Key Points
Question
Does exercising for 12 weeks using a suite of exercise applications (apps) affect health care workers’ depressive symptoms reported biweekly over the same time course?
Findings
In this randomized clinical trial including 288 health care workers, analyses revealed significant decreases in depressive symptoms among those randomized to the exercise condition compared with the wait-listed control condition. App use declined over the 12 weeks, however; by the end of the trial, only 33 intervention participants (23%) were using the apps regularly.
Meaning
Although the intervention reduced depressive symptoms among health care workers, adherence was low toward the end of the trial.
This randomized clinical trial investigates whether a 12-week application-based exercise intervention has an effect on depressive symptoms, burnout, and absenteeism among health care workers.
Abstract
Importance
During the COVID-19 pandemic, health care workers (HCWs) reported a significant decline in their mental health. One potential health behavior intervention that has been shown to be effective for improving mental health is exercise, which may be facilitated by taking advantage of mobile application (app) technologies.
Objective
To determine the extent to which a 12-week app-based exercise intervention can reduce depressive symptoms, burnout, and absenteeism in HCWs, compared with a wait list control condition.
Design, Setting, and Participants
A 2-group randomized clinical trial was conducted, with participants screened from April 6 to July 4, 2022. Participants were recruited from an urban health care organization in British Columbia, Canada. Participants completed measures before randomization and every 2 weeks thereafter.
Interventions
Exercise condition participants were asked to complete four 20-minute sessions per week using a suite of body weight interval training, yoga, barre, and running apps. Wait-listed control participants received the apps at the end of the trial.
Main Outcomes and Measures
The primary outcome consisted of the between-group difference in depressive symptoms measured with the 10-item Center for Epidemiological Studies Depression Scale. The secondary outcomes corresponded to 3 subfacets of burnout (cynicism, emotional exhaustion, and professional efficacy) and absenteeism. Intention-to-treat analyses were completed with multilevel structural equation modeling, and Feingold effect sizes (ES) were estimated every 2 weeks.
Results
A total of 288 participants (mean [SD] age, 41.0 [10.8] years; 246 [85.4%] women) were randomized to either exercise (n = 142) or wait list control (n = 146) conditions. Results revealed that ESs for depressive symptoms were in the small to medium range by trial’s end (week 12, −0.41 [95% CI, −0.69 to −0.13]). Significant and consistent treatment effects were revealed for 2 facets of burnout, namely cynicism (week 12 ES, −0.33 [95% CI, −0.53 to −0.13]) and emotional exhaustion (week 12 ES, −0.39 [95% CI, −0.64 to −0.14]), as well as absenteeism (r = 0.15 [95% CI, 0.03-0.26]). Adherence to the 80 minutes per week of exercise decreased from 78 (54.9%) to 33 (23.2%) participants between weeks 2 and 12.
Conclusions and Relevance
Although exercise was able to reduce depressive symptoms among HCWs, adherence was low toward the end of the trial. Optimizing adherence to exercise programming represents an important challenge to help maintain improvements in mental health among HCWs.
Trial Registration
ClinicalTrials.gov Identifier: NCT05271006
Introduction
The SARS-CoV-2 (COVID-19) pandemic has had devastating effects on mental health across the globe, with rates of depressive and anxiety symptoms doubling or even tripling in some countries compared with prepandemic levels.1 A segment of society particularly affected by the pandemic is health care workers (HCWs), including those directly involved in direct patient care (eg, nurses, physicians, paramedics, and allied health care professionals such as physical therapists) as well as those in supportive roles (eg, administrators, housekeeping, and security staff) who may be potentially exposed to the SARS-CoV-2 virus in health care settings.2 Since the start of the pandemic, HCWs have faced notable uncertainty, with increased risk of exposure to the virus compared with the general population, expanding job demands, rapidly changing protocols, and fears of spreading the virus to family members.3 Compounding these effects was the growing tension with many in the general population who were denying the severity of the pandemic and showing overt aggression toward hospital staff.4 Unsurprisingly, HCWs’ mental health problems are currently at high rates across the globe, leading to increased burnout5 and high staff absenteeism and turnover.6
As a result of the wide and growing effects of the pandemic on HCWs, managing this mental health crisis is now a global imperative.7,8 Attention to occupational influences (eg, work hours, contractual demands) is necessary to protect the workforce from loss of experienced HCWs. There is also a pressing need to deliver innovative and scalable interventions that can directly mitigate depleted mental health among HCWs,9 because without such interventions, HCWs’ mental health and intention to leave their professions will worsen to a devastating level, causing a potentially irretrievable strain on our health care systems.
A literature review of mental health initiatives from across the globe that were developed within health care institutions and delivered to their employees to address the pandemic’s mental health impact identified 9 such programs, all of which can be categorized as psychoeducational (eg, online information for stress reduction, behavior change) or psychosocial (eg, “talk therapy,” crisis lines)10 in nature. Behavioral approaches, including exercise, are well-evidenced as primary stand-alone strategies for the prevention and treatment of depressive symptoms.11 At the start of the COVID-19 pandemic, Puterman et al12 demonstrated significant reductions in depressive symptoms with at-home, application (app)-based exercise over a 6-week period in a sample of 334 Canadian participants. Whether these substantive mental health changes of app-based, at-home exercise can extend to HCWs as they manage the repercussions of the pandemic remains unknown.
The present efficacy trial was derived from a collaboration between university researchers and regional health care leadership in a large urban center. Health care workers with low levels of activity were invited to participate in a 12-week, at-home, app-based exercise intervention. The primary aim of the randomized clinical trial (RCT) was to investigate whether exercising for 12 weeks at home using a suite of apps has an effect on HCWs’ depressive symptoms compared with those who do not exercise, reported biweekly over the same time course. Secondary outcomes relevant to health care systems, specifically 3 subfacets of burnout (cynicism, emotional exhaustion, and professional efficacy) and absenteeism, were also tracked biweekly. We hypothesized that exercising for 12 weeks would lead to significant reductions in depressive symptoms, burnout, and absenteeism among HCWs compared with those who did not.
Methods
Trial Design
The study was a 2-group parallel RCT, with participants allocated randomly to an exercise or a wait list control condition. Participants were recruited from 10 acute and long-term care hospitals within the Providence Health Care Network in Vancouver, British Columbia, Canada. Providence Health Care employs or contracts approximately 10 000 HCWs. Ethics approval was provided by the University of British Columbia’s Behavioral Research and Providence Health Care’s Institutional Ethics Boards, and all participants provided written informed consent. The full trial protocol, sample size calculations, and statistical analysis plan are available in Supplement 1. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
Participants
Health care workers with low activity levels who were older than 18 years, were working full or part time as employees or contractors at Providence Health Care, and had access to the internet via a mobile device or computer were eligible to participate. Low activity level was determined with the Stanford Leisure-Time Categorical Activity Item.13 Health care workers were cleared for exercise with the Physical Activity Readiness Questionnaire for Everyone, with the Physical Activity Readiness Medical Examination,14 or by one of our team’s Canadian Society for Exercise Physiology–certified clinical exercise physiologists (A.M.-D. and S.H.). If eligible and interested, HCWs completed the consent form using the Qualtrics XM platform (Qualtrics XM). Following consent and prior to randomization, participants completed our baseline survey on Qualtrics (screening materials and procedures are provided in Supplement 1).
Randomization
One coauthor (B.A.H.) completed randomization with stratified blocks of 4. One of 2 members of the research team (V.G.B. and B.L.H.), with no participant contact, assigned participants to either condition via random number generation through the R function in Excel, version 16.74 Microsoft 365 (Microsoft Corporation).
Intervention
Participants assigned to the exercise condition immediately received a free 1-year subscription to the Down Dog suite of apps (Yoga Buddhi Co), including body weight interval training, yoga, running, and barre.15 A study team member allocated anonymized identification numbers to participants and preregistered them on the Down Dog platform. Consistent with the previous trial by Puterman et al,12 participants were asked to complete a minimum of four 20-minute sessions/wk (total 80 min/wk) for 12 weeks at home or any convenient location. Participants could use any of the Down Dog apps and were not required to use all of them. Participants assigned to the wait list control condition were asked to maintain current physical activity levels. Following completion of the trial, they received a free 1-year subscription to the Down Dog apps.
Measures and Outcome
Outcomes were measured at baseline (prerandomization) and then biweekly after randomization, until the end of the 12-week trial. The primary outcome measure was the between-group difference in depressive symptoms every 2 weeks as measured using the 10-item Center for Epidemiological Studies Depression Scale.16 Secondary outcomes were burnout symptoms (subscales: cynicism, emotional exhaustion, professional efficacy) as measured using the 16-item Maslach Burnout Inventory17 and absenteeism as measured with the question “In the past 2 weeks, how many days did you call in sick when you were scheduled to work?” Scoring information and reliabilities of the measures can be found in the eMethods in Supplement 2. Adherence was measured by summing the weekly minutes of app use across the 4 apps.
Statistical Analysis
We used Optimal Design Software, version 3.0,18 to detect small (δ = 0.30), small to medium (δ = 0.40), and medium (δ = 0.50) effect sizes (ESs) with power set at 0.80 and α set at .05 for a 7–time point repeated-measures design. For the small ES, 367 participants would be required across the 2 groups; for the small to medium ESs, 203 participants; and for the medium ES, 131 participants. To account for 20% attrition and the 10 centers, 560 HCWs would be required for enrollment in the trial for the small ES; 366, for the small to medium ES; and 276, for the medium ES.19,20 We decided on the largest sample size, 560 participants, to ensure sufficient power to detect the full range of small to medium treatment ESs.
Means (SDs) or counts and percentages were computed for all continuous or categorical demographic variables. Random forest–based imputation21 was used for partially completed weekly questionnaires. Imputation was not performed for cases where participants completed none of the instrument items for a given week. All randomized participants were included in the analyses based on intention-to-treat principles for depressive symptoms and measures derived from the burnout scales.22 Quadratic growth models estimate a latent intercept, slope, and curve for each outcome, with experimental condition regressed on the latent estimates to quantify the treatment effect. This framework is similar to traditional multilevel regression models using robust maximum likelihood estimation23 that can account for missing data when missing fully at random or at random. Biweekly ESs were computed based on the Feingold24 approach, equivalent to Cohen d. For absenteeism, conditions were compared using a Wilcoxon rank sum test because number of weeks with reported sick days was skewed. Wilcoxon rank sum ES is an r score,25 interpreted similarly to a Pearson correlation coefficient. The software description and code are provided in the eMethods in Supplement 2. Two-sided P < .05 indicated statistical significance.
Changes to the Trial
Recruitment ended on July 4, 2022 (details are provided in Supplement 1). In brief, while there was rapid uptake at the start of the trial, interest slowed in June 2022 as the weather changed. Additionally, because most participants were recruited from only 1 site, the requirement to account for nesting within the 10 sites was removed. As there were no previous efficacy data to sufficiently gauge the size of the predicted treatment effect in the context of a pandemic in HCWs, small to medium (δ = 0.40) or medium (δ = 0.50) effects could have been expected, consistent with previous meta-analyses with general and clinical populations.26 Acknowledging that we risked completing an insufficiently powered trial to detect small effects but wanting to disseminate potentially important findings, we determined it would still be well powered to detect small to medium and medium effects with the recruited sample.
Results
Participants
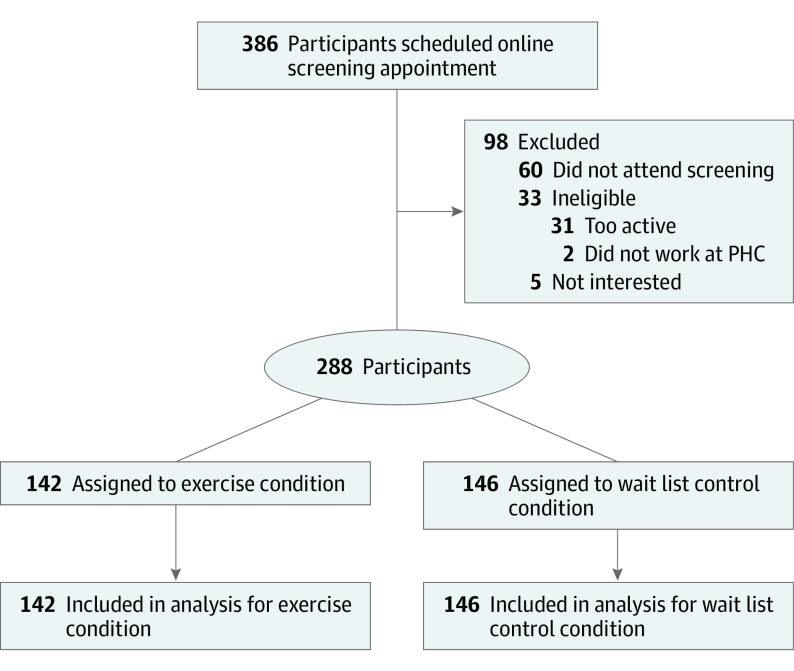
Between April 6, 2022, and July 4, 2022, 386 potential participants indicated an interest in the study through the trial website and 326 completed screening. Of these, 288 were eligible and were randomized to either the exercise (142 [49.3%]) or the wait list control (146 [50.7%]) condition. The CONSORT flow diagram is shown in Figure 1. A total of 246 participants (85.4%) were women, 36 (12.5%) were men, and 6 (2.1%) were nonbinary, preferred not to answer, or missing. The mean (SD) age was 41.0 (10.8) years. In terms of self-reported race and ethnicity, 55 participants (19.1%) identified as Chinese; 24 (8.3%), as Filipino; 9 (3.1%), as Latin American; 33 (11.5%), as South Asian; 5 (1.7%), as Southeast Asian; 107 (37.2%), as White; 24 (8.3%), as multiple races or ethnicities; and 26 (10.1%), as other race or ethnicity (including Arab, Armenian, Black, Central Asian–Kazakhstani, East European, European, Indigenous, Indian, Italian, Japanese, Korean, settler descendant, seventh-generation Canadian, South American, Taiwanese, Ukrainian, and West Asian). Table 1 presents descriptive statistics for sociodemographic factors, counts of participants from the recruitment sites, and mean baseline (prerandomization) depressive symptoms, burnout scores, and sick days.
Figure 1. Study Flow Diagram.
PHC indicates Providence Health Care.
Table 1. Baseline Participant Characteristics and Outcome Information.
| Characteristic | Participant groupa | |
|---|---|---|
| Exercise condition (n = 142) | Wait list control condition (n = 146) | |
| Age, mean (SD), y | 40.5 (11.3) | 42.2 (10.2) |
| Sex | ||
| Women | 120 (84.5) | 126 (86.3) |
| Men | 19 (13.4) | 17 (11.6) |
| Other (nonbinary, preferred not to answer, or missing)b | 3 (2.1) | 3 (2.1) |
| Transgender life experience | ||
| None | 140 (98.6) | 142 (97.3) |
| Other (lived experience, preferred not to answer, or missing)b | 2 (1.4) | 4 (2.7) |
| Marital status | ||
| Married | 63 (44.4) | 72 (49.3) |
| Common law | 28 (19.7) | 20 (13.7) |
| Single | 33 (23.2) | 31 (21.2) |
| Other (widowed, separated, or divorced)b | 12 (8.5) | 17 (11.6) |
| Preferred not to answer or missing | 6 (4.2) | 6 (4.1) |
| Indigenous status | ||
| Does not identify as Indigenous | 139 (97.9) | 142 (97.3) |
| Other (identifies as Indigenous, preferred not to answer, or missing)b | 3 (2.1) | 4 (2.7) |
| Disability status | ||
| Does not identify as a person with a disability | 139 (97.9) | 142 (97.3) |
| Other (identifies as a person with a disability, preferred not to answer, or missing)b | 3 (2.1) | 4 (2.7) |
| Visible member of racial or ethnic minority groupc | ||
| Identifies as a member of a visible minority group | 66 (46.5) | 50 (34.2) |
| Does not identify as a member of a visible minority group | 71 (50.0) | 89 (61.0) |
| Preferred not to answer or missing | 5 (3.5) | 7 (4.8) |
| Educational attainment | ||
| High school or less | 0 | 2 (1.4) |
| Trade certificate or diploma | 6 (4.2) | 9 (6.2) |
| College, CEGEP, or other nonuniversity certificate or diploma | 16 (11.3) | 16 (11.0) |
| University certificate or diploma below the bachelor’s level | 10 (7.0) | 10 (6.8) |
| Bachelor’s degree | 63 (44.4) | 64 (43.8) |
| University certificate, diploma, degree above the bachelor’s level | 47 (33.1) | 43 (29.5) |
| Preferred not to answer or missing | 0 | 2 (1.4) |
| Household income, CAD$d | ||
| 0-40 000 | 2 (1.4) | 4 (2.7) |
| 40 001-80 000 | 22 (15.5) | 27 (18.5) |
| 80 001-120 000 | 35 (24.6) | 37 (25.3) |
| 120 001-160 000 | 21 (14.8) | 26 (17.8) |
| 160 001-200 000 | 27 (19.0) | 23 (15.8) |
| 200 001-240 000 | 9 (6.3) | 9 (6.2) |
| >240 000 | 10 (7.0) | 10 (6.8) |
| Preferred not to answer or missing | 16 (11.3) | 10 (6.8) |
| Race or ethnicity | ||
| Chinese | 29 (20.4) | 26 (17.8) |
| Filipino | 15 (10.6) | 9 (6.2) |
| Latin American | 3 (1.4) | 6 (4.1) |
| South Asian | 21 (14.8) | 12 (8.2) |
| Southeast Asian | 3 (1.4) | 2 (1.4) |
| White | 47 (33.1) | 60 (41.1) |
| Identify as ≥2 | 12 (8.4) | 14 (9.6) |
| Other ethnicitye | 12 (8.4) | 14 (9.6) |
| Preferred not to answer or missing | 2 (1.4) | 3 (2.1) |
| Employment status | ||
| Working full time | 114 (80.3) | 115 (78.8) |
| Working part time | 26 (18.3) | 28 (19.2) |
| Maternity leave or sick leave | 1 (0.7) | 2 (1.4) |
| Preferred not to answer or missing | 1 (0.7) | 1 (0.7) |
| Role | ||
| Nurses (registered nurse, registered psychiatric nurse, licensed practice nurse, nurse practitioner) | 58 (40.8) | 64 (43.8) |
| Allied health professional | 39 (27.5) | 41 (28.1) |
| Administrative staff | 38 (26.8) | 30 (20.5) |
| Pharmacist | 5 (3.5) | 6 (4.1) |
| Physician or surgeon | 2 (1.4) | 3 (2.1) |
| Preferred not to answer or missing | 0 | 2 (1.4) |
| Primary outcome of depressive symptoms, baseline CES-D score, mean (SD)f | 21.3 (5.0) | 20.5 (5.4) |
| Secondary outcomes | ||
| Burnout symptoms, baseline MBI score, mean (SD) | ||
| Cynicismg | 18.9 (8.0) | 17.1 (7.7) |
| Emotional exhaustionh | 25.0 (7.3) | 23.1 (7.8) |
| Professional efficacyi | 33.1 (5.8) | 33.5 (5.7) |
| No. of sick days at baseline, mean (SD) | 0.23 (0.42) | 0.22 (0.41) |
Abbreviations: CEGEP, Collège d’Enseignement General et Professionnel; CES-D, Center for Epidemiologic Studies Depression Scale; MBI, Maslach Burnout Inventory.
Unless otherwise indicated, data are expressed as No. (%) of participants. Percentages have been rounded and may not total 100.
Other categories were created to prevent identifiability.
Statistics Canada defines visible minority individuals as “persons, other than aboriginal peoples, who are non-Caucasian in race or non-white in colour.”27
Average 2022 CAD$ to US$ exchange rate: $0.74.
Includes Arab, Armenian, Black, Central Asian–Kazakhstan, East European, European, German and Japanese, Indian, Italian, Jewish, Korean, settler descendant, seventh-generation Canadian, South American, Taiwanese, Ukrainian, and West Asian.
Scores range from 0 to 30, with higher scores indicating more depressive symptoms.
Scores range from 0 to 30, with higher scores indicating higher cynicism.
Scores range from 0 to 30, with higher scores indicating higher emotional exhaustion.
Scores range from 0 to 36, with higher scores indicating higher professional efficacy.
Missingness of Data
The number of biweekly surveys with partial missingness (where participants missed at least 1, but not all, responses to items in an instrument) and complete missingness of all instrument items are presented in eTable 1 in Supplement 2. The partial item missingness was less than 1% across the 7 biweekly assessments. Complete missingness of instrument data at the biweekly assessments was approximately 15%. To examine whether biweekly measures were missing at random, we regressed the number of missing surveys per participant on demographic factors (age, sex, income, educational attainment, direct vs indirect care role) and baseline outcome data (depressive symptoms, burnout subfacets). Age and income were associated with missingness (eTable 2 in Supplement 2); thus, data may be considered missing at random, and analyses provide robust estimators.28 Even accounting for age and income, estimates of treatment effects were consistent with the more parsimonious results reported hereinafter, which excluded these 2 factors (eTables 3 and 4 in Supplement 2 provide ESs accounting for age and income).
Adherence Results
In the first week of the trial, a mean (SD) 73.3 (41.5) minutes of exercise and 3.9 (2.2) workouts were completed with the Down Dog apps. Seventy-eight participants (54.9%) completed 80 minutes or more of exercise using the apps in the first week. At week 12, a mean (SD) of 34.7 (46.0) minutes of exercise and 1.6 (1.9) workouts were completed. Thirty-three participants (23.2%) completed 80 minutes or more at week 12. A week-by-week total amount of minutes and sessions completed is found in eTable 5 in Supplement 2. Only age was associated with weekly mean minutes of app use (see eTable 6 in Supplement 2).
Intention-to-Treat Analysis
Primary Outcome: Depressive Symptoms
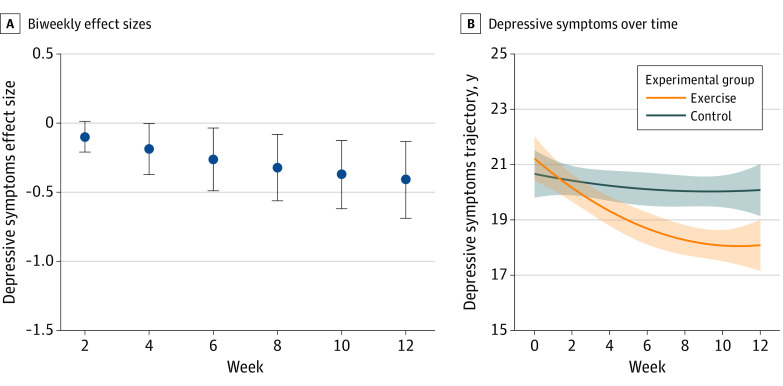
By week 4, exercise effects on depressive symptoms were significant but very small (ES, −0.19 [95% CI, −0.37 to 0.002]), and at week 6, effects were significant and within the small range (ES, −0.26 [95% CI, −0.49 to −0.04]). By trial’s end (week 12), a significant small to medium treatment effect was observed (ES, −0.41 [95% CI, −0.69 to −0.13]), whereby participants in the exercise condition had significant reductions in depressive symptoms compared with the wait list control condition. Table 2 and Figure 2A provide ES estimates per assessment period, and Figure 2B shows visualization of the exercise and wait list control conditions trajectories over time (based on within-condition estimated intercepts, slopes, and curves [eTable 7 in the Supplement 2]).
Table 2. Biweekly Feingold Treatment ES for Depressive (Primary Outcome) and Burnout (Secondary Outcome) Symptoms.
| Outcome | Assessment time point, ES (95% CI) | |||||
|---|---|---|---|---|---|---|
| Week 2 | Week 4 | Week 6 | Week 8 | Week 10 | Week 12 | |
| Depressive symptoms | −0.10 (−0.21 to 0.01) | −0.19 (−0.37 to −0.002)a | −0.26 (−0.49 to −0.04)a | −0.32 (−0.56 to −0.08)a | −0.37 (−0.62 to −0.13)a | −0.41 (−0.69 to −0.13)a |
| Burnout symptoms | ||||||
| Cynicism | −0.10 (−0.18 to −0.02)a | −0.19 (−0.31 to −0.04)a | −0.24 (−0.40 to −0.08)a | −0.28 (−0.45 to −0.11)a | −0.31 (−0.49 to −0.14)a | −0.33 (−0.53 to −0.13)a |
| Emotional exhaustion | −0.13 (−0.23 to −0.03)a | −0.23 (−0.40 to −0.07)a | −0.31 (−0.51 to −0.11)a | −0.36 (−0.58 to −0.14)a | −0.39 (−0.61 to −0.16)a | −0.39 (−0.64 to −0.14)a |
| Professional efficacy | 0.10 (−0.01 to 0.20) | 0.17 (0.005 to 0.34)a | 0.20 (0.005 to 0.40)a | 0.22 (0.01 to 0.43)a | 0.22 (0.001 to 0.43)a | 0.18 (−0.06 to 0.43) |
Abbreviation: ES, effect size.
Designates significant effects (P < .05).
Figure 2. Biweekly Effect Sizes and Trajectories for Depressive Symptoms (Primary Outcome) Over Time.
A, Biweekly effect sizes for decreases in depressive symptoms for participants in the exercise condition vs the wait list control condition. B, Trajectories in depressive symptoms over time in the exercise and wait list control conditions. Error bars and shaded areas indicate 95% CIs.
Secondary Outcomes: Burnout Subfacets and Absenteeism
Table 2 gives ES estimates per assessment period. Figure 3 shows the biweekly effect sizes for the burnout subfacets of cynicism, emotional exhaustion, and professional efficacy (Figure 3A-C) and trajectories over time for these subfacets in both conditions (Figures 3D-F, based on within-condition estimated intercepts, slopes, and curves [eTable 7 in Supplement 2]).
Figure 3. Burnout Subfacet Trajectories and Biweekly Effect Sizes Across Time.
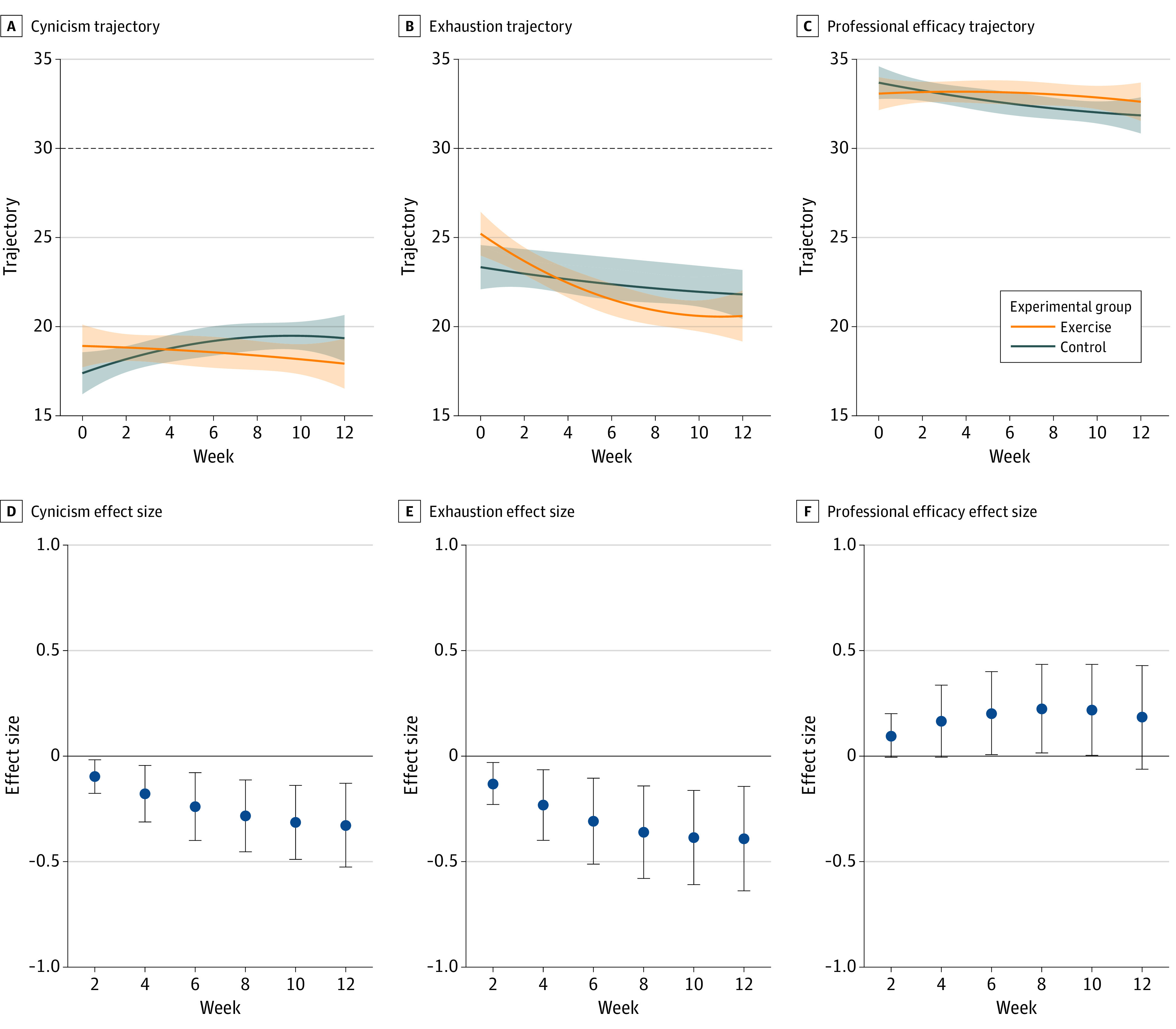
Trajectories across time and biweekly effect sizes for burnout subfacets are shown for the exercise and wait list control conditions. Horizontal dashed lines indicate scale maximums; shaded areas and error bars indicate 95% CIs.
Cynicism
At the first assessment following randomization, treatment effects on cynicism were significant and very small (week 2 ES, −0.10 [95% CI, −0.18 to −0.02]) and significant and within the small to medium effect range by trial’s end (week 12 ES, −0.33 [95% CI, −0.53 to −0.13]). Treatment effects favored the exercise condition.
Emotional Exhaustion
Treatment effects for the intervention on emotional exhaustion were significant and very small at the first assessment point (week 2 ES, −0.13 [95% CI, −0.23 to −0.03]). Treatment effects were significant and within the small to medium ES range by week 12 (ES, −0.39 [95% CI, −0.64 to −0.14]) and favored the exercise condition.
Professional Efficacy
Treatment effects on professional efficacy were significant at weeks 4 (ES, 0.17 [95% CI, 0.005-0.34]) to 10 (ES, 0.22 [95% CI, 0.001 to 0.43]). Very small improvements in efficacy were observed in the exercise condition compared with the wait list control condition.
Sick Days
The exercise condition had fewer weeks in which participants reported taking sick days (mean [SD], 0.86 [1.05]; median, 0 [range, 0-4]) than the wait list control condition (mean [SD]. 1.26 [1.32]; median, 1 [range, 0-5]). The intervention had a small effect on the number of weeks with reported sick days (r = 0.15 [95% CI, 0.03-0.26]). eTable 8 in Supplement 2 provides the distribution of number of weeks in which participants reported sick days.
Per-Protocol Analysis
Per-protocol analyses demonstrated large reductions in depressive symptoms (week 12 ES, −0.71 [95% CI, −1.21 to −0.20]) and medium reductions in cynicism (week 12 ES, −0.47 [95% CI, −0.72 to −0.21]), emotional exhaustion (week 12 ES, −0.57 [95% CI, −1.01 to −0.14]), and professional efficacy (week 12 ES, 0.50 [95% CI, 0.14-0.86]) for participants who completed at least 80 min/wk during the trial (30 [21.1%]) compared with wait list control participants. Small and significant effects in cynicism (week 12 ES, −0.34 [95% CI, 0.58 to −0.09]) and emotional exhaustion (week 12 ES, −0.39 [95% CI, −0.68 to −0.09]) were revealed for those who completed 20 to 79 min/wk (73 [51.4%]). There were no significant treatment effects for those who had very low engagement of less than 20 min/wk (37 [26.1%]). eTables 9 and 10 in Supplement 2 provide biweekly ESs for depressive symptoms and burnout subfactors by adherence categories, respectively; eFigures 1 to 4 in Supplement 2 show ESs and trajectories.
Discussion
In this RCT, a 12-week app-based exercise intervention yielded significant reductions in depressive symptoms among HCWs that became more pronounced as time progressed. Similar consistent patterns were observed for 2 subfacets of burnout, cynicism, and emotional exhaustion. A small effect was also observed for the number of weeks HCWs reported taking sick days, with an apparent stabilization of sick days for participants in the exercise apps condition and an increase for those in the wait list control condition. Importantly, in our per-protocol analyses, exercise was found to be particularly effective for participants who engaged with the apps at the recommended amount of at least 80 minutes per week. It is possible that these findings reflect a methodological artifact whereby participants with lower levels of depression sought out more opportunities to be active, rather than those who made greater use of the exercise apps deriving superior reductions in depression and burnout. That said, baseline depression and burnout were unrelated to subsequent exercise app adherence, so such reverse causality appears unlikely. Indeed, our results suggest that at-home exercise can have meaningful effects on HCWs’ well-being and absenteeism when they are given free access to mobile-based exercise apps, provided they continue using these apps. The significant treatment effects of app-based exercise are supported by research that shows incremental increases in exercise lead to incremental increases in physical29 and mental health,30 even at levels that fall below recommended guidelines.
Even though all the participants volunteered and were generally willing, ready, and able to start exercising with the apps at home (and most did so in the first few weeks), adherence was suboptimal among some participants, with older adults more likely to use the apps. While we ruled out baseline depressive symptoms or burnout as causal factors of adherence, it is likely that stressors at home or at work, not measured in the present study, interfered with adherence. Throughout the COVID-19 pandemic, HCWs faced considerable challenges and stressors, including early fears of a virus with unknown transmissibility, ever-changing workplace protocols, isolation requirements, and potential increases in at-home childcare responsibilities and relationship problems.31
To address work-related challenges, a 2022 Mental Health Commission of Canada report30 suggested that improving psychological self-care among HCWs should occur at 3 intersecting levels: the organization (government, hospital), the team (or unit), and the individual. At the organizational level, governments have announced investments into HCW retention and new hires.32 At the team level, some organizations have developed health and safety training programs to promote better functioning and communication within teams.11 As a complement to both organizational and team level supports and infrastructure, individual-level initiatives (if low cost and scalable) also have potential to support the well-being of HCWs.
In our efficacy trial, we sought to support mental health at the individual level, and determined that at-home, app-based exercise improves mental health with some success. The challenge at the individual level, then, is to determine not only for whom providing free apps is effective in promoting new engagement and maintenance of exercise, but also who—based on demographics and baseline characteristics—needs additional behavioral (eg, health coaches32 trained in motivational interviewing33 to increase exercise levels) or psychological (eg, psychiatric and/or psychological professionals) supports.11 Appropriate programs can be developed to meet these needs and tested in future trials. It will then be important to scale the programs up and determine their effectiveness and cost-benefits to adequately address part of the current mental health crisis in HCWs.
Limitations
This study is not without its limitations. Mass emails and advertisements were circulated to leaders within all the units at the network’s affiliated hospitals and across HCW categories, relying on unit heads to spread study information to the approximately 10 000 staff or contracted employees across the 10 sites. While most participants primarily came from one of the affiliated hospitals, 1 hospital accounted for 69% of employees across the network. Similarly, the greatest proportion of participating HCWs were nurses, reflecting the fact that nurses accounted for 32% of employees (the largest job category) within the network. Very few physicians participated in the trial, demonstrating that advertisements were either not circulated as expected or physicians were not interested in participating. We are also unaware which leaders circulated the advertisements. Consultations with leaders and underrepresented employee groups will be required to recruit a broader spectrum of employees.
Additionally, engagement in exercise was only monitored through use of the apps, and not in other ways (eg, step counts from mobile devices, monitors). Supplementing measurement with accelerometers may reveal new insights into the effects of physical activity and exercise on mental health among HCWs. Additionally, cost-benefit analyses were not calculated in the current study in terms of direct and indirect health care expenditures when mental health improves, which is important to developing appropriate wellness programs. Finally, while participants were of diverse ethnic and racial identities and educational backgrounds, most participants were women. Developing strategies to recruit more men will require innovative solutions.
Conclusion
To our knowledge, this RCT provides the first evidence that exercising at home with a suite of exercise apps, using little to no equipment, can improve the mental health of HCWs. Scaled-up effectiveness trials are needed whereby all HCWs from an organization are provided longer opportunities to access the suite of apps to determine interest, uptake, adherence, and mental, physical, and economic effects.32 Such trials may reveal a potential low-cost, high-reward opportunity for health care networks to use at large, embedded within wellness programs, to reduce health care’s growing mental health crisis.
Trial Protocol
eMethods. Outcomes, Syntax Example, Effect Size Methods, and Software
eTable 1. Missingness for Outcome Scales
eTable 2. Predicting Number of Missing Surveys per Participant From Baseline Outcome and Sociodemographic Data
eTable 3. Biweekly Feingold Treatment Effect Sizes and 95% CIs for Depressive (Primary Outcome) and Burnout Symptoms (Secondary Outcome), Covarying the Effects of Age
eTable 4. Biweekly Feingold Treatment Effect Sizes and 95% CIs for Depressive (Primary Outcome) and Burnout Symptoms (Secondary Outcome), Covarying the Effects of Income
eTable 5. Weekly Use of Down Dog Apps for All Exercise Condition Participants and by Average Adherence Group Over the Course of the Intervention
eTable 6. Predicting Average Weekly Minutes of App Use per Participant From Baseline Outcome and Sociodemographic Data
eTable 7. Within Condition Changes Over Time for Depressive Symptoms and for Burnout Symptoms (Cynicism, Exhaustion, Professional Efficacy)
eTable 8. Biweekly Average Number of Sick Days
eTable 9. Biweekly Effect Sizes for Depressive Symptoms With Use of the Down Dog Apps Over the Course of the Intervention Compared With the Wait List Control Condition (n = 146)
eTable 10. Biweekly Effect Sizes for Burnout Symptoms (Cynicism, Exhaustion, Professional Efficacy) With Use of the Down Dog Apps Compared With the Wait List Control Condition (n = 146)
eFigure 1. Biweekly Effect Sizes for Depressive Symptoms for Participants With Use of the Down Dog Apps Over the Course of the Intervention Compared With the Wait List Control Condition (n = 146)
eFigure 2. Depressive Symptoms Trajectories for Participants With Use of the Down Dog Apps and Wait List Control Condition Over the Course of the Intervention
eFigure 3. Biweekly Effect Sizes for Burnout Symptoms (Cynicism, Exhaustion, Professional Efficacy) for Participants With Use of the Down Dog Apps Over the Course of the Intervention Compared With the Wait List Control Condition (n = 146)
eFigure 4. Trajectories of Burnout Symptoms (Cynicism, Exhaustion, Professional Efficacy) for Participants With Use of the Down Dog Apps and Wait List Control Condition Over the Course of the Intervention
Data Sharing Statement
References
- 1.Robinson E, Sutin AR, Daly M, Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J Affect Disord. 2022;296:567-576. doi: 10.1016/j.jad.2021.09.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control Prevention . Interim list of categories of 3 essential workers mapped to standardized industry codes and titles. Reviewed March 29, 2021. Accessed March 29, 2021. https://www.cdc.gov/vaccines/covid-19/categories-essential-workers.html
- 3.Tran BX, Vu GT, Latkin CA, Ho RCM. Multilevel and amplified effects of COVID-19 pandemic on health workers. Lancet Reg Health West Pac. 2022;23:100478. doi: 10.1016/j.lanwpc.2022.100478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Braule Pinto ALC, Serpa ALO, de Paula JJ, et al. Increased risk of health professionals to feel traumatized during the COVID-19 pandemic. Sci Rep. 2021;11(1):18286. doi: 10.1038/s41598-021-97783-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sexton JB, Adair KC, Proulx J, et al. Emotional exhaustion among US health care workers before and during the COVID-19 pandemic, 2019-2021. JAMA Netw Open. 2022;5(9):e2232748. doi: 10.1001/jamanetworkopen.2022.32748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poon YR, Lin YP, Griffiths P, Yong KK, Seah B, Liaw SY. A global overview of healthcare workers’ turnover intention amid COVID-19 pandemic: a systematic review with future directions. Hum Resour Health. 2022;20(1):70. doi: 10.1186/s12960-022-00764-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211 [DOI] [PubMed] [Google Scholar]
- 8.Kaushik D. COVID-19 and health care workers burnout: a call for global action. EClinicalMedicine. 2021;35:100808. doi: 10.1016/j.eclinm.2021.100808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campion J, Javed A, Lund C, et al. Public mental health: required actions to address implementation failure in the context of COVID-19. Lancet Psychiatry. 2022;9(2):169-182. doi: 10.1016/S2215-0366(21)00199-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buselli R, Corsi M, Veltri A, et al. Mental health of health care workers (HCWs): a review of organizational interventions put in place by local institutions to cope with new psychosocial challenges resulting from COVID-19. Psychiatry Res. 2021;299:113847. doi: 10.1016/j.psychres.2021.113847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Firth J, Solmi M, Wootton RE, et al. A meta-review of “lifestyle psychiatry”: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry. 2020;19(3):360-380. doi: 10.1002/wps.20773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puterman E, Hives B, Mazara N, et al. COVID-19 Pandemic and Exercise (COPE) trial: a multigroup pragmatic randomised controlled trial examining effects of app-based at-home exercise programs on depressive symptoms. Br J Sports Med. 2022;56(10):546-552. doi: 10.1136/bjsports-2021-104379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kiernan M, Schoffman DE, Lee K, et al. The Stanford Leisure-Time Activity Categorical Item (L-Cat): a single categorical item sensitive to physical activity changes in overweight/obese women. Int J Obes (Lond). 2013;37(12):1597-1602. doi: 10.1038/ijo.2013.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bredin SS, Gledhill N, Jamnik VK, Warburton DE. PAR-Q+ and ePARmed-X+: new risk stratification and physical activity clearance strategy for physicians and patients alike. Can Fam Physician. 2013;59(3):273-277. [PMC free article] [PubMed] [Google Scholar]
- 15.Center for Open Science . Participant guide to Down Dog. Updated November 16, 2022. Accessed April 28, 2023. https://osf.io/q3u86
- 16.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10(2):77-84. doi: 10.1016/S0749-3797(18)30622-6 [DOI] [PubMed] [Google Scholar]
- 17.Maslach C, Jackson SE, Leither MP, Schaufeli WB, Schwab RL. Maslach Burnout Inventory. 4th ed. Mind Garden Inc; 2018. [Google Scholar]
- 18.Spybrook J, Bloom H, Congdon R, Hill C, Martinez A, Raudenbush S. Optimal Design plus empirical evidence, version 3.0. Revised October 16, 2011. Accessed October 16, 2011. http://www-personal.umich.edu/~amzzz/od/od-manual-20111016-v300.pdf
- 19.Crawley MJ. Statistical Computing: An Introduction to Data Analysis Using S-Plus. Wiley; 2002. [Google Scholar]
- 20.Bentler PM, Chou C-P. Practical issues in structural modeling. Sociol Methods Res. 1987;16(1):78-117. doi: 10.1177/0049124187016001004 [DOI] [Google Scholar]
- 21.Mayer M. MissRanger: fast imputation of missing values, version 2.2.1. R package version 2019. April 28, 2023. Accessed April 28, 2023. https://cran.r-project.org/web/packages/missRanger/missRanger.pdf
- 22.Gupta SK. Intention-to-treat concept: a review. Perspect Clin Res. 2011;2(3):109-112. doi: 10.4103/2229-3485.83221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Felt JM, Depaoli S, Tiemensma J. Latent growth curve models for biomarkers of the stress response. Front Neurosci. 2017;11:315. doi: 10.3389/fnins.2017.00315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feingold A. New approaches for estimation of effect sizes and their confidence intervals for treatment effects from randomized controlled trials. Quant Method Psychol. 2019;15(2):96-111. doi: 10.20982/tqmp.15.2.p096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141(1):2-18. doi: 10.1037/a0024338 [DOI] [PubMed] [Google Scholar]
- 26.Heissel A, Heinen D, Brokmeier LL, et al. Exercise as medicine for depressive symptoms? A systematic review and meta-analysis with meta-regression. Br J Sports Med. 2023;bjsports-2022-106282. doi: 10.1136/bjsports-2022-106282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Statistics Canada . Visible minority of person. Updated November 1, 2021. Accessed July 13, 2023. https://www23.statcan.gc.ca/imdb/p3Var.pl?Function=DEC&Id=45152
- 28.Little RJ, Rubin DB. Statistical Analysis With Missing Data. 3rd ed. John Wiley & Sons; 2020. [Google Scholar]
- 29.Hobby J, Crowley J, Barnes K, Mitchell L, Parkinson J, Ball L. Effectiveness of interventions to improve health behaviours of health professionals: a systematic review. BMJ Open. 2022;12(9):e058955. doi: 10.1136/bmjopen-2021-058955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teychenne M, White RL, Richards J, Schuch FB, Rosenbaum S, Bennie JA. Do we need physical activity guidelines for mental health: what does the evidence tell us? Ment Health Phys Act. 2020;18:100315. doi: 10.1016/j.mhpa.2019.100315 [DOI] [Google Scholar]
- 31.Pietromonaco PR, Overall NC. Implications of social isolation, separation, and loss during the COVID-19 pandemic for couples’ relationships. Curr Opin Psychol. 2022;43:189-194. doi: 10.1016/j.copsyc.2021.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93(8):1261-1267. doi: 10.2105/AJPH.93.8.1261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. Guilford Press; 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eMethods. Outcomes, Syntax Example, Effect Size Methods, and Software
eTable 1. Missingness for Outcome Scales
eTable 2. Predicting Number of Missing Surveys per Participant From Baseline Outcome and Sociodemographic Data
eTable 3. Biweekly Feingold Treatment Effect Sizes and 95% CIs for Depressive (Primary Outcome) and Burnout Symptoms (Secondary Outcome), Covarying the Effects of Age
eTable 4. Biweekly Feingold Treatment Effect Sizes and 95% CIs for Depressive (Primary Outcome) and Burnout Symptoms (Secondary Outcome), Covarying the Effects of Income
eTable 5. Weekly Use of Down Dog Apps for All Exercise Condition Participants and by Average Adherence Group Over the Course of the Intervention
eTable 6. Predicting Average Weekly Minutes of App Use per Participant From Baseline Outcome and Sociodemographic Data
eTable 7. Within Condition Changes Over Time for Depressive Symptoms and for Burnout Symptoms (Cynicism, Exhaustion, Professional Efficacy)
eTable 8. Biweekly Average Number of Sick Days
eTable 9. Biweekly Effect Sizes for Depressive Symptoms With Use of the Down Dog Apps Over the Course of the Intervention Compared With the Wait List Control Condition (n = 146)
eTable 10. Biweekly Effect Sizes for Burnout Symptoms (Cynicism, Exhaustion, Professional Efficacy) With Use of the Down Dog Apps Compared With the Wait List Control Condition (n = 146)
eFigure 1. Biweekly Effect Sizes for Depressive Symptoms for Participants With Use of the Down Dog Apps Over the Course of the Intervention Compared With the Wait List Control Condition (n = 146)
eFigure 2. Depressive Symptoms Trajectories for Participants With Use of the Down Dog Apps and Wait List Control Condition Over the Course of the Intervention
eFigure 3. Biweekly Effect Sizes for Burnout Symptoms (Cynicism, Exhaustion, Professional Efficacy) for Participants With Use of the Down Dog Apps Over the Course of the Intervention Compared With the Wait List Control Condition (n = 146)
eFigure 4. Trajectories of Burnout Symptoms (Cynicism, Exhaustion, Professional Efficacy) for Participants With Use of the Down Dog Apps and Wait List Control Condition Over the Course of the Intervention
Data Sharing Statement