Summary
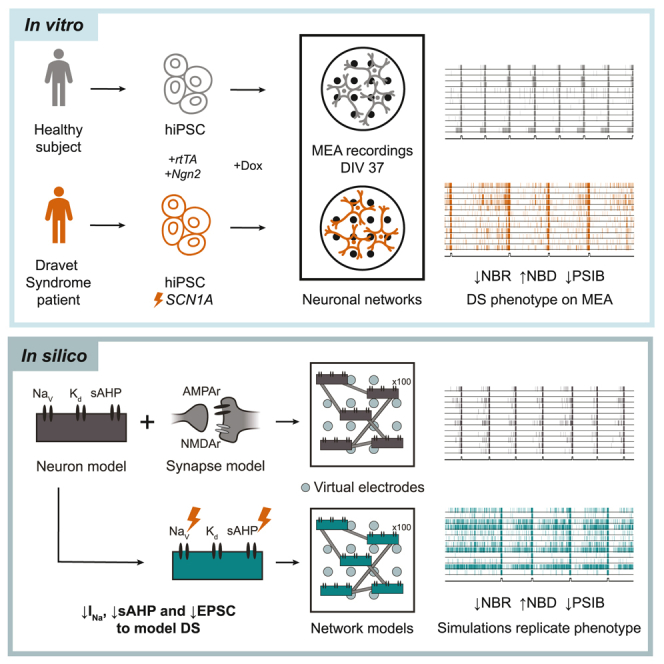
Human induced pluripotent stem cell (hiPSC)-derived neuronal networks on multi-electrode arrays (MEAs) provide a unique phenotyping tool to study neurological disorders. However, it is difficult to infer cellular mechanisms underlying these phenotypes. Computational modeling can utilize the rich dataset generated by MEAs, and advance understanding of disease mechanisms. However, existing models lack biophysical detail, or validation and calibration to relevant experimental data. We developed a biophysical in silico model that accurately simulates healthy neuronal networks on MEAs. To demonstrate the potential of our model, we studied neuronal networks derived from a Dravet syndrome (DS) patient with a missense mutation in SCN1A, encoding sodium channel NaV1.1. Our in silico model revealed that sodium channel dysfunctions were insufficient to replicate the in vitro DS phenotype, and predicted decreased slow afterhyperpolarization and synaptic strengths. We verified these changes in DS patient-derived neurons, demonstrating the utility of our in silico model to predict disease mechanisms.
Keywords: humen induced pluripotent stem cells, iPSC, disease modeling, Dravet Syndrome, SCN1A, multi-electrode arrays, neuronal network activity, computational model
Graphical abstract
Highlights
-
•
Our in silico model replicates hiPSC-derived excitatory neuronal network behavior on MEA
-
•
Our in silico model can identify disease mechanisms in patient-derived networks
-
•
The model predicts the contribution of mechanisms beyond NaV1.1 to the DS phenotype
-
•
We substantiated the in silico predictions in vitro
Doorn and colleagues developed an in silico model of hiPSC-derived neuronal networks on MEA to predict disease mechanisms based on network phenotypes. This model accurately simulated divergent behaviors of healthy networks, and predicted that disease mechanisms beyond NaV1.1 contribute to the phenotype seen in DS patient-derived excitatory neuronal networks, which was subsequently verified in vitro.
Introduction
Human induced pluripotent stem cell (hiPSC)-derived neuronal networks have become a key in vitro approach to study normal and abnormal formation of neural circuits, neurological disorders, or drug effects (Linda et al., 2022; Pires Monteiro et al., 2021; Yokoi et al., 2022). Networks cultured on multi-electrode arrays (MEAs) allow for non-invasive recording of neuronal network activity through embedded extracellular electrodes (Obien et al., 2015). In vitro neuronal networks derived from healthy subjects or patients show robust and replicable functional phenotypes (Mossink et al., 2021), and various genotype/phenotype correlations have been established (Frega et al., 2019; Marchetto et al., 2017; Klein Gunnewiek et al., 2021; Klein Gunnewiek et al., 2020). Despite these advances, the identification of cellular and synaptic mechanisms underlying the abnormal network phenotype remains challenging, as these are not trivial to deduce from the neuronal networks’ electrical activity (Obien et al., 2015).
In silico modeling can complement experimental research and facilitate the identification of mechanisms underlying the observed neuronal network phenotype (Brodland 2015). Computational models have provided insight into various phenomena of in vitro neuronal networks such as network bursting (Masquelier and Deco 2013; Kumar et al., 2020), the effect of stimulation (Wen et al., 2022), and the role of astrocytes (Lenk et al., 2016). However, most of these in silico network models use phenomenological neuron models that can simulate simple neuronal behavior such as spikes, but do not describe how this behavior results from the intricate interplay of ion channels (Masquelier and Deco 2013; Wen et al., 2022; Lenk et al., 2016; Park et al., 2006; Pasquale et al., 2008; Mok et al., 2022). Moreover, most models are not calibrated and validated to data from human neuronal networks (Kumar et al., 2020; Trujillo et al., 2021; Wen et al., 2022; Masquelier and Deco 2013; Park et al., 2006; Lenk et al., 2016). Thus, the available models are ill-suited to study the effect of detailed cellular mechanisms on network activity and most lack the biophysical realism to simulate disorders that arise from channelopathies.
Here, we developed a biophysically detailed in silico model of hiPSC-derived excitatory neuronal networks on MEA, that accurately reproduces the main bursting activity measured in in vitro control neuronal networks. Furthermore, blocking of particular ion channels in silico and in vitro resulted in similar network phenotypes, serving as model validation. To illustrate the potential of the model to test hypotheses and predict factors underlying disease mechanisms, we investigated excitatory neuronal networks derived from a Dravet syndrome (DS) patient. DS is a severe infantile epileptic encephalopathy, caused by de novo mutations in SCN1A (Takayama et al., 2014; Dravet 2011; Ragona 2011), encoding the α-1 subunit of the voltage-gated sodium channel NaV1.1 (Dravet 2011). It remains unresolved how excitatory neurons are affected by changes in sodium channel dynamics, and how this contributes to epileptogenesis (Isom 2014). Our in silico model revealed that sodium channel dysfunctions were insufficient to transition from a model of healthy networks to one that resembles the in vitro DS network behavior, and that additional alterations were needed. In particular, based on systematic model simulations, we predicted reduced slow afterhyperpolarization and synaptic strengths in the DS neuronal networks, which was subsequently confirmed in vitro. These results illustrate the utility of our in silico model to identify important mechanisms that can then be investigated in vitro in a targeted manner, expanding our understanding of disease mechanisms.
Results
Our in silico model accurately reproduces activity of hiPSC-derived neuronal networks
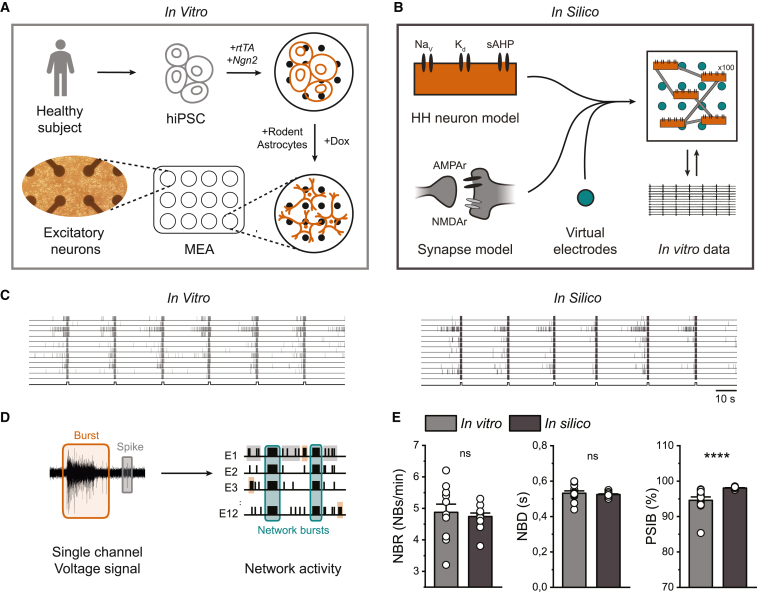
To allow in silico investigation of cellular and network mechanisms of hiPSC-derived neuronal networks on MEA, we developed a biophysically detailed computational model (Figure 1B). The model consisted of 100 Hodgkin-Huxley (HH)-type neurons with voltage-gated sodium and potassium channels, leak channels accounting for the natural permeability of the neural membrane, and a slow, spike-dependent afterhyperpolarizing current (sAHP), corresponding to slow calcium- and sodium-activated potassium currents. The neurons were sparsely connected via synapses modeling AMPA receptors (AMPAr) and NMDA receptors (NMDAr), including short-term depression (STD). In this way, the model allows the investigation of the effect of specific changes to both ion channels and synaptic processes. The in silico model contained “virtual electrodes” similar to in vitro electrodes to represent the network activity. We based parameter choices on experimental measurements where possible, and chose the remaining parameters such that the simulated activity resembled the activity observed from in vitro control neuronal networks. The in vitro neuronal networks were differentiated from hiPSCs derived from a healthy subject through forced expression of Ngn2 (Frega et al., 2017), and activity was recorded at 37 days in vitro (DIV) (Figure 1A). Both in vitro and in silico network activity consisted of spikes and bursts (short periods of high-frequency firing), which self-organized into synchronous network bursts (NBs) recorded in all electrodes (Figures 1C and 1D). In vitro neuronal networks exhibited stable periodic NBs, which were highly reproducible and previously observed across 10 independent control lines (Mossink et al., 2021). To quantitatively compare in silico simulations to in vitro measurements, we defined three NB features that remained stable over time (Mossink et al., 2021), the NB rate (NBR), the NB duration (NBD), and the percentage of spikes in NBs (PSIB). We analyzed the in vitro measurements and in silico simulations identically. There were no significant differences between the NBR and NBD in vitro and in silico, and the PSIB was similar (Figure 1E), showing that our in silico model can accurately simulate the main features of in vitro neuronal networks.
Figure 1.
The in silico model resembles the network phenotype of hiPSC-derived excitatory neuronal networks
(A) Schematic overview of the differentiation protocol. hiPSCs were obtained by reprogramming somatic cells of a healthy subject. Excitatory neurons were generated through doxycycline (Dox)-inducible overexpression of Neurogenin2 (Ngn2). At 2 days in vitro (DIV), embryonic day 18 (E18) rodent astrocytes were added in a 1:1 ratio. Activity was recorded at 37 DIV.
(B) Schematic overview of the biophysical in silico model consisting of 100 Hodgkin-Huxley (HH)-type neurons, containing voltage-dependent sodium- (NaV), delayed rectifier potassium (Kd), and slow afterhyperpolarizing currents (sAHPs), sparsely connected via AMPA receptor (AMPAr)- and NMDA receptor (NMDAr)-mediated synapse models, using virtual electrodes to measure network activity. The model is calibrated and validated to in vitro data.
(C) Representative raster plots showing 100 s of activity from a control network in vitro (left) and in silico (right). Black lines at the bottom of the raster plots indicate detected network bursts (NBs).
(D) Schematic overview of the analysis of MEA and “virtual electrode” signals.
(E) Quantification of network burst rate (NBR), network burst duration (NBD), and percentage of spikes in network bursts (PSIB) for 12 wells in vitro and 12 simulated networks in silico. Data represent mean ± SEM ns p > 0.05, ∗∗∗∗p < 0.0001, Mann-Whitney test was performed between two groups.
The in silico and in vitro neuronal networks show similar network behavior after pharmacological interventions with specific ion channel blockers
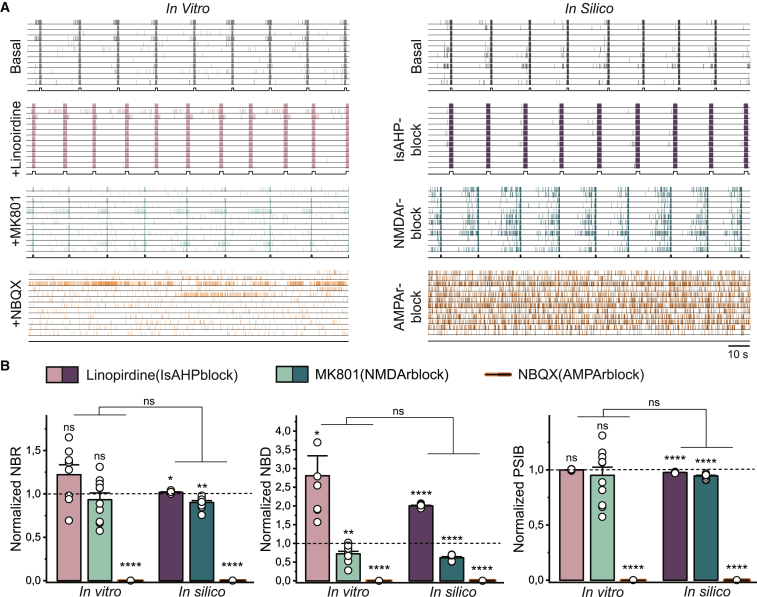
After establishing that the in silico model accurately simulated control neuronal network behavior, we aimed to further validate the model. We therefore performed interventions to both in vitro and in silico control networks and compared the effect without adjusting any other model parameters. First, we blocked KCNQ potassium channels in vitro using linopirdine (1.5 μM) (Schnee and Brown 1998; Noda et al., 1998; Guan et al., 2011). KCNQ potassium channels underlie part of the sAHP (Larsson 2013), and we therefore halved the conductance of the sAHP channels in silico. The addition of linopirdine resulted in a substantial increase in the NBD, both in vitro and in silico, while the NBR and PSIB were unaffected (Figure 2). Second, we inhibited sodium channels using tetrodotoxin (TTX) (1 μM) in vitro and blocked all sodium channels in silico. In both cases, the activity was completely abolished (data not shown). Third, we blocked NMDArs in vitro, using NMDAr antagonist MK-801 (1 μM), and in silico by setting the NMDA conductance to zero. Both resulted in a decreased NBD with minimal effect on the NBR and PSIB (Frega et al., 2019) (Figure 2). Finally, we inhibited AMPArs both in vitro, using AMPAr antagonists 2,3-dioxo-6-nitro-1,2,3,4-tetrahydrobenzo[f]quinoxaline7-sulfonamide (NBQX) (50 μM) and 1-naphthyl acetyl spermine trihydrochloride (NASPM) (10 μM), and in silico by abolishing the AMPA conductance. All bursting behavior vanished in both cultures and simulations (Figure 2). Although the variability of the effects of most blockers, reflected by a reduced SEM was noticeably smaller in simulations compared with experiments, there were no significant differences between the observations in vitro and in silico (Figure 2B). Because there were no remaining NBs after AMPA blockage, we also quantified the mean firing rate (MFR). There was a considerable reduction in MFR upon AMPA blockage, both in vitro and in silico. Nevertheless, the reduction ([mean ± SEM] 0.27 ± 0.08 spikes/s in vitro and 0.43 ± 0.04 spikes/s in silico) was significantly different (p = 0.0163) between the in vitro and in silico observations. Our observations, both in vitro and in silico, are in line with previous literature describing the effect of ion channel blockers on neuronal network behavior (Frega et al., 2019; Kasteel and Westerink 2017). Thus, we conclude that our in silico model is an adequate computational representation of the in vitro recorded control excitatory neuronal networks.
Figure 2.
Blocking specific ion channels in vitro and in silico results in similar network phenotypes
(A) Left: representative raster plots showing 100 s of spontaneous activity from a control network in vitro in basal conditions, treated with 1.5 μM linopirdine to block KCNQ potassium currents, 1 μM MK-801 to block NMDArs, and 50 μM NBQX and 10 μM NASPM to block AMPArs. Right: representative raster plots showing 100 s of simulated activity from the in silico model in basal conditions, when the conductance of the sAHP channels is halved to model the effect of linopirdine, when all the NMDArs are blocked, and when all AMPArs are blocked. Black lines at the bottom of the raster plots indicate detected NBs.
(B) Quantification of the normalized NBD, normalized NBR, and normalized PSIB in vitro and in silico with 8 networks for linopirdine (sAHPblock), 10 networks for MK-801 (NMDArblock), and 4 networks for NBQX (AMPArblock) per condition. Data represent mean ± SEM ns p > 0.05, ∗p < 0.05, ∗∗p < 0.005, ∗∗∗∗p < 0.0001. Groups were compared using a mixed effect model with multiple comparisons and Bonferroni correction.
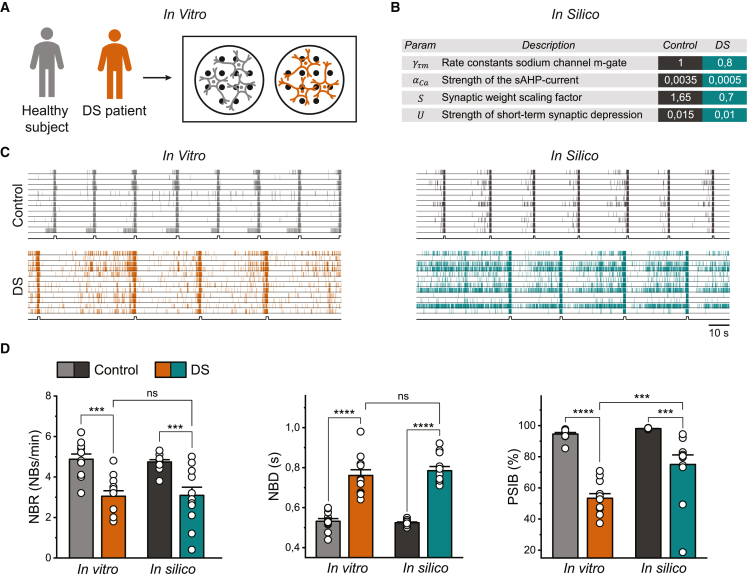
The in silico model predicts alterations to the sAHP and synaptic strengths in DS neuronal networks
To assess the potential of the model to generate meaningful hypotheses about underlying disease mechanisms, we studied neuronal networks derived from a DS patient with a heterozygous missense mutation in the pore domain of SCN1A (c.4168G>A p.Val1390Met). DS neuronal networks showed less frequent NBs with a significantly longer duration compared with control (Figures 3C and 3D). Moreover, DS networks exhibited more spiking outside the NBs, resulting in a lower PSIB (Figure 3D). Thus, excitatory neuronal networks derived from DS patients show a distinct phenotype on MEA, which was in line with the addition of proconvulsive compounds in previous literature (Bradley et al., 2018). Previous modeling studies argued that alterations in sodium channel dynamics could explain the DS phenotypes (Berecki et al., 2019; Kahlig et al., 2006). To test this hypothesis, we explored in silico all sodium channel alterations that could arise from mutations in SCN1A to transition from the control neuronal network model to a DS model that resembled the situation in vitro (see supplemental experimental procedures and Figure S1A). We observed that every possible (combination of) sodium channel modification(s) could qualitatively only either increase or decrease the neuronal excitability. On a network level, this led to either an increased or decreased NBR, while other features were largely unaffected (Figure S1C). In DS cultures, we observed a lower NBR compared with control, but also a lower PSIB and higher NBD (Figure S1B). In simulations with sodium channel modifications, the PSIB never significantly decreased and the NBD never increased in combination with a decreased NBR, comparable with the in vitro situation (Figure S1D). This suggests that changes in sodium channel dynamics are insufficient to transition from a functional phenotype of a control in silico model to a model of DS networks.
Figure 3.
In silico model of DS neuronal networks replicates in vitro phenotype by altering sAHP and synaptic strengths
(A) Schematic overview of the in vitro data.
(B) Table with in silico altered parameters to transition from a model of control networks to a model of DS neuronal networks.
(C) Representative raster plots showing 100 s of spontaneous activity from an in vitro control network and an in vitro DS network (left), and simulated activity from the control and the DS in silico model (right). Black lines at the bottom of the raster plots indicate detected NBs.
(D) Quantification of NBR, NBD, and PSIB for 12 wells per condition in vitro and 12 simulated networks per model in silico. Data represent mean ± SEM, ns p > 0.05, ∗∗∗p < 0.0005, ∗∗∗∗p < 0.0001. Means were compared with a two-way ANOVA with Bonferroni correction for multiple testing.
Since sodium channel modifications were insufficient, we explored other alterations, in particular synaptic properties and adaptive mechanisms. We observed that decreasing the conductance of the sAHP channels and decreasing the synaptic strengths (i.e., the magnitude of the excitatory post-synaptic currents [EPSCs]) lowered both the PSIB and NBR while increasing the NBD, similar to in vitro observations. Furthermore, we slightly reduced the amount of STD to obtain an NBD matching the in vitro observations. Although we could thus model the DS phenotype in silico independent of sodium channel modifications, the DS neurons in vitro exhibited decreased peak sodium current. To mimic this, we decreased the rate constants of the sodium channel activation gate in silico. This did not change the in silico modeled DS network phenotype, confirming that the alterations in sAHP, synaptic strength, and STD could still reproduce a DS network phenotype in a DS biophysically relevant context. An overview of the modified parameters can be found in Figure 3B. The obtained model could replicate the differences between the in vitro observed control and DS neuronal network phenotypes (Figure 3C). There were no significant differences between the NBR and NBD of the in vitro and in silico DS models (Figure 3D). While there was a significant difference in PSIB between in silico and in vitro DS networks, the difference in PSIB between healthy and DS networks was similar in vitro and in silico. These results suggest that the DS excitatory neuronal network phenotype arises from disease mechanisms beyond NaV1.1.
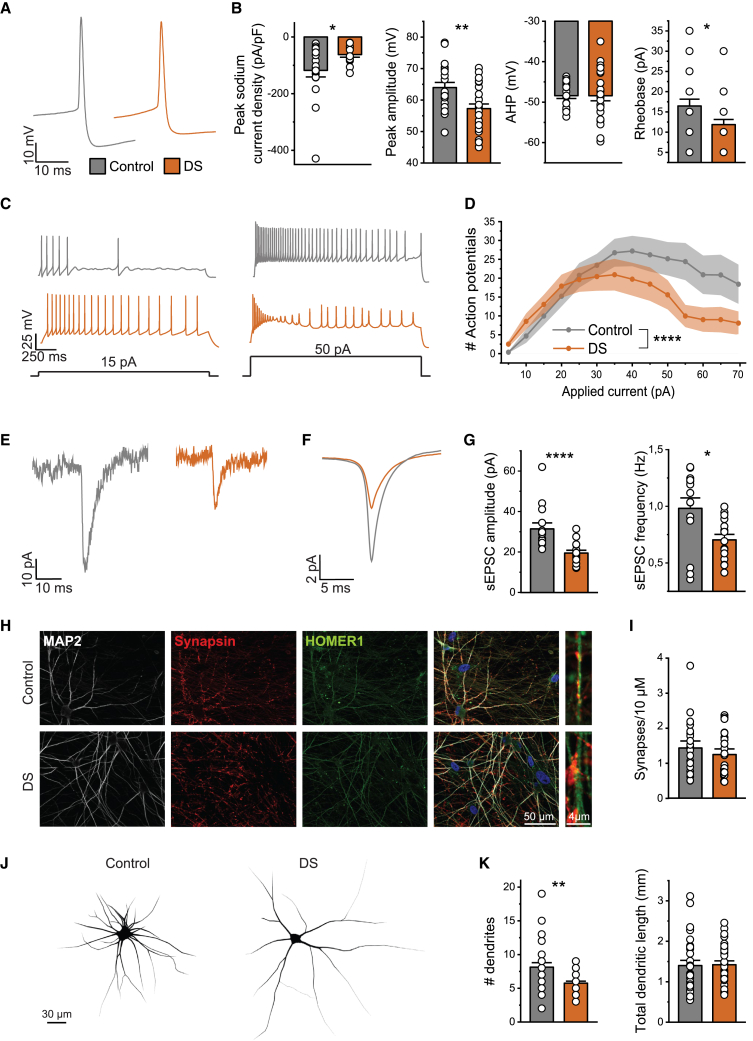
The in silico generated hypotheses are substantiated in vitro
The candidate cellular mechanisms in DS networks identified with our in silico model were subsequently investigated in vitro. We hypothesized that reduced sAHP, modeled as a potassium current that can be both calcium and sodium activated, could result from either reduced calcium or sodium currents. To this end, we measured the peak sodium current density and AP intrinsic properties using whole-cell current-clamp recordings. We observed decreased peak sodium current densities in DS neurons and a reduced AP amplitude, indicative of a reduction in both sodium- and voltage-dependent calcium currents (Gerlach et al., 2004). Similar to the in silico neurons, DS neurons in vitro were more excitable, reflected by a decreased rheobase, increased number of APs at lower current injections, and earlier depolarization block (Figures 4B–4D). To test the in silico prediction of reduced synaptic strengths in DS networks, we measured spontaneous EPSCs (sEPSCs) in control and DS network neurons using whole-cell voltage clamp. Indeed, both the sEPSC amplitudes and frequencies were significantly decreased in DS neurons (Figures 4E–4G). We found no significant difference in the synapse density or total dendritic length between control and DS neurons (Figures 4H and 4J), indicating that the decreased sEPSC amplitude and frequency are attributable to reduced synaptic strengths, and not to a decrease in the number of synapses. To conclude, DS neurons in vitro were hyperexcitable, and showed reductions in synaptic strengths, confirming the in silico predictions.
Figure 4.
In vitro DS neurons show hyperexcitability and reduced synaptic strengths
(A) Representative AP shapes in control (gray) and DS neurons (orange).
(B) Quantification of the peak sodium current density, AP peak amplitude, afterhyperpolarization (AHP) potential, and rheobase of control and DS neurons.
(C) Representative voltage traces from control and DS neurons in response to an applied current of 15 and 50 pA.
(D) The number of APs per current injection. Two-way ANOVA with Geisser-Greenhouse correction was performed to compare groups. For all intrinsic property data n = 20 for control and n = 26 for DS (3 independent experimental replicates).
(E and F) Representative (E) sEPSC traces and (F) average sEPSC traces of control and DS neurons.
(G) Quantification of sEPSC amplitudes and frequency in control (n = 14) and DS (n = 15) neurons (2 independent experimental replicates).
(H and I) Representative images of (H) control and DS neurons stained for MAP2, Synapsin1/2, and Homer1 at 35 DIV for the (I) quantification of the synaptic density in control (n = 21) and DS (n = 22) neurons (2 independent experimental replicates).
(J) Representative reconstructions of control (left) and DS (right) neurons.
(K) Quantification of the number of dendrites and the total dendritic length of control (n = 30) and DS (n = 30) neurons (3 independent experimental replicates).
Data represent mean ± SEM ∗p < 0.05, ∗∗p < 0.005, ∗∗∗∗p < 0.0001, Mann-Whitney test was performed between two groups.
Discussion
We here describe an in silico network model with detailed neuron dynamics, successfully calibrated and validated to experimental data from hiPSC-derived neuronal networks, able to generate meaningful hypotheses confirmed in vitro. Our model can be used to distinguish the effect of specific cellular changes on network dynamics, allowing for hypothesis testing and the development of mechanistic theories. With this model, researchers can leverage MEA data to identify potential cellular mechanisms underlying the neuronal network behavior, even if they lack the resources to do so in vitro.
Previously available models of in vitro neuronal networks were either not validated to data from human networks (Park et al., 2006; Masquelier and Deco 2013; Kumar et al., 2020; Pasquale et al., 2008; Trujillo et al., 2021), showed limited agreement between experimental and simulated data (Wen et al., 2022; Lenk et al., 2016), or used phenomenological neuron models, without detailed ion channel dynamics (Wen et al., 2022; Masquelier and Deco 2013; Park et al., 2006; Pasquale et al., 2008; Mok et al., 2022; Lenk et al., 2016). In contrast, we used a detailed neuron model with a biophysical description of how APs are generated by the interplay of ion channels, which allows for in-depth modeling of channelopathies, and a high agreement with in-vitro-generated data. However, increasing the model complexity also increases the number of parameters, which can potentially lead to a higher parameter degeneracy (Prinz et al., 2004; Achard and De Schutter 2006), meaning that multiple parameter combinations can lead to similar behavior. In that case, tuning model parameters is more difficult and predictions are more ambiguous. Conversely, it is important to keep in mind the simplifications in our model, such as the use of a one-compartmental neuron model that neglects the possible influence of neuronal morphology, or the lack of inhibitory neurons both in vitro and in silico, even though they might play a considerable role in the studied diseases (Kurbatova et al., 2016; Jansen et al., 2021; Lemaire et al., 2021; Chizhov et al., 2017). Depending on the research question, it might be relevant to reduce model complexity or, conversely, to increase it by the inclusion of inhibitory neurons or neuronal morphology.
Although our in silico model reproduced most electrophysiological signatures of in vitro neuronal networks, the PSIB in simulations was slightly higher than observed experimentally. This is likely due to the higher connectivity in silico, necessary to compensate for the lower number of neurons, and resulting in a higher synaptic input during an NB and consequently rapid firing. When we dramatically increased the number of neurons and proportionally decreased the connectivity, we observed a decrease in PSIB while the overall behavior of the network remained similar (Figure S2). This might also explain the slightly higher MFR after AMPA blockage in silico. Another slight disparity between experiment and simulation was the variability of the effect of ion channel blockers used for validation, likely due to the biological variability in cultures (Volpato and Webber 2020; Strube et al., 2017). For example, while the number of NMDArs and the effectiveness of MK-801 in vitro might differ per culture, the contribution of NMDA currents was always the same in silico. Thus, blocking the NMDArs in silico had quantitatively the same effect in all networks.
To illustrate the potential of our in silico model to test and generate hypotheses, we applied it to DS patient-derived excitatory networks. Previous work investigating DS has identified several sodium channel dysfunctions in excitatory neurons but it remains unexplained how this influences neuronal network behavior and epileptogenesis (Yu et al., 2006; Stein et al., 2019; Han et al., 2012; Liu et al., 2013; Jiao et al., 2013; Xie et al., 2020). In our in silico model, alterations to the sodium channel could not explain the aberrant network behavior observed in vitro. To replicate the DS phenotype in silico, we decreased the contribution of sAHP currents, synaptic strength, and the strength of STD, giving rise to the hypothesis that mechanisms beyond NaV1.1 might contribute to the DS phenotype in excitatory neuronal networks.
Our in silico model predicted that DS excitatory neurons were hyperexcitable, caused by a reduced sAHP. Multiple potassium conductances constitute the AHP, which is comprised of a fast (f), medium (m), and sAHP component. While the fAHP and mAHP are mostly voltage dependent, the sAHP is largely voltage independent but can be both calcium and sodium activated (Gerlach et al., 2004; Wallen et al., 2007). We did not observe a reduction in absolute AHP potential in DS neurons, both in silico and in vitro. Indeed, the effect of sAHP on the AHP potential is negligible (Larsson 2013). As we were unable to dissect the sAHP potential from the general AHP potential, we attempted to quantify the possible contributors to the sAHP. We observed a decreased peak sodium current density, which could in turn reduce the contribution of sodium-dependent potassium currents. These potassium channels exhibit a large outward current under physiological conditions, activated by TTX-sensitive sodium currents, the major sodium current in our in vitro model (Budelli et al., 2009; Hage and Salkoff 2012). Therefore, we speculate that reduced sodium currents might lead to reduced sodium-activated potassium currents, decreasing the sAHP as predicted by our in silico model. Another large contributor to the sAHP is the slow calcium-activated potassium current (Larsson 2013). The decreased AP amplitude observed in DS neurons in vitro could lead to a reduced calcium influx, which in turn lowers the activation of calcium-activated potassium currents. Spratt et al. (2021) observed a similar reduction in AP amplitude in an Scn2a knockout mouse model, and correspondingly explained neocortical pyramidal cell hyperexcitability by attenuated hyperpolarizing potassium currents. Thus, reduced potassium currents might explain excitatory neuronal hyperexcitability, as a secondary effect to SCN1A deficiency in DS. Future work should confirm this by dissecting the contribution of different voltage-, calcium-, and sodium-dependent potassium currents in DS neurons.
Although we measured neuronal hyperexcitability both in vitro and in silico, the network activity appeared less synchronized, reflected by a lower NBR and PSIB. Our in silico model predicted that this resulted from reduced synaptic strengths, which might be a homeostatic response to the hyperexcitability observed both in vitro and in silico. Homeostatic synaptic downscaling is observed in in vitro networks when the neuronal activity is artificially elevated (Siddoway et al., 2014; Frega et al., 2019). The primary mechanism for synaptic downscaling is the remodeling of AMPArs in the post-synaptic membrane leading to lower EPSC amplitudes (Turrigiano et al., 1998). We observed decreased sEPSC amplitudes and frequencies in DS cultures compared with control, without a reduced synapse number. Therefore, lowered sEPSC amplitudes and frequencies might be a result of reduced synaptic function in the in vitro DS networks. Homeostatic plasticity might also cause a reduction in STD, as our in silico model predicted (Deperrois and Graupner 2020; Almog et al., 2022). Based on these findings, we hypothesize that DS neuronal network activity is persistently increased due to neuronal hyperexcitability and that, consequently, synapses are downscaled as a form of homeostatic plasticity. Future studies should confirm the disease mechanisms proposed here for DS networks, as we used only one patient/control line at one developmental time point, to give a comprehensible example of how the computational model can be used. A possible obstacle in tuning our in silico model to other patient lines is the difficulty in finding the optimal model parameters. This could be overcome with the use of parameter optimization techniques that are widely available and tested on similar neuronal models (Sunnaker et al., 2013; Goncalves et al., 2020).
In sum, we developed a biophysically detailed in silico model that faithfully replicates in vitro observations from hiPSC-derived neuronal networks. Our model is a valuable tool complementary to in vitro measurements to strengthen the conclusions derived from these data.
Experimental procedures
Resource availability
Corresponding author
Further information and requests for resources and reagents should be directed to and will be fulfilled by the corresponding author Nina Doorn (n.doorn-1@utwente.nl).
Materials availability
All reagents, vectors, or cell lines used in this study are available from the lead contact upon request with a completed materials transfer agreement.
Data and code availability
The python code to run simulations in silico, together with the MATLAB code for data analysis is published on GitLab (https://gitlab.utwente.nl/m7706783/mea-model). All data are available from the lead contact upon request.
iPSC generation and neuronal differentiation
Experiments concerning patient-derived cells were carried out after informed consent and approval by the medical ethical committee of the Radboudumc, Nijmegen (2018-4525). The healthy donor was a 30-year-old male, as described previously and characterized (Frega et al., 2019; Mandegar et al., 2016). The DS patient was female and 4 years of age at the time of sampling. Direct target sequencing showed a missense mutation in the pore domain of SCN1A (c.4168G>A p.Val1390Met), which was confirmed in the hiPSC line (see Figure S2A). Peripheral mononuclear blood cells (PBMCs) were derived from a blood sample during scheduled routine diagnostic testing. hiPSC lines were obtained by episomal-vector-based reprogramming of PBMCs (Takahashi and Yamanaka 2006), and expressed pluripotency markers and displayed normal karyotype (see Figure S2B). To ensure sufficient quality, hiPSCs were passaged 2 times a week but not more than 16 times, and hiPSCs were checked for microplasm contamination every 8 passages. hiPSC cells were differentiated into excitatory cortical Layer 2/3 neurons through doxycycline-inducible overexpression of Neurogenin2 (Ngn2) as described previously (Frega et al., 2017; Mossink et al., 2021). Neurons were cultured in a density of 600 neurons/mm2 and co-cultured with embryonic day 18 rodent astrocytes in a 1:1 ratio to support maturation.
MEA recording
Spontaneous network activity was recorded using the 24-well MEA system (Multi Channel Systems, Reutlingen, Germany). Each well consisted of 12 gold electrodes with a diameter of 30 μm, spaced 300 μm. The network activity was recorded at 37 DIV for 600 s with a 10 kHz sampling frequency in a recording chamber maintained at 37°C/95% O2/5% CO2. The experimental design adhered to previously published guidelines (Mossink et al., 2021), and included experiments with a minimum of 12 wells per hiPSC line across two independent batches. Recordings were analyzed using a custom MATLAB (The MathWorks, Natick, MA) script as described under data comparison and statistics.
Pharmacology
For pharmacological experiments on MEA we used the following compounds: linopirdine (1.5 μM in MQ, Sigma, no. 105431-72-9), TTX (1 μM in MQ, Tocris, no. 1069), NASPM (10 μM in MQ, Tocris, no. 2766), MK 801 maleate (MK-801), (1 μM in DMSO, Tocris no. 0924), and NBQX (50 μM in DMSO, no. 0373). The DMSO concentration in each experiment remained below 0.5% v/v.
Single-cell electrophysiology
For single-cell electrophysiology, cells were visualized using an Olympus BX51WI upright microscope (Olympus Life Science, Center Valley, PA) and a DAGE-MTI IR-1000E (DAGE-MTI, Michigan, IN) camera. Data were acquired through a Digidata 1440-A digitizer and a MultiClamp 700B amplifier (Molecular Devices, San Jose, CA). The data were sampled at 20 kHz and filtered using a low-pass 1 kHz filter. Filamented patch pipettes, with open tip resistance of 5–7 MΩ, were pulled from borosilicate glass (Science Products, Hofheim, Germany) with a PC-10 micropipette puller (Narishige, London, UK). Coverslips were placed at the recording chamber continuously perfused with artificial cerebrospinal fluid (ACSF) containing 124 mM NaCl, 1.25 mM NaH2PO4, 3 mM KCl, 26 mM NaHCO3, 11 mM glucose, 2 mM CaCl2, 1 mM MgCl2 (adjusted to pH 7.4). The ACSF was maintained constant at 37°C/95% O2/5% CO2. Recordings were not analyzed if series resistance was above 20 MΩ, or the series to membrane resistance was lower than a 1:10 ratio. AP intrinsic properties were measured in current clamp using a potassium-based internal solution containing 130 mM K-gluconate, 5 mM KCl, 10 mM HEPES, 2.5 mM MgCl2, 2 mM Na2-ATP, 0.4 mM Na3-ATP, 10 mM Na-phosphocreatine, 0.6 mM EGTA (adjusted to pH 7.25 and osmolarity 290 mOsmol). Active intrinsic properties were measured using a stepwise current injection protocol ranging from −30 to +50 pA, and determined by analyzing the first action potential that was elicited by the protocol. All intrinsic properties were analyzed using Clampfit 10.7 (Molecular Devices). Both sEPSCs and sodium currents were measured in voltage clamp using a cesium-based solution containing 115 mM CsMeSO3, 20 mM CsCl, 10 mM HEPES, 2.5 mM MgCl2, 4 mM Na2-ATP, 0.4 mM Na3-ATP, 10 mM Na-phosphocreatine, 0.6 mM EGTA (adjusted to pH 7.2 and osmolarity 304 mOsmol), and recorded in ACSF at −60 mV. sEPSCs amplitude and frequency were quantified using an in-house MATLAB script using a threshold-based method. For sodium current measurements, P/8 leak subtraction was used and CNQX was present in the ACSF to block all synaptic activity during recording. Cells were measured using a stepwise protocol, cell membrane potential was increased from a holding potential of −90 mV in 10 mV increments to 60 mV for 100 ms. Peak currents recorded at the corresponding voltage step were determined using Clampfit 10.7, and divided by the cell capacitance.
Immunocytochemistry and neuronal morphology
Before immunostaining, cells were fixated with 4% PFA/4% sucrose for 15 min. Fixated coverslips were washed 3 times, and permeabilized with Triton X-100 (0.2%, Sigma-Aldrich, no. T8787) for 10 min, followed by 1 h of blocking with normal goat serum (NGS) (5%, Invitrogen, no. 10000C). Primary antibodies raised against Synapsin (1:500, Merck Milipore, no. AB1543P), MAP2 (1:1,000, Synaptic Systems, no. 188004), and Homer (1:500, Synaptic Systems, no. 160 011) were diluted in 1% NGS, and incubated overnight at 4°C. After 10 PBS washes, secondary antibodies diluted in 1% NGS were incubated for 1 h. Coverslips were washed 10 times with PBS, and stained with Hoechst (0.01%, Thermo Fisher Scientific, no. H3570) for 10 min, followed by 10 washes. Coverslips were mounted in DAKO mounting medium (Agilent, no. S3023) on microscope slides. Images were taken on a Zeiss Axio Imager Z2 at 63× magnification, and Fiji was used to quantify Synapsin/Homer double-positive puncta (Schindelin et al., 2012). MAP2-stained neurons were digitally reconstructed using Neurolucida 360 software (version 11, MBF-Bioscience, Williston, ND). The number of dendrites and dendritic length were quantified from reconstructed images.
Computational model
Our in silico model consists of several existing submodels. Neuron, synapse, and network parameter values are based on experiments and literature where possible, and the remaining parameters were chosen such that the simulations resembled the activity from control cultures.
Neuron model
We used an HH-type neuron model (Hodgkin and Huxley 1952), with expressions for the rate constants well suited for cortical pyramidal neurons (Traub and Miles 1991), and adapted these expressions to experimentally observed single-cell electrophysiology:
is the membrane potential of the neuron. allows for adjusting the spike threshold to our experimental data. Maximal conductances were taken from Traub and Miles (1991). Nernst potentials and were adapted such that the simulated neurons had the same average resting membrane potential, spike threshold potential, and AP amplitude as our in vitro neurons (Figure S4). All parameter values can be found in Table 1.
Table 1.
Overview of the parameters of the control in silico model
| Parameter | Description | Value | Unit |
|---|---|---|---|
| Cm | membrane capacitance | 1 | μF · cm−2 |
| maximum delayed rectifier potassium conductance | 5 | mS · cm−2 | |
| maximum voltage-gated sodium conductance | 50 | mS · cm−2 | |
| leak conductance | 0.3 | mS · cm−2 | |
| Nernst potential of potassium | −80 | mV | |
| Nernst potential of sodium | 70 | mV | |
| El | Nernst potential of the leak current | −39.2 | mV |
| VT | potential to adapt spike threshold | −30.4 | mV |
| strength of sAHP | 0.0035 | nS | |
| recovery timescale of sAHP currents | 6 | s | |
| σ | standard deviation of the noisy input | 4.1 | mV |
| maximal conductance of AMPA | 0.2808 | nS | |
| maximal conductance of NMDA | 0.0981 | nS | |
| Nernst potential of AMPA | 0 | mV | |
| Nernst potential of NMDA | 0 | mV | |
| multiplicative constant of NMDA dynamics | 0.5 | kHz | |
| decay time for AMPA synapses | 2 | ms | |
| decay time for NMDA synapses | 100 | ms | |
| rise time for NMDA synapses | 2 | ms |
Adaptation model
We included spike-frequency adaptation in every neuron in the form of an additional sAHP current , given by:
The current is modeled as a spike-activated potassium current. When a neuron exhibits a spike at time , we increase the conductance with an amount . The conductance then decays with time constant . The resulting equation for the conductance is:
where the delta function is zero for and leads to a step response at t0 of size 1 (multiplied by ). The current might correspond to slow sodium- or calcium-dependent potassium currents, but also other fatigue mechanisms. is the apparent recovery timescale of these mechanisms combined, which was chosen in the 2–8 s range found in the literature (Masquelier and Deco 2013; Gerlach et al., 2004). Parameters for the control model can be found in Table 1.
Noise and heterogeneity
We induced voltage fluctuations in every neuron, using:
where is Gaussian white noise with zero mean and σ the standard deviation of the resulting noise in the membrane potential. This noise can mimic synaptic or membrane noise.
We made the neurons heterogeneously excitable by drawing the amplitude of their constant applied current I from a uniform distribution between −9.5 and 9.5 pA.
Thus, the resulting neuron equations are:
Synapses and plasticity
EPSCs in vitro had both AMPA and NMDA components. We added a synaptic current to the HH equations:
AMPArs are modeled as an ohmic conductance gAMPA multiplied with the difference between the membrane potential Vm of the post-synaptic neuron and the Nernst potential EAMPA of the AMPA channels (Roth and van Rossum, 2013). NMDAr-mediated conductance also depends on the post-synaptic voltage, caused by blocking of the pore of the NMDAr by a magnesium ion. When the cell depolarizes, the magnesium block is lifted. The fraction of unblocked channels is fitted to:
where is the membrane potential of the post-synaptic neuron and is the extracellular magnesium concentration, which we took to be 1 mM as in Jahr and Stevens (1990). We set = 0.062 mV−1 and = 3.57 mM (Jahr and Stevens 1990). We assumed that the magnesium block changes instantaneously with voltage and is independent of the gating of the channel. The synaptic conductances can be modeled as maximal conductances of all the AMPA and NMDA channels, and , respectively, times the fraction of open channels. The fraction of open NMDA channels is the sum of the fractions of open channels per synapse with pre-synaptic neuron , , multiplied with the synaptic weight from pre-synaptic neuron j to the post-synaptic neuron . The equations for both synaptic currents are thus given by:
The fraction of open channels is given by:
Here, is an auxiliary gating variable for NMDA, and is a multiplicative constant. The fraction of open channels increases every time the pre-synaptic neuron spikes at time . and are the rise and decay times for the NMDA synapses and the decay time for AMPA synapses. These equations and the values for the time constants were taken from Masquelier and Deco (2013). We neglected the AMPA rise time because it is very short (Masquelier and Deco 2013). Δ is a conduction delay. All synaptic weights are multiplied with a synaptic scaling factor S. We took synaptic weights wij from a normal distribution with a mean of 1 and a standard deviation of 0.7. We set values below 0 to 0, and values above 2 to 2. This caused about 1 in 15 synapses to perish. Other parameter values can be found in Table 1.
STD
All synapses are modulated by STD. We used the phenomenological model proposed by Markram et al. (1998). The model is based on the concept of synaptic resources, of which only a fraction, x, is available. The synaptic weight wj is multiplied with , where obeys:
where is the time constant of STD, set to be 813 ms (Markram et al., 1998). is the strength of STD, set to = 0.015 (Markram et al., 1998).
Network properties
We constructed a sparsely connected network of N = 100 neurons. Neurons were randomly connected with a connection probability of 30%. Neurons were placed on a grid, allowing for the inclusion of distance-dependent conduction delays and virtual electrodes. Every virtual electrode measured the weighted sum of the membrane potential of the surrounding neurons, mimicking MEA measurements.
Simulations
Simulations were performed with the Brian2 simulator (Stimberg et al., 2019) in a Python 3.9 environment. Differential equations were integrated using either the exponential Euler or Euler forward method. To account for noise with these procedures, we kept the noise term constant over the timestep, where this noise term is as described in the noise and heterogeneity section, but ξ is replaced by a random number drawn from a normal distribution and divided by . This way, we implemented the Euler-Maruyama scheme. To mimic the in vitro measurement time and sampling frequency, simulations were 650 s long, with a timestep of 0.1 ms, where the first 50 s were discarded as transient. We simulated 12 networks per condition with different connectivities, initial synaptic weights, and neuron heterogeneity, to mimic the 12 experimental wells. We validated the computational model by comparing the effects of pharmacological intervention in vitro and in silico. In vitro, we blocked potassium channels, sodium channels, AMPArs, and NMDArs using the inhibitors described under pharmacology. In silico, we simulated 650 s of basal network behavior in 30 networks. Then, we halved the conductance of the sAHP current in 8 of these networks, blocked all sodium channels in 8 networks, blocked NMDArs in 10 networks, and blocked AMPArs in four networks, and simulated for 650 s.
Data comparison and statistics
Data obtained from in vitro and in silico “MEA” recordings were handled identically. Signals were filtered between 100 and 3,500 Hz using a fifth-order Butterworth filter. We detected APs using an amplitude threshold-based method, where the threshold was 4 times the root mean-square of the electrode signal. NB detection started when the total spike rate remained above a threshold (1/4th of the maximum spike rate) for 60 ms, and stopped when the spike rate dropped below a second threshold (1/100th of the maximum spike rate). The NB was excluded if more than 80% of the spikes originated from a single electrode. We defined three features that were representative of network behavior and the differences between the control and DS network phenotypes, which were the NBR in NBs per minute, the NBD in seconds, and the PSIB.
We performed statistical analysis using GraphPad Prism 5 (GraphPad Software, San Diego, CA). We ensured normal distributions using a Kolmogorov-Smirnov test. When normality was not ensured, non-parametric testing using a Mann-Whitney test was performed. Equal variances of the to-be-compared groups were ensured using Levene’s test. When comparing two means of distributions with unequal variances, a Welch’s t test was performed. When equal variances and normality were ensured, a Student’s t test was performed. For multiple comparisons, we used one-way ANOVA with Bonferroni correction. For repeated measures (model validation) we used a mixed-effect model with Geisser-Greenhouse correction for unequal variability of differences and Bonferroni test for multiple comparisons. To compare groups with measurements at multiple conditions, we used a two-way ANOVA with Geisser-Greenhouse correction. p values <0.05 were considered significant in all cases. All summary data, statistics and p values can be found in Table S1.
Author contributions
N.D. developed the in silico model and designed and performed in silico experiments. E.J.H.v.H., U.C., and A.M. designed and performed in vitro experiments. N.D., E.J.H.v.H., and U.C. performed data analyses. E.J.H.v.H., M.F., and N.N.K. contributed to development of the in vitro model. N.D. and E.J.H.v.H. wrote the manuscript with input from all authors. H.G.E.M. and D.S. provided conceptualization and intellectual content. M.F., N.N.K., and M.J.A.M.v.P. conceived and supervised the project.
Acknowledgments
This work was supported by the Netherlands Organisation for Health Research and Development ZonMw grant 91217055 (to N.N.K.), BRAINMODEL ZonMw PSIDER program 10250022110003 (to N.N.K. and M.F.), the European Joint Programme on Rare Diseases JTC2020-SCN1A-up! (to N.N.K.), and the Dutch epilepsiefonds WAR 18-02 (to N.N.K.). We thank Judith Verhoeven for providing patient material.
Conflict of interests
The authors declare no competing interests.
Published: July 6, 2023
Footnotes
Supplemental information can be found online at https://doi.org/10.1016/j.stemcr.2023.06.003.
Supplemental information
References
- Achard P., De Schutter E. Complex parameter landscape for a complex neuron model. PLoS Comput. Biol. 2006;2:e94. doi: 10.1371/JOURNAL.PCBI.0020094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almog Y., Mavashov A., Brusel M., Rubinstein M. Functional investigation of a neuronal microcircuit in the CA1 area of the Hippocampus reveals synaptic dysfunction in dravet syndrome mice. Front. Mol. Neurosci. 2022;15:97. doi: 10.3389/FNMOL.2022.823640/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berecki G., Bryson A., Terhag J., Maljevic S., Gazina E.V., Hill S.L., Petrou S. SCN1A gain of function in early infantile encephalopathy. Ann. Neurol. 2019;85:514–525. doi: 10.1002/ana.25438. [DOI] [PubMed] [Google Scholar]
- Bradley J.A., Luithardt H.H., Metea M.R., Strock C.J. In vitro screening for seizure liability using microelectrode array technology. Toxicol. Sci. 2018;163:240–253. doi: 10.1093/TOXSCI/KFY029. [DOI] [PubMed] [Google Scholar]
- Brodland G.W. How computational models can help unlock biological systems. Semin. Cell Dev. Biol. 2015;47–48:62–73. doi: 10.1016/j.semcdb.2015.07.001. [DOI] [PubMed] [Google Scholar]
- Budelli G., Hage T.A., Wei A., Rojas P., Jong Y.J.I., O’Malley K., Salkoff L. Na+-activated K+ channels express a large delayed outward current in neurons during normal physiology. Nat. Neurosci. 2009;12:745–750. doi: 10.1038/nn.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chizhov A.V., Amakhin D.V., Zaitsev A.V. Computational model of interictal discharges triggered by interneurons. PLoS One. 2017;12:e0185752. doi: 10.1371/JOURNAL.PONE.0185752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deperrois N., Graupner M. Short-term depression and long-term plasticity together tune sensitive range of synaptic plasticity. Cuntz H., editor. PLoS Comput. Biol. 2020;16:e1008265. doi: 10.1371/journal.pcbi.1008265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dravet C. The core Dravet syndrome phenotype. Epilepsia. 2011;52:3–9. doi: 10.1111/j.1528-1167.2011.02994.x. [DOI] [PubMed] [Google Scholar]
- Frega M., Linda K., Keller J.M., Gümüş-Akay G., Mossink B., van Rhijn J.R., Negwer M., Klein Gunnewiek T., Foreman K., Kompier N., et al. Neuronal network dysfunction in a model for Kleefstra syndrome mediated by enhanced NMDAR signaling. Nat. Commun. 2019;10:1–15. doi: 10.1038/s41467-019-12947-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frega M., van Gestel S.H.C., Linda K., Van Der Raadt J., Keller J., Van Rhijn J.R., Schubert D., Albers C.A., Nadif Kasri N. Rapid neuronal differentiation of induced pluripotent stem cells for measuring network activity on micro-electrode arrays. J. Vis. Exp. 2017;119:54900. doi: 10.3791/54900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerlach A.C., Maylie J., Adelman J.P. Activation kinetics of the slow afterhyperpolarization in hippocampal CA1 neurons. Pflügers Archiv. 2004;448:187–196. doi: 10.1007/S00424-003-1237-2/FIGURES/8. [DOI] [PubMed] [Google Scholar]
- Goncalves P.J., Lueckmann J.M., Deistler M., Nonnenmacher M., Öcal K., Bassetto G., Chintaluri C., Podlaski W.F., Haddad S.A., Vogels T.P., et al. Training deep neural density estimators to identify mechanistic models of neural dynamics. Elife. 2020;9:1–46. doi: 10.7554/ELIFE.56261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan D., Higgs M.H., Horton L.R., Spain W.J., Foehring R.C. Contributions of Kv7-mediated potassium current to sub- and suprathreshold responses of rat layer II/III neocortical pyramidal neurons. J. Neurophysiol. 2011;106:1722–1733. doi: 10.1152/jn.00211.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hage T.A., Salkoff L. Sodium-activated potassium channels are functionally coupled to persistent sodium currents. J. Neurosci. 2012;32:2714–2721. doi: 10.1523/JNEUROSCI.5088-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han S., Tai C., Westenbroek R.E., Yu F.H., Cheah C.S., Potter G.B., Rubenstein J.L., Scheuer T., De La Iglesia H.O., Catterall W.A. Autistic-like behaviour in Scn1a+/- mice and rescue by enhanced GABA-mediated neurotransmission. Nature. 2012;489:385–390. doi: 10.1038/nature11356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgkin A.L., Huxley A.F. A quantitative description of membrane current and its application to conduction and excitation in nerve. J. Physiol. 1952;117:500–544. doi: 10.1113/jphysiol.1952.sp004764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isom L.L. It was the interneuron with the parvalbumin in the hippocampus!” ”No, it was the pyramidal cell with the glutamate in the cortex!” searching for clues to the mechanism of dravet syndrome - the plot thickens. Epilepsy Curr. 2014;14:350–352. doi: 10.5698/1535-7597-14.6.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahr C.E., Stevens C.F. Voltage dependence of NMDA-activated macroscopic conductances predicted by single-channel kinetics. J. Neurosci. 1990;10:3178–3182. doi: 10.1523/jneurosci.10-09-03178.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen N.A., Perez C., Schenke M., Van Beurden A.W., Dehghani A., Voskuyl R.A., Thijs R.D., Ullah G., Van Den Maagdenberg A.M., Tolner E.A. Impaired θ-γ coupling indicates inhibitory dysfunction and seizure risk in a dravet syndrome mouse model. J. Neurosci. 2021;41:524–537. doi: 10.1523/JNEUROSCI.2132-20.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao J., Yang Y., Shi Y., Chen J., Gao R., Fan Y., Yao H., Liao W., Sun X.F., Gao S. Modeling Dravet syndrome using induced pluripotent stem cells (iPSCs) and directly converted neurons. Hum. Mol. Genet. 2013;22:4241–4252. doi: 10.1093/hmg/ddt275. [DOI] [PubMed] [Google Scholar]
- Kahlig K.M., Misra S.N., George A.L. Impaired inactivation gate stabilization predicts increased persistent current for an epilepsy-associated SCN1A mutation. J. Neurosci. 2006;26:10958–10966. doi: 10.1523/JNEUROSCI.3378-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasteel E.E.J., Westerink R.H.S. Comparison of the acute inhibitory effects of Tetrodotoxin (TTX) in rat and human neuronal networks for risk assessment purposes. Toxicol. Lett. 2017;270:12–16. doi: 10.1016/J.TOXLET.2017.02.014. [DOI] [PubMed] [Google Scholar]
- Klein Gunnewiek T., Van Hugte E.J.H., Frega M., Guardia G.S., Foreman K.B., Panneman D., Mossink B., Linda K., Keller J.M., Schubert D., et al. Mitochondrial dysfunction impairs human neuronal development and reduces neuronal network activity and synchronicity. Cell Rep. 2020:720227. doi: 10.1101/720227. [DOI] [PubMed] [Google Scholar]
- Klein Gunnewiek T.M., Verboven A.H.A., Pelgrim I., Hogeweg M., Schoenmaker C., Renkema H., Beyrath J., Smeitink J., de Vries B.B.A., Hoen P.B.A.C.'t., et al. Sonlicromanol improves neuronal network dysfunction and transcriptome changes linked to m.3243A¿G heteroplasmy in iPSC-derived neurons. Stem Cell Rep. 2021;16:2197–2212. doi: 10.1016/J.STEMCR.2021.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar R., Huang Y.-T., Chen C.-C., Tzeng S.-F., Chan C.-K. Astrocytic regulation of synchronous bursting in cortical cultures: from local to global. Cereb. Cortex Commun. 2020;1:tgaa053. doi: 10.1093/TEXCOM/TGAA053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurbatova P., Wendling F., Kaminska A., Rosati A., Nabbout R., Guerrini R., Dulac O., Pons G., Cornu C., Nony P., et al. Dynamic changes of depolarizing GABA in a computational model of epileptogenic brain: insight for Dravet syndrome. Exp. Neurol. 2016;283:57–72. doi: 10.1016/J.EXPNEUROL.2016.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsson H.P. What determines the kinetics of the slow afterhyperpolarization(sAHP) in neurons? Biophys. J. 2013;104:281–283. doi: 10.1016/J.BPJ.2012.11.3832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemaire L., Desroches M., Krupa M., Pizzamiglio L., Scalmani P., Mantegazza M. Modeling NaV1.1/SCN1A sodium channel mutations in a microcircuit with realistic ion concentration dynamics suggests differential GABAergic mechanisms leading to hyperexcitability in epilepsy and hemiplegic migraine. PLoS Comput. Biol. 2021;17 doi: 10.1371/JOURNAL.PCBI.1009239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenk K., Priwitzer B., Ylä-Outinen L., Tietz L.H., Narkilahti S., Hyttinen J.A. Simulation of developing human neuronal cell networks. Biomed. Eng. Online. 2016;15:1–16. doi: 10.1186/S12938-016-0226-6/FIGURES/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linda K., Lewerissa E.I., Verboven A.H.A., Gabriele M., Frega M., Klein Gunnewiek T.M., Devilee L., Ulferts E., Hommersom M., Oudakker A., et al. Imbalanced autophagy causes synaptic deficits in a human model for neurodevelopmental disorders. Autophagy. 2022;18:423–442. doi: 10.1080/15548627.2021.1936777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Lopez-Santiago L.F., Yuan Y., Jones J.M., Zhang H., O'Malley H.A., Patino G.A., O'Brien J.E., Rusconi R., Gupta A., et al. Dravet syndrome patient-derived neurons suggest a novel epilepsy mechanism. Ann. Neurol. 2013;74:128–139. doi: 10.1002/ana.23897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandegar M.A., Huebsch N., Frolov E.B., Shin E., Truong A., Olvera M.P., Chan A.H., Miyaoka Y., Holmes K., Spencer C.I., et al. CRISPR interference efficiently induces specific and reversible gene silencing in human iPSCs. Cell Stem Cell. 2016;18:541–553. doi: 10.1016/j.stem.2016.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchetto M.C., Belinson H., Tian Y., Freitas B.C., Fu C., Vadodaria K., Beltrao-Braga P., Trujillo C.A., Mendes A.P.D., Padmanabhan K., et al. Altered proliferation and networks in neural cells derived from idiopathic autistic individuals. Mol. Psychiatr. 2017;22:820–835. doi: 10.1038/MP.2016.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markram H., Wang Y., Tsodyks M. Differential signaling via the same axon of neocortical pyramidal neurons. Proc. Natl. Acad. Sci. USA. 1998;95:5323–5328. doi: 10.1073/pnas.95.9.5323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masquelier T., Deco G. Network bursting dynamics in excitatory cortical neuron cultures results from the combination of different adaptive mechanism. PLoS One. 2013;8 doi: 10.1371/journal.pone.0075824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mok R.S.F., Zhang W., Sheikh T.I., Pradeepan K., Fernandes I.R., DeJong L.C., Benigno G., Hildebrandt M.R., Mufteev M., Rodrigues D.C., et al. Wide spectrum of neuronal and network phenotypes in human stem cell-derived excitatory neurons with Rett syndrome-associated MECP2 mutations. Transl. Psychiatry. 2022;12:450. doi: 10.1038/s41398-022-02216-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossink B., Verboven A.H.A., van Hugte E.J.H., Klein Gunnewiek T.M., Parodi G., Linda K., Schoenmaker C., Kleefstra T., Kozicz T., van Bokhoven H., et al. Human neuronal networks on micro-electrode arrays are a highly robust tool to study disease-specific genotype-phenotype correlations in vitro. Stem Cell Rep. 2021;16:2182–2196. doi: 10.1016/J.STEMCR.2021.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noda M., Obana M., Akaike N. Inhibition of M-type K+ current by linopirdine, a neurotransmitter-release enhancer, in NG108-15 neuronal cells and rat cerebral neurons in culture. Brain Res. 1998;794:274–280. doi: 10.1016/S0006-8993(98)00235-2. [DOI] [PubMed] [Google Scholar]
- Obien M.E.J., Deligkaris K., Bullmann T., Bakkum D.J., Frey U. Revealing neuronal function through microelectrode array recordings. Front. Neurosci. 2015;9:423. doi: 10.3389/fnins.2014.00423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park I., Xu D., Demarse T.B., Principe J.C. IEEE International Conference on Neural Networks - Conference Proceedings. 2006. Modeling of synchronized burst in dissociated cortical tissue: an exploration of parameter space; pp. 581–586. [DOI] [Google Scholar]
- Pasquale V., Massobrio P., Bologna L.L., Chiappalone M., Martinoia S. Selforganization and neuronal avalanches in networks of dissociated cortical neurons. Neuroscience. 2008;153:1354–1369. doi: 10.1016/j.neuroscience.2008.03.050. [DOI] [PubMed] [Google Scholar]
- Pires Monteiro S., Voogd E., Muzzi L., De Vecchis G., Mossink B., Levers M., Hassink G., Van Putten M., Le Feber J., Hofmeijer J., Frega M. Neuroprotective effect of hypoxic preconditioning and neuronal activation in a in vitro human model of the ischemic penumbra. J. Neural. Eng. 2021;18:036016. doi: 10.1088/1741-2552/ABE68A. [DOI] [PubMed] [Google Scholar]
- Prinz A.A., Bucher D., Marder E. Similar network activity from disparate circuit parameters. Nat. Neurosci. 2004;7:1345–1352. doi: 10.1038/nn1352. [DOI] [PubMed] [Google Scholar]
- Ragona F. Cognitive development in children with Dravet syndrome. Epilepsia. 2011;52:39–43. doi: 10.1111/J.1528-1167.2011.03000.X. [DOI] [PubMed] [Google Scholar]
- Roth A., van Rossum M.C.W. Computational Modeling Methods for Neuroscientists. The MIT Press; 2013. Modeling synapses; pp. 139–160. [DOI] [Google Scholar]
- Schindelin J., Arganda-Carreras I., Frise E., Kaynig V., Longair M., Pietzsch T., Preibisch S., Rueden C., Saalfeld S., Schmid B., et al. Fiji: an open-source platform for biological-image analysis. Nat. Methods. 2012;9:676–682. doi: 10.1038/nmeth.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnee M.E., Brown B.S. Selectivity of linopirdine (DuP 996), a neurotransmitter release enhancer, in blocking voltage-dependent and calcium-activated potassium currents in hippocampal neurons. J. Pharmacol. Exp. Therapeut. 1998;286:709–717. [PubMed] [Google Scholar]
- Siddoway B., Hou H., Xia H. Molecular mechanisms of homeostatic synaptic downscaling. Neuropharmacology. 2014;78:38–44. doi: 10.1016/j.neuropharm.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spratt P.W.E., Alexander R.P.D., Ben-Shalom R., Sahagun A., Kyoung H., Keeshen C.M., Sanders S.J., Bender K.J. Paradoxical hyperexcitability from NaV1.2 sodium channel loss in neocortical pyramidal cells. Cell Rep. 2021;36:109483. doi: 10.1016/j.celrep.2021.109483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein R.E., Kaplan J.S., Li J., Catterall W.A. Hippocampal deletion of NaV1.1 channels in mice causes thermal seizures and cognitive deficit characteristic of Dravet Syndrome. Proc. Natl. Acad. Sci. USA. 2019;116:16571–16576. doi: 10.1073/PNAS.1906833116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stimberg M., Brette R., Goodman D.F. Brian 2, an intuitive and efficient neural simulator. Elife. 2019;8 doi: 10.7554/eLife.47314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strube C., Gackière F., Saliba L., Tell F., Kessler J.-P. Variability of quantal NMDA to AMPA current ratio in nucleus tractus solitarii neurons. bioRxiv. 2017 doi: 10.1101/110569. [DOI] [Google Scholar]
- Sunnaker M., Busetto A.G., Numminen E., Corander J., Foll M., Dessimoz C. Approximate bayesian computation. PLoS Comput. Biol. 2013;9 doi: 10.1371/JOURNAL.PCBI.1002803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi K., Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- Takayama R., Fujiwara T., Shigematsu H., Imai K., Takahashi Y., Yamakawa K., Inoue Y. Long-term course of Dravet syndrome: a study from an epilepsy center in Japan. Epilepsia. 2014;55.4:528–538. doi: 10.1111/EPI.12532. [DOI] [PubMed] [Google Scholar]
- Traub R.D., Miles R. Cambridge University Press; 1991. Neuronal Networks of the Hippocampus. [DOI] [Google Scholar]
- Trujillo C.A., Adams J.W., Negraes P.D., Carromeu C., Tejwani L., Acab A., Tsuda B., Thomas C.A., Sodhi N., Fichter K.M., et al. Pharmacological reversal of synaptic and network pathology in human MECP2 -KO neurons and cortical organoids. EMBO Mol. Med. 2021;13:1. doi: 10.15252/EMMM.202012523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turrigiano G.G., Leslie K.R., Desai N.S., Rutherford L.C., Nelson S.B. Activity-dependent scaling of quantal amplitude in neocortical neurons. Nature. 1998;391:892–896. doi: 10.1038/36103. [DOI] [PubMed] [Google Scholar]
- Volpato V., Webber C. Addressing variability in iPSC-derived models of human disease: guidelines to promote reproducibility. DMM Disease Models and Mechanisms. 2020;13 doi: 10.1242/dmm.042317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallén P., Robertson B., Cangiano L., Löw P., Bhattacharjee A., Kaczmarek L.K., Grillner S. Sodium-dependent potassium channels of a Slack-like subtype contribute to the slow afterhyperpolarization in lamprey spinal neurons. J. Physiol. 2007;585:75–90. doi: 10.1113/JPHYSIOL.2007.138156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen J., Peitz M., Brüstle O. A defined human-specific platform for modeling neuronal network stimulation in vitro and in silico. J. Neurosci. Methods. 2022;373:109562. doi: 10.1016/J.JNEUMETH.2022.109562. [DOI] [PubMed] [Google Scholar]
- Xie Y., Ng N.N., Safrina O.S., Ramos C.M., Ess K.C., Schwartz P.H., Smith M.A., O’Dowd D.K. Comparisons of dual isogenic human iPSC pairs identify functional alterations directly caused by an epilepsy associated SCN1A mutation. Neurobiol. Dis. 2020;134:104627. doi: 10.1016/J.NBD.2019.104627. [DOI] [PubMed] [Google Scholar]
- Yokoi R., Shigemoto-Kuroda T., Matsuda N., Odawara A., Suzuki I. Electrophysiological responses to seizurogenic compounds dependent on E/I balance in human iPSCderived cortical neural networks. J. Pharmacol. Sci. 2022;148:267–278. doi: 10.1016/J.JPHS.2021.12.006. [DOI] [PubMed] [Google Scholar]
- Yu F.H., Mantegazza M., Westenbroek R.E., Robbins C.A., Kalume F., Burton K.A., Spain W.J., McKnight G.S., Scheuer T., Catterall W.A. Reduced sodium current in GABAergic interneurons in a mouse model of severe myoclonic epilepsy in infancy. Nat. Neurosci. 2006;9:1142–1149. doi: 10.1038/NN1754. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The python code to run simulations in silico, together with the MATLAB code for data analysis is published on GitLab (https://gitlab.utwente.nl/m7706783/mea-model). All data are available from the lead contact upon request.