Abstract
Background and Objective
Pediatric residents are at high risk for moral distress, which is associated with poor patient care and burnout. Researchers have proposed numerous interventions to reduced distress, but few (if any) have been supported by experimental evidence. In this study, we used an experimental method to provide proof-of-concept evidence regarding the effect of various simple supports on pediatric residents’ reported degree of moral distress.
Methods
We conducted a national study of pediatric residents using a split sample experimental design. The questionnaire contained six clinical vignettes describing scenarios expected to cause moral distress. For each case, participants were randomly assigned to see one of two versions that varied only regarding whether they included a supportive statement. After reading each of the six cases, participants reported the likelihood that the case would cause moral distress.
Results
Two hundred and twenty respondents from five residency programs completed the experiment. Cases were perceived to represent common scenarios that cause distress for pediatric residents. The addition of a supportive statement reduced the likelihood of moral distress in four of the six cases.
Conclusions
In this proof-of-concept study, simple yet effective interventions provided support by offering the resident empathy and shared perspective or responsibility. Interventions that were purely informational were not effective in reducing the likelihood of distress.
Keywords: ethics/bioethics, medical education, pediatrics
INTRODUCTION
Pediatric residents are at high risk for moral distress, which is to say the psychological, emotional, and physiological suffering that clinicians experience when they are involved in situations they perceive as morally undesirable.1–6 Within the hierarchical structure of healthcare, residents often must implement plans without the authority to alter the plans, dissent, or refuse.7–10 This experience can cause moral distress, particularly in the setting of poor communication and collaboration.7,8,11 For residents, moral distress is most often related to inexperience, concerns over telling the truth, respecting patients’ wishes, concerns about competency, and worries of failing to prevent harm.9 Residents in pediatrics must also deal with issues of parental authority regarding the care of their children that may amplify moral distress.12 In studies of internal medicine and pediatric residents, moral distress has been linked to depersonalization,13 medical errors,14 considerations of quitting medicine, and burnout.15–17 Understanding the causes of moral distress and developing successful strategies to address distress is, therefore, essential for medical educators.
Three aspects of the response to pediatric resident moral distress thus far are noteworthy. First, techniques proposed to combat moral distress have included expanded education in medical ethics,18,19 resilience/wellness interventions,20 and workload modifications.21 These are easier said than done: expanded education and interventions compete for residents’ scarce time while structural change regarding resident workload is not always feasible. Second, supervisors and educators are increasingly called upon to mitigate moral distress by using good leadership and communication to create a supportive environment.11,22,23 How to actually create such an environment is, however, unclear, and validation of such strategies is limited. Third, most studies on interventions for moral distress have been theoretical or observational.1,12–14,21,24A few cohort studies have been completed,14,25,26 but no randomized trials have been published, nor have any preliminary proof-of-concept experimental results upon which interventions could (and should) be designed.27
For this study, working within an established intervention development and testing paradigm,28 we sought to quantify the effects of various simple supports on pediatric residents’ reported moral distress using a proof-of-concept randomized, controlled experiment. Using a questionnaire with clinical vignettes (a technique that has been shown to accurately simulate responses observed in practice29), these supports were either a statement by a supervising physician, containing either informational or empathic content, or a residency program structural element. We sought to test the broad hypothesis that adding a support to a vignette would decrease residents’ moral distress. As a secondary aim, we sought to compare the efficacy of both statements by a supervising physician and elements of program structure.
METHODS
Study Participants
We distributed the questionnaire entitled “MD-REST: Minimizing Moral Distress in pediatric RESidency Training Questionnaire” through the program directors of five pediatric residency programs. We used intentional sampling to invite pediatric residency programs with diverse geographic distribution and situated at large volume, high acuity hospitals where residents would be more likely to have experienced the scenarios described in the questionnaire. We initially emailed program directors about their willingness to participate in February 2022, and we provided them with a sample introductory email and link to distribute. We offered a $10 Amazon gift card to every participant who completed the questionnaire and asked program directors to send one reminder email at the two week mark in accordance with the tailored design method.30
We sent the questionnaire to 607 residents from the five participating residency programs: Children’s Hospital of Philadelphia, PA (~150 residents); Seattle Children’s, WA (~131 residents); Zucker School of Medicine at Hofstra/Northwell at Cohen Children’s Medical Center, NY (~ 126 residents); Children’s National Medical Center, DC (~120 residents); and New York Presbyterian Hospital-Columbia Campus, NY (~80 residents).31 We collected data for 16 weeks and managed the data using the Research Electronic Data Capture tool (REDCap) hosted at Children’s Hospital of Philadelphia.32 This study received Institutional Review Board exemption from the Children’s Hospital of Philadelphia.
Instrument Development and Design
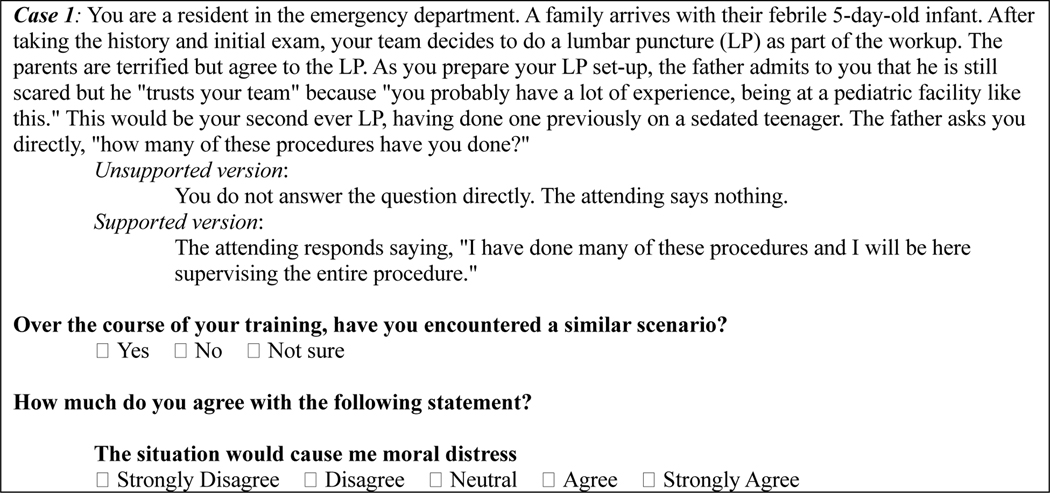
We developed a case-based randomized, controlled experimental questionnaire after review of the literature and consultation with pediatric residents and ethicists. The questionnaire consisted of six hypothetical clinical cases expected to cause moral distress for residents. We pilot-tested the cases for clarity with 12 fellow physicians from diverse clinical specialties who had recently completed pediatrics residency and revised the cases based on their feedback. Case 1 is included as an example in Figure 1, and the full questionnaire is available in the supplemental material. We developed two versions of each case that differed only in whether they included a resident support, either from a supervising physician or the program structure, (henceforth, supported version) or excluded this support (unsupported version). For each participant, each case in the questionnaire was randomly displayed as either the supported or unsupported version for each participant. Random assignment was performed by a hidden calculated field that upon opening the questionnaire link randomly generated a number 1 or 2, representing one of the two versions. Another hidden calculated field rebalanced the makeup of the groups if the difference between supported and unsupported versions in any group exceeded 10 participants, keeping the number of participants seeing the supported and unsupported versions of the cases roughly equal. Each case presented was followed by the same two questions: (1) “Over the course of your training, have you encountered a similar scenario?” and (2) “How much do you agree with the following statement? The situation would cause me moral distress.” Answer options for the first question were “yes,” “no,” or “not sure,” and for the second were on a 5-point Likert scale from strongly disagree (low likelihood of moral distress) to strongly agree (high likelihood of moral distress).
Figure 1: Full Sample Case.
Sample Case Vignette. This provides the full case describing a resident’s procedural distress. Half of residents saw the unsupported version; the remainder saw the supported version with an additional supportive statement by the supervising attending.
Case Descriptions
The first three cases evaluate the effect of supportive statements by a supervising physician. Case 1 centers on a resident preforming a lumbar puncture for only the second time. The patient’s parent asks the resident how many prior procedures they have performed. In the unsupported version, the supervising attending says nothing. In the supported version, the supervising attending reassures the parent that the supervisor has ample experience and will oversee the procedure. In Case 2, the resident is asked to place a nasoduodenal tube, a procedure they are not comfortable performing. In the unsupported version, the supervising physician states that the task is easy and asks the resident to reach out if they run into trouble. In the supported version, the supervising physician offers to be present for the procedure. In Case 3, the resident is tasked with coordinating a tracheostomy for a child with neurologic devastation, which the resident believes is futile care. In the unsupported version, the supervising physician does not engage the resident’s concerns. In the supported version, the supervising physician describes previous discussions with the family and assures the resident that the family is making an informed, thoughtful decision.
The latter three cases evaluate the effect of a simple element of program structure. In Case 4, a resident discovers that their co-resident made a medication error. In the unsupported version, the resident is left to navigate the situation alone and chooses not to raise the issue with their co-resident. In the supported version, the care system has a built-in review process to investigate such errors. In Case 5, the resident must oversee nasogastric tube placement in a patient with anorexia nervosa against the patient’s wishes. In the supported version, the resident has the additional experience of time spent in an eating disorders follow-up clinic and has met patients with anorexia who have recovered; the unsupported version lacks this additional context. In Case 6, a parent in the newborn nursery declines a routine Vitamin K shot for their child. In the unsupported version, the supervising physician tells the resident to make sure to document the refusal. In the supported version, the supervising physician provides additional educational material that the resident can share with the parents. Respondents saw the cases in this order: 1, 5, 4, 2, 3, and 6. We re-ordered the cases in this paper to aggregate the types of scenarios and interventions and facilitate interpretation of the study.
Statistical Analysis
We analyzed the responses using Stata version 17.1 (StataCorp, College Station, TX). We examined pediatric resident demographics, residency program size, level in residency and gender for the entire study population, as well as for randomization subgroups that saw each version of each case. We calculated a mean moral distress value for each participant by averaging their reported moral distress from all six cases. Our primary outcome was reported moral distress, which we compared between the supported and unsupported version of each case. We compared data between case versions using two-tailed tests with significance set at p<0.05. Because this outcome was ordinal output from a 5-point Likert scale, we used the Wilcoxon–Mann-Whitney test to assess for differences in responses between the groups that saw unsupported and supported versions of each case. We calculated Cohen’s d effect size to determine the magnitude of difference in the degree of moral distress reported between case versions, as this is a commonly used measure of the importance of an effect in decision-making.33,34
RESULTS
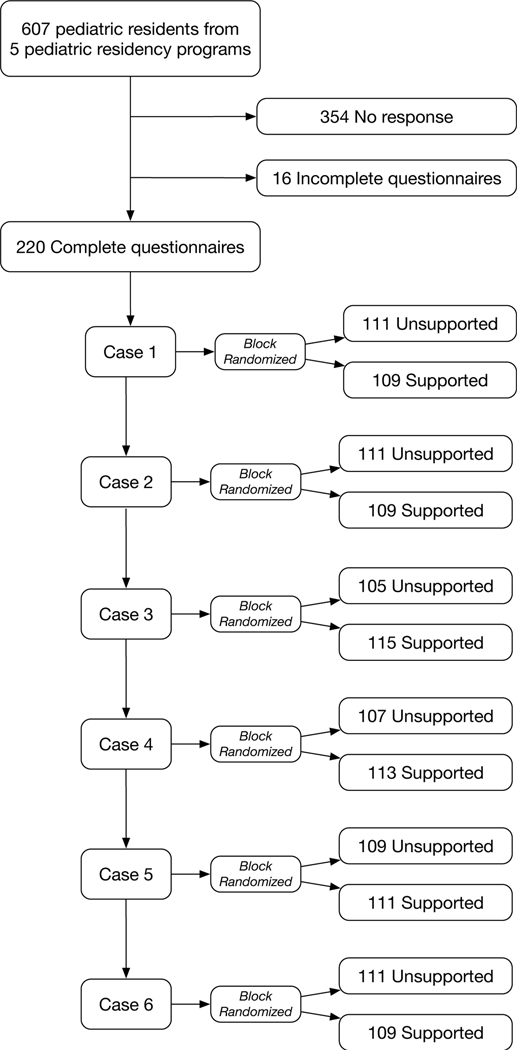
A total of 220 pediatric residents from five residency programs completed the entire questionnaire (Figure 1), representing an evaluable response rate of 36% (220 of 607 possible respondents). Randomization successfully balanced groups for a between-group difference of 10 participants or less for all cases (Figure 2). Respondents were distributed across all training years with 39%, 33%, and 25% in their first, second, and third years, respectively. Most respondents were female (78%), similar to nationwide data for all pediatric residents (71% female).35 Demographic characteristics were balanced by randomization in each case, with no significant differences between the residents who saw the supported and unsupported versions of the cases (Table 1).
Figure 2: CONsolidated Standards of Reporting Trials (CONSORT) Flow Diagram of the Experimental Study.
This flow diagram displays the progress through the phases of sequential randomization into two groups for each case.
Table 1-.
Characteristics of Respondents
| All | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N=220 | Un=111 | Sn=109 | P-value | Un=111 | Sn=109 | P-value | Un=105 | Sn=115 | P-value | Un=109 | Sn=111 | P-value | Un=107 | Sn=113 | P-value | Un=111 | Sn=109 | P-value | |
| PGY1 | 38.5 | 35.1 | 42.1 | 0.56 | 35.8 | 41.3 | 0.55 | 32.7 | 43.9 | 0.07 | 40.4 | 36.7 | 0.61 | 37.1 | 39.8 | 0.54 | 42.2 | 34.9 | 0.50 |
| PGY2 | 33.5 | 36.9 | 29.9 | 37.6 | 29.4 | 42.3 | 25.4 | 33.9 | 33.0 | 30.5 | 36.3 | 33.9 | 33.0 | ||||||
| PGY3 | 23.9 | 25.2 | 22.4 | 22.0 | 25.7 | 21.2 | 26.3 | 22.9 | 24.8 | 27.6 | 20.4 | 22.0 | 25.7 | ||||||
| PGY4 | 3.2 | 2.7 | 3.7 | 3.7 | 2.8 | 1.9 | 4.4 | 1.8 | 4.6 | 3.8 | 2.7 | 1.8 | 4.6 | ||||||
| PGY5 | 1.0 | 0.0 | 1.9 | 0.9 | 0.9 | 2.0 | 0.0 | 0.9 | 0.9 | 1.0 | 0.9 | 0.0 | 1.9 | ||||||
| Female | 77.0 | 76.4 | 77.6 | 0.98 | 78.7 | 75.2 | 0.25 | 76.9 | 77.0 | 1.00 | 78.9 | 75.0 | 0.79 | 75.0 | 78.8 | 0.26 | 76.9 | 77.1 | 1.00 |
| Male | 22.1 | 22.7 | 21.5 | 19.4 | 24.8 | 22.1 | 22.1 | 24.1 | 25.0 | 20.2 | 19.5 | 22.2 | 22.0 | ||||||
| Other | 0.9 | 0.9 | 0.9 | 1.9 | 0.0 | 1.0 | 0.9 | 0.9 | 0.09 | 0.0 | 1.8 | 0.9 | 0.9 | ||||||
For all but Case 2, >70% of residents reported having encountered a similar situation during their training (84%, 48%, 77%, 73%, 86%, and 87% for Cases 1–6, respectively). Mean likelihood of experiencing moral distress of all cases was 3.5 (SD 0.63) on the 5-point Likert scale, with 1 being “strongly disagree” that a case would cause moral distress and 5 being “strongly agree”. Reported likelihood of moral distress was highest for Case 3 (3.9, SD: 1.1), independent of the presented version, followed by Cases 1 (3.8, SD: 0.9), 6 (3.6, SD: 1.2), 2 (3.6, SD: 1.2), 5 (3.4, SD: 1.1), and 4 (3.3, SD: 1.1).
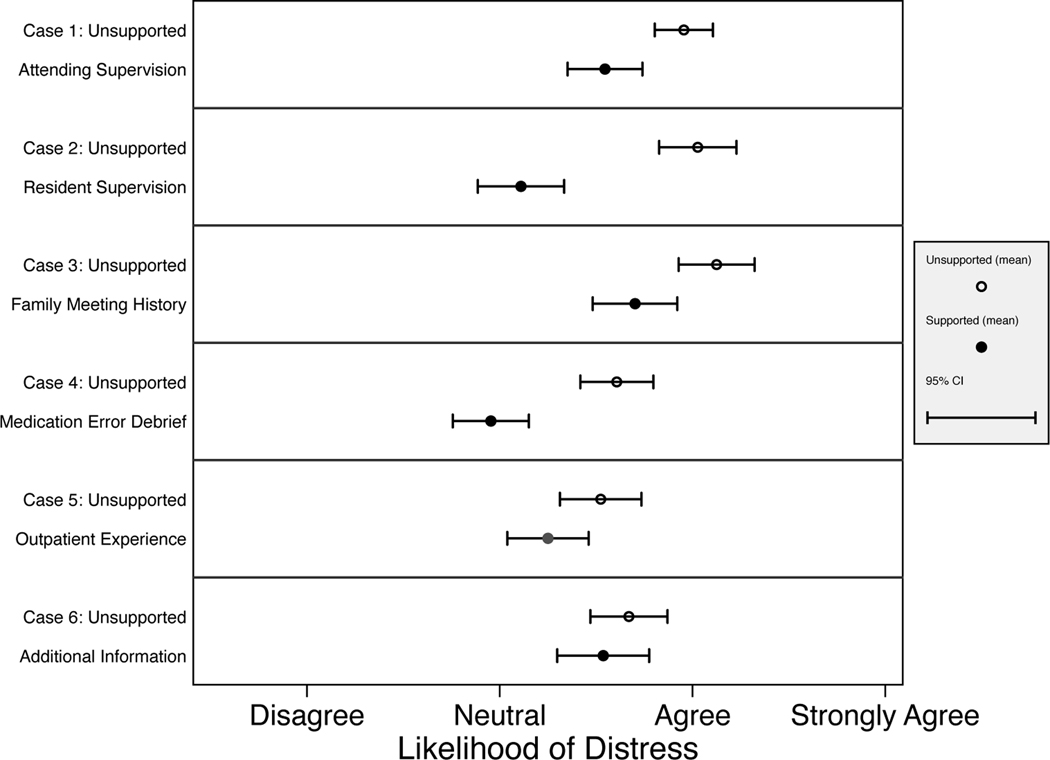
The primary outcome, reported likelihood of moral distress, differed between the supported and unsupported versions of the cases in four out of six cases (Cases 1, 2, 3 and 4; Figure 3). In Case 1, a supervising physician’s response to a parent’s query about procedural inexperience reduced the likelihood of moral distress (p< 0.002; Cohen’s d: 0.45). In Case 2, a supervising physician’s offer to be present during a procedure also reduced the likelihood of moral distress (p<0.001; Cohen’s d: 0.82). In Case 3, resident likelihood of moral distress was reduced when a supervising physician provided additional context for care the resident feared was futile (p<0.006; Cohen’s d: 0.38). In Case 4, a standardized system for addressing errors decreased reported likelihood of moral distress (p<0.001; Cohen’s d: 0.65).
Figure 3: Effect of Supports on Moral Distress.
Primary Outcome Measures by Case. This matrix displays means and confidence intervals for the primary outcome measure, reported moral distress. For each case, responses are stratified by whether participants saw the unsupported or supported version of the case. CI= confidence interval
By contrast, in Cases 5 and 6, providing additional information to a resident through an outpatient experience and to a parent through educational materials, respectively, did not reduce the likelihood of moral distress (p=0.59 and p=0.57, respectively).
DISCUSSION
This randomized controlled experiment evaluated the effect of simple supports from a supervising physician or program structure on the degree of moral distress reported by pediatric residents. Of the six cases presented in the questionnaire, residents reported that all were more likely than not to cause moral distress and were commonly experienced. The likelihood of reported distress and residents’ familiarity with the cases together suggest that the questionnaire created an accurate simulation of resident moral distress. Four out of the six interventions trialed were effective in decreasing the likelihood of resident moral distress, with effect sizes in the moderate (Case 1 and 3) to large (Case 2 and 4) range.33
How can we interpret these findings? We suggest that what the successful interventions had in common was what we might call EASER aspects: they provided the resident with both empathy and shared perspective or responsibility, in partnership with a supervisor, or shared accountability with structural aspect of the program. (Of note, an “easer” is an object or process that eases stress or tension.) Three of the successful interventions (Case 1, 2, and 3) entailed statements by a supervising physician that were empathic in nature and one (Case 6) was a structural support. Case 1 and 2 both involve distress related to a resident’s inexperience preforming a procedure. In both cases, a supervising physician recognizes potential distress and affirms their presence and supervision, and thereby their shared responsibility. Though the supportive statements in these cases were similar, the intervention had a larger effect on distress in Case 2. Perhaps a supportive statement from a peer, in this case a senior resident, is more effective than one from an attending, though our ability to generalize is limited. Case 3 trials a supportive statement by an attending in response to a resident’s concern that a tracheostomy is not the best interest of their patient. In the supported version, the attending shares the resident’s recognition of the limitations of this intervention and provides context for the family’s informed decision to proceed. Thereby, the supervising attending presumably offloads some of the resident’s feeling of responsibility as they call to schedule a tracheostomy. The intervention in Case 4, a standardized process for reviewing medication errors is also effective in decreasing moral distress. The standardized process relieves a resident of feeling they must independently confront their colleague or accepting the guilt of choosing not to. This in turn diffuses responsibility and creates a collaborative environment.
The ability for emotional support and shared responsibility to reduce distress is consistent with evidence from related studies of relationships, leadership, and medical education. Research in the context of relationships has shown that emotional support from another person can be more effective than using intrapersonal/individual strategies to reduce distress.36 For instance, having another person name or label a negative emotion related to an aversive experience is more effective in reducing distress than self-labeling the emotion.37 The supportive statements trialed here may additionally be effective because they occur in “real time,” during a distressing scenario. Recent work demonstrates that more proximal event debriefings or “microdebriefings” embedded during an event may be more effective for reducing distress than interventions following the event.38 Research on leadership shows that good leaders reduce distress by identifying situations likely to cause negative feelings and sharing responsibility—and even blame.39,40 Medical education experts recognize this, as shared responsibility with supervisors and tailoring of this responsibility to meet a trainee’s practice level is a central tenet of effective medical education.41,42 Similarly, error reporting systems that emphasize shared and systemic over individual failures have been demonstrated to patient safety, in large part because clinicians are more comfortable reporting errors if they feel responsibility will be shared.43,44 Recognition and targeting of distress through supportive statements or program structure imply that supervisors care about residents, thereby creating an environment that feels supportive and collaborative.22,45 As residents learn and confront new and distressing scenarios, they need to know that they are not alone in their responsibility or distress.
In contrast, the interventions that were unsuccessful provide information without empathy or partnership. In Case 5, the resident is provided additional information through meeting patients who have recovered from eating disorders. In Case 6, a supervising physician provides additional information on Vitamin K and asks the asks the resident to share it with the parents, assigning responsibility to the parents. The failure of these interventions calls into question the common suggestion that information and education alone can alleviate residents’ moral distress.7,46,47
We interpret our findings within the constraints of our study design. First, the clinical cases and interventions were hypothetical and we cannot evaluate the extent to which our findings would generalize to actual practice.29 Relatedly, some interventions (e.g., supportive statements) may be more realistically captured in a hypothetical case than others (e.g., experience of meeting outpatients). Nevertheless the reported high moral distress and residents’ familiarity with the hypothetical scenarios suggest fidelity to residents’ experience, and substantial prior evidence supports the ability of hypothetical clinical vignettes to capture clinical practice.48–50 Second, our response rate of 36%, while not affecting the internal validity of our findings, and while typical of national resident questionnaires,51–53 may nonetheless limit the findings’ generalizability to residents who declined to participate.
Our study design also has strengths. First, randomization and control enhance internal validity. We are therefore able to confidently conclude that the one experimental variable—the presence or absence of a support—is responsible for the between-version differences we document. Because randomization occurred after respondents enrolled, this mechanism ensures that response rate does not affect the recorded efficacy of interventions. Another strength of our study design is that it could in the future be adapted to evaluate the efficacy of other interventions for moral distress. The method offers a way to “pre-trial test” such supports experimentally before investing resources to trial them in practice. Third, all the interventions in this experiment require relatively few resources for residency programs, particularly compared to larger scale curricula in ethics or wellness that have been proposed. Therefore, implementation may be faster and easier, or an excellent complement to larger-scale changes.
CONCLUSIONS
This study provides proof-of-concept experimental evidence that several simple EASER interventions, focused on empathy and sharing or partnership, may be effective in reducing moral distress among pediatric residents. Purely informational interventions did not decrease distress. The effective interventions can be interpreted as offloading some moral responsibility to either a supervising physician or program system. Future work should evaluate the efficacy of the studied interventions in practice.
Supplementary Material
Supplemental Figure 1: Full Questionnaire. Unsupported versions of cases precede supported versions. Participants saw only one version of each case.
Article Summary:
This study demonstrates the efficacy of simple interventions that offer empathy and shared perspective or responsibility in reducing pediatric residents’ moral distress.
What’s Known on This Subject:
Moral distress is pervasive and problematic among pediatric residents. Interventions to mitigate distress lack rigorous experimental evidence.
What This Study Adds:
On the basis of responses to our split sample, randomized, controlled experiment, simple interventions that offer empathy and shared perspective or responsibility were effective in decreasing residents’ moral distress. Interventions that were purely informational were not effective in reducing distress.
Funding/Support:
This study was supported by T32 Training Grant No. HG009496 from the National Human Genome Research Institute (K.P.C.) and the Steven D. Handler Endowed Chair of Medical Ethics at the Children’s Hospital of Philadelphia.
Role of the Sponsor:
The funder/sponsor had no role in the reported work.
Footnotes
Conflict of Interest Disclosures: The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Jameton A. Nursing Practice: The Ethical Issues. Prentice-Hall; 1984. [Google Scholar]
- 2.Epstein EG, Hamric AB. Moral distress, moral residue, and the crescendo effect. J Clin Ethics. 2009;20(4):330–342. [PubMed] [Google Scholar]
- 3.Jameton A. What Moral Distress in Nursing History Could Suggest about the Future of Health Care. AMA J Ethics. 2017;19(6):617–628. doi: 10.1001/journalofethics.2017.19.6.mhst1-1706 [DOI] [PubMed] [Google Scholar]
- 4.Campbell SM, Ulrich CM, Grady C. A Broader Understanding of Moral Distress. Am J Bioeth. 2016;16(12):2–9. doi: 10.1080/15265161.2016.1239782 [DOI] [PubMed] [Google Scholar]
- 5.McCarthy J, Deady R. Moral Distress Reconsidered. Nurs Ethics. 2008;15(2):254–262. doi: 10.1177/0969733007086023 [DOI] [PubMed] [Google Scholar]
- 6.Morley G, Ives J, Bradbury-Jones C, Irvine F. What is ‘moral distress’? A narrative synthesis of the literature. Nurs Ethics. 2019;26(3):646–662. doi: 10.1177/0969733017724354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hilliard R, Harrison C, Madden S. Ethical conflicts and moral distress experienced by paediatric residents during their training. Paediatr Child Health. 2007;12(1):29–35. doi: 10.1093/pch/12.1.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jacobs B, Manfredi RA. Moral Distress During COVID-19: Residents in Training Are at High Risk. AEM Educ Train. 2020;4(4):447–449. doi: 10.1002/aet2.10488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenbaum JR, Bradley EH, Holmboe ES, Farrell MH, Krumholz HM. Sources of ethical conflict in medical housestaff training: a qualitative study. Am J Med. 2004;116(6):402–407. doi: 10.1016/j.amjmed.2003.09.044 [DOI] [PubMed] [Google Scholar]
- 10.Rushton CH, Caldwell M, Kurtz M. Moral Distress: A Catalyst in Building Moral Resilience. Am J Nurs. 2016;116(7):40–49. [DOI] [PubMed] [Google Scholar]
- 11.Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behav. 2006;27(7):941–966. doi: 10.1002/job.413 [DOI] [Google Scholar]
- 12.Dryden-Palmer K, Moore G, McNeil C, et al. Moral Distress of Clinicians in Canadian Pediatric and Neonatal ICUs*: Pediatr Crit Care Med. 2020;21(4):314–323. doi: 10.1097/PCC.0000000000002189 [DOI] [PubMed] [Google Scholar]
- 13.Baer TE, Feraco AM, Tuysuzoglu Sagalowsky S, Williams D, Litman HJ, Vinci RJ. Pediatric Resident Burnout and Attitudes Toward Patients. Pediatrics. 2017;139(3):e20162163. doi: 10.1542/peds.2016-2163 [DOI] [PubMed] [Google Scholar]
- 14.Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336(7642):488–491. doi: 10.1136/bmj.39469.763218.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kemper KJ, Schwartz A, Wilson PM, et al. Burnout in Pediatric Residents: Three Years of National Survey Data. Pediatrics. 2020;145(1):e20191030. doi: 10.1542/peds.2019-1030 [DOI] [PubMed] [Google Scholar]
- 16.Sajjadi S, Norena M, Wong H, Dodek P. Moral distress and burnout in internal medicine residents. Can Med Educ J. 2017;8(1):e36–43. doi: 10.36834/cmej.36639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236–242. doi: 10.4300/JGME-D-09-00054.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deonandan R, Khan H. Ethics education for pediatric residents: a review of the literature. Can Med Educ J. 2015;6(1):e61–67. [PMC free article] [PubMed] [Google Scholar]
- 19.Lang KR. The professional ills of moral distress and nurse retention: is ethics education an antidote? Am J Bioeth AJOB. 2008;8(4):19–21; author reply W1–2. doi: 10.1080/15265160802147181 [DOI] [PubMed] [Google Scholar]
- 20.Jennings ML, Slavin SJ. Resident Wellness Matters: Optimizing Resident Education and Wellness Through the Learning Environment. Acad Med J Assoc Am Med Coll. 2015;90(9):1246–1250. doi: 10.1097/ACM.0000000000000842 [DOI] [PubMed] [Google Scholar]
- 21.Goitein L, Shanafelt TD, Wipf JE, Slatore CG, Back AL. The Effects of Work-Hour Limitations on Resident Well-being, Patient Care, and Education in an Internal Medicine Residency Program. Arch Intern Med. 2005;165(22):2601–2606. doi: 10.1001/archinte.165.22.2601 [DOI] [PubMed] [Google Scholar]
- 22.Beck J, O’Hara KL, Falco CN, et al. How Attendings Can Help Residents Navigate Moral Distress: A Qualitative Study. Acad Pediatr. 2021;21(8):1458–1466. doi: 10.1016/j.acap.2021.06.006 [DOI] [PubMed] [Google Scholar]
- 23.Bail K, Morrison P. Interprofessional communication of prognosis: teaching to bridge the gaps. Educ Health Abingdon Engl. 2011;24(1):326. [PubMed] [Google Scholar]
- 24.Pauly BM, Varcoe C, Storch J. Framing the Issues: Moral Distress in Health Care. HEC Forum. 2012;24(1):1–11. doi: 10.1007/s10730-012-9176-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chiafery MC, Hopkins P, Norton SA, Shaw MH. Nursing Ethics Huddles to Decrease Moral Distress among Nurses in the Intensive Care Unit. J Clin Ethics. 2018;29(3):217–226. [PubMed] [Google Scholar]
- 26.Hamric AB, Epstein EG. A Health System-wide Moral Distress Consultation Service: Development and Evaluation. HEC Forum Interdiscip J Hosp Ethical Leg Issues. 2017;29(2):127–143. doi: 10.1007/s10730-016-9315-y [DOI] [PubMed] [Google Scholar]
- 27.Hamric AB. Empirical Research on Moral Distress: Issues, Challenges, and Opportunities. HEC Forum. 2012;24(1):39–49. doi: 10.1007/s10730-012-9177-x [DOI] [PubMed] [Google Scholar]
- 28.Czajkowski SM, Powell LH, Adler N, et al. From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2015;34(10):971–982. doi: 10.1037/hea0000161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality. JAMA. 2000;283(13):1715–1722. doi: 10.1001/jama.283.13.1715 [DOI] [PubMed] [Google Scholar]
- 30.Dillman DA, Smyth JD, Christian LM. Internet, Phone, Mail, and Mixed-Mode Surveys: The Tailored Design Method. John Wiley & Sons; 2014. [Google Scholar]
- 31.Welcome to Residency Navigator | Doximity. Accessed August 3, 2022. https://www.doximity.com/residency/?gclid=Cj0KCQjwuaiXBhCCARIsAKZLt3nKeX5bjOUCEUqjmshEWs_8-FlPDMNASzaevxo2DBFuxofchA-TtckaAgy1EALw_wcB
- 32.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Durlak JA. How to Select, Calculate, and Interpret Effect Sizes. J Pediatr Psychol. 2009;34(9):917–928. doi: 10.1093/jpepsy/jsp004 [DOI] [PubMed] [Google Scholar]
- 34.Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141(1):2–18. doi: 10.1037/a0024338 [DOI] [PubMed] [Google Scholar]
- 35.ACGME Data Resource Book. Accessed July 18, 2022. https://www.acgme.org/about-us/publications-and-resources/graduate-medical-education-data-resource-book/
- 36.Levy-Gigi E, Shamay-Tsoory SG. Help me if you can: Evaluating the effectiveness of interpersonal compared to intrapersonal emotion regulation in reducing distress. J Behav Ther Exp Psychiatry. 2017;55:33–40. doi: 10.1016/j.jbtep.2016.11.008 [DOI] [PubMed] [Google Scholar]
- 37.Shamay-Tsoory SG, Levy-Gigi E. You Name It: Interpersonal Affect Labeling Diminishes Distress in Romantic Couples. Behav Ther. 2021;52(2):455–464. doi: 10.1016/j.beth.2020.06.004 [DOI] [PubMed] [Google Scholar]
- 38.Hunt EA, Duval-Arnould JM, Nelson-McMillan KL, et al. Pediatric resident resuscitation skills improve after “Rapid Cycle Deliberate Practice” training. Resuscitation. 2014;85(7):945–951. doi: 10.1016/j.resuscitation.2014.02.025 [DOI] [PubMed] [Google Scholar]
- 39.Fredberg T. Why Good Leaders Pass the Credit and Take the Blame. Harv Bus Rev. Published online October 6, 2011. Accessed August 17, 2022. https://hbr.org/2011/10/why-good-leaders-pass-the-cred [Google Scholar]
- 40.Baker DP, Day R, Salas E. Teamwork as an Essential Component of High-Reliability Organizations. Health Serv Res. 2006;41(4 Pt 2):1576–1598. doi: 10.1111/j.1475-6773.2006.00566.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Drolet BC, Brower JP, Miller BM. Trainee Involvement in Patient Care: A Necessity and Reality in Teaching Hospitals. J Grad Med Educ. 2017;9(2):159–161. doi: 10.4300/JGME-D-16-00232.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Edgar L, Hamstra S. ACGME Milestones Project: Lessons Learned and What’s Next. :43. [Google Scholar]
- 43.Louis MY, Hussain LR, Dhanraj DN, et al. Improving Patient Safety Event Reporting Among Residents and Teaching Faculty. Ochsner J. 2016;16(1):73–80. [PMC free article] [PubMed] [Google Scholar]
- 44.Institute of Medicine (US) Committee on Quality of Health Care in America. To Err Is Human: Building a Safer Health System. (Kohn LT, Corrigan JM, Donaldson MS, eds.). National Academies Press (US); 2000. Accessed August 3, 2022. http://www.ncbi.nlm.nih.gov/books/NBK225182/ [PubMed] [Google Scholar]
- 45.Brend DM, Collin-Vézina D. Stronger together: Workplace social support among residential child welfare professionals. Child Abuse Negl. 2022;130(Pt 3):105302. doi: 10.1016/j.chiabu.2021.105302 [DOI] [PubMed] [Google Scholar]
- 46.Aultman J, Wurzel R. Recognizing and Alleviating Moral Distress Among Obstetrics and Gynecology Residents. J Grad Med Educ. 2014;6(3):457–462. doi: 10.4300/JGME-D-13-00256.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rosenthal MS, Clay M. Initiatives for Responding to Medical Trainees’ Moral Distress about End-of-Life Cases. AMA J Ethics. 2017;19(6):585–594. doi: 10.1001/journalofethics.2017.19.6.stas1-1706 [DOI] [PubMed] [Google Scholar]
- 48.Hainmueller J, Hangartner D, Yamamoto T. Validating vignette and conjoint survey experiments against real-world behavior. Proc Natl Acad Sci. 2015;112(8):2395–2400. doi: 10.1073/pnas.1416587112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sices L, Feudtner C, McLaughlin J, Drotar D, Williams M. How do primary care physicians manage children with possible developmental delays? A national survey with an experimental design. Pediatrics. 2004;113(2):274–282. doi: 10.1542/peds.113.2.274 [DOI] [PubMed] [Google Scholar]
- 50.Callahan KP, Flibotte J, Skraban C, et al. Influence of Genetic Information on Neonatologists’ Decisions: A Psychological Experiment. Pediatrics. Published online February 16, 2022:e2021052130. doi: 10.1542/peds.2021-052130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hoops K, Crifasi C. Pediatric resident firearm-related anticipatory guidance: Why are we still not talking about guns? Prev Med. 2019;124:29–32. doi: 10.1016/j.ypmed.2019.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Davis SA, Braykov NP, Lathrop E, Haddad LB. Familiarity with Long-acting Reversible Contraceptives among Obstetrics and Gynecology, Family Medicine, and Pediatrics Residents: Results of a 2015 National Survey and Implications for Contraceptive Provision for Adolescents. J Pediatr Adolesc Gynecol. 2018;31(1):40–44. doi: 10.1016/j.jpag.2017.09.007 [DOI] [PubMed] [Google Scholar]
- 53.AlSohime F, NurHussen A, Temsah MH, et al. Factors that influence the self-reported confidence of pediatric residents as team leaders during cardiopulmonary resuscitation: A national survey. Int J Pediatr Adolesc Med. 2018;5(3):116–121. doi: 10.1016/j.ijpam.2018.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1: Full Questionnaire. Unsupported versions of cases precede supported versions. Participants saw only one version of each case.