Abstract
Background/Aim: Emergency medicine (EM) settings are very stressful, given the high workload, intense working environment, and prolonged working time. In turn, the rate of burnout and its three domains have been increasingly reported among healthcare workers (HCWs). Therefore, we conducted this meta-analysis to determine the prevalence and risk factors of burnout among EM HCWs. Methods: Six databases were searched in February 2023, yielding 29 articles (16,619 EM HCWs) reporting burnout or its three domains (emotional exhaustion “EE”, depersonalization “DP”, and personal accomplishment “PA”). The primary outcome was the prevalence of burnout and its domains, while secondary outcomes included the risk factors of high burnout, EE, DP, or low PA. Burnout rates were pooled across studies using STATA software. The prevalence was measured using the pooled effect size (ES), and the random-effects model was used when heterogeneity was encountered; otherwise, the fixed-effects model was used. Results: The prevalence of overall burnout was high (43%), with 35% of EM HCWs having a high risk of burnout. Meanwhile, 39%, 43%, and 36% of EM workers reported having high levels of EE and DP and low levels of PA, respectively. Country-specific changes in the rate of burnout were observed. The rate of high burnout, high EE, high DP, and low PA was higher during the COVID-19 pandemic as compared to the pre-pandemic period. The type of profession (nurses, physicians, residents, etc.) played a significant role in modifying the rate of burnout and its domains. However, gender was not a significant determinant of high burnout or its domains among EM workers. Conclusions: Burnout is a prevalent problem in emergency medicine practice, affecting all workers. As residents progress through their training years, their likelihood of experiencing burnout intensifies. Nurses are most affected by this problem, followed by physicians. Country-associated differences in burnout and its domains are evident.
Keywords: burnout, emotional exhaustion, personal accomplishment, depersonalization, emergency medicine
1. Introduction
Emergency medicine (EM) training and clinical practice are very stressful ventures [1]. Time is usually a critical consideration, and emergency physicians are expected to be well-versed in assessing and caring for surgical, medical, and trauma situations. It is sometimes considered “a young person’s specialty” due to the high intensity of the working environment. EM physicians are required to assess patients in a more constrained time window and make judgments under pressure, unlike departments such as outpatient. They are sometimes required to make crucial decisions with insufficient information, for instance, when the patient is unconscious [2]. As a result of these challenges, emergency services are the most hectic of the services offered in the hospital. This puts EM healthcare workers at risk of developing “burnout syndrome”.
Burnout refers to a three-dimensional response to long-term emotional as well as interpersonal pressures at work. The three dimensions of burnout are depersonalization (DP), emotional exhaustion (EE), and a decreased feeling of personal accomplishment (PA). Maslach went on to summarize the triad of burnout as “exhaustion”, “cynicism”, and “inefficacy”, providing definitions that were more specific and aligned well with her measuring tool [3]. Those with high exhaustion scores feel overworked and their mental and physical resources depleted. People who score high on cynicism appear colder or more detached than regular people who are “coping”. Those who lack confidence or believe they have had little work success have a high efficacy score (decreased feeling of personal accomplishment) [4].
These definitions were used by Maslach to create the Maslach Burnout Inventory (MBI), the most widely used evaluation tool for detecting burnout [3]. This tool has 22 questions covering all three categories and gives you a score for each. The degree of burnout in a particular dimension is evaluated by the score. The higher the score, the higher the degree of burnout. It describes a range with higher scores corresponding to more severe symptoms and consequences rather than a definitive cut-off score for burnout as a diagnostic. The MBI is adjusted and condensed for specific populations and ease of use [3]. For instance, Maslach Burnout Inventory-Human Services Survey for Medical Professionals (MBI-HSS) is used in the medical setting [3].
Generally, burnout has been observed to occur in 18–80% of residents of different specialties, while EM healthcare workers’ rate ranges from 32 to 60% [5]. Burnout has numerous detrimental effects on healthcare workers’ personal and professional life. In the professional domain, it leads to the delivery of poor services and consequently reduced patient satisfaction, more medical errors, higher physician turnover, and decreased productivity. On the physician’s side, it may lead to suicide ideation, sadness, addiction, or even physical illness [6]. While burnout is widespread among EM staff and is linked to various adverse outcomes, not all EM workers experience it. In the same presumably challenging situation, some of the members will thrive. The coping style is one significant aspect that may influence the likelihood of developing burnout [7].
Little is known about the exact burden of burnout in EM settings, and previous reports indicate a wide variability in the reported rates that might be attributable to the profession type, pandemic status, year of training, and other factors [7,8,9,10,11,12,13]. Therefore, we are conducting this research to systematically analyze the available literature to determine whether or not burnout among EM healthcare workers exceeds the rare event assumption (of ≤5%), as well as to determine the key factors that affect the prevalence of this problem statement in EM settings.
2. Materials and Methods
2.1. Literature Search
This systematic review was performed per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). To obtain the relevant studies, a systematic search was conducted on major e-databases, including PubMed, Scopus, Web of Science, PsycINFO, and EMBASE. We retrieved records that were published from inception until February 2023. Additionally, we searched and retrieved the first 200 studies from Google Scholar, as a source of Grey Literature, as per recent recommendations [14]. Articles were selected based on their relevance to the topic. All studies relevant to burnout in emergency medical services were included in this research. Keywords used to perform the search in the online databases were (burnout OR “emotional exhaustion” OR depersonalization OR “personal accomplishment”) AND (“emergency medicine” OR “emergency healthcare” OR “emergency physicians” OR “emergency nurses” OR “emergency care” OR “emergency medical technicians”). The detailed search strategy is provided in Supplementary Table S1. A manual search process was carried out where the references of finally included studies were screened, and their titles were inserted into PubMed to look for relevant articles using the “similar articles” function [15].
2.2. Selection Criteria
After selecting the initial cross-sectional studies, their titles and abstracts were scanned to check whether they were relevant to the research topic. The studies were further examined to determine whether or not they met the predetermined eligibility criteria. Relevant studies were included if they fulfilled all of the following criteria: (a) cross-sectional in design, (b) including EM healthcare workers (including but not limited to physicians, nurses, administration, paramedics, etc.), (c) reporting the rate of burnout or one of its domains (emotional exhaustion (EE), depersonalization (DP), or personal accomplishment (PA)), (d) measured burnout using the Maslach Burnout Inventory-Health Service Survey (MBI-HSS) scale [16], and (e) published in the English language. On the other hand, studies were excluded if they included: (a) duplicated studies, (b) irrelevant populations, outcomes, or burnout measures, or (c) secondary research (i.e., reviews, commentaries, editorials, guidelines, etc.). The authors thoroughly read and evaluated all of the studies that met the predetermined inclusion criteria for this systematic review to determine their implications and relevance to the research. Consultation or consensus with the senior author addressed any conflicts or discrepancies.
2.3. Data Extraction and Quality Assessment
The data extraction process was conducted after an initial pilot testing to determine the key variables to be included in the data extraction sheet. The sheet was then designed using Excel Software, and it was composed of three parts. The first part included publications (i.e., year of publication, authors’ names, country, and study design) and included populations’ characteristics (i.e., sample size, profession level of EM workers, age, and gender). The second part included the main outcomes: burnout, EE, DP, and PA. The third part included the variables that will be analyzed as subgroups, including severity, profession type (nurses, physicians, etc.), training years (postgraduate year “PGY”), COVID-19 pandemic timing (pre vs. post), and gender (male vs. female).
For each study, the risk of bias was determined using the Newcastle Ottawa Scale for cross-sectional studies [17]. This scale assesses the quality of cross-sectional studies across three domains: selection (maximum five points), comparability (maximum two points), and outcome (maximum 3 points). Both the data extraction and risk of bias assessment processes were done by at least two authors, and any contradictions were solved by consultation with the senior author.
2.4. Data Synthesis
All statistical analyses were performed using STATA Software (version 17). The prevalence of burnout, along with its subscales, was measured using the metaprop command [18]. The cimethod (score) method was used to pool the effect size (ES) and the corresponding 95% confidence interval (CI) across studies. The fixed-effects model was selected when statistical heterogeneity was not significant. On the contrary, the random-effects model was chosen. Statistical heterogeneity was measured by the I2 statistic and its associated p-value. A p-value of more than 0.05 indicated significant heterogeneity. In the latter, a leave-one-out sensitivity analysis was performed to determine whether or not the reported estimate was mainly driven by a particular study. Subgroup analyses were carried out based on the participating country, the COVID-19 pandemic timing (before vs. during), the profession type of EM workers (physician vs. nurse vs. A/T vs. paramedic) and year of training, and gender (male vs. female).
3. Results
3.1. Search Results
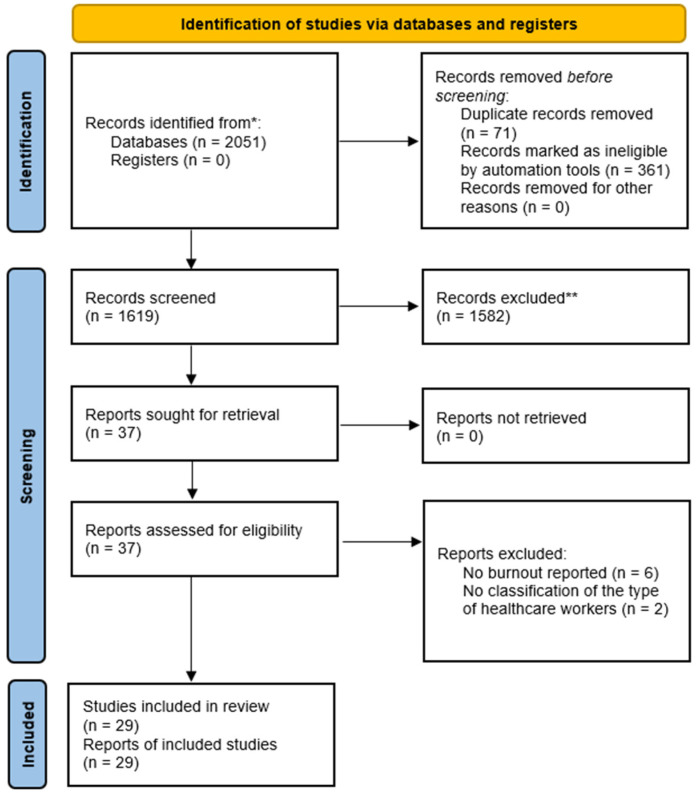
A schematic diagram of the database search and screening processes is presented in Figure 1. The electronic search resulted in 2051 studies, all of which were inserted into EndNote Software for duplicate removal, where 361 were automatically removed. Then, the remaining articles were exported into an Excel sheet for screening. In this stage, 71 additional duplicated articles were removed, resulting in 1619 articles eligible for title and abstract screening, out of which 1582 studies were excluded based on our predetermined eligibility criteria. The full text of 37 articles was screened, and only 29 studies met our criteria [5,8,9,10,11,12,13,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40]. Meanwhile, eight studies were excluded either because burnout was not reported (n = 6) or because the authors failed to classify the type of included healthcare worker (n = 2). Of note, the manual search yielded no additional results.
Figure 1.
PRISMA flow diagram illustrating the database search and study selection processes. * records were identified through original database search; ** records were excluded based on title/abstract screening after the removal of duplicates through EndNote software (https://endnote.com/).
3.2. Characteristics of Included Studies
The baseline characteristics of included reports are presented in Table 1. All of the included studies were cross-sectional in design, the majority of which were conducted in the United States of America (USA) (n = 9), followed by Turkey (n = 3), Canada (n = 2), France (n = 2), Iran (n = 2), and Singapore (n = 2). A total of 16,619 EM healthcare workers were included, and most of whom were males (10,026/16,619; 60.32%). Two studies included ambulance crew, 16 studies included only EM physicians, and the remaining 11 studies included mixed EM healthcare workers (physicians “attendings, residents, or fellows”, registered nurses, paramedics, and/or administrative and technical (A/T) staff. Meanwhile, ten studies included resident physicians only. The mean age of included population ranged from 31.2 to 44 years of age. Noteworthy, more than one-third (11/30 studies) did not report data regarding age.
Table 1.
Baseline characteristics of included studies and EM populations.
| Author (YOP) | Study Design | Country | Population | Sample | Age (Mean) | Male | Female |
|---|---|---|---|---|---|---|---|
| Ferraro (2020) [11] | CS | Italy | Ambulance Crew | 2361 | 34.8 | 2090 | 594 |
| Rajan (2018) [36] | CS | South Africa | Physicians | 100 | 35.1 | 42 | 51 |
| Alqahtani (2019) [8] | CS | Saudi Arabia | Mixed | 282 | 37 | 82 | 200 |
| Takayesu (2014) [5] | CS | USA | Physicians | 218 | 31.2 | 129 | 89 |
| Mourkazel (2019) [32] | CS | France | Mixed | 379 | 37.4 | 98 | 279 |
| Soltanifar (2018) [39] | CS | Iran | Physicians | 77 | 36 | 0 | 77 |
| Lin (2019) [12] | CS | USA | Physicians | 1522 | 31.3 | 879 | 643 |
| Hamdan (2017) [26] | CS | Palestine | Mixed | 444 | 32.5 | 341 | 103 |
| Williams (2020) [40] | CS | USA | Physicians | 30 | 32.1 | - | - |
| Durand (2019) [10] | CS | France | Mixed | 166 | 37.7 | 33 | 133 |
| Schooley (2016) [37] | CS | Turkey | Mixed | 250 | - | 135 | 115 |
| Lu (2015) [31] | CS | USA | Physicians | 77 | - | 48 | 29 |
| Dam (2019) [23] | CS | USA | Physicians | 222 | 31.8 | 150 | 70 |
| Hutchison (2014) [27] | CS | Jamaica | Physicians | 30 | - | 12 | 15 |
| Jalili (2013) [28] | CS | Iran | Physicians | 165 | 33.6 | 150 | 14 |
| Lloyd (1994) [30] | CS | Canada | Physicians | 268 | 38 | 233 | 35 |
| Kuhn (2009) [29] | CS | USA | Mixed | 193 | - | 140 | 53 |
| Patterson (2020) [33] | CS | UK | Physicians | 131 | - | 52 | 79 |
| Popa (2010) [35] | CS | USA | Mixed | 4725 | 33.6 | 3213 | 1512 |
| Erdur (2015) [24] | CS | Turkey | Physicians | 174 | 36.8 | 138 | 36 |
| Bergemueler (2016) [20] | CS | Germany | Ambulance Crew | 97 | 37 | 40 | 57 |
| Escribà-Agüir (2007) [25] | CS | Spain | Mixed | 639 | - | 356 | 279 |
| Petrino (2022) [34] | CS | Turkey | Mixed | 1925 | - | 1007 | 915 |
| Mercuri (2022) [13] | CS | Canada | Physicians | 416 | 44 | 220 | 196 |
| Chang (2021) [9] | CS | USA | Physicians | 22 | - | - | - |
| Bhanja (2021) [21] | CS | USA | Mixed | 944 | 39.3 | 221 | 421 |
| Shopen (2022) [38] | CS | Israel | Physicians | 88 | - | 59 | 29 |
| Chor (2021) [22] | CS | Singapore | Mixed | 337 | - | 109 | 228 |
| Ben-Itzhak (2015) [19] | CS | Singapore | Physicians | 337 | - | 49 | 21 |
YOP: year of publication; CS: cross-sectional; USA: United States of America.
3.3. Quality of Included Studies
The overall quality of included cross-sectional studies was graded as fair in 5 studies, poor in 7 studies, and good in 17 studies. The main reason why some studies were graded as poor was the comparability domain due to the lack of a comparator group in the majority of included cross-sectional studies (Table 2).
Table 2.
The quality of included cross-sectional studies as per the Newcastle Ottawa Scale.
| Author (YOP) | Selection | Comparability | Outcomes | Overall Rating |
|---|---|---|---|---|
| Ferraro (2020) [11] | 4 | 2 | 2 | Good |
| Rajan (2018) [36] | 3 | 2 | 2 | Good |
| Alqahtani (2019) [8] | 4 | 2 | 2 | Good |
| Takayesu (2014) [5] | 3 | 0 | 2 | Poor |
| Mourkazel (2019) [32] | 3 | 2 | 2 | Good |
| Soltanifar (2018) [39] | 2 | 2 | 2 | Fair |
| Lin (2019) [12] | 3 | 2 | 2 | Good |
| Hamdan (2017) [26] | 3 | 2 | 2 | Good |
| Williams (2020) [40] | 3 | 0 | 2 | Poor |
| Durand (2019) [10] | 2 | 2 | 2 | Fair |
| Schooley (2016) [37] | 3 | 2 | 2 | Good |
| Lu (2015) [31] | 2 | 2 | 2 | Fair |
| Dam (2019) [23] | 3 | 2 | 2 | Good |
| Hutchison (2014) [27] | 3 | 2 | 2 | Good |
| Jalili (2013) [28] | 4 | 0 | 2 | Poor |
| Lloyd (1994) [30] | 3 | 2 | 2 | Good |
| Kuhn (2009) [29] | 3 | 2 | 2 | Good |
| Patterson (2020) [33] | 4 | 2 | 2 | Good |
| Popa (2010) [35] | 2 | 0 | 2 | Poor |
| Erdur (2015) [24] | 4 | 2 | 2 | Good |
| Bergemueler (2016) [20] | 3 | 0 | 2 | Poor |
| Escribà-Agüir (2007) [25] | 2 | 0 | 2 | Poor |
| Petrino (2022) [34] | 4 | 2 | 2 | Good |
| Mercuri (2022) [13] | 3 | 0 | 2 | Poor |
| Chang (2021) [9] | 4 | 2 | 2 | Good |
| Bhanja (2021) [21] | 2 | 2 | 2 | Fair |
| Shopen (2022) [38] | 3 | 2 | 2 | Good |
| Chor (2021) [22] | 2 | 2 | 2 | Fair |
| Ben-Itzhak (2015) [19] | 3 | 2 | 2 | Good |
YOP: year of publication. The selection domain was given an overall score of 4, and the comparability and outcomes domains were given overall scores of 2 and 3, respectively.
3.4. Meta-Analysis of Prevalence
3.4.1. Burnout
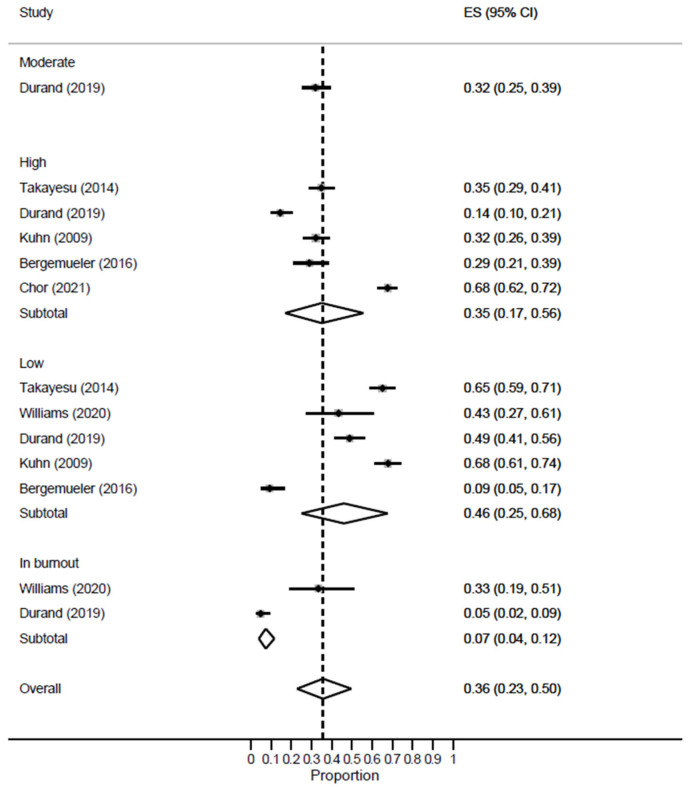
Eleven studies reported the rate of burnout in EM healthcare workers, and the meta-analysis revealed a high prevalence rate of 43% [95% CI: 32–54%; I2 = 0]. The leave-one-out sensitivity analysis revealed no significant change in the reported rate. According to severity [Figure 2], the majority of EM healthcare workers had a low risk of burnout [ES = 46%; 95% CI: 25–68%], while 35% [95% CI: 17–56%] of them had a high risk of burnout. Meanwhile, those with evident burnout at the time of patient recruitment constituted 7% [95% CI: 4–12%] of EM workers.
Figure 2.
Forest plot of the prevalence of overall burnout among EM healthcare workers based on severity.
3.4.2. EE
Twenty-nine studies reported the severity of EE among EM workers. The meta-analysis revealed that EM workers had a higher prevalence of high EE [22 studies, ES = 39%; 95% CI: 28–49%], while less than one-quarter of them had moderate EE [15 studies, ES = 23%; 95% CI: 20–28%] [Supplementary Figure S1].
3.4.3. DP
Twenty-nine studies reported the severity of DP among EM workers. The meta-analysis revealed that EM workers had a higher prevalence of high DP [21 studies, ES = 43%; 95% CI: 36–50%], while less than one-quarter of them had moderate DP [15 studies, ES = 25%; 95% CI: 18–32%] [Supplementary Figure S2].
3.4.4. PA
Twenty-nine studies reported the severity of PA among EM workers. The meta-analysis revealed that EM workers had a higher prevalence of low PA [20 studies, ES = 36%; 95% CI: 28–44%], while less than one-quarter of them had moderate PA [15 studies, ES = 28%; 95% CI: 22–34%] [Supplementary Figure S3].
3.5. Subgroup Analysis of High Burnout
3.5.1. Country
Singapore showed the highest rate of burnout [ES = 68%; 95% CI: 64–73%] among EM workers, followed by the US [ES = 43%; 95% CI: 25–63%] and France [ES = 30%; 26–34%], respectively [Supplementary Figure S4].
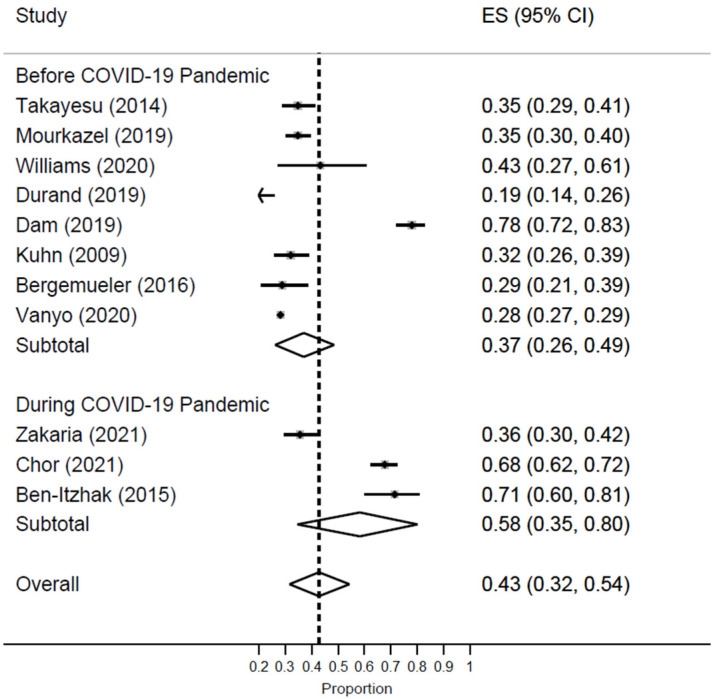
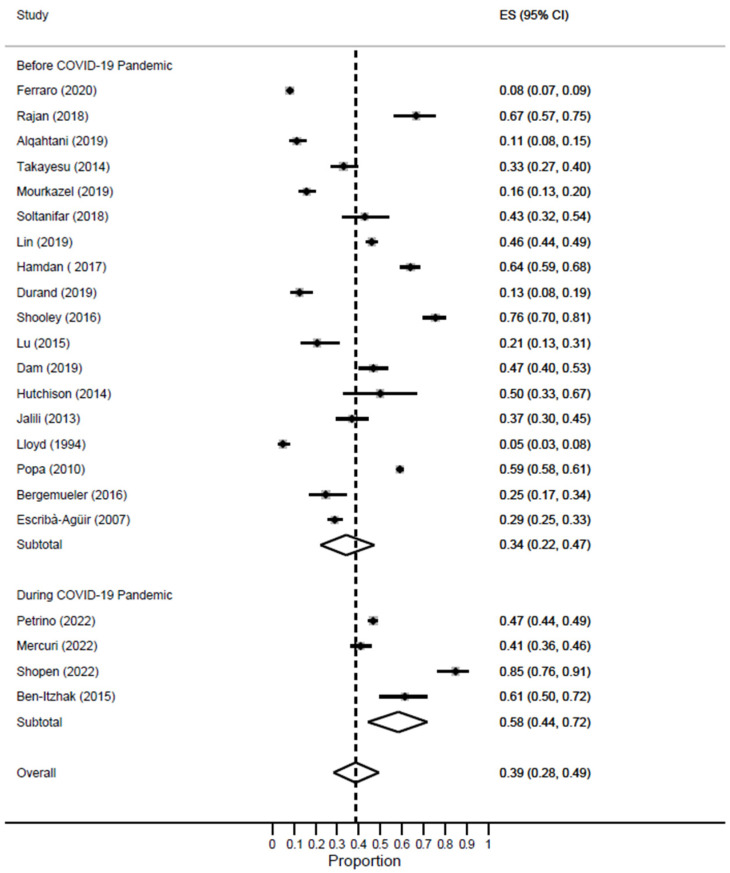
3.5.2. COVID-19 Pandemic
A significant difference in the prevalence of burnout was noted based on the timing of the COVID-19 pandemic. EM workers had drastically higher rates of burnout during the pandemic [ES = 58%; 95% CI: 35–80%] as compared to the pre-pandemic time [ES = 37%; 95% CI: 26–49%] [Figure 3].
Figure 3.
Forest plot of the prevalence of high burnout among EM healthcare workers based on COVID-19 pandemic status.
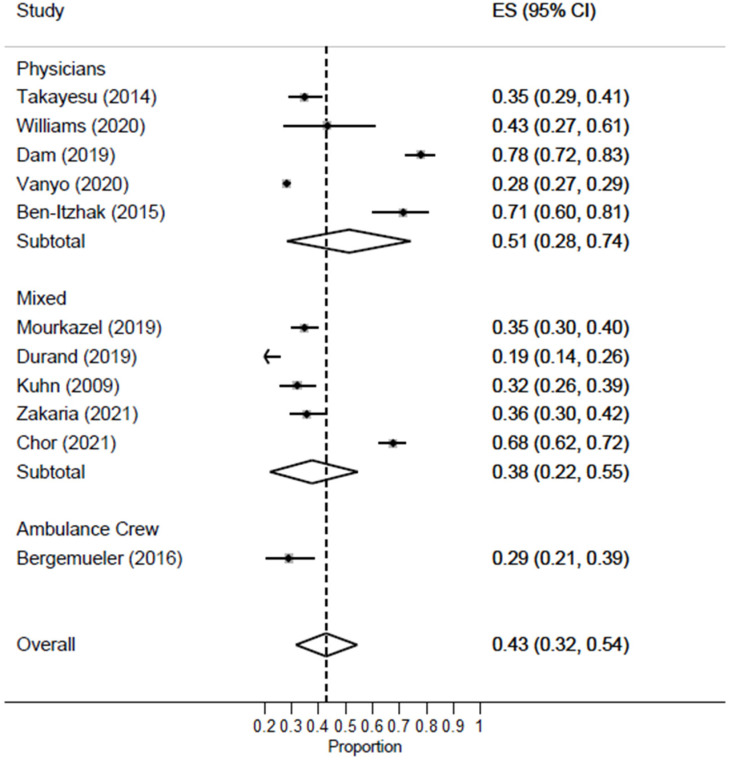
3.5.3. Profession and Year of Training
Studies including only EM physicians [ES = 51%; 95% CI: 28–74%] had a higher prevalence rate of burnout as compared to studies including mixed EM healthcare workers [ES = 38%; 95% CI: 22–55%] [Figure 4]. Only one study reported burnout in ambulance crew, revealing a rate of 29% [95% CI: 21–39%].
Figure 4.
Forest plot of the prevalence of high burnout among EM healthcare workers based on profession.
Noteworthy, among studies including mixed EM workers, burnout was highest among nurses [ES = 47%; 95% CI: 42–52%], followed by paramedics [ES = 41%; 95% CI: 19–65%] and physicians [ES = 34%; 95% CI: 0–66%], respectively. Meanwhile, the A/T staff had the lowest prevalence of burnout, accounting for 11% of the population [95% CI: 7–16%] [Supplementary Figure S5].
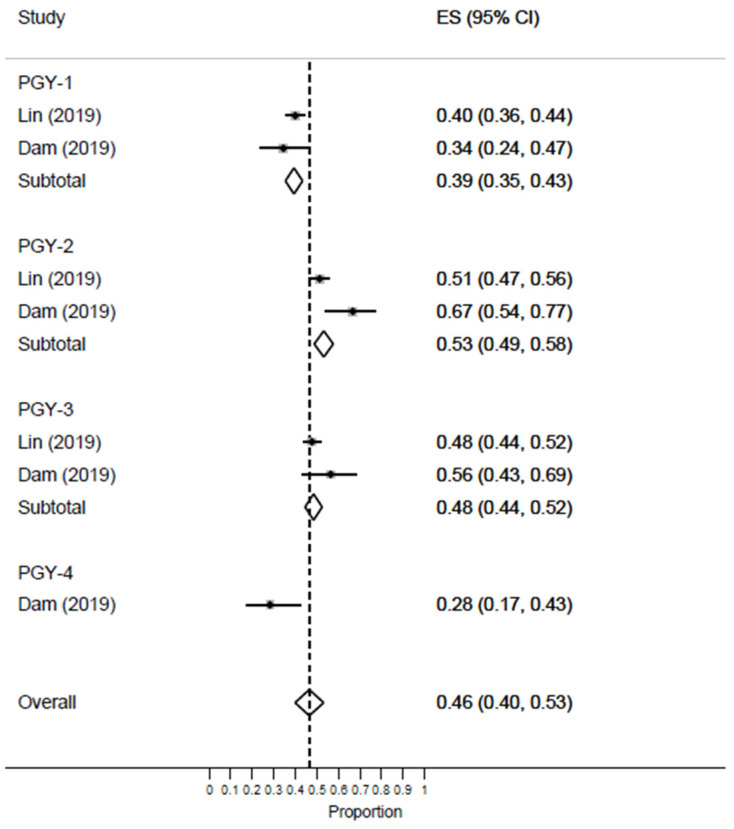
Three studies reported the rate of burnout among EM residents. In the meta-analysis, we noted a steady progressive increase in the prevalence of burnout as residents advanced through their training from PGY-1 [ES = 45%; 95% CI: 11–82%] to PGY-4 [ES = 63%; 95% CI: 25–93%] [Supplementary Figure S6].
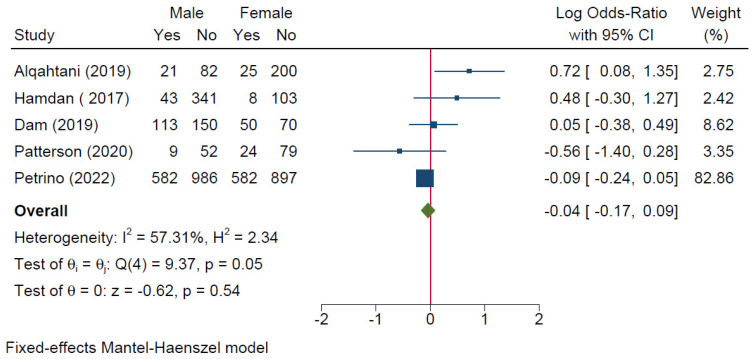
3.5.4. Gender
Five studies compared the occurrence of burnout between males and females. The meta-analysis revealed no significant difference in the risk of burnout based on gender [logOR = −0.04; 95% CI: −0.17: 0.09; I2 = 57.31%, p = 0.053] [Figure 5].
Figure 5.
Forest plot of the risk of high burnout among EM healthcare workers based on gender.
3.6. Subgroup Analysis of High EE
3.6.1. Country
A total of 22 studies were included in this meta-analysis. Turkey showed the highest prevalence of high EE among EM workers [ES = 50%; 95% CI: 48–54%], followed by the US [ES = 42%; 95% CI: 32–52%]. Meanwhile, France had the lowest prevalence of all [ES = 15%; 12–18%] [Supplementary Figure S7].
3.6.2. COVID-19 Pandemic
In this meta-analysis, 18 studies were conducted during the pre-pandemic period, while 4 studies were conducted during the COVID-19 pandemic. The prevalence of high EE almost doubled during the pandemic [ES = 58%; 95% CI: 44–72%] as compared to the pre-pandemic period [ES = 34%; 95% CI: 22–47%] [Figure 6].
Figure 6.
Forest plot of the prevalence of high EE among EM healthcare workers based on COVID-19 pandemic status.
3.6.3. Profession and Year of Training
Studies including only EM physicians [ES = 44%; 95% CI: 32–55%] had the highest prevalence of high EE as compared to studies including mixed EM workers [8 studies, ES = 38%; 95% CI: 25–52%] or ambulance crew [2 studies, ES = 8%; 95% CI: 7–10%] [Supplementary Figure S8].
Noteworthy, among studies including mixed EM workers, high EE was highest among nurses [ES = 51%; 95% CI: 16–85%] followed by physicians [ES = 42%; 95% CI: 21–64%] and A/T staff [ES = 34%; 95% CI: 6–71%], respectively. Meanwhile, paramedics had the lowest prevalence of high EE, accounting for 15% of the population [95% CI: 12–19%] [Supplementary Figure S9].
Two studies reported the rate of high EE among EM residents. The meta-analysis revealed an increase during PGY-2 [ES = 53%; 95% CI: 49–58%], which was similar to that of PGY-3 [ES = 48%; 95% CI: 44–52%] as compared to PGY-1 [ES = 39%; 95% CI: 35–43%] [Figure 7].
Figure 7.
Forest plot of the prevalence of high EE among EM healthcare workers based on residents’ years of training.
3.6.4. Gender
Two studies reported the difference in high EE based on gender. The meta-analysis revealed no significant difference in the risk of developing high EE between males and females [logOR = 0.47; 95% CI: −0.79: 1.73; I2 = 87.39%, p = 0.001] [Supplementary Figure S10].
3.7. Subgroup Analysis of High DP
3.7.1. Country
A total of 22 studies were included in this meta-analysis. The US showed the highest prevalence of high DP among EM workers [ES = 53%; 95% CI: 34–76%], followed by Turkey [ES = 50%; 95% CI: 48–52%]. Meanwhile, Iran had the lowest prevalence of all [ES = 29%; 23–35%] [Supplementary Figure S11].
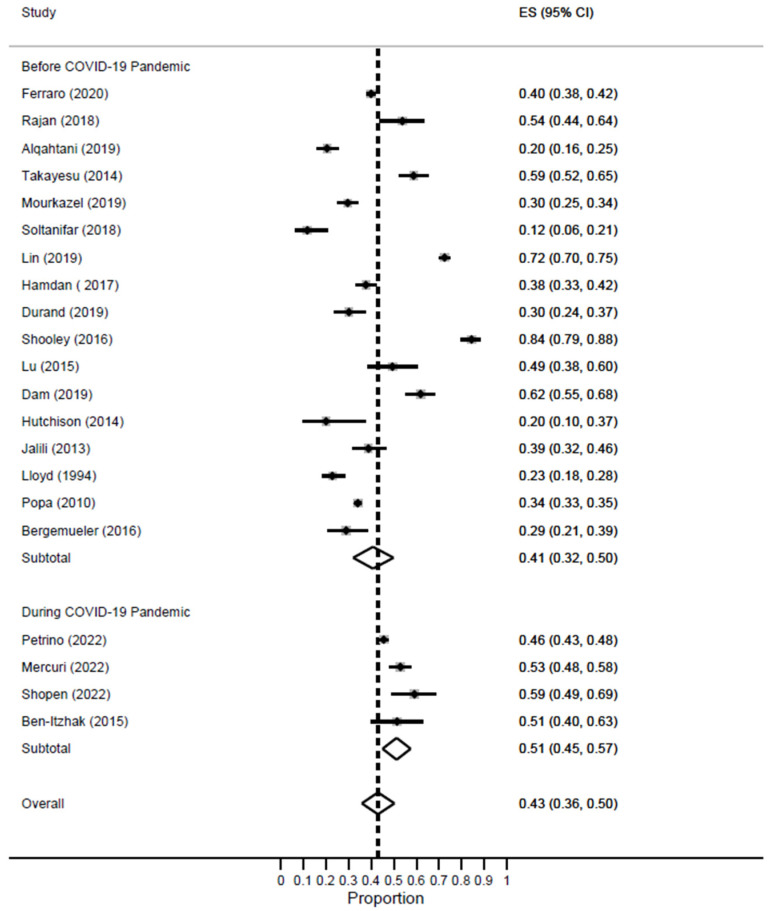
3.7.2. COVID-19 Pandemic
In this meta-analysis, 18 studies were conducted during the pre-pandemic period, while 4 studies were conducted during the COVID-19 pandemic. The prevalence of high DP was higher during the pandemic [ES = 51%; 95% CI: 45–57%] as compared to the pre-pandemic period [ES = 41%; 95% CI: 32–50%] [Figure 8].
Figure 8.
Forest plot of the prevalence of high DP among EM healthcare workers based on COVID-19 pandemic status.
3.7.3. Profession and Year of Training
Studies including only EM physicians [ES = 46%; 95% CI: 34–58%] had the highest prevalence of high DP as compared to studies including mixed EM workers [7 studies, ES = 40%; 95% CI: 30–51%] or ambulance crew [2 studies, ES = 39%; 95% CI: 37–41%] [Supplementary Figure S12].
Noteworthy, among studies including mixed EM workers, high DP was highest among nurses [ES = 60%; 95% CI: 54–66%], and it was nearly equal between physicians [ES = 50%; 95% CI: 30–69%] and A/T staff [ES = 49%; 95% CI: 11–88%]. Meanwhile, paramedics had the lowest prevalence of high DP, accounting for 28% of the population [95% CI: 24–32%] [Supplementary Figure S13].
Two studies reported the rate of high DP among EM residents. The meta-analysis revealed an increase in the prevalence of high DP as residents progressed from PGY-1 [ES = 65%; 95% CI: 61–68%] to PGY-2 [ES = 76%; 95% CI: 72–80%], which was equal to that of PGY-3 [ES = 76%; 95% CI: 72–79%] [Supplementary Figure S14].
3.7.4. Gender
Two studies reported the difference in high DP based on gender. The meta-analysis revealed no significant difference in the risk of developing high EE between males and females [logOR = 0.33; 95% CI: −0.04: 0.69; I2 = 33.26%, p = 0.22] [Supplementary Figure S15].
3.8. Subgroup Analysis of Low PA
3.8.1. Country
A total of 22 studies were included in this meta-analysis. Both Turkey and Iran showed the highest prevalence of low PA among EM workers [ES = 49%; 95% CI: 47–51%] and [ES = 49%; 95% CI: 43–56%]. Meanwhile, the US had the lowest prevalence of all [ES = 26%; 14–41%] [Supplementary Figure S16].
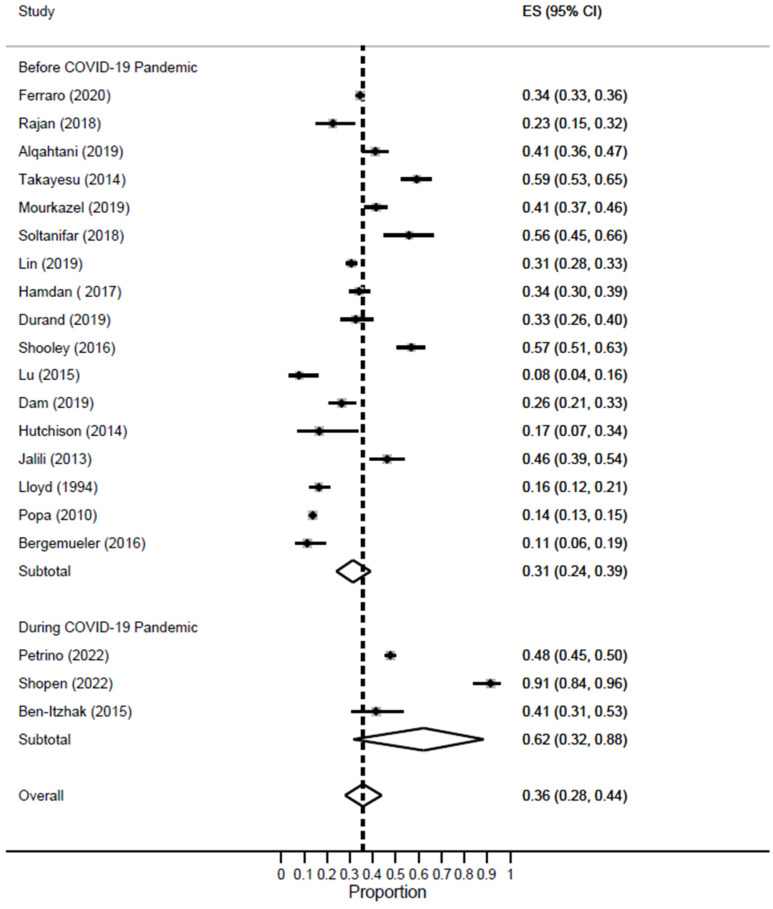
3.8.2. COVID-19 Pandemic
In this meta-analysis, 17 studies were conducted during the pre-pandemic period, while three studies were conducted during the COVID-19 pandemic. The prevalence of low PA doubled during the pandemic [ES = 62%; 95% CI: 32–88%] as compared to the pre-pandemic period [ES = 31%; 95% CI: 24–39%] [Figure 9].
Figure 9.
Forest plot of the prevalence of low PA among EM healthcare workers based on COVID-19 pandemic status.
3.8.3. Profession and Year of Training
Studies including mixed EM workers [7 studies, ES = 38; 95% CI: 22–55%] had the highest prevalence of low PA as compared to studies including physicians only [11 studies, ES = 37%; 95% CI: 25–50%] or ambulance crew [2 studies, ES = 33%; 95% CI: 31–35%] [Supplementary Figure S17].
Noteworthy, among studies including mixed EM workers, low PA was highest among nurses [ES = 55%; 95% CI: 49–61%], and it was nearly equal between physicians [ES = 43%; 95% CI: 32–53%] and A/T staff [ES = 40%; 95% CI: 33–46%]. Meanwhile, paramedics had the lowest prevalence of low PA, accounting for 35% of the population [95% CI: 30–40%] [Supplementary Figure S18].
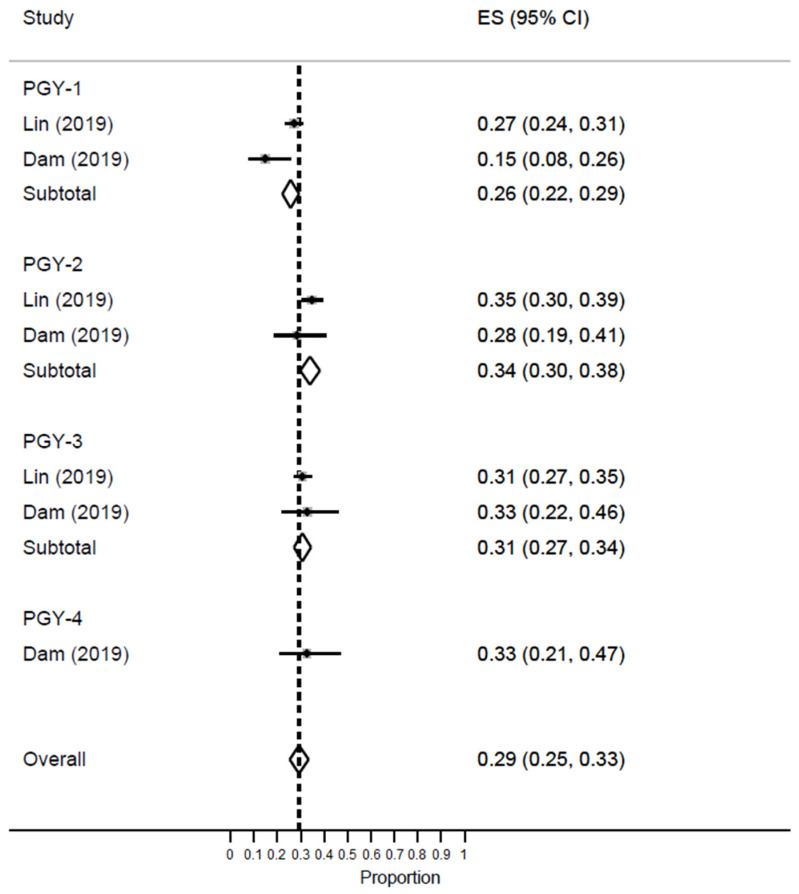
Two studies reported the rate of high DP among EM residents. The meta-analysis revealed an increase in the prevalence of low PA as residents progressed from PGY-1 [ES = 26%; 95% CI: 22–29%] to PGY-2 [ES = 34%; 95% CI: 30–38%] and PGY-3 [ES = 31%; 95% CI: 27–34%] [Figure 10].
Figure 10.
Forest plot of the prevalence of low PA among EM healthcare workers based on residents’ years of training.
3.8.4. Gender
Two studies reported the difference in low PA based on gender. The meta-analysis revealed no significant difference in the risk of developing high EE between males and females [logOR = −0.11; 95% CI: −0.50: 0.27; I2 = 0%, p = 0.37] [Supplementary Figure S19].
4. Discussion
This systematic review provides, by far, the greatest level of evidence regarding the global prevalence of burnout and its subdomains among healthcare workers in emergency care. Burnout is a prevalent problem in EM settings, ranging from 49.3% [22] to 58% [41], based on previous reports. A number of systematic reviews investigating the burden of burnout on EM personnel have been published in the past decade [42,43,44,45,46]. That being said, all of them were conducted prior to the occurrence of the COVID-19 pandemic. Additionally, all of them searched a small number of electronic databases which resulted in a limited number of studies, and therefore, their results are not generalizable. In our study, we included 29 studies (16,619 participants) which is the largest pool of EM populations across the literature. Our meta-analysis revealed an alarmingly high prevalence rate of burnout, high EE, high DP, and low PA of 43%, 39%, 43%, and 36%, respectively. Noteworthy, although 43% of the population suffered from burnout, regardless of the degree of severity, only 7% of participants were in burnout during the time of their interview. This supports our initial hypothesis that the prevalence of burnout, high EE or DP, and low PA surpass the rare event assumption (5%), and therefore, this problem is worthy of attention and addressed in clinical care. Our findings are quite different from those reported in the literature. In the systematic review of Adriaenssens et al. [42], burnout was reported in 26% of EM personnel. This difference could be attributed to the small sample size of the previous review (17 studies, 2021 participants) or to the fact that only nurses were analyzed, not the whole EM population (including physicians, A/T, paramedics, etc.).
Burnout can be attributed to numerous factors. High levels of emotional exhaustion (EE) are mainly attributed to factors such as overload of work, failure to balance work and personal life, fatigue, and the fear of making mistakes while practicing or second victim syndrome. High depersonalization (DA) levels occur due to an increased number of patients being subjected to hostile criticism by seniors and even patients, short temper, and sleep disturbance [2]. EM doctors also witness death almost daily and are burdened with the responsibility of relaying the information to friends and family of the deceased. Over time, a person becomes detached from almost all emotional feelings.
Beyond the prevalence of overall burnout, the present study highlights several key factors that could modify the prevalence of this phenomenon in this population. The occurrence of the COVID-19 pandemic has imposed a substantial psychological impact on the mental health of the world population, with a higher burden on EM personnel who were on the frontline against this disease [47]. This has been observed in our study, where we noted an increased rate of burnout and its subdomains during the pandemic, which doubled in the low PA domain as compared to the pre-pandemic period. This finding, although novel and has not been previously reported in the literature, warrants the attention of healthcare authorities in providing adequate measures to reduce the burden of burnout and its subsequent impact on EM workers’ intention to leave [48], quitting [49], and lowered medical care [50].
In our study, the prevalence of overall burnout, high EE and DP, and low PA were the highest among nurses, while physicians came in second. On the other hand, in the majority of cases, paramedics and A/T staff had the lowest rates of overall burnout, high EE, high DP, or low PA. This can be explained by the nature of nurses’ work, with demands them to do many tasks, spend a prolonged period of time with patients and their family members and friends [51], and be in greater proximity to traumatic cases and events (including workplace violence) [52]. That being said, our finding is inconsistent with that in the literature, where both physicians and nurses had similar rates of burnout across all of the study domains. For example, Zhang et al. [46] conducted a systematic review and included studies that only reported burnout among physicians. The authors reported a prevalence rate of high EE, high DP, and low PA of 40%, 41%, and 35%, respectively. Meanwhile, the review of Li et al. [43], who included nurses, only reported similar rates of 40.50%, 44.30%, and 42.70%, respectively. This difference in our observations could be related to the difference in the number of included studies and participants, along with the presence of substantial heterogeneity (>90%) in the previous two reviews as compared to ours.
In terms of geographical distribution, Singapore showed the highest prevalence of overall burnout, while the US had the highest prevalence of high DP, and Turkey/Iran had the highest prevalence of low PA. This finding is of great importance in directing the efforts needed to prevent and combat this problem among EM personnel. Additionally, gender-related differences in the prevalence of burnout have been previously reported in the literature, where women were more likely to experience burnout as compared to male peers [53]. In our study, we did not find any significant differences in the risk of experiencing overall burnout, high EE, high DP, or low PA among EM personnel based on gender. However, this finding is inconclusive secondary to the small number of analyzed studies in this subgroup (2 studies). Therefore, future studies are still needed to provide better evidence to either confirm or reject this observation.
5. Limitations and Future Directions
Although our study provides the biggest evidence, to date, regarding the worldwide prevalence of burnout among EM personnel, with special emphasis on the current COVID-19 pandemic, our research has several limitations. First, the number of included studies in certain subgroups (gender, year of training) was small, which further limits the applicability and generalizability of our findings. Second, the wide confidence interval reported in some of our findings limits the precision of our results, as the true effect estimate could lie anywhere between both ends of the spectrum. Third, several factors, like smoking [8] and marital status [8], have been reported to affect the risk of experiencing burnout among EM workers; however, due to the lack of enough data, we could not analyze these factors. Therefore, future studies are needed to focus on investigating more risk factors and effect-modifying variables to burnout and its subdomains. Finally, country-specific differences, which were noted particularly during the COVID-19 pandemic, could be related to the wide variability in the approach each country took in dealing with the pandemic, which might have resulted in an altered impact on healthcare workers’ work conditions, mental health, and burnout.
6. Conclusions
Burnout is a prevalent problem in emergency medicine practice, affecting all workers, including residents, physicians, nurses, paramedics, and administrative/technical staff. As residents progress through their training years, their likelihood of experiencing burnout intensifies. Nurses are most affected by this problem, followed by physicians. Country-associated differences in the rate of burnout and subdomains are evident. Organized efforts should be devoted to reducing the prevalence and associated burden of this problem. Given these findings, we advise the issuance of country-specific protocols that can address all of the mentioned issues in an attempt to lower the burden of burnout in healthcare settings, particularly at times of emergency, like the COVID-19 pandemic.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare11152220/s1, Supplementary Figure S1. Forest plot of the prevalence of high EE among EM healthcare workers based on severity; Figure S2. Forest plot of the prevalence of high DP among EM healthcare workers based on severity; Figure S3. Forest plot of the prevalence of low PA among EM healthcare workers based on severity; Figure S4. Forest plot of the prevalence of high burnout among EM healthcare workers based on country; Figure S5. Forest plot of the prevalence of high burnout among EM healthcare workers based on profession among studies including mixed populations; Figure S6. Forest plot of the prevalence of high burnout among EM healthcare workers based on residents’ years of training; Figure S7. Forest plot of the prevalence of high EE among EM healthcare workers based on country; Figure S8. Forest plot of the prevalence of high EE among EM healthcare workers based on profession; Figure S9. Forest plot of the prevalence of high EE among EM healthcare workers based on profession among studies including mixed populations; Figure S10. Forest plot of the prevalence of high EE among EM healthcare workers based on gender; Figure S11. Forest plot of the prevalence of high DP among EM healthcare workers based on country; Figure S12. Forest plot of the prevalence of high DP among EM healthcare workers based on profession; Figure S13. Forest plot of the prevalence of high DP among EM healthcare workers based on profession among studies including mixed populations; Figure S14. Forest plot of the prevalence of high DP among EM healthcare workers based on residents’ year of training; Figure S15. Forest plot of the prevalence of high DP among EM healthcare workers based on gender; Figure S16. Forest plot of the prevalence of low PA among EM healthcare workers based on country; Figure S17. Forest plot of the prevalence of low PA among EM healthcare workers based on profession; Figure S18. Forest plot of the prevalence of low PA among EM healthcare workers based on profession among studies including mixed populations; Figure S19. Forest plot of the prevalence of low PA among EM healthcare workers based on gender. Table S1. The detailed search strategy employed in each of the searched databases.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Accessibility to the analyzed dataset can be granted upon reasonable request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Arora M., Asha S., Chinnappa J., Diwan A.D. Burnout in emergency medicine physicians. Emerg. Med. Australas. 2013;25:491–495. doi: 10.1111/1742-6723.12135. [DOI] [PubMed] [Google Scholar]
- 2.Wilson W., Raj J.P., Narayan G., Ghiya M., Murty S., Joseph B. Quantifying burnout among emergency medicine professionals. J. Emergencies Trauma Shock. 2017;10:199. doi: 10.4103/JETS.JETS_36_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maslach C., Jackson S.E., Leiter M.P. Maslach Burnout Inventory. Scarecrow Education; Lanham, MD, USA: 1997. [Google Scholar]
- 4.Stehman C.R., Testo Z., Gershaw R.S., Kellogg A.R. Burnout, drop out, suicide: Physician loss in emergency medicine, part I. West. J. Emerg. Med. 2019;20:485. doi: 10.5811/westjem.2019.4.40970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kimo Takayesu J., Ramoska E.A., Clark T.R., Hansoti B., Dougherty J., Freeman W., Weaver K.R., Chang Y., Gross E. Factors associated with burnout during emergency medicine residency. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2014;21:1031–1035. doi: 10.1111/acem.12464. [DOI] [PubMed] [Google Scholar]
- 6.Lim R., Van Aarsen K., Gray S., Rang L., Fitzpatrick J., Fischer L. Emergency medicine physician burnout and wellness in Canada before COVID19: A national survey. Can. J. Emerg. Med. 2020;22:603–607. doi: 10.1017/cem.2020.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howlett M., Doody K., Murray J., LeBlanc-Duchin D., Fraser J., Atkinson P. Burnout in emergency department healthcare professionals is associated with coping style: A cross-sectional survey. Emerg. Med. J. 2015;32:722–727. doi: 10.1136/emermed-2014-203750. [DOI] [PubMed] [Google Scholar]
- 8.Alqahtani A.M., Awadalla N.J., Alsaleem S.A., Alsamghan A.S., Alsaleem M.A. Burnout Syndrome among Emergency Physicians and Nurses in Abha and Khamis Mushait Cities, Aseer Region, Southwestern Saudi Arabia. Sci. World J. 2019;2019:4515972. doi: 10.1155/2019/4515972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang J., Ray J.M., Joseph D., Evans L.V., Joseph M. Burnout and Post-traumatic Stress Disorder Symptoms Among Emergency Medicine Resident Physicians During the COVID-19 Pandemic. West. J. Emerg. Med. 2022;23:251–257. doi: 10.5811/westjem.2021.11.53186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Durand A.-C., Bompard C., Sportiello J., Michelet P., Gentile S. Stress and burnout among professionals working in the emergency department in a French university hospital: Prevalence and associated factors. Work. 2019;63:57–67. doi: 10.3233/WOR-192908. [DOI] [PubMed] [Google Scholar]
- 11.Ferraro L., La Cascia C., De Santis A., Sideli L., Maniaci G., Orlando I.M., Chifari A., Maniaci L., La Barbera D. A Cross-Sectional Survey on Burnout Prevalence and Profile in the Sicilian Population of Ambulance Driver-Rescuers. Prehospital Disaster Med. 2020;35:133–140. doi: 10.1017/S1049023X20000059. [DOI] [PubMed] [Google Scholar]
- 12.Lin M., Battaglioli N., Melamed M., Mott S.E., Chung A.S., Robinson D.W. High Prevalence of Burnout Among US Emergency Medicine Residents: Results From the 2017 National Emergency Medicine Wellness Survey. Ann. Emerg. Med. 2019;74:682–690. doi: 10.1016/j.annemergmed.2019.01.037. [DOI] [PubMed] [Google Scholar]
- 13.Mercuri M., Clayton N., Archambault P., Wallner C., Boulos M.E., Chan T.M., Gérin-Lajoie C., Gray S., Schwartz L., Ritchie K., et al. Canadian emergency medicine physician burnout: A survey of Canadian emergency physicians during the second wave of the COVID-19 pandemic. Can. J. Emerg. Med. 2022;24:288–292. doi: 10.1007/s43678-021-00259-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muka T., Glisic M., Milic J., Verhoog S., Bohlius J., Bramer W., Chowdhury R., Franco O.H. A 24-step guide on how to design, conduct, and successfully publish a systematic review and meta-analysis in medical research. Eur. J. Epidemiol. 2020;35:49–60. doi: 10.1007/s10654-019-00576-5. [DOI] [PubMed] [Google Scholar]
- 15.Cherif Y.Y.S., Djeffal C., Abu Serhan H., Elnahhas A., Yousef H., Katamesh B.E., Abdelazeem B., Abdelaal A. The Characteristics of COVID-19 Vaccine-Associated Uveitis: A Summative Systematic Review. Vaccines. 2022;11:69. doi: 10.3390/vaccines11010069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin C.-Y., Alimoradi Z., Griffiths M.D., Pakpour A.H. Psychometric properties of the Maslach Burnout Inventory for Medical Personnel (MBI-HSS-MP) Heliyon. 2022;8:e08868. doi: 10.1016/j.heliyon.2022.e08868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moskalewicz A., Oremus M. No clear choice between Newcastle–Ottawa Scale and Appraisal Tool for Cross-Sectional Studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer. J. Clin. Epidemiol. 2020;120:94–103. doi: 10.1016/j.jclinepi.2019.12.013. [DOI] [PubMed] [Google Scholar]
- 18.Nyaga V.N., Arbyn M., Aerts M. Metaprop: A Stata command to perform meta-analysis of binomial data. Arch. Public Health. 2014;72:39. doi: 10.1186/2049-3258-72-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ben-Itzhak S., Dvash J., Maor M., Rosenberg N., Halpern P. Sense of meaning as a predictor of burnout in emergency physicians in Israel: A national survey. Clin. Exp. Emerg. Med. 2015;2:217–225. doi: 10.15441/ceem.15.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bergmueller A., Zavgorodnii I., Zavgorodnia N., Kapustnik W., Boeckelmann I. Relationship between burnout syndrome and personality characteristics in emergency ambulance crew. Neurosci. Behav. Physiol. 2018;48:404–408. doi: 10.1007/s11055-018-0578-4. [DOI] [Google Scholar]
- 21.Bhanja A., Hayirli T., Stark N., Hardy J., Peabody C.R., Kerrissey M. Team and leadership factors and their relationship to burnout in emergency medicine during COVID-19: A 3-wave cross-sectional study. J. Am. Coll. Emerg. Physicians Open. 2022;3:e12761. doi: 10.1002/emp2.12761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chor W.P.D., Ng W.M., Cheng L., Situ W., Chong J.W., Ng L.Y.A., Mok P.L., Yau Y.W., Lin Z. Burnout amongst emergency healthcare workers during the COVID-19 pandemic: A multi-center study. Am. J. Emerg. Med. 2021;46:700–702. doi: 10.1016/j.ajem.2020.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dam A., Perera T., Jones M., Haughy M., Gaeta T. The Relationship Between Grit, Burnout, and Well-being in Emergency Medicine Residents. AEM Educ. Train. 2019;3:14–19. doi: 10.1002/aet2.10311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Erdur B., Ergın A., Yuksel A., Türkçüer İ., Ayrik C., Boz B. Assessment of the relation of violence and burnout among physicians working in the emergency departments in Turkey. Ulus Travma Acil Cerrahi Derg. 2015;21:175–181. doi: 10.5505/tjtes.2015.91298. [DOI] [PubMed] [Google Scholar]
- 25.Escribà-Agüir V., Pérez-Hoyos S. Psychological well-being and psychosocial work environment characteristics among emergency medical and nursing staff. Stress Health J. Int. Soc. Investig. Stress. 2007;23:153–160. doi: 10.1002/smi.1131. [DOI] [Google Scholar]
- 26.Hamdan M., Hamra A.A. Burnout among workers in emergency Departments in Palestinian hospitals: Prevalence and associated factors. BMC Health Serv. Res. 2017;17:407. doi: 10.1186/s12913-017-2356-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hutchinson T.A., Haase S., French S., McFarlane T.A. Stress, Burnout and Coping among Emergency Physicians at a Major Hospital in Kingston, Jamaica. West Indian Med. J. 2014;63:262–266. doi: 10.7727/wimj.2013.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jalili M., Sadeghipour Roodsari G., Bassir Nia A. Burnout and Associated Factors among Iranian Emergency Medicine Practitioners. Iran. J. Public Health. 2013;42:1034–1042. [PMC free article] [PubMed] [Google Scholar]
- 29.Kuhn G., Goldberg R., Compton S. Tolerance for uncertainty, burnout, and satisfaction with the career of emergency medicine. Ann. Emerg. Med. 2009;54:106–113.e6. doi: 10.1016/j.annemergmed.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 30.Lloyd S., Streiner D., Shannon S. Burnout, depression, life and job satisfaction among Canadian emergency physicians. J. Emerg. Med. 1994;12:559–565. doi: 10.1016/0736-4679(94)90360-3. [DOI] [PubMed] [Google Scholar]
- 31.Lu D.W., Dresden S., McCloskey C., Branzetti J., Gisondi M.A. Impact of Burnout on Self-Reported Patient Care Among Emergency Physicians. West. J. Emerg. Med. 2015;16:996–1001. doi: 10.5811/westjem.2015.9.27945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moukarzel A., Michelet P., Durand A.C., Sebbane M., Bourgeois S., Markarian T., Bompard C., Gentile S. Burnout Syndrome among Emergency Department Staff: Prevalence and Associated Factors. BioMed Res. Int. 2019;2019:6462472. doi: 10.1155/2019/6462472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patterson J., Gardner A. Burnout Rates in Pediatric Emergency Medicine Physicians. Pediatr. Emerg. Care. 2020;36:192–195. doi: 10.1097/PEC.0000000000001379. [DOI] [PubMed] [Google Scholar]
- 34.Petrino R., Riesgo L.G., Yilmaz B. Burnout in emergency medicine professionals after 2 years of the COVID-19 pandemic: A threat to the healthcare system? Eur. J. Emerg. Med. Off. J. Eur. Soc. Emerg. Med. 2022;29:279–284. doi: 10.1097/MEJ.0000000000000952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Popa F., Arafat R., Purcărea V.L., Lală A., Popa-Velea O., Bobirnac G. Occupational burnout levels in emergency medicine--a stage 2 nationwide study and analysis. J. Med. Life. 2010;3:449–453. [PMC free article] [PubMed] [Google Scholar]
- 36.Rajan S., Engelbrecht A. A cross-sectional survey of burnout amongst doctors in a cohort of public sector emergency centres in Gauteng, South Africa. Afr. J. Emerg. Med. 2018;8:95–99. doi: 10.1016/j.afjem.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schooley B., Hikmet N., Tarcan M., Yorgancioglu G. Comparing Burnout Across Emergency Physicians, Nurses, Technicians, and Health Information Technicians Working for the Same Organization. Medicine. 2016;95:e2856. doi: 10.1097/MD.0000000000002856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shopen N., Schneider A., Aviv Mordechai R., Katz Shalhav M., Zandberg E., Sharist M., Halpern P. Emergency medicine physician burnout before and during the COVID-19 pandemic. Isr. J. Health Policy Res. 2022;11:30. doi: 10.1186/s13584-022-00539-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Soltanifar A., Pishbin E., Attaran Mashhadi N., Najaf Najafi M., Siahtir M. Burnout among female emergency medicine physicians: A nationwide study. Emerg. Med. Australas. 2018;30:517–522. doi: 10.1111/1742-6723.12941. [DOI] [PubMed] [Google Scholar]
- 40.Williams B.J., Rudinsky S.L., Matteucci M.J. Burnout in Military Emergency Medicine Resident Physicians: A Cross-Sectional Study with Comparisons to Other Physician Groups. Mil. Med. 2020;185:e331–e334. doi: 10.1093/milmed/usz236. [DOI] [PubMed] [Google Scholar]
- 41.Sharma R., Saxena A., Magoon R., Jain M.K. A cross-sectional analysis of prevalence and factors related to depression, anxiety, and stress in health care workers amidst the COVID-19 pandemic. Indian J. Anaesth. 2020;64:S242. doi: 10.4103/ija.IJA_987_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adriaenssens J., De Gucht V., Maes S. Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. Int. J. Nurs. Stud. 2015;52:649–661. doi: 10.1016/j.ijnurstu.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 43.Li H., Cheng B., Zhu X.P. Quantification of burnout in emergency nurses: A systematic review and meta-analysis. Int. Emerg. Nurs. 2018;39:46–54. doi: 10.1016/j.ienj.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 44.Sahebi A., Golitaleb M., Jahangiri K. Occupational Burnout in Pre-Hospital Emergency Personnel in Iran: A Systematic Review and Meta-Analysis. Iran. J. Nurs. Midwifery Res. 2021;26:11–17. doi: 10.4103/ijnmr.IJNMR_175_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Verougstraete D., Hachimi Idrissi S. The impact of burn-out on emergency physicians and emergency medicine residents: A systematic review. Acta Clin. Belg. 2020;75:57–79. doi: 10.1080/17843286.2019.1699690. [DOI] [PubMed] [Google Scholar]
- 46.Zhang Q., Mu M.C., He Y., Cai Z.L., Li Z.C. Burnout in emergency medicine physicians: A meta-analysis and systematic review. Medicine. 2020;99:e21462. doi: 10.1097/MD.0000000000021462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nguyen J., Liu A., McKenney M., Liu H., Ang D., Elkbuli A. Impacts and challenges of the COVID-19 pandemic on emergency medicine physicians in the United States. Am. J. Emerg. Med. 2021;48:38–47. doi: 10.1016/j.ajem.2021.03.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nantsupawat A., Kunaviktikul W., Nantsupawat R., Wichaikhum O.A., Thienthong H., Poghosyan L. Effects of nurse work environment on job dissatisfaction, burnout, intention to leave. Int. Nurs. Rev. 2017;64:91–98. doi: 10.1111/inr.12342. [DOI] [PubMed] [Google Scholar]
- 49.Moon Y.-K., O'Brien K.E., Mann K.J. The role of extraversion in the great resignation: A burnout-quitting process during the pandemic. Personal. Individ. Differ. 2023;205:112074. doi: 10.1016/j.paid.2022.112074. [DOI] [Google Scholar]
- 50.Tawfik D.S., Scheid A., Profit J., Shanafelt T., Trockel M., Adair K.C., Sexton J.B., Ioannidis J.P. Evidence relating health care provider burnout and quality of care: A systematic review and meta-analysis. Ann. Intern. Med. 2019;171:555–567. doi: 10.7326/M19-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sahraian A., Fazelzadeh A., Mehdizadeh A., Toobaee S. Burnout in hospital nurses: A comparison of internal, surgery, psychiatry and burns wards. Int. Nurs. Rev. 2008;55:62–67. doi: 10.1111/j.1466-7657.2007.00582.x. [DOI] [PubMed] [Google Scholar]
- 52.Child R.H., Mentes J.C. Violence against women: The phenomenon of workplace violence against nurses. Issues Ment. Health Nurs. 2010;31:89–95. doi: 10.3109/01612840903267638. [DOI] [PubMed] [Google Scholar]
- 53.Templeton K., Bernstein C.A., Sukhera J., Nora L.M., Newman C., Burstin H., Guille C., Lynn L., Schwarze M.L., Sen S. Gender-based differences in burnout: Issues faced by women physicians. NAM Perspect. 2019 doi: 10.31478/201905a. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Accessibility to the analyzed dataset can be granted upon reasonable request from the corresponding author.