Abstract
Abstract
Multiple molecular pathways including the receptor for advanced glycation end-products-diaphanous related formin 1 (RAGE-Diaph1) signaling are known to play a role in diabetic peripheral neuropathy (DPN). Evidence suggests that neuropathological alterations in type 1 diabetic spinal cord may occur at the same time as or following peripheral nerve abnormalities. We demonstrated that DPN was associated with perturbations of RAGE-Diaph1 signaling pathway in peripheral nerve accompanied by widespread spinal cord molecular changes. More than 500 differentially expressed genes (DEGs) belonging to multiple functional pathways were identified in diabetic spinal cord and of those the most enriched was RAGE-Diaph1 related PI3K-Akt pathway. Only seven of spinal cord DEGs overlapped with DEGs from type 1 diabetic sciatic nerve and only a single gene cathepsin E (CTSE) was common for both type 1 and type 2 diabetic mice. In silico analysis suggests that molecular changes in spinal cord may act synergistically with RAGE-Diaph1 signaling axis in the peripheral nerve.
Key messages
Molecular perturbations in spinal cord may be involved in the progression of diabetic peripheral neuropathy.
Diabetic peripheral neuropathy was associated with perturbations of RAGE-Diaph1 signaling pathway in peripheral nerve accompanied by widespread spinal cord molecular changes.
In silico analysis revealed that PI3K-Akt signaling axis related to RAGE-Diaph1 was the most enriched biological pathway in diabetic spinal cord.
Cathepsin E may be the target molecular hub for intervention against diabetic peripheral neuropathy.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00109-023-02347-y.
Keywords: Spinal cord, Sciatic nerve, Cytoskeleton, Inflammation, Neuropathy, Diabetes
Introduction
Over years it has become apparent that abnormalities in diabetic peripheral neuropathy (DPN) are caused by several concurrent factors such as: accumulation of advanced glycation end-products (AGEs), receptor of AGEs-diaphanous related formin 1 (RAGE-Diaph1) pathway, axonal transport alteration concomitant with increased inflammation and oxidative stress [1–9]. However, clinical evidence demonstrates that besides peripheral effects, diabetes also affect central nervous system (CNS) neurons, with structural and metabolic alternations observed primarily in spinal cord (SC) [10–15]. Tesfaye and co-workers [10] revealed that high blood glucose level also affects CNS. Hence, we may suppose that long-term hyperglycemia may have an impact on SC transcriptome profile. To date however no study has used high throughput RNA sequencing experiments on SC in animal models of DPN. In this study, using a type 1 diabetes (T1D) mouse model we also carefully tested the timing of DPN initiation and its relation to changes in RAGE-Diaph1 signaling axis in sciatic nerve (SN).
The aim of our study was to investigate diabetes-triggered molecular alternations in SC as well as perturbations in RAGE-Diaph1 axis in SN. We uncovered that DPN initiation may precede altered RAGE-Diaph1 signaling in SN as well as gene expression profile within the SC of T1D mouse model.
Materials and methods
Animals
All experiments were approved by the Local Ethics Committee of Experiments on Animals in Olsztyn (Poland; decision no. 57/2019). Eight weeks old C57BL/6 males were randomly divided into control and experimental groups per defined time points (Fig. 1A). Streptozotocin (STZ, 50 mg/kg; Sigma-Aldrich, USA) or a vehicle (PBS, pH 7.4; Eurx®, Poland) were administered daily for a week (Fig. 1A). Mice were sacrificed eight, 16 and 24 weeks post the last STZ injection (two, four and six months of rendered diabetes, respectively). Animals with a blood glucose level ≥ 13 mmol/L (260 mg/dL) were considered diabetic.
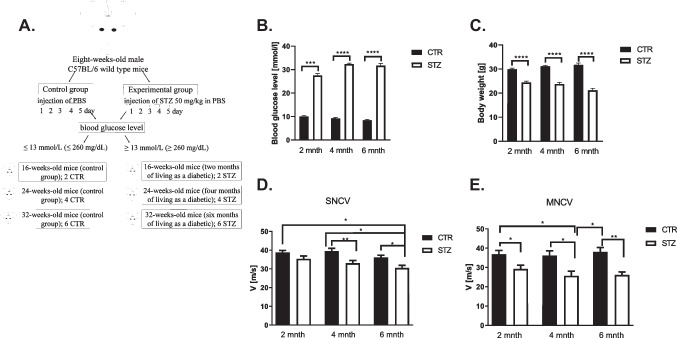
Fig. 1.
Diabetic neuropathy study. A Experiment diagram B The effect of type 1 diabetes (T1D) on glucose level. C The impact of T1D on body weight in mice, analyzed by Kruskal–Wallis test. Data are expressed as means ± SEM; * P ≤ 0.05, ** P ≤ 0.01; *** P ≤ 0.001; **** P ≤ 0.0001; n = 12 mice in each group. D Sensory nerve conduction velocity (SNCV) in the diagnosis of diabetic peripheral neuropathy (DPN). For SNCV, the sural nerve was stimulated orthodromically using needle electrodes placed in the fourth toe of the foot, with recording via needle electrodes in the gastrocnemius muscle. Sensory conduction velocity was calculated by dividing the distance between the stimulating and recording electrodes by this latency. E The effect of T1D on motor nerve conduction velocity (MNCV). The MNCV was calculated by the dividing in distance between electrodes placed upper thigh near midline at the sciatic notch and electrodes placed in the popliteal fossa (measured with a fine caliper) by a difference in latency during stimulation at the sciatic notch compared with that obtained during popliteal fossa stimulation to yield a velocity in meters per second. The studies were performed using Nicolet Viking Quest Apparatus and Nicolet Viking, version X computerized system (CareFusion, San Diego, CA, USA). One-way ANOVA followed by Tukey's HSD post hoc test was used to indicate the effect of diabetes on alterations in SNCV as well as MNCV. Finally, in case of SNCV and MNCV, two-way ANOVA was performed to evaluate the effects and interactions among factors (diabetes status and duration of diabetes) followed by the Tukey’s HSD post-hoc test. Data are expressed as means ± SEM; * P ≤ 0.05, ** P ≤ 0.01; n = 12 mice in each group. Abbreviation: CTR – control, STZ – diabetes, mnth – month
Nerve conduction velocity (NCV)
Measurement of SN electrophysiological activities was performed using Nicolet Viking Quest Apparatus (CareFusion, San Diego, CA, USA) as previously described [1, 5, 16]. Prior to motor (MNCV) as well as sensory nerve conduction velocity (SNCV) studies, all animals (n = 12; [17, 18]) were anesthetized as described previously [1].
Morphometric and ultrastructural studies (scanning electron microscope, SEM)
Nerve samples (n = 5 per group; at 6 months of experiment; [19]) were immersion-fixed in a mixture of 1% paraformaldehyde and 2.5% glutaraldehyde in 0.2 M cacodylate buffer (pH 7.4) for 2 h at 4 °C.
The morphometric and ultrastructural analysis of semithin sections
Semithin sections (n = 5, [19]) were stained with 1% toluidine blue and digitalized at 40× objective using PANNORAMIC 250 Flash III scanner (3DHistech, Budapest, Hungary). Samples for scanning electron microscopy (SEM) imaging were post-fixed in a solution containing 2% aqueous osmium tetroxide [20].
The expression of Diaph1, RAGE and beta-actin (ACTB) in SN
RNA isolation and reverse transcription
Total RNA was isolated from a whole, unilateral SN (n = 4, [19]) with the use of TRI Reagent® (Sigma Aldrich, USA), according to the manufacturer’s protocol. Reverse transcription was conducted using the QuantiNova Reverse Transcription Kit (Qiagen, Valencia, CA, USA).
The expression of Diaph1, gene encoding RAGE (AGER) and ACTB mRNAs
The expression of Diaph1, AGER and ACTB (Table 1) in SN harvested from each group (Fig. 1A) were analyzed in duplicates by LightCycler® 480 Instrument II (Roche Diagnostics, Switzerland). The relative amplification of genes was calculated using the ΔΔCt method.
Table 1.
TaqMan gene expression assays (ThermoFisher) used for qPCR
| Gene symbol (official) | Assay ID | Catalog no. | Amplicon lenght (nt) | Dye |
|---|---|---|---|---|
| DIAPH1 | Mm01258311_m1 | 4448892 | 64 | 6-carboxyfluorescein (6-FAM) |
| ACTB | Mm00607939_s1 | 4453320 | 115 | |
| AGER | Mm01134790_g1 | 4351368 | 65 | |
| 18S rRNA | Mm03928990_g1 | 4453320 | 61 |
Localization and immunoreactivity of Diaph1, RAGE and ACTB proteins
The presence of Diaph1, RAGE and ACTB in SN sections was determined using a two-day procedure for semi-quantitative immunohistochemical (IHC) staining [1] (Table 3). Eight micron tissue samples were air dried and incubated with primary antibodies (Table 3) diluted in 0.1% BSA, overnight. To visualize the immunoreactivity, slides were incubated with 3,3 diaminobenzidine tetrahydrochloride (DAB, Sigma-Aldrich, USA) as well as with hematoxylin (Sigma-Aldrich, USA).
Table 3.
Characteristics of antibodies used in experiments
| Primary antibody | ||||||
|---|---|---|---|---|---|---|
| Protein | Type | Species | Dilution | Usage | Manufacturer and catalog no. | |
| DIAPH1 | polyclonal | rabbit | 1:100 | IHC | Abcam, ab11173 | |
| polyclonal | rabbit | 1: 1 000 | WB | Abcam, ab129167 | ||
| polyclonal | rabbit | 1:50 | IF | ThermoFisher, PA5-96420 | ||
| ACTB | polyclonal | rabbit | 1:200 | IHC | Synaptic Systems, 251003 | |
| monoclonal | mouse | 1: 50 000 | WB | Abcam, ab6276 | ||
| polyclonal | chicken | 1:500 | IF | Synaptic System, 251006 | ||
| RAGE | polyclonal | rabbit | 1:50 | IHC | Abcam, ab37647 | |
| polyclonal | rabbit | 1:5 000 | WB | Abcam, ab37647 | ||
| PFN1 | monoclonal | rabbit | 1: 1 000 | WB | Abcam, ab232020 | |
| monoclonal | rabbit | 1:100 | IF | Abcam, ab232020 | ||
| CML | polyclonal | rabbit | 1: 5 000 | WB | Abcam, ab27684 | |
| HMGB1 | polyclonal | rabbit | 1: 1 000 | WB | Abcam, ab18256 | |
| S100B | monoclonal | rabbit | 1: 1 000 | WB | Abcam, ab52642 | |
| S100A6 | monoclonal | rabbit | 1: 1 000 | WB | Abcam, ab134149 | |
| SOD1 | polyclonal | rabbit | 1: 5 000 | WB | Abcam, ab13498 | |
| Secondary antibody | ||||||
|---|---|---|---|---|---|---|
| Reagent | Host | Species reactivity | Dilution | Usage | Manufacturer and catalog no | |
| StarBright Blue 700 IgG | goat | rabbit | 1: 10 000 | WB | BioRad, 12004162 | |
| StarBright Blue 800 IgG | goat | mouse | 1: 10 000 | WB | BioRad, 12004158 | |
| IgG (H + L), Alexa Fluor Plus 594 | goat | rabbit | 1: 2 000 | IF | ThermoFisher, A11039 | |
| IgY (H + L), Alexa Fluor 488 | goat | chicken | 1: 2 000 | IF | ThermoFisher, A-32740 | |
Explanation of abbreviations: WB Western blot analysis, IF immunofluorescence staining, IHC immunohistochemistry staining
The content of Diaph1, profilin 1 (PFN1), N(epsilon)-(carboxymethyl)lysine-AGEs (CML–AGEs), high mobility group box 1 (HMGB1), S100 calcium binding protein B (S100B), S100 calcium binding protein A6 (S100A6), superoxide dismutase type 1 (SOD1), ACTB and RAGE proteins in SN
Protein extraction
Whole SN (n = 6 per group; [19]) was homogenized with isolation buffers (Eurx®, Poland) in MagNA Lyser (Roche Diagnostics, Switzerland) according to the manufacturer’s protocol (Universal DNA/RNA/Protein Purification Kit, Eurx®). The protein concentration was determined using Direct Detect® Infrared Spectrometer for Total Protein Quantitation (Merck Millipore, Darmstadt, Germany).
Western blot analysis
Proteins were separated on gels and transferred onto nitrocellulose membrane using semi-dry system. Subsequently, the membrane was incubated in Blocking Buffer (Bio-Rad) and primary antibody solutions (Table 3). Images were quantified densitometrically with Image Lab v6.0.1 software.
Co-localization of Diaph1 and ACTB as well as ACTB and PFN1 in SN
To investigate the co-expression and co-localization between Diaph1 and ACTB as well as ACTB and PFN1 in mouse SN, samples were collected six months after induction of diabetes (Fig. 1A). Immunofluorescence staining was performed according to standard laboratory protocols [3–6].
Next-generation sequencing procedure
Total RNA was extracted from lumbar SC neuromere (n = 5 per group; [19]) harvested from 32-weeks-old mice. Subsequently, RNA integrity (RIN), quality and quantity were evaluated with microcapillary electrophoresis (2100 Bioanalyzer, Agilent Technologies, Santa Clara, CA, USA). Only samples with RIN above 8 were used for further analysis. The sequencing reactions were performed on the NovaSeq 6000 platform (Illumina®, USA) to generate 2 × 150 bp paired-end reads and 40 million readings per sample. Sequencing data was converted into raw data for the in silico analysis (Supplementary Fig. 1).
Functional analysis of differentially expressed genes (DEGs)
The list of DEGs was uploaded to DAVID 6.8 to identify enriched biological themes, Gene Ontology (GO) terms and visualize KEGG pathways [22–24]. Further, the list of selected genes among DEGs in lumbar SC of diabetic mice with AGER, Diaph1 and ACTB was uploaded to the GeneMANIA Prediction Server [25].
The expression of hydroxyacid oxidase 1 (HAO1), neuroepithelial cell transforming 1 (NET1), ras homolog family member J (RHOJ), thioredoxin interacting protein (TXNIP), cathepsin E (CTSE) mRNAs in lumbar SC neuromere harvested in six months of diabetes
The expression of selected genes (Table 2) in lumbar SC harvested from diabetic mice (Fig. 1) performed by quantitative PCR (qPCR).
Table 2.
Primers used for validation of NGS results
| Official gene symbol | Sequences | NCBI reference sequence | Amplicon lenght (nt) | References | |
|---|---|---|---|---|---|
| Differentially expressed genes | |||||
| HAO1 | F: AGAGTCAGCATGCCAATATG | NM_010403.2 | 155 | - | |
| R: GCTTCTGCCACTTCTTCTATT | |||||
| NET1 | F: ACACCCACCAAGAGAAGA | NM_019671.3 | 139 | - | |
| R: CCTCAATCAAGTCCTGTTCC | |||||
| RHOJ | F: TGTGTTTCTCATCTGCTTCTC | NM_023275.2 | 128 | - | |
| R: GATCAATCTGGGTTCCGATG | |||||
| TXNIP | F: CAGTCAGAGGCAATCACATTA | NM_023719.2 | 131 | - | |
| R: GTAGATCAGCAAGGAGTATTCG | |||||
| CTSE | F: CATATACCCTCAACCCAACTG | NM_007799.3 | 146 | - | |
| R: GTAGAACTGTCGGATGAAGAC | |||||
| Reference genes | |||||
| 18S rRNA | F: GGGAGCCTGAGAAACGGC | NR_003278.3 | 68 | [26] | |
| R: GGGTCGGGAGTGGGTAATTT | |||||
| IPO8 | F:CTATGCTCTCGTTCAGTATGC | NM_001081113.1 | 173 | [21] | |
| R: GAGCCCACTTCTTACACTTC | |||||
The comparison of SC and SN transcriptomes in diabetes
The comparison of DEGs in SC of T1D with the DEGs in T1D and T2D SN [27, 28] obtained from Gene Expression Omnibus (GEO) database (http://www.ncbi.nlm.nih.gov.geo/) was performed by creating a Venn diagram [29].
Statistical analyses
Analyses with P values ≤ 0.05 were considered statistically significant. All data were presented as mean ± SEM. Before selecting the appropriate statistical test, we have performed the normality and lognormality test, i.e. Shapiro–Wilk test. Moreover, all datasets were tested for presence of outliers by using the Grubbs’ test (α = 0.05). Statistical analyses and graphs were performed using GraphPad Prism 9.1.0. (CA, USA).
Results
Induction of diabetes and loss of weight in mice
Blood glucose was increased already by over two folds at two months post-STZ injections in the experimental group and remained elevated throughout the study as to control groups (P ≤ 0.001, P ≤ 0.0001, respectively, Fig. 1B). No differences in weight and blood glucose level between control groups of mice were observed (P ≥ 0.05, Fig. 1B, C), however following the progression of the disease, steady decline in body mass was noted in diabetic groups (P ≤ 0.0001 in all cases, Fig. 1C).
Effect on SN conduction velocity
We found that in T1D animal group, NCV was reduced both in MNCV and SNCV (Fig. 1D, E). The SNCV was lower at all time points in diabetic groups as compared to controls, however statistically significant reduction was noted first at 4 month and subsequently at 6 month of diabetes (P ≤ 0.01, P ≤ 0.05, respectively, Fig. 1D). In the control group no significant alteration of SNCV was observed during the entire period (P ≥ 0.05, Fig. 1D). MNCV was significantly decreased as early as two months when compared to controls and declined throughout the study in diabetic groups as compared to controls (P ≤ 0.05, P ≤ 0.05, P ≤ 0.01, respectively, Fig. 1E). Again, we did not observe a decline in MNCV during the examined period in the control group (P ≥ 0.05, Fig. 1D, E).
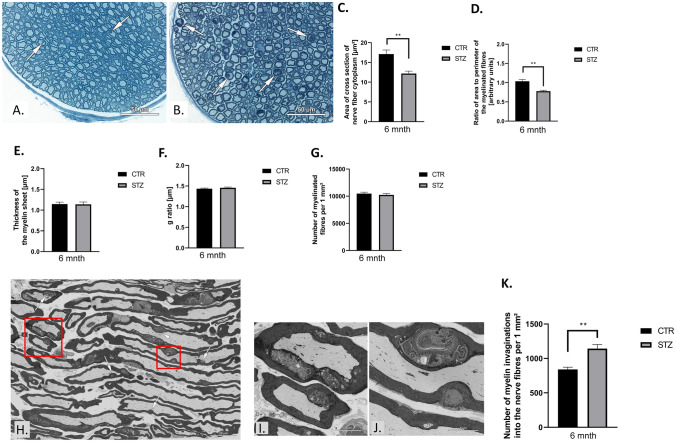
SN morphometry in T1D murine model
Toluidine blue stained semithin sections of diabetic SN showed no differences in the appearance of epineurium, perineurium and endoneurium (Fig. 2A, B). The analysis showed that the cytoplasm area of nerve fiber transverse section as well as the ratio of area to perimeter of these sections were decreased at sixth month of the experiment in the diabetic group (P ≤ 0.01 in both cases; Fig. 2C, D). Diabetes did not affect the myelin sheet thickness g-ratio as well as the number of myelinated nerve fibers per 1 mm2 of the nerve section (P ≥ 0.05, Fig. 2E−G, respectively).
Fig. 2.
Type 1 diabetes (T1D) leads to morphometric, morphological and ultrastructural alternations in mouse peripheral nerves. A, B Toluidine blue-stained semithin sections used for morphometrical and morphological analyses. Representative parts of the transverse sections through the nerves of control mouse (A) and (B) STZ-treated mouse. Arrows show myelin invaginations into nerve fibers. Digital scans of semithin sections were used for measurements of cross section perimeter of nerve fiber and the thickness of the myelin sheet, for counting of the myelinated fiber per area unit. The right upper part of the semithin section with the area of 25 000 µm2 was chosen for analysis and all myelinated fibers located inside this area were measured. No less than 200 nerve fibers were measured per animal. Measurements were made using CaseViewer 2.1 (3DHistech Ltd, Budapest, Hungary). Scale bar = 50 µm. C T1D alters the area of cross section of nerve fiber cytoplasm as well as D the ratio of area to perimeter of the myelinated fibers. The T1D in not affected on E the thickness of myelin, F g ratio and G number of myelinated fibers per 1 mm2. H Myelin structure of sciatic nerve per longitudinal section area. The areas marked with red rectangles in I-J after zooming in. Scale bar = 5 µm. K Myelin structure of diabetic nerve fibers shows alternations in frequency of myelin invaginations. The whole sections were imaged using a backscatter detector in SEM Gemini 450 at 1.5 kV controlled by Atlas 5 software (Carl Zeiss, Oberkochen Germany). The digital ultrastructural images of longitudinal sections obtained in SEM were used for the semiquantitative analysis of myelin structure alternations, which was performed in the ATLAS Browser-Based Viewer 3.0. The analysis of semithin sections was performed with Student's t-test or U Mann–Whitney test. Data are expressed as means ± SEM; * P ≤ 0.05, ** P ≤ 0.01; n = 5 mice in each group. Abbreviation: CTR – control, STZ – diabetes, mnth – month
The occurrence of myelin infoldings (Fig. 2H–K) was significantly higher in STZ-treated mice (P ≤ 0.01; Fig. 2K). These alterations locally affected diameter of the nerve fibers and the shape of their sections. Their occurrence was not usually close to the Schmidt-Lanterman’s incisures and the Ranvier’s nodes (Fig. 2H–K).
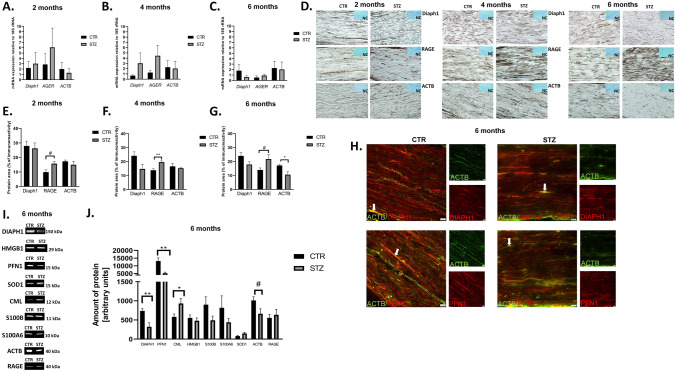
The effect of T1D on the expression of Diaph1, RAGE, ACTB in mouse SN
The expression of Diaph1, AGER (gene coding RAGE) and ACTB mRNAs did not reach statistical significance (Fig. 3A–C). IHC revealed that at all examined time points Diaph1, RAGE and ACTB proteins were present in mouse SN (Fig. 3D). We observed an increasing trend of RAGE immunoreactivity area at two and six months of diabetes when compared with controls (P = 0.0551, P = 0.0527, respectively; Fig. 3E, G). Intensity of RAGE immunostaining at four months of diabetes was significantly elevated when compared to control group (P ≤ 0.01; Fig. 3F). Moreover, IHC staining revealed that intensity of ACTB immunostaining was decreased at all time points and reached statistical significance at sixth month of T1D comparing to controls (P ≥ 0.05, P ≥ 0.05, P ≤ 0.05; respectively, Fig. 3G).
Fig. 3.
The effect of T1D on the expression of Diaph1, RAGE, ACTB in mouse SN. A B C The expression of Diaph1, AGER (gene encoding RAGE) and ACTB mRNAs in SN under hypoglycemic milieu vs. control group in two (A), four (B) and six (C) months of the experiment, respectively. Data are expressed as means ± SEM; n = 4 mice in each group. D Immunostaining of Diaph1, RAGE and ACTB under hyperglycemic conditions in mice SN. Negative control (NC) showed no immunostaining. Brown color demonstrated immunoreactive area of stain. Blue color demonstrated hematoxylin staining. Images were taken under 40× objective with 0.75 numerical aperture (40× /0.75). Scale bar = 100 µm. E F G The number of Diaph1, RAGE, ACTB fibers expression/immunoreactivity in diabetic SN as compared to control tissue in two (E), four (F) and six (G) months of the experiment, respectively. Data are expressed as means ± SEM; * P ≤ 0.05, ** P ≤ 0.01; # 0.05 ≤ P ≤ 0.056; n = 4 mice in each group. I Representative blots for Diaph1, PFN1, CML-AGE, HMGB1, S100B, S100A6, SOD1, ACTB and RAGE proteins of control (CTR) and after six months of T1D (STZ; see also supplementary files). Abbreviation: kDa – kilodalton. J The effect of T1D on the relative amount of Diaph1, PFN1, CML-AGE, HMGB1, S100B, S100A6, SOD1, ACTB and RAGE proteins in SN mice. Data are expressed as means ± SEM; * P ≤ 0.05, ** P ≤ 0.01; n = 6 CTR or 7 STZ. H Co-localization (arrows, yellow staining) of Diaph1-ACTB and ACTB-PFN1 in mice SN of T1D. Images were taken under 40× objective with 0.6 numerical aperture (40× /0.6). Scale bar = 20 µm. Abbreviation: CTR – control, STZ – diabetes, # - P = 0.07
The effect of diabetes on Diaph1, PFN1, CML–AGEs, HMGB1, S100B, S100A6, SOD1, ACTB and RAGE expression in mouse SN
Our results indicated that Diaph1 was reduced in diabetic SN compared to controls (P ≤ 0.01, Fig. 3J), consistent with earlier studies. At six months of diabetes the amount of Diaph1 as well as PFN1 was decreased and the relative amount of CML-AGE was elevated when compared to control mice (P ≤ 0.01, P ≤ 0.01, P ≤ 0.05, respectively, Fig. 3J). We did not observe differences in the relative amount of HMGB1, S100B, S100A6 and SOD1 proteins in SN harvested from diabetic and control mice at six months after diabetes induction in our experiment (P ≥ 0.05, Fig. 3J). Intensity of ACTB expression at six months of diabetes showed a downward trend compared to the control group (P = 0.07; Fig. 3J). However, we observed a trend towards increased RAGE expression in STZ mice, consistent with CML-AGE (Fig. 3J). Our analysis confirmed the specificity of antibody and protein expression patterns in mice sciatic nerve (Fig. 3I). Finally using immunofluorescence, we observed co-localization of Diaph1-ACTB and ACTB-PFN1 in SN of T1D mice (Fig. 3H).
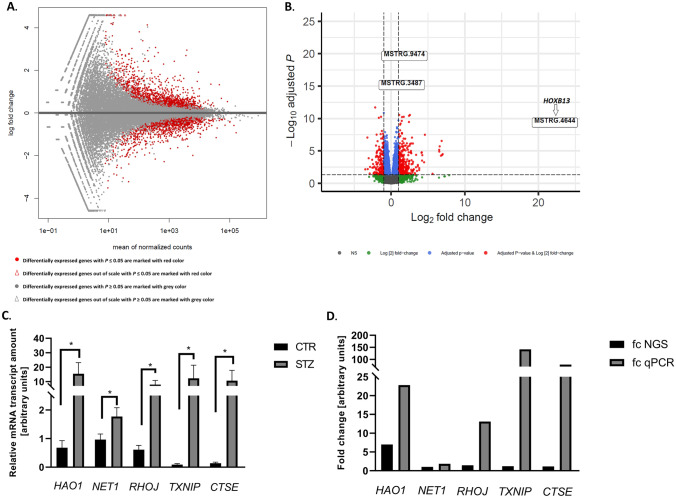
Sequencing results
More than 18 million (M) reads in each sample were achieved (Supplementary Fig. 1). After the trimming, reads were mapped to the reference mouse genome vGRCm39.104 from the Ensemble database (Supplementary Fig. 2). Principal component analysis (PCA) showed a high transcriptome differentiation between diabetics and controls (Supplementary Fig. 3).
We then analyzed the expression profiles of DEGs in the diabetic lumbar SC samples. Approximately 31 453 transcripts were identified in lumbar SC (Fig. 4A). Analysis revealed that among 31 453 transcripts, 538 genes revealed differential expression in studied samples (P ≤ 0.05; Fig. 4B, Supplementary Table 1). Among 538 (248 up- and 137 down-regulated) DEGs, 385 had known official gene symbol (Supplementary Table 1) and of those, 330 has known biological function as per DAVID database. The highest expression gene was homeobox B13 (HOXB13; Fig. 4B) and the most down-regulated gene was RIKEN cDNA 5033426O07 gene (5033426O07Rik, Supplementary Table 1). Further, of those 330 genes we found genes affiliated with long non-coding RNAs (lncRNAs), such as: small nucleolar RNA host gene 15 (SNHG15, up-regulated) and deleted in lymphocytic leukemia 2 (DLEU2, down-regulated). The expression of SPOC domain containing 1 (SPOCD1) piwi-interacting RNA (pi-RNA) was up-regulated in lumbar SC of mice with T1D (Supplementary Table 1). We were able to validate expression of many of the prominent DEGs, i.e. hydroxyacid oxidase 1 (HAO1), neuroepithelial cell transforming 1 (NET1), ras homolog family member J (RHOJ), thioredoxin interacting protein (TXNIP), cathepsin E (CTSE) with RNA-Seq results (Fig. 4C). Results of qPCR confirmed the veracity of the RNA-Seq data (Fig. 4D).
Fig. 4.
Overall statistics of RNA-seq data. A MA plot shows the logarithmic value of log fold change (fc; Y axis) and mean of normalized counts (X axis) for comparing STZ-treated and control libraries. B Volcano plot indicates logarithmic value of fold change (fc; X axis) and negative logarithmic adjusted P values (Y axis). On both plots DEGs with P ≤ 0.05 are marked red dots. The HOXB13 is the most altered genes in diabetic spinal cord. NS – no significant. C The relative mRNA expression of genes with altered expression in mouse lumbar SC under hyperglycemic conditions. The amount of mRNA transcript are presented as a mean 2−ΔΔCt values ± SEM. * P ≤ 0.05, ** P ≤ 0.01; n = 4 mice in each group. D Fold change (fc) of selected genes in lumbar SC harvested from T1D mice. The results were consistent throughout the study
Functional gene analysis
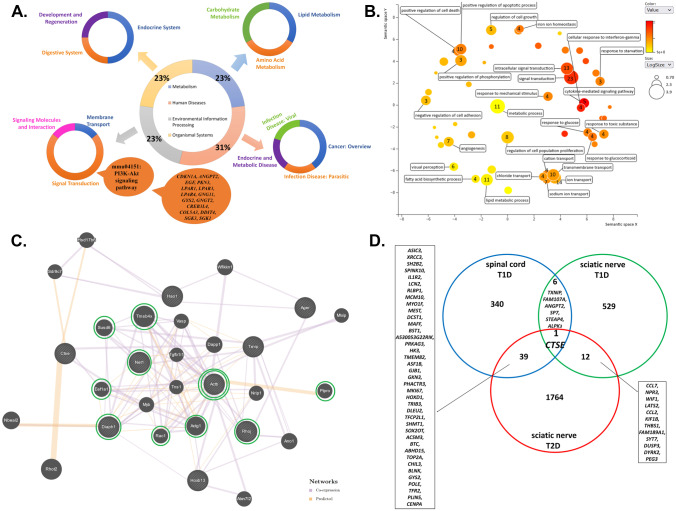
The gene ontology (GO) enrichment analysis suggested that among DEGs, a total of 330 with known biological functions could be categorized under the hierarchical GO terms (Supplementary Tables 2, 3 and 4). Briefly, within the biological process (BP) aspect, DEGs were enriched in 55 functions (Fig. 5B). In molecular function (MF) hierarchy, there were 17 significant GO terms; in case of cellular component (CC) hierarchy, DEGs were enriched to 10 GO terms (Supplementary Tables 2, 3 and 4). The further analysis of the 330 DEGs demonstrated four major categories, including environmental information processing, metabolism, human diseases, organismal systems and 13 subcategories (Fig. 5A) as well as 19 biological pathways (Supplementary Table 5). The most enriched biological pathway in lumbar SC neuromere from STZ-treated mice was PI3K-Akt signaling pathway (mmu04151, Fig. 5A, Supplementary Table 5). The DEGs in GO enriched categories of BP were mainly involved in signal transduction (GO:0007165), intracellular signal transduction (GO:0035556), ion transport (GO:0006811), metabolic process (GO:0008152), lipid metabolic process (GO:0006629), transmembrane transport (GO:0055085), positive regulation of apoptotic process (GO:0043065), regulation of cell proliferation (GO:0042127), sodium ion transport (GO:0006814) and angiogenesis (GO:0001525; Fig. 5B).
Fig. 5.
Functional DEGs analysis. A The diagram of expression data for DEGs with known biological functions and their participation in signaling pathways from KEGG database. The analysis of signaling pathways demonstrated four major categories, such as: environmental information processing, metabolism, human diseases, organismal systems (central pie chart), and 13 subcategories (lateral pie chart). The most enriched biological pathway in lumbar SC from STZ-treated mice was the PI3K-Akt signaling pathway (mmu04151). The cloud indicates genes involved in PI3K-Akt signaling pathway. B Functional analyses of DEGs by REVIGO gene ontology (GO) enrichment analysis [50]. The most representative GO terms for biological process (BP) were utilized for REVIGO functional annotation clustering that relies on semantic similarity measures. Bubble color corresponds the P-value obtained from GO enrichment analysis, whereas the bubble size corresponds to the GO term prevalence in the UniProt-GOA database for Mus musculus. Arabic numeral indicates the number of DEGs in SC. See also Supplementary Table 2 for details on the GO-BP terms. C Gene interaction network constructed with a use of GeneMANIA for selected set of genes, i.e. HOXB13, HAO1, NET1, RHOJ, TXNIP, CTSE, AGER, DIAPH1, ACTB (limited to Mus musculus). The selected genes are in a striped circle. The colors of the line suggest the type of interaction (see legend). In silico analysis indicated that ACTB gene has the most direct interactions (double green circle). Green circles indicate genes that have a direct interaction with ACTB, i.e. NET1, TMSB4X, SUSD6, EEF1A1, DIAPH1, RAC1, ACTG1, RHOJ, PTPRO genes. See also Supplementary Table 6 for details on the interaction network. D Venn diagram [29] representing DEGs in SC of T1D, SN of T1D and T2D [27, 28]. The analysis showed that the expression of a one, single gene, i.e. CTSE was altered for all tissue transcriptome profiles
Interaction network
The GeneMANIA analysis of selected genes, i.e. HAO1, NET1, RHOJ, TXNIP, CTSE (based on validation), DIAPH1, AGER and ACTB (based on our previous studies and literature) as well as the highest expressed gene in diabetic spinal cord, i.e. HOXB13, revealed that all of them were connected in single network (Fig. 5C). It was constructed by 29 genes (20 related genes) and consisted of a total number of 122 interactions. Moreover, genes building a network were involved in the following functions: transepithelial transport (ACTB, actin gamma 1 (ACTG1)), actin polymerization or depolymerization (thymosin beta 4 x-linked (TMSB4X), vasodilator stimulated phosphoprotein (VASP), DIAPH1, rac family small GTPase 1 (RAC1)), structural constituent of synapse (ACTB, ACTG1), regulation of actin filament organization (TMSB4X, VASP, ACTG1, RAC1), cell-substrate junction organization (tensin 1 (TNS1), ACTG1, RAC1), structural constituent of postsynapse (ACTB, ACTG1), ruffle (eukaryotic translation elongation factor 1 alpha 1 (EEF1A1), DIAPH1, RAC, cellular response to glucose stimulus (RAC1, anoctamin 1 (ANO1)), protein localization to cell–cell junction (ACTB, ACTG1) and protein polymerization (TMSB4X, VASP, DIAPH1, RAC1). In silico analysis revealed that ACTB was a node of the network and the most common interaction between genes was co-expression (Supplementary Table 6). We found that ACTB gene has direct interactions, i.e. co-expression, with sushi domain containing 6 (SUSD6), TMSB4X, EEF1A1, RHOJ, ACTG1, RAC1, NET1, DIAPH1 genes as well as predicted interaction with protein tyrosine phosphatase receptor type O (PTPRO) gene (Fig. 5C).
Comparison of SC and SN transcriptomes in diabetes
Among all studied DEGs, 385 in SC, 548 in SN of T1D and 1816 in SN of T2D, the expression of only one gene, i.e. Cathepsin E (CTSE) was altered in all cases (Fig. 5D; [27, 28]). Both in the SC of T1D and SN of T1D or T2D seven and 40 genes were commonly altered, respectively (Fig. 5D).
Discussion
Our results indicate that the progression of DPN is associated with alterations in NCV, morphometry and SN ultrastructure as well as the expression of molecules in RAGE-Diaph1 signaling pathway. Diaph1 has the ability to regulate actin polymerization and modification of actin cytoskeleton in nervous system [1, 2, 9, 30, 31]. The reduction in the amount of Diaph1 may lead to abnormal organization of actin cytoskeleton in diabetic SN [1, 2, 9, 30, 31]. In line with this reported association, our data revealed reduction of ACTB and PFN1 in SN after six months of T1D. PFN1 is a master regulator of cytoskeleton structure and may enhance F-actin elongation. Overexpression of PFN1 may however prevent the polymerization of ACTB [32]. PFN1 dysfunction may lead to changes in the structure of nuclear membrane, with the presence of frequent folds and invaginations [32]. Indeed we observed myelin invaginations into nerve fibers and a decline in SN myelinated axons in hyperglycemic environment. Moreover, we observed elevated presence of CML-AGEs in diabetic SN [3–9]. Evidence shows that excessive deposition of AGEs, reactive derivatives of methyl-glyoxal, is a hallmark of extensive glycation likely affecting cytoskeleton proteins and thus damage the actin cytoskeleton of nerve fibers in diabetic SN [33].
Overall, our data confirmed that T1D affects PNS. However, the soma of motor neuron for SN resides in lumbar SC, therefore we decided to look at molecular changes in lumbar SC in contrast to previous studies which focused solely on SN [9, 10].
Our sequencing analysis demonstrated that DEGs in lumbar SC were the most representative in BP GO term. The most enriched categories were those related to signal transduction, with PI3K-Akt signaling pathway (mmu04151) being the most enriched pathway. PI3K-Akt signaling pathway is engaged in multiple functions in cells, such as metabolism, cell survival, proliferation and angiogenesis in response to extracellular factors. It is also involved in the regulation of glucose level in cells and regeneration of PNS as well as nerves growth in CNS [34]. To date, countless previous studies have showed that the neurotrophins and nerve growth factor may active PI3K-Akt pathway in nervous system [34–37]. Hence, the PI3K-Akt signaling pathway plays a crucial role in mediating the survival as well as neurite outgrowth processes in PNS and CNS [34–37]. How aberrant function of this pathway may affect progression of DPN will be topic of future research and may provide target for intervention in DPN.
Our results suggest that the expression of SNHG15 lncRNAs was up-regluated in SC of diabetic mice. SNHG15 lncRNA alters the expression level of target proteins like TXNIP [38, 39]. Increase in expression of TXNIP was reported in the plasma of diabetic patients [40]. Dunn and co-workers [41] showed that elevated expression of TXNIP protein may trigger endothelial dysfunctions by inhibiting synthesis of vascular endothelial growth factor (VEGF). Our study demonstrates simultaneous overexpression of SNHG15 as well as TXNIP in lumbar SC of T1D mice. We speculate that elevated expression of SNHG15 may be compensatory to overexpression of TXNIP in lumbar SC in hyperglycemia. However, further studies are needed to elucidate SNHG15 lncRNA effect on the TXNIP expression pattern in diabetes.
The GeneMANIA analysis revealed that genes involved in oxidative stress (HAO1), RhoA signaling pathway (NET1, RHOJ), endothelial dysfunctions (TXNIP), transcription process (HOXB13), inflammation (AGER) neuronal death signaling pathway (CTSE), axonal cytoskeleton, actin polymerization (DIAPH1) and cytoskeleton remodeling (ACTB) were connected in singular network [3–9, 41–45]. The analysis showed that ACTB has direct links with genes related to RhoA signaling pathway (NET1), formation of F-actin-rich structures (RHOJ), axonal cytoskeleton, actin polymerization (DIAPH1, TMSB4X, EEF1A1, ACTG1, RAC1, ACTG1), growth-suppressive and cell death (SUSD6), GTPase and actin bundling protein (EEF1A1), glucose uptake as well as activate the PI3K kinase (RAC1), cell adhesion as well as cell-surface mediated signaling (ITGA6), transports of proteins to the lysosomes (CHAMP1A), diabetic kidney disease (PTPRO) [46–49]. Overall, we observed that most of the aforementioned genes are involved in cytoskeletal reorganization as well as actin polymerization.
Interestingly, we identified a single gene CTSE as an intersection point of DEGs from T1D SC, T1D and T2D SN. It is pertinent to mention that while the expression of CTSE in SN of T2D as well as lumbar SC of T1D was elevated it was declined in SN harvested from T1D mice [27, 28]. The function of CTSE is not well understood, however it may play a role in amyloid polyneuropathy, neuropathy in experimental autoimmune encephalitis and neuroinflammation associated with Alzheimer’s disease [47–49]. Cathepsin E enzyme is involved in neuronal death signaling pathway [45]. Moreover, bioinformatic analysis of DEGs associated with SC injury revealed that CTSE gene was up-regulated [49]. Thus it is likely that CTSE may be a common molecule that is dysregulated in neurological disorders and may serve as a broad target for DPN and other neurodegenerative diseases warranting further investigations. Our studies revealed that molecular perturbations in SC may also be involved in the progression of DPN.
Overall, our results showed that alterations of diabetic SC transcriptome may act synergistically with changes in RAGE-Diaph1 signaling pathway in diabetic SN. However, in both SC and SN in hyperglycemia, the expression of one, single gene, i.e. CTSE involved in neuronal death signaling pathway was affected. Further, our results revealed that PI3K-Akt axis may be involved in progression of DPN.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary Fig. 1. The diagram of raw data analysis – in silico analysis. The md5sum is designed to verify data integrity using Message Digest Algorithm 5 (MD5). Consequently, regions of row reads were trimmed with use of Trimmomatic v0.38 program. Next, mapping was performed using STAR tool. For mapping the Mus musculus GRCm39 was used as the reference genome with annotation version GRCm39.104 downloaded from Ensembl database (https://www.ensembl.org/index.html). Statistical analyses of differentially expressed genes (DEGs) for protein-coding RNA affected by long term hyperglycemia was performed using Ballgown, dedicated Bioconductor v3.14 (https://bioconductor.org/packages/release/bioc/html/ballgown.html) package prepared for the R environment v4.1.2, with the following operating parameters: P-value < 0.05 and |log2FC| ≥ 0.5 (TIF 2504 KB)
Supplementary Fig. 2. Summary of the results of RNA sequencing, preprocessing, and mapping of reads to the mice reference genome (Mus musculus GRCm39.104). (TIF 1032 KB)
Supplementary Fig. 3. Principle component analysis (PCA). The PCA revealed the high level of differentiation between control and STZ-treated samples. Principal component analysis (PCA) and Euclidean distances between samples analysis were performed using ggplot2 library v3.3.5 (https://www.rdocumentation.org/packages/ggplot2/versions/3.3.5) and self-developed R script, to assess the overall similarity between transcriptomic profiles of RNA samples derived from diabetic and non-diabetic mice. Wheel – control, triangle – diabetes/STZ-treated mice. (TIF 510 KB)
Supplementary Table 1. Altered transcripts in lumbar spinal cord (SC) neuromere under hyperglycemic condition. (DOCX 120 KB)
Supplementary Table 2. The table with GO-BP terms(DOCX 25 KB)
Supplementary Table 3. The table with GO-MF terms (DOCX 17 KB)
Supplementary Table 4. The table with GO-CC terms (DOCX 18 KB)
Supplementary Table 5. Functional enrichment analysis of DEGs in diabetic spinal cord (SC) of mice by KEGG database (DOCX 19 KB)
Supplementary Table 6. The table of interaction network in mouse diabetic spinal cord (SC) by GeneMANIA analysis (DOCX 20 KB)
Supplementary file 1: Western blot raw data (DOCX 3728 KB)
Supplementary file 2: Detailed methodology (DOCX 24 KB)
Acknowledgements
The study described here was supported by the National Science Centre, Poland (Grant UMO-2018/30/E/NZ5/00458). KM is supported by 5 R01 EY033391 grant from NEI.
Abbreviations
- ACTG1
Actin gamma 1
- ACTβ/ACTB
Beta (β) isoform of actin/ beta actin
- AGEs
Advanced glycation end products
- ALS
Amyotrophic lateral sclerosis
- ANO1
Anoctamin 1
- BP
Biological process
- CC
Cellular component
- CMAPs
Compound muscle action potentials
- CML
Carboxymethyl-lysine
- CNS
Central nervous system
- CTSE
Cathepsin E
- DAVID
Database for Annotation, Visualization and Integrated Discovery
- DEGs
Differentially expressed genes
- DIAPH1
Diaphanous related formin 1
- DPN
Diabetic peripheral neuropathy
- EEF1A1
Eukaryotic translation elongation factor 1 alpha 1
- F-actin
Actin filaments
- GEO
Gene Expression Omnibus database
- GO
Gene Ontology
- HAO1
Hydroxyacid oxidase 1
- HMGB1
High-mobility group box 1 protein
- HOXB13
Homeobox B13 actin gamma 1
- IPO8
Importin 8
- lncRNAs
Long non-coding RNAs
- MF
Molecular function
- MNCV
Motor nerve conduction velocity
- NCV
Nerve conduction velocity
- NET1
Neuroepithelial cell transforming 1
- NGS
Next-generation sequencing
- PFN1
Profilin 1
- pi-RNA
Piwi-interacting RNA
- PTPRO
Protein tyrosine phosphatase receptor type O
- PNS
Peripheral nervous system
- qPCR
Quantitative PCR
- RAC1
Rac family small GTPase 1
- RAGE
Receptor for advanced glycation end-products
- RHOJ
Ras homolog family member J
- RT
Room temperature
- SC
Spinal cord
- SEM
Scanning electron microscopy
- SN
Sciatic nerve
- SNCV
Sensory nerve conduction velocity
- SNHG15
Small nucleolar RNA host gene 15
- SOD1
Superoxide dismutase 1
- SPOCD1
SPOC domain containing 1
- STZ
Streptozotocin
- SUSD6
Sushi domain containing 6
- S100B
S100 calcium-binding protein B
- S100A6
S100 calcium binding protein A6
- T1D
Type 1 diabetes
- T2D
Type 2 diabetes
- TXNIP
Thioredoxin interacting protein
- 18S rRNA
18S ribosomal RNA
- TMSB4X
Thymosin beta 4 x-linked
- TNS1
Tensin 1
- VASP
Vasodilator stimulated phosphoprotein
Author contributions
K.Z-W. tissue preparation, conduction of NCV, NGS, qPCR, IHC, IF experiments, data analysis and interpretation, preparation of figures, tables and manuscript draft, manuscript edition, summary and conclusion, preparation of abbreviations and references; K.M. contribution to the manuscript draft; A.K. tissue preparation, participated in NCV study, conduction of WB experiment; B.L. conduction of SEM experiment, A.P. participated in NCV experiment, J.W. support in the IHC experiment; M.B. support in the NGS experiment; M.Z. assistance in the IF staining; N.N. assisted with tissue preparation for WB experiment; J.J. assistance in the WB experiment; B.K. assisted with tissue preparation for SEM experiment; K.W. tissue procurement support; J.K.J. study design, funding acquisition, contribution to the manuscript draft. All authors approved the final version of the manuscript.
Funding
This work was supported by the National Science Centre, Poland; Grant no. UMO-2018/30/E/NZ5/00458.
Data availability
The original results presented in the study are included in the article, further inquiries can be directed to the corresponding author. RNA-seq data have been deposited in the ArrayExpress database at EMBL-EBI (www.ebi.ac.uk/arrayexpress) under accession number E-MTAB 12252.
Declarations
Ethics approval
Mouse experiments were performed in accordance with the Local Ethical Committee of Experiments on Animals in Olsztyn (Poland; decision no. 57/2019) and the studies were reported in accordance with ARRIVE guidelines (https://arriveguidelines.org).
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Conflicts of interest
The authors have no conflicts of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kamila Zglejc-Waszak, Email: kamila.zglejc@uwm.edu.pl, Email: kamilazglejc@gmail.com.
Judyta K. Juranek, Email: judyta.juranek@uwm.edu.pl
References
- 1.Jaroslawska J, Korytko A, Zglejc-Waszak K, et al. Peripheral Neuropathy Presents Similar Symptoms and Pathological Changes in Both High-Fat Diet and Pharmacologically Induced Pre- and Diabetic Mouse Models. Life (Basel, Switzerland) 2021;11(11):1267. doi: 10.3390/life11111267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zglejc-Waszak K, Mukherjee K, Juranek JK. The cross-talk between RAGE and DIAPH1 in neurological complications of diabetes: A review. Eur J Neurosci. 2021;54(6):5982–5999. doi: 10.1111/ejn.15433. [DOI] [PubMed] [Google Scholar]
- 3.Juranek JK, Geddis MS, Roasario R, Schmidt AM. Impaired slow axonal transport in diabetic peripheral nerve is independent of RAGE. Eur J Neurosci. 2013;38(8):3159–3168. doi: 10.1111/ejn.12333. [DOI] [PubMed] [Google Scholar]
- 4.Juranek JK, Kothary P, Mehra A, Hays A, Brannagan TH, 3rd, Schmidt AM. Increased expression of the receptor for advanced glycation end-products in human peripheral neuropathies. Brain and Behavior. 2013;3(6):701–709. doi: 10.1002/brb3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Juranek JK, Geddis MS, Song F, et al. RAGE deficiency improves postinjury sciatic nerve regeneration in type 1 diabetic mice. Diabetes. 2013;62(3):931–943. doi: 10.2337/db12-0632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Juranek JK, Aleshin A, Rattigan EM, et al. Morphological Changes and Immunohistochemical Expression of RAGE and its Ligands in the Sciatic Nerve of Hyperglycemic Pig (Sus Scrofa) Biochem Insights. 2010;3:47–59. doi: 10.4137/BCI.S5340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manigrasso MB, Pan J, Rai V. Small Molecule Inhibition of Ligand-Stimulated RAGE-DIAPH1 Signal Transduction. Sci Rep. 2016;6:22450. doi: 10.1038/srep22450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramasamy R, Friedman RA, Shekhtman A, Schmidt AM. The receptor for advanced glycation end products (RAGE) and DIAPH1: unique mechanisms and healing the wounded vascular system. Expert Rev Proteomics. 2019;16(6):471–474. doi: 10.1080/14789450.2018.1536551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Juranek J, Mukherjee K, Kordas B, et al. Role of RAGE in the Pathogenesis of Neurological Disorders. Neurosci Bull. 2022;38(10):1248–1262. doi: 10.1007/s12264-022-00878-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tesfaye S, Sloan G. Involvement of the central nervous system in diabetic distal symmetrical polyneuropathy. Journal of Xiangya Medicine. 2021;41:710–725. doi: 10.21037/jxym.2020.02.03. [DOI] [Google Scholar]
- 11.Zhang Y, Qu M, Yi X, et al. Sensorimotor and pain-related alterations of the gray matter and white matter in Type 2 diabetic patients with peripheral neuropathy. Hum Brain Mapp. 2020;41(3):710–725. doi: 10.1002/hbm.24834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Selvarajah D, Wilkinson ID, Maxwell M, et al. Magnetic resonance neuroimaging study of brain structural differences in diabetic peripheral neuropathy. 2014;37(6):1681–1688. doi: 10.2337/dc13-2610. [DOI] [PubMed] [Google Scholar]
- 13.Eaton SE, Harris ND, Rajbhandari SM, et al. Spinal-cord involvement in diabetic peripheral neuropathy. Lancet. 2001;358(9275):35–36. doi: 10.1016/S0140-6736(00)05268-5. [DOI] [PubMed] [Google Scholar]
- 14.Reske-Nielsen E, Lundbaek K (1968) Pathological changes in the central and peripheral nervous system of young long- term diabetics. II. The spinal cord and peripheral nerves. Diabetologia 4(1):34–43. 10.1007/BF01241031 [DOI] [PubMed]
- 15.Reske-Nielsen E, Lundbæk K, Rafaelsen OJ. Pathological changes in the central and peripheral nervous system of young long-term diabetics: I. Diabetic encephalopathy Diabetologia. 1966;1(3–4):233–241. doi: 10.1007/BF01257917. [DOI] [PubMed] [Google Scholar]
- 16.Schulz A, Walther C, Morrison H, Bauer R. In vivo electrophysiological measurements on mouse sciatic nerves. Journal of visualized experiments: JoVE. 2014;86:51181. doi: 10.3791/51181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu Y (2021) Gold Standard for Diagnosis of DPN. Front Endocrinol 12:719356. 10.3389/fendo.2021.719356 [DOI] [PMC free article] [PubMed]
- 18.Petropoulos IN, Ponirakis G, Khan A, Almuhannadi H, Gad H, Malik RA. Diagnosing Diabetic Neuropathy: Something Old. Something New Diabetes & metabolism journal. 2018;42(4):255–269. doi: 10.4093/dmj.2018.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janušonis S. Comparing two small samples with an unstable, treatment-independent baseline. J Neurosci Methods. 2009;179(2):173–178. doi: 10.1016/j.jneumeth.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 20.Kasukurthi R, Brenner MJ, Moore AM, et al. Transcardial perfusion versus immersion fixation for assessment of peripheral nerve regeneration. J Neurosci Methods. 2009;184(2):303–309. doi: 10.1016/j.jneumeth.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 21.Nowicka N, Szymańska K, Juranek J, et al. The Involvement of RAGE and Its Ligands during Progression of ALS in SOD1 G93A Transgenic Mice. Int J Mol Sci. 2022;23(4):2184. doi: 10.3390/ijms23042184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.da Huang W, Sherman BT, Lempicki RA. Bioinformatics enrichment tools: Paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Res. 2009;37(1):1–13. doi: 10.1093/nar/gkn923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.da Huang W, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID Bioinformatics resources. Nat Protoc. 2009;4(1):44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- 24.Kanehisa M, Goto S, Sato Y, Furumichi M, Tanabe M. KEGG for integration and interpretation of large-scale molecular data set. Nucleic Acids Res. 2012;40:D109–D114. doi: 10.1093/nar/gkr988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Warde-Farley D, Donaldson SL, Comes O et al (2010) The GeneMANIA prediction server: Biological network integration for gene prioritization and predicting gene function. Nucleic Acids Res 38(Web Server issue):W214–20. 10.1093/nar/gkq537 [DOI] [PMC free article] [PubMed]
- 26.Espíndola S, Vilches-Flores A, Hernández-Echeagaray E. 3-Nitropropionic acid modifies neurotrophin mRNA expression in the mouse striatum: 18S-rRNA is a reliable control gene for studies of the striatum. Neuroscience Bull. 2012;28(5):517–531. doi: 10.1007/s12264-012-1259-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wiggin TD, Kretzler M, Pennathur S, Sullivan KA, Brosius FC, Feldman EL. Rosiglitazone treatment reduces diabetic neuropathy in streptozotocin-treated DBA/2J mice. Endocrinology. 2008;149(10):4928–4937. doi: 10.1210/en.2008-0869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pande M, Hur J, Hong Y, et al. Transcriptional profiling of diabetic neuropathy in the BKS db/db mouse: a model of type 2 diabetes. Diabetes. 2011;60(7):1981–1989. doi: 10.2337/db10-1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oliveros JC (2007–2015) Venny. An interactive tool for comparing lists with Venn's diagrams. http://bioinfogp.cnb.csic.es/tools/venny/index.html
- 30.Giampetruzzi A, Danielson EW, Gumina V, et al. Modulation of actin polymerization affects nucleocytoplasmic transport in multiple forms of amyotrophic lateral sclerosis. Nat Commun. 2019;10:3827. doi: 10.1038/s41467-019-11837-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arakawa Y, Bito H, Furuyashiki T, et al. Control of axon elongation via an SDF-1alpha/Rho/mDia pathway in cultured cerebellar granule neurons. J Cell Biol. 2003;161(2):381–391. doi: 10.1083/jcb.200210149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ding Z, Bae YH, Roy P. Molecular insights on context-specific role of profilin-1 in cell migration. Cell Adh Migr. 2012;6(5):442–449. doi: 10.4161/cam.21832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramasamy R, Shekhtman A, Schmidt AM. The RAGE/DIAPH1 Signaling Axis & Implications for the Pathogenesis of Diabetic Complications. Int J Mol Sci. 2022;23(9):4579. doi: 10.3390/ijms23094579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maffei A, Lembo G, Carnevale D. PI3Kinases in Diabetes Mellitus and Its Related Complications. Int J Mol Sci. 2018;19(12):4098. doi: 10.3390/ijms19124098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Du F, Liu S. Electroacupuncture with high frequency at acupoint ST-36 induces regeneration of lost enteric neurons in diabetic rats via GDNF and PI3K/AKT signal pathway. Am J Physiol Regul Integr Comp Physiol. 2015;309(2):R109–R118. doi: 10.1152/ajpregu.00396.2014. [DOI] [PubMed] [Google Scholar]
- 36.Bathina S, Das UN. Dysregulation of PI3K-Akt-mTOR pathway in brain of streptozotocin-induced type 2 diabetes mellitus in Wistar rats. Lipids Health Dis. 2018;17(1):168. doi: 10.1186/s12944-018-0809-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen L, Gong HY, Xu L. PVT1 protects diabetic peripheral neuropathy via PI3K/AKT pathway. Eur Rev Med Pharmacol Sci. 2018;22(20):6905–6911. doi: 10.26355/eurrev_201810_16160. [DOI] [PubMed] [Google Scholar]
- 38.Zhu QQ, Lai MC, Chen TC et al (2021) LncRNA SNHG15 relieves hyperglycemia-induced endothelial dysfunction via increasing ubiquitination of thioredoxin-interacting protein. Life Sci 23:119255. 10.1016/j.lfs.2021 [DOI] [PubMed]
- 39.Liu J, Cai D, Wang Y, Zou Y, Zhao T (2021) SNHG15 knockdown inhibits diabetic nephropathy progression in pediatric patients by regulating the miR-141/ICAM-1 axis in vitro. Biosci Rep 41(2):BSR20204099. 10.1042/BSR20204099 [DOI] [PMC free article] [PubMed]
- 40.Zhao Y, Li X, Tang S. Retrospective analysis of the relationship between elevated plasma levels of TXNIP and carotid intima-media thickness in subjects with impaired glucose tolerance and early Type 2 diabetes mellitus. Diabetes Res Clin Pract. 2015;109(2):372–377. doi: 10.1016/j.diabres.2015.05.028. [DOI] [PubMed] [Google Scholar]
- 41.Dunn LL, Simpson PJ, Prosser HC, et al. A critical role for thioredoxin-interacting protein in diabetes-related impairment of angiogenesis. Diabetes. 2014;63(2):675–687. doi: 10.2337/db13-0417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Recalcati S, Menotti E, Kühn LC. Peroxisomal targeting of mammalian hydroxyacid oxidase 1 requires the C-terminal tripeptide SKI. J Cell Sci. 2001;114(Pt 9):1625–1629. doi: 10.1242/jcs.114.9.1625. [DOI] [PubMed] [Google Scholar]
- 43.Kalpachidou T, Spiecker L, Kress M, Quarta S. Rho GTPases in the Physiology and Pathophysiology of Peripheral Sensory Neurons. Cells. 2019;8(6):591. doi: 10.3390/cells8060591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gu Y, Qiu ZL, Liu DZ, Sun GL, Guan YC, Hei ZQ, Li X. Differential gene expression profiling of the sciatic nerve in type 1 and type 2 diabetic mice. Biomed Rep. 2018;9(4):291–304. doi: 10.3892/br.2018.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tsukuba T, Okamoto K, Yasuda Y, Morikawa W, Nakanishi H, Yamamoto K. New functional aspects of cathepsin D and cathepsin E. Mol Cells. 2000;10(6):601–611. doi: 10.1007/s10059-000-0601-8. [DOI] [PubMed] [Google Scholar]
- 46.Howard TL, Stauffer DR, Degnin CR, Hollenberg SM. CHMP1 functions as a member of a newly defined family of vesicle trafficking proteins. J Cell Sci. 2001;114(Pt 13):2395–2404. doi: 10.1242/jcs.114.13.2395. [DOI] [PubMed] [Google Scholar]
- 47.Xie Z, Meng J, Kong W et al (2022) Microglial cathepsin E plays a role in neuroinflammation and amyloid β production in Alzheimer's disease. Aging Cell 21(3):e13565. 10.1111/acel.13565 [DOI] [PMC free article] [PubMed]
- 48.Gonçalves NP, Moreira J, Martins D, et al. Differential expression of Cathepsin E in transthyretin amyloidosis: from neuropathology to the immune system. J Neuroinflammation. 2017;4:115. doi: 10.1186/s12974-017-0891-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guo L, Lv J, Huang YF, Hao DJ, Liu JJ. Bioinformatics analyses of differentially expressed genes associated with spinal cord injury: A microarray-based analysis in a mouse model. Neural Regen Res. 2019;14(7):1262–1270. doi: 10.4103/1673-5374.251335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Supek F, Bošnjak M, Škunca N, Šmuc T (2011) REVIGO summarizes and visualizes long lists of gene ontology terms. PLoS One 6(7):e21800. 10.1371/journal.pone.0021800 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Fig. 1. The diagram of raw data analysis – in silico analysis. The md5sum is designed to verify data integrity using Message Digest Algorithm 5 (MD5). Consequently, regions of row reads were trimmed with use of Trimmomatic v0.38 program. Next, mapping was performed using STAR tool. For mapping the Mus musculus GRCm39 was used as the reference genome with annotation version GRCm39.104 downloaded from Ensembl database (https://www.ensembl.org/index.html). Statistical analyses of differentially expressed genes (DEGs) for protein-coding RNA affected by long term hyperglycemia was performed using Ballgown, dedicated Bioconductor v3.14 (https://bioconductor.org/packages/release/bioc/html/ballgown.html) package prepared for the R environment v4.1.2, with the following operating parameters: P-value < 0.05 and |log2FC| ≥ 0.5 (TIF 2504 KB)
Supplementary Fig. 2. Summary of the results of RNA sequencing, preprocessing, and mapping of reads to the mice reference genome (Mus musculus GRCm39.104). (TIF 1032 KB)
Supplementary Fig. 3. Principle component analysis (PCA). The PCA revealed the high level of differentiation between control and STZ-treated samples. Principal component analysis (PCA) and Euclidean distances between samples analysis were performed using ggplot2 library v3.3.5 (https://www.rdocumentation.org/packages/ggplot2/versions/3.3.5) and self-developed R script, to assess the overall similarity between transcriptomic profiles of RNA samples derived from diabetic and non-diabetic mice. Wheel – control, triangle – diabetes/STZ-treated mice. (TIF 510 KB)
Supplementary Table 1. Altered transcripts in lumbar spinal cord (SC) neuromere under hyperglycemic condition. (DOCX 120 KB)
Supplementary Table 2. The table with GO-BP terms(DOCX 25 KB)
Supplementary Table 3. The table with GO-MF terms (DOCX 17 KB)
Supplementary Table 4. The table with GO-CC terms (DOCX 18 KB)
Supplementary Table 5. Functional enrichment analysis of DEGs in diabetic spinal cord (SC) of mice by KEGG database (DOCX 19 KB)
Supplementary Table 6. The table of interaction network in mouse diabetic spinal cord (SC) by GeneMANIA analysis (DOCX 20 KB)
Supplementary file 1: Western blot raw data (DOCX 3728 KB)
Supplementary file 2: Detailed methodology (DOCX 24 KB)
Data Availability Statement
The original results presented in the study are included in the article, further inquiries can be directed to the corresponding author. RNA-seq data have been deposited in the ArrayExpress database at EMBL-EBI (www.ebi.ac.uk/arrayexpress) under accession number E-MTAB 12252.