Abstract
This network meta‐analysis aims to evaluate the comparative effectiveness and safety of suture anchors (SA), tendon grafts (TG), hook plates (HP), Tight‐Rope (TR), and EndoButton (EB) in the treatment of acute acromioclavicular joint (ACJ) dislocation. The Embase, PubMed, and Web of Science databases were searched from their inception date to June 3, 2022. Studies included all eligible randomized controlled trials (RCTs) and cohort studies with the comparison of five different fixation systems among SA, TG, HP, TR, and EB were identified. All studies were reviewed, performed data extraction, and assessed the risk of bias independently by two reviewers. The primary outcomes are Constant–Murley score (CMS) improvement for assessing clinical efficacy, and complications. The second outcomes are visual analog scale (VAS) for assessing pain relief and the coracoclavicular distance (CCD) for assessing postoperative joint reduction. Version 2 of the revised Cochrane risk of bias tool for randomized trials (RoB 2) and the risk of bias in nonrandomized studies of interventions (ROBINS‐I) were used to assess the RCTs and non‐randomized trials, respectively. The continuous outcomes were presented as mean differences (MD), and risk ratios (OR) were used for dichotomous outcomes, both with 95% confidence intervals (CI). Surface under the cumulative ranking curves (SUCRA) results were calculated to offer a ranking of each intervention. We identified 31 eligible trials, including 1687 patients in total. HP showed less CMS improvement than TR and EB in both the Network Meta‐analysis (NMA) and pairwise meta‐analysis. HP also showed less CMS improvement than SA in NMA. For pain relief, HP performed worse than TR both in pairwise meta‐analysis and NMA. No significant differences were found for the measured value of CCD. Both TR and EB showed a lower incidence of complications than HP in pairwise meta‐analysis. The rank of SUCRA for CMS improvement was as follows: SA, TR, EB, TG, and HP; for pain relief: TR, EB, TG, SA, and HP; for CCD: HP, TR, SA, EB, and TG. For complications, HP showed the highest rank, followed by TG, EB, TR, and SA. SA shows better clinical effectiveness and reliable safety in the treatment of acute ACJ dislocation. Although HP is the most widely used surgical option currently, it should be carefully taken into consideration for its high incidence of complications.
Keywords: Acute Acromioclavicular Joint Dislocation, Internal Fixation, Network Meta‐Analysis, Rockwood Classification, Surgery
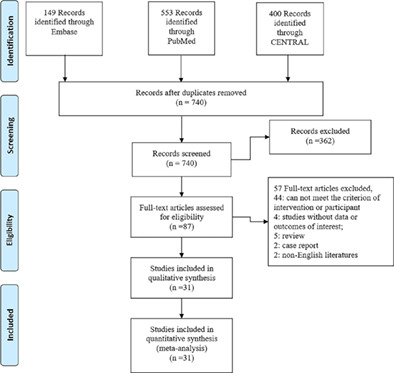
A PRISMA flow chart of article selection process for the network meta‐analysis. A total of 1102 potential titles were screened through the first search strategy, with 362 excluded due to duplications. Among the remaining 740 studies, 87 potentially qualified articles were acquired to check eligibility after carefully screening titles and abstracts and 56 studies were excluded after scanning of the entire body text. A total of 31 full‐text articles were assessed for eligibility.
Introduction
Acute acromioclavicular joint (ACJ) dislocation is the most common sports‐related injury accounting for more than 50% of cases. 1 , 2 Rockwood's classification of ACJ is the most commonly used in clinical practice. 3 , 4 It is based on the degree and direction of clavicle displacement. 4 Rockwood's classification suggests that surgery should be the first choice for some type III and all type IV–VI dislocations. 3 , 4
Given that acromioclavicular and coracoclavicular (CC) are the most important structures for holding the stability of the ACJ. 5 The current main surgery strategy for unstable acute ACJ dislocation is to reconstruct acromioclavicular (AC) or coracoclavicular (CC). Due to CC reconstruction being lower in difficulty than that AC reconstruction, CC reconstruction has become the clinically preferred surgical strategy. 6 The main surgical procedures reported for CC reconstruction in the literature so far include suture anchors (SA), tendon grafts (TG), hook plates (HP), Tight‐Rope (TR), and EndoButton (EB). 6 , 7 , 8 , 9 , 10 , 11 , 12
Each surgical procedure has its advantages and disadvantages, thus a multitude of evaluation methods from various perspectives was utilized to comprehensively access postoperative efficacy. Clinically Constant–Murley score (CMS) is the most commonly used scale to assess shoulder function. 1 The CMS is a 100‐point scale composed of several individual parameters. 2 It is divided into four subscales: pain, activities of daily living, strength, and range of motion. 2 Although CMS includes a pain assessment component, the visual analog scale (VAS) is still widely used to rate patients' postoperative pain. It is one of the pain rating scales used for the first time in 1921 by Hayes and Patterson, which is often used in epidemiologic and clinical research to measure the intensity or frequency of various symptoms. 3 Meanwhile, the radiological assessment is evaluated by coracoclavicular distance (CCD). The CCD is commonly defined as the height as a percentage to the contralateral shoulder between the upper border of the coracoid process and the inferior cortex of the clavicle. 4 Currently, CMS and VAS are the most important indicators for the evaluation of clinical efficacy, while CCD is used to access the radiological results.
Although all surgical procedures have been reported to achieve satisfactory clinical results, there is still debate as to which one is the best choice. The pairwise meta‐analyses have only directly compared HP with TR, 13 , 14 EB, 15 or other CC ligament fixation 16 previously, whereas the refined direct or indirect comparisons between the various surgical procedures are lacking. Therefore, adequate evidence was still insufficient to ensure which one is optimal for treating acute ACJ dislocation. Network meta‐analysis (NMA) has been developed to give indirect results of more than two options based on indirect outcomes and a rank of all the options. 17 Hence, we built an NMA to comprehensively analyze and rank the five surgical procedures from the aspects of the Constant–Murley score, visual analog scale, CC distance, and complications.
Methods
Our study complied with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analyses) and AMSTAR (Assessing the Methodological Quality of Systematic Reviews) guidelines inclusion and exclusion criteria.
Types of Studies
In our NMA, we identified relevant studies, including all RCTs or non‐RCT studies, to compare the efficacy and safety of SA, TR, TG, EB, and HP. For accessing literature quality assessment, papers with abstracts only and RCT protocols were excluded. Additionally, the following were all excluded: review articles, meta‐analyses, cadaveric and animal research, case report, conference paper, and incomplete or missing data. The study selection process was showed in detail in Figure 1.
FIGURE 1.
Flowchart of the study selection process.
Types of Participants
Participants were adults aged 18 years or older with ACJ dislocation, without distinction in terms of ethnicity, gender, and race.
Types of Interventions
The studies which aimed at any comparison of SA, TR, TG, EB, and HP were included. Each study contained at least two of the five surgical procedures.
Types of Outcomes
The following four main outcomes were obtained: Constant–Murley score (CMS), visual analog score (VAS), coracoclavicular distance (CCD), and complications.
Search Strategy
Embase, PubMed, and Web of Science were searched from their inception date to June 3, 2022. The following keywords were used for searching in an electronic database: acute acromioclavicular dislocation, hook plate, EndoButton, suture anchors, tightrope, Bosworth screws, screw, tension band wire, and Kirchner wires. Search strategies were described in detail in “Supplementary files.” Previously published systematic reviews and meta‐analyses were also screened to search for the relevant trials. Only English‐language articles were screened in our meta‐analysis.
Study Selection
After the removal of duplicates, two reviewers independently retrieved and reviewed the titles and abstracts of all publications. The full‐text papers were obtained to identify the eligibility of studies for inclusion when necessary. Then, the reviewers selected potentially relevant studies according to pre‐designed criteria. If discrepancies in judgment arose, a third reviewer was consulted.
Data Extraction and Quality Assessment
The basic information was extracted from each enrolled study using a specifically designed form. The extracted data was as follows: (1) general information: lead author, year of publication, study design, country of study, study period, and follow‐up time; (2) demographic information: the number and proportion of male or female patients, age at diagnosis, number of involved patients; (3) surgery information (intervention and comparison); (4) clinical outcome information: VAS, CCD, CMS, and complication. If SD is not available from the publication, we imputed the SD which used the method from the Cochrane Handbook. For the assessment of consistency, the value of the correlation coefficient (0.5 and 1) was also calculated.
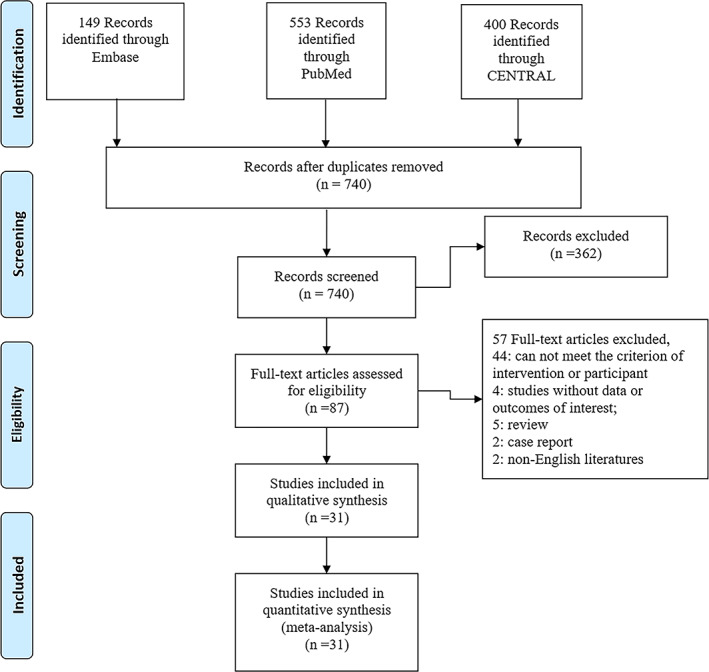
The Geometry of the Network
The network of four outcomes was presented summarily as graphs. The size of the circle and the thickness of the edge represented the number of patients included and the number of studies, respectively. A qualitative description of network geometry was provided.
Risk of Bias within Individual Studies
We applied the RoB 2 for randomized trials, 18 and ROBINS‐I for non‐randomized trials 19 to assess methodological quality. HY and YY were evaluated independently. The ROBINS‐I checklist included seven main domains: confounding, selection bias, classification of intervention, reporting bias, deviations from intervention, missing data, and measuring the outcome. According to the general guideline of the ROBINS‐I, each domain contains five levels of bias judgment: no information (0), low (1), moderate (2), serious (3), critical (4).The assessment was categorized as high quality if most of the domains were well‐described and scored low risk of bias. The strength of evidence of RCTs was evaluated by the five domains (randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, selection of the reported result) using RoB 2 tool. After the discrepancies in grading was discussed, researchers came to consensus on final rating.
Summary Measures
CMS improvement, VAS, and CCD were measured as mean difference (MD) with a 95% confidence interval (CI) individually. And the complications were measured as odds ratio (OR) with 95% CI. Surface under the cumulative ranking curves (SUCRA) values were calculated to offer a ranking of all interventions.
Planned Methods of Analysis
The data with treatments as well as clinical outcomes were extracted. Direct comparisons of the pairwise meta‐analysis were performed using a random‐effects model. MD with 95% CI for CMS improvement, VAS, and CCD as continuous variables of outcome were provided. And OR with 95% CI for complications as a dichotomous outcome was presented. The statistical heterogeneity across studies was assessed by the χ2 test and the inconsistency (I2). All statistical analyses were carried out using STATA with Metan package (Version 15.0; STATA Corporation, College Station, TX). Second, the NMA was built within the Bayesian framework by the Markov Chain Monte Carlo algorithm in WinBUGS 1.4.3 20 using a random effect model. Results presented for each model were simulated on three Markov chains for 100,000 iterations, after a burn‐in of 50,000.
The number of thinning intervals was set at 10 iterations. Subsequently, the direct and indirect variances of convergence were obtained through the Brooks–Gelman–Rubin method. 21 The potential scale reduction factor (PSRF) (approaching or equal to 1.0) indicated that convergence has been achieved. 21 The NMA results were also presented as OR or MD with a 95% confidence interval. The results of five fixation methods, which were calculated by WinBUGS, were input by STATA to generate the surface under the cumulative ranking curves (SUCRA). 22 The value of SUCRA was presented as 0% (the worst treatment) to 100% (the best treatment).
Assessment of Inconsistency
Risk of Bias Across Studies
The global inconsistency was measured by the consistency and inconsistency models. Model fit was compared using the deviance information criterion (DIC) and a reduction of larger than 3 in DIC shows the inconsistency existed. The local inconsistency was evaluated by the node‐splitting method. 23 If node‐splitting analysis showed a p‐value <0.05, inconsistency would be considered statistically significant.
RESULTS
Documentation Retrieval
A total of 1102 potential titles were screened through the first search strategy, with 362 excluded for duplications. Among the remaining 740 studies, 87 potentially qualified articles were acquired to check eligibility after carefully screening titles and abstracts. With careful full‐text reading, 56 studies were excluded for the reasons shown in Figure 1. Finally, 31 articles were included in our study. 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54
Network Graphs
All the network of comparisons were shown in Figure 2. The network for CMS included 21 studies, for VAS included 15 studies, for CCD included 13 studies, and for complications included 27 studies. Lines between two nodes indicate direct evidence between two interventions, with the thickness of the line corresponding to the number of studies. The size of the nodes corresponds to the number of treatments included.
FIGURE 2.
Network of comparisons of HP, TR, TG, EB, and Suture for AC dislocation. The circle means the number of patients, and the edge thickness means the number of studies. CCD, coracoclavicular distance; CMS, Constant–Murley score; EB, EndoButton; HP, hook plates; SA, suture anchors; TG, tendon grafts, TR, Tight‐Rope; AS, visual analog scale.
Characteristics of the Included Trials
A total of 1687 patients were recorded. The network for CCM included 1252, for VAS included 1000, for CCD included 615, and for complications included 1539. Three studies were RCTs and 28 were retrospective studies. We recorded the characteristics of all included studies in Table 1.
TABLE 1.
Characteristics of included trials
| Author | Year | Region | Design | Intervention | Number of patients (M/F) | Mean age (years) | Follow‐up (months) | CMS | VAS | CCD | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Leyi | 2017 | China | RCT | TR | 30(19/11) | 42.80 ± 11.88 | 12 | 91.97 ± 6.70 | 0.97 ± 1.03 | 12.13 ± 1.96 | 3/30 |
| HP | 39(26/13) | 41.79 ± 10.2 | 12 | 92.56 ± 6.37 | 1.92 ± 1.11 | 11.90 ± 2.51 | 5/39 | ||||
| Emre | 2021 | Turkey | R | TR | 21(19/2) | 39.2(20–60) | 12 | NR | NR | NR | 12/21 |
| HP | 14(13/1) | 41.8(18–85) | 12 | NR | NR | NR | 7/14 | ||||
| Frank | 2013 | Germany | R | EB | 13(NR) | 43.6(18–71) | 28.8(12–68.4) | NR | NR | NR | 3/13 |
| TG | 46(NR) | 43.6(18–71) | 28.8(12–68.4) | NR | NR | NR | 13/46 | ||||
| Athar | 2017 | Germany | RCT | HP | 52(0/52) | 44.8 ± 9.1 | ≥12 | NR | NR | NR | 17/52 |
| TR | 24(1/23) | 42.6 ± 11.6 | ≥12 | NR | NR | NR | 13/24 | ||||
| P. Vulliet | 2017 | France | R | TR | 22(19/3) | 38.8 ± 8.7 | 27.7 ± 8.3 | 94.3 ± 4.4 | 0.5 ± 1.1 | NR | 6/22 |
| EB | 18(15/3) | 37.4 ± 14.8 | 24.1 ± 5.0 | 95.0 ± 6.1 | 1.0 ± 1.9 | NR | 16/18 | ||||
| Si Nie | 2021 | China | R | TR | 28(11/17) | 35.9 ± 7.9 | 33.1 ± 6.0 | 89.3 ± 4.2 | 1.2 ± 0.6 | NR | 2/28 |
| HP | 84(33/51) | 36.0 ± 8.3 | 32.9 ± 6.4 | 83.3 ± 8.8 | 1.8 ± 1.1 | NR | 12/84 | ||||
| Michele | 2021 | Italy | R | HP | 22(16/6) | 48.2(22–70) | 40.6 ± 13.7 | 92.7 ± 5.1 | NR | NR | 13/22 |
| TR | 22(20/2) | 40.5(21–63) | 32.0 ± 10.1 | 96.1 ± 6.2 | NR | NR | 5/22 | ||||
| Jong Pil | 2015 | Korea | R | HP | 24(19/5) | 38.8 ± 14.2 | 16.0 ± 12.8 | 90.2 ± 9.9 | 1.6 ± 1.5 | NR | 9/24 |
| TG | 18(14/4) | 42.2 ± 12.3 | 17.4 ± 4.3 | 89.2 ± 3.5 | 1.3 ± 1.3 | NR | 6/18 | ||||
| Sandesh | 2022 | India | R | HP | 16(16/0) | 44.3 ± 12.82 | 55.38 ± 10.9 | 92.38 ± 6.64 | NR | 7.02 ± 2.36 | 12/16 |
| EB | 16(13/3) | 42.1 ± 11.85 | 32.88 ± 14.0 | 94.65 ± 2.38 | NR | 10.08 ± 4.08 | 11/16 | ||||
| Pei Yu | 2022 | China | R | HP | 60(35/25) | 56.43 ± 9.64 | 12 | 91.00 ± 4.82 | 0.97 ± 0.60 | 10.10 ± 3.01 | 2/60 |
| TR | 52(32/20) | 50.2 ± 15.39 | 12 | 92.08 ± 5.80 | 0.88 ± 0.58 | 11.38 ± 2.94 | 0/52 | ||||
| Song Liu | 2022 | China | R | TR | 32(23/9) | 39.6 ± 8.9 | 12 | 94.8 ± 3.5 | 0.3 ± 0.8 | 12.2 ± 1.6 | 1/32 |
| HP | 39(29/10) | 41.8 ± 10.5 | 12 | 94.4 ± 3.2 | 0.4 ± 0.8 | 12.6 ± 1.6 | 3/39 | ||||
| Hasan | 2018 | Iran | R | HP | 8(7/1) | 39.6 ± 16.2 | 19.8 ± 8.8 | 55 ± 22.9 | 0.76 ± 0.95 | 8.6 ± 0.9 | NR |
| EB | 9(8/1) | 37.3 ± 12.02 | 23.8 ± 19.2 | 91.7 ± 5.9 | 0.32 ± 0.89 | 11.6 ± 1.2 | NR | ||||
| Omer | 2020 | Turkey | R | HP | 21(6/15) | 30.7 ± 9.65 | 32.4 (26–42) | NR | NR | NR | 8/21 |
| EB | 18(5/13) | 31.7 ± 8.17 | 34.6 (21–45) | NR | NR | NR | 7/18 | ||||
| Anica | 2011 | Germany | R | HP | 27(NR) | 42.3(23–73) | >9 | 91.2 ± 2.2 | 0.77 ± 0.2 | 16.7 ± 0.77 | 10/27 |
| SA | 25(NR) | 42.3(23–73) | >9 | 94.6 ± 1.0 | 0.80 ± 0.2 | 23.9 ± 1.2 | 3/25 | ||||
| Yon‐Sik | 2020 | Korea | R | SA | 12(8/4) | 42.8 ± 5.4 | 30.1 ± 5.5 | NR | 1.02 ± 1.32 | 7.96 ± 2.52 | 2/12 |
| HP | 10(7/3) | 44.4 ± 6.5 | 33.8 ± 7.6 | NR | 1.14 ± 1.45 | 11.27 ± 2.59 | 4/10 | ||||
| L. Natera | 2015 | Spain | R | TR | 20(17/3) | 36(25–52) | 38.40 ± 4.34 | 95.30 ± 2.45 | 0.40 ± 0.50 | NR | 3/20 |
| HP | 11(11/0) | 41(19–55) | 32.5 ± 11.64 | 91.36 ± 6.84 | 1.45 ± 1.51 | NR | 2/11 | ||||
| Alexandre | 2016 | Brazil | R | SA | 12(11/1) | 35.4 ± 16.1 | >6 | NR | 1.2 ± 1.3 | NR | 0 |
| TR | 11(11/1) | 32.4 ± 11.05 | >6 | NR | 1.2 ± 2.0 | NR | 1/11 | ||||
| Murat | 2020 | Turkey. | R | SA | 9(9/0) | 39(24–56) | 13.7 ± 2.7 | 93.6 ± 3.7 | NR | 15.2 ± 3.9 | 0/9 |
| EB | 11(11/0) | 37(22–50) | 12.9 ± 1.4 | 89.6 ± 13.6 | NR | 16.0 ± 4.4 | 1/11 | ||||
| Ruchu | 2019 | Poland | R | SA | 11(NR) | 39(18–63) | 21.2 ± 13.1 | 95.22 ± 10.3 | NR | NR | NR |
| HP | 4(NR) | 39(18–63) | 10.8 ± 3.2 | 78.97 ± 12.1 | NR | NR | NR | ||||
| Gunnar | 2012 | Germany | R | HP | 30(28/2) | 39(16–68) | 48(7–77) | NR | 1.7 ± 2.3 | NR | 8/30 |
| TR | 26(23/3) | 39(18–54) | 17(7–29) | NR | 1.3 ± 1.8 | NR | 5/26 | ||||
| Hamid | 2017 | Singapore | R | TR | 16(15/1) | 41.4 ± 12.3 | 23(14–35) | 87.6 ± 11.7 | 1.0 ± 1.7 | 11.8 ± 1.7 | 0/16 |
| HP | 10(9/1) | 49.2 ± 16.9 | 23(14–35) | 77.5 ± 12.3 | 1.0 ± 0.7 | 13.6 ± 4.8 | 3/10 | ||||
| Yu‐chen | 2020 | China | R | TR | 30(18/12) | 39.4 ± 15.3 | 27.67 ± 2.48 | 93.70 ± 1.78 | NR | 11.40 ± 1.13 | 0/30 |
| EB | 30(12/18) | 42.20 ± 13.5 | 28.30 ± 2.51 | 93.27 ± 1.59 | NR | 11.47 ± 1.19 | 1/30 | ||||
| You‐Shui | 2015 | China | R | HP | 24(19/5) | 36.0 ± 6.7 | 18.3 ± 8.0 | 86.1 ± 5.7 | NR | NR | 16/24 |
| TR | 24(18/6) | 35.4 ± 8.6 | 18.8 ± 7.5 | 97.5 ± 2.7 | NR | NR | 6/24 | ||||
| Cheng | 2018 | China | R | SA | 25(15/20) | 43.7 ± 15.6 | 26.2(24–35) | NR | NR | NR | 10/25 |
| HP | 24(19/5) | 42.0 ± 14.9 | 26.2(24–35) | NR | NR | NR | 9/21 | ||||
| Guheng | 2018 | China | R | TG | 8(6/2) | 49.0 ± 17.8 | 29.8 ± 6.0 | NR | NR | NR | 0/8 |
| HP | 8(5/3) | 41.3 ± 13.4 | 30.9 ± 7.8 | NR | NR | NR | 0/8 | ||||
| Guangsi | 2021 | China | R | TR | 16(11/5) | 44.9 ± 11 | 27 | 95.7 ± 7.3 | 0.4 ± 0.6 | NR | 1/16 |
| HP | 19(10/9) | 40.2 ± 8.7 | 30 | 93.7 ± 6.6 | 0.7 ± 0.6 | NR | 1/19 | ||||
| Thomas | 2018 | Germany | RCT | HP | 27(26/1) | 37.65 ± 9.66 | 40.1 ± 23.64 | 90.19 ± 7.79 | NR | 19.38 ± 6.42 | NR |
| EB | 29(28/1) | 34.24 ± 9.68 | 30.75 ± 1.41 | 95.31 ± 4.42 | NR | 16.92 ± 4.16 | NR | ||||
| Jun Zhang | 2017 | China | R | EB | 30(NR) | 40.83 ± 10.2 | 24 | 91.2 ± 7.0 | NR | NR | 0/30 |
| HP | 30(NR) | 37.80 ± 13.9 | 24 | 89.6 ± 4.0 | NR | NR | 5/30 | ||||
|
Yingliang |
2021 | China | R | SA | 32(28/4) | 34 | 39.69 ± 7.42 | NR | NR | 11.62 ± 2.54 | NR |
| EB | 28(26/2) | 32 | 37.86 ± 8.23 | NR | NR | 16.78 ± 5.53 | NR | ||||
| Sujie | 2021 | China | R | HP | 146(45/101) | 40.2 | 3 | 87.4 ± 5.2 | 0.9 ± 0.7 | NR | 96/146 |
| EB | 146(47/99) | 38.7 | 3 | 88.4 ± 3.9 | 0.5 ± 0.5 | NR | 77/146 | ||||
| Alberto | 2015 | Italy | R | TR | 10(9/1) | 43.3 ± 12.9 | 43.3 ± 12.8 | 96.5 ± 4.9 | NR | 12.51 ± 3.48 | 6/10 |
| TG | 8(7/1) | 50.9 ± 10.4 | 62.7 ± 18.78 | 93.3 ± 7.0 | NR | 16.5 ± 4.4 | 5/8 |
Abbreviations: CCD, coracoclavicular distance; CMS, Constant–Murley score; EB, EndoButton; HP, hook plates; NR, not record; R, retrospective study; RCT, randomized controlled study; SA, suture anchors; TG, tendon grafts; TR, Tight‐Rope; VAS, visual analog scale.
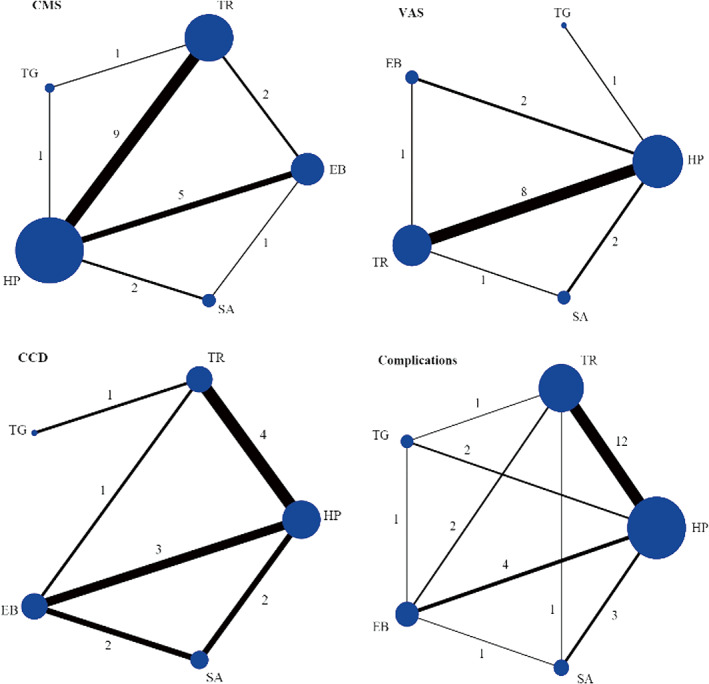
Risk of Bias and Quality Assessment
According to the ROBINS‐I tool analysis, Table 2 presented the quantification of the risk of bias assessment of retrospective studies. The outcome showed that the overall risk of bias in all eligible studies was moderate, indicating all of the studies were of high quality. However, selection bias was inevitable for none of these studies were randomized studies. The risk of bias analysis of the included three RCTs was evaluated by using RoB 2 tool analysis. The results were listed in Figure 3. Some concerns in the randomization process were mentioned in two studies, and the bias of measurement of the outcome was described in detail in one study. No study reported the deviations from intended interventions, missing outcome data, and selection. Thus, two domains, the randomization process and measurement of the outcome, possibly led to bias.
TABLE 2.
Evaluation of the quality of studies with the ROBINS‐I
| Bias Domain | Bias due to confounding | Selection of participants | Classification of interventions | Deviations from intended interventions | Bias due to missing data | Measurement of outcomes | Selection of the reported result | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|
| Song 2022 | Low | Low | Low | Low | Low | Low | Moderate | Moderate |
| Sandesh 2022 | Low | Low | Low | Low | Moderate | Moderate | Low | Moderate |
| Pei Yu 2022 | Moderate | Low | Low | Low | Low | Low | Low | Moderate |
| Yingliang 2021 | Moderate | Low | Low | Low | Low | Moderate | Moderate | Moderate |
| Sujie 2021 | Low | Low | Low | Low | Moderate | Moderate | Low | Moderate |
| Si Nie 2021 | Low | Low | Low | Low | Low | Moderate | Low | Moderate |
| Michele 2021 | Moderate | Low | Low | Low | Low | Moderate | Moderate | Moderate |
| Guangsi 2021 | Low | Low | Low | Low | Low | Moderate | Low | Moderate |
| Emre 2021 | Moderate | Low | Low | Moderate | Low | Moderate | Low | Moderate |
| Yon‐Sik 2020 | Moderate | Low | Low | Low | Low | Low | Low | Moderate |
| Omer 2020 | Low | Low | Low | Moderate | Low | Moderate | Low | Moderate |
| Murat 2020 | Moderate | Moderate | Low | Low | Low | Moderate | Low | Moderate |
| Yu‐chen 2020 | Low | Low | Low | Low | Low | Moderate | Low | Moderate |
| Klinika 2019 | Serious | Moderate | Low | Moderate | Low | Moderate | Moderate | Moderate |
| Ying‐Cheng 2018 | Low | Low | Low | Low | Low | Moderate | Low | Moderate |
| Hasan 2018 | Moderate | Moderate | Low | Low | Low | Moderate | Low | Moderate |
| Guheng 2018 | Moderate | Moderate | Low | Moderate | Low | Moderate | Low | Moderate |
| P. Vulliet 2017 | Moderate | Low | Low | Low | Low | Moderate | Low | Moderate |
| Jun Zhang 2017 | Moderate | Moderate | Low | Moderate | Low | Moderate | Moderate | Moderate |
| Hamid 2017 | Low | Low | Low | Moderate | Low | Low | Low | Moderate |
| Alexandre 2016 | Moderate | Low | Low | Moderate | Low | Moderate | Moderate | Moderate |
| You‐Shui 2015 | Moderate | Low | Low | Low | Low | Moderate | Low | Moderate |
| L. Natera 2015 | Low | Low | Low | Low | Low | Moderate | Low | Moderate |
| Jong Pil 2015 | Moderate | Low | Low | Moderate | Moderate | Low | Low | Moderate |
| Alberto 2015 | Moderate | Low | Low | Moderate | Moderate | Moderate | Low | Moderate |
| Frank 2013 | Low | Low | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Nasser 2012 | Low | Low | Low | Moderate | Low | Low | Low | Moderate |
| Anica 2011 | Low | Low | Low | Low | Moderate | Moderate | Low | Moderate |
FIGURE 3.
Results of Cochrane Risk of Bias tool (ROB 2) visualized in traffic light plots for each individual domain.
Figure 4 showed a funnel plot assessing publication bias, and the results indicated that small studies did not affect the primary (CMS and complications) and secondary outcomes (VAS, CCD).
FIGURE 4.
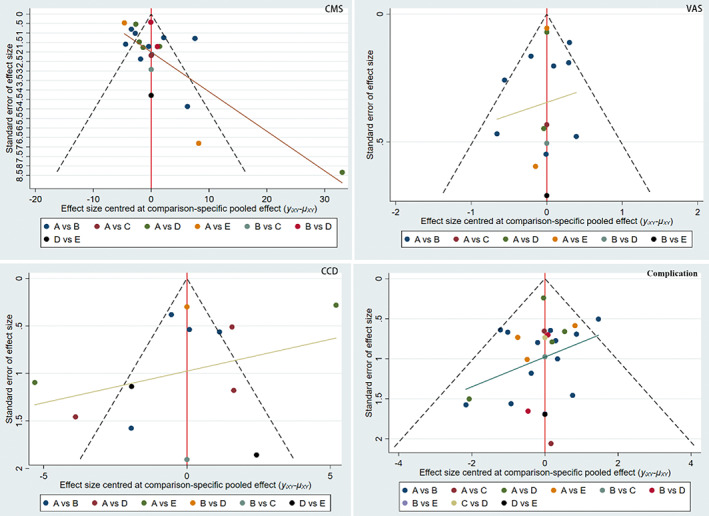
Comparison‐adjusted funnel plot. The red full line represents the null hypothesis that the study‐specific effect sizes do not differ from the respective comparison‐specific pooled effect estimates. The two black dashed lines represent a 95% CI for the difference between study specific effect sizes and comparison‐specific summary estimates. yixy is the noted effect size in study i that compares x with y. lxy is the comparison‐specific summary estimate for x versus y. A, HP; B, TR; C, TG; D, EB; E, SA.
Results of CMS
The results of CMS were shown in Table 3. The lower‐left triangle indicated pairwise meta‐analysis, and the upper‐right triangle indicated NMA. The shadows represented significant differences. HP showed less CMS improvement than TR and EB in both pairwise meta‐analyses [TR vs. HP, MD = 3.83, 95% CI: (0.99, 6.67); EB vs. HP, MD = 3.66, 95% CI: (0.30, 7.02)], and NMA [TR vs. HP, MD = 3.66, 95% CI: (1.47, 5.85); EB vs. HP, MD = 3.57, 95% CI: (0.71, 6.43)]. HP also showed less CMS improvement than SA in pairwise meta‐analysis [SA vs. HP, MD = 5.91, 95% CI: (0.58, 11.24)]. While other than that, no significant differences were found both in pairwise meta‐analysis and NMA. Based on the results obtained from SUCRA, close to 100% represents better CMS. Among them, SA ranked best (88.1%), followed by TR (66.0%), EB (63.7%), TG (18.2%), and HP (13.9%) (Figure 5).
TABLE 3.
Results of the pairwise and network meta‐analysis of CMS (MD, 95% CI)
| SA | 2.34 (−3.21, 7.88) | 6.26 (−1.52, 14.04) | 2.25 (−3.38, 7.88) | 5.91 (0.58, 11.24) |
|---|---|---|---|---|
| N = 1, 4.00 (−4.39, 12.39) | EB | 3.92 (−2.36, 10.20) | −0.09 (−3.18, 3.00) | 3.57 (0.71, 6.43) |
| TG | −4.01 (−9.79, 1.76) | −0.35 (−6.08, 5.38) | ||
| N = 2, −0.36 (−1.19, 0.47) | N = 1, −3.20 (−8.92, 2.52) | TR | 3.66 (1.47, 5.85) | |
| N = 2, 8.03 (−4.06, 20.12) | N = 5, 3.66 (0.30, 7.02) | N = 1, −1.00 (−5.28, 3.28) | N = 9, 3.83 (0.99, 6.67) | HP |
Note: Upper‐right triangle shows the results of the network meta‐analysis. Lower‐left triangle shows the results of the pairwise meta‐analyses. The N represents the numbers of studies which compared the two interventions directly. For MD with 95%CI, a negative MD favor the lower‐right intervention. For OR with 95%CI, a OR >1 favor the lower‐right intervention. Statistically significant findings are shaded.
Abbreviations: CCD, coracoclavicular distance; CI, confidence interval; CMS, Constant–Murley Score; EB, EndoButton; HP, hook plates; MD, mean difference; OR, odd ratio; SA, suture anchors; TG, tendon grafts; TR, Tight‐Rope; VAS, visual analog scale.
FIGURE 5.
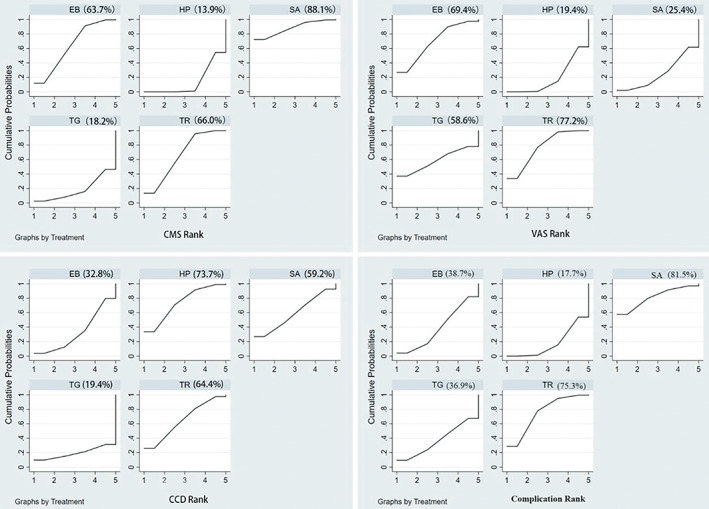
SUCRA of HP, TR, TG, EB, and Suture for AC dislocation. CCD, coracoclavicular distance; CMS, Constant–Murley Score; EB, EndoButton; HP, hook plates; SA, suture anchors; TG, tendon grafts, TR, Tight‐Rope; VAS, visual analog scale.
Results of VAS
The results of VAS were shown in Table 4. HP showed less pain relief than TR both in pairwise meta‐analysis [TR vs. HP, MD = −0.39, 95% CI: (−0.65, −0.14)] and NMA [TR vs. HP, MD = −0.39, 95% CI: (−0.63, −0.16)]. HP did not differ significantly from EB in the NMA but showed less pain relief than EB in pairwise meta‐analysis [EB vs. HP, MD = −0.40, 95% CI: (−0.54, −0.26)]. Other than that, no other significant differences were found. Based on the results obtained from SUCRA, close to 100% represents better pain relief. Among them, TR ranked best (77.2%), followed by EB (69.4%), TG (58.6%), SA (25.4%), and HP (19.4%) (Figure 5).
TABLE 4.
Results of the pairwise and network meta‐analysis of VAS (MD, 95% CI)
| SA | 0.32 (−0.26, 0.90) | 0.28 (−0.76, 1.32) | 0.37 (−0.09, 0.83) | −0.02 (−0.43, 0.40) |
|---|---|---|---|---|
| EB | −0.04 (−1.08, 0.99) | 0.05 (−0.40, 0.50) | −0.34 (−0.74, 0.05) | |
| TG | 0.09 (−0.89, 1.08) | −0.30 (−1.26,0.66) | ||
| N = 1, 0.00 (−1.39, 1.39) | N = 1, 0.50 (−0.49, 1.49) | TR | −0.39 (−0.63, −0.16) | |
| N = 2, 0.03 (−0.08, 0.14) | N = 2, −0.40 (−0.54, −0.26) | N = 1, −0.30 (−6.33, 5.73) | N = 8, −0.39 (−0.65, −0.14) | HP |
Note: Upper‐right triangle shows the results of the network meta‐analysis. Lower‐left triangle shows the results of the pairwise meta‐analyses. The N represents the numbers of studies which compared the two interventions directly. For MD with 95%CI, a negative MD favor the lower‐right intervention. For OR with 95%CI, a OR >1 favor the lower‐right intervention. Statistically significant findings are shaded.
Abbreviations: CCD, coracoclavicular distance; CI, confidence interval; CMS, Constant–Murley Score; EB, EndoButton; HP, hook plates; MD, mean difference; OR, odd ratio; SA, suture anchors; TG, tendon grafts; TR, Tight‐Rope; VAS, visual analog scale.
Results of CCD
The results of the CCD were shown in Table 5. TG showed larger CCD than TR in pairwise meta‐analysis [TG vs. TR, MD = 3.99, 95% CI: (0.26, 7.72)]. But given that there is only one set of direct comparisons, this result is not credible. No other significant differences were found between each other. For the results of SUCRA, close to 100% means better reduction. Among them, HP ranked best (73.7%), followed by TR (64.4%), SA (59.2%), EB (32.8%), and TG (19.4%) (Figure 5).
TABLE 5.
Results of the pairwise and network meta‐analysis of CCD (MD, 95% CI)
| SA | −1.31 (−5.12, 2.50) | −3.70 (−12.47, 5.07) | 0.29 (−4.32, 4.90) | 0.59 (−3.14, 4.32) |
|---|---|---|---|---|
| N = 2, −3.23 (−7.47, 1.02) | EB | −2.39 (−10.79, 6.01) | 1.60 (−2.25, 5.44) | 1.90 (−1.20, 4.99) |
| TG | 3.99 (−3.47, 11.45) | 4.29 (−3.77, 12.35) | ||
| N = 1, 0.07 (−0.52, 0.66) | N = 1, 3.99 (0.26, 7.72) | TR | 0.30 (−2.74, 3.34) | |
| N = 2, 2.00 (−8.30, 12.30) | N = 3, 1.43 (−1.50, 4.35) | N = 4, 0.14 (−1.09, 0.80) | HP |
Note: Upper‐right triangle shows the results of the network meta‐analysis. Lower‐left triangle shows the results of the pairwise meta‐analyses. The N represents the numbers of studies which compared the two interventions directly. For MD with 95%CI, a negative MD favor the lower‐right intervention. For OR with 95%CI, a OR >1 favor the lower‐right intervention. Statistically significant findings are shaded.
Abbreviations: CCD, coracoclavicular distance; CI, confidence interval; CMS, Constant–Murley Score; EB, EndoButton; HP, hook plates; MD, mean difference; OR, odd ratio; SA, suture anchors; TG, tendon grafts; TR, Tight‐Rope; VAS, visual analog scale.
Results of Complications
The results of complications are shown in Table 6. TR showed a lower incidence of complications than HP both in pairwise meta‐analysis [TR vs. HP, MD = 0.56, 95% CI: (0.30, 1.00)] and NMA [TR vs. HP, MD = 0.52, 95% CI: (0.31, 0.88)]. EB showed a higher incidence of complications than TR [EB vs. TR, MD = 0.56, 95% CI: (0.30, 1.00)] but lower than that of HP [EB vs. HP, MD = 0.58, 95% CI: (0.38, 0.88)] in pairwise meta‐analysis. Meanwhile, no significant differences were found between each other. For the results of SUCRA, close to 100% means a lower incidence of complications. Among them, SA ranked lowest (81.5%), followed by TR (75.3%), EB (38.7%), TG (36.9%), and HP being the highest incidence of complications (17.7%) (Figure 5).
TABLE 6.
Results of the pairwise and network meta‐analysis of complications (OR, 95% CI)
| SA | 0.53 (0.17, 1.70) | 0.51 (0.12, 2.14) | 0.82 (0.28, 2.43) | 0.43 (0.16, 1.14) |
|---|---|---|---|---|
| N = 1, 0.37 (0.01, 10.18) | EB | 0.96 (0.31, 2.99) | 1.55 (0.70, 3.45) | 0.81 (0.40, 1.62) |
| N = 1, 0.76 (0.18, 3.22) | TG | 1.62 (0.53, 4.98) | 0.84 (0.29, 2.46) | |
| N = 1, 0.28 (0.01, 7.62) | N = 2, 4.92 (1.39, 17.44) | N = 1, 1.11 (0.16, 7.51) | TR | 0.52 (0.31, 0.88) |
| N = 3, 0.52 (0.24, 1.14) | N = 4, 0.58 (0.38, 0.88) | N = 2, 0.83 (0.23, 3.00) | N = 12, 0.56 (0.30, 1.00) | HP |
Note: Upper‐right triangle shows the results of the network meta‐analysis. Lower‐left triangle shows the results of the pairwise meta‐analyses. The N represents the numbers of studies which compared the two interventions directly. For MD with 95%CI, a negative MD favor the lower‐right intervention. For OR with 95%CI, a OR >1 favor the lower‐right intervention. Statistically significant findings are shaded.
Abbreviations: CCD, coracoclavicular distance; CI, confidence interval; CMS, Constant–Murley Score; EB, EndoButton; HP, hook plates; MD, mean difference; OR, odd ratio; SA, suture anchors; TG, tendon grafts; TR, Tight‐Rope; VAS, visual analog scale.
We ranked the surgical procedures according to the two dimensions of clinical efficacy and complication rate (Figure 6). In general, SA showed the best clinical efficacy with the lowest complication rate. Additionally, the high loss of reduction rates should be paid more attention to the groups of EB (21.94%), HP (10.85%), and SA (9.57%). It should also be noted that the HP group was related to a higher ratio of erosion of the acromion and stiffness. The total complication incidence of HP (34.8%), TG (37.5%), and TR (35.8%) are similar, both more than double that of TR (14.8%) and SA (13.0%) (Table 7).
FIGURE 6.
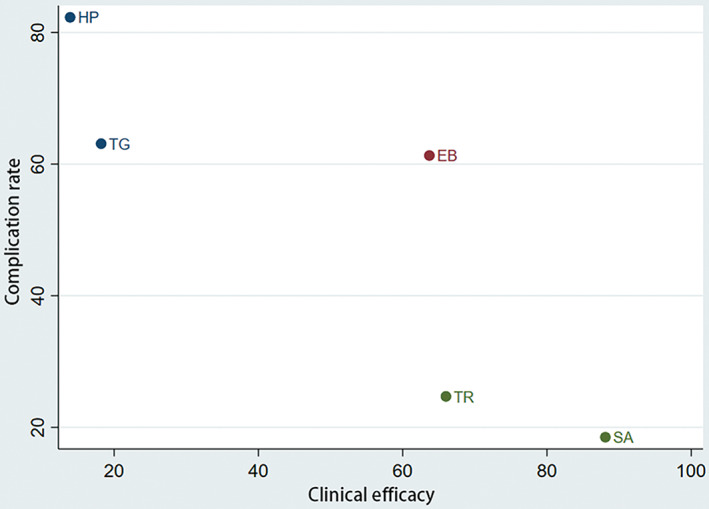
Ranking of the surgical procedures according to primary outcomes: clinical efficacy and complication rate. X axis represents clinical efficacy that close to 100% means better clinical efficacy. Y axis represents complication rate that close to 100% means higher incidence of complication.
TABLE 7.
Number and percentage of complications among the five different fixation systems [No. (%)]
| Complication | |||||
|---|---|---|---|---|---|
| HP (N = 710) | TR (N = 384) | TG (N = 80) | EB (N = 310) | SA (N = 115) | |
| Loss of reduction | 77(10.85%) | 16(4.17%) | 6(7.5%) | 68(21.94%) | 11(9.57%) |
| Impaired wound healing | 9(1.27%) | 5(1.30%) | — | — | 1(0.87%) |
| Impingement syndrome | 9(1.27%) | — | — | — | — |
| Plate/screw breakage or loosening | 21(2.96%) | 7(1.82%) | 7(8.75%) | 7(2.26%) | — |
| Neural injury | 1(0.14%) | — | 1(1.25%) | — | — |
| Bone fracture | 6(0.85%) | 2(0.52%) | 3(3.75%) | 7(2.26%) | — |
| Deep infection | 1(0.14%) | 1(0.26%) | — | 1(0.32%) | — |
| Erosion of the acromion | 36(5.07%) | 1(0.26%) | — | — | — |
| Internal fixation reaction | 1(0.14%) | 2(0.52%) | 8(10%) | 1(0.32%) | — |
| Osteolysis of distal clavicle | — | — | — | — | 1(0.87%) |
| AC joint osteoarthritis | 19(2.68%) | 17(4.43%) | 2(2.5%) | 1(0.32%) | 2(1.74%) |
| Stiffness | 44(6.2%) | 4(1.04%) | — | — | — |
| Ligament ossification | 21(2.96%) | 2(0.52%) | 3(3.75%) | 22(7.1%) | — |
| Skin numbness | 2(0.28%) | — | — | 1(0.32%) | — |
| Muscle tear and fraying | — | — | — | 3(0.97%) | — |
| Total | 34.79% | 14.84% | 37.50% | 35.81% | 13.04% |
Inconsistency Analysis
The results of inconsistency were listed in Table 8. For all outcomes, no local inconsistencies were detected (p values >0.05).
TABLE 8.
The result of inconsistency analysis
| CMS | VAS | CCD | Complications | |||||
|---|---|---|---|---|---|---|---|---|
| Local Inconsistency | Comparison | p value | Comparison | p value | Comparison | p value | Comparison | p value |
| HP versus TR | 0.86 | HP versus TR | 0.59 | HP versus TR | 0.71 | HP versus TR | 0.39 | |
| HP versus TG | 0.80 | HP versus TG | NA | HP versus TG | NA | HP versus TG | 0.98 | |
| HP versus EB | 0.91 | HP versus EB | 0.66 | HP versus EB | 0.38 | HP versus EB | 0.20 | |
| HP versus SA | 0.72 | HP versus SA | 0.26 | HP versus SA | 0.60 | HP versus SA | 0.53 | |
| TR versus TG | 0.80 | TR versus TG | 0.99 | TR versus TG | NA | TR versus TG | 0.70 | |
| TR versus EB | 0.96 | TR versus EB | 0.58 | TR versus EB | 0.38 | TR versus EB | 0.08 | |
| TR versus SA | NA | TR versus SA | NA | TR versus SA | 0.60 | TR versus SA | 0.52 | |
| TG versus EB | NA | TG versus EB | NA | TG versus EB | NA | TG versus EB | 0.75 | |
| EB versus SA | 0.72 | EB versus SA | 0.26 | EB versus SA | NA | EB versus SA | 0.83 | |
| Global inconsistency | Comparison | p value | Comparison | p value | Comparison | p value | Comparison | p value |
| HP versus TR | 0.001 | HP versus TR | 0.85 | HP versus TR | 0.001 | HP versus TR | 0.015 | |
| HP versus TG | 0.90 | HP versus TG | 0.30 | HP versus TG | 0.54 | HP versus TG | 0.75 | |
| HP versus EB | 0.01 | HP versus EB | 0.23 | HP versus EB | 0.09 | HP versus EB | 0.55 | |
| HP versus SA | 0.03 | HP versus SA | 0.76 | HP versus SA | 0.93 | HP versus SA | 0.09 | |
Discussion
To the best of our knowledge, this is the first comprehensive and integrated NMA to pool data focusing on CMS, VAS, CCD, and complications of five widely applied surgical procedures including HP, TR, TG, EB, and SA in the surgical treatment of ACJ; this information can be used to help surgeons choosing the optimal surgical procedure for their actual situations. The key findings of this systematic review and NMA here show that: (1) HP have a worse effect on the CMS improvement than TR, EB, and SA; (2) TR shows better pain relief than HP; (3) all of them have a significant effect in the CCD reduction with no significant difference between each other; (4) HP has a higher incidence of complications than TR, meanwhile no significant difference is observed among the others; (5) the SA has the best clinical efficacy with the lowest complication rate according to our primary outcomes.
Ligament Reconstruction for ACJ Dislocation
The CC ligament is one of the most important stabilizing structures of the ACJ. 5 CC fracture is a major factor in clavicle displacement; therefore, CC reconstruction is important for ACJ reduction and maintaining stability. 6 Since Rockwood's classification of ACJ is based on the degree and direction of clavicle displacement, reconstruction of the CC ligament is the most commonly applied clinical surgical strategy. 3 , 4 Although Bosworth screws have been reported in the literature in addition to the five surgical procedures included in this study, after a careful review of the literature we found that few studies met the criteria and no valid data were available. 55 , 56 , 57 Notably, in addition to CC reconstruction, AC reconstruction (tension band wires, Kirschner wires, or sutures), 8 , 58 AC and CC reconstruction (Weaver–Dunn procedures) 59 are also options for surgical treatment. However, the literature on AC reconstruction is scarce and valid data are not available. And Weaver–Dunn procedures were used to treat chronic ACJ dislocation. 60 Therefore, our study only includes TR, HP, EB, SA, and TG of CC reconstruction.
Results of Clinical Outcome
Regarding the clinical outcome measurements, the CMS is an effective indicator to evaluate the patient's functional recovery. Previous studies have proved that all of them have a significant improvement in CMS, indicating that all techniques could have sufficient functional recovery. 61 , 62 , 63 Although there is no difference in direct comparisons of SA and HP, the results of NMA are more plausible considering that there are only two studies for direct comparisons. Our results here show that the functional recovery of HP is worse than TR, EB, and SA. This is consistent with the results of the published literature head‐to‐head meta‐analyses. Pan et al. 13 and Qi et al. 14 both reported that TR showed an advantage over HP in terms of improving the function of ACJ. Arirachakaran et al. 64 performed a meta‐analysis and concluded that SA showed better effects in shoulder functional recovery than HP. Wang et al. 15 proved that EB resulted in better functional outcomes than HP. Our study subdivides the surgical procedures of CC reconstruction and ranks them systematically via our NMA.
Efficacy in Relieving Pain
As for the postoperative shoulder pain, our results show that TR had a slightly lower VAS than HP. This conclusion has already been proved by previous head‐to‐head meta‐analyses. 13 , 14 It may be due to more soft tissue destruction during HP surgery, as well as a postoperative high‐stress concentration between the hook and the acromion.65 All of the mean VAS reported in the included literature are below 2. Therefore, these differences in pain relief outcomes are not very significant. Nevertheless, the subtle ranking among them is still distinguished via our comprehensive analysis.
Results of Postoperative Reduction
The CCD is the main imaging indicator for postoperative confirmation of reduction. Though the direct comparison of TG and TR shows that TR had a better CCD than TG, the results of MNA are more plausible for only one direct comparison was available. Our results show that there is no difference in the effect of these five surgical procedures on repositioning, which is also consistent with previous pairwise meta‐analyses. 13 , 14 , 15 , 64 Maintaining anatomic reduction does not appear to be a prerequisite for regaining proper shoulder function, and a small increase in CCD does not appear to affect overall outcomes. 66 Interestingly, even elongated reconstructed ligaments can improve clavicular stability enough to relieve symptoms and improve shoulder function. 53 , 66 , 67 Thus, complete anatomic healing may be important only for cosmetic outcomes. Overreduction, on the other hand, maybe the cause of brachial plexus compression and should not be the first goal of surgery. 68
Incidence of Complications
The risk of surgery‐related complications is considered to be an important disadvantage of all surgical procedures. Our pooled data suggest that HP has a higher rate of complications than TR. This conclusion is consistent with the findings of previous pairwise meta‐analyses. 13 , 14 , 15 , 64 Compared to previous studies, our study here further ranks the five surgical procedures and indicates that SA had the lowest complication rate while HP had the highest complication rate. Our systematic review data (Table 7) indicate that the high loss of reduction rates should be paid more attention to the groups of EB (21.94%). It should also be noted that the HP group was related to a higher ratio of erosion of the acromion and stiffness. In general, our study is more comprehensive for synthesizing all existing evidence to provide simultaneous evidence and indicates that SA showed the best clinical efficacy with the lowest complication rate (Figure 6).
Limitation and Strengths
The strength of this study was the inclusion of a large number of articles. Including 31 articles and combining the results from 1102 patients allows for an adequate assessment of the five surgical procedures to compare the clinical efficacy, imaging findings, and safety. Meanwhile, a major limitation of this systematic review is that a small proportion of the included studies are RCTs. Moreover, the complications such as the loss of reduction are not uniformly reported across all studies. Nevertheless, given the high quality of the included studies, the results of our comparison are sufficiently convincing.
Conclusion
In conclusion, considering all the criteria evaluated, SA shows better clinical effectiveness and reliable safety in the treatment of acute ACJ dislocation. Although HP is the most widely used surgical option currently, it should be carefully considered for its high incidence of complications.
Author Contributions
Yuan Yan: data curation, formal analysis, writing—original draft preparation; Mingxin Liao: writing—reviewing, formal analysis; Huahao Lai: data curation, writing—original draft preparation; Ziyang Xu: data curation; Haobin Chen: data curation; Wenhan Huang: writing—reviewing; Hui Yu: writing—reviewing and editing, project administration; Yu Zhang: writing—reviewing, supervision, funding acquisition.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Ethics Statement
Not applicable.
Acknowledgments
This study was supported by the National Key R&D Program of China (Grant No. 2021YFC24007004), research project outlay of Guangdong Provincial People's Hospital (2021YFC2400704) and Startup Fund for Scientific Research, Fujian Medical University (2019QH1221). No other relationships or activities appear to have influenced the submitted work.
Grant sources: This study was supported by the National Key R&D Program of China (Grant No. 2021YFC24007004), the research project outlay of Guangdong Provincial People's Hospital (No. 2021YFC2400704), and the Startup Fund for Scientific Research, Fujian Medical University (No. 2019QH1221).
Disclosures: Our manuscript contains original unpublished work and is not being submitted for publication elsewhere at the same time. All authors have agreed with the submission in its present forms and disclose no potential conflicts of interest. Each of the authors has read and concurs with the content in the final manuscript.
Yuan Yan is the first author; Mingxin Liao and Huahao Lai are co‐first authors.
Contributor Information
Hui Yu, Email: yuhuijm@outlook.com.
Yu Zhang, Email: luck_2001@126.com.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.
References
- 1. Willimon SC, Gaskill TR, Millett PJ. Acromioclavicular joint injuries: anatomy, diagnosis, and treatment. Phys Sportsmed. 2011;39:116–22. 10.3810/psm.2011.02.1869 [DOI] [PubMed] [Google Scholar]
- 2. Balcik BJ, Monseau AJ, Krantz W. Evaluation and treatment of sternoclavicular, clavicular, and acromioclavicular injuries. Prim Care. 2013;40:911–23, viii‐ix. 10.1016/j.pop.2013.08.008 [DOI] [PubMed] [Google Scholar]
- 3. Lau ETC, Hong CC, Poh KS, Manohara R, Ng DZ, Lim JL, et al. A relook at the reliability of Rockwood classification for acromioclavicular joint injuries. J Shoulder Elbow Surg. 2021;30:2191–6. 10.1016/j.jse.2021.01.016 [DOI] [PubMed] [Google Scholar]
- 4. Gorbaty JD, Hsu JE, Gee AO. Classifications in brief: Rockwood classification of acromioclavicular joint separations. Clin Orthop Relat Res. 2017;475:283–7. 10.1007/s11999-016-5079-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Monica J, Vredenburgh Z, Korsh J, Gatt C. Acute shoulder injuries in adults. Am Fam Physician. 2016;94:119–27. [PubMed] [Google Scholar]
- 6. Stucken C, Cohen SB. Management of acromioclavicular joint injuries. Orthop Clin North Am. 2015;46:57–66. 10.1016/j.ocl.2014.09.003 [DOI] [PubMed] [Google Scholar]
- 7. Cetinkaya E, Arıkan Y, Beng K, Mutlu H, Yalçınkaya M, Üzümcügil O. Bosworth and modified Phemister techniques revisited. A comparison of intraarticular vs extraarticular fixation methods in the treatment of acute Rockwood type III acromioclavicular dislocations. Acta Orthop Traumatol Turc. 2017;51:455–8. 10.1016/j.aott.2017.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu T, Bao FL, Jiang T, Ji GW, Li JM, Jerosch J. Acromioclavicular joint separation: repair through suture anchors for Coracoclavicular ligament and nonabsorbable suture fixation for acromioclavicular joint. Orthop Surg. 2020;12:1362–71. 10.1111/os.12771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hessmann M, Gotzen L, Gehling H. Acromioclavicular reconstruction augmented with polydioxanonsulphate bands. Surgical technique and results. Am J Sports Med. 1995;23:552–6. 10.1177/036354659502300506 [DOI] [PubMed] [Google Scholar]
- 10. Morrison DS, Lemos MJ, Acromioclavicular separation . Reconstruction using synthetic loop augmentation. Am J Sports Med. 1995;23:105–10. 10.1177/036354659502300118 [DOI] [PubMed] [Google Scholar]
- 11. Sim E, Schwarz N, Höcker K, Berzlanovich A. Repair of complete acromioclavicular separations using the acromioclavicular‐hook plate. Clin Orthop Relat Res. 1995;134–42. [PubMed] [Google Scholar]
- 12. Breslow MJ, Jazrawi LM, Bernstein AD, Kummer FJ, Rokito AS. Treatment of acromioclavicular joint separation: suture or suture anchors? J Shoulder Elbow Surg. 2002;11:225–9. 10.1067/mse.2002.123904 [DOI] [PubMed] [Google Scholar]
- 13. Pan X, Lv RY, Lv MG, Zhang DG. TightRope vs clavicular hook plate for Rockwood III‐V acromioclavicular dislocations: a meta‐analysis. Orthop Surg. 2020;12:1045–52. 10.1111/os.12724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Qi W, Xu Y, Yan Z, Zhan J, Lin J, Pan X, et al. The tight‐rope technique versus clavicular hook plate for treatment of acute acromioclavicular joint dislocation: a systematic review and meta‐analysis. J Investig Surg. 2021;34:20–9. 10.1080/08941939.2019.1593558 [DOI] [PubMed] [Google Scholar]
- 15. Wang C, Meng JH, Zhang YW, Shi MM. Suture button versus hook plate for acute unstable acromioclavicular joint dislocation: a meta‐analysis. Am J Sports Med. 2020;48:1023–30. 10.1177/0363546519858745 [DOI] [PubMed] [Google Scholar]
- 16. Arirachakaran A, Boonard M, Piyapittayanun P, Phiphobmongkol V, Chaijenkij K, Kongtharvonskul J. Comparison of surgical outcomes between fixation with hook plate and loop suspensory fixation for acute unstable acromioclavicular joint dislocation: a systematic review and meta‐analysis. Eur J Orthop Surg Traumatol. 2016;26:565–74. 10.1007/s00590-016-1797-4 [DOI] [PubMed] [Google Scholar]
- 17. Jansen JP, Crawford B, Bergman G, Stam W. Bayesian meta‐analysis of multiple treatment comparisons: an introduction to mixed treatment comparisons. Value Health. 2008;11:956–64. 10.1111/j.1524-4733.2008.00347.x [DOI] [PubMed] [Google Scholar]
- 18. Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928–8. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta‐analysis of observational studies in epidemiology: a proposal for reporting. Meta‐analysis of observational studies in epidemiology (MOOSE) group. Jama. 2000;283:2008–12. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 20. Jonas DE, Wilkins TM, Bangdiwala S, Bann CM, Morgan LC, Thaler KJ, et al. AHRQ methods for effective health care. Findings of Bayesian mixed treatment comparison meta‐analyses: comparison and exploration using real‐world trial data and simulation. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013. [PubMed] [Google Scholar]
- 21. Brooks PS, Andrew G. General methods for monitoring convergence of iterative simulations. J Comput Graphical Stat. 1998;7:131–7. [Google Scholar]
- 22. Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta‐analysis in STATA. PloS One. 2013;8:e76654. 10.1371/journal.pone.0076654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta‐analysis. Stat Med. 2010;29:932–44. 10.1002/sim.3767 [DOI] [PubMed] [Google Scholar]
- 24. Athar MS, Ashwood N, Arealis G, Hamlet M, Salt E. Acromioclavicular joint disruptions: a comparison of two surgical approaches ‘hook’ and ‘rope’. J Orthop Surg (Hong Kong). 2018;26:2309499017749984. 10.1177/2309499017749984 [DOI] [PubMed] [Google Scholar]
- 25. Bin Abd Razak HR, Yeo EN, Yeo W, Lie TD. Short‐term outcomes of arthroscopic TightRope(I) fixation are better than hook plate fixation in acute unstable acromioclavicular joint dislocations. Eur J Orthop Surg Traumatol. 2018;28:869–75. 10.1007/s00590-017-2095-5 [DOI] [PubMed] [Google Scholar]
- 26. Cai L, Wang T, Lu D, Hu W, Hong J, Chen H. Comparison of the tight rope technique and clavicular hook plate for the treatment of Rockwood type III acromioclavicular joint dislocation. J Invest Surg. 2018;31:226–33. 10.1080/08941939.2017.1305022 [DOI] [PubMed] [Google Scholar]
- 27. Eschler A, Gradl G, Gierer P, Mittlmeier T, Beck M. Hook plate fixation for acromioclavicular joint separations restores coracoclavicular distance more accurately than PDS augmentation, however presents with a high rate of acromial osteolysis. Arch Orthop Trauma Surg. 2012;132:33–9. 10.1007/s00402-011-1399-x [DOI] [PubMed] [Google Scholar]
- 28. Fosser M, Camporese A. Operative treatment of acute acromioclavicular joint dislocations graded Rockwood III–V: a retrospective and comparative study between three different surgical techniques. Acta Biomed. 2021;92:e2021325. 10.23750/abm.v92i5.10678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gao YS, Zhang YL, Ai ZS, Sun YQ, Zhang CQ, Zhang W. Transarticular fixation by hook plate versus coracoclavicular stabilization by single multistrand titanium cable for acute Rockwood grade‐V acromioclavicular joint dislocation: a case‐control study. BMC Musculoskelet Disord. 2015;16:360. 10.1186/s12891-015-0820-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gultac E, Can FI, Kilinc CY, Aydogmus H, Topsakal FE, Acan AE, et al. Comparison of the radiological and functional results of tight rope and clavicular hook plate technique in the treatment of acute acromioclavicular joint dislocation. J Invest Surg. 2022;35:693–6. 10.1080/08941939.2021.1897196 [DOI] [PubMed] [Google Scholar]
- 31. Huang YC, Yang SW, Chen CY, Lin KC, Renn JH. Single coracoclavicular suture fixation with Mersilene tape versus hook plate in the treatment of acute type V acromioclavicular dislocation: a retrospective analysis. J Orthop Surg Res. 2018;13:110. 10.1186/s13018-018-0831-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jensen G, Katthagen JC, Alvarado LE, Lill H, Voigt C. Has the arthroscopically assisted reduction of acute AC joint separations with the double tight‐rope technique advantages over the clavicular hook plate fixation? Knee Surg Sports Traumatol Arthrosc. 2014;22:422–30. 10.1007/s00167-012-2270-5 [DOI] [PubMed] [Google Scholar]
- 33. Lazarski A, Sarzynska S, Struzik S, Jedral T, Legosz P, Maldyk P. Results of treatment of type 3 acromioclavicular joint dislocation with three methods. Ortop Traumatol Rehabil. 2019;21:167–79. 10.5604/01.3001.0013.2921 [DOI] [PubMed] [Google Scholar]
- 34. Liu S, Li C, Song Z, Bai X, Wu H. Comparison of open reduction and fixation with hook plate and modified closed reduction and fixation with tightrope loop plate for treatment of Rockwood type III acromioclavicular joint dislocation. BMC Musculoskelet Disord. 2022;23:301. 10.1186/s12891-022-05261-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Liu Y, Zhang X, Yu Y, Ding W, Gao Y, Wang Y, et al. Suture augmentation of acromioclavicular and coracoclavicular ligament reconstruction for acute acromioclavicular dislocation. Medicine (Baltimore). 2021;100:e27007. 10.1097/MD.0000000000027007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Madi S, Pandey V, Murali S, Acharya K. Clinical and radiological outcome of acute high‐grade acromioclavicular joint dislocation: a retrospective cohort study on hook plate versus arthroscopic assisted single coracoclavicular tunnel with DogBone button dual FiberTI(R) construct. J Clin Orthop Trauma. 2022;27:101825. 10.1016/j.jcot.2022.101825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Martetschlager F, Horan MP, Warth RJ, Millett PJ. Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2013;41:2896–903. 10.1177/0363546513502459 [DOI] [PubMed] [Google Scholar]
- 38. Nascimento AT, Claudio GK. Functional and radiological evaluation of acute acromioclavicular dislocation treated with anchors without eyelet: comparison with other techniques. Rev Bras Ortop. 2016;51:561–8. 10.1016/j.rboe.2016.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Natera‐Cisneros L, Sarasquete‐Reiriz J, Escola‐Benet A, Rodriguez‐Miralles J. Acute high‐grade acromioclavicular joint injuries treatment: arthroscopic non‐rigid coracoclavicular fixation provides better quality of life outcomes than hook plate ORIF. Orthop Traumatol Surg Res. 2016;102:31–9. 10.1016/j.otsr.2015.10.007 [DOI] [PubMed] [Google Scholar]
- 40. Nie S, Lan M. Comparison of clinical efficacy between arthroscopically assisted tight‐rope technique and clavicular hook plate fixation in treating acute high‐grade acromioclavicular joint separations. J Orthop Surg (Hong Kong). 2021;29:23094990211010562. 10.1177/23094990211010562 [DOI] [PubMed] [Google Scholar]
- 41. Shen G, Sun S, Tang C, Xie Y, Li L, Xu W, et al. Comparison of the TightRope system versus hook plate in acute acromioclavicular joint dislocations: a retrospective analysis. Sci Rep. 2021;11:11397. 10.1038/s41598-021-90989-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Stein T, Muller D, Blank M, Reinig Y, Saier T, Hoffmann R, et al. Stabilization of acute high‐grade acromioclavicular joint separation: a prospective assessment of the clavicular hook plate versus the double double‐button suture procedure. Am J Sports Med. 2018;46:2725–34. 10.1177/0363546518788355 [DOI] [PubMed] [Google Scholar]
- 43. Taleb H, Afshar A, Shariyate MJ, Tabrizi A. Comparison of short‐term clinical outcomes of hook plate and continuous loop double Endobutton fixations in acute acromioclavicular joint dislocation. Arch Bone Joint Surg. 2019;7:545–50. [PMC free article] [PubMed] [Google Scholar]
- 44. Topal M, Kose A. Surgical management of Rockwood type 3 acromioclavicular joint injuries: a retrospective comparison of outcomes of suture anchor fixation and double‐button fixation techniques. Medicine (Baltimore). 2020;99:e20312. 10.1097/MD.0000000000020312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Unal OK, Dagtas MZ. Comparison of the results of hook plate and Endo‐button used in the surgical treatment of acromioclavicular joint separation. Cureus. 2020;12:e11987. 10.7759/cureus.11987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Vulliet P, Le Hanneur M, Cladiere V, Loriaut P, Boyer P. A comparison between two double‐button endoscopically assisted surgical techniques for the treatment acute acromioclavicular dislocations. Musculoskelet Surg. 2018;102:73–9. 10.1007/s12306-017-0501-0 [DOI] [PubMed] [Google Scholar]
- 47. Wang G, Xie R, Mao T, Xing S. Treatment of AC dislocation by reconstructing CC and AC ligaments with allogenic tendons compared with hook plates. J Orthop Surg Res. 2018;13:175. 10.1186/s13018-018-0879-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wang YC, Yong MA, Wei‐zhong YU, Wang H. Surgical treatment of acute Rockwood III acromioclavicular dislocations‐comparative study between two flip‐button techniques. Sci Rep. 2020;10:4447. 10.1038/s41598-020-61488-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Yoo YS, Khil EK, Im W, Jeong JY. Comparison of hook plate fixation versus arthroscopic Coracoclavicular fixation using multiple soft anchor knots for the treatment of acute high‐grade acromioclavicular joint dislocations. Art Ther. 2021;37:1414–23. 10.1016/j.arthro.2020.12.189 [DOI] [PubMed] [Google Scholar]
- 50. Yoon JP, Lee BJ, Nam SJ, Chung SW, Jeong WJ, Min WK, et al. Comparison of results between hook plate fixation and ligament reconstruction for acute unstable acromioclavicular joint dislocation. Clin Orthop Surg. 2015;7:97–103. 10.4055/cios.2015.7.1.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Yu P, Zhang Y, Ye T, Liu J, Zhuang C, Wang L. Clinical and radiological outcomes of acute Rookwood type IIIB acromioclavicular joint dislocation: mini‐open tightrope technique versus hook plate. Injury. 2023;54:S63–9. 10.1016/j.injury.2022.02.019 [DOI] [PubMed] [Google Scholar]
- 52. Zhang S, Zhang H, Wang J, Ma X, Gu S. Triple‐Endobutton and clavicular hook: a propensity score matching analysis. Open Med (Wars). 2021;16:1328–35. 10.1515/med-2021-0339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Vascellari A, Schiavetti S, Battistella G, Rebuzzi E, Coletti N. Clinical and radiological results after coracoclavicular ligament reconstruction for type III acromioclavicular joint dislocation using three different techniques. A retrospective study. Joints. 2015;3:54–61. 10.11138/jts/2015.3.2.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Zhang J, Ying Z, Wang Y. Surgery for acromioclavicular dislocation: factors affecting functional recovery. Am Surg. 2017;83:1427–32. 10.1177/000313481708301231 [DOI] [PubMed] [Google Scholar]
- 55. Tavakoli Darestani R, Ghaffari A, Hosseinpour M. Acromioclavicular joint fixation using an acroplate combined with a coracoclavicular screw. Arch Trauma Res. 2013;2:36–9. 10.5812/atr.10338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zheng J, Chen J, Chen L, Ni Y, Lin Z. A novel hybrid fixation (coracoclavicular screw supplemented with K‐wire) for the treatment of acute acromioclavicular joint dislocation: a prospective study. Int J Surg. 2018;59:61–6. 10.1016/j.ijsu.2018.09.019 [DOI] [PubMed] [Google Scholar]
- 57. Chen YT, Wu KT, Jhan SW, Hsu SL, Liu HC, Wang CJ, et al. Is coracoclavicular reconstruction necessary in hook plate fixation for acute unstable acromioclavicular dislocation? BMC Musculoskelet Disord. 2021;22:127. 10.1186/s12891-021-03978-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Biz C, Berizzi A, Cappellari A, Crimì A, Tamburin S, Iacobellis C. The treatment of acute Rockwood type III acromio‐clavicular joint dislocations by two different surgical techniques. Acta Bio‐Med: Atenei Parmensis. 2015;86:251–9. [PubMed] [Google Scholar]
- 59. Costic RS, Labriola JE, Rodosky MW, Debski RE. Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med. 2004;32:1929–36. 10.1177/0363546504264637 [DOI] [PubMed] [Google Scholar]
- 60. Chang HM, Wang CH, Hsu KL, Kuan FC, Chen Y, Su WR, et al. Does weaver‐Dunn procedure have a role in chronic acromioclavicular dislocations? A meta‐analysis. J Orthop Surg Res. 2022;17:95. 10.1186/s13018-022-02995-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Nolte PC, Lacheta L, Dekker TJ, Elrick BP, Millett PJ. Optimal Management of Acromioclavicular Dislocation: current perspectives. Orthop Res Rev. 2020;12:27–44. 10.2147/orr.S218991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Bontempo NA, Mazzocca AD. Biomechanics and treatment of acromioclavicular and sternoclavicular joint injuries. Br J Sports Med. 2010;44:361–9. 10.1136/bjsm.2009.059295 [DOI] [PubMed] [Google Scholar]
- 63. Cisneros LN, Reiriz JS. Management of acute unstable acromioclavicular joint injuries. Eur J Orthop Surg Traumatol. 2016;26:817–30. 10.1007/s00590-016-1836-1 [DOI] [PubMed] [Google Scholar]
- 64. Arirachakaran A, Boonard M, Piyapittayanun P, Kanchanatawan W, Chaijenkij K, Prommahachai A, et al. Post‐operative outcomes and complications of suspensory loop fixation device versus hook plate in acute unstable acromioclavicular joint dislocation: a systematic review and meta‐analysis. J Orthop Traumatol. 2017;18:293–304. 10.1007/s10195-017-0451-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Struhl S, Wolfson TS. Continuous loop double Endobutton reconstruction for acromioclavicular joint dislocation. Am J Sports Med. 2015;43:2437–44. 10.1177/0363546515596409 [DOI] [PubMed] [Google Scholar]
- 66. Boström Windhamre HA, von Heideken JP, Une‐Larsson VE, Ekelund AL. Surgical treatment of chronic acromioclavicular dislocations: a comparative study of weaver‐Dunn augmented with PDS‐braid or hook plate. J Shoulder Elbow Surg. 2010;19:1040–8. 10.1016/j.jse.2010.02.006 [DOI] [PubMed] [Google Scholar]
- 67. Frank RM, Cotter EJ, Leroux TS, Romeo AA. Acromioclavicular joint injuries: evidence‐based treatment. J Am Acad Orthop Surg. 2019;27:e775–88. 10.5435/jaaos-d-17-00105 [DOI] [PubMed] [Google Scholar]
- 68. Beitzel K, Cote MP, Apostolakos J, Solovyova O, Judson CH, Ziegler CG, et al. Current concepts in the treatment of acromioclavicular joint dislocations. Arthrosc: J Arthrosc Relat Surg. 2013;29:387–97. 10.1016/j.arthro.2012.11.023 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.


