Abstract
Objective
To present a systematic review of randomized controlled trials which summarizes the effects of community-based resistance, balance, and multi-component exercise interventions on the parameters of functional ability (e.g., lower extremities muscle strength, balance performance and mobility).
Methods
This PROSPERO-registered systematic review (registration no. CRD42023434808) followed the PRISMA guidelines. Literature search was conducted in Cochrane, Embase, Ovid Medline, PEDro, Pubmed, Science Direct, Scopus and Web of Science. We included RCTs that investigated the following interventions: lower extremity strengthening, balance and multi-component exercise interventions on ambulatory community-dwelling adults aged ≥65 years.
Results
Lower extremity strengthening exercises revealed significant effects on the strength of lower extremity, balance outcomes and mobility. Balance exercises reduce the rate of injurious falls, improve static, dynamic and reactive balance, lower extremity strength as well as mobility. Multi-component exercise training reduces medically-attended injurious falls and fallers, incidence of falls, fall-related emergency department visits as well as improves mobility, balance, and lower extremity strength.
Conclusion
Physical exercises are effective in improving the components of balance, lower extremity strength, mobility, and reducing falls and fall-related injuries. Further research on fall prevention in low-income countries as well as for older adults in vulnerable context is needed.
Keywords: fall, older adults, exercise, strength, balance, multi-component
1. Introduction
One-third of older adults aged 65 years or over fall each year, and 50% of them fall repeatedly (1). According to the World Health Organization (WHO) (2), falls are the second leading cause of unintentional injury deaths globally, and the literature shows that 40% of community-dwelling older adults who are over 65 years experience fall accidents annually (3). In Europe, every year approximately 36,000 older adults (65 years and above) die from falls (data 2010–2012). Of these, 88% of cases are related to people aged 75 years or older and 59% of cases are related to women (4).
Physical inactivity and deficits in functional ability (e.g., reduced lower limbs muscular strength and impaired balance ability) have been identified as independent contributors to falls and fall-related injuries (e.g., head injuries and hip fractures) among older adults (5–8). Even though they are critical risk factors for older adults, they are modifiable and preventable through exercises (7, 9, 10). Falls also have economic burdens such as medications, hospital admissions, and extended rehabilitation services (2, 11).
Exercise training is broadly recognized as an appropriate intervention strategy for improving functional performance in older adults, reducing the aforementioned risk factors, and consequently minimizing the risk of falling (12–14). Additionally, the reduction of physical inactivity has been shown to have positive economic impacts on national, social, and individual levels (15).
Cognitive decline also occurs during normal aging (16), which is considered a significant factor in increased functional dependence and fewer activities of daily living among older adults (17). According to previous studies, older adults who exercised three times a week for 6 months showed improvements in global and executive cognitive functions as well as a general deceleration of the aging process (18, 19).
Accordingly, the WHO recommends that older adults aged over 65 years adopt an active lifestyle that ensures the performance of physical activity of moderate intensity for a minimum of 150 min weekly (20, 21), as well as engage in fall prevention exercises (22). This moderate amount of physical activity has been shown to reduce the risk factors associated with falls by up to 50% by reducing functional limitation in older persons, and eventually reducing the risk of falls (13).
Several studies (23–28) have concluded that strength, balance, and aerobic-based training is effective in reducing falls among older adults in general and up to 50% in community-dwelling older adults specifically, with gains that may last as the training is maintained (29). In their clinical guideline for the prevention of falls, the American Geriatrics Society and British Geriatrics Society Clinical Practice recommend that the prevention of fall risk factors should include gait training, resistance, and balance exercises (30).
Studies on resistance exercises reported their effectiveness in mitigating reduced muscle strength, and that these types of exercises are considered an essential element of a multi-component exercise fall prevention strategy (31, 32). Furthermore, there is a considerable body of literature on balance exercises and their effectiveness in reducing the risk of falling among community-dwelling older adults (23, 33–36).
Previous systematic reviews and meta-analyses explored the effects of exercise on fall prevention among older people. However, these reviews and meta-analyses were conducted in a younger age group (60 years and over) (23, 27) compared with our present review and in participants with Parkinson’s disease, stroke, and cognitive impairment (26) who had mixed living settings (living in the community, nursing homes, and higher dependency places of residence) (35, 37). They concluded that exercises as a stand-alone intervention can significantly reduce the rate of falls (23, 26, 27, 35, 37) and the risk of falling (23, 27).
To the best of our knowledge, despite the current interest in the topic, there is a lack of systematic reviews on fall prevention strategies that address the effectiveness of exercise training, specifically on ambulatory community-dwelling older adults aged 65 years or older. Therefore, our current review aims to present a systematic review of randomized controlled trials (RCTs) that summarizes the effects of resistance, balance, and multi-component exercise interventions. These interventions consist mainly of combined resistance and balance exercises in addition to one or more types of exercises, namely, aerobic, walking, and weight-bearing, on the parameters of functional ability (e.g., lower extremities muscle strength, balance performance, and mobility), which accordingly prevent falls in ambulatory community-dwelling adults aged 65 years and over.
2. Methods
The current systematic review is presented in accordance with the guidelines of PRISMA 2020 (Preferred Reporting Items for Systematic Reviews and Meta-Analyses literature search extension) (38). The review was registered on PROSPERO with the following registration no. CRD42023434808.
2.1. Data sources and search strategies
Two consecutive searches were conducted by two researchers (MS and ZN) independently. The initial search was limited to studies in English published from 1 January 2015 to 30 December 2020, then the search was conducted again on 7 August 2021 for publications published from 1 January 2021 to 7 August 2021 in the following electronic databases: Cochrane Central Register of Controlled Trials, Embase, Ovid Medline, PEDro, Pubmed, Science Direct, Scopus, and Web of Science. The search was supplemented by a manual review of reference lists from included primary studies and review articles to find additional studies on the subject (Table 1).
Table 1.
Search strategy.
| Database | Search strategy |
|---|---|
| Cochrane Library, Embase, Pubmed, Science Direct, Scopus, and Web of Science | ((senior* OR elder* OR old) AND (exercis* OR train*) AND (effect* OR benefit*) AND (lower limb* OR lower extremit*) AND (fall*)) |
| PEDro | Abstract & Title: fall* exercis* Subdiscipline: gerontology Method: clinical trial/practice guideline Published Since: 2015 When Searching: Match all search terms (AND) |
| Ovid Medline |
|
All research papers were first retrieved, and Zotero 6.0.26 (a reference manager created at the Roy Rosenzweig Center for History and New Media at George Mason University, Virginia, United States) was utilized to remove duplicates. Next, titles and abstracts were screened independently by two researchers (MS and ZN), and finally, the full texts of the remaining studies were assessed to determine eligibility. Disagreements between the two researchers were resolved through discussion and mutual consent, or by a third assessor (MH). After the abstract and full-text analysis, the Cohen’s Kappa-coefficient (K score) was calculated to weigh the level of agreement between the two reviewers.
2.2. Eligibility criteria
Based on PICOTS, studies were included if they were written in English, were RCTs on community-dwelling adults aged ≥65 years, and included the following interventions: lower limb strengthening exercises, balance exercises, and multi-component exercise interventions that consist of resistance and balance exercises in addition to one or more types of exercises, namely, aerobic, walking, and weight-bearing. Studies were excluded if (I) they involved residents of nursing homes and inpatients, (II) involved participants with a diagnosis of multiple sclerosis, cancer, Parkinson’s or Alzheimer’s disease, stroke, recent fractures, vision or cognitive impairments, or other chronic conditions associated with aging, (III) they were on non-human participants, (IV) they were based on interventions of video games, web-based programs, Tai Chi, Otago exercise program, multifactorial components that combine exercises and non-exercise interventions, yoga, dance therapy, or water-based exercise program, and (V) were non-RCTs, cohort studies, cross-sectional studies, reviews, conference abstract/papers, surveys, opinion pieces, commentaries, books, periodicals, editorials, case studies, non-peer-reviewed articles, masters dissertations, and doctoral theses.
2.3. Data extraction
Two reviewers independently extracted the following data from each study: author, publication year, study title, aim and design, number and demographic data of participants, the type of intervention such as lower limb strengthening exercise training, balance exercise training, and multi-component exercise training, duration, frequency, and settings of intervention, equipment used, outcome measures, results, and limitations.
2.4. Risk of bias assessment
One review author (MS) carried out the risk of bias assessment using Cochrane’s Risk of bias tool among six domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective reporting (38).
3. Results
3.1. Study selection
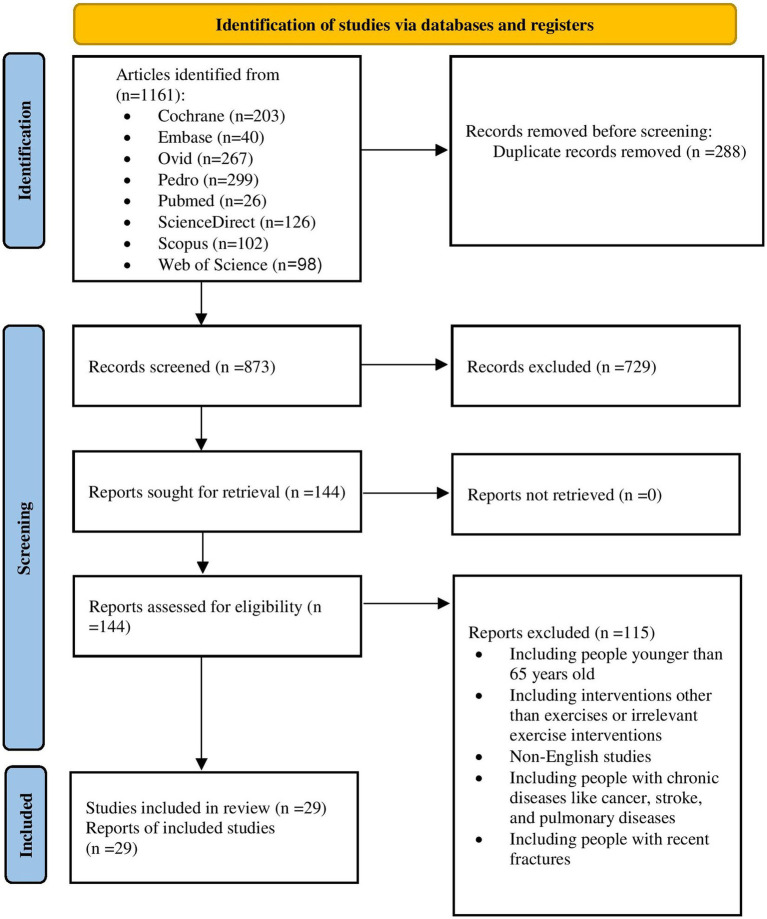
From 1,161 yielded studies, 288 duplicates were excluded. Then, following title and abstract screening, another 729 were excluded. The remaining studies were assessed against the inclusion and exclusion criteria and 29 studies in total were eligible to be included in the systematic review (Figure 1). To measure the inter-rater reliability between the two reviewers, a K score was calculated at abstract level (0.82) and at full-text level (0.86), which showed a high level of agreement. The included studies involved 4,330 participants, of which 4,121 adhered to the end of the studies and were analyzed for the outcome measures. The participants’ average age ranged from 66.4 to 82.4 years, and all were community-dwelling older adults. The 29 included studies were only RCTs.
Figure 1.
Flow of the studies screened.
3.2. Setting and training equipment
Interventions were mainly conducted in gyms, exercise halls, community facilities (5, 32, 39–41), combined gyms, home-based locations (42–45), and laboratories (46, 47). Some studies did not report the intervention setting, however, a gym/community setting was likely from the description of interventions (48–65).
A variety of training equipment was used: resistance training machines (32, 45, 46, 49, 52, 53, 55, 61), recumbent trainer, seated stationary cycle ergometer, treadmills, climber, bike recline (32, 47, 49, 52), weighted equipment such as cuff and vest weights (5, 32, 39–41, 45, 50, 55, 63, 65), elastic bands/tubing (39–41, 53, 56, 58, 59), free weights (45, 52), body weight (5, 44, 48), balls (39, 42, 44, 50, 51), step-boards (5, 39, 45), chairs (5, 50), equipment used for balance training such as tripping boards, slipping tiles, balance foams, wedged soft mat, soft pads, non-inverted BOSU® balls, inverted BOSU® balls, balance cushions, balance beams, semicircular blocks, Posturomed®, wobble boards, and inflatable discs (39–41, 43, 48, 52, 53, 57). One study reported that they used small, low-cost equipment as well (e.g., towels and bottles) (44), whereas five studies did not clearly report any equipment used, however, they could have merely used body weight for exercises (54, 60, 62, 64, 65).
3.3. Dosage of exercise programs
The duration of exercise interventions ranged from 15 min (44) to 90 min (53, 64, 65) per session, the frequency of interventions ranged from once a day (43) to five times a week (62), and the duration of the exercise programs ranged from 1 week (47, 57) to 2 years (5, 42).
3.4. Results according to intervention
3.4.1. Lower limb strengthening exercise training
Seven of the included studies contained lower limb strengthening exercises as the only intervention or one of a multi-component intervention. They used different modalities and showed significant improvements in lower extremities strength (using dynamometer, five times sit to stand test, and chair rise test), balance (activities specific balance confidence (ABC) scale, berg balance scale, one leg standing test, Y-balance test, and functional reach test), mobility (6-minute walk test, timed up and go test (TUGT), and 30-second chair stand test), days survived without a fall or near-fall, gait (functional gait assessment) (32, 46, 52–54, 56, 59). One study did not show significant change in static balance (single leg stance assessment with eyes closed on the dominant and single leg stance assessment with eyes closed on the non-dominant) or eccentric strength (maximal eccentric strength) (46). Another study did not show significant improvement in TUGT, except when exercise was combined with neuromuscular electrical stimulation (54). Table 2 shows a complete summary of the key data extracted from the studies on strengthening exercise interventions.
Table 2.
A complete summary of the key data extracted from studies of strengthening exercise intervention.
| References | Participants | Interventions modality | Duration | Outcomes | Summary of results |
|---|---|---|---|---|---|
| Eckardt (52) | 83 (48 women, 35 men) Age 65–80 |
|
10 weeks |
|
|
| Hamed et al. (53) | 63 (women and men) Age 65–80 |
|
14 weeks |
|
- Significant improvements for MoS and knee and ankle momentum in muscle strength group -Significant improvement for LoS, MoS and ankle momentum muscle strength group |
| Jang and Park (54) | 30 (women only) Age ≥ 65 |
|
4 weeks |
|
- Significant differences in STST, OLST and YBT - No significant difference with TUGT |
| Johnson et al. (46) | 30 (16 women, 14 men) Age 68.2 ± 3.7 |
|
8 weeks |
|
- Significant improvement in for 30SCST, BBS, FGA and TUGT - No significant improvement in SLS-EC:D, SLS-EC:ND and MES |
| LaStayo et al. (32) | 134 (47 men, 87 women) Age ≥ 65 |
|
3 months |
|
-No significant difference between RENEW and TRAD in 6 MWT -No significant difference between RENEW and TRAD in ABC Scale -No significant difference between RENEW and TRAD in leg extensor muscle power -No significant difference between RENEW and TRAD in the number of days survived without fall |
| Lee and Lee (56) | 30 (women only) Age ≥ 65 |
|
4 weeks |
|
- Significant difference in OLST and FRT - No significant difference between the two groups |
| Pourtaghi et al. (59) | 70 (48 women, 22 men) Age ≥ 65 |
|
6 weeks |
|
- Significant ↑ in both lower extremities strength |
30SCST, 30-Second Chair Stand Test; 6 MWT, 6-Minute Walk Test; ABC, Activities Specific Balance Confidence; BBS, Berg Balance Scale; BoS, Base of support; CRT, chair Rise Test; F-URT, Free-weight Unstable Resistance Training; FGA, Functional Gait Assessment; FRT, Functional Reach Test; LoS, Limits of Stability; M-SRT, Machine-based Stable Resistance Training; M-URT, Machine-based Unstable Resistance Training; MES, Maximal Eccentric Strength; MoS, Margin of Stability; OLST, One Leg Standing Test; PRT, Push and Release Test; SLS-EC,D, Single Leg Stance assessment with Eyes Closed on the Dominant; SLS-EC,ND, Single Leg Stance assessment with Eyes Closed on the Non-Dominant; STST, Sit To Stand Test; TUGT, Timed Up and Go Test; YBT, Y-Balance Test.
3.4.2. Balance exercise training
Ten studies compared balance exercise interventions to non-active controls (usual daily activities and social programs), and those that used different balance interventions methods showed significant improvements in muscle strength [chair standing test (CST), four square step test (FSST), and 2-min step test (2MST)], balance [single leg stance test (SLST), one leg standing test, tandem stance test, ABC scale, modified Clinical Test of Sensory Organization and Balance, local dynamic stability, and balance recovery], gait and mobility (TUGT, 6-min walk test, five times chair stand test, and functional reach test), lower rate of falls, reduction in the rate ratio of all falls, and slip falls (42, 43, 47, 50, 53, 57, 60, 62, 64, 65).
One RCT compared an enhanced balance program with a standard balance program on sit-to-stand test repetitions. The study revealed no significant difference between the two groups in sit-to-stand test repetitions. There was a statistically significant improvement in sit-to-stand test repetitions from pre- to post-intervention for both standard balance and enhanced balance exercise groups (39).
A study in this review scrutinized the effects of an 8-week square-step exercise in older fallers. The composite balance score as a marker of postural control was significantly higher in the square-step exercise group compared with the vestibular exercise group. Adaptation test was utilized to assess the ability to control motor reactions after an unexpected change in position (dynamic balance). Square step exercise did not show significant results compared with vestibular exercise neither in toes up nor in toes down (48). Table 3 shows a complete summary of the key data extracted from the studies on balance exercise interventions.
Table 3.
A complete summary of the key data extracted from studies of balance exercise intervention.
| References | Participants | Interventions modality | Duration | Outcomes | Summary of results |
|---|---|---|---|---|---|
| Arghavani et al. (50) | 60 (men only) Age 65–80 |
|
8 weeks |
|
- Significant ↑ in Balance confidence in both training programs |
| Arnold et al. (39) | 28 (women and men) Age ≥ 65 |
|
9 weeks |
|
- Significant improvement in STST for both interventions - No significant improvement in MoS for both interventions |
| El-Khoury et al. (42) | 706 (women only) Age 75–85 |
|
2 years |
|
- Significant improvements in all balance and gait tests at one and 2 years |
| Hamed et al. (53) | 63 (women and men) Age 65–80 |
|
14 weeks |
|
- Significant improvements for MoS and knee and ankle momentum in muscle strength group -Significant improvement for LoS, MoS and ankle momentum muscle strength group |
| Hirase et al. (43) | 93 (65 women, 28 men) Age > 65 |
|
4 months |
|
- Significant ↑time (Improvement) in OLST on foam rubber, but not significant in stable surfaces - Significant ↓time (Improvement) in CST and TUGT for both intervention groups - Significant ↑time (Improvement) in TST for both intervention groups |
| Kocaman et al. (48) | 42 (women and men) Age > 65 |
|
8 weeks |
|
- Significant improvements in composite balance score and ADT for both interventions |
| Okubo et al. (57) | 44 (25 women, 19 men) Age 65–90 |
|
1 week |
|
- Significant ↓ in all falls and slip falls, but not significant in trip falls |
| Rieger et al. (47) | 30 (women and men) Age > 65 |
|
1 week | Local divergence exponent for anterior–posterior: local dynamic stability Local divergence exponent for medio-lateral: local dynamic stability |
- Significant differences for all outcome measures in the intervention group |
| Sadeghi et al. (60) | 64 (men only) Age ≥ 65 |
|
8 weeks |
|
- No significant difference in muscle strength - Significant ↑ time (Improvement) in SLST -Significant ↑ time (Improvement) in TST - Significant ↓time (Improvement) in TUGT (improvement) - Significant ↓ time (Improvement) in 10mWT |
| Sitthiracha et al. (62) | 60 (53 women, 7 men) Age 65 to 75 |
|
8 weeks |
|
- Significant ↓ time (Improvement) in TUGT - No significant improvement in OLST - Significant ↓ time (Improvement) in FTSST - Significant ↑ steps (Improvement) in 2MST |
| Zhao et al. (64) | 61 (42 women, 19 men) Age 65–74 |
|
16 weeks |
|
- Significant improvement in FRT and m-CTSIB |
| Zhao et al. (65) | 61 (42 women, 19 men) Age 65–74 |
|
16 weeks |
|
- Significant ↑ repetition (Improvement) in 30SCST - Significant ↓ time (Improvement) in UG |
5TSST, Five Times Sit to Stand Test; 10mWT, 10-Meter Walk Test; 30SCST, 30-Second Chair Stand Test; 6 MWT, 6-Minute Walk Test; ABC, Activities Specific Balance Confidence; ADT, Adaptation Test; BoS, Base of support; CST, Chair Standing Test; FRT, Functional Reach Test; LoS, Limits of Stability; m-CTSIB, Modified Clinical Test of Sensory Organization and Balance; MoS, Margin of Stability; OLST, One Leg Standing Test; SLST, Single Leg Stance Test; STST, Sit To Stand Test; TST, Tandem Stance Tet; TUGT, Timed Up and Go Test, UG, 8 ft Up-and-Go Test.
3.4.3. Multi-component exercise training
Seven studies that compared multi-component exercise interventions to non-active controls showed significant improvements in lower extremities strength (isometric leg extension strength, CST, and knee extensors strength), static balance (backward walking, Romberg test, and postural sway), proactive balance (functional reach test), reactive balance, and mobility, as well as showed lower medically-attended injurious falls and a decrease in the frequency of fallers (5, 44, 45, 49, 51, 55, 58).
An RCT by Li and colleagues aimed to assess the effectiveness of multimodal exercise (MME) training consisting of balance, aerobics, strength, and flexibility activities relative to stretching exercises (SE) in reducing the incidence of falls in older adults. MME showed a significantly lower incidence of falls (16 per 100 person-months) compared with SE (27 per 100 person-months). For total walking duration in instrumented-TUGT and short physical performance battery, which measured repeated chair stands, three increasingly challenging standing balance tasks, and a 4-m speed walk, the MME group performed significantly better than those in the SE group (40).
Another RCT aimed to assess the longer-term effectiveness of multimodal exercise (MME) training consisting of balance, aerobics, strength, and flexibility activities relative to therapeutic Tai Ji Quan: Moving for Better Balance (TJQMBB) and SE in decreasing injurious falls among older adults at high risk of falling. For moderate and serious injurious falls, MME demonstrated significantly lower incidence compared with SE (41). One RCT examined the effect of an 8-week-long two-exercise routine: 1. Strength and core stability training, which consisted of core stability (planks, climb exercise, and supine bridge) and strengthening exercises and 2. Strength and aerobic training, which consisted of aerobic exercises (bike recline and treadmill) and strengthening exercises. Lower limb strength was assessed by a 30-s chair stand test, aerobic ability by 2MST, and finally static balance by SLST. In the strength and core stability training group, tests revealed significant differences in the 30-s chair stand test, in the left SLST, in the right SLST, and finally in 2MST (61). In the strength and aerobic training group, there was only a significant difference between pre- and post-tests for 2MST. Others examined the effectiveness of an 8-week complex exercise program on walking ability and fall efficacy compared to a general exercise program. The complex exercise program consisted of resistance exercises to strengthen trunk, stretching exercises to increase flexibility, and aerobic exercises. FSST was used to assess complex walking ability. Figure-of-8 walking test (F8WT) is another test that is used to measure curved walking ability. During F8WT, the subject is asked to walk a “figure of 8” pattern around cones, the number of steps and time to accomplish the test are considered. For FSST and F8WT, in the complex exercise program and general exercise program there was significant difference between pre and post-tests. In addition, there was a significant difference between the complex exercise program and general exercise program for FSST, but not for F8WT. The results signify complex exercise program effectiveness in improving balance skills while changing direction and following a curved line (63). Table 4 shows a complete summary of the key data extracted from the studies on multi-component exercise interventions.
Table 4.
A complete summary of the key data extracted from studies of multi-component exercise intervention.
| References | Participants | Interventions modality | Duration | Outcomes | Summary of results |
|---|---|---|---|---|---|
| Ansai et al. (49) | 69 (47 women, 22 men) Age > 80 |
|
16 weeks |
|
- Significant improvements for all outcome measures |
| Chittrakul et al. (51) | 72 (women and men) Age ≥ 65 |
|
12 weeks |
|
- Significant improvements for knee extension strength and Postural sway |
| Karinkanta et al. (55) | 149 (women only) Age 70–78 |
|
12 months |
|
- ↓ rate of injured fallers for COMB - ↓ risk for injurious falls for COMB - ↓ risk for fractures COMB |
| Lacroix et al. (44) | 66 (41 women, 25 men) Age 65–80 |
|
12 weeks |
|
- Significant (Improvement) in ROMT, stride velocity and length, for supervised group only - Significant (Improvement) in FRT, TUGT, PRT, CST and SADT for both supervised and unsupervised groups - Significant (Improvement) in mediolateral perturbation for unsupervised group only |
| Li et al. (40) | 670 (436 women, 234 men) Age ≥ 70 |
|
24 weeks |
|
- Significant ↓incidence of falls - Significant ↓ time (Improvement) in iTUGT - Significant ↑score (Improvement) in SPPB |
| Li et al. (41) | 670 (436 women, 234 men) Age ≥ 70 |
|
24 weeks |
|
- Significant ↓ injurious falls - Significant ↓ serious injurious falls - Significant ↓ fall-related emergency department visits - No significant ↓ in fall-related hospitalizations |
| Park et al. (58) | 22 (women only) Age ≥ 65 |
|
12 weeks |
|
- Significant ↑ in muscles activation |
| Patil et al. (45) | 409 (women only) Age 70–80 |
|
24 months |
|
- Significant improvement in isometric leg strength and fast walking speed - No significant differences between groups in TUGT - Significant probability of completing backward walking -No significant difference between groups in the total falls incidence rate ratio or falls with any reported injury - Significant ↓medically attended fall injuries and medically attended fallers -No significant difference in the number of fallers who were injured |
| Sannicandro (61) | 65 (34 women, 31 men) Age ≥ 65 |
|
8 weeks |
|
- Significant difference (Improvement) in CST and SLST for SCG - No significant differences in CST and SLST for SAG |
| Song and Kim (63) | 40 (women and men) Age 68.81 ± 3.48 |
|
8 weeks |
|
- Significant improvements in FSST, F8WT and FES for both interventions |
| Uusi-Rasi et al. (5) | 409 (women only) Age 70–80 |
|
2 years |
|
- No differences in all falls or minor injurious falls IRR. - ↓ medically attended injurious falls. - ↓ medically attended injured fallers. - TUGT time remained unchanged at follow up tests. - Significant ↑of maximal isometric leg extensor strength |
5TSST, Five Times Sit to Stand Test; CST, Chair Standing Test; F8WT, Figure-of-8 Walking Test; FES, Falls Efficacy Scale; FRT, Functional Reach Test; FSST, Four Square Step Test; HR, Hazard Ratio; IRR, Incidence Rate Ratio; iTUGT, Instrumented Timed Up and Go Test; OLST, One Leg Standing Test; PRT, Push and Release Test; ROMT, Romberg Test; SADT, Stair Ascent and Descent Test; SLST, Single Leg Stance Test; SPPB, Short Physical Performance Battery; TT, Tandem Test; TUGT, Timed Up and Go Test.
3.4.4. Risk of bias
The result of the risk of bias summary and risk of bias graph are available in Supplementary Figures S1, S2, respectively. For random sequence generation and allocation concealment, more than 50% of the studies showed unclear risks as they were not clearly described. For blinding of participants and personnel and blinding of outcome assessment, slightly over 50% of the studies showed low risk. Almost 75% of the studies had low risk in the domain of incomplete outcomes. All studies except one demonstrated a low risk for selective reporting.
4. Discussion
This systematic review aimed to present a summary of the effectiveness of resistance, balance, and multi-component exercise interventions, which consist mainly of combined resistance and balance exercises in addition to one or more types of exercises, namely, aerobic, walking, and weight-bearing, on the parameters of functional ability (e.g., lower extremities muscle strength, balance performance, and mobility), which accordingly prevent falls in ambulatory community-dwelling adults aged 65 years or above.
Although poor muscle strength is an established risk factor for falls (66), it has been found that the inclusion of strength training had no substantial effect on falls (23, 35, 37) when the person has sufficient strength to avoid falling (35). Moreover, strength training as a single intervention showed no evidence to be effective in fall prevention (23). However, strength training is likely to offer older adults with longer-term fall prevention and other health gains (37, 67–69), and these types of exercises are recommended to be included in addition to other training (i.e., balance training) (37). To be effective, strength training should provide a certain amount of resistance in an exercise and maximally 10–15 repetitions should be completed before reaching muscle fatigue (67). A systematic review concluded that there is a positive association between the type of resistance exercise and the effect on strength gain and that resistance exercises also help in preserving functional independence and quality of life in older adults (70). In a previous study, eccentric strengthening exercise, when compared to traditional strengthening exercise, yielded greater improvements in muscle strength, balance, and mobility (71). Concerning the improvement in balance abilities after strengthening exercises, previous studies showed that they are able to improve balance recovery and dynamic and static balance skills in older adults, and consequently prevent falls (72, 73), whereas for others, the use of strengthening exercises alone failed to show clear effects on balance abilities (68, 74). One RCT in this review found that resistance exercises when done on either stable or unstable surfaces using exercise machines or free weights, demonstrated significant improvements in muscle power and reactive balance, with no significant differences between the three interventions, though gains in muscle strength (isometric leg extension strength) and gains in muscle power (chair rise test) were greater in exercises accomplished on unstable surfaces. Therefore, the authors recommended following resistance training with unstable surfaces and moderate instability as in machine-based unstable resistance training if the goal is to enhance muscle strength and the power of the lower extremities. While if great load is a concern and limited to a degree, then free-weight unstable resistance training is recommended (52).
In the same way as strength training, balance training when followed as a single intervention revealed no evidence to be effective in reducing the rate of falls and the risk of falling (23), yet the inclusion of balance training in exercise programs appeared to be a crucial factor in reducing falls (23, 27, 35, 37). Additionally, it is recommended that exercises must provide a moderate or high challenge to balance in order to prevent falls (37). Hence, this explained that different exercise programs that included balance training were similarly effective in reducing falls (35, 75, 76). According to one RCT in our review, a higher effect of balance intervention in reducing falls can be found in studies that are of a single-center nature (42). A previous study found that balance training on a foam rubber affected postural reflex in older adults (77) through improvement in the proprioception and sensitivity of lower limbs and cutaneous receptors in the soles (78). An interesting result in our review is that both foam rubber and stable surface interventions improved lower extremity muscle strength in addition to balance, with no significant difference between both (43). This is consistent with other studies that reported improvement in muscle strength after balance interventions (33, 34, 36). Other studies found a relationship between single-leg standing similar to the intervention in this trial and muscle activation (79, 80). This would prove that the progressive step marching exercise in our review is able to improve lower limb strength and eventually reduce the rate of falls in older adults (62). On the contrary, one trial we investigated did not reveal significant improvement in leg strength outcomes at the end of the balance intervention compared with pre-intervention, however, it was significant when compared to a combined intervention of virtual balance and static and dynamic balance exercises (60).
Perturbation-based balance exercises showed improvement in local dynamic stability and balance recovery with effects lasting for a week after the intervention, though it was a one-session intervention (47), others showed a reduction in the rate of all falls and slip falls (57). This is in agreement with other studies that showed quick effects (81, 82) and long-lasting ones with marginal reduction in gains (83, 84). Other trials of perturbation training in this review with longer intervention exhibited significant improvement in balance confidence using the ABC scale, dynamic stability, balance ability, and functional capacity compared to control, even more effective than traditional balance training (50, 53). Mean scores on the ABC scale improved from 65 to 80. One study revealed that the ABC scale is a strong predictor of falls in older adults, with those with a score < 67 having a high probability to fall (82). Others reported improvement in balance confidence after 4 weeks of perturbation training (85).
The multi-component intervention included a combination of trunk stability exercises and stretching (63), demonstrating significant improvement in complex walking ability. Combined strength and aerobic exercise interventions led to enhancement of lower limb strength (58), and improvement in aerobic capacity (63). In a study, it was found that improvements in balance and mobility persisted for up to 1 year after participating in a-32 week combined resistance and flexibility training program (86). Others reported that multi-component interventions had positive effects on the rate of falls (23, 27, 87, 88) and the risk of falling (23, 27) in addition to improvements in strength and balance outcomes (87, 88). Multiple categories of exercise programs containing balance training and muscle strengthening demonstrated their effectiveness in reducing both rate of falls and the risk of falling (23), whereas for others, balance and functional exercises plus strengthening revealed the same effectiveness (27). A previous study of combined strengthening and balance interventions found that physical performance was maintained during the follow-up, and that medically-attended injurious falls were significantly less after 5 years, while gains diminished in strengthening-only or balance-only interventions (89). It has been recommended that exercises for fall prevention must be of sufficient doses (i.e., at least 2 h a week) as well as in an ongoing manner (37).
Chronic diseases and multimorbidity (i.e., the coexistence of ≥2 chronic diseases in the same person) are prevalent among adults over the age of 65 years (90–93), and studies found that coronary artery diseases, stroke, diabetes, and arthritis are associated with physical inactivity in the older population (94, 95). However, participating in physical activity is believed to prevent and reduce the number of chronic diseases in older adults. (96). Others reported that the risks of falls and recurrent falling are directly proportional to the number of chronic diseases (97, 98). Frailty (99) and polypharmacy (100) (i.e., taking ≥2 drugs) are possible explanations for the connections with multimorbidity.
When studying the multimorbidity patterns (i.e., the classification of chronic diseases into different combinations based on the associations between them), the increased risk of falls was higher in the visceral-arthritic and mental-sensory patterns (97), while recurrent falling was significantly associated with a cluster of the highest prevalence of osteoporosis and a cluster that had the highest number of chronic conditions (98).
Therefore, practicing regular physical activity is crucial in reducing and preventing chronic diseases, maintaining a healthy musculoskeletal system and balance, and reducing the risk of falling.
A major strength of our review is that, to our knowledge, it is the first systematic review of RCTs to investigate the effects of different exercise interventions on ambulatory community-dwelling older adults. This study has several limitations that need to be taken into consideration. First, this review was limited to older adults who were free of dementia, stroke, Parkinson’s disease, multiple sclerosis, or recent fractures, therefore findings cannot be generalized to higher-risk populations. Second, trials with home exercise programs and virtual reality exercises were excluded. Third, the review results can only be generalized to home-dwelling older adults; trials with institutionalized older adults were excluded as well. Fourth, performing a meta-analysis was not possible due to the heterogeneity available in the included studies; variabilities in outcomes and interventions that obviously appear in prior sections of the current review. Therefore, as an alternative to a meta-analysis, we used other methods to compare the effects among the included studies. Finally, there is a lack of RCTs that particularly consider older adults with limited access to health care or in low-income countries.
5. Conclusion
In conclusion, our review addressed numerous RCTs of physical exercises composed of strengthening, balance, or multi-component interventions on physical functionality and risk of falls in community-dwelling older adults. The present review confirms the previous findings that physical exercise improves the components of functional ability, i.e., lower extremity strength, balance, and mobility. Additionally, physical exercise reduces falls and minimizes their serious sequelae. Further research on fall prevention is required that specifically considers high-risk older adults, low-income countries, and older adults in vulnerable contexts with limited access to health care.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MS: conceptualization, methodology, investigation, writing—original draft, and supervision. ZN: methodology and investigation. AM: proofreading and editing. VP: proofreading, editing, administrative support, and coordination. MH: conceptualization, methodology, proofreading, editing, and supervision. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by the Thematic Excellence Program 2020—Institutional Excellence Sub-program/National Excellence Sub-program of the Ministry for Innovation and Technology in Hungary, within the framework of the 3. thematic program of the University of Pécs (TKP2021-EGA-10) and supported by the ÚNKP-22-4-II-PTE-1667 New National Excellence Program of the Ministry for Innovation and Technology from the source of the National Research, Development, and Innovation Fund. The authors declare that the funding sources did not have any role in the study design; in the collection, analysis, and interpretation of the data, or in writing and submitting this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1209319/full#supplementary-material
Risk of bias summary.
Risk of bias graph.
Glossary
Abbreviations
- 2MST
2-minutes step test
- ABC
Activities-specific balance confidence
- CST
Chair standing test
- F8WT
Figure-of-8 walking test
- FSST
Four square step test
- MME
Multimodal exercise
- RCT
Randomized controlled trial
- SE
Stretching exercises
- SLST
Single leg stance test
- TUGT
Timed up and go test
- WHO
World Health Organization
References
- 1.Tinetti ME. Preventing falls in elderly persons. N Engl J Med. (2003) 348:42–9. doi: 10.1056/NEJMcp020719 [DOI] [PubMed] [Google Scholar]
- 2.Kalache A, Fu D, Yoshida S, Al-Faisal W, Beattie L, Chodzko-Zajko W, et al. World Health Organisation global report on falls prevention in older age. Geneva: World Health Organization; (2007). Available at: http://www.who.int/ageing/publications/Falls_prevention7March.pdf (Accessed March 10, 2021). [Google Scholar]
- 3.Peeters G, van Schoor NM, Lips P. Fall risk: the clinical relevance of falls and how to integrate fall risk with fracture risk. Best Pract Res Clin Rheumatol. (2009) 23:797–804. doi: 10.1016/j.berh.2009.09.004, PMID: [DOI] [PubMed] [Google Scholar]
- 4.Turner S, Kisser R, Rogmans W. Fall among older adults in the EU-28. The European Public Health Association. (2015) Available at: https://eupha.org/repository/sections/ipsp/Factsheet_falls_in_older_adults_in_EU.pdf (Accessed March 10, 2021). [Google Scholar]
- 5.Uusi-Rasi K, Patil R, Karinkanta S, Kannus P, Tokola K, Lamberg-Allardt C, et al. A 2-year follow-up after a 2-year RCT with vitamin D and exercise: effects on falls, injurious falls and physical functioning among older women. J Gerontol Ser A. (2017) 72:1239–45. doi: 10.1093/gerona/glx044, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and Meta-analysis. Epidemiology. (2010) 21:658–68. doi: 10.1097/EDE.0b013e3181e89905 [DOI] [PubMed] [Google Scholar]
- 7.Karinkanta S, Piirtola M, Sievänen H, Uusi-Rasi K, Kannus P. Physical therapy approaches to reduce fall and fracture risk among older adults. Nat Rev Endocrinol. (2010) 6:396–407. doi: 10.1038/nrendo.2010.70, PMID: [DOI] [PubMed] [Google Scholar]
- 8.Lee TW, Ko IS, Lee KJ. Health promotion behaviors and quality of life among community-dwelling elderly in Korea: a cross-sectional survey. Int J Nurs Stud. (2006) 43:293–300. doi: 10.1016/j.ijnurstu.2005.06.009, PMID: [DOI] [PubMed] [Google Scholar]
- 9.Benichou O, Lord SR. Rationale for strengthening muscle to prevent falls and fractures: a review of the evidence. Calcif Tissue Int. (2016) 98:531–45. doi: 10.1007/s00223-016-0107-9, PMID: [DOI] [PubMed] [Google Scholar]
- 10.Toraman A, Yıldırım NÜ. The falling risk and physical fitness in older people. Arch Gerontol Geriatr. (2010) 51:222–6. doi: 10.1016/j.archger.2009.10.012 [DOI] [PubMed] [Google Scholar]
- 11.Boyé ND, Van Lieshout EM, Van Beeck EF, Hartholt KA, Van der Cammen TJ, Patka P. The impact of falls in the elderly. Trauma. (2013) 15:29–35. doi: 10.1177/1460408612463145 [DOI] [Google Scholar]
- 12.Franco MR, Pereira LS, Ferreira PH. Exercise interventions for preventing falls in older people living in the community. Br J Sports Med. (2014) 48:867–8. doi: 10.1136/bjsports-2012-092065 [DOI] [PubMed] [Google Scholar]
- 13.Paterson DH, Warburton DE. Physical activity and functional limitations in older adults: a systematic review related to Canada’s physical activity guidelines. Int J Behav Nutr Phys Act. (2010) 7:38. doi: 10.1186/1479-5868-7-38, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang RY, Wang YL, Cheng FY, Chao YH, Chen CL, Yang YR. Effects of combined exercise on gait variability in community-dwelling older adults. Age. (2015) 37:9780. doi: 10.1007/s11357-015-9780-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ács P, Stocker M, Füge K, Paár D, Oláh A, Kovács A. Economic and public health benefits: the result of increased regular physical activity. Eur J Integr Med. (2016) 8:8–12. doi: 10.1016/j.eujim.2016.11.003 [DOI] [Google Scholar]
- 16.Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. (1999) 56:303–8. doi: 10.1001/archneur.56.3.303 [DOI] [PubMed] [Google Scholar]
- 17.Lara E, Koyanagi A, Caballero F, Domènech-Abella J, Miret M, Olaya B, et al. Cognitive reserve is associated with quality of life: a population-based study. Exp Gerontol. (2017) 87:67–73. doi: 10.1016/j.exger.2016.10.012, PMID: [DOI] [PubMed] [Google Scholar]
- 18.Sánchez-González JL, Calvo-Arenillas JI, Sánchez-Rodríguez JL. The effects of moderate physical exercise on cognition in adults over 60 years of age. Rev Neurol. (2018) 66:230–6. doi: 10.33588/rn.6607.2017449, PMID: [DOI] [PubMed] [Google Scholar]
- 19.Sánchez-González JL, Sánchez-Rodríguez JL, Martín-Vallejo J, Martel-Martel A, González-Sarmiento R. Effects of physical exercise on cognition and telomere length in healthy older women. Brain Sci. (2021) 11:1417. doi: 10.3390/brainsci11111417, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boente-Antela B, Leirós-Rodríguez R, García-Soidán JL. Compliance with the recommendations of the World Health Organization on the practice of physical activity in people over 65 years in Spain. J Hum Sport Exerc. (2020) 17:29–38. doi: 10.14198/jhse.2022.171.04 [DOI] [Google Scholar]
- 21.World Health Organization . Global recommendations on physical activity for health (2010). Available at: https://www.who.int/publications/i/item/9789241599979 (Accessed March 14, 2021). [PubMed]
- 22.World Health Organization . WHO global report on falls prevention in older age. (2008). Available at: https://apps.who.int/iris/handle/10665/43811 (Accessed March 14, 2021).
- 23.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson L, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. (2012) 2021:CD007146. doi: 10.1002/14651858.CD007146.pub3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paillard T, Lafont C, Costes-Salon MC, Rivière D, Dupui P. Effects of brisk walking on static and dynamic balance, locomotion, body composition, and aerobic capacity in ageing healthy active men. Int J Sports Med. (2004) 25:539–46. doi: 10.1055/s-2004-820948, PMID: [DOI] [PubMed] [Google Scholar]
- 25.Palvanen M, Kannus P, Piirtola M, Niemi S, Parkkari J, Järvinen M. Effectiveness of the Chaos falls clinic in preventing falls and injuries of home-dwelling older adults: a randomised controlled trial. Injury. (2014) 45:265–71. doi: 10.1016/j.injury.2013.03.010 [DOI] [PubMed] [Google Scholar]
- 26.Sherrington C, Michaleff ZA, Fairhall N, Paul SS, Tiedemann A, Whitney J, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. (2017) 51:1750–8. doi: 10.1136/bjsports-2016-096547 [DOI] [PubMed] [Google Scholar]
- 27.Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. (2019) 2019:CD012424. doi: 10.1002/14651858.CD012424.pub2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shimada H, Obuchi S, Furuna T, Suzuki T. New intervention program for preventing falls among frail elderly people: the effects of perturbed walking exercise using a bilateral separated treadmill. Am J Phys Med Rehabil. (2004) 83:493–9. doi: 10.1097/01.PHM.0000130025.54168.91 [DOI] [PubMed] [Google Scholar]
- 29.Korpelainen R, Keinänen-Kiukaanniemi S, Nieminen P, Heikkinen J, Väänänen K, Korpelainen J. Long-term outcomes of exercise: follow-up of a randomized trial in older women with osteopenia. Arch Intern Med. (2010) 170:1548–56. doi: 10.1001/archinternmed.2010.311 [DOI] [PubMed] [Google Scholar]
- 30.Panel on Prevention of Falls in Older Persons, American Geriatrics Society, and British geriatrics society . Summary of the updated American Geriatrics Society/British geriatrics society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. (2011) 59:148–57. doi: 10.1111/j.1532-5415.2010.03234.x [DOI] [PubMed] [Google Scholar]
- 31.Grgic J, Garofolini A, Orazem J, Sabol F, Schoenfeld BJ, Pedisic Z. Effects of resistance training on muscle size and strength in very elderly adults: a systematic review and meta-analysis of randomized controlled trials. Sports Med. (2020) 50:1983–99. doi: 10.1007/s40279-020-01331-7, PMID: [DOI] [PubMed] [Google Scholar]
- 32.LaStayo P, Marcus R, Dibble L, Wong B, Pepper G. Eccentric versus traditional resistance exercise for older adult fallers in the community: a randomized trial within a multi-component fall reduction program. BMC Geriatr. (2017) 17:149. doi: 10.1186/s12877-017-0539-8, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Audette JF, Jin YS, Newcomer R, Stein L, Duncan G, Frontera WR. Tai Chi versus brisk walking in elderly women. Age Ageing. (2006) 35:388–93. doi: 10.1093/ageing/afl006, PMID: [DOI] [PubMed] [Google Scholar]
- 34.Heitkamp HC, Horstmann T, Mayer F, Weller J, Dickhuth HH. Gain in strength and muscular balance after balance training. Int J Sports Med. (2001) 22:285–90. doi: 10.1055/s-2001-13819, PMID: [DOI] [PubMed] [Google Scholar]
- 35.Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JCT. Effective exercise for the prevention of falls: a systematic review and Meta-analysis. J Am Geriatr Soc. (2008) 56:2234–43. doi: 10.1111/j.1532-5415.2008.02014.x, PMID: [DOI] [PubMed] [Google Scholar]
- 36.Taylor-Piliae RE, Haskell WL, Stotts NA, Froelicher ES. Improvement in balance, strength, and flexibility after 12 weeks of tai chi exercise in ethnic Chinese adults with cardiovascular disease risk factors. Altern Ther Health Med. (2006) 12:50–8. doi: 10.1016/j.ejcnurse.2005.10.008, PMID: [DOI] [PubMed] [Google Scholar]
- 37.Sherrington C, Tiedemann A, Fairhall N, Close JCT, Lord SR. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. N S W Public Health Bull. (2011) 22:78–83. doi: 10.1071/NB10056 [DOI] [PubMed] [Google Scholar]
- 38.Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arnold C, Lanovaz J, Oates A, Craven B, Butcher S. The effect of adding core stability training to a standard balance exercise program on sit to stand performance in older adults: a pilot study. J Aging Phys Act. (2015) 23:95–102. doi: 10.1123/JAPA.2013-0115, PMID: [DOI] [PubMed] [Google Scholar]
- 40.Li F, Harmer P, Fitzgerald K, Eckstrom E, Akers L, Chou LS, et al. Effectiveness of a therapeutic tai Ji Quan intervention vs a multimodal exercise intervention to prevent falls among older adults at high risk of falling: a randomized clinical trial. JAMA Intern Med. (2018) 178:1301–10. doi: 10.1001/jamainternmed.2018.3915, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li F, Harmer P, Eckstrom E, Fitzgerald K, Chou LS, Liu Y. Effectiveness of tai Ji Quan vs multimodal and stretching exercise interventions for reducing injurious falls in older adults at high risk of falling: follow-up analysis of a randomized clinical trial. JAMA Netw Open. (2019) 2:e188280. doi: 10.1001/jamanetworkopen.2018.8280, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.El-Khoury F, Cassou B, Latouche A, Aegerter P, Charles MA, Dargent-Molina P. Effectiveness of two year balance training programme on prevention of fall induced injuries in at risk women aged 75-85 living in community: Ossébo randomised controlled trial. BMJ. (2015) 351:h3830. doi: 10.1136/bmj.h3830, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hirase T, Inokuchi S, Matsusaka N, Okita M. Effects of a balance training program using a foam rubber pad in community-based older adults: a randomized controlled trial. J Geriatr Phys Ther. (2015) 38:62–70. doi: 10.1519/JPT.0000000000000023, PMID: [DOI] [PubMed] [Google Scholar]
- 44.Lacroix A, Kressig RW, Muehlbauer T, Gschwind YJ, Pfenninger B, Bruegger O, et al. Effects of a supervised versus an unsupervised combined balance and strength training program on balance and muscle power in healthy older adults: a randomized controlled trial. Gerontology. (2016) 62:275–88. doi: 10.1159/000442087, PMID: [DOI] [PubMed] [Google Scholar]
- 45.Patil R, Uusi-Rasi K, Tokola K, Karinkanta S, Kannus P, Sievänen H. Effects of a multimodal exercise program on physical function, falls, and injuries in older women: a 2-year community-based, randomized controlled trial. J Am Geriatr Soc. (2015) 63:1306–13. doi: 10.1111/jgs.13489, PMID: [DOI] [PubMed] [Google Scholar]
- 46.Johnson SL, Stevens SL, Fuller DK, Caputo JL. Effect of lower-extremity eccentric training on physical function in community-dwelling older adults. Phys Occup Ther Geriatr. (2019) 37:298–312. doi: 10.1080/02703181.2019.1648626 [DOI] [Google Scholar]
- 47.Rieger MM, Papegaaij S, Pijnappels M, Steenbrink F, van Dieën JH. Transfer and retention effects of gait training with anterior-posterior perturbations to postural responses after medio-lateral gait perturbations in older adults. Clin Biomech. (2020) 75:104988. doi: 10.1016/j.clinbiomech.2020.104988, PMID: [DOI] [PubMed] [Google Scholar]
- 48.Kocaman AA, Kırdı N, Aksoy S, Elmas Ö, Dogu BB. The effect of different exercise training types on functionality in older fallers: a pilot randomized controlled trial. Top Geriatr Rehabil. (2021) 37:114–27. doi: 10.1097/TGR.0000000000000312 [DOI] [Google Scholar]
- 49.Ansai JH, Aurichio TR, Gonçalves R, Rebelatto JR. Effects of two physical exercise protocols on physical performance related to falls in the oldest old: a randomized controlled trial: exercises protocols in oldest old. Geriatr Gerontol Int. (2016) 16:492–9. doi: 10.1111/ggi.12497, PMID: [DOI] [PubMed] [Google Scholar]
- 50.Arghavani H, Zolaktaf V, Lenjannejadian S. Comparing the effects of anticipatory postural adjustments focused training and balance training on postural preparation, balance confidence and quality of life in elderly with history of a fall. Aging Clin Exp Res. (2020) 32:1757–65. doi: 10.1007/s40520-019-01358-5, PMID: [DOI] [PubMed] [Google Scholar]
- 51.Chittrakul J, Siviroj P, Sungkarat S, Sapbamrer R. Multi-system physical exercise intervention for fall prevention and quality of life in pre-frail older adults: a randomized controlled trial. Int J Environ Res Public Health. (2020) 17:3102. doi: 10.3390/ijerph17093102, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eckardt N. Lower-extremity resistance training on unstable surfaces improves proxies of muscle strength, power and balance in healthy older adults: a randomised control trial. BMC Geriatr. (2016) 16:191. doi: 10.1186/s12877-016-0366-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hamed A, Bohm S, Mersmann F, Arampatzis A. Exercises of dynamic stability under unstable conditions increase muscle strength and balance ability in the elderly. Scand J Med Sci Sports. (2018) 28:961–71. doi: 10.1111/sms.13019, PMID: [DOI] [PubMed] [Google Scholar]
- 54.Jang EM, Park SH. Effects of neuromuscular electrical stimulation combined with exercises versus an exercise program on the physical characteristics and functions of the elderly: a randomized controlled trial. Int J Environ Res Public Health. (2021) 18:2463. doi: 10.3390/ijerph18052463, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Karinkanta S, Kannus P, Uusi-Rasi K, Heinonen A, Sievänen H. Combined resistance and balance-jumping exercise reduces older women’s injurious falls and fractures: 5-year follow-up study. Age Ageing. (2015) 44:784–9. doi: 10.1093/ageing/afv064, PMID: [DOI] [PubMed] [Google Scholar]
- 56.Lee SH, Lee DY. Effects of open and closed kinetic chain exercises on the balance using elastic bands for the health Care of the Elderly Females. Medico-Leg Update. (2019) 19:728. doi: 10.5958/0974-1283.2019.00263.9 [DOI] [Google Scholar]
- 57.Okubo Y, Sturnieks DL, Brodie MA, Duran L, Lord SR. Effect of reactive balance training involving repeated slips and trips on balance recovery among older adults: a blinded randomized controlled trial. J Gerontol Ser A (2019) 16;74:1489–1496. doi: 10.1093/gerona/glz021 [DOI] [PubMed] [Google Scholar]
- 58.Park J, Lee J, Yang J, Lee B, Han D. Effects of combined exercise on changes of lower extremity muscle activation during walking in older women. J Phys Ther Sci. (2015) 27:1515–8. doi: 10.1589/jpts.27.1515, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pourtaghi F, Moghadam ZE, Ramezani M, Vashani HB, Mohajer S. The effect of resistance training using Thera-band on muscular strength and quality of life among the elderly in the City of Mashhad. Evid Based Care. (2017). 7:7–16. doi: 10.22038/ebcj.2017.25876.1584 [DOI] [Google Scholar]
- 60.Sadeghi H, Jehu DA, Daneshjoo A, Shakoor E, Razeghi M, Amani A, et al. Effects of 8 weeks of balance training, virtual reality training, and combined exercise on lower limb muscle strength, balance, and functional mobility among older men: a randomized controlled trial. Sports Health Multidiscip Approach. (2021) 13:606–12. doi: 10.1177/1941738120986803, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sannicandro I. Effects of strength and core stability training versus strength and aerobic training in subjects aged over 65. Med Sport. (2018) 70:410–8. doi: 10.23736/S0025-7826.17.03132-5 [DOI] [Google Scholar]
- 62.Sitthiracha P, Eungpinichpong W, Chatchawan U. Effect of progressive step marching exercise on balance ability in the elderly: a cluster randomized clinical trial. Int J Environ Res Public Health. (2021) 18:3146. doi: 10.3390/ijerph18063146, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Song HS, Kim JY. The effects of complex exercise on walking ability during direction change and falls efficacy in the elderly. J Phys Ther Sci. (2015) 27:1365–7. doi: 10.1589/jpts.27.1365, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhao Y, Chung PK, Tong TK. Effectiveness of a community-based exercise program on balance performance and fear of falling in older nonfallers at risk for falling: a randomized. Control Study J Aging Phys Act. (2016) 24:516–24. doi: 10.1123/japa.2015-0224, PMID: [DOI] [PubMed] [Google Scholar]
- 65.Zhao Y, Chung PK, Tong TK. Effectiveness of a balance-focused exercise program for enhancing functional fitness of older adults at risk of falling: a randomised controlled trial. Geriatr Nur. (2017) 38:491–7. doi: 10.1016/j.gerinurse.2017.02.011, PMID: [DOI] [PubMed] [Google Scholar]
- 66.Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. (2004) 52:1121–9. doi: 10.1111/j.1532-5415.2004.52310.x [DOI] [PubMed] [Google Scholar]
- 67.American College of Sports Medicine. Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. (2009) 41:1510–30. doi: 10.1249/MSS.0b013e3181a0c95c, PMID: [DOI] [PubMed] [Google Scholar]
- 68.Latham N, Anderson C, Bennett D, Stretton C. Progressive resistance strength training for physical disability in older people. Cochrane Database Syst Rev. (2003) 2003:CD002759. doi: 10.1002/14651858.CD002759 [DOI] [PubMed] [Google Scholar]
- 69.Singh NA, Stavrinos TM, Scarbek Y, Galambos G, Liber C, Fiatarone Singh MA. A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. J Gerontol A Biol Sci Med Sci. (2005) 60:768–76. doi: 10.1093/gerona/60.6.768, PMID: [DOI] [PubMed] [Google Scholar]
- 70.Martins WR, de Oliveira RJ, Carvalho RS, de Oliveira DV, da Silva VZM, Silva MS. Elastic resistance training to increase muscle strength in elderly: a systematic review with meta-analysis. Arch Gerontol Geriatr. (2013) 57:8–15. doi: 10.1016/j.archger.2013.03.002, PMID: [DOI] [PubMed] [Google Scholar]
- 71.LaStayo PC, Ewy GA, Pierotti DD, Johns RK, Lindstedt S. The positive effects of negative work: increased muscle strength and decreased fall risk in a frail elderly population. J Gerontol Ser A. (2003) 58:M419–24. doi: 10.1093/gerona/58.5.M419, PMID: [DOI] [PubMed] [Google Scholar]
- 72.Arampatzis A, Peper A, Bierbaum S. Exercise of mechanisms for dynamic stability control increases stability performance in the elderly. J Biomech. (2011) 44:52–8. doi: 10.1016/j.jbiomech.2010.08.023, PMID: [DOI] [PubMed] [Google Scholar]
- 73.Marques EA, Figueiredo P, Harris TB, Wanderley FA, Carvalho J. Are resistance and aerobic exercise training equally effective at improving knee muscle strength and balance in older women? Arch Gerontol Geriatr. (2017) 68:106–12. doi: 10.1016/j.archger.2016.10.002, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Orr R, Raymond J, Fiatarone SM. Efficacy of progressive resistance training on balance performance in older adults: a systematic review of randomized controlled trials. Sports Med Auckl NZ. (2008) 38:317–43. doi: 10.2165/00007256-200838040-00004 [DOI] [PubMed] [Google Scholar]
- 75.Li F, Harmer P, Fisher KJ, McAuley E, Chaumeton N, Eckstrom E, et al. Tai chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. (2005) 60:187–94. doi: 10.1093/gerona/60.2.187 [DOI] [PubMed] [Google Scholar]
- 76.Robertson MC, Campbell AJ, Gardner MM, Devlin N. Preventing injuries in older people by preventing falls: a meta-analysis of individual-level data. J Am Geriatr Soc. (2002) 50:905–11. doi: 10.1046/j.1532-5415.2002.50218.x [DOI] [PubMed] [Google Scholar]
- 77.Granacher U, Gollhofer A, Strass D. Training induced adaptations in characteristics of postural reflexes in elderly men. Gait Posture. (2006) 24:459–66. doi: 10.1016/j.gaitpost.2005.12.007, PMID: [DOI] [PubMed] [Google Scholar]
- 78.McIlroy WE, Bishop DC, Staines WR, Nelson AJ, Maki BE, Brooke JD. Modulation of afferent inflow during the control of balancing tasks using the lower limbs. Brain Res. (2003) 961:73–80. doi: 10.1016/S0006-8993(02)03845-3, PMID: [DOI] [PubMed] [Google Scholar]
- 79.Dingenen B, Janssens L, Claes S, Bellemans J, Staes FF. Lower extremity muscle activation onset times during the transition from double-leg stance to single-leg stance in anterior cruciate ligament reconstructed subjects. Clin Biomech. (2016) 35:116–23. doi: 10.1016/j.clinbiomech.2016.04.014 [DOI] [PubMed] [Google Scholar]
- 80.Iverson BD, Gossman MR, Shaddeau SA, Turner ME, Jr. Balance performance, force production, and activity levels in noninstitutionalized men 60 to 90 years of age. Phys Ther. (1990) 70:348–55. doi: 10.1093/ptj/70.6.348, PMID: [DOI] [PubMed] [Google Scholar]
- 81.Okubo Y, Schoene D, Lord SR. Step training improves reaction time, gait and balance and reduces falls in older people: a systematic review and meta-analysis. Br J Sports Med. (2017) 51:586–93. doi: 10.1136/bjsports-2015-095452, PMID: [DOI] [PubMed] [Google Scholar]
- 82.Pai YC, Bhatt T, Wang E, Espy D, Pavol MJ. Inoculation against falls: rapid adaptation by young and older adults to slips during daily activities. Arch Phys Med Rehabil. (2010) 91:452–9. doi: 10.1016/j.apmr.2009.10.032, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Parijat P, Lockhart TE. Effects of moveable platform training in preventing slip-induced falls in older adults. Ann Biomed Eng. (2012) 40:1111–21. doi: 10.1007/s10439-011-0477-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tanvi B, Feng Y, Yi-Chung P. Learning to resist gait-slip falls: long-term retention in community-dwelling older adults. Arch Phys Med Rehabil. (2012) 93:557–64. doi: 10.1016/j.apmr.2011.10.027, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pijnappels M, Reeves ND, Maganaris CN, van Dieën JH. Tripping without falling; lower limb strength, a limitation for balance recovery and a target for training in the elderly. J Electromyogr Kinesiol. (2008) 18:188–96. doi: 10.1016/j.jelekin.2007.06.004 [DOI] [PubMed] [Google Scholar]
- 86.Bird M, Hill KD, Ball M, Hetherington S, Williams AD. The long-term benefits of a multi-component exercise intervention to balance and mobility in healthy older adults. Arch Gerontol Geriatr. (2011) 52:211–6. doi: 10.1016/j.archger.2010.03.021, PMID: [DOI] [PubMed] [Google Scholar]
- 87.Clemson L, Munro J, Singh MF. Lifestyle-integrated functional exercise (LiFE) program to prevent falls [Participant’s manual]. Sydney University Press; (2014). Available at: https://www.jstor.org/stable/j.ctv176kt7j (Accessed March 14, 2021). [Google Scholar]
- 88.Taguchi N, Higaki Y, Inoue S, Kimura H, Tanaka K. Effects of a 12-month multicomponent exercise program on physical performance, daily physical activity, and quality of life in very elderly people with minor disabilities: an intervention study. J Epidemiol. (2010) 20:21–9. doi: 10.2188/jea.je20081033, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Karinkanta S, Heinonen A, Sievänen H, Uusi-Rasi K, Fogelholm M, Kannus P. Maintenance of exercise-induced benefits in physical functioning and bone among elderly women. Osteoporos Int. (2009) 20:665–74. doi: 10.1007/s00198-008-0703-2, PMID: [DOI] [PubMed] [Google Scholar]
- 90.Thorpe KE, Howard DH. The rise in spending among Medicare beneficiaries: the role of chronic disease prevalence and changes in treatment intensity. Health Aff. (2006) 25:w378–88. doi: 10.1377/hlthaff.25.w378 [DOI] [PubMed] [Google Scholar]
- 91.Freedman VA, Martin LG. Contribution of chronic conditions to aggregate changes in old-age functioning. Am J Public Health. (2000) 90:1755–60. doi: 10.2105/ajph.90.11.1755, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. (2002) 162:2269–76. doi: 10.1001/archinte.162.20.2269, PMID: [DOI] [PubMed] [Google Scholar]
- 93.Vogeli C, Shields AE, Lee TA, Gibson TB, Marder WD, Weiss KB, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. (2007) 22 Suppl 3:391–5. doi: 10.1007/s11606-007-0322-1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kruger J, Ham SA, Sanker S. Physical inactivity during leisure time among older adults--behavioral risk factor surveillance system, 2005. J Aging Phys Act. (2008) 16:280–91. doi: 10.1123/japa.16.3.280 [DOI] [PubMed] [Google Scholar]
- 95.Kumthekar A, Pedro S, Michaud K, Ozen G, Katz P, Baker J, et al. Physical activity habits among older adults living with rheumatic disease. J Rheumatol. (2023) 50:835–41. doi: 10.3899/jrheum.211244, PMID: [DOI] [PubMed] [Google Scholar]
- 96.Marques A, Peralta M, Martins J, de Matos MG, Brownson RC. Cross-sectional and prospective relationship between physical activity and chronic diseases in European older adults. Int J Public Health. (2017) 62:495–502. doi: 10.1007/s00038-016-0919-4, PMID: [DOI] [PubMed] [Google Scholar]
- 97.Yan J, Wang M, Cao Y. Patterns of multimorbidity in association with falls among the middle-aged and older adults: results from the China health and retirement longitudinal study. BMC Public Health. (2022) 22:1814. doi: 10.1186/s12889-022-14124-6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Immonen M, Haapea M, Similä H, Enwald H, Keränen N, Kangas M, et al. Association between chronic diseases and falls among a sample of older people in Finland. BMC Geriatr. (2020) 20:225. doi: 10.1186/s12877-020-01621-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Abad-Díez JM, Calderón-Larrañaga A, Poncel-Falcó A, Poblador-Plou B, Calderón-Meza JM, Sicras-Mainar A, et al. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr. (2014) 14:75. doi: 10.1186/1471-2318-14-75, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fried TR, O’Leary J, Towle V, Goldstein MK, Trentalange M, Martin DK. Health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J Am Geriatr Soc. (2014) 62:2261–72. doi: 10.1111/jgs.13153, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Risk of bias summary.
Risk of bias graph.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.