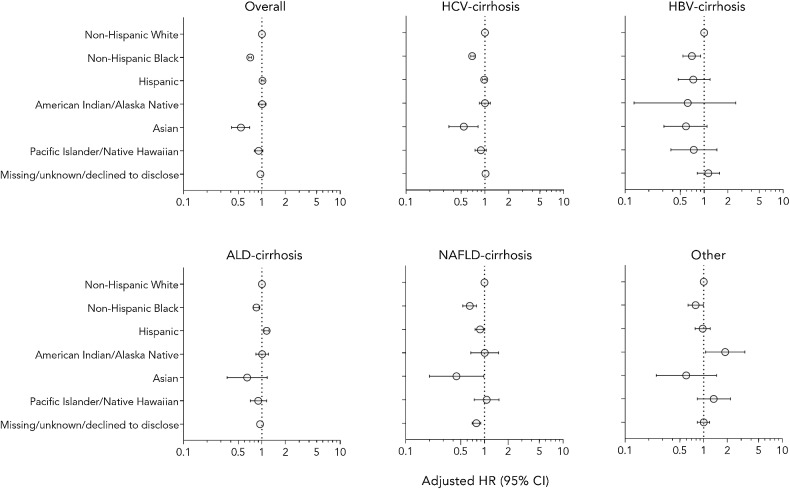
Among 111,938 patients with cirrhosis who were at risk, 27,887 developed cirrhosis decompensation during a mean follow-up of 4.9 years (Supplementary Table S5). Overall incidence was 5.13 cases per 100 patient-years, which was highest among Hispanic patients (6.04 per 100), followed by AI/AN (5.86 per 100), non-Hispanic White (5.29 per 100), PI/NH (4.95 per 100), non-Hispanic Black (3.81 per 100), and Asian patients (2.71 per 100). Overall, compared with non-Hispanic White patients, non-Hispanic Black (aHR, 0.71; 95% CI, 0.68–0.74) and Asian patients (aHR, 0.54; 95% CI, 0.41–0.70) had a lower risk for cirrhosis decompensation (Fig. 2). Among patients with HCV-cirrhosis, non-Hispanic Black (aHR, 0.69; 95% CI, 0.66–0.73) and Asian patients (aHR, 0.54; 95% CI, 0.35–0.82) had a lower risk for decompensation compared with non-Hispanic White patients. Among those with HBV-cirrhosis, non-Hispanic Black patients had a lower risk for decompensation (aHR, 0.70; 95% CI, 0.54–0.90); a suggestive inverse association was observed among Asian patients. For ALD-cirrhosis, non-Hispanic Black patients (aHR, 0.85; 95% CI, 0.78–0.92) had a lower risk for decompensation, while Hispanic patients (aHR, 1.15; 95% CI, 1.07–1.23) had a higher risk for decompensation compared with non-Hispanic White patients. Among patients with NAFLD-cirrhosis, non-Hispanic Black (aHR, 0.65; 95% CI, 0.53–0.79) and Asian patients (aHR, 0.44; 95% CI, 0.20–0.98) had a lower risk for decompensation compared with non-Hispanic White patients. Among patients with other etiology, there was a lower risk for decompensation among non-Hispanic Black patients (aHR, 0.79; 95% CI, 0.64–0.99) and a higher risk among AI/AN patients (aHR, 1.88; 95% CI, 1.06–3.34) compared with non-Hispanic White patients. Competing risks proportional hazards analyses showed similar results (Supplementary Table S4).
Figure 2.
Adjusted associations for race/ethnicity and cirrhosis decompensation risk. The reference group is non-Hispanic White patients and results are shown for all patients (overall) and for cirrhosis etiologies of HCV, HBV, ALD, NAFLD, and other. Cox regression models are adjusted for age, sex, BMI, diabetes, cirrhosis etiology, history of HCC, CCI, alcohol use disorders, substance use disorders, albumin, bilirubin, creatinine, platelet count, AST/√ALT ratio, and SES.
Association between race/ethnicity and all-cause mortality risk
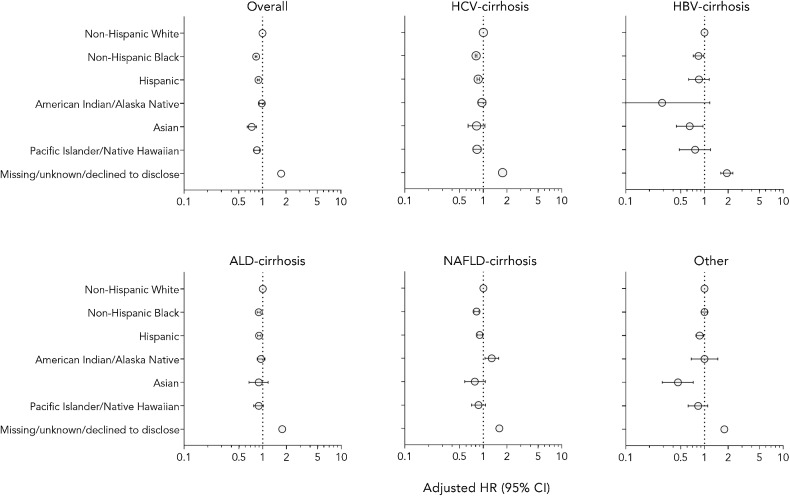
Among 120,992 patients with cirrhosis, 81,441 died during a mean follow-up of 5.4 years; the overall mortality rate was 12.37 deaths per 100 patient-years (Supplementary Table S6). Mortality was highest among non-Hispanic White patients (11.92 per 100), followed by AI/AN (11.25 per 100), Hispanic (10.93 per 100), non-Hispanic Black (10.00 per 100), PI/NH (10.00 per 100), and Asian patients (8.35 per 100). Overall, there was a lower risk for mortality among non-Hispanic Black (aHR, 0.83; 95% CI, 0.81–0.85), Hispanic (aHR, 0.89; 95% CI, 0.86–0.91), Asian (aHR, 0.73; 95% CI, 0.64–0.84), and PI/NH patients (aHR, 0.85; 95% CI, 0.78–0.92) compared with non-Hispanic White patients (Fig. 3). Among patients with HCV-cirrhosis, non-Hispanic Black (aHR, 0.81; 95% CI, 0.78–0.83), Hispanic (aHR, 0.86; 95% CI, 0.83–0.90), and PI/NH patients (aHR, 0.83; 95% CI, 0.74–0.93) had a lower mortality risk compared with non-Hispanic White patients. For HBV-cirrhosis, there was a lower risk for mortality among non-Hispanic Black (aHR, 0.84; 95% CI, 0.72–0.98) and Asian patients (aHR, 0.65; 95% CI, 0.44–0.96). Among those with ALD-cirrhosis, non-Hispanic Black (aHR, 0.89; 95% CI, 0.85–0.93) and Hispanic patients (aHR, 0.90; 95% CI, 0.86–0.95) had a lower risk for mortality compared with non-Hispanic White patients. Among patients with NAFLD-cirrhosis, non-Hispanic Black (aHR, 0.82; 95% CI, 0.76–0.88) and Hispanic patients (aHR, 0.90; 95% CI 0.84–0.97) had a lower risk for mortality, whereas AI/AN patients had an increased risk (aHR, 1.28; 95% CI, 1.05–1.57) compared with non-Hispanic White patients. Among those with other cirrhosis etiology, there was a lower risk for mortality among Hispanic (aHR, 0.87; 95% CI, 0.78–0.98) and Asian patients (aHR, 0.46; 95% CI, 0.29–0.72) compared with non-Hispanic White patients.
Figure 3.
Adjusted associations for race/ethnicity and all-cause mortality risk. The reference group is non-Hispanic White patients and results are shown for all patients (overall) and for cirrhosis etiologies of HCV, HBV, ALD, NAFLD, and other. Cox regression models are adjusted for age, sex, BMI, diabetes, cirrhosis etiology, history of HCC or cirrhosis decompensation, CCI, alcohol use disorders, substance use disorders, albumin, bilirubin, creatinine, platelet count, AST/√ALT ratio, and SES.
Discussion
In this national cohort of US Veterans with cirrhosis, race/ethnicity was an important predictor in the risk of developing HCC, cirrhosis decompensation, and all-cause mortality, adjusting for risk factors, including age, sex, diabetes, BMI, alcohol use disorders, substance use disorders, comorbidities, and SES. Analyses according to cirrhosis etiology revealed further differential associations with race/ethnicity by HCV, HBV, ALD, NAFLD, and other etiology. These findings provide clinical and public health insights for prevention, screening, and treatment of these complications in patients with cirrhosis.
Race/ethnicity and HCC risk
Compared with non-Hispanic White patients, Hispanic patients were generally at increased risk for HCC overall and across cirrhosis etiologies. Our results are consistent with prior research showing higher risk for HCC among Hispanic patients with NAFLD-cirrhosis (26) and HCV-cirrhosis (27) in the US, while further extending these positive associations to other cirrhosis etiologies. Differences in the prevalence of metabolic factors may contribute to increased risk for HCC, as obesity and insulin resistance are more prevalent among Hispanic persons (28). The inflammatory and hormonal sequelae associated with these metabolic risk factors may contribute to increased hepatocarcinogenesis beyond the risk conferred by NAFLD alone (28). In patients with HCV-cirrhosis, Hispanic patients with at least two metabolic risk factors were at increased risk of developing HCC compared with non-Hispanic patients with fewer than two metabolic risk factors (aHR, 1.89; 95% CI, 1.20–2.97; ref. 27). Although we adjusted for BMI and diabetes in this analysis, there may be residual confounding from unadjusted metabolic risk factors (e.g., pre-diabetes, dyslipidemia, abdominal circumference) that may have contributed to the observed results. In addition, there may be heterogeneity in genetics and other exposures associated with Hispanic ethnicity (29, 30). Additional research on specific demographic characteristics, such as country of origin and US location residence, may be informative in better characterizing the risk of HCC within the Hispanic population.
Overall, the strongest association between race/ethnicity and HCC risk was observed among Asian patients, which was driven by higher risk among those with HBV- or HCV-cirrhosis. Prevalence of behavioral factors (e.g., smoking), as well as other factors related to HBV infection (e.g., genotype, duration of infection), may differ by race/ethnicity and be associated with more severe liver disease and higher risk for HCC (31–33). Our findings are consistent with studies showing increased HCC risk among Asian patients with HCV-cirrhosis compared with White patients (OR, 4.3; 95% CI, 2.1–9.0; ref. 34) as well as Asian/Pacific Islander patients with HBV compared with White patients (HR, 2.04; 95% CI, 1.31–3.17; ref. 35). One potential explanation for higher rates of HCC among Asian patients with HCV-cirrhosis is a higher likelihood of prior exposure to HBV. Patients may have low levels of HBV in their liver tissue in the absence of detectable HBsAg in serum, which is a phenomenon known as occult hepatitis B infection (OBI) and has been associated with increased HCC incidence (36, 37). OBI has been observed in upwards of 50% of patients with chronic HCV (38). In addition, Asian persons born outside of the US may experience longer periods of infection with HCV due to younger age at infection, which may increase HCC risk (39). Furthermore, HCV-risk factors are less common among Asians, which may contribute to delayed access to screening (40, 41). Compared with non-Hispanic White patients with cirrhosis, we observed differences in HCC risk for AI/AN patients with ALD-cirrhosis and PI/NH patients with NAFLD-cirrhosis. We also found that non-Hispanic Black patients with HBV-cirrhosis, ALD-cirrhosis, or NAFLD-cirrhosis had a relatively lower risk for HCC. Previous research has demonstrated a lower risk for mortality and other outcomes among Black compared with White Veterans, potentially due to Black Veterans being less severely ill and using health care earlier because they have less access to the private sector health care options (42). Biological, genetic, lifestyle (e.g., dietary), behavioral, social, environmental, and other factors potentially underlying these racial/ethnic differences in HCC incidence should be further investigated.
Race/ethnicity and cirrhosis decompensation risk
The clinical course of cirrhosis is characterized by three primary complications (i.e., decompensations) of variceal bleeding, ascites, and hepatic encephalopathy, and includes two major periods of compensated (i.e., asymptomatic) and decompensated cirrhosis (43). In this study, non-Hispanic Black patients had a lower risk for cirrhosis decompensation compared with non-Hispanic White patients overall and by cirrhosis etiology. This finding is in contrast with studies, suggesting that Black patients with cirrhosis have higher hospital readmission rates compared with White patients with cirrhosis (44). Asian patients also had a lower risk for decompensation overall and for several cirrhosis etiologies (HCV, HBV, and NAFLD), although the inverse association for HBV-cirrhosis was not statistically significant. Among those with ALD-cirrhosis, Hispanic patients had a higher risk for decompensation, whereas among those with other cirrhosis, AI/AN patients had an increased risk for decompensation. These results are in line with research showing differential rates of decompensation according to cirrhosis etiology, where the rate of decompensation was higher among patients with ALD-cirrhosis (7.3%; 95% CI; 6.5%–8.2%) versus non-ALD-related cirrhosis (5.5%; 95% CI, 4.8%–6.2%; ref. 45). Differences in health care utilization by race/ethnicity may play a role in decompensation outcomes (46). Decompensation symptoms, ascites, encephalopathy, hepatorenal syndrome, and hepatopulmonary syndrome can present on a spectrum of severity, and patients with mild symptoms may delay seeking care (46). As the study population in this analysis was of patients within the VA health care system, differing access to health care due to insurance coverage should not be a contributing factor in the results. However, VA health care coverage does not preclude other individual- and/or multi-level contributing factors and inequities from having important implications for disease progression to cirrhosis decompensation. For example, patients with compensated cirrhosis may have differential access to resources that would promote adherence to clinical guidance and patient education regarding alcohol abstinence, medication usage, nutrition, and/or exercise, which may be further influenced by sociocultural contexts (47, 48). Despite how our analysis adjusted for SES, differences in neighborhood contextual factors may persist and influence health care–seeking behavior, diet, and lifestyle, such as proximity and/or transportation access to health care facilities, access to greenspace, parks, and neighborhood infrastructure (e.g., sidewalks) to promote physical activity, food insecurity (e.g., access to healthy food options) to facilitate maintenance of a recommended low-sodium, high-protein diet, and enduring neighborhood and health inequities of structural racism (49–54). Furthermore, this study was not able to capture psychosocial factors, such as social support, which have been shown to improve health status and impact a person's uptake of healthy behaviors (53, 55). Further research is needed to explore factors that may influence susceptibility to and progression rate of cirrhosis decompensation according to subgroups defined by race/ethnicity (as this is a social construct; ref. 56) and cirrhosis etiology.
Race/ethnicity and all-cause mortality risk
In general, there was a lower risk for all-cause mortality among all racial/ethnic groups compared with non-Hispanic White patients with cirrhosis overall and by cirrhosis etiology. In this study population, incidence rates for HCC were not elevated among non-Hispanic White patients compared with other racial/ethnic groups, suggesting other causes of death may drive these results. This is supported by results from a US nationwide study of cirrhosis- and HCC-related mortality from 2007 to 2016, showing that HCC-related mortality was higher among non-Hispanic Asian and non-Hispanic Black compared with non-Hispanic White patients (results were similar for Hispanic patients; ref. 6). However, cirrhosis-related mortality was higher among non-Hispanic White compared with Hispanic, non-Hispanic Black, and non-Hispanic Asian patients (6).
AI/AN patients with NAFLD-cirrhosis were at higher risk for all-cause mortality compared with non-Hispanic White patients. This finding is consistent with research showing that AI/AN patients have a higher prevalence of NAFLD (57) and also experience relatively higher incidence rates of HCC (58). As HCC is associated with low 5-year relative survival (8.1%; ref. 59), this increased mortality among AI/AN patients may be impacted by HCC-related deaths. Future research should examine racial/ethnic disparities related to health care usage, such as medical adherence, physician trust, and health care–seeking behavior, as well as potential differences in health system factors (e.g., hospital characteristics; ref. 60) that may contribute to differences in mortality (46). Studies addressing genetic factors may be warranted, for example, racial/ethnic differences in palatin-like phospholipase domain-containing 3 (PNPLA3) genotype and its associations with NAFLD, HCC, and all-cause mortality (61).
This study had several limitations. As patients in this cohort were predominantly male, the generalizability of results to women may be limited. Although we were able to examine different racial/ethnic groups and stratify by major cirrhosis etiologies, some subgroups (e.g., Asian patients, HBV-cirrhosis etiology) were limited by relatively small sample sizes. Patients with less common etiologies of cirrhosis, such as cholestatic liver diseases, were not separately examined. There may be misclassification in using ICD diagnosis codes to identify cirrhosis and HCC, although these methods have been previously validated compared with chart review. Furthermore, there may be residual confounding from unmeasured variables such as changes in diet and/or lifestyle factors implemented following cirrhosis diagnosis that may have been associated with disease progression. There are several strengths of this study, including examining a nationwide cohort of patients with a large number of incident outcomes accruing over a long follow-up period. Using information extracted from the CDW, we were able to evaluate potential confounding by many risk factors. Furthermore, examining these associations among patients within the VA health care system, which provides comprehensive health care to all enrollees, may limit the impact of differences due to health care access.
In conclusion, race/ethnicity was associated with the risk for HCC, decompensation, and all-cause mortality in this nationwide cohort of US Veterans with cirrhosis. Future research should examine the contribution of biological, sociodemographic, environmental, and other factors (e.g., health care utilization) potentially underlying these racial/ethnic differences while accounting for cirrhosis etiology, which would inform risk stratification, prevention, and control efforts.
Supplementary Material
Supplementary Table S1. ICD-9 and ICD-10 codes for cirrhosis, decompensated cirrhosis, liver transplantation, and hepatocellular carcinoma
Supplementary Table S2. ICD-9 codes for type 2 diabetes mellitus, alcohol use disorders, hemochromatosis, primary biliary cirrhosis, primary sclerosing cholangitis, autoimmune hepatitis, human immunodeficiency virus, and low socioeconomic status
Supplementary Table S3. Association between race/ethnicity and risk of HCC in patients with cirrhosis overall and by cirrhosis etiology: follow-up from cirrhosis diagnosis (2001-2014) to 2020
Supplementary Table S4. Competing risks proportional hazards regression for the associations between race/ethnicity and risk of HCC, decompensated cirrhosis, and death in patients with cirrhosis overall and by cirrhosis etiology
Supplementary Table S5. Association between race/ethnicity and risk of cirrhosis decompensation in patients with cirrhosis overall and by cirrhosis etiology: follow-up from cirrhosis diagnosis (2001-2014) to 2020
Supplementary Table S6. Association between race/ethnicity and risk of all-cause mortality in patients with cirrhosis overall and by cirrhosis etiology: follow-up from cirrhosis diagnosis (2001-2014) to 2020
Acknowledgments
This research was funded by the National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) K01 DK125612 (to T. VoPham) and T32 DK007742 (to N.J. Kim and P. Vutien), the NIH National Cancer Institute (NCI) R01 CA196692 and P20 CA252732 (to G.N. Ioannou), and the Department of Veterans Affairs CX001156 and HX003062 (to G.N. Ioannou).
The publication costs of this article were defrayed in part by the payment of publication fees. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Footnotes
Note: Supplementary data for this article are available at Cancer Epidemiology, Biomarkers & Prevention Online (http://cebp.aacrjournals.org/).
Authors' Disclosures
T. VoPham reports grants from NIH/NIDDK K01DK125612 during the conduct of the study; as well as grants from Fred Hutchinson Cancer Center Pilot Project, Fred Hutch/University of Washington Cancer Consortium New Investigator Award, NIH/NHLBI 75N92021D00001, and NIH/NCI P20CA252732, and personal fees from Georgetown Lombardi Comprehensive Cancer Center, as well as grants from University of Washington Exposures, Diseases, Genomics, and Environment (EDGE) Center Pilot Project and Prevent Cancer Foundation outside the submitted work. N.J. Kim reports grants from NIDDK during the conduct of the study. J.A. Mendoza reports grants from NIH during the conduct of the study. No disclosures were reported by the other authors.
Authors' Contributions
T. VoPham: Writing–original draft, writing–review and editing. A. Cravero: Writing–original draft, writing–review and editing. L.D. Feld: Writing–review and editing. P. Green: Data curation, formal analysis, writing–review and editing. Z. Feng: Writing–review and editing. K. Berry: Formal analysis, investigation, methodology, writing–review and editing. N.J. Kim: Writing–review and editing. P. Vutien: Writing–review and editing. J.A. Mendoza: Writing–review and editing. G.N. Ioannou: Conceptualization, supervision, funding acquisition, methodology, writing–review and editing.
References
- 1. Moon AM, Singal AG, Tapper EB. Contemporary epidemiology of chronic liver disease and cirrhosis. Clin Gastroenterol Hepatol 2020;18:2650–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Younossi ZM, Stepanova M, Younossi Y, Golabi P, Mishra A, Rafiq N, et al. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut 2020;69:564–8. [DOI] [PubMed] [Google Scholar]
- 3. Paik JM, Golabi P, Younossi Y, Mishra A, Younossi ZM. Changes in the global burden of chronic liver diseases from 2012 to 2017: the growing impact of NAFLD. Hepatology 2020;72:1605–16. [DOI] [PubMed] [Google Scholar]
- 4. Younossi ZM, Henry L. Epidemiology of non-alcoholic fatty liver disease and hepatocellular carcinoma. JHEP Rep 2021;3:100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Beste LA, Leipertz SL, Green PK, Dominitz JA, Ross D, Ioannou GN. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001–2013. Gastroenterology 2015;149:1471–82. [DOI] [PubMed] [Google Scholar]
- 6. Kim D, Li AA, Perumpail BJ, Gadiparthi C, Kim W, Cholankeril G, et al. Changing trends in etiology-based and ethnicity-based annual mortality rates of cirrhosis and hepatocellular carcinoma in the United States. Hepatology 2019;69:1064–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ 2018;362:k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zou B, Yeo YH, Le MH, Henry L, Chang ET, Lok AS, et al. Prevalence of viremic hepatitis C virus infection by age, race/ethnicity, and birthplace and disease awareness among viremic persons in the United States, 1999–2016. J Infect Dis 2020;221:408–18. [DOI] [PubMed] [Google Scholar]
- 9. Kim HS, Rotundo L, Yang JD, Kim D, Kothari N, Feurdean M, et al. Racial/ethnic disparities in the prevalence and awareness of Hepatitis B virus infection and immunity in the United States. J Viral Hepat 2017;24:1052–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rich NE, Oji S, Mufti AR, Browning JD, Parikh ND, Odewole M, et al. Racial and ethnic disparities in nonalcoholic fatty liver disease prevalence, severity, and outcomes in the United States: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2018;16:198–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Scaglione S, Kliethermes S, Cao G, Shoham D, Durazo R, Luke A, et al. The epidemiology of cirrhosis in the United States: a population-based study. J Clin Gastroenterol 2015;49:690–6. [DOI] [PubMed] [Google Scholar]
- 12. Ha J, Yan M, Aguilar M, Bhuket T, Tana MM, Liu B, et al. Race/ethnicity-specific disparities in cancer incidence, burden of disease, and overall survival among patients with hepatocellular carcinoma in the United States. Cancer 2016;122:2512–23. [DOI] [PubMed] [Google Scholar]
- 13. Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology 2004;127:S35–50. [DOI] [PubMed] [Google Scholar]
- 14. Setiawan VW, Stram DO, Porcel J, Lu SC, Le Marchand L, Noureddin M. Prevalence of chronic liver disease and cirrhosis by underlying cause in understudied ethnic groups: The multiethnic cohort. Hepatology 2016;64:1969–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. U.S. Department of Veterans Affairs. Veterans Health Administration. [cited 2023 Apr 28]. Available from:https://www.va.gov/health/.
- 16. Ioannou GN, Green P, Lowy E, Mun EJ, Berry K. Differences in hepatocellular carcinoma risk, predictors and trends over time according to etiology of cirrhosis. PLoS ONE 2018;13:e0204412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pearson MM, Kim NJ, Berry K, Moon AM, Su F, Vutien P, et al. Associations between alcohol use and liver-related outcomes in a large national cohort of patients with cirrhosis. Hepatol Commun 2021;5:2080–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Petersen LA, Byrne MM, Daw CN, Hasche J, Reis B, Pietz K. Relationship between clinical conditions and use of veterans affairs health care among medicare-enrolled veterans. Health Serv Res 2010;45:762–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Humensky J, Carretta H, de Groot K, Brown MM, Tarlov E, Hynes DM. Service utilization of veterans dually eligible for VA and medicare fee-for-service: 1999–2004. Medicare Medicaid Res Rev 2012;2:mmrr.002.03.a06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. U.S. Department of Veterans Affairs. National Veteran Health Equity Report 2021. [cited 2023 Apr 28]. Available from:https://www.va.gov/HEALTHEQUITY/docs/NVHER_2021_Report_508_Conformant.pdf.
- 21. Kind AJ, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med 2014;161:765–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible—the neighborhood atlas. N Engl J Med 2018;378:2456–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Beste LA, Green PK, Berry K, Kogut MJ, Allison SK, Ioannou GN. Effectiveness of hepatitis C antiviral treatment in a USA cohort of veteran patients with hepatocellular carcinoma. J Hepatol 2017;67:32–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. El-Serag HB, Kanwal F, Richardson P, Kramer J. Risk of hepatocellular carcinoma after sustained virological response in veterans with hepatitis C virus infection. Hepatology 2016;64:130–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology 2017;65:310–35. [DOI] [PubMed] [Google Scholar]
- 26. Kanwal F, Kramer JR, Mapakshi S, Natarajan Y, Chayanupatkul M, Richardson PA, et al. Risk of hepatocellular cancer in patients with non-alcoholic fatty liver disease. Gastroenterology 2018;155:1828–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wong A, Le A, Lee MH, Lin YJ, Nguyen P, Trinh S, et al. Higher risk of hepatocellular carcinoma in hispanic patients with hepatitis C cirrhosis and metabolic risk factors. Sci Rep 2018;8:7164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carrion AF, Ghanta R, Carrasquillo O, Martin P. Chronic liver disease in the hispanic population of the United States. Clin Gastroenterol Hepatol 2011;9:834–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Conomos MP, Laurie CA, Stilp AM, Gogarten SM, McHugh CP, Nelson SC, et al. Genetic diversity and association studies in US hispanic/latino populations: applications in the hispanic community health study/study of latinos. Am J Hum Genet 2016;98:165–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stern MC, Fejerman L, Das R, Setiawan VW, Cruz-Correa MR, Perez-Stable EJ, et al. Variability in cancer risk and outcomes within US latinos by national origin and genetic ancestry. Curr Epidemiol Rep 2016;3:181–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology 2012;142:1264–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wang YH, Chuang YH, Wu CF, Jan MC, Wu WJ, Lin CL, et al. Smoking and hepatitis B virus-related hepatocellular carcinoma risk: the mediating roles of viral load and alanine aminotransferase. Hepatology 2019;69:1412–25. [DOI] [PubMed] [Google Scholar]
- 33. Nguyen-Grozavu FT, Pierce JP, Sakuma KK, Leas EC, McMenamin SB, Kealey S, et al. Widening disparities in cigarette smoking by race/ethnicity across education level in the United States. Prev Med 2020;139:106220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nguyen MH, Whittemore AS, Garcia RT, Tawfeek SA, Ning J, Lam S, et al. Role of ethnicity in risk for hepatocellular carcinoma in patients with chronic hepatitis C and cirrhosis. Clin Gastroenterol Hepatol 2004;2:820–4. [DOI] [PubMed] [Google Scholar]
- 35. Mittal S, Kramer JR, Omino R, Chayanupatkul M, Richardson PA, El-Serag HB, et al. Role of age and race in the risk of hepatocellular carcinoma in veterans with hepatitis B virus infection. Clin Gastroenterol Hepatol 2018;16:252–9. [DOI] [PubMed] [Google Scholar]
- 36. Pollicino T, Saitta C. Occult hepatitis B virus and hepatocellular carcinoma. World J Gastroenterol 2014;20:5951–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ioannou GN, Splan MF, Weiss NS, McDonald GB, Beretta L, Lee SP. Incidence and predictors of hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol 2007;5:938–45. [DOI] [PubMed] [Google Scholar]
- 38. Coppola N, Onorato L, Pisaturo M, Macera M, Sagnelli C, Martini S, et al. Role of occult hepatitis B virus infection in chronic hepatitis C. World J Gastroenterol 2015;21:11931–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. D'Souza R, Glynn MJ, Ushiro-Lumb I, Feakins R, Domizio P, Mears L, et al. Prevalence of hepatitis C-related cirrhosis in elderly Asian patients infected in childhood. Clin Gastroenterol Hepatol 2005;3:910–7. [DOI] [PubMed] [Google Scholar]
- 40. Kin KC, Lin B, Chaung KT, Ha NB, Trinh HN, Garcia RT, et al. Less-established risk factors are common in Asian Americans with hepatitis C virus: a case–controlled study. Dig Dis Sci 2013;58:3342–7. [DOI] [PubMed] [Google Scholar]
- 41. Yip B, Wantuck JM, Kim LH, Wong RJ, Ahmed A, Garcia G, et al. Clinical presentation and survival of Asian and non-Asian patients with HCV-related hepatocellular carcinoma. Dig Dis Sci 2014;59:192–200. [DOI] [PubMed] [Google Scholar]
- 42. Peterson K, Anderson J, Boundy E, Ferguson L, McCleery E, Waldrip K. Mortality disparities in racial/ethnic minority groups in the veterans health administration: an evidence review and map. Am J Public Health 2018;108:e1–e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Arroyo V, Angeli P, Moreau R, Jalan R, Claria J, Trebicka J, et al. The systemic inflammation hypothesis: towards a new paradigm of acute decompensation and multiorgan failure in cirrhosis. J Hepatol 2021;74:670–85. [DOI] [PubMed] [Google Scholar]
- 44. Spiewak T, Taefi A, Patel S, Li CS, Chak E. Racial disparities of black Americans hospitalized for decompensated liver cirrhosis. BMC Gastroenterol 2020;20:245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fleming KM, Aithal GP, Card TR, West J. The rate of decompensation and clinical progression of disease in people with cirrhosis: a cohort study. Aliment Pharmacol Ther 2010;32:1343–50. [DOI] [PubMed] [Google Scholar]
- 46. Nguyen GC, Thuluvath PJ. Racial disparity in liver disease: biological, cultural, or socioeconomic factors. Hepatology 2008;47:1058–66. [DOI] [PubMed] [Google Scholar]
- 47. Saffer H, Dave D, Grossman M, Leung LA. Racial, ethnic, and gender differences in physical activity. J Hum Cap 2013;7:378–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sudhinaraset M, Wigglesworth C, Takeuchi DT. Social and cultural contexts of alcohol use: influences in a social-ecological framework. Alcohol Res 2016;38:35–45. [PMC free article] [PubMed] [Google Scholar]
- 49. Heo S, Bell ML. Investigation on urban greenspace in relation to sociodemographic factors and health inequity based on different greenspace metrics in 3 US urban communities. J Expo Sci Environ Epidemiol 2022;33:218–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sansom G, Hannibal B. Disparate access to nutritional food; place, race and equity in the United States. BMC Nutr 2021;7:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Eberth JM, Hung P, Benavidez GA, Probst JC, Zahnd WE, McNatt MK, et al. The problem of the color line: spatial access to hospital services for minoritized racial and ethnic groups. Health Aff 2022;41:237–46. [DOI] [PubMed] [Google Scholar]
- 52. Yao CK, Fung J, Chu NHS, Tan VPY. Dietary interventions in liver cirrhosis. J Clin Gastroenterol 2018;52:663–73. [DOI] [PubMed] [Google Scholar]
- 53. Kardashian A, Serper M, Terrault N, Nephew LD. Health disparities in chronic liver disease. Hepatology 2022;77:1382–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017;389:1453–63. [DOI] [PubMed] [Google Scholar]
- 55. Bell CN, Thorpe RJ Jr, Laveist TA. Race/ethnicity and hypertension: the role of social support. Am J Hypertens 2010;23:534–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Flanagin A, Frey T, Christiansen SL. Committee AMAMoS. Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA 2021;326:621–7. [DOI] [PubMed] [Google Scholar]
- 57. Bialek SR, Redd JT, Lynch A, Vogt T, Lewis S, Wilson C, et al. Chronic liver disease among two American Indian patient populations in the southwestern United States, 2000–2003. J Clin Gastroenterol 2008;42:949–54. [DOI] [PubMed] [Google Scholar]
- 58. Melkonian SC, Jim MA, Reilley B, Erdrich J, Berkowitz Z, Wiggins CL, et al. Incidence of primary liver cancer in American Indians and Alaska Natives, US, 1999–2009. Cancer Causes Control 2018;29:833–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Zhang X, El-Serag HB, Thrift AP. Predictors of five-year survival among patients with hepatocellular carcinoma in the United States: an analysis of SEER-medicare. Cancer Causes Control 2021;32:317–25. [DOI] [PubMed] [Google Scholar]
- 60. Serper M, Kaplan DE, Shults J, Reese PP, Beste LA, Taddei TH, et al. Quality measures, all-cause mortality, and health care use in a national cohort of veterans with cirrhosis. Hepatology 2019;70:2062–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wijarnpreecha K, Scribani M, Raymond P, Harnois DM, Keaveny AP, Ahmed A, et al. PNPLA3 gene polymorphism and overall and cardiovascular mortality in the United States. J Gastroenterol Hepatol 2020;35:1789–94. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1. ICD-9 and ICD-10 codes for cirrhosis, decompensated cirrhosis, liver transplantation, and hepatocellular carcinoma
Supplementary Table S2. ICD-9 codes for type 2 diabetes mellitus, alcohol use disorders, hemochromatosis, primary biliary cirrhosis, primary sclerosing cholangitis, autoimmune hepatitis, human immunodeficiency virus, and low socioeconomic status
Supplementary Table S3. Association between race/ethnicity and risk of HCC in patients with cirrhosis overall and by cirrhosis etiology: follow-up from cirrhosis diagnosis (2001-2014) to 2020
Supplementary Table S4. Competing risks proportional hazards regression for the associations between race/ethnicity and risk of HCC, decompensated cirrhosis, and death in patients with cirrhosis overall and by cirrhosis etiology
Supplementary Table S5. Association between race/ethnicity and risk of cirrhosis decompensation in patients with cirrhosis overall and by cirrhosis etiology: follow-up from cirrhosis diagnosis (2001-2014) to 2020
Supplementary Table S6. Association between race/ethnicity and risk of all-cause mortality in patients with cirrhosis overall and by cirrhosis etiology: follow-up from cirrhosis diagnosis (2001-2014) to 2020
Data Availability Statement
The data used in this research belong to the Veterans Health Administration. Although the data can be accessed by VA researchers with requisite approvals, they are not publicly available. However, the study methodology has been described to facilitate reproduction of the study results by VA researchers with access to the CDW.