Abstract
Sialic acids (Sias) are a class of sugar molecules with a parent nine-carbon neuraminic acid, generally present at the ends of carbohydrate chains, either attached to cellular surfaces or as secreted glycoconjugates. Given their position and structural diversity, Sias modulate a wide variety of biological processes. However, little is known about the role of Sias in human adipose tissue, or their implications for health and disease, particularly among individuals following different dietary patterns. The goal of this study was to measure N-Acetylneuraminic acid (Neu5Ac), N-Glycolylneuraminic acid (Neu5Gc), and 2-keto-3-deoxy-d-glycero-d-galacto-nononic acid (KDN) concentrations in adipose tissue samples from participants in the Adventist Health Study-2 (AHS-2) and to compare the abundance of these Sias in individuals following habitual, long-term vegetarian or non-vegetarian dietary patterns. A method was successfully developed for the extraction and detection of Sias in adipose tissue. Sias levels were quantified in 52 vegans, 56 lacto-vegetarians, and 48 non-vegetarians using LC–MS/MS with Neu5Ac-D-1,2,3-13C3 as an internal standard. Dietary groups were compared using linear regression. Vegans and lacto-ovo-vegetarians had significantly higher concentrations of Neu5Ac relative to non-vegetarians. While KDN levels tended to be higher in vegans and lacto-ovo-vegetarians, these differences were not statistically significant. However, KDN levels were significantly inversely associated with body mass index. In contrast, Neu5Gc was not detected in human adipose samples. It is plausible that different Neu5Ac concentrations in adipose tissues of vegetarians, compared to those of non-vegetarians, reflect a difference in the baseline inflammatory status between the two groups. Epidemiologic studies examining levels of Sias in human adipose tissue and other biospecimens will help to further explore their roles in development and progression of inflammatory conditions and chronic diseases.
Subject terms: Glycobiology, Molecular medicine
Introduction
The sialic acids (Sias) are a diverse family of sugar molecules derived from the parent nine-carbon compound, neuraminic acid1–3. Given their position and structural diversity, Sias modulate a wide variety of biological processes relevant to health and disease, and consequently are of growing interest in the field of glycobiology4–6.
N-Acetylneuraminic acid (Neu5Ac) and its hydroxylated derivative N-glycolylneuraminic acid (Neu5Gc) are the most prevalent Sia forms in mammals7. Spontaneously occurring derivatives of Sia are formed by modification of the parent Sia with phosphate, sulphate, lactyl, or acetyl groups4,8,9. Humans, however, do not produce Neu5Gc, because of an absence of cytidine monophosphate-N-acetylneuraminic acid hydroxylase which converts CMP-Neu5Ac to CMP-Neu5Gc3,10. Nevertheless, Neu5Gc can be metabolically incorporated into human tissues from dietary sources, mainly red meats, and dairy products11–13. The more recently described Sia family member, 2-keto-3-deoxy-d-glycero-d-galacto-nononic acid (KDN), is generally expressed in mammals at low levels.
The negatively charged Sias are involved in interactions with Sia-binding proteins in multiple biological processes including immunity and cancer14. Moreover, the negative surface charges of Sias can mask glycan ligands or serve as attachment sites for pathogens and toxins4,15,16. In addition to their presence in various mammalian cells and tissues, Sias may be present in various body fluids including saliva, urine, plasma, milk, and cerebrospinal fluid17–20.
The production and abundance of Sias appears to be site-specific and context dependent8,21. Higher Sia levels may be due either to increased synthesis and dietary intake or due to upregulated sialidase function (releasing free Sia). On the one hand, dietary supplementation in animals was shown to be protective against atherosclerotic and cardiovascular disease (CVD), and associated with lower inflammatory tone22–24. This might suggest that higher levels of Sias have a moderating effect on inflammation. However, Sias are elevated in the serum of patients with coronary artery disease and may correlate with disease severity25. Additionally, increasing levels of Sias have been associated with inflammation, hemolytic-uremic syndrome, diabetes26–28, CVD29–31, and cancer6,32,33. In part, this is consistent with a recognized association between elevated sialidase function and inflammation34–38. In this context, Sias may serve as general indicators of an inflammatory acute-phase response39.
In contrast to serum, limited information is available about Sias in human adipose tissues. In addition to its function as the primary site for excess energy storage, adipose tissue also serves as an endocrine organ synthesizing several biologically active agents involved in the regulation of metabolic homeostasis40,41. The cellular constituents of adipose tissue include adipocytes, blood cells, endothelial cells, pericytes, and adipose precursor cells40,42–44. Excessive adipose accumulation can lead to abnormal secretion of adipocytokines or other signaling molecules, which may trigger processes associated with diabetes, cancer, and cardiovascular diseases (CVDs)40–42,45,46. Adiposity is the basis for increased body mass index (BMI), which is known to be a major risk factor for CVD, diabetes, cancer and other diseases47,48. At present, the functional roles of Sias are unclear in the context of obesity, chronic inflammation, and CVD.
While it is not clear how human dietary patterns impact Sias levels, it seems reasonable to expect that Sias levels are regulated either by components of the diet or by diet-induced changes in adiposity and inflammatory responses. Consumption of red and processed meats, and in some cases dairy, has been associated with heart disease, diabetes, and cancer (particularly colorectal cancer)49,49–52. Vegetarians have more favorable cardiometabolic profiles and lower risks for type 2 diabetes, CVD, and various types of cancers including colorectal, gastrointestinal, breast, prostate, lung and female-specific cancers49,50,53,54. From this perspective, differences in Sias between dietary groups may help to explain the more favorable health outcomes associated with a vegetarian dietary pattern. The extraction and quantification of Sias from human adipose samples, particularly, may shed light on the role of Sias in metabolic health and the development of chronic diseases.
The goal of this study was to determine Neu5Ac, Neu5Gc, and KDN concentrations in adipose tissue samples from participants of the Adventist Health Study-2 (AHS-2) and to compare the abundance of these Sias in 156 individuals who follow habitual, long-term vegetarian or non-vegetarian dietary patterns. In order to accomplish this, a method for measurement of Sias was developed and optimized using LC–MS/MS.
Materials and methods
Materials
The Accucore HILIC column (150 mm × 4.6 mm, 2.6 μm particles) was obtained from Thermo Scientific (Waltham, MA) and connected with an Accucore HILIC precolumn (10 mm × 4.6 mm, 2.6 μm). Ammonium formate, trifluoroacetic acid (TFA), and acetonitrile were obtained from Fisher Scientific (Carlbad, CA). Neu5Ac-D-1,2,3-13C3, KDN, Neu5Ac, Neu5Gc, and methanol were purchased from Sigma-Aldrich (St. Louis, MI), and chloroform was obtained from EMD Millipore (Burlington, MA). Milli-Q water (GenPure Pro ultrapure water system with UV-photo-oxidation and TOC monitor, by Thermo Scientific Inc) was used throughout the study protocol.
Ethical approvals
All procedures associated with this project were conducted following the international ethical standards proposed by the Helsinki protocol for human research and informed consent was obtained from all participants. This study was reviewed and approved by the Institutional Review Board of Loma Linda University School of Medicine (IRB #5190039).
Adipose tissue samples
The present study measured Sias concentrations in 156 human adipose tissue samples from participants of the Adventist Health Study-2 (AHS-2) cohort. The AHS-2 cohort was established between 2002 and 2007 and consists of over 96,000 Seventh Day Adventists in the USA and Canada, with a considerable proportion (~ 50%) of vegetarians. Study participants completed a food frequency questionnaire at baseline and were defined as vegan (n = 52; strict vegetarians with complete avoidance of all animal products or consumption < 1/month), lacto-ovo-vegetarians (n = 56; avoidance of all flesh meats but consuming dairy and/or eggs ≥ 1/month) and non-vegetarians (n = 48; consuming flesh meats, not only fish, ≥ 1/month). Sociodemographic information and body mass index (BMI) were calculated from the baseline questionnaire. The current study included selection of approximately equal numbers of samples from vegan, lacto-ovo-vegetarian, and non-vegetarian participants who previously provided biospecimens, including adipose tissue and blood, in one of two sub-studies. The first was the Biological Manifestations of Religion and Health study, where participants were recruited to clinic sites in Southern California55. The second sub-study included pilot work with biospecimen collections from field clinics and church halls56. Adipose tissue samples were obtained by aspirating a subcutaneous sample of fat from the buttock with a needle and syringe, and were maintained frozen in liquid nitrogen57. Samples of adipose tissue from cow, pork, lamb, and poultry were obtained from local supermarkets in Southern California, USA.
Preparation of standard samples
Sample standards were prepared by dilution in Milli-Q water. Neu5Ac-D-1,2,3-13C3 was used as an internal standard (IS), due to its similar structure and behavior to analytes during chromatography separation of Sias, thereby enabling corrections for possible ion suppression/enhancement effects58,59. Moreover, the internal standard provides internal quality control and facilitates correction for unaccounted measurement variables. Additionally, positive controls with IS (30 ng/mL) in water were run before, during, and after each batch analysis.
Standard calibration curves
Calibration curves with varying Sia concentrations were prepared. To improve the quantification range of the LC–MS/MS equipment, two separate calibration curves with good linearity in the low and high ranges were constructed for Neu5Ac and KDN. Additionally, a fixed concentration of IS was added to each calibrator. The Neu5Gc standard concentrations were: 0.0004, 0.0005, 0.00078, 0.0010, 0.0015, 0.0021, 0.0029, 0.0042, 0.0058, 0.0081, 0.0114, and 0.016 μg/mL. The KDN standard concentrations were: 0.0004, 0.0005, 0.0010, 0.0015, 0.0021, 0.0029, 0.0042, 0.0058, 0.0081, 0.0114, and 0.0160 μg/mL for low range, and 0.0050, 0.0100, 0.0150, 0.0200, 0.0400, 0.0600, 0.0900, 0.0120, 0.0160, 0.20, and 0.26 μg/mL for high range. Similarly, the Neu5Ac standard concentrations were: 0.001, 0.0019, 0.0036, 0.013, 0.091, 0.174, 0.330, 0.629, and 1.2 μg/mL for low range, and 0.8, 1.6, 2.4, 3.2, 4.0, 4.8, 5.6, 6.4, and 7.2 μg/mL for high range. After correction for IS peak amplitude variations, the LC–MS/MS peak signal amplitudes for KDN, Neu5Ac, or Neu5Gc were used to construct the calibration lines. In addition, IS was injected as a reference at regular intervals60 for added quality control. Supplementary Fig. S4 presents the LC–MS/MS calibration curves, with detector response as a function of the concentrations of Neu5Ac, KDN, and Neu5Gc. The calculated lower limits of detection were ≥ 2.0 ng/mL for all three Sias61. The lower ranges of standard lines were extended by employing ln-ln transformations. The correlation coefficients (r2) for all three Sias were > 0.980.
Extraction of Neu5Ac, Neu5Gc, and KDN from adipose tissue
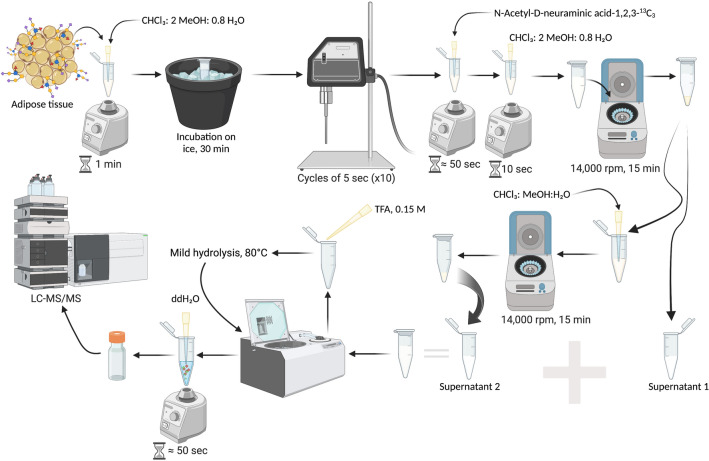
Sample processing is illustrated in Fig. 1. A solution of 100 μL of chloroform, methanol, and water (1:2:0.8) was added to human or animal samples and vortexed thoroughly for 1 min, followed by incubation for 30 min on ice before sonication. Ten sonication cycles of 5 s each with an amplitude of 20% were performed (120 Sonic Dismembrator, Fisher Scientific Sonicator) producing a mixture of free and conjugated Sias. After sonication, 20 μL (150 ng/mL) of the internal standard was added to a final concentration of 30 ng/mL, to help control for extraction, loading, and detection variables62. Then, the sample was vortexed for ~ 50 s. At this point, a solution of chloroform in water (26.4 μL) was added to generate a final concentration of 2:2:1.8 for chloroform, methanol, and water, respectively. Then, the sample was vortexed for 10 s and centrifuged at 14,000 rpm for 15 min. The first supernatant was separated (70 μL) and 100 μL of chloroform, methanol, and water (1:2:0.8) was added to the remaining volume. The second round of centrifugation was followed by supernatant separation (50 μL). The supernatant fractions were combined and dried by SpeedVac (Savant SC 110A, Thermo Electron Corporation). After drying, TFA 0.15 M (100 μL) was added to the sample and incubated at 80 °C (Labnet, Vortemp 56 Shaking incubator) with shaking at 400 rpm for 2 h for release of Sias from lipids or proteins by hydrolysis27. The sample was spun down and evaporated using SpeedVac. Then this dried processed sample was reconstituted in 100 μL of water and analyzed by LC–MS/MS.
Figure 1.
Processing of samples for the extraction, detection, and quantification of Sias from adipose tissue using LC/MS/MS. Created with BioRender.com.
LC–MS/MS quantification of sialic acids
Measurement of Sias was done using LC–MS/MS, following FDA Bioanalytical Method Guidelines63–66. The LC–MS/MS based approach was chosen with some adaptations from previous methods based on its selectivity, sensitivity, and reproducibility in identifying Sias27,67–69. Briefly, the instrumentation included an Agilent 1200 HPLC coupled with a triple quadruple mass spectrometer 6410 Agilent Technologies detector (Santa Clara, CA). Data processing was performed using Agilent Mass Hunter Software, version B.07.01.
The column temperature was set at 30 °C using an Accucore HILIC column (150 mm × 4.6 mm, 2.6 μm particles) connected with an Accucore HILIC precolumn (10 mm × 4.6 mm, 2.6 μm). The mobile phase flow rate was set to 0.3 mL/min. The mobile phase consisted of solution A (10% ammonium formate in water), and solution B (10% of ammonium formate in acetonitrile) with the following protocol: during the first min, 2% B; 1–2 min, gradient 2–90% B; 2–4 min, 90% B; 4–5 min, gradient 90–2% B; 5–7 min, 2% B. (See Supplementary Table S1, and Fig. S5). A blank with water was run as a negative control between each individual standard or sample run. The injection volume for standards and samples was set at 20 μL.
Chromatography and electrospray ion source (ESI) parameters were used as previously described20,27. Quantification of Sias from adipose tissue, including that of the added internal standard (Neu5Ac-D-1,2,3-13C3) (IS), was carried out in negative electrospray ionization (ESI) mode. (Supplementary Fig. S3). The ion spray voltage was operated at − 4 kV, and the source temperature was 300 °C. The nebulizer was set at 35 psi and the gas flow setting was 11 L/min. The singly charged [M-H]- parent ions were identified for: KDN at m/z 267.1, Neu5Ac at m/z 308.0, Neu5Gc at m/z 324.1, and Neu5Ac-D-1,2,3-13C3 at m/z 311.1. Selected daughter ions for KDN, Neu5Ac, Neu5Gc, and Neu5Ac-D-1,2,3-13C3 were at m/z 87.1, 87.0, 116.1, and 90.0, respectively. (Supplementary Table S2). Multiple reaction monitoring (MRM) mode was used. Peak areas for KDN, Neu5Ac, or Neu5Gc were corrected for variations in peak areas of the IS (Neu5Ac-D-1,2,3-13C3), followed by calculations of respective Sia concentrations based on the regression lines of standards.
Sialic acid levels in adipose tissue
Sias concentrations in samples were determined using standard calibration lines (Supplementary Fig. S4). The weight of human samples ranged from 5 to 30 mg, and animal samples ranged 10–20 mg, measured using an analytical balance (Mettler-Toledo, AB54-S). Sias concentrations were expressed in relative terms to the weight of the adipose tissue sample before extraction in (ng Sia)/(mg adipose) or ppm.
The standard lines were developed using varying respective Sias concentrations in the presence of a fixed concentration of 30 ng/ml for the internal standard (IS). Linearization was obtained following the natural logarithmic transformations of the MS detector signal intensity ratios and known concentration ratios , to produce the line Eq. (1) in the standard format . Then a rearrangement, illustrated by Eq. (2), was employed to convert MS detector signal intensities for sample Sias with known IS to appropriate Sias concentrations (3), after taking dilution factor (DF) into account. The specific equations of the form (2) for each Sia are presented with Supplementary Fig. S4. Two different standard lines are employed for both Neu5Ac and for KDN measurements, to accommodate potential low and high concentration ranges.
| 1 |
| 2 |
| 3 |
Statistical analysis
Descriptive analyses were carried out adjusting for demographic data, comparing the three dietary groups—vegans, lacto-ovo-vegetarians, and non-vegetarians. To compare Sias between diet groups, sialic acids were first log-transformed, and then a linear regression model was fitted to examine the association between vegetarian dietary status (vegan or lacto-ovo-vegetarian vs non-vegetarian, and vegan vs lacto-ovo-vegetarian) and Sia abundance, where the Sia was the dependent/response variable, and dietary pattern was the predictor variable of interest. Covariates included race (Black vs non-Black), age at blood collection (continuous), gender (male vs female), batch (continuous), sub-study (Adventist Religion and Health vs pilot), and BMI (kg/m2; continuous). Beta coefficients and 95% confidence intervals were obtained for each diet group/Sia comparison, along with the adjusted predicted means (R package emmeans) and 95% confidence intervals, providing a marginal estimate of the log of the mean of untransformed Sia values for vegetarians and non-vegetarians, and subsequently back-transformed. Linear regression analysis was also used to examine associations of BMI with Sias, adjusting for race, age at blood collection, gender, batch, and sub-study. All analyses were conducted in R version 4.0.2.
Results
Separation of sialic acids
The chemical structures of the studied Sias are shown in Supplementary Fig. S1. The HPLC peaks for Neu5Ac, Neu5Gc, and KDN standards are well resolved using LC–MS/MS with stable retention times (Supplementary Fig. S2). The retention times for KDN, Neu5Gc, Neu5Ac-D-1,2,3-13C3, and Neu5Ac were found to be 5.028, 5.036, 5.070, and 5.079 min, respectively. The ESI mass spectra of parent and daughter ions, as shown in Supplementary Fig. S2, for Neu5Ac, KDN, Neu5Ac-D-1,2,3-13C3 and Neu5Gc were chosen because of their relative abundances27,70–72.
Sialic acids from animal adipose tissue
Sias were extracted from adipose tissue samples from pig, lamb, cow, or chicken. All three Sias were released from adipose tissues and were measurable by the LC–MS/MS method (Supplementary Table S1). Total adipose tissue Sias (μg/mg) were highest in pork (5.669 μg/mg), followed by beef (4.958 μg/mg), lamb (3.592 μg/mg) and chicken (2.438 μg/mg). Neu5Ac was the major Sia form in all animal samples. As expected, Neu5Gc was not detected in chicken samples. (Supplementary Table S3).
Study population characteristics
Characteristics of the study population are presented in Table 1. The study cohort included 156 participants distributed among vegan, lacto-ovo vegetarian, and non-vegetarian dietary groups. Some statistical differences were evident among dietary groups. A significantly lower proportion of Black participants were vegan (p = 0.0007). Compared to other dietary groups, the vegans had significantly lower mean BMI (p = 0.004) and significantly higher adipose Neu5Ac (p = 0.02) considering unadjusted means.
Table 1.
Demographic characteristics of study population.
| Vegan | Lacto-ovo | Non-vegetarian | p value1 | |
|---|---|---|---|---|
| Participants | 52 (33.3) | 56 (35.8) | 48 (30.7) | |
| Age (years) | 61.3 (14.2) | 58.1 (13.3) | 60.8 (14.0) | 0.45 |
| Sex | ||||
| Female | 35 (31.8) | 40 (36.3) | 35 (31.8) | |
| Male | 17 (36.9) | 16 (34.7) | 13 (28.2) | 0.81 |
| Race | ||||
| Black | 23 (22.7) | 41 (40.5) | 37 (36.6) | |
| Non-Black | 29 (52.7) | 15 (27.2) | 11 (20.0) | 0.0007 |
| BMI (kg/m2) | 27.5 (5.4) | 31.2 (7.5) | 31.6 (7.4) | 0.004 |
| KDN (ng/mg) | 1.4 (0.91) | 1.6 (1.5) | 1.04 (1.06) | 0.083 |
| Neu5Ac (ng/mg) | 40.2 (38.9) | 36.5 (46.4) | 20.6 (21.7) | 0.024 |
Values are presented as n (%), or mean (SD).
1p value computed using chi-square test for categorical variables and ANOVA for continuous variables.
Associations of sialic acids from human adipose tissue with dietary patterns and BMI
Neu5Ac and KDN were measured and quantified in adipose tissue samples of vegans, lacto-ovo-vegetarians, and non-vegetarians as described. These Sia concentrations (ng/mg) were compared between diet groups using linear regression analysis, and adjusted means were obtained (Table 2). Neu5Ac was significantly higher in adipose tissues from vegans (mean: 17.1, 95% CI 12.5–23.6) compared to non-vegetarians (mean: 9.8, 95% CI 7.1–13.7). Similarly, Neu5Ac was higher in adipose of lacto-ovo-vegetarians (mean: 12.7, 95% CI 9.2–17.5) compared to non-vegetarians (mean: 7.7, 95% CI 5.4–10.8) (Table 2). These means were statistically different (p = 0.01 and p = 0.02, respectively), even after inclusion of BMI as a covariate (Table 2). KDN concentrations were higher in vegans and lacto-ovo-vegetarians relative to non-vegetarians, though differences were not statistically significant. Moreover, linear regression revealed an inverse association between BMI and KDN (p = 0.02), independent of diet group (Table 3). Neu5Gc was not detected in any adipose samples of participants in any diet group.
Table 2.
Adjusted means from linear regression model of associations of dietary patterns with Neu5Ac and KDN.
| Model 11 | Model 22 | |||||
|---|---|---|---|---|---|---|
| Vegan | Non-vegetarian | p value | Vegan | Non-vegetarian | p value | |
| Neu5Ac | 17.13 (12.45, 23.58) | 9.84 (7.09, 13.67) | 0.01 | 17.55 (12.67, 24.30) | 9.70 (6.96, 13.51) | 0.01 |
| KDN | 0.79 (0.63, 0.99) | 0.63 (0.50, 0.79) | 0.15 | 0.78 (0.62, 0.98) | 0.63 (0.50, 0.80) | 0.19 |
| Vegan | Lacto-ovo | p value | Vegan | Lacto-ovo | p value | |
|---|---|---|---|---|---|---|
| Neu5Ac | 16.97 (12.08, 23.84) | 15.20 (10.97, 21.06) | 0.46 | 16.97 (12.08, 23.84) | 16.44 (11.92, 22.69) | 0.88 |
| KDN | 0.80 (0.62, 1.02) | 0.82 (0.63, 1.07) | 0.85 | 0.79 (0.61, 1.03) | 0.85 (0.66, 1.09) | 0.66 |
| Lacto-ovo | Non-vegetarian | p value | Lacto-ovo | Non-vegetarian | p value | |
|---|---|---|---|---|---|---|
| Neu5Ac | 12.71 (9.23, 17.49) | 7.65 (5.40, 10.83) | 0.02 | 12.55 (9.13, 17.24) | 7.62 (5.39, 10.76) | 0.02 |
| KDN | 0.74 (0.56, 0.97) | 0.54 (0.40, 0.74) | 0.1 | 0.73 (0.55, 0.95) | 0.54 (0.40, 0.73) | 0.11 |
Estimated marginal (least-squares) means (ng/mg) and 95% confidence intervals obtained from linear regression.
BMI body mass index.
1Adjusted for age at blood collection, sub-study, race, gender, and batch.
2Adjusted for covariates in model 1, in addition to BMI.
Table 3.
Associations of BMI with KDN and Neu5Ac.
| Model 11 | Model 22 | |||||
|---|---|---|---|---|---|---|
| β coefficient | Std. Err | P value | β coefficient | Std. Err | p value | |
| KDN | − 0.023 | 0.009 | 0.013 | − 0.020 | 0.009 | 0.02 |
| Neu5Ac | − 0.020 | 0.01 | 0.09 | − 0.016 | 0.012 | 0.18 |
Beta-coefficients obtained from linear regression and represent change in sialic acid concentrations per unit increase in BMI.
BMI body mass index.
1Adjusted for sub-study, race, gender, age at blood collection, and batch.
2Adjusted for covariates in Model 1 in addition to diet group.
Discussion
Biological processes or alterations associated with cardiometabolic and other chronic diseases are still poorly understood. In this context, development of new biomarkers with recognized associations with such disorders is potentially helpful. Sias are known to accumulate in mammalian cells and tissues, and were proposed as biomarkers for some metabolic conditions30,72–75. If concentrations of Sias change with onset or progression of metabolic diseases, it is plausible that they are also impacted by dietary patterns which influence metabolic health.
In the current study we compared Sias among individuals following habitually vegetarian or non-vegetarian dietary patterns and found significantly higher levels of Neu5Ac in vegans and lacto-ovo-vegetarians relative to non-vegetarians. To our knowledge, this is the first study comparing Sias in adipose tissues from individuals in an epidemiological cohort specifically characterized by their dietary patterns. Hence, we compare our findings to other mostly in vivo studies reporting beneficial cardiometabolic effects of Neu5Ac supplementation. Such dietary supplementation has been found to have an intrinsic protective effect against atherosclerosis in mice76. Additionally, a reduction in coagulation-related cardiovascular events in hyperlipidemic conditions26,77, and prevention of clinical manifestations of cardiovascular disease have been documented24,76. Moreover, Neu5Ac dietary supplementation in experimental animals reduced the procoagulant, prothrombotic and antifibrinolytic effects of a high fat diet24,76.
Despite these promising findings, the usefulness of dietary supplementation with exogenous Sias in humans to reduce atherosclerosis, and consequently cardiovascular disease, remains questionable29. Furthermore, Sia levels in various human tissues have not been thoroughly investigated, and their physiological relevance is not well understood. Nevertheless, some trends have been identified. Obesity and systolic blood pressure in humans tend to be inversely associated with IgG sialylation22. This is consistent with in vivo studies demonstrating that dietary supplementation with N-acetyl-D-mannosamine (ManNAc), the first committed precursor of Neu5Ac, prevents obesity and systolic hypertension in mice, breaking the association between obesity and hypertension78. Additionally, increases in Sias due to dietary uptake appear to be associated with mechanisms that counter atherosclerosis, since Sias serve as substrates for re-sialylation of vascular endothelium. Thus, the presence of Sias on the vascular endothelium may alter these surfaces to reduce the risks of thrombosis26. However, the mechanisms for these effects are still largely unknown. Similarly, a positive impact on health by diet-related Sias, or by Sia supplementation, has not yet been established.
In contrast, there is evidence that total serum Sia is a risk factor for CVD, and correlates with CVD severity and mortality79–81. Similarly, increased plasma Sias are known to be associated with inflammation82,83. Since increased sialidase function is known to be associated with inflammation84, this could explain the higher circulatory Sias in these circumstances.
Given the pleiotropic roles of Sias, therefore, it is not unexpected for concentrations in serum or plasma to not correlate with those in adipose or other tissues. In this context, it appears that uptake of Sias by certain cell types may be associated with a dampened immune response85,86. Thus, while the physiologic relevance of higher adipose Sias in vegetarians is unclear, this may reflect a dampened immune or inflammatory response, relative to non-vegetarians.
KDN, similarly to Neu5Ac, was higher in vegans and lacto-ovo-vegetarians relative to non-vegetarians, though not reaching statistical significance, likely due to insufficient statistical power. However, similarly to Neu5Ac, KDN residues can be linked to almost all glycan structures. These linkage types include α2,3-, α2,4-, α2,6-, and α2,8-87. In this context, it might be expected that KDN and Neu5Ac follow a similar pattern of association with dietary groups.
The synthetic pathway for Sias is well described9,88. However, it is not clear why vegetarians would have higher Neu5Ac or KDN levels. While Sias are commonly present in dairy and animal products, they are not directly consumed from plant foods. Thus, it is not known to what degree (a) some raw precursors from natural sources in a vegan diet lead to increased incorporation of Sias into human tissues via de novo synthesis of Neu5Ac and KDN, or (b) some adverse impact of a non-vegetarian diet, such as increased inflammation, leads to reduction of Sias. Comparing vegans and non-vegetarians from the AHS-2 cohort, significant differences were found in monosaccharides, particularly metabolites in the fructose, mannose, galactose, and pentose subclasses, and other compounds that could impact precursors of Sias89. These vegans and other vegetarians, from the AHS-2 cohort, also have lower levels of pro-inflammatory compounds such as interleukin-6 and C-reactive protein relative to non-vegetarians90. Vegetarians also tend to have lower biomarkers related to meat or dairy consumption, lower saturated fatty acids and lipids known to be associated with cardiovascular disease and diabetes89. High consumption of red and processed meat has been associated with inflammation91,92. Hence, lower levels of Neu5Ac may imply a prolonged or higher baseline pro-inflammatory status.
Diet could also indirectly affect Sias through alterations in BMI or adiposity. In our study, KDN levels were lower with increasing BMI (Table 3), apparently independent of diet. While the relationship between BMI and Sias needs further elucidation, our findings are consistent with previous reports of lower Sias in obese individuals78. Compared to non-vegetarians, individuals following plant-based or vegetarian diets in AHS-2 were reported to have a lower risk of metabolic syndrome including lower BMI and waist circumference93, diabetes94, or cardiovascular disease mortality54. Therefore, the effects of diet on Sias could be attributable in part to adiposity. That is, a vegan diet promotes a lower BMI and anti-inflammatory environment, which may be associated with higher abundance of Sias in adipose tissue. The Sias in turn may help regulate or prevent the development of cardiovascular and other chronic diseases. From this perspective, a higher abundance of Neu5Ac might be expected in adipose tissue of vegans and lacto-ovo-vegetarians, considering the favorable cardiometabolic outcomes previously observed in vegetarians49,95,96. This is consistent with a role for Neu5Ac in the prevention of atherosclerosis76. Nonetheless, larger epidemiological or clinical studies are needed to specifically tease apart the contributions of diet and BMI to Sia levels.
In contrast to Neu5Ac and KDN, Neu5Gc was not detectable in human adipose tissue, although it was detected in animal adipose tissues from cows, lambs, and pigs. This is not surprising since Neu5Gc is known to be commonly expressed in mammals but not in humans67,97–99. Neu5Gc has been reported in some human tissues and fluids16,27, probably due to incorporation from food sources11,100. It has not been reported in human adipose tissue. This may be because Neu5Gc, if present, is below the current detection limits. It should be noted that even the non-vegetarian AHS-2 participants consume less red meat than the general population, or compared to participants of other studies such as the EPIC-Oxford101.
The relevance and potentially unique role of Sias in adipose tissue, in contrast to Sias in plasma or cancer cells, is noteworthy32,33,102,103. Although contributions from pathology-associated desialylation to human blood Sias remain speculative84, it is recognized that desialylation may lead to cellular dysfunction104. While Neu5Ac has been proposed as a potential factor counteracting atherosclerosis76, the source of Neu5Ac also needs to be considered. For example, sialidases may induce cleavage of Neu5Ac from the glycan chains of the LDL glycoprotein and glycolipids during the initial phase of atherosclerosis29. Following this, during CVD progression, while desialylation occurs in glycoconjugates, the serum sialic acid totals may increase75,105. Consequently, it could be hypothesized that in CVD, Sias may be released from adipose storage or other tissues as a compensatory response to reduce or counter inflammation. The development or discovery of biomarkers relevant to CVD will lead to more sensitive and effective screening approaches106.
Strengths of this study include the large number of habitual vegetarians and non-vegetarians in the Adventist Health Study-2 cohort, and the detailed diet and health history records for these participants. Additionally, the use of internal standards and other quality control procedures helped to ensure accurate and consistent measurement of Sias in human adipose samples. Furthermore, Sias were quantitatively measured using a direct and relatively straightforward method, without derivatization steps. The principal limitation of this study is its modest sample size. This likely reduced the statistical significance for the association between KDN and dietary pattern, and the contributing role of adiposity. Levels of free and conjugated Sias in the human adipose are not clear from the current study, as these were not measured separately, and consequently could not be compared. All Sia measurements were made using single time point biopsy samples, which may obscure seasonal or other temporal variations. Additionally, while adipose tissue samples are expected to largely include adipose cells, other cell types, including some vascular endothelial and fibroblast cells, were likely represented to some extent. Therefore, the source of Sias could not be fully ascertained. Moreover, Neu5Gc, which also has important implications for inflammatory or metabolic diseases, was below detection limits in human samples in the current study. Due to limitations of sample size, the analysis of associations of Sia concentrations with various physiologic parameters of interest have been limited to BMI. Finally, it would be useful to measure and compare adipose Sia concentrations with those in plasma or serum samples to further elucidate their biological roles. Such studies remain to be conducted.
Conclusions
In the present study, we report successful detection of the Sias, Neu5Ac and KDN, in adipose tissue samples from individuals following habitual vegetarian and non-vegetarian diets. Neu5Ac was present at significantly higher concentrations in adipose tissue of vegans and lacto-ovo-vegetarians compared to non-vegetarians, while Neu5Gc was not detected in human adipose samples. KDN levels were modestly but significantly inversely associated with BMI. It is conceivable that dietary patterns regulate levels of Sias by influencing the accumulation of adipose tissue or by regulating inflammation. Such processes, in turn, may impact the onset or progression of chronic diseases.
This method for determination of Sias may be applied in future studies with human adipose tissues to quantify Sias and to elucidate their roles in human health or the development and progression of chronic diseases. In the longer term, assessing the impact of dietary patterns on Sia concentrations in human tissues will improve understanding of their associations with health and disease. Similarly, studies utilizing natural dietary components for de novo synthesis of Sias, may be helpful in the development of prevention strategies for cardiovascular and related diseases.
Supplementary Information
Acknowledgements
We thank Dr. Josef Voglmeir (Glycomics and Glycan Bioengineering Research Center (GGBRC), College of Food Science and Technology, Nanjing Agricultural University, Nanjing, China), for providing the opportunity for an interchange research experience for GNGF in the analytical chemistry of sialic acids. We thank Dr. Christopher Perry for his valuable technical advice on LC-MS/MS and internal standards. Also, we would like to thank DrPH Rawiwan Sirirat for helping with the handling of adipose tissue samples from the AHS-2 participants.
Author contributions
F.L.M., F.J.P., G.F., and G.N.G.F. participated in the conceptualization and design of the study. G.N.G.F., D.S.B., G.Z. and F.J.P. participated in the method development and protocol optimization for sialic acid extraction and quantification, and processing of the samples and data acquisition at the LC–MS/MS. F.L.M. and S.O.S.P. participated in statistical analysis. G.N.G.F., D.S.B., F.J.P., S.O.S.P., G.Z. and F.L.M. participated in the writing of the original draft of the manuscript. G.N.G.F., D.S.B., F.J.P., S.O.S.P., F.L.M. and G.F. participated in the writing, reviewing and final editing of the manuscript. All authors reviewed the content of the manuscript and approved the final version.
Funding
This study was supported by the Grants for Research and School Partnerships (GRASP) from Loma Linda University (#2170258), California, USA. And The Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET), from the Ministry of Science and Technology of Argentina, granted a doctoral scholarship to GNGF (RESOL-2018-2704-APN-DIR#CONICET). Also, it includes a Research grant from the Adventist University of River Plate, School of Medicine.
Data availability
Correspondence and requests for materials should be addressed to Fayth L. Miles.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-023-38102-z.
References
- 1.Varki, A. et al. Essentials of Glycobiology. (Cold Spring Harbor, 2022). [PubMed]
- 2.Cai Z-P, et al. Enzymatic synthesis of trideuterated sialosides. Molecules. 2019;24:1368. doi: 10.3390/molecules24071368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cao C, et al. Determination of sialic acids in liver and milk samples of wild-type and CMAH knock-out mice. J. Vis. Exp. 2017;e56030:1–6. doi: 10.3791/56030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen X, Varki A. Advances in the biology and chemistry of sialic acids. ACS Chem. Biol. 2010;5:163–176. doi: 10.1021/cb900266r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Büll C, Stoel MA, Den Brok MH, Adema GJ. Sialic acids sweeten a tumor’s life. Cancer Res. 2014;74:3199–3204. doi: 10.1158/0008-5472.CAN-14-0728. [DOI] [PubMed] [Google Scholar]
- 6.Pearce OMT, Läubli H. Sialic acids in cancer biology and immunity. Glycobiology. 2016;26:111–128. doi: 10.1093/glycob/cwv097. [DOI] [PubMed] [Google Scholar]
- 7.Yao HL, et al. Quantification of sialic acids in red meat by UPLC-FLD using indoxylsialosides as internal standards. Glycoconj. J. 2016;33:219–226. doi: 10.1007/s10719-016-9659-1. [DOI] [PubMed] [Google Scholar]
- 8.Traving C, Schauer R. Structure, function and metabolism of sialic acids. Cell. Mol. Life Sci. 1998;54:1330–1349. doi: 10.1007/s000180050258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chou WK, Hinderlich S, Reutter W, Tanner ME. Sialic acid biosynthesis: Stereochemistry and mechanism of the reaction catalyzed by the mammalian UDP-N-acetylglucosamine 2-epimerase. J. Am. Chem. Soc. 2003;125:2455–2461. doi: 10.1021/ja021309g. [DOI] [PubMed] [Google Scholar]
- 10.Amon R, et al. Glycan microarray reveal induced IgGs repertoire shift against a dietary carbohydrate in response to rabbit anti-human thymocyte therapy. Oncotarget. 2017;8:112236–112244. doi: 10.18632/oncotarget.23096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tangvoranuntakul P, et al. Human uptake and incorporation of an immunogenic nonhuman dietary sialic acid. Proc. Natl. Acad. Sci. U. S. A. 2003;100:12045–12050. doi: 10.1073/pnas.2131556100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leviatan Ben-Arye S, Yu H, Chen X, Padler-Karavani V. Profiling anti-Neu5Gc IgG in human sera with a sialoglycan microarray assay. J. Vis. Exp. 2017 doi: 10.3791/56094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bashir S, et al. Association between Neu5Gc carbohydrate and serum antibodies against it provides the molecular link to cancer: French NutriNet-Santé study. BMC Med. 2020;18:1–19. doi: 10.1186/s12916-020-01721-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boligan KF, Mesa C, Fernandez LE, Von Gunten S. Cancer intelligence acquired (CIA): Tumor glycosylation and sialylation codes dismantling antitumor defense. Cell. Mol. Life Sci. 2015;72:1231–1248. doi: 10.1007/s00018-014-1799-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dhar C, et al. Are sialic acids involved in COVID-19 pathogenesis? Glycobiology. 2021;31:1068–1071. doi: 10.1093/glycob/cwab063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Varki A. Sialic acids in human health and disease. Trends Mol. Med. 2008;14:351–360. doi: 10.1016/j.molmed.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Limsuwat N, et al. Sialic acid content in human saliva and anti-influenza activity against human and avian influenza viruses. Arch. Virol. 2016;161:649–656. doi: 10.1007/s00705-015-2700-z. [DOI] [PubMed] [Google Scholar]
- 18.Wang D, Zhou X, Wang L, Wang S, Sun XL. Quantification of free sialic acid in human plasma through a robust quinoxalinone derivatization and LC-MS/MS using isotope-labeled standard calibration. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2014;944:75–81. doi: 10.1016/j.jchromb.2013.11.016. [DOI] [PubMed] [Google Scholar]
- 19.Wang B, Brand-Miller J, McVeagh P, Petocz P. Concentration and distribution of sialic acid in human milk and infant formulas. Am. J. Clin. Nutr. 2001;74:510–515. doi: 10.1093/ajcn/74.4.510. [DOI] [PubMed] [Google Scholar]
- 20.Halvorsen TG, et al. Quantification of free and total sialic acid excretion by LC-MS/MS. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2014;28:251–257. doi: 10.1016/j.jchromb.2006.10.066. [DOI] [PubMed] [Google Scholar]
- 21.Schnaar RL, Gerardy-Schahn R, Hildebrandt H. Sialic acids in the brain: Gangliosides and polysialic acid in nervous system development, stability, disease, and regeneration. Physiol. Rev. 2014;94:461–518. doi: 10.1152/physrev.00033.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peng J, et al. Supplementation with the sialic acid precursor N-acetyl-D-mannosamine breaks the link between obesity and hypertension. Circulation. 2019;140:2005–2018. doi: 10.1161/CIRCULATIONAHA.119.043490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kawanishi K, et al. Dietary Neu5Ac intervention protects against atherosclerosis associated with human-like Neu5Gc loss—Brief report. Arterioscler. Thromb. Vasc. Biol. 2021;41:2730–2739. doi: 10.1161/ATVBAHA.120.315280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yida Z, et al. N-Acetylneuraminic acid attenuates hypercoagulation on high fat diet-induced hyperlipidemic rats. Food Nutr. Res. 2015;59:29046. doi: 10.3402/fnr.v59.29046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang L, et al. Functional metabolomics characterizes a key role for N -Acetylneuraminic acid in coronary artery diseases. Circulation. 2018;137:1374–1390. doi: 10.1161/CIRCULATIONAHA.117.031139. [DOI] [PubMed] [Google Scholar]
- 26.Yida, Z. et al. N-Acetylneuraminic acid supplementation prevents high fat diet-induced insulin resistance in rats through transcriptional and nontranscriptional mechanisms. BioMed Res. Int.2015 (2015). [DOI] [PMC free article] [PubMed]
- 27.Wang F, Xie B, Wang B, Troy FA. LC-MS/MS glycomic analyses of free and conjugated forms of the sialic acids, Neu5Ac, Neu5Gc and KDN in human throat cancers. Glycobiology. 2015;25:1362–1374. doi: 10.1093/glycob/cwv051. [DOI] [PubMed] [Google Scholar]
- 28.Wakabayashi I, Masuda H. Relation of serum sialic acid to blood coagulation activity in type 2 diabetes. Blood Coagul. Fibrinolysis. 2002;13:691–696. doi: 10.1097/00001721-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Zhang C, Chen J, Liu Y, Xu D. Sialic acid metabolism as a potential therapeutic target of atherosclerosis. Lipids Health Dis. 2019;18:1–11. doi: 10.1186/s12944-019-1113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Serdar Z, Yeşilbursa D, Dirican M, Sarandöl E, Serdar A. Sialic acid and oxidizability of lipid and proteins and antioxidant status in patients with coronary artery disease. Cell. Biochem. Funct. 2007;25:655–664. doi: 10.1002/cbf.1369. [DOI] [PubMed] [Google Scholar]
- 31.Lindbohm N, Gylling H, Miettinen TA. Sialic acid content of low density lipoprotein and its relation to lipid concentrations and metabolism of low density lipoprotein and cholesterol. J. Lipid Res. 2000;41:1110–1117. [PubMed] [Google Scholar]
- 32.Yabu M, et al. Accumulation of free Neu5Ac-containing complex-type N-glycans in human pancreatic cancers. Glycoconj. J. 2013;30:247–256. doi: 10.1007/s10719-012-9435-9. [DOI] [PubMed] [Google Scholar]
- 33.Aykan NF. Red meat and colorectal cancer. Oncol. Rev. 2015;9:38–44. doi: 10.4081/oncol.2015.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kakugawa Y, et al. Up-regulation of plasma membrane-associated ganglioside sialidase (Neu3) in human colon cancer and its involvement in apoptosis suppression. Proc. Natl. Acad. Sci. 2002;99:10718–10723. doi: 10.1073/pnas.152597199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen W, Pilling D, Gomer RH. The mRNA-binding protein DDX3 mediates TGF-β1 upregulation of translation and promotes pulmonary fibrosis. JCI Insight. 2023;8:e167566. doi: 10.1172/jci.insight.167566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang WH, et al. Neu3 neuraminidase induction triggers intestinal inflammation and colitis in a model of recurrent human food-poisoning. Proc. Natl. Acad. Sci. 2021;118:e2100937118. doi: 10.1073/pnas.2100937118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seyrantepe V, et al. Murine Sialidase Neu3 facilitates GM2 degradation and bypass in mouse model of Tay-Sachs disease. Exp. Neurol. 2018;299:26–41. doi: 10.1016/j.expneurol.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 38.Karhadkar TR, Pilling D, Cox N, Gomer RH. Sialidase inhibitors attenuate pulmonary fibrosis in a mouse model. Sci. Rep. 2017;7:15069. doi: 10.1038/s41598-017-15198-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Browning LM, et al. Elevated sialic acid, but not CRP, predicts features of the metabolic syndrome independently of BMI in women. Int. J. Obes. 2004;28:1004–1010. doi: 10.1038/sj.ijo.0802711. [DOI] [PubMed] [Google Scholar]
- 40.Coelho M, Oliveira T, Fernandes R. Biochemistry of adipose tissue: An endocrine organ. Arch. Med. Sci. 2013;9:191–200. doi: 10.5114/aoms.2013.33181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ouchi N. Adipocytokines in cardiovascular and metabolic diseases. J. Atheroscler. Thromb. 2016;23:645–654. doi: 10.5551/jat.34918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ahima RS, Flier JS. Adipose tissue as an endocrine organ. Trends Endocrinol. Metab. 2000;11:327–332. doi: 10.1016/s1043-2760(00)00301-5. [DOI] [PubMed] [Google Scholar]
- 43.Zamboni M, Nori N, Brunelli A, Zoico E. How does adipose tissue contribute to inflammageing? Exp. Gerontol. 2021;143:111162. doi: 10.1016/j.exger.2020.111162. [DOI] [PubMed] [Google Scholar]
- 44.Oikonomou EK, Antoniades C. The role of adipose tissue in cardiovascular health and disease. Nat. Rev. Cardiol. 2019;16:83–99. doi: 10.1038/s41569-018-0097-6. [DOI] [PubMed] [Google Scholar]
- 45.Kaburagi T, Kizuka Y, Kitazume S, Taniguchi N. The inhibitory role of α2,6-sialylation in adipogenesis. J. Biol. Chem. 2017;292:2278–2286. doi: 10.1074/jbc.M116.747667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liberale L, et al. The role of adipocytokines in coronary atherosclerosis. Curr. Atheroscler. Rep. 2017;19:10. doi: 10.1007/s11883-017-0644-3. [DOI] [PubMed] [Google Scholar]
- 47.Iona A, et al. Adiposity and risks of vascular and non-vascular mortality among Chinese adults with type 2 diabetes: A 10-year prospective study. BMJ Open Diabetes Res. Care. 2022;10:e002489. doi: 10.1136/bmjdrc-2021-002489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bhaskaran K, et al. Body-mass index and risk of 22 specific cancers: A population-based cohort study of 5·24 million UK adults. Lancet. 2014;384:755–765. doi: 10.1016/S0140-6736(14)60892-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Matsumoto S, et al. Association between vegetarian diets and cardiovascular risk factors in non-Hispanic white participants of the adventist health study-2. J. Nutr. Sci. 2019;8:e6. doi: 10.1017/jns.2019.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Orlich MJ, et al. Vegetarian dietary patterns and the risk of colorectal cancers. JAMA Intern. Med. 2015;175:767–767. doi: 10.1001/jamainternmed.2015.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Singh PN, Sabaté J, Fraser GE. Does low meat consumption increase life expectancy in humans? Am. J. Clin. Nutr. 2003;78:526–532. doi: 10.1093/ajcn/78.3.526S. [DOI] [PubMed] [Google Scholar]
- 52.Fraser, G., Miles, F., Orlich, M., Jaceldo-Siegl, K. & Mashchak, A. Dairy milk is associated with increased risk of breast cancer in the adventist health study-2 (AHS-2) cohort (P05-026-19). Curr. Dev. Nutr.3, nzz030.P05-026-19 (2019).
- 53.Le L, Sabaté J. Beyond meatless, the health effects of vegan diets: Findings from the adventist cohorts. Nutrients. 2014;6:2131–2147. doi: 10.3390/nu6062131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Orlich MJ, et al. Vegetarian dietary patterns and mortality in adventist health study 2. JAMA Intern. Med. 2013;173:1230–1238. doi: 10.1001/jamainternmed.2013.6473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee JW, et al. Cohort profile: The biopsychosocial religion and health study (BRHS) Int. J. Epidemiol. 2009;38:1470–1478. doi: 10.1093/ije/dyn244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chan J, et al. Feasibility of running clinics to collect biological specimens in a nationwide cohort study—Adventist health study-2. Ann. Epidemiol. 2007;17:454–457. doi: 10.1016/j.annepidem.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 57.Butler TL, et al. Cohort profile: The adventist health study-2 (AHS-2) Int. J. Epidemiol. 2008;37:260–265. doi: 10.1093/ije/dym165. [DOI] [PubMed] [Google Scholar]
- 58.Panuwet P, et al. Biological matrix effects in quantitative tandem mass spectrometry-based analytical methods: Advancing biomonitoring. Crit. Rev. Anal. Chem. 2016;46:93–105. doi: 10.1080/10408347.2014.980775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Berg T, Strand DH. 13C labelled internal standards-A solution to minimize ion suppression effects in liquid chromatography-tandem mass spectrometry analyses of drugs in biological samples? J. Chromatogr. A. 2011;1218:9366–9374. doi: 10.1016/j.chroma.2011.10.081. [DOI] [PubMed] [Google Scholar]
- 60.Wehrens R, et al. Improved batch correction in untargeted MS-based metabolomics. Metabolomics. 2016;12:88. doi: 10.1007/s11306-016-1015-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mohammadipanah F, Kazemi Shariat Panahi H, Imanparast F, Hamedi J. Development of a reversed-phase liquid chromatographic assay for the quantification of total persipeptides in fermentation broth. Chromatographia. 2016;79:1325–1332. [Google Scholar]
- 62.Salerno S, et al. RRmix: A method for simultaneous batch effect correction and analysis of metabolomics data in the absence of internal standards. PLoS ONE. 2017;12:e0179530. doi: 10.1371/journal.pone.0179530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mendes VM, Coelho M, Tomé AR, Cunha RA, Manadas B. Validation of an LC-MS/MS Method for the quantification of caffeine and theobromine using non-matched matrix calibration curve. Molecules. 2019;24:2863. doi: 10.3390/molecules24162863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Orfanidis A, et al. Determination of drugs of abuse and pharmaceuticals in skeletal tissue by UHPLC–MS/MS. Forensic Sci. Int. 2018;290:137–145. doi: 10.1016/j.forsciint.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 65.Berg T, Strand DH. 13C labelled internal standards-A solution to minimize ion suppression effects in liquid chromatography-tandem mass spectrometry analyses of drugs in biological samples? J. Chromatogr. A. 2011;1218:9366–9374. doi: 10.1016/j.chroma.2011.10.081. [DOI] [PubMed] [Google Scholar]
- 66.FDA, F. & D. A. Bioanalytical method validation guidance. Food Drug Adm.1043, 25–25 (2018).
- 67.Ji S, et al. Developmental changes in the level of free and conjugated sialic acids, Neu5Ac, Neu5Gc and KDN in different organs of pig: A LC-MS/MS quantitative analyses. Glycoconj. J. 2017;34:21–30. doi: 10.1007/s10719-016-9724-9. [DOI] [PubMed] [Google Scholar]
- 68.Zhou S, Dong X, Veillon L, Huang Y, M Y. LC-MS/MS analysis of pemethylated N-glycans facilitating isomeric characterization. Physiol. Behav. 2017;409:453–466. doi: 10.1007/s00216-016-9996-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Novotny MV, Alley Jr WR. Recent trends in analytical and structural glycobiology. Curr. Opin. Chem. Biol. 2013;17:832–840. doi: 10.1016/j.cbpa.2013.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen Y, Pan L, Liu N, Troy FA, Wang B. LC-MS/MS quantification of N-acetylneuraminic acid, N-glycolylneuraminic acid and ketodeoxynonulosonic acid levels in the urine and potential relationship with dietary sialic acid intake and disease in 3-to 5-year-old children. Br. J. Nutr. 2014;111:332–341. doi: 10.1017/S0007114513002468. [DOI] [PubMed] [Google Scholar]
- 71.van der Ham M, et al. Quantification of free and total sialic acid excretion by LC-MS/MS. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2007;848:251–257. doi: 10.1016/j.jchromb.2006.10.066. [DOI] [PubMed] [Google Scholar]
- 72.Nayak BS, Bhaktha G. Relationship between Sialic acid and metabolic variables in Indian type 2 diabetic patients. Lipids Health Dis. 2005;4:15. doi: 10.1186/1476-511X-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.White EJ, et al. Sialidase down-regulation reduces non-HDL cholesterol, inhibits leukocyte transmigration, and attenuates atherosclerosis in ApoE knockout mice. J. Biol. Chem. 2018;293:14689–14706. doi: 10.1074/jbc.RA118.004589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Englyst NA, et al. Percentage of body fat and plasma glucose predict plasma sialic acid concentration in type 2 diabetes mellitus. Metabolism. 2006;55:1165–1170. doi: 10.1016/j.metabol.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 75.Gopaul KP, Crook MA. Sialic acid: A novel marker of cardiovascular disease? Clin. Biochem. 2006;39:667–681. doi: 10.1016/j.clinbiochem.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 76.Kawanishi K, et al. Dietary Neu5Ac intervention protects against atherosclerosis associated with human-like Neu5Gc loss—Brief report. Arterioscler. Thromb. Vasc. Biol. 2021;41:2730–2739. doi: 10.1161/ATVBAHA.120.315280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yida Z, et al. High fat diet-induced inflammation and oxidative stress are attenuated by N-acetylneuraminic acid in rats. J. Biomed. Sci. 2015;22:96. doi: 10.1186/s12929-015-0211-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Peng J, et al. Supplementation with the sialic acid precursor N-acetyl-D-mannosamine breaks the link between obesity and hypertension. Circulation. 2019;140:2005–2018. doi: 10.1161/CIRCULATIONAHA.119.043490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Doostkam A, et al. Sialic acid: An attractive biomarker with promising biomedical applications. Asian Biomed. 2022;16:153–167. doi: 10.2478/abm-2022-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Abolhasani S, Shahbazloo SV, Saadati HM, Mahmoodi N, Khanbabaei N. Evaluation of serum levels of inflammation, fibrinolysis and oxidative stress markers in coronary artery disease prediction: A cross-sectional study. Arq. Bras. Cardiol. 2019 doi: 10.5935/abc.20190159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Christ ER, et al. Growth hormone (GH) replacement therapy reduces serum sialic acid concentrations in adults with GH-deficiency: A double-blind placebo-controlled study. Clin. Endocrinol. (Oxf.) 1999;51:173–179. doi: 10.1046/j.1365-2265.1999.00751.x. [DOI] [PubMed] [Google Scholar]
- 82.Tseke P, et al. Correlations of sialic acid with markers of inflammation, atherosclerosis and cardiovascular events in hemodialysis patients. Blood Purif. 2008;26:261–266. doi: 10.1159/000124850. [DOI] [PubMed] [Google Scholar]
- 83.Bakri RS, et al. Cardiovascular disease in renal allograft recipients is associated with elevated sialic acid or markers of inflammation. Clin. Transplant. 2004;18:201–204. doi: 10.1111/j.1399-0012.2004.00156.x. [DOI] [PubMed] [Google Scholar]
- 84.Glanz VY, et al. Sialidase activity in human blood serum has a distinct seasonal pattern: A pilot study. Biology. 2020;9:184. doi: 10.3390/biology9080184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lübbers J, Rodríguez E, van Kooyk Y. Modulation of immune tolerance via siglec-sialic acid interactions. Front. Immunol. 2018;9:2807–2807. doi: 10.3389/fimmu.2018.02807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Perdicchio M, et al. Sialic acid-modified antigens impose tolerance via inhibition of T-cell proliferation and de novo induction of regulatory T cells. Proc. Natl. Acad. Sci. 2016;113:3329–3334. doi: 10.1073/pnas.1507706113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Inoue S, Kitajima K. KDN (Deaminated neuraminic acid): Dreamful past and exciting future of the newest member of the sialic acid family. Glycoconj. J. 2006;23:277–290. doi: 10.1007/s10719-006-6484-y. [DOI] [PubMed] [Google Scholar]
- 88.Crich D, Navuluri C. Practical Synthesis of 2-Keto-3-deoxy-D-glycero-D-galactononulosonic Acid (KDN) Org. Lett. 2011;13:6288–6291. doi: 10.1021/ol202773t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Miles FL, et al. The biology of veganism: Plasma metabolomics analysis reveals distinct profiles of vegans and non-vegetarians in the adventist health study-2 cohort. Nutrients. 2022;14:709. doi: 10.3390/nu14030709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Miles FL, et al. Plasma, urine, and adipose tissue biomarkers of dietary intake differ between vegetarian and non-vegetarian diet groups in the adventist health study-2. J. Nutr. 2019;149:667–675. doi: 10.1093/jn/nxy292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chai W, et al. Dietary red and processed meat intake and markers of adiposity and inflammation: The multiethnic cohort study. J. Am. Coll. Nutr. 2017;36:378–385. doi: 10.1080/07315724.2017.1318317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Guagnano MT, et al. Improvement of inflammation and pain after three months’ exclusion diet in rheumatoid arthritis patients. Nutrients. 2021;13:3535. doi: 10.3390/nu13103535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rizzo NS, Sabaté J, Jaceldo-Siegl K, Fraser GE. Vegetarian dietary patterns are associated with a lower risk of metabolic syndrome: The adventist health study 2. Diabetes Care. 2011;34:1225–1227. doi: 10.2337/dc10-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tonstad S, et al. Vegetarian diets and incidence of diabetes in the adventist health study-2. Nutr. Metab. Cardiovasc. Dis. 2013;23:292–299. doi: 10.1016/j.numecd.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tharrey M, et al. Patterns of plant and animal protein intake are strongly associated with cardiovascular mortality: The adventist health study-2 cohort. Int. J. Epidemiol. 2018;47:1603–1612. doi: 10.1093/ije/dyy030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fraser G, et al. Vegetarian diets and cardiovascular risk factors in black members of the adventist health study-2. Public Health Nutr. 2015;18:537–545. doi: 10.1017/S1368980014000263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dhar C, Sasmal A, Varki A. From ‘serum sickness’ to ‘xenosialitis’: Past, present, and future significance of the non-human sialic acid Neu5Gc. Front. Immunol. 2019;10:807–807. doi: 10.3389/fimmu.2019.00807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jahan M, Thomson PC, Wynn PC, Wang B. The non-human glycan, N-glycolylneuraminic acid (Neu5Gc), is not expressed in all organs and skeletal muscles of nine animal species. Food Chem. 2021;343:128439–128439. doi: 10.1016/j.foodchem.2020.128439. [DOI] [PubMed] [Google Scholar]
- 99.Gao B, et al. Anti-Neu5Gc and anti-non-Neu5Gc antibodies in healthy humans. PLoS ONE. 2017;12:1–17. doi: 10.1371/journal.pone.0180768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Alisson-Silva F, Kawanishi K, Varki A. Human risk of diseases associated with red meat intake: Analysis of current theories and proposed role for metabolic incorporation of a non-human sialic acid. Mol. Asp. Med. 2016;51:16–30. doi: 10.1016/j.mam.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Davey GK, et al. EPIC–Oxford: Lifestyle characteristics and nutrient intakes in a cohort of 33 883 meat-eaters and 31 546 non meat-eaters in the UK. Public Health Nutr. 2003;6:259–268. doi: 10.1079/PHN2002430. [DOI] [PubMed] [Google Scholar]
- 102.Samraj AN, Läubli H, Varki N, Varki A. Involvement of a non-human sialic acid in human cancer. Front. Oncol. 2014;4:1–13. doi: 10.3389/fonc.2014.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Berghuis AY, Pijnenborg JFA, Boltje TJ, Pijnenborg JMA. Sialic acids in gynecological cancer development and progression: Impact on diagnosis and treatment. Int. J. Cancer. 2022;150:678–687. doi: 10.1002/ijc.33866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tian H, et al. Synthesis and cardiovascular protective effects of quercetin 7-O-sialic acid. J. Cell. Mol. Med. 2017;21:107–120. doi: 10.1111/jcmm.12943. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 105.Gokmen SS, Kilicli G, Ozcelik F, Ture M, Gulen S. Association between serum total and lipid-bound sialic acid concentration and the severity of coronary atherosclerosis. J. Lab. Clin. Med. 2002;140:110–118. doi: 10.1067/mlc.2002.126344. [DOI] [PubMed] [Google Scholar]
- 106.Dhingra R, Vasan RS. Biomarkers in cardiovascular disease: Statistical assessment and section on key novel heart failure biomarkers. Trends Cardiovasc. Med. 2017;27:123–133. doi: 10.1016/j.tcm.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Correspondence and requests for materials should be addressed to Fayth L. Miles.