Abstract
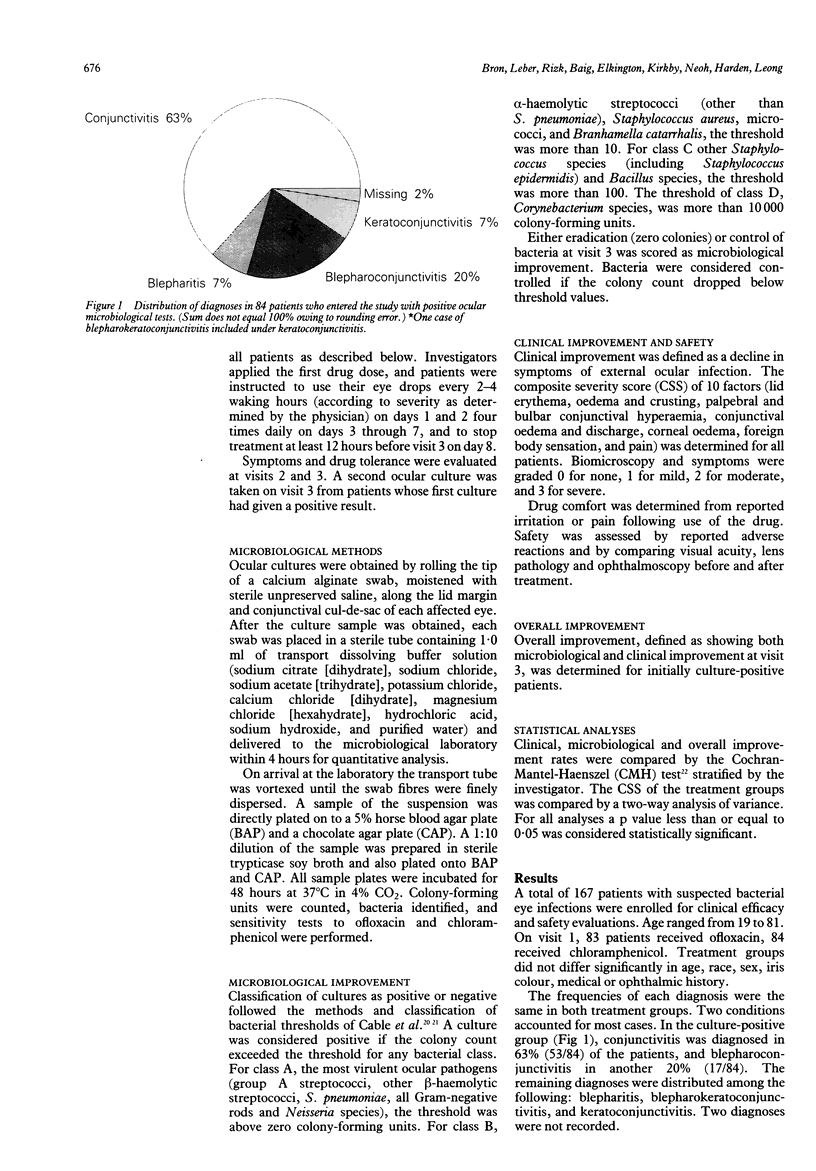
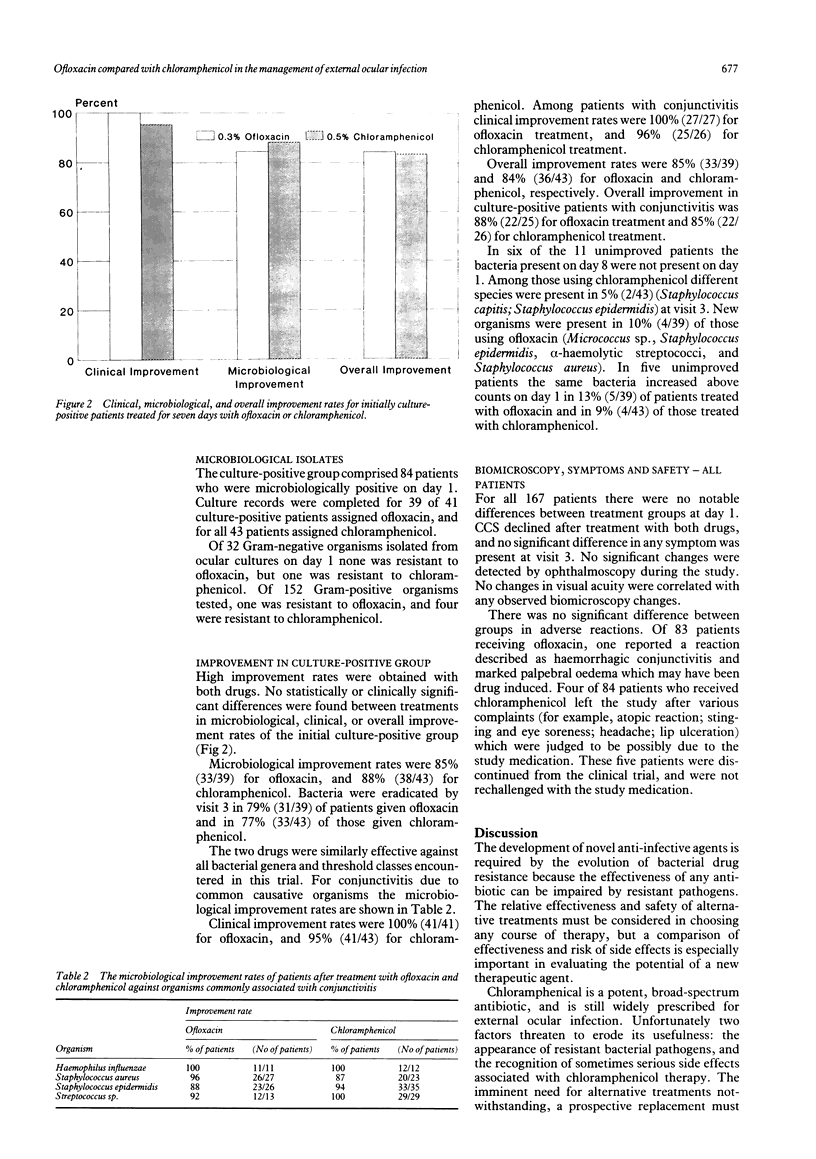
The safety and efficacy of 0.3% ofloxacin in treating bacterial ocular infections was compared with that of 0.5% chloramphenicol in a parallel-group, randomised clinical trial at five sites. Clinical and microbiological improvement rates were studied in 84 culture-positive patients. Patients with suspected bacterial ocular infections were evaluated for clinical improvement and were included in drug safety and comfort analyses. Clinical improvement did not differ significantly between drug treatments. All patients completing the study (79 assigned ofloxacin, and 74 chloramphenicol) showed clinical improvement. Clinical improvement in the culture-positive groups was 100% (41/41) after ofloxacin treatment, and 95% (41/43) after chloramphenicol treatment. Microbiological improvement rates were similar for the two drugs: 85% (33/39) improved with ofloxacin, and 88% (38/43) improved with chloramphenicol. Both drugs were well tolerated. Adverse reactions possibly due to the study medication occurred in 1% (1/89) of those who received ofloxacin, and in 4% (4/93) of those who received chloramphenicol.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abrams S. M., Degnan T. J., Vinciguerra V. Marrow aplasia following topical application of chloramphenicol eye ointment. Arch Intern Med. 1980 Apr;140(4):576–577. [PubMed] [Google Scholar]
- Borrmann L. R., Leopold I. H. The potential use of quinolones in future ocular antimicrobial therapy. Am J Ophthalmol. 1988 Aug 15;106(2):227–229. doi: 10.1016/0002-9394(88)90840-9. [DOI] [PubMed] [Google Scholar]
- Brodsky E., Biger Y., Zeidan Z., Schneider M. Topical application of chloramphenicol eye ointment followed by fatal bone marrow aplasia. Isr J Med Sci. 1989 Jan;25(1):54–54. [PubMed] [Google Scholar]
- Cagle G. D., Abshire R. L. Quantitative ocular bacteriology: a method for the enumeration and identification of bacteria from the skin-lash margin and conjunctiva. Invest Ophthalmol Vis Sci. 1981 Jun;20(6):751–757. [PubMed] [Google Scholar]
- Cagle G., Davis S., Rosenthal A., Smith J. Topical tobramycin and gentamicin sulfate in the treatment of ocular infections: multicenter study. Curr Eye Res. 1981;1(9):523–534. doi: 10.3109/02713688109069178. [DOI] [PubMed] [Google Scholar]
- Chantot J. F., Bryskier A. Antibacterial activity of ofloxacin and other 4-quinolone derivatives: in-vitro and in-vivo comparison. J Antimicrob Chemother. 1985 Oct;16(4):475–484. doi: 10.1093/jac/16.4.475. [DOI] [PubMed] [Google Scholar]
- Crumplin G. C., Odell M. Development of resistance to ofloxacin. Drugs. 1987;34 (Suppl 1):1–8. doi: 10.2165/00003495-198700341-00002. [DOI] [PubMed] [Google Scholar]
- Debbia E., Mannelli S., Gianrossi G., Schito G. C. Susceptibility in vitro of gram-positive aerobe and anaerobe bacteria to ofloxacin. Drugs Exp Clin Res. 1987;13(4):213–217. [PubMed] [Google Scholar]
- Dirdal M. Fucithalmic in acute conjunctivitis. Open, randomized comparison of fusidic acid, chloramphenicol and framycetin eye drops. Acta Ophthalmol (Copenh) 1987 Apr;65(2):129–133. doi: 10.1111/j.1755-3768.1987.tb06989.x. [DOI] [PubMed] [Google Scholar]
- Feder H. M., Jr Chloramphenicol: what we have learned in the last decade. South Med J. 1986 Sep;79(9):1129–1134. [PubMed] [Google Scholar]
- Fernandes P. B. Mode of action, and in vitro and in vivo activities of the fluoroquinolones. J Clin Pharmacol. 1988 Feb;28(2):156–168. doi: 10.1002/j.1552-4604.1988.tb05967.x. [DOI] [PubMed] [Google Scholar]
- Fraunfelder F. T., Bagby G. C., Jr, Kelly D. J. Fatal aplastic anemia following topical administration of ophthalmic chloramphenicol. Am J Ophthalmol. 1982 Mar;93(3):356–360. doi: 10.1016/0002-9394(82)90540-2. [DOI] [PubMed] [Google Scholar]
- Fraunfelder F. T. Fatal aplastic anemia. JAMA. 1982 May 14;247(18):2499–2499. [PubMed] [Google Scholar]
- Fraunfelder F. T., Meyer S. M. Systemic reactions to ophthalmic drug preparations. Med Toxicol Adverse Drug Exp. 1987 Jul-Aug;2(4):287–293. doi: 10.1007/BF03259870. [DOI] [PubMed] [Google Scholar]
- French G. L., Ling J., Ling T., Hui Y. W. Susceptibility of Hong Kong isolates of methicillin-resistant Staphylococcus aureus to antimicrobial agents. J Antimicrob Chemother. 1988 May;21(5):581–588. doi: 10.1093/jac/21.5.581. [DOI] [PubMed] [Google Scholar]
- Jüngst G., Mohr R. Overview of postmarketing experience with ofloxacin in Germany. J Antimicrob Chemother. 1988 Sep;22 (Suppl 100):167–175. doi: 10.1093/jac/22.supplement_c.167. [DOI] [PubMed] [Google Scholar]
- Jüngst G., Mohr R. Side effects of ofloxacin in clinical trials and in postmarketing surveillance. Drugs. 1987;34 (Suppl 1):144–149. doi: 10.2165/00003495-198700341-00031. [DOI] [PubMed] [Google Scholar]
- Kenny J. F., Isburg C. D., Michaels R. H. Meningitis due to Haemophilus influenzae type b resistant to both ampicillin and chloramphenicol. Pediatrics. 1980 Jul;66(1):14–16. [PubMed] [Google Scholar]
- Kresken M., Wiedemann B. Development of resistance to nalidixic acid and the fluoroquinolones after the introduction of norfloxacin and ofloxacin. Antimicrob Agents Chemother. 1988 Aug;32(8):1285–1288. doi: 10.1128/aac.32.8.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumada T., Neu H. C. In-vitro activity of ofloxacin, a quinolone carboxylic acid compared to other quinolones and other antimicrobial agents. J Antimicrob Chemother. 1985 Nov;16(5):563–574. doi: 10.1093/jac/16.5.563. [DOI] [PubMed] [Google Scholar]
- Mahajan V. M. Acute bacterial infections of the eye: their aetiology and treatment. Br J Ophthalmol. 1983 Mar;67(3):191–194. doi: 10.1136/bjo.67.3.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk J. P., Campoli-Richards D. M. Ofloxacin. A review of its antibacterial activity, pharmacokinetic properties and therapeutic use. Drugs. 1987 Apr;33(4):346–391. doi: 10.2165/00003495-198733040-00003. [DOI] [PubMed] [Google Scholar]
- Osato M. S., Jensen H. G., Trousdale M. D., Bosso J. A., Borrmann L. R., Frank J., Akers P. The comparative in vitro activity of ofloxacin and selected ophthalmic antimicrobial agents against ocular bacterial isolates. Am J Ophthalmol. 1989 Oct 15;108(4):380–386. doi: 10.1016/s0002-9394(14)73305-7. [DOI] [PubMed] [Google Scholar]
- Pepper K., Le Bouguénec C., de Cespédès G., Horaud T. Dispersal of a plasmid-borne chloramphenicol resistance gene in streptococcal and enterococcal plasmids. Plasmid. 1986 Nov;16(3):195–203. doi: 10.1016/0147-619x(86)90057-0. [DOI] [PubMed] [Google Scholar]
- Powell D. A., Nahata M. C. Chloramphenicol: new perspectives on an old drug. Drug Intell Clin Pharm. 1982 Apr;16(4):295–300. doi: 10.1177/106002808201600404. [DOI] [PubMed] [Google Scholar]
- Radetsky M. S., Istre G. R., Johansen T. L., Parmelee S. W., Lauer B. A., Wiesenthal A. M., Glode M. P. Multiply resistant pneumococcus causing meningitis: its epidemiology within a day-care centre. Lancet. 1981 Oct 10;2(8250):771–773. doi: 10.1016/s0140-6736(81)90184-7. [DOI] [PubMed] [Google Scholar]
- Rahal J. J., Jr, Simberkoff M. S. Bactericidal and bacteriostatic action of chloramphenicol against memingeal pathogens. Antimicrob Agents Chemother. 1979 Jul;16(1):13–18. doi: 10.1128/aac.16.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridgway G. L., O'Hare M. D., Felmingham D., Grüneberg R. N. The comparative activity of twelve 4-quinolone antimicrobials against Haemophilus influenzae and Streptococcus pneumoniae. Drugs Exp Clin Res. 1985;11(4):259–262. [PubMed] [Google Scholar]
- Roberts M. C., Swenson C. D., Owens L. M., Smith A. L. Characterization of chloramphenicol-resistant Haemophilus influenzae. Antimicrob Agents Chemother. 1980 Oct;18(4):610–615. doi: 10.1128/aac.18.4.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato K., Inoue Y., Fujii T., Aoyama H., Mitsuhashi S. Antibacterial activity of ofloxacin and its mode of action. Infection. 1986;14 (Suppl 4):S226–S230. doi: 10.1007/BF01661277. [DOI] [PubMed] [Google Scholar]
- Sato K., Matsuura Y., Inoue M., Une T., Osada Y., Ogawa H., Mitsuhashi S. In vitro and in vivo activity of DL-8280, a new oxazine derivative. Antimicrob Agents Chemother. 1982 Oct;22(4):548–553. doi: 10.1128/aac.22.4.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw W. V. The problems of drug-resistant pathogenic bacteria. Comparative enzymology of chloramphenicol resistance. Ann N Y Acad Sci. 1971 Jun 11;182:234–242. doi: 10.1111/j.1749-6632.1971.tb30660.x. [DOI] [PubMed] [Google Scholar]
- Speciale A., Stefani S., Caccamo F., Nicolosi V. M., Nicoletti G. The sensitivity of gram-negative and gram-positive bacteria to ofloxacin. Drugs Exp Clin Res. 1987;13(9):555–561. [PubMed] [Google Scholar]
- Wallerstein R. O., Condit P. K., Kasper C. K., Brown J. W., Morrison F. R. Statewide study of chloramphenicol therapy and fatal aplastic anemia. JAMA. 1969 Jun 16;208(11):2045–2050. [PubMed] [Google Scholar]
- West B. C., DeVault G. A., Jr, Clement J. C., Williams D. M. Aplastic anemia associated with parenteral chloramphenicol: review of 10 cases, including the second case of possible increased risk with cimetidine. Rev Infect Dis. 1988 Sep-Oct;10(5):1048–1051. doi: 10.1093/clinids/10.5.1048. [DOI] [PubMed] [Google Scholar]
- van Klingeren B., van Embden J. D., Dessens-Kroon M. Plasmid-mediated chloramphenicol resistance in Haemophilus influenzae. Antimicrob Agents Chemother. 1977 Mar;11(3):383–387. doi: 10.1128/aac.11.3.383. [DOI] [PMC free article] [PubMed] [Google Scholar]


