Key Points
Question
Is the Semont-plus maneuver (SM-plus) or the Epley maneuver (EM) a better therapeutic option in patients with posterior canal benign paroxysmal positional vertigo?
Findings
In this randomized clinical trial of 195 participants, the mean (SD) days until no positional vertigo attacks could be induced was 2.0 (1.6; median, 1 [range, 1-8]) in the SM-plus group and 3.3 (3.6; median, 2 [range, 1-20]) in the EM group.
Meaning
The SM-plus is superior to the EM in terms of the number of days until recovery in posterior canal benign paroxysmal positional vertigo.
This randomized clinical trial compares the efficacy of the Semont-plus maneuver and the Epley maneuver in patients with posterior canal benign paroxysmal positional vertigo.
Abstract
Importance
Questions remain concerning treatment efficacy for the common condition of benign paroxysmal positional vertigo (BPPV).
Objective
To compare the effectiveness of the Semont-plus maneuver (SM-plus) and the Epley maneuver (EM) for treatment of posterior canal benign paroxysmal positional vertigo (pcBPPV) canalolithiasis.
Design, Setting, and Participants
This prospective randomized clinical trial was performed at 3 national referral centers (in Munich, Germany; Siena, Italy; and Bruges, Belgium) over 2 years, with a follow-up to 4 weeks after the initial examination. Recruitment took place from June 1, 2020, until March 10, 2022. Patients were selected randomly during routine outpatient care after being referred to 1 of the 3 centers. Two hundred fifty-three patients were assessed for eligibility. After consideration of the exclusion criteria as well as informed consent, 56 patients were excluded and 2 declined to participate, with 195 participants included in the final analysis. The analysis was prespecified and per-protocol.
Interventions
After being randomized to the SM-plus or the EM group, patients received 1 initial maneuver from a physician, then subsequently performed self-maneuvers at home 3 times in the morning, 3 times at noon, and 3 times in the evening.
Main Outcome and Measures
Patients had to document whether they could provoke positional vertigo every morning. The primary end point was the number of days until no positional vertigo could be induced on 3 consecutive mornings. The secondary end point was the effect of the single maneuver performed by the physician.
Results
Of the 195 participants included in the analysis, the mean (SD) age was 62.6 (13.9) years, and 125 (64.1%) were women. The mean (SD) time until no positional vertigo attacks could be induced in the SM-plus group was 2.0 (1.6) days (median, 1 [range, 1-8] day; 95% CI, 1.64-2.28 days); in the EM group, 3.3 (3.6) days (median, 2 [range, 1-20] days; 95% CI, 2.62-4.06 days) (P = .01; α = .05, 2-tailed Mann-Whitney test). For the secondary end point (effect of a single maneuver), no significant difference was detected (67 of 98 [68.4%] vs 61 of 97 [62.9%]; P = .42; α = .05). No serious adverse event was detected with both maneuvers. Nineteen patients (19.6%) in the EM group and 24 (24.5%) in the SM-plus group experienced relevant nausea.
Conclusions and Relevance
The SM-plus self-maneuver is superior to the EM self-maneuver in terms of the number of days until recovery in pcBPPV.
Trial Registration
ClinicalTrials.gov Identifier: NCT05853328
Introduction
Benign paroxysmal positional vertigo (BPPV) is characterized by recurrent brief episodes of spinning positional vertigo, provoked by lying down or turning over in the supine position.1 Benign paroxysmal positional vertigo is caused by otoconia that most often move freely in the affected semicircular canal (canalolithiasis).2 In about 60% to 90% of cases, the posterior canal is affected,3,4 termed posterior canal BPPV (pcBPPV) canalolithiasis.
Changes of head position relative to gravity can move the otoconia out of the affected canal. At present, the therapy of choice for pcBPPV is the Epley repositioning maneuver (EM)5 and the Semont maneuver (SM).6 Both treatments are classified as level 1 efficacy based on evidence-based medicine with a high success rate of up to 95%7,8 if performed correctly.
The EM requires the supine patient’s head and trunk to be rotated after being tilted backward into a slightly head-hanging position5 with a pillow under the patient’s shoulder to reduce the discomfort.9 The success rate can be improved by repeating the maneuver 2 to 3 times in 1 session.10
With the SM, the patient’s head is first rotated by 45° to the side of the nonaffected labyrinth to bring the affected posterior canal into the plane of the positional maneuver.6 Then the patient is turned 90° to the side of the affected labyrinth; he or she should maintain this position for 1 minute, lying on their side.11 Afterward, the patient is quickly turned by 180° to the side of the unaffected labyrinth, where he or she again has to remain lying for 1 minute. Finally, the patient sits up and has to maintain this position for 1 minute.
A direct comparison of the SM and the EM found no differences in their efficacy.7,12,13,14,15,16 The choice of the maneuver should depend on which maneuver the therapist has the most experience with or whether there are any individual contraindications. Patients with obesity are easier to treat with the EM, while the SM is more suitable for patients with shoulder and neck problems. Although the treatment maneuvers per se are effective for the treatment of BPPV, a meta-analysis17 showed that elderly patients in particular experience BPPV longer and are more impaired than previously assumed.
The SM and EM can also be successfully applied as self-maneuvers, namely with the modified Epley self-maneuvers with a pillow under the shoulder,18 which was also used in this study. For self-maneuvers, thorough guidance by demonstration and pictures is necessary. The success rates (50%-90% after 1 week containing 21 treatment sessions) are not as high as when a therapist performs the maneuver, and it takes longer until the patient is symptom-free.19
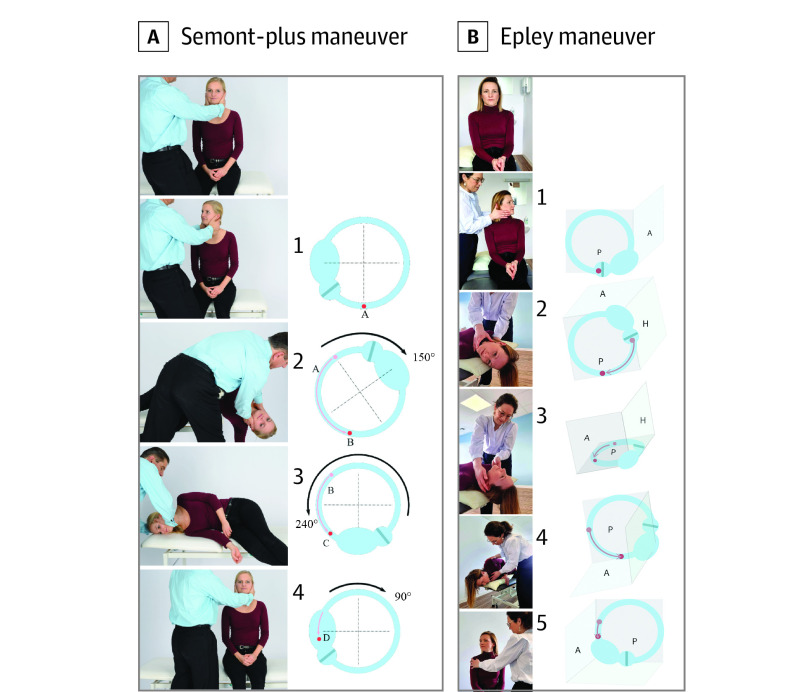
A biophysical model and computer simulations showed that during the rotation of the labyrinth, the crystals move about 25° less than during rotation in the plane of the affected canal.11 Based on these findings, the SM-plus was developed (Figure 1, Video 1 [demonstration of the SM-plus], and Video 2 [demonstration and computer simulation of the SM-plus]; the EM is shown in Figure 1 and in Video 3). When the patient’s body is moved toward the affected side, the angle should be at least 150°, that is, 60° below the earth horizontal; in this way, the otoconia move much further in the direction of the utricle. Subsequently, the patient is moved by at least 240° toward the nonaffected side and the clot of otoconia is then already putatively beyond the vertex of the canal,11 which increases the efficacy of the maneuver. In a previous prospective randomized tricenter study,20 it was found that the SM-plus is superior to the regular SM; in the 194 patients analyzed (96 receiving SM and 98 receiving SM-plus), a median of 2 (range, 1-21; mean, 3.6) days was needed for recovery with SM and 1 (range, 1-8; mean, 1.8) day with SM-plus (P < .001; α = .05, Mann-Whitney test).
Figure 1. Schematic Drawing of the Movement of the Otoconia of the Semont-plus Maneuver and Epley Maneuver for Benign Paroxysmal Positional Vertigo of the Left Posterior Canal.
A, The Semont-plus maneuver includes the upright position with (1) turning of the head by 45° toward the nonaffected side; (2) movement of the body by 150° toward the affected side, which moves the otoconia further in the direction in which they should move (A toward B); (3) and since the clot is beyond the vertex (B toward C), the movement of body by 240° moves the clot into the direction (4) of the vestibulum (position D of the otoconia). B, The Epley maneuver includes upright position and (1) rotation of the head 45° toward the affected ear; (2) movement of the body backward so that the head is in a hanging position below the earth horizontal; (3) rotation of the head 90° toward the nonaffected ear; (4) rotation of the whole body downward so that the patient faces the floor and their affected ear is pointing toward the ceiling; and (5) going into the upright position while keeping a rotation of the head 45° toward the nonaffected ear, and turning the head back to the neutral position at the end. A indicates anterior semicircular canal; H, horizontal semicircular canal; and P, posterior semicircular canal.
Video 1. Demonstration of the Semont-Plus Self-maneuver for Right Posterior Canal Canalithiasis.
The patient first turns her head 45° to the left. Then she extends her right arm and subsequently moves the whole body by 150°or more to the right side. This position is kept for 60 seconds. Subsequently, the patient moves her whole body by 240° toward the nonaffected side. Finally, after another 60 seconds, the patient sits up for another 60 seconds.
Video 2. Semont-Plus Maneuver for Right Posterior Canal Benign Paroxysmal Positional Vertigo.
Demonstration of the maneuver (left) and computer simulation of the movement of the otoconia within the semicircular canal (right). According to the simulation, the otoconia move beyond the vertex of the canal after the first body movement toward the affected ear. Used with permission from Anita Bhandari, MD (Vertigo and Ear Clinic, Jaipur, India).
Video 3. Demonstration of the Epley Self-maneuver for a Right Posterior Canal Canalithiasis.
The patient is sitting with both feet on the table or bed, looking forward. Subsequently, she lets herself fall backward with a pillow under her shoulder and the head is turned 45° to the right. She stays in this position for 30 seconds. Afterward, she turns her head quickly 90° to the left side followed by a turn of the whole body to the left so that her nose is pointing at the floor. She stays in this position for another 30 seconds. Subsequently, the patient sits up with her head still turned 45° to the left. She can help herself by using both arms. After a few seconds, she can turn her head slowly back to the neutral position, facing forward.
In the current study, we applied a similar study design with the same primary end point (mornings until recovery) to compare the efficacy of the SM-plus with the EM in patients with pcBPPV canalolithiasis. Because patients with BPPV typically have symptoms more frequently in the morning, we chose morning symptoms as an end point measurement. This can be explained by an aggregation of the otoconia during rest in the night, which has a higher hydrodynamic impact on the endolymphatic fluid than a single otoconium.11 Further, since self-maneuvers are less effective than those by a therapist, patients should perform the treatment maneuvers 3 times in the morning, 3 times at noon, and 3 times at night (ie, 9 times per day) in this study.
Methods
Study Population and Randomization
Patients were recruited in 3 academic centers in 3 countries: Department of Neurology and German Center for Vertigo and Balance Disorders, Ludwig Maximilian University Hospital, Munich, Germany; Department of ENT (Ear, Nose, and Throat), AZ Sint-Jan Brugge, Brugge, Belgium; and Department of ENT, University of Siena, Siena, Italy. Recruitment took place from June 1, 2020, until March 10, 2022. The analysis was prespecified and per protocol (Supplement 1). Written consent was obtained from all participants. The study was approved by the local ethics committees of each center, with an exception for Siena. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
This study was retrospectively registered because, according to German and European regulators, registration was not required; however, we registered the trial at the request of the editors. (Regulation EU No. 536/2014 of the European Parliament and of the Council of 16 April 2014 on clinical trials on medicinal products for human use, and repealing Directive 2001/20/EC.)
Inclusion Criteria
Patients were eligible for inclusion if 18 years or older with a capacity to consent and a diagnosed pcBPPV canalolithiasis according to the diagnostic criteria of the Classification Committee of Vestibular Disorders of the Bárány Society in 2015.1 The diagnostic criteria include repetitive episodes of vertigo or dizziness provoked by rapid head acceleration or deceleration, duration of attacks of less than 1 minute, and positional vertical-torsional nystagmus provoked in the diagnostic Dix-Hallpike maneuver14 or diagnostic SM with a crescendo-decrescendo time course.
Exclusion Criteria
Patients without a capacity for consent, younger than 18 years, and/or not willing or not able to perform the assigned maneuver were excluded. A method of simple randomization was used to generate the random allocation sequence (coin flip or a random number generator).
Treatment and Study Flow
The patients presented to routine outpatient care in 1 of the 3 centers. The patient history was taken followed by a standard neurological and neuro-otological examination, a video head impulse test, and caloric testing. After performing the routine diagnostic maneuvers, a pcBPPV canalolithiasis was diagnosed according to the aforementioned criteria.1 The patient was informed about the study, consented, and was allocated randomly 1:1 to one of the treatment groups (EM or SM-plus) in a consecutive order.
A first treatment maneuver was performed once by a physician according to the assigned treatment group. For the SM-plus, the angle of the 60° overextended head and body was measured by an inclinometer application. The patient simultaneously received verbal instructions on how to perform the maneuver. Fifteen minutes after the first diagnostic maneuver, a second diagnostic maneuver was performed to evaluate the effect of a single maneuver.
For the self-maneuvers, patients received written instructions with figures on how to perform the SM-plus or the EM independently in a home environment. For the self-maneuver at home, the modified Epley self-maneuver19 was done by the patient with a pillow under the shoulders. The frequency of performance at home was 3 times in the morning, 3 times at noon, and 3 times in the evening (ie, 9 times per day).
The patient received a standardized documentation form. The study participant had to fill out the form, documenting how many mornings it took until the patient experienced no more positional vertigo; in addition, patients could also add additional comments, such as adverse effects of the maneuvers. The morning when the first maneuver induced no positional vertigo was noted and the patient then had to perform the diagnostic maneuvers for another 2 days to make sure that he or she was free of symptoms. If this was the case, they could stop the treatment. If not, the treatment had to be continued as well as the evaluation. The filled-out form was sent back by the patient to the study center in an envelope that the participant had received at inclusion in the study.
End Points
The primary end point is the number of days, specifically the first morning, until the patient was free of positional vertigo for that morning and 2 subsequent mornings. The day of inclusion was defined as day 0.
As a secondary end point, the success rate of a single performance of the maneuver by a physician was tested. In the study population, we investigated how many patients in both treatment groups become free of vertigo and nystagmus after a single performance of the allocated treatment maneuver by a physician.
Statistical Analysis
Since the parameter mornings to recovery was not normally distributed, a 2-tailed Mann-Whitney test was performed to compare the 2 study groups, considering P < .05 as statistically significant. For the secondary outcome, χ2 testing was applied. Dropouts were not replaced or imputed in the end point analyses. Computations and illustrations used R, version 4.1.2 (R Project for Statistical Computing), and Adobe Illustrator, version 27.2 (Adobe). Data management and sorting were executed using Excel LTSC MSO, version 16.0.14332 (Microsoft Corp).
Results
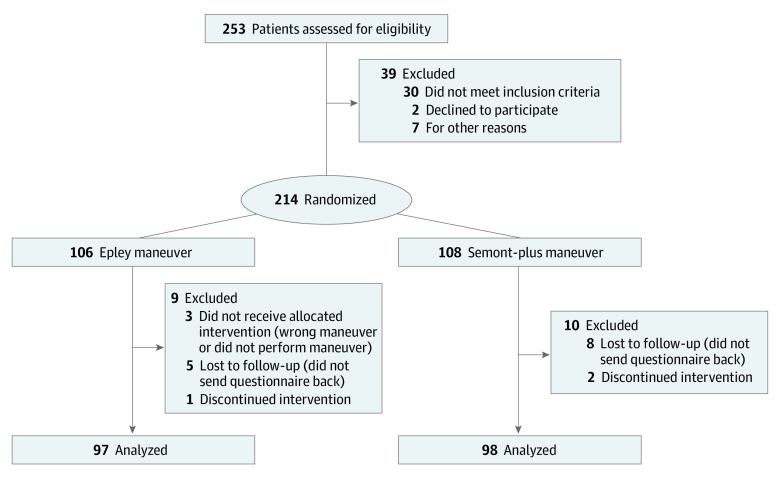
In total, 253 patients were assessed for eligibility (Figure 2). Thirty were excluded due to not meeting the inclusion criteria, 2 declined to participate, and 7 were excluded for other reasons. Two hundred fourteen patients were randomized in the 2 treatment groups, with 106 allocated to EM and 108 to SM-plus. Of the EM group, 3 patients did not receive the allocated treatment, 1 discontinued the intervention due to anxiety, and 5 were lost to follow-up. Of the SM-plus group, 2 patients were excluded due to discontinued intervention and performing the wrong maneuver and 8 were lost to follow-up. One of these patients went to a physiotherapist who performed the wrong maneuver and 1 more did not apply the 60° overextension of the head due to anxiety; both patients confirmed these experiences during the follow-up. In total, 195 patients were included in the analysis (mean [SD] age, 62.6 [13.9] years; 125 women [64.1%] and 70 men [35.9%]). Of these, 97 patients were allocated to the EM group and 98 to the SM-plus group, with 45 from the center in Germany, 54 from the center in Belgium, and 96 from the center in Italy. The mean (SD) age of the patients allocated to the EM group was 60.9 (13.8) years; for those in the SM-plus group, 64.4 (13.9) years. Thirty men and 67 women were allocated to the EM group; 40 men and 58 women, to SM-plus group. In the SM-plus group, 56 patients were experiencing a first BPPV episode, while the condition was recurrent in 36 and data were missing on 6 occasions; the etiology was idiopathic in 84 of 98 patients. Of the 97 patients who were treated with the EM, 62 had their first BPPV manifestation and in 33 the condition was recurrent. The etiology in the EM group was idiopathic in 84 of 97 patients. Fifty-eight of 97 patients in the EM group and 61 of 98 in the SM-plus group had a right-sided BPPV (Table).
Figure 2. Study Flowchart.
Table. Characteristics of the Study Population.
| Characteristic | Intervention | |
|---|---|---|
| Epley maneuver (n = 97) | Semont-plus maneuver (n = 98) | |
| Age, mean (SD) [range], y | 60.9 (13.8] [26-88] | 64.4 (13.9) [25-91] |
| Sex, No. (%) | ||
| Men | 30 (31) | 40 (41) |
| Women | 67 (69) | 58 (59) |
| Time until recovery, da | ||
| Mean (SD) | 3.3 (3.6) | 2.0 (1.6) |
| Median (range) | 2 (1-20) | 1 (1-8) |
| 95% CI | 2.62-4.06 | 1.64-2.28 |
| No. with first-time/recurrent episode/missing data | 62/33/2 | 56/36/6 |
| No. with affected right side/affected left side/missing data | 58/38/1 | 61/35/2 |
| No. with etiology idiopathic/nonidiopathic/missing data | 84/11/2 | 84/9/5 |
| Time until recovery for patients with a first-time BPPV, d | ||
| Mean (SD) | 2.9 (3.6) | 1.5 (0.9) |
| Median (range) | 1 (1-20) | 1 (1-5) |
| 95% CI | 1.96-3.77 | 1.22-1.67 |
| Time until recovery for patients with a recurrent BPPV, d | ||
| Mean (SD) | 4.1 (3.5) | 2.7 (2.2) |
| Median (range) | 3 (1-13) | 2 (1-8) |
| 95% CI | 2.85-5.27 | 2.02-3.43 |
| Time until recovery for patients with an idiopathic BPPV, d | ||
| Mean (SD) | 2.8 (2.9) | 2.0 (1.6) |
| Median (range) | 1 (1-14) | 1 (1-8) |
| 95% CI | 2.20-3.45 | 1.61-2.29 |
| Time until recovery for patients with a nonidiopathic BPPV, d | ||
| Mean (SD) | 6.8 (5.8)b | 2.0 (1.8)b |
| Median (range) | 5 (1-20) | 1 (1-8) |
| 95% CI | 3.39-10.25 | 0.80-3.20 |
Abbreviation: BPPV, benign paroxysmal positional vertigo.
Indicates number of days until no vertigo could be induced after performing a single self-maneuver (P = .01; α = .05, 2-tailed Mann-Whitney test).
Population SD was used due to small sample size.
The mean (SD) time until no more positional vertigo attacks could be induced by patients in the SM-plus group was 2.0 (1.6) days (median, 1 [range, 1-8] days; 95% CI, 1.64-2.28 days) (Figure 3). In the EM group, the mean (SD) time until recovery was 3.3 (3.6) days (median, 2 [range, 1-20] days; 95% CI, 2.62-4.06 days). The 2-tailed Mann-Whitney test revealed a statistically significant difference (P = .01; α = .05). A post hoc descriptive subgroup analysis is given in the Table.
Figure 3. Primary End Point.
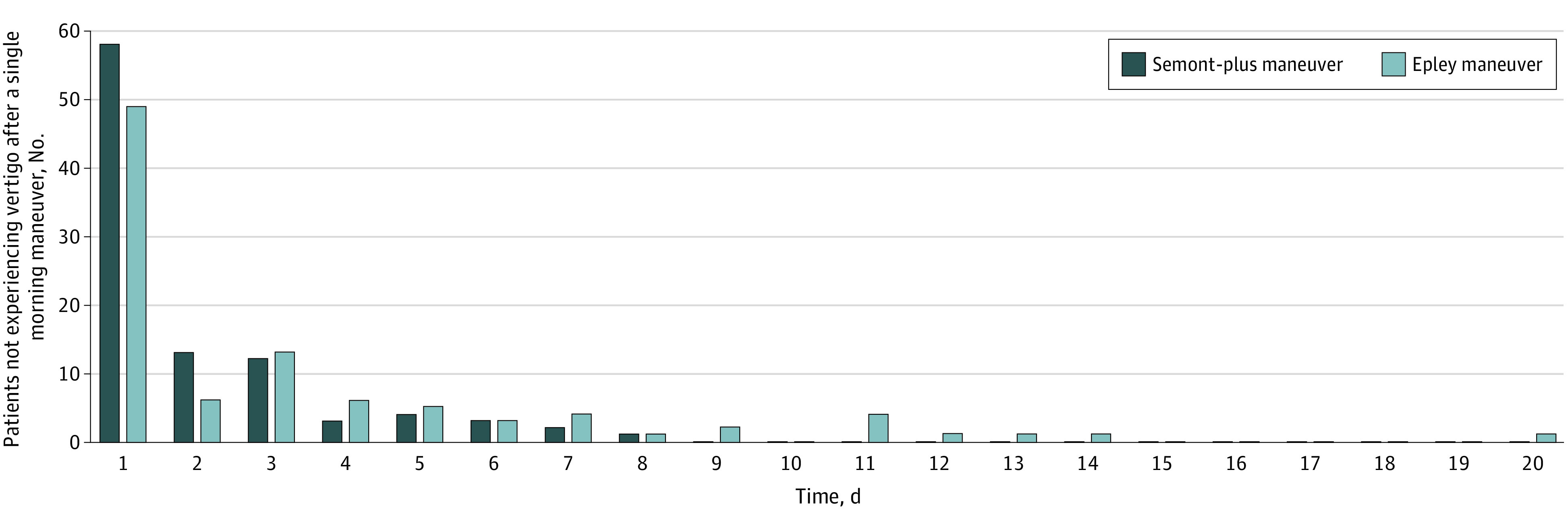
Histogram of days until no positional vertigo could be induced with the Semont-plus maneuver and Epley maneuver.
For the secondary end point, effects of a single SM-plus or EM, 67 of 98 patients (68.4%) in the SM-plus group did not experience any vertigo and/or positional nystagmus after performance of a single therapeutic maneuver. In the EM group, this applied to 61 of 97 patients (62.9%). The χ2 test revealed no difference between groups (P = .42; α = .05). However, of those patients who had no BPPV after the first maneuver, 17 of 67 (25.4%) in the SM-plus group and 15 of 61 (24.6%) in the EM group experienced positional vertigo again the next morning.
Safety
No severe adverse effects were detected in both the SM-plus and the EM group. Nineteen patients assigned to the EM group (19.6%) experienced nausea during the therapeutic self-maneuver, 1 was too anxious during the maneuver, and 1 experienced strong dizziness after the maneuver. A patient in the EM group reported severe transpiration and dizziness during the maneuver. In the SM-plus group, 24 patients experienced severe nausea (24.5%), 1 patient reported vomiting after performing the maneuver, and 1 found the maneuver physically too difficult to execute because of severe anxiety.
Discussion
In this prospective randomized clinical trial, we found that in pcBPPV canalolithiasis, the SM-plus is more effective than the EM in terms of days until recovery (median, 1 [range, 1-8] vs 2 [range, 1-20] days). We could confirm and thereby reproduce the findings of the previous study with the SM-plus20 in terms of the time until patients become free of symptoms (median, 1 day). Additionally, previous direct comparisons of the SM and the EM found no differences in their efficacy.7,12,13,14,15,16 This agrees with an indirect comparison of the days it takes for the SM to produce recovery in the previous study20 (mean, 3.6 days) and the EM in the current study (mean, 3.3 days). Both findings show that our data are evidently robust.
In terms of the effect of the first treatment maneuver, which was done by a physician, 68.4% of patients who received the SM-plus and 62.9% of those who received the EM did not experience vertigo or positional nystagmus. However, of those patients who had no BPPV after this first maneuver, 25.4% in the SM-plus group and 24.6% in the EM group experienced positional vertigo again the next morning (ie, they were not cured by a single maneuver). This underlines that in many patients, several maneuvers are needed.
The explanation for the superiority of the SM-plus over the SM20 was the overextension by 60° of the head and body below earth horizontal during step 2 of the SM-plus. A biophysical model11 showed that (1) the otoconia move after, for instance, a 90° turn, about 25° less, and (2) by increasing the angle by, for instance, 60°, they move another 60° into the direction of the exit of the canal, positioning them already beyond the apex of the vertex canal when the patient moves by 240° into the opposite direction. If this model is accurate, it demonstrates why the likelihood of expelling the otoconia is increased.
How can the superiority of the SM-plus over the EM be explained? First, in another biophysical study it was demonstrated how important the orientation of the affected canal is during the maneuvers relative to the gravitational vector21: angles larger than 67° or smaller than 21° did not lead to a successful repositioning, even after a waiting period of 5 minutes. It is conceivable that for the EM, the orientation relative to the gravitational vector is not always perfect during each step of the movements (Figure 1). This interpretation is supported by 2 recent studies22,23 in which the angular accuracy of the EM was measured showing a wide range of angular inaccuracy at each stage. Second, recommended duration for each maneuver is different, at 60 seconds for SM-plus and 30 seconds for EM. Since time matters for the movement of the otoconia to reach the lowest point relative to gravity, as was also demonstrated in the biophysical model—namely, if there are only single crystals and not a large agglomerate11—this may also explain the difference between the EM and SM-plus.
For the discussion of other aspects of our findings, namely immediate success rate, issues of self-treatment, combination of treatment maneuvers, and total number of maneuvers needed, we refer to the Discussion in the previous study by Strupp et al with a similar design.20 As for the safety of both maneuvers, no serious adverse effects were detected. The percentage of people who experienced nausea in both study groups was similar and comparable. A systematic review7 revealed nausea during the EM in 16.7% to 32% of patients, similar to our study. The exaggerated head positions when performing the SM-plus may cause more anxiety and may be more difficult to execute in patients with a limited physical capability as well as cervical issues.
Limitations
The following limitations must be taken into account when considering this trial. First, we had no control over how well patients performed self-maneuvers at home. However, the combination of an initial treatment by the clinician and subsequent self-maneuvers by the patient reflects clinical treatment of BPPV. This issue can be addressed by remote management (eg, with cell phone videos taken by a third person or by the patient themselves). That would also help the physician to evaluate how the maneuvers are performed during an online or an in-person consultation.24 Second, the primary end point (days until recovery) was left to the patients’ self-report. Despite extensive instructions by the examiners, there is no real control over how patients reported this, leaving a margin for falsely documented primary outcome. However, there should be no difference for the SM-plus and EM in our study. Third, we did not compare the efficacy of the SM-plus and EM when performed repeatedly by therapists only.
Conclusions
This prospective randomized study provides evidence that, in patients with pcBPPV canalolithiasis, the SM-plus maneuver is superior to the EM in terms of the time until no positional vertigo could be induced by the patient. Hence, the SM-plus can be recommended in clinical practice.
Trial Protocol
Data Sharing Statement
References
- 1.von Brevern M, Bertholon P, Brandt T, et al. Benign paroxysmal positional vertigo: diagnostic criteria. J Vestib Res. 2015;25(3-4):105-117. doi: 10.3233/VES-150553 [DOI] [PubMed] [Google Scholar]
- 2.Brandt T, Steddin S, Daroff RB. Therapy for benign paroxysmal positioning vertigo, revisited. Neurology. 1994;44(5):796-800. doi: 10.1212/WNL.44.5.796 [DOI] [PubMed] [Google Scholar]
- 3.Korres S, Balatsouras DG, Kaberos A, Economou C, Kandiloros D, Ferekidis E. Occurrence of semicircular canal involvement in benign paroxysmal positional vertigo. Otol Neurotol. 2002;23(6):926-932. doi: 10.1097/00129492-200211000-00019 [DOI] [PubMed] [Google Scholar]
- 4.Moon SY, Kim JS, Kim BK, et al. Clinical characteristics of benign paroxysmal positional vertigo in Korea: a multicenter study. J Korean Med Sci. 2006;21(3):539-543. doi: 10.3346/jkms.2006.21.3.539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992;107(3):399-404. doi: 10.1177/019459989210700310 [DOI] [PubMed] [Google Scholar]
- 6.Semont A, Freyss G, Vitte E. Curing the BPPV with a liberatory maneuver. Adv Otorhinolaryngol. 1988;42:290-293. doi: 10.1159/000416126 [DOI] [PubMed] [Google Scholar]
- 7.Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014;(12):CD003162. doi: 10.1002/14651858.CD003162.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhattacharyya N, Gubbels SP, Schwartz SR, et al. Clinical practice guideline: benign paroxysmal positional vertigo (update). Otolaryngol Head Neck Surg. 2017;156(3_suppl):S1-S47. doi: 10.1177/0194599816689667 [DOI] [PubMed] [Google Scholar]
- 9.Lee HJ, Jeon EJ, Lee DH, Seo JH. Therapeutic efficacy of the modified Epley maneuver with a pillow under the shoulders. Clin Exp Otorhinolaryngol. 2020;13(4):376-380. doi: 10.21053/ceo.2019.01830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gordon CR, Gadoth N. Repeated vs single physical maneuver in benign paroxysmal positional vertigo. Acta Neurol Scand. 2004;110(3):166-169. doi: 10.1111/j.1600-0404.2004.00296.x [DOI] [PubMed] [Google Scholar]
- 11.Obrist D, Nienhaus A, Zamaro E, Kalla R, Mantokoudis G, Strupp M. Determinants for a successful Sémont maneuver: an in vitro study with a semicircular canal model. Front Neurol. 2016;7:150. doi: 10.3389/fneur.2016.00150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen HS, Jerabek J. Efficacy of treatments for posterior canal benign paroxysmal positional vertigo. Laryngoscope. 1999;109(4):584-590. doi: 10.1097/00005537-199904000-00012 [DOI] [PubMed] [Google Scholar]
- 13.Herdman SJ, Tusa RJ. Complications of the canalith repositioning procedure. Arch Otolaryngol Head Neck Surg. 1996;122(3):281-286. doi: 10.1001/archotol.1996.01890150059011 [DOI] [PubMed] [Google Scholar]
- 14.Massoud EA, Ireland DJ. Post-treatment instructions in the nonsurgical management of benign paroxysmal positional vertigo. J Otolaryngol. 1996;25(2):121-125. [PubMed] [Google Scholar]
- 15.Soto Varela A, Bartual Magro J, Santos Pérez S, et al. Benign paroxysmal vertigo: a comparative prospective study of the efficacy of Brandt and Daroff exercises, Semont and Epley maneuver. Rev Laryngol Otol Rhinol (Bord). 2001;122(3):179-183. [PubMed] [Google Scholar]
- 16.Steenerson RL, Cronin GW. Comparison of the canalith repositioning procedure and vestibular habituation training in forty patients with benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1996;114(1):61-64. doi: 10.1016/S0194-59989670284-X [DOI] [PubMed] [Google Scholar]
- 17.Sim E, Tan D, Hill K. Poor treatment outcomes following repositioning maneuvers in younger and older adults with benign paroxysmal positional vertigo: a systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20(2):224.e1-224.e23. doi: 10.1016/j.jamda.2018.11.019 [DOI] [PubMed] [Google Scholar]
- 18.Radtke A, von Brevern M, Tiel-Wilck K, Mainz-Perchalla A, Neuhauser H, Lempert T. Self-treatment of benign paroxysmal positional vertigo: Semont maneuver vs Epley procedure. Neurology. 2004;63(1):150-152. doi: 10.1212/01.WNL.0000130250.62842.C9 [DOI] [PubMed] [Google Scholar]
- 19.Radtke A, Neuhauser H, von Brevern M, Lempert T. A modified Epley’s procedure for self-treatment of benign paroxysmal positional vertigo. Neurology. 1999;53(6):1358-1360. doi: 10.1212/WNL.53.6.1358 [DOI] [PubMed] [Google Scholar]
- 20.Strupp M, Goldschagg N, Vinck AS, et al. BPPV: Comparison of the SémontPLUS With the Sémont maneuver: a prospective randomized trial. Front Neurol. 2021;12(65257):652573. doi: 10.3389/fneur.2021.652573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gebhart I, Götting C, Hool SL, et al. Sémont maneuver for benign paroxysmal positional vertigo treatment: moving in the correct plane matters. Otol Neurotol. 2021;42(3):e341-e347. doi: 10.1097/MAO.0000000000002992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kwon C, Ku Y, Seo S, et al. Quantitative assessment of self-treated canalith repositioning procedures using inertial measurement unit sensors. J Vestib Res. 2021;31(5):423-431. doi: 10.3233/VES-190747 [DOI] [PubMed] [Google Scholar]
- 23.Murphy C, Keogh IJ. Measuring the angular accuracy of a clinician-performed Epley maneuver used to treat benign paroxysmal positional vertigo. Otol Neurotol. 2023;44(1):61-65. doi: 10.1097/MAO.0000000000003751 [DOI] [PubMed] [Google Scholar]
- 24.Strupp M, Mavordiev V, Goldschagg N. Triple benign paroxysmal positional vertigo and the strength of remote video-based management. JAMA Neurol. 2023. doi: 10.1001/jamaneurol.2022.4861 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
Data Sharing Statement