Abstract
OBJECTIVE
To estimate the global, regional, and national prevalence of prediabetes, defined by impaired glucose tolerance (IGT) or impaired fasting glucose (IFG).
RESEARCH DESIGN AND METHODS
We reviewed 7,014 publications for high-quality estimates of IGT (2-h glucose, 7.8–11.0 mmol/L [140–199 mg/dL]) and IFG (fasting glucose, 6.1–6.9 mmol/L [110–125 mg/dL]) prevalence for each country. We used logistic regression to generate prevalence estimates for IGT and IFG among adults aged 20–79 years in 2021 and projections for 2045. For countries without in-country data, we extrapolated estimates from countries with available data with similar geography, income, ethnicity, and language. Estimates were standardized to the age distribution for each country from the United Nations.
RESULTS
Approximately two-thirds of countries did not have high-quality IGT or IFG data. There were 50 high-quality studies for IGT from 43 countries and 43 high-quality studies for IFG from 40 countries. Eleven countries had data for both IGT and IFG. The global prevalence of IGT in 2021 was 9.1% (464 million) and is projected to increase to 10.0% (638 million) in 2045. The global prevalence of IFG in 2021 was 5.8% (298 million) and is projected to increase to 6.5% (414 million) in 2045. The 2021 prevalence of IGT and IFG was highest in high-income countries. In 2045, the largest relative growth in cases of IGT and IFG would be in low-income countries.
CONCLUSIONS
The global burden of prediabetes is substantial and growing. Enhancing prediabetes surveillance is necessary to effectively implement diabetes prevention policies and interventions.
Graphical Abstract
Introduction
Prediabetes is a condition characterized by elevated blood glucose levels below the threshold for a diagnosis of diabetes but associated with a higher risk of developing diabetes. Impaired glucose tolerance (IGT) (2-h glucose 7.8–11.0 mol/L [140–199 mg/dL]) and impaired fasting glucose (IFG) (fasting glucose 6.1–6.9 mmol/L [110–125 mg/dL]), based on the World Health Organization (WHO) criteria, are commonly used to define prediabetes (1). IGT tends to be characterized by insulin resistance in muscle and decreased glucose uptake, while IFG is generally driven by insulin resistance in the liver and excess hepatic glucose production (2). There is limited overlap between IGT and IFG; only 20–25% of people with IGT have IFG, and 30–45% of individuals with IFG have IGT (3).
While IGT and IFG may reflect different but overlapping underlying pathogenic processes (4), people with IGT or IFG are at high risk for developing diabetes, with up to 50% progressing to diabetes within 5 years (5). People with IFG or IGT are also at elevated risk of chronic kidney disease, cardiovascular disease, and mortality (6,7). Intensive lifestyle intervention (e.g., dietary modification and increased physical activity) and pharmacological intervention (e.g., metformin) can significantly reduce the risk of progression to diabetes in those with IGT or IFG (8–10).
Characterizing the global prevalence of IGT and IFG is important for developing and implementing diabetes prevention policies and interventions worldwide. These data can also inform public health planning, since they highlight the population at high risk of needing diabetes treatment and people who may require care for complications in the future. In 2019, the IDF Diabetes Atlas, 9th edition (here termed Atlas 9) (11), estimated that, worldwide, 7.5% of adults aged 20–79 years, or 374 million people, had IGT, with the highest prevalence in North American and Caribbean countries. However, IGT only captures a portion of the population with prediabetes. Characterizing the prevalence of IFG can provide a more complete assessment of the global burden of prediabetes, but Atlas 9 lacked high-quality data that could be used to generate reliable estimates.
Drawing on over 80 high-quality, contemporary studies, we estimated the global burden of prediabetes in 2021 using WHO definitions of IFG and IGT and provided projections for 2045.
Research Design and Methods
Literature Search
We used long-standing methods established by the International Diabetes Federation (IDF) to systematically select and analyze studies from the peer-reviewed and gray literature (12). The search terms used are provided in the Supplementary Appendix. We originally searched PubMed, Medline, and Google Scholar in November 2020 for publications (available up to the time of the search) that reported age-stratified (>3 strata required) prevalence estimates for IGT and/or for IFG. Articles identified as a result of this systematic review were used to generate the 2021 prevalence estimates for IGT and IFG in IDF Diabetes Atlas, 10th edition (13). The search was not rerun. Each abstract was first screened by two independent reviewers for potential relevance, and then the full text was reviewed by two independent reviewers. Conflicts were resolved by a third reviewer.
Eligible data sources included population-based studies (national or regional), registries, or insurance-based data on adults (Supplementary Table 1). Only studies published in English were included in the initial literature search and extraction process, but a later search of publications in non-English languages (Spanish, French, Portuguese, and Russian) was conducted, where possible, via the IDF network. In addition to peer-reviewed publications, we considered national estimates from the gray literature, including WHO STEPwise approach to noncommunicable disease risk factor surveillance (STEPS) survey reports, in the estimation process. We also contacted ministries of health and all IDF regional partners for unpublished data related to IFG and IGT. Data sources reporting prediabetes in hospital or clinic populations, occupational cohorts, or other specific populations (e.g., older adults and adults with kidney disease) were excluded. Newly identified studies were combined with previous IDF data for IGT. Only estimates of prediabetes prevalence after 2005 were included in the estimation, except for countries whose only data predated 2005. Data sources that included three or more age-stratified estimates of IFG or IGT were required for the analysis. Where age-specific data were not reported in the original publication, we reached out to study authors for this information.
Scoring the Quality of the Data
Newly identified studies and previous IDF data sources were scored for quality using the Analytical Hierarchy Process (12,14). The data source was scored according to national representativeness, diagnostic criteria, sample size, year of data source, etc. Only studies that met the 0.29 threshold for high-quality data were included. When more than one study met the threshold, study estimates were weighted for sample size.
Estimating the Prevalence of Impaired Glucose Tolerance and Impaired Fasting Glucose in 2021 and 2045
Using established methods developed by the IDF (15), we estimated the global prevalence of prediabetes based on WHO definitions of IFG and IGT. Briefly, we built separate logistic regression models to produce smoothed prevalence estimates of IGT and IFG. The models included adjustment for age (modeled continuously using the midpoint of each available age group) and the quadratic of age. We ran models stratified by sex (male or female), setting (urban or rural), and age (adults aged 20–79 years, 5-year increments) category–specific estimates. Prevalence estimates for IGT and IFG were standardized to the 2021 age distribution for each country from the United Nations (15,16).
For countries without high-quality in-country data, we used methods established by the IDF to extrapolate prevalence estimates from countries deemed to be similar based on geography, IDF region, ethnicity, language, and World Bank income classification (15). IDF selected these measures to guide extrapolation based on extensive discussions and consensus from experts around the world. For studies that did not report results stratified by urbanization, urban and rural ratios were calculated according to the weighted average of the ratios reported in various data sources from the seven IDF regions and the four World Bank income classifications (15).
Using standard IDF methods (15), we estimated CI for each IGT and IFG prevalence estimate separately for each country using a process that included 1) a simulation analysis to estimate uncertainty for each study and 2) a jackknife analysis to estimate uncertainty due to study inclusion. The simulation analysis involved production of 500 random samples from a binomial distribution to produce lower and upper bounds, which represent the confidence intervals. The jackknife analysis involved 1,000 iterations. In each loop, a study was randomly removed from the data set and the global prevalence was estimated. CI for each estimate of IGT and of IFG prevalence were identified using the lower and upper bound for each age group, sex, and country. The lower and upper bounds from the simulation and jackknife analyses were combined to produce the widest overall CI (15).
We derived the projections of IGT and IFG prevalence estimates in 2045 using data from the United Nations on midyear population projections (17). Future projections were calculated using the United Nations population predictions for age, sex, and urbanization (urban-to-rural ratio). The projections for IGT and IFG prevalence in 2045 were standardized to the United Nations’ projected age distribution for each country (15,16). Analyses were performed using R software version 4.0.3. Graphics were generated using Microsoft Excel.
Results
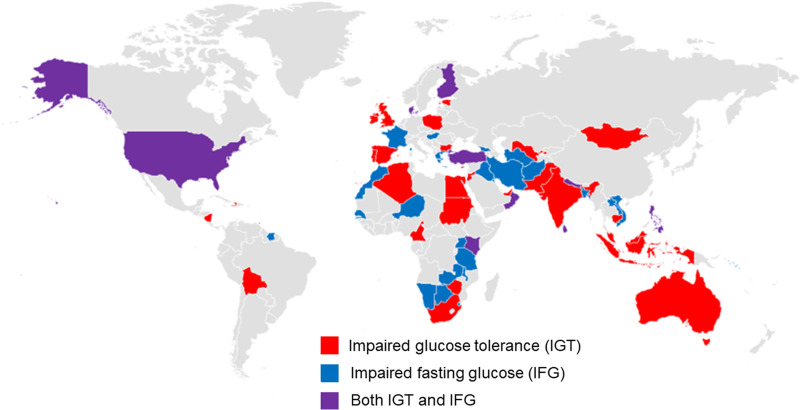
We screened 7,014 articles as part of the literature review. Of the 215 world countries and territories, 43 countries (20.0%) had high-quality data sources for estimating IGT and 40 countries (18.6%) had high-quality data sources for estimating IFG (Supplementary Table 2) (Fig. 1). Only 11 countries (4.8%) had estimates for both IGT and IFG (Fig. 1). Approximately 40% of the world population was represented in IGT data sources, while 18% was represented in studies of IFG.
Figure 1.
Countries with data sources for IGT and/or for IFG.
In 2021, the age-adjusted prevalence of IGT among adults aged 20–79 years worldwide was 9.1% (464 million); by 2045, this figure is projected to increase to 10.0% (638 million) (Table 1). In 2021, 5.8% (298 million) of the global adult population aged 20–79 years was estimated to have IFG, which will increase to an estimated 6.5% (414 million) in 2045. Age-adjusted prevalence of IGT and IGT for each country and territory worldwide (with extrapolation for countries without in-country data) are available in Supplementary Table 2.
Table 1.
Age-adjusted* prevalence for IGT and IFG in adults aged 20–79 years globally and by IDF region
| Rank | IDF region | 2021 | 2045 | ||
|---|---|---|---|---|---|
| Prevalence, % | No. of people with condition, millions | Prevalence, % | No. of people with condition, millions | ||
| IGT | |||||
| World | 9.1 (7.9, 10.8) | 464 (404, 552) | 10.0 (8.6, 11.7) | 638 (548, 752) | |
| 1 | NAC | 13.1 (10.8, 13.6) | 47 (39, 49) | 13.8 (11.0, 14.4) | 57 (46, 59) |
| 2 | SACA | 11.6 (10.7, 12.5) | 40 (37, 43) | 12.8 (11.8, 13.8) | 53 (49, 57) |
| 3 | WP | 11.1 (9.9, 13.2) | 193 (172, 229) | 11.8 (10.8, 13.7) | 213 (195, 248) |
| 4 | MENA | 10.6 (9.7, 11.9) | 48 (43, 54) | 11.5 (10.5, 12.9) | 81 (74, 91) |
| 5 | AFR | 9.7 (6.6, 12.6) | 51 (35, 66) | 11.1 (7.3, 14.3) | 117 (77, 151) |
| 6 | EUR | 5.9 (4.9, 8.8) | 39 (33, 59) | 6.2 (5.2, 9.3) | 41 (35, 62) |
| 7 | SEA | 4.5 (4.4, 5.0) | 47 (45, 52) | 5.7 (5.5, 6.2) | 77 (74, 83) |
| IFG | |||||
| World | 5.8 (5.4, 6.3) | 298 (275, 324) | 6.5 (6.0, 7.1) | 414 (382, 452) | |
| 1 | SEA | 9.4 (9.0, 9.8) | 97 (93, 101) | 9.6 (9.1, 10.1) | 128 (122, 135) |
| 2 | MENA | 7.9 (7.5, 8.3) | 35 (33, 37) | 8.5 (8.1, 9.0) | 60 (57, 63) |
| 3 | NAC | 7.6 (7.0, 8.2) | 28 (25, 30) | 8.0 (7.4, 8.7) | 33 (31, 36) |
| 4 | AFR | 5.7 (5.3, 6.2) | 30 (28, 33) | 6.3 (5.9, 6.9) | 67 (62, 72) |
| 5 | SACA | 5.0 (4.1, 5.7) | 17 (14, 20) | 5.6 (4.6, 6.5) | 23 (19, 27) |
| 6 | EUR | 4.8 (4.2, 5.6) | 32 (28, 38) | 5.2 (4.5, 6.1) | 34 (30, 41) |
| 7 | WP | 3.4 (3.1, 3.8) | 60 (54, 66) | 3.8 (3.4, 4.3) | 69 (62, 78) |
CI are reported in parentheses. IGT was defined as 2-h postload glucose levels of 7.8–11.1 mmol/L (140–199 mg/dL). IFG was defined as fasting plasma glucose levels of 6.1 to 6.9 mmol/L (110–125 mg/dL). AFR, Africa; EUR, Europe; MENA, Middle East and North Africa; NAC, North America and Caribbean; SACA, South and Central America; SEA, Southeast Asia; WP, Western Pacific.
Age adjustment was based on United Nations age distribution data for each country.
The age-adjusted prevalence of IGT in 2021 was highest in the North America and Caribbean regions (13.1%) and lowest in the Southeast Asia region (4.5%) (Table 2). Southeast Asia (9.4%) had the highest age-adjusted prevalence of IFG in 2021, while the Western Pacific region (3.4%) had the lowest prevalence.
Table 2.
Age-adjusted* prevalence of IGT and IFG in adults aged 20–79 years globally and by World Bank income classification
| Condition and World Bank income classification | 2021 | 2045 (projected) | ||
|---|---|---|---|---|
| Prevalence, % | No. of people with condition, millions | Prevalence, % | No. of people with condition, millions | |
| IGT | ||||
| High | 11.2 (9.5, 12.7) | 105 (89, 119) | 12.0 (10.1, 13.5) | 113 (96, 128) |
| Middle | 8.5 (7.6, 10.2) | 327 (292, 391) | 9.4 (8.4, 11.1) | 450 (402, 529) |
| Low | 9.5 (6.6, 12.1) | 33 (23, 41) | 10.9 (7.3, 13.7) | 75 (50, 95) |
| IFG | ||||
| High | 6.4 (5.6, 7.2) | 60 (53, 68) | 6.7 (5.9, 7.7) | 63 (56, 73) |
| Middle | 5.8 (5.4, 6.2) | 221 (206, 237) | 6.6 (6.1, 7.1) | 312 (290, 337) |
| Low | 5.0 (4.7, 5.5) | 17 (16, 19) | 5.6 (5.2, 6.1) | 38 (36, 42) |
CI are reported in parentheses. IGT was defined as 2-h postload glucose levels of 7.8–11.1 mmol/L (140–199 mg/dL). IFG was defined as fasting plasma glucose levels of 6.1–6.9 mmol/L (110–125 mg/dL).
Age adjustment was based on United Nations age distribution data for each country.
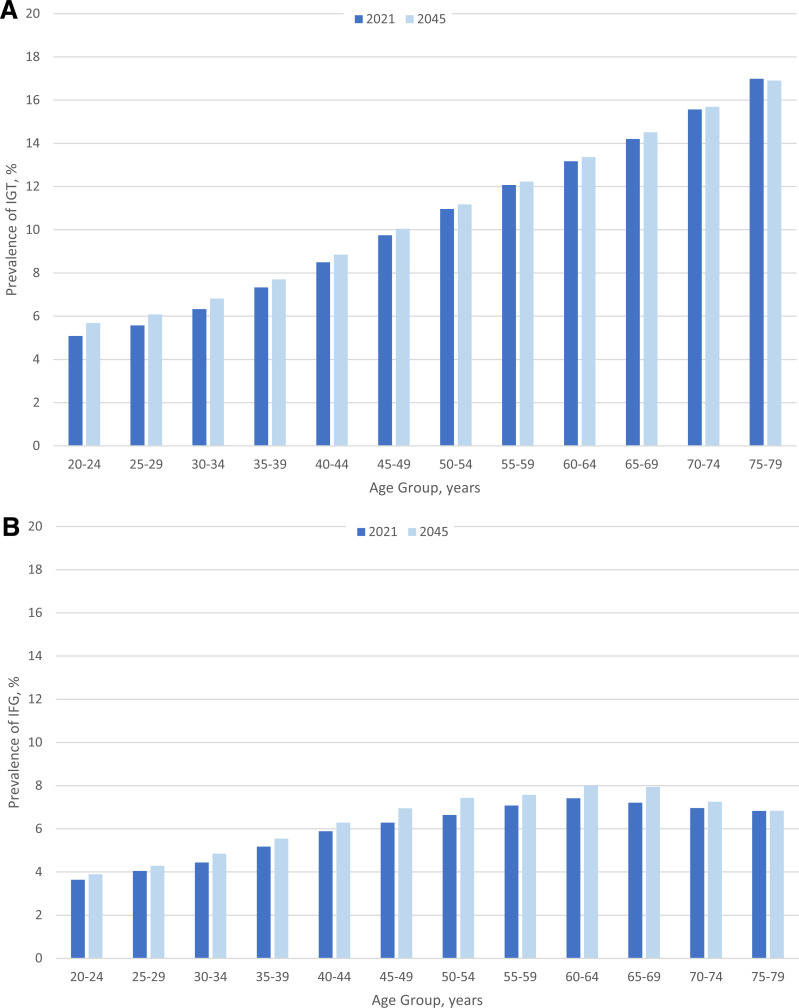
The proportion of adults with IGT increased significantly with age (Fig. 2). By 2045, the prevalence of IGT is projected to grow in adults aged 20–74 years but slightly decline among those aged 75–79 years. The prevalence of IFG in 2021 was higher in older age, peaking among adults aged 60–64 years at 7.4%. By the year 2045, the global prevalence of IFG in adults is projected to increase across most age categories, but the prevalence of IFG among adults aged 75–79 years is projected to be similar to that in 2021.
Figure 2.
Prevalence of IGT (A) and IFG (B) in adults aged 20–79 years in 2021 and 2045 by age group. IGT was defined as 2-h postload glucose levels of 7.8–11.1 mmol/L (140–99 mg/dL). IFG was defined as fasting plasma glucose levels of 6.1–.9 mmol/L (110–125 mg/dL).
Across World Bank income classification categories, the age-adjusted IGT prevalence in 2021 was highest for high-income countries (11.2%) and was lowest for middle-income countries (8.5%) (Table 2). For IFG, the age-adjusted prevalence estimates in 2021 were highest among high-income countries (6.4%) and lowest among low-income countries (5.0%). The age-adjusted prevalence of IFG and IGT is projected to increase across all income classification categories, with the largest relative growth in the number of people with prediabetes occurring in low-income countries. There will be a projected 130% increase in the number of people in low-income countries with IGT from 2021 to 2045 versus 38% in middle-income and 8% in high-income countries. For IFG, there will be a projected 122% increase in the number of people with IFG from 2021 to 2045 versus 41% in middle-income countries and 6% in high-income countries.
The prevalence of IGT and IFG in 2021 was similar for males and females (Supplementary Fig. 1). IGT was more common in urban (vs. rural) areas in 2021, but the prevalence of IFG did not differ across setting (Supplementary Fig. 2).
Conclusions
In 2021, the age-adjusted prevalence of IGT and IFG was 9.1% (464 million) and 5.8% (298 million) among adults aged 20–79 years worldwide. The 2021 prevalence estimates for both IGT and IFG rose substantially with increasing age. The 2021 prevalence estimates for both IGT and IFG were highest in high-income countries, with the largest relative growth in the number of people in 2045 with IGT and IFG occurring in low-income countries. By 2045, the global prevalence of IGT and IFG is projected to increase to 10.0% (638 million) and 6.5% (414 million), respectively.
Our estimate of the global prevalence of IGT was consistent with previous estimates. Atlas 9 estimated the age-adjusted global prevalence to be 8.6% (18), compared with 9.1% in our analyses. This difference indicates a small increase in the global prevalence of IGT from 2019 to 2021. However, there was considerable overlap in the 95% CI for both estimates. Additionally, our analysis and Atlas 9 used a different set of studies to generate global estimates of IGT, which may limit direct comparison.
The growing burden of prediabetes underscores the importance of effectively implementing diabetes prevention policies and interventions. In the U.S., a national program modeled after the Diabetes Prevention Program was established in 2010 to slow the progression from prediabetes to diabetes at the population level (19). Similar programs have been created in other high-income and middle-income countries (10,20,21). However, lower-income countries are less likely to have the resources, personnel, and public health and health care infrastructure needed to implement and maintain these efforts at a national level. There is an urgent need for effective strategies that can prevent diabetes progression in low-income settings, such as community-based and group-based lifestyle interventions using lay personnel (22). Other diabetes prevention strategies could be addressed through population-level changes in public health policy (e.g., regulation of food marketing and taxation) and educational campaigns (e.g., transparency in food labeling) without adding extra burden to the existing health care infrastructure (23). This is particularly important because these countries are expected to have the largest relative growth in prediabetes prevalence over the next 25 years. It is not clear whether these countries have the infrastructure to manage prediabetes cases and subsequent diabetes cases and the complications that may follow.
Urbanization is associated with an increased prevalence of obesity and diabetes (24). Consistent with prior research, we found that the prevalence of IGT was higher in urban (vs. rural) settings. The adoption of sedentary behaviors and “Western” dietary patterns may explain the link between urbanization and worse cardiometabolic health (24).
The availability of global data on prediabetes in the literature was poor. We had high-quality data sources from 43 countries with which to generate estimates of IGT. We also provided the first global estimates of IFG based on high-quality information for 40 countries. Overall, only about one-third of all countries had high-quality data for IFG or IGT. This highlights the need for improvements in population surveillance for prediabetes, especially in low-income settings, where few data were available. Continuing and expanding global surveillance efforts, such as the WHO STEPS surveys, can help to provide data to fill this gap.
Our study provides a comprehensive assessment of the global burden of prediabetes by including data on both IGT and IFG. We systematically reviewed and extracted data from over 7,000 published articles and used rigorous methods to estimate prevalence. We also attempted to source data from the gray literature by way of contacting ministries of health and regional partners and requesting data.
The limitations of our systematic review reflect those of the existing literature on prediabetes. First, the studies included in our analyses had considerable differences in population, sampling methodology, and date or period of data collection. We sought to reduce this heterogeneity by analyzing contemporary, high-quality studies. Nonetheless, these methodological differences likely influenced the comparability of estimates across countries. Second, we only examined two definitions of prediabetes (IGT and IFG based on the WHO criteria). Currently, there is no consensus definition of prediabetes. There are at least five different definitions endorsed by different professional organizations and guidelines based on fasting glucose, 2-h glucose, or HbA1c (1). Studies that reported only the American Diabetes Association (ADA) criteria for IFG were not considered in this report. The prevalence of IFG based on ADA criteria (5.5–6.9 mmol/L or 100–125 mg/dL) is, by definition, higher than that for estimates based on the WHO IFG criteria (6.1–6.9 mmol/L or 110–125 mg/dL). We also did not estimate the prevalence of prediabetes defined by HbA1c due to the limited availability of prediabetes defined by HbA1c in the international scientific literature. Broadening the use of HbA1c testing may be useful for improving global surveillance efforts on prediabetes, as HbA1c is a non–fasting test (no participant preparation is required) and can be convenient for large-scale surveys and thus population surveillance. Again, there is a lack of consensus on HbA1c-defined prediabetes, with the ADA endorsing 39–46 mmol/mol (5.7–6.4%) (1,25) and the International Expert Committee endorsing the more specific definition of 42–46 mmol/mol (6.0–6.4%) (1,26). Third, we considered the prevalence of IGT and IFG separately, as studies rarely had both measures available; however, the overlap between the IFG and IGT populations may be limited (3). Fourth, our projections to 2045 are based on projected demographic changes in age and sex distribution and the urban-to-rural ratio and did not factor in changes in other important determinants of prediabetes, e.g., changes in BMI. Fifth, our extrapolation approach for missing data was informed by expert consensus but has not been formally validated. Nonetheless, extensive extrapolation for sparse or missing data are required for generating global estimates for any health condition (27,28). Lastly, publications that were published after our initial search for the IDF Diabetes Atlas, 10th edition, were not considered.
In conclusion, the global burden of prediabetes based on WHO definitions of IFG and IGT is substantial and growing. Effective prevention, especially in low-income countries, is needed to slow the diabetes epidemic. High-quality data, which are currently unavailable for approximately two-thirds of countries worldwide, will be critical for global surveillance efforts. Reaching consensus definitions for prediabetes will facilitate comparisons of prevalence estimates across regions and time. Our findings highlight opportunities for improved epidemiologic surveillance of prediabetes and the need for improved efforts to reduce its global burden.
Article Information
Acknowledgments. The authors thank all those who have supported the production of the IDF Diabetes Atlas, 10th edition, by providing additional diabetes data where needed. We thank Professors Agus Salim and Baker Heart and the Diabetes Institute Australia for reviewing the statistical methodology employed in this edition. We also thank all our collaborators from Johns Hopkins University: Daisy Duan, Kathryn Foti, Fernando Mijares Diaz, Olive Tang, Amelia Wallace, Sui Zhang, and Dan Wang for their involvement in the abstract and full-text reviews.
Funding. The IDF Diabetes Atlas, 10th edition, was supported by an educational grant from the Pfizer-MSD Alliance, with the additional support of Sanofi and Novo Nordisk.
Duality of Interest. E.S. is an associate editor at Diabetes Care and recused herself from consideration of the manuscript. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. Authors made the following contributions: conception and design, M.R.R., M.F., D.J.M., and E.S.; analysis of data, K.O.; initial drafting of the article, M.R.R. and M.F.; critical revision of the article, M.R.R., M.F., K.O., B.O., J.B.E.-T., E.J.B., D.J.M., and E.S.; and final approval of the version to be submitted, M.R.R., M.F., K.O., B.O., J.B.E.-T., E.J.B., D.J.M., and E.S. M.R.R. and M.F. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this work were presented in abstract form at the European Association for the Study of Diabetes, 19–23 September 2022.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.22639039.
M.R.R. and M.F. contributed equally.
References
- 1. Echouffo-Tcheugui JB, Selvin E. Prediabetes and what it means: the epidemiological evidence. Annu Rev Public Health 2020;42:59–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Defronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009;58:773–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Abdul-Ghani MA, Tripathy D, DeFronzo RA. Contributions of β-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting glucose. Diabetes Care 2006;29:1130–1139 [DOI] [PubMed] [Google Scholar]
- 4. Nathan DM, Davidson MB, DeFronzo RA, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care 2007;30:753–759 [DOI] [PubMed] [Google Scholar]
- 5. Richter B, Hemmingsen B, Metzendorf MI, Takwoingi Y. Development of type 2 diabetes mellitus in people with intermediate hyperglycaemia. Cochrane Database Syst Rev 2018;10:CD012661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Warren B, Pankow JS, Matsushita K, et al. Comparative prognostic performance of definitions of prediabetes: a prospective cohort analysis of the Atherosclerosis Risk in Communities (ARIC) study. Lancet Diabetes Endocrinol 2017;5:34–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huang Y, Cai X, Mai W, Li M, Hu Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ 2016;355:i5953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Howells L, Musaddaq B, McKay AJ, Majeed A. Clinical impact of lifestyle interventions for the prevention of diabetes: an overview of systematic reviews. BMJ Open 2016;6:e013806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tuomilehto J, Lindström J, Eriksson JG, et al.; Finnish Diabetes Prevention Study Group . Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344:1343–1350 [DOI] [PubMed] [Google Scholar]
- 10. Pan X-R, Li GW, Hu Y-H, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 1997;20:537–544 [DOI] [PubMed] [Google Scholar]
- 11. International Diabetes Federation . IDF Diabetes Atlas, 9th edition. Brussels, Belgium, International Diabetes Federation, 2019 [Google Scholar]
- 12. Guariguata L, Whiting D, Weil C, Unwin N. The International Diabetes Federation Diabetes Atlas methodology for estimating global and national prevalence of diabetes in adults. Diabetes Res Clin Pract 2011;94:322–332 [DOI] [PubMed] [Google Scholar]
- 13. International Diabetes Federation . IDF Diabetes Atlas, 10th edition. Brussels, Belgium, International Diabetes Federation, 2021 [Google Scholar]
- 14. Saaty TL. Decision making with the analytic hierarchy process. Int J Serv Sci 2008;1:83–98 [Google Scholar]
- 15. Sun H, Saeedi P, Karuranga S, et al. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 2022;183:109119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. United Nations . 2018 Revision of World Urbanization Prospects. New York, NY, United Nations Department of Economic and Social Affairs, Population Division, 2018 [Google Scholar]
- 17. The World Bank . World Bank Country and Lending Groups. Washington, DC, The World Bank, 2020. Accessed 1 March 2023. Available from https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- 18. Saeedi P, Petersohn I, Salpea P, et al.; IDF Diabetes Atlas Committee . Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract 2019;157:107843. [DOI] [PubMed] [Google Scholar]
- 19. Ely EK, Gruss SM, Luman ET, et al. A national effort to prevent type 2 diabetes: participant-level evaluation of CDC’s National Diabetes Prevention Program. Diabetes Care 2017;40:1331–1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Valabhji J, Barron E, Bradley D, et al. Early outcomes from the English National Health Service Diabetes Prevention Programme. Diabetes Care 2020;43:152–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 2006;49:289–297 [DOI] [PubMed] [Google Scholar]
- 22. Shirinzadeh M, Afshin-Pour B, Angeles R, Gaber J, Agarwal G. The effect of community-based programs on diabetes prevention in low- and middle-income countries: a systematic review and meta-analysis. Global Health 2019;15:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Galaviz KI, Weber MB, Straus A, Haw JS, Narayan KMV, Ali MK. Global diabetes prevention interventions: a systematic review and network meta-analysis of the real-world impact on incidence, weight, and glucose. Diabetes Care 2018;41:1526–1534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications. Nat Rev Endocrinol 2013;9:13–27 [DOI] [PubMed] [Google Scholar]
- 25. American Diabetes Association . Standards of Medical Care in Diabetes—2022. Diabetes Care 2022;45(Suppl. 1) [DOI] [PubMed] [Google Scholar]
- 26. International Expert Committee . International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32:1327–1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Roth GA, Mensah GA, Johnson CO, et al.; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group . Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol 2020;76:2982–3021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zhou B, Lu Y, Hajifathalian K, et al.; NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016;387:1513–1530 [DOI] [PMC free article] [PubMed] [Google Scholar]