Abstract
Human herpesvirus 6 (HHV-6) has been implicated as a cofactor in the progressive loss of CD4+ T cells observed in AIDS patients. Because dendritic cells (DC) play an important role in the immunopathogenesis of human immunodeficiency virus (HIV) disease, we studied the infection of DC by HHV-6 and coinfection of DC by HHV-6 and HIV. Purified immature DC (derived from adherent peripheral blood mononuclear cells in the presence of granulocyte-macrophage colony-stimulating factor and interleukin-4) could be infected with HHV-6, as determined by PCR analyses, intracellular monoclonal antibody staining, and presence of virus in culture supernatants. However, HHV-6-infected DC demonstrated neither cytopathic changes nor functional defects. Interestingly, HHV-6 markedly suppressed HIV replication and syncytium formation in coinfected DC cultures. This HHV-6-mediated anti-HIV effect was DC specific, occurred when HHV-6 was added either before or after HIV, and was not due to decreased surface expression or function of CD4, CXCR4, or CCR5. Conversely, HIV had no demonstrable effect on HHV-6 replication. These findings suggest that HHV-6 may protect DC from HIV-induced cytopathicity in AIDS patients. We also demonstrate that interactions between HIV and herpesviruses are complex and that the observable outcome of dual infection is dependent on the target cell type.
Human herpesvirus 6 (HHV-6) is a betaherpesvirus and was first discovered in 1986 (54). Primary infection with HHV-6 causes the childhood illness roseola (also known as exanthem subitum) (65), as well as other childhood febrile illnesses (50), and nearly ubiquitous infection occurs by the age of 3 years (30, 46). Reactivation of HHV-6 during immunosuppression (e.g., after transplantation and during AIDS), a common feature of human herpesviruses as a group, has been linked to a variety of other diseases and pathologic processes. These include rejection of transplanted kidneys (43), chronic bone marrow suppression (17), interstitial pneumonitis (15), retinitis (52), encephalitis (18), and active widespread disseminated infection (2, 16, 26). In particular, because HHV-6 has been implicated as a cofactor in the immunopathogenesis of AIDS (7, 36), interactions between HHV-6 and human immunodeficiency virus (HIV) have been intensely studied.
Although HHV-6 was first reported as a B-cell-tropic virus (54), it soon became clear that the predominant cell type infected by HHV-6 is the CD4+ T cell (TC) (40, 61). This led Lusso, Gallo, and colleagues to perform a series of HHV-6–HIV coinfection studies with a variety of CD4+ and CD4− cells (35, 37–39). They found that HHV-6 and HIV could coinfect CD4+ TC in a synergistic manner (35) and that HHV-6 could induce CD4 expression on CD8+ TC, NK cells, and γ/δ TC and thereby render these cells susceptible to HIV infection (37–39). Other investigators have supported the concept that HHV-6 and HIV could synergistically enhance viral replication in coinfected cells (21, 24, 33, 57). However, other research groups have demonstrated that HHV-6 is capable of suppressing HIV replication (12, 31, 32, 47). The reasons for these discrepancies are unclear but may be related to cell types, viral strains, and doses of viruses used for the experiments.
Dendritic cells (DC) are bone marrow-derived potent antigen-presenting cells, present in lymphoid and nonlymphoid tissues, that are critical for the generation of primary and secondary immune responses (3). Although no previous studies have examined HHV-6 infection in DC, numerous investigators have implicated DC in the immunopathogenesis of HIV disease (for recent reviews, see references 9, 63, and 67). For example, Langerhan’s cells (prototypic nonlymphoid DC of the epidermis and genital mucosal epithelium) have been proposed to be the first cell type infected following mucosal exposure to HIV (5, 49, 58, 59, 66). DC are also extremely efficient at transmitting HIV to CD4+ TC during the generation of antigen-specific immune responses (5, 11, 48), and thus DC may be important in the depletion of TC as observed in AIDS patients (22, 62). Since DC serve a key function within the immune system, it has also been postulated that DC dysfunction contributes to the onset and maintenance of immune system dysregulation observed in HIV-infected individuals (41, 42).
We therefore studied HHV-6–HIV interactions by using immature DC propagated from plastic-adherent peripheral blood mononuclear cells (PBMC). The ability to generate DC from human blood in the presence of stimulating and differentiating cytokines (e.g., granulocyte-macrophage colony-stimulating factor [GM-CSF] and interleukin-4 [IL-4]) has provided an opportunity to perform detailed studies on DC biology with large numbers of relatively pure cells (53, 55). We demonstrate that HHV-6 can infect DC and that HHV-6 infection markedly suppresses HIV replication in coinfected DC cultures. The mechanism of this suppression is explored and the possible clinical implications of our findings are discussed.
MATERIALS AND METHODS
Preparation of cells.
DC were propagated from adult plastic-adherent PBMC as previously described (5). Briefly, PBMC from healthy blood donors were resuspended in RPMI 1640 (Gibco Laboratories, Grand Island, N.Y.) supplemented with 10% heat-inactivated fetal calf serum (Biofluids, Rockville, Md.), 100 U of penicillin (Gibco) per ml, 100 μg of streptomycin (Gibco) per ml, 2 mM l-glutamine (Gibco), 10 mM HEPES (Gibco), and 5 × 10−5 M 2-mercaptoethanol (Sigma Chemical Co., St. Louis, Mo.) (complete medium) at 5 × 106 to 8 × 106 cells/ml and placed into 35-mm-diameter tissue culture plates (Becton Dickinson Labware, Lincoln Park, N.J.) for 2 h at 37°C. Nonadherent cells were gently drawn off, and fresh complete media were returned to culture wells supplemented with 1,000 U of recombinant human GM-CSF (rhGM-CSF) (Immunex Corp., Seattle, Wash.) per ml and 1,000 U of rhIL-4 (R&D Systems, Minneapolis, Minn.) per ml. Half of the total volume of medium was replaced with fresh complete medium and cytokines every other day. On day 7, DC were harvested and washed, and contaminating TC, macrophages, NK cells, and B cells were removed from CD3− CD14− CD16− CD19− cells (i.e., DC) by immunomagnetic bead separation as described previously (5). DC isolated by this method were regularly >99% pure; the morphologic, phenotypic, and functional characteristics of these DC populations have been characterized in detail previously (5).
To obtain macrophages, highly purified monocytes were elutriated by centrifugation of PBMC from healthy blood donors, resuspended in complete medium supplemented with 1,000 U of rhGM-CSF per ml alone, and placed into 35-mm-diameter tissue culture plates at 106/ml. Half of the total volume of medium was replaced with fresh complete medium and rhGM-CSF every other day. On day 7, cells were scraped from the culture dishes, washed, and used for infection experiments.
To obtain CD4+ TC, PBMC were washed, resuspended in Hanks balanced salt solution supplemented with 10% fetal calf serum, and placed into 75-cm2 plastic culture flasks (Costar) for 1 h at 37°C. Nonadherent cells were drawn off and were enriched for CD4+ TC by negative selection with a commercially prepared monoclonal antibody (MAb) cocktail/complement reagent (Lympho-Kwik; One Lambda Inc., Los Angeles, Calif.) as recommended by the manufacturer.
For some experiments, 106 PBMC or CD4+ TC per ml were cultured in complete medium supplemented with 2 μg of phytohemagglutinin (PHA; Sigma) per ml for 3 days, harvested, washed, and used for infection experiments or 50% tissue culture infective dose assays.
Viruses and infection protocols.
All viruses were purchased from Advanced Biotechnologies Inc. (Columbia, Md.). Direct-pelleted HHV-6Z29 (variant B of HHV-6) and HHV-6U1102 (variant A of HHV-6) were used at a multiplicity of infection (MOI) of 0.0001 to 0.1 and 0.002, respectively. Direct-pelleted HIVBaL (a macrophage-tropic strain of HIV-1) and direct-pelleted HIVIIIB (a TC-tropic strain of HIV-1) were used at an MOI of 0.005 to 0.01 and 0.05 to 0.1, respectively. For infection, target cells (i.e., DC, macrophages, or PHA-stimulated PBMC) were resuspended in complete medium supplemented with cytokines (GM-CSF and IL-4 for DC and GM-CSF for macrophages) at 2 × 106/ml, inoculated with either HHV-6 or HIV at a variety of MOIs (as listed above), and incubated overnight at 37°C. This culture period was assigned the designation of day −1 to day 0. The cells were then washed three times in 50-ml volumes and resuspended in cytokine-supplemented complete medium (GM-CSF and IL-4 for DC, GM-CSF for macrophages, and 10 U of rhIL-2 [Boehringer Mannheim, Indianapolis, Ind.] per ml for PHA-stimulated PBMC) at 106 cells/ml. Half the total volume of cultures was removed, stored at −70°C, and replaced with fresh medium and cytokines every other day. In most coinfection experiments, HHV-6 was inoculated 2 days before or after HIV infection.
To determine whether infectious HHV-6 was required to suppress HIV replication, HHV-6 was either heat inactivated for 30 min at 56°C or neutralized with MAb prior to inoculation onto target cells. For neutralization studies, the murine neutralizing anti-HHV-6 MAb OHV3 (44) was serially diluted and added to 4 × 105 HHV-6Z29 infectious virions in 25 μl of diluted MAb. These mixtures were incubated at 37°C for 1 h. HHV-6Z29 was also incubated with the murine nonneutralizing anti-HHV-6 MAb OHV1 (45) in a similar manner. The MAbs were kind gifts of Koichi Yamanishi, Osaka, Japan. Additionally, MAb solutions were incubated in the absence of HHV-6 and then added directly to DC cultures to assess the direct anti-HIV effects of the MAbs.
Assays to determine infection.
HHV-6 infection in DC was assessed by PCR, immunofluorescence (IF) staining, and examination of culture supernatants for infectious virus. For PCR, DNA was extracted from cells on days 1, 3, 7, and 14 following HHV-6 infection by using a kit as recommended by the manufacturer (Stratagene, La Jolla, Calif.). The presence of HHV-6-specific DNA was examined by PCR with previously published primers specific for an immediate-early gene of HHV-6 (64). The cycling conditions were 23 cycles of denaturation for 1 min at 90°C, annealing for 2 min at 62°C, and polymerization for 3 min at 72°C. Amplified PCR products were hybridized to an excess of 32P-end-labeled internal probe (5′-TTCAGACCCGGTCTCTACAACTACTGAGTC-3′). Following hybridization, the samples were electrophoresed on 4% polyacrylamide gels, dried, and developed for 4 to 24 h (Kodak BIO-MAX films). Purified HHV-6 DNA (Advanced Biotechnologies Inc.) was used as positive PCR control DNA.
To specifically identify HHV-6-infected DC, two-color IF analysis was performed. DC were harvested on day 7 following infection, washed, cytospun onto glass slides (20,000 cells/slide), and fixed for 10 min in cold acetone. They were then incubated with the anti-HHV-6 MAb OHV3 at a dilution of 1:100 for 1 h, washed three times, incubated for 30 min with biotinylated rat anti-mouse immunoglobulin G2a (IgG2a) MAb (Pharmingen, San Diego, Calif.) at a dilution of 1:100, washed three times, and finally incubated for 30 min with a mixture of Texas Red-conjugated streptavidin (Pharmingen) at a final dilution of 1:100 and fluorescein isothiocyanate (FITC)-conjugated mouse anti-human CD1a at a final dilution of 1:10. Finally, the slides were washed three times and examined with an IF microscope. All incubations were performed at room temperature in a wet chamber protected from visible light. HHV-6-infected DC incubated with isotype-matched MAbs directed against irrelevant antigens and HHV6-uninfected DC incubated with HHV-6-specific MAbs were used as negative controls for all IF assays.
Culture supernatants from HHV-6-infected DC were assessed for infectious HHV-6 by inoculating supernatants onto susceptible target cells and monitoring for HHV-6 Ag expression and cytopathic effects. Briefly, cell-free supernatants from HHV-6-infected DC were collected, serially diluted, and placed into cultures of PHA-stimulated CD4+ TC for 2 weeks. IF staining for expression of HHV-6 antigens as described above was performed on target cells, and the 50% tissue culture infective dose end point was calculated by the method of Reed and Muench (51).
Productive HIV infection was monitored by measuring HIV-1 p24 protein levels in culture supernatants (collected as described above) by a radioimmunofluorescence assay (RIA; DuPont, Wilmington, Del.) as recommended by the manufacturer.
Assessment of viability, cellular proliferation, and immune function of HHV-6-infected DC.
By using trypan blue exclusion and a hemocytometer, DC viability was assessed by counting live cells at various time points following infection. To assess the effects of HHV-6 on cellular proliferation, DC were harvested 7 days after HHV-6 infection, washed, counted, and placed back into culture for 2 days. The cells were pulsed with 1 mCi of [3H]thymidine 30 h later and harvested 16 to 18 h later, and thymidine incorporation was detected with a β-counter. To assess APC function, DC were harvested 7 days after HHV-6 infection, washed, irradiated (2,000 rads, 137Cs source), and tested for their ability to stimulate the proliferation of allogeneic CD4+ TC. CD4+ TC (105) were resuspended in complete medium and cocultured with different numbers of HHV-6-infected or uninfected DC. Cultures were performed in triplicate in 96-well flat-bottom wells (Costar) and incubated in a humidified 5% CO2 atmosphere at 37°C for 6 days. The cultures were pulsed with 1 mCi of [3H]thymidine on day 5.5 and harvested 16 to 18 h later, and thymidine incorporation was detected with a β-counter.
Cell surface expression and function of CD4, CXCR4, and CCR5 on HHV-6-infected DC.
To determine whether HHV-6 could affect CD4 or HIV coreceptor expression, DC were harvested 7 days after HHV-6 infection and washed, and surface expression for these Ags was determined by Ab labeling and flow cytometry. A total of 2 × 105 to 5 × 105 DC were resuspended in phosphate-buffered 0.1% saline–bovine serum albumin–0.01% sodium azide (Fisher Scientific Co., Fair Lawn, N.J.) containing either FITC-conjugated mouse anti-human CD4 MAbs (Becton Dickinson, San Jose, Calif.), unconjugated rabbit anti-human CXCR4 polyclonal IgG, or unconjugated rabbit anti-human CCR5 polyclonal IgG (the last two Abs have been previously characterized [66]). Each Ab solution was diluted to 10 μg/ml and incubated with DC for 1 h. FITC-labeled cells (i.e., DC incubated with anti-CD4 MAbs) were then washed and analyzed by flow cytometry with a FACScan (Becton Dickinson) equipped with CellQuest software (Becton Dickinson). Propidium iodide-permeable cells were excluded from all analyses. CXCR4- and CCR5-immunolabeled cells were further incubated with biotinylated goat F(ab′)2 anti-rabbit IgG (Caltag Labs, San Francisco, Calif.) at a dilution of 1:50 for 30 min, washed, and incubated with FITC-conjugated streptavidin (Caltag) at a dilution of 1:50 for an additional 30 min. The cells were then washed and examined by flow cytometry as above. All incubations were performed in V-bottom 96-well plates at 4°C and protected from visible light. HHV-6-infected DC incubated with either isotype-matched MAbs directed against irrelevant Ags or preimmune rabbit serum and HHV-6-uninfected DC incubated with CD4- and HIV coreceptor-specific Abs were used as controls for all flow-cytometric experiments.
To assess the function of cell surface CXCR4 and CCR5, DC were harvested 7 days after HHV-6 infection, washed, and cocultured with 12E1 cells infected with vaccinia virus constructs expressing either monocytotropic or TC line-tropic HIV-1 envelope proteins as described previously (66). Briefly, 12E1 cells were infected with recombinant vaccinia viruses engineered to express envelope genes isolated from HIVIIIB, HIVJR-FL, or HIVBaL strains at 10 PFU/cell. At 5 h later, 105 vaccinia virus-infected 12E1 cells were mixed with 105 HHV-6-infected or uninfected DC and cocultured overnight. The formation of multinucleated syncytia was used as a measurement of HIV-1 envelope-mediated cell fusion. Syncytium formation could be blocked by anti-CD4 and anticoreceptor antibodies (66). The CD4+ CXCR4+ CCR5+ cell line PM1 was used as a positive control for these experiments (14).
RESULTS
HHV-6 infects DC.
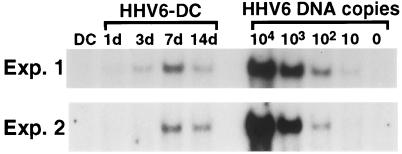
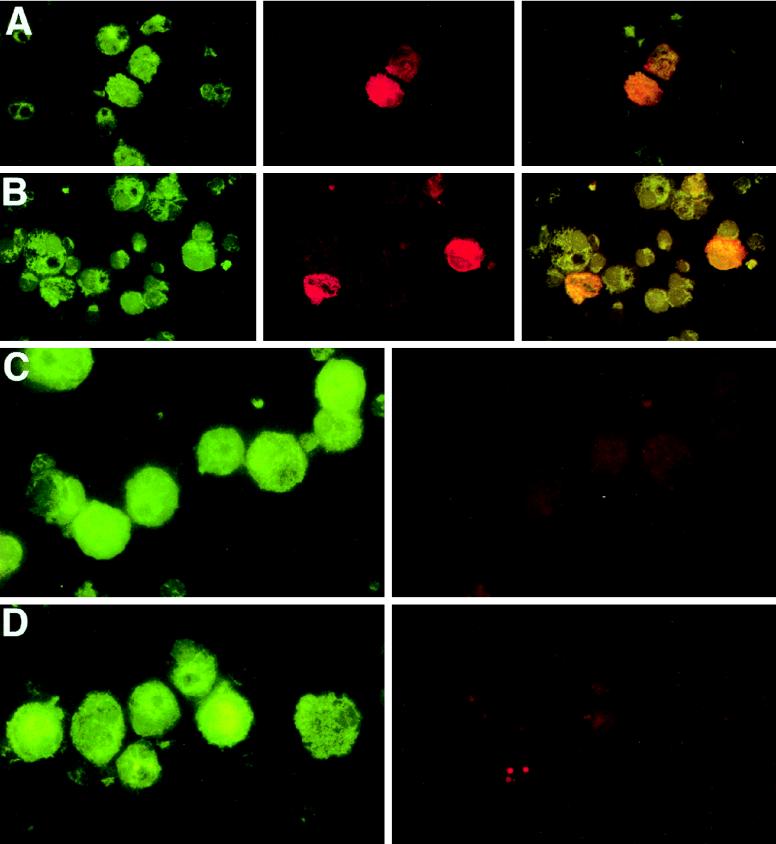
HHV-6 infects a wide variety of cell types (7), although infection in DC has not been previously studied. To evaluate the ability of HHV-6 to replicate in purified DC populations, DC were propagated from adult PBMC in the presence of GM-CSF and IL-4 as previously described (5). The DC were exposed overnight to two different HHV-6 strains at a variety of MOIs, excess virus was washed away, and the cells were placed back into culture. As detected by PCR with HHV-6-specific primers, viral DNA was detected in DC in increasing amounts, with the peak level of viral DNA being detected on day 7 after infection (Fig. 1). Demonstrable viral DNA was still present 14 days after infection (Fig. 1). DC could be infected with both a prototypic variant A strain of HHV-6 (i.e., HHV6U1102) (results not shown) and a prototypic variant B strain of HHV-6 (i.e., HHV-6Z29) (Fig. 1 and 2). HHV-6 infection was also assessed by IF staining for lytic-phase HHV-6 proteins. On day 7 after infection, productively infected DC could be visualized by this method (∼2% of total CD1a+ cells) (Fig. 2). Importantly, no HHV6+ CD1a− cells were detected by IF. It is possible that more DC were latently infected by HHV-6 (and therefore not detectable by our MAb staining), as is often the case for herpesvirus infection of other cell types. In addition, infectious virus could be recovered from DC culture supernatants as detected by cytopathic effects and IF staining in PHA-stimulated PBMC inoculated with supernatant from HHV-6-infected DC cultures (see below). Thus, we have demonstrated by several criteria that DC are susceptible to HHV-6 infection in vitro.
FIG. 1.
HHV-6 infects DC. DC were propagated from either adherent PBMC (Exp. 1) or elutriated monocytes (Exp. 2) in the presence of GM-CSF and IL-4, purified, and exposed overnight to HHV-6Z29 at an MOI of 0.1. Excess virus was washed out, and the cells were placed back into culture. DNA was extracted from the cells at the indicated time points, and PCR was performed to amplify HHV-6-specific sequences. Purified HHV-6 virions were used as positive PCR controls. Peak infection was detected on day 7 following HHV-6 exposure. The results shown are representative of at least five separate experiments.
FIG. 2.
HHV-6 infects DC. DC were propagated from either adherent PBMC (A and C) or elutriated monocytes (B) in the presence of GM-CSF and IL-4, purified, and exposed overnight to HHV6Z29 at an MOI of 0.1. Excess virus was washed out, and cells were placed back into culture. Uninfected DC were cultured in parallel (D). The cells were cytospun onto glass slides 7 days after infection, fixed, and incubated with anti-CD1a MAbs (green [A to D]), anti-HHV-6 MAbs (red [A, B, and D]), or isotype control MAbs (red [C]). Yellow cells (A and B) represent CD1a+ DC productively infected with HHV-6.
Viability, cellular proliferation, and immune function of HHV-6-infected DC.
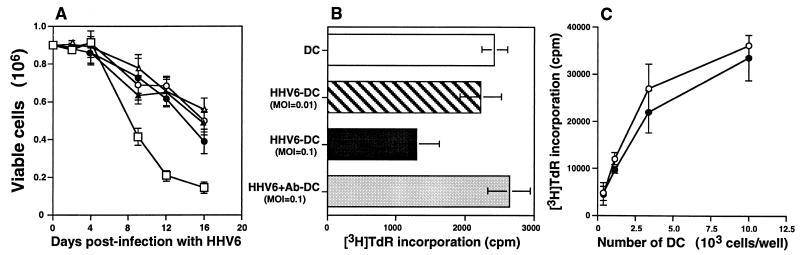
HHV-6 is cytopathic to many cell types (7); therefore, we examined the viability of DC after HHV-6 infection. The viability of DC infected with MOIs from 0.0001 to 0.01 was not different from the viability of uninfected control DC cultured in parallel; accelerated cell death was observed only when HHV-6-infected DC were infected with a high titer of virus (MOI = 0.1) (Fig. 3A). HHV-6 infection has also been reported to decrease cellular proliferation (23). We found that HHV-6 decreased DC proliferation slightly yet only when infected at a high MOI (0.1) (Fig. 3B). HHV-6 can induce defects in monocyte function as well (8). To determine whether HHV-6 could induce defects in DC immune function, we tested the ability of HHV-6-infected DC to stimulate allogeneic CD4+ TC in a mixed lymphocyte reaction. As shown in Fig. 3C, DC infected with HHV-6 at an MOI of 0.01 stimulated allogeneic TC as strongly as uninfected control DC did in a 6-day coculture assay. Interestingly, HHV-6-infected DC transmitted infection and induced cytopathic effects in cocultured allogeneic CD4+ TC when the cocultures were continued for 10 to 14 days (results not shown). This ability of HHV-6-infected DC to retain TC-stimulating potential and to transmit a vigorous cytopathic viral infection to cocultured TC is similar to the ability of HIV-exposed DC to transmit virus to TC during the process of immune system activation (5, 11, 48, 49).
FIG. 3.
Viability, cellular proliferation, and immune function of HHV-6-infected DC. Purified DC were exposed overnight to HHV-6 (variety of MOIs for panels A and B; MOI of 0.01 for panel C) or to HHV-6 pretreated with neutralizing anti-HHV6 MAb (B), washed, and placed back into culture. (A) Aliquots of viable cells were counted on the indicated days. (B) DC were harvested 7 days after HHV-6 infection, replated with an equal number of cells/well, and pulsed for 16 h with [3H]thymidine to determine cellular proliferation. (C) DC infected with HHV-6 for 7 days were harvested and cocultured with 105 allogeneic CD4+ T cells for 6 days. The cells were pulsed with [3H]thymidine for the last 16 h of culture to determine cellular proliferation. Values represent means and standard deviations in triplicate cultures. The results shown are representative of at least three separate experiments. □, MOI = 0.1; ●, MOI = 0.01; ▵, MOI = 0.001; ▴, MOI = 0.0001; ○, no HHV-6.
HHV-6 suppresses HIV replication in coinfected DC cultures.
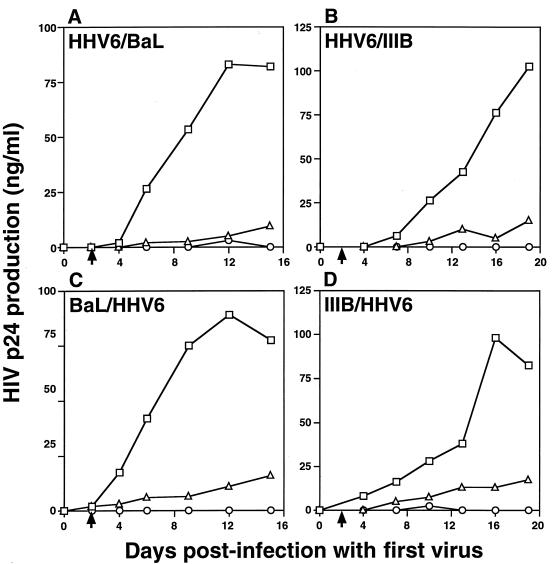
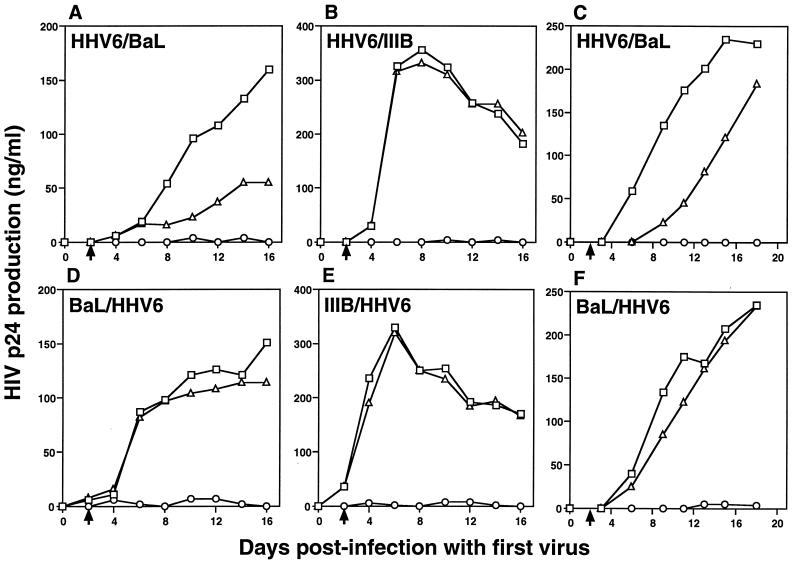
HHV-6 dramatically suppressed HIV replication in coinfected DC cultures. Both HHV-6U1102 and HHV-6Z29 exhibited anti-HIV effects, and both HIVIIIB and HIVBaL were suppressed by HHV-6 (Fig. 4). This HHV-6-mediated suppressive effect on HIV replication was observed when DC were inoculated with HHV-6 either 2 days before or 2 days after HIV inoculation (Fig. 4). The cell viability of coinfected cultures was not significantly different from that of cultures infected with either virus alone or of uninfected control DC (results not shown). However, HHV-6 at high MOI protected DC from HIV-induced syncytium formation, which was readily observed in DC cultures infected with HIV alone 1 to 2 weeks after infection (see below). Interestingly, the pattern and magnitude of the HHV-6-mediated HIV suppression was specific for DC cultures. Although preinfection of PHA-stimulated PBMC or macrophages with HHV-6 had some suppressive effects on the replication of HIVBaL (Fig. 5A and C), these effects were not observed with HIVIIIB (Fig. 5B) and were not observed if HHV-6 inoculation occurred after HIV inoculation (Fig. 5D to F).
FIG. 4.
HHV-6 dramatically suppresses HIV replication in coinfected DC cultures. (A and B) Purified DC were exposed overnight to HHV-6Z29 at an MOI of 0.1, washed, placed back into culture for 2 days, and exposed to HIVBaL (A) or HIVIIIB (B) at an MOI of 0.1 (arrows). (C and D) Purified DC were exposed overnight to HIVBaL (C) or HIVIIIB (D) at an MOI of 0.1, washed, placed back into culture for 2 days, and exposed to HHV-6Z29 at an MOI of 0.1 (arrows). Culture supernatants were assessed for HIV-1 p24 content every other day by RIA. The results shown are representative of at least five separate experiments. □, HIV alone; ▵, coinfection; ○, HHV-6 alone.
FIG. 5.
Pattern of HIV replication in PHA-stimulated PBMC and macrophages coinfected with HHV-6. PBMC were activated with PHA for 3 days prior to infection and maintained in media containing IL-2 following infection. Macrophages were propagated from elutriated monocytes cultured for 7 days in the presence of GM-CSF and maintained in media containing GM-CSF following infection. (A to C) PHA-stimulated PBMC (A and B) or macrophages (C) were exposed overnight to HHV-6Z29 at an MOI of 0.1, washed, placed back into culture for 2 days, and exposed to HIVBaL (A and C) or HIVIIIB (B) at an MOI of 0.1 (arrows). (D to F) PHA-stimulated PBMC (D and E) or macrophages (F) were exposed overnight to HIVBaL (D and F) or HIVIIIB (E) at an MOI of 0.1, washed, placed back into culture for 2 days, and exposed to HHV-6Z29 at an MOI of 0.1 (arrows). Culture supernatants were assessed for HIV-1 p24 content every other day by RIA. The results shown are representative of at least three separate experiments. □, HIV alone; ▵, coinfection; ○, HHV-6 alone.
Mechanisms involved in the HHV-6-mediated suppression of HIV replication in DC.
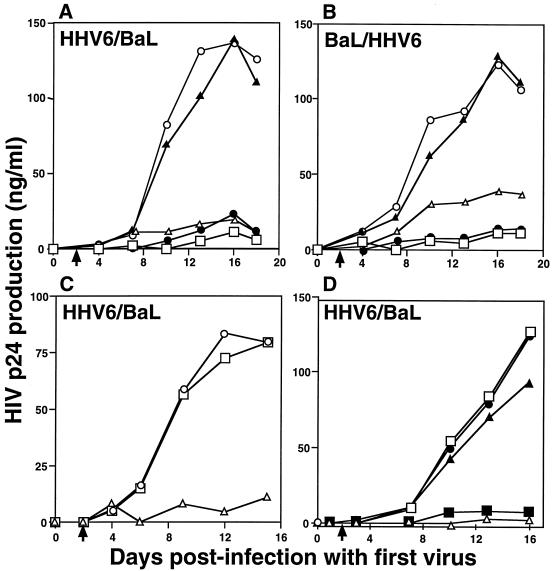
To more accurately determine the amount of HHV-6 necessary to suppress HIV replication, HHV-6 was diluted from an MOI of 0.1 to 0.0001 before inoculation. As shown in Fig. 6A and B, HHV-6 at MOIs of ≥0.001 was able to effectively block HIV replication. At the very low MOI of 0.001, this suppressive effect was more dramatic when HHV-6 was added to DC cultures before HIV addition (compare Fig. 6A and B). These data argue that only a relatively small number of HHV-6-infected DC are necessary to induce an anti-HIV effect in coinfected DC cultures.
FIG. 6.
Infectious HHV-6 is required to suppress HIV replication in coinfected DC cultures. (A, C, and D) Purified DC were exposed overnight to HHV-6Z29 at a variety of MOIs (A) or at an MOI of 0.1 (C and D), washed, placed back into culture for 2 days, and exposed to HIVBaL at an MOI of 0.1 (arrows). (B) Purified DC were exposed overnight to HIVBaL at an MOI of 0.1, washed, placed back into culture for 2 days, and exposed to HHV-6Z29 at a variety of MOIs (arrows). (C) Some DC were exposed to HHV-6 that had been heat inactivated at 56°C for 30 min. (D) Some DC were exposed to HHV-6 that had been preincubated with different concentrations of neutralizing anti-HHV-6 MAbs for 1 h at 37°C. HHV-6 preincubated with nonneutralizing anti-HHV-6 MAbs suppressed HIV replication in coinfected DC cultures (results not shown). Culture supernatants were assessed for HIV-1 p24 content every other day by RIA. The results shown are representative of at least three separate experiments. (A and B): □, MOI = 0.1; ●, MOI = 0.01; ▵, MOI = 0.001; ▴, MOI = 0.0001; ○, HIV alone. (C) □, HIV alone; ▵, coinfection; ○, coinfection with heat-inactivated HHV-6. (D) □, HIV alone; ▵, coinfection; ●, coinfection with HHV-6 preincubated with 500 μg of the HHV-6 neutralizing MAb OHV3 per ml; ▴, coinfection with HHV-6 pre-incubated with 5 μg of OHV3 per ml; ■, coinfection with HHV-6 preincubated with 0.5 μg of OHV3 per ml.
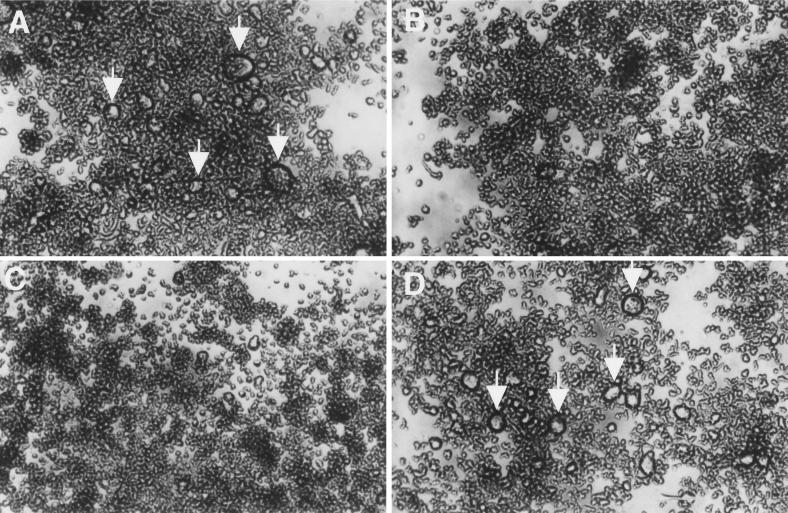
To address the possibility that suppression of HIV replication was due to factors (other than HHV-6) that may be present in viral stock solutions, HHV-6 was either heat inactivated or neutralized with MAbs before being inoculated onto DC. Heat-inactivated HHV-6 did not show any suppressive effects on HIV p24 antigen production, whereas equal amounts of nonheated virus suppressed HIV replication completely (Fig. 6C). Similarly, neutralization of infectious HHV-6 with an HHV-6-specific MAb (OHV3) blocked the ability of HHV-6 to suppress HIV in coinfected DC cultures (Fig. 6D). Incubating HHV-6 with dilute amounts of neutralizing MAb OHV3 (Fig. 6D), as well as incubating HHV-6 with the HHV-6-specific nonneutralizing MAb OHV1 (results not shown), had no effect on the ability of HHV-6 to suppress HIV. For these experiments, the p24 data correlated with the formation of syncytia in DC cultures. That is, DC infected with HIV alone and cultures coinfected with HIV and neutralized HHV-6 exhibited numerous syncytia (Fig. 7A and D); by contrast, syncytia were not observed in DC infected with HHV-6 alone or in cultures coinfected with HIV and HHV-6 pretreated with low concentrations of MAb (Fig. 7B and C). Thus, these data strongly suggest that infectious HHV-6 is required to mediate anti-HIV effects in coinfected DC.
FIG. 7.
Infectious HHV-6 is required to suppress HIV-induced syncytium formation in coinfected DC cultures. (A) Purified DC were exposed overnight to HIVBaL at an MOI of 0.1, washed, and placed back into culture. (B to D) Purified DC were exposed overnight to HHV-6Z29 at an MOI of 0.1, washed, placed back into culture for 2 days, and exposed to HIVBaL at an MOI of 0.1. (C and D) DC were exposed to HHV-6 that had been preincubated with 0.5 (C) or 500 (D) μg of neutralizing anti-HHV-6 MAbs per ml for 1 h at 37°C. Photographs of culture dishes were taken 14 days following infection and show numerous large HIV-induced syncytia (arrows) in panels A (no HHV-6) and D (neutralized HHV-6).
In studies where HHV-6 had been shown to facilitate HIV replication, upregulation of CD4 expression was demonstrated (37–39). As a possible mechanism for suppressing HIV, we postulated that HHV-6 may be downregulating CD4 and/or HIV coreceptor expression on the surface of DC. However, cell surface expression of CD4, CXCR4, and CCR5 was not changed on DC 7 days after HHV-6 infection compared to the situation with uninfected DC (data not shown). The functions of CXCR4 and CCR5, as determined in a fusion assay, were also not markedly different in HHV-6-infected and control DC (Table 1).
TABLE 1.
Syncytium formation between target cells expressing CXCR4/CCR5 and HIV env-expressing cells
| Expt | Target cells | No. of syncytiaa for HIV env-expressingb:
|
||
|---|---|---|---|---|
| IIIB | JR-FL | BaL | ||
| 1 | DC | 164 ± 4 | 159 ± 13 | 158 ± 25 |
| HHV-6–DCc | 157 ± 15 | 253 ± 10 | 188 ± 18 | |
| 2 | DC | 34 ± 9 | 244 ± 17 | 159 ± 22 |
| HHV-6–DCc | 93 ± 18 | 208 ± 15 | 147 ± 11 | |
| PM1 (positive control) | 300 ± 10 | 238 ± 22 | 201 ± 1 | |
Mean syncytium number ± standard deviation of triplicate wells after overnight coculture at 37°C.
12E1 cells infected with recombinant vaccinia virus expressing TC-tropic HIV env (e.g., HIVIIIB) fuse with target cells expressing CXCR4; 12E1 cells infected with recombinant vaccinia virus expressing macrophage-tropic HIV env (e.g., HIVJR-FL and HIVBaL) fuse with target cells expressing CCR5.
DC were harvested 7 days after infection with HHV-6 (MOI, 0.1).
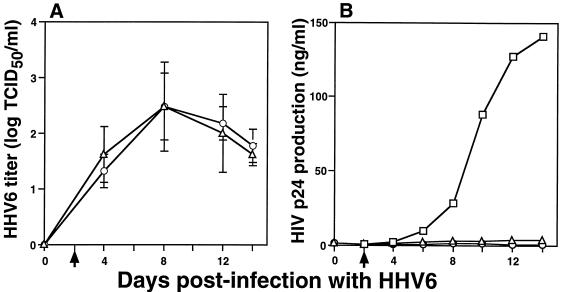
HIV does not suppress HHV-6 replication in coinfected DC cultures.
Since HHV-6 suppressed HIV replication, we next determined whether the reverse was true, i.e., whether HIV suppressed HHV6 replication. As shown in Fig. 8, this was not the case. HIV did not enhance or suppress HHV-6 replication in coinfected DC cultures. Also, comparable numbers of HHV-6-infected cells (∼2%) and HHV-6 Ag staining intensity were detected by IF in DC from coinfected cultures and in DC infected with HHV-6 alone.
FIG. 8.
HIV does not affect HHV-6 replication in coinfected DC cultures. Purified DC were exposed overnight to HHV-6Z29 at an MOI of 0.1, washed, placed back into culture for 2 days, and exposed to HIVBaL at an MOI of 0.1 (arrows). (A) Culture supernatants were assessed for infectious HHV-6 content every other day by a plaque assay with PHA-stimulated PBMC as targets. Values represent means and standard deviations in triplicate cultures. (B) Culture supernatants were assessed for HIV-1 p24 content every other day by RIA. The results shown are representative of at least three separate experiments. □, HIV alone; ▵, coinfection; ○, HHV-6 alone. TCID50, 50% tissue culture infective dose.
DISCUSSION
HHV6 has been previously shown to infect a wide variety of cell types, including TC, monocytes/macrophages, NK cells, transformed cervical epithelial cells, and cell lines of TC, B-cell, megakaryocyte, and glial-cell origin (1, 13, 25, 27, 37–40, 54, 61). There also has been a report of HHV-6 infection of tissue histiocytes (29, 34, 56) and a report suggesting that tumors of Langerhan’s cell histiocytosis contain HHV-6 DNA (28). In this study, we demonstrate that HHV-6 can also infect DC in vitro. Unlike many other cells infected with HHV-6, DC showed no cytopathic or functional changes at low HHV-6 MOIs. Interestingly, HHV-6-infected DC could strongly stimulate allogeneic CD4+ lymphocytes and could transmit virus to TC during immune system activation. DC-mediated viral infection of TC has also been previously reported for HIV (5, 11, 48). We speculate that TC infection with other viruses may also be transmitted by DC during antigen-specific activation, perhaps counteracting beneficial effects of DC-mediated induction of primary antiviral CD8+ TC responses (4). Further study is needed to determine whether this is a general pathway for viral infection of TC or whether it is restricted to certain viruses.
Because of a predominant tropism for CD4+ TC, HHV-6 has also been suggested to be a cofactor in the progressive loss of CD4+ TC which occurs in AIDS patients (7, 36). There is substantial in vitro (21, 24, 33, 35, 37–39, 57) and in vivo (2, 16, 26) evidence for this theory; however, other studies have not supported it (12, 19, 31, 32, 47, 60). Viral strain and dose differences may account for some of the discrepancies in the laboratory studies, whereas differences in the clinical studies with HIV-infected individuals may be influenced by drug histories or other unknown confounding variables. We show here that HHV-6 dramatically suppresses HIV replication in coinfected DC cultures and that HHV-6 protects DC from HIV-induced syncytium formation (Fig. 4 and 7). By contrast, HIV infection had no effect on HHV-6 infection in DC (Fig. 8). Although DC can serve as targets for HIV infection in vivo (20, 41) and in vitro (5, 58), most studies have demonstrated that the absolute number and function of DC present in tissues from HIV-infected patients are relatively normal (6, 10). A possible implication of our findings is that HHV-6 is protecting DC from HIV-induced dysfunction and death in vivo. Thus, to determine the in vivo relevance of our data, it will be important to determine whether HHV6-infected DC can be detected in tissues from healthy as well as HIV-infected individuals.
Interestingly, the pattern of HHV-6-mediated anti-HIV effects observed in DC cultures was not observed in coinfected macrophages or PHA-stimulated PBMC (compare Fig. 4 and 5). Although preinfection of macrophages and PHA-stimulated PBMC with HHV-6 did suppress the subsequent replication of HIVBaL somewhat, the suppression was not as dramatic as that observed in DC. Unlike DC cultures, neither HIVBaL nor HIVIIIB was suppressed in macrophages and PBMC when HHV-6 was added 2 days after HIV infection. These data suggest that the cell type and viral strain affect the observable outcome caused by dual infection with HIV and HHV-6. In part, this may explain some of the different results obtained in previous experimental and clinical studies examining the relationship between HIV and HHV-6.
The mechanism by which HHV-6 suppresses HIV replication in coinfected DC cultures is not clear. We show that relatively small amounts of infectious HHV-6 are required; HHV-6 MOIs of <0.001, heat-inactivated HHV-6, and HHV-6 neutralized with MAbs fail to suppress HIV replication (Fig. 6 and 7). Decreased expression or function of CD4 or HIV coreceptors do not appear to be involved (Table 1). Based on these results, we believe that there are at least two additional possible mechanisms in coinfected DC cultures. (i) HHV-6 could be blocking HIV transcription and translation in individually coinfected cells (i.e., the intracellular hypothesis). Because the sensitivity of our assay to detect productively infected cells by IF was low (∼2% of total cells), this hypothesis could not be tested directly. (ii) HHV-6-infected DC may be secreting an anti-HIV factor. This hypothesis is supported by preliminary experiments in our laboratory, where we have found that HHV-6-infected DC can suppress HIV replication in DC when these two DC populations are separated by 0.45-μm-pore-size membranes that restrict cell passage but allow the passage of small soluble factors such as cytokines and viruses (2a). This hypothesis does not necessarily require coinfection of individual cells. Understanding the exact mechanisms involved in HHV-6-mediated suppression of HIV in DC cultures will require additional study. Importantly, we have demonstrated that interactions between HIV and herpesviruses are complex and that the observable outcome induced by dual infection is dependent on the target cell type.
ACKNOWLEDGMENTS
We thank Sandra S. Cohen for providing technical assistance, Harry Schaefer for preparing the figures, and Kuan-Teh Jeang and Jonathan Vogel for giving a critical review of the manuscript.
REFERENCES
- 1.Ablashi D V, Lusso P, Hung C L, Salahuddin S Z, Josephs S F, Llana T, Kramarsky B, Biberfeld P, Markham P D, Gallo R C. Utilization of human hematopoietic cell lines for the propagation and characterization of HBLV (human herpesvirus 6) Int J Cancer. 1988;42:787–791. doi: 10.1002/ijc.2910420526. [DOI] [PubMed] [Google Scholar]
- 2.Ablashi D V, Marsh S, Kaplan M, Whitman J E, Pearson G R. HHV-6 infection in HIV-infected asymptomatic and AIDS patients. Intervirology. 1998;41:1–9. doi: 10.1159/000024909. [DOI] [PubMed] [Google Scholar]
- 2a.Asada, H., and A. Blauvelt. Unpublished results.
- 3.Banchereau J, Steinman R M. Dendritic cells and the control of immunity. Nature. 1998;392:245–252. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- 4.Bhardwaj N. Interactions of viruses with dendritic cells: a double-edged sword. J Exp Med. 1997;186:795–799. doi: 10.1084/jem.186.6.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blauvelt A, Asada H, Saville M W, Klaus-Kovtun V, Altman D J, Yarchoan R, Katz S I. Productive infection of dendritic cells by HIV-1 and their ability to capture virus are mediated through separate pathways. J Clin Investig. 1997;100:2043–2053. doi: 10.1172/JCI119737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blauvelt A, Clerici M, Lucey D R, Steinberg S M, Yarchoan R, Walker R, Shearer G M, Katz S I. Functional studies of epidermal Langerhans cells and blood monocytes in HIV-infected persons. J Immunol. 1995;154:3506–3515. [PubMed] [Google Scholar]
- 7.Braun D K, Dominguez G, Pellett P E. Human herpesvirus 6. Clin Microbiol Rev. 1997;10:521–567. doi: 10.1128/cmr.10.3.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burd E M, Carrigan D R. Human herpesvirus 6 (HHV-6)-associated dysfunction of blood monocytes. Virus Res. 1992;29:79–90. doi: 10.1016/0168-1702(93)90127-9. [DOI] [PubMed] [Google Scholar]
- 9.Cameron P, Pope M, Granelli-Piperno A, Steinman R M. Dendritic cells and the replication of HIV-1. J Leukoc Biol. 1996;59:158–171. doi: 10.1002/jlb.59.2.158. [DOI] [PubMed] [Google Scholar]
- 10.Cameron P U, Forsum U, Teppler H, Granelli-Piperno A, Steinman R M. During HIV-1 infection most blood dendritic cells are not productively infected and can induce allogeneic CD4+ T cells clonal expansion. Clin Exp Immunol. 1992;88:226–236. doi: 10.1111/j.1365-2249.1992.tb03066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cameron P U, Freudenthal P S, Barker J M, Gezelter S, Inaba K, Steinman R M. Dendritic cells exposed to human immunodeficiency virus type-1 transmit a vigorous cytopathic infection to CD4+ cells. Science. 1992;257:383–387. doi: 10.1126/science.1352913. [DOI] [PubMed] [Google Scholar]
- 12.Carrigan D R, Knox K K, Tapper M A. Suppression of human immunodeficiency virus type 1 replication by human herpesvirus-6. J Infect Dis. 1990;162:844–851. doi: 10.1093/infdis/162.4.844. [DOI] [PubMed] [Google Scholar]
- 13.Chen M, Popescu N, Woodworth C, Berneman Z, Corbellino M, Lusso P, Ablashi D V, DiPaolo J A. Human herpesvirus 6 infects cervical epithelial cells and transactivates human papillomavirus gene expression. J Virol. 1994;68:1173–1178. doi: 10.1128/jvi.68.2.1173-1178.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cocchi F, DeVico A L, Garzino-Demo A, Arya S K, Gallo R C, Lusso P. Identification of RANTES, MIP1α, and MIP-1β as the major HIV-suppressive factors produced by CD8+ T cells. Science. 1995;270:1811–1815. doi: 10.1126/science.270.5243.1811. [DOI] [PubMed] [Google Scholar]
- 15.Cone R W, Hackman R C, Huang M L W, Bowden R A, Meyers J D, Metcalf M, Zeh J, Ashley R, Corey L. Human herpesvirus 6 in lung tissue from patients with pneumonitis after bone marrow transplantation. N Engl J Med. 1993;329:156–161. doi: 10.1056/NEJM199307153290302. [DOI] [PubMed] [Google Scholar]
- 16.Corbellino M, Lusso P, Gallo R C, Parravicini C, Galli M, Moroni M. Disseminated human herpesvirus 6 infection in AIDS. Lancet. 1993;342:1242. doi: 10.1016/0140-6736(93)92226-j. [DOI] [PubMed] [Google Scholar]
- 17.Drobyski W R, Dunne W M, Burd E M, Knox K K, Ash R C, Horowitz M M, Flomemberg M, Carrigan D R. Human herpesvirus-6 (HHV-6) infection in allogeneic bone marrow transplant recipients: evidence of a marrow suppressive role for HHV-6 in vivo. J Infect Dis. 1993;167:735–739. doi: 10.1093/infdis/167.3.735. [DOI] [PubMed] [Google Scholar]
- 18.Drobyski W R, Knox K K, Majewski A, Carrigan D R. Fatal encephalitis due to variant B human herpesvirus-6 infection in a bone marrow-transplant recipient. N Engl J Med. 1994;330:1356–1360. doi: 10.1056/NEJM199405123301905. [DOI] [PubMed] [Google Scholar]
- 19.Fairfax M R, Schacker T, Cone R W, Collier A C, Corey L. Human herpesvirus 6 DNA in blood cells of human immunodeficiency virus-infected men: correlation of high levels with high CD4 cell counts. J Infect Dis. 1994;169:1342–1345. doi: 10.1093/infdis/169.6.1342. [DOI] [PubMed] [Google Scholar]
- 20.Frankel S S, Wenig B M, Burke A P, Mannan P, Thompson L D, Abbondanzo S L, Nelson A M, Pope M, Steinman R M. Replication of HIV-1 in dendritic cell-derived syncytia at the mucosal surface of the adenoid. Science. 1996;272:115–117. doi: 10.1126/science.272.5258.115. [DOI] [PubMed] [Google Scholar]
- 21.Geng Y, Balachandran N, Josephs S F, Wood C. Identification and characterization of a human herpesvirus-6 gene segment that transactivates the human immunodeficiency virus type 1 promoter. J Virol. 1992;66:1564–1570. doi: 10.1128/jvi.66.3.1564-1570.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ho D D, Neumann A U, Perelson A S, Chen W, Leonard J M, Markovitz M. Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection. Nature. 1995;373:123–126. doi: 10.1038/373123a0. [DOI] [PubMed] [Google Scholar]
- 23.Horvat R T, Parmely M J, Chandran B. Human herpesvirus 6 inhibits the proliferative responses of human peripheral blood mononuclear cells. J Infect Dis. 1993;167:1274–1280. doi: 10.1093/infdis/167.6.1274. [DOI] [PubMed] [Google Scholar]
- 24.Horvat R T, Wood C, Balachandran N. Transactivation of human immunodeficiency virus promoter by human herpesvirus 6. J Virol. 1989;63:326–335. doi: 10.1128/jvi.63.2.970-973.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kempf W, Adams V, Whey N, Moos R, Schmid M, Avitabile E, Campadelli-Fiume G. CD68+ cells of monocyte/macrophage lineage in the environment of AIDS-associated and classic-sporadic Kaposi sarcoma are singly or doubly infected with human herpesviruses 7 and 6B. Proc Natl Acad Sci USA. 1997;94:7600–7605. doi: 10.1073/pnas.94.14.7600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Knox K K, Carrigan D R. Disseminated active HHV-6 infections in patients with AIDS. Lancet. 1994;343:577–578. doi: 10.1016/s0140-6736(94)91524-5. [DOI] [PubMed] [Google Scholar]
- 27.Kondo K, Kondo T, Okuno T, Takahashi M, Yamanishi K. Latent human herpesvirus 6 infection of human monocytes/macrophages. J Gen Virol. 1991;72:1401–1408. doi: 10.1099/0022-1317-72-6-1401. [DOI] [PubMed] [Google Scholar]
- 28.Leahy M A, Krejci S M, Friednash M, Stockert S S, Wilson H, Huff J C, Weston W L, Brice S L. Human herpesvirus 6 is present in lesions of Langerhans cell histiocytosis. J Investig Dermatol. 1993;101:642–645. doi: 10.1111/1523-1747.ep12371669. [DOI] [PubMed] [Google Scholar]
- 29.Levine P H, Jahan N, Murari P, Manak M, Jaffe E S. Detection of human herpesvirus 6 in tissues involved by sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease) J Infect Dis. 1992;166:291–295. doi: 10.1093/infdis/166.2.291. [DOI] [PubMed] [Google Scholar]
- 30.Levy J A, Ferro F, Greenspan D, Lennette E T. Frequent isolation of HHV-6 from saliva and high seroprevalence to the virus in the population. Lancet. 1990;335:1047–1050. doi: 10.1016/0140-6736(90)92628-u. [DOI] [PubMed] [Google Scholar]
- 31.Levy J A, Landay A, Lennette E T. Human herpesvirus 6 inhibits human immunodeficiency virus type 1 replication in cell culture. J Clin Microbiol. 1990;28:2362–2364. doi: 10.1128/jcm.28.10.2362-2364.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lopez C, Pellett P, Stewart J, Goldsmith C, Sanderlin K, Black J, Warfield D, Feorino P. Characteristics of human herpesvirus-6. J Infect Dis. 1988;157:1271–1273. doi: 10.1093/infdis/157.6.1271. [DOI] [PubMed] [Google Scholar]
- 33.Luca D D, Secchiero P, Bovenzi P, Rotola A, Caputo A, Monini P, Cassai E. Reciprocal in vitro interactions between human herpesvirus-6 and HIV-1 Tat. AIDS. 1991;5:1095–1098. doi: 10.1097/00002030-199109000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Luppi M, Barozzi P, Garber R, Maiorana A, Bonacorsi G, Artusi T, Trovato R, Marasca R, Torelli G. Expression of human herpesvirus-6 antigens in benign and malignant lymphoproliferative diseases. Am J Pathol. 1998;153:815–823. doi: 10.1016/S0002-9440(10)65623-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lusso P, Ensoli B, Markham P D, Ablashi D V, Salahuddin S Z, Tschachler E, Wong-Staal F, Gallo R C. Productive dual infection of human CD4+ T-lymphocytes by HIV-1 and HHV-6. Nature. 1989;337:370–373. doi: 10.1038/337370a0. [DOI] [PubMed] [Google Scholar]
- 36.Lusso P, Gallo R C. Human herpesvirus 6 in AIDS. Immunol Today. 1995;16:67–71. doi: 10.1016/0167-5699(95)80090-5. [DOI] [PubMed] [Google Scholar]
- 37.Lusso P, Garzino-Demo A, Crowley R W, Malnati M S. Infection of γ/δ T lymphocytes by human herpesvirus 6: transcriptional induction of CD4 and susceptibility to HIV infection. J Exp Med. 1995;181:1303–1310. doi: 10.1084/jem.181.4.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lusso P, Malnati M, Garzino-Demo A, Crowley R W, Long E O, Gallo R C. Infection of natural killer cells by human herpesvirus 6. Nature. 1993;362:458–462. doi: 10.1038/362458a0. [DOI] [PubMed] [Google Scholar]
- 39.Lusso P, Maria A D, Malnati M, Lori F, Rocco S E D, Baseler M, Gallo R C. Induction of CD4 and susceptibility to HIV-1 infection in CD8+ human T lymphocytes by human herpesvirus 6. Nature. 1991;349:533–535. doi: 10.1038/349533a0. [DOI] [PubMed] [Google Scholar]
- 40.Lusso P, Markham P D, Tschachler E, Di Marzo Veronese F, Salahuddin S Z, Ablashi D V, Pawha S, Krohn K J, Gallo R C. In vitro cellular tropism of human B-lymphotropic virus (human herpesvirus 6) J Exp Med. 1988;167:1659–1670. doi: 10.1084/jem.167.5.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Macatonia S E, Lau R, Patterson S, Pinching A J, Knight S C. Dendritic cell infection, depletion and dysfunction in HIV-infected individuals. Immunology. 1990;71:38–45. [PMC free article] [PubMed] [Google Scholar]
- 42.Meyaard L, Schuitemaker H, Miedema F. T-cell dysfunction in HIV infection: anergy due to defective antigen-presenting cell function? Immunol Today. 1993;14:161–164. doi: 10.1016/0167-5699(93)90279-T. [DOI] [PubMed] [Google Scholar]
- 43.Okuno T, Higashi K, Shiraki K, Yamanishi K, Takahashi M, Kokado Y, Ishibashi M, Takahara S, Sonoda T, Tanaka K, Baba K, Yabuuchi H, Kurata T. Human herpesvirus 6 infection in renal transplantation. Transplantation. 1990;49:519–522. doi: 10.1097/00007890-199003000-00009. [DOI] [PubMed] [Google Scholar]
- 44.Okuno T, Sao H, Asada H, Shiraki K, Takahashi M, Yamanishi K. Analysis of a glycoprotein of human herpesvirus 6 (HHV-6) using monoclonal antibodies. Virology. 1990;176:625–628. doi: 10.1016/0042-6822(90)90033-n. [DOI] [PubMed] [Google Scholar]
- 45.Okuno T, Shao H, Asada H, Shiraki K, Takahashi M, Yamanishi K. Analysis of human herpesvirus 6 glycoproteins recognized by monoclonal antibody OHV1. J Gen Virol. 1992;73:443–447. doi: 10.1099/0022-1317-73-2-443. [DOI] [PubMed] [Google Scholar]
- 46.Okuno T, Takahashi K, Balachandra K, Shiraki K, Yamanishi K, Takahashi M, Baba K. Seroepidemiology of human herpesvirus 6 infection in normal children and adults. J Clin Microbiol. 1989;27:651–653. doi: 10.1128/jcm.27.4.651-653.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pietroboni G R, Harnett G B, Farr T J, Bucens M R. Human herpesvirus type 6 (HHV-6) and its in vitro effect on human immunodeficiency virus (HIV) J Clin Pathol. 1988;41:1310–1312. doi: 10.1136/jcp.41.12.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pinchuk L M, Polacino P S, Agy M B, Klaus S J, Clark E A. The role of CD40 and CD80 accessory cell molecules in dendritic cell-dependent HIV-1 infection. Immunity. 1994;1:317–325. doi: 10.1016/1074-7613(94)90083-3. [DOI] [PubMed] [Google Scholar]
- 49.Pope M, Betjes M G H, Romani N, Cameron P U, Hoffman L, Gezelter S, Schuler G, Steinman R M. Conjugates of dendritic cells and memory T lymphocytes from skin facilitate productive infection with HIV-1. Cell. 1994;78:389–398. doi: 10.1016/0092-8674(94)90418-9. [DOI] [PubMed] [Google Scholar]
- 50.Pruksananonda P, Hall C B, Insel R A, McIntyre K, Pellet P E, Long C E. Primary human herpesvirus 6 infection in young children. N Engl J Med. 1992;326:1445–1452. doi: 10.1056/NEJM199205283262201. [DOI] [PubMed] [Google Scholar]
- 51.Reed L J, Muench H. A simple method of estimating fifty per cent endpoints. Am J Hyg. 1938;27:493–497. [Google Scholar]
- 52.Reux I, Fillet A M, Agut H, Katlama C, Hauw J J, Le-Hoang P. In situ detection of human herpesvirus 6 in retinitis associated with acquired immunodeficiency syndrome. Am J Ophthalmol. 1992;114:375–377. doi: 10.1016/s0002-9394(14)71814-8. [DOI] [PubMed] [Google Scholar]
- 53.Romani N, Gruner S, Brang D, Kampgen E, Lenz A, Trockenbacher B, Konwalinka G, Fritsch P O, Steinman R M, Schuler G. Proliferating dendritic cell progenitors in human blood. J Exp Med. 1994;180:83–93. doi: 10.1084/jem.180.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Salahuddin S Z, Ablashi D V, Markham P D, Josephs S F, Sturzenegger S, Kaplan M, Halligan G, Biberfeld P, Wong-Staal F, Kramarsky B, Gallo R C. Isolation of a new virus, HBLV, in patients with lymphoproliferative disorders. Science. 1986;234:596–601. doi: 10.1126/science.2876520. [DOI] [PubMed] [Google Scholar]
- 55.Sallusto F, Lanzavecchia A. Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by granulocyte/macrophage colony-stimulating factor plus interleukin 4 and downregulated by tumor necrosis factor α. J Exp Med. 1994;179:1109–1108. doi: 10.1084/jem.179.4.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Scheel M M, Rady P L, Tyring S K, Pandya A G. Sinus histiocytosis with massive lymphadenopathy: presentation as giant granuloma annulare and detection of human herpesvirus 6. J Am Acad Dermatol. 1997;37:643–646. doi: 10.1016/s0190-9622(97)70186-5. [DOI] [PubMed] [Google Scholar]
- 57.Sieczkowski L, Chandran B, Wood C. The human immunodeficiency virus tat gene enhances replication of human herpesvirus-6. Virology. 1995;211:544–553. doi: 10.1006/viro.1995.1436. [DOI] [PubMed] [Google Scholar]
- 58.Soto-Ramirez L E, Renjifo B, McLane M F, Marlink R, O’Hara C, Sutthent R, Wasi C, Vithayasai P, Vithayasai V, Apichartpiyakul C, Auewarakul P, Cruz V P, Chui D S, Osathanondh R, Mayer K, Lee T H, Essex M. HIV-1 Langerhans’ cell tropism associated with heterosexual transmission of HIV. Science. 1996;271:1291–1293. doi: 10.1126/science.271.5253.1291. [DOI] [PubMed] [Google Scholar]
- 59.Spira A I, Marx P A, Patterson B K, Mahoney J, Koup R A, Wolinsky S M, Ho D D. Cellular targets of infection and route of viral dissemination after an intravaginal inoculation of simian immunodeficiency virus into rhesus macaques. J Exp Med. 1996;183:215–225. doi: 10.1084/jem.183.1.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Spira T J, Bozeman L H, Sanderlin K C, Warfield D T, Feorino P M, Holman R C, Kaplan J E, Fishbein D B, Lopez C. Lack of correlation between human herpesvirus-6 infection and the course of human immunodeficiency virus infection. J Infect Dis. 1990;161:567–570. doi: 10.1093/infdis/161.3.567. [DOI] [PubMed] [Google Scholar]
- 61.Takahashi K, Sonoda S, Higashi K, Kondo T, Takahashi H, Takahashi M, Yamanishi K. Predominant CD4 T-lymphocyte tropism of human herpesvirus 6-related virus. J Virol. 1989;63:3161–3163. doi: 10.1128/jvi.63.7.3161-3163.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wei X, Ghosh S K, Taylor M E, Johnson V A, Emini E A, Deutsch P, Lifson J D, Bonhoeffer S, Nowak M A, Hahn B H, Saag M S, Shaw G M. Viral dynamics in human immunodeficiency virus type 1 infection. Nature. 1995;373:117–122. doi: 10.1038/373117a0. [DOI] [PubMed] [Google Scholar]
- 63.Weissman D, Fauci A S. Role of dendritic cells in immunopathogenesis of human immunodeficiency virus infection. Clin Microbiol Rev. 1997;10:358–367. doi: 10.1128/cmr.10.2.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yamamoto T, Mukai T, Kondo K, Yamanishi K. Variation of DNA sequence in immediate-early gene of human herpesvirus 6 and variant identification by PCR. J Clin Microbiol. 1994;32:473–476. doi: 10.1128/jcm.32.2.473-476.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yamanishi K, Okuno T, Shiraki K, Takahashi M, Kondo T, Asano Y, Kurata T. Identification of human herpesvirus-6 as a causal agent for exanthem subitum. Lancet. 1988;i:1065–1067. doi: 10.1016/s0140-6736(88)91893-4. [DOI] [PubMed] [Google Scholar]
- 66.Zaitseva M, Blauvelt A, Lee S, Lapham C K, Klaus-Kovtun V, Mostowski H, Manischewitz J, Golding H. Expression and function of CCR5 and CXCR4 on human Langerhans cells and macrophages: implications for HIV primary infection. Nat Med. 1997;3:1369–1375. doi: 10.1038/nm1297-1369. [DOI] [PubMed] [Google Scholar]
- 67.Zoeteweij J P, Blauvelt A. HIV-dendritic cell interactions promote efficient viral infection of T cells. J Biomed Sci. 1998;5:253–259. doi: 10.1007/BF02255856. [DOI] [PubMed] [Google Scholar]