Key Points
Question
Are there associations between a history of adverse pregnancy outcomes and coronary atherosclerosis independent of cardiovascular risk in women aged 50 to 65 years?
Findings
In this population-based cross-sectional analysis of Swedish women undergoing screening coronary computed tomography (CT) angiography, there was a statistically significant association between history of adverse pregnancy outcomes and image-identified coronary artery disease, including preeclampsia (prevalence, 36.3% vs 28.3%) and gestational hypertension (prevalence, 40.9% vs 28.3%). This association was present in the subgroup of women estimated to be at low cardiovascular disease risk.
Meaning
A history of adverse pregnancy outcomes was significantly associated with coronary CT image–identified coronary artery disease.
Abstract
Importance
Adverse pregnancy outcomes are recognized risk enhancers for cardiovascular disease, but the prevalence of subclinical coronary atherosclerosis after these conditions is unknown.
Objective
To assess associations between history of adverse pregnancy outcomes and coronary artery disease assessed by coronary computed tomography angiography screening.
Design, Setting, and Participants
Cross-sectional study of a population-based cohort of women in Sweden (n = 10 528) with 1 or more deliveries in 1973 or later, ascertained via the Swedish National Medical Birth Register, who subsequently participated in the Swedish Cardiopulmonary Bioimage Study at age 50 to 65 (median, 57.3) years in 2013-2018. Delivery data were prospectively collected.
Exposures
Adverse pregnancy outcomes, including preeclampsia, gestational hypertension, preterm delivery, small-for-gestational-age infant, and gestational diabetes. The reference category included women with no history of these exposures.
Main Outcomes and Measures
Coronary computed tomography angiography indexes, including any coronary atherosclerosis, significant stenosis, noncalcified plaque, segment involvement score of 4 or greater, and coronary artery calcium score greater than 100.
Results
A median 29.6 (IQR, 25.0-34.9) years after first registered delivery, 18.9% of women had a history of adverse pregnancy outcomes, with specific pregnancy histories ranging from 1.4% (gestational diabetes) to 9.5% (preterm delivery). The prevalence of any coronary atherosclerosis in women with a history of any adverse pregnancy outcome was 32.1% (95% CI, 30.0%-34.2%), which was significantly higher (prevalence difference, 3.8% [95% CI, 1.6%-6.1%]; prevalence ratio, 1.14 [95% CI, 1.06-1.22]) compared with reference women. History of gestational hypertension and preeclampsia were both significantly associated with higher and similar prevalence of all outcome indexes. For preeclampsia, the highest prevalence difference was observed for any coronary atherosclerosis (prevalence difference, 8.0% [95% CI, 3.7%-12.3%]; prevalence ratio, 1.28 [95% CI, 1.14-1.45]), and the highest prevalence ratio was observed for significant stenosis (prevalence difference, 3.1% [95% CI, 1.1%-5.1%]; prevalence ratio, 2.46 [95% CI, 1.65-3.67]). In adjusted models, odds ratios for preeclampsia ranged from 1.31 (95% CI, 1.07-1.61) for any coronary atherosclerosis to 2.21 (95% CI, 1.42-3.44) for significant stenosis. Similar associations were observed for history of preeclampsia or gestational hypertension among women with low predicted cardiovascular risk.
Conclusions and Relevance
Among Swedish women undergoing coronary computed tomography angiography screening, there was a statistically significant association between history of adverse pregnancy outcomes and image-identified coronary artery disease, including among women estimated to be at low cardiovascular disease risk. Further research is needed to understand the clinical importance of these associations.
This study assesses the association of history of adverse pregnancy outcomes with subsequent image-identified coronary artery disease among a population-based cohort of women in Sweden.
Introduction
Coronary artery disease is the most common cardiovascular disease and the leading cause of death, and women and men share most of its modifiable risk factors.1,2 However, some risk factors, such as adverse pregnancy outcomes3 are unique to women. Women with previous preeclampsia,4,5,6,7 gestational hypertension, small for gestational age infant,8 preterm delivery,9 or gestational diabetes10,11 all have higher risk of coronary artery disease compared with women without these complications. While some adverse pregnancy outcomes are associated with cardiovascular disease independent of conventional risk factors, pregnancy history does not seem to improve cardiovascular risk prediction models substantially.12,13 Younger women are generally estimated to have low cardiovascular risk, and prevention efforts are often overlooked despite a previous adverse pregnancy outcome.3 Coronary computed tomography (CT) angiography allows for noninvasive visualization of the coronary arteries and can serve as an effective tool for screening for subclinical coronary artery disease.14 By elucidating the extent to which the development of coronary atherosclerosis differs by adverse pregnancy outcome history and predicted cardiovascular risk, the association between pregnancy history and coronary artery disease could be better understood. To accomplish this, the purpose of this study was to assess associations between subclinical coronary artery disease assessed by coronary CT angiography screening in women aged 50 to 65 years and history of adverse pregnancy outcomes.
Methods
In this cross-sectional study of a population-based cohort, women with 1 or more deliveries in 1973 or later, ascertained via the Swedish National Medical Birth Register, who subsequently at age 50 to 65 years had participated in the Swedish Cardiopulmonary Bioimage Study (SCAPIS) in 2013-2018, were included. Study participants were invited based on their legal sex (male or female) in the Swedish population register at the time of study recruitment. The study was approved by the Swedish Ethical Review Authority (2019-03229) following approval of data collection (2010-228-31M), and all participants provided written informed consent.
Study Population
In 2013-2018, 30 154 women and men (aged 50-65 years) were recruited at random from the Swedish census population, and during multiple visits underwent cardiovascular examinations and laboratory testing, including completing a questionnaire regarding their health, social circumstances, and lifestyle.15,16 Of the 15 508 women included, 12 825 underwent coronary CT angiography with assessable images of the proximal coronary segments (segments 1, 5, 6, and 11),15,16 and of these, 10 528 women had ascertainable registry data on pregnancy history (Figure 1). For the analysis on subclinical coronary atherosclerosis in women with low (<5%) 10-year cardiovascular risk, we further excluded 502 women with a history of myocardial infarction, coronary revascularization, or stroke and/or missing data for cardiovascular risk prediction variables.
Figure 1. Participant Flow in the Study of Adverse Pregnancy Outcomes and Coronary CT Findings.
CT indicates computed tomography. Participant numbers in the main study cohort based on adverse pregnancy outcomes (not mutually exclusive categories): any adverse pregnancy outcome, n = 1991; gestational diabetes, n = 144; gestational hypertension, n = 252; preeclampsia, n = 499; preterm delivery, n = 999; small-for-gestational-age infant, n = 526; no adverse pregnancy outcome, n = 8537. The SCORE2 algorithm predicts fatal and nonfatal cardiovascular disease and was developed using data on age, sex, smoking, diabetes, systolic blood pressure, and total and high-density lipoprotein cholesterol. For individuals aged 50 to 69 years, the 10-year cardiovascular risk is classified as follows: less than 5% = low risk; 5% to less than 10% = intermediate risk; 10% or higher = high risk. Among 179 participants with missing SCORE2 data, 164 were missing 1 variable and 15 were missing 2 variables.
History of Adverse Pregnancy Outcomes
All adverse pregnancy outcomes except gestational diabetes were identified through linkage with the Swedish National Medical Birth Register 1973-2018 (eAppendix in Supplement 1), containing data for more than 98% of all deliveries in Sweden.17 Preeclampsia and gestational hypertension were mainly defined by having received any qualifying International Classification of Diseases (eighth, ninth, or tenth revisions) diagnosis (eAppendix in Supplement 1) at any delivery. A small-for-gestational-age infant was defined as a singleton infant with birth weight more than 2 SDs below the mean according to gestational week and sex.18 Preterm delivery was defined as delivery at 36 weeks 6 days’ gestation or earlier. History of gestational diabetes was self-reported at the time of coronary CT angiography. Each adverse pregnancy outcome was independently defined irrespective of any other adverse pregnancy outcomes occurring during the same or other pregnancies.
Coronary Atherosclerosis Assessed by Coronary CT Angiography
The collection of coronary CT angiography and coronary artery calcium data have been previously reported.15,16 In summary, noncontrast coronary artery calcium images were obtained using electrocardiogram (ECG)-gated CT imaging at 120 kV. Coronary CT angiography was performed with a dual-source CT scanner equipped with a Stellar detector (Somatom Definition Flash, Siemens Medical Solutions), with iohexol, 325 mg iodine per kilogram, used as a contrast medium (350 mg iodine per milliliter; GE HealthCare). For coronary assessment, the 18-coronary-segment model was used, with segments 1 through 3, 5 through 7, 9, 11 through 13, and 17 compulsorily reported.16 Five complementary coronary atherosclerosis indexes were used as outcomes: (1) any coronary atherosclerosis; (2) any significant stenosis (≥50% lumen obstruction); (3) any noncalcified plaque; (4) segment involvement score of 4 or greater (indicating elevated risk of cardiovascular events)19; and (5) coronary artery calcium score of greater than 100 Agatston units (indicating highly calcified atherosclerosis).20
Covariables and 10-Year Cardiovascular Risk Algorithm
The data collected at the time of coronary CT angiography were used to describe the study sample, as covariables in regression modeling and for calculation of 10-year cardiovascular risk according to the SCORE2 algorithm (eAppendix in Supplement 1).15 Using data on age, sex, smoking, diabetes, systolic blood pressure, and total and high-density lipoprotein cholesterol, the SCORE2 algorithm was developed, calibrated, and validated to predict the 10-year risk of first-onset fatal and nonfatal cardiovascular disease in European populations aged 40 to 69 years without diabetes or previous cardiovascular disease.21
Statistical Analyses
Descriptive data are presented as numbers and percentages or medians and interquartile ranges as appropriate.
To study the segment-specific pattern of coronary atherosclerosis by adverse pregnancy outcome history, χ2 tests were applied to the “any coronary atherosclerosis” counts in 6 coronary artery segments with high known prevalence of coronary atherosclerosis (eAppendix in Supplement 1).16
All comparisons of prevalence were made with women without any adverse pregnancy outcome as the reference. To examine associations between each adverse pregnancy outcome and the coronary CT angiography outcomes, multivariable logistic regression modeling was performed (see the eAppendix in Supplement 1 for further rationale), and odds ratios (ORs) with 95% CIs were calculated. The confounder models included covariables collected at the time of coronary CT angiography that were not postpregnancy predictors or mediators, including age, smoking, reported body mass index at age 20 years, educational level, financial strain, family history of myocardial infarction, family history of stroke, and total number of deliveries. The clinical predictor models included established predictors of coronary atherosclerosis collected at the time of coronary CT angiography: age, smoking, diabetes, systolic blood pressure, hypertension medication, lipid-lowering medication, body mass index, high-density lipoprotein cholesterol, and total cholesterol.
To enhance interpretation, the associations between adverse pregnancy outcome history and coronary CT angiography outcomes were calculated as difference in vascular age, ie, the hypothetical mean age increase that the magnitude of each association corresponds to (eAppendix in Supplement 1).
To investigate subclinical coronary atherosclerosis in women with low cardiovascular risk, women with previous cardiovascular disease were excluded. The 10-year cardiovascular risk was calculated using the SCORE2 algorithm.21 In women with low (<5%) predicted risk, the prevalence of coronary atherosclerosis indexes by pregnancy history was analyzed, as were prevalence differences and prevalence ratios compared with women without previous adverse pregnancy outcomes. Methods of complementary analyses are described in the eAppendix in Supplement 1.
Multiple imputations of covariables with chained equations were used as needed for the regression models (eAppendix in Supplement 1). A 2-sided P < .05 was set for statistical significance. Because of the potential for type I error due to multiple comparisons, findings should be interpreted as exploratory. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc).
Results
Study Cohort Characteristics
The main study cohort, described in Table 1, comprised 10 528 women with at least 1 delivery registered in the Swedish National Medical Birth Register and subsequent assessable coronary CT angiography. Of all women (median age, 57.3 years), 1991 (18.9%) had a history of any adverse pregnancy outcome. The prevalence of each of these was as follows: preeclampsia, 4.7%; gestational hypertension, 2.4%; preterm delivery, 9.5%; small-for-gestational-age infant, 5.0%; and gestational diabetes, 1.4%. Compared with women with no adverse pregnancy outcome history, women with previous preeclampsia or gestational hypertension had numerically higher systolic blood pressure and women with previous gestational diabetes had higher prevalence of diabetes. The median time between first registered delivery and angiography was 29.6 years (range, 0.7-45.5 [IQR, 25.0-34.9] years).
Table 1. Baseline Participant Characteristics (N = 10 528).
| Characteristics | Any adverse pregnancy outcome (n = 1991) | Gestational diabetes (n = 144)a | Gestational hypertension (n = 252) | Preeclampsia (n = 499) | Preterm delivery (n = 999) | Small-for-gestational-age infant (n = 526)b | No adverse pregnancy outcome (n = 8537) |
|---|---|---|---|---|---|---|---|
| Age, median (IQR), y | 57.40 (53.70-60.90) | 56.00 (53.05-59.30) | 58.60 (55.65-61.35) | 56.80 (53.10-60.70) | 57.10 (53.40-60.80) | 58.00 (54.00-61.20) | 57.20 (53.60-61.10) |
| More than 9 y of school, No. (%)c | 1764 (88.6) | 136 (94.4) | 229 (90.9) | 430 (86.2) | 894 (89.5) | 448 (85.2) | 7743 (90.7) |
| Financial strain, No./total (%)d | 164/1895 (8.7) | 19/139 (13.7) | 19/244 (7.8) | 35/473 (7.4) | 82/943 (8.7) | 52/496 (10.5) | 554/8271 (6.7) |
| Smoking status, No./total (%) | |||||||
| Never | 905/1912 (47.3) | 62/139 (44.6) | 128/240 (53.3) | 252/473 (53.3) | 478/962 (49.7) | 215/497 (43.3) | 4012/8309 (48.3) |
| Previous | 743/1912 (38.9) | 59/139 (42.4) | 87/240 (36.3) | 179/473 (37.8) | 355/962 (36.9) | 189/497 (38.0) | 3286/8309 (39.5) |
| Current | 264/1912 (13.8) | 18/139 (12.9) | 25/240 (10.4) | 42/473 (8.9) | 129/962 (13.4) | 93/497 (18.7) | 1011/8309 (12.2) |
| No. of deliveries, median (IQR)e | 2 (2-3) | 2 (2-3) | 2 (2-3) | 2 (2-3) | 2 (2-3) | 2 (2-3) | 2 (2-3) |
| Diabetes, No. (%) | 147/1988 (7.4) | 45 (31.3) | 18 (7.1) | 26/497 (5.2) | 64/997 (6.4) | 26 (4.9) | 323/8530 (3.8) |
| Previous stroke, No. (%) | 64 (3.2) | 2 (1.4) | 3 (1.2) | 22 (4.4) | 30 (3.0) | 28 (5.3) | 201 (2.4) |
| Previous myocardial infarction, No. (%) | 58 (2.9) | 2 (1.4) | 4 (1.6) | 21 (4.2) | 25 (2.5) | 24 (4.6) | 149 (1.8) |
| Previous coronary revascularization, No. (%) | 54 (2.7) | 1 (0.7) | 4 (1.6) | 20 (4.0) | 24 (2.4) | 23 (4.4) | 122 (1.4) |
| Medically treated hypertension, No./total (%) | 511/1926 (26.5) | 38/143 (26.6) | 114/250 (45.6) | 181/479 (37.8) | 203/966 (21.0) | 125/497 (25.2) | 1278/8335 (15.3) |
| Medically treated hyperlipidemia, No./total (%) | 146/1926 (7.6) | 21/143 (14.7) | 18/250 (7.2) | 36/479 (7.5) | 72/966 (7.5) | 32/497 (6.4) | 396/8335 (4.8) |
| Family history of myocardial infarction, No./total (%) | 143/1941 (7.4) | 12/143 (8.4) | 23/248 (9.3) | 31/482 (6.4) | 65/975 (6.7) | 31/506 (6.1) | 605/8406 (7.2) |
| Family history of stroke, No./total (%) | 126/1941 (6.5) | 11/143 (7.7) | 21/248 (8.5) | 35/482 (7.3) | 57/975 (5.8) | 27/506 (5.3) | 551/8406 (6.6) |
| Body mass index at age 20 y, median (IQR)f | 20.81 (19.38-22.58) [n = 1865] | 21.50 (20.05-23.09) [n = 136] | 21.36 (19.84-23.31) [n = 235] | 21.22 (19.71-22.86) [n = 470] | 20.57 (19.15-22.38) [n = 934] | 20.70 (19.23-22.06) [n = 487] | 20.75 (19.38-22.31) [n = 8110] |
| Body mass index at CCTA, median (IQR)f | 25.80 (23.10-29.30) | 27.50 (24.75-30.45) | 27.10 (24.25-30.25) | 26.50 (23.90-30.00) | 25.30 (22.70-28.70) | 25.20 (22.70-28.50) | 25.40 (23.00-28.60) |
| Systolic blood pressure, median (IQR), mm Hg | 124 (113-136) | 123 (113-135) | 132 (118-143) | 126 (116-140) | 122 (111-134) | 124 (114-135) | 120 (110-133) [n = 8535] |
| Total cholesterol, median (IQR), mg/dL | 216.2 (189.2-239.4) [n = 1987] | 202.7 (185.3-231.7) | 216.2 (196.9-239.4) [n = 251] | 216.2 (193.1-239.4) | 216.2 (189.2-239.4) [n = 997] | 216.2 (189.2-243.2) [n = 523] | 216.2 (189.2-243.2) [n = 8524] |
| High-density lipoprotein cholesterol, median (IQR), mg/dL | 69.5 (57.9-81.1) [n = 1984] | 61.8 (50.2-73.4) | 65.6 (54.1-77.2) [n = 251] | 65.6 (57.9-81.1) [n = 498] | 69.5 (57.9-81.1) [n = 995] | 69.5 (57.9-84.9) [n = 522] | 69.5 (57.9-84.9) [n = 8524] |
Abbreviation: CCTA, coronary computed tomography angiography.
SI conversions: To convert total and high-density lipoprotein cholesterol to millimoles per liter, multiply values by 0.0259.
Self-reported.
Birth weight more than 2 SDs below the mean for gestational age and sex.
Nine years of school is compulsory in Sweden.
Not able to pay an unforeseen cost of 20 000 Swedish kronor (approximately US $2000).
Number of deliveries per participant registered in the Swedish National Medical Birth Register.
Calculated as weight in kilograms divided by height in meters squared.
Prevalence, Characteristics, and Odds of Coronary Atherosclerosis by Pregnancy History
The prevalence, prevalence ratios, and crude and multivariable adjusted ORs of all indexes are presented in Figure 2, Figure 3, and Figure 4. Among women with a history of any adverse pregnancy outcome, 32.1% (95% CI, 30.0%-34.2%) had any coronary atherosclerosis, which was significantly higher (prevalence difference, 3.8% [95% CI, 1.6%-6.1%]; prevalence ratio, 1.14 [95% CI, 1.06-1.22]) compared with women without any history of adverse pregnancy outcomes. History of gestational hypertension and preeclampsia were both significantly associated with higher and similar prevalence of all outcome indexes. For preeclampsia, the highest prevalence difference was observed for any coronary atherosclerosis (prevalence difference, 8.0% [95% CI, 3.7%-12.3%]; prevalence ratio, 1.28 [95% CI, 1.14-1.45]) and the highest prevalence ratio was observed for significant stenosis (prevalence difference, 3.1% [95% CI, 1.1%-5.1%]; prevalence ratio, 2.46 [95% CI, 1.65-3.67]). For preeclampsia, the predictor-adjusted ORs ranged from 1.31 (95% CI, 1.07-1.61) for coronary atherosclerosis to 2.21 (95% CI, 1.42-3.44) for significant stenosis, with similar findings for gestational hypertension (ORs, 1.33 [95% CI, 1.01-1.74] and 1.83 [95% CI, 1.00-3.33], respectively). Women with a previous preterm delivery, small-for-gestational-age infant, or gestational diabetes also had significantly higher prevalences of most indexes, but numerically lower prevalences compared with those with previous preeclampsia or gestational hypertension. In models including clinical predictors, having a small-for-gestational-age infant was significantly associated with a segment involvement score of 4 or greater (OR, 1.51; 95% CI, 1.06-2.14) and significant stenosis (OR, 1.80; 95% CI, 1.13-2.87). Preterm delivery and gestational diabetes were not significantly associated with any of the outcome indexes in the model including clinical predictors, although the 95% CIs for gestational diabetes were wide.
Figure 2. Coronary Artery Disease Assessed by Coronary Computed Tomography Angiography According to Any Adverse Pregnancy Outcome History and Gestational Diabetes.

The crude model included the adverse pregnancy outcome; the confounder model included the adverse pregnancy outcome, age, smoking, body mass index (BMI) at age 20 years, educational level, financial strain, family history of myocardial infarction and stroke, and total number of deliveries; the predictor model included the adverse pregnancy outcome, age, smoking, diabetes, systolic blood pressure, hypertension and lipid-lowering medications, BMI, and high-density lipoprotein and total cholesterol. In panel B, women without gestational diabetes but with any of gestational hypertension, preeclampsia, preterm delivery, or having a small-for-gestational-age infant contributed to the multivariable models, but their estimates are not shown.
aTotal numbers are different for coronary artery calcium score because of missing outcome data.
Figure 3. Coronary Artery Disease Assessed by Coronary Computed Tomography Angiography According to Gestational Hypertension and Preeclampsia.
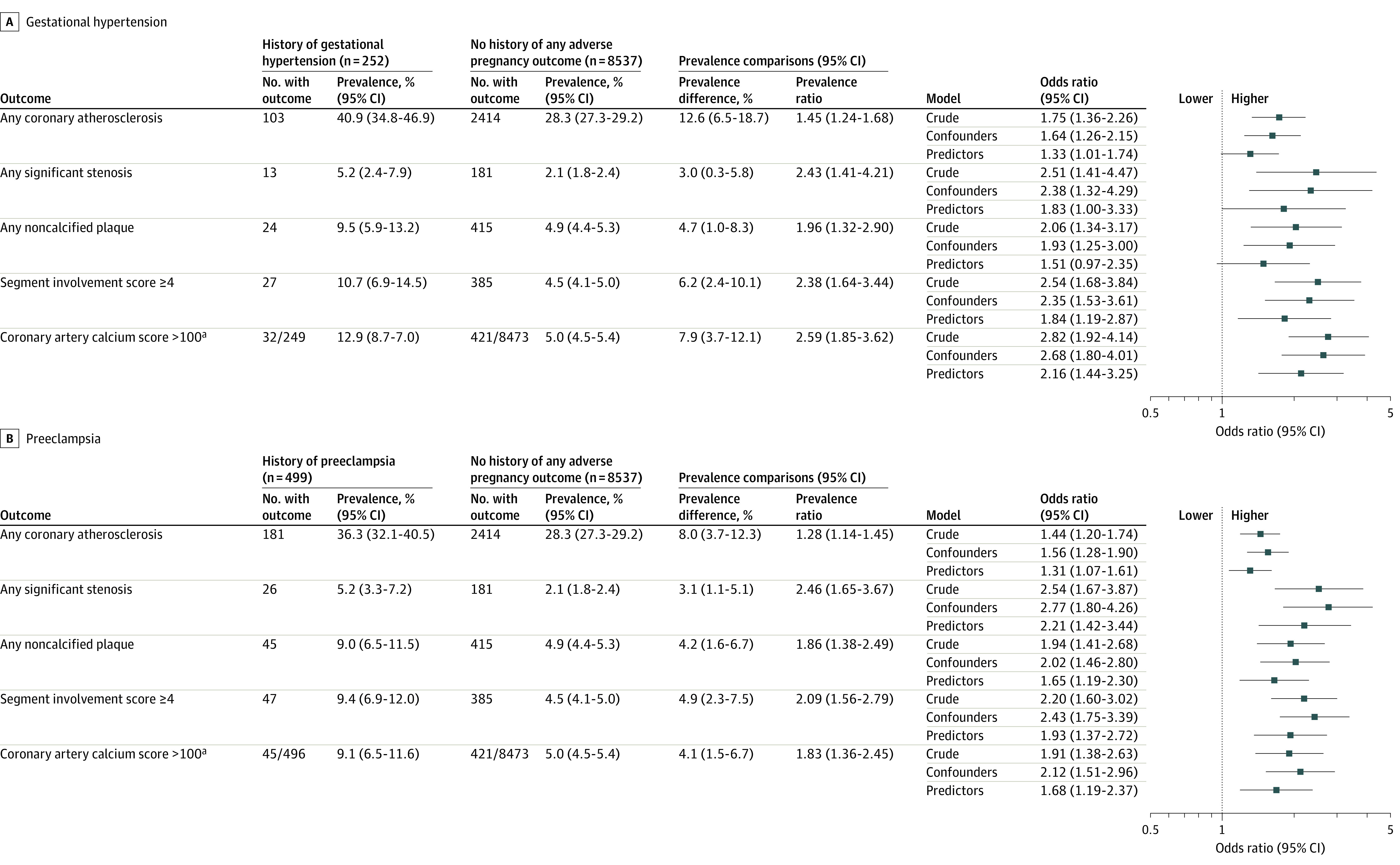
See Figure 2 legend for description of crude, confounder, and predictor models. In panel A, women without gestational hypertension but with any of gestational diabetes, preeclampsia, preterm delivery, or having a small-for-gestational-age infant contributed to the multivariable models, but their estimates are not shown; in panel B, women without preeclampsia but with any of gestational diabetes, gestational hypertension, preterm delivery, or having a small-for-gestational-age infant contributed to the multivariable models, but their estimates are not shown.
aTotal numbers are different for coronary artery calcium score because of missing outcome data.
Figure 4. Coronary Artery Disease Assessed by Coronary Computed Tomography Angiography According to Preterm Delivery and Having a Small-for-Gestational-Age Infant.

See Figure 2 legend for descriptions of crude, confounder, and predictor models. In panel A, women without preterm delivery but with any of gestational diabetes, gestational hypertension, preeclampsia, or having a small-for-gestational-age infant contributed to the multivariable models, but their estimates are not shown; in panel B, women without a small-for-gestational-age infant but with any of gestational diabetes, gestational hypertension, preeclampsia, or preterm delivery contributed to the multivariable models, but their estimates are not shown.
aTotal numbers are different for coronary artery calcium score because of missing outcome data.
When estimating vascular age by adverse pregnancy outcome, women with a history of preeclampsia or gestational hypertension were 4 years older than those without any history according to the “any coronary atherosclerosis” outcome and 6 to 11 years older according to the more severe indexes (eTable 1 in Supplement 1). The corresponding findings for small-for-gestational-age infant, preterm delivery, and gestational diabetes history were more scattered and attenuated.
The distribution of segment-specific coronary atherosclerosis in women with any adverse pregnancy outcome, preeclampsia, gestational hypertension, or small-for-gestational-age infant differed significantly from that of women with no adverse pregnancy outcome (eTable 2 in Supplement 1). No significant difference in distribution was observed for preterm delivery or gestational diabetes. The proximal left anterior descending coronary artery was most frequently affected by atherosclerosis, regardless of adverse pregnancy outcome history, and all adverse pregnancy outcomes were typically associated with higher prevalence of coronary atherosclerosis in all studied segments.
Coronary Atherosclerosis by Adverse Pregnancy Outcome History in Women With Low Predicted Cardiovascular Risk
In total, 8334 (83.1% of eligible) women were classified as having a low 10-year cardiovascular risk. Among these women, a history of any adverse pregnancy outcome was associated with significantly higher prevalence of all outcomes compared with women with no history of adverse pregnancy outcomes (Table 2). Among the specific adverse pregnancy outcomes, preeclampsia and gestational hypertension were statistically associated with higher prevalence of all coronary indexes, except for the association between gestational hypertension and significant stenosis. The highest prevalence ratio was observed for the association between preeclampsia and significant stenosis (3.15; 95% CI, 1.90-5.21) and the highest prevalence difference between gestational hypertension and any coronary atherosclerosis (10.4%; 95% CI, 3.3%-17.5%). There were no significantly increased prevalence ratios observed for the other adverse pregnancy outcomes. The prevalence of significant stenosis (4.5%) in women with a history of preeclampsia and low predicted cardiovascular risk was numerically on par with that observed in women with no adverse pregnancy outcome history and intermediate (5% to <10%) cardiovascular risk (4.8%; eTable 3 in Supplement 1).
Table 2. Subclinical Coronary Artery Disease in Women With Low Cardiovascular Risk by Adverse Pregnancy Outcome History (N = 8334).
| Any adverse pregnancy outcome (n = 1498) | Gestational diabetes (n = 100) | Gestational hypertension (n = 177) | Preeclampsia (n = 377) | Preterm delivery (n = 772) | Small-for-gestational-age infant (n = 384) | No adverse pregnancy outcome (n = 6836) | |
|---|---|---|---|---|---|---|---|
| Any atherosclerosis | |||||||
| No. with outcome | 409 | 26 | 61 | 119 | 193 | 106 | 1646 |
| Prevalence of outcome, % (95% CI) | 27.3 (25.1 to 29:6) | 26.0 (17.4 to 34.6) | 34.5 (27.5 to 41.5) | 31.6 (26.9 to 36.3) | 25.0 (22.0 to 28.1) | 27.6 (23.1 to 32.1) | 24.1 (23.1 to 25.1) |
| Prevalence difference, % (95% CI)a | 3.2 (0.8 to 5.7) | 1.9 (−6.7 to 10.6) | 10.4 (3.3 to 17.5) | 7.5 (2.7 to 12.3) | 0.9 (−2.3 to 4.1) | 3.5 (−1.1 to 8.1) | [Reference] |
| Prevalence ratio (95% CI)a | 1.14 (1.03 to 1.24) | 1.08 (0.77 to 1.51) | 1.43 (1.16 to 1.76) | 1.31 (1.12 to 1.53) | 1.04 (0.91 to 1.18) | 1.15 (0.97 to 1.36) | 1 [Reference] |
| Any significant stenosis | |||||||
| No. with outcome | 32 | 3 | 4 | 17 | 9 | 10 | 98 |
| Prevalence of outcome, % (95% CI) | 2.1 (1.4 to 2.9) | 3.0 (0 to 6.3) | 2.3 (0.1 to 4.5) | 4.5 (2.4 to 6.6) | 1.2 (0.4 to 1.9) | 2.6 (1.0 to 4.2) | 1.4 (1.2 to 1.7) |
| Prevalence difference, % (95% CI)a | 0.7 (−0.1 to 1.5) | 1.6 (−1.8 to 4.9) | 0.8 (−1.4 to 3.0) | 3.1 (1.0 to 5.2) | −0.3 (−1.1 to 0.5) | 1.2 (−0.5 to 2.8) | [Reference] |
| Prevalence ratio (95% CI)a | 1.49 (1.00 to 2.21) | 2.09 (0.67 to 6.49) | 1.58 (0.59 to 4.24) | 3.15 (1.90 to 5.21) | 0.81 (0.41 to 1.60) | 1.82 (0.96 to 3.45) | 1 [Reference] |
| Any noncalcified plaque | |||||||
| No. with outcome | 85 | 6 | 14 | 30 | 37 | 16 | 268 |
| Prevalence of outcome, % (95% CI) | 5.7 (4.5 to 6.9) | 6.0 (1.4 to 10.7) | 7.9 (3.9 to 11.9) | 8.0 (5.2 to 10.7) | 4.8 (3.3 to 6.3) | 4.2 (2.2 to 6.2) | 3.9 (3.5 to 4.4) |
| Prevalence difference, % (95% CI)a | 1.8 (0.5 to 3.0) | 2.1 (−2.6 to 6.8) | 4.0 (−0.01 to 8.0) | 4.0 (1.3 to 6.8) | 0.9 (−0.7 to 2.5) | 0.3 (−1.8 to 2.3) | [Reference] |
| Prevalence ratio (95% CI)a | 1.45 (1.14 to 1.84) | 1.53 (0.70 to 3.35) | 2.02 (1.20 to 3.38) | 2.03 (1.41 to 2.92) | 1.22 (0.87 to 1.71) | 1.06 (0.65 to 1.74) | 1 [Reference] |
| Segment involvement score ≥4 | |||||||
| No. with outcome | 64 | 4 | 14 | 25 | 24 | 17 | 205 |
| Prevalence of outcome, % (95% CI) | 4.3 (3.3 to 5.3) | 4.0 (0.2 to 7.8) | 7.9 (3.9 to 11.9) | 6.6 (4.1 to 9.1) | 3.1 (1.9 to 4.3) | 4.4 (2.4 to 6.5) | 3.0 (2.6 to 3.4) |
| Prevalence difference, % (95% CI)a | 1.3 (0.2 to 2.4) | 1.0 (−2.9 to 4.9) | 4.9 (0.9 to 8.9) | 3.6 (1.1 to 6.2) | 0.1 (−1.2 to 1.4) | 1.4 (−0.7 to 3.5) | [Reference] |
| Prevalence ratio (95% CI)a | 1.42 (1.08 to 1.88) | 1.33 (0.51 to 3.52) | 2.64 (1.57 to 4.44) | 2.21 (1.48 to 3.31) | 1.04 (0.68 to 1.57) | 1.48 (0.91 to 2.40) | 1 [Reference] |
| Coronary artery calcium score >100 | |||||||
| No./total with outcomeb | 74/1484 | 4/98 | 17/176 | 24/375 | 32/765 | 19/381 | 240/6797 |
| Prevalence of outcome, % (95% CI) | 5.0 (3.9 to 6.1) | 4.1 (0.2 to 8.0) | 9.7 (5.3 to 14.0) | 6.4 (3.9 to 8.9) | 4.2 (2.8 to 5.6) | 5.0 (2.8 to 7.2) | 3.5 (3.1 to 4.0) |
| Prevalence difference, % (95% CI)a | 1.5 (0.3 to 2.7) | 0.6 (−3.4 to 4.5) | 6.1 (1.7 to 10.5) | 2.9 (0.4 to 5.4) | 0.7 (−0.8 to 2.1) | 1.5 (−0.8 to 3.7) | [Reference] |
| Prevalence ratio (95% CI)a | 1.41 (1.09 to 1.82) | 1.16 (0.44 to 3.04) | 2.74 (1.71 to 4.37) | 1.81 (1.21 to 2.72) | 1.18 (0.83 to 1.70) | 1.41 (0.90 to 2.23) | 1 [Reference] |
Prevalence differences and prevalence ratios are comparisons with individuals with no adverse pregnancy outcome.
In total, 53 women had missing data on coronary artery calcium score and are excluded from this analysis.
Complementary Analyses
Adding the covariables included in the confounder model to the predictor model did not substantially affect model estimates reported in the main analyses (eTable 4 in Supplement 1). Instead defining history of preeclampsia through self-report (n = 652 [6.2%]) attenuated model estimates but did not change the overall pattern (eTable 5 in Supplement 1). In women with at least 2 registered deliveries, having any adverse pregnancy outcome in more than 1 pregnancy (vs having any adverse pregnancy outcome only once) was significantly associated with a segment involvement score of 4 or greater (OR, 1.63; 95% CI, 1.06-2.51) and a coronary artery calcium score of greater than 100 (OR, 1.67; 95% CI, 1.11-2.52) in predictor-adjusted models (eTable 6 in Supplement 1). Limiting the sample to postmenopausal women slightly attenuated estimates overall (eTable 7 in Supplement 1). Extended coronary artery calcium score descriptive data by adverse pregnancy outcome history are shown in eTable 8 in Supplement 1. All adverse pregnancy outcomes were associated with numerically higher median coronary artery calcium scores.
Discussion
Among Swedish women aged 50 to 65 years undergoing coronary CT angiography screening, there was a statistically significant association between history of adverse pregnancy outcomes and image-identified coronary artery disease, including among women estimated to be at low risk of cardiovascular disease. These associations were primarily found for hypertensive disorders of pregnancy—ie, preeclampsia or gestational hypertension—which were associated with all 5 coronary artery disease indexes. A history of preeclampsia or gestational hypertension was associated with a different distribution of segment-specific coronary atherosclerosis and more than 2 times higher risk of subclinical obstructive and widespread coronary artery disease, which is comparable with studies of incident clinical events.5,22,23,24
Recent observations from the Nurses’ Health Study II suggest that a larger proportion of the associated cardiovascular risk is mediated by postpregnancy risk factors in gestational hypertension compared with preeclampsia.25 As highlighted by another recent study, women with a history of hypertensive disorders of pregnancy are at increased risk of cardiac remodeling 10 years postpartum due to their higher risk of hypertension.26 As endothelial dysfunction is impaired in women with a history of preeclampsia27 or a small-for-gestational-age infant,28 it might constitute an etiological pathway to understanding atherosclerosis development in women with previous preeclampsia, gestational hypertension, or a small-for-gestational-age infant. It is notable that it is for these 3 complications, which have etiological and clinical overlaps during pregnancy,29 that the most consistent findings with coronary atherosclerosis in middle age were found.
In contrast, preterm delivery is a much more heterogeneous entity; it can for instance be caused by iatrogenic delivery due to preeclampsia, infection, or premature contractions. While women with a history of preterm delivery, compared with those without, had a higher coronary artery calcium score, no higher prevalence of abnormal coronary CT angiography findings was found. As in the CARDIA study, women with previous gestational diabetes had a higher coronary artery calcium score than those without.10 The results of the current study support that the risk of coronary atherosclerosis in these women is mainly mediated by conventional risk factors, especially diabetes,30 as the higher odds of a high calcium score and high atherosclerotic burden were abrogated following multivariable adjustment.
While this study supports previous reports that women with, compared with those without, a history of preeclampsia have higher coronary artery calcium score,4,31,32,33 studies on subclinical coronary artery disease by adverse pregnancy outcome history are scarce. Still, 2 previous European studies have provided important information on the prevalence of coronary atherosclerosis in women with a history of preeclampsia. In the CREW-IMAGO study, 34.5% of women aged 40 to 63 years with a history of preeclampsia had any coronary atherosclerosis and 2.9% had significant stenosis.32 In the recent Danish CPH-PRECIOUS study, coronary atherosclerosis was detected in 27.4% of women aged 40 to 55 years with previous preeclampsia, compared with 20% in age- and parity-matched controls.34 These prevalence numbers are in line with those reported herein, given the older mean age of women in the study.
The results of the complementary analyses on a dose-response association of adverse pregnancy outcomes on coronary artery disease indexes warrant detailed investigation in future studies. The attenuated model estimates observed in postmenopausal women are in line with previous findings, suggesting that the relative association between adverse pregnancy outcomes and incident cardiovascular disease decreases over decades.35
Strengths
A major strength of the present study is the utilization of a cohort with data on pregnancy history for all women ascertained via a population-based medical birth registry covering 5 decades. Thus, the study was not limited to comparing women with history of an adverse pregnancy outcome with a general sample of parous women with unknown pregnancy outcome status or relying on self-reported data collected many years after delivery, which is associated with recall bias. Another advantage is the investigation of 5 relevant adverse pregnancy outcomes for coronary atherosclerosis, and not only preeclampsia. Furthermore, all women included in the cohort also underwent standardized coronary CT angiography at a time point that was independent of adverse pregnancy outcome status. Altogether, this allows for better estimations of the prevalence of coronary atherosclerosis in women with a history of each respective adverse pregnancy outcome compared with those without, ultimately providing considerably more informative evidence for clinical decisions in the preventive context.
Limitations
This study has several limitations. First, as is the case with many statistical comparisons, there is a potential for type I error. The results are to some degree exploratory and should be interpreted based on their overall pattern, rather than by any specific finding, as false-positive associations may have been found. Second, as women had to survive until they were aged 50 to 65 years to be included in the study, the focus was on women who are potential targets for prevention efforts at this age and the results should not be interpreted as an effort to estimate causal effects. Third, information on smoking, as well as gestational diabetes at the time of pregnancy, was not available for all women, and was captured at the time of coronary CT angiography. The prevalence of previous gestational diabetes was low in this cohort, but this was expected given the low past prevalence of gestational diabetes in Sweden in areas both with and without universal screening.36 Fourth, although the Swedish National Medical Birth Register has been shown to be complete and accurate, misclassification may have occurred. Still, an underestimation of associations is most likely if misclassification occurred at random and was not related to outcomes. Fifth, because of the population-based design, low-dose radiation was used for coronary CT angiography, and thus high-quality images could not be obtained from all participants. However, a low-dose protocol is more feasible for clinical use in the prevention setting.
Conclusions
Among Swedish women undergoing screening coronary CT angiography, there was a statistically significant association between history of adverse pregnancy outcomes and image-identified coronary artery disease, including among women estimated to be at low cardiovascular disease risk. Further research is needed to understand the clinical importance of these associations.
eAppendix. Supplemental Methods
eReferences
eTable 1. Coronary Artery Disease Prevalence Differences as Vascular Age in Years by Adverse Pregnancy Outcome History
eTable 2. Overall Distribution and Prevalence of Segment-Specific Coronary Atherosclerosis by Adverse Pregnancy Outcome History
eTable 3. Subclinical Coronary Artery Disease in Women With Intermediate 10-Year Cardiovascular Disease Risk by Adverse Pregnancy Outcome History
eTable 4. Associations Between Adverse Pregnancy Outcome and Coronary Artery Disease Indices in Combined Model
eTable 5. Associations Between Preeclampsia History Ascertained by Self-Report and Coronary Artery Disease Indices
eTable 6. Dose Response Association Between Adverse Pregnancy Outcome and Coronary Artery Disease
eTable 7. Association Between Adverse Pregnancy Outcomes and Coronary Artery Disease Indices in Postmenopausal Women
eTable 8. Extended Coronary Artery Calcium Score Data by Adverse Pregnancy Outcome History
Data Sharing Statement
References
- 1.Virani SS, Alonso A, Benjamin EJ, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139-e596. doi: 10.1161/CIR.0000000000000757 [DOI] [PubMed] [Google Scholar]
- 2.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation. 2022;145(8):e153-e639. doi: 10.1161/CIR.0000000000001052 [DOI] [PubMed] [Google Scholar]
- 3.Parikh NI, Gonzalez JM, Anderson CAM, et al. ; American Heart Association Council on Epidemiology and Prevention, Council on Arteriosclerosis, Thrombosis and Vascular Biology, and Council on Cardiovascular and Stroke Nursing; Stroke Council . Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women: a scientific statement from the American Heart Association. Circulation. 2021;143(18):e902-e916. doi: 10.1161/CIR.0000000000000961 [DOI] [PubMed] [Google Scholar]
- 4.White WM, Mielke MM, Araoz PA, et al. A history of preeclampsia is associated with a risk for coronary artery calcification 3 decades later. Am J Obstet Gynecol. 2016;214(4):519.e1-519.e8. doi: 10.1016/j.ajog.2016.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Honigberg MC, Zekavat SM, Aragam K, et al. Long-term cardiovascular risk in women with hypertension during pregnancy. J Am Coll Cardiol. 2019;74(22):2743-2754. doi: 10.1016/j.jacc.2019.09.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu P, Haththotuwa R, Kwok CS, et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2017;10(2):e003497. doi: 10.1161/CIRCOUTCOMES.116.003497 [DOI] [PubMed] [Google Scholar]
- 7.Grandi SM, Filion KB, Yoon S, et al. Cardiovascular disease-related morbidity and mortality in women with a history of pregnancy complications. Circulation. 2019;139(8):1069-1079. doi: 10.1161/CIRCULATIONAHA.118.036748 [DOI] [PubMed] [Google Scholar]
- 8.Bonamy AK, Parikh NI, Cnattingius S, Ludvigsson JF, Ingelsson E. Birth characteristics and subsequent risks of maternal cardiovascular disease: effects of gestational age and fetal growth. Circulation. 2011;124(25):2839-2846. doi: 10.1161/CIRCULATIONAHA.111.034884 [DOI] [PubMed] [Google Scholar]
- 9.Wu P, Gulati M, Kwok CS, et al. Preterm delivery and future risk of maternal cardiovascular disease: a systematic review and meta-analysis. J Am Heart Assoc. 2018;7(2):e007809. doi: 10.1161/JAHA.117.007809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gunderson EP, Sun B, Catov JM, et al. Gestational diabetes history and glucose tolerance after pregnancy associated with coronary artery calcium in women during midlife: the CARDIA study. Circulation. 2021;143(10):974-987. doi: 10.1161/CIRCULATIONAHA.120.047320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kramer CK, Campbell S, Retnakaran R. Gestational diabetes and the risk of cardiovascular disease in women: a systematic review and meta-analysis. Diabetologia. 2019;62(6):905-914. doi: 10.1007/s00125-019-4840-2 [DOI] [PubMed] [Google Scholar]
- 12.Timpka S, Fraser A, Schyman T, et al. The value of pregnancy complication history for 10-year cardiovascular disease risk prediction in middle-aged women. Eur J Epidemiol. 2018;33(10):1003-1010. doi: 10.1007/s10654-018-0429-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Markovitz AR, Stuart JJ, Horn J, et al. Does pregnancy complication history improve cardiovascular disease risk prediction? findings from the HUNT study in Norway. Eur Heart J. 2019;40(14):1113-1120. doi: 10.1093/eurheartj/ehy863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mortensen MB, Blaha MJ. Is there a role of coronary CTA in primary prevention? current state and future directions. Curr Atheroscler Rep. 2021;23(8):44. doi: 10.1007/s11883-021-00943-2 [DOI] [PubMed] [Google Scholar]
- 15.Bergström G, Berglund G, Blomberg A, et al. The Swedish Cardiopulmonary Bioimage Study: objectives and design. J Intern Med. 2015;278(6):645-659. doi: 10.1111/joim.12384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bergström G, Persson M, Adiels M, et al. Prevalence of subclinical coronary artery atherosclerosis in the general population. Circulation. 2021;144(12):916-929. doi: 10.1161/CIRCULATIONAHA.121.055340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cnattingius S, Ericson A, Gunnarskog J, Källén B. A quality study of a medical birth registry. Scand J Soc Med. 1990;18(2):143-148. doi: 10.1177/140349489001800209 [DOI] [PubMed] [Google Scholar]
- 18.Marsál K, Persson PH, Larsen T, Lilja H, Selbing A, Sultan B. Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr. 1996;85(7):843-848. doi: 10.1111/j.1651-2227.1996.tb14164.x [DOI] [PubMed] [Google Scholar]
- 19.Bittencourt MS, Hulten E, Ghoshhajra B, et al. Prognostic value of nonobstructive and obstructive coronary artery disease detected by coronary computed tomography angiography to identify cardiovascular events. Circ Cardiovasc Imaging. 2014;7(2):282-291. doi: 10.1161/CIRCIMAGING.113.001047 [DOI] [PubMed] [Google Scholar]
- 20.Budoff MJ, Young R, Burke G, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: the Multi-ethnic Study of Atherosclerosis (MESA). Eur Heart J. 2018;39(25):2401-2408. doi: 10.1093/eurheartj/ehy217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.SCORE2 Working Group and ESC Cardiovascular Risk Collaboration . SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42(25):2439-2454. doi: 10.1093/eurheartj/ehab309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Canoy D, Cairns BJ, Balkwill A, et al. ; Million Women Study Collaborators . Hypertension in pregnancy and risk of coronary heart disease and stroke: a prospective study in a large UK cohort. Int J Cardiol. 2016;222:1012-1018. doi: 10.1016/j.ijcard.2016.07.170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bokslag A, Teunissen PW, Franssen C, et al. Effect of early-onset preeclampsia on cardiovascular risk in the fifth decade of life. Am J Obstet Gynecol. 2017;216(5):523.e1-523.e7. doi: 10.1016/j.ajog.2017.02.015 [DOI] [PubMed] [Google Scholar]
- 24.Wikström AK, Haglund B, Olovsson M, Lindeberg SN. The risk of maternal ischaemic heart disease after gestational hypertensive disease. BJOG. 2005;112(11):1486-1491. doi: 10.1111/j.1471-0528.2005.00733.x [DOI] [PubMed] [Google Scholar]
- 25.Stuart JJ, Tanz LJ, Rimm EB, et al. Cardiovascular risk factors mediate the long-term maternal risk associated with hypertensive disorders of pregnancy. J Am Coll Cardiol. 2022;79(19):1901-1913. doi: 10.1016/j.jacc.2022.03.335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levine LD, Ky B, Chirinos JA, et al. Prospective evaluation of cardiovascular risk 10 years after a hypertensive disorder of pregnancy. J Am Coll Cardiol. 2022;79(24):2401-2411. doi: 10.1016/j.jacc.2022.03.383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weissgerber TL, Milic NM, Milin-Lazovic JS, Garovic VD. Impaired flow-mediated dilation before, during, and after preeclampsia: a systematic review and meta-analysis. Hypertension. 2016;67(2):415-423. doi: 10.1161/HYPERTENSIONAHA.115.06554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hillman SL, Kubba T, Williams DJ. Delivery of small-for-gestational-age neonate and association with early-onset impaired maternal endothelial function. Ultrasound Obstet Gynecol. 2017;49(1):150-154. doi: 10.1002/uog.17342 [DOI] [PubMed] [Google Scholar]
- 29.Roberts JM, Rich-Edwards JW, McElrath TF, Garmire L, Myatt L; Global Pregnancy Collaboration . Subtypes of preeclampsia: recognition and determining clinical usefulness. Hypertension. 2021;77(5):1430-1441. doi: 10.1161/HYPERTENSIONAHA.120.14781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Z, Cheng Y, Wang D, et al. Incidence rate of type 2 diabetes mellitus after gestational diabetes mellitus: a systematic review and meta-analysis of 170,139 women. J Diabetes Res. 2020;2020:3076463. doi: 10.1155/2020/3076463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beckman JP, Camp JJ, Lahr BD, et al. Pregnancy history, coronary artery calcification and bone mineral density in menopausal women. Climacteric. 2018;21(1):53-59. doi: 10.1080/13697137.2017.1406910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Benschop L, Brouwers L, Zoet GA, et al. ; CREW Consortium . Early onset of coronary artery calcification in women with previous preeclampsia. Circ Cardiovasc Imaging. 2020;13(11):e010340. doi: 10.1161/CIRCIMAGING.119.010340 [DOI] [PubMed] [Google Scholar]
- 33.Zoet GA, Benschop L, Boersma E, et al. ; CREW Consortium . Prevalence of subclinical coronary artery disease assessed by coronary computed tomography angiography in 45- to 55-year-old women with a history of preeclampsia. Circulation. 2018;137(8):877-879. doi: 10.1161/CIRCULATIONAHA.117.032695 [DOI] [PubMed] [Google Scholar]
- 34.Hauge MG, Damm P, Kofoed KF, et al. Early coronary atherosclerosis in women with previous preeclampsia. J Am Coll Cardiol. 2022;79(23):2310-2321. doi: 10.1016/j.jacc.2022.03.381 [DOI] [PubMed] [Google Scholar]
- 35.Cirillo PM, Cohn BA. Pregnancy complications and cardiovascular disease death: 50-year follow-up of the Child Health and Development Studies pregnancy cohort. Circulation. 2015;132(13):1234-1242. doi: 10.1161/CIRCULATIONAHA.113.003901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Anderberg E, Källén K, Berntorp K, Frid A, Åberg A. A simplified oral glucose tolerance test in pregnancy: compliance and results. Acta Obstet Gynecol Scand. 2007;86(12):1432-1436. doi: 10.1080/00016340701532444 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Supplemental Methods
eReferences
eTable 1. Coronary Artery Disease Prevalence Differences as Vascular Age in Years by Adverse Pregnancy Outcome History
eTable 2. Overall Distribution and Prevalence of Segment-Specific Coronary Atherosclerosis by Adverse Pregnancy Outcome History
eTable 3. Subclinical Coronary Artery Disease in Women With Intermediate 10-Year Cardiovascular Disease Risk by Adverse Pregnancy Outcome History
eTable 4. Associations Between Adverse Pregnancy Outcome and Coronary Artery Disease Indices in Combined Model
eTable 5. Associations Between Preeclampsia History Ascertained by Self-Report and Coronary Artery Disease Indices
eTable 6. Dose Response Association Between Adverse Pregnancy Outcome and Coronary Artery Disease
eTable 7. Association Between Adverse Pregnancy Outcomes and Coronary Artery Disease Indices in Postmenopausal Women
eTable 8. Extended Coronary Artery Calcium Score Data by Adverse Pregnancy Outcome History
Data Sharing Statement



