Key Points
Question
What is the rate of regret and satisfaction with decision after 2 years or more following gender-affirming mastectomy?
Findings
In this cross-sectional study of 139 survey respondents who underwent gender-affirming mastectomy, the median satisfaction score was 5 on a 5-point scale, with higher scores indicating higher satisfaction. The median decisional regret score was 0 on a 100-point scale, with lower scores indicating lower levels of regret.
Meaning
This study’s findings indicate low patient-reported long-term rates of regret and high satisfaction with the decision to undergo gender-affirming mastectomy, although the need exists for condition-specific instruments to assess satisfaction with decision and decisional regret for gender-affirming surgery.
This cross-sectional study uses validated instruments to assess long-term decisional regret and satisfaction following gender-affirming mastectomy.
Abstract
Importance
There has been increasing legislative interest in regulating gender-affirming surgery, in part due to the concern about decisional regret. The regret rate following gender-affirming surgery is thought to be approximately 1%; however, previous studies relied heavily on ad hoc instruments.
Objective
To evaluate long-term decisional regret and satisfaction with decision using validated instruments following gender-affirming mastectomy.
Design, Setting, and Participants
For this cross-sectional study, a survey of patient-reported outcomes was sent between February 1 and July 31, 2022, to patients who had undergone gender-affirming mastectomy at a US tertiary referral center between January 1, 1990, and February 29, 2020.
Exposure
Decisional regret and satisfaction with decision to undergo gender-affirming mastectomy.
Main Outcomes and Measures
Long-term patient-reported outcomes, including the Holmes-Rovner Satisfaction With Decision scale, the Decision Regret Scale, and demographic characteristics, were collected. Additional information was collected via medical record review. Descriptive statistics and univariable analysis using Fisher exact and Wilcoxon rank sum tests were performed to compare responders and nonresponders.
Results
A total of 235 patients were deemed eligible for the study, and 139 responded (59.1% response rate). Median age at the time of surgery was 27.1 (IQR, 23.0-33.4) years for responders and 26.4 (IQR, 23.1-32.7) years for nonresponders. Nonresponders (n = 96) had a longer postoperative follow-up period than responders (median follow-up, 4.6 [IQR, 3.1-8.6] vs 3.6 [IQR, 2.7-5.3] years, respectively; P = .002). Nonresponders vs responders also had lower rates of depression (42 [44%] vs 94 [68%]; P < .001) and anxiety (42 [44%] vs 97 [70%]; P < .001). No responders or nonresponders requested or underwent a reversal procedure. The median Satisfaction With Decision Scale score was 5.0 (IQR, 5.0-5.0) on a 5-point scale, with higher scores noting higher satisfaction. The median Decision Regret Scale score was 0.0 (IQR, 0.0-0.0) on a 100-point scale, with lower scores noting lower levels of regret. A univariable regression analysis could not be performed to identify characteristics associated with low satisfaction with decision or high decisional regret due to the lack of variation in these responses.
Conclusions and Relevance
In this cross-sectional survey study, the results of validated survey instruments indicated low rates of decisional regret and high levels of satisfaction with decision following gender-affirming mastectomy. The lack of dissatisfaction and regret impeded the ability to perform a more complex statistical analysis, highlighting the need for condition-specific instruments to assess decisional regret and satisfaction with decision following gender-affirming surgery.
Introduction
An estimated 1.6% of US adults identify as transgender or nonbinary.1 For many transgender or nonbinary individuals, medical and surgical affirmation is essential to treating gender dysphoria and ensuring social acceptance. A common concern for patients, physicians, and policy makers is the potential irreversibility of gender-affirming therapies, particularly surgery, and the possibility of regret following these procedures. Regret is a complex feeling with many theorized constructs combining negative emotion with the evaluation of past decisions and can occur for multiple reasons.2 In the context of gender-affirming surgery, regret has previously been categorized into 3 etiologies, including social regret (eg, lack of social support), medical regret (eg, complications), and gender-related regret (eg, initially mistaken or later evolving transgender identity).3
Although regret is often discussed as a serious concern surrounding gender-affirming surgery, evidence that supports this claim is limited. A recent systematic review reported a regret rate of 1% following transfeminine and transmasculine procedures; however, this analysis relied on secondary coding of studies with a variety of measures and a broad range of follow-up periods from 0.8 to 9 years.4 Individual studies have also shown low rates of regret but have been limited by sample size and measurements that relied on chart review, ad hoc instruments, and use of changes in gender identity postoperatively as a proxy measure.4,5,6,7,8,9 While prospective studies have shown high short-term satisfaction with decision, follow-up time has remained limited, ranging from months to 1 year.10,11 The lack of data surrounding satisfaction with decision and decisional regret leaves clinicians unable to counsel patients on these important long-term outcome measures and legislators ill-equipped to draft evidence-based policy.
Gender-affirming mastectomy is the most common gender-affirming procedure in the US and is performed on transgender or nonbinary individuals who were assigned female sex at birth.12 We aimed to measure long-term satisfaction with decision and decisional regret using previously validated instruments in individuals who had gender-affirming mastectomy more than 2 years ago in order to inform patients considering gender-affirming mastectomy and policy makers regulating these operations.
Methods
Patient Recruitment
Participants were recruited from February 1 through July 31, 2022. Patients were eligible for this cross-sectional study if they underwent gender-affirming mastectomy at our institution (a tertiary referral center and the oldest continually operating gender-affirming surgical unit at a US academic center) between January 1, 1990, and February 29, 2020, were older than 18 years at the time of survey administration, and spoke English. All eligible patients were identified via medical record review. All patients met the World Professional Association for Transgender Health standards of care surgical requirements at the time of their operation prior to undergoing mastectomy.13 A 3-pronged communication approach (email, telephone, and mail) was used to recruit participants for the study. The study was approved by the University of Michigan’s institutional review board (HUM00196040). Written consent was obtained for respondents, and a Health Insurance Portability and Accountability Act waiver was given for medical record review of nonresponders. The study is in accordance with the American Association for Public Opinion Research (AAPOR) reporting guideline.
Survey Instruments
Participants were administered a 1-time survey either electronically or by mail. The instruments included ad hoc demographic information, the Holmes-Rovner Satisfaction With Decision scale, and the Decision Regret Scale. Satisfaction with decision was measured using the revised Holmes-Rovner Satisfaction With Decision scale.14 Originally published in 1996, this scale was validated for both postmenopausal hormone replacement therapy and antidepressant use in primary care patients.14,15 The revised tool consists of 4 statements rated on a 5-point Likert scale. Responses are averaged for a score of 1 to 5, with a higher score corresponding to higher satisfaction.16 The scale has high reliability (Cronbach α, 0.85-86) and has been applied to decisions regarding breast cancer, prostate cancer, and ovarian cancer.16,17
Decisional regret was assessed using the Decision Regret Scale.2 The scale contains 5 items that are rated on a 5-point Likert scale. Scores are converted to a 100-point scale, with higher scores corresponding to higher levels of regret. The instrument was validated originally in 4 patient populations: menopausal women considering hormone replacement therapy, men considering prostate cancer treatment, women considering breast cancer treatment, and women considering breast cancer adjuvant treatment.2,18 It has high reliability (Cronbach α, 0.81-0.92) and is well correlated with decision satisfaction, decisional conflict, and overall rated quality of life.2,18 The instrument has been used extensively for oncologic screening and treatment decisions as well as in nonclinical contexts.19,20,21,22
Clinical Data
Patient demographic characteristics, including age, recorded gender identity at last encounter in the medical record, hormonal therapy information, and preexisting medical and mental health comorbidities at the time of surgery, were collected from the electronic medical record for both responders and nonresponders. Surgical data were also collected, including the type of surgery performed (periareolar, double incision simple mastectomy, or another technique), complications, revision procedures, and any additional gender-affirming procedures. Furthermore, self-reported demographic, clinical, and surgical data were collected from respondents via an ad hoc survey. Specifically, self-reported sex assigned at birth; self-reported gender at the time of the surgery; and life partner status, education, and testosterone use at the time of the survey were collected. Self-reported race and ethnicity were recorded as a single item that asked, “How would you describe yourself?” Patients were able to select multiple classifications based on the US Office of Management and Budget race and ethnicity classification guidelines.23 This information was recorded for the purpose of examining possible differences in patient-reported outcomes.
Statistical Analysis
Descriptive statistics are presented for categorical data as counts and percentages and for continuous data as medians and IQRs. All univariable comparisons were performed using the Fisher exact test for categorical variables and Wilcoxon rank sum test for continuous variables. A 2-tailed P < .05 was considered statistically significant. Scales were scored in accordance with the previous literature.2,14 While previous cutoffs for both scales have been published, the clinical utility and rigor of establishing these cutoffs are not well described; thus, they were not used.16,22 Thirteen individuals had strong discordance among their satisfaction with decision and decisional regret scores (9 with complete discordance, 3 with a Satisfaction With Decision scale score of 4.75 and a Decision Regret Scale score of 100, and 1 with a Satisfaction With Decision scale score of 5.00 and a Decision Regret Scale score of 95). As these scales are reverse scored from each other, there was concern that these individuals did not read the directions to these instruments. The Satisfaction With Decision scale was ordered first, and these 13 participants were noted to have high satisfaction and high regret, suggesting a possible error due to item order. This concern is further compounded by the established high correlation between satisfaction with decision and decisional regret.2 For this reason, these individuals were excluded from the analysis. All analyses were performed using SAS, version 9.4 statistical software (SAS Institute Inc).
Results
Demographic Characteristics and Clinical Outcomes
A total of 235 patients were eligible for the study, of whom 139 responded (59% response rate). There were no significant differences in median age at the time of surgery (responders, 27.1 [IQR, 23.0-33.4] years; nonresponders, 26.4 [IQR, 23.1-32.7] years), surgical technique, complication rate within 30 days, or reoperation rate (Table 1). Nonresponders (n = 96) had a longer postoperative period than responders (median follow-up, 4.6 [IQR, 3.1-8.6] years vs 3.6 [IQR, 2.7-5.3] years; P = .002). Nonresponders also had lower rates than responders of diagnoses of depression (42 [44%] vs 94 [68%]; P < .001) and anxiety (42 [44%] vs 97 [70%]; P < .001) in the past medical history section of the medical record at the time of surgery (Table 1). However, the rates of medication use associated with anxiety and depression at the time of surgery did not differ between respondent groups (eTable 3 in Supplement 1). Approximately one-quarter of responders (35 [25%]) and nonresponders (22 [23%]) underwent an additional gender-affirming procedure following mastectomy (Table 1). No individuals in this study presented with or underwent a reversal procedure (ie, breast reconstruction) at our institution following mastectomy.
Table 1. Demographic Characteristics of Responders and Nonrespondersa.
| Characteristic | No. (%) | P valueb | |
|---|---|---|---|
| Responders (n = 139) | Nonresponders (n = 96) | ||
| Age at time of surgery, median (IQR), y | 27.1 (23.0-33.4) | 26.4 (23.1-32.7) | .65 |
| Time since surgery, median (IQR), y | 3.6 (2.7-5.3) | 4.6 (3.1-8.6) | .002 |
| Recorded gender at last medical encounterc | |||
| Male | 119 (86) | 86 (90) | NA |
| Female | 0 | 2 (2) | |
| Nonbinary | 12 (9) | 5 (5) | |
| Otherd | 7 (5) | 0 | |
| Multiple | 1 (1) | 1 (1) | |
| No gender identified | 0 | 2 (2) | |
| Mastectomy techniquee | |||
| Double incision | 128 (92) | 84 (88) | .26 |
| Periareolar | 8 (6) | 11 (11) | |
| Other | 3 (2) | 1 (1) | |
| Nipple technique | |||
| Free nipple graft | 126 (91) | 84 (88) | .55 |
| No procedure performed to nipples | 10 (7) | 11 (11) | |
| Other | 3 (2) | 1 (1) | |
| Complicationf within 30 d postoperatively | |||
| Yes | 33 (24) | 18 (19) | .42 |
| No | 106 (76) | 78 (81) | |
| Complication requiring reoperation or readmission | |||
| Yes | 9 (6) | 8 (1) | .62 |
| No | 130 (94) | 88 (92) | |
| Revision procedure | |||
| Yes | 30 (22) | 14 (15) | .18 |
| No | 108 (78) | 82 (85) | |
| Gender-affirming procedures prior to mastectomy | |||
| Yes | 13 (9) | 14 (14) | .22 |
| No | 126 (91) | 82 (86) | |
| Procedures prior to mastectomy | |||
| Vaginectomy or vulvectomyc | 1 (1) | 2 (2) | NA |
| Hysterectomy | 11 (8) | 9 (9) | .81 |
| Oophorectomy | 4 (3) | 6 (6) | .33 |
| Phalloplastyc | 0 | 1 (1) | NA |
| Facial masculinizationc | 1 (1) | 1 (1) | NA |
| Breast reductionc | 3 (2) | 1 (1) | NA |
| Additional gender-affirming procedures since the mastectomy | |||
| Yes | 35 (25) | 22 (23) | .76 |
| No | 104 (75) | 74 (77) | |
| Procedure following mastectomy | |||
| Vaginectomy or vulvectomy | 12 (9) | 8 (8) | >.99 |
| Hysterectomy | 30 (22) | 22 (23) | .87 |
| Oophorectomy | 24 (17) | 15 (16) | .86 |
| Metoidioplasty | 7 (5) | 5 (5) | >.99 |
| Phalloplasty | 5 (4) | 2 (2) | .70 |
| Scrotoplasty | 6 (4) | 4 (4) | >.99 |
| Other | 3 (2) | 2 (2) | >.99 |
| Charlson Comorbidity Index scorec | |||
| 0 | 113 (81) | 83 (86) | NA |
| 1 | 16 (12) | 9 (9) | |
| 2 | 6 (4) | 3 (3) | |
| 3 | 1 (1) | 1 (1) | |
| 5 | 2 (1) | 0 | |
| 7 | 1 (1) | 0 | |
| BMI at time of surgery, median (IQR) | 29.4 (25.5-35.9) | 28.9 (25.3-34.5) | .68 |
| Depressive disorder | |||
| Yes | 94 (68) | 42 (44) | <.001 |
| No | 45 (32) | 54 (56) | |
| Anxiety disorder | |||
| Yes | 97 (70) | 42 (44) | <.001 |
| No | 42 (30) | 54 (56) | |
| Trauma/stressor disorder | |||
| Yes | 3 (2) | 7 (7) | .10 |
| No | 136 (98) | 89 (93) | |
| Bipolar disorder | |||
| Yes | 14 (10) | 11 (11) | .83 |
| No | 125 (90) | 85 (89) | |
| Other mental health diagnosis | |||
| Yes | 19 (14) | 13 (14) | >.99 |
| No | 120 (86) | 83 (86) | |
Abbreviations: BMI, body mass index (measured as weight in kilograms divided by height in meters squared); NA, not available.
Data were collected from the medical record.
For categorical variables, P values are from Fisher exact tests. For continuous variables, P values are from Wilcoxon rank sum tests.
For characteristics with fewer than 5 individuals in a class or group, Fisher exact tests were not conducted.
Other gender identity included individuals who identified as genderqueer, demiboy, and agender as recorded in the medical record.
The test was run without class other due to small sample size (n <5).
Recorded complications included wound dehiscence, delayed wound healing, hematoma, seroma, nipple loss, and infection.
Postoperative time for respondents ranged from 2.0 to 23.6 years. Regarding self-reported gender identity at the time of survey completion, 88 (63%) identified as male, 17 (12%) identified as nonbinary, and 29 (21%) identified with multiple gender identities (Table 2). There were 27 individuals (19%) who had incongruent self-reported gender identity at the time of surgery compared with current self-reported gender identity. Thirteen self-reported as male at the time of surgery and currently self-report their identity as other, multiple, or no identified gender (eTable 1 in Supplement 1). The majority of the respondents in the cohort were White (105 [76%] vs 4 Asian [3%], 7 Black or African American [5%], 5 Hispanic or Latinx [4%], and 17 multiracial or other [12%]) and had a college degree or higher (Table 2). Well over three-quarters of respondents took testosterone at the time of surgery (123 of 138 [89%] [1 participant did not respond]) and were taking hormone therapy at the time of survey completion (117 of 139 [84%]) (Table 2). No participants self-reported reversal procedures (ie, breast reconstruction following mastectomy).
Table 2. Self-Reported Demographic Descriptive Statistics From 139 Survey Responders.
| Characteristic | No. (%) |
|---|---|
| Sex assigned at birth | |
| Female | 138 (99) |
| No sex identified | 1 (1) |
| Current gender identity | |
| Male | 88 (63) |
| Nonbinary | 17 (12) |
| Othera | 2 (1) |
| Multiple | 29 (21) |
| No gender identified | 3 (2) |
| Race | |
| Asian | 4 (3) |
| Black or African American | 7 (5) |
| Hispanic or Latinx | 5 (4) |
| White | 105 (76) |
| Multiracial | 15 (11) |
| Otherb | 2 (1) |
| Current life partner status | |
| Single | 50 (36) |
| Married | 39 (28) |
| Significant other | 39 (28) |
| Separated or divorced | 9 (7) |
| Widowed | 1 (1) |
| Highest level of education | |
| High school | 45 (33) |
| College | 54 (39) |
| Graduate degree | 39 (28) |
| Taking testosterone at the time of the mastectomy | |
| Yes | 123 (89) |
| No | 15 (11) |
| Taking testosterone currently | |
| Yes | 117 (84) |
| No | 22 (16) |
Other gender identity included individuals reporting transgender and “nothing but confused at this point.”
Individuals who selected other reported identifying as multiracial.
Satisfaction With Decision and Decisional Regret
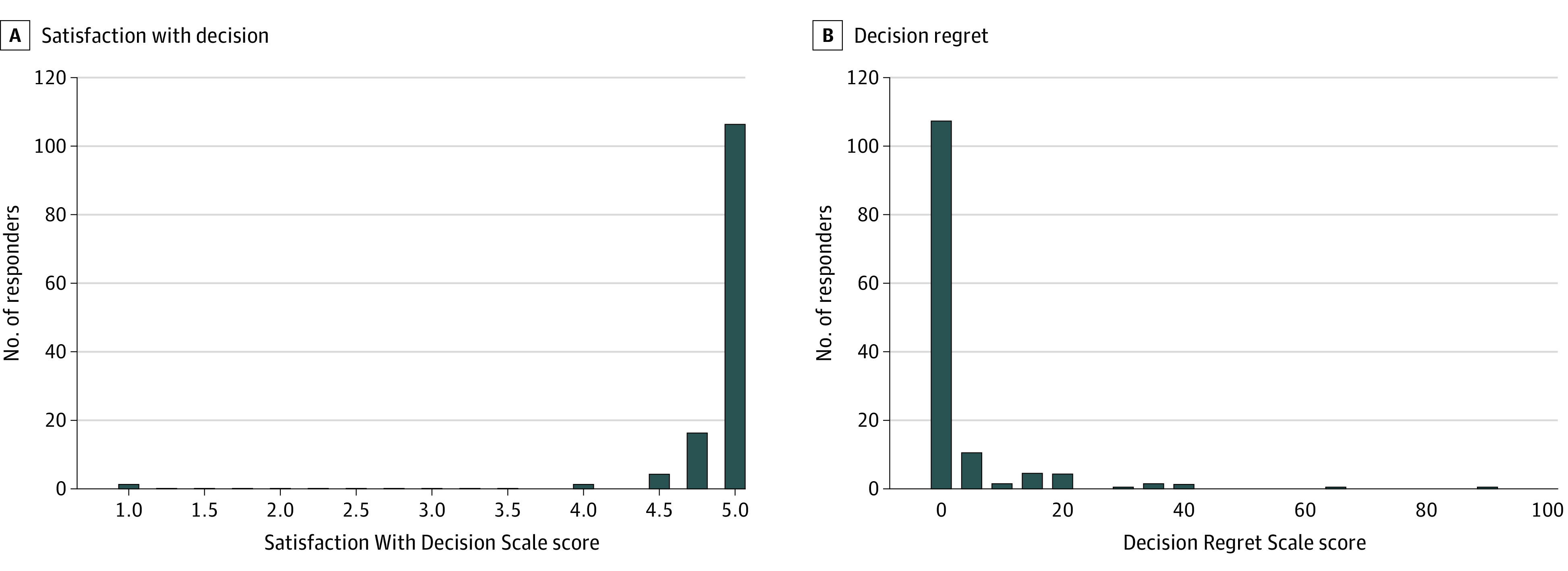
Regarding satisfaction with decision, the median Holmes-Rovner Satisfaction With Decision score was 5.0 (IQR, 5.0-5.0) (mean [SD], 4.8 [0.6]) (Table 3; Figure). Regarding decisional regret, the median Decision Regret Scale score was 0.0 (IQR, 0.0-0.0) (mean [SD], 4.2 [12.1]) (Table 3; Figure). Individuals who had incongruent gender identities at the time of surgery and survey administration (n = 27) had a median Satisfaction With Decision score of 5.0 (IQR, 5.0-5.0) and decisional regret score of 0 (IQR, 0.0-5.0) (eTable 2 in Supplement 1).
Table 3. Satisfaction With Decision and Decisional Regret.
| Survey instrument | Score (n = 138) |
|---|---|
| Satisfaction With Decision Scale score (n = 139)a | |
| Mean (SD) | 4.8 (0.6) |
| Median (IQR) | 5.0 (5.0-5.0) |
| Decision Regret Scale score (n = 138)b | |
| Mean (SD) | 4.2 (12.1) |
| Median (IQR) | 0.0 (0.0-0.0) |
A 5-point scale, with higher scores noting higher satisfaction.
A 100-point scale, with lower scores noting lower levels of regret.
Figure. Distribution of Satisfaction With Decision and Decision Regret Scores.
Discussion
In this cross-sectional survey study of participants who underwent gender-affirming mastectomy 2.0 to 23.6 years ago, respondents had a high level of satisfaction with their decision and low rates of decisional regret. The median Satisfaction With Decision score was 5 on a 5-point scale, and the median decisional regret score was 0 on a 100-point scale. This extremely low level of regret and dissatisfaction and lack of variance in scores impeded the ability to determine meaningful associations among these results, clinical outcomes, and demographic information.
The results are overwhelmingly positive compared with other medical and nonmedical decisions. Participants had a mean (SD) decisional regret score of 4.2 (12.1) on a 100-point scale. In a systematic review of 44 studies of multiple conditions using the Decision Regret Scale, including breast cancer treatment and reconstruction, only 1 study of urinary incontinence had a lower level of decisional regret (mean score, 2.5).22 With regard to satisfaction with decision, the mean (SD) score was 4.8 (0.6) on a 5-point scale, which is higher than reported scores of mastectomy with reconstruction (mean, 3.97).17 Placed in context with other procedures assessed by the same instruments, there was low long-term decisional regret and high satisfaction with decision following gender-affirming mastectomy. Beyond the scales, approximately one-quarter of both responders and nonresponders had an additional gender-affirming procedure following mastectomy. These results suggest sustained intent and consistency in decision-making.
Previous qualitative work suggested that the notion of regret, requests for reversal, and changes in gender identity have a nuanced, diverse association with one another, and patients presenting with concerns in any of these domains deserve multidisciplinary care.5,24 Our reversal rate was 0% and consistent with recent reports of 0.3% in a larger single-center cohort.5 With regard to changes in gender identity, 19% of our cohort had a different self-reported gender identity at the time of surgery compared with the time of survey administration. This finding could represent continued gender exploration or could additionally represent the pressures nonbinary patients face to conform to gender binaries in medical settings.25 Individuals with different gender identities had instrument scores similar to those of individuals with concordant gender identities (eTable 2 in Supplement 1). These findings support the notion that ongoing gender exploration should not be used as a proxy measure for regret.24 We did not observe any individuals presenting for surgical reversal, and individuals with changing gender identities had high levels of satisfaction and low regret.
While our findings show substantially low levels of decisional regret, they suggest the need for instruments calibrated specifically to the experience of undergoing gender-affirming surgery. Although a strength of this study is the use of validated instruments that can be compared with other surgical conditions, our findings suggest the need for condition-specific instruments and validation in the transgender population. Floor and ceiling effects limited our ability to perform statistical analysis to establish cutoffs specific to our cohort and identify characteristics associated with regret and satisfaction that could aid patient counseling in the future. While there are established cutoffs for both instruments, the establishment of said cutoffs is not well described, and the actual clinical utility is not clear.16,22 Furthermore, these instruments do not capture the dimensions of regret unique to gender-affirming surgery. It is not known whether the individuals expressing dissatisfaction and regret in our cohort were experiencing these in relation to gender identity or experiencing other forms of regret known to follow gender-affirming surgery, such as social regret associated with increased stigma and discrimination or medical regret associated with complications and outcomes.3 This finding supports the urgent need for condition-specific instruments for gender-affirming surgery, which is currently under development by the GENDER-Q team.25
Limitations
This study had several limitations. Although this study includes robust long-term data surrounding regret and satisfaction with decision following gender-affirming mastectomy, the cross-sectional nature of this study and variation in follow-up time among participants pose the possibility of recall bias. The association of time elapsed with regret specifically is unclear, with systematic review suggesting that regret may increase over time.22 There were also 13 individuals with completely discordant regret and satisfaction scores, which may represent difficulty with following survey instructions, as these instruments are reverse coded from each other. These individuals were not included in the analysis given this concern. Unaccounted responder bias may also skew results. Interestingly, the only significant differences between responders and nonresponders were time since surgery and the rates of depression and anxiety diagnoses at the time of surgery in the medical record, with responders having higher diagnosis rates. While the rates of diagnoses differed between groups, the rates of medication use associated with anxiety and depression at the time of surgery did not (eTable 3 in Supplement 1). This discrepancy suggests that variation in documentation may contribute to this difference between responders and nonresponders. Furthermore, we were unable to determine procedures performed outside of our institution, which might have led to an underestimation of procedures following mastectomy. Clinician-level factors, such as patient counseling, were not collected and have been shown to be associated with regret and satisfaction with decision.16,17,22 Finally, participants were recruited from a single academic center with a uniform approval process to undergo surgery and may not be representative of other sites. A multicenter study with multiple practice types is needed to ensure the generalizability of these results and to examine subpopulations.
Conclusions
In this cross-sectional study of individuals who underwent gender-affirming mastectomy 2.0 to 23.6 years ago, we observed long-term low levels of decisional regret and high satisfaction with decision using available validated instruments. The lack of variation in scores impeded the ability to perform a statistical analysis to establish characteristics associated with satisfaction with decision and regret. There were no individuals who underwent reversal procedures. While prospective, multicenter work is needed, these results are consistent with previous ad hoc studies and affirm the overwhelmingly low levels of regret following gender-affirming surgery.
eTable 1. Cross Tabulation of Self-Reported Current Gender and Gender at the Time of Surgery
eTable 2. Satisfaction With Decision and Decision Regret Scale Scores by Congruence of Gender at the Time of Surgery vs the Time of Survey Administration
eTable 3. Mental Health–Associated Medication Use at the Time of Surgery
Data Sharing Statement
References
- 1.Brown A. About 5% of young adults in the U.S. say their gender is different from their sex assigned at birth. Pew Research Center . June 7, 2022. Accessed December 9, 2022. https://www.pewresearch.org/fact-tank/2022/06/07/about-5-of-young-adults-in-the-u-s-say-their-gender-is-different-from-their-sex-assigned-at-birth/
- 2.Brehaut JC, O’Connor AM, Wood TJ, et al. Validation of a decision regret scale. Med Decis Making. 2003;23(4):281-292. doi: 10.1177/0272989X03256005 [DOI] [PubMed] [Google Scholar]
- 3.Narayan SK, Hontscharuk R, Danker S, et al. Guiding the conversation-types of regret after gender-affirming surgery and their associated etiologies. Ann Transl Med. 2021;9(7):605. doi: 10.21037/atm-20-6204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bustos VP, Bustos SS, Mascaro A, et al. Regret after gender-affirmation surgery: a systematic review and meta-analysis of prevalence. Plast Reconstr Surg Glob Open. 2021;9(3):e3477. doi: 10.1097/GOX.0000000000003477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jedrzejewski BY, Marsiglio MC, Guerriero J, Penkin A, Berli JU; OHSU Transgender Health Program “Regret and Request for Reversal” Workgroup . Regret after gender affirming surgery—a multidisciplinary approach to a multifaceted patient experience. Plast Reconstr Surg. 2023;152(1):206-214. doi: 10.1097/PRS.0000000000010243 [DOI] [PubMed] [Google Scholar]
- 6.Wiepjes CM, Nota NM, de Blok CJM, et al. The Amsterdam Cohort of Gender Dysphoria Study (1972-2015): trends in prevalence, treatment, and regrets. J Sex Med. 2018;15(4):582-590. doi: 10.1016/j.jsxm.2018.01.016 [DOI] [PubMed] [Google Scholar]
- 7.Pfafflin F. Regrets after sex reassignment surgery. J Psychol Human Sex. 1993;5(4):69-85. doi: 10.1300/J056v05n04_05 [DOI] [Google Scholar]
- 8.Landén M, Wålinder J, Hambert G, Lundström B. Factors predictive of regret in sex reassignment. Acta Psychiatr Scand. 1998;97(4):284-289. doi: 10.1111/j.1600-0447.1998.tb10001.x [DOI] [PubMed] [Google Scholar]
- 9.Johansson A, Sundbom E, Höjerback T, Bodlund O. A five-year follow-up study of Swedish adults with gender identity disorder. Arch Sex Behav. 2010;39(6):1429-1437. doi: 10.1007/s10508-009-9551-1 [DOI] [PubMed] [Google Scholar]
- 10.Agarwal CA, Scheefer MF, Wright LN, Walzer NK, Rivera A. Quality of life improvement after chest wall masculinization in female-to-male transgender patients: a prospective study using the BREAST-Q and Body Uneasiness Test. J Plast Reconstr Aesthet Surg. 2018;71(5):651-657. doi: 10.1016/j.bjps.2018.01.003 [DOI] [PubMed] [Google Scholar]
- 11.Lane M, Kirsch MJ, Sluiter EC, et al. Gender affirming mastectomy improves quality of life in transmasculine patients: a single-center prospective study. Ann Surg. 2021;277(3):e725-e729. doi: 10.1097/SLA.0000000000005158 [DOI] [PubMed] [Google Scholar]
- 12.Plastic surgery statistics report. American Society of Plastic Surgeons . 2021. Accessed November 1, 2021. https://www.plasticsurgery.org/documents/News/Statistics/2020/plastic-surgery-statistics-full-report-2020.pdf
- 13.Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgenderism. 2012;13(4):165-232. doi: 10.1080/15532739.2011.700873 [DOI] [Google Scholar]
- 14.Holmes-Rovner M, Kroll J, Schmitt N, et al. Patient satisfaction with health care decisions: the satisfaction with decision scale. Med Decis Making. 1996;16(1):58-64. doi: 10.1177/0272989X9601600114 [DOI] [PubMed] [Google Scholar]
- 15.Wills CE, Holmes-Rovner M. Preliminary validation of the Satisfaction With Decision scale with depressed primary care patients. Health Expect. 2003;6(2):149-159. doi: 10.1046/j.1369-6513.2003.00220.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Waljee JF, Hu ES, Newman LA, Alderman AK. Correlates of patient satisfaction and provider trust after breast-conserving surgery. Cancer. 2008;112(8):1679-1687. doi: 10.1002/cncr.23351 [DOI] [PubMed] [Google Scholar]
- 17.Lantz PM, Janz NK, Fagerlin A, et al. Satisfaction with surgery outcomes and the decision process in a population-based sample of women with breast cancer. Health Serv Res. 2005;40(3):745-767. doi: 10.1111/j.1475-6773.2005.00383.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Calderon C, Ferrando PJ, Lorenzo-Seva U, et al. Validity and reliability of the Decision Regret Scale in cancer patients receiving adjuvant chemotherapy. J Pain Symptom Manage. 2019;57(4):828-834. doi: 10.1016/j.jpainsymman.2018.11.017 [DOI] [PubMed] [Google Scholar]
- 19.Violette PD, Agoritsas T, Alexander P, et al. Decision aids for localized prostate cancer treatment choice: systematic review and meta-analysis. CA Cancer J Clin. 2015;65(3):239-251. doi: 10.3322/caac.21272 [DOI] [PubMed] [Google Scholar]
- 20.Lin SQ, Su CM, Wu HC, Chou YY, Yen YC, Tam KW. Effect of patient decision aids on decisional conflict and regret associated with breast cancer surgery: a randomized controlled trial. Breast Cancer. 2022;29(5):880-888. doi: 10.1007/s12282-022-01370-0 [DOI] [PubMed] [Google Scholar]
- 21.Liu J, Hunter S, Zhu J, Lee RL, Chan SW. Decision regret regarding treatments among women with early-stage breast cancer: a systematic review protocol. BMJ Open. 2022;12(3):e058425. doi: 10.1136/bmjopen-2021-058425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Becerra Pérez MM, Menear M, Brehaut JC, Légaré F. Extent and predictors of decision regret about health care decisions: a systematic review. Med Decis Making. 2016;36(6):777-790. doi: 10.1177/0272989X16636113 [DOI] [PubMed] [Google Scholar]
- 23.Office of Management and Budget. Revisions to the standards for the classification of federal data on race and ethnicity. Fed Reg. 1997;62(210):58782-58790. [Google Scholar]
- 24.MacKinnon KR, Kia H, Salway T, et al. Health care experiences of patients discontinuing or reversing prior gender-affirming treatments. JAMA Netw Open. 2022;5(7):e2224717. doi: 10.1001/jamanetworkopen.2022.24717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bindman J, Ngo A, Zamudio-Haas S, Sevelius J. Health care experiences of patients with nonbinary gender identities. Transgend Health. 2022;7(5):423-429. doi: 10.1089/trgh.2021.0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Cross Tabulation of Self-Reported Current Gender and Gender at the Time of Surgery
eTable 2. Satisfaction With Decision and Decision Regret Scale Scores by Congruence of Gender at the Time of Surgery vs the Time of Survey Administration
eTable 3. Mental Health–Associated Medication Use at the Time of Surgery
Data Sharing Statement


