Abstract
Cisplatin-based chemotherapy has been associated with durable disease control in a small subset of patients with metastatic urothelial cancer. However, the mechanistic basis for this phenomenon has remained elusive. Antitumor immunity may underlie these exceptional responders. In a phase II trial evaluating a phased schedule of gemcitabine and cisplatin followed by gemcitabine and cisplatin with ipilimumab for metastatic urothelial cancer, 4 of 36 patients achieved durable disease-free treatment-free survival (DDFTFS) and remain in remission over 5 years after enrolment on the study. We sought to identify the genomic and immunological mechanisms associated with functional cures of such patients. Whole exome sequencing was performed on pretreatment archival tumor tissue. Neoantigen prediction and ranking were performed using a novel pipeline. For a subset of patients with available biospecimens, selected peptides were tested for neoantigen-specific T cell reactivity in peripheral blood CD4+ and CD8+ T cells cultured with autologous antigen-presenting cells at baseline, postchemotherapy, and postchemotherapy and ipilimumab timepoints. Multiplex assays of serum protein analytes were also assessed at each time point. Serum proteomic analysis revealed that pretreatment, patients achieving DDFTFS demonstrated an immune activated phenotype with elevations in TH1 adaptive immunity, costimulatory molecules, and immune checkpoint markers. After combination cisplatin-based chemotherapy and ipilimumab treatment, DDFTFS patients again displayed enrichment for markers of adaptive immunity, as well as T cell cytotoxicity. CD27 was uniquely enriched in DDFTFS patients at all timepoints. Neoantigen reactivity was not detected in any patient at baseline or post two cycles of chemotherapy. Both CD4+ and CD8+ neoantigen-specific T cell reactivity was detected in two of two DDFTFS patients in comparison to zero of five non-DDFTFS patients after combination cisplatin-based chemotherapy and ipilimumab treatment. Antitumor immunity may underlie functional cures achieved in patients with metastatic urothelial cancer treated with cisplatin-based chemotherapy and immune checkpoint blockade. Probing the mechanistic basis for DDFTFS may facilitate the identification of biomarkers, therapeutic components, and optimal treatment sequences necessary to extend this ultimate goal to a larger subset of patients.
Keywords: urinary bladder neoplasms, urologic neoplasms, immunotherapy, tumor biomarkers, adaptive immunity
Background
Metastatic urothelial cancer (mUC) is generally considered an incurable illness. Cisplatin-based chemotherapy has been standard first-line treatment for mUC for decades, and while objective responses are observed in 40%–60% of patients, most responses are short-lived with a median survival of ~13–15 months.1 Despite poor outcomes in the majority of patients, a ‘tail’ exists on the progression-free survival curves in most trials of cisplatin-based chemotherapy for mUC and ~10%–20% of patients are progression-free at 5 years.2 3 Dissecting the underpinnings of durable disease control achieved in this subset of patients with mUC treated with cisplatin-based chemotherapy has the potential to identify biomarkers, or mechanisms, which can be exploited to extend such benefits to a larger subset of patients.
Features associated with durable disease control achieved with cisplatin-based chemotherapy in mUC are understudied, at least in part related to a paucity of cohorts with long-term follow-up with associated detailed clinical annotation and linked biospecimens. Though cancer cell-intrinsic molecular vulnerabilities to cisplatin have been identified,4–6 measures of adaptive immunity in pretreatment tumors have also been linked to improved long-term outcomes in patients with advanced UC.7 Cisplatin-based chemotherapy has been associated with favorable immunomodulatory effects in model systems,8 raising the possibility that anti-tumor immunity may play a role in durable disease control with chemotherapy in mUC. To better understand durable disease control achieved with cisplatin-based chemotherapy in mUC, and to potentially increase the subset of patients achieving this outcome, in 2010 we designed a phase II clinical trial (NCT01524991) evaluating a phased schedule of gemcitabine and cisplatin chemotherapy (GC) followed by GC in combination with the CTLA-4-targeting immune checkpoint inhibitor (ICI) ipilimumab (Ipi).9 Remarkably, extended follow-up reveals 4/36 patients who remain disease-free and treatment-free 5+ years after the initiation of treatment (hereafter referred to as durable disease-free treatment-free survival (DDFTFS)]). Here, we sought to identify genomic and immunological features associated with ‘functional cures’ of mUC.
Methods
Clinical classification
Patients were characterized as having achieved DDFTFS (no evidence of disease and >2 years off all treatment at the time of last follow-up) or non-DDFTFS, which included patients achieving transient objective responses (short responders) as well as patients with best response of stable disease or progressive disease (PD) (non-responders), as outlined in online supplemental table S1.
jitc-2023-007613supp001.pdf (595.6KB, pdf)
Plasma proteomic analysis
Multiplex proteomic assays were performed at baseline (cycle 1 day 1) and on-treatment (cycle 3 day 1 and cycle 6 day 1) using the Olink Target 96 Immuno-Oncology Panel (Olink Proteomics) and Milliplex MAP Human Cytokine/Chemokine Magnetic Bead Panel—Premixed 41 Plex—Immunology Multiplex Assay (Millipore Sigma) per manufacturer instructions. Quality control measures included exclusion of samples (N=2) that failed quality analysis and Olink targets (N=9) with >75% of samples below the lower limit of detection. Olink data, extracted in normalized protein expression (NPX) units, were transformed to a linear scale (2NPX). An area-proportional Venn diagram was created using BioVenn.10
Neoantigen prediction pipeline
Whole exome sequencing was completed as previously reported.9 Neoantigen prediction was performed using a combination of a major histocompatibility complex binding affinity score from previously described methodology11 and a novel composite score. Full details of the novel composite score, human leukocyte antigen typing, and peptide selection and synthesis are provided in online supplemental methods.
ELISpot
Autologous peripheral blood mononuclear cells (PBMCs) were pulsed with polypeptide pools as previously described.12 Full details on the ELISpot methodology are provided in online supplemental methods.
Flow cytometry
Flow cytometry was performed on PBMCs collected at baseline, cycle 3 day 1, and cycle 6 day 1, as previously described.9 Samples were considered positive for neoantigen reactivity if there was both ≥0.5% IFNγ positivity and ≥2 fold increase positivity compared with that of the respective negative control. Data acquisition was performed on a BD LSR Fortessa flow cytometer and analyzed using TreeStar Flowjo software.
Statistical analyses
Statistical analyses were performed in GraphPad Prism V.9 software. Volcano plots were analyzed using a false discovery rate Q value of 10% corrected for multiple comparisons via the two-stage set-up method of Benjamini, Krieger, and Yekutieli. Means were analyzed using Kruskal-Wallis testing with multiple comparisons performed by Dunn’s test. Data are presented as mean±SE of the mean unless otherwise indicated. All data were included, no outliers were excluded. Results were considered significant with p<0.05; *p<0.05, **p<0.01.
Results
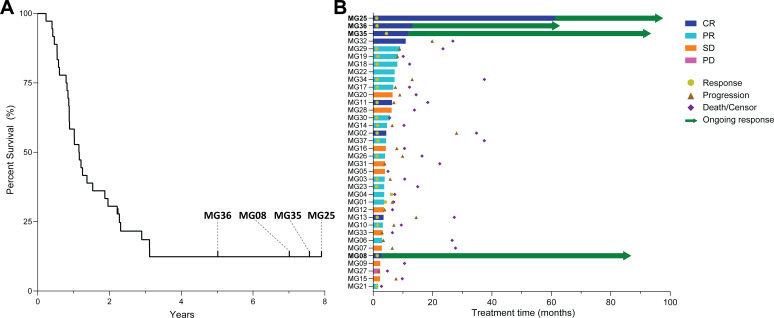
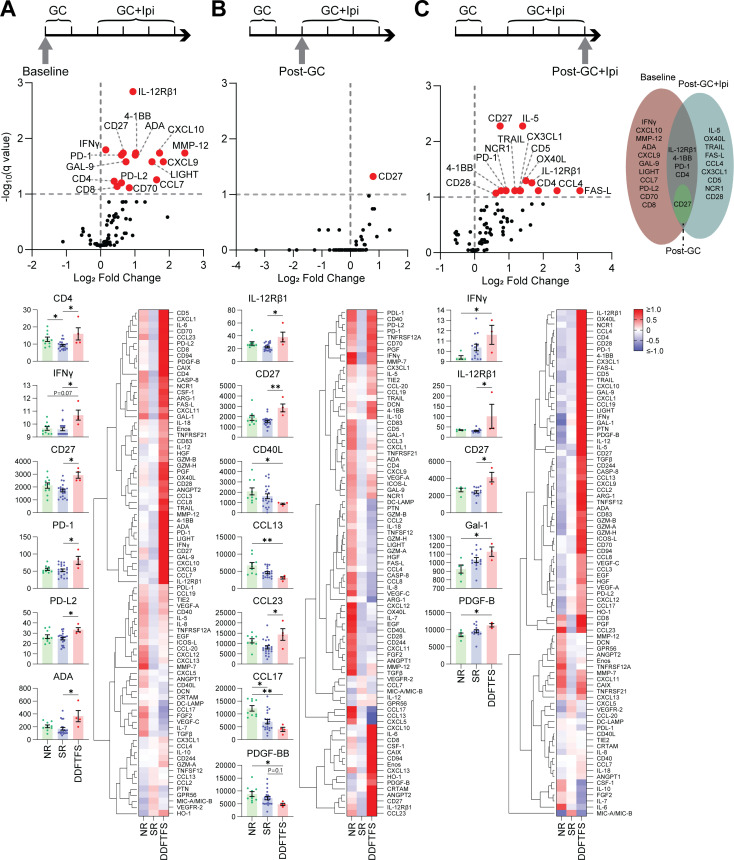
Among the 36 patients enrolled, 4 patients achieved DDFTFS and remain disease-free and treatment-free 5+ years after the initiation of treatment (figure 1). The clinical characteristics of patients achieving, and not achieving, DDFTFS are outlined in online supplemental table S9. To determine baseline immune characteristics unique to DDFTFS patients, we performed multiplex analysis of serum analytes pretreatment. Multiple analytes were significantly enriched in DDFTFS patients compared with all non-DDFTFS patients, including markers of adaptive TH1 T cell activity (CD8, CD4, IL-12Rβ1, IFNγ, CXCL9, CXCL10), costimulatory molecules (4-1BB, CD27, CD70, LIGHT), and immune checkpoints (PD-1, GAL-9, PD-L2). Hierarchical clustering revealed similar patterns of analyte elevations differential to the DDFTFS patients (figure 2A, online supplemental figure S1A). Many of these analytes were significantly elevated in DDFTFS patients compared with short responders (figure 2A), and normalizing both DDFTFS patients and short responders to non-responders further highlighted similar patterns of immune enrichment unique to DDFTFS patients (online supplemental figure S2A).
Figure 1.
Long-term follow-up reveals a subset of extraordinary responders after treatment with cisplatin-based chemotherapy and ipilimumab. (A) Kaplan-Meier survival curve with the four DDFTFS patients labeled (MG36, MG08, MG35, MG25). (B) Swimmer plot indicating the duration of treatment, clinical response, and time of progression, death/censor, or ongoing response, with DDFTFS patients bolded. CR, complete response; DDFTFS, durable disease-free treatment-free survival; PD, progressive disease; PR, partial response; SD, stable disease.
Figure 2.
DDFTFS patients demonstrate a unique immunophenotype at baseline and after treatment with cisplatin-based chemotherapy and ipilimumab. Analysis was performed at (A) baseline, (B) post-GC, and (C) post-GC+Ipi. Top, volcano plot represents all Olink analytes comparing DDFTFS patients with all non-DDFTFS patients, significant analytes labeled with red datapoints, horizontal line indicates the threshold for significant discovery, vertical line separates relative increased (right) or decreased (left) protein level, with an area-proportional Venn diagram of significant analytes. Bottom left, scatter bar plots of individual analytes with significantly altered levels when comparing DDFTFS patients to non-responders or short responders, with data displayed as mean±SEM, y-axis is transformed NPX values. Bottom right, heatmaps of average z-scores per response grouping with the Olink assay, columns indicate patient grouping by response, rows indicate individual analytes, with unsupervised hierarchical clustering performed on rows. *P<0.05, **p<0.01, and p values<0.1 and >0.05 are reported. DDFTFS, durable disease-free treatment-free survival; GC, gemcitabine and cisplatin; Ipi, ipilimumab; NR, non-responder; SR, short responder.
Analysis post-GC revealed an overall dampening of the differential immunophenotype of DDFTFS patients. While clustering identified increased analytes (including CD8, CD27, IL-12Rβ1, IL-12p70, CXCL10) and decreased analytes (including various chemokines, ARG-1, VEGF-C, IL-8) in DDFTFS patients versus patients not achieving DDFTFS, CD27 was the only significantly increased analyte in DDFTFS patients. Individually, post-GC timepoint values for IL-12Rβ1, CD27, and CCL23 were significantly increased and CD40L, CCL13, PDGF-BB, and CCL17 were significantly decreased in DDFTFS patients in comparison to either short responders or non-responders (figure 2B, online supplemental figures S1B and S2B).
To assess the immunomodulatory impact of ICI, we repeated the analysis post-GC+Ipi. Several patterns of analyte enrichment were again observed specific to DDFTFS patients, including elevations in analytes also observed at baseline (CD4, IL-12Rβ1, PD-1, CD27, 4-1BB). Also increased were markers of cytotoxicity (FAS-L, TRAIL), costimulation (CD28, OX40L), chemokines (CX3CL1, CCL4), and NK cell activity (NCR1). These findings were overall absent from short responders, including a significant elevation in IFNγ in DDFTFS patients compared with non-responders (figure 2C, online supplemental figure S1C). IL-1α was the most downregulated marker in DDFTFS patients compared with non-responders, which was consistent at all time points and was not observed among short responders (online supplemental figure S2A–C).
Evaluation of immunomodulatory changes over sequential timepoints within DDFTFS patients identified a significant increase post-GC+Ipi in DC-LAMP, a marker of mature dendritic cells (DCs) enriched in immunoregulatory molecules (mregDCs),13 soluble PD-1, and CD28 (online supplemental figure S3).
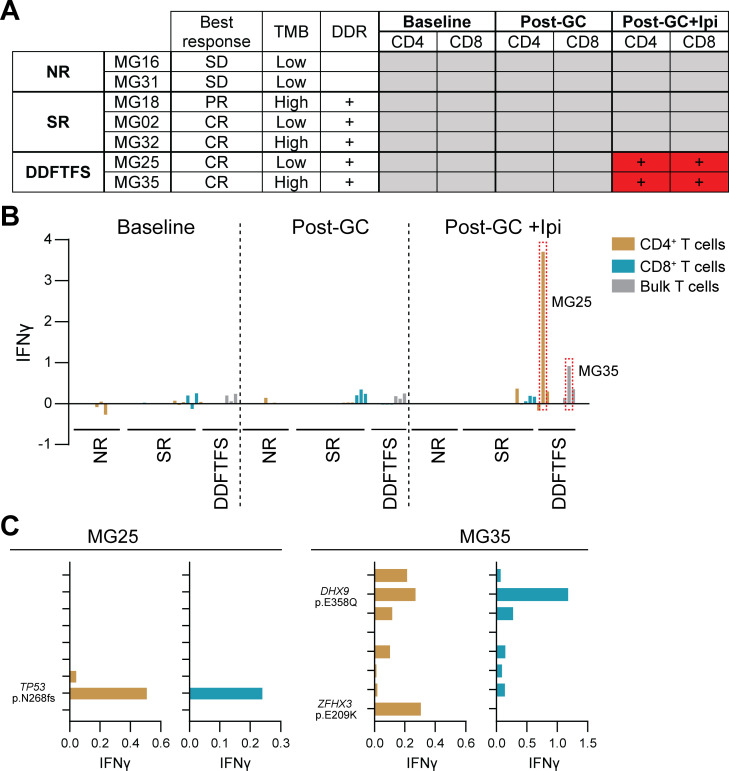
Non-self antigens encoded by somatic mutations arising in cancer cells, termed neoantigens, can stimulate anti-tumor immunity.14 Given the profile of circulating analytes reminiscent of heightened adaptive cytotoxic immunity among DDFTFS patients post-GC+Ipi, we evaluated whether neoantigen-driven immunity could be playing a role in these long-term remissions. We utilized a unique prediction pipeline to rank candidate neoantigen peptide immunogenicity for a subset of patients (N=7) with sufficient available biospecimens that encompassed DDFTFS patients, short responders, and non-responders with high and low tumor mutational burdens and present and absent somatic DNA damage response (DDR) alterations (figure 3A). No neoantigen-specific T cell responses were detected in any patients at baseline and post-GC. However, post-GC+Ipi, neoantigen-specific T cell reactivity was detected in two of two DDFTFS patients, while zero of five non-DDFTFS patients demonstrated neoantigen-specific reactivity (figure 3A,B). This reactivity was specific to neoantigens generated from a frameshift in TP53 in patient MG25 and substitutions in DHX9 and ZFHX3 in patient MG35, and both DDFTFS patients exhibited CD4+ and CD8+ T cell reactivity (figure 3A,C).
Figure 3.
Neoantigen-specific CD4+ and CD8+ T cell reactivity is only detectable in DDFTFS patients after treatment with cisplatin-based chemotherapy and ipilimumab. (A) Table of the patient subset for which neoantigen prediction, peptide synthesis, and T cell reactivity assays were performed. The presence of DDR alterations is indicated with +. Positive T cell responses are indicated with + in red cells. (B) IFNγ ELISpot values per patient at each time point, performed with pooled peptides. Positive detections are highlighted in dotted red boxes. (C) CD4+ and CD8+ T cell ELISpots (MG25) and flow cytometry (MG35) of individual peptides for patients and matching peptide pools with positive detections. The y-axis represents individually tested peptides with positive detected neoantigen variants reported. CR, complete response; DDFTFS, durable disease-free treatment-free survival; DDR, DNA damage response; GC, gemcitabine and cisplatin; Ipi, ipilimumab; NR, non-responder; PD, progressive disease; PR, partial response; SD, stable disease; SR, short responder; TMB, total mutational burden.
Discussion
A ‘tail’ on the survival curve in studies of patients with mUC treated with cisplatin-based chemotherapy has been demonstrated across multiple datasets over the last several decades.2 3 However, the mechanistic basis underlying this observation has been elusive. While ‘functional cures’ of mUC only occur in a small subset of patients, probing the features associated with such outcomes can uncover therapeutic targets, and/or biomarkers, with the potential to extend such benefits to an even larger subset of patients.
Here, we sought to understand the genomic and immunological features associated with DDFTFS from a phase II study of gemcitabine, cisplatin, and ipilimumab in which 4/36 patients were alive and disease-free and treatment-free at 5+ years after enrolment on the study. Our results demonstrate that patients achieving DDFTFS had a unique immune phenotype at baseline, characterized by increased markers of adaptive TH1 T cell activity, costimulatory molecules, and immune checkpoints. Interestingly, post-GC, peripheral blood analytes reminiscent of TH1 immunity were dampened, even in patients achieving DDFTFS, though levels of CD27 remained significantly increased compared with non-DDFTFS patients. Post-GC+Ipi, patients experiencing DDFTFS demonstrated elevated analytes associated with T cell cytotoxicity, costimulation, chemokines, and NK cell activity, which were absent from short responders. Importantly, neoantigen-specific T cell reactivity was detected post-GC+Ipi in two of two patients achieving DDFTFS but not in any non-DDFTFS patients. Together, our findings suggest that patients with mUC achieving DDFTFS exhibited evidence of a pre-existing adaptive immune response which was enhanced with cisplatin-based chemotherapy and/or ipilimumab. The detection of neoantigen-specific T cell reactivity in patients achieving DDFTFS post-GC+Ipi provides, to our knowledge, among the first reported associations between neoantigen-specific immunity and functional cure of mUC.
Key strengths of our study include the very long duration of follow-up, multiplex analyses, novel neoantigen prediction pipeline with functional T cell assays, and both pretreatment and on-treatment sequential analyses, allowing for the identification of both differential and consistent immune-related patterns specific to DDFTFS patients. Limitations to our study include the relatively small sample size and the difficulty delineating the potential contribution of cisplatin-based chemotherapy versus ipilimumab versus combination therapy to these observations. The rate of durable disease control is similar to what has been reported in prior studies with cisplatin-based chemotherapy.2 3 Cisplatin-based chemotherapy has been shown to exert distinct immunomodulatory effects in patients with mUC,8 and a recent study demonstrated that measures of pretreatment adaptive immunity, specifically PD-L1 expression on immune cells in the tumor microenvironment, was associated with a higher likelihood of durable disease control.15 Somatic mutations in DDR genes have also been associated with increased sensitivity to cisplatin-based chemotherapy, as they induce DNA damage which is repaired primarily by the nucleotide excision repair pathway.16 DDR alterations, specifically those causing deficiencies in the mismatch repair pathway, are also linked to response to ICIs across multiple cancer types,17 thought to be driven by enhanced mutagenicity and neoantigen exposure. In this study, while pretreatment somatic mutations in DDR genes were observed in two of three patients achieving DDFTFS (online supplemental figure S4), this was similar to the 57% DDR alteration rate observed among the entire cohort,9 suggesting that DDR deficiencies may play a role but other mechanisms are likely involved. Single-agent CTLA-4 blockade has been understudied in patients with mUC, though one small phase II study reported an objective response rate of ~19%.18 Though peripheral blood analytes reminiscent of adaptive immunity were dampened from baseline to cycle 3 with chemotherapy alone in patients achieving DDFTFS, and neoantigen specific T cell reactivity did not emerge until post-GC+Ipi, whether this is related to the addition of Ipi versus simply a longer treatment duration cannot be determined. Whether CTLA-4 blockade improves outcomes when added to platinum-based chemotherapy (plus PD-L1 blockade) in patients with mUC is currently being tested in the large international phase 3 NILE study (NCT03682068).19 While combination trials with platinum-based chemotherapy plus PD-1/PD-L1 blockade in patients with mUC have not demonstrated significant improvements in overall survival, these trials included patients receiving both cisplatin-based and carboplatin-based chemotherapy which may be associated with different immunomodulatory effects.15 Analyses of ongoing randomized studies will be needed to better understand the contribution of individual treatment components.
Our analysis might facilitate the identification of therapeutic targets on which to build additional combination regimens to further enhance the likelihood of achieving DDFTFS in patients with mUC. For example, CD27 was the most consistently elevated analyte, increased in DDFTFS patients at each timepoint, and its binding partner, CD70, was also elevated at baseline. CD27 is a T cell costimulatory molecule that promotes CXCL10 and IFNγ production, T cell cytotoxicity, and maintains memory CD8+ T cells. Experimental agonistic agents are currently under evaluation targeting CD27 and CD70, including in combination with CTLA-4 blockade and OX40 agonism.20 Conversely, features associated with a lower likelihood of achieving DDFTFS may also facilitate identification of therapeutic targets. A recent study identified poor outcomes with PD-1/PD-L1 ICI in UC patients with pretreatment enrichment for pro-tumorigenic monocyte-macrophages with increased IL1B and CXCL8 (encodes IL-8) and decreased CXCL9, CXCL10, and antigen-presenting cell-related genes, a transcriptional program that was inferred to be regulated by IL-1α and IL-1β.21 Consistent with those findings, at baseline, we identified increased CXCL9 and CXCL10 and decreased IL-1α and IL-8 in the peripheral blood of patients achieving, vs not achieving, DDFTFS.
Our results suggest that neoantigen-specific immunity may be associated with DDFTFS in patients with mUC. Prior studies in UC identified neoantigen-specific CD4+ TILs,22 and, in a cohort of patients with mUC treated with PD-L1 blockade, neoantigen-specific CD8+ T cells on-treatment were associated with improved outcomes.23 A phase 1b trial of a personalized neoantigen peptide vaccine with ICI reported de novo CD4+ and CD8+ T cell responses with a 27% response rate, increased circulating memory CD8+ T cells, and epitope spreading.24 Here, we detected neoantigen-specific CD4+ and CD8+ T cell responses in two of two analyzed DDFTFS patients, in comparison to zero of five non-DDFTFS patients (including short responders). These T cell clones were not detectable pretreatment, suggesting a role for GC and/or Ipi in the expansion of neoantigen-specific T cell clones in patients achieving DDFTFS.
In conclusion, the results of this study provide insights into the immunobiology of DDFTFS in mUC patients treated with cisplatin-based chemotherapy and ipilimumab. These findings suggest that a pre-existing adaptive immune response, enhanced by treatment with cisplatin-based chemotherapy and ipilimumab, may be responsible for long-term remission. Neoantigen-specific T cells may play a critical role in this response. The identification of markers of response may help identify patients most likely to benefit from chemotherapy plus ICI-based therapy.
Footnotes
Twitter: @JonAnker1, @MattGalsky
NB, SG and MDG contributed equally.
Contributors: Conceptualization: MDG, NB and SG. Formal analysis: JA, MDG and SG. Investigation: JA, MDG, SK-S, HW, RH, AU, NI, SE, TS, RS, NMH, MP, JQ, HX, NB and SG. Resources: MDG, NB and SG. Writing-original draft: JA and MDG. Writing-review and editing: JA, MDG, NB and SG. Visualization: JA, MDG and SG. Supervision: MDG and SG. Funding acquisition: MDG, NB and SG. Guarantor: MDG and SG.
Funding: This analysis was supported by Bristol-Myers Squibb, Cancer Research Institute Clinical Strategy Team Grant, and NIH P30 CA196521, CA224319, and DK124165.
Competing interests: SKP: Travel Support from CRISPR Therapeutics, Ipsen. HW: Employment from Sema4. AU: Employment from Sema4. RS: Employment from Sema4. NMH: Research funding from Novartis, OncoGenex, Mirati Therapeutics, Heat Biologics, Acerta Pharma, and Principia Biopharma; research funding and personal fees from Merck & Co, Bristol-Myers Squibb, AstraZeneca, Seattle Genetics, and Genentech; personal fees from Inovio, Pieris Pharmaceuticals, TARIS Biomedical, Champions Oncology, and Health Advances. NB: Extramural member of the Parker Institute for Cancer Immunotherapy; research funding from Regeneron, Harbor Biomedical, DC Prime, and Dragonfly Therapeutics; advisory boards of Neon Therapeutics, Novartis, Avidea, Boehringer Ingelheim, Rome Therapeutics, Rubius Therapeutics, Roswell Park Comprehensive Cancer Center, BreakBio, Carisma Therapeutics, CureVac, Genotwin, BioNTech, Gilead Therapeutics, Tempest Therapeutics, and the Cancer Research Institute. SG: Research funding from Genentech, Boehringer-Ingelheim, Celgene, Takeda, and Regeneron. MDG: Research funding from Bristol Myers Squibb, Novartis, Dendreon, Astra Zeneca, Merck, Genentech; advisory board/consultant for Bristol Myers Squibb, Merck, Genentech, AstraZeneca, Pfizer, EMD Serono, SeaGen, Janssen, Numab, Dragonfly, GlaxoSmithKline, Basilea, UroGen, Rappta Therapeutics, Alligator, Silverback, Fujifilm, Curis, Gilead, Bicycle, Asieris, Abbvie, Analog Devices.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The clinical trial, as previously reported, was conducted in accordance with the Declaration of Helsinki. The protocol was approved by the local ethics committees at each participating site and informed consent was provided by all patients before enrollment. Ethics committees/institutional review boards (IRBs) that approved the initial clinical trial included: Icahn School of Medicine at Mount Sinai IRB (GCO12-0026), Indiana University Melvin and Bren Simon Comprehensive Cancer Center IRB (1110007307), Virginia Oncology Associates Western IRB (1133348), Goshen Center for Cancer Care IRB (HCRN GU10-148), Nebraska Methodist Hospital IRB (1097), Texas Oncology-Baylor Charles A. Sammons Cancer Center IntegReview IRB (GU10-148), City of Hope Western IRB (1144435).
References
- 1. von der Maase H, Hansen SW, Roberts JT, et al. Gemcitabine and cisplatin versus methotrexate, Vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J Clin Oncol 2000;18:3068–77. 10.1200/JCO.2000.18.17.3068 [DOI] [PubMed] [Google Scholar]
- 2. von der Maase H, Sengelov L, Roberts JT, et al. Long-term survival results of a randomized trial comparing Gemcitabine plus cisplatin, with methotrexate, Vinblastine, doxorubicin, plus cisplatin in patients with bladder cancer. J Clin Oncol 2005;23:4602–8. 10.1200/JCO.2005.07.757 [DOI] [PubMed] [Google Scholar]
- 3. Sternberg CN, de Mulder P, Schornagel JH, et al. Seven year update of an EORTC phase III trial of high-dose intensity M-VAC chemotherapy and G-CSF versus classic M-VAC in advanced urothelial tract tumours. Eur J Cancer 2006;42:50–4. 10.1016/j.ejca.2005.08.032 [DOI] [PubMed] [Google Scholar]
- 4. Iyer G, Balar AV, Milowsky MI, et al. Multicenter prospective phase II trial of Neoadjuvant dose-dense Gemcitabine plus cisplatin in patients with muscle-invasive bladder cancer. J Clin Oncol 2018;36:1949–56. 10.1200/JCO.2017.75.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Van Allen EM, Mouw KW, Kim P, et al. Somatic Ercc2 mutations correlate with cisplatin sensitivity in muscle-invasive urothelial carcinoma. Cancer Discov 2014;4:1140–53. 10.1158/2159-8290.CD-14-0623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Plimack ER, Dunbrack RL, Brennan TA, et al. Defects in DNA repair genes predict response to Neoadjuvant cisplatin-based chemotherapy in muscle-invasive bladder cancer. European Urology 2015;68:959–67. 10.1016/j.eururo.2015.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sharma P, Shen Y, Wen S, et al. Cd8 tumor-infiltrating lymphocytes are predictive of survival in muscle-invasive urothelial carcinoma. Proc Natl Acad Sci USA 2007;104:3967–72. 10.1073/pnas.0611618104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. de Biasi AR, Villena-Vargas J, Adusumilli PS. Cisplatin-induced antitumor Immunomodulation: A review of Preclinical and clinical evidence. Clinical Cancer Research 2014;20:5384–91. 10.1158/1078-0432.CCR-14-1298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Galsky MD, Wang H, Hahn NM, et al. Phase 2 trial of Gemcitabine, cisplatin, plus Ipilimumab in patients with metastatic urothelial cancer and impact of DNA damage response gene mutations on outcomes. Eur Urol 2018;73:751–9. 10.1016/j.eururo.2017.12.001 [DOI] [PubMed] [Google Scholar]
- 10. Hulsen T, de Vlieg J, Alkema W. Biovenn – a web application for the comparison and visualization of biological lists using area-proportional Venn diagrams. BMC Genomics 2008;9:488. 10.1186/1471-2164-9-488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rubinsteyn A, Kodysh J, Hodes I, et al. Computational pipeline for the PGV-001 Neoantigen vaccine trial. Front Immunol 2017;8:1807. 10.3389/fimmu.2017.01807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Formenti SC, Rudqvist N-P, Golden E, et al. Radiotherapy induces responses of lung cancer to CTLA-4 blockade. Nat Med 2018;24:1845–51. 10.1038/s41591-018-0232-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Maier B, Leader AM, Chen ST, et al. A conserved Dendritic-cell regulatory program limits Antitumour immunity. Nature 2020;582:257–62.:E17. 10.1038/s41586-020-2326-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schumacher TN, Schreiber RD. Neoantigens in cancer Immunotherapy. Science 2015;348:69–74. 10.1126/science.aaa4971 [DOI] [PubMed] [Google Scholar]
- 15. Galsky MD, Guan X, Banchereau R, et al. 658Mo cisplatin (Cis)-Related Immunomodulation and efficacy with Atezolizumab (Atezo) + Cis- vs carboplatin (Carbo)-Based chemotherapy (Chemo) in metastatic urothelial cancer (mUC). Annals of Oncology 2021;32:S682–3. 10.1016/j.annonc.2021.08.054 [DOI] [Google Scholar]
- 16. Kiss RC, Xia F, Acklin S. Targeting DNA damage response and repair to enhance therapeutic index in cisplatin-based cancer treatment. Int J Mol Sci 2021;22:8199. 10.3390/ijms22158199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Diaz LA, Le DT. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med 2015;373:2509–20.:1979. 10.1056/NEJMc1510353 [DOI] [PubMed] [Google Scholar]
- 18. Sharma P, Sohn J, Shin SJ, et al. Efficacy and tolerability of Tremelimumab in locally advanced or metastatic urothelial carcinoma patients who have failed first-line platinum-based chemotherapy. Clinical Cancer Research 2020;26:61–70. 10.1158/1078-0432.CCR-19-1635 [DOI] [PubMed] [Google Scholar]
- 19. Galsky MD, Necchi A, Sridhar SS, et al. A phase III, randomized, open-label, multicenter, global study of first-line (1L) Durvalumab in combination with standard of care (Soc) chemotherapy and Durvalumab in combination with Tremelimumab and Soc chemotherapy versus Soc chemotherapy alone in patients with Unresectable locally advanced or metastatic urothelial cancer (UC). JCO 2019;37:TPS499. 10.1200/JCO.2019.37.7_suppl.TPS499 [DOI] [Google Scholar]
- 20. Lutfi F, Wu L, Sunshine S, et al. Targeting the Cd27-Cd70 pathway to improve outcomes in both Checkpoint Immunotherapy and allogeneic hematopoietic cell transplantation. Front Immunol 2021;12:715909. 10.3389/fimmu.2021.715909 Available: https://www.frontiersin.org/articles/10.3389/fimmu.2021.715909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wang L, Sfakianos JP, Beaumont KG, et al. Myeloid cell-associated resistance to PD-1/PD-L1 blockade in urothelial cancer revealed through bulk and single-cell RNA sequencing. Clinical Cancer Research 2021;27:4287–300. 10.1158/1078-0432.CCR-20-4574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Leko V, McDuffie LA, Zheng Z, et al. Identification of Neoantigen-reactive tumor-infiltrating lymphocytes in primary bladder cancer. The Journal of Immunology 2019;202:3458–67. 10.4049/jimmunol.1801022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Holm JS, Funt SA, Borch A, et al. Neoantigen-specific Cd8 T cell responses in the peripheral blood following PD-L1 blockade might predict therapy outcome in metastatic urothelial carcinoma. Nat Commun 2022;13:1935. 10.1038/s41467-022-29342-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ott PA, Hu-Lieskovan S, Chmielowski B, et al. A phase IB trial of personalized Neoantigen therapy plus anti-PD-1 in patients with advanced Melanoma, non-small cell lung cancer, or bladder cancer. Cell 2020;183:347–62. 10.1016/j.cell.2020.08.053 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2023-007613supp001.pdf (595.6KB, pdf)
Data Availability Statement
Data are available on reasonable request.