Abstract
Caffeine (1,3,7-trimethylxanthine, also abbreviated to CAF) is a natural chemical with stimulant effects and is commonly included in many drinks and foods, including coffee, tea, cola, energy drinks, cocoa, chocolates, and so on. Our group previously reported that oral administration of CAF efficiently suppressed the development of intestinal inflammation in a dextran sulfate sodium (DSS)-induced murine acute colitis model by suppressing the expression of chitinase 3-like 1, one of the mammalian chitinases without enzymatic activity. Chitinases are hydrolytic enzymes that break down chitin, a polymer of N-acetylglucosamine, and chitinase-like proteins have no enzymatic activity with preserving chitin-binding ability. CAF binds a cleft of the chitinase active site and plays a role as a pan-chitinase inhibitor. Although CAF showed an anti-inflammatory effect in the above model, oral administration of low-dose CAF with 10% sucrose showed potentially neoplastic effects in colonic epithelial cells in a DSS-induced murine chronic colitis model. In this review, we would like to discuss the pros and cons of coffee/CAF in colonic inflammation and neoplasia with an example of pathological finding.
Keywords: Inflammatory bowel disease, Colitis-associated neoplasms, Sucrose, Caffeine, Chitinase 3-like 1
INTRODUCTION
Coffee is one of the most widely consumed beverages worldwide and is a major source of dietary antioxidants [1]. Several groups have previously reported that coffee or caffeine (1,3,7-trimethyxanthine, also abbreviated to CAF) consumption reduces both the frequency of liver disease [2,3] and the incidence of cancer [4,5]; these effects appear to be mediated by inhibition of cell proliferation [6,7] and enhancement of autophagy via PI3K (phosphatidylinositol-3 kinase)/Akt (protein kinase B)/mTOR inhibition [8]. Some reports strongly suggest the anti-inflammatory and antioxidant effects of coffee extracts and selected constituents (including CAF and kahweol) in intestinal inflammation [9-13]. Although the anti-inflammatory and anti-tumor effects of CAF have been reported by many groups in several organs, the possibility for coffee (but not only CAF) to affect intestinal inflammatory diseases is still controversial, as nicely reviewed by 2 recent review articles [14,15]. Notably, coffee is likely to play a protective role in mucosal inflammation based on a meta-analysis of the association between Crohn’s disease (CD) and beverage intake [16]. However, the biological mechanisms underlying the CAF-mediated effects on colonic epithelial cells (CECs) and colon cancer, especially colitis-associated cancer, remain controversial for almost the past 2 decades [17-21] and have not been fully explained scientifically.
As one of the CAF-oriented research groups, we do not intend to discuss the detail of immunological or biological mechanisms of action on low-dose CAF and sugar (mainly sucrose) combinational administration in the incidence of inflammation-associated carcinogenesis, but we would like to suggest new possibilities for the relationship between the 2 factors in a chronic colitis model, of which may throw a stone into the controversy over the effects of CAF under intestinal inflammatory conditions in this review.
CAF BELONGS TO THE GROUP OF METHYLXANTHINE DERIVATIVES, WHICH ARE KNOWN AS PAN-CHITINASE INHIBITORS
CAF belongs to a group of alkaloid chemicals, so-called methylxanthines, which originated from purine-based xanthine [22]. Methylxanthines, as the name suggests, are methylated derivatives and include compounds such as CAF, theophylline, pentoxifylline (PTXN), aminophylline, theobromine, paraxanthine, 3-isobutyl-methylxanthine, and so on. Several methylxanthine derivatives are known as chitinase inhibitors [23]. Schüttelkopf et al. [24] have demonstrated clearly that 2 linked CAF moieties specifically bind in the active site of pan-family 18 chitinases (which family includes most of the mammalian and bacterial chitinases) and work as the inhibitor of these enzymes, as shown by X-ray crystallography. Interestingly, methylxanthine derivatives, including CAF, PTXN and theophylline, and the family 18 chitinases show a similar form of binding and have a common position for docking revealed by X-ray diffraction analysis [23].
If compared with a parameter of IC50 (half maximal inhibitory concentration), PTXN (126 μmol/L) shows 4 times and 12 times higher chitinase inhibitory effect as compared to CAF (469 μmol/L) and theophylline (1,500 μmol/L), respectively [23]. However, the above 3 methylxanthine derivatives show a significantly lower affinity against fungal chitinase than allosamidin (IC50: 10 μmol/L), a chitinase derived from Candida albicans [23]. Within the mammalian chitinases, enzymatic inactive chitinase 3-like 1 (CHI3L1, also known as YKL-40) has been identified as a critical factor in regulating the innate and acquired immune responses in chronic inflammatory diseases including asthma, chronic obstructive pulmonary disease, and inflammatory bowel disease (IBD) [25-28]. For these reasons, methylxanthine derivatives have the potential to be useful as chitinase inhibitors, including CHI3L1 and acidic mammalian chitinase, in chronic inflammatory disorders as well as inflammation-associated cancers [25,29].
COMMONLY ACCEPTED CONCEPTS AND ACTUAL EXAMPLES ABOUT THE COFFEE/CAF INTAKE IN GENERAL
CAF is the most widely recognized psychoactive compound in the world and is found in a wide variety of beverages and foods, which are consumed by men, women, and children of all ages [30,31]. CAF is also easily absorbed through the digestive tract [32], and the U.S. Food and Drug Administration recommends that CAF has no dangerous adverse effects on health if consumed in amounts up to 400 mg per day (4–5 cups of coffee).
The structural similarity of CAF to adenosine causes it to bind to the adenosine A2A receptor, resulting in the induction of an antagonistic effect of CAF on adenosine, which promotes arousal and insomnia [33-35]. Additionally, CAF has also been postulated to be involved in a wide range of physiological activities, including nonselective inhibition of phosphodiesterase [36], sensitization of calcium channels [37], antagonism of γ-aminobutyric acid receptors,38 stimulation of adrenal corticosteroids [39,40], and improvement of glucose metabolism by enhancing insulin responsiveness through inhibition of glucose absorption [41]. Moderate consumption of CAF (coffee) is thought to have beneficial associations with pain, reduced risk of type 2 diabetes [42,43], Parkinson and Alzheimer disease [44], and reduced risk of developing colon cancer [45], kidney as well as liver diseases (Fig. 1) [46]. In contrast, the consumption of CAF-rich products has potential risks such as anxiety, insomnia, tremors, and palpitations (Fig. 1).
Fig. 1.
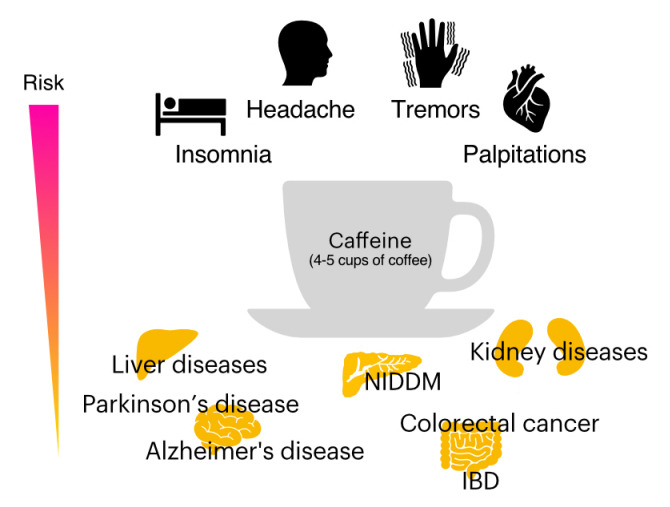
Risk may be altered depending on the intake of high amounts of caffeine (CAF). Diseases for which CAF is associated with decreased risk (advantages) include non-insulin-dependent diabetes mellitus (NIDDM), Parkinson’s disease, Alzheimer’s disease, colorectal cancer, and inflammatory bowel disease (IBD), as well as renal and hepatic disorders. In contrast, diseases for which CAF increases the risk (disadvantages) include insomnia due to CAF’s stimulant effects, headaches, and many other effects. CAF also influences the risk of maintaining pregnancy as well as increasing DNA-damaged sperm.
Bessler et al. [9] have shown that coffee consumption may generally reduce the inflammatory process in the colon and lower the risk of colorectal cancer (CRC) mortality for several mechanistic reasons. In addition, large amounts of coffee consumption (4–6 cups or more per day) have been suggested to reduce the risk of developing colitis-associated cancers [45]. Furthermore, caffeinated coffee consumption has been suggested to reduce the overall risk of CRC [20] and may be associated with reduced recurrence and death in patients with stage III CRC [47]. However, a similarly low incidence of CRC has been observed with a higher intake of decaffeinated coffee [20,48]. Moreover, some studies have reported no useful data to support an association between CAF intake and the risk of developing CRC [49]. Therefore, the association between CAF intake and CRC incidence is still controversial. We have summarized the overall pros and cons of coffee/CAF intake in colonic inflammation and CRC later in this review article.
Moderate coffee intake has been suggested to have beneficial effects (hepatoprotective effect) on various liver diseases, including alcoholic liver disease [50], nonalcoholic fatty liver disease [51,52], liver cirrhosis [53], hepatitis caused by hepatitis B virus [54], and hepatitis C virus [55], possibly by inhibiting the binding of adenosine to its receptor [56,57]. Furthermore, espresso coffee has been shown to have no beneficial effect on liver disease, particularly nonalcoholic fatty liver disease [58]. This may be due to the effect of the addition of sucrose, which is composed of glucose and fructose, to the coffee, which may counteract the effect. Fructose has also been associated with increased severity of liver fibrosis in nonalcoholic steatohepatitis [59]. Thus, the hepatoprotective effect of coffee may depend on various factors, such as the presence or absence of additives (sucrose, etc.), and the impact of these factors should be studied in the future.
ORAL CAF ADMINISTRATION AMELIORATES INTESTINAL INFLAMMATION IN A MOUSE ACUTE DSS-INDUCED COLITIS MODEL
Many studies reported that xanthine derivatives have anti-inflammatory effects. Paiva et al. [60] conducted a systematic review, showing that CAF intake upregulates interleukin (IL)-10 on serum levels. Freedman et al. [61] performed the most extensive cohort study (229,119 men and 173,141 women over 14 years) in 2012 and revealed a dose-dependent inverse association between coffee drinking and total mortality. The primary anti-inflammatory mechanisms result from the nonselective inhibition of phosphodiesterase and the nonselective antagonist of the adenosine receptor. These effects cause the activation of protein kinase A, leading to the inhibition of pro-inflammatory cytokine production, such as tumor necrosis factor α (TNF-α). Nevertheless, some studies insist that CAF consumption induced limited anti-inflammatory effects [62]. Here we reviewed some possible mechanisms of the anti-inflammatory effects of xanthine derivatives on IBD utilizing a colitis mouse model.
IBD is well-known as a group of intestinal inflammatory disorders, which includes CD and ulcerative colitis (UC). Our group previously reported that CECs and macrophages produce CHI3L1 during acute and chronic phases of colitis in the murine colitis models [63]. CHI3L1 in colonic tissue samples of CD and UC patients is upregulated compared to inactive CD and UC patients, and normal individuals positively correlated to the severity of colitis [63]. CHI3L1 has been reported as a significant mediator in many inflammatory disorders, such as asthma, hepatitis, and rheumatoid arthritis [64-67].
It is well-known that dysregulated host-microbial interactions lead to the development of intestinal inflammation in IBD [68,69]. Therefore, possible pathogenic commensal bacteria invasion into CECs could relate to the pathogenesis of IBD. Our group previously revealed that CHI3L1 mediates PI3K/Akt signaling in CECs, enhancing the secretion of IL-8 and TNF-α in a concentration-dependent manner [70]. Several studies have shown that Akt signaling increases in colitis mouse models, CD, and UC patients [71,72]. Conversely, IBD patients on 5-aminosalicylic acid treatment exhibited reduced levels of active phosphorylated Akt in inflamed colitis tissue, suggesting a positive correlation between colitis severity and Akt signal activation [73]. Given these mechanisms, CHI3L1 could play a significant role in colitis in IBD. Therefore, we hypothesized that xanthine derivatives, pan-chitinase inhibitors, could be a novel therapeutic strategy for IBD by suppressing the CHI3L1 expression and activation.
To explore how xanthine derivatives work on IBD, we first conducted in vitro experiments. We incubated SW480 (a human colon cancer cell line) with 2.5 mM or 5 mM of CAF. Subsequently, we treated them with adherent-invasive Escherichia coli (AIEC) as potential pathogenic bacteria in the normal flora. After gentamycin treatment to eliminate the extracellular AIECs, the SW480 were stained with anti-E. coli lipopolysaccharide antibody. The 2.5 mM CAF treatment group showed a reduced number of intracellular AIECs compared to the control group. Moreover, the 5 mM CAF treatment group showed fewer intracellular bacteria [74]. CHI3L1 mRNA expression in SW480 was also reduced in a dose-dependent manner by incubating with CAF [74]. This result suggested that CAF could prevent AIECs invasion into CECs by decreasing the expression of CHI3L1. Theophylline and PTXN showed reduced CHI3L1 mRNA expression in a dose-dependent manner as well [22].
Given these results, we shifted to in vivo experiments using C57BL/6J wild-type (WT) mice, which were purchased from The Jackson Laboratory (Bar Harbor, ME, USA), to examine the anti-inflammation effect of CAF in an acute colitis model. Those mice were first treated with CAF in their drinking water for 7 days, followed by 3.5% dextran sulfate sodium (DSS) with CAF for 5 days. Normal drinking water was given for an additional 7 days until the mice were sacrificed. The mice treated with CAF showed resistance to body weight loss and enhanced body weight and clinical score recovery after DSS treatment compared to the control group of mice [74]. Consistent with the in vitro experiment, mRNA expression of CHI3L1 was completely suppressed in the CAF-treated mice [74]. The colonic histology displayed milder colitis and less inflammatory cell infiltration in the CAF-treated mice compared to the control [74]. Inflammation-associated cytokines (TNF-α, IL-17F, interferon-γ, and IL-4) were decreased, and anti-inflammatory IL-10 was increased in colons of the CAF-treated mice compared to the control [74]. In conclusion, we demonstrated that CAF ameliorates acute DSS-induced colitis by suppressing CHI3L1 expression and its functions.
Similarly, another animal model of colitis treated with other xanthine derivatives exhibited protective effects: Theophylline treatment reduced myeloperoxidase activity and TNF-α, IL-1β, and IL-6 in the colons in an acetic acid-induced colitis rat model [75]. Karatay et al. [76] treated trinitrobenzene sulfonic acidinduced colitis rat model with PTXN intraperitoneal or intrarectal injection. Both groups displayed reduced damage in colitis by PTXN, but the intraperitoneal route was more effective.
Although many in vivo studies support the positive effect of the xanthine derivatives, there is no clear evidence between coffee consumption and human IBD flare. According to the in vivo studies, regular intake of a suitable amount of CAF may prevent intestinal inflammation, especially in IBD gene susceptible individuals. Barthel et al. [77] conducted a questionnaire among IBD patients in Switzerland. Seventy-two point six percent of the total 442 patients regularly drink coffee, and 91% of the group reported no impact of coffee consumption on IBD. Recently, Georgiou utilized Mendelian randomization analysis to evaluate the effect of the exposure factor, smoking, coffee, and alcohol, on CD and UC risk. They revealed that there is no clear evidence that either is related to the risk of CD or UC [78]. Compared to the xanthine derivatives, coffee is a mix of complex compounds; some might work with counteractive effects to the anti-inflammatory mechanisms. Moreover, before it reaches the intestine, coffee is absorbed throughout the digestive tract. Therefore, although CAF may have some effect in colitis mouse models, many factors could explain why coffee intake does not demonstrate apparent protective effects on human IBD.
PROS AND CONS OF COFFEE/CAF INTAKE ON THE EFFECT OF INFLAMMATION AND CARCINOGENESIS IN THE COLON
As summarized in Table 1, the effects of CAF intake on the effect of inflammation and carcinogenesis in the colon are highly controversial. Although coffee/CAF intake seems to reduce the inflammatory responses in the colon [9,74,79], recent 2 reports suggest that CAF consumption is positively associated with the prevalence of CD or UC [75] as well as irritable bowel syndrome [80]. Relationship between coffee/CAF consumption and colonic inflammation has been summarized in Table 1 [81-86].
Table 1.
Relationship between Coffee/CAF Consumption and Colonic Inflammation Based on the Selected Reports in the Past 2 Decades
| Pros or cons | Study type | Outcome | Year | Reference |
|---|---|---|---|---|
| Inconclusive | Metabolomic study | There is a relationship between UC to disturbed glutathione metabolism and CAF metabolism. | 2022 | [81] |
| Cons | Cross-section study | The higher intake of CAF was positively associated with irritable bowel disease prevalence. | 2021 | [80] |
| Cons | Randomized study | CAF consumption is causally associated with the risk for CD or UC. | 2021 | [79] |
| Pros | Population-based study | High CAF intake is protective against UC incidence in Australia. | 2016 | [82] |
| Pros | In vivo (mouse) | CAF-treated mice developed lower tumors and milder inflammation than control in the murine model of colitis. | 2014 | [45] |
| Pros | In vivo (mouse) | Oral CAF administration ameliorates acute colitis in a murine DSS colitis model. | 2014 | [74] |
| Inconclusive | Cohort study | Sugar intake was higher in IBD patients from Eastern Europe than in Western Europe, while no geographic differences regarding CAF intake in these 2 regions. | 2014 | [83] |
| Pros | In vitro (human) | CAF may reduce the inflammatory process in the colon. | 2012 | [9] |
| Pros | Review article | Avoiding CAF would worsen clinical symptoms in IBD patients. | 2011 | [84] |
| Inconclusive | Review article | Coffee and CAF have not been shown to be risk factors for diverticulitis but beneficial effects are still unclear. | 2008 | [85] |
| Pros | In vivo (human) | Serum CAF profiles were significantly prolonged for the pH and time delivery system. | 2004 | [86] |
CAF, caffeine; UC, ulcerative colitis; CD, Crohn’s disease; DSS, dextran sulfate sodium; IBD, inflammatory bowel disease.
An association between coffee/CAF consumption and colonic tumorigenesis has been summarized in Table 2 [87-102]. Within this table, about 84% of studies showed the beneficial effects of coffee/CAF intake for CRC development among the various type of studies. Still, the remaining less than 20% of studies show the opposite or inconclusive effects. In particular, high levels of coffee intake (more than 4 cups of coffee) reduce the risk of CRC recurrence and death in advanced CRC patients [99]. In contrast, high levels of coffee consumption are also associated with the initiation and promotion of CRC development but not associated with the incidence of earlier-stage cancers [49]. Overall, the relationship between coffee/CAF consumption and CRC incidence is largely variable [15] and we cannot explain the reasons logically at present.
Table 2.
Relationship between Coffee/CAF Consumption and Colonic Tumorigenesis Based on the Selected Reports in the Past Decade
| Pros or cons | Study type | Outcome | Year | Reference |
|---|---|---|---|---|
| Pros | In vitro (human) | CAF promotes apoptosis of colon cancer by inactivating PI3K/Akt signaling pathway. | 2022 | [87] |
| Pros | In vivo (mouse) | CAF and chlorogenic acid combination suppress early-stage DMA/DCA-induced colon cancer in mice. | 2022 | [88] |
| Pros | A case-control study | There is a significant protective effect of coffee against CRC in the overall and male populations. | 2022 | [89] |
| Pros | In vitro (human) | Regular coffee consumption may display protective effects against CRC. | 2021 | [90] |
| Cons | Meta-analysis | High levels of CAF intake are associated with the initiation and promotion of CRC. | 2020 | [49] |
| Pros | In vitro (human) | CAF reduced the promotion of the S phase in DLD-1 human colon cancer cells. | 2020 | [91] |
| Inconclusive | Meta-analysis | No evidence of the protective effect of coffee on CRC was found. | 2020 | [92] |
| Pros | Follow-up study | CAF has a protective effect on CRC. | 2020 | [39] |
| Pros | In vitro (human) | Low CAF-containing tea species induce mitochondria-dependent apoptosis in HCT116 human colon cancer cells. | 2020 | [93] |
| Pros | In vitro (human) | CAF induces a significant increase in apoptosis of Dox-treated cells compared with proliferative cells. | 2020 | [94] |
| Pros | Meta-analysis | CAF proved to exert a protective effect in men/women combined and in men alone for CRC but shows ethnicity. | 2019 | [95] |
| Pros | In vivo (rat) | Coffee but not CAF decreased the development of colonic dysplastic crypts in the MNNG-exposed rat model. | 2019 | [96] |
| Pros | Follow-up study | Intake of CAF and decaffeinated coffee after diagnosis of CRC results in a lower risk of CRC-specific death and overall death. | 2018 | [47] |
| Pros | Meta-analysis | Coffee was associated with a probable decreased risk of CRC. | 2017 | [97] |
| Pros | In vitro (human) | Low-dose coffee inhibited the proliferation of Caco-2 cells. | 2017 | [98] |
| Cons | Prospective cohort study | Increased coffee consumption significantly increased colorectal tumor recurrence in the distal colon. | 2016 | [79] |
| Pros | Prospective reported study | High coffee intake may significantly reduce cancer recurrence and death in advanced CRC patients. | 2015 | [99] |
| Cons | In vitro (human) | CAF showed no significant cytotoxic effect in HT29 human CRC cells. | 2015 | [100] |
| Pros | In vitro (human), in vivo (mouse) | CAF-treated mice developed fewer tumors and milder inflammation in a murine model of CRC. | 2014 | [45] |
| Pros | In vitro (human) | Moderate coffee consumption is associated with a lower risk of CRC by reducing estrogen SULT activity. | 2013 | [101] |
| Pros | Review article | Coffee may reduce CRC risk, increasing colon motility and antioxidant status. | 2012 | [102] |
| Pros | Prospective study | Coffee was inversely associated with colon cancer, particularly proximal tumors. | 2012 | [48] |
CAF, caffeine; PI3K/Akt, phosphatidylinositol-3; DMA/DCA, 1,2-dimethylhydrazine/deoxycholic acid; CRC, colorectal cancer; Dox, doxorubicin; MNNG, N-methyl-N-nitro-N-nitrosoguanidine; SULT, sulfotransferases; DLD-1, HCT116, and HT29, human colon cancer cell lines.
ORAL ADMINISTRATION OF CAF WITH SUCROSE SEEMS TO HAVE A POTENT CARCINOGENIC EFFECT IN A MURINE MODEL OF CHRONIC COLITIS
To examine the physiological anti-inflammatory effects of CAF under chronic colitis in vivo, C57Bl/6N WT mice (female, 6–8 weeks old) were purchased from Kyudo Corporation (Tosu, Saga, Japan) and maintained under SPF conditions in the animal facility at Kurume University School of Medicine (Kurume, Fukuoka, Japan). The animal protocols (#2020-049, #2021-042, #2022-035) have been reviewed and approved by the Kurume University School of Medicine Subcommittee on Research Animal Care. Unexpectedly, these mice did not drink 2.5 mM CAF-contained water since CAF may stimulate nerve terminals in the tongue by activating mouse transient receptor potential A1, which results in some pain and bitter sensations in the mice [103]. To overcome the remarkable aversion to CAF-containing water, we diluted the concentration of CAF up to 0.17 mM with water and added 10% sucrose (Sigma-Aldrich, St. Louis, MO, USA). Because 2.5 mM CAF is almost equivalent to 3–5 cups of coffee, 0.17 mM CAF is equivalent to 0.2–0.4 cups of coffee. Surprisingly, this phenomenon was unobserved in our previous experiments performed at Massachusetts General Hospital (Boston, MA, USA) by utilizing C57Bl/6J WT mice (male, 6–8 weeks old), which were purchased from Jackson Laboratories [74]. We have not been able to determine whether the differential responsiveness to CAF is due to differences in mouse subtypes (C57Bl/6J versus C57Bl/6N) or to the housing environment in the US (Massachusetts General Hospital) versus Japan (Kurume University School of Medicine). In our previous experiment, we knew that a CAF concentration of less than 1 mM did not significantly influence CHI3L1 expression in SW480, a human colon cancer cell line [22]. The 0.17 mM CAF concentration we used in this current experiment is about 14.7 times less concentrated than 2.5 mM. It is suspicious that 0.17 mM CAF has enough effects in blocking the biological functions of the family 18 chitinase or affects their transcriptional expression levels compared to the former 2.5 mM CAF administrating experiment performed in 2013 [74].
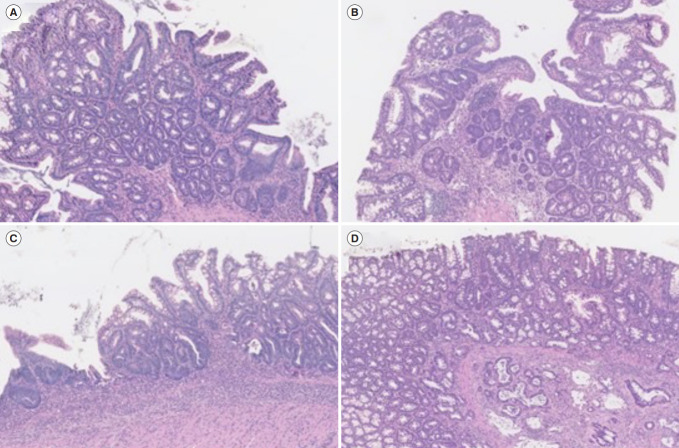
The chronic colitis was induced by the 3 cycles of 2.5% DSS administration. Briefly, mice were treated with 2.5% DSS in water for 4 days and then with 10% sucrose water with or without CAF or PTXN for the next 10 days for 3 cycles. After the 3rd cycle of DSS treatment, all the mice were treated with water without 10% sucrose. Diagnostic criteria for the tumors and colitis were described in Tables 3 and 4, respectively. In general, only 3 cycles of DSS treatments without pretreatment of azoxymethane, a carcinogenic reagent, in C57Bl/6N WT mice do not show carcinogenic changes in CECs. However, 6 out of 7 mice (85.7%) treated with 0.17 mM CAF with 10% sucrose developed dysplasia, carcinoma in situ, or invasive cancer. In contrast, none of the mice treated with 10% sucrose or 1.0 mM PTXN with 10% sucrose had any neoplastic changes in their CECs. Inflammatory scores determined by the hematoxylin and eosin sections are shown in Fig. 2. The average histological scores in 10% sucrose, CAF with 10% sucrose, and PTXN with 10% sucrose were 2.85, 8.42, and 4.3, respectively. This result suggests that low-dose CAF treatment with 10% sucrose induced severe inflammation accompanied by neoplastic changes in CECs during the DSS-induced chronic inflammation in mice. Surprisingly, 2 out of 7 (28.5%) showed carcinogenic changes of colonic epithelium after treatment with low-dose CAF with 10% sucrose after 3 cycles of DSS administration without azoxymethane treatment. Representative images of low-grade dysplasia (Fig. 2A), high-grade dysplasia (Fig. 2B), carcinoma in situ (Fig. 2C), and invasive carcinoma (Fig. 2D) in the low-dose CAF with 10% sucrose-treated mice have been shown.
Table 3.
Tumor Criteria in This Study
| Score | Definition |
|---|---|
| 0 | No tumor |
| 1 | Low-grade dysplasia |
| 2 | High-grade dysplasia |
| 3 | Intra-mucosal adenocarcinoma (carcinoma in situ) |
| 4 | Invasive carcinoma |
| 5 | Distant metastasis |
Table 4.
Inflammatory Criteria of Chronic Dextran Sulfate Sodium-Induced Colitis in This Study
| Sub-criteria | Score |
|---|---|
| Inflammation | 0: None to normal lymphoid aggregates |
| 1: Increased lymphoid aggregates | |
| 2: Cryptitis (neutrophils within crypt epithelium) | |
| 3: Crypt abscess (neutrophils accumulating within crypt lumen, sometimes with crypt rupture) | |
| 4: Ulceration (loss of mucosal components and presence of granulation tissue) | |
| Extent of leukocyte infiltration | 0: None |
| 1: Infiltration confined to the mucosa | |
| 2: Infiltration extending to the submucosa | |
| 3: Transmural extension of infiltration | |
| Severity of leukocyte infiltration | 0: None |
| 1: Mild | |
| 2: Moderate | |
| 3: Severe | |
| The extent of colonic infiltration | 0: None |
| 1: Patchy (focal) | |
| 2: Intermediate | |
| 3: Diffuse (extensive) |
Fig. 2.
Representative histological images of low-dose caffeine (CAF) with sucrose-treated mice. Low-grade dysplasia (A), high-grade dysplasia (B), carcinoma in situ (C), and invasive cancer (D) in the CAF with 10% sucrose-treated mice were shown (all hematoxylin and eosin stain, ×10).
Sucrose consists of fructose and glucose, and there are a couple of papers, which suggest that sucrose or fructose enhances intestinal tumor growth in the colon [104-106]. Further experiments would be required to monitor the exact serum concentration of CAF in the 3 (sucrose, glucose, or fructose-treated) groups in association with the expression of chitinase/CHI3L1 on CECs of mice more strictly. Sugar is commonly used as a sweetener for coffee and other caffeinated foods and beverages, and sucrose is the main component of sugar. For this reason, we urgently need to continue some selected biological and physiological experiments to prove the carcinogenic mechanisms under the additive effects of low-dose CAF and sucrose.
CONCLUSIONS
Coffee is one of the most frequently consumed beverages and is a complex of more than 1,000 bioactive compounds, including CAF. Of note, methylxanthine derivatives, including CAF, PTXN, and theophylline, are known as pan-chitinase inhibitors, which exert anti-inflammatory effects both in vitro and in vivo. In general, regular as well as large amounts of coffee consumption are believed to lower the risks of colonic inflammation and CRC mortality, and there are numerous reports on the relationship between coffee/CAF intake and CRC development. Unexpectedly, we have found that low-dose CAF with 10% sucrose (a major component of sugar) causes carcinogenic changes in CECs under chronic inflammatory conditions. Clarifying the anti-inflammatory as well as pro-tumorigenic mechanisms of CAF at the cellular levels could be the key to seeking more therapeutic as well as prophylactic options in IBD, colitis-associated cancer, and CRC development.
Footnotes
Funding Source
This work has been supported by grants from the Ishibashi Foundation for the Promotion of Science (to Mizoguchi E), the Japan Society for the Women’s Health Science (to Mizoguchi E), the Fukuoka Clinical Medical Research Award (to Mizoguchi E), and the Japanese Society for the Promotion of Science to EM (18K07987 and 21K07996).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Data Availability Statement
Not applicable.
Author Contribution
Conceptualization: Mizoguchi E, Okada T, Sadanaga T, Minagawa T. Data curation: all authors. Formal analysis: Mizoguchi E, Okada T, Minagawa T, Akiba J. Funding acquisition: Mizoguchi E. Investigation: all authors. Methodology: all authors. Project administration: Mizoguchi E, Okada T, Minagawa T. Resources: Mizoguchi E. Software: Mizoguchi E, Okada T, Minagawa T. Supervision: Mizoguchi E, Akiba J. Validation: all authors. Visualization: all authors. Writing - original draft: Mizoguchi E, Okada T, Sadanaga T. Writing - review & editing: all authors. Approval of final manuscript: all authors.
REFERENCES
- 1.Andersen LF, Jacobs DR, Jr, Carlsen MH, Blomhoff R. Consumption of coffee is associated with reduced risk of death attributed to inflammatory and cardiovascular diseases in the Iowa Women’s Health Study. Am J Clin Nutr. 2006;83:1039–1046. doi: 10.1093/ajcn/83.5.1039. [DOI] [PubMed] [Google Scholar]
- 2.Ruhl CE, Everhart JE. Coffee and tea consumption are associated with a lower incidence of chronic liver disease in the United States. Gastroenterology. 2005;129:1928–1936. doi: 10.1053/j.gastro.2005.08.056. [DOI] [PubMed] [Google Scholar]
- 3.Modi AA, Feld JJ, Park Y, et al. Increased caffeine consumption is associated with reduced hepatic fibrosis. Hepatology. 2010;51:201–209. doi: 10.1002/hep.23279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang H, Rouse J, Lukes L, et al. Caffeine suppresses metastasis in a transgenic mouse model: a prototype molecule for prophylaxis of metastasis. Clin Exp Metastasis. 2004;21:719–735. doi: 10.1007/s10585-004-8251-4. [DOI] [PubMed] [Google Scholar]
- 5.Lu YP, Lou YR, Xie JG, et al. Caffeine and caffeine sodium benzoate have a sunscreen effect, enhance UVB-induced apoptosis, and inhibit UVB-induced skin carcinogenesis in SKH-1 mice. Carcinogenesis. 2007;28:199–206. doi: 10.1093/carcin/bgl112. [DOI] [PubMed] [Google Scholar]
- 6.Alao JP, Sunnerhagen P. The ATM and ATR inhibitors CGK733 and caffeine suppress cyclin D1 levels and inhibit cell proliferation. Radiat Oncol. 2009;4:51. doi: 10.1186/1748-717X-4-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kang SS, Han KS, Ku BM, et al. Caffeine-mediated inhibition of calcium release channel inositol 1,4,5-trisphosphate receptor subtype 3 blocks glioblastoma invasion and extends survival. Cancer Res. 2010;70:1173–1183. doi: 10.1158/0008-5472.CAN-09-2886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saiki S, Sasazawa Y, Imamichi Y, et al. Caffeine induces apoptosis by enhancement of autophagy via PI3K/Akt/mTOR/p70S6K inhibition. Autophagy. 2011;7:176–187. doi: 10.4161/auto.7.2.14074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bessler H, Salman H, Bergman M, Djaldetti M. Caffeine alters cytokine secretion by PBMC induced by colon cancer cells. Cancer Invest. 2012;30:87–91. doi: 10.3109/07357907.2011.636113. [DOI] [PubMed] [Google Scholar]
- 10.Bakuradze T, Lang R, Hofmann T, et al. Antioxidant effectiveness of coffee extracts and selected constituents in cell-free systems and human colon cell lines. Mol Nutr Food Res. 2010;54:1734–1743. doi: 10.1002/mnfr.201000147. [DOI] [PubMed] [Google Scholar]
- 11.Jaquet M, Rochat I, Moulin J, Cavin C, Bibiloni R. Impact of coffee consumption on the gut microbiota: a human volunteer study. Int J Food Microbiol. 2009;130:117–121. doi: 10.1016/j.ijfoodmicro.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 12.Kim JY, Kim DH, Jeong HG. Inhibitory effect of the coffee diterpene kahweol on carrageenan-induced inflammation in rats. Biofactors. 2006;26:17–28. doi: 10.1002/biof.5520260103. [DOI] [PubMed] [Google Scholar]
- 13.Ng SC, Tang W, Leong RW, et al. Environmental risk factors in inflammatory bowel disease: a population-based case-control study in Asia-Pacific. Gut. 2015;64:1063–1071. doi: 10.1136/gutjnl-2014-307410. [DOI] [PubMed] [Google Scholar]
- 14.Iriondo-DeHond A, Uranga JA, Del Castillo MD, Abalo R. Effects of coffee and its components on the gastrointestinal tract and the brain-gut axis. Nutrients. 2020;13:88. doi: 10.3390/nu13010088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nehlig A. Effects of coffee on the gastro-intestinal tract: a narrative review and literature update. Nutrients. 2022;14:399. doi: 10.3390/nu14020399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang Y, Xiang L, He J. Beverage intake and risk of Crohn disease: a meta-analysis of 16 epidemiological studies. Medicine (Baltimore) 2019;98:e15795. doi: 10.1097/MD.0000000000015795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Michels KB, Willett WC, Fuchs CS, Giovannucci E. Coffee, tea, and caffeine consumption and incidence of colon and rectal cancer. J Natl Cancer Inst. 2005;97:282–292. doi: 10.1093/jnci/dji039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang R, Dashwood WM, Löhr CV, et al. Protective versus promotional effects of white tea and caffeine on PhIP-induced tumorigenesis and beta-catenin expression in the rat. Carcinogenesis. 2008;29:834–839. doi: 10.1093/carcin/bgn051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bae JM, Shim SR. Coffee consumption and pancreatic cancer risk: a meta-epidemiological study of population-based cohort studies. Asian Pac J Cancer Prev. 2020;21:2793–2798. doi: 10.31557/APJCP.2020.21.9.2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Um CY, McCullough ML, Guinter MA, Campbell PT, Jacobs EJ, Gapstur SM. Coffee consumption and risk of colorectal cancer in the Cancer Prevention Study-II Nutrition Cohort. Cancer Epidemiol. 2020;67:101730. doi: 10.1016/j.canep.2020.101730. [DOI] [PubMed] [Google Scholar]
- 21.Mackintosh C, Yuan C, Ou FS, et al. Association of coffee intake with survival in patients with advanced or metastatic colorectal cancer. JAMA Oncol. 2020;6:1713–1721. doi: 10.1001/jamaoncol.2020.3938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee IA, Kamba A, Low D, Mizoguchi E. Novel methylxanthine derivative-mediated anti-inflammatory effects in inflammatory bowel disease. World J Gastroenterol. 2014;20:1127–1138. doi: 10.3748/wjg.v20.i5.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rao FV, Andersen OA, Vora KA, Demartino JA, van Aalten DM. Methylxanthine drugs are chitinase inhibitors: investigation of inhibition and binding modes. Chem Biol. 2005;12:973–980. doi: 10.1016/j.chembiol.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 24.Schüttelkopf AW, Andersen OA, Rao FV, et al. Screening-based discovery and structural dissection of a novel family 18 chitinase inhibitor. J Biol Chem. 2006;281:27278–27285. doi: 10.1074/jbc.M604048200. [DOI] [PubMed] [Google Scholar]
- 25.Lee CG, Da Silva CA, Dela Cruz CS, et al. Role of chitin and chitinase/chitinase-like proteins in inflammation, tissue remodeling, and injury. Annu Rev Physiol. 2011;73:479–501. doi: 10.1146/annurev-physiol-012110-142250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kawada M, Hachiya Y, Arihiro A, Mizoguchi E. Role of mammalian chitinases in inflammatory conditions. Keio J Med. 2007;56:21–27. doi: 10.2302/kjm.56.21. [DOI] [PubMed] [Google Scholar]
- 27.Mazur M, Zielińska A, Grzybowski MM, Olczak J, Fichna J. Chitinases and chitinase-like proteins as therapeutic targets in inflammatory diseases, with a special focus on inflammatory bowel diseases. Int J Mol Sci. 2021;22:6966. doi: 10.3390/ijms22136966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ober C, Chupp GL. The chitinase and chitinase-like proteins: a review of genetic and functional studies in asthma and immune-mediated diseases. Curr Opin Allergy Clin Immunol. 2009;9:401–408. doi: 10.1097/ACI.0b013e3283306533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eurich K, Segawa M, Toei-Shimizu S, Mizoguchi E. Potential role of chitinase 3-like-1 in inflammation-associated carcinogenic changes of epithelial cells. World J Gastroenterol. 2009;15:5249–5259. doi: 10.3748/wjg.15.5249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nawrot P, Jordan S, Eastwood J, Rotstein J, Hugenholtz A, Feeley M. Effects of caffeine on human health. Food Addit Contam. 2003;20:1–30. doi: 10.1080/0265203021000007840. [DOI] [PubMed] [Google Scholar]
- 31.Singh N, Shreshtha AK, Thakur MS, Patra S. Xanthine scaffold: scope and potential in drug development. Heliyon. 2018;4:e00829. doi: 10.1016/j.heliyon.2018.e00829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cappelletti S, Piacentino D, Sani G, Aromatario M. Caffeine: cognitive and physical performance enhancer or psychoactive drug? Curr Neuropharmacol. 2015;13:71–88. doi: 10.2174/1570159X13666141210215655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Varani K, Portaluppi F, Merighi S, Ongini E, Belardinelli L, Borea PA. Caffeine alters A2A adenosine receptors and their function in human platelets. Circulation. 1999;99:2499–2502. doi: 10.1161/01.cir.99.19.2499. [DOI] [PubMed] [Google Scholar]
- 34.Lazarus M, Shen HY, Cherasse Y, et al. Arousal effect of caffeine depends on adenosine A2A receptors in the shell of the nucleus accumbens. J Neurosci. 2011;31:10067–10075. doi: 10.1523/JNEUROSCI.6730-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fredholm BB, Bättig K, Holmén J, Nehlig A, Zvartau EE. Actions of caffeine in the brain with special reference to factors that contribute to its widespread use. Pharmacol Rev. 1999;51:83–133. [PubMed] [Google Scholar]
- 36.Boswell-Smith V, Spina D, Page CP. Phosphodiesterase inhibitors. Br J Pharmacol. 2006;147(Suppl 1):S252–S257. doi: 10.1038/sj.bjp.0706495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guo Y, Zhang Z, Wu HE, Luo ZD, Hogan QH, Pan B. Increased thrombospondin-4 after nerve injury mediates disruption of intracellular calcium signaling in primary sensory neurons. Neuropharmacology. 2017;117:292–304. doi: 10.1016/j.neuropharm.2017.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roca DJ, Schiller GD, Farb DH. Chronic caffeine or theophylline exposure reduces gamma-aminobutyric acid/benzodiazepine receptor site interactions. Mol Pharmacol. 1988;33:481–485. [PubMed] [Google Scholar]
- 39.Mattioli AV, Farinetti A. Espresso coffee, caffeine and colon cancer. World J Gastrointest Oncol. 2020;12:601–603. doi: 10.4251/wjgo.v12.i5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lovallo WR, Farag NH, Vincent AS, Thomas TL, Wilson MF. Cortisol responses to mental stress, exercise, and meals following caffeine intake in men and women. Pharmacol Biochem Behav. 2006;83:441–447. doi: 10.1016/j.pbb.2006.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reis CEG, Dórea JG, da Costa THM. Effects of coffee consumption on glucose metabolism: a systematic review of clinical trials. J Tradit Complement Med. 2018;9:184–191. doi: 10.1016/j.jtcme.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O’Keefe JH, DiNicolantonio JJ, Lavie CJ. Coffee for cardioprotection and longevity. Prog Cardiovasc Dis. 2018;61:38–42. doi: 10.1016/j.pcad.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 43.Moisey LL, Kacker S, Bickerton AC, Robinson LE, Graham TE. Caffeinated coffee consumption impairs blood glucose homeostasis in response to high and low glycemic index meals in healthy men. Am J Clin Nutr. 2008;87:1254–1261. doi: 10.1093/ajcn/87.5.1254. [DOI] [PubMed] [Google Scholar]
- 44.Gabbert C, König IR, Lüth T, et al. Coffee, smoking and aspirin are associated with age at onset in idiopathic Parkinson’s disease. J Neurol. 2022;269:4195–4203. doi: 10.1007/s00415-022-11041-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ma JY, Li RH, Huang K, Tan G, Li C, Zhi FC. Increased expression and possible role of chitinase 3-like-1 in a colitis-associated carcinoma model. World J Gastroenterol. 2014;20:15736–15744. doi: 10.3748/wjg.v20.i42.15736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nieber K. The impact of coffee on health. Planta Med. 2017;83:1256–1263. doi: 10.1055/s-0043-115007. [DOI] [PubMed] [Google Scholar]
- 47.Hu Y, Ding M, Yuan C, et al. Association between coffee intake after diagnosis of colorectal cancer and reduced mortality. Gastroenterology. 2018;154:916–926. doi: 10.1053/j.gastro.2017.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sinha R, Cross AJ, Daniel CR, et al. Caffeinated and decaffeinated coffee and tea intakes and risk of colorectal cancer in a large prospective study. Am J Clin Nutr. 2012;96:374–381. doi: 10.3945/ajcn.111.031328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shojaei-Zarghani S, Yari Khosroushahi A, Rafraf M, Asghari-Jafarabadi M, Azami-Aghdash S. Dietary natural methylxanthines and colorectal cancer: a systematic review and meta-analysis. Food Funct. 2020;11:10290–10305. doi: 10.1039/d0fo02518f. [DOI] [PubMed] [Google Scholar]
- 50.van Dam RM, Hu FB, Willett WC. Coffee, caffeine, and health. N Engl J Med. 2020;383:369–378. doi: 10.1056/NEJMra1816604. [DOI] [PubMed] [Google Scholar]
- 51.Sewter R, Heaney S, Patterson A. Coffee consumption and the progression of NAFLD: a systematic review. Nutrients. 2021;13:2381. doi: 10.3390/nu13072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ebadi M, Ip S, Bhanji RA, Montano-Loza AJ. Effect of coffee consumption on non-alcoholic fatty liver disease incidence, prevalence and risk of significant liver fibrosis: systematic review with meta-analysis of observational studies. Nutrients. 2021;13:3042. doi: 10.3390/nu13093042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Desmond PV, Patwardhan RV, Johnson RF, Schenker S. Impaired elimination of caffeine in cirrhosis. Dig Dis Sci. 1980;25:193–197. doi: 10.1007/BF01308138. [DOI] [PubMed] [Google Scholar]
- 54.Leung WW, Ho SC, Chan HL, Wong V, Yeo W, Mok TS. Moderate coffee consumption reduces the risk of hepatocellular carcinoma in hepatitis B chronic carriers: a case-control study. J Epidemiol Community Health. 2011;65:556–558. doi: 10.1136/jech.2009.104125. [DOI] [PubMed] [Google Scholar]
- 55.Batista MN, Carneiro BM, Braga AC, Rahal P. Caffeine inhibits hepatitis C virus replication in vitro. Arch Virol. 2015;160:399–407. doi: 10.1007/s00705-014-2302-1. [DOI] [PubMed] [Google Scholar]
- 56.Shan L, Wang F, Zhai D, Meng X, Liu J, Lv X. Caffeine in liver diseases: pharmacology and toxicology. Front Pharmacol. 2022;13:1030173. doi: 10.3389/fphar.2022.1030173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Torres DM, Harrison SA. Is it time to write a prescription for coffee? Coffee and liver disease. Gastroenterology. 2013;144:670–672. doi: 10.1053/j.gastro.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 58.Anty R, Marjoux S, Iannelli A, et al. Regular coffee but not espresso drinking is protective against fibrosis in a cohort mainly composed of morbidly obese European women with NAFLD undergoing bariatric surgery. J Hepatol. 2012;57:1090–1096. doi: 10.1016/j.jhep.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 59.Ouyang X, Cirillo P, Sautin Y, et al. Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J Hepatol. 2008;48:993–999. doi: 10.1016/j.jhep.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Paiva C, Beserra B, Reis C, Dorea JG, Da Costa T, Amato AA. Consumption of coffee or caffeine and serum concentration of inflammatory markers: a systematic review. Crit Rev Food Sci Nutr. 2019;59:652–663. doi: 10.1080/10408398.2017.1386159. [DOI] [PubMed] [Google Scholar]
- 61.Freedman ND, Park Y, Abnet CC, Hollenbeck AR, Sinha R. Association of coffee drinking with total and cause-specific mortality. N Engl J Med. 2012;366:1891–1904. doi: 10.1056/NEJMoa1112010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rodas L, Riera-Sampol A, Aguilo A, Martínez S, Tauler P. Effects of habitual caffeine intake, physical activity levels, and sedentary behavior on the inflammatory status in a healthy population. Nutrients. 2020;12:2325. doi: 10.3390/nu12082325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mizoguchi E. Chitinase 3-like-1 exacerbates intestinal inflammation by enhancing bacterial adhesion and invasion in colonic epithelial cells. Gastroenterology. 2006;130:398–411. doi: 10.1053/j.gastro.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 64.Tang H, Fang Z, Sun Y, et al. YKL-40 in asthmatic patients, and its correlations with exacerbation, eosinophils and immunoglobulin E. Eur Respir J. 2010;35:757–760. doi: 10.1183/09031936.00034409. [DOI] [PubMed] [Google Scholar]
- 65.Shan Z, Liu X, Chen Y, et al. Chitinase 3-like-1 promotes intrahepatic activation of coagulation through induction of tissue factor in mice. Hepatology. 2018;67:2384–2396. doi: 10.1002/hep.29733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Matsumoto T, Tsurumoto T. Serum YKL-40 levels in rheumatoid arthritis: correlations between clinical and laborarory parameters. Clin Exp Rheumatol. 2001;19:655–660. [PubMed] [Google Scholar]
- 67.Zhao T, Su Z, Li Y, Zhang X, You Q. Chitinase-3 like-protein-1 function and its role in diseases. Signal Transduct Target Ther. 2020;5:201. doi: 10.1038/s41392-020-00303-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nell S, Suerbaum S, Josenhans C. The impact of the microbiota on the pathogenesis of IBD: lessons from mouse infection models. Nat Rev Microbiol. 2010;8:564–577. doi: 10.1038/nrmicro2403. [DOI] [PubMed] [Google Scholar]
- 69.Uniken Venema WT, Voskuil MD, Dijkstra G, Weersma RK, Festen EA. The genetic background of inflammatory bowel disease: from correlation to causality. J Pathol. 2017;241:146–158. doi: 10.1002/path.4817. [DOI] [PubMed] [Google Scholar]
- 70.Chen CC, Llado V, Eurich K, Tran HT, Mizoguchi E. Carbohydrate-binding motif in chitinase 3-like 1 (CHI3L1/YKL-40) specifically activates Akt signaling pathway in colonic epithelial cells. Clin Immunol. 2011;140:268–275. doi: 10.1016/j.clim.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dahan S, Roda G, Pinn D, et al. Epithelial: lamina propria lymphocyte interactions promote epithelial cell differentiation. Gastroenterology. 2008;134:192–203. doi: 10.1053/j.gastro.2007.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Huang XL, Xu J, Zhang XH, et al. PI3K/Akt signaling pathway is involved in the pathogenesis of ulcerative colitis. Inflamm Res. 2011;60:727–734. doi: 10.1007/s00011-011-0325-6. [DOI] [PubMed] [Google Scholar]
- 73.Managlia E, Katzman RB, Brown JB, Barrett TA. Antioxidant properties of mesalamine in colitis inhibit phosphoinositide 3-kinase signaling in progenitor cells. Inflamm Bowel Dis. 2013;19:2051–2060. doi: 10.1097/MIB.0b013e318297d741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lee IA, Low D, Kamba A, Llado V, Mizoguchi E. Oral caffeine administration ameliorates acute colitis by suppressing chitinase 3-like 1 expression in intestinal epithelial cells. J Gastroenterol. 2014;49:1206–1216. doi: 10.1007/s00535-013-0865-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ghasemi-Pirbaluti M, Motaghi E, Najafi A, Hosseini MJ. The effect of theophylline on acetic acid induced ulcerative colitis in rats. Biomed Pharmacother. 2017;90:153–159. doi: 10.1016/j.biopha.2017.03.038. [DOI] [PubMed] [Google Scholar]
- 76.Karatay E, Gül Utku Ö, Erdal H, et al. Pentoxifylline attenuates mucosal damage in an experimental model of rat colitis by modulating tissue biomarkers of inflammation, oxidative stress, and fibrosis. Turk J Med Sci. 2017;47:348–356. doi: 10.3906/sag-1508-98. [DOI] [PubMed] [Google Scholar]
- 77.Barthel C, Wiegand S, Scharl S, et al. Patients’ perceptions on the impact of coffee consumption in inflammatory bowel disease: friend or foe? A patient survey. Nutr J. 2015;14:78. doi: 10.1186/s12937-015-0070-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Georgiou AN, Ntritsos G, Papadimitriou N, Dimou N, Evangelou E. Cigarette smoking, coffee consumption, alcohol intake, and risk of Crohn’s disease and ulcerative colitis: a Mendelian randomization study. Inflamm Bowel Dis. 2021;27:162–168. doi: 10.1093/ibd/izaa152. [DOI] [PubMed] [Google Scholar]
- 79.Nakamura T, Ishikawa H, Mutoh M, et al. Coffee prevents proximal colorectal adenomas in Japanese men: a prospective cohort study. Eur J Cancer Prev. 2016;25:388–394. doi: 10.1097/CEJ.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 80.Roudi F, Khayyatzadeh SS, Ghazizadeh H, et al. The relationship between dietary intakes and prevalence of irritable bowel syndrome in adolescent girls: a cross-sectional study. Indian J Gastroenterol. 2021;40:220–226. doi: 10.1007/s12664-020-01126-8. [DOI] [PubMed] [Google Scholar]
- 81.Li M, Zhang R, Xin M, et al. Discovery and validation of potential serum biomarkers with pro-inflammatory and DNA damage activities in ulcerative colitis: a comprehensive untargeted metabolomic study. Metabolites. 2022;12:997. doi: 10.3390/metabo12100997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Niewiadomski O, Studd C, Wilson J, et al. Influence of food and lifestyle on the risk of developing inflammatory bowel disease. Intern Med J. 2016;46:669–676. doi: 10.1111/imj.13094. [DOI] [PubMed] [Google Scholar]
- 83.Burisch J, Pedersen N, Cukovic-Cavka S, et al. Environmental factors in a population-based inception cohort of inflammatory bowel disease patients in Europe: an ECCO-EpiCom study. J Crohns Colitis. 2014;8:607–616. doi: 10.1016/j.crohns.2013.11.021. [DOI] [PubMed] [Google Scholar]
- 84.Brown AC, Rampertab SD, Mullin GE. Existing dietary guidelines for Crohn’s disease and ulcerative colitis. Expert Rev Gastroenterol Hepatol. 2011;5:411–425. doi: 10.1586/egh.11.29. [DOI] [PubMed] [Google Scholar]
- 85.Korzenik JR, NDSG Diverticulitis: new frontiers for an old country: risk factors and pathogenesis. J Clin Gastroenterol. 2008;42:1128–1129. doi: 10.1097/MCG.0b013e318188adb1. [DOI] [PubMed] [Google Scholar]
- 86.Bott C, Rudolph MW, Schneider AR, et al. In vivo evaluation of a novel pH- and time-based multiunit colonic drug delivery system. Aliment Pharmacol Ther. 2004;20:347–353. doi: 10.1111/j.1365-2036.2004.02033.x. [DOI] [PubMed] [Google Scholar]
- 87.Zhang X, Huang H, Sun S, et al. Induction of apoptosis via inactivating PI3K/AKT pathway in colorectal cancer cells using aged Chinese Hakka stir-fried green tea extract. Molecules. 2022;27:8272. doi: 10.3390/molecules27238272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bartolomeu AR, Romualdo GR, Lisón CG, et al. Caffeine and chlorogenic acid combination attenuate early-stage chemically induced colon carcinogenesis in mice: involvement of oncomiR miR-21a-5p. Int J Mol Sci. 2022;23:6292. doi: 10.3390/ijms23116292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lu YT, Gunathilake M, Lee J, et al. Coffee consumption and its interaction with the genetic variant AhR rs2066853 in colorectal cancer risk: a case-control study in Korea. Carcinogenesis. 2022;43:203–216. doi: 10.1093/carcin/bgac007. [DOI] [PubMed] [Google Scholar]
- 90.Castaldo L, Izzo L, Narváez A, Rodríguez-Carrasco Y, Grosso M, Ritieni A. Colon bioaccessibility under in vitro gastrointestinal digestion of different coffee brews chemically profiled through UHPLC-Q-Orbitrap HRMS. Foods. 2021;10:179. doi: 10.3390/foods10010179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bai B, Shan L, Wang J, et al. Small molecule 2,3-DCPE induces S phase arrest by activating the ATM/ATR-Chk1-Cdc25A signaling pathway in DLD-1 colon cancer cells. Oncol Lett. 2020;20:294. doi: 10.3892/ol.2020.12157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chapelle N, Martel M, Toes-Zoutendijk E, Barkun AN, Bardou M. Recent advances in clinical practice: colorectal cancer chemoprevention in the average-risk population. Gut. 2020;69:2244–2255. doi: 10.1136/gutjnl-2020-320990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gao X, Li X, Ho CT, et al. Cocoa tea (Camellia ptilophylla) induces mitochondria-dependent apoptosis in HCT116 cells via ROS generation and PI3K/Akt signaling pathway. Food Res Int. 2020;129:108854. doi: 10.1016/j.foodres.2019.108854. [DOI] [PubMed] [Google Scholar]
- 94.El-Far AH, Darwish NH, Mousa SA. Senescent colon and breast cancer cells induced by doxorubicin exhibit enhanced sensitivity to curcumin, caffeine, and thymoquinone. Integr Cancer Ther. 2020;19:1534735419901160. doi: 10.1177/1534735419901160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sartini M, Bragazzi NL, Spagnolo AM, et al. Coffee consumption and risk of colorectal cancer: a systematic review and meta-analysis of prospective studies. Nutrients. 2019;11:694. doi: 10.3390/nu11030694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Soares PV, Kannen V, Jordão Junior AA, Garcia SB. Coffee, but neither decaffeinated coffee nor caffeine, elicits chemoprotection against a direct carcinogen in the colon of Wistar rats. Nutr Cancer. 2019;71:615–623. doi: 10.1080/01635581.2018.1506489. [DOI] [PubMed] [Google Scholar]
- 97.Grosso G, Godos J, Galvano F, Giovannucci EL. Coffee, caffeine, and health outcomes: an umbrella review. Annu Rev Nutr. 2017;37:131–156. doi: 10.1146/annurev-nutr-071816-064941. [DOI] [PubMed] [Google Scholar]
- 98.Nakayama T, Funakoshi-Tago M, Tamura H. Coffee reduces KRAS expression in Caco-2 human colon carcinoma cells via regulation of miRNAs. Oncol Lett. 2017;14:1109–1114. doi: 10.3892/ol.2017.6227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Guercio BJ, Sato K, Niedzwiecki D, et al. Coffee intake, recurrence, and mortality in stage III colon cancer: results from CALGB 89803 (Alliance) J Clin Oncol. 2015;33:3598–3607. doi: 10.1200/JCO.2015.61.5062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Choi DW, Lim MS, Lee JW, et al. The cytotoxicity of kahweol in HT-29 human colorectal cancer cells is mediated by apoptosis and suppression of heat shock protein 70 expression. Biomol Ther (Seoul) 2015;23:128–133. doi: 10.4062/biomolther.2014.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Isshiki M, Ohta H, Tamura H. Coffee reduces SULT1E1 expression in human colon carcinoma Caco-2 cells. Biol Pharm Bull. 2013;36:299–304. doi: 10.1248/bpb.b12-00902. [DOI] [PubMed] [Google Scholar]
- 102.Vitaglione P, Fogliano V, Pellegrini N. Coffee, colon function and colorectal cancer. Food Funct. 2012;3:916–922. doi: 10.1039/c2fo30037k. [DOI] [PubMed] [Google Scholar]
- 103.Nagatomo K, Kubo Y. Caffeine activates mouse TRPA1 channels but suppresses human TRPA1 channels. Proc Natl Acad Sci U S A. 2008;105:17373–17378. doi: 10.1073/pnas.0809769105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Goncalves MD, Lu C, Tutnauer J, et al. High-fructose corn syrup enhances intestinal tumor growth in mice. Science. 2019;363:1345–1349. doi: 10.1126/science.aat8515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jacobsen H, Poulsen M, Dragsted LO, Ravn-Haren G, Meyer O, Lindecrona RH. Carbohydrate digestibility predicts colon carcinogenesis in azoxymethane-treated rats. Nutr Cancer. 2006;55:163–170. doi: 10.1207/s15327914nc5502_7. [DOI] [PubMed] [Google Scholar]
- 106.Wang B, Bobe G, LaPres JJ, Bourquin LD. Dietary carbohydrate source alters gene expression profile of intestinal epithelium in mice. Nutr Cancer. 2009;61:146–155. doi: 10.1080/01635580802372617. [DOI] [PubMed] [Google Scholar]