Abstract
Background
Simulation based training (SBT) has become an important tool in medical education, yet a comprehensive review of its effect in anesthesiology is currently lacking. This study was aimed to compare the effect of SBT versus non-simulation based training (NSBT) in anesthesia education.
Methods
Data were derived from PubMed, Ovid (EMBASE and MEDLINE), China National Knowledge Infrastructure (CNKI) and China Biology Medicine (CBM) from database inception up to June 2022. We included published randomized controlled trials (RCTs) that assessed the impact of Simulation-Based Training (SBT) on anesthesiology training and compared it to Non-Simulation-Based Training (NSBT).
Results
25 eligible studies were included, with a total sample size of 1621 medical students. SBT was associated with improved theoretical scores [mean difference (MD):5.28, 95%CI 3.06 to 7.49, P < 0.01] and skill scores (MD: 7.63, 95% CI 5.7 to 9.57, P < 0.01) in comparison with NSBT. And SBT significantly improved teaching effects, including success rate, analytic skill in clinical setting, learning interest, learn efficiency and satisfaction survey. Also, a dramatic promotion was observed in the evaluation of non-technical ability consisting of cooperative ability, problem solving ability and situational awareness after trainees with SBT.
Conclusions
Simulation-based training is an effective method for improving theoretical scores, skill scores, teaching effects and non-technical ability. Yet, further good-quality RCTs are required to confirm these changes translate to improved patient outcomes. Furthermore, it is important to carefully consider the cost-benefit effect to conduct simulation-based in anesthesiology education.
Keywords: Anesthesiology, Simulation based training, Non-simulation based training
1. Introduction
As an important aspect of clinical medicine, anesthesiologists are required to be capable of handling life-threatening events without making any mistakes [1]. Therefore, anesthesia education focuses on cultivating well-rounded clinicians who have a firm grasp of both theoretical knowledge and clinical skill [2]. Traditionally, non-simulation based training (NSBT) has been used to mainly teach theoretical knowledge through an apprenticeship model, such as didactic training, lecture-based training (LBL), problem-based learning (PBL) [3]. However, students under this type of training often lack sufficient experience in handling critical events and struggle with teamwork. Meanwhile, the tension of the doctor-patient relationship also adds difficulty to the clinical teaching. It is hard for medical students to combine theory and practice in clinical work.
To address this contradiction, anesthesia educators introduced simulation-based training (SBT) to imitate real-life clinical events in the late 1960s [4]. Since then, a wider application for simulation has been called for. Simulation teaching pioneers the use of full-body Mannikins, which can mimic some common skills, including tracheal intubation, nerve block, central venous catheter placement, etc [[5], [6], [7], [8]]. Additionally, SBT offers trainees opportunities to deal with rare conditions such as difficult airway management and malignant hyperthermia [3,9]. With the recent emphasis on crisis resource management (CRM), scenario simulation has become a hot topic. It is designed to target specific scenarios and foster technical and teamwork skills through role play within the context of those scenarios [10].
Although an increasing number of reports have indicated the efficacy of simulation in medical education [11,12], reviews comparing SBT to NSBT have been limited by nonsystematic identification of studies and a lack of quantitative synthesis. This study aimed to compare the effectiveness of SBT versus NSBT in anesthesia education and provide the latest evidence for anesthesia educational designs.
2. Methods
This study was planned, conducted and reported according to the recommended PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines [13].
2.1. Search strategy and criteria
With assistance from an experienced reference librarian, a systematic search of PubMed and Ovid (EMBASE and MEDLINE) was performed to identify published potential trails. Also, data was retrieved from two Chinese databases, including China National Knowledge Infrastructure (CNKI) and the China Biology Medicine (CBM). The search strategy is presented in Appendix 1. The last retrieval was performed on June 14, 2022.
The Population, Intervention, Comparison, Outcome, Study type approach as incorporated in the PRISMA Statement was used to define eligibility criteria to search for relevant literature. (1) The population consisted of students, residents, or workers within anesthesiology. (2) The intervention was featured SBT as any ‘tool with which the learner can physically interact in order to mimic a clinical scenario for purposes of training and/or assessment including computer-based simulators, mannikins, animal specimens, and cadavers, High-fidelity simulator’ [14]. (3) The comparator was NSBT defined as no technology-enhanced simulation. (4) Relevant studies were centered on the primary data of assessing learner and/or patient outcomes; (5) Study designs could be two-group randomized controlled trials (RCTs). Hand-searching was conducted to identify additional eligible studies from previously published review articles or google scholar.
The eligible included RCTs was assessed independently by two researchers (YS and YZ). Firstly, references were imported into EndNote X9 software (Thomson Reuters, New York, NY) to eliminate repeated literature. Then, the literatures were excluded according to information from title and abstract. Finally, full-text reading was screened for meta-analysis. Disagreements were reconciled through discussion among the team members.
2.2. Data extraction
The authors' information, publication date, sample size, anesthesia topic, characteristics of trainees, intervention, and outcomes were extracted. The primary outcomes consisted of scores on the theory and skill test. The secondary outcomes involved non-technical ability including cooperative ability, problem solving ability and situational awareness. Additionally, teaching effectiveness was evaluated for secondary outcomes, which included success rate, analytic skills in a clinical setting, learning interest, learning efficiency, ease of comprehension, and satisfaction with the training program.
2.3. Assessment of risk of bias
The methodological quality for the included RCTs was assessed independently by two researchers (YS and YZ) based on Cochrane risk-of-bias [15], and each quality item was graded as low risk, high risk, or unclear risk. The seven items used to evaluate bias in each trial included the randomization sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias.
2.4. Quality of evidence
The quality of evidence for each outcome was rated based on criteria established by the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) group. Quality of evidence was classified as very low, low, moderate, or high [15]. Any disagreement was settled through discussion among the research team.
2.5. Subgroup analysis
We planned subgroup analysis according to the following categories: 1) perioperative anesthesia: the whole operative anesthesia including preoperative assessment, plan formulation, anesthesia administration, postoperative resuscitation; 2) regional anesthesia: neuraxial or nerve blockade; 3) inhalation anesthesia: researches based on GasMan computer-based simulation; 4) CRM: studies that address CRM training.
2.6. Statistical analysis
Review Manager (RevMan for Windows, version 5.4; Cochrane Collaboration, Oxford, UK) was applied to perform all meta-analysis. For continuous variables, the data was expressed as mean difference (MD) or standardized mean differences (SMD). For dichotomous variables, the data was indicated as relative risk ratio (RR). The 95% confidence interval (95% CI) and point estimate were given for each outcome. I2 test and chi-square test were used to assess heterogeneity (I2 > 50% indicating high heterogeneity, I2 < 50% indicating low heterogeneity) [16,17]. When P > 0.10 or I2 < 50%, a fixed-effect model was used for combined analysis. Conversely, when P < 0.10 or I2 > 50%, a random-effects model was used to pool the data, and we conducted a subgroup analysis to verify the outcome. And a sensitivity analysis was performed by leave-out method to identify the sources of heterogeneity. We assessed publication bias by examining funnel plots. All tests were 2-tailed, and P < 0.05 was statistically significant. The analysis plan was written before the data had been accessed. No significant deviated from the protocol during analyses procedure.
3. Results
3.1. Search results
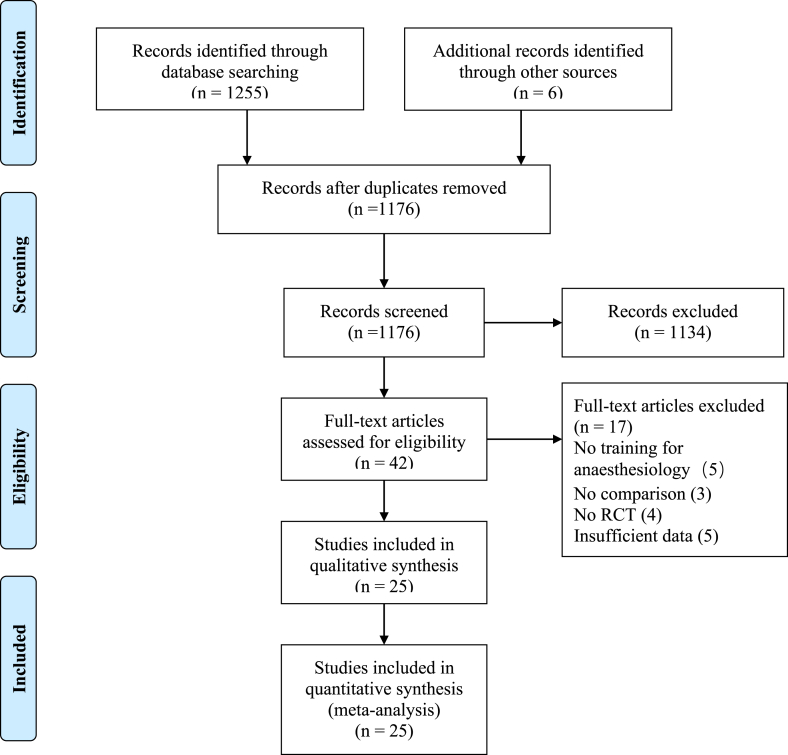
1255 studies were preliminarily identified from Pubmed (1029), Ovid (38), CNKI (136) and CBM (52). 6 additional eligible studies were screened by Google Scholar. After duplicates were removed, 1176 studies were analyzed based on the title and abstract and 1134 studies were excluded. The remaining 42 articles were checked for eligibility based on full text reading and 17 studies being excluded, the 17 excluded studies consisted of five that had no training for anesthesiology, three lacking comparisons, four that were not randomized controlled trials, and five that had insufficient data (see details in Appendix 2). Ultimately, 25 articles [[5], [6], [7],9,[18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37]] met the inclusion criteria with a total of 1638 trainees. A Prisma-flow diagram of the literature search and the exclusion criteria is listed in Fig. 1.
Fig. 1.
Prisma-flow diagram for the literature search and exclusion criteria.
3.2. Study characteristics
The characteristics of the 25 studies included in this meta-analysis are listed in Table 1. These studies encompassed a total of 1638 trainees, with 819 trainees in the SBT group and 802 trainees in the NSBT group. The majority of trainees were interns, residents and junior anesthesiologists with limited related clinical experience. All the studies included in the analysis were published between 2005 and 2022. The sample size ranged from 10 to 108 trainees. Among these studies, 8 studies [3,5,9,[33], [34], [35], [36], [37]] were published in English and the other 17 studies [6,7,[18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32]] were published in Chinese. The areas of anesthesia topics covered during the training were perioperative anesthesia (9 studies), airway management (3 studies), inhalation anesthesia (2 studies), regional anesthesia (2 studies), cardiopulmonary resuscitation (2 studies), CRM (2 studies). Each of the following subjects-anesthesia induction, cardiopulmonary bypass, transesophageal echocardiography, central venous catheterization, malignant hyperthermia-was the focus of one study. Outcomes reported in 15 studies reflected assessments in theoretical settings. And 12 studies were focused on assessments in clinical skills.
Table 1.
Demographic characteristics of the included studies.
| Author/year |
Sample size |
Anesthesia |
Intervention |
Outcomes |
|||||
|---|---|---|---|---|---|---|---|---|---|
| SBT | NSBT | topic | Trainees | SBT |
NSBT |
||||
| Methods | Duration of the training | Methods | Duration of the training | ||||||
| Hall et al. 2005 | 18 | 18 | AM | Intern | Manikin | 10-h per trainee | RP | 15 intubation attempts | SR |
| Wang et al. 2008 | 21 | 21 | CPR | Intern | Manikin + PBL | 6 CPR attempts +1 Manikin | PBL | 6 CPR attempts | TT, ST, TEE (SS, AS, LI) |
| Hallikainen et al. 2009 | 23 | 18 | AI | Intern | Manikin | 1 week of lectures + 3 h instruction | RP | 1 week of lectures + 3 h instruction | SR |
| Bruppacher et al. 2010 | 10 | 10 | CPB | Junior | Manikin | 1 week of lectures + 2 h instruction | ST | 1 week of lectures + 2 h instruction | NTA(CA, PSA, SA) |
| Campos et al. 2011 | 13 | 14 | AM | Postgraduate | Manikin | 45-min per trainee | Video | 14-min long video, maximum of two replays | SR |
| Ferrero et al. 2014 | 21 | 21 | TEE | Residents | Manikin | 45-min per trainee | DT | 45-min per trainee | ST |
| Minai et al. 2014 | 28 | 29 | AM | Intern | SS + Manikin | 10–15 min per trainee | LBL + Observation | 10–15 min per trainee | SR |
| Li et al. 2014 | 16 | 16 | IA | Resident | CBS | 6 lectures | LBL | 6 lectures | TT |
| Lin et al. 2015 | 67 | 67 | PA | Undergraduate | Manikin + CBL | Did not provide | CBL | Did not provide | TT, TEE (SS) |
| Wei et al. 2015 | 29 | 29 | PA | Intern | SS + Manikin + CBL | Did not provide | CBL | Did not provide | TT, ST, TEE (SS) |
| Zou et al.2015 | 50 | 50 | PA | Intern | HFS | 20 lectures | DT | 20 lectures | TT, ST |
| Gong et al. 2016 | 107 | 107 | PA | Undergraduate | Manikin | Did not provide | DT | Did not provide | TT, ST |
| Guan et al. 2016 | 10 | 10 | RA | Resident | Manikin | Did not provide | DT | Did not provide | TT, ST |
| Sheng et al. 2016 | 10 | 10 | RA | Resident | Manikin + Multimedia | Did not provide | Multimedia | Did not provide | TT, ST |
| Wu et al. 2016 | 30 | 30 | CVC | Undergraduate | Manikin + Multimedia | Did not provide | Multimedia | Did not provide | TT |
| Xie et al. 2016 | 10 | 10 | CRM | Junior | Manikin + CBL | Did not provide | CBL | Did not provide | TT, ST |
| Ke et al. 2017 | 50 | 50 | IA | Undergraduate | CBS + LBL | 4 lectures | LBL | 4 lectures | TT, TEE (AS, LI, LE, EU) |
| Zhao et al. 2017 | 20 | 20 | PA | Intern | Manikin | Did not provide | LBL | Did not provide | TT, ST, TEE (SS, AS, LI, LE, EU) |
| Mejíaa et al. 2017 | 16 | 15 | MH | Resident | HFS | A lecture and read 2 complementary literature reviews + one HFS lecture | CBL | A lecture and read 2 complementary literature reviews + one lecture | NTA(CA, PSA, SA) |
| Wei et al. 2018 | 19 | 19 | CRM | Intern, Resident, Junior | HFS | 4 lectures | PBL | 4 lectures | ST, TEE (SS), NTA(CA) |
| Zhong et al. 2018 | 108 | 99 | PA | Undergraduate | SS | Did not provide | DT | Did not provide | TT, ST, TEE (AS, LI, LE) |
| Berger et al. 2019 | 58 | 54 | CPR | Intern | HFS | 30-min per trainee | PBL | 30-min per trainee | SR |
| Su et al. 2019 | 25 | 25 | PA | Intern | HFS + CBL | Did not provide | DT | Did not provide | TT, ST, TEE (SS) |
| Wang et al. 2019 | 36 | 36 | PA | Intern | SS | Did not provide | DT | Did not provide | TT, ST, TEE (SS) |
| Cao et al. 2020 | 24 | 24 | PA | Resident | HFS | 2-h theory + 2-h skill training | DT | 2-h theory + 2-h skill training | SR, TT, NTA(PSA, SA) |
Sample size/Intervention: SBT, simulation-based training; NSBT, non-simulation based training; Anesthesia topic: AM, airway management; CPR, cardiopulmonary resuscitation; AI, anesthesia induction; CPB, cardiopulmonary bypass; TEE, transesophageal echocardiography; IA, inhalation anesthesia; PA, perioperative anesthesia; RA, regional anesthesia; CVC, central venous catheterization; CRM, crisis resource management; MH, malignant hyperthermia; Trainees: Junior, junior anesthesiologist; Intervention: PBL, problem-based learning; SS, scenario simulation; CBS, computer-based simulation; LBL, lecture-based training; CBL, case-based learning; HFS, high-fidelity simulator; DT, didactic training; Outcomes: SR, success rate; TT, theory test; ST, skill test; TEE, teaching effect evaluation; SS, satisfaction survey for teaching; AS, analytic skill in clinical setting; LI, learning interest; LE, learning efficiency; EU, easy to understand; NTA, non-technical ability; CA, cooperative ability; PSA, problem solving ability; SA, situational awareness.
3.3. Risk of bias and quality of evidence
For the generation of random sequences, 16 studies describing the method was judged as low risks including random number table in 10 studies [3,5,8,22,23,31,[33], [34], [35],37] and random draw in 6 studies [6,21,24,26,28,30]. 3 studies randomly assigned with odd or even numbers were judged as high risks. The remaining 6 studies did not provide relevant information about the generation of random sequences and were judged as unclear risks. Only 3 studies described the method of allocation concealment, using sealed enveloping, and were classified as low risk. Other studies did not mention the allocation concealment method and were rated as unclear risk. Out of the total of nine studies, where blinding was implemented for participants and personnel, nine studies were categorized as low risk, as participants and implementers were not informed about the group assignment, while the remaining studies were evaluated as unclear risk, with no blinding information. However, 5 studies mentioning that independents assessed outcomes were classified as low risk. 5 studies were at high risks in which implementers took part in assessing outcomes and others were regarded as unclear risk without any information. The risk of bias item for each included study is shown in Supplementary Fig. 1. All studies were at low risk in incomplete outcome data, selective reporting, and other bias.
3.4. Meta-analysis
3.4.1. Theory test and skill performance
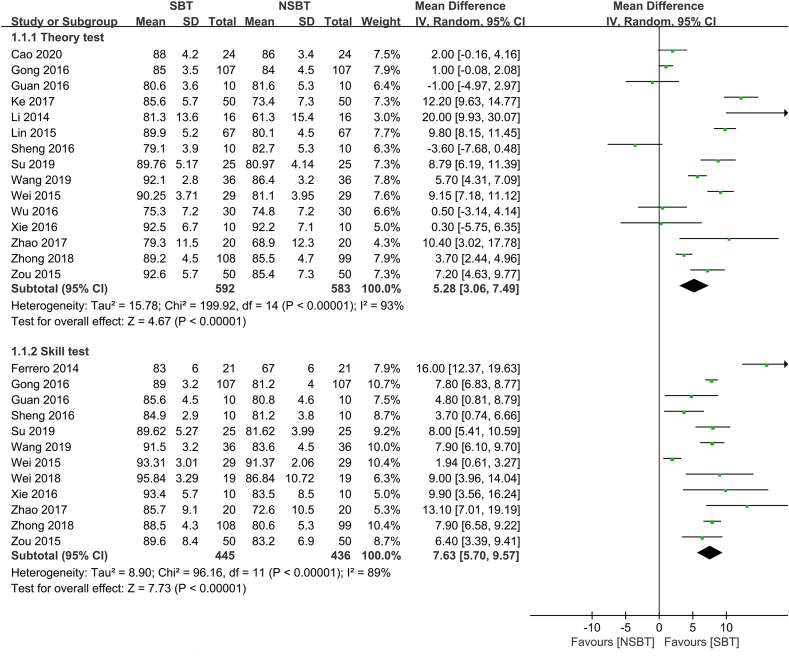
As shown in Fig. 2, 15 studies presented relevant data on theoretical scores (592 trainees in SBT and 583 trainees in NSBT). The pooled estimates of these studies showed significant improvement in SBT compared with NSBT (MD 5.28, 95%CI 3.06 to 7.49, P < 0.01, I2 = 93%). GRADE evidence for theoretical scores within all included studies was moderate and downgraded for ‘inconsistency’ (Appendix 2).12 studies reported suitable data on skill test (445 trainees in SBT and 436 trainees in NSBT). SBT had favorable effect on skill scores in comparison with NSBT controls with (MD 7.63, 95% CI 5.7 to 9.57, P < 0.01, I2 = 89%) (Fig. 2) GRADE evidence for skill scores within all included studies was moderate and downgraded for ‘inconsistency’ (Appendix 3). An assessment of the publication bias is shown in Supplementary Fig. 2 by using funnel plots of knowledge scores and skill scores, and no publication bias was found.
Fig. 2.
Forest plot of theoretical and skill test.
3.4.2. Subgroup analysis
Owing to the high heterogeneity in theory and skill test, we conducted sensitivity analysis. After eliminating studies one by one, the value of I2 in theory and skill test was ranged 91%–93% and 70%–90%, respectively and the results of meta-analysis had no significant change. To further explore the sources of heterogeneity, we conducted subgroup analysis (Table 2). For theoretical scores, 8 studies [19,[23], [24], [25],28,[30], [31], [32]] included in perioperative anesthesia favored on SBT group compared with NSBT group and random-effects MD was 6.67 (95%CI 4.06 to 9.27, P < 0.01, I2 = 94%). Simultaneously, sensitivity analysis showed no significant change in heterogeneity (I2 ranged for 87%–95%). 2 studies [21,22] consisted in inhalation anesthesia showed a favorable effect on SBT in comparison with NSBT (MD 14.52, 95%CI 7.53 to 21.52, P < 0.01, I2 = 54%). No significant difference was observed in the category of regional anesthesia [6,20] and random-effects MD was −2.27 (95%CI -5.11to 0.58, P = 0.08, I2 = 0). The rest 3 studies [7,18,29] involved in airway management, central venous catheterization and CRM were excluded from subgroup analysis.
Table 2.
Results of subgroup analysis.
| No. of | Incidence | Subgroup difference | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcomes | Subgroups | Studies | SBT | NSBT | MD | 95%CI | Chi2 | P | I2 | ||
| Theory test | Perioperative anesthesia | 8 | 442 | 443 | 6.67 | [4.06,9.27] | 120.48 | <0.01 | 94% | ||
| Inhalation anesthesia | 2 | 66 | 66 | 14.52 | [7.53,21.51] | 2.17 | <0.01 | 54% | |||
| Regional anesthesia | 2 | 20 | 20 | −2.27 | [-5.11,0.58] | 0.80 | 0.12 | 0% | |||
| Skill test | Perioperative anesthesia | 6 | 346 | 337 | 7.85 | [7.18,8.52] | 3.78 | <0.01 | 0% | ||
| Regional anesthesia | 2 | 20 | 20 | 4.09 | [1.71,6.47] | 0.19 | <0.01 | 0% | |||
| Crisis resource management | 2 | 29 | 29 | 9.35 | [5.40,13.30] | 0.05 | <0.01 | 0% | |||
No., number; SBT, simulation based training; NSBT, non-simulation based training, MD: Mean differences, CI: confidence interval.
In the subgroup analysis of skill test, 7 studies [19,24,25,28,[30], [31], [32]], Refs. [18,23,24,27,[29], [30], [31]] were classified into perioperative anesthesia had a favorable effect on SBT group (MD 7.11, 95%CI 4.19 to 9.31, P < 0.01, I2 = 91%) and after eliminating one study [28], the heterogeneity was significantly reduced (MD 7.85, 95%CI 7.18 to 8.52, P < 0.01, I2 = 0%). The subgroup of regional anesthesia [6,20] and CRM [27,29] included 2 studies respectively and trainees in SBT group showed higher scores than NSBT group. The meta-analysis showed MD of regional anesthesia was 4.09 (95%CI 1.71 to 6.47, P < 0.01, I2 = 0%) and CRM was 9.53 (95%CI 5.4 to 13.3, P < 0.01, I2 = 0%).
3.4.3. Evaluation of teaching effect and non-technical ability
The study used 6 items which evaluated teaching effect, including success rate, analytic skill in clinical setting, learning interest, learn efficiency, easy to understand and satisfaction survey. All evaluation items except easy to understand showed a favorable effect on SBT compared with NSBT (P < 0.05). Additionally, the evaluation of non-technical abilities, which included cooperative ability, problem-solving ability, and situational awareness, favored the SBT method over the NSBT method (P < 0.05). Table 3 presents the detailed results of the meta-analysis, which underwent sensitivity analysis by eliminating studies one by one.
Table 3.
Results of secondary outcomes analysis.
| Secondary outcomes | No. of |
|||||||
|---|---|---|---|---|---|---|---|---|
| Studies | SBT | NSBT | RR (95%CI) | P | I2 | |||
| Teaching effect evaluation | Success rate | 6 | 433 | 425 | 1.64 | [1.11, 2.43] | 0.01 | 86% |
| Analytic skill in clinical setting | 4 | 101 | 101 | 1.95 | [1.47, 2.59] | <0.01 | 22% | |
| Learning interest | 4 | 101 | 101 | 2 | [1.5, 2.56] | <0.01 | 30% | |
| Learning efficiency | 4 | 188 | 179 | 1.76 | [1.04, 2.99] | 0.04 | 88% | |
| Easy to understand | 2 | 70 | 70 | 2.45 | [0.96, 6.26] | 0.06 | 82% | |
| Satisfactory survey | 5 | 177 | 177 | 1.47 | [1.28, 1.68] | <0.01 | 0% | |
| No. of | ||||||||
| Secondary outcomes | Studies | SBT | NSBT | SMD (95%CI) | P | I2 | ||
| Non-technical ability | Cooperative ability | 2 | 34 | 35 | 0.76 | [0.27, 1.26] | <0.01 | 0% |
| Problem solving ability | 3 | 34 | 34 | 5.71 | [4.58, 6.84] | <0.01 | 0% | |
| Situational awareness | 3 | 34 | 34 | 5.88 | [4.73, 7.04] | <0.01 | 0% | |
No., number; SBT, simulation based training; NSBT, non-simulation based training; RR: risk ratio, SMD: standardized mean differences, CI: confidence interval.
4. Discussion
Based on our findings in this systematic review of 25 studies, simulation training appears to be effective for acquiring knowledge and skills. However, the clinical or knowledge advantage remains a significant concern to justify the implementation of simulation in a medical program [38]. As indicated by a previous systematic review for anesthesia education, six studies (299 trainees) assessed skills and six studies (380 trainees) assessed knowledge both favoring simulation [39]. Similarly, in the current meta-analysis, we demonstrated the benefit of simulation education in theoretical knowledge acquisition and skill performance improvement. To exclude the influence of high heterogeneity on the results, we conducted sensitivity analysis by eliminating studies one by one, while the heterogeneity was still high. We then performed subgroup analysis, which showed that simulation teaching significantly improved the scores of theoretical and skill tests in perioperative anesthesia, inhalation anesthesia, regional anesthesia, and CRM. However, the subgroup analysis of regional anesthesia failed to demonstrate a significant benefit of SBT in theoretical knowledge acquisition. Only two studies with small sample sizes have reported on this field, which may help to explain the negative effect on theoretical knowledge acquisition among different anesthesia subjects [6,20]. Moreover, the tests used to evaluate theoretical knowledge acquisition are highly heterogeneous across studies, including differences in test content, training duration and so on. Thus, given these limitations, our results need to be interpreted with caution.
Anesthesiology is a subject with strong operational capability, and this traditional method is not enough for handling emergency situation. Therefore, simulation-based education has become a prevalent topic with offering an experiential learning paradigm for training and assessment, with opportunities to improve learning interest, communication, and decision-making skills for common as well as rare events [40]. Together with our study, we found all included studies showed a preferred effect on simulation teaching in comparison with no-simulation teaching including success rate, analytic skill in clinical setting, learn interesting, learn efficiency and satisfactory survey.
Anesthesiologists should possess high clinical skill, quick reaction ability and good teamwork ability to deal with CRM. Therefore, non-technical skills such as communication, team work, situation awareness, and decision-making are also indispensable skills for anesthesiology residents [41]. In our study, we found that trainees following simulation teaching showed a better capability in cooperative ability, problem solving ability and situational awareness. Admittedly, simulation teaching can mimic the clinical environment, the actual diagnosis, and treatment process, so that these trainees can fully grasp the key points and procedures of emergency anesthesia. As a result, the clinical teaching effect of simulation teaching is remarkable, and students can improve their clinical levels and adapt to clinical work more quickly.
5. Limitations
In this systematic review, we included only two-group (SBT versus NSBT) RCTs, which is both a strength and limitation [42]. In education, some have argued that RCTs have confused results, with possibly no practical application to the field of human affairs [43]. Then, we found high heterogeneity in most analyses, which was most likely caused by special requirements for schools and teachers to conduct simulation training. The different training levels of teachers and schools may have a significant impact on outcomes. Besides, anesthesiology is an integrated discipline involving perioperative anesthesia, regional anesthesia, CRM and some special items. One outcome measurement cannot cover all categories. Another important limitation to consider is the potential impact of trainee experience and training duration on the effectiveness of SBT and NSBT. Unfortunately, there is limited data available from primary studies that addresses this issue. Training duration varies greatly among studies and the experience level of training teachers is often unknown, which calls for caution when interpreting the conclusions of the current study. Besides, course content, the difficulty of examination, duration of courses, and preparation of teachers and students were different, which might have led to heterogeneity in the evaluation results. All of these may have contributed to the low score on GRADE. Finally, except for scores of theory and skill test, the questionnaire for teaching effect and non-technical ability is mainly derived from satisfaction survey, which lacked systematic and scientific evaluation indexes.
6. Suggestions for future study
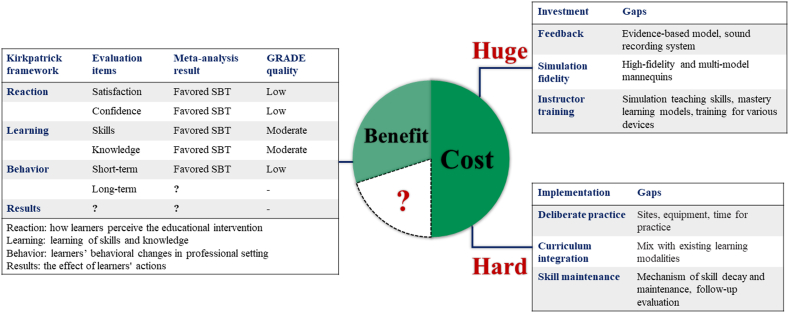
From this system review, we have some suggestion for future study. Firstly, all literatures included in this meta-analysis can be classified into three Kirkpatrick levels: teaching effect for reaction (Kirkpatrick level 1), theory and skill test for learning (Kirkpatrick level 2), non-technical ability for behavior (Kirkpatrick level 3) [44]. However, no literature is included in level 4 (measured changes in patient outcomes) (Fig. 3). Without fully evaluation the patient outcome in anesthesia simulation research, it is unlikely that decision makers will devote the necessary resources and personnel toward this venture. Also, in these included trails, only 2 studies reported long-term retention including 5 weeks [34] and 6 months later [33]. Considering the different evaluation items, these results cannot be combined for quantitative analysis. Therefore, a more comprehensive and reasonable way to evaluate he potential advantages and benefits of simulation education in anesthesiology should be directed toward patient outcomes.
Fig. 3.
A summary for the benefit and cost of simulation training.
While we have objectively demonstrated that SBT is a promising method for anesthesia education, the huge financial and human resources should not be ignored (Fig. 3). First, feedback is the most important and frequently cited variable to assess the effectiveness of SBT [45]. Debriefing is the core and soul of simulation teaching feedback, while it’s a huge cost to establish different evidence-based model and sound recording system for variable disciplines. Moreover, not every teaching institution can afford to procure the necessary quantity of high-fidelity and multi-model mannequins required to replicate real clinical conditions. The instructors' role in facilitating, guiding and motivating learners is essential and there is a great need for a uniform mechanism to educate, evaluate and certify simulation instructors for the health care professions [46]. The implementation of simulation training for resource-limited regions and countries is limited. Deliberate practice is grounded in information processing and skill acquisition, while it’s hard to fill these gaps among sites, equipment and time for long-time deliberate practice. Educational experts have suggested that simulator practice should be carefully integrated with present educational events, including clinical experience, lectures and laboratory work [47]. The optimal approach to integrate SBT into existing curricula and the impact of this introduction on faculty and administrative resources remain to be explored. Although a growing number of studies are being performed to explore the mechanisms of skill decay, the results are inconsistent, and more research is clearly needed here. Additionally, we lack human resources for long-term follow-up evaluation in the current educational resources.
Overall, the results of this meta-analysis indicate that anesthesiology simulation-based training not only improves knowledge scores and skill scores but also enhances teaching effect and non-technical ability. However, it would be unwise to blindly expand applications, considering the significant resource investment it requires. There is a significant gap in outcome assessment, particularly regarding patient improvement. At a practical level, we should carefully balance the benefits and costs of SBT implementation in resource-limited regions and countries to meet the needs of social development for anesthesiology talents.
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Data availability statement
Data included in article/supplementary material/referenced in article.
Authors' contributions
YS was responsible for the original study proposal. YS and YZ drafted the original study protocol and independently screened papers, extracted data and methodological quality. YS wrote the initial draft of the manuscript. YZ provided writing advice and methodological guidance. All the authors contributed to consecutive drafts and approved the final manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
Acknowledgment
Useful suggestions given by professors of the Chinese Cochrane Center are acknowledged.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e18249.
Abbreviations
- SBT
simulation-based training
- NSBT
non-simulation based training
- Anesthesia topic:AM
airway management
- CPR
cardiopulmonary resuscitation
- AI
anesthesia induction
- CPB
cardiopulmonary bypass
- TEE
transesophageal echocardiography
- IA
inhalation anesthesia
- PA
perioperative anesthesia
- RA
regional anesthesia
- CVC
central venous catheterization
- CRM
crisis resource management
- MH
malignant hyperthermia
- Trainees:Junior
junior anesthesiologist
- Intervention:PBL
problem-based learning
- SS
scenario simulation
- CBS
computer-based simulation
- LBL
lecture-based training
- CBL
case-based learning
- HFS
high-fidelity simulator
- Outcomes:SR
success rate
- TT
theory test
- ST
skill test
- TEE
teaching effect evaluation
- SS
satisfaction survey for teaching
- AS
analytic skill in clinical setting
- LI
learning interest
- LE
learning efficiency
- EU
easy to understand
- NTA
non-technical ability
- CA
cooperative ability
- PSA
problem solving ability
- SA
situational awareness
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Nelsen B.R., Chen Y.K., Lasic M., Bader A.M., Arriaga A.F. Advances in anesthesia education: increasing access and collaboration in medical education, from E-learning to telesimulation. Curr. Opin. Anaesthesiol. 2020;33(6):800–807. doi: 10.1097/ACO.0000000000000931. [DOI] [PubMed] [Google Scholar]
- 2.Beutler S., McEvoy M.D., Ferrari L., Vetter T.R., Bader A.M. The future of anesthesia education: developing frameworks for perioperative medicine and population health. Anesth. Analg. 2020;130(4):1103–1108. doi: 10.1213/ANE.0000000000004686. [DOI] [PubMed] [Google Scholar]
- 3.Mejia V., Gonzalez C., Delfino A.E., Altermatt F.R., Corvetto M.A. Acquiring skills in malignant hyperthermia crisis management: comparison of high-fidelity simulation versus computer-based case study. Rev. Bras. Anestesiol. 2018;68(3):292–298. doi: 10.1016/j.bjan.2018.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Denson J.S., Abrahamson S. A computer-controlled patient simulator. JAMA. 1969;208(3):504–508. [PubMed] [Google Scholar]
- 5.Minai F., Shafiq F., Ul Haq M.I. Value of real life (in situ) simulation training for tracheal intubation skills in medical undergraduates during short duration anesthesia rotation. J. Anaesthesiol. Clin. Pharmacol. 2014;30(4):484–487. doi: 10.4103/0970-9185.142807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sheng W.X., Feng F., Zhao B.J. The application of medical simulation teaching method in nerve block teaching. Cont. Med. Educ. 2016;30(10):12–13. doi: 10.3969/j.issn.1004-6763.2016.10.008. [DOI] [Google Scholar]
- 7.Wu J.Y., Wang T., Wang Z., Qin X.M., Lu W.H., Jin X.J. The value of simulation based medical education in central venous catherization multi-media teaching. Chin. J. Clin. 2016;10(2):303–306. CNKI:SUN:ZLYD.0.2016-02-033. [Google Scholar]
- 8.Muriel-Fernández J., Alonso C.P., López-Valverde N., López-Millán J.M., Juánes Méndez J.A., Sánchez-Ledesma M.J. Results of the use of a simulator for training in anesthesia and regional analgesia guided by ultrasound. J. Med. Syst. 2019;43(4):79. doi: 10.1007/s10916-019-1196-6. [DOI] [PubMed] [Google Scholar]
- 9.Campos J.H., Hallam E.A., Ueda K. Training in placement of the left-sided double-lumen tube among non-thoracic anaesthesiologists: intubation model simulator versus computer-based digital video disc, a randomised controlled trial. Eur. J. Anaesthesiol. 2011;28(3):169–174. doi: 10.1097/EJA.0b013e328340c332. [DOI] [PubMed] [Google Scholar]
- 10.Ciporen J., Gillham H., Noles M., Dillman D., Baskerville M., Haley C., Spight D., Turner R.C., Lucke-Wold B.P. Crisis management simulation: establishing a dual neurosurgery and anesthesia training experience. J. Neurosurg. Anesthesiol. 2018;30(1):65–70. doi: 10.1097/ANA.0000000000000401. [DOI] [PubMed] [Google Scholar]
- 11.Ferguson J., Astbury J., Willis S., Silverthorne J., Schafheutle E. Implementing, embedding and sustaining simulation-based education: what helps, what hinders. Med. Educ. 2020;54(10):915–924. doi: 10.1111/medu.14182. [DOI] [PubMed] [Google Scholar]
- 12.Friederichs H., Marschall B., Weissenstein A. Simulation-based mastery learning in medical students: skill retention at 1-year follow up. Med. Teach. 2019;41(5):539–546. doi: 10.1080/0142159x.2018.1503411. [DOI] [PubMed] [Google Scholar]
- 13.Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M., Shekelle P., Stewart L.A., Group P.-P. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cook D.A., Hatala R., Brydges R., Zendejas B., Szostek J.H., Wang A.T., Erwin P.J., Hamstra S.J. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306(9):978–988. doi: 10.1001/jama.2011.1234. [DOI] [PubMed] [Google Scholar]
- 15.Higgins J.P., Altman D.G., Gotzsche P.C., Juni P., Moher D., Oxman A.D., Savovic J., Schulz K.F., Weeks L., Sterne J.A. Cochrane bias methods G., Cochrane statistical methods G. The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gomes C.A., Andriolo R.B., Bennett C., Lustosa S.A., Matos D., Waisberg D.R., Waisberg J. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. Cochrane Database Syst. Rev. 2015;2015(5) doi: 10.1002/14651858.CD008096.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basta M.N., Rao V., Paiva M., Liu P.Y., Woo A.S., Fischer J.P., Breuing K.H. Evaluating the inaccuracy of the national surgical quality improvement project surgical risk calculator in plastic surgery: a meta-analysis of short-term predicted complications. Ann. Plast. Surg. 2022;88(3 Suppl 3):S219–s223. doi: 10.1097/sap.0000000000003189. [DOI] [PubMed] [Google Scholar]
- 18.Cao Y., Ding F., Lu Y., Gong S.Y., Jiang L.X. Effect evaluation of airway crisis situation simulation laryngeal mask management. Chin. J. Med. Educ. 2020;(3):217–220. doi: 10.3760/cma.j.issn.1673-677X.2020.03.014. [DOI] [Google Scholar]
- 19.Gong X.F., li H., luo X.H., li Q., Wang X.Y. Discussion on the application of simulation teaching in practice teaching of anesthesiology. China Higher Med. Educ. 2016;(12) doi: 10.3969/j.issn.1002-1701.2016.12.042. [DOI] [Google Scholar]
- 20.Guan L., Sheng W.X., Chen L.F., li T.Z. The application of multimedia combined with medical simulation teaching method in spinal anesthesia teaching. Cont. Med. Educ. 2016;30(9) doi: 10.3969/j.issn.1004-6763.2016.09.021. [DOI] [Google Scholar]
- 21.Ke J.J., Chen C., Wu Y., Zhang Z.Z. Application of GasMan software simulation teaching method in the teaching of inhalation anesthesia. Chin Med. Herald. 2017;14(22) CNKI:SUN:YYCY.0.2017-22-038. [Google Scholar]
- 22.Li Q., Fang L.Q., li Q., Lv P.L., Zhu T. Preliminary application and evaluation of GAS MAN assisted instruction in anesthesiology residency training. Chin. J. Med. Educ. Res. 2014;13(4):398–401. doi: 10.3760/cma.j.issn.2095-1485.2014.04.020. [DOI] [Google Scholar]
- 23.Lin J.Y., Yang L.Y., He J. Application of case-based learning combined with medical simulation in the teaching of anesthesiology. Chin. Med. Record. 2015;(3) doi: 10.3969/j.issn.1672-2566.2015.03.031. [DOI] [Google Scholar]
- 24.Su M.P., Li L.J., Jing S.X., Reng P.S. Application of CBL teaching mode combined with simulation training in clinical anesthesiology teaching. Chin. Med. Herald. 2019;16(10):71–74. CNKI:SUN:YYCY.0.2019-10-018. [Google Scholar]
- 25.Wang R.J. Feasibility study of scenario simulation teaching in clinical anesthesia. Chin. Commun. Doctors. 2019;35(14) doi: 10.3969/j.issn.1007-614x.2019.14.125. [DOI] [Google Scholar]
- 26.Wang X.P., Martin S.M., Li Y.L., Chen J., Zhang M.Y. Effect of emergency care simulator combined with problem-based learning in teaching of cardiopulmonary resuscitation. Natl. Med. J. China (Peking) 2008;(23):1651–1653. doi: 10.3321/j.issn:0376-2491.2008.23.018. [DOI] [PubMed] [Google Scholar]
- 27.Wei H., Feng J.H., Li C.Y., Zhang J., Zhang P., Luo X.M. The application of high simulation teaching in anaesthesia crisis management training. Guangxi Med. J. 2018;40(12) doi: 10.11675/j.issn.0253-4304.2018.12.38. [DOI] [Google Scholar]
- 28.Wei X., Zhang B. The application of scenario simulation teaching in clinical practice in anesthesiology undergraduates. Chin. Cont. Med. Educ. 2015;7(27) doi: 10.3969/j.issn.1674-9308.2015.27.005. [DOI] [Google Scholar]
- 29.Xie Y.H., Zhang M., Cai X.Q. Application of medical simulation teaching in anesthesiology crisis emergency events. Anhui Med. J. 2016;(6) doi: 10.3969/j.issn.1000-0399.2016.06.043. [DOI] [Google Scholar]
- 30.Zhao G., Zhu Y.L., Wang Q. Application of medical simulation teaching in clinical practice teaching of anesthesia specialty undergraduates. Chin. Cont. Med. Educ. 2017;9(4) CNKI:SUN:JXUY.0.2017-04-017. [Google Scholar]
- 31.Zhong H.H., Wang Y.D., Wang Y.Q., Zhang J.F. Application of simulation teaching in practice teaching of anesthesiology. China Higher Med. Educ. 2018;(11) CNKI:SUN:ZOGU.0.2018-11-016. [Google Scholar]
- 32.Zou L., Liu D.Y. Application of scene Simulation Teaching in clinical teaching of anesthesiology. China Health Ind. 2015;12(10) CNKI:SUN:WSCY.0.2015-10-025. [Google Scholar]
- 33.Berger C., Brinkrolf P., Ertmer C., Becker J., Friederichs H., Wenk M., Van Aken H., Hahnenkamp K. Combination of problem-based learning with high-fidelity simulation in CPR training improves short and long-term CPR skills: a randomised single blinded trial. BMC Med. Educ. 2019;19(1):180. doi: 10.1186/s12909-019-1626-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bruppacher H.R., Alam S.K., LeBlanc V.R., Latter D., Naik V.N., Savoldelli G.L., Mazer C.D., Kurrek M.M., Joo H.S. Simulation-based training improves physicians' performance in patient care in high-stakes clinical setting of cardiac surgery. Anesthesiology. 2010;112(4):985–992. doi: 10.1097/ALN.0b013e3181d3e31c. [DOI] [PubMed] [Google Scholar]
- 35.Ferrero N.A., Bortsov A.V., Arora H., Martinelli S.M., Kolarczyk L.M., Teeter E.C., Zvara D.A., Kumar P.A. Simulator training enhances resident performance in transesophageal echocardiography. Anesthesiology. 2014;120(1):149–159. doi: 10.1097/aln.0000000000000063. [DOI] [PubMed] [Google Scholar]
- 36.Hall R.E., Plant J.R., Bands C.J., Wall A.R., Kang J., Hall C.A. Human patient simulation is effective for teaching paramedic students endotracheal intubation. Acad. Emerg. Med. 2005;12(9):850–855. doi: 10.1197/j.aem.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 37.Hallikainen J., Väisänen O., Randell T., Tarkkila P., Rosenberg P.H., Niemi-Murola L. Teaching anaesthesia induction to medical students: comparison between full-scale simulation and supervised teaching in the operating theatre. Eur. J. Anaesthesiol. 2009;26(2):101–104. doi: 10.1097/EJA.0b013e32831a6a76. [DOI] [PubMed] [Google Scholar]
- 38.Zeng H.L., Chen D.X., Li Q., Wang X.Y. Effects of seminar teaching method versus lecture-based learning in medical education: a meta-analysis of randomized controlled trials. Med. Teach. 2020:1–7. doi: 10.1080/0142159X.2020.1805100. [DOI] [PubMed] [Google Scholar]
- 39.Lorello G.R., Cook D.A., Johnson R.L., Brydges R. Simulation-based training in anaesthesiology: a systematic review and meta-analysis. Br. J. Anaesth. 2014;112(2):231–245. doi: 10.1093/bja/aet414. [DOI] [PubMed] [Google Scholar]
- 40.Shah A., Mai C.L., Shah R., Levine A.I. Simulation-based education and team training. Otolaryngol. Clin. 2019;52(6):995–1003. doi: 10.1016/j.otc.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 41.Sidi A., Gravenstein N., Vasilopoulos T., Lampotang S. Simulation-based assessment identifies longitudinal changes in cognitive skills in an anesthesiology residency training program. J. Patient Saf. 2017 doi: 10.1097/PTS.0000000000000392. [DOI] [PubMed] [Google Scholar]
- 42.Sibbald B., Roland M. Understanding controlled trials. Why are randomised controlled trials important? BMJ. 1998;316(7126):201. doi: 10.1136/bmj.316.7126.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Deaton A., Cartwright N. Understanding and misunderstanding randomized controlled trials. Soc. Sci. Med. 2018;210:2–21. doi: 10.1016/j.socscimed.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen X.X., Trivedi V., AlSaflan A.A., Todd S.C., Tricco A.C., McCartney C.J.L., Boet S. Ultrasound-guided regional anesthesia simulation training: a systematic review. Reg. Anesth. Pain Med. 2017;42(6):741–750. doi: 10.1097/AAP.0000000000000639. [DOI] [PubMed] [Google Scholar]
- 45.Sweeney R.E., Clapp J.T., Arriaga A.F., Muralidharan M., Burson R.C., 2nd, Gordon E.K.B., Falk S.A., Baranov D.Y., Fleisher L.A. Understanding debriefing: a qualitative study of event reconstruction at an academic medical center. Acad. Med. 2020;95(7):1089–1097. doi: 10.1097/ACM.0000000000002999. [DOI] [PubMed] [Google Scholar]
- 46.McGaghie W.C., Issenberg S.B., Petrusa E.R., Scalese R.J. Revisiting 'A critical review of simulation-based medical education research: 2003-2009’. Med. Educ. 2016;50(10):986–991. doi: 10.1111/medu.12795. [DOI] [PubMed] [Google Scholar]
- 47.Flanagan J.L., De Souza N. Simulation in ophthalmic training. Asia Pac. J. Ophthalmol. (Phila). 2018;7(6):427–435. doi: 10.22608/APO.2018129. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data included in article/supplementary material/referenced in article.