Abstract
The aim of this manuscript was to summarize the demography and changing trends of geriatric spinal injuries and to enumerate the challenges and special considerations in the care of geriatric spinal injuries. PubMed, Scopus and Embase databases were searched for literature on geriatric spine fractures using MeSH terms ‘aged’, ‘aged, 80 and over’, ‘elderly’, ‘spinal fracture/epidemiology’, spinal fracture/therapy∗’ and keywords pertaining to the same. The search results were screened for appropriate articles and reviewed. There is a high community prevalence of elderly vertebral fractures ranging from 18% to as high as 51%. The proportion of older patients among the spinal injured is rising as well. There is a higher chance of missing spinal injuries in the elderly and clinical guidelines may not be applicable to this patient group. Classification and surgical treatment are different from younger adult counterparts as the elderly osteoporotic spine behaves differently biomechanically. There is a high incidence of respiratory complications both for surgically and conservatively managed groups. Older age generally is associated with a higher complication rate including mortality.
1. Introduction
As the world is moving towards a population structure where the aged are increasing in numbers rapidly,1 musculoskeletal disorders, among them spine fractures, are becoming exceedingly prevalent.2,3 Spinal injuries in the elderly are to be considered as a separate entity due to multiple etiological, epidemiological and clinical differences when compared to young adult spinal injuries. Evaluation, treatment modalities and outcomes are vastly different in the elderly population.4,5
Several factors need to be considered in the management of these injuries.6, 7, 8 Difficulty in diagnosis owing to impaired perception and cognitive dysfunction, comorbidities and the resultant polypharmacy, poor bone quality (osteopenia/osteoporosis) resulting in unique morphological characteristics and creating difficulty in surgical fixation are the initial concerns that should arise. Higher incidence of rigid spine (ankylosing spondylitis/DISH/degenerative rigidity) which alters the biomechanics, reduced capacity of the body to tolerate injury (frailty – indicating aging), poor healing and propensity for more fractures in the future should be kept in focus while planning the management. Increased risk of malignancy and differentiating benign from malignant fractures, psychiatric complications, caregiver burden and reduced family support are some of the special aspects of care that should be included in the follow-up of geriatric patients. Some unique situations like post-surgical fractures and rebound associated fractures after stoppage of denosumab therapy are also noteworthy.
As healthcare providers face increasing numbers of geriatric spinal injuries, it has become imperative to be conversant with the epidemiology, etiology, mechanism of injury, management, possible complications and differences in outcome which make these injuries unique. As new evidence surfaces, there is a need to consolidate the data. Thus, a comprehensive and up-to-date review of literature pertaining to these injuries is required.
The aim of this narrative review was to summarize the demography and changing trends of geriatric spinal injuries and to enumerate the challenges and special considerations in the care of geriatric spinal injuries.
2. Methodology
The manuscript has been prepared adhering to the quality standards for narrative reviews, as defined and quantified by "SANRA - a scale for the quality assessment of narrative review articles".
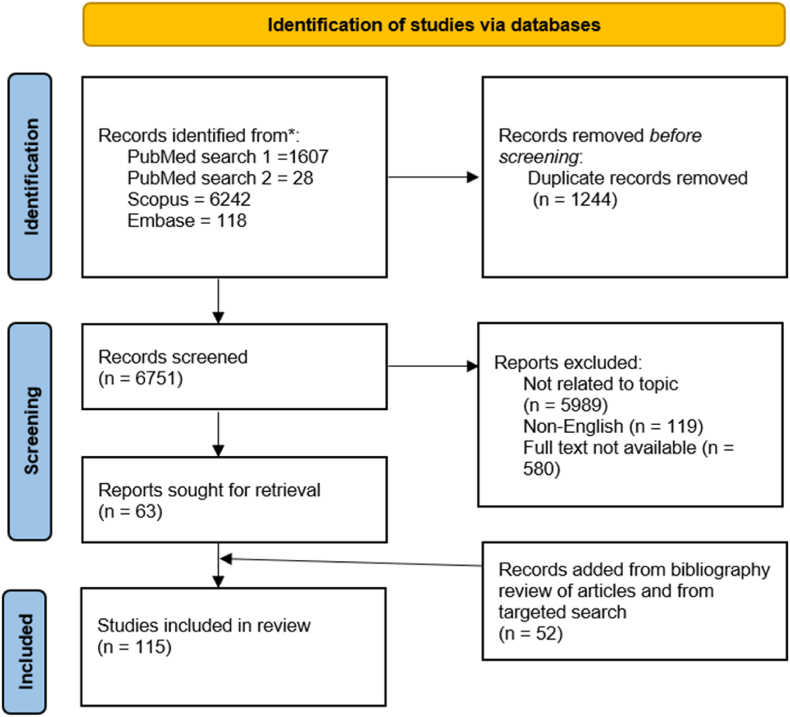
A comprehensive literature search of PubMed, Scopus and Embase databases from inception of database to December 2022 was carried out and relevant articles in English language with abstract or available full text (free full text or access available to the authors) were included. PubMed search was carried out using the search string (((aged[MeSH Terms]) OR (aged, 80 and over[MeSH Terms])) OR (elderly[MeSH Terms])) AND (spinal fracture∗[MeSH Terms]) which yielded 7699 results. The search was refined using the strings (((aged[MeSH Terms]) OR (aged, 80 and over[MeSH Terms])) OR (elderly[MeSH Terms])) AND (spinal fracture/epidemiology[MeSH Terms]) – 1607 results, and (((aged[MeSH Terms]) OR (aged, 80 and over[MeSH Terms])) OR (elderly[MeSH Terms])) AND (spinal fracture/therapy∗[MeSH Terms]) – 28 results. Advanced search in Scopus was carried out using the string (geriatric OR elderly) AND (spine OR spinal) AND (injuries OR fractures) AND ((demography OR trends OR challenges OR (special AND considerations) OR considerations)) in TITLE-ABS-KEYWORD format which yielded 8757 Scopus (6242 articles in the ‘medicine’ subgroup) search results. Embase search was carried out using the search string ('geriatric':ab,ti OR 'elderly':ab,ti) AND ('spine':ab,ti OR 'spinal':ab,ti) AND ('injuries':ab,ti OR 'fractures':ab,ti) AND ('demography':ab,ti OR 'trends':ab,ti OR 'challenges':ab,ti OR 'considerations':ab,ti OR 'special considerations':ab,ti). Additional targeted literature search was carried out for various guidelines and specific keywords. Reference lists of the included articles have also been reviewed for relevant articles and pertinent articles from these were added. After screening the articles, a total of 115 articles were included for data extraction and review (Fig. 1).
Fig. 1.
Literature Search strategy.
3. Demography
The studies referred for demographics and trends in geriatric spinal injuries are enumerated in Table 1.
Table 1.
Studies referred for demographics and trends in geriatric spine fractures.
| S.no. | Authors | Article | Journal | Type of Study | Sample size | Age | Outcome/Conclusion |
|---|---|---|---|---|---|---|---|
| 1 | WHO (World health Organization)1 | SHIFTING DEMOGRAPHICS [Internet]. Available from: https://www.un.org/en/un75/shifting-demographics | WHO website | Web page | NA | NA | Proportion of aged persons in the world is increasing |
| 2 | Baidwan N et al.2 | Epidemiology and recent trends of geriatric fractures presenting to the emergency department for United States population from year 2004–2014. | Public Health. 2017 | Epidemiologic (Database) study - NEISS | na | 65 years and above | Lower trunk (lumbar spine, pelvis and hip) were the most common sites for geriatric fractures. However there were decreasing trends for incidence of these fractures over the years 2004–2014. |
| 3 | Nagassima Rodrigues Dos Reis K et al.3 | Changing Demographic Trends in spine trauma: The presentation and outcome of Major Spine Trauma in the elderly. | Surgeon. 2021 | Epidemiologic (Database) study – local TARN | 669 | >65 vs < 65 years | The demographics of major trauma has shifted in the recent decades, with the average age of trauma patients progressively increasing. Also, the average age within the elderly cohort is also increasing, with those at the greater extreme of this age group sustaining major traumatic injuries. |
| 4 | Bonne S et al.4 | Trauma in the Older Adult. Epidemiology and Evolving Geriatric Trauma Principles. | Clinics in Geriatric Medicine. 2013 | Review article | NA | NA | Geriatric trauma patients are different from younger patients, multiple factors affect their evaluation and treatment |
| 5 | Lin PC et al.5 | Comprehensive comparison between geriatric and nongeriatric patients with trauma. | Medicine (United States). 2022 | Retrospective observational study | 273 | >65 years | Higher trauma incidence, higher ISS and higher mortality in >65 years |
| 6 | Ensrud KE6 | Epidemiology of fracture risk with advancing age. | Journals of Gerontology - Series A Biological Sciences and Medical Sciences. 2013 | Review article | NA | NA | Advanced age, low bone mass, and previous fracture -strong risk factors for fractures at nearly all skeletal sites. Vertebral fractures – most common fragility fracture |
| 7 | Ikpeze TC et al.7 | Spinal Cord Injury in the Geriatric Population: Risk Factors, Treatment Options, and Long-Term Management. | Geriatr Orthop Surg Rehabil. 2017 | Review article | NA | NA | Elderly are more affected by SCI than younger persons, pre-existing rigid spine is a risk factor for injury |
| 8 | van der Jagt-Willems HC et al.8 | Why do geriatric outpatients have so many moderate and severe vertebral fractures? Exploring prevalence and risk factors. | Age Ageing. 2012 | Prospective cohort study (observational) | 303 | 81 ± 8 (no fracture), 82 ± 6 (vertebral fracture) | 51% elderly have asymptomatic vertebral fractures. Comorbidities, cognitive decline, prednisolone usage, lower serum albumin were associated with fractures. |
| 9 | Jabbour P et al.9 | Traumatic spine injuries in the geriatric population. | Neurosurg Focus. 2008 | Literature review | NA | >65 years | Traumatic spine injuries are increasing in number, there are several factors contributing to the risk |
| 10 | Arul K et al.10 | Traumatic spinal cord injuries in geriatric population: etiology, management, and complications. | Journal of Spine Surgery. 2019 | Cross-sectional study | 73 | Average 74 years | Fractures and central cord syndrome were the most common diagnoses and typically due to falls. |
| 11 | Ballane G et al.11 | Worldwide prevalence and incidence of osteoporotic vertebral fractures. | Osteoporosis International. 2017 | Literature review of epidemiologic studies | NA | na | Highest prevalence of osteoporotic fractures is in Scandinavia (26%), lowest in Eastern Europe (18%) |
| 12 | Marwaha RK et al.12 | The prevalence of and risk factors for radiographic vertebral fractures in older Indian women and men: Delhi Vertebral Osteoporosis Study (DeVOS). | Arch Osteoporos. 2012 | Cross-sectional study | 808 | >50 years | High prevalence – 17.9% of vertebral fractures |
| 13 | Cosman F et al.13 | Spine fracture prevalence in a nationally representative sample of US women and men aged ≥40 years: results from the National Health and Nutrition Examination Survey (NHANES) 2013–2014. | Osteoporosis International. 2017 | Cross-sectional study | 3330 | ≥40 years | Spine fracture is highly prevalent in older adults and increases with age (<5%–18% - average 5.4%) |
| 14 | Li Y et al.14 | The prevalence and under-diagnosis of vertebral fractures on chest radiograph. | BMC Musculoskelet Disord. 2018 | Retrospective observational study | 3216 | ≥50 years | Spine fracture is highly prevalent in older adults and increases with age (2.4–21.9% - average 9.2%) |
| 15 | Wilson J et al.15 | Epidemiology and Impact of Spinal Cord Injury in the Elderly: Results of a Fifteen-Year Population-Based Cohort Study. | J Neurotrauma. 2020 | Population-based cohort study | 1207 vs 658 | <65 years vs > 65 years | 4% per year rise of fracture risk in >65 year old females, higher cervical and incomplete SCI compared to <65 year olds |
| 16 | Bank M et al.16 | Age and Other Risk Factors Influencing Long-Term Mortality in Patients With Traumatic Cervical Spine Fracture. | Geriatr Orthop Surg Rehabil. 2018 | Epidemiologic (Database) study | 632 | >64 years vs < 64 years | 66% traumatic cervical spine fractures are in patients older than 64 years, long-term survival decreased significantly for >65 year-olds |
| 17 | McCaughey EJ et al.17 | Changing demographics of spinal cord injury over a 20-year period: A longitudinal population-based study in Scotland. | Spinal Cord. 2016 | Longitudinal population-based study | 1638 | All ages | Mean age at the time of SCI increased significantly over 20 years (44.1–52.6 years) |
| 18 | Wáng YXJ et al.18 | Radiographic osteoporotic vertebral fractures in elderly men: A brief review focusing on differences between the sexes. | Quantitative Imaging in Medicine and Surgery. 2020 | Literature review | NA | NA | Higher incidence of secondary osteoporosis in men than in women; Caucasian men are at a higher risk than Chinese men |
| 19 | Jawa RS et al.19 | Spinal Fractures in Older Adult Patients Admitted After Low-Level Falls: 10-Year Incidence and Outcomes. | J Am Geriatr Soc. 2017 | Retrospective registry review | 4202 | ≥65 years | Low level falls cause spinal fractures in upto 18% or elderly people, cervical spine (43%) is the most common, followed by sacrococcygeal (36%) |
| 20 | Lomoschitz FM et al.20 | Cervical Spine Injuries in Patients 65 Years Old and Older. | American Journal of Roentgenology. 2002 | Retrospective cohort study | 225 | >65 years | 64% had upper cervical fractures, older patients (>75 years) and patients who had a fall from standing height had more upper cervical fractures |
| 21 | Wang H et al.21 | Multiple-level Noncontiguous Spinal Fractures Difference Between the Young and the Elderly | J Spinal Disorders. 2013 | Retrospective cohort study | 213 | <60 years vs > 60 years | Older patients had a higher incidence of low-height falls and osteoporotic fractures, and had thoracic + lumbar as the most common pattern of multilevel injuries |
| 22 | Smith S et al.22 | The epidemiology of geriatric spinal cord injury. | Top Spinal Cord Inj Rehabil. 2010 | Literature review | NA | Mode - 65 | Most common cause of SCI is fall, with multiple risk factors |
| 23 | Rizvi S et al.23 | Odontoid fractures: impact of age and comorbidities on surgical decision making | BMC Surg. 2020 | Prospective observational cohort study | 337 | Median 80 years | Major comorbidities and an older age appear to be significant factors contributing to physicians' decision to refrain from the surgical fixation of OFx. |
| 24 | Smith RM et al.24 | Atlas Fractures. | Clinical Spine Surgery: A Spine Publication. 2018 | Review article | NA | NA | While much attention has been placed on odontoid fractures in the elderly, the current findings in the literature suggest that atlas fractures are becoming more common in that population, especially in the “young elderly” age range. |
Abbreviations.
ISS – Injury Severity Score.
NA - Not Applicable.
Na - not available.
NEISS - National Electronic Injury Surveillance System.
SCI - Spinal Cord Injury.
TARN – Trauma Audit and Research Network.
Factors for higher risk - Elderly patients are at a higher risk for spine fractures due to various reasons such as bone quality deterioration, frequent falls due to poor sensory mechanism and balance loss as a result of sarcopenia, side-effects of medication, sagittal imbalance, stiff spine due to cervical degeneration and also other joint issues such as knee osteoarthritis and genu varum.6,7,9,10
Prevalence and gender distribution - There is a high community prevalence of spine fractures in the elderly all around the globe, and the statistics are consistent across various regions. The prevalence of vertebral fractures in European women ranges from 18 to 26%. In North America, White women ≥50 years old have a 20–24% prevalence and are more affected than the Black population. Latin American countries have lower overall rates in women ≥50 years (11–19%). In Asia, rates in women above ≥65 range from 9% in Indonesia to 20% in the Middle East and are highest in Japan (24%).11 A community study in India found spine fractures in 17.7% of community dwellers aged >50 years, similar to that of Western countries.12 Similar studies found that incidence is very high – in the range of 11–18%,13 2.4–21.9%14 and up to 51% in some populations.8 In Korea, vertebral fractures accounted for >75% of all osteoporotic fractures. Incidence of spine fractures in geriatrics has been increasing over time. In a Canadian population study, over a period of 15 years a significant increase in incidence of 4% per year was observed in older females and 1.2% in elderly males when compared to younger population. The proportion of injuries in older individuals, cervical injuries and incomplete injuries was observed to have increased as well. This prevalence increases with age, more in the eighth decade when compared to the 6th and 7th decades.13,14 This clearly shows the gradual shift of the incidence of spinal injuries towards the older demographic.15 The bulk of cervical injuries among the population occurred in elderly patients >64 years old.16 A similar study in Scotland showed significant raise in the mean age at the time of traumatic spinal cord injury and also the incidence of cervical injuries and injuries due to ground level falls.17
Osteoporotic Vertebral Compression Fractures (OVCF) in males have been much less studied than those in females. They are different from those in females in that the radiologic prevalence is half that of women after age-matching. Nevertheless, if men have poor Bone Mineral Density (BMD), fracture risk is as high as that of osteoporotic women.18
Causes and level of injury - The fractures often develop due to ground-level falls or falls from a short height – up to 18% of trauma patients who had a fall from a height of 3 feet or less can have a spine fracture.19 In adults admitted for low-level falls, the most common spinal injuries are cervical spine fractures, followed by sacrococcygeal, multi-level, thoracic and lumbar fractures in the decreasing order of frequency.19 Among cervical fractures, upper cervical are the majority (up to 64%) and the rest are subaxial fractures.20 For multiple fractures, a clear difference between younger and older patients is seen in the pattern of injuries where younger patients have TL junction injuries commonly followed by CT junction injuries, older individuals have TL injuries followed by thoracic spine injuries.
Severity of neurological deficit - There is also significantly less chance of neurologic deficit in older patients.21 While this is true, there is always the risk of delayed onset of neuro deficit in this population. Incomplete injuries are more common in these patients than complete.15,22
Costs - The direct and indirect cost of managing these fractures acutely and in the long term have drastically increased over the years, even when the costs associated with morbidity and mortality are excluded.25
4. Challenges
The studies referred for literature on Challenges and special considerations in geriatric spinal injuries are briefly described in Table 2.
Table 2.
Studies referred for Challenges in Evaluation and Special Considerations in the Management of Geriatric Spinal Fractures.
| S.no. | Authors | Article | Journal | Type of Study | Sample size | Age | Outcome/Conclusion |
|---|---|---|---|---|---|---|---|
| 1 | Kim J et al.25 | Economic Burden of Osteoporotic Fracture of the Elderly in South Korea: A National Survey. | Value Health Reg Issues. 2016 | Retrospective (Database) study | 2,44,798 | >65 years | There is a high direct and indirect cost associated with osteoporotic fractures |
| 2 | Park HY et al.39 | Clinical and Radiologic Features of Osteoporotic Spine Fracture with Delayed Neurologic Compromises. | World Neurosurg. 2018 | Retrospective case-control study | 30 vs 30 | 73.5 years vs 71.9 years | Initial height loss and midportion-type fracture were correlated with delayed neurodeficit |
| 3 | Jones L et al.26 | Prevalence of vertebral fractures in CTPA's in adults aged 75 and older and their association with subsequent fractures and mortality. | Geriatrics (Switzerland). 2020 | Retrospective study | 161 | >75 years | 33.5% incidence of vertebral fractures in CT pulmonary angiogram images |
| 4 | Goode T et al.27 | Evaluation of Cervical Spine Fracture in the Elderly: Can We Trust Our Physical Examination? | Am Surg. 2014 | Prospective comparative study | 320 vs 2465 | >65 years vs <65 years | NEXUS criteria had a sensitivity of 65.9% in detecting cervical fracture in >65 year olds, where the incidence (12.8%) was more than in <65 year-olds (7.4%) |
| 5 | Healey CD et al.28 | Asymptomatic cervical spine fractures: Current guidelines can fail older patients. | Journal of Trauma and Acute Care Surgery. 2017 | Retrospective study | 173 | >55 years | 21% of the cervical fractures were asymptomatic. Those without neck pain with fractures had other region injuries and higher ISS scores. |
| 6 | Genant HK et al.40 | Vertebral Fracture Assessment Using a Semiquantitative Technique. | Journal of Bone and Mineral Research. 1993 | Prospective study | 57 | 65–75 years | Semi-quantitative method of classifying osteoporotic fractures is described |
| 7 | Sugita M et al.41 | Classification of Vertebral Compression Fractures in the Osteoporotic Spine. | J Spinal Disord Tech. 2005 | Retrospective review | 73 | 75 years (mean) | 5 types of osteoporotic fractures were classified |
| 8 | Schnake KJ et al.42 | Classification of Osteoporotic Thoracolumbar Spine Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). | Global Spine J. 2018 | Expert opinion | NA | NA | 5 types of osteoporotic fractures were classified |
| 9 | Rajasekaran S et al.43 | Osteoporotic Thoracolumbar Fractures-How Are They Different?-Classification and Treatment Algorithm. | J Orthop Trauma. 2017 | Literature review | NA | NA | Fracture classification, complications, management are described |
| 10 | Katoh H et al.29 | A comparison of cervical and thoracolumbar fractures associated with diffuse idiopathic skeletal hyperostosis—A nationwide multicenter study. | J Clin Med. 2020 | Retrospective multicentre study | 285 | 74.5 years–75.4 years | DISH patients had a higher neurologic involvement rate in cervical as compared to thoracolumbar fractures, but there was a higher rate of delay in diagnosis |
| 11 | Hiyama A et al.30 | Prevalence of diffuse idiopathic skeletal hyperostosis (DISH) assessed with whole-spine computed tomography in 1479 subjects. | BMC Musculoskelet Disord. 2018 | Retrospective study | 1479 | >20 years | Patients with DISH were older than patients without, prevalence is 19.5% |
| 12 | Okano I et al.31 | Conservative treatment for stable low-energy thoracolumbar vertebral fractures in nonfused segments among elderly patients with diffuse idiopathic skeletal hyperostosis: A matched case-control study. | Medicine (United States). 2019 | Retrospective case-control study | 14 | 77.7 years | Fractures in DISH is difficult to diagnose with plain x-rays, fusion rate after surgery is similar to general population |
| 13 | Yoshihara H et al.32 | Prevalence and characteristics of thoracic diffuse idiopathic skeletal hyperostosis in 3299 black patients. | Sci Rep. 2021 | Cross-sectional study | 3299 | 57.6 years | Thoracic DISH – 7.7% incidence on average, mean age is 70 years |
| 14 | Shah NG et al.33 | Injuries to the rigid spine: What the spine surgeon wants to know. | Radiographics. 2019 | Review article | NA | NA | Imaging for DISH patients explained |
| 15 | Teunissen FR et al.34 | Spinal cord injury after traumatic spine fracture in patients with ankylosing spinal disorders. | J Neurosurg Spine. 2017 | Retrospective observational study | 172 | 69.3 years | Cervical spine is the most common fracture site in Ankylosing spondylitis, complications and hospital stay were higher in patients with SCI from the fracture |
| 16 | Kim HJ et al.44 | Prevalence of frailty in patients with osteoporotic vertebral compression fracture and its association with numbers of fractures. | Yonsei Med J. 2018 | Prospective case-control study | 59 (with OVCF) vs 701 (controls) | 73.5 ± 6.2 years vs 71.0 ± 4.3 years | Patients with OVCF were significantly frailer (as per standard frailty phenotypes), and patients with ≥3 fractures had higher odds of being frail |
| 17 | Carlstrom LP et al.45 | Too frail is to fail: Frailty portends poor outcomes in the elderly with type II odontoid fractures independent of management strategy. | Journal of Clinical Neuroscience. 2021 | Retrospective cohort study | 63 non-frail vs 34 frail | 88 ± 6 years vs 88 ± 5 years | Higher frailty was associated with higher mortality as assessed by frailty indices |
| 18 | Kessler RA et al.46 | Impact of frailty on complications in patients with thoracic and thoracolumbar spinal fracture. | Clin Neurol Neurosurg. 2018 | Retrospective database study | 249 non-frail vs 54 frail | 60.5 ± 19 years vs 72.6 ± 12 years | Frailty and surgical intervention entail a higher 30-day complication rate in patients with thoracic/thoracolumbar fractures |
| 19 | Veronesi F37 | The impact of frailty on spine surgery: Systematic review on 10 years clinical studies. | Aging and Disease. 2021 | Systematic review | NA | NA | Higher frailty correlates with higher incidence of minor/major postoperative complications, mortality and length of stay |
| 20 | Malgo F et al.48 | Value and potential limitations of vertebral fracture assessment (VFA) compared to conventional spine radiography: experience from a fracture liaison service (FLS) and a meta-analysis. | Osteoporosis International. 2017 | Retrospective cohort study | 542 | 67.5 ± 10.1 years | Low-radiation VFA has 77% sensitivity and 80% specificity in detecting OVCF |
| 21 | Mauch JT et al.49 | Review of the imaging features of benign osteoporotic and malignant vertebral compression fractures. | American Journal of Neuroradiology. 2018 | Literature review | NA | NA | Imaging features of benign and malignant OVCF are contrasted using CT, PET, SPECT, MRI |
| 22 | Tsujio T et al.50 | Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: A prospective multicenter study. | Spine (Phila Pa 1976). 2011 | Prospective multicentre cohort study | 350 (314 united vs 49 non-union) | 75.7 ± 6.5 years vs 77.3 ± 6.4 years | 13.5% non-union rate for conservative management of OVCF, risk factors include thoracolumbar fracture level, middle column injury, confined high-intensity/diffuse low-intensity area in the vertebra on MRI |
| 23 | Smith RM et al.24 | Atlas Fractures. | Clinical Spine Surgery: A Spine Publication. 2018 | Review article | NA | NA | No level 1 evidence regarding treatment of C1 fractures in the elderly |
| 24 | Osterhoff G et al.51 | Recommendations for diagnosis and treatment of odontoid fractures in geriatric patients. | Zeitschrift fur Orthopadie und Unfallchirurgie. Georg Thieme Verlag; 2020 | Review article | NA | NA | Posterior stabilization techniques are biomechanically advantageous. The isolated anterior odontoid screw connection is associated with significantly higher failure rates in geriatric patients; with strict indication and when performed technically correct, anterior procedures can offer a less invasive alternative in selected cases. |
| 25 | Pal D et al.52 | Type II odontoid fractures in the elderly: An evidence-based narrative review of management. | European Spine Journal. 2011 | Narrative Review | NA | NA | While most authors agree that cervical immobilization yields satisfactory results for type I and III fractures in the elderly, the optimal management for type II fractures remain unsolved. |
Abbreviations.
CT - Computed Tomography.
CTPA - CT Pulmonary Angiogram.
DISH - Diffuse Idiopathic Skeletal Hyperostosis.
FLS - Fracture Liaison Services.
ISS - Injury Severity Score.
MRI - Magnetic Resonance Imaging.
NA - Not Applicable.
NEXUS - National Emergency X-Radiography Utilization Study.
OVCF - Osteoporotic Vertebral Compression Fracture.
PET - Positron Emission Tomography.
SCI - Spinal Cord Injury.
SPECT - Single Photon Emission Computed Tomography.
VFA - Vertebral Fracture Assessment.
4.1. Missed injuries
A worrisome aspect of geriatric spine fractures is that the proportion of undetected fracture load is very high. These undetected fractures affect the longevity and quality of life very significantly.15 Some of these are incidentally found out on imaging done for other conditions. A study showed that there is a 33.5% incidence of vertebral fracture in CT Pulmonary Angiogram, and on a 4.5-year follow-up, the patients with vertebral fractures had a high risk of developing subsequent fractures.26 Lateral chest radiographs have a high incidence of unreported vertebral fractures that have higher prevalence as the age progresses. Even multiple fractures were ignored by the initial reporting radiologists showing the general disregard to these fractures.14
Clinical criteria may not be adequate in detecting spine fractures in the elderly. In blunt trauma patients older than 65 years, the specificity of NEXUS criteria to detect cervical spine fractures was 42.6% (NPV 97.1%) and sensitivity was 65.9% (PPV of 19.3%), when compared to CT scan. Thus, some experts advocate performing CT in all geriatric blunt trauma patients regardless of NEXUS criteria.27 In patients older than 55 years, nearly 21% with cervical spine fractures may not have pain in the neck and have no tenderness on palpation of the neck. If imaging is not done on high suspicion, these injuries are likely be missed, causing delayed presentation and further complicating the management.28
4.2. Rigid spine and its challenges
In this context, clinico-radiological features of rigid spine viz. Ankylosing spondylitis (AS) and Diffuse Idiopathic Skeletal Hyperostisis (DISH) need to be specially reviewed. The incidence of DISH and the resultant reduced mobility of the spine increases with age.29, 30, 31, 32 These fractures are difficult to diagnose, as patients present with a minor back trauma with a background of chronic diffuse back pain. This may lead to inadequate evaluation and missed injuries. General findings of AS like sacroiliitis, bamboo and dagger appearance of spine, shiny corners and squaring of vertebral bodies should prompt further evaluation. Performing a CT scan is the first step in radiologic evaluation of patients with rigid spines. This will reduce missed injuries and may prompt MRI evaluation which shows epidural hematomas that may prove catastrophic if untreated. AO classification of spine fractures has a modifier – ‘M2’ that indicates injuries in rigid spines, by which the management plan may change.33 SCI after fractures in ankylosing disorders may be nearly 34%, much higher than in elderly without rigid spines. Cervical level injuries and epidural hematomas predict the occurrence of SCI in these individuals. Not only that, nearly 20% of SCI is delayed in onset and complication rate is much higher as well. Higher mortality in these rigid spines also mandates thorough evaluation so as to not miss these deadly injuries.34
4.3. Osteoporosis
Weak bones in the elderly inherently produce higher fracture risk. Up to 67.82% of patients aged 60–69 years and up to 41.18% of patients aged 50–59 years with normal BMD (as measured by Dual Energy X-ray Absorptiometry, DEXA scan) can also develop vertebral fragility fractures (VFF) – especially elderly females with lower Body Mass Index (BMI). The proportion of VFFs increased with age in all WHO osteoporosis classifications. When compared with normal BMD patients, there is a 1.57 and 2.62-fold higher risk of having vertebral compression fractures in osteopenia and osteoporosis respectively.35 A Korean study of patients who underwent vertebroplasty or kyphoplasty procedures found that 332 of 600 patients in the sample had osteoporotic BMD at both spine and hip, with significantly older age, 189 had only spine BMD and 79 had only hip BMD in the osteoporotic range. As in the pervious study, they found females and lower BMI correlated with poorer BMD.36 Conversely, measured bone density in the spine may be spuriously high due to compression of vertebrae. It may also be high in the case of deformity and sclerotic changes. In a study of 185 patients aged 76.9 ± 7.5 years, the same was found (0.830 ± 0.229 of 132 compression fractured bodies and 0.765 ± 0.178 g/cm3 of 608 non-compression fractured bodies) (20 males and 165 females, average). Hence, the reports of DEXA scan must be interpreted with caution.37 Interestingly, the BMD also is related to the site of the vertebral column fracture. In 120 patients of a fracture clinic (median age 75, 84.2% female, history of trauma in only 46.7%), a vertebral fracture in the lower thoracolumbar spine (T11–L4) was associated with significantly higher BMD T-scores at the hip and the spine, when compared to those at the upper thoracic level. Expectedly, an upper thoracolumbar spine fracture (T4–T10) decreased the odds of having a history of trauma.38
4.4. Frailty
The prevalence of frailty is higher in geriatric patients who have OVCF than those without. Those with compression fractures but not frail (measured by frailty indices) fare better with disability rates and quality of life. In addition, patients with more than 3 OVCF and low body mass index have a high rate of frailty.44 In octogenarians with Type-2 odontoid fractures, frailty is an independent risk factor for mortality no matter how they are treated.45 A study found that surgical complications are much higher in frail patients (33.3%) than in non-frail patients (4.2%), and that 30-day mortality was much higher (16.7% vs 4.0%).46 Frailty can be measured using various scales – Frailty Index, modified Frailty Index, Fried criteria, Cervical Deformity Frailty Index, Canadian Study of Health and Aging Frailty Index etc. and can be useful tool in prognosticating and anticipating complications.44,47
5. Special considerations
5.1. Imaging in geriatric spine fractures
In addition to traditional x-rays, vertebral fracture assessment (VFA), also known as vertebral morphometry, can be done using images acquired by BMD machines during the same sitting. This modality presumably reduces radiation exposure and improves patient comfort. Even though the image quality is poor, a meta-analysis of studies using this modality showed 84% sensitivity and 90% specificity for osteoporotic fractures of Genant grade 2 or more.48
Age related changes and multiple fractures in various stages of healing may confound radiographic pictures. In such situations, magnetic resonance imaging (MRI) Short Tau Inversion Recovery (STIR-also termed TIRM) sequences help to differentiate fresh osteoporotic vertebral fractures from old fractures by identifying vertebral body edema. Pseudo arthrosis can be diagnosed by MRI showing fluid sign, pathognomonic for patients having chronic pain with radiological features.43 Pitfalls in diagnosis by MRI may be due to acute/subacute vertebral collapse fractures having large areas of MR signal intensity (SI) change similar to malignancy. The converse can also happen, with multiple myeloma affected vertebrae presenting with normal bone signal due to complete collapse. 38% of VCF due to myeloma may appear benign.49
MRI can also be used for prognosticating these fractures, as multivariate analysis in a study demonstrated risk factors of thoracolumbar region fracture, presence of a middle column injury (indicative of a burst fracture), and a confined high-intensity or a diffuse low-intensity area in the injured vertebral body on T2-weighted MRI films for non-union.50 CT scans are useful in identifying posterior vertebral wall fractures and in evaluating any injury of the posterior bony elements. BMD assessment is essential to diagnose and quantify osteoporosis and to judge the chances of subsequent fractures. This is most commonly done through DEXA of multiple skeletal regions (spine, hip), and is also used to monitor the response to treatment, via multiple measurements at set intervals.43
5.2. Possibility of malignancy
Back pain in general when evaluated requires a high suspicion and clinical acumen to diagnose and not miss serious conditions like malignancy. Even though many ‘red flags’ such as history of malignancy, age >50 years, unexplained weight loss and no clinical improvement after 1 month have been proposed by clinical practice guidelines, none of these are specific except cancer history.51
When there is a patient with an osteoporotic fracture, there is only imaging to assist the clinician to differentiate simple osteoporotic fracture from malignancy, if no surgical intervention is planned immediately. Non-invasive blood evaluation (differential white blood cell counts, serum electrophoresis for M-band) and urine analysis (for Bence-Jones proteins) can be done to rule out multiple myeloma, as recommended by guidelines for osteoporosis management. Multiple researchers have consolidated the findings of malignant VCFs on various imaging modalities.52, 53, 54 MRI features include abnormal posterior element signal, epidural or paravertebral soft-tissue mass, expanded posterior vertebral contour, metastasis in other vertebrae, Geographic replacement of normal marrow signal, irregular margins, increased enhancement relative to adjacent vertebrae and at 3 months. Advanced MRI techniques like diffusion and chemical shift show increased restricted diffusion, no change or slight loss of SI on opposed-phase, and ratio of opposed-phase to in-phase SI 0.8–1.0. CT scan shows bone destruction, epidural or focal paravertebral soft tissue mass in malignant fractures as opposed to retropulsed bone, puzzle sign, sharp fracture lines and intravertebral vacuum phenomenon in benign fractures. Similarly, PET scan findings are also distinct – benign fractures have an Standardized Uptake Value (SUV) 2 SDs below liver SUV whereas Malignant fractures SUV of >3–4.7 or 2 SDs above liver SUV.52 In cases where MRI is nondiagnostic, PET-CT due to its high sensitivity and semi-quantitative nature provides better information and may clinch the diagnosis.55
Routine transpedicular biopsies during kyphoplasty or vertebroplasty detect unexpected malignant lesions in 0.4–6% of the patients. Hence, whenever an intervention is planned, it is wise to take biopsy especially in ambiguous imaging findings.56
5.3. Classification of osteoporotic spine fractures
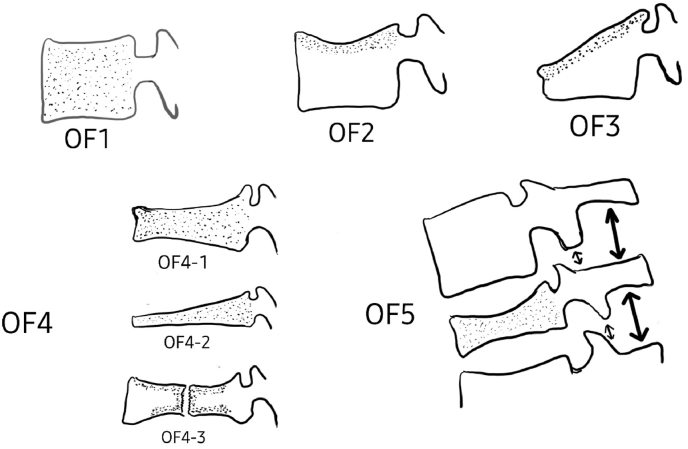
Classification of osteoporotic fractures is also different from fractures in normal vertebrae. A semi-quantitative classification was introduced in 1993 by Genant et al. where there are three types of deformities (wedge, biconcave, crush) and 3 grades of severity.40 Sugita et al. have described a classification system for OVF (5 types based on the initial lateral x-ray films performed after injury: “1. the swelled-front type, 2. the bow type, 3. the projecting type, 4. the concave type and 5. the dented type”).41 On follow-up, they found that types 1, 2 and 3 had a higher incidence of late collapse, with a vacuum cleft seen in the vertebral body. They classified these as predicting a poor prognosis. Schnake et al. introduced a new classification for these fractures, again based on the fracture morphology (OF classification) with 5 subgroups: “OF 1: no vertebral deformation (vertebral body edema in MRI-STIR only), OF 2: deformation without or with only minor involvement of the posterior wall (<1/5), OF 3: deformation with distinct involvement of the posterior wall (>1/5); OF 4: loss of vertebral frame structure, vertebral body collapse, or pincer type fracture, and OF 5: injuries with distraction or rotation”.42 (Fig. 2)
Fig. 2.
Redrawn from: Classification of Osteoporotic Thoracolumbar Spine Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU), Global Spine Journal 2018, Vol.8(2S)46S–49S, DOI:10.1177/2192568217717972.
6. Management –
The studies referred for management of geriatric spine injuries are enumerated in Table 3.
Table 3.
Studies referred for the Management of Geriatric Spinal Fractures.
| S.no. | Authors | Article | Journal | Type of Study | Sample size | Age | Outcome/Conclusion |
|---|---|---|---|---|---|---|---|
| 1 | Arul K et al.10 | Traumatic spinal cord injuries in geriatric population: etiology, management, and complications. | Journal of Spine Surgery. 2019 | Cross-sectional study | 73 | Average 74 years | 4% underwent operative management, SCI severity was lower with advancing age |
| 2 | Chhabra HS et al.51 | Geriatric Spinal Cord Injuires - Surgical Perspective. | ISCoS Textbook on Comprehensive management of Spinal Cord Injuries, Wolters Kluwer India Pvt. Limited. 2015 | Book chapter | NA | NA | The aims of treating spine fractures in the elderly are early mobilization, maintain good respiratory function, maintain general and mental health. Rehabilitation is a major part of the management, maximizing mobilization while managing co-existing medical conditions and counselling regarding slow progress. |
| 3 | Aubrun F et al.52 | The elderly patient and postoperative pain treatment. | Best Practice and Research - Clinical Anaesthesiology. 2007 | Literature review | NA | NA | Multimodal analgesia with analgesic ladder to be optimized, opioids to be minimized, concurrent medications and comorbidities to be considered while planning |
| 4 | Arceo-Mendoza RM et al.53 | Postmenopausal Osteoporosis: Latest Guidelines. | Endocrinology and Metabolism Clinics of North America. 2021 | Clinical Guidelines – AACE/ACE | NA | NA | Medical management of postmenopausal osteoporosis advised as per available evidence |
| 5 | Gheorghita A et al.54 | Long-term experiences of pain after a fragility fracture. | Osteoporosis International. 2018 | Secondary analysis of data collected for other studies | 67 | 47–89 years | Pain influences life even 1 year after fragility fracture |
| 6 | Rizvi S et al.55 | Odontoid fractures: impact of age and comorbidities on surgical decision making | BMC Surg. 2020 | Prospective observational cohort study | 337 | Median 80 years | Comorbidities and age should be considered for inclusion in the decision tree for the choice of treatment for odontoid fractures in future guidelines |
| 7 | Chapman J et al.56 | The AOSpine North America geriatric odontoid fracture mortality study: A retrospective review of mortality outcomes for operative versus nonoperative treatment of 322 patients with long-term follow-up. | Spine. 2013 | Retrospective study | 332 | Mean 81.8 years | Surgical treatment of type II odontoid fracture in this elderly population did not negatively impact survival, even after adjusting for age, sex, and comorbidities. The data suggest a trend toward improved longer-term survival for operatively treated over nonoperatively treated patients. |
| 8 | Smith RM et al.24 | Atlas Fractures. | Clinical Spine Surgery: A Spine Publication. 2018 | Review article | NA | NA | In general, most isolated atlas fractures are stable with a low risk of mortality and neurological complications. |
| Primary management of stable isolated fractures is mainly non-operative care via external cervical immobilization. Surgery is primarily recommended for complicated fractures such as comminuted fractures, patients displaying neurological compromise, or those with Jefferson fractures with transverse ligament ruptures. | |||||||
| 9 | Osterhoff G et al.60 | Recommendations for diagnosis and treatment of odontoid fractures in geriatric patients. | Zeitschrift fur Orthopadie und Unfallchirurgie. Georg Thieme Verlag; 2020 | Review article | NA | NA | Fractures type 1, type 3 and non-displaced fractures type 2 according to Anderson/DʼAlonzo can be treated conservatively. For fractures Anderson/DʼAlonzo type 2, surgical treatment offers the advantage of higher bone healing rates. |
| 10 | Schroeder GD et al.61 | A systematic review of the treatment of geriatric type II Odontoid fractures. | Neurosurgery. 2015 | Systematic review | 1233 | NA | Well-selected patients >60 years of age undergoing surgical treatment for a type II odontoid fracture have a decreased risk of short-term and long-term mortality without an increase in the risk of complications |
| 11 | Pal D et al.62 | Type II odontoid fractures in the elderly: An evidence-based narrative review of management. | European Spine Journal. 2011 | Narrative Review | NA | NA | While it is true that osseous union is a measurable absolute outcome measure, the views of several authors that stable fibrous union may be adequate aim of treatment in the elderly cannot be ignored |
| 12 | Peck GE et al.63 | Cervical spine immobilization in the elderly: a literature review. | British Journal of Neurosurgery. 2018 | Literature review | NA | NA | Multiple complications are associated with c-spine immobilization in the elderly – raised ICP, pressure sores, dysphagia, breathing difficulties, delirium etc. |
| 13 | Grabel ZJ et al.64 | Thoracolumbar spinal fractures associated with ground level falls in the elderly: An analysis of 254,486 emergency department visits. | J Clin Orthop Trauma. 2020 | Retrospective (Database) study | 2,54,486 | 82.0 ± 7.6 years | 38.5% had multiple injuries, 72.6% were female, 77.7% treated non-operatively, inpatient mortality was 2.14% |
| 14 | Kweh BTS et al.65 | The Role of Spinal Orthoses in Osteoporotic Vertebral Fractures of the Elderly Population (Age 60 Years or Older): Systematic Review. | Global Spine Journal. 2021 | Systematic review | 1157 | 77.2 years | The use of spinal orthoses in neurologically intact OVCF patients >60 years of age results in improved stability, reduced kyphotic deformity, superior functional outcomes |
| 15 | Abe T et al.66 | Initial hospitalization with rigorous bed rest followed by bracing and rehabilitation as an option of conservative treatment for osteoporotic vertebral fractures in elderly patients: a pilot one arm safety and feasibility study. | Arch Osteoporos. 2018 | Prospective, pilot one arm safety and feasibility study | 154 | Mean 81.2 years | Rigorous in-hospital bed rest initially, followed by a meticulous rehabilitation program with brace was safe and feasible for patients with OVCF, without severe adverse events related to bed rest. |
| 16 | Cankaya D et al.67 | Clinical and radiological outcomes of conservative treatment after stable post-traumatic thoracolumbar fractures in elderly: Is it really best option for all elderly patients? | Annals of Medicine and Surgery. 2015 | 21 | Mean 71.3 years | Conservative treatment can be challenge in the elderly with post-traumatic compression fractures, especially in in the junctional region. These cases are at a risk of conservative treatment failure. | |
| 17 | Park HY et al.39 | Clinical and Radiologic Features of Osteoporotic Spine Fracture with Delayed Neurologic Compromises. | World Neurosurg. 2018 | Retrospective case-control study | 30 vs 30 | 73.5 years vs 71.9 years | Although most OVFs could be successfully treated by conservatively, it is necessary to note that complicated OVFs can be developed under certain conditions, requiring further intervention |
| 18 | Mattie R et al.68 | Comparing percutaneous vertebroplasty and conservative therapy for treating osteoporotic compression fractures in the thoracic and lumbar spine a systematic review and meta-analysis. | Journal of Bone and Joint Surgery - American Volume. 2016 | Systematic review and meta-analysis | 1048 (531 vertebroplasty vs 517 conservatively treated) | na | Significant pair relief in vertebroplasty patients compared to conservatively managed patients upto 1 year post injury |
| 19 | Zhang T et al.69 | Does Percutaneous Vertebroplasty or Balloon Kyphoplasty for Osteoporotic Vertebral Compression Fractures Increase the Incidence of New Vertebral Fractures? A Meta-Analysis | Pain Physician. 2017 | Systematic review and meta-analysis | 1328 (768 vertebro/kyphoplasty vs 560 non-operative) | na | No risk of increased adjacent/non-adjacent vertebral fractures after vertebroplasty/kyphoplasty procedures |
| 20 | Thomas EN et al.70 | Osteoporotic fracture of the sacrum: Sacroplasty and physical medicine. | Ann Phys Rehabil Med. 2009 | Case report and literature review | 1 | 83 years | Indication, results, complications of scaroplasty are reviewed |
| 21 | Nowak S et al.71 | Incidence of unexpected positive histology in kyphoplasty. | European Spine Journal. 2018 | Retrospective cohort study | 97 | na | 3.1% unexpected positive histology for malignancy rate in kypho/vertebroplasty patients |
| 22 | Liu C et al.72 | Vertebral Compression Fractures—The First Manifestations in the Elderly Acute Lymphoblastic Leukemia. | Geriatr Orthop Surg Rehabil. 2021 | Case report | 1 | 65 years | ALL must be considered in the differential diagnosis of OVCF after low-energy injuries |
| 23 | Delpla A et al.73 | Preventive Vertebroplasty for Long-Term Consolidation of Vertebral Metastases. | Cardiovasc Intervent Radiol. 2019 | Retrospective case-control study | 138 vertebroplasty vs 77 conservatively treated | na | Pathologic fracture in vertebral metastases is significantly high in spite of low SINS score at initial presentation. Quality of vertebroplasty affects the rate of post-procedure pathologic fractures. |
| 24 | Iyer S et al.74 | Management of odontoid fractures in the elderly: A review of the literature and an evidence-based treatment algorithm. | Clinical Neurosurgery. 2018 | Literature review | NA | NA | Most odontoid fractures in the elderly can be managed non-operatively, fibrous union is an acceptable outcome. Surgical management must be undertaken after optimizing the patient. |
| 25 | Kohno M et al.75 | Surgical intervention for osteoporotic vertebral burst fractures in middle-low lumbar spine with special reference to postoperative complications affecting surgical outcomes. | Neurol Med Chir (Tokyo). 2019 | Prospective cohort study | 38 | 74.8 years mean | Instrumented fusion along with augmentation and anti-osteoporotic medications is essential to achieve good outcome in elderly burst fracture patients |
| 26 | Spiegl U et al.76 | Osteoporotic vertebral body fractures of the thoracolumbar spine: indications and techniques of a 360°-stabilization. | European Journal of Trauma and Emergency Surgery. 2017 | Literature review | NA | NA | Anterior and posterior combined instrumentation – indications and results enumerated |
| 27 | Girardo M et al.77 | Long versus Short Segment Instrumentation in Osteoporotic Thoracolumbar Vertebral Fracture. | Asian Spine J. 2021 | Retrospective comparative study | 37 | >65 years | Long- and short-segment fixation of osteoporotic thoracolumbar fractures give similar clinical outcomes, but long segment fixation has fewer mechanical complications |
| 28 | Tandon V et al.78 | Advancements in osteoporotic spine fixation. | J Clin Orthop Trauma. 2020 | Literature review | NA | NA | Various techniques for vertebral augmentation and increasing construct strength in osteoporotic vertebrae enumerated |
| 29 | Kanno H et al.79 | Innovation of Surgical Techniques for Screw Fixation in Patients with Osteoporotic Spine. | J Clin Med. 2022 | Literature review | NA | NA | Various techniques for vertebral augmentation and increasing construct strength in osteoporotic vertebrae enumerated |
| 30 | Fiani B et al.80 | Special considerations to improve clinical outcomes in patients with osteoporosis undergoing spine surgery. | Int J Spine Surg. 2021 | Literature review | NA | NA | Various techniques for vertebral augmentation and increasing construct strength in osteoporotic vertebrae enumerated |
| 31 | Cosman F et al.13 | Spine fracture prevalence in a nationally representative sample of US women and men aged ≥40 years: results from the National Health and Nutrition Examination Survey (NHANES) 2013–2014. | Osteoporosis International. 2017 | Cross-sectional study | 3330 | ≥40 years | Most patients diagnosed with a vertebral fracture would be recommended for osteoporosis treatment based on current guidelines. The choice of therapeutic agent might differ after the diagnosis of vertebral fracture compared to a BMD diagnosis alone, since vertebral fractures suggest a much higher risk for fracture at any BMD. |
| 32 | Kirk B et al.81 | Nutrients to mitigate osteosarcopenia: the role of protein, vitamin D and calcium. | Curr Opin Clin Nutr Metab Care. 2021 | Literature review | NA | NA | Protein intake of 1.2–1.5 g/kg/day,vitamin D 800 IU/day, calcium 1000–1200 mg/day is effective to reduce effects of osteosarcopenia |
| 33 | Nagendra L et al.82 | FRAX-based osteoporosis treatment guidelines for resource-poor settings in India. | Arch Osteoporos. 2021 | Prospective cohort study | 300 | na | Ethnicity specified FRAX scores help optimize osteoporosis treatment in the community |
| 34 | Dupont J et al.83 | Vertebral fractures after denosumab cessation. | Cleve Clin J Med. 2020 | Case report and literature review | 1 | 63 years | Rebound fractures occur after denosumab cessation, within 2–10 months. There is no protocol to stop denosumab with high level evidence. Bisphosphonate bridging may be useful. |
| 35 | Curtis JR et al.84 | Commentary: The five ws of a fracture liaison service: Why, who, what, where, and how? in osteoporosis, we reap what we sow. | Curr Osteoporos Rep. 2013 | Literature review | NA | NA | Feasibility, management issues and organization of fracture liaison services are enumerated |
| 36 | Kelm N et al.85 | Role of Fracture Liaison Service Program in Reducing Refracture Rate in the Elderly Osteoporotic Trauma Patients Presenting With Vertebral Compression Fracture: A Six-Year Study. | American Surgeon. 2021 | Retrospective cohort study | 720 (142 pre-FLS, 578 post-FLS) | Significant reduction in refracture rate is seen with patients after enrolment in FLS (48.9% vs 37%) | |
| 37 | Lorentzon M et al.86 | Osteoporosis and fractures in women: the burden of disease. | Climacteric 2022 | Literature review | NA | NA | Osteoporotic fractures in women cause a high number of DALYs lost and medical expenditure. Prevention is lacking, with only a small proportion of eligible females being prescribed medication. Primary and secondary prevention strategies may be effective reducing the burden. |
Abbreviations.
AACE/ACE – American Association Of Clinical Endocrinologists/American College Of Endocrinology.
BMD – Bone Mineral Density.
DALY – Disability Adjusted Life Years.
FLS – Fracture Liaison Services.
FRAX – Fracture Risk Assessment Tool.
g – grams.
ICP- Intracranial Pressure.
IU – International Units.
Kg - kilograms.
Mg – milligrams.
NA – Not Applicable.
Na – not available.
OVCF – Osteoporotic Vertebral Compression Fracture.
OVF – Osteoporotic Vertebral Fracture.
SINS – Spinal Instability Neoplasia Score.
The aims of treating spine fractures in the elderly are early mobilization, maintain good respiratory function, maintain general and mental health to continue productive life. Various conservative and surgical methods are available for the same. Cervical injuries deserve a special mention as it is the most common spinal fracture in the elderly, and particularly upper cervical region. Health care professionals need to be better educated to evaluate and manage these fractures and refer to specialised spinal injury centres when required. Rehabilitation is a major part of the management, maximizing mobilization while managing co-existing medical conditions and counselling regarding slow progress. It is best achieved by realistic team-based goal planning, expectation management, and emphasizing on task-specific exercises while acknowledging the possibility of limited regain of function.57
6.1. Pain management
Pain management in elderly patients is a major challenge. Evaluation of pain is made difficult due to cognitive impairment and inability to communicate. Frequently pain is underestimated in geriatric patients. There are several cardiac, hepatic-metabolic, neurological considerations before initiating pain medications. Multimodal analgesia must be used with the analgesic ladder starting with acetaminophen, escalating to NSAIDs, low risk opioid agonists like tramadol or codeine and resorting to opioids only when warranted. Analgesics must be prescribed on an ‘as required’ basis rather than continuously. A ‘start low-go slow’ approach is the most prudent one for elderly patients.58 In acute cases, calcitonin can be good tool due to its systemic analgesic properties.59 Many under-treated patients suffer from chronic pain that responds poorly to analgesics and affects the ADLs, sleep and overall energy adversely.87
6.2. Nonsurgical treatment
Fracture Management depends upon multiple factors including comorbidities and frailty. Fracture management can be done conservatively/with vertebral augmentation/surgically.
The decision of the treating clinicians regarding surgical/non-surgical modality is very much dependent on the age and comorbidities as perceived by them,23,88 and there is a significant deviation from the clinical guidelines due to this, leading to a lower rate of surgical management.23 Cervical immobilization is the mainstay of treatment recommendations in most C1 and C2 (type I and III) fractures in older persons.24,60 Many researchers found better survival results with surgery for most type II odontoid fractures.61,62,88 As opposed to soft/hard collars, halo immobilization is associated with a high rate of complications and mortality. Although soft collars restrict less than rigid collars, clinical efficacy in immobilizing may be similar. Complications of rigid external cervical spine immobilization are manifold – pressure sores, reduced FEV1 and FVC, swallowing difficulty, delirium etc.63
In a study, it was found that among more than 2,50,000 thoracolumbar fractures in geriatric population diagnosed in the emergency department the majority (77%) were treated without surgery.64 In thoracolumbar osteoporotic fractures without neurologic deficits, there has been conflicting low level evidence regarding bracing but a recent systematic review found that in patients older than 60 years treated with brace had improved stability, reduced kyphotic deformity and superior functional outcomes. Pain scores were also improved.65 Another study explored the efficacy and safety of absolute bed rest for 2 weeks post trauma followed by mobilization with Jewett orthosis in a small cohort and found no significant adverse events and 63% fracture union at 6 months, suggesting that conservative management is a viable option in these patients.66 However, risks of further fracture collapse and height loss, chronic pain and delayed neurologic deficit must always be kept in mind.39,67
6.3. Percutaneous interventions
Single level stable fractures can be treated conservatively or with percutaneous interventions like vertebroplasty and balloon kyphoplasty. A meta-analysis showed that vertebroplasty in osteoporotic thoracolumbar fractures gives significant pain relief lasting up to 1 year post procedure when compared to conservative management.68 Although there are many studies that quote 10–38% rate of increase in new compression fractures in patients who had vertebroplasty/kyphoplasty, consolidation of evidence showed that there is no increased new fractures in patients treated with percutaneous vertebroplasty/kyphoplasty when compared to patients treated conservatively.69 Osteoporotic fractures of the sacrum may present without trauma history. Sacroplasty under CT or image intensifier guidance similar to vertbroplasty/kyphoplasty may be a good option for pain relief and improvement in mobility.70 Notably, there is a 3–4.9% chance of finding positive malignancy in biopsies from kyphoplasty patients even when the clinical suspicion is minimal and MRI findings do not suggest malignancy. So, sampling for histopathology is warranted in all of the vertebral augmentation patients.71 Possibility of malignancy should be suspected in all patients as vertebral compression fractures may be the first manifestation of lymphoma/leukemia in the elderly.72 In patients with diagnosed vertebral malignancy and without collapse, preventive vertebroplasty is a good option, but even after vertebroplasty, the involved vertebra may collapse – in case of high SINS score >8, poor cement filling and cement not being in contact with the endplates.73
6.4. Surgical treatment
Surgery is commonly advised when the injury is unstable, produces neurologic deficit and the patient is fit to undergo surgery. Among the upper cervical fractures, unstable anterior and posterior ring fractures of C1 (indicated by displaced fractures with combined lateral mass displacement >7 mm, ligament rupture along with fracture, and concomitant fractures of other cervical vertebrae) are warranted surgery. Patients who have undergone unsuccessful conservative treatment with malunion or non-union are also surgical candidates. Depending upon the severity of the injury, surgical options ranging from C1–C2 posterior fusion to cranio-cervical fusion are available.24 Axis fractures have been widely studied in literature, particularly type-II injuries. Most of the pooled data favours operative treatment for type-II fractures while type-I and type-III fractures are preferably managed non-operatively.74 Type-II injuries may be operated via an anterior approach (C2 screw fixation) in the absence of comminution, transverse atlantal ligament injury or unfavourable anatomy of the neck. If any of these contra-indications are present, C1–C2 posterior fixation by any of the described methods should be the choice.74 One level or 2 level pedicle screw fixation with or without cement augmentation and anterior cage insertion may be advised based on Magerl classification, with adequate caution that there may be a high incidence of implant related complications.75 360-degree stabilization may be recommended in 3 column (unstable) thoracolumbar and thoracic fractures to reduce risk of implant failure. Hybrid fixation with cement augmented pedicle instrumentation and kyphoplasty is also highly effective in patients with unstable fractures.76 Long segment fixation may give better x-ray measurements of kyphotic angle and fewer mechanical complications like screw loosening, pullout or PJK but this may not translate to clinical efficacy. A study found that ODI and VAS scores were the same in long or short segment fixation for osteoporotic TL fractures.77 Fixation techniques in elderly patients need to be specialised due to the inherently weak bone. Various techniques to increase the construct strength and reduced chances of implant failure have been described like altering the screw diameter/trajectory, augmenting with PMMA bone cement, using newer screw models like tapered/variable pitch/hydroxyapatite coated screws etc.78 Modification in surgical techniques and construct building has also been described – such as S2AI screws, intrasacral buttress, etc. 79, 80 (Fig. 3, Fig. 4, Fig. 5, Fig. 6)
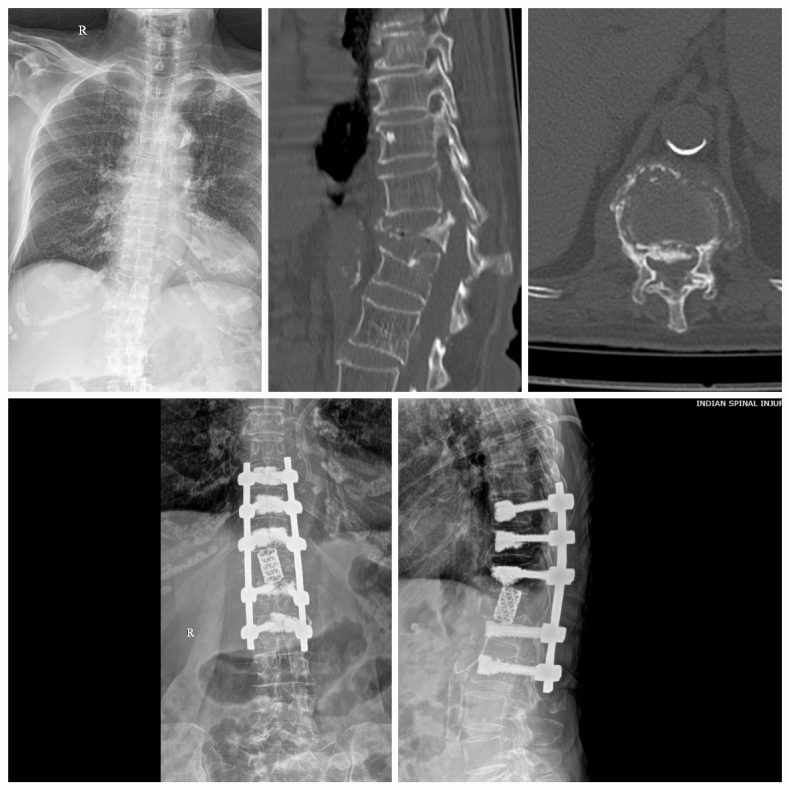
Fig. 3.
A 65-year-old diabetic lady with severe osteoporosis (T-score at LS spine = -4.2) presented with severe low back pain and gradual lower limb weakness after a trivial fall at home. Her L1 osteoporotic fracture was treated with partial corpectomy and anterior cage support, with cement augmented pedicle screw fixation for posterior support. Vertebroplasty was performed at the level proximal to the upper end vertebra to prevent proximal junctional collapse.
Fig. 4.
An 82-year-old retired gynecologist had presented with a chronic history of mid-low back pain after undergoing unsuccessful conservative treatment elsewhere. The patient had partial weakness in her lower limbs and started developing loss of bladder control. Imaging showed a collapsed L1 vertebra. L1 corpectomy and cement-augmented long segment posterior stabilization was done. Intra-operative biopsy only showed bone trabeculae with no evidence of malignancy. She was later started on anti-osteoporotic medication and multimodal rehabilitation was initiated. She improved gradually and was walking with the support of a walker at the last follow-up visit.
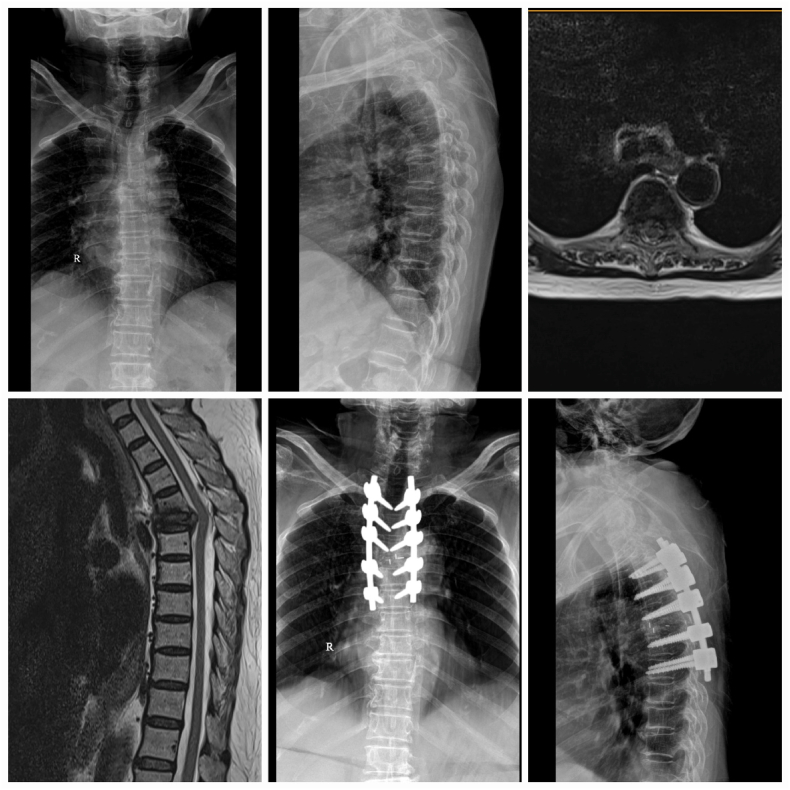
Fig. 5.
A 73-year-old diabetic, hypertensive, hypothyroid, morbidly obese female presented with a short history (5 weeks) of bilateral leg pain and inability to stand and walk after a trivial fall at home. The L4 fracture caused significant neurologic deficit and neuropathic pain consistent with the imaging finding that most of the vertebral canal was involved. L4 partial corpectomy and anterior cage support was done to supplement a long posterior fixation. The L5-S1 interbody fusion was done to prevent later degenerative changes in the disc and failure. She developed unexplained bleeding from multiple sites in the post-operative period and ultimately succumbed 3 weeks later.
Fig. 6.
A 79-year-old lady came to the ER with complaints of acute upper back pain after a history of sudden jerk and fall. Initially the family was hesitant to get her operated but within 2 days of admission she started developing neurologic deficit in both her lower limbs. She was operated with posterior fixation, decompression, corpectomy and poly-ether-ether-ketone (PEEK) cage anterior support. She was transferred to the rehabilitation unit of the hospital where over several months she regained her abillty to walk.
6.5. Osteoporosis treatment
Among the elderly who develop spinal fractures, only 22% have normal bone mineral density at both the hip and the lumbar spine. Thus, osteoporosis is an inseparable part of fracture treatment in the elderly.13 Osteoporosis management is essential for prevention of refractures. WHO criteria for osteoporosis (based on young adult bone density comparison) are well known – classified into normal/osteopenia/osteoporosis/severe osteoporosis. American Association of Clinical Endocrinologists (AACE) guidelines add spine or hip fragility fracture irrespective of BMD in the diagnostic criteria. Non-pharmacologic and pharmacologic treatment must be initiated in all diagnosed patients. Initial screening for secondary causes like metabolic, endocrine, nutritional and drug-induced osteoporosis must be undertaken and corrected if present. Calcium and vitamin D supplementation, fall prevention education, treatment compliance reinforcement need to be done. Randomized trials show that correcting vitamin D and calcium deficiencies increases bone density and reduces fracture risk. Supplementation with proteins and vitamin D over and above the RDA (recommended daily allowance) supports increase in lean muscle mass and lumbar-spine bone density.81 Fracture Risk Assessment Tool (FRAX) can be used to evaluate risk of major osteoporotic fracture and pharmacologic treatment started according to guidelines.59 Country specific FRAX scoring and evaluation criteria may help in optimizing treatment in the population in resource-poor settings.82
Risk stratification can be performed according to guidelines (AACE/ES/ESCEO) into very high risk/high risk/moderate/low risk grades and drugs started accordingly. A broad dictum is to start with anabolic drugs like teriparatide/strontium or newer drugs in very high risk patients. High risk and moderate risk patients may be started with antiresorptive – oral/IV bisphosphonates. Options like calcitonin and hormone replacement therapy may be given on case-to-case basis. Newer drugs like romosozumab (approved for females only currently) and abaloparatide are currently available in the market with multiple studies showing effectiveness.59
If denosumab is stopped after a duration of treatment without bridging with anabolics or bisphosphonates, there is a risk of rebound associated fracture as its effects are reversible. The fracture risk may increase to pre-treatment levels. These fractures are usually seen 2–10 months after the last dose of denosumab. There is currently no evidence on management of these fractures which has led to the absence of any protocols or guidelines for such cases.83
6.6. Post-discharge continuation of care
Fracture liaison services (FLS) have been initiated to streamline the management of osteoporotic fracture patients during and after the hospital stay and to maintain a continuity of care. This service has at its centre a bone health expert who initiates the system in their hospital. Identification of a patient with fragility fracture, diagnosing osteoporosis, educating the patient and family about the condition are the initial steps after the FLS is set up. Once these are done, appropriate medical treatment is initiated and the patient is followed up either directly or through the primary care provider. FLS, due to its systematic institution helps reduce refracture rates and reduce long term health-care costs.84 Studies found significant reduction in the refracture rate of pre-FLS vs post-FLS vertebral fractures.85 Secondary fracture prevention via FLS can be used to increase fracture risk assessment, bone density evaluation and prescribing anti-osteoporosis drugs in order to reduce fracture incidence. In additional, primary prevention must be undertaken by community case-finding methods using fracture risk prediction tools (FRAX), and identify women without fracture but with high risk, to reduce fracture numbers even more.86
7. Complications
The studies reviewed for data on complications both of geriatric spinal injuries and the management of geriatric spine fractures are enumerated in Table 4.
Table 4.
Studies referred for the Complications of Geriatric Spinal Fractures.
| S.no. | Authors | Article | Journal | Type of Study | Sample size | Age | Outcome/Conclusion |
|---|---|---|---|---|---|---|---|
| 1 | Radcliff K et al.89 | Cervical spine surgery complications and risks in the elderly. | Spine (Phila Pa 1976). 2017 | Retrospective (Database) study | 1519 (decompression), 1273 (fusion) | na | High risk of respiratory complications, delirium, nausea/vomiting in elderly patients. Age is a risk factor (>85 years) for acute delirium. |
| 2 | Kobayashi K et al.90 | Postoperative Complications Associated With Spine Surgery in Patients Older Than 90 Years: A Multicenter Retrospective Study. | Global Spine Journal. 2018 | Retrospective cohort study | 35 | >90 years | High rate of medical complications after surgery (stroke, MI, PE) |
| 3 | Jubert P et al.91 | Complications of upper cervical spine trauma in elderly subjects. A systematic review of the literature. | Orthopaedics and Traumatology: Surgery and Research. 2013 | Systematic review | 857 | >60 years | Nearly all upper cervical injuries were odontoid fractures, 57% treated surgically, median mortality rate was 9.2%, median short term complication rate was 15.4%, non-union rate was 10–12% |
| 4 | Watanabe T et al.92 | Perioperative complications of spine surgery in patients 80 years of age or older: A multicenter prospective cohort study. | Journal of Neurosurgery: Spine. 2020 | Prospective cohort study | 270 | >80 years | Overall minor complication rate 20% |
| 5 | Spiegl UJ et al.93 | Effect of subsequent vertebral body fractures on the outcome after posterior stabilization of unstable geriatric fractures of the thoracolumbar spine. | BMC Musculoskelet Disord. 2022 | Retrospective cohort study | 73 | Mean 72 years | Patients with subsequent vertebral body fractures were associated with significant worse outcomes |
| 6 | Spiegl UJ et al.94 | Midterm outcome after posterior stabilization of unstable Midthoracic spine fractures in the elderly. | BMC Musculoskelet Disord. 2021 | Retrospective cohort study | 59 | 76.9 ± 6.3 years | 35.6% patients (were older, had poorer ASA scores) died within 5 years of trauma. In the remaining, 35.3% had subsequent vertebral fractures – those with long segment fixation had fewer subsequent fractures. |
| 7 | Iyer S et al.74 | Management of odontoid fractures in the elderly: A review of the literature and an evidence-based treatment algorithm. | Clinical Neurosurgery. 2018 | Literature review | NA | NA | Overall poor prognosis for associated morbidity and mortality in the geriatric age group with odontoid fractures underscores the key importance of medical co-management and optimization of bone health following diagnosis |
| 8 | Amanat M et al.95 | Neurological conditions associated with spinal cord injury. | Informatics in Medicine Unlocked. 2019 | Literature review | NA | All age ranges | SCI patients are at a high risk of stroke, cognitive impairment dementia, etc. |
| 9 | Park HY et al.39 | Clinical and Radiologic Features of Osteoporotic Spine Fracture with Delayed Neurologic Compromises. | World Neurosurg. 2018 | Retrospective case-control study | 30 vs 30 | 73.5 years vs 71.9 years | Delayed neurologic deficits may occur in elderly patients who have initially undetected spinal fractures |
| 10 | McColl MA et al.96 | A house of cards: Women, aging and spinal cord injury. | Spinal Cord. 2002 | Editorial | NA | NA | Females with SCI are at a higher risk of multiple socioeconomic adverse effects like poor employment, reduced mobility, reduced likelihood of getting personal care from caregivers, reduced access to preventive health services, etc. |
| 11 | Arul K et al.10 | Traumatic spinal cord injuries in geriatric population: etiology, management, and complications | Journal of Spine Surgery. 2019 | Cross-sectional study | 73 | Average 74 years | The complication rate in this population is high and due to complex causes |
| 12 | Jörgensen S et al.97 | Depressive symptoms among older adults with long-term spinal cord injury: Associations with secondary health conditions, sense of coherence, coping strategies and physical activity. | J Rehabil Med. 2017 | Cross-sectional study | 122 | 63 years | With a mean time of 24 years post SCI, 29% patients have clinically significant depressive symptoms, 5% have probable depression |
| 13 | Krause JS et al.98 | Depression after spinal cord injury: Relation to gender, ethnicity, aging, and socioeconomic. | Arch Phys Med Rehabil. 2000 | Cross-sectional study | 1391 | na | Depression after SCI is correlated to aging |
| 14 | Chung MC et al.99 | Cord Injury, Posttraumatic Stress, and Locus of Control Among the Elderly: A Comparison with Young and Middle–Aged Patients. | . Psychiatry: Interpersonal and Biological Processes. 2006 | Cross-sectional study | 62 | na | PTSD symptoms are prevalent in all age groups but the elderly are significantly more socially dysfunctional |
| 15 | Dryden DM et al.100 | Depression following Traumatic Spinal Cord Injury. | Neuroepidemiology. 2005 | Prospective cohort study | 201 | na | Pre-injury depression, complete injury and substance abuse predispose to depression in SCI patients |
Abbreviations.
ASA – American Society Of Anesthesiologists.
MI – Myocardial Infarction.
NA – Not Applicable.
Na – not available.
PE – Pulmonary Embolism.
PTSD – Post-Traumatic Stress Disorder.
SCI - Spinal Cord Injury.
7.1. Complications – surgical
Cervical spine surgery, either decompression or fusion procedures, entails a high complication rate in the elderly as discovered by a medicare data study by Radcliff et al. They found respiratory complications (12.1%–14.6%), urinary retention (8.2%–9.1%), acute delirium (5.3%–6.0%), and nausea/vomiting (2.8%–3.1%) were the most common, with older patients at a higher risk of respiratory complications and acute delirium, and males at higher risk of urinary retention.89 Nonagenarians are at a risk of postoperative delirium as well as major complications like cerebral infarcts, angina and pulmonary embolism.90 Long-term complication of upper cervical fractures (most commonly odontoid fracture) is non-union – whether operated or not.91 Whereas the study by Radcliff et al. was a large database study that found major complications, there are other smaller cohort studies of specialised populations that found different results. In patients older than 80 years a study found minor complications (including anemia and delirium), surgery related complications (dural tear, wound infection/dehiscence) and implant related complications to be the most common, in a heterogenous mixture of cervical, thoracic and lumbar level surgeries.92
Post-surgical spine fracture is also a special consideration as it effects outcomes. There may be subsequent spinal fractures in 19.2–35.3% of elderly spine trauma patients treated with posterior fixation.93,94
7.2. Complications - other
Non-operative treatment of odontoid fractures may lead to non-union, which is commonly asymptomatic but sometimes may cause chronic neck pain, C1–C2 instability with myelopathy and may cause acute cord injury from subsequent falls.74 Elderly SCI patients have a high risk of other neurologic complications as well. They are at a higher risk of stroke with a 3-fold increase when compared to normal population. There is a 13-fold increased risk of cognitive impairment. Other disorders like multiple sclerosis, seizure disorder, Parkinsonism, multiple sclerosis and restless leg syndrome are also much more common in this population.95 Delayed neurologic deficits may occur in elderly patients who have initially undetected spinal fractures. Predictors of this late spinal cord compromise are posterior vertebral wall involvement, unstable fracture with non-union, aortic calcification, and midthoracic level fractures among others.39
Older women with SCI have a distinct disadvantage when compared to men. Several factors like higher incidence of UTIs, being prone to postmenopausal osteoporosis over and top of which SCI induced osteoporosis develops, contribute to this. These women are less likely to be employed – impairing financial freedom, less likely to be cared by a spouse and less likely to use transportation independently. Access to regular preventive care services is also extremely hampered with pap smears, mammograms and pelvic examinations missed in most of these patients.96
7.3. Complications -secondary (Psychosocial)
The most common cause of spinal cord injury (SCI) in the elderly is spinal trauma.10 Among all SCI patients, 29%–48% have clinically significant depression and advanced age has a positive correlation with the presence and severity of depression.97,98 Elderly patients with PTSD following SCI are significantly more socially dysfunctional than younger counterparts.99 The highest risk of depression is in those with permanent neurologic deficits, prior history of depression and substance abuse history.100 Variance in depressive symptoms is influenced by inconsistent acceptance of their condition, neuropathic pain, activities participated in leisure time as well as secondary health conditions.97
8. Outcomes
The studies referred for data on outcomes of geriatric spine injuries are discussed briefly in Table 5.
Table 5.
Studies referred for the Outcomes of Geriatric Spinal Fractures.
| S.no. | Authors | Article | Journal | Type of Study | Sample size | Age | Outcome/Conclusion |
|---|---|---|---|---|---|---|---|
| 1 | Zhou J et al.101 | Long-term clinical outcomes following surgical management of cervical spine fractures in elderly patients. | Interdiscip Neurosurg. 2018 | Retrospective cohort study | 107 | 65–75 years, >75 years | Length of stay, mortality during after admission, mental status decline are similar in <75-year-olds and >75-year-olds |
| 2 | Spiegl UJ et al.94 | Midterm outcome after posterior stabilization of unstable midthoracic spine fractures in the elderly. | BMC Musculoskelet Disord. 2021 | Retrospective cohort study | 59 | 76.9 ± 6.3 years | The occurrence of further vertebral fractures was associated with poor outcomes. |
| 3 | Sasagawa T et al.102 | A multicenter study of 1-year mortality and walking capacity after spinal fusion surgery for cervical fracture in elderly patients. | BMC Musculoskelet Disord. 2022 | Prospective cohort study | 313 | ≥65 years | 8% mortality rate in 1 year (higher CCI, higher AIS score, long surgical time were risk factors), 33% deteriorated walking capacity compared to pre-trauma (more severe AIS, low albumin and hemoglobin, longer fusions were risk factors) |
| 4 | Kohno M et al.75 | Surgical intervention for osteoporotic vertebral burst fractures in middle-low lumbar spine with special reference to postoperative complications affecting surgical outcomes. | Neurol Med Chir (Tokyo). 2019 | Prospective cohort study | 38 | Mean - 74.8 years | Posterior instrumented fusion leads to a good clinical outcome; especially when supplemented with some augmentation techniques, together with appropriate anti-osteoporotic medications. |
| 5 | Nagassima Rodrigues Dos Reis K et al.3 | Changing Demographic Trends in spine trauma: The presentation and outcome of Major Spine Trauma in the elderly. | Surgeon. 2021 | Epidemiologic (Database) study – local TARN | 669 | >65 vs < 65 years | Orthopaedic spinal injuries in older people is associated with a significantly higher mortality rate as well as a longer duration of hospitalization. |
| 6 | Irwin ZN et al.103 | Variations in Injury Patterns, Treatment, and Outcome for Spinal Fracture and Paralysis in Adult Versus Geriatric Patients. | Spine (Phila Pa 1976). 2004 | Retrospective cohort study | 6029 adult vs 3973 geriatric | 16–64 years vs ≥ 65 years | 26.5% elderly patients had ≥1 comorbidities, higher 60-day mortality, less severe overall injury |
| 7 | Malik SA et al.104 | Evaluation of morbidity, mortality and outcome following cervical spine injuries in elderly patients. | European Spine Journal. 2008 | Cross-sectional study | 107 | Mean −74 years | Outcome of the injury was related to increasing age, co-morbidities and the severity of neurological deficit. Particularly, low-energy injuries pose a high risk for cervical spine injury in the elderly population. |
| 8 | Gulati A et al.105 | Functional outcome and discharge destination in elderly patients with spinal cord injuries. | Spinal cord. 2011 | Retrospective cohort study | 30 | Mean −73 years | Elderly patients with a traumatic spinal cord injury can benefit from a dedicated spinal cord rehabilitation centre. However this population does pose acute management and rehabilitation challenges. |
| 9 | Jawa RS et al.19 | Spinal Fractures in Older Adult Patients Admitted After Low-Level Falls: 10-Year Incidence and Outcomes. | J Am Geriatr Soc. 2017 | Retrospective registry review | 4202 | ≥65 years | In the elderly, more spinal fracture patients went to acute/subacute rehabilitation and fewer were discharged home |
| 10 | Bank M et al.16 | Age and Other Risk Factors Influencing Long-Term Mortality in Patients With Traumatic Cervical Spine Fracture. | Geriatr Orthop Surg Rehabil. 2018 | Epidemiologic (Database) study | 632 | >64 years vs < 64 years | Long-term survival of patients more than 65 years was also found to be significantly reduced |
| 11 | Lau D et al.106 | Value of aggressive surgical and intensive care unit in elderly patients with traumatic spinal cord injury. | Neurosurg Focus. 2019 | Retrospective cohort study | 106 (83 young, 23 elderly) | na | The elderly had a higher rate of cervical injuries, higher complication rates (1.7 x that of younger patients), higher mortality (10.8 x that of younger patients) |
| 12 | Mora-Boga R et al.107 | Características clínicas y pronóstico de la lesión medular traumática en pacientes mayores de 75 años. | Neurocirugia. 2021 | Retrospective comparative study | 103 | >75 years | In-hospital mortality is high in elderly patients sustaining traumatic SCI |
| 13 | Bokhari AR et al.108 | Morbidity and mortality in cervical spine injuries in the elderly. | ANZ J Surg. 2019 | Retrospective cohort study | 225 | 79.7 years | Most common fracture was odontoid fracture, 24% were operated, operative group had higher pneumonia, arrhythmia and respiratory failure rates. There is a high mortality rate (18.5% operated patients and 12.9% non-operative patients) |
| 14 | Soon EL et al.109 | Factors impacting mortality in geriatric patients with acute spine fractures: A 12-year study of 613 patients in Singapore. | Asian Spine J. 2019 | Retrospective cohort study | 613 | 85.7 ± 4.5 years | 10.4% mortality at 1 year, risk factors – older age at trauma, male sex, higher AIS grade |
| 15 | Daneshvar P et al.110 | Spinal cord injuries related to cervical spine fractures in elderly patients: Factors affecting mortality. | Spine Journal. 2013 | Retrospective cohort study | 37 | >60 years | 38% in-hospital mortality, main cause – respiratory failure, injury at or above C4 was associated with 7.1 times higher risk of mortality |
| 16 | Barkay G et al.111 | Early surgery for thoracolumbar extension-type fractures in geriatric patients with ankylosing disorders reduces patient complications and mortality. | Spine Journal. 2022 | Retrospective cohort study | 50 | >65 years | Patients who had surgery within 72 h of presentation had less mortality than those who were operated >72 h later |
Abbreviations.
NA – Not Applicable.
Na – not available.
SCI- Spinal Cord Injury.
CCI – Charlson Comorbidity Index.
AIS – ASIA Impairment Scale (American Spinal Injury Association).
TARN – Trauma Audit and Research Network.
8.1. Outcomes - surgical
The rate of fusion in surgically treated elderly (>65-year age) cervical spine fracture patients was found to be satisfactory after a minimum follow-up of 11.9 months in a study, where the authors also observed that there was no difference in fusion between >75-year and <75-year age old patients in this cohort.101 In a study of midthoracic fracture surgery in the elderly, the researchers found that most patients (41.1% ± 17.6%) had a mild or moderate disability as per the Oswestry Disability Index (ODI), with 8.8% having crippling back pain during a median follow-up of 56.6 months. They also found that 12 patients who had subsequent post-operative vertebral fractures were frailer, were initially treated with short segment fixation, and had higher ODI scores. They observed a final median reduction loss of 5°.94 A study from Japan found that 33% of operated elderly cervical spine fracture patients had reduced walking capacity 1 year after the surgery. They found higher AIS grade, hypoproteinaemia and longer fusions to be predictive of reduced walking capacity.102 In geriatric patients, after surgical management of spine fractures, even though there is a good rate of neurologic improvement, postoperative complications were high due to post-operative vertebral collapse and implant failure.75 Even though patients aged more than 60 years have higher 60-day mortality than younger patients, surgical intervention may reduce mortality in them.103
8.2. Outcomes - neurologic and general
Outcome in the elderly after spinal fractures and spinal cord injuries is not favourable when compared to general population.3,103, 104, 105 In the elderly, more spinal fracture patients went to acute/subacute rehabilitation and fewer were discharged home than non-spinal fracture patients.19 Among the elderly, there are also differences between young elderly and old elderly populations. A 10-year follow-up study found that the patients aging 65–79 years have higher grade of neurologic deficits and complication rates when compared to 80 years or older individuals.10
Failure of treatment with conservative management has been reported widely. In a systematic review of 6 studies, as many as 17.5% of the patients suffered treatment failure. Among these, 36.3% were subsequent vertebral fractures, 32.4% had significant functional disability at follow-up, and 31.4% had progression of kyphotic deformity. Older age, previous history of vertebral compression fractures, BMD at lumbar spine, Cobb angle and vertebral height loss were found to be contributing factors for treatment failure.112 Other studies found potential risk factors for the progression of OVCF - thoraco-lumbar junction fractures, swelling type and the bow-shaped fracture morphology, and a linear black signal pattern on STIR images. On the other hand, concave type fractures and post-traumatic fractures had lower risks of fracture progression.113 Risk factors for each specific complication were also delineated - ‘hypointense-wide-type’ and complete body signal on T2 weighted MRI and presence of intravertebral cleft (for vertebral collapse progression), thoraco-lumbar level, middle column involvement, confined high-intensity pattern and diffuse low intensity pattern on T2 weighted MRI (for non-union), thoraco-lumbar fracture and superior endplate fracture (for kyphotic deformity) and >42% sagittal canal occupancy by retropulsed fragment, >15° difference in kyphosis on dynamic lateral x-rays (for neurologic impairment).114 Others also additionally classified risk factors into patient related and radiological - age>73 years, T-score < −2.95, body mass index more than 23 and a modified frailty index of more than 2.5 define patients at high risk of failure. Posterior vertebral body wall involvement, high initial height loss, midportion type fracture, intravertebral cleft, thoraco-lumbar junctional fracture, fracture involvement of both endplates were radiologic fracture characteristics that predisposed to failure.115
8.3. Outcomes - survival and mortality
Long-term survival of patients more than 65 years was also found to be significantly reduced.16 The risk of complications in patients older than 70 years was reported to be 1.7 times than that of younger individuals and the risk of death up to 10.8 times more.106 Patients older than 65 years stayed for longer durations in the hospital and also had higher 30-day in-hospital mortality rate much higher than general population.3 A six-fold higher incidence of death, higher costs, higher rates of readmission were found in those older than 65 years.15 The in-hospital mortality may exceed 34% in patients older than 75 years.107 Notably, as compared to younger counterparts, the risk of pneumonia, arrhythmias and respiratory failure are much higher in elderly patients, which may contribute to mortality.108 On regression analysis, older age at presentation, male sex, AIS grade A-C were found to be independent risk factors for increased mortality.109 The risk of in-hospital mortality is as high as 38% in some studies. The leading cause of death is respiratory failure. There is no significant correlation between death and pre-injury comorbidities or whether or not the patient had a surgery. With injuries at or above C4 there is 7.1 times higher risk of death, with complete SCI producing 5.1 times higher risk of dying than incomplete injury.110 In patients with rigid spines with extension injuries, it has been found that early surgery (within 72 h of injury) reduced the rate of peri-operative complications and mortality at 6 months.111
9. Conclusions –
Spinal fractures in the elderly are on the rise, at par with the global upsurge in the aged population. The proportion of the elderly among the spinal injured is also increasing, posing a unique challenge for clinicians. Spinal fractures in the elderly are biomechanically different from fractures in younger adults, and need separate classification. They are commonly asymptomatic but where symptomatic affect the well-being all the same, have poor detectability by clinical examination and standard clinical guidelines may not be applicable. Comorbidities, high co-existence of rigid spine, polypharmacy and frailty complicate the management of these patients. The lower incidence of neurologic involvement makes a high proportion of these injuries amenable to non-operative management. These injuries carry a high risk of respiratory, vascular, wound and delayed neurologic complications and also a high mortality rate due to the frailty of geriatric patients. The outcomes after surgery or conservative treatment are not as good as in the younger population. Moreover, depression and post-traumatic stress and family burden complicate the care of the patients. Efforts to mitigate all these poor prognostic factors undertaken after anticipating these, may improve outcomes in this vulnerable patient group. Post-hospital care in the form of fracture liaison services, when used efficiently, are effective in reducing recurrent spine fractures and reducing morbidity.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Aditya Sunder, Email: adityaorthosurgeon@gmail.com.
H.S. Chhabra, Email: drhschhabra@gmail.com.
Aayush Aryal, Email: aayushkaryal@gmail.com.
References
- 1.Shifting demographics. https://www.un.org/en/un75/shifting-demographics
- 2.Baidwan N.K., Naranje S.M. Epidemiology and recent trends of geriatric fractures presenting to the emergency department for United States population from year 2004–2014. Publ Health. 2017;142:64–69. doi: 10.1016/j.puhe.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 3.Nagassima Rodrigues Dos Reis K., McDonnell J.M., Ahern D.P., Evans S., Gibbons D., Butler J.S. Changing demographic trends in spine trauma: the presentation and outcome of major spine trauma in the elderly. Surgeon. 2021 doi: 10.1016/j.surge.2021.08.010. Published online. [DOI] [PubMed] [Google Scholar]
- 4.Bonne S., Schuerer D.J.E. Trauma in the older adult. Epidemiology and evolving geriatric trauma principles. Clin Geriatr Med. 2013;29(1):137–150. doi: 10.1016/j.cger.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Lin P.C., Wu N.C., Su H.C., Hsu C.C., Chen K.T. Comprehensive comparison between geriatric and nongeriatric patients with trauma. Medicine (United States). 2022;101(7) doi: 10.1097/MD.0000000000028913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ensrud K.E. Epidemiology of fracture risk with advancing age. J Gerontol Ser A Biol Sci Med Sci. 2013;68(10):1236–1242. doi: 10.1093/gerona/glt092. [DOI] [PubMed] [Google Scholar]
- 7.Ikpeze T.C., Mesfin A. Spinal cord injury in the geriatric population: risk factors, treatment options, and long-term management. Geriatr Orthop Surg Rehabil. 2017;8(2):115–118. doi: 10.1177/2151458517696680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van der Jagt-Willems H.C., van Hengel M., Vis M., et al. Why do geriatric outpatients have so many moderate and severe vertebral fractures? Exploring prevalence and risk factors. Age Ageing. 2012;41(2):200–206. doi: 10.1093/ageing/afr174. [DOI] [PubMed] [Google Scholar]
- 9.Jabbour P., Fehlings M., Vaccaro A.R., Harrop J.S. Traumatic spine injuries in the geriatric population. Neurosurg Focus. 2008;25(5) doi: 10.3171/FOC.2008.25.11.E16. [DOI] [PubMed] [Google Scholar]
- 10.Arul K., Ge L., Ikpeze T., Baldwin A., Mesfin A. Traumatic spinal cord injuries in geriatric population: etiology, management, and complications. J Spine Surg. 2019;5(1):38–45. doi: 10.21037/jss.2019.02.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ballane G., Cauley J.A., Luckey M.M., El-Hajj Fuleihan G. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int. 2017;28(5):1531–1542. doi: 10.1007/s00198-017-3909-3. [DOI] [PubMed] [Google Scholar]
- 12.Marwaha R.K., Tandon N., Gupta Y., et al. The prevalence of and risk factors for radiographic vertebral fractures in older Indian women and men: Delhi Vertebral Osteoporosis Study (DeVOS) Arch Osteoporosis. 2012;7(1-2):201–207. doi: 10.1007/s11657-012-0098-8. [DOI] [PubMed] [Google Scholar]
- 13.Cosman F., Krege J.H., Looker A.C., et al. Spine fracture prevalence in a nationally representative sample of US women and men aged ≥40 years: results from the National Health and Nutrition Examination Survey (NHANES) 2013-2014. Osteoporos Int. 2017;28(6):1857–1866. doi: 10.1007/s00198-017-3948-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li Y., Yan L., Cai S., Wang P., Zhuang H., Yu H. The prevalence and under-diagnosis of vertebral fractures on chest radiograph. BMC Muscoskel Disord. 2018;19(1) doi: 10.1186/s12891-018-2171-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson J.R., Cronin S., Fehlings M.G., et al. Epidemiology and impact of spinal cord injury in the elderly: results of a fifteen-year population-based cohort study. J Neurotrauma. 2020;37(15):1740–1751. doi: 10.1089/neu.2020.6985. [DOI] [PubMed] [Google Scholar]
- 16.Bank M., Gibbs K., Sison C., et al. Age and other risk factors influencing long-term mortality in patients with traumatic cervical spine fracture. Geriatr Orthop Surg Rehabil. 2018;9 doi: 10.1177/2151459318770882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCaughey E.J., Purcell M., Mclean A.N., et al. Changing demographics of spinal cord injury over a 20-year period: a longitudinal population-based study in Scotland. Spinal Cord. 2016;54(4):270–276. doi: 10.1038/sc.2015.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wáng Y.X.J., Lentle B.C. Radiographic osteoporotic vertebral fractures in elderly men: a brief review focusing on differences between the sexes. Quant Imag Med Surg. 2020;10(9):1863–1876. doi: 10.21037/QIMS-2020-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jawa R.S., Singer A.J., Rutigliano D.N., et al. Spinal fractures in older adult patients admitted after low-level falls: 10-year incidence and outcomes. J Am Geriatr Soc. 2017;65(5):909–915. doi: 10.1111/jgs.14669. [DOI] [PubMed] [Google Scholar]
- 20.Lomoschitz F.M., Blackmore C.C., Mirza S.K., Mann F.A. Cervical spine injuries in patients 65 Years old and older. Am J Roentgenol. 2002;178(3):573–577. doi: 10.2214/ajr.178.3.1780573. [DOI] [PubMed] [Google Scholar]
- 21.Wang H., Xiang Q., Li C., Zhou Y. 2013. Multiple-Level Noncontiguous Spinal Fractures Difference between the Young and the Elderly.www.jspinaldisorders.com [DOI] [PubMed] [Google Scholar]
- 22.Smith S., Purzner T., Fehlings M. The epidemiology of geriatric spinal cord injury. Top Spinal Cord Inj Rehabil. 2010;15(3):54–64. doi: 10.1310/sci1503-54. [DOI] [Google Scholar]
- 23.Rizvi S.A.M., Helseth E., Rønning P., et al. Odontoid fractures: impact of age and comorbidities on surgical decision making. BMC Surg. 2020;20(1) doi: 10.1186/s12893-020-00893-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith R.M., Bhandutia A.K., Jauregui J.J., Shasti M., Ludwig S.C. Atlas fractures. Clin Spine Surg: A Spine Publ. 2018;31(7):278–284. doi: 10.1097/BSD.0000000000000631. [DOI] [PubMed] [Google Scholar]
- 25.Kim J., Lee E., Kim S., Lee T.J. Economic burden of osteoporotic fracture of the elderly in South Korea: a national survey. Value Health Reg Issues. 2016;9:36–41. doi: 10.1016/j.vhri.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 26.Jones L., Singh S., Edwards C., Goyal N., Singh I. Prevalence of vertebral fractures in CTPA's in adults aged 75 and older and their association with subsequent fractures and mortality. Geriatrics. 2020;5(3) doi: 10.3390/GERIATRICS5030056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goode T., Young A., Wilson S.P., Katzen J., Wolfe L.G., Duane T.M. Evaluation of cervical spine fracture in the elderly: can we trust our physical examination? Am Surg. 2014;80(2):182–184. doi: 10.1177/000313481408000228. [DOI] [PubMed] [Google Scholar]
- 28.Healey C.D., Spilman S.K., King B.D., Sherrill J.E., Pelaez C.A. Journal of Trauma and Acute Care Surgery. Lippincott Williams and Wilkins; 2017. Asymptomatic cervical spine fractures: current guidelines can fail older patients; pp. 119–125. 83. [DOI] [PubMed] [Google Scholar]
- 29.Katoh H., Okada E., Yoshii T., et al. A comparison of cervical and thoracolumbar fractures associated with diffuse idiopathic skeletal hyperostosis—a nationwide multicenter study. J Clin Med. 2020;9(1) doi: 10.3390/jcm9010208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hiyama A., Katoh H., Sakai D., Sato M., Tanaka M., Watanabe M. Prevalence of diffuse idiopathic skeletal hyperostosis (DISH) assessed with whole-spine computed tomography in 1479 subjects. BMC Muscoskel Disord. 2018;19(1) doi: 10.1186/s12891-018-2108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Okano I., Tachibana T., Nishi M., et al. Conservative treatment for stable low-energy thoracolumbar vertebral fractures in nonfused segments among elderly patients with diffuse idiopathic skeletal hyperostosis: a matched case-control study. Medicine (United States) 2019;98(24) doi: 10.1097/MD.0000000000016032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yoshihara H., Nadarajah V., Horowitz E. Prevalence and characteristics of thoracic diffuse idiopathic skeletal hyperostosis in 3299 black patients. Sci Rep. 2021;11(1) doi: 10.1038/s41598-021-01092-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shah N.G., Keraliya A., Nunez D.B., et al. Injuries to the rigid spine: what the spine surgeon wants to know. Radiographics. 2019;39(2):449–466. doi: 10.1148/rg.2019180125. [DOI] [PubMed] [Google Scholar]
- 34.Teunissen F.R., Verbeek B.M., Cha T.D., Schwab J.H. Spinal cord injury after traumatic spine fracture in patients with ankylosing spinal disorders. J Neurosurg Spine. 2017;27(6):709–716. doi: 10.3171/2017.5.SPINE1722. [DOI] [PubMed] [Google Scholar]
- 35.Lee J., Chang G., Kang H., et al. Impact of bone mineral density on the incidence of age-related vertebral fragility fracture. J Kor Med Sci. 2020;35(17) doi: 10.3346/JKMS.2020.35.E116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee S.K., Jun D.S., Lee D.K., Baik J.M. Clinical characteristics of elderly people with osteoporotic vertebral compression fracture based on a 12-year single-center experience in Korea. Geriatrics. 2022;7(6) doi: 10.3390/geriatrics7060123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Takahashi T., Takada T., Narushima T., Tsukada A., Ishikawa E., Matsumura A. Correlation between bone density and lumbar compression fractures. Gerontol Geriatr Med. 2020;6 doi: 10.1177/2333721420914771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Watt J., Crilly R. Location of vertebral fractures is associated with bone mineral density and history of traumatic injury. Calcif Tissue Int. 2017;100(4):412–419. doi: 10.1007/s00223-017-0244-9. [DOI] [PubMed] [Google Scholar]
- 39.Park H.Y., Ahn J.H., Ha K.Y., et al. Clinical and radiologic features of osteoporotic spine fracture with delayed neurologic compromises. World Neurosurg. 2018;120:e1295–e1300. doi: 10.1016/j.wneu.2018.09.056. [DOI] [PubMed] [Google Scholar]
- 40.Genant H.K., Wu, Van Kuijk Cornelis, Arid C.Y., Nevitt M.C. 1993. Vertebral Fracture Assessment Using a Semiquantitative Technique; p. 8. [DOI] [PubMed] [Google Scholar]
- 41.Sugita M, Watanabe N, Mikami Y, Hase H, Kubo T. Classification of Vertebral Compression Fractures in the Osteoporotic Spine. [DOI] [PubMed]
- 42.Schnake K.J., Blattert T.R., Hahn P., et al. Classification of osteoporotic thoracolumbar spine fractures: recommendations of the spine section of the German society for Orthopaedics and trauma (DGOU) Global Spine J. 2018;8(2_suppl):46S–49S. doi: 10.1177/2192568217717972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rajasekaran S., Kanna R.M., Schnake K.J., et al. Osteoporotic thoracolumbar fractures-how are they different?-classification and treatment algorithm. J Orthop Trauma. 2017;31:S49–S56. doi: 10.1097/BOT.0000000000000949. [DOI] [PubMed] [Google Scholar]
- 44.Kim H.J., Park S., Park S.H., et al. Prevalence of frailty in patients with osteoporotic vertebral compression fracture and its association with numbers of fractures. Yonsei Med J. 2018;59(2):317–324. doi: 10.3349/ymj.2018.59.2.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carlstrom L.P., Helal A., Perry A., Lakomkin N., Graffeo C.S., Clarke M.J. Too frail is to fail: frailty portends poor outcomes in the elderly with type II odontoid fractures independent of management strategy. J Clin Neurosci. 2021;93:48–53. doi: 10.1016/j.jocn.2021.08.027. [DOI] [PubMed] [Google Scholar]
- 46.Kessler R.A., Ramos RD. la G., Purvis T.E., et al. Impact of frailty on complications in patients with thoracic and thoracolumbar spinal fracture. Clin Neurol Neurosurg. 2018;169:161–165. doi: 10.1016/j.clineuro.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 47.Veronesi F., Borsari V., Martini L., et al. The impact of frailty on spine surgery: systematic review on 10 years clinical studies. Aging Dis. 2021;12(2):625–645. doi: 10.14336/AD.2020.0904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Malgo F., Hamdy N.A.T., Ticheler C.H.J.M., et al. Value and potential limitations of vertebral fracture assessment (VFA) compared to conventional spine radiography: experience from a fracture liaison service (FLS) and a meta-analysis. Osteoporos Int. 2017;28(10):2955–2965. doi: 10.1007/s00198-017-4137-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mauch J.T., Carr C.M., Cloft H., Diehn F.E. Review of the imaging features of benign osteoporotic and malignant vertebral compression fractures. Am J Neuroradiol. 2018;39(9):1584–1592. doi: 10.3174/ajnr.A5528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tsujio T., Nakamura H., Terai H., et al. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: a prospective multicenter study. Spine. 2011;36(15):1229–1235. doi: 10.1097/BRS.0b013e3181f29e8d. [DOI] [PubMed] [Google Scholar]
- 51.Downie A., Williams C.M., Henschke N., et al. Red flags to screen for malignancy and fracture in patients with low back pain: systematic review. BMJ (Online) 2013;347 doi: 10.1136/bmj.f7095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mauch J.T., Carr C.M., Cloft H., Diehn F.E. Review of the imaging features of benign osteoporotic and malignant vertebral compression fractures. Am J Neuroradiol. 2018;39(9):1584–1592. doi: 10.3174/ajnr.A5528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Takigawa T., Tanaka M., Sugimoto Y., Tetsunaga T., Nishida K., Ozaki T. Discrimination between malignant and benign vertebral fractures using magnetic resonance imaging. Asian Spine J. 2017;11(3):478–483. doi: 10.4184/asj.2017.11.3.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li Z., Guan M., Sun D., Xu Y., Li F., Xiong W. A novel MRI- and CT-based scoring system to differentiate malignant from osteoporotic vertebral fractures in Chinese patients. BMC Muscoskel Disord. 2018;19(1) doi: 10.1186/s12891-018-2331-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.He X., Zhao L., Guo X., et al. Differential diagnostic value of18F-FDG PET/CT for benign and malignant vertebral compression fractures: comparison with magnetic resonance imaging. Cancer Manag Res. 2018;10:2105–2115. doi: 10.2147/CMAR.S168374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Osterhoff G., Scheyerer M.J., Spiegl U.J.A., Schnake K.J. The role of routine transpedicular biopsies during kyphoplasty or vertebroplasty for vertebral compression fractures in the detection of malignant diseases: a systematic review. Arch Orthop Trauma Surg. 2022 doi: 10.1007/s00402-022-04392-7. Published online April 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chhabra H.S., D'Souza A. In: ISCoS Textbook on Comprehensive Management of Spinal Cord Injuries. first ed. Chhabra H.S., editor. Wolters Kluwer India Pvt. Limited; 2015. Geriatric spinal cord injuires - surgical perspective; pp. 355–371. [Google Scholar]
- 58.Aubrun F., Marmion F. The elderly patient and postoperative pain treatment. Best Pract Res Clin Anaesthesiol. 2007;21(1):109–127. doi: 10.1016/j.bpa.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 59.Arceo-Mendoza R.M., Camacho P.M. Postmenopausal osteoporosis: latest guidelines. Endocrinol Metab Clin North Am. 2021;50(2):167–178. doi: 10.1016/j.ecl.2021.03.009. [DOI] [PubMed] [Google Scholar]
- 60.Osterhoff G., Schnake K., Scheyerer M.J., et al. Recommendations for diagnosis and treatment of odontoid fractures in geriatric patients. Z Orthop Unfall. 2020;158(6):647–656. doi: 10.1055/a-0989-2791. [DOI] [PubMed] [Google Scholar]
- 61.Schroeder G.D., Kepler C.K., Kurd M.F., et al. A systematic review of the treatment of geriatric type II Odontoid fractures. Neurosurgery. 2015;77(4):S6–S14. doi: 10.1227/NEU.0000000000000942. [DOI] [PubMed] [Google Scholar]
- 62.Pal D., Sell P., Grevitt M. Type II odontoid fractures in the elderly: an evidence-based narrative review of management. Eur Spine J. 2011;20(2):195–204. doi: 10.1007/s00586-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Peck G.E., Shipway D.J.H., Tsang K., Fertleman M. Cervical spine immobilisation in the elderly: a literature review. Br J Neurosurg. 2018;32(3):286–290. doi: 10.1080/02688697.2018.1445828. [DOI] [PubMed] [Google Scholar]
- 64.Grabel Z.J., Lunati M.P., Segal D.N., Kukowski N.R., Yoon S.T., Jain A. Thoracolumbar spinal fractures associated with ground level falls in the elderly: an analysis of 254,486 emergency department visits. J Clin Orthop Trauma. 2020;11(5):916–920. doi: 10.1016/j.jcot.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kweh B.T.S., Lee H.Q., Tan T., et al. The role of spinal orthoses in osteoporotic vertebral fractures of the elderly population (age 60 Years or older): systematic review. Global Spine J. 2021;11(6):975–987. doi: 10.1177/2192568220948036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Abe T., Shibao Y., Takeuchi Y., et al. Initial hospitalization with rigorous bed rest followed by bracing and rehabilitation as an option of conservative treatment for osteoporotic vertebral fractures in elderly patients: a pilot one arm safety and feasibility study. Arch Osteoporosis. 2018;13(1) doi: 10.1007/s11657-018-0547-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cankaya D., Yilmaz S., Deveci A., et al. Clinical and radiological outcomes of conservative treatment after stable post-traumatic thoracolumbar fractures in elderly: is it really best option for all elderly patients? Ann Med Surg. 2015;4(4):346–350. doi: 10.1016/j.amsu.2015.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mattie R., Laimi K., Yu S., Saltychev M. Comparing percutaneous vertebroplasty and conservative therapy for treating osteoporotic compression fractures in the thoracic and lumbar spine a systematic review and meta-analysis. Journal of Bone and Joint Surgery - American. 2016;98(12):1041–1051. doi: 10.2106/JBJS.15.00425. [DOI] [PubMed] [Google Scholar]
- 69.Zhang T. Does percutaneous vertebroplasty or balloon kyphoplasty for osteoporotic vertebral compression fractures increase the incidence of new vertebral fractures? A meta-analysis. Pain Physician. 2017;1(21):E13–E28. doi: 10.36076/ppj.2017.1.E13. 1. [DOI] [PubMed] [Google Scholar]
- 70.Thomas E.N., Cyteval C., Herisson C., Leonard L., Blotman F. Osteoporotic fracture of the sacrum: sacroplasty and physical medecine. Ann Phys Rehabil Med. 2009;52(5):427–435. doi: 10.1016/j.rehab.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 71.Nowak S., Müller J., Schroeder H.W.S., Ju Müller. Incidence of unexpected positive histology in kyphoplasty. Eur Spine J. 2018;27(4):847–850. doi: 10.1007/s00586-017-5458-z. [DOI] [PubMed] [Google Scholar]
- 72.Liu C., Shu C. Vertebral compression fractures—the first manifestations in the elderly acute lymphoblastic leukemia. Geriatr Orthop Surg Rehabil. 2021;12 doi: 10.1177/21514593211026803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Delpla A., Tselikas L., De Baere T., et al. Preventive vertebroplasty for long-term consolidation of vertebral metastases. Cardiovasc Intervent Radiol. 2019;42(12):1726–1737. doi: 10.1007/s00270-019-02314-6. [DOI] [PubMed] [Google Scholar]
- 74.Iyer S., Hurlbert R.J., Albert T.J. Management of odontoid fractures in the elderly: a review of the literature and an evidence-based treatment algorithm. Clin Neurosurg. 2018;82(4):419–430. doi: 10.1093/neuros/nyx546. [DOI] [PubMed] [Google Scholar]
- 75.Kohno M., Iwamura Y., Inasaka R., et al. Surgical intervention for osteoporotic vertebral burst fractures in middle-low lumbar spine with special reference to postoperative complications affecting surgical outcomes. Neurol Med -Chir. 2019;59(3):98–105. doi: 10.2176/nmc.oa.2018-0232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Spiegl U., Jarvers J.S., Heyde C.E., Josten C. Osteoporotic vertebral body fractures of the thoracolumbar spine: indications and techniques of a 360°-stabilization. Eur J Trauma Emerg Surg. 2017;43(1):27–33. doi: 10.1007/s00068-016-0751-9. [DOI] [PubMed] [Google Scholar]
- 77.Girardo M., Massè A., Risitano S., Fusini F. Long versus short segment instrumentation in osteoporotic thoracolumbar vertebral fracture. Asian Spine J. 2021;15(4):424–430. doi: 10.31616/asj.2020.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tandon V., Franke J., Kalidindi K.K.V. Advancements in osteoporotic spine fixation. J Clin Orthop Trauma. 2020;11(5):778–785. doi: 10.1016/j.jcot.2020.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kanno H., Onoda Y., Hashimoto K., Aizawa T., Ozawa H. Innovation of surgical techniques for screw fixation in patients with osteoporotic spine. J Clin Med. 2022;11(9):2577. doi: 10.3390/jcm11092577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fiani B., Newhouse A., Sarhadi K.J., Arshad M., Soula M., Cathel A. Special considerations to improve clinical outcomes in patients with osteoporosis undergoing spine surgery. Internet J Spine Surg. 2021;15(2):386–401. doi: 10.14444/8050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kirk B., Prokopidis K., Duque G. Nutrients to mitigate osteosarcopenia: the role of protein, vitamin D and calcium. Curr Opin Clin Nutr Metab Care. 2021;24(1):25–32. doi: 10.1097/MCO.0000000000000711. [DOI] [PubMed] [Google Scholar]
- 82.Nagendra L., Bhavani N., Menon V.U., et al. FRAX-based osteoporosis treatment guidelines for resource-poor settings in India. Arch Osteoporosis. 2021;16(1) doi: 10.1007/s11657-021-00931-8. [DOI] [PubMed] [Google Scholar]
- 83.Dupont J., Luyten F.P., Laurent M.R., Gielen E., Dedeyne L., Dejaeger M. Vertebral fractures after denosumab cessation. Cleve Clin J Med. 2020;87(6):337–338. doi: 10.3949/CCJM.87A.19152. [DOI] [PubMed] [Google Scholar]
- 84.Curtis J.R., Silverman S.L. Commentary: the five ws of a fracture liaison service: why, who, what, where, and how? in osteoporosis, we reap what we sow. Curr Osteoporos Rep. 2013;11(4):365–368. doi: 10.1007/s11914-013-0177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kelm N., Wasfie T., Volk M., et al. American Surgeon; 2021. Role of Fracture Liaison Service Program in Reducing Refracture Rate in the Elderly Osteoporotic Trauma Patients Presenting with Vertebral Compression Fracture: A Six-Year Study. Published online. [DOI] [PubMed] [Google Scholar]
- 86.Lorentzon M., Johansson H., Harvey N.C., et al. Osteoporosis and fractures in women: the burden of disease. Climacteric. 2022;25(1):4–10. doi: 10.1080/13697137.2021.1951206. [DOI] [PubMed] [Google Scholar]
- 87.Gheorghita A., Webster F., Thielke S., Sale J.E.M. Long-term experiences of pain after a fragility fracture. Osteoporos Int. 2018;29(5):1093–1104. doi: 10.1007/s00198-018-4399-7. [DOI] [PubMed] [Google Scholar]
- 88.Chapman J., Smith J.S., Kopjar B., et al. The AOSpine North America geriatric odontoid fracture mortality study: a retrospective review of mortality outcomes for operative versus nonoperative treatment of 322 patients with long-term follow-up. Spine. 2013;38(13):1098–1104. doi: 10.1097/BRS.0b013e318286f0cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Radcliff K., Ong K.L., Lovald S., Lau E., Kurd M. Cervical spine surgery complications and risks in the elderly. Spine (Phila Pa 1976. 2017;42(6):E347–E354. doi: 10.1097/BRS.0000000000001799. [DOI] [PubMed] [Google Scholar]
- 90.Kobayashi K., Imagama S., Sato K., et al. Postoperative complications associated with spine surgery in patients older than 90 Years: a multicenter retrospective study. Global Spine J. 2018;8(8):887–891. doi: 10.1177/2192568218767430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jubert P., Lonjon G., Garreau de Loubresse C. Complications of upper cervical spine trauma in elderly subjects. A systematic review of the literature. J Orthop Traumatol: Surg Res. 2013;99(6 suppl L) doi: 10.1016/j.otsr.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 92.Watanabe T., Kanayama M., Takahata M., et al. Perioperative complications of spine surgery in patients 80 years of age or older: a multicenter prospective cohort study. J Neurosurg Spine. 2020;32(4):622–630. doi: 10.3171/2019.9.SPINE19754. [DOI] [PubMed] [Google Scholar]
- 93.Spiegl U.J., Jarvers J.S., Osterhoff G., et al. Effect of subsequent vertebral body fractures on the outcome after posterior stabilization of unstable geriatric fractures of the thoracolumbar spine. BMC Muscoskel Disord. 2022;23(1):1064. doi: 10.1186/s12891-022-06031-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Spiegl U.J., Hölbing P.L., Jarvers J.S., et al. Midterm outcome after posterior stabilization of unstable Midthoracic spine fractures in the elderly. BMC Muscoskel Disord. 2021;22(1) doi: 10.1186/s12891-021-04049-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Amanat M., Vaccaro A.R., Salehi M., Rahimi-Movaghar V. Neurological conditions associated with spinal cord injury. Inform Med Unlocked. 2019;16 doi: 10.1016/j.imu.2019.100245. [DOI] [Google Scholar]
- 96.McColl M.A. A house of cards: women, aging and spinal cord injury. Spinal Cord. 2002;40(8):371–373. doi: 10.1038/sj.sc.3101332. [DOI] [PubMed] [Google Scholar]
- 97.Jörgensen S., Martin Ginis K.A., Iwarsson S., Lexell J. Depressive symptoms among older adults with long-Term spinal cord injury: associations with secondary health conditions, sense of coherence, coping strategies and physical activity. J Rehabil Med. 2017;49(8):644–651. doi: 10.2340/16501977-2259. [DOI] [PubMed] [Google Scholar]
- 98.Krause J.S., Kemp B., Coker J. Depression after spinal cord injury: relation to gender, ethnicity, aging, and socioeconomic. Arch Phys Med Rehabil. 2000;81(8):1099–1109. doi: 10.1053/apmr.2000.7167. [DOI] [PubMed] [Google Scholar]
- 99.Chung M.C., Preveza E., Papandreou K., Prevezas N. Spinal cord injury, posttraumatic stress, and locus of control among the elderly: a comparison with young and middle–aged patients. Psychiatr Interpers Biol Process. 2006;69(1):69–80. doi: 10.1521/psyc.2006.69.1.69. [DOI] [PubMed] [Google Scholar]
- 100.Dryden D.M., Saunders L.D., Rowe B.H., et al. Depression following traumatic spinal cord injury. Neuroepidemiology. 2005;25(2):55–61. doi: 10.1159/000086284. [DOI] [PubMed] [Google Scholar]
- 101.Zhou J., Agarwal N., Gandhoke G.S., et al. Long-term clinical outcomes following surgical management of cervical spine fractures in elderly patients. Interdiscip Neurosurg. 2018;12:10–14. doi: 10.1016/j.inat.2017.10.003. [DOI] [Google Scholar]
- 102.Sasagawa T., Yokogawa N., Hayashi H., et al. A multicenter study of 1-year mortality and walking capacity after spinal fusion surgery for cervical fracture in elderly patients. BMC Muscoskel Disord. 2022;23(1) doi: 10.1186/s12891-022-05752-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Irwin Z.N., Arthur M., Mullins R.J., Hart R.A. Variations in injury patterns, treatment, and outcome for spinal fracture and paralysis in adult versus geriatric patients. Spine (Phila Pa 1976. 2004;29(7):796–802. doi: 10.1097/01.BRS.0000119400.92204.B5. [DOI] [PubMed] [Google Scholar]
- 104.Malik S.A., Murphy M., Connolly P., O'Byrne J. Evaluation of morbidity, mortality and outcome following cervical spine injuries in elderly patients. Eur Spine J. 2008;17(4):585–591. doi: 10.1007/s00586-008-0603-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gulati A., Yeo C.J., Cooney A.D., McLean A.N., Fraser M.H., Allan D.B. Functional outcome and discharge destination in elderly patients with spinal cord injuries. Spinal Cord. 2011;49(2):215–218. doi: 10.1038/sc.2010.82. [DOI] [PubMed] [Google Scholar]
- 106.Lau D., Dalle Ore C.L., Tarapore P.E., et al. Value of aggressive surgical and intensive care unit in elderly patients with traumatic spinal cord injury. Neurosurg Focus. 2019;46(3) doi: 10.3171/2018.12.FOCUS18555. [DOI] [PubMed] [Google Scholar]
- 107.Mora-Boga R., Canosa-Hermida E., Toral-Guisasola I., et al. Características clínicas y pronóstico de la lesión medular traumática en pacientes mayores de 75 años. Neurocirugia. 2021;32(5):209–216. doi: 10.1016/j.neucir.2020.06.003. [DOI] [PubMed] [Google Scholar]
- 108.Bokhari A.R., Sivakumar B., Sefton A., et al. Morbidity and mortality in cervical spine injuries in the elderly. ANZ J Surg. 2019;89(4):412–417. doi: 10.1111/ans.14875. [DOI] [PubMed] [Google Scholar]
- 109.Soon E.L., Leong A.Z., Chiew J., Kaliya-Perumal A.K., Yu C.S., Oh J.Y.L. Factors impacting mortality in geriatric patients with acute spine fractures: a 12-year study of 613 patients in Singapore. Asian Spine J. 2019;13(4):563–568. doi: 10.31616/asj.2018.0231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Daneshvar P., Roffey D.M., Brikeet Y.A., Tsai E.C., Bailey C.S., Wai E.K. Spinal cord injuries related to cervical spine fractures in elderly patients: factors affecting mortality. Spine J. 2013;13(8):862–866. doi: 10.1016/j.spinee.2013.01.045. [DOI] [PubMed] [Google Scholar]
- 111.Barkay G., Apterman S., Ackshota N., Shtewe A.H., Sissman E., Friedlander A. Early surgery for thoracolumbar extension-type fractures in geriatric patients with ankylosing disorders reduces patient complications and mortality. Spine J Publ online Jan. 2022;1 doi: 10.1016/j.spinee.2022.08.016. [DOI] [PubMed] [Google Scholar]
- 112.Petitt J.C., Desai A., Kashkoush A., et al. Failure of conservatively managed traumatic vertebral compression fractures: a systematic review. World Neurosurg. 2022;165:81–88. doi: 10.1016/j.wneu.2022.06.053. [DOI] [PubMed] [Google Scholar]
- 113.Muratore M., Ferrera A., Masse A., Bistolfi A. Can we predict the progression of vertebral collapse in conservative treatment of osteoporotic vertebral fractures? A 3-Year retrospective study of 180 patients from the emergency department. Internet J Spine Surg. 2020;14(4):641–648. doi: 10.14444/7084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Muratore M., Ferrera A., Masse A., Bistolfi A. Osteoporotic vertebral fractures: predictive factors for conservative treatment failure. A systematic review. Eur Spine J. 2018;27(10):2565–2576. doi: 10.1007/s00586-017-5340-z. [DOI] [PubMed] [Google Scholar]
- 115.Scheyerer M.J., Spiegl U.J.A., Grueninger S., et al. Risk factors for failure in conservatively treated osteoporotic vertebral fractures: a systematic review. Global Spine J. 2022;12(2):289–297. doi: 10.1177/2192568220982279. [DOI] [PMC free article] [PubMed] [Google Scholar]