Abstract
Background
Reiki is a biofield therapy which is based on the explanatory model that the fields of energy and information of living systems can be influenced to promote relaxation and stimulate a healing response.
Objective
To conduct a pragmatic within-subject pilot trial of a remote Reiki program for frontline healthcare workers’ health-related symptoms during the COVID-19 pandemic.
Methods
Healthcare professionals in the UK (eg, physicians, nurses, and paramedics) were eligible to sign up for a distance Reiki program and were also invited to participate in the research study. Eight Reiki practitioners simultaneously gave each participant Reiki remotely for 20 minutes on 4 consecutive days. Feasibility of the research was assessed, including recruitment, data completeness, acceptability and intervention fidelity, and preliminary evaluation of changes in outcome measures. Participants’ stress, anxiety, pain, wellbeing, and sleep quality were evaluated with 7-point numerical rating scales. Measures were completed when signing up to receive Reiki (pre) and following the final Reiki session (post). Pre and post data were analyzed using Wilcoxon signed ranks tests.
Results
Seventy-nine healthcare professionals signed up to receive Reiki and took the baseline measures. Of those, 40 completed post-measures after the 4-day intervention and were therefore included in the pre-post analysis. Most participants were female (97.5%), and the mean age was 43.9 years old (standard deviations = 11.2). The study was feasible to conduct, with satisfactory recruitment, data completeness, acceptability, and fidelity. Wilcoxon signed ranks tests revealed statistically significant decreases in stress (M = −2.33; P < .001), anxiety (M = −2.79; P < .001) and pain (M = −.79; P < .001), and significant increases in wellbeing (M = −1.79; P < .001) and sleep quality (M = −1.33; P = .019).
Conclusions
The Reiki program was feasible and was associated with decreased stress, anxiety and pain, and increased wellbeing and sleep quality in frontline healthcare workers impacted by the COVID-19 pandemic.
Keywords: Reiki, healthcare professionals, stress, anxiety, pain, COVID-19
Introduction
The COVID-19 pandemic has caused considerable workplace stress for healthcare professionals throughout the world,1-4 resulting in a critical public health issue. Meta-analyses of studies across different countries revealed that healthcare workers’ anxiety, stress, depression, sleep, and post-traumatic stress disorder were significantly increased during the pandemic.5-7 The United Kingdom (UK) had 1 of the highest death rates from COVID-19 for those under 65 years old and 1 of the highest levels of hospitalizations.8,9 Likewise, the pandemic increased health-related symptoms in frontline healthcare workers in the UK, including moderate to severe levels of anxiety and depression. 2 The main factors that determined healthcare workers’ reduced wellbeing during the pandemic included having direct patient contact as a frontline healthcare worker, being reassigned to a different job or role than usual,1,2 and fear of the coronavirus. 10 Strategies that improve the mental health of frontline healthcare workers are needed to mitigate this increased stress from the pandemic, particularly those that can be administered remotely within the constraints of social distancing.
Reiki is a form of biofield therapy originating in Japan and is based on the explanatory model that fields of energy and information surrounding and within living systems can be influenced to promote relaxation and stimulate a healing response. 11 Reiki is commonly provided as part of integrative medicine programs and offerings in many hospitals throughout the UK and US12,13 due to its low-cost, minimal risk, and ability to promote relaxation, reduce pain and stress, and theoretically promote the body’s natural ability to heal. 14 Reiki can be practiced in person, with practitioners’ hands placed on and/or above the body, or remotely from a distance with or without any direct communication or contact between practitioner and receiver. Because Reiki can be administered remotely, it is an especially useful therapy during times of social distancing and community lockdowns, such as during the COVID-19 pandemic. 15
Meta-analyses and systematic reviews report that Reiki can improve psychological and physical health symptoms,16-21 including under randomized controlled conditions (eg, compared to sham-Reiki or standard-of-care), where Reiki has been shown to reduce anxiety,22-24 depression,25,26 burnout,27,28 pain,22,29-32 and increase relaxation and well-being.33,34 There are only a few studies evaluating Reiki in healthcare worker populations, with results showing reductions in stress in nurses administering self-Reiki, 35 reduced burnout in mental health clinicians, 28 reduced stress, respiratory rate, and heart rate 36 and improved stress coping and fatigue in nurses. 37
Distance Reiki use is on the rise since the pandemic, given the need for social distancing, limited contacts, and with many businesses required to be closed. A qualitative study with ten Reiki practitioners in the UK reported that they saw value in adapting their practice by using technology and distance Reiki but believed that distance Reiki could not replace in-person practice. 38 While many studies support in person Reiki for mental and physical health outcomes, less is known about the effects of distance Reiki. To date, 7 studies on distance Reiki have been conducted which have shown benefits to psychological health, but mixed results with respect to pain.37,39-44 For example, a randomized controlled trial (RCT) found a significantly lower heart rate and blood pressure with distance Reiki after caesarian section, but no difference in pain, compared to usual care. 39 Whereas in another study, Reiki decreased pain, anxiety, and fatigue in oncology patients compared to usual care. 40 Another study resulted in improvements in pain and quality of life following distance Reiki for patients with rheumatoid arthritis compared to an unspecified control group. 41
In terms of Reiki studies with professional nonpatient populations, distance Reiki for software professionals reduced perceived stress, but there was no statistical comparison between the Reiki and control groups. 42 A recent study evaluated distance Reiki for digital health employees during the COVID-19 isolation period and observed reductions in stress and anxiety compared to no treatment control. 43 To date, only 1 distance Reiki study has been conducted with healthcare professionals. The RCT assessed distance Reiki with nurses and found improvement in fatigue and coping strategies toward stress compared to control. 44 However, there was an inadequate description of the recruitment procedure, data collection, and the Reiki intervention, and the study was conducted in only 1 hospital.
This is the first study evaluating distance Reiki for health symptoms with populations of physicians, nurses, and other frontline healthcare workers across multiple healthcare organizations. We conducted a pragmatic within-subjects pilot trial of the UK Reiki Medic-Care program during the COVID-19 pandemic. Reiki Medic-Care is a non-profit organization that offers no-cost distance Reiki to National Health Service (NHS) frontline healthcare professionals in the UK. The primary objective was to test the feasibility of research procedures for a future RCT by assessing participant recruitment and retention, data completeness, acceptability, and fidelity of the intervention. The secondary objective was to evaluate preliminary changes in outcome measures, including clinically relevant changes. We assessed stress, anxiety, pain, wellbeing, and sleep quality before (pre) and after (post) 4 consecutive days of distance Reiki. Based on previous studies, we expected all outcome measures to significantly improve following Reiki.
Materials and Method
Participants and Recruitment
Participants were frontline healthcare professionals, including nurses, physicians, ambulance paramedics, and medical personnel working for the National Health Service (NHS) in the UK. Any frontline NHS worker could receive distance Reiki at no cost as part of the Reiki Medic-Care program. A sample size calculation was not performed due to the study being a pilot pragmatic within-subjects trial. Healthcare workers were notified of the Reiki program through word of mouth, friends and family, social media, and flyers distributed through hospital/senior ward staff and doctors. Those who were interested signed up using the online booking system and opted into the study by ticking a box (yes or no). Because this study was evaluating a pre-existing program for NHS healthcare workers, it was exempt from Institutional Review Board approval from the NHS Health Research Authority. The STROBE guidelines were used to ensure proper reporting of this observational study. 45
The Reiki Medic-Care Program
The Reiki Medic-Care is a non-profit initiative founded in June 2020 and launched in September 2020. The goal of the program is to extend free Reiki services to public hospital medical professionals who are suffering from burnout symptoms through setting up insured practitioner teams in multiple countries. To date, 592 sessions have been administered in the UK, including England, Scotland, Wales, and Northern Ireland. The program is entirely based on word of mouth with currently no public marketing operations.
There were 260 Reiki practitioners in the program at the time of this study. Reiki practitioners are recruited into the program through their membership with Reiki organisations all of which are members of The Reiki Council, the UK’s governing board for Reiki. All Reiki practitioners were trained and initiated in person to Reiki level II or Master level in Usui Reiki and were fully insured for public practice. They also had to be a current, verified member of an organisation that is a member of the Reiki Council. All Reiki practitioners agreed to terms and conditions including a non-disclosure statement. Reiki Medic-Care and all directors were insured for public liability. A Reiki Medic-Care volunteer acted as the Booking and Portal Administrator.
Procedure
Reiki Practitioners
Eight Reiki practitioners were allocated per participant, based on the untested theory by Reiki Medic-Care that use of more practitioners might provide a stronger effect than use of only 1 practitioner. The participants were not given any information about the Reiki practitioners. The same 8 Reiki practitioners were used for the same participant each day unless an unavoidable conflict occurred. If a Reiki practitioner was unavailable at the time of a request allocated to their team, a practitioner from another group would be arranged on a first response basis through a private Facebook page for practitioners. Reiki practitioners could see a list of names of the other practitioners in their group, but without any contact details. They were not formally introduced to each other but may have recognised names of people they already knew on the list. Practitioners were asked not to communicate with anyone other than the program administration about a specific request or client. Reiki practitioners were given the name, date of birth, location, and picture of the participant to facilitate the connection.
Reiki Sessions
Participants scheduled their sessions via self-referral using the online booking system. Participants were encouraged to book their appointments outside of working hours, when they could make themselves comfortable while receiving the treatment. They were also told that the treatment could be delivered during their sleep. Each participant chose the dates and times that suited them best within opening hours (between 8am – 11:30pm). Reiki requests were allocated systematically to practitioner groups in the order in which the request was accepted.
Participants received 20 minutes of Reiki for 4 consecutive days from the 8 practitioners. In addition to a standard distance Reiki treatment being 20 min, selection of this duration was also due to authors’ discussions with medical professionals, particularly medics, relating to the amount of time that they might ‘allow’ themselves to receive or fit into their busy schedule. The 4 sessions were to build up a cumulative effect, recommended by Hawayo Takata, who helped bring Reiki from Japan to the Western World. 46 Other studies have used the same duration and frequency.42,43
There was no communication between the practitioner and client before, during, or after the session.
Healthcare workers who signed up for the Reiki program were provided with text and video instructions for the sessions, with a link to a YouTube video. They were instructed to sit or lie down quietly for the 20 minutes while the team sent them Reiki. They were instructed to find a quiet place, turn off electronic devices, sit in a chair or lie down on a sofa or bed. They were also told they could have music on during the session. They were told to breathe slowly and relax. They were told that they might notice subtle signs in their body, feel relaxed, or fall asleep, and that these are all normal reactions to receiving Reiki. They were told to drink water after the session and make a note of anything that came up for them. We do not know how many participants followed the instructions.
The Reiki procedure was semi-structured, with practitioners either following a systematic approach using set hand positions, or an intuitive approach (eg, byosen scanning, or identifying the areas of the body most in need of healing) following perceived responses from the body, depending on the practitioners' preferred way of working. Reiki practitioners were told to cover each of the following locations over the 20-minute session, if using the systematic approach: 1) the forehead/frontal lobe, eyes, sinus, pituitary gland/hypothalamus; 2) ears, temporal lobe, upper jaw; 3) pineal gland, occipital area, brain stem/top of spinal cord; 4) heart/thymus; 5) lungs; 6) liver/gallbladder/stomach/pancreas; 7) kidneys/adrenals; 8) large and small intestines.
Data Collection
Measures were taken on a custom-built online data collection system when signing up for Reiki and immediately after the fourth and final session, in which they were emailed a link to the questionnaire. The data were entered directly by the participant and stored on an online system until downloaded as a.csv file. Participants’ names were automatically deidentified before details were added to the data system.
Feasibility
Feasibility of the study was assessed via recruitment, data completeness, acceptability, and fidelity.
Recruitment
We assessed recruitment rates, eligibility criteria, and how relevant the intervention is to the intended study population. We assessed variables across different participant groups when possible, including age, gender, and occupation.
Data Completeness
We assessed whether the data were relatively complete and usable, and whether the measures are appropriate for the specific population and intervention. Using study records and administrative data, loss to follow up rates were tracked and documented. Data collected at each time point were evaluated for quality and completeness using Microsoft Excel.
Acceptability
We assessed retention; adherence to study procedures, intervention attendance, and understanding of the procedures and intervention; burden; acceptability and satisfaction of the intervention; and safety and unexpected adverse events.
Fidelity of the Intervention
We assessed the proportion of Reiki sessions that were delivered in a manner consistent with the manualized consensus intervention, including total number of Reiki practitioners per participant, and sequencing and timing of sessions.
Health-Related Symptoms
The questionnaire was based on the Measure Yourself Medical Outcome Profile (MYMOP), a validated patient reported outcome tool to assess general health. 47 The questionnaire was adapted by the authors to include preestablished symptoms based on their negative impact by the pandemic, including stress, anxiety, pain, wellbeing, and sleep quality.1-7 This preselection was implemented to enable comparing participants scores within symptoms. Participants report on each symptom on a 7-point numeric rating scale from “as good as it could be” (0) to “as bad as it could be” (6), with a lower score indicating better general health/quality of life.
Minimal Clinically Important Difference
In addition to statistical significance, it is important to understand the changes in outcomes in a clinically meaningful way. Based on previous studies using the MYMOP,47,48 we defined the minimal clinically important difference (MCID) as a ≥1 point improvement (decrease) in scores, rounding up from the recommended .8, which is stated to be a clinically relevant change.47,48 Furthermore, improvements of 1.11 points have been stated to represent “a little better” and improvements of 2.05 points have been stated to represent “much better.” 47 Thus, we will report the proportion of participants that met MCID (≥1 point improvement) at post, as well as the proportion that achieved improvements that were “a little better” (≥1.11) and “much better” (≥2.05).
Qualitative Feedback
At the end of the questionnaire for the pre measure, participants could add any additional symptoms/complaints in a text box and at the end of the post measure, they could provide any comments about the session. Participants could also provide feedback via email.
Data Analysis
Normality of the data was assessed using a Shapiro-Wilks test. Data that were not normally distributed were analyzed via Mann-Whitney U test or Kruskal-Wallis H test to compare pre scores and change scores between completers and non-completers and between job categories, respectively. A Wilcoxon signed-ranks test was conducted to analyze changes in scores from pre to post and effect sizes (r) were also calculated. A post hoc power analysis of means was conducted with power set to .80. P values were set to P < .05. All analyses were conducted using IBM’s SPSS version 22.0.
Results
Feasibility
Recruitment
Recruitment for research began in September 2020 and went until October 2021. Recruitment was achieved primarily through word of mouth, flyers posted in hospitals, and social media posts. Thus, it was not possible to determine how many healthcare professionals were exposed to information about the study during the study period.
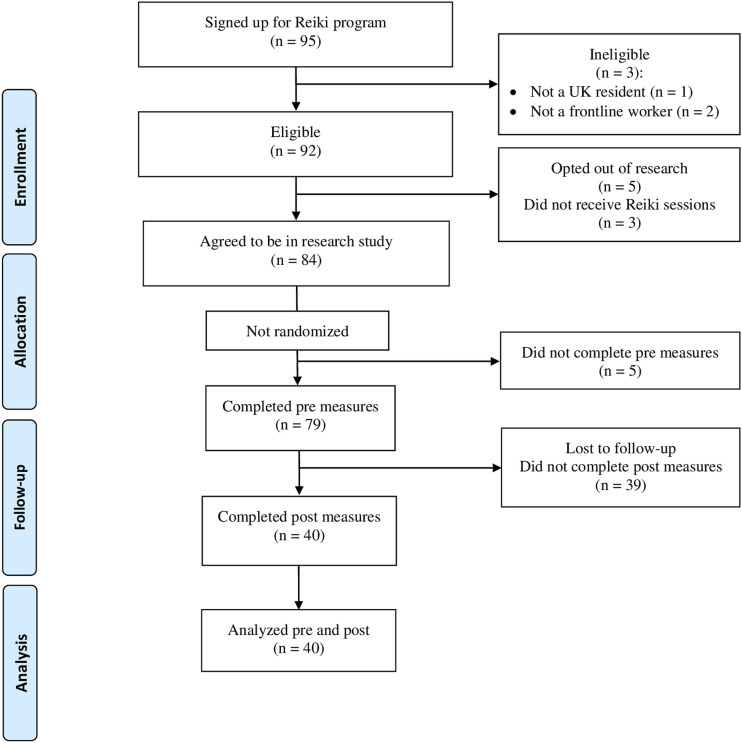
Of those who signed up to receive Reiki (N = 95), 3 were ineligible for the program due to not being a frontline healthcare worker (n = 2) or a UK resident (n = 1). Of the ninety-two eligible frontline healthcare workers that signed up for the Reiki program, N = 84 agreed to be in study (91.3%). Of those who agreed to be in the study, N = 79 took the measures at pre, and of those, N = 40 also took the measures at post (51% retention). For further details, see the participant CONSORT diagram displayed in Figure 1.
Figure 1.
Participant flow diagram.
Demographics
The majority of participants (N = 40) were female (97.5%) and the mean age was 43.9 years (range 21-64). Participants were from 32 different locations across the UK, including London, Nottingham, Sheffield, Leeds, Glasgow, and many others. In terms of occupation type, the sample included nurses (n = 15; 37.5%), physicians (n = 14; 35%), and other clinical staff such as therapists or patient care assistants (n = 11; 27.5%).
Data Completeness
Levels of data completion were satisfactory. At baseline (pre), 94.0% of participants completed the measures, and 50.6% of those participants completed the measures at post. There was no missing data for the outcome measures. Some participants were recorded with multiple IDs (#8 instances) with different numbers, but this was able to be rectified and all participants’ data were consolidated.
The measures were appropriate for the specific population and intervention based on typed qualitative feedback of their symptoms and concerns. Many participants reported having covid or long covid, suffering from covid vaccine side effects, or feeling stressed about working with COVID-19 patients. In terms of symptoms, they reported experiencing a lot of stress and anxiety, PTSD, pain, fatigue, and sleep problems. These complaints are line with the outcome measures used in the current study (stress, anxiety, pain, wellbeing, and sleep quality).
Using a Mann-Whitney U test, there were no significant differences (all P values >.4) in occupation for those that completed the pre and post measures (completers, N = 40) and those that did not (non-completers/dropouts, N = 39). We were unable to test gender differences with only 1 male. With respect to age, completers were significantly older (M = 43.9, SD = 11.2; mean rank = 49.6) than non-completers (M = 37.3, SD = 8.8; mean rank = 34.9), P = .005.
In terms of outcome measures, there were no significant differences between pre scores for participant completers (ie, completed pre and post measures) and non-completers (ie, did not complete post measures) (Table 1).
Table 1.
Means (M) and Standard Deviations (SD) for all Outcome Measures at Pre for Completers (n = 40) and Non-completers (n = 39).
| Measure | Completers n = 40 | Non-completers n = 39 | p | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Stress | 3.90 | 1.34 | 3.90 | 1.05 | .790 |
| Anxiety | 3.78 | 1.49 | 3.92 | 1.48 | .717 |
| Pain | 1.98 | 1.59 | 2.46 | 1.57 | .135 |
| Wellbeing | 3.53 | 1.30 | 3.62 | 1.14 | .406 |
| Sleep quality | 3.40 | 1.57 | 3.15 | 1.63 | .996 |
Note: Analysis was via Mann-Whitney U Test.
Acceptability
Of the 92 eligible participants that signed up for the Reiki program, 5 opted out of research procedures (5.3%). Adherence to procedures was achieved in all but 6 participants; 3 signed up but did not receive Reiki (3.2%) because they did not provide dates that they were available, and 3 participants received Reiki but reported in the qualitative feedback that they were not able to “access the session” (n = 1), “receive the phone call to start the treatment” (n = 1) or they forgot about the session (n = 1). Two of those, those that did not understand the procedure and intervention, did not complete the post outcome measures, and were not included in the final analysis.
There was very little study burden since the participants could sleep during their Reiki sessions and the outcome measures took 5 min or less to complete.
Acceptability and satisfaction of the intervention to participants via qualitative feedback (n = 20) was overwhelmingly positive, with just 1 neutral or negative comment: “I hate to say so, but I didn’t feel anything and my life seems to be more stressful, hectic and with obstacles than usual. I wasn’t tuned in and I kind of forgot on the sessions at the time of sending reiki but still... Cannot say it worked for me at all. Maybe I will see benefits a few days later … Thanks for trying though and I really do appreciate it. I hope it will work better for other people.” This was the participant who forgot about the session, limiting the weight of this comment. Some sample brief positive comments include: “I have had sinus problems for over a year. Almost fully resolved after my sessions. Sleeping better. Less reactive to stress.” “Just amazing. Thank you so much. My stress levels and associated back pain have reduced considerably.” “Thank you very much for facilitating the Reiki sessions this week. I was slightly sceptical as to how/if I would experience the same benefits as receiving Reiki in person, however I found it to be deeply relaxing, and instantly felt positive physical and emotional responses both during and after the sessions.”
There were no adverse events reported and no safety concerns, as it was a remote, no contact intervention.
Fidelity
The Reiki Medic-Care program displayed high fidelity, with 100% of the sessions being delivered in accordance with the intervention protocol, including the total number of Reiki practitioners, sequencing, and timing of sessions.
Health-Related Symptoms
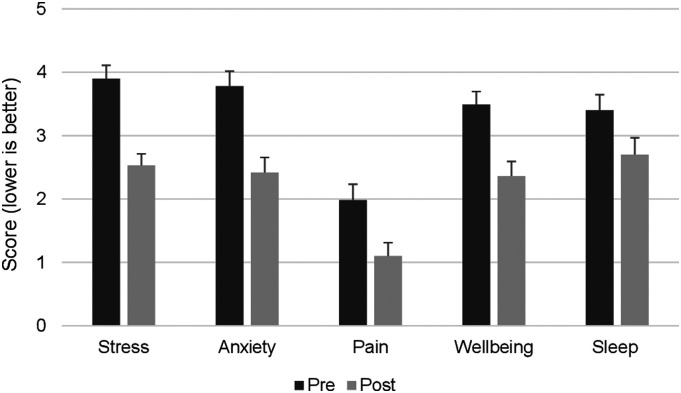
The means and standard errors of the mean scores for all outcomes at pre and post are displayed in Figure 2. Shapiro-Wilk test revealed that the data were not normally distributed (all P values <.05), therefore, nonparametric tests were employed. A Wilcoxon signed rank test revealed a significant difference between pre and post for all outcome measures: stress (pre Mdn (IQR) = 4.0 (2), post Mdn (IQR) = 2.0 (1); P < .001, r = .634), anxiety (pre Mdn (IQR) = 4.0 (2), post Mdn (IQR) = 2.0 (2); P < .001, r = .698), pain (pre Mdn (IQR) = 2.0 (2), post Mdn (IQR) = 1.0 (2); P < .001, r = .630), wellbeing (pre Mdn (IQR) = 4.0 (1), post Mdn (IQR) = 2.0 (2); P < .001, r = .578), and sleep quality (pre Mdn (IQR) = 4.0 (1), post Mdn (IQR) = 3.0 (3); P = .019, r = .371). The mean ranks, sum of ranks, and statistics for all symptoms from pre to post are displayed in Table 2. Effect sizes (r) ranged from medium (.30-.50) to large (>.50).
Figure 2.
Means and standard errors of mean for all outcome measures at pre and post (N = 40). A decrease in scores indicates an improvement.
Table 2.
Mean Ranks, Sum of Ranks, and Statistics for all Symptoms from Pre to Post (n = 40).
| Measure Pre-Post | Negative Ranks | Positive Ranks | z | p | r | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean | Sum of Ranks | n | Mean | Sum of Ranks | ||||
| Stress | 29 | 16.41 | 476.00 | 3 | 17.33 | 52.00 | −4.013 | <.0001 | .634 |
| Anxiety | 30 | 18.40 | 552.00 | 4 | 10.75 | 43.00 | −4.416 | <.0001 | .698 |
| Pain | 21 | 11.74 | 246.50 | 1 | 6.50 | 6.50 | −3.982 | <.0001 | .630 |
| Wellbeing | 29 | 17.50 | 507.50 | 5 | 17.50 | 87.50 | −3.656 | <.0001 | .578 |
| Sleep quality | 18 | 13.81 | 248.50 | 7 | 10.93 | 76.50 | −2.347 | .019 | .371 |
Note: Analysis was via Wilcoxon Signed Ranks test.
Clinical Relevance
The percentage of participants that met MCID at post ranged from 45% for sleep quality to 75% for anxiety, the percentage of participant that were “a little better” ranged from 25% for pain to 50% for stress, and the percentage of participant that were “much better” ranged from 12.5% for pain and sleep quality to 20% for stress and anxiety (see Table 3).
Table 3.
Percentage of Participants That Met a Minimal Clinically Important Difference. (MCID), and Were “a Little Better”, and “Much Better” at Post (n = 40).
| Measure | MCID (≥1) | “A Little Better” (≥1.11) | “Much Better” (≥2.05) |
|---|---|---|---|
| Stress | 72.5 | 50.0 | 20.0 |
| Anxiety | 75.0 | 47.5 | 20.0 |
| Pain | 52.5 | 25.0 | 12.5 |
| Wellbeing | 72.5 | 48.7 | 12.8 |
| Sleep quality | 45.0 | 32.5 | 12.5 |
Spearman correlations revealed no significant association between pre scores or change scores and age (all P values >.3). We were unable to test differences based on gender as there was only 1 male. Further, there were no significant differences in pre scores or change scores between nurses, physicians, or other healthcare workers, thereby justifying their inclusion as 1 cohort (see Table 4).
Table 4.
Means (M) and Standard Deviations (SD) for All Symptoms at Pre, and Symptom Change Scores (Δ) From Pre to Post for Nurses (n = 15), Physicians (n = 14), and Other Healthcare Workers (n = 11).
| Measure | Nurses | Physicians | Other Workers | p |
|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | ||
| Stress | 4.13 (1.06) | 3.50 (1.61) | 4.09 (1.30) | .570 |
| Δ Stress | −1.60 (1.50) | −1.00 (1.96) | −1.54 (1.69) | .973 |
| Anxiety | 3.80 (1.37) | 3.50 (1.74) | 4.09 (1.37) | .675 |
| Δ Anxiety | −1.40 (.98) | −1.07 (1.59) | −1.64 (1.69) | .808 |
| Pain | 2.00 (1.41) | 2.00 (1.80) | 1.91 (1.70) | .297 |
| Δ Pain | −.93 (1.16) | −.93 (1.07) | −.73 (1.10) | .760 |
| Wellbeing | 3.73 (1.16) | 3.50 (1.56) | 3.27 (1.19) | .921 |
| Δ Wellbeing | −1.47 (1.24) | −.85 (1.86) | −1.00 (1.67) | .525 |
| Sleep quality | 3.60 (1.45) | 2.86 (1.99) | 3.82 (.87) | .700 |
| Δ Sleep | −.87 (1.24) | −.21 (2.04) | −1.09 (1.87) | .413 |
Note: Analysis was via Kruskall-Wallis H test.
Post Hoc Power Analysis
A post hoc power analysis at .80 power revealed a needed sample size ranging from 9 to 40 to meet statistical significance. Specifically, a sample size of n = 11 would be required for stress at .800 power with an effect size of .806; n = 9 for anxiety at .837 power with an effect size of .960; n = 14 for wellbeing at .813 power with an effect size of. 716; n = 12 for pain, at .831 power with an effect size of .803; and n = 40 for sleep at .808 power with an effect size of .405. Thus, we have met the appropriate sample size to detect statistically significant changes for all outcome measures.
Discussion
This is the first study of distance Reiki for healthcare professionals including physicians, nurses, and other frontline healthcare workers. Results revealed the study to be feasible, demonstrating satisfactory recruitment, data completeness, acceptability, and fidelity. Strategies to improve the retention rate will be employed in future work, including providing remuneration and reminders to complete the measures. The intervention was acceptable to participants and demonstrated high fidelity. Preliminary results revealed significant improvement in all outcome measures from pre to post: stress, anxiety, pain, wellbeing, and sleep quality. The medium to large effect sizes and high proportion of participants meeting MCID indicates that the observed improvements following Reiki were clinically relevant. There were no statistically significant differences in baseline scores or changes in scores based on sociodemographic variables of age or occupation (nurses, physicians, and other healthcare workers).
The sample was mostly female with only 1 male participant, meaning gender differences could not be analyzed. The current study had a larger sample size than all other distance Reiki studies except for 1, which had the same sample size for the experimental group (N = 40). 38 The other distance Reiki studies ranged from a sample size of 8 39 to 3041,43 for the Reiki group. Therefore, the larger than average sample size of the current study is a strength compared to other distance Reiki studies. Further, a post hoc power analysis resulted in a needed sample size ranging from n = 9 – 40 depending on the symptom. Thus, our sample size of 40 met the requirements to be appropriately powered to reach statistical significance for all outcome measures.
While no other distance Reiki study has used the MYMOP, it has been used in studies of in-person Reiki.28,49-51 2 of those studies did not report means,28,49 making comparisons not possible. One study of 200 patients with irritable bowel syndrome or disease administered 5 Reiki sessions reported an overall pre score mean of 4.0 on the MYMOP, which decreased to 2.6 after 6 weeks of Reiki, 50 comparable to the results of the current study. In another study with a general population of adults seeking healing, MYMOP pre score means were 4.9 for symptom 1, which decreased to 2.1; 4.5 for symptom 2, which decreased to 2.3; and 4.3 for wellbeing, which decreased to 2.1 after 4 sessions of Reiki. 51 It is important to note that we preselected symptoms for the MYMOP, meaning comparisons with other studies are limited.
Only a few studies have been conducted on distance Reiki, and they also report benefits to psychological health and pain37,40-44 similar to in-person Reiki studies,16-21 but much more research is needed to confirm whether this is consistently the case. Future work comparing in-person with distance Reiki would better our understanding of the effects of Reiki across these different administration styles. Distance Reiki treatments are often 20 min, whereas in person Reiki sessions tend to be between 45-90 min. Like the current study, other distance Reiki studies have also used 20 min sessions,39,41,44 including 20 min over 4 consecutive days, where results indicated reduced stress and fatigue in nurses during COVID-19 pandemic, 44 and reduced pain and increased quality of life in arthritic patients. 41 1 study administered 20 min distance Reiki sessions over 3 consecutive days and the authors reported lower heart rates and blood pressure, but not pain, in patients following Caesarean section. 39 Variation in duration and frequency occurred across the rest of the distance Reiki studies, with 30 min sessions over 5 consecutive days, 40 5 min sessions over 21 consecutive days, 42 6 60-90 min sessions over 6 consecutive weeks, 37 and 7 42 min sessions over 3 consecutive weeks. 43 Therefore, there has yet to be a consensus on the appropriate duration and frequency of Reiki for any given population and/or condition, and thus, future work evaluating different Reiki “doses” and responses is needed.
Reiki may partially work through promoting the relaxation response,52,53 which is mediated by the parasympathetic nervous system 54 and therefore potentially reducing inflammation. 55 Studies of Reiki show reductions in some physiological markers of stress and inflammation, including reduced heart rate,56,57 blood pressure,22,27,56,57 and increased salivary immunoglobulin-A. 27 However, no studies have examined how the changes in symptoms following Reiki are mediated through biological mechanisms. Future research would benefit from including similar objective physiological measures to investigate mediators of improvements in stress, anxiety, pain, and other symptoms.
Limitations
There were several limitations of the current study that warrant discussion. First, as a pilot pragmatic within-subjects trial, there was no comparison group, limiting our ability to account for effects of attention, being observed, taking time to rest, or natural changes over time (eg, Hawthorne effect). However, not including a control group at this stage of research is recommended because the purpose is not to assess efficacy. Second, participants self-selected into the Reiki program, which cannot rule out expectation effects for the sessions. We were unable to prevent or account for these biases that may have had an influence on the results. Further, we did not ask participants about their level of expectation for the Reiki sessions. Future research will include questions on expectancy to assess its role in changes in outcomes.
We did not obtain information related to workplace variables that may have been impacted by the pandemic (eg, number of patients seen, work hours), though collecting those data would have strengthened the study. While we wanted to minimize participant burden with this pilot trial, we will be expanding on the questions with the addition of remuneration for participants in subsequent studies. We also do not know where participants took the measures, whether at work or outside of work, meaning it is possible they took the pre measures in a high stress environment (eg, work) and the post measures in a more relaxed environment (eg, home), for example.
Although nearly half of the participants did not take the post measures, this attrition rate is within normal range for observational studies of integrative and complementary medicine programs.58,59 It is not possible to ascertain why some participants did not complete the post measures, although time constraints of the frontline health professionals could be 1 reason. Regardless, there were no significant differences in pre-scores between participants that completed the post measures and those who did not, nor by occupation type. However, older participants were more likely to complete the measures than younger participants, highlighting the need to implement strategies to increase retention for younger participants in the future. We also do not know how many healthcare workers received information about the Reiki program, as recruitment was through word of mouth and paper and digital flyers. Efforts to increase recruitment in the future will include more direct recruitment methods such as emailing the healthcare workers about the program.
A major limitation is the lack of assessment of COVID-related variables which may have influenced outcome measures, such as whether the healthcare workers had direct COVID patient contact, changes in their workplace role, or fear of the virus, which are all main factors that determined healthcare workers’ reduced wellbeing during the pandemic1,2,10 However, we aimed to minimize participant burden for this pilot study. Future work will account for workplace-related variables and stressors.
Unlike in-person Reiki, the distance Reiki did not include communication between practitioner and client. This could be seen as a limitation; however, it also meant that the observed changes were not due to the therapeutic relationship. Furthermore, there was no compensation for participating in the study, and integrative medicine studies with monetary incentives tend to show higher retention rates.58,59 Therefore, future work will include compensation for questionnaire completion to increase participant retention. Lastly, the MYMOP was modified to include pre-established symptoms, which can be seen to limit its validity. However, its use is common practice in the UK healthcare system and enabled comparing the same symptoms across participants. Future research will use additional validated self-report measures to detect changes following Reiki.
This pilot study provided promising results to support conducting an RCT of the Reiki Medic-Care program in frontline healthcare professionals. Future work will also extend the Reiki program to other countries, in addition to the UK, providing a multinational data set. Subsequent studies will also aim to include a waitlist control group, larger sample size, and longitudinal data to evaluate whether the observed improvements in stress, anxiety, pain, wellbeing, and sleep quality are sustained over time. To date, no study of distance Reiki has assessed outcomes at a time longer than within 2 days of receiving the final Reiki session, Qualitative interviews will be employed to understand improvements from the participants’ perspective to provide a more robust understanding of the benefits of Reiki in this population.
Conclusions
This was the first distance Reiki study with a heterogenous group of healthcare workers from multiple hospitals. The goal of this study was to provide preliminary data to prepare for an RCT to evaluate the efficacy of the intervention with a fully powered trial. Results revealed the study to be feasible, demonstrating satisfactory recruitment, data completeness, acceptability, and fidelity. There were significant improvements in all outcome measures following Reiki, including stress, anxiety, pain, wellbeing, and sleep quality. More research is needed to determine whether improvements in outcomes exceed those of controls and/or are sustained over time. To address these questions, future work will continue to evaluate the program with use of a waitlist control group, as well as a larger sample size and additional follow-up assessments. We will first use a waitlist control group, as the Reiki Medic-Care program considers sham Reiki sessions to be unethical. Subsequent work will also include an active control from another integrative health treatment we expect to improve quality of life symptoms, such as massage. Taken together, the remote Reiki program showed encouraging benefits to health-related symptoms of healthcare workers impacted by workplace stress, such as during a pandemic.
Acknowledgments
We would like to thank the Japanese Reiki Healing Association for funding this research study. We are grateful to Caroline Gray for her work as the Booking and Portal Administrator. We also want to thank the Reiki-Medic Care Reiki practitioners for their participation in the Reiki program.
Footnotes
Author Contributions: NLD was involved in the methodology, formal analysis, interpretation, and writing of the manuscript. ALB was involved in the conceptualization of the study, methodology, interpretation, and writing of the manuscript. FG and RP were involved in the conceptualization of the study, methodology, and interpretation. All authors reviewed, edited, and approved of the manuscript in its current form.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by the Japanese Reiki Healing Association.
ORCID iD
Natalie L. Dyer https://orcid.org/0000-0002-9592-194X
References
- 1.Denning M, Goh ET, Tan B, et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: A multinational cross-sectional study. PLoS One. 2021;16(4):e0238666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gilleen J, Santaolalla A, Valdearenas L, et al. Impact of the COVID-19 pandemic on the mental health and well-being of UK healthcare workers. BJPsych Open. 2021;7(3):e88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rathod S, Pallikadavath S, Young AH, et al. Psychological impact of COVID-19 pandemic: protocol and results of first three weeks from an international cross-section survey-focus on health professionals. J Affect Disord Rep. 2020;1:100005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vanhaecht K, Seys D, Bruyneel L, et al. COVID-19 is having a destructive impact on health-care workers’ mental well-being. Int J Qual Health Care. 2021;33(1):mzaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Beh Immun. 2020;88:901-907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phiri P, Ramakrishnan R, Rathod S, et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: A systematic review and meta-analysis. EClinicalMedicine. 2021;34:100806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2021;126:252-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iacobucci G. COVID-19: UK had one of Europe’s highest excess death rates in under 65s last year. BMJ (Online). 2021;372:1-2. [DOI] [PubMed] [Google Scholar]
- 9.Merchant HA, Kow CS, Hasan SS. COVID-19 first anniversary review of cases, hospitalization, and mortality in the UK. Expert Rev Respir Med. 2021;15(8):973-978. [DOI] [PubMed] [Google Scholar]
- 10.Yıldırım M, Arslan G, Özaslan A. Perceived risk and mental health problems among healthcare professionals during COVID-19 pandemic: Exploring the mediating effects of resilience and coronavirus fear. Int J Ment Health Addict. 2020;20:1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain S, Hammerschlag R, Mills P, et al. Clinical studies of biofield therapies: Summary, methodological challenges, and recommendations. Glob Adv Health Med. 2015;4:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.IARP . Reiki in the Clinical Settings; 2021. https://iarp.org/reiki-clinical-setting/?fbclid=IwAR2tmr5dfhaDgZEEZ5wDAjgKhd2CUSaBSTBuPl0MCYGBXk_Rtu6V9ctHi58. accessed on August 7, 2021. [Google Scholar]
- 13.Herron-Marx S, Price-Knol F, Burden B, Hicks C. A systematic review of the use of Reiki in health care. Altern Complement Ther. 2008;14(1):37-42. [Google Scholar]
- 14.Vitale AT, O’Connor PC. The effect of Reiki on pain and anxiety in women with abdominal hysterectomies: A quasiexperimental pilot study. Holist Nurs Pract. 2006;20:263-272. [PubMed] [Google Scholar]
- 15.Billot M, Daycard M, Rigoard P. Self-Reiki, consideration of a potential option for managing chronic pain during pandemic COVID-19 period. Medicina. 2021;57(9):867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferraz GA, Rodrigues MR, Lima SA, et al. Is Reiki or prayer effective in relieving pain during hospitalization for cesarean? A systematic review and meta-analysis of randomized controlled trials. Sao Paulo Med J. 2017;135:123-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McManus DE. Reiki is better than placebo and has broad potential as a complementary health therapy. J Evid-Based Complement Altern Med. 2017;22(4):1051-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Senthil KP, Prabha A, Jeganathan PS, D'Souza C, Misri ZK. Efficacy of therapeutic touch and Reiki therapy for pain relief in disease conditions: A systematic review. J Psychiatr Nurs. 2014;3(1):15. [Google Scholar]
- 19.Singg S. Use of Reiki as a biofield therapy: An adjunct to conventional medical care. Clin Case Rep Rev. 2015;1(3):54-60. [Google Scholar]
- 20.Thrane S, Cohen SM. Effect of Reiki therapy on pain and anxiety in adults: An in-depth literature review of randomized trials with effect size calculations. Pain Manag Nurs. 2014;15(4):897-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rao A, Hickman LD, Sibbritt D, Newton PJ, Phillips JL. Is energy healing an effective non-pharmacological therapy for improving symptom management of chronic illnesses? A systematic review. Complement Ther Clin Pract. 2016;25:26-41. [DOI] [PubMed] [Google Scholar]
- 22.Baldwin AL, Vitale A, Brownell E, Kryak E, Rand W. Effects of Reiki on pain, anxiety, and blood pressure in patients undergoing knee replacement: A pilot study. Holist Nurs Pract. 2017;31(2):80-89. [DOI] [PubMed] [Google Scholar]
- 23.Charkhandeh M, Talib MA, Hunt CJ. The clinical effectiveness of cognitive behavior therapy and an alternative medicine approach in reducing symptoms of depression in adolescents. Psychiatry Res. 2016;239:325-330. [DOI] [PubMed] [Google Scholar]
- 24.Chirico A. Self-efficacy for coping with cancer enhances the effect of Reiki treatments during the pre- surgery phase of breast cancer patients. Anticancer Res. 2017;37:3657-3665. [DOI] [PubMed] [Google Scholar]
- 25.Bremner MN, Blake BJ, Wagner VD, et al. Effects of Reiki with music compared to music only among people living with HIV. J Assoc Nurses AIDS Care. 2016;27(5):635-647. [DOI] [PubMed] [Google Scholar]
- 26.Richeson NE, Spross JA, Lutz K, et al. Effects of Reiki on anxiety, depression, pain and physiological factors in community‐dwelling older adults. Res Gerontol Nurs. 2010;3:187‐199. [DOI] [PubMed] [Google Scholar]
- 27.Díaz-Rodríguez L, Arroyo-Morales M, Fernández-de-Las-Peñas C, et al. Immediate effects of reiki on heart rate variability, cortisol levels, and body temperature in health care professionals with burnout. Biol Res Nurs. 2011;13(4):376-382. [DOI] [PubMed] [Google Scholar]
- 28.Rosada RM, Rubik B, Mainguy B, et al. Reiki reduces burnout among community mental health clinicians. J Altern Complement Med. 2015;21:489-495. [DOI] [PubMed] [Google Scholar]
- 29.Buyukbayram Z, Saritas SC. The effect of Reiki and guided imagery intervention on pain and fatigue in oncology patients: A non-randomized controlled study. Explore. 2020;31:1-5. [DOI] [PubMed] [Google Scholar]
- 30.Kurebayashi LFS, Turrini RNT, Souza TPB, et al. Massage and Reiki used to reduce stress and anxiety: Randomized clinical trial. Rev. Latino-Am. Enfermagem. 2016;24:e2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Notte BB, Fazzini C, Mooney RA. Reiki’s effect on patient with total knee arthroplasty: A pilot study. Nursing. 2016;46:17-23. [DOI] [PubMed] [Google Scholar]
- 32.Shaybak E, Abdollahimohammad A, Rahnama M, et al. Effects of Reiki energy therapy on saphenous vein incision pain: A randomized clinical trial structure. Der Pharmacy Lettre. 2017;9:100-109. [Google Scholar]
- 33.Bowden D, Goddard L, Gruzelier J. A randomised controlled single-blind trial of the efficacy of reiki at benefitting mood and well-being. eCAM. 2011;2011:381862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yuce UO, Tasci S. Effect of Reiki on the stress level of caregivers of patients with cancer: Qualitative and single-blind randomized controlled trial. Complement Ther Med. 2021;58:102708. [DOI] [PubMed] [Google Scholar]
- 35.Cuneo CL, Curtis Cooper MR, Drew CS, et al. The effect of Reiki on work-related stress of the registered nurse. JHN. 2011;29(1):33-43. [DOI] [PubMed] [Google Scholar]
- 36.Hailey K, Fortin J, Pratt P, Forbes PW, McCabe M. Feasibility and effect of Reiki on the physiology and self-perceived stress of nurses in a large US hospital. Holist Nurs Pract. 2022;36(2):105-111. [DOI] [PubMed] [Google Scholar]
- 37.Shore AL. The long-term effects of energetic healing on symptoms of psychological depression and self-perceived stress. Altern Ther Health Med. 2004;10(3):42-48. [PubMed] [Google Scholar]
- 38.Abdurahman F, Payne N. Reiki practitioners’ perceptions of the impact of the COVID-19 pandemic on the experience, practice and future of Reiki. Complement Ther Clin Pract. 2022;46:101530. DOI: 10.1016/j.ctcp.2021.101530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.VanderVaart S, Berger H, Tam C, Goh YI, Gijsen VM, de Wildt SN, et al. The effect of distant Reiki on pain in women after elective Caesarean section: A double-blinded randomised controlled trial. BMJ Open. 2011;1(1):e000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Demir M, Can G, Kelam A, Aydiner A. Effects of distant Reiki on pain, anxiety and fatigue in oncology patients in Turkey: A pilot study. Asian Pac J Cancer Prev APJCP. 2015;16(12):4859-4862. [DOI] [PubMed] [Google Scholar]
- 41.Shirani N, Abdollahimohammad A, Firouzkouhi M, Masinaeinezhad N, Shahraki-Vahed A. The effect of Reiki energy therapy on the severity of pain and quality of life in patients with rheumatoid arthritis: A randomized clinical trial study. Med Sci. 2019;23(96):205-210. [Google Scholar]
- 42.Vasudev SS, Shastri S. Effect of distance Reiki on perceived stress among software professionals in Bangalore. Int J Indian Psychol. 2016;3(58):136-142. [Google Scholar]
- 43.Escudero DG, Reyes-Bossio M. Stress and anxiety reduction effects of a Reiki program during the COVID-19 pandemic among employees in Lima, Peru. Holist Nurs Pract. 2022;36(5):E48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Akpınar NB, Yüce UÖ, Yurtsever S. The effect of distant reiki on the stress and fatigue levels of nurses working in COVID-19 clinics: A randomized-controlled, single-blind study. Holist Nurs Pract. 2022:10-97. [DOI] [PubMed] [Google Scholar]
- 45.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453-1457. [DOI] [PubMed] [Google Scholar]
- 46.Bonney K. The Reiki Association; 2023. https://www.reikiassociation.net/reiki-faqs. accessed Jun 15th, 2023. [Google Scholar]
- 47.Paterson C. Measuring outcomes in primary care: a patient generated measure, MYMOP, compared with the SF-36 health survey. BMJ. 1996;312(7037):1016-1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thompson EA, Montgomery A, Douglas D, Reilly D. A pilot, randomized, double-blinded, placebo-controlled trial of individualized homeopathy for symptoms of estrogen withdrawal in breast-cancer survivors. J Altern Complement Med. 2005;11(1):13-20. [DOI] [PubMed] [Google Scholar]
- 49.Siegel P, da Motta PM, da Silva LG, Stephan C, Lima CS, de Barros NF. Reiki for cancer patients undergoing chemotherapy in a Brazilian Hospital. Holist Nurs Pract. 2016;30(3):174-182. [DOI] [PubMed] [Google Scholar]
- 50.Lee RT, Kingstone T, Roberts L, Edwards S, Soundy A, Shah PR, et al. A pragmatic randomised controlled trial of healing therapy in a gastroenterology outpatient setting. Eur J Integr Med. 2017;9:110-119. [Google Scholar]
- 51.Kristoffersen AE, Stub T, Knudsen-Baas O, Udal AH, Musial F. Self-reported effects of energy healing: A prospective observational study with pre–post design. Explore. 2019;15(2):115-125. [DOI] [PubMed] [Google Scholar]
- 52.Dyer NL, Ali A, Baldwin AL, Kowalski S, Rand WL. An evaluation of the subjective experience of receiving Reiki: Qualitative results from a pragmatic effectiveness study. J Integr Complement Med. 2022;28(9):739-748. Available online May 25. DOI: 10.1089/jicm.2022.0477 [DOI] [PubMed] [Google Scholar]
- 53.Engebretson J, Wardell DW. Experience of a Reiki session. Altern Ther Health Med. 2002;8(2):48. [PubMed] [Google Scholar]
- 54.Benson H, Beary JF, Carol MP. The relaxation response. Psychiatry. 1974;37(1):37-46. [DOI] [PubMed] [Google Scholar]
- 55.Bhasin MK, Dusek JA, Chang BH, Joseph MG, Denninger JW, Fricchione GL, et al. Relaxation response induces temporal transcriptome changes in energy metabolism, insulin secretion and inflammatory pathways. PLoS One. 2013;8(5):e62817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mackay N, Hansen S, McFarlane O. Autonomic nervous system changes during Reiki treatment: a preliminary study. J Altern Complement Med. 2004;10(6):1077-1081. DOI: 10.1089/acm.2004.10.1077 [DOI] [PubMed] [Google Scholar]
- 57.Salles LF, Vannucci L, Salles A, Silva MJ. The effect of Reiki on blood hypertension. Acta Paul Enferm. 2014;27:479-484. [Google Scholar]
- 58.Dyer NL, Surdam J, Dusek JA. A systematic review of practiced-based research of complementary and integrative health therapies as provided for pain management in clinical settings: Recommendations for the future and a call to action. Pain Med. 2022;23(1):189-210. DOI: 10.1093/pm/pnab151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dyer NL, Surdam J, Srinivasan R, Agarwal A, Dusek JA. The impact of individualized complementary and integrative health interventions provided in clinical settings on quality of life: A systematic review of practice-based research. J Integr Complement Med. 2022;8(8):618-640. DOI: 10.1089/jicm.2021.0413 [DOI] [PMC free article] [PubMed] [Google Scholar]