Abstract
Background
Infants with chronic kidney disease (CKD) form a vulnerable population who are highly prone to mineral and bone disorders (MBD) including biochemical abnormalities, growth retardation, bone deformities, and fractures. We present a position paper on the diagnosis and management of CKD-MBD in infants based on available evidence and the opinion of experts from the European Society for Paediatric Nephrology (ESPN) CKD-MBD and Dialysis working groups and the Pediatric Renal Nutrition Taskforce.
Methods
PICO (Patient, Intervention, Comparator, Outcomes) questions were generated, and relevant literature searches performed covering a population of infants below 2 years of age with CKD stages 2–5 or on dialysis. Clinical practice points (CPPs) were developed and leveled using the American Academy of Pediatrics grading matrix. A Delphi consensus approach was followed.
Results
We present 34 CPPs for diagnosis and management of CKD-MBD in infants, including dietary control of calcium and phosphate, and medications to prevent and treat CKD-MBD (native and active vitamin D, calcium supplementation, phosphate binders).
Conclusion
As there are few high-quality studies in this field, the strength of most statements is weak to moderate, and may need to be adapted to individual patient needs by the treating physician. Research recommendations to study key outcome measures in this unique population are suggested.
Graphical Abstract
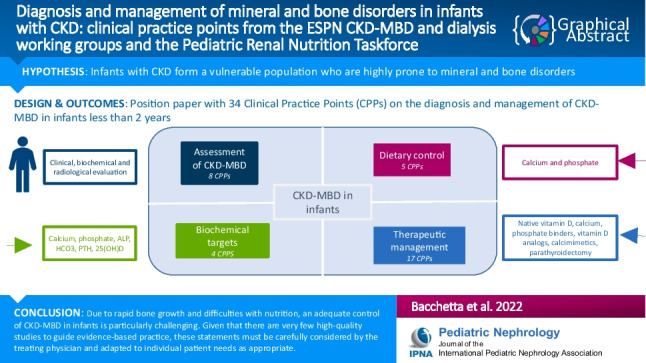
A higher resolution version of the Graphical abstract is available as Supplementary information
Supplementary Information
The online version contains supplementary material available at 10.1007/s00467-022-05825-6.
Keywords: Infants, Dialysis, Mineral and bone disorders, Calcium, Phosphate, PTH, Bone, Clinical practice points
Introduction
Chronic kidney disease (CKD) affects 1 in 10,000 live births. Although survival of infants requiring chronic dialysis has improved over the past years, both morbidities and mortality remain higher in the youngest patients [1–5]. Infants with CKD are especially prone to mineral and bone disorders (MBD). Infancy represents the period of most rapid growth resulting in high demands of calcium (Ca) and phosphate (P) in order to build a positive mineral balance and adequate endochondral ossification [6]. This makes infants with CKD particularly vulnerable for complications such as rickets, skeletal deformities, bone pain, and growth retardation. Ca deficiency may further worsen secondary hyperparathyroidism (SHPT), especially in conjunction with P deficiency, lead to mineralization abnormalities and rickets [7, 8]. These problems are compounded as the youngest of these infants depend largely on a milk-based diet, and commonly have feeding difficulties that may further complicate the management of CKD-MBD.
Pediatric guidelines have been published for bone and nutritional evaluation in children with CKD 2-5D [9, 10], but there are few studies on the diagnosis and management of CKD-MBD in neonates and infants, and therapeutic decisions are largely based on limited evidence. Here, we present clinical practice points addressing the diagnosis and management of CKD-MBD in children up to 2 years of age based on the available evidence, extrapolation from studies in older children where appropriate, and expert opinion of the European Society for Paediatric Nephrology (ESPN), CKD-MBD and Dialysis working groups (WGs) and the Pediatric Renal Nutrition Taskforce (PRNT).
Methods
The consensus development group
Two groups were assembled: a core working group and a Delphi panel. The core group comprised pediatric nephrologists and a pediatric kidney dietitian who were members of at least one of the above WG (i.e., ESPN dialysis, ESPN CKD-MBD, and/or PRNT), and who defined the scope of the project, formulated the PICO questions, performed a critical appraisal of the literature, rated the quality of evidence, GRADE-ed recommendations, conducted the Delphi process, and drafted the manuscript. The Delphi group included members of ESPN CKD-MBD and dialysis WGs, PRNT, and two neonatologists with a special interest in neonatal nephrology.
Developing PICO questions
In order to give specific actionable advice, we developed PICO questions and formulated into actionable statements supported by the available evidence as follows:
Patient (or population) includes children below 2 years with CKD or on dialysis, but three age ranges will be identified when necessary: neonates (0–1 month), 1–12 months, and 1–2 years. Indeed, while neonates correspond to a very specific group with distinct clinical and ethical issues [11–13], in infants less than 1 year kidney maturation, rapid growth and weaning may present additional issues that impact on MBD. We will also include infants born pre-term (with corrected gestational age) as there is an increased incidence of prematurity in infants with CKD [14, 15], and as nephrons continue to form up to 36 weeks of corrected gestational age [16–18].
CKD in infants is defined by persistent abnormal creatinine levels above the 97.5th percentile in the first 12 months of life [19, 20], and with estimated glomerular filtration rate (eGFR) < 90 mL/min per 1.73 m2 using the Schwartz formula thereafter [19, 21]. The assessment of kidney function in infants is highly challenging and beyond the scope of this guideline.
Intervention may be “no action,” placebo, or an alternative therapeutic intervention.
Comparison: Growth and biochemical markers were compared to healthy infants [22, 23], accounting for the effect of prematurity where relevant.
Outcomes included growth, delayed motor milestones (e.g., walking and standing), bone disease (e.g., rickets, fractures, bowing), as well as the evolution of the biochemical parameters including Ca, P, bicarbonate (HCO3), parathyroid hormone (PTH), 25-hydroxyvitamin D (25(OH)D), and alkaline phosphatase (ALP) levels.
Literature review and studies included
The PubMed database was searched until March 2022. We included the following articles: randomized controlled trials (RCTs), prospective studies (uncontrolled or observational) irrespective of number of patients, and retrospective studies including more than 5 cases, and registry data, all restricted to human studies in English, as summarized in Tables 1 and 2 [1–3, 5, 24–37].
Table 1.
Review of the evidence for observational studies with an evaluation of MBD in infants under 2 years with CKD
| Authors | Year | Ref | Population | Study design | Aim | Outcome |
|---|---|---|---|---|---|---|
| Rees et al. | 2011 | [24] | 153 infants from 18 countries starting chronic peritoneal dialysis < 24 months | Registry study | Associations of feeding practices and other dialysis-related factors with length and weight gain in children |
PTH levels 222 (85 to 529) pg/mL No data on associations of PTH with growth |
| Borzych et al. | 2010 | [26] | 890 children from 24 countries | Registry study | Assessments of CKD-MBD in peritoneal dialysis |
6% < 1 year and 16% < 1–5 years had hypophosphatemia 15% < 1 year and 21% 1–5 years had PTH 9 × above normal (KDIGO) Clinical and radiological symptoms markedly increased when PTH exceeded 300 pg/mL, the risk of hypercalcemia increased with levels below 100 pg/mL, and time-averaged PTH concentrations above 500 pg/mL were associated with impair longitudinal growth Associations were not analyzed separately in infants |
| Seikaly et al. | 2006 | [27] | 5165 children with GFR < 75 | Registry study | Correlates of short stature (< − 1.88) at entry to the registry |
0–2 years had a mean height SDS of − 2.3 Ca, P, and PTH were NOT associated with short statures at entry |
| Schmitz et al. | 2021 | [74] | 41 children, median age 1.1 year, range 0.5–8.0, CKD stage 3 to dialysis | Retrospective multi-center study | To evaluate enteral Ca intake and its association with PTH levels in pre-school children with CKD | Severe Ca deficiency found in 26% of children (with a significant variation between the first and second dietary data collection); 10% of children received enteral Ca above the upper target for age. Negative correlation between dietary calcium intake and PTH levels |
| Cansick et al. | 2007 | [28] | 35 children aged 0.25 to 8.9 years | Retrospective single center study | Association of growth with PTH in children on dialysis |
17 children under 2 years, the median change in HtSDS in the first year on dialysis was + 0.31 (range − 0.78 to 3.13) Significant association of change in HtSDS with ALP but no association of height with PTH in the study population Infants 0–2 years were not analyzed separately |
| Vidal et al. | 2017 | [1] | 1063 infants 12 months or younger who initiated dialysis therapy in 1991 to 2013 | Registry study | The impact of different dialysis modalities on clinical outcomes in young infants with chronic kidney failure | Mean PTH at dialysis initiation 496 (438 to 555) pg/mL similar in PD and HD |
| Shroff et al. | 2006 | [30] | 98 children (61 boys), twenty-one < 1 year of age and 54 under < 5 years | Single center study | Outcome since 1984 of all children receiving chronic dialysis for > 3 months with a minimum follow-up of 5 (median 7.2) years |
The measured intact PTH level at the start of dialysis was less than twice the ULN in 15 (16%) children as compared to a considerably improved control with 80 (88%) children having a PTH level within twice the upper limit of normal at final follow-up or pre-transplantation Separate analysis for infants not available |
| Shroff et al. | 2003 | [31] | 18 children under 2 years of age received chronic hemodialysis (HD) | Single center study | Morbidity and outcome of chronic HD in children under 2 years of age | Intact PTH was less than twice the upper limit of the reference range for the assay in 41% of the children when HD was started and in 69% (n = 11) after 3 months |
| Paglialonga et al. | 2016 | [32] | 21 children < 2 yrs at initiation of HD | Registry study | Outcomes in HD | PTH 169 (76–628) pg/mL at baseline, 336 (136–1088) at 6 months, and 207 (64–900) at 12 months |
| Ledermann et al. | 2000 | [33] | 20 infants with a mean age of 0.34 year (range, 0.02–1 year) | Single center study | Outcome in PD |
Intact PTH was less than twice the upper limit of the reference range in 58% of the infants (n = 12) after 6 months of PD and 100% (n = 14) after 1 year, with the values falling within the normal range in 79% Associations with growth were not assessed |
| Dachy et al. | 2020 | [5] | 17 infants with age 2.6 (0.1;5.9) months at peritoneal dialysis initiation | Retrospective study | Experience of two French tertiary pediatric nephrology centers on 17 infants who began chronic PD before 6 months of age |
Before PD, median PTH levels were 212 (6;799) ng/L, decreasing to 130 (23;732) ng/L 3 months after the beginning of PD, and reaching 123 (44;1540) ng/L at the end of PD (p = NS between PD initiation and the end of PD) Associations of PTH with growth were not assessed |
| Vidal et al. | 2012 | [34] | 84 infants who started CPD at < 1 year of age | Registry study | Growth data analysis was performed only in infants with complete auxological parameters at 0, 6, and 12 months of follow-up |
No significant association of catch-up growth with PTH intact PTH at initiation of dialysis was 508 (10–1760) ng/L at t0 and 351 (33–1650) at t12 in those with catch-up growth vs. 683 (163–2000) at t0 and 398 (81–3500) at t12 in those without catch-up growth |
Table 2.
Review of the evidence for interventional studies with an evaluation of MBD in infants under 2 years with CKD
| Authors | Year | Ref | Population | Study design | Aim | Outcome |
|---|---|---|---|---|---|---|
| Arenas Morales et al. | 2019 | [35] | 10 young pediatric patients median age 18 months (IQR 6–36), CKD5 and dialysis | Case series | Severe sHPT with intact parathyroid hormone (iPTH) levels ≥ 500 pg/mL refractory to standard therapy for > 30 days receiving cinacalcet |
Linear growth improved significantly during cinacalcet therapy in 80% (ΔSDS − 0.62 ± 1.2 versus + 0.91 ± 1.4; p < 0.005). By multiple regression analysis, the primary determinants of growth were concurrent treatment with growth hormone and age < 2 years (R2 = 89.6%; p < 0.001) Average starting dose of 0.7 ± 0.2 mg/kg/day; median effective dose required to reach PTH goal: 2.8 mg/kg/day (IQR 2.0–3.1); 4 patients with asymptomatic hypocalcemia |
| Joseph et al. | 2019 | [36] | 18 patients (9 male) less than 5 years, mean age at initiation of cinacalcet was 2.3 years (range 8 months–4.5 years); 13 PD and 5 HD | Single center case series | Efficacy and safety of cinacalcet for treatment of secondary hyperparathyroidism in chronic dialysis patients younger than 5 years | Significant improvement in linear growth was observed while on cinacalcet and growth hormone; average starting dose of cinacalcet 0.55 mg/kg/day |
| Saarinen et al. | 2007 | [37] | 16 bilaterally nephrectomized infants with congenital nephrosis of the Finnish type (median age 0.54 years) on peritoneal dialysis | Single center case series | 9 were receiving intermittent 1-alpha calcidol therapy and 7 daily with target serum parathyroid hormone (PTH) level 2–3 times the upper limit of normal (ULN) |
Intermittent or daily vitamin D analog therapy prevents secondary hyperparathyroidism equally well, but intermittent therapy might be more favorable for growth Only a weak but significant correlation between alkaline phosphatase and the change in HtSDS from 3 to 6 months |
| Schmitt et al. | 2003 | [64] | 24 prepubertal children with CKD; among them 2 infants were included | Randomized multi-center study | To compare the effect of daily versus twice-weekly calcitriol on PTH and growth | No difference in PTH, calcium, and phosphate levels in the two arms. Identical growth over 1 year |
Grading system
We applied the grading system from the AAP [38], as previously described [39], and illustrated in Supplemental Fig. 1. Delphi participants were required to complete an e-questionnaire, stating their level of agreement for all 34 clinical practice points on a 5-point scale (strongly disagree, disagree, neither agree/disagree, agree, strongly agree). A consensus level of at least 70% was required, and statements that achieved below 70% required rewording. We obtained 20 responses to the validation questionnaire.
Clinical practice points
How to assess CKD-MBD in infants?
Clinical evaluation
-
1.1.1
We suggest physical examination for clinical signs of CKD-MBD in infants with the frequency of assessment based on the infant’s corrected gestational age, stage of CKD, comorbidities, and severity of MBD (level X, moderate recommendation).
-
1.1.2
We suggest regular monitoring of growth (weight, length, and head circumference), and plotted serially on centile growth charts (level C, weak recommendation).
-
1.1.3
In children with inherited disorders that affect bone health, we suggest specific follow-up tailored to their underlying kidney disease (level C, weak recommendation).
Rationale
A complete history divided into prenatal-antenatal and postnatal clinical history should be taken once at the first visit, while the history of CKD-MBD symptoms (e.g., gait, limping, and pains) should be taken at each follow-up visit. Growth, including weight, length, and head circumference, should be carefully followed, notably by plotting serial measurements on age- and sex-appropriate growth charts [10].
Comorbidities that can affect motor milestones should be kept in mind. Caregivers must be asked about the achievement of age-appropriate developmental milestones including standing and walking ages, and any difficulties in routine daily physical activity. A detailed musculo-skeletal examination focusing on range of motion in joints, the presence of any point tenderness or pain, limping, and bony deformities is recommended, as summarized in Supplemental Table 1 [9]. Infants should be evaluated for clinical signs of rickets, i.e., widening of the forearm at the wrist due to widened metaphyses, thickening of the costochondral junctions, Harrison’s groove, and long bone bowing once they start weight bearing.
Infants with inherited kidney disorders that affect bone health, and notably phosphate-wasting tubulopathies (including but not restricted to nephropathic cystinosis) and primary hyperoxaluria (PH), should be followed and managed accordingly [40–42].
Biochemical evaluation
-
1.2.1
We suggest measuring biomarkers of CKD-MBD (Ca, P, ALP, PTH, 25(OH)D, HCO3) with frequency of assessment based on the infant’s (corrected) age, stage of CKD, underlying disease, and the presence and severity of MBD (level C, moderate recommendation).
-
1.2.2
We suggest to measure ionized Ca levels where available (level C, weak recommendation).
Rationale
Serum bone biomarkers including Ca (ionized Ca, where available), P, ALP, PTH, and 25(OH)D should be monitored regularly depending on CKD stage, underlying kidney disease, and presence and severity of MBD-related clinical and biochemical abnormalities, as suggested in Table 3. The first year of life and puberty are periods of rapid growth, requiring the highest Ca intake [43]. These higher Ca requirements are reflected in higher normal values for serum total Ca, particularly during infancy, and reach adult levels by 5 years of age. Age-dependent normal values as shown in Table 4 [9, 44, 45] should be used.
Table 3.
Proposed minimal frequency of clinical, biochemical, and radiological assessment (in months) of CKD-MBD in infants by CKD stage and age
| Mild CKD | Moderate CKD | Severe CKD and dialysis | ||
|---|---|---|---|---|
| Age 0–1 years | Anthropometry and clinical evaluation | 1–3 | 0.5–2 | 0.25–1 |
| Biochemicals (Ca, P, bicarbonate, PTH, ALP) | 3–6 | 1–3 | 0.25–1 | |
| Biochemicals (25OH) | 6 | 3–6 | 3 | |
| X-raysa | Only in case of clinical signs | Only in case of clinical signs | Only in case of clinical signs | |
| Age 1–2 years | Anthropometry and clinical evaluation | 3–6 | 1–3 | 0.5–2 |
| Biochemicals (Ca, P, bicarbonate, PTH) | 3–6 | 1–3 | 0.5–1 | |
| Biochemicals (25OH) | 6–12 | 3–6 | 3 | |
| X-raysa | Only in case of clinical signs | Only in case of clinical signs | Only in case of clinical signs | |
The clinical and nutritional assessment may even be more frequent if needed, especially in the youngest infants and in those with kidney failure. aWe suggest plain X-rays of areas of rapid growth such as wrist, knee, and ankle in infants with clinical or biochemical features of rickets, gait abnormalities, limping, bone pain, and suspected atraumatic fractures
Table 4.
Age-specific reference ranges of the main parameters of phosphate/calcium metabolism in term infants, adapted from [9, 44, 45]
| iCa mmol/L |
Ca mg/dL |
Ca mmol/L |
P mg/dL |
P mmol/L |
ALP IU/L |
Albumin g/L |
Creatinine mg/dL |
Creatinine µmol/L |
PTH | 25 OH-D nmol/L |
25OH-D ng/mL |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0–14 days | 1.22–1.40 | 8.5–11.0 | 2.13–2.75 | 5.6–10.5 | 1.81–3.39 | 90–273 | 33–45 | 0.32–0.92 | 28–81 | No assessment before 4 weeks of life | 75–120 | 30–48 |
| 15–30 days | 1.22–1.40 | 8.5–11.0 | 2.13–2.75 | 4.8–8.4 | 1.55–2.71 | 134–518 | 28–47 | 0.10–0.36 | 9–32 | No assessment before 4 weeks of life | 75–120 | 30–48 |
| 30 days to 6 months | 1.22–1.40 | 8.5–11.0 | 2.13–2.75 | 4.8–8.4 | 1.55–2.71 | 134–518 | 28–47 | 0.10–0.36 | 9–32 |
Mild CKD: normal levels Moderate CKD: 1–2 ULN Advanced CKD/dialysis: 2–3 ULN |
75–120 | 30–48 |
| 6 months to 1 year | 1.20–1.40 | 8.5–11.0 | 2.13–2.75 | 4.8–8.4 | 1.55–2.71 | 134–518 | 28–47 | 0.10–0.36 | 9–32 |
Mild CKD: normal levels Moderate CKD: 1–2 ULN Advanced CKD/dialysis: 2–3 ULN |
75–120 | 30–48 |
| 1 to 2 years | 1.22–1.32 | 9.2–10.5 | 2.30–2.63 | 4.3–6.8 | 1.39–2.20 | 156–369 | 38–47 | 0.10–0.36 | 9–32 |
Mild CKD: normal levels Moderate CKD: 1–2 ULN Advanced CKD/dialysis: 2–3 ULN |
75–120 | 30–48 |
Results are presented as lower and upper limit. For calcium, the conversion factor from mg/dL to mmol/L is to divide by 4.0. The calculation formula for corrected calcium (CaC, mmol/L) using measured calcium (mmol/L) and serum albumin (g/L) is the following: CaC = Ca − 0.25 × (serum albumin − 40). If serum albumin is not available, CaC may be calculated with protidemia (g/L) with the following formula: CaC = Ca/(0.55 + P/16). For phosphate, the conversion factor from mg/dL to mmol/L is to divide by 3.1. For creatinine, the conversion factor from mg/dL to µmol/L is to multiply by 88.4. In the CALIPER database, albumin was assessed with bromocresol green and creatinine with an enzymatic assay. ULN, upper limit normal for the local assay
Mineralization defects were noted in 29% of children in CKD stage 2, and in nearly 80% in those with CKD stages 4–5, in a cohort of 52 pre-dialysis children between 2 and 21 years of age, at a mean age of 12.2 ± 5.2 years [46]. In children on peritoneal dialysis (PD), deficient bone mineralization was more common than turnover abnormalities in a cohort of 161 children between 0.7 and 20 years of age (among them 21 were under 5 years) [8]. Similarly, a high P demand should be considered in infants attributable both to rapid skeletal growth and high renal tubular and dialysate phosphate losses. Chronic hypocalcemia and/or hypophosphatemia can develop in infants receiving intensified dialysis regimens such as frequent daily or nocturnal hemodialysis (HD), leading to impaired bone mineralization and rickets [47]. In addition, patients with phosphate-wasting tubulopathies (including nephropathic cystinosis) may have low fibroblast growth factor 23 (FGF23) and PTH levels despite advanced CKD, and significant metabolic bone disease characterized by hypophosphatemic rickets in infancy, bone pain, and deformities [40, 48].
Because of the specific kinetics of PTH and vitamin D metabolism during the neonatal period, the interpretation of these two biomarkers, and especially PTH, is challenging during the first weeks of life. Indeed, after birth, when mineral transfer from the placenta is interrupted and PTH-related peptide is not secreted any more, there is a transition from fetal to neonatal regulation characterized by a fall of serum Ca during the first 24–48 h of life and a rise of P, leading to increased PTH and 1–25(OH)2 vitamin D levels [49]. The fetal parathyroid gland starts secreting PTH at 10 weeks of gestation, and maternal PTH does not cross the placental barrier [49]. In contrast, calcitriol levels in the neonate reflect maternal levels, and there are early changes because of the interruption of its secretion by the placenta [49]. Serum mineral levels normalize over several days to almost-adult values, regulated by PTH, calcitriol, calcitonin and FGF23, and also dependent on enteral sources of minerals [49]; several factors also affect gastro-intestinal absorption of minerals in neonates such as type of milk, enteral phosphorus, and vitamin D supplementation. As a consequence and as illustrated in Table 4, PTH levels should not be assessed before 4 weeks of life and should be interpreted cautiously; the timing of first PTH measurement will depend on the child’s overall health context, and should not happen before 1 month in case of advanced CKD but not later than 3 months in case of mild CKD. Preterm infants are prone to vitamin D deficiency due to incomplete transplacental transfer during the third trimester, low body stores, low vitamin D in parenteral nutrition, decreased absorption, and negligible sun exposure during hospital stay [50], in addition to the classical risk factors of vitamin D deficiency in newborns such as use of breast milk, ethnicity, and/or vitamin D deficiency in the mother. Thus, an earlier assessment of 25(OH)D levels should be performed in the first 2 weeks of life, because of the high proportion of native vitamin D deficiency at birth, both in term and especially in preterm infants [50], but also because with standard vitamin D supplementation preterm infants may display 25(OH)D under- or over-dosing at term-corrected age [51]. Some studies in preterm infants without CKD have shown the importance of an early monitoring of 25(OH)D levels so as to adapt supplementation [52]. After the first evaluation, 25(OH)D levels should not be measured more than quarterly [45], except for preterm infants receiving more than 1000 IU per day. More generally, preterm infants are prone to mineral bone disease, and several risk factors have been identified such as medications (steroids, diuretics, caffeine, antacids) and morbidities (broncho-pulmonary dysplasia, necrotizing enterocolitis, and cholestasis) [53, 54], that may also be present in CKD preterm infants.
Bicarbonate levels may be lower in infants: bicarbonate threshold is 18 mmol/L in preterm infants (being as low as 14 mmol/L in the extremely low gestational age neonate) and 21 mmol/L in term infants, reaching adult levels (i.e., 24–26 mmol/L) only after the first post-natal year [55], and more likely around 2 years of age [56]. Even though evidence is scarce in infants, there is experimental evidence showing that acidosis is deleterious for bone by inhibiting osteoblastic mineralization and stimulating both osteoclastic differentiation and resorption [57, 58]. In older children, acidosis (bicarbonate levels < 22 mmol/L) is shown to be a risk factor for CKD progression [59], and correcting acidosis prevents the progression of CKD [60]. As such, we may hypothesize that compensation of metabolic acidosis for bone and CKD progression is at least as important in vulnerable infants with rapid development as in older children. Also, metabolic alkalosis may develop in infants who have frequent vomiting; this might affect the interpretation of serum calcium levels. Hence, we recommend that ionized calcium levels are measured when possible so that hypocalcemia can be detected and managed appropriately. It remains to be determined whether blood pH may be useful for CKD-MBD evaluation and management in infants.
Radiological evaluation
-
1.3.1
Do not perform routine X-rays in infants with CKD (level D, weak recommendation).
-
1.3.2
We suggest plain X-rays in infants with clinical suspicion of rickets or other bone involvement (level D, weak recommendation).
-
1.3.3
We suggest an individualized approach to radiological monitoring in infants with genetic diseases with specific bone involvement (level C, moderate recommendation).
Rationale
As previously detailed in the guidelines of bone evaluation in pediatric CKD, X-rays should not be performed on a routine basis [9]. There may be a lower threshold for performing X-rays in infants than in older children, but evidence is very scarce. Plain X-rays can visualize common radiographical signs of CKD-MBD including osteopenia, erosions and radiolucent zones in metaphyses, and signs of rickets such as an increased thickness of the growth plates of long bones, with irregular, hazy appearance at the diaphyseal line, and rachitic rosaries [9]. Thus, in case of suspicion of inadequate control of CKD-MBD and early signs in infants, we suggest performing X-rays, preferentially of areas of rapid growth such as wrist, knee, and ankle in the absence of overt clinical symptoms. The use of “low-dose” radiographs and scans whenever possible should be favored. Other imaging techniques, including dual-energy X-ray absorptiometry (DXA), magnetic resonance imaging (MRI), or ultrasounds, are not recommended for routine monitoring, but may be used for research purposes or special circumstances such as the diagnosis of osteomyelitis. Some authors have reported an interest in quantitative ultrasounds in this age group to assess metabolic bone disease in preterm infants [61], but this was not evaluated in CKD patients.
Last, the hand/wrist method of Greulich and Pyle for bone age evaluation is suboptimal in infants because the ossification centers of the hand and wrist do not change significantly during infancy; as such, in children under the age of 3 the bone maturation process is better characterized by the X-rays of the knee [62].
What targets optimize management of CKD-MBD in children under 2 years of age?
Biochemical targets
-
2.1
We suggest maintaining serum Ca, P, ALP, and HCO3 within the age-related normal ranges (level D, weak recommendation).
-
2.2
We suggest maintaining PTH levels within the CKD-stage dependent target ranges (level D, weak recommendation).
-
2.3
2.3 We suggest maintaining 25(OH)D within the target range defined in older children (level C, weak recommendation).
-
2.4
We recommend that therapeutic decisions be based on trends rather than on a single laboratory value, considering all available CKD-MBD assessments (level X, strong recommendation).
Rationale
Several registry and single center studies reported on PTH levels in infants on dialysis. Data from the International Pediatric Dialysis Network (IPPN) registry on 890 children on peritoneal dialysis from 24 countries have rather found a negative effect on longitudinal growth of high PTH levels above 500 pg/mL [26]. Less than 20% of children < 5 years had PTH within the KDOQI limits in the IPPN registry [26], and PTH above twice the upper normal limit was found in 39% of infants < 1 year and 54% of children between 1 and 5 years [26]. Similarly, 59% of children under 2 years displayed PTH above twice the upper normal limit in a single center study including 20 infants on dialysis < 1 year [33]. Most studies showed regression of PTH values after initiation of dialysis in infants [1, 2, 5, 24, 28, 31, 32, 34]. However, these studies have not assessed the associations of temporal trends in PTH levels and combination of biomarkers with growth and/or bone disease, which are considered to better reflect underlying osteodystrophy based on evidence in older CKD children and adolescents [9]. Some studies have suggested a positive relation between PTH and growth, with likely deleterious effects of active vitamin D therapy on growth [63, 64].
In infants starting dialysis before the age of 12 months, there was no significant difference in PTH levels between hemodialysis (HD) and PD [1]. In the Italian registry which included 84 infants, PTH levels at dialysis initiation and 12 months later did not differ between infants who displayed catch-up growth as opposed to those who failed to present catch-up growth [34]. Last, hemoglobin levels have been associated with PTH levels, reflecting possible bone marrow suppression because of the fibrosis observed in SHPT [65]. However, there is still no clear consensus on the target PTH level [66–68]. PTH alone does not accurately reflect underlying renal bone disease; high bone turnover may occur at lower thresholds than currently recommended PTH targets [9]. The ideal target according to CKD stage would be a balanced approach avoiding high, but also too low, PTH levels that could be associated with adynamic bone disease and vascular calcifications. This is especially true for infants in whom long-term consequences may develop and progress from an early age [69, 70].
The only study including infants (among older children) with CKD before dialysis failed to show associations of Ca, P, and PTH with clinical symptoms of CKD-MBD and short stature at entry [27]; interestingly, infants of 0–2 years had the lowest height standard deviation score (SDS) at study entry, but the analysis for the aforementioned associations was not separated by age groups [27]. Only half of the infants < 1 year and children 1–5 years had Ca and P levels within the KDOQI recommendations in the IPPN registry [26]. The evidence of targeting serum Ca and P to normal values for age derives mainly from studies in older CKD patients as well as non-CKD infants and preterm infants [9]. It has been proposed that an individualized approach using biological age (height age) would be more appropriate in this age group [71]. In addition to CKD-MBD, metabolic bone disease of prematurity may further complicate the management of preterm infants with CKD [72].
The dietary management of CKD-MBD in infants
Consensus statements:
-
3.1
We suggest that the dietary Ca and P intake in infants with CKD should be assessed regularly (level C, weak recommendation).
-
3.2
We suggest that the total Ca intake from feed, food, and medications is within the suggested dietary intake (SDI) in infants with CKD. The Ca requirement may need to exceed twice the SDI in infants with rapid growth or those with mineral depleted bone, with careful monitoring (level C, weak recommendation).
-
3.3
We suggest that the dietary P intake from feed and food is within the SDI for age (level C, weak recommendation).
-
3.4
A phosphate restricted diet must not compromise protein or calcium intake, with addition of phosphate binders as required (level X, strong recommendation).
-
3.5
We recommend using preterm infant nutritional requirements as a guide for preterm infants with CKD, adjusting their intake according to growth and biochemistry (level D, weak recommendation).
Rationale
A dietary assessment of infants with CKD should include energy, protein, and micronutrients aiming for the SDIs for calcium and phosphate, as outlined in previous recommendations [7, 10, 73–75] from the PRNT and illustrated in Table 5 [7]. A specialist pediatric kidney dietitian or healthcare professional who has the necessary skills and training should carry out the dietary assessment [76]. The optimal frequency of dietary assessment depends on the infant’s CKD stage, growth, biochemical control, and any feeding-related problems. We suggest a dietetic contact at least every 4 weeks and taking a diet history at least every 8 weeks [10, 56].
Table 5.
Suggested dietary intakes (SDIs) per day for Ca and P in infants with CKD2-5D, adapted from [7]
| Age | SDI calcium (mg/d) | SDI phosphate (mg/d) |
|---|---|---|
| 0– < 4 months | 220 | 120 |
| 4– < 12 months | 330–540 | 275–420 |
| 12–24 months | 450–700 | 250–500 |
Recommendations on dietary management of Ca and P in children with CKD stages 2–5 and on dialysis have been published [7], as well as on nutritional management of infants [75]. An upper limit for Ca intake for healthy children of different ages has not been defined; however, 200% of the SDIs has been suggested as a safe upper limit for Ca intake from diet and phosphate binders in CKD [7, 47]. Of note, the Ca intake from the diet may not provide sufficient Ca [74], particularly as most Ca-rich foods also contain large amounts of P, and are likely to be restricted in CKD patients [77]. In some situations, such as during periods of rapid catch-up growth, when there is a late presentation with untreated CKD, or in infants on daily hemodialysis, greater Ca intake than the SDI may be required [24, 78]. Also, intestinal Ca absorption may be impaired in vitamin D-deficient infants [45]. When there is either persistent hyperphosphatemia or persistent SHPT in the presence of normal Ca levels, limiting dietary P intake to the lower limit of the SDI may be required [76]. Care needs to be taken not to compromise the intake of protein and other nutrients when restricting dietary P, with the use of P binders to control P and PTH levels if necessary. Ca supplements may be necessary to achieve an adequate intake of Ca. Infants with tubular disorders and those on intensified dialysis regimens are likely to have phosphate wasting and will need phosphate supplementation. All standard and most specialized infant formulas have a higher concentration of Ca relative to human milk (because of a lower bioavailability of Ca from formulas) [79], but a lower concentration than cow’s milk (Supplemental Table 2) [75].
Breastfeeding is the preferred method for feeding an infant with CKD [75]. If an infant is drinking infant formula, vitamin D intake from infant formula should be assessed (Supplemental Table 2), and any vitamin D supplementation adjusted accordingly [45].
Given the high Ca and P requirements of preterm infants, the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) recommends 120–140 mg/kg/day of Ca, 60–90 mg/kg/day of P, Ca-P ratio of 1.5–2.0:1, and 800–1000 IU/day of vitamin D [80]. The recommendations relate to ranges of enteral intakes for stable-growing preterm infants up to a weight of 1.8 kg. No recommendations are made for infants < 1 kg as data are lacking. ESPGHAN/ESPN/ESPR/CSPEN guidelines are available for preterm infants requiring parental nutrition (PN) [81, 82]. Chinoy et al. recommend that all infants with a birth weight less than 1500 g should be screened for metabolic bone disease of prematurity and the treatment path based on plasma PTH levels [53]. These enteral and PN recommendations may be considered for preterm infants with CKD as a guide but each infant needs to be assessed individually, adjusting their nutrition and supplementation according to growth and biochemical parameters. In infants who are unable to meet their nutritional requirements orally, supplemental or exclusive enteral tube feeding should be commenced [73].
Complementary foods should be introduced in an age-appropriate form around 6 months of age for term infants (but not before 4 months corrected age) [83]. All infants should be assessed individually for their readiness for solids. Advice on the introduction of complementary foods must include controlling the intake of higher P foods such as dairy and animal protein. In contrast, a plant-based diet that is rich in phytates will reduce phosphate absorption. Processed foods that are likely to contain inorganic highly bioavailable P additives should be avoided as much as possible [7].
Specific aspects of the medical management of MBD in infancy
Native vitamin D
-
4.1.1
We suggest that all newborns, including preterm infants, with CKD receive vitamin D supplements from birth (level C, moderate recommendation).
-
4.1.2
We suggest that serum 25(OH)D concentrations are kept within a target range of 75–120 nmol/L (level D, weak recommendation).
Calcium supplementation and calcium in the dialysate
-
4.2.1
We recommend Ca supplementation in case of hypocalcemia (level X, strong recommendation).
-
4.2.2
We suggest oral Ca supplementation in case of persistently high PTH levels, provided P levels are controlled (level D, weak recommendation).
-
4.2.3
Use intravenous Ca to correct serum Ca levels in acute hypocalcemic emergencies (level X, strong recommendation).
-
4.2.4
We suggest increasing dialysate Ca concentrations in order to keep serum Ca (ionized Ca where available) levels in the normal range in infants undergoing dialysis (level D, weak recommendation).
-
4.2.5
We recommend avoiding vitamin A supplementation in infants with CKD (level X, strong recommendation).
Phosphate binders and phosphate supplementation
-
4.3.1
Maintain P levels within the normal range for age, by adapting nutrition first but without compromising protein intake (level C, moderate recommendation).
-
4.3.2
Introduce P binders if serum P is not controlled with optimized nutritional management (level C, moderate recommendation).
-
4.3.3
We suggest using Ca-based P binders as first-line therapy (level D, weak recommendation).
-
4.3.4
We suggest considering sevelamer carbonate in infants with hypercalcemia (level D, weak recommendation).
-
4.3.5
We suggest providing P supplementation after optimization of nutritional phosphate intake in case of persistent hypophosphatemia (level D, weak recommendation).
Management of secondary hyperparathyroidism
-
4.4.1
We suggest starting active vitamin D in the lowest dose to achieve target PTH and normal calcium levels (level C, moderate recommendation).
-
4.4.2
We recommend giving native vitamin D and active vitamin D analogs directly by mouth, and avoiding nasogastric or gastrostomy tubes (level X, strong recommendation).
-
4.4.3
We recommend considering initiation or optimization of dialysis in infants with persistently uncontrolled SHPT and/or hyperphosphatemia despite optimized nutritional and medical management (level C, moderate recommendation).
-
4.4.4
Cinacalcet may be considered with extreme caution in infants on dialysis who have persistent and severe hyperparathyroidism in the presence of high or high-normal calcium levels, despite optimized conventional management, including active vitamin D (level D, weak recommendation).
-
4.4.5
Parathyroidectomy may be considered as a last resort treatment when all medical management fails to control SHPT (level D, weak recommendation).
Rationale-Native vitamin D
The recommended daily vitamin D intake for healthy infants without risk factors for vitamin D deficiency amounts to 400 IU during the first year of life, as stated in the 2013 ESPGHAN guidelines [84]. Even though a daily supply of 400 IU vitamin D may not be sufficient in children older than 12 months, ESPGHAN did not propose a daily dose after 1 year, rather encouraging countries to adopt policies to improve vitamin D status through food fortification, dietary recommendations, and judicious sun exposure, with oral supplementation of vitamin D to be considered beyond 1 year of age depending on local circumstances [84]. In accordance with the European Food Safety Authority, the upper limit of safety is set at 1000 IU/day for infants and 2000 IU/day for children aged 1 to 10 years [85]. Higher doses may be required in infants with CKD, as previously demonstrated in older children with CKD [86, 87].
A few RCTs on native vitamin D supplementation have been performed in preterm infants [88–95], showing that a daily dose between 600 and 1000 IU per day is sufficient to prevent rickets. We therefore recommend this procedure also for infants with CKD for prophylaxis of rickets. The “intensive replacement phase” may follow the 2017 European guidelines, providing infants less than 1 year with 600 IU per day and infants older than 1 year a regimen depending on their baseline 25(OH)D levels [45]. However, the evidence for these doses and weight-related vitamin D dosages is low, since the RCTs on treatment with native vitamin D in children did not include children below 2 years of age [86, 87, 96]. In children with CKD stages 2–5 (no infants) started on supplementation with native vitamin D, body surface area (BSA)-related vitamin D dosage and PTH and phosphate levels at baseline were independently associated with final serum 25(OH)D levels by multiple linear regression analysis. Likewise, the change in 25(OH)D levels was positively associated with vitamin D dosage [97]. Model-based simulations showed that current dosing recommendations for cholecalciferol can be optimized using a weight-based dosing strategy [98].
Calcium supplementation and calcium in the dialysis fluid
Infants on dialysis are much more likely to need a higher dialysate Ca concentration than older children, especially if enteral intake (from diet and medications) cannot maintain normal serum Ca levels to control PTH. One additional point that one should not forget is the risk of hypervitaminosis A with some formulas (especially in case of parenteral nutrition) and subsequent hypercalcemia; some authors even discuss monitoring vitamin A levels as part of routine nutritional assessments in pediatric CKD [99, 100].
Phosphate binders and phosphate supplementation
Physiological serum P concentrations are substantially higher in infants compared to older children [44]. Higher serum P concentrations may be acceptable in infants with CKD-MBD, even though the impact is uncertain. Two RCTs have been performed in CKD children to compare sevelamer hydrochloride with calcium carbonate [101, 102], but only one included infants under 2 years [102]. P control was similar with the two compounds; however, an increased risk of hypercalcemia was found with calcium acetate, as opposed to an increased risk of acidosis with sevelamer hydrochloride [102]. The latter side effect has not been observed with sevelamer carbonate [103]. In the youngest infants, there are practical limitations, notably the multiple feeding episodes during 24 h and the risk of blocking nasogastric or gastrostomy tubes with the compounds. It was therefore proposed to add binders directly into the formula and then feed the treated supernatant [104, 105], but this procedure may modify the composition of the formula and decrease the content of micronutrients [106]. This technique should not be used in countries where adapted renal formulas are available or where experienced kidney dietitians can give advice. Of note, breastfeeding is low in phosphate.
Active vitamin D
We refer the reader to the previously published guidelines on active vitamin D in CKD children [107]. Both daily and intermittent (thrice weekly) alfacalcidol prevented the development of SHPT in 18 infants with congenital nephrotic syndrome undergoing PD (median age 0.54 years) [37]. Importantly, both native and active vitamin D should be given directly by mouth, since they have the potential to stick to plastic tubes. Caregivers should be regularly reminded of this, especially in case of uncontrolled SHPT.
Calcimimetics
Calcimimetics are not licensed in children under 3 years of age [39], but some authors have reported their use in infants with advanced CKD or on dialysis, however with greater average doses at initiation than the current guidelines in older children (0.2 mg/kg/day to begin, maximum 2.5 mg/kg/day), as illustrated in Table 2 [35, 36]. Cinacalcet in combination with recombinant human growth hormone (rhGH) treatment was associated with a significant improvement of standardized height in children undergoing dialysis and aged less than 5 years; treatment was effective in decreasing PTH levels and well tolerated [36]. In the second study, cinacalcet was given to 10 infants (median age 18 months) on dialysis, with a significant median overall decline in PTH of 82% from baseline by 6 months; the median effective dose required to reach such a control was 2.8 mg/kg/day (IQR 2.0; 3.1) [35]. Linear growth significantly improved during cinacalcet therapy [35]. Thus, calcimimetics may be considered as an alternative to parathyroidectomy in individual cases after informed consent of the family, provided a close follow-up of ionized Ca and Ca levels and the subsequent risk of hypocalcemia. A recent European survey was performed to evaluate the use of cinacalcet in dialysis children below 3 years of age. In this study, 22 patients received cinacalcet at a median age of 28 (15–28) months and a median starting dose of 0.4 (0.2–0.8) mg/kg/day. Cinacalcet was described as giving an efficient control of PTH levels. Despite the fact that overall median calcium levels remained stable, three infants nevertheless developed hypocalcemic episodes < 2.0 mmol/L, of which one child suffered from a hypocalcemia-related convulsion, due to non-adherence to calcium substitution [108]. Interestingly, precocious puberty was reported in two children, as already described in older children [109].
Parathyroidectomy
One paper reported the outcomes of parathyroidectomy in 18 CKD children, among them two patients who were below 2 years of age; results showed that it is an effective procedure with long-term control of serum PTH, Ca, and P [110, 111]. Postoperative complications comprised one episode of hypocalcemic seizure due to non-adherence with oral Ca supplements, one hemopericardium in a patient with thoracic adenoma, and transient bilateral vocal cord palsy, thus highlighting the non-negligible risks of such a procedure. The two infants experienced no complications. Thus, parathyroidectomy may be considered in case of SHPT, but only as a last resort, when all other medical management including calcimimetics have failed. In infants, the risk of severe hypocalcemia and growth retardation following parathyroidectomy are very high and sub-total parathyroidectomy may be considered when all medical management fails.
Conclusions
Due to rapid bone growth and difficulties with nutrition, an adequate control of CKD-MBD in infants is particularly challenging. Here, we present 34 CPPs on diagnosis and management of CKD-MBD in infants under 2 years of age, as summarized in Table 6. We also include suggestions for daily practice. The practice points developed in previous guidelines of the working groups that are also valid for this age group were not considered separately [7, 9, 10, 39, 45, 73, 107, 112]. Given that there are very few high-quality studies to guide evidence-based practice, these statements must be carefully considered by the treating physician and adapted to individual patient needs as appropriate. We also propose future research topics in the field (Table 7).
Table 6.
Summary of the 34 consensus statements with their respective grading
| PICO question | Consensus statement |
|---|---|
| 1 How to assess CKD-MBD in infants under 2 years of age? |
1.1 Clinical evaluation 1.1.1 We suggest physical examination for clinical signs of CKD-MBD in infants with the frequency of assessment based on the infant’s corrected gestational age, stage of CKD, comorbidities, and severity of MBD (level X, moderate recommendation) 1.1.2 We suggest regular monitoring of growth (weight, length, and head circumference), and plotted serially on centile growth charts (level C, weak recommendation) 1.1.3 In children with inherited disorders that affect bone health, we suggest specific follow-up tailored to their underlying kidney disease (level C, weak recommendation) 1.2 Biochemical evaluation 1.2.1 We suggest measuring biomarkers of CKD-MBD (Ca, P, ALP, PTH, 25(OH)D, HCO3) with frequency of assessment based on the infant’s (corrected) age, stage of CKD, underlying disease, and the presence and severity of MBD (level C, moderate recommendation) 1.2.2 We suggest to measure ionized Ca levels where available (level C, weak recommendation) 1.3 Radiological evaluation 1.3.1 Do not perform routine X-rays in infants with CKD (level D, weak recommendation) 1.3.2 We suggest plain X-rays in infants with clinical suspicion of rickets or other bone involvement (level D, weak recommendation) 1.3.3 We suggest an individualized approach to radiological monitoring in infants with genetic diseases with specific bone involvement (level C, moderate recommendation) |
| 2 What are the biochemical targets so as to optimize management of CKD-MBD? |
2.1 We suggest maintaining serum Ca, P, ALP, and HCO3 within the age-related normal ranges (level D, weak recommendation) 2.2 We suggest maintaining PTH levels within the CKD-stage dependent target ranges (level D, weak recommendation) 2.3 We suggest maintaining 25(OH)D within the target range defined in older children (level C, weak recommendation) 2.4 We recommend that therapeutic decisions are based on trends rather than on a single laboratory value, taking into account all available CKD-MBD assessments (level X, strong recommendation) |
| 3 What are the targets of dietary control of CKD-MBD in this age group? |
3.1 We suggest that the dietary Ca and P intake in infants with CKD should be assessed regularly (level C, weak recommendation) 3.2 We suggest that the total Ca intake from feed, food, and medications is within the suggested dietary intake (SDI) in infants with CKD. The Ca requirement may need to exceed twice the SDI in infants with rapid growth or those with mineral depleted bone, with careful monitoring (level C, weak recommendation) 3.3 We suggest that the dietary P intake from feed and food is within the SDI for age (level C, weak recommendation) 3.4 A phosphate restricted diet must not compromise protein or calcium intake, with addition of phosphate binders as required (level X, strong recommendation) 3.5 We recommend using preterm infant nutritional requirements as a guide for preterm infants with CKD, adjusting their intake according to growth and biochemistry (level D, weak recommendation) |
| 4 What are the specificities of therapeutic management in this age group? |
4.1 Native vitamin D 4.1.1 We suggest that all newborns, including preterm infants, with CKD receive vitamin D supplements from birth (level C, moderate recommendation) 4.1.2 We suggest that serum 25(OH)D concentrations are kept within a target range of 75–120 nmol/L (level D, weak recommendation) 4.2 Calcium supplementation and calcium in the dialysate 4.2.1 We recommend Ca supplementation in case of hypocalcemia (level X, strong recommendation) 4.2.2 We suggest oral Ca supplementation in case of persistently high PTH levels, provided P levels are controlled (level D, weak recommendation) 4.2.3 Use intravenous Ca to correct serum Ca levels in acute hypocalcemic emergencies (level X, strong recommendation) 4.2.4 We suggest increasing dialysate Ca concentrations in order to keep serum Ca (ionized Ca where available) levels in the normal range in infants undergoing dialysis (level D, weak recommendation) 4.2.5 We recommend avoiding vitamin A supplementation in infants with CKD (level X, strong recommendation) 4.3 Phosphate binders and phosphate supplementation 4.3.1 Maintain P levels within the normal range for age, by adapting nutrition first but without compromising protein intake (level C, moderate recommendation) 4.3.2 Introduce P binders if serum P is not controlled with optimized nutritional management (level C, moderate recommendation) 4.3.3 We suggest using Ca-based P binders as first-line therapy (level D, weak recommendation) 4.3.4 We suggest considering sevelamer carbonate in infants with hypercalcemia (level D, weak recommendation) 4.3.5 We suggest providing P supplementation after optimization of nutritional phosphate intake in case of persistent hypophosphatemia (level D, weak recommendation) 4.4 Management of secondary hyperparathyroidism 4.4.1 We suggest starting active vitamin D in the lowest dose to achieve target PTH and normal calcium levels (level C, moderate recommendation) 4.4.2 We recommend giving native vitamin D and active vitamin D analogs directly by mouth, and avoiding nasogastric or gastrostomy tubes (level X, strong) 4.4.3 We recommend considering initiation or optimization of dialysis in infants with persistently uncontrolled SHPT and/or hyperphosphatemia despite an optimized nutritional and medical management (level C, moderate recommendation) 4.4.4 Cinacalcet may be considered with extreme caution in infants on dialysis who have persistent and severe hyperparathyroidism in the presence of high or high-normal calcium levels, despite optimized conventional management, including active vitamin D (level D, weak recommendation) 4.4.5 Parathyroidectomy may be considered as a last resort treatment when all medical management fails to control SHPT (level D, weak recommendation) |
Table 7.
Research questions
| PICO question | Consensus statement |
|---|---|
| Clinical targets | To develop outcome and quality of life measures for neonates and young infants on kidney replacement therapy, similarly to what is done with the SONG (Standardized Outcomes in Nephrology) initiative in older children and adults |
| Biochemical targets | To determine the targets for the main biomarkers in this age group in case of CKD, and notably PTH, 25(OH)D, and ALP |
| Nutritional specificities | Balance studies to determine the true Ca requirements in infants for optimal bone quality and without a risk of vascular calcifications. To determine if urinary calcium excretion in healthy infants and those with CKD can be used to evaluate optimal calcium intakes |
| Therapeutic specificities |
Cinacalcet data in infants in a real-life setting CKD-MBD in preterm infants |
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This work was supported by members (JB, DH, CPS, JVD, BR) of the European Reference Network for Rare Kidney Diseases (ERK-Net).
The authors also acknowledge the valuable contributions of two experts in neonatology and neonatal intensive care, Pr Silvia Iacobelli (MD, PhD, CHU La Réunion, Site Sud, Saint Pierre, France) and Pr Helmut Küster (MD, Clinic for Paediatric Cardiology, Intensive Care and Neonatology, University Medical Center Göttingen, Germany) in the reviewing of the manuscript.
The authors also acknowledge the valuable contributions of the expert panel who participated in the Delphi technique.
The expert panel consisted of:
Members of the ESPN CKD-MBD Working Group
Belgium: France: Lyon; C. Pietrement, Reims. Germany: Hannover; M. Gessner, Cologne; G. Klaus, Marburg; J. Oh, Hamburg; Heidelberg. Greece: S. Stabouli, Thessaloniki. Hungary: G. Reusz, Budapest. Italy: I. Guzzo, Roma; Padova; E. Verrina, Genoa. Netherlands: J. Groothoff, Amsterdam. Norway: C. Tondel, Bergen. Poland: D. Drozdz, Krakow. Spain: MA. Gamero, Córdoba. Russia: E. Petrosyan, Moscow. Turkey: Ankara; I. Dursun, Kayseri; A. Karabay Bayazit, UK: C. Booth, and M. Sinha, London.
Members of the ESPN Dialysis Working Group
Austria: C. Aufricht, Vienna. Belgium: J. Vande Walle, Ghent. Czech Republic: K. Vondrak, Prague. Finland: T. Holtta, Helsinki. France: Lyon; M. Fila, Montpellier; C Pietrement, Reims; A. Zalozsyc, Strasbourg. Germany: G. Klaus, Marburg; D. Muller and J. Thumfart, Berlin; Heidelberg. Greece: V. Askiti, C. Stefanidis, and P. Kyriakou, Athens; S. Stabouli and N. Printza, Thessaloniki. Italy: M. Allinovi, Florence; A. Edefonti and F. Paglialonga, Milan; I Guzzo, Roma; L. Peruzzi, Torino; E. Verrina, Genova; Padova; M. Allinovi, Florence. Lithuania: A. Jankauskiene, Vilnius. Poland: M Tkaczyk, Lodz; A. Zurowska, Gdańsk. Portugal: M. Do Sameiro Faria, Porto. Spain: G. Ariceta, Barcelona. Sweden: L. Sartz, Lasarettsgatan. Turkey: H. Alpay and S. Caliskan, Istanbul; A. Duzova, and M. Ekim, Ankara; I. Dursun, Melikgazi; R. Dusunsel, Kayseri; A. Karabay-Bayazit, Adana. UK: D. Hothi, and M. Sinha, London.
Members of the Pediatric Renal Nutrition Taskforce
Belgium: J. Van de Walle, Ghent. Canada: N. Polderman, Vancouver. Finland: J. Tuokkola, Helsinki. Germany: Hannover. Greece: S. Stabouli, Thessaloniki. Italy: F. Paglialonga, Milan. Netherlands: J.W.M. Renken, Utrecht. UK: C. Anderson, Southampton; L. Qizalbash, Newcastle; V. Shaw and R. Shroff, London. USA: L. Greenbaum, Atlanta; C. Nelms, Kearney; B. Warady, Kansas City.
Funding
This project was financially supported by the European Society for Paediatric Nephrology. The funder had no influence on the content of the recommendation.
Declarations
Conflict of interest
JB received consulting fees from Amgen and Bayer. JB is an investigator of the cinacalcet and etelcalcetide Amgen-sponsored trials. EV received consulting fees from Bellco-Medtronics and Alnylam. DH received speaker and/or consulting fees from Amgen, Bayer, Biologix, Chiesi, and Kyowa Kirin, and research grants from Amgen, Chiesi, and Kyowa Kirin. CPS received consultancy honoraria from Baxter, Iperboreal Pharma, STADAPHARM, and lecturing honoraria from Fresenius. CPS is an investigator of the etelcalcetide Amgen-sponsored trial. SAB, MLN, BR, SS, SC, AP, AS, JVW, and RS have nothing to declare.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Justine Bacchetta, Email: justine.bacchetta@chu-lyon.fr.
Rukshana Shroff, Email: rukshana.shroff@gosh.nhs.uk.
References
- 1.Vidal E, van Stralen KJ, Chesnaye NC, Bonthuis M, et al. Infants requiring maintenance dialysis: outcomes of hemodialysis and peritoneal dialysis. Am J Kidney Dis. 2017;69:617–625. doi: 10.1053/j.ajkd.2016.09.024. [DOI] [PubMed] [Google Scholar]
- 2.van Stralen KJ, Borzych-Dużalka D, Hataya H, Kennedy SE, et al. Survival and clinical outcomes of children starting renal replacement therapy in the neonatal period. Kidney Int. 2014;86:168–174. doi: 10.1038/ki.2013.561. [DOI] [PubMed] [Google Scholar]
- 3.Carey WA, Martz KL, Warady BA. Outcome of patients initiating chronic peritoneal dialysis during the first year of life. Pediatrics. 2015;136:e615–e622. doi: 10.1542/peds.2015-0980. [DOI] [PubMed] [Google Scholar]
- 4.Sanderson KR, Yu Y, Dai H, Willig LK, et al. Outcomes of infants receiving chronic peritoneal dialysis: an analysis of the USRDS registry. Pediatr Nephrol. 2019;34:155–162. doi: 10.1007/s00467-018-4056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dachy A, Bacchetta J, Sellier-Leclerc A-L, Demède D, et al. Long-term outcomes of peritoneal dialysis started in infants below 6 months of age: an experience from two tertiary centres. Nephrol Ther. 2020;16:424–430. doi: 10.1016/j.nephro.2020.08.002. [DOI] [PubMed] [Google Scholar]
- 6.Salusky IB, Kuizon BG, Jüppner H. Special aspects of renal osteodystrophy in children. Semin Nephrol. 2004;24:69–77. doi: 10.1053/j.semnephrol.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 7.McAlister L, Pugh P, Greenbaum L, Haffner D, et al. The dietary management of calcium and phosphate in children with CKD stages 2–5 and on dialysis-clinical practice recommendation from the Pediatric Renal Nutrition Taskforce. Pediatr Nephrol. 2020;35:501–518. doi: 10.1007/s00467-019-04370-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bakkaloglu SA, Wesseling-Perry K, Pereira RC, Gales B, et al. Value of the new bone classification system in pediatric renal osteodystrophy. Clin J Am Soc Nephrol. 2010;5:1860–1866. doi: 10.2215/CJN.01330210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bakkaloglu SA, Bacchetta J, Lalayiannis AD, Leifheit-Nestler M, et al. Bone evaluation in paediatric chronic kidney disease: clinical practice points from the European Society for Paediatric Nephrology CKD-MBD and Dialysis working groups and CKD-MBD working group of the ERA-EDTA. Nephrol Dial Transplant. 2021;36:413–425. doi: 10.1093/ndt/gfaa210. [DOI] [PubMed] [Google Scholar]
- 10.Nelms CL, Shaw V, Greenbaum LA, Anderson C, et al. Assessment of nutritional status in children with kidney diseases-clinical practice recommendations from the Pediatric Renal Nutrition Taskforce. Pediatr Nephrol. 2021;36:995–1010. doi: 10.1007/s00467-020-04852-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jetton JG, Boohaker LJ, Sethi SK, Wazir S, et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Health. 2017;1:184–194. doi: 10.1016/S2352-4642(17)30069-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Selewski DT, Charlton JR, Jetton JG, Guillet R, et al. Neonatal acute kidney injury. Pediatrics. 2015;136:e463–e473. doi: 10.1542/peds.2014-3819. [DOI] [PubMed] [Google Scholar]
- 13.Ranchin B, Plaisant F, Demède D, de Guillebon JM, et al. Review: neonatal dialysis is technically feasible but ethical and global issues need to be addressed. Acta Paediatr. 2021;110:781–788. doi: 10.1111/apa.15539. [DOI] [PubMed] [Google Scholar]
- 14.Greenbaum LA, Muñoz A, Schneider MF, Kaskel F, et al. The association between abnormal birth history and growth in children with CKD. Clin J Am Soc Nephrol. 2011;6:14–21. doi: 10.2215/CJN.08481109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Franke D, Völker S, Haase S, Pavicic L, et al. Prematurity, small for gestational age and perinatal parameters in children with congenital, hereditary and acquired chronic kidney disease. Nephrol Dial Transplant. 2010;25:3918–3924. doi: 10.1093/ndt/gfq300. [DOI] [PubMed] [Google Scholar]
- 16.Sutherland MR, Gubhaju L, Moore L, Kent A, et al. Accelerated maturation and abnormal morphology in the preterm neonatal kidney. J Am Soc Nephrol. 2011;22:1365–1374. doi: 10.1681/ASN.2010121266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodríguez MM, Gómez AH, Abitbol CL, Chandar JJ, et al. Histomorphometric analysis of postnatal glomerulogenesis in extremely preterm infants. Pediatr Dev Pathol. 2004;7:17–25. doi: 10.1007/s10024-003-3029-2. [DOI] [PubMed] [Google Scholar]
- 18.Hoogenboom LA, Wolfs TGAM, Hütten MC, Peutz-Kootstra CJ, et al. Prematurity, perinatal inflammatory stress, and the predisposition to develop chronic kidney disease beyond oligonephropathy. Pediatr Nephrol. 2021;36:1673–1681. doi: 10.1007/s00467-020-04712-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stevens PE, Levin A, Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158:825–830. doi: 10.7326/0003-4819-158-11-201306040-00007. [DOI] [PubMed] [Google Scholar]
- 20.Boer DP, de Rijke YB, Hop WC, Cransberg K, et al. Reference values for serum creatinine in children younger than 1 year of age. Pediatr Nephrol. 2010;25:2107–2113. doi: 10.1007/s00467-010-1533-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwartz GJ, Work DF. Measurement and estimation of GFR in children and adolescents. Clin J Am Soc Nephrol. 2009;4:1832–1843. doi: 10.2215/CJN.01640309. [DOI] [PubMed] [Google Scholar]
- 22.Ardeshirpour L, Cole DEC, Carpenter TO. Evaluation of bone and mineral disorders. Pediatr Endocrinol Rev. 2007;5(Suppl 1):584–598. [PubMed] [Google Scholar]
- 23.Shaw JLV, Cohen A, Konforte D, Binesh-Marvasti T, et al. Validity of establishing pediatric reference intervals based on hospital patient data: a comparison of the modified Hoffmann approach to CALIPER reference intervals obtained in healthy children. Clin Biochem. 2014;47:166–172. doi: 10.1016/j.clinbiochem.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 24.Rees L, Azocar M, Borzych D, Watson AR, et al. Growth in very young children undergoing chronic peritoneal dialysis. J Am Soc Nephrol. 2011;22:2303–2312. doi: 10.1681/ASN.2010020192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schaefer F, Benner L, Borzych-Dużałka D, Zaritsky J, et al. Global variation of nutritional status in children undergoing chronic peritoneal dialysis: a longitudinal study of the International Pediatric Peritoneal Dialysis Network. Sci Rep. 2019;9:4886. doi: 10.1038/s41598-018-36975-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Borzych D, Rees L, Ha IS, Chua A, et al. The bone and mineral disorder of children undergoing chronic peritoneal dialysis. Kidney Int. 2010;78:1295–1304. doi: 10.1038/ki.2010.316. [DOI] [PubMed] [Google Scholar]
- 27.Seikaly MG, Salhab N, Gipson D, Yiu V, et al. Stature in children with chronic kidney disease: analysis of NAPRTCS database. Pediatr Nephrol. 2006;21:793–799. doi: 10.1007/s00467-006-0040-7. [DOI] [PubMed] [Google Scholar]
- 28.Cansick J, Waller S, Ridout D, Rees L. Growth and PTH in prepubertal children on long-term dialysis. Pediatr Nephrol. 2007;22:1349–1354. doi: 10.1007/s00467-006-0348-3. [DOI] [PubMed] [Google Scholar]
- 29.Mekahli D, Shaw V, Ledermann SE, Rees L. Long-term outcome of infants with severe chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:10–17. doi: 10.2215/CJN.05600809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shroff R, Rees L, Trompeter R, Hutchinson C, et al. Long-term outcome of chronic dialysis in children. Pediatr Nephrol. 2006;21:257–264. doi: 10.1007/s00467-005-2067-6. [DOI] [PubMed] [Google Scholar]
- 31.Shroff R, Wright E, Ledermann S, Hutchinson C, et al. Chronic hemodialysis in infants and children under 2 years of age. Pediatr Nephrol. 2003;18:378–383. doi: 10.1007/s00467-003-1070-z. [DOI] [PubMed] [Google Scholar]
- 32.Paglialonga F, Consolo S, Pecoraro C, Vidal E, et al. Chronic haemodialysis in small children: a retrospective study of the Italian Pediatric Dialysis Registry. Pediatr Nephrol. 2016;31:833–841. doi: 10.1007/s00467-015-3272-6. [DOI] [PubMed] [Google Scholar]
- 33.Ledermann SE, Scanes ME, Fernando ON, Duffy PG, et al. Long-term outcome of peritoneal dialysis in infants. J Pediatr. 2000;136:24–29. doi: 10.1016/s0022-3476(00)90044-1. [DOI] [PubMed] [Google Scholar]
- 34.Vidal E, Edefonti A, Murer L, Gianoglio B, et al. Peritoneal dialysis in infants: the experience of the Italian Registry of Paediatric Chronic Dialysis. Nephrol Dial Transplant. 2012;27:388–395. doi: 10.1093/ndt/gfr322. [DOI] [PubMed] [Google Scholar]
- 35.Arenas Morales AJ, DeFreitas MJ, Katsoufis CP, Seeherunvong W, et al. Cinacalcet as rescue therapy for refractory hyperparathyroidism in young children with advanced chronic kidney disease. Pediatr Nephrol. 2019;34:129–135. doi: 10.1007/s00467-018-4055-7. [DOI] [PubMed] [Google Scholar]
- 36.Joseph C, Shah S, Geer J, Juarez-Calderon M, et al. Cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients below age 5 years. Clin Nephrol. 2019;92:279–286. doi: 10.5414/CN109871. [DOI] [PubMed] [Google Scholar]
- 37.Saarinen TT, Arikoski P, Holmberg C, Rönnholm K. Intermittent or daily administration of 1-alpha calcidol for nephrectomised infants on peritoneal dialysis? Pediatr Nephrol. 2007;22:1931–1938. doi: 10.1007/s00467-007-0592-1. [DOI] [PubMed] [Google Scholar]
- 38.American Academy of Pediatrics Steering Committee on Quality Improvement and Management Classifying recommendations for clinical practice guidelines. Pediatrics. 2004;114:874–877. doi: 10.1542/peds.2004-1260. [DOI] [PubMed] [Google Scholar]
- 39.Bacchetta J, Schmitt CP, Ariceta G, et al. Cinacalcet use in paediatric dialysis: a position statement from the European society for paediatric nephrology and the chronic kidney disease-mineral and bone disorders working group of the ERA-EDTA. Nephrol Dial Transplant. 2020;35:47–64. doi: 10.1093/ndt/gfz159. [DOI] [PubMed] [Google Scholar]
- 40.Hohenfellner K, Rauch F, Ariceta G, Bakkaloglu S, et al. Management of bone disease in cystinosis: statement from an international conference. J Inherit Metab Dis. 2019;42:1019–1029. doi: 10.1002/jimd.12134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bacchetta J, Boivin G, Cochat P. Bone impairment in primary hyperoxaluria: a review. Pediatr Nephrol. 2016;31:1–6. doi: 10.1007/s00467-015-3048-z. [DOI] [PubMed] [Google Scholar]
- 42.Bacchetta J, Fargue S, Boutroy S, Basmaison O, et al. Bone metabolism in oxalosis: a single-center study using new imaging techniques and biomarkers. Pediatr Nephrol. 2010;25:1081–1089. doi: 10.1007/s00467-010-1453-x. [DOI] [PubMed] [Google Scholar]
- 43.Matkovic V, Heaney RP. Calcium balance during human growth: evidence for threshold behavior. Am J Clin Nutr. 1992;55:992–996. doi: 10.1093/ajcn/55.5.992. [DOI] [PubMed] [Google Scholar]
- 44.Colantonio DA, Kyriakopoulou L, Chan MK, Daly CH, et al. Closing the gaps in pediatric laboratory reference intervals: a CALIPER database of 40 biochemical markers in a healthy and multiethnic population of children. Clin Chem. 2012;58:854–868. doi: 10.1373/clinchem.2011.177741. [DOI] [PubMed] [Google Scholar]
- 45.Shroff R, Wan M, Nagler EV, Bakkaloglu S, et al. Clinical practice recommendations for native vitamin D therapy in children with chronic kidney disease stages 2–5 and on dialysis. Nephrol Dial Transplant. 2017;32:1098–1113. doi: 10.1093/ndt/gfx065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wesseling-Perry K, Pereira RC, Tseng C-H, Elashoff R, et al. Early skeletal and biochemical alterations in pediatric chronic kidney disease. Clin J Am Soc Nephrol. 2012;7:146–152. doi: 10.2215/CJN.05940611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ketteler M, Block GA, Evenepoel P, Fukagawa M, et al. Executive summary of the 2017 KDIGO Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Guideline Update: what’s changed and why it matters. Kidney Int. 2017;92:26–36. doi: 10.1016/j.kint.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 48.Ewert A, Leifheit-Nestler M, Hohenfellner K, Büscher A, et al. Bone and mineral metabolism in children with nephropathic cystinosis compared with other CKD entities. J Clin Endocrinol Metab. 2020;105:dgaa267. doi: 10.1210/clinem/dgaa267. [DOI] [PubMed] [Google Scholar]
- 49.Sethi A, Priyadarshi M, Agarwal R. Mineral and bone physiology in the foetus, preterm and full-term neonates. Semin Fetal Neonatal Med. 2020;25:101076. doi: 10.1016/j.siny.2019.101076. [DOI] [PubMed] [Google Scholar]
- 50.Burris HH, Van Marter LJ, McElrath TF, Tabatabai P, et al. Vitamin D status among preterm and full-term infants at birth. Pediatr Res. 2014;75:75–80. doi: 10.1038/pr.2013.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Laborie S, Denis A, Raverot V, Claris O, et al. A third of premature neonates displayed inadequate 25-hydroxyvitamin D levels before being discharged from a French neonatal intensive care unit. Acta Paediatr. 2021;111:104–106. doi: 10.1111/apa.16126. [DOI] [PubMed] [Google Scholar]
- 52.Mathilde M, Butin M, Pascal R, Plaisant F, et al. Local protocol helped to deliver vitamin D levels more accurately in preterm infants. Acta Paediatr. 2021;111:76–85. doi: 10.1111/apa.16088. [DOI] [PubMed] [Google Scholar]
- 53.Chinoy A, Mughal MZ, Padidela R. Metabolic bone disease of prematurity: causes, recognition, prevention, treatment and long-term consequences. Arch Dis Child Fetal Neonatal Ed. 2019;104:F560–F566. doi: 10.1136/archdischild-2018-316330. [DOI] [PubMed] [Google Scholar]
- 54.Ali E, Rockman-Greenberg C, Moffatt M, Narvey M, et al. Caffeine is a risk factor for osteopenia of prematurity in preterm infants: a cohort study. BMC Pediatr. 2018;18:9. doi: 10.1186/s12887-017-0978-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Seri I. Acid-base homeostasis in the fetus and newborn. In: Oh W, editor. Nephrology and fluid/electrolyte physiology; neonatology questions and controversies. 3. Amsterdam: Elsevier; 2008. pp. 85–95. [Google Scholar]
- 56.KDOQI Work Group KDOQI clinical practice guideline for nutrition in children with CKD: 2008 update. Executive summary Am J Kidney Dis. 2009;53:S11–S104. doi: 10.1053/j.ajkd.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 57.Kraut JA, Mishler DR, Singer FR, Goodman WG. The effects of metabolic acidosis on bone formation and bone resorption in the rat. Kidney Int. 1986;30:694–700. doi: 10.1038/ki.1986.242. [DOI] [PubMed] [Google Scholar]
- 58.Kato K, Morita I. Promotion of osteoclast differentiation and activation in spite of impeded osteoblast-lineage differentiation under acidosis: effects of acidosis on bone metabolism. Biosci Trends. 2013;7:33–41. [PubMed] [Google Scholar]
- 59.Harambat J, Kunzmann K, Azukaitis K, Bayazit AK, et al. Metabolic acidosis is common and associates with disease progression in children with chronic kidney disease. Kidney Int. 2017;92:1507–1514. doi: 10.1016/j.kint.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 60.Brown DD, Roem J, Ng DK, Reidy KJ, et al. Low serum bicarbonate and CKD progression in children. Clin J Am Soc Nephrol. 2020;15:755–765. doi: 10.2215/CJN.07060619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.de Lange A, Maaskant JM, van Weissenbruch MM. Is quantitative ultrasound a measure for metabolic bone disease in preterm-born infants? A prospective subcohort study. Eur J Pediatr. 2021;180:3009–3017. doi: 10.1007/s00431-021-04081-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cavallo F, Mohn A, Chiarelli F, Giannini C. Evaluation of bone age in children: a mini-review. Front Pediatr. 2021;9:580314. doi: 10.3389/fped.2021.580314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kuizon BD, Goodman WG, Jüppner H, Boechat I, et al. Diminished linear growth during intermittent calcitriol therapy in children undergoing CCPD. Kidney Int. 1998;53:205–211. doi: 10.1046/j.1523-1755.1998.00724.x. [DOI] [PubMed] [Google Scholar]
- 64.Schmitt CP, Ardissino G, Testa S, Claris-Appiani A, et al. Growth in children with chronic renal failure on intermittent versus daily calcitriol. Pediatr Nephrol. 2003;18:440–444. doi: 10.1007/s00467-003-1091-7. [DOI] [PubMed] [Google Scholar]
- 65.van Stralen KJ, Krischock L, Schaefer F, Verrina E, et al. Prevalence and predictors of the sub-target Hb level in children on dialysis. Nephrol Dial Transplant. 2012;27:3950–3957. doi: 10.1093/ndt/gfs178. [DOI] [PubMed] [Google Scholar]
- 66.Haffner D, Schaefer F. Searching the optimal PTH target range in children undergoing peritoneal dialysis: new insights from international cohort studies. Pediatr Nephrol. 2013;28:537–545. doi: 10.1007/s00467-012-2270-1. [DOI] [PubMed] [Google Scholar]
- 67.Bacchetta J. Treatment of hyperphosphatemia: the dangers of high PTH levels. Pediatr Nephrol. 2020;35:493–500. doi: 10.1007/s00467-019-04400-w. [DOI] [PubMed] [Google Scholar]
- 68.Haffner D, Leifheit-Nestler M. Treatment of hyperphosphatemia: the dangers of aiming for normal PTH levels. Pediatr Nephrol. 2020;35:485–491. doi: 10.1007/s00467-019-04399-0. [DOI] [PubMed] [Google Scholar]
- 69.Sanchis P, Ho CY, Liu Y, Beltran LE, et al. Arterial “inflammaging” drives vascular calcification in children on dialysis. Kidney Int. 2019;95:958–972. doi: 10.1016/j.kint.2018.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rinat C, Becker-Cohen R, Nir A, Feinstein S, et al. A comprehensive study of cardiovascular risk factors, cardiac function and vascular disease in children with chronic renal failure. Nephrol Dial Transplant. 2010;25:785–793. doi: 10.1093/ndt/gfp570. [DOI] [PubMed] [Google Scholar]
- 71.Schmitt CP, Mehls O. Mineral and bone disorders in children with chronic kidney disease. Nat Rev Nephrol. 2011;7:624–634. doi: 10.1038/nrneph.2011.139. [DOI] [PubMed] [Google Scholar]
- 72.Rayannavar A, Calabria AC. Screening for metabolic bone disease of prematurity. Semin Fetal Neonatal Med. 2020;25:101086. doi: 10.1016/j.siny.2020.101086. [DOI] [PubMed] [Google Scholar]
- 73.Rees L, Shaw V, Qizalbash L, Anderson C, et al. Delivery of a nutritional prescription by enteral tube feeding in children with chronic kidney disease stages 2–5 and on dialysis-clinical practice recommendations from the Pediatric Renal Nutrition Taskforce. Pediatr Nephrol. 2021;36:187–204. doi: 10.1007/s00467-020-04623-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schmitz L, Hoermann P, Trutnau B, Jankauskiene A, et al. Enteral Ca-intake may be low and affects serum-PTH-levels in pre-school children with chronic kidney disease. Front Pediatr. 2021;9:666101. doi: 10.3389/fped.2021.666101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shaw V, Anderson C, Desloovere A, Greenbaum LA, et al. Nutritional management of the infant with chronic kidney disease stages 2–5 and on dialysis. Pediatr Nephrol. 2022 doi: 10.1007/s00467-022-05529-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dasgupta I, Shroff R, Bennett-Jones D, McVeigh G, et al. Management of hyperphosphataemia in chronic kidney disease: summary of National Institute for Health and Clinical Excellence (NICE) guideline. Nephron Clin Pract. 2013;124:1–9. doi: 10.1159/000354711. [DOI] [PubMed] [Google Scholar]
- 77.McAlister L, Silva S, Shaw V, Shroff R. Dietary calcium intake does not meet the nutritional requirements of children with chronic kidney disease and on dialysis. Pediatr Nephrol. 2020;35:1915–1923. doi: 10.1007/s00467-020-04571-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rees L. Paediatrics: infant dialysis—what makes it special? Nat Rev Nephrol. 2013;9:15–17. doi: 10.1038/nrneph.2012.263. [DOI] [PubMed] [Google Scholar]
- 79.Abrams SA. Calcium absorption in infants and small children: methods of determination and recent findings. Nutrients. 2010;2:474–480. doi: 10.3390/nu2040474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Agostoni C, Buonocore G, Carnielli VP, De Curtis M, et al. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010;50:85–91. doi: 10.1097/MPG.0b013e3181adaee0. [DOI] [PubMed] [Google Scholar]
- 81.Bronsky J, Campoy C, Braegger C. ESPGHAN/ESPEN/ESPR/CSPEN working group on pediatric parenteral nutrition ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: vitamins. Clin Nutr. 2018;37:2366–2378. doi: 10.1016/j.clnu.2018.06.951. [DOI] [PubMed] [Google Scholar]
- 82.Mihatsch W, Fewtrell M, Goulet O, Molgaard C, et al. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: calcium, phosphorus and magnesium. Clin Nutr. 2018;37:2360–2365. doi: 10.1016/j.clnu.2018.06.950. [DOI] [PubMed] [Google Scholar]
- 83.Gupta S, Agarwal R, Aggarwal KC, Chellani H, et al. Complementary feeding at 4 versus 6 months of age for preterm infants born at less than 34 weeks of gestation: a randomised, open-label, multicentre trial. Lancet Glob Health. 2017;5:e501–e511. doi: 10.1016/S2214-109X(17)30074-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Braegger C, Campoy C, Colomb V, Decsi T, et al. Vitamin D in the healthy European paediatric population. J Pediatr Gastroenterol Nutr. 2013;56:692–701. doi: 10.1097/MPG.0b013e31828f3c05. [DOI] [PubMed] [Google Scholar]
- 85.European Food Safety Authority Scientific opinion on nutrient requirements and dietary intakes of infants and young children in the European Union. EFSA J. 2013;11:3408. [Google Scholar]
- 86.Iyengar A, Kamath N, Reddy HV, Sharma J, et al. Determining the optimal cholecalciferol dosing regimen in children with CKD: a randomized controlled trial. Nephrol Dial Transplant. 2020 doi: 10.1093/ndt/gfaa369. [DOI] [PubMed] [Google Scholar]
- 87.Nadeem S, Tangpricha V, Ziegler TR, Rhodes JE, et al. Randomized trial of two maintenance doses of vitamin D in children with chronic kidney disease. Pediatr Nephrol. 2022;37:415–422. doi: 10.1007/s00467-021-05228-z. [DOI] [PubMed] [Google Scholar]
- 88.Natarajan CK, Sankar MJ, Agarwal R, Pratap OT, et al. Trial of daily vitamin D supplementation in preterm infants. Pediatrics. 2014;133:e628–634. doi: 10.1542/peds.2012-3395. [DOI] [PubMed] [Google Scholar]
- 89.Fort P, Salas AA, Nicola T, Craig CM, et al. A comparison of 3 vitamin D dosing regimens in extremely preterm infants: a randomized controlled trial. J Pediatr. 2016;174:132–138.e1. doi: 10.1016/j.jpeds.2016.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Backström MC, Mäki R, Kuusela AL, Sievänen H, et al. Randomised controlled trial of vitamin D supplementation on bone density and biochemical indices in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1999;80:F161–F166. doi: 10.1136/fn.80.3.f161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mathur NB, Saini A, Mishra TK. Assessment of adequacy of supplementation of vitamin D in very low birth weight preterm neonates: a randomized controlled trial. J Trop Pediatr. 2016;62:429–435. doi: 10.1093/tropej/fmv110. [DOI] [PubMed] [Google Scholar]
- 92.Alizadeh Taheri P, Sajjadian N, Beyrami B, Shariat M. Prophylactic effect of low dose vitamin D in osteopenia of prematurity: a clinical trial study. Acta Med Iran. 2014;52:671–674. [PubMed] [Google Scholar]
- 93.Anderson-Berry A, Thoene M, Wagner J, Lyden E, et al. Randomized trial of two doses of vitamin D3 in preterm infants <32 weeks: dose impact on achieving desired serum 25(OH)D3 in a NICU population. PLoS ONE. 2017;12:e0185950. doi: 10.1371/journal.pone.0185950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Al-Beltagi M, Rowiesha M, Elmashad A, Elrifaey SM, et al. Vitamin D status in preterm neonates and the effects of its supplementation on respiratory distress syndrome. Pediatr Pulmonol. 2020;55:108–115. doi: 10.1002/ppul.24552. [DOI] [PubMed] [Google Scholar]
- 95.Bozkurt O, Uras N, Sari FN, Atay FY, et al. Multi-dose vitamin D supplementation in stable very preterm infants: prospective randomized trial response to three different vitamin D supplementation doses. Early Hum Dev. 2017;112:54–59. doi: 10.1016/j.earlhumdev.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 96.Shroff R, Wan M, Gullett A, Ledermann S, et al. Ergocalciferol supplementation in children with CKD delays the onset of secondary hyperparathyroidism: a randomized trial. Clin J Am Soc Nephrol. 2012;7:216–223. doi: 10.2215/CJN.04760511. [DOI] [PubMed] [Google Scholar]
- 97.Lerch C, Shroff R, Wan M, Rees L, et al. Effects of nutritional vitamin D supplementation on markers of bone and mineral metabolism in children with chronic kidney disease. Nephrol Dial Transplant. 2018;33:2208–2217. doi: 10.1093/ndt/gfy012. [DOI] [PubMed] [Google Scholar]
- 98.Wan M, Green B, Iyengar AA, Kamath N, et al. Population pharmacokinetics and dose optimisation of colecalciferol in paediatric patients with chronic kidney disease. Br J Clin Pharmacol. 2022;88:1223–1234. doi: 10.1111/bcp.15064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Harris M, Varnell C, Taylor V, Tulley Nehus S, et al. Hypervitaminosis A in pediatric patients with advanced chronic kidney disease. J Ren Nutr. 2021;S1051–2276(21):00092–93. doi: 10.1053/j.jrn.2021.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Manickavasagar B, McArdle AJ, Yadav P, Shaw V, et al. Hypervitaminosis A is prevalent in children with CKD and contributes to hypercalcemia. Pediatr Nephrol. 2015;30:317–325. doi: 10.1007/s00467-014-2916-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Salusky IB, Goodman WG, Sahney S, Gales B, et al. Sevelamer controls parathyroid hormone-induced bone disease as efficiently as calcium carbonate without increasing serum calcium levels during therapy with active vitamin D sterols. J Am Soc Nephrol. 2005;16:2501–2508. doi: 10.1681/ASN.2004100885. [DOI] [PubMed] [Google Scholar]
- 102.Pieper A-K, Haffner D, Hoppe B, Dittrich K, et al. A randomized crossover trial comparing sevelamer with calcium acetate in children with CKD. Am J Kidney Dis. 2006;47:625–635. doi: 10.1053/j.ajkd.2005.12.039. [DOI] [PubMed] [Google Scholar]
- 103.Gonzalez E, Schomberg J, Amin N, Salusky IB, et al. Sevelamer carbonate increases serum bicarbonate in pediatric dialysis patients. Pediatr Nephrol. 2010;25:373–375. doi: 10.1007/s00467-009-1328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ferrara E, Lemire J, Reznik VM, Grimm PC. Dietary phosphorus reduction by pretreatment of human breast milk with sevelamer. Pediatr Nephrol. 2004;19:775–779. doi: 10.1007/s00467-004-1448-6. [DOI] [PubMed] [Google Scholar]
- 105.Raaijmakers R, Houkes LMW, Schröder CH, Willems JL, et al. Pre-treatment of dairy and breast milk with sevelamer hydrochloride and sevelamer carbonate to reduce phosphate. Perit Dial Int. 2013;33:565–572. doi: 10.3747/pdi.2012.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Taylor JM, Oladitan L, Carlson S, Hamilton-Reeves JM. Renal formulas pretreated with medications alters the nutrient profile. Pediatr Nephrol. 2015;30:1815–1823. doi: 10.1007/s00467-015-3115-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Shroff R, Wan M, Nagler EV, Bakkaloglu S, et al. Clinical practice recommendations for treatment with active vitamin D analogues in children with chronic kidney disease stages 2–5 and on dialysis. Nephrol Dial Transplant. 2017;32:1114–1127. doi: 10.1093/ndt/gfx080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bernardor J, Flammier S, Zagozdzon I, Lalayiannis A et al (2022) The use of cinacalcet in dialysis infants: data from a European survey. 19th IPNA Congress, Calgary, Canada.
- 109.Bacchetta J, Plotton I, Ranchin B, Vial T, et al. Precocious puberty and unlicensed paediatric drugs for severe hyperparathyroidism. Nephrol Dial Transplant. 2009;24:2595–2598. doi: 10.1093/ndt/gfp211. [DOI] [PubMed] [Google Scholar]
- 110.Schaefer B, Schlosser K, Wühl E, Schall P, et al. Long-term control of parathyroid hormone and calcium-phosphate metabolism after parathyroidectomy in children with chronic kidney disease. Nephrol Dial Transplant. 2010;25:2590–2595. doi: 10.1093/ndt/gfq074. [DOI] [PubMed] [Google Scholar]
- 111.Schlosser K, Schmitt CP, Bartholomaeus JE, Suchan KL, et al. Parathyroidectomy for renal hyperparathyroidism in children and adolescents. World J Surg. 2008;32:801–806. doi: 10.1007/s00268-007-9318-6. [DOI] [PubMed] [Google Scholar]
- 112.Drube J, Wan M, Bonthuis M, Wühl E, et al. Clinical practice recommendations for growth hormone treatment in children with chronic kidney disease. Nat Rev Nephrol. 2019;15:577–589. doi: 10.1038/s41581-019-0161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


