Abstract
Background
The perimenopausal and postmenopausal periods are associated with many symptoms, including sexual complaints. This review is an update of a review first published in 2013.
Objectives
We aimed to assess the effect of hormone therapy on sexual function in perimenopausal and postmenopausal women.
Search methods
On 19 December 2022 we searched the Gynaecology and Fertility Group Specialised Register, CENTRAL, MEDLINE, Embase, PsycINFO, CINAHL, LILACS, ISI Web of Science, two trials registries, and OpenGrey, together with reference checking and contact with experts in the field for any additional studies.
Selection criteria
We included randomized controlled trials that compared hormone therapy to either placebo or no intervention (control) using any validated assessment tool to evaluate sexual function. We considered hormone therapy: estrogen alone; estrogen in combination with progestogens; synthetic steroids, for example, tibolone; selective estrogen receptor modulators (SERMs), for example, raloxifene, bazedoxifene; and SERMs in combination with estrogen.
Data collection and analysis
We used standard methodological procedures recommended by Cochrane. We analyzed data using mean differences (MDs) and standardized mean differences (SMDs). The primary outcome was the sexual function score. Secondary outcomes were the domains of sexual response: desire; arousal; lubrication; orgasm; satisfaction; and pain. We assessed the certainty of the evidence using the GRADE approach.
Main results
We included 36 studies (23,299 women; 12,225 intervention group; 11,074 control group), of which 35 evaluated postmenopausal women; only one study evaluated perimenopausal women. The 'symptomatic or early postmenopausal women' subgroup included 10 studies, which included women experiencing menopausal symptoms (symptoms such as hot flushes, night sweats, sleep disturbance, vaginal atrophy, and dyspareunia) or early postmenopausal women (within five years after menopause). The 'unselected postmenopausal women’ subgroup included 26 studies, which included women regardless of menopausal symptoms and women whose last menstrual period was more than five years earlier. No study included only women with sexual dysfunction and only seven studies evaluated sexual function as a primary outcome. We deemed 20 studies at high risk of bias, two studies at low risk, and the other 14 studies at unclear risk of bias. Nineteen studies received commercial funding.
Estrogen alone versus control probably slightly improves the sexual function composite score in symptomatic or early postmenopausal women (SMD 0.50, 95% confidence interval (CI) (0.04 to 0.96; I² = 88%; 3 studies, 699 women; moderate‐quality evidence), and probably makes little or no difference to the sexual function composite score in unselected postmenopausal women (SMD 0.64, 95% CI −0.12 to 1.41; I² = 94%; 6 studies, 608 women; moderate‐quality evidence). The pooled result suggests that estrogen alone versus placebo or no intervention probably slightly improves sexual function composite score (SMD 0.60, 95% CI 0.16 to 1.04; I² = 92%; 9 studies, 1307 women, moderate‐quality evidence).
We are uncertain of the effect of estrogen combined with progestogens versus placebo or no intervention on the sexual function composite score in unselected postmenopausal women (MD 0.08 95% CI −1.52 to 1.68; 1 study, 104 women; very low‐quality evidence).
We are uncertain of the effect of synthetic steroids versus control on the sexual function composite score in symptomatic or early postmenopausal women (SMD 1.32, 95% CI 1.18 to 1.47; 1 study, 883 women; very low‐quality evidence) and of their effect in unselected postmenopausal women (SMD 0.46, 95% CI 0.07 to 0.85; 1 study, 105 women; very low‐quality evidence).
We are uncertain of the effect of SERMs versus control on the sexual function composite score in symptomatic or early postmenopausal women (MD −1.00, 95% CI −2.00 to ‐0.00; 1 study, 215 women; very low‐quality evidence) and of their effect in unselected postmenopausal women (MD 2.24, 95% 1.37 to 3.11 2 studies, 1525 women, I² = 1%, low‐quality evidence).
We are uncertain of the effect of SERMs combined with estrogen versus control on the sexual function composite score in symptomatic or early postmenopausal women (SMD 0.22, 95% CI 0.00 to 0.43; 1 study, 542 women; very low‐quality evidence) and of their effect in unselected postmenopausal women (SMD 2.79, 95% CI 2.41 to 3.18; 1 study, 272 women; very low‐quality evidence).
The observed heterogeneity in many analyses may be caused by variations in the interventions and doses used, and by different tools used for assessment.
Authors' conclusions
Hormone therapy treatment with estrogen alone probably slightly improves the sexual function composite score in women with menopausal symptoms or in early postmenopause (within five years of amenorrhoea), and in unselected postmenopausal women, especially in the lubrication, pain, and satisfaction domains. We are uncertain whether estrogen combined with progestogens improves the sexual function composite score in unselected postmenopausal women. Evidence regarding other hormone therapies (synthetic steroids and SERMs) is of very low quality and we are uncertain of their effect on sexual function. The current evidence does not suggest the beneficial effects of synthetic steroids (for example tibolone) or SERMs alone or combined with estrogen on sexual function. More studies that evaluate the effect of estrogen combined with progestogens, synthetic steroids, SERMs, and SERMs combined with estrogen would improve the quality of the evidence for the effect of these treatments on sexual function in perimenopausal and postmenopausal women.
Keywords: Female, Humans, Estrogens, Estrogens/therapeutic use, Perimenopause, Postmenopause, Progestins, Selective Estrogen Receptor Modulators
Plain language summary
Does hormone therapy improve sexual function in women going through or after menopause?
Key messages
• Estrogen (the hormone associated with sexual and reproductive development in women) alone probably improves sexual function scores compared to placebo.
• We are unsure of the effect of estrogen plus progestogens (another female hormone), synthetic steroids (such as tibolone), selective estrogen receptor modulators (that affect how estrogen works) or selective estrogen receptor modulators plus estrogen on sexual function compared to placebo or no treatment.
• Different hormone treatments and doses, and questionnaires used for assessment, may have caused the variation seen in results.
What is menopause and its effects on women?
Menopause is when women's periods stop, usually at around the age of 45 to 55 years. During menopause the ovaries gradually stop producing estrogen, the hormone that regulates periods. The reduction in estrogen can cause unwanted symptoms before periods stop (perimenopausal), during menopause and after menopause (postmenopausal). Symptoms include mood changes, hot flushes, and night sweats. Sexual complaints such as painful intercourse, lack of interest in sex, and problems related to arousal or orgasm are common after menopause and can affect women's self‐esteem, self‐confidence, and sexual health.
What is hormone therapy, and how might it help women’s sexual function?
Hormone therapy consists of various hormones or combinations of hormones that can help reduce menopausal symptoms. It can be given as skin patches, sprays or gels, tablets, or implants, and is used to treat a wide range of perimenopausal and postmenopausal symptoms. Hormone therapy might improve symptoms affecting sexual function such as dryness, itching, and painful intercourse by increasing lubrication, blood flow, and sensation in vaginal tissues.
What did we want to find out?
We wanted to find out if hormone therapy improves women's sexual functioning and whether effects are different in different stages of menopause. We were also interested in which types of hormone therapy were most effective: estrogen alone, estrogen combined with other hormones, or synthetic (manufactured) steroids or hormones.
What did we do?
We searched for studies that looked at the different types of hormone therapy compared to placebo (a dummy drug) or no treatment and its effect on sexual function in perimenopausal or postmenopausal women. We searched for studies that used estrogen alone; estrogen in combination with progestogens; synthetic steroids, (such as tibolone); selective estrogen receptor modulators (SERMs, that affect how estrogen works by blocking or activating different parts of the body, such as raloxifene or bazedoxifene); and selective estrogen receptor modulators combined with estrogen.
We were most interested in the effect of hormone therapy on the global sexual function score, which measures the effect of hormone therapy on all the areas of sexual function combined: desire, arousal, lubrication, orgasm, satisfaction and pain. We also wanted to know the effect of hormone therapy on the individual areas that make up the global sexual function score. Scores had to be evaluated using a recognised and validated questionnaire.
We divided women by length of time since their last period:
• within 5 years of their last period with or without menopausal symptoms; and
• more than 5 years since their last menstrual period, regardless of menopausal symptoms.
We compared and summarized the results of the studies and assessed our confidence in the evidence based on factors such as study methods and sizes.
What did we find?
We found 36 studies including 23,299 women. All but one study involved women after menopause; the other included women during menopause. Some but not all women had bothersome symptoms such as hot flushes, night sweats, and vaginal dryness.
• For women within 5 years of their last period, treatment with estrogen alone probably slightly improves sexual function based on the sexual function composite score compared to placebo.
• For women whose last period was more than 5 years earlier, estrogen alone probably makes little or no difference to sexual function based on sexual function scores compared to a placebo.
• For both groups of women, we are unsure of the effect of estrogen plus progestogens, synthetic steroids, selective estrogen receptor modulators alone, or selective estrogen receptor modulators plus estrogen on sexual function compared to placebo or no treatment.
What are the limitations of the evidence?
Our confidence in the evidence is moderate to very low due to variation in the results. This was probably because studies used different drugs and doses, and different questionnaires for assessment.
How up‐to‐date is the evidence?
The evidence is current to December 2022.
Summary of findings
Summary of findings 1. Hormonal therapy compared with placebo or no intervention for sexual function in symptomatic or early postmenopausal women.
| Hormonal therapy compared with placebo or no intervention for sexual function in symptomatic or early postmenopausal women | ||||||
|
Patient or population: symptomatic or early postmenopausal womena Settings: outpatient health centres in different regions of the world Interventionsb: estrogen alone, estrogen + progestogens, synthetic steroids (tibolone), SERMs, SERMs + estrogen Comparison: placebo or no intervention | ||||||
| Outcomes | Ilustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
|
Assumed risk (placebo or no intervention) |
Corresponding risk (hormonal therapy) |
|||||
| Estrogen alone Sexual function score measured by MENQoL sexual subscore (higher score = better sexual functioning); GCS sexual subscore (higher score = worse sexual functioning and for analysis, the scoring direction was reversed); and MSQ (higher score = better sexual functioning) | The mean score ranged from 0.71 to 46 | SMD 0.50, 95% higher (0.04 to 0.96 higher) | Not estimable | 699 (3 studies) |
⊕⊕⊕⊝ Moderatec | Probably slightly improves sexual function |
| Estrogen + progestogens | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported by any study in this comparison |
|
Synthetic steroids Sexual function score measured by WHQ sexual subscore (higher score = better sexual functioning) |
The mean score was 0.16 | SMD 1.32, 95% higher (1.18 to 1.47 higher) | Not estimable | 883 (1 study) |
⊕⊝⊝⊝ Verylowd,e | We are uncertain whether synthetic steroids improve sexual function |
|
SERMs Composite sexual function score measured by AESEX scale (higher score = worse sexual functioning and for analysis, the scoring direction was reversed) |
The mean score was 0.34 | MD −1.00, 95% lower (−2.00 lower to −0.00) | Not estimable | 215 (1 study) |
⊕⊝⊝⊝ Very lowc,d | We are uncertain whether SERMs improve sexual function |
|
SERMs + estrogen Composite sexual function score measured by ASEX scale (higher score = worse sexual functioning and for analysis, the scoring direction was reversed) |
The mean score was 2.0 | SMD 0.22, 95% higher (0.00 to 0.43 higher) | Not estimable | 542 (1 study) |
⊕⊝⊝⊝ Very lowc,d | We are uncertain whether SERMs + estrogen improve sexual function |
| *The basis for the assumed risk is the mean score. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group ‐ expressed as change in standardized mean difference. ASEX: Arizona Sexual Experiences scale; CI: confidence interval; GCS: Greene Climacteric Scale, sexual subscore (symptom 21); MD: mean difference; MENQoL: Menopause‐specific Quality of Life Questionnaire, sexual subscore; MSQ: McCoy Sex Scale Questionnaire; SERMs: selective estrogen receptor modulators; SMD: standardized mean difference; WHQ: Women's Health Questionnaire, sexual subscore | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aSymptomatic or early postmenopausal women: this subgroup included women with any menopause‐related symptoms (not only sexual dysfunction) or postmenopausal women less than 5 years from the last menstrual period. In this group, only one study included perimenopausal women, defined as women who had their last menstrual period within 12 months of inclusion.
bInterventions
- Oral hormone therapy: tibolone 2.5 mg/day; bazedoxifene 20 mg/day; bazedoxifene 20 mg conjugated estrogen 0.45 mg /day; bazedoxifene 20 mg, conjugated estrogen 0.625 mg /day.
- Transdermal hormone therapy: estradiol 0.014 mg/d, patch delivering micro‐dose; estradiol 50 ug, twice a week.
- Local hormone therapy: estradiol 50 ug/day, vaginal route.
cDowngraded by one level for serious risk of bias: most domains of risk of bias were assessed as 'unclear'. dDowngraded by two levels for serious imprecision or inconsistency: wide confidence interval and only one study in this analysis, small sample size, and low event rate. eDowngraded by two levels for very serious risk of bias; inadequate randomization, allocation concealment, and/or no evidence of blinding or other sources of bias.
Summary of findings 2. Hormonal therapy compared with placebo or no intervention for sexual function in unselected postmenopausal women.
| Hormonal therapy compared with placebo or no intervention for sexual function in unselected postmenopausalwomen | ||||||
|
Population: unselected postmenopausal womena Settings: outpatient health centres in different regions of the world Interventionsb: estrogen alone, estrogen + progestogens, synthetic steroids (tibolone), SERMs, SERMs + estrogen Comparison: placebo or no intervention | ||||||
| Outcomes | Ilustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
|
Assumed risk (placebo or no intervention) |
Corresponding risk (hormonal therapy) |
|||||
|
Estrogen alone Sexual function score measured by FSFI (higher score = better sexual functioning); WHQ sexual subscore (higher score = better sexual functioning); MENQoL sexual subscore (higher score = better sexual functioning) |
The mean score ranged from 2.3 to 25.14 | SMD 0.64, 95% higher (−0.12 lower to 1.41 higher) | Not estimable | 608 (6 studies) |
⊕⊕⊕⊝ Moderatec | Probably little or no difference in sexual function |
|
Estrogen + progestogens Sexual function score measured by WHQ sexual subscore (higher score = better sexual functioning) |
The mean score was 12.72 | MD 0.08, 95% higher (−1.52 to 1.68 higher) | Not estimable | 104 (1 study) |
⊕⊝⊝⊝ Very lowc,d | We are uncertain whether estrogen + progestogens improve sexual function |
|
Synthetic steroids Sexual function score measured by FSFI; WHQ sexual subscore (higher score = better sexual functioning) |
The mean score ranged from 0.16 to 14.4 | SMD 0.46 higher (0.07 to 0.85 higher) | Not estimable | 105 (1 study) |
⊕⊝⊝⊝ Very lowc,d | We are uncertain whether synthetic steroids improve sexual function |
|
SERMs Sexual function score measured by FSFI (higher score = better sexual functioning) |
The mean score ranged from 5.7 to 6.69 | MD 2.24, 95% higher (1.3715 to 3.11 higher) | Not estimable | 1525 (2 studies) |
⊕⊕⊝⊝ Lowd |
May slightly improve sexual function |
|
SERMs + estrogen Sexual function score measured by MENQoL sexual subscore (higher score = better sexual functioning) |
The mean score was 1.35 | SMD 2.79, 95% higher (2.41 to 3.18 higher) | Not estimable | 272 (1 study) |
⊕⊝⊝⊝ Very lowc,d | We are uncertain whether SERMs + estrogen improve sexual function |
| *The basis for the assumed risk is the mean score ranged. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group ‐ standardized mean difference. CI: confidence interval; FSFI: Female Sexual Function Index; MD: mean difference; MENQoL: Menopause‐specific Quality of Life Questionnaire, sexual subscore; SERMs: selective estrogen receptor modulators; SMD: standardized mean difference; WHQ: Women's Health Questionnaire, sexual subscore | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate or other sources of bias. Very low quality: we are very uncertain about the estimate. | ||||||
aUnselected postmenopausal women: this subgroup included women regardless of menopausal symptoms and allowed inclusion of women whose final menstrual period was more than five years earlier. bInterventions
- Oral hormone therapy: equine estrogen 0.625 mg/day; estradiol valerate 2 mg/day; tibolone 2.5 mg/day; ospemifene 60 mg/day; bazedoxifene 20 mg conjugated estrogen 0.45 mg/day; bazedoxifene 20 mg conjugated estrogen 0.625 mg/day.
- Local hormone therapy: conjugated estrogen 0.625 mg/day, vaginal route; estradiol ovule 0.03 mg/day, vaginal route; estradiol tablet 10 mg/day, vaginal route; estradiol 10.3 tablet ug/day, vaginal route; estradiol 0.625 mg/day.
cDowngraded by one level for serious risk of bias: most domains of risk of bias were assessed as 'unclear'. dDowngraded by two levels for serious imprecision and inconsistency: wide confidence interval and only one study in this analysis, small sample size, and low event rate. eDowngraded by two levels for very serious risk of bias; inadequate randomization, allocation concealment, and/or no evidence of blinding or other sources of bias.
Background
Sexual function is a very important aspect of women’s health. In theory, hormone therapy may benefit aspects of a woman's sexual health. Medical counselling about hormone therapy should balance the benefits and risks, and take into account the aggregate value of hormone therapy (NAMS 2017; Santen 2010). Thus, information regarding the influence of hormone therapy on sexual function is important when considering the use of these drugs (Wierman 2010). This review was developed to help healthcare professionals make decisions about the use of hormone therapy to alleviate symptoms related to sexual dysfunction during perimenopause and postmenopause.
Description of the condition
Menopause is defined as occurring after 12 consecutive months of spontaneous amenorrhoea with no obvious pathologic cause (NAMS 2017); induced menopause is defined as the permanent cessation of menstruation after either surgical removal of the ovaries or iatrogenic ablation of ovarian function, for example, chemotherapy or pelvic radiation therapy (NAMS 2017). With the onset of menopause, women can experience problems related to hormonal changes (Avis 2015; Nappi 2009a; Whiteley 2013), such as vasomotor symptoms (hot flushes and night sweats; 75%), sleep disruption (40% to 60%), mood changes, cognitive decline, headaches (12%), vaginal dryness (83%), pain during intercourse (42%), soreness (27%), itching (26%), and burning (14%) (Monteleone 2018). Another important problem is the increase in sexual disorders, which increase from 27.2% in women aged 18 to 44 years to 44.6% in women between 45 and 64 years (Simon 2018). Hypoestrogenism associated with menopause promotes changes in the vaginal wall such as vaginal epithelium thinning and reduction in vessel density in the lamina propria layer (da Silva Lara 2009a; da Silva Lara 2009b), leading to poor lubrication and dyspareunia (Worsley 2017).
The most frequent sexual complaint in women after menopause is hypoactive sexual desire disorder (HSDD) (McCabe 2016a; Worsley 2017), defined as a persistent absence of sexual drive, sexual fantasies, and reduced desire for sexual activities for at least six months, followed by interpersonal difficulties or personal distress, or both (Basson 2000). Hormone therapy is a generic term that refers to any hormone therapy used in postmenopausal women for the alleviation of menopause‐related symptoms including vasomotor symptoms and genitourinary syndrome of menopause. Hormone therapy also has a positive effect on bone health (Flores 2021), and has also been studied in various settings. Clinical benefit has been observed when hormone therapy is used to relieve hot flushes and night sweats (Formoso 2012; MacLennan 2004), and for the relief of vaginal atrophy symptoms (Lethaby 2016). There is evidence that women using estrogen therapy are more likely to report sexual activity compared to controls using a placebo (Gass 2019). The most commonly used types of hormone therapy are estrogen alone, estrogen in combination with progestogens, synthetic steroids (for example tibolone), and selective estrogen receptor modulators (SERMs, for example, raloxifene). Other substances, such as androgens and phytoestrogen, might be used to relieve some menopausal‐related symptoms; however, we will not evaluate the effect of these drugs in this review because they are not widely accepted as hormone therapy.
Description of the intervention
Hormone therapy is a generic term that refers to any type of hormone therapy used during menopause for the alleviation of menopause‐related symptoms (Santen 2010). Clinical benefit has been observed when hormone therapy is used for the relief of hot flushes and night sweats (Formoso 2012; MacLennan 2004), and for the relief of vaginal atrophy symptoms (Lethaby 2016). Hormone therapy may be indicated to alleviate vasomotor symptoms and dyspareunia (Lethaby 2016; NAMS 2017). A meta‐analysis showed that hormone therapy treatment with estrogen alone or in combination with progestogens was associated with a small to moderate improvement in sexual problems, particularly in pain, when used in women with menopausal symptoms or even in asymptomatic women in early postmenopause (within five years of amenorrhoea), but not in postmenopausal women (Nastri 2013). The most commonly used types of hormone therapy are estrogen alone, estrogen in combination with progestogen, synthetic steroids such as tibolone, and selective estrogen receptor modulators (SERMs), for example, raloxifene. We examined the effect of these types of hormone therapy on sexual function in perimenopausal and postmenopausal women.
How the intervention might work
Sexual desire seems to be regulated by hormones and neurotransmitters of excitatory pathways such as dopamine, norepinephrine, melanocortin, and oxytocin (Clayton 2010). In animal models, estrogen facilitates dopamine release, and dopamine appears to enhance sexual desire, subjective arousal, and the interest to engage in sex following sexual stimulus (Hull 1999). This mechanism may be compromised by hypoestrogenism after menopause. Women with hot flushes and night sweats may find that their subsequent poor sleep patterns lead to tiredness and loss of energy. In addition, vaginal symptoms may affect women’s self‐esteem, self‐confidence, and sexual health (Portman 2014b). For perimenopausal and postmenopausal women, hormone therapy might improve hot flushes and night sweats as well as the symptoms of vulvovaginal atrophy increasing lubrication, blood flow, and sensation in vaginal tissues (NAMS 2017), and consequently, improve sexual functioning by directly impacting the dimensions of desire, arousal, lubrication, orgasm, satisfaction and sexual pain described in the literature (Basson 2000).
Why it is important to do this review
The World Health Organization (WHO) classifies sexual function as a cornerstone of quality of life irrespective of ageing (Few 1997). In fact, a cohort study with middle‐aged women in the USA showed that almost half of them considered sexual activity to be of moderate to extreme importance for a good quality of life, and thus, doctors should address this issue mainly in gynaecological outpatient care (Cain 2003). Despite its importance, female sexual function is not easy to investigate because it depends on several factors such as health, well‐being, cultural habits, socioeconomic status, relationship issues, and the presence of a partner, who may also have some health issues (Davis 2009). Female sexual dysfunction might be evaluated in different domains: sexual desire; arousal; orgasm; satisfaction; and pain (Basson 2000, McCabe 2016b). Although sexual function declines throughout the menopause transition (NAMS 2017; Rosen 2012), it is unclear whether this is caused by the lowering of estrogen levels, ageing, or both (da Silva Lara 2009a; Nappi 2009a).
The true effect of hormone therapy on sexual function is difficult to determine based on the literature published so far (McCabe 2016b); partially because of the different drugs and doses, different tools to evaluate the sexual function, and the particular population studied in each study. All these aspects highlight the importance of carrying out this review, which seeks to provide new evidence regarding the prescription of hormone therapy for the relief of sexual disorders during menopause. This review includes meta‐analysis data obtained using Review Manager software (Review Manager 2020), and includes the latest evidence on the effect of hormone therapy (HT) on sexual function in perimenopausal and postmenopausal women.
Objectives
We aimed to assess the effect of hormone therapy on sexual function in perimenopausal and postmenopausal women.
Methods
Criteria for considering studies for this review
Types of studies
We included published and unpublished randomized controlled trials (RCTs). We excluded non‐randomized studies (for example studies with evidence of inadequate sequence generation such as alternate days, and patient numbers) as they are associated with a high risk of bias. We included cross‐over studies but we planned to include in the meta‐analysis only data from the first phase, as the cross‐over is not a valid design in this context. The withdrawal of hormone therapy may cause symptoms, being a potential source of bias.
Types of participants
We defined perimenopausal women as women with menopausal symptoms who had their last menstrual period within the 12 months before inclusion in the study. We defined postmenopausal women as women with induced menopause (bilateral oophorectomy, as a result of chemotherapy or pelvic radiation therapy) or natural menopause (12 consecutive months of spontaneous amenorrhoea with no obvious pathologic cause or with at least six months of amenorrhoea and elevated follicle‐stimulating hormone (FSH)). We grouped the studies by participant characteristics with regard to menopausal symptoms. The symptomatic (women who experienced vasomotor or other menopausal symptoms) or early menopausal (up to five years postmenopause) group, and the unselected postmenopausal group, which included women regardless of menopausal symptoms and allowed inclusion of women whose last menstrual period was more than five years earlier.
Types of interventions
Prescription of hormone therapy compared with the prescription of placebo or no intervention. We considered hormone therapy, estrogen alone; estrogen in combination with progestogens; synthetic steroids (for example tibolone); SERMs (for example raloxifene, bazedoxifene); and SERMs in combination with estrogen. We did not include other drugs possibly used in the relief of menopausal symptoms in this review. In particular, we did not review studies on testosterone as this is the topic of another Cochrane Review (Somboonporn 2005). We only included studies in which the interval between the onset of the intervention and the assessment of outcomes was one month or more. In studies with multiple assessments, we considered only assessments between three and six months after starting the intervention.
Types of outcome measures
Primary outcomes
Sexual function
The primary outcome was the evaluation of the sexual function composite score, measured by validated tools.
Sexual function composite score
Secondary outcomes
Domains of sexual function
The secondary outcomes were the evaluation of the multidimensional domains of sexual function: desire, arousal, lubrication, orgasm, satisfaction, and pain (Basson 2000; McCabe 2016b), scored by validated tools.
Desire
Arousal
Lubrication
Orgasm
Satisfaction
Pain
We did not include adverse events related to hormone therapy as outcomes because we only included studies that reported sexual function; therefore, evidence for these topics would be a subset of the overall body of evidence, which could not be representative of the complete current evidence. In order to help weigh the benefits and harms of the treatments, we took into account the findings of other systematic reviews that addressed adverse events (see Discussion).
Search methods for identification of studies
We searched for RCTs following a search strategy developed in consultation with the Cochrane Gynaecology and Fertility Information Specialist. There was no language restriction in these searches.
Electronic searches
We searched for RCTs using the following electronic databases:
Cochrane Gynaecology and Fertility Specialised Register, ProCite platform, searched 19 December 2022 (Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL; 2022, Issue 12) via the Cochrane Register of Studies Online (CRSO), Web platform, searched 19 December 2022 (Appendix 2);
MEDLINE, Ovid platform, searched from 1946 to 19 December 2022 (Appendix 3), this search was combined with the Cochrane highly sensitive search strategy for identifying randomized trials (Lefebvre 2022);
Embase, Ovid platform, searched from 1980 to 19 December 2022 (Appendix 4), this search was combined with trial filters developed by Scottish Intercollegiate Guidelines Network (SIGN) www.sign.ac.uk/what-we-do/methodology/search-filters/);
PsycINFO, Ovid platform, searched form 1806 to 19 December 2022 (Appendix 5);
CINAHL (Cumulative Index to Nursing and Allied Health Literature), Ebsco platform, searched from 1961 to 19 December 2022 (Appendix 6);
LILACS (Literatura Latino‐Americana e do Caribe em Ciências da Saúde), Web platform, searched 19 December 2022 (Appendix 7);
We searched for study protocols and ongoing trials using the following websites: ClinicalTrials.gov (Appendix 8); ISRCTN registry (Appendix 9); and the World Health Organization International Clinical Trials Registry Platform search portal (Appendix 10), Web platforms, searched 21 May 2018, more recent trial registrations were found in the CENTRAL 2022 output;
We searched for conference abstracts in the Web of Science, Web platform, and searched 19 December 2022 (Appendix 11).
Searching other resources
We handsearched the reference list of relevant articles retrieved by the search and contacted experts in the field for any additional studies. We also handsearched relevant journals and conference abstracts.
Data collection and analysis
Selection of studies
In this update, two review authors (MFT and JBPF) independently performed an initial screen of the titles and abstracts retrieved by the search; disagreements were resolved by discussion with another review author (LASL). We retrieved the full texts of all potentially eligible studies. Two review authors (MFT and DCR) independently examined these full‐text articles for compliance with the inclusion criteria and selected studies eligible for inclusion in the review. We resolved disagreements about study eligibility by discussion with another review author (WMP). We corresponded with study authors, as required, to clarify study eligibility. The selection process is documented in a PRISMA flow chart (Moher 2009; Figure 1).
1.
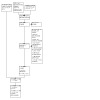
Study flow diagram
Data extraction and management
In this update, two review authors (MFT and DCR) independently extracted data from eligible studies using a data extraction form designed and pilot‐tested by the review authors. We resolved any disagreements by discussion or by consulting a third review author (LASL). Data extracted included study characteristics and outcome data. Where studies had multiple publications, we used the main trial report as the reference and derived additional details from secondary papers. We corresponded with study investigators for further data on methods or results as required.
Assessment of risk of bias in included studies
Two review authors (MFT and LASL) independently assessed the included studies for risk of bias using Cochrane RoB 1 (Higgins 2011), to assess: selection (random sequence generation and allocation concealment); performance (blinding of participants and personnel); detection (blinding of outcome assessors); attrition (incomplete outcome data); reporting (selective reporting); and other bias. We assigned judgements as recommended in section 8.5 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved disagreements through discussion. We described all judgements fully and presented the conclusions in the risk of bias table. We incorporated the consideration of bias risk into the interpretation of review findings by means of sensitivity analyses (see Sensitivity analysis).
When evaluating selective reporting bias, we took care to search for within‐trial selective reporting, such as studies failing to report obvious outcomes, or reporting them in insufficient detail to allow inclusion. We sought published protocols and compared the outcomes between the protocol and the final published study.
Measures of treatment effect
For continuous data measured with the same scale, we calculated the mean difference (MD) using the inverse variance method and for continuous data measured with different scales, we calculated the standardized mean difference (SMD; Suissa 1991; Walter 2001), using the inverse variance method. We used a fixed‐effect model unless we considered statistical heterogeneity to be substantially high, that is, with I² statistic (Higgins 2003), values of above 50%, then we used a random‐effects model. Wherever studies presented two groups with the same intervention (for example two different dosages), we combined them to create a single pair‐wise comparison to prevent loss of information related to the results (Higgins 2022). We reversed the direction of the effect of individual studies, if required, to ensure consistency across studies. We treated ordinal data as continuous data. We presented 95% confidence intervals (CI) for all outcomes. Where data to calculate SMDs were not available, we utilized the most detailed numerical data available that might facilitate a similar analysis of included studies (for example, P values). When studies reported sufficient detail to calculate MDs but gave no information on the associated standard deviation (SD), we assumed the outcome to have an SD equal to the highest SD from other studies using the same assessment scale. We compared the magnitude and direction of effects reported by studies with how they were presented in the review, taking into account legitimate differences. We included both data reported as final mean scores in each group and mean change scores from baseline in each group. Where studies reported both values, we preferentially included mean change scores from the baseline.
We graded the effect size according to the SMD or MD, based on the following criteria: SMD or MD less than 0.41 was equivalent to a small effect, SMD or MD from 0.40 to 0.70 was a moderate effect, SMD or MD more than 0.70 was a large effect (Norman 2003). We interpreted the effect size according to the recommendations of Cochrane Gynaecology and Fertility. We interpreted the categories based on the following criteria: SMD more than 0.7 was equivalent to important results; SMD from 0.2 to 0.7 means less important results; and SMD less than 0.2 means non‐important results, based on established criteria for effect size (Norman 2003).
Unit of analysis issues
The primary analysis was per randomized woman.
Dealing with missing data
We analyzed the data on an intention‐to‐treat basis as far as possible and attempted to obtain missing data from the original studies. If studies reported sufficient detail to calculate MDs but did not give any information on the associated SDs, we assumed the outcomes to have SDs equal to the highest SD from other studies within the same analysis.
Assessment of heterogeneity
We considered whether the clinical (participants and type of hormonal therapy) and methodological (study design, time cut‐off points in the measurement of sexual function) characteristics of the included studies were sufficiently similar for meta‐analysis to provide a clinically meaningful summary. We assessed statistical heterogeneity by the I² statistic (Higgins 2003). An I² statistic value greater than 50% was taken to indicate substantial heterogeneity (Deeks 2022). Where we found substantial heterogeneity, we explored additional sources of heterogeneity in the cases of the diversity of measurement tools used to assess sexual function and different doses and routes of administration of hormonal therapy.
Assessment of reporting biases
In view of the difficulty in detecting and correcting for publication bias and other reporting biases, the review authors aimed to minimize their potential impact by ensuring a comprehensive search for eligible studies and by being alert for duplication of data. If there were 10 or more studies in an analysis, we planned to use a funnel plot to explore the possibility of small study effects (a tendency for estimates of the intervention effect to be more beneficial in smaller studies).
Data synthesis
If the studies were sufficiently similar, we combined the data using a fixed‐effect or random‐effects model in the following comparisons.
-
Estrogen alone versus placebo or no intervention, stratified by the characteristics of the included participants:
studies that only included symptomatic women (symptoms such as hot flushes, night sweats, sleep disturbance, vaginal atrophy, and dyspareunia) or early postmenopausal women (within the five years after menopause), to verify if hormone therapy could improve the sexual function of women complaining of sexual dysfunction with the onset of menopause;
studies that included unselected postmenopausal women (regardless of menopausal symptoms, with or without sexual dysfunction) to verify whether hormone therapy can improve the sexual function of these women.
-
Estrogen combined with progestogens versus placebo or no intervention:
studies that only included women with menopausal symptoms or women with less than five years since the onset of menopause, or both (early postmenopausal);
studies that included unselected postmenopausal women.
-
Synthetic steroids (tibolone) versus placebo or no intervention:
studies that only included women with menopausal symptoms or women with less than five years since the onset of menopause, or both (early postmenopausal);
studies that included unselected postmenopausal women.
-
SERMs (raloxifene and bazedoxifene) versus placebo or no intervention:
studies that only included women with menopausal symptoms or women with less than five years since the onset of menopause, or both (early postmenopausal);
studies that included unselected postmenopausal women.
-
SERMs (bazedoxifene) combined with estrogen versus placebo or no intervention:
studies that only included women with menopausal symptoms or women with less than five years since the onset of menopause, or both (early postmenopausal);
studies that included unselected postmenopausal women.
An increase in a particular outcome, which may be beneficial (for example composite score) or detrimental (for example dyspareunia), was displayed graphically in the meta‐analysis to the right of the centre‐line and a decrease in an outcome to the left of the centre‐line. We merged women with menopausal symptoms with early postmenopausal women (STRAW stage +1; STRAW 2008), because menopausal‐related symptoms are common in early postmenopausal women with almost half of such women reporting experiencing vasomotor symptoms (Gold 2000). We did not observe any important heterogeneity when we compared the subgroups used for stratification. We planned to carry out pooled analysis when there was no significant heterogeneity, that is, when we observed an I² statistic of less than 50% in the subgroup difference test.
Subgroup analysis and investigation of heterogeneity
We planned the stratification based on the characteristics of the included participants described above (studies that only included women with menopausal symptoms or less than five years since the onset of menopause, or both; and studies that included unselected postmenopausal women) and according to clinically reasonable time points after the intervention (a group between 12 and 16 weeks; and a group between 22 and 26 weeks, depending on the available studies). When we detected substantial heterogeneity, we explored possible explanations by again checking the data and by sensitivity analyses. If it persisted, we adopted a random‐effects model in order to have a more conservative estimate of the effect. We took any statistical heterogeneity into account when interpreting the results, especially if there was a variation in the direction of effect.
Sensitivity analysis
We conducted sensitivity analyses for the primary outcome (sexual function composite score) to determine whether the conclusion would be different if we restricted eligibility to studies without a high risk of bias for our main comparison, hormone therapy compared with placebo or no intervention for sexual function composite score in symptomatic or recently postmenopausal women; and unselected postmenopausal women.
Summary of findings and assessment of the certainty of the evidence
We prepared summary of findings tables using GRADEpro GDT and Cochrane methods for hormonal therapy compared with no intervention or placebo for the main review outcome, sexual function composite score (Schünemann 2021a). The summary of findings tables show the evaluation of the overall quality of the body of evidence for sexual function composite score for the review comparisons (estrogen alone; estrogen in combination with progestogens; synthetic steroids; SERMs; and SERMs in combination with estrogen) for symptomatic or recently postmenopausal women (Table 1) and unselected postmenopausal women (Table 2).
We assessed the quality of the evidence using GRADE criteria: risk of bias, consistency of effect, indirectness, imprecision, and publication bias (Schünemann 2021b). Two review authors working independently made judgements about evidence quality (high, moderate, low, or very low), with disagreements resolved by discussion. We justified, documented, and incorporated our judgements into the reporting of results for each outcome. We interpreted the effect according to guidance from Cochrane Gynaecology and Fertility.
Results
Description of studies
Results of the search
We performed the last search for this updated review on 19 December 2022. We included nine new studies in this update (Archer 2019; Bumphenkiatikul 2020; Bushmakin 2014; Caruso 2020; Constantine 2015; Diem 2018; Mitchell 2018; Seyyedi 2016; Taylor 2017).
At the update, we assessed 80 studies at the full‐text stage and excluded 59 studies. See Figure 1 for an overview of the search results. We tried to contact all study authors to retrieve unpublished details. See details of included studies in Characteristics of included studies and reasons for excluding studies in the Characteristics of excluded studies.
Seven studies are awaiting classification because we are awaiting a response from the authors (Hirschberg 2020; NCT01845649; NCT02460302; NCT02834312; NCT03363997; Pinkerton 2017; Tanmahasamut 2020), and four studies are ongoing because they are still at the protocol stage or have not yet reported the results on the effect of hormone therapy on sexual function (NCT02668796; NCT02859285; NCT02670785; NCT03116022).
Included studies
We included 36 studies: 34 parallel‐group and two cross‐over studies (Fonseca 2007; Laan 2001). Sixteen studies were single‐centre studies. Four were conducted in the USA (Constantine 2015; Dayal 2005; Mitchell 2018; Taylor 2017), three in Brazil (Fonseca 2007; Mameri Filho 2005; Morais‐Socorro 2012), two in Italy (Caruso 2020; Gambacciani 2011), one in Iran (Seyyedi 2016), one in Poland (Czarnecka 2000), one in Romania (Hudita 2003), one in Taiwan (Yang 2004), one in Thailand (Bumphenkiatikul 2020), one in Turkey (Osmanagaoglu 2006) and one in the Netherlands (Laan 2001). Fourteen studies were multi‐centre, performed in only one country: nine in the USA (Archer 2019;Bushmakin 2014;Diem 2018; Huang 2008; Maki 2007; SMART‐3; Speroff 2003; Strickler 2000; WHI 1999), two in Estonia (Hemminki 2009; Veerus 2006), two in Sweden (Nathorst‐Böös 1993; Wiklund 1993), and one in Denmark (Nielsen 2006). Seven studies were multi‐centre studies conducted in more than one country: two in Canada and USA (Modugno 2003; Simon 2007); one in Brazil and USA (Gast 2009); one in Hong Kong, Malaysia, Philippines, Singapore, and Thailand (Haines 2009); one in Australia, New Zealand, and UK (WISDOM 2008); and one study was conducted in 31 countries (Liberate 2011).
Twenty studies were suitable for meta‐analysis, of these, 12 were included in the previous review (Dayal 2005; Haines 2009; Laan 2001; Liberate 2011; Maki 2007; Morais‐Socorro 2012; Nathorst‐Böös 1993; Osmanagaoglu 2006; SMART‐3; Speroff 2003; Wiklund 1993; Yang 2004), and eight were newly included studies for meta‐analysis (Archer 2019; Bumphenkiatikul 2020; Bushmakin 2014; Caruso 2020; Constantine 2015; Diem 2018; Mitchell 2018; Seyyedi 2016). Sixteen studies evaluated sexual function, but the reported data were not suitable for meta‐analysis (Czarnecka 2000; Fonseca 2007; Gambacciani 2011; Gast 2009; Hemminki 2009; Huang 2008; Hudita 2003; Mameri Filho 2005; Modugno 2003; Nielsen 2006; Simon 2007; Strickler 2000; Taylor 2017; Veerus 2006; WHI 1999; WISDOM 2008). Twenty‐five studies received funding from the manufacturer of the study drug .
Participants
The studies included 12,225 women in the treatment groups and 11,074 in the control groups: the total score and all domains of sexual function were assessed in 2554 women in the treatment groups and 2296 women in the control groups. We divided the available trial subgroups according to the participants’ characteristics (symptomatic or early postmenopausal, or unselected postmenopausal women; Types of participants).
Ten studies included symptomatic or early postmenopausal women (Bumphenkiatikul 2020; Bushmakin 2014; Gambacciani 2011; Haines 2009; Liberate 2011; Mameri Filho 2005; Morais‐Socorro 2012; SMART‐3; Speroff 2003; Wiklund 1993), and 26 studies included unselected postmenopausal women (Archer 2019; Caruso 2020; Constantine 2015; Czarnecka 2000; Dayal 2005; Diem 2018; Fonseca 2007; Gast 2009; Hemminki 2009; Huang 2008; Hudita 2003; Laan 2001; Maki 2007; Mitchell 2018; Modugno 2003; Nathorst‐Böös 1993; Nielsen 2006; Osmanagaoglu 2006; Seyyedi 2016; Simon 2007; Strickler 2000; Taylor 2017; Veerus 2006; WHI 1999; WISDOM 2008; Yang 2004). No study included only women with sexual dysfunction, and only seven studies evaluated sexual function as a primary outcome (Constantine 2015; Fonseca 2007; Gast 2009; Mameri Filho 2005; Nathorst‐Böös 1993; Osmanagaoglu 2006; Taylor 2017). One study included only women in perimenopause (Morais‐Socorro 2012); two studies included only women within 36 months of menopause (Maki 2007; Taylor 2017); one included only women up to five years after the last menstrual period (Nielsen 2006); six studies included only women with vasomotor or other menopausal symptoms (Archer 2019; Gambacciani 2011; Haines 2009; Nathorst‐Böös 1993; Speroff 2003; Wiklund 1993); one study included women with hot flushes and sexual dysfunction (Mameri Filho 2005).
Interventions
Out of the 36 included studies:
18 studies compared estrogen alone versus control (Caruso 2020; Czarnecka 2000; Dayal 2005; Diem 2018; Fonseca 2007; Haines 2009; Huang 2008; Mameri Filho 2005; Mitchell 2018; Nathorst‐Böös 1993; Nielsen 2006; Seyyedi 2016; Simon 2007; Speroff 2003; Taylor 2017; WHI 1999; Wiklund 1993; WISDOM 2008);
nine studies compared estrogen combined with progestogens versus control (Gambacciani 2011; Gast 2009; Hemminki 2009; Maki 2007; Osmanagaoglu 2006; Strickler 2000; Veerus 2006; WHI 1999; Yang 2004);
five studies compared synthetic steroids (tibolone) versus control (Hudita 2003; Laan 2001; Liberate 2011; Morais‐Socorro 2012; Osmanagaoglu 2006);
five studies compared SERMs (raloxifene, bazedoxifene, ospemifene) versus control (Archer 2019; Bushmakin 2014; Modugno 2003; SMART‐3; Strickler 2000);
two studies compared SERMs combined with estrogen versus control (Bushmakin 2014; SMART‐3);
five studies investigated the effect of more than one hormone versus control (Bushmakin 2014; Osmanagaoglu 2006; SMART‐3; Strickler 2000; WHI 1999).
In 19 studies the follow‐up period was three months (Archer 2019; Bumphenkiatikul 2020; Constantine 2015; Czarnecka 2000; Dayal 2005; Diem 2018; Gambacciani 2011; Gast 2009; Haines 2009; Laan 2001; Mameri Filho 2005; Mitchell 2018; Morais‐Socorro 2012; Nathorst‐Böös 1993; Seyyedi 2016; Simon 2007; Speroff 2003; Taylor 2017; Wiklund 1993); in one study the follow‐up period was 5.5 months (Yang 2004); in three studies the follow‐up was 12 weeks (Bushmakin 2014; Hemminki 2009; SMART‐3); in two studies the follow‐up period was four months (Caruso 2020; Maki 2007); in four studies the follow‐up period was six months (Fonseca 2007; Hudita 2003; Osmanagaoglu 2006; Veerus 2006); in one study the follow‐up period was 26 weeks (Liberate 2011); in three studies the follow‐up period was 12 months (Strickler 2000; WHI 1999; WISDOM 2008); in two studies the follow‐up period was 24 months (Huang 2008; Nielsen 2006); and in one study the follow‐up period was 36 months (Modugno 2003).
In 33 studies women in the control group used a matching placebo and in three studies women in the control group did not receive any intervention (Czarnecka 2000; Osmanagaoglu 2006; Veerus 2006). We merged groups where studies had more than one group that used the same drug, in different doses (Bushmakin 2014; Caruso 2020; SMART‐3; Speroff 2003; Strickler 2000). Sixteen studies evaluated sexual function but the reported data were not suitable for meta‐analysis (Czarnecka 2000; Fonseca 2007; Gambacciani 2011; Gast 2009; Hemminki 2009; Huang 2008; Hudita 2003; Mameri Filho 2005; Modugno 2003; Nielsen 2006; Simon 2007; Strickler 2000; Taylor 2017; Veerus 2006; WHI 1999; WISDOM 2008). Of those studies, eight compared estrogen combined with progestogens against placebo (Fonseca 2007; Gambacciani 2011; Gast 2009; Hemminki 2009; Maki 2007; Veerus 2006; WHI 1999; WISDOM 2008), and two studies compared synthetic steroids (tibolone) with placebo (Liberate 2011; Osmanagaoglu 2006)
Most interventions were delivered orally (Archer 2019; Bushmakin 2014; Constantine 2015; Dayal 2005; Fonseca 2007; Gambacciani 2011; Gast 2009; Hemminki 2009; Hudita 2003; Laan 2001; Liberate 2011; Maki 2007; Mameri Filho 2005; Modugno 2003; Morais‐Socorro 2012; Osmanagaoglu 2006; SMART‐3; Strickler 2000; Veerus 2006; Yang 2004), however, some were administered transdermally (Czarnecka 2000; Haines 2009; Huang 2008; Nathorst‐Böös 1993; Simon 2007; Wiklund 1993), vaginally (Bumphenkiatikul 2020; Caruso 2020; Diem 2018; Gast 2009; Mitchell 2018; Seyyedi 2016; Speroff 2003), orally and transdermally in separate groups (Taylor 2017), and nasally (Nielsen 2006).
Outcomes
Studies used the following tools for assessing sexual function:
Arizona Sexual Experiences (ASEX) scale (McGahuey 2000 (SMART‐3))
Menopause‐specific Quality of Life (MENQOL; Hilditch 1996 (Bushmakin 2014; Diem 2018; Haines 2009; Seyyedi 2016; SMART‐3))
Golombok‐Rust Inventory of Sexual Satisfaction (GRISS; Rust 1986 (Fonseca 2007))
McCoy Female Sexuality Questionnaire (MFSQ; McCoy 2000 (Gast 2009))
Greene Climacteric Scale (GCS; Greene 2008 (Laan 2001; Maki 2007; Morais‐Socorro 2012; Speroff 2003; Yang 2004))
McCoy Sex Scale Questionnaire (MSQ; McCoy 1985 (Hudita 2003; Mameri Filho 2005; Modugno 2003; Nathorst‐Böös 1993; Wiklund 1993))
Brief Index of Sexual Functioning‐Women (BISF‐W; Taylor 1994 (Gast 2009))
Medical Outcomes Study (MOS; McHorney 1994 (Huang 2008))
Modified Mini‐Mental State Examination (3MS; Teng 1987 (SMART‐3; WHI 1999))
Female Sexual Function Index (FSFI; Rosen 2000 (Archer 2019; Bumphenkiatikul 2020; Caruso 2020; Constantine 2015; Mitchell 2018; Osmanagaoglu 2006; Taylor 2017))
Subjective Symptoms Assessment Profile (SSA‐P; Dimenäs 1990 (Czarnecka 2000))
Utian Quality of Life Women's Health Questionnaire (WHQ; Hunter 2000 (Dayal 2005; Gambacciani 2011; Hemminki 2009; Liberate 2011; Mameri Filho 2005; Nathorst‐Böös 1993; Nielsen 2006; Simon 2007; Strickler 2000; Veerus 2006; WISDOM 2008))
See the Characteristics of included studies for details.
Where studies reported composite scores, they evaluated the following domains.
All domains studied ‐ desire, arousal, lubrication, orgasm, satisfaction, and pain (Archer 2019; Constantine 2015; Mitchell 2018; Osmanagaoglu 2006; Taylor 2017)
Arousal and orgasm (Czarnecka 2000; SMART‐3)
Arousal and pain (Haines 2009; Liberate 2011; Nielsen 2006; Strickler 2000; WISDOM 2008)
Of the 16 studies included in the qualitative analysis, 20 studies presented complete data for all outcomes (Archer 2019; Bushmakin 2014; Bumphenkiatikul 2020; Caruso 2020; Constantine 2015; Dayal 2005; Diem 2018; Haines 2009; Laan 2001; Liberate 2011; Maki 2007; Mitchell 2018; Morais‐Socorro 2012; Nathorst‐Böös 1993; Osmanagaoglu 2006; Seyyedi 2016; SMART‐3; Speroff 2003; Wiklund 1993; Yang 2004). From three studies we could only include the final scores (Bumphenkiatikul 2020; Laan 2001; Morais‐Socorro 2012). We used the calculator in Review Manager 2020 to estimate missing SDs for seven studies (Bushmakin 2014; Caruso 2020; Liberate 2011; Maki 2007; Nathorst‐Böös 1993; SMART‐3; Speroff 2003).
Excluded studies
We excluded 59 studies at this update. Of these:
36 studies did not evaluate sexual function (2010‐024603‐26; 2014‐000179‐18; Abraham 2014; Archer 2011; Bosak 2022; Bride 2014; Cano 2012; Daneshmand 2015; Fabian 2019; Galesanu 2010; Garcia de Arriba 2022; Gaspard 2021; Griesser 2012; Harman 2014; IRCT138809032766N1; ISRCTN46661996; Kagan 2014; Kingsberg 2017; Kroll 2018; L'Hermite 2022; Liu 2012; Lobo 2017; NCT01585558; NCT01779947; NCT02253173; NCT02638337; Noguchi 2018; Paraiso 2020; Portman 2013; Portman 2014a; Pradeep 2016; Santofimia 2022; Silverman 2012; Simon 2012; Sun 2016; Tansupswatdikul 2012);
six studies were not randomized or were pseudo‐randomized (Bennink 2016; Islam 2021; Ju 2021; NCT01822288; NCT03018106; Tungmunsakulchai 2015);
three studies compared sexual function with another intervention (Cruz 2018; Fernandes 2014; Bianchi‐Ferraro 2022);
four studies did not evaluate sexual function by a validated questionnaire (Aptecar 2021; Bachmann 2011; Mittal 2020; Saeideh 2010);
eight studies did not use hormone therapy (Abedi 2018; Abedi 2020; Arêas 2019; Dalil 2020; RBR‐94dx93/1; Raz 2014; Serebani 2020; Yeo 2020);
one study did not have a control group (Eftekhar 2020);
one study's patient population was ineligible (Marschalek 2022).
Studies awaiting classification
Seven studies (Hirschberg 2020; NCT01845649; NCT02460302; NCT02834312; NCT03363997; Pinkerton 2017; Tanmahasamut 2020 ) are awaiting classification because we suspect that they evaluated the effect of hormone therapy on sexual function, but we have not yet obtained these data, and we are awaiting information from the authors.
Ongoing studies
Four studies were still at the protocol stage and had not yet reported results on the effect of hormone therapy on sexual function (NCT02668796; NCT02670785; NCT02859285; NCT03116022).
Risk of bias in included studies
We deemed 20 of 36 studies included in this review to have a high risk of bias in at least one domain. We considered 14 of 36 studies not to be at high risk of bias in any domain but to have an unclear risk of bias in at least one domain. We considered two of 36 studies to have a low risk of bias over all domains. See Figure 2 and Figure 3 for the graph and summary of the review authors' judgements about the risk of bias for included studies. The risk of bias and imprecision of evidence for many comparisons were reasons for downgrading evidence quality. Many included studies were supported by the pharmaceutical industry, in most cases the manufacturer of the studied drug (see Characteristics of included studies).
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Sequence generation
We judged 14 studies to have unclear risk of selection bias as they did not describe the method of randomization (Caruso 2020; Constantine 2015; Czarnecka 2000; Fonseca 2007; Gast 2009; Haines 2009; Hudita 2003; Laan 2001; Modugno 2003; Morais‐Socorro 2012; Nathorst‐Böös 1993; Osmanagaoglu 2006; Wiklund 1993; Yang 2004). The other 22 studies reported adequate methods of randomization, and we deemed them to be at low risk of bias (Archer 2019; Bumphenkiatikul 2020; Bushmakin 2014; Dayal 2005; Diem 2018; Gambacciani 2011; Hemminki 2009; Huang 2008; Liberate 2011; Maki 2007; Mameri Filho 2005; Mitchell 2018; Nielsen 2006; Seyyedi 2016; Simon 2007; SMART‐3; Speroff 2003; Strickler 2000; Taylor 2017; Veerus 2006; WHI 1999; WISDOM 2008).
Allocation concealment
Twenty‐seven studies did not report the method used for allocation concealment, and thus we considered them to be at unclear risk of selection bias (Archer 2019; Bushmakin 2014; Caruso 2020; Constantine 2015; Czarnecka 2000; Dayal 2005; Fonseca 2007; Gambacciani 2011; Gast 2009; Haines 2009; Hudita 2003; Laan 2001; Liberate 2011; Maki 2007; Mameri Filho 2005; Mitchell 2018; Modugno 2003; Morais‐Socorro 2012; Nathorst‐Böös 1993; Osmanagaoglu 2006; Simon 2007; SMART‐3; Speroff 2003; Strickler 2000; WHI 1999; Wiklund 1993; Yang 2004). The other nine studies reported adequate allocation concealment methods, and we deemed them to be at low risk of selection bias (Bumphenkiatikul 2020; Diem 2018; Hemminki 2009; Huang 2008; Nielsen 2006; Seyyedi 2016; Taylor 2017; Veerus 2006; WISDOM 2008).
Blinding
Blinding of participants and personnel
Three studies did not blind the participants or the personnel administering the intervention, and we considered them to be at high risk of performance bias (Czarnecka 2000; Osmanagaoglu 2006; Veerus 2006). Six studies did not describe how they blinded participants, and we considered them to be at unclear risk of performance bias (Caruso 2020; Constantine 2015; Gambacciani 2011; Laan 2001; Modugno 2003; Nathorst‐Böös 1993), whilst we deemed 27 studies to be at low risk of performance bias (Archer 2019; Bumphenkiatikul 2020; Bushmakin 2014; Dayal 2005; Diem 2018; Fonseca 2007; Gast 2009; Haines 2009; Hemminki 2009; Huang 2008; Hudita 2003; Liberate 2011; Maki 2007; Mameri Filho 2005; Mitchell 2018; Morais‐Socorro 2012; Nielsen 2006; Seyyedi 2016; Simon 2007; SMART‐3; Speroff 2003; Strickler 2000; Taylor 2017; WHI 1999; Wiklund 1993; WISDOM 2008; Yang 2004).
Blinding of outcome assessment
Seven studies described attempts to blind the outcome assessment, and we deemed them to be at low risk of detection bias (Bumphenkiatikul 2020; Liberate 2011; Mitchell 2018; Simon 2007; Taylor 2017; Wiklund 1993; WISDOM 2008), whilst we considered 29 studies to be at unclear risk of detection bias (Archer 2019; Bushmakin 2014; Caruso 2020; Constantine 2015; Czarnecka 2000; Dayal 2005; Diem 2018; Fonseca 2007; Gambacciani 2011; Gast 2009; Haines 2009; Hemminki 2009; Huang 2008; Hudita 2003; Laan 2001; Maki 2007; Mameri Filho 2005; Modugno 2003; Morais‐Socorro 2012; Nathorst‐Böös 1993; Nielsen 2006; Osmanagaoglu 2006; Seyyedi 2016; SMART‐3; Speroff 2003; Strickler 2000; Veerus 2006; WHI 1999; Yang 2004).
Incomplete outcome data
Ten studies reported an important or unbalanced loss of participants, and we deemed them to be at high risk of attrition bias (Constantine 2015; Haines 2009; Huang 2008; Laan 2001; Liberate 2011; Modugno 2003; Nielsen 2006; Simon 2007; WHI 1999; WISDOM 2008). In six studies, losses to follow‐up were high or not clear, and we deemed them to be at unclear risk of bias (Bushmakin 2014; Gambacciani 2011; Hudita 2003; Nathorst‐Böös 1993; SMART‐3; Yang 2004); and in 19 studies, there was no suspicion of incomplete data, and we considered them to be at low risk of bias (Archer 2019; Bumphenkiatikul 2020; Caruso 2020; Czarnecka 2000; Dayal 2005; Diem 2018; Fonseca 2007; Gast 2009; Hemminki 2009; Maki 2007; Mameri Filho 2005; Mitchell 2018; Morais‐Socorro 2012; Osmanagaoglu 2006; Seyyedi 2016; Speroff 2003; Strickler 2000; Taylor 2017; Veerus 2006; Wiklund 1993).
Selective reporting
Six studies applied a validated questionnaire to evaluate the sexual function (Caruso 2020; Constantine 2015; Fonseca 2007; Gambacciani 2011; Gast 2009; Hudita 2003), but one study did not provide the protocol and showed selective reporting and other bias (possible biases in randomization or blinding; Caruso 2020), one did not provide baseline domain scores or demographic data after losses, and losses were unbalanced in the groups (Constantine 2015); one provided only results for significant differences (Fonseca 2007), and three did not provide numeric results (Gambacciani 2011; Gast 2009; Hudita 2003). One study assessed sexuality, sexual thoughts/interest, or quality of sexual life, not sexual function, by validated questionnaires, but provided only partial results (total score and some domains) of one questionnaire, which do not represent sexual function itself (Maki 2007). Thus, we deemed all seven of these studies to be at high risk of reporting bias. One study was at unclear risk (Seyyedi 2016), while the remaining 28 were considered at low risk (Archer 2019; Bumphenkiatikul 2020; Bushmakin 2014; Czarnecka 2000; Dayal 2005; Diem 2018; Haines 2009; Hemminki 2009; Huang 2008; Laan 2001; Liberate 2011; Mameri Filho 2005; Mitchell 2018; Modugno 2003; Morais‐Socorro 2012; Nathorst‐Böös 1993; Nielsen 2006; Osmanagaoglu 2006; Simon 2007; SMART‐3; Speroff 2003; Strickler 2000; Taylor 2017; Veerus 2006; WHI 1999; Wiklund 1993; WISDOM 2008; Yang 2004).
Other potential sources of bias
We considered four studies to be at high risk of bias because they had unbalanced groups at baseline and we could use only final scores in the meta‐analysis, or due to lack of detailed information about randomization of the participants (Caruso 2020; Czarnecka 2000; Dayal 2005; Osmanagaoglu 2006). We considered four studies to be at unclear risk of bias due to problems in the study design, or absence of a declaration of conflicts of interest, or lack of sample size (Constantine 2015; Maki 2007; Wiklund 1993; Yang 2004). We considered the other 28 studies to be at low risk of other bias (Archer 2019; Bumphenkiatikul 2020; Bushmakin 2014; Diem 2018; Fonseca 2007; Gambacciani 2011; Gast 2009; Haines 2009; Hemminki 2009; Huang 2008; Hudita 2003; Laan 2001; Liberate 2011; Mameri Filho 2005; Mitchell 2018; Modugno 2003; Morais‐Socorro 2012; Nathorst‐Böös 1993; Nielsen 2006; Seyyedi 2016; Simon 2007; SMART‐3; Speroff 2003; Strickler 2000; Taylor 2017; Veerus 2006; WHI 1999; WISDOM 2008).
Effects of interventions
See Table 1 for the main comparison, hormone therapy compared with placebo or no intervention for sexual function in symptomatic or early postmenopausal women; see Table 2 for hormone therapy compared with placebo or no intervention for sexual function in unselected postmenopausal women.
Qualitative analysis
We did not include 16 studies in the meta‐analysis (Czarnecka 2000; Fonseca 2007; Gambacciani 2011; Gast 2009; Hemminki 2009; Huang 2008; Hudita 2003; Mameri Filho 2005; Modugno 2003; Nielsen 2006; Simon 2007; Strickler 2000; Taylor 2017; Veerus 2006; WHI 1999; WISDOM 2008).
Six of 16 studies administered estrogen alone versus placebo (Huang 2008; Mameri Filho 2005; Nielsen 2006; Simon 2007; Taylor 2017; WHI 1999). Of these:
Huang 2008 administered 0.014 mg of estrogen per day via transdermal patch for 24 months and reported no significant difference in sexual function when comparing the effect of the intervention with placebo in unselected postmenopausal women;
Mameri Filho 2005 administered 0.625 mg of conjugated equine estrogen per day, orally, for six months and reported no significant difference in sexual function when comparing the effect of the intervention with placebo in unselected postmenopausal women;
Nielsen 2006 administered 150 mcg or 300 mcg of estrogen daily for six months, intranasally, and reported a slight improvement in sexual function when comparing the effect of the intervention with placebo in symptomatic or early postmenopausal women;
Simon 2007 administered 0.87 g or 1.7 g or 2.6 g of estrogen per day for 12 months, by transdermal gel and reported a significant improvement in sexual function when comparing the effect of the intervention with placebo in postmenopausal women;
Taylor 2017 administered oral estrogen 0.45 mg per day, orally, for 36 months and reported a significant improvement in sexual function when comparing the effect of the intervention with placebo in postmenopausal women;
WHI 1999 administered 0.625 mg of conjugated equine estrogen per day for 12 months, orally, and reported no significant difference in effect in the domain of sexual satisfaction when comparing the intervention with placebo in postmenopausal women.
Eight of 16 studies administered estrogen in combination with progesterone (Czarnecka 2000; Fonseca 2007; Gambacciani 2011; Gast 2009; Hemminki 2009; Veerus 2006; WHI 1999; WISDOM 2008). Of these:
Gast 2009 administered conjugated estrogen 0.45 mg + 1.5 mg medroxyprogesterone acetate daily for six 28‐day cycles intravaginally and reported a significant improvement in sexual function in postmenopausal women;
-
Czarnecka 2000 and Fonseca 2007 administered for three and six months, respectively, 17β‐estradiol 2 mg in combination with 1 mg of norethisterone acetate daily in postmenopausal women.
Czarnecka 2000 reported no significant differences between women who received the intervention and controls;
Fonseca 2007 reported an improvement in sexual function, specifically, in the decrease in dyspareunia and increase in sexual satisfaction;
Hemminki 2009 administered oral conjugated equine estrogen 0.625 mg + medroxyprogesterone acetate 5.0 daily with assessment at 12 months, and reported no significant difference in effect on sexual functioning when compared with placebo in postmenopausal women;
Gambacciani 2011, on the other hand, administered 1 mg of estradiol in combination with 2 mg drospirenone orally for three months and did not report significant differences in sexual function in symptomatic or early postmenopausal women;
Veerus 2006 administered oral conjugated equine estrogen 0.625 mg + medroxyprogesterone acetate 5.0 daily with assessment at 12 months, and reported no significant difference in effect on sexual functioning when compared with placebo in postmenopausal women, according to the final data reported in the study protocol.
-
WHI 1999 and WISDOM 2008 administered 0.625 mg of conjugated equine estrogen in combination with 2.5 or 0.625 mg of medroxyprogesterone acetate (MPA) per day orally, for more than three years
WHI 1999 reported a significant improvement in sexual function;
WISDOM 2008, however, reported no significant differences in sexual function in postmenopausal women.
Two of 16 studies administered SERMs (Strickler 2000; Modugno 2003). Strickler 2000 administered 60 mg or 150 mg of raloxifene for six months, and Modugno 2003 administered 60 mg or 120 mg of raloxifene per day orally for 36 months. Both studies found no significant difference in sexual function in postmenopausal women.
Finally, a further study on tibolone (1.25 or 2.5 mg/day orally for 24 weeks) did not report data in a form that could be used in meta‐analysis but reported significant improvement in sexual function in postmenopausal women (Hudita 2003).
Regarding the quality of these 16 studies, two had no suspected risk of bias (Hemminki 2009; Taylor 2017), while 14 had suspected risk of bias mainly associated with incomplete data (Huang 2008; Modugno 2003; Mameri Filho 2005Nielsen 2006; Simon 2007; Strickler 2000; WHI 1999; WISDOM 2008), blinding of participants and staff (Czarnecka 2000; Veerus 2006), and selective reporting (Fonseca 2007; Gambacciani 2011; Gast 2009; Hudita 2003). See Figure 3.
Quantitative analysis
1. Estrogen alone versus placebo or no intervention
Primary outcome
1.1 Sexual function composite score
In the subgroup of symptomatic or early postmenopausal women, estrogen alone versus placebo or no intervention probably slightly improves the sexual function composite score (SMD 0.50, 95% CI 0.04 to 0.96; I² = 88%; 3 studies, 699 women; moderate‐quality evidence; Analysis 1.1; Figure 4). This means that the sexual function composite score is compatible with a moderate effect of 0.50 standard units with the use of estrogen alone versus placebo or no intervention. The sensitivity analysis (restricting eligibility criteria only to studies judged not be at high risk of bias) was compatible with a moderate effect (SMD 0.68, 95% CI 0.20 to 1.16; I² = 86%; 2 studies, 548 women; moderate‐quality evidence) of estrogen alone versus placebo or no intervention in this subgroup of women. Investigation of additional sources of bias suggests that the high heterogeneity observed in this subgroup (I² = 88%) could be due to:
1.1. Analysis.

Comparison 1: Estrogen alone versus placebo/no treatment, Outcome 1: Sexual function composite score
4.

Forest plot of comparison: 1 Estrogens alone versus placebo/no treatment, outcome: 1.1 Sexual function composite score.
clinical heterogeneity related to variability in the intervention (Haines 2009, estradiol 0.014 mg, transdermal route; Speroff 2003, estradiol 50 ug/day and 100 ug/day or placebo, vaginal route; Wiklund 1993, estradiol 50 ug twice a week or placebo, transdermal route);
methodological heterogeneity related to variability in the measurement tool (Haines 2009, MENQoL; Speroff 2003, Greene Climacteric Scale sub‐score; Wiklund 1993, McCoy sex scale total score), and high risk of bias in one of three studies; and
statistical heterogeneity related to the variability of effect (Haines 2009, SMD 0.12, 95% CI −0.20 to 0.44; Speroff 2003, SMD 0.92, 95% CI 0.68 to 1.17; Wiklund 1993, SMD 0.43, 95% CI 0.17 to 0.70).
In the subgroup of unselected postmenopausal women, estrogen alone versus placebo or no intervention probably makes little or no difference to the sexual function composite score (SMD 0.64, 95% CI −0.12 to 1.41; I² = 94%; 6 studies, 608 women; moderate‐quality evidence; Analysis 1.1; Figure 4). This means that the sexual function composite score is compatible with a moderate effect of 0.64 standard units with the use of estrogen alone versus placebo or no intervention. The sensitivity analysis (restricting eligibility criteria only to studies judged not be at high risk of bias) was compatible with a small effect (SMD 0.35, 95% CI 0.02 to 0.68; I² = 63%; 4 studies, 434 women) of estrogen alone versus placebo or no intervention in this subgroup of women. Investigation of additional sources of bias suggests that the high heterogeneity observed in this subgroup (I² = 94%) could be due to:
clinical heterogeneity related to variability in the intervention (Bumphenkiatikul 2020, conjugated estrogen 0.625 mg, daily for 3 weeks then twice‐weekly for 9 weeks or placebo, vaginal route; Caruso 2020, estradiol ovule 0.03 mg/day or placebo, vaginal route; Dayal 2005, equine estrogen 0.625 mg/day or placebo, oral route; Diem 2018, estradiol 10 mg tablet/day or placebo, vaginal route; Mitchell 2018, estradiol 10.3 ug/day or placebo, vaginal route; and Seyyedi 2016, estradiol 0.625 mg/day or placebo, vaginal route);
methodological heterogeneity related to variability in the measurement tool (Bumphenkiatikul 2020, Female Sexual Function Index; Caruso 2020, Female Sexual Function Index; Dayal 2005, health‐related quality of life; Diem 2018, MENQoL; Mitchell 2018, Female Sexual Function Index; Seyyedi 2016, MENQoL), and high risk of bias in two of six studies; and
statistical heterogeneity related to global variability of effect.
Considering the pooled analysis, estrogen alone versus placebo or no intervention probably slightly improves the sexual function composite score (SMD 0.60, 95% CI 0.16 to 1.04; I² = 92%; 9 studies, 1307 women; moderate‐quality evidence; Analysis 1.1; Figure 4). This means that the sexual function composite score is compatible with a moderate effect of 0.60 standard units with the use of estrogen alone. The sensitivity analysis (restricting eligibility criteria only to studies judged not be at high risk of bias) was compatible with a moderate effect (SMD 0.48, 95% CI 0.18 to 0.79; I² = 80%; 6 studies, 982 women) of estrogen alone versus placebo or no intervention in this subgroup of women. The investigation of additional sources of bias for the high heterogeneity observed in the pooled analysis (I² = 94%), is related to the sources of clinical, methodological, and statistical heterogeneity explored in the two previous subgroups (symptomatic or early postmenopausal women and unselected postmenopausal women).
Secondary outcomes
1.2 Desire
No study reported results for the subgroup of symptomatic or early postmenopausal women.
In unselected postmenopausal women, we are uncertain of the effect of estrogen alone versus placebo or no intervention in desire score (MD 0.33, 95% CI −0.27 to 0.93; I² = 77%; 3 studies, 416 women; low‐quality evidence; Analysis 1.2). This is compatible with a small effect of 0.06 standard units with the use of estrogen alone. Investigation of additional sources of bias suggests that the high heterogeneity observed in this subgroup (I² = 77%) could be due to:
1.2. Analysis.

Comparison 1: Estrogen alone versus placebo/no treatment, Outcome 2: Desire
clinical heterogeneity related to variability in the intervention (Bumphenkiatikul 2020, conjugated estrogen 0.625 mg, daily for 3 weeks then twice‐weekly for 9 weeks or placebo, vaginal route; Caruso 2020, estradiol ovule 0.03 mg/day or placebo, vaginal route; Mitchell 2018, estradiol 10.3 ug /day or placebo, vaginal route);
methodological heterogeneity related to high risk of bias in one of three studies; and
statistical heterogeneity related to the variability of effect (Bumphenkiatikul 2020, MD 0.22, 95% CI −1.39 to 1.83; Caruso 2020, MD 0.71, 95% CI 0.33 to 1.08; Mitchell 2018, MD 0.00, 95% CI −0.29 to 0.29).
1.3 Arousal
In symptomatic or early postmenopausal women, we are uncertain of the effect of estrogen alone versus placebo or no intervention on arousal (SMD 0.14, 95% CI −0.12 to 0.39; 1 study, 239 women; low‐quality evidence; Analysis 1.3). This is compatible with a small effect of 0.14 standard units with the use of estrogen alone.
1.3. Analysis.

Comparison 1: Estrogen alone versus placebo/no treatment, Outcome 3: Arousal
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of estrogen alone versus placebo or no intervention on arousal (SMD 0.14, 95% CI −0.29 to 0.58; I² = 77%; 3 studies, 384 women; low‐quality evidence; Analysis 1.3). This is compatible with a small effect of 0.14 standard units with the use of estrogen alone. Investigation of additional sources of bias suggests that the high heterogeneity observed in this subgroup (I² = 77%) could be related to:
clinical heterogeneity related to variability in the intervention (Bumphenkiatikul 2020, conjugated estrogen 0.625 mg, daily for 3 weeks then twice‐weekly for 9 weeks or placebo, vaginal route; Caruso 2020, estradiol ovule 0.03 mg/day or placebo, vaginal route; Mitchell 2018, estradiol 10.3 ug /day or placebo, vaginal route);
methodological heterogeneity related to high risk of bias in one of three studies; and
statistical heterogeneity related to variability of effect (Bumphenkiatikul 2020, SMD 0.22, 95% CI −0.26 to 0.70; Caruso 2020, SMD 0.44, 95% CI 0.13 to 0.75; Mitchell 2018, SMD −0.22, 95% CI −0.54 to 0.10).
Considering the pooled analysis, we are uncertain of the effect of estrogen alone versus placebo or no intervention (SMD 0.14, 95% CI −0.14 to 0.42; I² = 65%; 4 studies, 623 women; low‐quality evidence; Analysis 1.3). This is compatible with a small effect of 0.14 standard units with the use of estrogen alone. The investigation of additional sources of bias for the high heterogeneity observed in the pooled analysis (I² = 65%), is related to the sources of clinical, and statistical heterogeneity explored in the subgroup of unselected postmenopausal women.
1.4 Lubrication
In the subgroup of symptomatic or early postmenopausal women, estrogen alone versus placebo or no intervention may slightly improve lubrication (SMD 0.47, 95% CI 0.21 to 0.73; 1 study, 239 women; low‐quality evidence; Analysis 1.4). This is compatible with a moderate effect of 0.47 standard units with the use of estrogen alone.
1.4. Analysis.

Comparison 1: Estrogen alone versus placebo/no treatment, Outcome 4: Lubrication
In the subgroup of unselected postmenopausal women, estrogen alone versus placebo or no intervention probably slightly improves lubrication (SMD 0.47, 95% CI −0.09 to 1.02; I² = 85%; 3 studies, 380 women; moderate‐quality evidence; Analysis 1.4). This is compatible with a moderate effect of 0.47 standard units with the use of estrogen alone. Investigation of additional sources of bias suggests that the high heterogeneity observed in this subgroup (I² = 85%) could be due to:
clinical heterogeneity related to variability in the intervention (Bumphenkiatikul 2020, conjugated estrogen 0.625 mg daily for 3 weeks then twice‐weekly for 9 weeks or placebo, vaginal route; Caruso 2020, estradiol ovule 0.03 mg/day or placebo, vaginal route; Mitchell 2018, estradiol 10.3 ug /day or placebo, vaginal route);
methodological heterogeneity related to high risk of bias in one of three studies; and
statistical heterogeneity related to variability of effect (Bumphenkiatikul 2020, SMD 0.31, 95% CI −0.18 to 0.79; Caruso 2020, SMD 0.96, 95% CI 0.63 to 1.28; Mitchell 2018, SMD 0.12, 95% CI −0.20 to 0.44).
Considering the pooled analysis, estrogen alone versus placebo or no intervention probably slightly improves lubrication (SMD 0.47, 95% CI 0.12 to 0.83; I² = 78%; 4 studies, 619 women; moderate‐quality evidence; Analysis 1.4). This is compatible with a small effect of 0.47 standard units with the use of estrogen alone. The investigation of additional sources of bias suggests that the high heterogeneity observed in the pooled analysis (I² = 78%) is related to the sources of clinical, and statistical heterogeneity explored in the subgroup of unselected postmenopausal women.
1.5 Orgasm
No study reported results for the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of estrogen alone versus placebo or no intervention for orgasm (MD 0.14, 95% CI −0.72 to 0.99; I² = 90%; 3 studies, 383 women; low‐quality evidence; Analysis 1.5). This is compatible with a small effect of 0.14 standard units with the use of estrogen alone. Investigation of additional sources of bias suggests that the high heterogeneity observed in this subgroup (I² = 90%) could be due to:
1.5. Analysis.

Comparison 1: Estrogen alone versus placebo/no treatment, Outcome 5: Orgasm
clinical heterogeneity related to variability in the intervention (Bumphenkiatikul 2020, conjugated estrogen 0.625 mg, daily for 3 weeks then twice‐weekly for 9 weeks or placebo, vaginal route; Caruso 2020, estradiol ovule 0.03 mg/day or placebo, vaginal route; Mitchell 2018, estradiol 10.3 ug /day or placebo, vaginal route);
methodological heterogeneity related to high risk of bias in one of three studies; and
statistical heterogeneity related to the variability of effect (Bumphenkiatikul 2020, MD 0.36, 95% CI −0.93 to 0.21; Caruso 2020, MD 0.92, 95% CI 0.54 to 1.30; Mitchell 2018, MD −0.20, 95% CI −0.69 to 0.29).
1.6 Satisfaction
In the subgroup of symptomatic or early postmenopausal women, estrogen alone versus placebo or no intervention may slightly improve satisfaction (SMD 0.29, 95% CI 0.08 to 0.51; I² = 24%; 2 studies, 446 women; moderate‐quality evidence; Analysis 1.6). This is compatible with a small effect of 0.29 standard units with the use of estrogen alone.
1.6. Analysis.

Comparison 1: Estrogen alone versus placebo/no treatment, Outcome 6: Satisfaction
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of estrogen alone versus placebo or no intervention on satisfaction (SMD 0.48, 95% CI −0.21 to 1.16; I² = 90%; 3 studies, 378 women; low‐quality evidence; Analysis 1.6). This is compatible with a moderate effect of 0.48 standard units with the use of estrogen alone. Investigation of additional sources of bias suggests that the high heterogeneity observed in this subgroup (I² = 90%) could be due to:
clinical heterogeneity related to variability in the intervention (Bumphenkiatikul 2020, conjugated estrogen 0.625 mg, daily for 3 weeks then twice‐weekly for 9 weeks or placebo, vaginal route; Caruso 2020, estradiol ovule 0.03 mg/day or placebo, vaginal route; Mitchell 2018, estradiol 10.3 ug /day or placebo, vaginal route);
methodological heterogeneity related to high risk of bias in one of three studies; and
statistical heterogeneity related to the variability of effect (Bumphenkiatikul 2020, SMD −0.06, 95% CI −0.54 to 0.42; Caruso 2020, SMD 1.14, 95% CI 0.81 to 1.47; Mitchell 2018, SMD 0.31, 95% CI −0.02 to 0.63).
Considering the pooled analysis, estrogen alone versus placebo or no intervention probably slightly improves satisfaction (SMD 0.41, 95% CI 0.04 to 0.77; I² = 84%; 5 studies, 824 women; moderate‐quality evidence; Analysis 1.6). This is compatible with a small effect of 0.41 standard units with the use of estrogen alone. The investigation of additional sources of bias for the high heterogeneity observed in the pooled analysis (I² = 84%), is related to the sources of clinical, and statistical heterogeneity explored in the subgroup of unselected postmenopausal women.
1.7 Pain
In the subgroup of symptomatic or early postmenopausal women, estrogen alone versus placebo or no intervention probably slightly improves pain (SMD 0.35, 95% CI 0.14 to 0.56; I² = 29%; 2 studies, 548 women; moderate‐quality evidence; Analysis 1.7). This is compatible with a small effect of 0.35 standard units with the use of estrogen alone.
1.7. Analysis.

Comparison 1: Estrogen alone versus placebo/no treatment, Outcome 7: Pain
In the subgroup of unselected postmenopausal women, estrogen alone versus placebo or no intervention may improve pain (SMD 0.72, 95% CI −0.09 to 1.52; I² = 93%; 3 studies, 410 women; low‐quality evidence; Analysis 1.7). This is compatible with a large effect of 0.72 standard units with the use of estrogen alone. Investigation of additional sources of bias suggests that the high heterogeneity observed in this subgroup (I² = 93%) could be due to:
clinical heterogeneity related to variability in the intervention (Bumphenkiatikul 2020, conjugated estrogen 0.625 mg, daily for 3 weeks then twice‐weekly for 9 weeks or placebo, vaginal route; Caruso 2020, estradiol ovule 0.03 mg/day or placebo, vaginal route; Mitchell 2018, estradiol 10.3 ug /day or placebo, vaginal route);
methodological heterogeneity related to high risk of bias in one of three studies; and
statistical heterogeneity related to variability of effect (Bumphenkiatikul 2020, SMD 0.46, 95% CI −0.02 to 0.95; Caruso 2020, SMD 1.44, 95% CI 1.12 to 1.77; Mitchell 2018, SMD 0.23 95% CI −0.08 to 0.54).
Considering the pooled analysis, estrogen alone versus placebo or no intervention may slightly improve pain (SMD 0.57, 95% CI 0.14 to 1.0; I² = 90%; 5 studies, 958 women; low‐quality evidence; Analysis 1.7). This is compatible with a moderate effect of 0.57 standard units with the use of estrogen alone. The investigation of additional sources of bias for the high heterogeneity observed in the pooled analysis (I² = 90%), is related to the sources of clinical, and statistical heterogeneity explored in the subgroup of unselected postmenopausal women.
2. Estrogen combined with progestogens versus placebo or no intervention
Primary outcome
2.1 Sexual function composite score
No study reported results for the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of estrogen combined with progestogens versus placebo or no intervention on the sexual function composite score (MD 0.08 95% CI −1.52 to 1.68; 1 study, 104 women; very low‐quality evidence; Analysis 2.1; Figure 5). This means that sexual function is compatible with a small effect of 0.08 standard units with the use of estrogen combined with progestogens. Due to the limited studies available, it was not possible to perform sensitivity analyses.
2.1. Analysis.

Comparison 2: Estrogen + progestogens versus placebo/no treatment, Outcome 1: Sexual function composite score
5.

Forest plot of comparison: 2 Estrogens + progestogens versus placebo/no treatment, outcome: 2.1 Sexual function composite score.
Secondary outcomes
2.2 Desire at 16‐month follow‐up
No study reported results for the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of estrogen combined with progestogens versus placebo or no intervention on desire (MD 0.70, 95% CI 0.21 to 1.19, 1 study, 158 women, very low‐quality evidence; Analysis 2.2). This is compatible with a moderate effect of 0.70 standard units with the use of estrogen combined with progestogens.
2.2. Analysis.

Comparison 2: Estrogen + progestogens versus placebo/no treatment, Outcome 2: Desire at 16‐month follow‐up
2.3 Desire at 22‐ and 24‐month follow‐up
No study reported results for the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of estrogen combined with progestogens versus placebo or no intervention on desire (SMD 0.19, 95% CI −0.12 to 0.51; I² = 0%; 2 studies, 155 women; low‐quality evidence; Analysis 2.3). This is compatible with a small effect of 0.19 standard units with the use of estrogen combined with progestogens.
2.3. Analysis.

Comparison 2: Estrogen + progestogens versus placebo/no treatment, Outcome 3: Desire at 22‐ and 24‐month follow‐up
2.4 Arousal
No study reported results for the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of estrogen combined with progestogens versus placebo or no intervention on arousal (MD 0.32, 95% CI −0.11 to 0.75; 1 study, 104 women; very low‐quality evidence; Analysis 2.4). This is compatible with a small effect of 0.32 standard units with the use of estrogen combined with progestogens.
2.4. Analysis.

Comparison 2: Estrogen + progestogens versus placebo/no treatment, Outcome 4: Arousal
2.5 Lubrication
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, estrogen combined with progestogens versus placebo or no intervention may slightly improve lubrication (MD 0.45, 95% CI 0.13 to 0.77; 1 study, 104 women; low‐quality evidence; Analysis 2.5). This is compatible with a moderate effect of 0.45 standard units with the use of estrogen combined with progestogens.
2.5. Analysis.

Comparison 2: Estrogen + progestogens versus placebo/no treatment, Outcome 5: Lubrication
2.6 Orgasm
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of estrogen combined with progestogens versus placebo or no intervention on orgasm (MD 0.04, 95% CI −0.53 to 0.61; 1 study, 104 women; very low‐quality evidence; Analysis 2.6). This is compatible with a small effect of 0.04 standard units with the use of estrogen combined with progestogens.
2.6. Analysis.

Comparison 2: Estrogen + progestogens versus placebo/no treatment, Outcome 6: Orgasm
2.7 Satisfaction
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of estrogen combined with progestogens versus placebo or no intervention on satisfaction (MD 0.13, 95% CI −0.28 to 0.54; 1 study, 104 women; very low‐quality evidence; Analysis 2.7). This is compatible with a small effect of 0.13 standard units with the use of estrogen combined with progestogens.
2.7. Analysis.

Comparison 2: Estrogen + progestogens versus placebo/no treatment, Outcome 7: Satisfaction
2.8 Pain
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of estrogen combined with progestogens versus placebo or no intervention on pain (MD 0.93, 95% CI 0.02 to 1.84; 1 study, 104 women; very low‐quality evidence; Analysis 2.8). This is compatible with a large effect of 0.93 standard units with the use of estrogen combined with progestogens.
2.8. Analysis.

Comparison 2: Estrogen + progestogens versus placebo/no treatment, Outcome 8: Pain
3. Synthetic steroids versus placebo or no intervention
Primary outcome
3.1 Sexual function ‐ composite score
In the subgroup of symptomatic or early postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on the sexual function composite score (SMD 1.32, 95% CI 1.18 to 1.47; 1 study, 883 women; very low‐quality evidence; Analysis 3.1; Figure 6). This means that the sexual function composite score is compatible with a large effect of 1.32 standard units with the use of synthetic steroids versus placebo or no intervention. Due to the limited studies available, it was not possible to perform sensitivity analyses.
3.1. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 1: Sexual function composite score
6.

Forest plot of comparison: 3 Synthetic steroids versus placebo/no treatment, outcome: 3.1 Sexual function composite score.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on the sexual function composite score (SMD 0.46, 95% CI 0.07 to 0.86; 1 study, 105 women; very low‐quality evidence; Analysis 3.1; Figure 6). This means that the sexual function composite score is compatible with a small effect of 0.46 standard units with the use of synthetic steroids versus placebo or no intervention. Sensitivity analysis was not possible due to the suspected risk of bias in individual studies.
There was considerable heterogeneity (I² = 94%) when comparing these two subgroups and so pooled analysis was not appropriate (Figure 6). The investigation of additional sources of bias for the high heterogeneity observed in the pooled analysis (I² = 94%), is related to the sources of clinical, and statistical heterogeneity explored in the subgroup of unselected postmenopausal women.
Secondary outcomes
3.2 Desire at 12‐month follow‐up
In the subgroup of symptomatic or early postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on desire (SMD 1.19, 95% CI 0.62 to 1.75; 1 study, 57 women; very low‐quality evidence; Analysis 3.2). This is compatible with a large effect of 1.19 standard units with the use of synthetic steroids.
3.2. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 2: Desire at 12‐month follow‐up
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on desire (SMD 0.19, 95% CI −0.44 to 0.82; 1 study, 39 women; very low‐quality evidence; Analysis 3.2). This is compatible with a small effect of 0.19 standard units with the use of synthetic steroids.
3.3 Desire at 24‐month follow‐up
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on desire (MD 0.35, 95% CI 0.21 to 0.49; 1 study, 105 women; very low‐quality evidence; Analysis 3.3). This is compatible with a moderate effect of 0.35 standard units with the use of synthetic steroids.
3.3. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 3: Desire at 24‐month follow‐up
3.4 Arousal at 12‐month follow‐up
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on arousal (MD 0.19, 95% CI −0.43 to 0.81; 1 study, 39 women; very low‐quality evidence; Analysis 3.4). This is compatible with a small effect of 0.19 standard units with the use of synthetic steroids.
3.4. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 4: Arousal at 12‐month follow‐up
3.5 Arousal at 24‐month follow‐up
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on arousal (MD 0.87, 95% CI 0.47 to 1.27; 1 study, 105 women; very low‐quality evidence; Analysis 3.5). This is compatible with a large effect of 0.87 standard units with the use of synthetic steroids.
3.5. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 5: Arousal at 24‐month follow‐up
3.6 Lubrication at 12‐month follow‐up
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on lubrication (MD 0.56, 95% CI 0.04 to 1.08; 1 study, 39 women; very low‐quality evidence; Analysis 3.6). This is compatible with a moderate effect of 0.56 standard units with the use of synthetic steroids.
3.6. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 6: Lubrication at 12‐month follow‐up
3.7 Lubrication at 24‐month follow‐up
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on lubrication (MD 0.62, 95% CI 0.28 to 0.96; 1 study, 105 women; very low‐quality evidence; Analysis 3.7). This is compatible with a moderate effect of 0.62 standard units with the use of synthetic steroids.
3.7. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 7: Lubrication at 24‐month follow‐up
3.8 Orgasm at 12‐month follow‐up
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on orgasm (MD 0.25, 95% CI −0.98 to 1.48; 1 study, 39 women; very low‐quality evidence; Analysis 3.8). This is compatible with a small effect of 0.25 standard units with the use of synthetic steroids.
3.8. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 8: Orgasm at 12‐month follow‐up
3.9 Orgasm at 24‐month follow‐up
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on orgasm (MD 0.31, 95% CI −0.19 to 0.81; 1 study, 105 women; very low‐quality evidence; Analysis 3.9). This is compatible with a small effect of 0.31 standard units with the use of synthetic steroids.
3.9. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 9: Orgasm at 24‐month follow‐up
3.10 Satisfaction
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on satisfaction (MD 0.51, 95% CI 0.12 to 0.90; 1 study, 105 women; very low‐quality evidence; Analysis 3.10). This is compatible with a moderate effect of 0.51 standard units with the use of synthetic steroids.
3.10. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 10: Satisfaction
3.11 Pain at 12‐month follow‐up
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on pain (MD 0.12, 95% CI −0.18 to 0.42; 1 study, 39 women; very low‐quality evidence; Analysis 3.11). This is compatible with a small effect of 0.12 standard units with the use of synthetic steroids.
3.11. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 11: Pain at 12‐month follow‐up
3.12 Pain at 24‐month follow‐up
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of synthetic steroids versus placebo or no intervention on pain (MD 0.90, 95% CI 0.01 to 1.79; 1 study, 105 women; very low‐quality evidence; Analysis 3.12). This is compatible with a large effect of 0.90 standard units with the use of synthetic steroids.
3.12. Analysis.

Comparison 3: Synthetic steroids versus placebo/no treatment, Outcome 12: Pain at 24‐month follow‐up
4. Comparison of selective estrogen receptor modulators (SERMs) versus placebo or no intervention
Primary outcome
4.1 Sexual function composite score
In the subgroup of symptomatic or early postmenopausal women, we are uncertain of the effect of SERMs versus placebo or no intervention on the sexual function composite score (MD −1.00, 95% CI −2.00 to −0.00; 1 study, 215 women; low‐quality evidence; Analysis 4.1; Figure 7). This means that the sexual function composite score is compatible with a large effect of 1.0 standard unit with the use of SERMs. Due to the limited studies available, it was not possible to perform sensitivity analyses.
4.1. Analysis.

Comparison 4: Selective estrogen receptor modulators (SERMs) versus placebo/no treatment, Outcome 1: Sexual function composite score
7.

Forest plot of comparison: 4 Selective estrogen receptor modulators (SERMs) versus placebo/no treatment, outcome: 4.1 Sexual function composite score.
In the subgroup of unselected postmenopausal women, SERMs versus placebo or no intervention may slightly improve the sexual function composite score (MD 2.24, 95% CI 1.37 to 3.11; 2 studies, 1525 women; low‐quality evidence; Analysis 4.1; Figure 7). This means that the sexual function composite score is compatible with a small effect of 0.25 standard units with the use of SERMs versus placebo or no intervention. Due to the limited studies available, it was not possible to perform sensitivity analysis.
Considerable heterogeneity was observed (I² = 92%) when comparing these two subgroups and so pooled analysis was not appropriate (Figure 7).
Secondary outcomes
4.2 Desire
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, SERMs versus placebo or no intervention probably slightly improve desire (MD 0.25, 95% CI 0.14 to 0.36; I² = 31%; 2 studies, 1545 women; low‐quality evidence; Analysis 4.2). This is compatible with a small effect of 0.25 standard units with the use of SERMs.
4.2. Analysis.

Comparison 4: Selective estrogen receptor modulators (SERMs) versus placebo/no treatment, Outcome 2: Desire
4.3 Arousal
In the subgroup of symptomatic or early postmenopausal women, we are uncertain of the effect of SERMs versus placebo or no intervention on arousal (MD −0.22, 95% CI −0.44 to −00.0; 1 study, 215 women; very low‐quality evidence; Analysis 4.3). This is compatible with a small effect of 0.22 standard units with the use of SERMs.
4.3. Analysis.

Comparison 4: Selective estrogen receptor modulators (SERMs) versus placebo/no treatment, Outcome 3: Arousal
In the subgroup of unselected postmenopausal women, SERMs versus placebo or no intervention probably slightly improve arousal (MD 0.28, 95% CI 0.11 to 0.46; I² = 0%; 2 studies, 1543 women; low‐quality evidence; Analysis 4.3). This is compatible with a small effect of 0.28 standard units with the use of SERMs.
4.4 Lubrication
In the subgroup of symptomatic or early postmenopausal women, we are uncertain of the effect of SERMs versus placebo or no intervention on lubrication (MD −0.17, 95% CI −1.44 to 1.10, 1 study, 215 women, very low‐quality evidence; Analysis 4.4). This is compatible with a small effect of 0.17 standard units with the use of SERMs.
4.4. Analysis.

Comparison 4: Selective estrogen receptor modulators (SERMs) versus placebo/no treatment, Outcome 4: Lubrication
In the subgroup of unselected postmenopausal women, SERMs versus placebo or no intervention probably slightly improve lubrication (MD 0.62, 95% CI 0.42 to 0.82; I² = 64%; 2 studies, 1546 women; low‐quality evidence; Analysis 4.4). This is compatible with a small effect of 0.62 standard units with the use of SERMs. Investigation of additional sources of bias suggests that the high heterogeneity observed in this subgroup (I² = 64%) could be due to:
clinical heterogeneity related to variability in the participants (Archer 2019 included women with postmenopausal symptoms with an intact uterus; Constantine 2015 included women with symptoms of vaginal atrophy or a bothersome symptom of dyspareunia); and
methodological heterogeneity related to variability in the risk of bias (Archer 2019 high risk of bias; Constantine 2015, moderate risk of bias).
4.5 Orgasm
In the subgroup of symptomatic or early postmenopausal women, we are uncertain of the effect of SERMs versus placebo or no intervention on orgasm (MD −0.38, 95% CI −0.66 to −0.10; 1 study, 215 women; very low‐quality evidence; Analysis 4.5). This is compatible with a small effect of 0.38 standard units with the use of SERMs.
4.5. Analysis.

Comparison 4: Selective estrogen receptor modulators (SERMs) versus placebo/no treatment, Outcome 5: Orgasm
In the subgroup of unselected postmenopausal women, SERMs versus placebo or no intervention probably slightly improve orgasm (MD 0.35, 95% CI 0.15 to 0.55; I² = 55%; 2 studies, 1546 women; very low‐quality evidence; Analysis 4.5). This is compatible with a large effect of 0.35 standard units with the use of SERMs. Investigation of additional sources of bias suggests that the high heterogeneity observed in this subgroup (I² = 55%) could be due to:
clinical heterogeneity related to variability in the participants (Archer 2019 included women with postmenopausal symptoms with an intact uterus; Constantine 2015 included women with symptoms of vaginal atrophy or a bothersome symptom of dyspareunia); and
methodological heterogeneity related to variability in the risk of bias (Archer 2019, high risk of bias; Constantine 2015, moderate risk of bias).
4.6 Satisfaction
In the subgroup of symptomatic or early postmenopausal women, we are uncertain of the effect of SERMs versus placebo or no intervention on satisfaction (MD −0.28, 95% CI −0.56 to −0.00; 1 study, 215 women; very low‐quality evidence; Analysis 4.6). This is compatible with a small effect of 0.28 standard units with the use of SERMs.
4.6. Analysis.

Comparison 4: Selective estrogen receptor modulators (SERMs) versus placebo/no treatment, Outcome 6: Satisfaction
In the subgroup of unselected postmenopausal women, SERMs versus placebo or no intervention probably slightly improve satisfaction (MD 0.23, 95% CI 0.07 to 0.39; I² = 0.0%; 2 studies, 1527 women; low‐quality evidence; Analysis 4.6). This is compatible with a small effect of 0.23 standard units with the use of SERMs.
4.7 Pain
No study reported this outcome in the subgroup of symptomatic or early postmenopausal women.
In the subgroup of unselected postmenopausal women, the effect of SERMs versus placebo or no intervention probably slightly improve pain (MD 0.53, 95% CI 0.33 to 0.74; I² = 0%, 2 studies, 1543 women; low‐quality evidence; Analysis 4.7). This is compatible with a moderate effect of 0.53 standard units with the use of SERMs.
4.7. Analysis.

Comparison 4: Selective estrogen receptor modulators (SERMs) versus placebo/no treatment, Outcome 7: Pain
5. Comparison of SERMs combined with estrogen versus placebo or no intervention
Primary outcome
5.1 Sexual function composite score
In the subgroup of symptomatic or early postmenopausal women, we are uncertain of the effect of SERMs combined with estrogen versus placebo or no intervention on the sexual function composite score (SMD 0.22, 95% CI 0.00 to 0.43; 1 study, 542 women; very low‐quality evidence; Analysis 5.1, Figure 8). This means that the sexual function composite score is compatible with a small effect of 0.22 standard units with the use of SERMs combined with estrogen. Due to the limited studies available, it was not possible to perform sensitivity analyses.
5.1. Analysis.

Comparison 5: Selective estrogen receptor modulators (SERMs) + estrogens versus placebo/no treatment, Outcome 1: Sexual function composite score
8.

Forest plot of comparison: 5 Selective estrogen receptor modulators (SERMs) + estrogens versus placebo/no treatment, outcome: 5.1 Sexual function composite score.
In the subgroup of unselected postmenopausal women, we are uncertain of the effect of SERMs combined with estrogen versus placebo or no intervention on the sexual function composite score (SMD 2.79, 95% CI 2.41 to 3.18; 1 study, 272 women; very low‐quality evidence; Analysis 5.1, Figure 8). This means that the sexual function composite score is compatible with a large effect of 2.79 standard units with the use of SERMs combined with estrogen versus placebo or no intervention. Due to the limited studies available, it was not possible to perform sensitivity analyses.
We observed considerable heterogeneity (I² = 99.2%) when comparing these two subgroups and so pooled analysis was not appropriate (Figure 8).
Secondary outcomes
5.2 Desire
No study reported this outcome.
5.3 Arousal
In the subgroup symptomatic or early postmenopausal women, we are uncertain of the effect of SERMs combined with estrogen versus placebo or no intervention on arousal (MD 0.07, 95% CI 0.03 to 0.10; 1 study, 542 women; very low‐quality evidence; Analysis 5.3). This is compatible with a small effect of 0.07 standard units with the use of SERMs combined with estrogen.
5.3. Analysis.

Comparison 5: Selective estrogen receptor modulators (SERMs) + estrogens versus placebo/no treatment, Outcome 3: Arousal
No study reported this outcome in unselected postmenopausal women.
5.4 Lubrication
In the subgroup symptomatic or early postmenopausal women, we are uncertain of the effect of SERMs combined with estrogen versus placebo or no intervention on lubrication (MD −0.33, 95% CI −0.51 to −0.16; 1 study, 542 women; very low‐quality evidence; Analysis 5.4). This is compatible with a small effect of 0.33 standard units with the use of SERMs combined with estrogen.
5.4. Analysis.

Comparison 5: Selective estrogen receptor modulators (SERMs) + estrogens versus placebo/no treatment, Outcome 4: Lubrication
No study reported this outcome in unselected postmenopausal women.
5.5 Orgasm
In the subgroup symptomatic or early postmenopausal women, we are uncertain of the effect of SERMs combined with estrogen versus placebo or no intervention on orgasm (MD −0.05, 95% CI −0.42 to 0.32; 1 study, 542 women; very low‐quality evidence; Analysis 5.5). This is compatible with a small effect of 0.05 standard units with the use of SERMs combined with estrogen.
5.5. Analysis.

Comparison 5: Selective estrogen receptor modulators (SERMs) + estrogens versus placebo/no treatment, Outcome 5: Orgasm
No study reported this outcome in unselected postmenopausal women.
5.6 Satisfaction
In the subgroup symptomatic or early postmenopausal women, we are uncertain of the effect of SERMs combined with estrogen versus placebo or no intervention on satisfaction (MD −0.02, 95% CI −0.27 to 0.22; 1 study, 542 women; very low‐quality evidence; Analysis 5.6). This is compatible with a small effect of 0.02 standard units with the use of SERMs combined with estrogen.
5.6. Analysis.

Comparison 5: Selective estrogen receptor modulators (SERMs) + estrogens versus placebo/no treatment, Outcome 6: Satisfaction
No study reported this outcome in unselected postmenopausal women.
5.7 Pain
No study reported this outcome.
Comments
We could not use a funnel plot to assess publication bias because no analysis included 10 or more studies.
Discussion
Summary of main results
We observed from the included studies that estrogen alone (moderate‐quality evidence) probably promotes a slight improvement in the sexual function composite score in women with menopause‐related symptoms (e.g. hot flushes, night sweats, vaginal dryness) or during the early postmenopausal period, or both. We are uncertain whether synthetic steroids (very low‐quality evidence), SERMs (very low‐quality evidence), and SERMs combined with estrogen (very low‐quality evidence) improve sexual function in these women (Table 1).
In the subgroup of unselected postmenopausal women, estrogen alone probably makes little or no difference to the sexual function composite score (moderate‐quality evidence). Findings for estrogen combined with progestogens (very low‐quality evidence) and synthetic steroids (very low‐quality evidence) showed that it is uncertain whether these treatments improve sexual function. Findings for SERMs versus placebo (very low‐quality evidence) showed that this treatment probably improves sexual function. For SERMs combined with estrogen (very low‐quality evidence), it is uncertain whether this hormone therapy improves sexual function (Table 2).
When examining the effect of estrogen alone on the specific sexual domains (sexual desire, arousal, lubrication, orgasm, satisfaction, and pain), we observed that only lubrication, pain, and satisfaction may slightly improve in the subgroup of symptomatic or early postmenopausal women (low‐quality evidence). In the subgroup of unselected postmenopausal women (moderate‐quality evidence), estrogen alone probably slightly improves lubrication. Regarding the effect of estrogen combined with progestogens, this intervention may slightly improve only lubrication in unselected postmenopausal women. SERMs (low‐quality evidence) probably slightly improve desire, arousal, lubrication, orgasm, satisfaction, and pain in the subgroup of unselected women.
Women considering the use of hormone therapy for other reasons may consider the observed effect on sexual function in the decision‐making process. Sexual complaints progressively increase with advancing age. The prospective observational Melbourne Women's Midlife Health Project annually assessed the sexual function of Australian women aged 45 years to 55 years for an eight‐year period. In this population, there was an increase in the prevalence of sexual complaints from 42% to 88% in this period, correlated with decreasing levels of estradiol (Dennerstein 2003)
The progressive decrease in sex hormones during the climacteric period until menopause can negatively affect sexual function (Ali 2020). This condition affects the ability to achieve vaginal lubrication due to atrophic changes in the vaginal mucosa that reduce vaginal lubrication and, therefore, generate a greater occurrence of dyspareunia and consequently, cause higher rates of sexual dissatisfaction in the pre‐ and postmenopausal period (da Silva Lara 2009a; Lara 2009; Simon 2011). It is also known that estrogen modulates the synthesis, action, and expression of receptors in the central nervous system such as nitric oxide and dopamine (Jacobs 2011), which modulate sexual response. The hypoestrogenism that occurs with the onset of menopause increases the risk for sexual dysfunction (Santoro 2016), such as reduced sexual desire, orgasmic disorder, and dyspareunia (Avis 2017).
The Global Study of Sexual Attitudes and Behaviors was carried out in 29 countries in a sample of 13,882 women ranging from 53 years to 58 years old. The most prevalent sexual dysfunction in this sample was lack of sexual interest, followed by the inability to reach orgasm, and poor lubrication (Nicolosi 2004). The Study of Women’s Health Across the Nation (SWAN) showed that 33% of women avoid sex due to lack of interest. However, regardless of age and menopausal status, sexual interest remained extremely important for a third of middle‐aged women (Cain 2003), reinforcing that sexual issues should be addressed by physicians in this period.
In the menopausal transition, sexual dysfunction is multifactorial and may result from several aetiologies including psychosocial factors (Yazdanpanahi 2018), chronic illness (Tabatabaeichehr 2018), medication side effects, and sexual partner problems (Lonnèe‐Hoffmann 2014), and hypoestrogenism in the menopausal transition. The exact mechanism by which hypoestrogenism affects female sexual dysfunction, particularly sexual desire disorder is unknown.
The mechanism for sexual pain involves a decline in gonadal steroid hormone levels leading to genitourinary menopause syndrome (SGUM; dryness, burning, irritation, dysuria, sexual pain; Kim 2015) resulting in sexual discomfort and pain during penis‐vagina intercourse (Portman 2014b). The structural changes in the vaginal wall due to hypoestrogenism include a reduction in the number of epithelial layers, greater deposition of short‐chain collagen, which increases tissue resistance, and increased apoptosis leading to wall fibrosis making the vagina tighter, which favours dyspareunia (Lara 2009). This in turn can lead to hypoactive sexual desire disorder (Tabatabaeichehr 2018).
The use of estrogen can mitigate the effects of hypoestrogenism on sexual function in women with menopause‐related symptoms or during the early postmenopausal period, or both (Other published versions of this review). However, before this intervention, it is crucial first to establish the role of other factors such as psychosocial and interpersonal factors, medication use, and concomitant illnesses in the sexual function of menopausal women. In addition, it is important to evaluate the sexual response as a whole (Basson 2000). In addition, it is crucial to use only appropriate terminologies related to sexual health issues, as sexual response should be evaluated in all phases including sexual satisfaction and distress (Basson 2000).
Currently, short‐term hormone therapy is recommended to alleviate menopausal symptoms and SGUM, and has been shown to prevent bone loss and fracture (NAMS 2017). Local estrogen is effective to improve SGUM symptoms (Biehl 2019). A recent study showed that ultra‐low‐dose (0.03 mg) vaginal estriol in postmenopausal women was effective to improve sexual function in women who underwent surgical treatment for stress urinary incontinence (Caruso 2020), probably due to the beneficial effect of estriol on SGUM symptoms in these women. The available data do not support systemic estrogen therapy for the treatment of female sexual dysfunction (Santoro 2016). However, systemic hormone therapy and low‐dose vaginal estrogen provide improvement of sexual problems by increasing lubrication, blood flow, and sensation in vaginal tissues (NAMS 2017).
Our findings demonstrate that hormone therapy treatment with estrogen alone is associated with a small improvement in sexual function when used in women with menopausal symptoms or early postmenopause (within five years of amenorrhoea). In addition, hormone therapy is associated with a small improvement in the domains of sexual response (sexual arousal, orgasm, and satisfaction) when used in women with menopausal symptoms or early postmenopausal women, as well as in the pain domain in unselected women. We found that estrogen alone is more effective than estrogen combined with progestogen to improve sexual function. This is in agreement with a previous study that demonstrated that sexual motivation is positively related to the level of salivary estradiol and negatively related to progesterone in women (Roney 2013). These findings should be considered as an added value to the use of hormone therapy. However, the evidence is still low quality to consider hormone therapy as a formal indication to improve sexual complaints in perimenopausal and postmenopausal women.
Finally, hormone therapy is not currently recommended for the treatment of female sexual dysfunction. However, when sexual complaints appear with the onset of menopause, not being associated with other causes of sexual dysfunction, women may benefit from hormone therapy. When the sexual complaint is limited to pain, topical estrogen works well with minimal absorption to reduce this symptom (Lethaby 2016), as confirmed by our findings, which demonstrated that estrogen and SERMs may decrease sexual pain.
Overall completeness and applicability of evidence
The review included 36 studies. Eighteen received funding from industry (Archer 2019; Bushmakin 2014; Fonseca 2007; Gast 2009; Haines 2009; Hemminki 2009; Huang 2008; Hudita 2003; Laan 2001; Liberate 2011; Maki 2007; Simon 2007; SMART‐3; Speroff 2003; Strickler 2000; Veerus 2006; WHI 1999; WISDOM 2008). Sixteen did not have data suitable for meta‐analysis (Czarnecka 2000; Fonseca 2007; Gambacciani 2011; Gast 2009; Hemminki 2009; Huang 2008; Hudita 2003; Mameri Filho 2005; Modugno 2003; Nielsen 2006; Simon 2007; Strickler 2000; Taylor 2017; Veerus 2006; WHI 1999; WISDOM 2008). Nine of them compared conjugated equine estrogen with placebo (Gast 2009; Hemminki 2009; Mameri Filho 2005; Modugno 2003; Strickler 2000; Taylor 2017; Veerus 2006; WHI 1999; WISDOM 2008); six compared estrogen alone with placebo (Huang 2008; Mameri Filho 2005; Nielsen 2006; Simon 2007; Strickler 2000; Taylor 2017); six compared estrogen in combination with medroxyprogesterone acetate with placebo (Gast 2009; Hemminki 2009; Modugno 2003; Veerus 2006; WHI 1999; WISDOM 2008); three compared estrogen in combination with progestogens with placebo (Czarnecka 2000; Fonseca 2007; Gambacciani 2011); one compared synthetic steroids (tibolone) with placebo (Hudita 2003); and one compared SERMs with placebo (Modugno 2003). In seven studies the use of hormone therapy did not improve sexual function (Hemminki 2009; Huang 2008; Mameri Filho 2005; Modugno 2003; Strickler 2000; Veerus 2006; WISDOM 2008).
We were able to draw some conclusions on the effect of hormone therapy on the sexual function of women. One relevant finding of this review was that while we included 36 studies, 35 included studies evaluated postmenopausal women with at least six months of amenorrhoea and elevated follicle‐stimulating hormone (FSH). Only one study included perimenopausal women, using tibolone 2.5 mg, and provided data for the meta‐analysis (Morais‐Socorro 2012). So the conclusions are mostly based on postmenopausal women. Other relevant findings are that the studies differed in the type of participants, drugs used, dosages, administration routes, and the tools used to assess sexual function, which explains the observed heterogeneity. In addition, 20 of the 36 studies included in this review were at high risk of bias, 14 were at moderate risk, and only two were graded as low risk of bias. Thus, it is relevant to take all this information into account when deciding to prescribe hormone therapy in order to improve the sexual function of the woman.
Quality of the evidence
Of the 36 studies included in this review, 20 are at high risk of bias for at least one risk of bias domain, 14 are at unclear risk of bias for at least one risk of bias domain, and two are low risk of bias in all risk of bias domains. This degree of bias was responsible for reducing the quality and imprecision of the evidence for many comparisons. Many included studies were supported by the pharmaceutical industry, in most cases the manufacturer of the studied drug (see Characteristics of included studies). The quality of the evidence for specific comparisons was as follows.
Symptomatic and early postmenopausal women ‐ sexual function composite score
See Table 1.
We considered the evidence on the effect of estrogen alone to be of moderate quality because we assessed most risk of bias domains as 'unclear'.
We considered the evidence on the effect of synthetic steroids (tibolone) to be of very low quality because the sample size was small with a low event rate or an effect estimate with a wide confidence interval or both, or because random allocation was inadequate or absent.
We considered the evidence on the effect of SERMs to be of very low quality because we assessed most risk of bias domains as 'unclear' or because the sample size was small with a low event rate or an effect estimate with a wide confidence interval, or both.
We considered the evidence on the effect of SERMs combined with estrogen to be of very low quality because we assessed most risk of bias domains as 'unclear' or because the sample size was small with a low event rate or an effect estimate with a wide confidence interval, or both.
Unselected postmenopausal women ‐ sexual function composite score
See Table 2.
We considered the evidence on the effect of estrogen alone to be of moderate quality because we assessed most risk of bias domains as 'unclear'.
We considered the evidence on the effect of estrogen combined with progestogens to be of very low quality because we assessed most risk of bias domains as 'unclear' or because the sample size was small with a low event rate or an effect estimate with a wide confidence interval, or both.
We considered the evidence on the effect of synthetic steroids (tibolone) to be of very low quality because we assessed most risk of bias domains as 'unclear' or because the sample size was small with a low event rate or an effect estimate with a wide confidence interval, or both, or because of inadequate randomization, allocation concealment or no evidence of blinding.
We considered the evidence on the effect of SERMs to be of low quality because we assessed most risk of bias domains as 'unclear' or because the sample size was small with a low event rate or an effect estimate with a wide confidence interval, or both.
We considered the evidence on the effect of SERMs combined with estrogen to be of very low quality because we assessed most risk of bias domains as 'unclear' or because the sample size was small with a low event rate or an effect estimate with a wide confidence interval, or both.
Potential biases in the review process
We undertook an extensive electronic and manual search and carefully evaluated the study reports for eligibility. Some studies assessed sexual function as a secondary outcome, which could impair the identification of all relevant studies. During data extraction, we made many arbitrary decisions. Each decision was reasoned by the authors, and we tried to take the most conservative decision. We contacted the authors of the majority of the included studies.
Agreements and disagreements with other studies or reviews
Systematic reviews and scientific institutions' statements are controversial regarding the use of estrogen to improve sexual function. Some reviews conclude that some types of estrogen therapy could improve some domains of sexual function (Alexander 2004; McCabe 2016b; Nappi 2009b), and some conclude they do not (NAMS 2012; Santen 2010). We observed a small benefit of hormone therapy with estrogen alone on the composite scores for sexual function. Regarding the specific domains, we observed that estrogen probably slightly improves lubrication, pain in unselected women and in women with menopause‐related symptoms, and satisfaction in symptomatic or early postmenopausal women. In unselected postmenopausal women, estrogen combined with progestogens may slightly improve lubrication, but we are uncertain of the effect of this treatment on desire, pain, orgasm, satisfaction, and arousal. SERMs may slightly improve pain in unselected postmenopausal women. Regarding synthetic steroids, other reviews agree that evidence of the effect of tibolone on sexual function is scarce (Kenemans 2005; Santen 2010).
Authors' conclusions
Implications for practice.
We included nine new studies in this update. This review brought further information on the effect of estrogen and the use of synthetic steroids and selective estrogen receptor modulators (SERMS) on female sexual function. The previous review showed that estrogen alone was associated with a small to moderate improvement in sexual function, particularly in pain in women with menopausal symptoms, or in early postmenopause, but not in unselected women. Findings for this review showed that estrogen alone probably promotes a slight improvement in the sexual function composite score in women with menopause‐related symptoms (e.g. hot flushes, night sweats, vaginal dryness) and in unselected women (moderate‐quality evidence). The domains of lubrication, pain, and satisfaction were improved in women with menopause‐related symptoms. It is uncertain whether estrogen combined with progestogen, synthetic steroids, and SERMS combined with estrogen increase sexual function due to insufficient data, poor quality of the studies, and serious risk of bias (small sample size, low event rate, or effect estimate with a wide confidence interval, or both, inadequate randomization, or inadequate blinding). This new information on the effect of estrogen therapy and also on the use of synthetic steroids and SERMS on female sexual function is possibly due to the use of validated questionnaires in most studies. These instruments are composed of domains of sexual function and do not use inaccurate denominations (e.g. libido) that may impair the evaluation of sexual function.
Implications for research.
Questions still remain on the true effect of hormone therapy in sexual function in perimenopausal and postmenopausal women. Further randomized controlled trials (RCTs) should focus on estrogen in combination with progestogens, synthetic steroids, SERMs alone, or in combination with estrogen. Most studies were at high risk of bias. Future clinical trials require a follow‐up period of at least six months to assess the effect of hormone therapy on sexual function during the climacteric period and menopause. There is a need for well‐designed randomized controlled trials to evaluate the real effect of hormone therapy on women's sexual function. Furthermore, future trials should endeavour to report the effect of hormone therapy when used specifically in women with sexual complaints. Studies including perimenopausal women (who had their last menstrual period within 12 months) are limited and further evidence is needed to clarify the real effect of hormone therapy on sexual function in this group of women.
What's new
| Date | Event | Description |
|---|---|---|
| 24 August 2023 | New citation required but conclusions have not changed | The addition of nine new studies has not led to a change in the conclusions of this review. |
| 24 August 2023 | New search has been performed | The date of the last search was 19 December 2022. The text has been revised. Nine new studies added at this update: Archer 2019; Bumphenkiatikul 2020; Bushmakin 2014; Caruso 2020; Constantine 2015; Diem 2018; Mitchell 2018; Seyyedi 2016; Taylor 2017. |
History
Protocol first published: Issue 2, 2012 Review first published: Issue 6, 2013
Acknowledgements
We acknowledge Marian Showell, Cochrane Gynaecology and Fertility's Information Specialist, for her valuable help in the search strategy.
We thank Mrs Anne Lethaby and Dr Theresa Mittermeier for providing peer review comments.
Appendices
Appendix 1. Cochrane Gynaecology and Fertility (CGF) Group Specialised Register search strategy
ProCite platform
Searched 19 December 2022
Keywords CONTAINS "menopausal" or "*Menopause" or "perimenopausal" or "perimenopause" or "Postmenopausal" or "postmenopause" or "climacteric " or Title CONTAINS "menopausal" or "*Menopause" or "perimenopausal" or "perimenopause" or "Postmenopausal" or "postmenopause" or "climacteric "
AND
Keywords CONTAINS "Hormone Replacement Therapy" or "*Hormone Substitution" or "hormone therapy" or "hormone therapy estrogen" or "estraderm" or "estradiol" or "Estriol" or "estrofen" or "estrogen" or "estrogen‐progestogen" or "*Estrogens" or "Estrone" or "estroprogestin" or "ethinyl‐estradiol" or "ethinyl estradiol‐cyproterone acetate" or "ethinyl estradiol + drospirenone" or "oestrodiol" or "oestrogen" or "conjugated equine " or "conjugated estrogen" or "conjugated estrogens" or "CEE" or "HRT" or "HT " or "premarin" or "Prempro" or "SERM" or "selective estrogen receptor modulator" or "*Clomiphene" or "raloxifene" or "toremifen" or "toremifene" or "bazedoxifene acetate" or "Evista" or "tamoxifen" or "tibolone" or "ospemifene" or Title CONTAINS "SERM" or "selective estrogen receptor modulator" or "*Clomiphene" or "raloxifene" or "toremifen" or "toremifene" or "bazedoxifene acetate" or "Evista" or "tamoxifen" or "Hormone Replacement Therapy" or "*Hormone Substitution" or "hormone therapy" or "ospemifene" or "tibolone"
AND
Keywords CONTAINS "sex drive" or "sexual" or "*Sexuality" or "dyspareunia" or "hypoactive sexual desire" or "hypoactive sexual desire disorder" or "orgasm" or "vaginal acidification" or "vaginal atrophy" or "vaginal dryness" or "vaginal lubrication" or "vaginal matuation "or "vaginal symptoms" or"*Vaginitis" or "vaginosis" or "libido" or "Vulvar Atrophy" or "vulvo‐vaginal symptoms" or "Vulvovaginal atrophy" or "vulvodynia "or "sexual arousal" or "sexual activity" or "sexual arousal disorder" or "sexual complain" or "sexual desire" or "sexual desire disorder" or "sexual dysfunction" or "sexual function" or "Sexual functioning" or "sexual interest" or "sexual life quality" or "sexual problems" or "sexual response" or "sexual satisfaction" or "sexual score" or "sexual wellbeing"
527 records
Appendix 2. CENTRAL via the Cochrane Register of Studies Online (CRSO) search strategy
Web platform
Searched 19 December 2022 #1 MESH DESCRIPTOR Climacteric EXPLODE ALL TREES 7550 #2 (climacter* or menopaus* or perimenopaus* or post?menopaus*):TI,AB,KY 26859 #3 #1 OR #2 27399 #4 MESH DESCRIPTOR Hormone Replacement Therapy EXPLODE ALL TREES 2985 #5 (HT or HRT):TI,AB,KY 5946 #6 (estrogen* or oestrogen*):TI,AB,KY 14478 #7 (estradiol* or oestradiol*):TI,AB,KY 11638 #8 (estrone* or estriol* or CEE):TI,AB,KY 1581 #9 (Dienestrol or estriol or estetrol):TI,AB,KY 490 #10 (premarin or prempro):TI,AB,KY 217 #11 MESH DESCRIPTOR Estrogens EXPLODE ALL TREES 7975 #12 MESH DESCRIPTOR Selective Estrogen Receptor Modulators EXPLODE ALL TREES 3067 #13 (SERMS or SERM):TI,AB,KY 284 #14 (selective estrogen receptor modulator*):TI,AB,KY 767 #15 (clomiphene or clomid):TI,AB,KY 1808 #16 (clomifene or clomifert):TI,AB,KY 336 #17 tamoxifen:TI,AB,KY 4939 #18 (serophene or raloxifene):TI,AB,KY 965 #19 (ly?139481 or ly?156758):TI,AB,KY 1 #20 evista:TI,AB,KY 48 #21 (dimethylamine* or novaldex):TI,AB,KY 60 #22 zitazonium:TI,AB,KY 1 #23 MF?101:TI,AB,KY 8 #24 femarelle:TI,AB,KY 3 #25 DT56a:TI,AB,KY 4 #26 toremifene:TI,AB,KY 193 #27 (bazedoxifene or ospemifene):TI,AB,KY 262 #28 tibolone:TI,AB,KY 541 #29 #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 32355 #30 #3 AND #29 12139 #31 MESH DESCRIPTOR Sexual Dysfunction, Physiological EXPLODE ALL TREES 2366 #32 MESH DESCRIPTOR Sexual Dysfunctions, Psychological EXPLODE ALL TREES 2233 #33 sex*:TI,AB,KY 71835 #34 dyspareunia:TI,AB,KY 1215 #35 (?vagina* adj2 atroph*):TI,AB,KY 560 #36 (?vagina* adj3 dry*):TI,AB,KY 608 #37 (orgasm* or libido):TI,AB,KY 1829 #38 (frigid* or arousal*):TI,AB,KY 7596 #39 HSDD:TI,AB,KY 177 #40 (hypoactive adj2 desire*):TI,AB,KY 299 #41 MESH DESCRIPTOR Libido EXPLODE ALL TREES 321 #42 psychosexual*:TI,AB,KY 218 #43 #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 80727 #44 #30 AND #43 1758
Appendix 3. MEDLINE search strategy
Ovid platform
Searched from 1946 to 19 January 2022
1 exp climacteric/ or exp menopause/ or exp menopause, premature/ or exp perimenopause/ or exp postmenopause/ (64824) 2 climacter$.tw. (5143) 3 menopaus$.tw. (53491) 4 perimenopaus$.tw. (4967) 5 post?menopaus$.tw. (60052) 6 or/1‐5 (118189) 7 exp hormone replacement therapy/ or exp estrogen replacement therapy/ (26245) 8 HRT.tw. (11260) 9 (hormon$ adj2 therap$).tw. (43608) 10 exp estrogens/ or exp epimestrol/ or exp estradiol/ or exp estrogenic steroids, alkylated/ or exp "estrogens, conjugated (usp)"/ or exp "estrogens, esterified (usp)"/ or exp estrone/ or exp ethinyl estradiol/ or exp mestranol/ or exp quinestrol/ (169730) 11 (estrogen$ or oestrogen$).tw. (171042) 12 estradiol$.tw. (85493) 13 oestradiol$.tw. (13587) 14 CEE.tw. (1391) 15 (estrone$ or estriol$).tw. (12481) 16 exp Dienestrol/ (187) 17 Dienestrol$.tw. (231) 18 exp estriol/ or exp estetrol/ or exp ethinyl estradiol‐norgestrel combination/ (6628) 19 (estriol or estetrol).tw. (4563) 20 premarin.tw. (527) 21 prempro.tw. (29) 22 exp selective estrogen receptor modulators/ or exp clomiphene/ or exp raloxifene/ or exp tamoxifen/ or exp toremifene/ (29414) 23 SERMS.tw. (1577) 24 selective estrogen receptor modulator$.tw. (3279) 25 Ospemifene.tw. (204) 26 (clomiphene or clomid).tw. (5422) 27 (clomifene or clomifert).tw. (147) 28 serophene.tw. (4) 29 raloxifene.tw. (3474) 30 keoxifene.tw. (49) 31 ly?139481.tw. (8) 32 ly?156758.tw. (32) 33 evista.tw. (67) 34 tamoxifen.tw. (24510) 35 dimethylamine$.tw. (2001) 36 novaldex.tw. (1) 37 tomaxithen.tw. (0) 38 soltamox.tw. (0) 39 zitazonium.tw. (6) 40 menerba.tw. (0) 41 MF?101.tw. (10) 42 femarelle.tw. (13) 43 DT56a.tw. (17) 44 LY?117018.tw. (82) 45 toremifene.tw. (699) 46 serm.tw. (1341) 47 bazedoxifene.tw. (438) 48 tibolone.tw. (1031) 49 or/7‐48 (350728) 50 6 and 49 (51133) 51 exp sexual dysfunction, physiological/ or exp dyspareunia/ (32912) 52 exp Sexual Dysfunctions, Psychological/ (29593) 53 sex$.tw. (858533) 54 dyspareunia.tw. (4456) 55 (vagina$ adj2 atroph$).tw. (771) 56 (vulva$ adj2 atroph$).tw. (80) 57 (vulvo$ adj2 atroph$).tw. (418) 58 (vagina$ adj2 dry$).tw. (1197) 59 orgasm.tw. (3339) 60 libido.tw. (4224) 61 orgasmic.tw. (1210) 62 frigid$.tw. (1003) 63 arousal.tw. (31381) 64 HSDD.tw. (315) 65 (hypoactive adj2 desire).tw. (657) 66 exp Libido/ (4994) 67 psychosexual$.tw. (2031) 68 or/51‐67 (909629) 69 randomized controlled trial.pt. (582929) 70 controlled clinical trial.pt. (95137) 71 randomized.ab. (576755) 72 placebo.tw. (237952) 73 clinical trials as topic.sh. (200654) 74 randomly.ab. (393184) 75 trial.ti. (271269) 76 (crossover or cross‐over or cross over).tw. (94919) 77 or/69‐76 (1510979) 78 exp animals/ not humans.sh. (5074784) 79 77 not 78 (1387646) 80 50 and 68 and 79 (1417)
Appendix 4. Embase search strategy
Ovid platform
Searched from 1980 to 19 January 2022
1 exp climacterium/ (8862) 2 exp menopause/ or exp early menopause/ or exp menopause related disorder/ or exp "menopause and climacterium"/ (149229) 3 exp postmenopause/ (73252) 4 climacter$.tw. (5276) 5 menopaus$.tw. (80877) 6 perimenopaus$.tw. (7260) 7 post?menopaus$.tw. (85922) 8 or/1‐7 (188612) 9 exp hormone substitution/ or exp hormonal therapy/ or exp substitution therapy/ or exp estrogen therapy/ (411894) 10 (hormon$ adj2 therap$).tw. (64008) 11 HRT.tw. (16283) 12 exp estrogen/ (272789) 13 exp estradiol/ or exp drospirenone plus estradiol/ or estradiol valerate/ or exp desogestrel plus estradiol/ or estradiol valerate plus medroxyprogesterone acetate/ or exp cyproterone acetate plus estradiol valerate/ or exp dydrogesterone plus estradiol/ or exp 17alpha estradiol/ or exp dienogest plus estradiol valerate/ (122369) 14 exp conjugated estrogen/ (9922) 15 (estrogen$ or oestrogen$).tw. (201745) 16 estradiol$.tw. (97338) 17 oestradiol$.tw. (12815) 18 CEE.tw. (1944) 19 (estrone$ or estriol$).tw. (11826) 20 exp dienestrol/ (543) 21 Dienestrol$.tw. (192) 22 exp estriol/ (6472) 23 exp estetrol/ (259) 24 exp ethinylestradiol/ (16833) 25 (estriol or estetrol).tw. (3977) 26 premarin.tw. (2934) 27 prempro.tw. (394) 28 exp selective estrogen receptor modulator/ (8538) 29 exp clomifene/ (4960) 30 exp raloxifene/ (12076) 31 exp tamoxifen/ (69084) 32 exp toremifene/ (2362) 33 (SERMS or SERM).tw. (3559) 34 selective estrogen receptor modulator$.tw. (4505) 35 Ospemifene.tw. (320) 36 (clomiphene or clomid).tw. (6808) 37 (clomifene or clomifert).tw. (245) 38 serophene.tw. (202) 39 raloxifene.tw. (4945) 40 keoxifene.tw. (57) 41 ly?139481.tw. (11) 42 ly?156758.tw. (31) 43 evista.tw. (1032) 44 (tamoxifen or toremifene).tw. (37443) 45 dimethylamine$.tw. (2138) 46 novaldex.tw. (118) 47 tomaxithen.tw. (0) 48 soltamox.tw. (19) 49 zitazonium.tw. (29) 50 menerba.tw. (5) 51 MF?101.tw. (20) 52 femarelle.tw. (23) 53 DT56a.tw. (24) 54 LY?117018.tw. (89) 55 bazedoxifene.tw. (729) 56 tibolone.tw. (1415) 57 or/9‐56 (793078) 58 exp sexual dysfunction/ (93080) 59 exp dyspareunia/ or exp female sexual dysfunction/ or exp pain/ (1548735) 60 dyspareunia.tw. (8557) 61 sexual$.tw. (328134) 62 (vagina$ adj2 atroph$).tw. (1408) 63 (vulva$ adj2 atroph$).tw. (124) 64 (vulvo$ adj2 atroph$).tw. (710) 65 (vagina$ adj2 dry$).tw. (2208) 66 orgasm.tw. (5844) 67 libido.tw. (6132) 68 orgasmic.tw. (2092) 69 exp libido disorder/ or exp libido/ (13718) 70 frigid$.tw. (818) 71 arousal.tw. (40139) 72 HSDD.tw. (702) 73 exp hypoactive sexual desire disorder/ or exp psychosexual disorder/ (23653) 74 psychosexual$.tw. (2923) 75 (hypoactive adj2 desire).tw. (1278) 76 or/58‐75 (1932729) 77 Clinical Trial/ (1039669) 78 Randomized Controlled Trial/ (736575) 79 exp randomization/ (95813) 80 Single Blind Procedure/ (48500) 81 Double Blind Procedure/ (198511) 82 Crossover Procedure/ (72218) 83 Placebo/ (375048) 84 Randomi?ed controlled trial$.tw. (302029) 85 Rct.tw. (49762) 86 random allocation.tw. (2405) 87 randomly allocated.tw. (42909) 88 allocated randomly.tw. (2831) 89 (allocated adj2 random).tw. (854) 90 Single blind$.tw. (29718) 91 Double blind$.tw. (229040) 92 ((treble or triple) adj blind$).tw. (1689) 93 placebo$.tw. (346574) 94 prospective study/ (814176) 95 or/77‐94 (2612946) 96 case study/ (90165) 97 case report.tw. (497427) 98 abstract report/ or letter/ (1214388) 99 or/96‐98 (1788047) 100 95 not 99 (2550726) 101 8 and 57 and 76 and 100 (4917)
Appendix 5. PsycINFO search strategy
Ovid platform
Searched from 1806 to 19 December 2022
1 exp menopause/ (4044) 2 climacter$.tw. (541) 3 menopaus$.tw. (5387) 4 perimenopaus$.tw. (767) 5 post?menopaus$.tw. (2816) 6 or/1‐5 (7492) 7 exp Hormone Therapy/ or exp Estrogens/ (8782) 8 (hormon$ adj2 therap$).tw. (2807) 9 HRT.tw. (675) 10 exp Estradiol/ (3320) 11 (estrogen$ or oestrogen$).tw. (9144) 12 (estradiol$ or oestradiol$).tw. (7022) 13 CEE.tw. (227) 14 (estrone$ or estriol$).tw. (256) 15 Dienestrol.tw. (0) 16 exp Estradiol/ (3320) 17 (estriol or estetrol).tw. (67) 18 premarin.tw. (43) 19 prempro.tw. (11) 20 selective estrogen receptor modulator$.tw. (187) 21 Ospemifene.tw. (9) 22 (clomiphene or clomid).tw. (57) 23 (clomifene or clomifert).tw. (0) 24 raloxifene.tw. (149) 25 tamoxifen.tw. (620) 26 toremifene.tw. (5) 27 (SERMS or SERM).tw. (113) 28 serophene.tw. (0) 29 bazedoxifene.tw. (9) 30 menerba.tw. (0) 31 MF?101.tw. (0) 32 tibolone.tw. (42) 33 or/7‐32 (16484) 34 exp sexual satisfaction/ or exp sexuality/ (19348) 35 sexual$.tw. (198107) 36 dyspareunia.tw. (634) 37 (vagina$ adj2 atroph$).tw. (57) 38 (vagina$ adj2 dry$).tw. (177) 39 orgasm$.tw. (3392) 40 libido.tw. (2895) 41 orgasmic.tw. (943) 42 frigid$.tw. (446) 43 arousal.tw. (34189) 44 HSDD.tw. (231) 45 (hypoactive adj2 desire).tw. (505) 46 exp Libido/ (885) 47 psychosexual$.tw. (3673) 48 or/34‐47 (231715) 49 6 and 33 and 48 (414) 50 random.tw. (67215) 51 control.tw. (495413) 52 double‐blind.tw. (24631) 53 clinical trials/ (12127) 54 placebo/ (6375) 55 exp Treatment/ (1169415) 56 or/50‐55 (1608917) 57 49 and 56 (268)
Appendix 6. CINAHL search strategy
Ebsco platform
Searched from 1961 to 12 January 2021
(menopaus*) AND (sexual) AND ((trial) OR (random*))
CINAHL (Dec‐12‐2012) = 51 records
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
Search strategy (May‐21‐2018)
(menopaus*) AND (sexual) AND ((trial) OR (random*))
CINAHL (May‐21‐2018) = 48 records
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
Search strategy (Jan‐11‐2021)
(menopaus*) AND (sexual) AND ((trial) OR (random*))
CINAHL (May‐21‐2018) = 32 records
Appendix 7. LILACS search strategy
Web platform
Searched 11 January 2021
(menopaus$) AND (sexual) AND ((trial) OR (random$))
= 37 records
Appendix 8. ClinicalTrials.gov search strategy
Web platform
Searched 21 May 2018, more recent trial registrations were found in the CENTRAL 2020 output
(menopause) AND (sexual)
= 181 records
NOTE: The search was not carried out in 2021, because since 2021, the trials are included in CENTRAL
Appendix 9. Controlled‐Trials search strategy
Web platform
Searched 21 May 2018, more recent trial registrations were found in the CENTRAL 2020 output
(menopause) AND (sexual)
= 21 records
NOTE: The search was not carried out in 2021, because since 2021, the trials are included in CENTRAL
Appendix 10. WHO International Clinical Trials Registry Platform search strategy
Web platform
Searched 27 May 2018, more recent trial registrations were found in the CENTRAL 2020 output
(menopause) AND (sexual)
= 87 records
NOTE: The search was not carried out in 2021, because since 2021, the trials are included in CENTRAL
Appendix 11. Web of Science search strategy
Web platform
Searched 11 January 2021
(menopause) AND (sexual) AND ((trial) OR (random$))
= 457 records
Data and analyses
Comparison 1. Estrogen alone versus placebo/no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Sexual function composite score | 9 | 1307 | Std. Mean Difference (IV, Random, 95% CI) | 0.60 [0.16, 1.04] |
| 1.1.1 Symptomatic or early post‐menopausal | 3 | 699 | Std. Mean Difference (IV, Random, 95% CI) | 0.50 [0.04, 0.96] |
| 1.1.2 Unselected post‐menopausal women | 6 | 608 | Std. Mean Difference (IV, Random, 95% CI) | 0.64 [‐0.12, 1.41] |
| 1.2 Desire | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.3 Arousal | 4 | 623 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.14, 0.42] |
| 1.3.1 Symptomatic or early post‐menopausal | 1 | 239 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.12, 0.39] |
| 1.3.2 Unselected post‐menopausal women | 3 | 384 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.29, 0.58] |
| 1.4 Lubrication | 4 | 619 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [0.12, 0.83] |
| 1.4.1 Symptomatic or early post‐menopausal | 1 | 239 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [0.21, 0.73] |
| 1.4.2 Unselected post‐menopausal women | 3 | 380 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [‐0.09, 1.02] |
| 1.5 Orgasm | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.6 Satisfaction | 5 | 824 | Std. Mean Difference (IV, Random, 95% CI) | 0.41 [0.04, 0.77] |
| 1.6.1 Symptomatic or early post‐menopausal | 2 | 446 | Std. Mean Difference (IV, Random, 95% CI) | 0.29 [0.08, 0.51] |
| 1.6.2 Unselected post‐menopausal women | 3 | 378 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [‐0.21, 1.16] |
| 1.7 Pain | 5 | 958 | Std. Mean Difference (IV, Random, 95% CI) | 0.57 [0.14, 1.00] |
| 1.7.1 Symptomatic or early post‐menopausal | 2 | 548 | Std. Mean Difference (IV, Random, 95% CI) | 0.35 [0.14, 0.56] |
| 1.7.2 Unselected post‐menopausal women | 3 | 410 | Std. Mean Difference (IV, Random, 95% CI) | 0.72 [‐0.09, 1.52] |
Comparison 2. Estrogen + progestogens versus placebo/no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Sexual function composite score | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1.1 Unselected post‐menopausal women | 1 | 104 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐1.52, 1.68] |
| 2.2 Desire at 16‐month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.2.1 Symptomatic or early post‐menopausal | 1 | 158 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [0.21, 1.19] |
| 2.3 Desire at 22‐ and 24‐month follow‐up | 2 | 155 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.12, 0.51] |
| 2.3.1 Unselected post‐menopausal women | 2 | 155 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.12, 0.51] |
| 2.4 Arousal | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.4.1 Unselected post‐menopausal women | 1 | 104 | Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.11, 0.75] |
| 2.5 Lubrication | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.5.1 Unselected post‐menopausal women | 1 | 104 | Mean Difference (IV, Fixed, 95% CI) | 0.45 [0.13, 0.77] |
| 2.6 Orgasm | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.6.1 Unselected post‐menopausal women | 1 | 104 | Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.53, 0.61] |
| 2.7 Satisfaction | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.7.1 Unselected post‐menopausal women | 1 | 104 | Mean Difference (IV, Fixed, 95% CI) | 0.13 [‐0.28, 0.54] |
| 2.8 Pain | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.8.1 Unselected post‐menopausal women | 1 | 104 | Mean Difference (IV, Fixed, 95% CI) | 0.93 [0.02, 1.84] |
Comparison 3. Synthetic steroids versus placebo/no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Sexual function composite score | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1.1 Symptomatic or early post‐menopausal | 1 | 883 | Std. Mean Difference (IV, Random, 95% CI) | 1.32 [1.18, 1.47] |
| 3.1.2 Unselected post‐menopausal women | 1 | 105 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.07, 0.85] |
| 3.2 Desire at 12‐month follow‐up | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.2.1 Symptomatic or early post‐menopausal | 1 | 57 | Std. Mean Difference (IV, Fixed, 95% CI) | 1.19 [0.62, 1.75] |
| 3.2.2 Unselected post‐menopausal women | 1 | 39 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.44, 0.82] |
| 3.3 Desire at 24‐month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.3.1 Unselected post‐menopausal women | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.35 [0.21, 0.49] |
| 3.4 Arousal at 12‐month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.4.1 Unselected post‐menopausal women | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.43, 0.81] |
| 3.5 Arousal at 24‐month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.5.1 Unselected post‐menopausal women | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.87 [0.47, 1.27] |
| 3.6 Lubrication at 12‐month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.6.1 Unselected post‐menopausal women | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | 0.56 [0.04, 1.08] |
| 3.7 Lubrication at 24‐month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.7.1 Unselected post‐menopausal women | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.62 [0.28, 0.96] |
| 3.8 Orgasm at 12‐month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.8.1 Unselected post‐menopausal women | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.98, 1.48] |
| 3.9 Orgasm at 24‐month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.9.1 Unselected post‐menopausal women | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.31 [‐0.19, 0.81] |
| 3.10 Satisfaction | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.10.1 Unselected post‐menopausal women | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.51 [0.12, 0.90] |
| 3.11 Pain at 12‐month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.11.1 Unselected post‐menopausal women | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.18, 0.42] |
| 3.12 Pain at 24‐month follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.12.1 Unselected post‐menopausal women | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [0.01, 1.79] |
Comparison 4. Selective estrogen receptor modulators (SERMs) versus placebo/no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Sexual function composite score | 3 | 1740 | Mean Difference (IV, Fixed, 95% CI) | 0.84 [0.18, 1.49] |
| 4.1.1 Symptomatic or early post‐menopausal women | 1 | 215 | Mean Difference (IV, Fixed, 95% CI) | ‐1.00 [‐2.00, ‐0.00] |
| 4.1.2 Unselected post‐menopuasal women | 2 | 1525 | Mean Difference (IV, Fixed, 95% CI) | 2.24 [1.37, 3.11] |
| 4.2 Desire | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.2.1 Unselected post‐menopausal women | 2 | 1545 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [0.14, 0.36] |
| 4.3 Arousal | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.3.1 Symptomatic or early post‐menopausal | 1 | 215 | Mean Difference (IV, Fixed, 95% CI) | ‐0.22 [‐0.44, ‐0.00] |
| 4.3.2 Unselected post‐menopausal women | 2 | 1543 | Mean Difference (IV, Fixed, 95% CI) | 0.28 [0.11, 0.46] |
| 4.4 Lubrication | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.4.1 Symptomatic or early post‐menopausal | 1 | 215 | Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐1.44, 1.10] |
| 4.4.2 Unselected post‐menopausal women | 2 | 1546 | Mean Difference (IV, Fixed, 95% CI) | 0.62 [0.42, 0.82] |
| 4.5 Orgasm | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.5.1 Symptomatic or early post‐menopausal | 1 | 215 | Mean Difference (IV, Fixed, 95% CI) | ‐0.38 [‐0.66, ‐0.10] |
| 4.5.2 Unselected post‐menopausal women | 2 | 1546 | Mean Difference (IV, Fixed, 95% CI) | 0.35 [0.15, 0.55] |
| 4.6 Satisfaction | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.6.1 Symptomatic or early post‐menopausal | 1 | 215 | Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.56, ‐0.00] |
| 4.6.2 Unselected post‐menopausal women | 2 | 1527 | Mean Difference (IV, Fixed, 95% CI) | 0.23 [0.07, 0.39] |
| 4.7 Pain | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.7.1 Unselected post‐menopausal women | 2 | 1543 | Mean Difference (IV, Fixed, 95% CI) | 0.53 [0.33, 0.74] |
Comparison 5. Selective estrogen receptor modulators (SERMs) + estrogens versus placebo/no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Sexual function composite score | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1.1 Symptomatic or early post‐menopausal | 1 | 542 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.22 [0.00, 0.43] |
| 5.1.2 Unselected post‐menopausal women | 1 | 272 | Std. Mean Difference (IV, Fixed, 95% CI) | 2.79 [2.41, 3.18] |
| 5.3 Arousal | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.3.1 Symptomatic or early post‐menopausal | 1 | 542 | Mean Difference (IV, Fixed, 95% CI) | 0.07 [0.03, 0.10] |
| 5.4 Lubrication | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.4.1 Symptomatic or early post‐menopausal | 1 | 542 | Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐0.51, ‐0.16] |
| 5.5 Orgasm | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.5.1 Symptomatic or early post‐menopausal | 1 | 542 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.42, 0.32] |
| 5.6 Satisfaction | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.6.1 Symptomatic or early post‐menopausal | 1 | 542 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.27, 0.22] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Archer 2019.
| Study characteristics | ||
| Methods | RCT phase 3, multicentre, 68 centres in the USA | |
| Participants | Inclusion criteria: "postmenopausal women aged 40‐80 years with intact uterus, or having a serum follicle‐stimulating hormone level > 40 IU/L for hysterectomized women with intact ovaries, or 6 weeks since bilateral oophorectomy, or women aged 45 years with an unknown date of their last spontaneous menstrual bleed reporting moderate or severe vaginal dryness as their MBS with ≤ 5% superficial cells on their vaginal wall smear and a vaginal pH Inclusion criteria > 5.0 were eligible to participate". | |
| Interventions | Intervention for up to 12 weeks: oral ospemifene 60 mg once daily Control: placebo (local‐based lubricant K‐Y Jelly as needed during penis‐vagina sexual relation) |
|
| Outcomes | FSFI scores were also secondary endpoint, collected at weeks 4, 8, and 12 | |
| Notes | Dr Archer has received research support from Actavis, Bayer Healthcare, Endoceutics, Glenmark, Merck, Radius Health, Shionogi, and Therapeutics MD; has served as consultant to AbbVie, Actavis, Agile Therapeutics, Bayer Healthcare, Endoceutics, Exeltis, InnovaGyn, Merck, Pfizer, Radius Health, Sermonix, Shionogi, Teva Women’s Healthcare, and Therapeutics. Dr Goldstein serves on the advisory board for AbbVie, Allergan, IBSA, Pfizer, and Therapeutics MD; and is a consultant for Cook ObGyn and Cooper Surgical. Dr Simon has served as consultant/advisor to AbbVie, Allergan, AMAG, Amgen, Ascend Therapeutics, Azure Biotech, Bayer Healthcare, CEEK Enterprises, Covance, Millendo Therapeutics, Mitsubishi Tanage |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization schedule prepared by an independent statistician before study start |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | All study staff and participants were blinded throughout the study; ospemifene 60 mg and placebo tablets were identical in appearance and packaging |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | FSFI total scores and scores for all domains of FSFI |
| Selective reporting (reporting bias) | Low risk | Participant withdrawal (ospemifene, 4.1%; placebo, 5.1%). Study discontinuation due to AEs was low (ospemifene, 1.9%; placebo, 3.2%). The majority of women who received ospemifene and placebo were included in the intention to treat (ITT) population (99.1% vs 99.7%) and completed the 12‐week study (89.6% vs 88.6%) |
| Other bias | Low risk | Not suspected |
Bumphenkiatikul 2020.
| Study characteristics | ||
| Methods | RCT, single centre, Thailand | |
| Participants | Inclusion criteria: women aged 45–70 years who experienced spontaneous menopause with penile‐vaginal penetrative sexual intercourse at least once a month and reported at least one self‐assessed vaginal atrophy symptom in moderate or severe intensity | |
| Interventions | Intervention: intravaginal ovule containing 0.03 mg estriol Control: matching placebo |
|
| Outcomes | FSFI total scores and scores for all domains of FSFI | |
| Notes | The study was supported by THE 90TH ANNIVERSARY OF CHULALONGKORN UNIVERSITY FUND (Ratchadaphiseksomphot Endowment Fund). The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerized randomization |
| Allocation concealment (selection bias) | Low risk | The allocation and concealment of placebo and the drugs into identical opaque envelopes were done by a nurse... |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | ...who was not involved in contacting patients or analysing any data |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding complete and unlikely that the blinding could have been broken |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasosns for missing data not related to outcome |
| Selective reporting (reporting bias) | Low risk | The protocol is available |
| Other bias | Low risk | The study appears to be free from sources of risk |
Bushmakin 2014.
| Study characteristics | ||
| Methods | RCT, multi centre, 43 sites in the USA | |
| Participants | Inclusion criteria: postmenopausal women aged 40‐65 years with an intact uterus who had ≥ 7 moderate‐severe hot flushes/d at baseline (or ≥ 50/week) | |
| Interventions | Intervention 12 weeks: bazedoxifene 20 mg + conjugate estrogens 0.45 mg, bazedoxifene 20 mg + conjugate estrogens 0.625 mg Control: matching placebo |
|
| Outcomes | MENQOL, sexual function domain score | |
| Notes | Funding and conflict of interest was copied in full from the manuscript: "The demographic data and the risk of bias has been reported in the first SMART‐2 study. This study was sponsored by Pfizer. The SMART‐2 trial was sponsored by Wyeth Research, which was acquired by Pfizer in October 2009. The medical writing support was provided by Katie McClendon, PhD, of MedErgy, and Diane M. Sloan, PharmD, of Peloton Advantage and was funded by Pfizer. Three authors of the study (AGB, JCC, and SM) are employees of Pfizer Inc. One author of the study (LA) is an employee of Pfizer Ltd. One author of the study (JVP) has served as a consultant (fees to the University of Virginia) for Pfizer, Noven Pharmaceuticals, Shionogi, and DepoMed; has received grants/research support (fees to the University of Virginia) from DepoMed, Bionova, and Endoceutics; and has received travel funds from Pfizer, Noven Pharmaceuticals, Shionogi, and DepoMed" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerized randomization/enrolment system generated by Wyeth Research |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinded, matching placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is not clear how many women answered the final questionnaires, and if the women who withdrew from treatment had the final evaluation |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Caruso 2020.
| Study characteristics | ||
| Methods | RCT, single‐centre, Italy | |
| Participants | Inclusion criteria: "Ninety‐six postmenopausal women ranging in age from 47 to 73 years (mean age 57.5 ± 6.8), affected by SUI requiring surgical treatment, were eligible for this study" Exclusion: "body mass index (BMI) ≥ 35 kg/m2, endometrial thickness ≥ 4 mm, abnormal uterine bleeding,hormone‐dependent malignancies, history of thromboembolic disease,liver disease, and/or using systemic or local hormone therapy for less than 3 months, phytoestrogens use, use of nonhormonal lubricants or moisturizers within 30 days before the start of the study, without sexual relation for more than a month, having a partner with a sexual disorder" |
|
| Interventions | Intervention: 0.03 mg daily estriol vaginal ovule for 8 weeks before and 8 weeks after transobturator tape (TOT) surgical placement. | |
| Outcomes | FSFI total scores and scores for all domains of FSFI are reported | |
| Notes | Funding and financial disclosure/conflicts of interest: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The participants were enroled by a single operator |
| Allocation concealment (selection bias) | Unclear risk | We are not sure how the assignments were hidden |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | We are not sure how the participants and personnel were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | We are not sure how the outcome assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasosns for missing data not related to outcomes |
| Selective reporting (reporting bias) | High risk | The protocol was not available |
| Other bias | High risk | Possible biases in randomization or blinding |
Constantine 2015.
| Study characteristics | ||
| Methods | RCT, parallel‐group, phase‐3, USA | |
| Participants | Inclusion criteria: women with symptoms of vaginal atrophy and bothersome symptoms of either dyspareunia or vaginal dryness. Exclusion criteria are unclear. |
|
| Interventions | Intervention: ospemifene 60 mg/day administered for 12 weeks Control: placebo |
|
| Outcomes | The total FSFI score is the sum of the scores for the 6 individual domains | |
| Notes | Study does not report RCT protocol | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Does not report demographic data after losses. Suspected unbalance of losses in the groups |
| Selective reporting (reporting bias) | High risk | Does not report baseline scores of FSFI domains |
| Other bias | Unclear risk | Does not report details of randomization in recruitment. Recruitment bias suspected |
Czarnecka 2000.
| Study characteristics | ||
| Methods | RCT, single centre, Poland | |
| Participants | Inclusion: postmenopausal women (amenorrhoea > 6 months and estradiol < 50 pg/mL + FSH 21U/L) with mild and moderate essential hypertension Exclusion criteria are unclear. |
|
| Interventions | Intervention: 17‐β‐estradiol and norethisterone acetate (Estracomb TTS, Norvatis) Control: no treatment |
|
| Outcomes | SSA‐P Final scores |
|
| Notes | Age: intervention (49.4 ± 5.8 years), control (52.0 ± 6.4 years) BMI: intervention (27.4 ± 4.7kg/m²), control (25.0 ± 3.6kg/m²) Follow‐up: 12 weeks Do not report conflict of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described in detail |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described in detail |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | High risk | The groups differed in baseline characteristics. We observed relevant differences in the baseline sexual function (74.8 ± 24.7 vs 66.0 ± 22.4, treatment and control respectively), QoL (12.6 ± 2.3 vs 11.4 ± 2.5), and hot flushes (74.8 ± 24.7 vs 66.0 ± 22.4) scores. Study authors did not present the results as change from baseline. |
Dayal 2005.
| Study characteristics | ||
| Methods | RCT, single‐centre, USA | |
| Participants | Inclusion: menopausal women, aged 44–70 years, with a history of no menstrual cycle for at least 1 year or at least 6 months of amenorrhoea with a documented FSH level > 40 mIU/mL. "These women had no exposure to HT (specifically estrogen therapy or DHEA supplementation) for at least 60 days prior to enrolment, had a normal Pap smear and mammogram within the last year, and had normal liver transaminase levels, renal function, total cholesterol, and triglyceride levels". Exclusion: "any contraindication to estrogen therapy (known or suspected cancer of the breast, endometrial hyperplasia/carcinoma, undiagnosed vaginal bleeding, active thromboembolic disorders, or history of cerebrovascular disease, coronary artery disease, or myocardial infarction), a current diagnosis of diabetes mellitus, uncontrolled hypertension, abnormal liver or renal function, major psychiatric disorder (major depression, bipolar disorder, psychotic disorder, drug addiction), or any contraindication to the use of magnetic resonance imaging (pacemaker, magnetic aneurysm clip, severe claustrophobia)" |
|
| Interventions | Intervention: conjugated equine estrogen 0.625 mg daily Control: placebo (We included only the arms without DHEA in this review) |
|
| Outcomes | WHQ (bigger values correspond to better conditions) | |
| Notes | We excluded 2 arms with use of DHEA from the analysis Follow‐up: 3 months Mean age 56.6; ranging from 44‐77 Corresponding author did not respond to our contact via email Article presents the differences from baseline (in %) without SD or P values For sexual function, depression, and QoL, we determined the final value based on the (%) difference and considered the final SD to be equal to the baseline SD This study was supported by an unrestricted grant from the Berlex Foundation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerized program generating random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss after allocation |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | High risk | There was a relevant difference in baseline values between intervention and control groups for sexual function (4.33 ± 1.53 vs 5.00 ± 2.12, intervention and control respectively), and QoL (15.25 ± 3.40 vs 13.00 ± 4.90). Although study authors provided relative change from baseline (in %) we could not use these data because we were not able to estimate SDs. |
Diem 2018.
| Study characteristics | ||
| Methods | RCT, 2 centres, USA | |
| Participants | 302 women were randomized to receive vaginal estradiol tablet plus placebo gel (n = 102), placebo tablet plus vaginal moisturizer (n = 100), or dual placebo (n = 100) Inclusion: women aged 45‐70 years old, ≥ 2 years since last menses, reported ≥ 1 moderate–severe symptom of vulvovaginal itching, pain, dryness, or irritation experienced at least weekly within the past 30 days; or pain with penetration at least once monthly. Exclusion: current vaginal infection; use of hormonal medication in past 2 months; use of antibiotics, vaginal moisturizer, probiotic, prebiotic, or douche in past month; and chronic premenopausal vulvovaginal symptoms |
|
| Interventions | Intervention: vaginal estradiol 10 mcg tablet (Vagifem) + placebo vaginal gel (hydroxyethyl cellulose); placebo vaginal tablet + vaginal moisturizer (Replens); or placebo tablet + placebo gel | |
| Outcomes | MENQOL questionnaire (higher scores indicated poorer QoL), PHQ‐8, FSFI, and the Female Sexual Distress Scale‐Revised | |
| Notes | Data on ≥ 1 domains of the MENQOL were available on 301 women (> 99%) at baseline and 298 (99%) at 4 and/or 12 weeks of follow‐up. PHQ‐8 and GAD‐7, data were available on 301 (> 99%) women at baseline and 297 (97%) at follow‐up. Women with both baseline and follow‐up MENQOL data, 83% women randomized to estradiol tablets were inclusion criteria 80% adherent, compared to 80% women randomized to placebo tablets. 74% women randomized to vaginal moisturizer were inclusion criteria 80% adherent, compared to 79% of women randomized to placebo gel Total MENQOL scores declined, that is, menopause‐related QoL improved, in all treatment groups Vaginal estradiol group significantly improved the sexual function domain (Table 2) (mean difference at 12 weeks of 0.4 (95% CI 1.0, 0.1; P = 0.005) PHQ‐8 scores improved in all treatment groups at week 12 No evidence of interactions between treatment assignment and selected characteristics (i.e. presence or absence of sexual function–related MBS and baseline FSFI) on total MENQOL score or sexual function domain score (data not shown) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization by permuted blocks |
| Allocation concealment (selection bias) | Low risk | Used a computerized inventory system for dispensing identical‐appearing tablets in bottles and gel in tubes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, study personnel, and clinical providers were blinded to treatment assignments |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unknown if there was blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost data were reported |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Contamination and recruitment bias not suspected |
Fonseca 2007.
| Study characteristics | ||
| Methods | Cross‐over, single centre, Brazil March 2001‐February 2003 |
|
| Participants | Inclusion: postmenopausal women aged 42–61 years; with uterus and no contraindications to HT Exclusion: systemic, psychiatric or endocrine disease; smoking > 10 cigarettes/d; use of any medication that could interfere with climacteric symptoms or with their sexuality |
|
| Interventions | Intervention: 17β‐estradiol 2 mg with norethisterone acetate 1 mg (Cliane, Schering) Control: matching placebo |
|
| Outcomes | GRISS Data not suitable for meta‐analysis |
|
| Notes | Follow‐up: 6 months each part of the cross‐over trial No available data to report Financial support for this study from Schering do Brasil Quimica e Farmaceutica Ltda |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind, details not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | High risk | The study authors did not report all the results obtained. They reported only FSFI domains with statistically significant differences |
| Other bias | Low risk | Not suspected |
Gambacciani 2011.
| Study characteristics | ||
| Methods | RCT, parallel‐group, single centre, Italy | |
| Participants | Inclusion: amenorrhoea for at least 12 months before treatment, plasma gonadotropin and estradiol levels in the postmenopausal range, office BPs in the normal rang, vasomotor symptoms. Exclusion: age > 60 years; previous intolerance to HT; absence of vasomotor symptoms; history of hypertension and/or treatment with antihypertensive drugs within the last 3 months; diabetes or any other metabolic disorder including dyslipidaemia, history of CVD, venous thromboembolic disease or haemostatic disorder predisposing to thromboembolic complications; abnormal uterine bleeding; any unstable medical condition; or history of alcoholism, drug abuse, psychosis, or other emotional or intellectual problems likely to invalidate informed consent or to limit compliance with protocol requirements. |
|
| Interventions | Intervention: estradiol 1 mg + drosperinone 2 mg (Angeliq, Bayer Schering Pharma AG, Berlin, Germany) Control: calcium (1 g/d) |
|
| Outcomes | WHQ Data not suitable for meta‐analysis |
|
| Notes | Follow‐up: 3 months 70 women evaluated; 35 allocated Data from WHQ not given in numbers, just presented as a graphic No third‐party sources provided financial support for the study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 70 consecutive eligible women were randomized to treatment using a randomization list (yes – no) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts: 3/23 in the control group; 0/32 in the intervention group |
| Selective reporting (reporting bias) | High risk | Although sexual function was measured by a questionnaire, the study authors did not provide the numeric results. They stated that the scores improved after intervention |
| Other bias | Low risk | Not suspected |
Gast 2009.
| Study characteristics | ||
| Methods | RCT, double‐blind, placebo‐controlled, multi‐centre (25 sites), Brazil and USA May 2001‐April 2004 |
|
| Participants | Inclusion: women aged 45‐65 years at enrolment, had a sexual partner or partners, and had an intact uterus, their last natural menstrual cycle at least 12 months before screening (or 6 months and high FSH). Maximum of 10% superficial cells on the Vaginal Maturation Index. Endometrial thickness ≤ 5 mm by TVUS. Exclusion: history or presence of neoplasia or endometrial hyperplasia, history of thrombophlebitis, thrombosis, or thromboembolic disorders (cerebrovascular accident, stroke, or transient ischaemic attack) related to estrogen use; neuro‐ocular disorders; myocardial infarction or ischaemic heart disease; chronic renal or hepatic disease; or a known hypersensitivity to estrogen, progestogen, or other ingredients of the hormonal preparations used in the study. Also, women were excluded if they had used any oral or vaginal estrogen‐, progestogen‐, or androgen‐containing medications within 8 weeks of screening or any transdermal hormone therapy within 4 weeks before screening. In addition women diagnosed with sexual dysfunctions other than dyspareunia were excluded. |
|
| Interventions | Intervention: conjugated estrogen 0.45 mg + 1.5 mg MPA for six 28‐d cycles along with initial vaginal priming with 1 g CEE (Premarin) cream (0.625 mg CEE/g) intravaginally for the first 6 weeks Control: matching placebo |
|
| Outcomes | MFSQ BISF‐W Data not suitable for meta‐analysis |
|
| Notes | Reported the results of the questionnaire in figures, no numeric data presented This study was funded by Wyeth, Collegeville, PA. Premarin and Premarin Vaginal Cream are manufactured and marketed by Wyeth. Alberta Vieweg and Michael Gast are current or former employees of Wyeth Follow‐up: 3 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Claim to be double‐blind, no details described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts: 41/144 in the intervention group; 29/112 in the control group |
| Selective reporting (reporting bias) | High risk | Although sexual function was evaluated by a validated questionnaire the scores are not reported, the results are shown in graphics |
| Other bias | Low risk | None |
Haines 2009.
| Study characteristics | ||
| Methods | RCT, multicentre: Thailand, the Philippines, Singapore, Hong Kong and Malaysia | |
| Participants | Inclusion: aged 40‐65 years, had undergone natural menopause (12 months’ amenorrhoea or 6 months’ amenorrhoea with FSH > 40 mIU/mL) or bilateral oophorectomy (6 weeks postsurgery) and had at least 24 hot flushes (of any severity) within a 7‐d screening period Exclusion: recently used estrogen‐containing products, an abnormal cervical smear test, endometrial thickness of 5.0 mm, any condition that could interfere with study medication or interpretation of results, concomitant use of inducers or inhibitors of CYP3A4 or drugs effective in treating hot flushes, received anticoagulant treatment for the past 6 months, or known severe dyslipoproteinaemia" |
|
| Interventions | Intervention: transdermal patch delivering micro‐dose E2 (0.014 mg/d) Control: placebo |
|
| Outcomes | MENQOL questionnaire Change from baseline scores |
|
| Notes | Follow‐up: 12 weeks Age: intervention (52.6 ± 3.99 years); control (52.2 ± 4.73 years) The following outcomes could not be pooled because of lack of details:
This study was supported financially by Bayer Schering Pharma AG. Editorial support was provided by Parexel MMS |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization was by a centrally provided computer‐generated list |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Although it is not clear how many women were assessed for sexual function; we assumed it was only those who completed the study. Those participants had > 75% overall study drug compliance; thus not respecting the ITT principle |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Hemminki 2009.
| Study characteristics | ||
| Methods | RCT, parallel‐group, 3 clinical centres in Estonia 777 women randomized, January 1999‐December 2001 |
|
| Participants | Inclusion: aged 50–64 years, postmenopausal Exclusion: none |
|
| Interventions | Intervention: CEE 0.625 mg/d + MPA 5.0 mg/d Control: matching placebo |
|
| Outcomes | WHQ Percentage of women satisfied and who lost interest in sex |
|
| Notes | Follow‐up: 1 year for the included evaluation (3.6 years total) Trial register: ISRCTN35338757 Potentially eligible women were randomized into 4 trial groups resulting in 2 substudies:
1001 women were recruited into the non‐blind substudy and 777 in the blind substudy. The Estonian Postmenopausal Hormone Therapy trial was originally planned to be a part of the Women’s International Study of Long Duration Oestrogen After Menopause (WISDOM) The study was financially supported by grants from the Academy of Finland (grants 69838, 201490, 115088), STAKES (National Research and Development Centre for Welfare and Health), Finland, and the Estonian Ministry of Education and Research Drugs were donated by Wyeth Ayerst Company via the Women's International Study of Long Duration Oestrogen After Menopause (WISDOM) in the UK This study did not contribute data to meta‐analyses |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization in permuted blocks, each of a size 16 and each block of the 3 clinics separately, at the National Research and Development Centre for Welfare and Health in Finland |
| Allocation concealment (selection bias) | Low risk | The treatment allocation was enclosed in a non‐transparent sealed envelope and sent to trial clinics |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Use of matching placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Balanced dropouts Blind trial ‐ intervention 98/404; control 101/372 |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Huang 2008.
| Study characteristics | ||
| Methods | RCT, multicentre, 9 clinical centres in USA ‐ ULTRA trial | |
| Participants | Inclusion: aged 60‐80 years, with an intact uterus but who had not had a menstrual period in at least 5 years, normal bone mineral density for age (z‐score ≥ 2.0 at the lumbar spine) and could not have used estrogen or progestogen in the 3 previous months Exclusion: unexplained uterine bleeding, endometrial hyperplasia, abnormal mammogram suggestive of breast cancer, CVD, venous thromboembolism, uncontrolled hypertension, uncontrolled thyroid disease, liver disease, fasting triglyceride level > 300 mg/dL, or fasting glucose level > 180 mg/dL |
|
| Interventions | Intervention: 3.25 cm² patch releasing 0.014 mg/d estradiol Control: matching placebo |
|
| Outcomes | MOS Sexual Problems Index Final scores, data sent by the study authors |
|
| Notes | Follow‐up: 24 months Age: intervention = 66.8 (± 5.1); control = 66.7 (± 4.8) years This research was supported in part by a grant from Berlex Laboratories Inc and manufacturer of the estradiol patch used; and by Grant KLZRR024130 from the National Center for Research Resource, a component of the NIH |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly permuted blocks of size 4 |
| Allocation concealment (selection bias) | Low risk | Participants, investigators and outcome assessors were blinded to treatment assignment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, investigators and outcome assessors were blinded to treatment assignment, and no blinding occurred during the trial |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Participants, investigators and outcome assessors were blinded to treatment assignment, and no blinding occurred during the trial |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Sexual function evaluated only in women who were sexually active during in the previous 4 weeks: sexual function was evaluated on 186/208 participants in the intervention group, and on 180/209 in the control group |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Hudita 2003.
| Study characteristics | ||
| Methods | RCT, parallel‐group, single centre, Romania | |
| Participants | Inclusion: healthy women aged 40‐65 years, non‐obese, postmenopausal, with an intact uterus Exclusion:
|
|
| Interventions | Intervention 1: tibolone 1.25 mg Intervention 2: tibolone 2.5 mg Control > matching placebo |
|
| Outcomes | MFSQ Data not suitable for meta‐analysis |
|
| Notes | Follow‐up: 24 weeks Tibolone 1.25 and 2.50 mg tablets were supplied by Libbs as Libiam |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described in detail |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Used matching placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 42/162 women dropped out after inclusion, groups not described |
| Selective reporting (reporting bias) | High risk | Although sexual function was evaluated by a validated questionnaire, the scores are not reported. The study authors reported only the proportion of women with acceptable quality of sexual life |
| Other bias | Low risk | Not reported |
Laan 2001.
| Study characteristics | ||
| Methods | Cross‐over trial, single centre, the Netherlands | |
| Participants | Inclusion: postmenopausal women with intact uteri and ovaries, aged < 65 years with BMI of 18–29 kg/m², last menstrual period ≥ 12 months prior to the study Exclusion: women using medication known to influence sexual desire and/or response or who had used HT in the 3 months prior to enrolment |
|
| Interventions | Intervention: tibolone 2.5 mg/d for 3 months Control: placebo |
|
| Outcomes | Greene Climacteric Scale Change from baseline scores of the first phase of the cross‐over; provided by the study author |
|
| Notes | We included only the results concerning the first phase (before cross‐over): these data were obtained by correspondence with the study authors. This work was supported by NV Organon Follow‐up: 3 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data were available from only 37 women (17 in the intervention group and 20 in the control group): 44 women were randomly allocated |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Liberate 2011.
| Study characteristics | ||
| Methods | RCT, multicentre, 245 sites from 31 countries. Sexual function was examined only in women from 8 countries (Austria, Belgium, Germany, Spain, France, UK, Italy, The Netherlands) June 2002‐July 2007 |
|
| Participants | Inclusion: women with climacteric symptoms were eligible if they had been surgically treated within the previous 5 years for histologically confirmed breast cancer. Participants had to be postmenopausal and < 75 years. Exclusion: non‐hysterectomized women with endometrial abnormalities | |
| Interventions | Intervention: tibolone 2.5 mg daily, orally
Control: matching placebo About 75% of participants in both groups were using either tamoxifen, aromatase inhibitor, or GnRH analogues |
|
| Outcomes | WHQ Change from baseline scores WHQ 'sexual' and 'depression': the smaller the values the better the condition |
|
| Notes | Follow‐up: 26 weeks
Mean age: 52.7 (± 7.3) years
For sexual function and vasomotor domain/hot flushes, SD was calculated from P values Depression could not be included because P values were lacking Vaginal dryness could not be included because only stratified data were reported (no difference observed on any strata) Funding: Schering‐Plough (formerly NV Organon, Oss, Netherlands). The sponsor conducted the trial and collected the data. An Advisory Board had overall scientific responsibility for trial design and protocol, and advised the sponsor as to the conduct of the trial. The corresponding author had full access to all data relevant for the article publication and all authors were involved in its submission. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Centralized interactive voice response system, stratified by centre, with a block size of 4 |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, investigators, sponsor personnel, and outcome assessors were blinded to treatment assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Sexual function was evaluated in only 438/1575 women in the treatment group, and on 445/1558 in the placebo group |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Maki 2007.
| Study characteristics | ||
| Methods | RCT, multi‐centre, 19 medical centres, USA | |
| Participants | Inclusion: healthy postmenopausal women with intact uteri and whose last natural menstrual cycle had been completed ≥ 12 and ≤ 36 months prior to screening, or last natural menstrual cycle between 6 and ≤ 12 months before screening, provided their serum FSH more than the lower limit reference of normal level for postmenopausal women. Participants spoke English as their primary language and were required to demonstrate verbal knowledge with a total score 10 on the Primary Mental Abilities Vocabulary Test. Women were required to have reported at least 1 cognitive complaint on the Self‐Reported Cognitive Function Questionnaire, a brief subjective survey of memory and concentration, and to be free of neurologic, systemic, or psychiatric disease that would influence cognition. Exclusion: known or suspected estrogen‐dependent neoplasia, endometrial hyperplasia, thrombophlebitis, thrombosis, thromboembolic disorders, myocardial infarction, ischaemic heart disease, cerebrovascular accident, stroke, transient ischaemic attack, or hypersensitivity to estrogen or progestogens were not included in the study. Other exclusion criteria included recent (≤ 8 weeks prior to screening) use of estrogen or progestogen as estrogen modulates memory‐related synaptic plasticity, excessive smoking (≥ 0.5 pack of cigarettes/d), a history of alcohol abuse (based on a Michigan Alcohol Screening Test score of ≥ 5), evidence of cognitive impairment on the Mini‐Mental State Examination (total score < 24), or use of any medication that might influence central nervous system function. |
|
| Interventions | Intervention: CEE 0.625 mg + medroxiprogesterone acetate 2.5 mg daily Control: matching placebo |
|
| Outcomes | Greene Climacteric Scale Change from baseline |
|
| Notes | SD calculated from the P values of the differences between the groups MFSQ–level of interest in sex was considered as sexual function Mean age: intervention (51.9 ± 3.6 years); control (52.4 ± 3.3 years) Weight: intervention (70 ± 16.1 kg); control (67.8 ± 16.4 kg) Follow‐up: 4 months This study was funded by Wyeth, Collegeville, PA. Prempro is manufactured and marketed by Wyeth. Dr. Maki has received grants (in excess of USD 10,000) and honoraria from Wyeth. Dr. Yaffe has received grants (in excess of USD 10,000) and honoraria from Wyeth. Dr. Gast, A.J. Vieweg, and S.W. Burriss are current or former employees of Wyeth. Dr. Gast has ownership interest in the company. Dr. Yaffe received compensation through the University of California for her role as a consultant throughout the trial. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Permuted block design |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind, matching placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts: intervention (11), control (11) |
| Selective reporting (reporting bias) | High risk | Sexuality, not sexual function, was assessed by the Greene Climateric Scale, sexual QoL (not sexual function) was assessed by Utian Quality, and the levels of sexual thoughts and interest were assessed by the MFSQ. However, only the partial results (total score and some domains) of the MFSQ were reported, which do not represent the sexual function itself. |
| Other bias | Unclear risk | Statistical analyses were performed by Wyeth Research, whose conflict of interest was stated in the article. |
Mameri Filho 2005.
| Study characteristics | ||
| Methods | RCT, single centre, Brazil | |
| Participants | The diagnosis of menopause was based on clinical data, i.e. amenorrhoea for at least 12 months confirmed by elevated gonadotropin, FSH > 40 mIU/mL). Inclusion: women with vasomotor symptoms or moderate or marked Kupperman index > 39 points, with complaints of sexual function. Exclusion: women with absolute contraindication to HT, BMI > 30 (obese); Ferriman, Gallwey and Lorenzo > 8 (hirsute). In addition, women who were not on HT prior and did not use herbal or diet high in soy‐based foods (use prior 6 months) were selected for this study. |
|
| Interventions | Intervention 1: CEE 0.625 mg/d Control: placebo Intervention 2: arm not included: CEE (0.625 mg/d) associated with methyltestosterone (2.5 mg/d) |
|
| Outcomes | WHQ: composite scores MFSQ: sexual domains Final scores |
|
| Notes | We did not include the group using intervention 2 in this review Study authors provided baseline and final values for WHQ without SD. We estimated the SD from P values The article does not report any conflict of interest disclosure The drugs were donated by the university hospital Follow‐up: 3 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐based |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Use of placebo matching pills |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Mitchell 2018.
| Study characteristics | ||
| Methods | RCT, multicentre, 2 centres USA | |
| Participants | "Women aged 50‐70 years within 20 miles of the clinical sites at least 2 years since last menses, report of at least 1 moderate‐severe symptom of vulvovaginal itching, pain, irritation, or dryness experienced at least weekly within the past 30 days; or pain with penetration at least once monthly." Exclusion criteria included "current vaginal infection, use of hormonal medication in past 2 months, use of antibiotics or vaginal moisturiser in past month, and chronic premenopausal vulvovaginal symptoms" |
|
| Interventions | Intervention "1:1:1 to Vagifem 10‐μg tablet + placebo vaginal gel, placebo vaginal tablet + Replens vaginal moisturiser, or placebo tablet + placebo gel. Women were instructed to use the vaginal tablet daily for 2 weeks, then twice weekly for the remaining 10 weeks, and the vaginal moisturiser every 3 days throughout the trial". "During the first 2 weeks, participants were advised to use the tablet in the morning and gel in the evening. After that, participants were instructed to use products on alternate days." |
|
| Outcomes | The primary outcome was change in severity of the MBS Secondary outcomes were composite VSI, satisfaction with treatment received (Likert scale: 0 = not satisfied to 10 = completely satisfied), meaningful benefit from the study medications (yes or no), FSFI |
|
| Notes | The 302 women had a mean (SD) age of 61 (4) years Mean total FSFI improvement was similar between estradiol (5.4; 95% CI, 4.0 to 6.9) and placebo (4.5, 95% CI 2.8 to 6.1; P = 0.64), and between moisturizer (3.1, 95% CI 1.7 to 4.5) and placebo (P = 0.17) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratification through permuted blocks |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, study personnel, and clinicians were blinded to treatment assignments |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding, and unlikely that the blinding could have been broken |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data balanced across groups, and reasons similar |
| Selective reporting (reporting bias) | Low risk | Protocol is available |
| Other bias | Low risk | Study appears to be free of other sources of risk |
Modugno 2003.
| Study characteristics | ||
| Methods | RCT, multicentre, USA and Canada This trial is a subset of older postmenopausal women participating in the Multiple Outcomes of Raloxifene Evaluation study, a multi‐centre, randomized, double‐blind, placebo‐controlled trial. However, only English‐speaking participants at selected study sites in the USA and Canada were administered the sexual function questionnaire (n = 1218). |
|
| Participants | Inclusion: women aged 31–80 years, postmenopausal for at least 2 years, meet the WHO criteria for having osteoporosis, English as a native language, completing the sexual function questionnaire at both the baseline and the 36‐month follow‐up visits | |
| Interventions | Intervention 1: raloxifene 60 mg/d Intervention 2: raloxifene 120 mg/d Control: matching placebo |
|
| Outcomes | MSFQ Percentage of women with improved scores Data not suitable for meta‐analysis |
|
| Notes | Follow‐up: 36 months This work was supported by Eli Lilly and Company, maker of raloxifene. The company provided salary support to SE and research support to JAC, who is also a member of the speaker’s bureau of Eli Lilly and Company. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Block randomization by clinical site |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 7705 women were randomized in 25 countries, data of women from only 2 countries were included in this analysis (1218). Women with unsatisfactory questionnaire answers were excluded from analysis (275) |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Morais‐Socorro 2012.
| Study characteristics | ||
| Methods | RCT, single centre, Brazil | |
| Participants | Inclusion: aged 40‐55 years; menstrual irregularity during the previous 6 months but < 12 months of amenorrhoea; the presence of a uterus without anomalies in an initial vaginal ultrasonography evaluation and an endometrial thickness measurement ≤ 10 mm; plasma FSH level ≥ 30 mUI/mL; total cholesterol < 250 mg/dL; triglycerides ≤ 200 mg/dL; glycaemia ≤ 100 mg/dL; a Blatt‐Kupperman Menopausal Index score ≥ 14; mammography with BI‐RADS = 1 or 2 Exclusion criteria: current smoker; use of any hormonal, psychotropic or other medications that could interfere with the lipid glycaemic profile within 90 days of trial; history of clinical hepatic or kidney disease or diabetes mellitus; cerebrovascular, thyroid, CVD or thromboembolic disorders; any neoplastic disease; hypertensive disorder (systolic BP ≥ 160 mmHg and/or diastolic BP ≥ 105 mmHg); BMI > 30 kg/m²; and mammography with BI‐RADS = 3 or 4 |
|
| Interventions | Intervention: tibolone 2.5 mg/d (ReduClim®, Farmoquímica, Brazil) Control: placebo (identical capsules containing lactose) |
|
| Outcomes | Greene Climacteric Scale Final scores |
|
| Notes | Age: intervention (48.0 ± 3.6 years), control (49.0 ± 3.6 years) BMI: intervention (26.2 ± 0.6 kg/m²), control (26.0 ± 0.6 kg/m²) Follow‐up: 12 weeks Loss to follow‐up: 3/30 in the intervention group; 5/35 in the control group Reduclin 2.5 mg was donated by the laboratory Farmoquímica, Brazil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Use of placebo matching pills |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Balanced dropouts (3/30 in the intervention group; 5/35 in the control group) |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Nathorst‐Böös 1993.
| Study characteristics | ||
| Methods | RCT, parallel‐group, 15 centres in Sweden | |
| Participants | Inclusion: postmenopausal women aged 45‐65 years requiring HT for climacteric symptoms Exclusion: malignant tumours, surgical menopause, CVD or respiratory diseases, diabetes, psychiatric illness, endometriosis or vaginal bleeding |
|
| Interventions | Intervention: estradiol therapy (Estraderm 50 mcg/d) Control: matching placebo |
|
| Outcomes | MSFQ WHQ Change form baseline scores |
|
| Notes | Follow‐up: 12 weeks No conflict of interests disclosure |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described in detail |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts: 3/242; groups not specified |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Nielsen 2006.
| Study characteristics | ||
| Methods | RCT, multicentre, 2 centres, Denmark | |
| Participants | Inclusion: 40–65 years of age at baseline, were randomized if they were < 5 years past menopause at study entry. Menopause was defined as amenorrhoea > 12 months or > 6 months and a concomitant serum level of estradiol < 0.16 nmol/L and a FSH > 42 IU/L. All women who had undergone hysterectomy had menopause confirmed by measurement of serum estradiol and FSH at least 2 months before study entry. Women who had undergone surgical menopause (bilateral oophorectomy) could be included, if the operation was performed at least 6 weeks before study entry. Women who previously had received estrogen replacement therapy, had to go through a 6‐month wash‐out period before randomization. To be in good general health with no clinical or laboratory evidence of systemic disease or conditions with known influence on bone metabolism. Women had to be osteopenic (BMD T score < −1) Exclusions: women with nasal disease incompatible with nasal therapy such as frequent epistaxis, chronic rhinitis or sinusitis, severe allergic rhinitis, or frequent nasal treatment; women with contraindications for the use of HT. |
|
| Interventions | Wash out: 6 months Intervention: intranasal sprays estrogen (Aerodiol, France) 150 mcg/d (n = 114) or 300 mcg/d. Women with an intact uterus also received 200 mg of micronized progestogen (Effik, Spain), combined with the nasal spray for the last 14 days of each 28‐day cycle Control: matching placebo (n = 118) |
|
| Outcomes | WHQ Change from baseline scores |
|
| Notes | Age: mean 53 years BMI: mean 25.2 kg/m² 6.3% of participants did not have a uterus and therefore used only estrogen Follow‐up: 2 years The article does not report any conflict of interest disclosure Included women up to 5 years of amenorrhoea |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was performed according to the order of inclusion. Thus, the first participant received the lowest numbered therapeutic unit in the block of units supplied to the centre concerned |
| Allocation concealment (selection bias) | Low risk | The treatment allocation lists were drawn up and encoded by Servier Laboratoires |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 268 women from the 335 allocated completed the evaluation questionnaires |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Osmanagaoglu 2006.
| Study characteristics | ||
| Methods | RCT, single centre, Turkey | |
| Participants | Inclusion: postmenopausal women (amenorrhoea > 1 year, confirmed by FSH ≥ 30 IU/L), had not undergone any gynaecological operation, and no absolute contraindication for HT Exclusion: aged > 60 years, smokers, with diabetes, cancer, liver, renal or haematological, disease or other medical disorders or with a, history of sexual pain disorders or disharmony with their husbands |
|
| Interventions | Intervention 1: tibolone 2.5 mg (Livial, Organon) Intervention 2: estradiol valerate 2 mg + dienogest 2 mg (Climodien, Schering) Control: no intervention |
|
| Outcomes | Rosen’s FSFI Final scores |
|
| Notes | Age: intervention 1 (50 ± 1.87 years); intervention 2 (50 ± 2.20 years); control (51+1.94 years) BMI: intervention 1 (26 ± 0.84 kg/m²); intervention (25 ± 0.97 kg/m²); control (25 ± 0.97 kg/m²) Follow‐up: 6 months Report no conflict of interest and no external funding |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described in detail |
| Allocation concealment (selection bias) | Unclear risk | Not described in detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Although the authors claim study to be single‐blind, the study's limitations make it an open‐label design |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Few and balanced dropouts |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | High risk | The groups differed in baseline characteristics. The baseline sexual function score in tibolone (13.23 ± 6.63) group was higher than in control group (12.60 ± 3.58) and results were presented only as final score (not change from baseline) |
Seyyedi 2016.
| Study characteristics | ||
| Methods | RCT, single centre, Iran January 2013 to January 2014 |
|
| Participants | Inclusion: "lack of vaginal douching in the last 48 hours, refraining from using vaginal cream within the last week, 'lack of having luggage vaginal' within the last 24 hours, not having spotting, age between 50 and 65 years old, at least 12 months of amenorrhea and/or having FSH test more than 40 IU, normal Pap smear within the last 3 years, symptoms of vaginal atrophy, vaginal pH>5, having sexual activity, and naturally menopause women". Exclusion criteria: "dissatisfaction to participate in the study, prolapse grade 2 and more of bladder and uterus, surgery of anterior posterior repair (APR), history of sexual problems, chronic or systemic disease (e.g., diabetes, personal and family [first‐degree family] history of breast or endometrial cancer, history of endometriosis, personal and family [first‐degree family] history of thromboembolism, optic nerve disease, chronic liver disease, migraine, epilepsy and hereditary dyslipidemia), use of hormones, sensitivity to estrogenic compounds, allergy to honey and its products and divorced women, non‐normal TVS" | |
| Interventions | Intervention: vaginal estrogen 0.625 mg (Premarin, Aburaihan Pharmaceutical Company) Control: matching placebo (KY Jelly, Aburaihan Pharmaceutical Company) |
|
| Outcomes | MENQOL, sexual function domain score | |
| Notes | Age: intervention (49.44 ± 2.52 years), control (49.16 ± 3.8 years) BMI: intervention (26.97 ± 4.16 kg/m²), control (29.43 ± 3.95 kg/m²) Follow‐up: 12 weeks Do not report conflict of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation sequence: the women were randomly assigned in this clinical trial. The women were randomly distributed into three groups of 30 royal jelly vaginal cream 15%, vaginal Premarin, and placebo (lubricant), for three months |
| Allocation concealment (selection bias) | Low risk | To conceal allocation, all the tubes were prepared the same and were named A, B, C. Those who entered the study randomly received the creams. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinded, matching placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for missing data not related to outcome. Missing data balanced across groups, and reasons similar. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available but it is clear that all prespecified and expected outcomes of interest are reported |
| Other bias | Low risk | Study appears to be free of other sources of risk |
Simon 2007.
| Study characteristics | ||
| Methods | RCT, multicentre: 28 sites in USA and Canada | |
| Participants | Inclusion: healthy women aged ≥ 18 years who had undergone natural (amenorrhoea for ≥ 12 months) or surgical menopause (bilateral oophorectomy with or without hysterectomy ≥ 6 months before screening), who had serum E2 < 20 pg/mL, FSH > 40 mUI/mL, and BMI of 18‐35 kg/m² Exclusion: history of estrogen‐dependent neoplasia; endometrial hyperplasia; active hepatic, gallbladder, renal, or endocrine disease other than controlled thyroid abnormalities; or if they were receiving concomitant medications that could potentially interfere with hot flush frequency, severity, or their assessment |
|
| Interventions | Intervention 1: estradiol gel 0.87 g/d transdermal Intervention 2: estradiol gel 1.7 g/d transdermal Intervention 3: estradiol gel 2.6 g/d transdermal. This regimen was discontinued from further enrolment in the middle of the study because FDA advised so, in light of WHI results Control: placebo |
|
| Outcomes | Utian Quality of Life Change from baseline scores |
|
| Notes | Follow‐up: 12 weeks Age: intervention 1 (54.4 ± 6.3 years); intervention 2 (53.9 ± 6.2 years); intervention 3 (55.3 ± 8.5 years); control group (54.4 ± 5.8 years); range 28‐74 BMI: intervention 1 (26.4 ± 4.0 kg/m²); intervention 2 (26.2 ± 3.8 kg/m²); intervention 3 (26.6 ± 3.6 kg/m²); control (25.8 ± 3.8 kg/m²) As intervention 3 was considered unsafe in the middle of the study and is not used in clinical practice, we did not include this group in the analysis. For sexual function only data from intervention 2 (1.7 g/d) could be retrieved, data from intervention 1 (0.87 g/d) was omitted from the report. For vaginal maturation and pain outcomes, we combined data from intervention groups 1 and 2. This study was supported by a grant From BioSante Pharmaceuticals, Inc. (Lincolnshire, IL). Drs Bouchard, Simon, Waldbaum, and Utian have participated in clinical research as principal investigators for estradiol gel supported by BioSante Pharmaceuticals. They received payment under a research contract for the conduct of the study. Dr Simon was a consultant on this research and was paid by BioSante Pharmaceuticals. Ms Zborowski and Dr Snabes are paid independent consultants for BioSante Pharmaceuticals. Writing support was paid for by BioSante Pharmaceuticals. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization list |
| Allocation concealment (selection bias) | Unclear risk | Study co‐ordinators assigned treatment numbers to participants entering the 12‐week double‐blind treatment period |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, investigators, and outcome assessors were blinded to treatment assignment, and no unblinding occurred during the trial |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants, investigators, and outcome assessors were blinded to treatment assignment, and no blinding occurred during the trial |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The assessment of sexual function is only reported for the higher doses, 1.7 g/d and 2.6 g/d. The intervention group of 2.6 g/d discontinued enrolment in the middle of the study because of safety issues. The results for sexual function for the lower‐dose group "E2 gel 0.87 G/day" is omitted. |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
SMART‐3.
| Study characteristics | ||
| Methods | RCT, multi‐centre, 66 sites in USA | |
| Participants | Inclusion: "healthy women with an intact uterus, aged 40‐65 years, BMI ≤ 34.0 kg/m², postmenopausal ‐ defined as ≥ 12 months of spontaneous amenorrhoea or ≥ 6 months of spontaneous amenorrhoea with FSH > 40 mIU/mL. At screening, all women had to have a vaginal cytological smear showing ≤ 5% superficial cells and vaginal pH > 5 and had to identify on the symptom questionnaire at least 1 moderate‐severe vulvar/vaginal symptom that was most bothersome to them ‐ either vaginal dryness, irritation/itching, or pain with intercourse". Exclusion: "history of or clinically active medical disease such as endometrial hyperplasia; known or suspected estrogen dependent neoplasia; undiagnosed vaginal bleeding; chronic renal or hepatic disease; thrombophlebitis, thrombosis, or thromboembolic disorders; cerebrovascular accident; neuro‐ocular disorders; myocardial infarction or ischaemic heart disease; gallbladder disease; malignancy or treatment for malignancy within the previous 5 years (with the exception of carcinoma of the skin); or history of breast cancer, melanoma, or any gynaecologic cancer at any time. In addition, women with a transvaginal ultrasound screening that could not measure endometrial thickness or indicating double‐walled endometrial thickness > 4 mm, focal endometrial abnormality (other than fluid), complex ovarian cyst of any diameter, or simple ovarian cyst > 20 mm were excluded. Women who were hypersensitive to estrogen, had an active endocrine disease, had a known alcohol or drug abuse, were heavy smokers (> 15 cigarettes/d), had unresolved or abnormal cervical cytologic smear reports, had unresolved findings suspicious for malignancy on breast examination, and had uncontrolled hypertension were also excluded. All women should have had a normal endometrial biopsy at baseline." |
|
| Interventions | Wash out: "use of oral estrogen‐, progestin‐, androgen‐, or SERM‐containing drugs, transdermal hormone products, or intrauterine progestins within 8 weeks before screening; vaginal hormone products within 4 weeks; progestin implants/injectables or estrogen pellets/injectables within 6 months; intrauterine device within 12 weeks; or any investigational drug within 60 days" as these conditions may interfere with the basal dosage of endogenous hormones." Intervention 1: bazedoxifene 20 mg + conjugated estrogens 0.45 mg daily Intervention 2: bazedoxifene 20 mg + conjugated estrogens 0.625 mg Intervention 3: bazedoxifene 20 mg Control: placebo |
|
| Outcomes | Arizona Sexual Experiences (ASEX) scale domains and MENQOL | |
| Notes | Follow‐up: 12 weeks Mean age in each group: 56.4 (± 4.7); 56.3 (± 4.4); 56.4 (± 4.5); 56.1 (± 4.2) BMI: intervention 1 (25.4 ± 3.8); 2 (25.2 ± 3.8); 3 (25.3 ± 3.9); and placebo (25.7 ± 4.1) We merged intervention groups 1 and 2 for analysis and calculated SDs from the standard errors using the calculator in RevMan. Wyeth Research, Collegeville, PA, sponsored the study and supported the medical writing assistance of Kathleen Ohleth PhD, and Chastity Bradley PhD. "G Bachmann has served as a Research Consultant‐PI for Wyeth, Bayer, GlaxoSmithKline, Duramed, Novartis, Pfizer, Boehringer‐Ingelheim, Johnson & Johnson, Roche, Boston Scientific, Novo Nordisk, Procter & Gamble, Merck, Xanodyne, Hormos, and Femme Pharma. J Bobula and S Mirkin are current employees of Wyeth. Dr Risa Kagan received research grants from Proctor & Gamble, Lilly, Boehringer Ingelheim, Depomed, and Wyeth. Dr Kagan is a consultant for Proctor & Gamble, Lilly, Medtronic, and Wyeth and is a speaker for GlaxoSmithKline, Roche, Novogyne, Novartis, and Lilly. Dr Williams received research grants from Wyeth, Xanodyne, and Organon and is also a speaker for Wyeth. Drs Mirkin and Pickar and Kaijie Pan are full‐time employees of Wyeth Research, Collegeville, PA." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerized randomization/enrolment system generated by Wyeth Research |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinded, matching placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is not clear how many women in fact answered the final questionnaires, and if the women who withdrew from treatment had the final evaluation |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Speroff 2003.
| Study characteristics | ||
| Methods | RCT, multicentre, 35 sites in USA | |
| Participants | Inclusion: postmenopausal woman, with or without a uterus, with at least 7 moderate‐severe hot flushes per day or an average of at least 56 moderate‐severe vasomotor symptoms per week for the 2 weeks before randomization. In addition, a woman with a uterus was required to have had amenorrhoea > 12 months before randomization; if amenorrhoea < 12 months and > 6 months, she was also required to have a FSH > 40 IU and an E2 < 20 pg/mL. A woman was also eligible if she had a hysterectomy and bilateral oophorectomy performed 6 weeks before randomization. Finally, a woman who had a hysterectomy without bilateral oophorectomy was eligible if she had FSH > 40 IU and an E2 < 20 pg/mL. Exclusion: past or current thromboembolic disorder, or cerebrovascular accident; endometriosis; allergy or intolerance to previous estrogen therapy only or HT, including disabling breakthrough bleeding; past or current estrogen‐dependent neoplasia; abnormal uninvestigated vaginal bleeding within 6 months of randomization; and known or suspected pregnancy. Previous treatment with any of the following was also reason for exclusion: estrogen, progestogen, androgen, or systemic corticosteroids by the oral route within 8 weeks of screening, by transdermal or buccal delivery within 4 weeks of screening, or by injection within 6 months of screening; hormone pellets or implants inserted within the previous 5 years or an implant removed within the past 3 months; unopposed estrogen therapy only for ≥ 6 months in women with an intact uterus; or selective estrogen receptor modulators within 8 weeks of screening. |
|
| Interventions | Intervention: vaginal ring (Femring, UK) delivering estradiol 50 mcg/d (n = 113) or 100 mcg/d (n = 112). The ring contains E2 acetate in a reservoir system within the ring polymer, which is released steadily over 3 months Control: matching placebo (n = 108) |
|
| Outcomes | Greene Climacteric Scale Change from baseline scores |
|
| Notes | Follow‐up: 13 weeks Mean age: 51.7 (± 7.2) years BMI 28 kg/m² SD calculated from P values of the "changes from baseline" values between the groups There were no differences on 'vaginal dryness' and 'urinary leakage' between groups, but there were not sufficient details to pool data. Not enough data to pool the outcome 'vaginal maturation'; the study authors claim it was significantly improved with the treatment. This study was supported by Warner Chilcott, a division of Galen Holdings PLC, which has developed this product. Research support was provided for costs of the study. Study authors have received speaking and consulting honoraria from the company. Dr Speroff owns stock in the company. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated schedule |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind, matching placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Few and balanced dropouts |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Strickler 2000.
| Study characteristics | ||
| Methods | RCT, multicentre (USA), 32 sites | |
| Participants | Inclusion: 47‐60 years, 2‐8 years after final menstrual period, serum E2 < 73 pmol/L (< 20 pg/mL), and lumbar spine bone mineral density 2‐2.5 SD, the mean peak lumbar spine bone mineral density of premenopausal women. Exclusion: intolerable menopausal symptoms requiring therapy; uterine bleeding of unknown cause; BMI < 18 kg/m² or > 31 kg/m², history of deep venous thromboembolic disease; use of corticosteroids, estrogen, or progestogen within 6 months before beginning the study; and chronic illness |
|
| Interventions | Washout: 6 months (because of the influence of estrogen on some subscales of WHQ assessing physical capacity that indirectly is related to bone health status) Intervention 1: CEE 0.625 mg/d Intervention 2: raloxifene 60 mg/d (n = 97) or 150 mg/d (n = 100) Control: placebo |
|
| Outcomes | WHQ Change from baseline scores |
|
| Notes | Age: 54.7 ± 3.6 years BMI: intervention groups 25.9 ± 3.3kg/m², 25.5 ± 3.5kg/m², 25.4 ± 3.4kg/m²; control group 25.5 ± 3.5kg/m² Follow‐up: 12 months SD calculated from P values Sponsored study: the research was supported by Eli Lilly and Company, maker of raloxifene. Doctors Shen, Wong, and Silfen are employees of and hold stock in Eli Lilly and Company. Doctors Strickler, Stovall, and Merritt have received honoraria for their services to Eli Lilly and Company. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were assigned randomly in blocks of four to 1 of 4 therapy groups |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind, placebo was similar to the drug |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT approach on data from women who had at least 1 follow‐up visit after randomization. Missing values were replaced with values from a previous post‐randomization visit (last observation carried forward) |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
Taylor 2017.
| Study characteristics | ||
| Methods | RCT, double‐blinded, placebo‐controlled | |
| Participants | Inclusion: "women between 42 and 58 years of age and at least 6 months and no more than 36
months from last menstrual period, with plasma follicle stimulating hormone level at least 35 mIU/mL (to convert to IU per liter, multiply by 1.0) and/or E2 levels less than 40 pg/mL". Exclusion: use of HT or supplement, endometrial thickness > 5 mm, current smoking > 10 cigarettes/d, bone mass index > 35 kg/m2, history of clinical CVD, history of cerebrovascular and/or thromboembolic disease, coronary calcium score ≥ 50 units, dyslipidemia‐LDL cholesterol > 190 mg/dL, hypertriglyceridemia‐triglycerides > 400 mg/dL, lipid‐lowering medication, nut allergy, uncontrolled hypertension‐systolic, hysterectomy, history of, or prevalent, chronic diseases including any cancer (other than basal cell skin cancers), renal failure, cirrhosis, diabetes mellitus, and endocrinopathies other than adequately treated thyroid disease, known HIV infection and/or medications for HIV infection results of any safety laboratory test chemistries, inclusion criteria 20% abnormal |
|
| Interventions | 727 participants enroled in the parent trial; of these 670 agreed to participate in the sexual function ancillary study (n = 209 in the o‐CEE group, n = 204 in the t‐E2 group, and n = 257 in the placebo group). Intervention: "oral o‐CEE, 0.45 mg/d and placebo patches with micronized progesterone, 200 mg, for 12 days each month; t‐E2, 50 μg/d, and placebo pills with micronized progesterone, 200 mg, for 12 days each month”. |
|
| Outcomes | Primary: rate of change of carotid intimal medial thickness by ultrasound. Secondary: change in coronary calcium score by X‐ray tomography, plasma lipid profiles, blood clotting factors, serum inflammatory factors, hormone levels, cognitive and affective scores on standard psychometric tests, and QoL FSFI |
|
| Notes | ClinicalTrials.gov Identifier: NCT00154180 We failed to obtain data from 12 weeks of follow‐up |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Low risk | Hidden allocation sequence |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding, and unlikely that the blinding could have been broken |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | There is no suspicion that the blinding has been broken |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data balanced across groups, and reasons similar |
| Selective reporting (reporting bias) | Low risk | Protocol is available |
| Other bias | Low risk | Study appears to be free of other sources of risk |
Veerus 2006.
| Study characteristics | ||
| Methods | RCT, parallel‐group, 3 clinical centres in Estonia 1001 women randomized January 1999‐December 2001 |
|
| Participants | Inclusion: aged 50–64 years, postmenopausal Exclusion: none Potentially eligible women were randomized into 4 trial groups:
|
|
| Interventions | Intervention: CEE 0.625 mg + MPA 5.0 mg daily (2 groups: open and blind) Control: matching placebo in the blind arm and no intervention in the open arm |
|
| Outcomes | WHQ Percentage of women satisfied and who lost interest in sex |
|
| Notes | Follow‐up: 1 year for the included evaluation (3.6 years total) Trial register: ISRCTN35338757 Potentially eligible women were randomized into 4 trial groups resulting in two substudies
1001 women were recruited into the non‐blind subtrial and 777 in the blind subtrial. The Estonian Postmenopausal Hormone Therapy trial was originally planned to be a part of the Women’s International Study of Long Duration Oestrogen After Menopause (WISDOM) The study was financially supported by grants from the Academy of Finland (grants 69838, 201490, 115088), STAKES (National Research and Development Centre for Welfare and Health), Finland, and the Estonian Ministry of Education and Research Drugs were donated by Wyeth Ayerst Company via the Women's International Study of Long Duration Oestrogen After Menopause (WISDOM) in the UK |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization in permuted blocks, each of 16 and each block of the 3 clinics separately, at the National Research and Development Centre for Welfare and Health in Finland |
| Allocation concealment (selection bias) | Low risk | The treatment allocation was enclosed in a non‐transparent sealed envelope and sent to trial clinics |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open study compared with no treatment |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Balanced dropouts Blind trial ‐ intervention 98/404; control 101/372 Open trial ‐ intervention 130/494; control 125/507 |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | Not suspected |
WHI 1999.
| Study characteristics | ||
| Methods | RCT, multicentre (40 clinical centres), USA | |
| Participants | Inclusion criteria: women aged 50‐79 years with either an intact uterus or with hysterectomy 3 months earlier (with or without oophorectomy), and were likely to reside in the area for 3 years. Exclusion criteria: medical condition predicted survival of < 3 years or if there were diagnoses of previous breast cancer or melanoma, other cancer within the past 10 years (except non‐melanoma skin cancer), low haematocrit or platelet counts, or any condition that would interfere with acceptable adherence and retention (e.g. alcoholism or dementia). Failing the 4‐week compliance schedule of placebo pill taking. Potential participants who were using postmenopausal hormones at the initial screening visit were required to undergo a 3‐month 'washout' period before enrolment. Women who reported moderate or severe menopausal symptoms during the washout period were discouraged from participating in the study but were not excluded. |
|
| Interventions | Intervention 1: CEE 0.625 mg, (Premarin; Wyeth, St Davids, Pa) orally, daily Intervention 2: CEE 0.625 mg + MPA 2.5 mg (Prempro, Wyeth) Control: matching placebo pills |
|
| Outcomes | Modified Mini‐Mental State Examination (QoL): sexual satisfaction (range from 1/worst to 4/best) Change from baseline scores |
|
| Notes | Part of WHI study; included data from 1‐year follow‐up period Intervention: 5310 women allocated Control: 5429 women allocated Funding: WHI is funded by the National Heart, Lung, and Blood Institute, US Department of Health and Human Services, National Institutes of Health (NIH), Bethesda, MD, USA. Drs Shumaker and LaCroix report having served as paid consultants to Pfizer. Dr Shumaker reports having served as a paid lecturer for Wyeth–Ayerst and Pfizer. Drs Hays, Brunner, and Shumaker report having received grant support from Wyeth–Ayerst. Dr Shumaker reports having received grant support from Pfizer. Dr Brzyski reports having received grant support from Berlex. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomized permuted block algorithm, stratified by clinical centre site and age group |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. All study medication bottles had a unique bottle number and bar code to allow for blinded dispensing |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | About half of the allocated participants were evaluated for sexual function |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | None |
Wiklund 1993.
| Study characteristics | ||
| Methods | RCT, multicentre, 15 sites, Sweden | |
| Participants | Inclusion: postmenopausal women between 45 and 65 years old requiring hormone replacement therapy for climacteric symptoms, amenorrhoea > 6 months, no hormone replacement therapy within the last 6 months. Exclusion: surgically induced menopause, previous or current estrogen‐dependent tumours, other current malignant or life‐threatening disease, severe metabolic, endocrine, or gastrointestinal disease, concomitant heart disease, insulin‐treated diabetes, uncontrolled hypertension, endometriosis, undiagnosed vaginal bleeding, active skin disease, and unstable medical conditions such as rheumatoid arthritis or chronic obstructive lung disease. Women with psychiatric disorders and/or those receiving continuous tranquillizer or antidepressant therapy. |
|
| Interventions | Washout: 6 months Intervention: transdermal estradiol therapy, 50mcg/24 hours, changed twice a week Control: matching placebo |
|
| Outcomes | Simplified McCoy Sex Scale ('sexual problems' was included as 'dyspareunia', because it refers to the question 'do you currently experience any pain during intercourse?') Change from baseline |
|
| Notes | Follow‐up: 12 weeks Mean age: intervention = 52.4 (±4.3) years; control = 52.9 (±4.0) years Do not report conflict of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind, matching placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Described in details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts: intervention (5), control (10) |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Unclear risk | The article does not report any conflict of interest disclosure |
WISDOM 2008.
| Study characteristics | ||
| Methods | RCT, multi‐centre (499 general practices): UK, Australia, New Zealand (WISDOM trial) | |
| Participants | Inclusion: postmenopausal women aged 50‐69 years at randomization were eligible for the trial. Postmenopausal was defined as no menstrual period in the last 12 months or having had a hysterectomy. Women who had started taking HT before their menstrual periods had stopped were considered eligible when they had been taking HT for 12 months. Exclusion "
|
|
| Interventions | Intervention: oral CEE 0.625 mg daily, plus oral MPA 2.5/5.0 mg daily (Prempro, Wyeth Ayerst, USA) Control: matching placebo |
|
| Outcomes | WHQ Final scores |
|
| Notes | Follow‐up: 1 year Mean age at randomization: 63.8 years Drugs were donated by Wyeth Ayerst Company |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐based, stratified block randomization program |
| Allocation concealment (selection bias) | Low risk | Randomized centrally and appropriate medication dispatched to the practice |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No‐one involved with assessment of outcomes was aware of treatment assignment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Sexual function was evaluated in only 588/1043 participants in the intervention group and in only 569/1087 participants in the control group |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Low risk | None |
Yang 2004.
| Study characteristics | ||
| Methods | RCT, single centre, Taiwan | |
| Participants | Inclusion: postmenopausal women with intact uterus and natural menopause of at least 6 months’ duration, FSH > 18 mIU/L, and estradiol level < 30 pg/mL Exclusion: history of liver disease, breast cancer, endometrial cancer, thrombophlebitis, thromboembolic disorders related to estrogen use, myocardial infarction or ischaemic heart disease, chronic renal disease, cerebrovascular accident, uncontrolled hypertension, diabetes or metabolic bone disease, or had received any hormone treatment within 1 year previously, chronic use of steroids, fluoride, Vitamin D, rifampin, barbiturates, sulfenamide, and herbal medications, or the use of estrogen and progestogen other than the study medications. |
|
| Interventions | Intervention: CEE 0.625 mg + MPA 2.5 mg orally daily for 5.5 months Control: matching placebo |
|
| Outcomes | Greene Climacteric Scale Change from baseline |
|
| Notes | Follow‐up: 5.5 months Age: intervention (53.2 ± 3.1 years); control (53.3 ± 3.4 years) Weight: intervention (56.0 ± 8.3 kg); control (55.7 ± 6.6 kg) Do not report conflict of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported in detail |
| Allocation concealment (selection bias) | Unclear risk | Not reported in detail |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | High rates, but balanced, dropouts: intervention (6/33); control (8/33) |
| Selective reporting (reporting bias) | Low risk | Not suspected |
| Other bias | Unclear risk | We observed relevant difference between intervention and control groups at baseline (0.6 ± 0.8 vs 1.0 ± 0.9, intervention vs control respectively). However, we were able to analyse data as change from baseline. There is no conflict of interest disclosure. |
AE: adverse effect; BISF‐W: Brief Index of Sexual Functioning‐Women; BMI: body mass index; BP: blood pressure; CE: conjugated estrogen; CEE: conjugated equine estrogen; CVD: cardiovascular disease; DHEA: dehydroepiandrosterone; FDA: Food and Drug Administration; FSFI: Female Sexual Function Index; FSH: follicle stimulating hormone; GAD‐7: Generalised Anxiety Disorder Assessment; GRISS: Golombok‐Rust Inventory of Sexual Satisfaction; HT: hormone therapy; ITT: intention‐to‐treat; IUD: intrauterine device; LDL: low‐density lipoprotein; MBS: most bothersome symptom; MENQOL: Menopause‐specific Quality of Life; MFSQ: McCoy Female Sexuality Questionnaire; MOS: Medical Outcomes Study; MPA: medroxyprogesterone acetate; NIH: National Institutes of Health; PHQ: Patient Health Questionnaire; QoL: quality of life; RCT: randomized controlled trial; SD: standard deviation; SERM: selective oestrogen receptor modulator; SSA‐P: Subjective Symptoms Assessment Profile; SUI: stress urinary incontinence; TVUS: transvaginal ultrasound; VSI: Vaginal Symptom Index; WHI: Women's Health Initiative; WHO: World Health Organization; WHQ: Women's Health Questionnaire
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| 2010‐024603‐26 | Did not evaluate sexual function |
| 2014‐000179‐18 | Did not evaluate sexual function |
| Abedi 2018 | Did not use HT |
| Abedi 2020 | Did not use HT |
| Abraham 2014 | Did not evaluate sexual function |
| Adler 2005 | Not randomized |
| Almeida 2006 | Did not evaluate sexual function |
| Aptecar 2021 | Did not evaluate sexual function by a validated tool |
| Archer 2011 | Did not evaluate sexual function |
| Argyroudis 1997 | Not randomized |
| Arêas 2019 | Did not use HT |
| Bachmann 2008 | Did not evaluate sexual function |
| Bachmann 2009 | Did not evaluate sexual function |
| Bachmann 2010 | Did not evaluate sexual function |
| Bachmann 2011 | Did not evaluate sexual function with a validated instrument |
| Barnabei 2002 | Did not evaluate sexual function |
| Bennink 2016 | Did not evaluate sexual function |
| Bianchi‐Ferraro 2022 | Had another intervention for a comparator |
| Binder 2001 | Did not evaluate sexual function |
| Blumel 2008 | Addition of testosterone to estrogen/progesterone in the study group |
| Bosak 2022 | Did not evaluate sexual function |
| Bride 2014 | Did not evaluate sexual function |
| Bruno 2012 | Pseudo‐randomized |
| Cano 2012 | Did not evaluate sexual function |
| Cardozo 2001 | Did not evaluate sexual function |
| Casper 1999 | Did not evaluate sexual function |
| Castelo‐Branco 2000 | Pseudo‐randomized |
| Cayan 2008 | Pseudo‐randomized |
| Ceausu 2011 | Did not evaluate sexual function |
| Concepcion 2011 | Did not evaluate sexual function |
| Cruz 2018 | Comparator is another intervention (does not use placebo or no intervention) |
| Dalil 2020 | Did not use HT |
| Daneshmand 2015 | Did not evaluate sexual function |
| Dennerstein 1980 | Did not evaluate sexual function |
| Dessole 2004 | Did not evaluate sexual function |
| Diem 2006 | Did not evaluate sexual function |
| Ditkoff 1991 | Did not evaluate sexual function |
| DRKS00006888 | Did not evaluate sexual function |
| Duka 2000 | Did not evaluate sexual function |
| Eftekhar 2009 | Not randomized, compares before and after treatment |
| Eftekhar 2020 | Control group used Premarin |
| Eriksen 1992 | Did not evaluate sexual function |
| Eriksen 1999 | Did not evaluate sexual function |
| Fabian 2019 | Did not evaluate sexual function |
| Fernandes 2014 | Comparator is another intervention (does not use placebo or no intervention) |
| Freedman 2009 | Did not evaluate sexual function |
| Galesanu 2010 | Did not evaluate sexual function |
| Galhardo 2006 | Did not evaluate sexual function by a validated questionnaire |
| Garcia de Arriba 2022 | Did not evaluate sexual function |
| Gaspard 2021 | Did not evaluate sexual function |
| Gonenne 2006 | Did not evaluate sexual function |
| Gorenstein 2011 | Did not evaluate sexual function |
| Griesser 2012 | Did not evaluate sexual function |
| Guan 2010 | Did not evaluate sexual function |
| Hachul 2008 | Did not evaluate sexual function |
| Harman 2014 | Did not evaluate sexual function |
| Hedrick 2009 | Did not evaluate sexual function |
| Hendrix 2005 | Did not evaluate sexual function |
| Hodis 2001 | Did not evaluate sexual function |
| Hofling 2005 | Did not evaluate sexual function |
| IRCT138809032766N1 | Did not evaluate sexual function |
| IRCT2017050433817N1 | Did not evaluate sexual function |
| Islam 2021 | Were not or pseudo‐randomized |
| ISRCTN46661996 | Did not evaluate sexual function |
| Jensen 1983 | Did not evaluate sexual function |
| Ju 2021 | Were not or pseudo‐randomized |
| Kagan 2014 | Did not evaluate sexual function |
| Kenny 2005 | Did not evaluate sexual function |
| Kessel 2003 | No group without HT |
| Kimura 1995 | Not randomized |
| Kingsberg 2017 | Did not evaluate sexual function |
| Kocoska‐Maras 2011 | Did not evaluate sexual function |
| Kornafel 1992 | Did not evaluate sexual function |
| Kroll 2018 | Did not evaluate sexual function |
| Krychman 2016 | Did not evaluate sexual function |
| Kumru 2008 | Did not evaluate sexual function |
| L'Hermite 2022 | Did not evaluate sexual function |
| Lin 2011 | Did not evaluate sexual function |
| Lindsay 2002 | Did not evaluate sexual function |
| Liu 2012 | Did not evaluate sexual function |
| Lobo 2009 | No group without HT |
| Lobo 2017 | Did not evaluate sexual function |
| MacDonald 1994 | Did not evaluate sexual function |
| Marschalek 2022 | Were a different population |
| Marsden 2000 | Did not evaluate sexual function |
| Marx 2004 | Did not evaluate sexual function |
| Miller 2019 | Did not evaluate sexual function |
| Mittal 2020 | Did not evaluate sexual function by a validated tool |
| Mizunuma 2011 | Did not evaluate sexual function |
| Naessen 2001 | Did not evaluate sexual function |
| NCT01543399 | Did not evaluate sexual function |
| NCT01585558 | Did not evaluate sexual function |
| NCT01779947 | Did not evaluate sexual function |
| NCT01822288 | It is not a randomized controlled study (RCT) |
| NCT02253173 | Did not evaluate sexual function |
| NCT02638337 | Did not evaluate sexual function |
| NCT03018106 | Not randomized |
| Nevinny‐Stickel 1983 | Did not evaluate sexual function by a validated questionnaire |
| Nieto 2011 | Did not evaluate sexual function |
| Noguchi 2018 | Did not evaluate sexual function |
| Notelovitz 2000 | Did not evaluate sexual function |
| Obel 1993 | Did not evaluate sexual function |
| Palacios 1995 | Control group used a different intervention, did not use a validated questionnaire |
| Palacios 2005 | Did not evaluate sexual function |
| Paraiso 2020 | Did not evaluate sexual function |
| Pinkerton 2014 | No positive response after contacting the authors |
| Poetry 2011 | Did not evaluate sexual function |
| Polo‐Kantola 1998 | Did not evaluate sexual function |
| Portman 2013 | Did not evaluate sexual function |
| Portman 2014a | Did not evaluate sexual function |
| Pradeep 2016 | Did not evaluate sexual function |
| Prestwood 2003 | Did not evaluate sexual function |
| Raz 2014 | Without HT |
| RBR‐94dx93/1 | Without HT |
| Rebar 2000 | A questionnaire that includes assessment of sexual function is applied; however, the study authors do not report the results for the sexual domains |
| Reindollar 2002 | Did not evaluate sexual function |
| Ribom 2011 | Did not evaluate sexual function |
| Rigano 2001 | Did not evaluate sexual function by a validated questionnaire |
| Russu 2011 | Did not evaluate sexual function |
| Saeideh 2010 | Did not evaluate sexual function by a validated questionnaire |
| Saletu 2002 | Did not evaluate sexual function |
| Samaras 1999 | Did not evaluate sexual function by a validated questionnaire |
| Santofimia 2022 | Did not evaluate sexual function |
| Santoro 2012 | Did not evaluate sexual function |
| Serebani 2020 | Did not use HT |
| Shah 2006 | Did not evaluate sexual function |
| Sherman 2003 | Did not evaluate sexual function |
| Shulman 2002 | Did not evaluate sexual function |
| Silverman 2012 | Did not evaluate sexual function |
| Simon 1999 | Did not evaluate sexual function |
| Simon 2008a | Did not evaluate sexual function |
| Simon 2008b | Did not evaluate sexual function |
| Simon 2012 | Did not evaluate sexual function |
| Simunic 2003 | Did not evaluate sexual function |
| SMART‐5 | Did not evaluate sexual function |
| Sorensen 2001 | Did not evaluate sexual function |
| Speroff 2006 | Did not evaluate sexual function |
| Stening 2011 | Did not evaluate sexual function |
| Stevenson 2010 | Did not evaluate sexual function |
| Sun 2016 | Did not evaluate sexual function |
| Swanson 2006 | Did not evaluate sexual function |
| Tansupswatdikul 2012 | Dis not evaluate sexual function |
| Tinelli 2002 | Did not evaluate sexual function by a validated questionnaire |
| Tungmunsakulchai 2015 | Control group included an intervention (not or pseudo‐randomized) |
| Tuomikoski 2010 | Did not evaluate sexual function |
| Usall 2011 | Did not evaluate sexual function |
| Utian 2001 | Did not evaluate sexual function |
| Utian 2004 | Did not evaluate sexual function |
| Vardy 2003 | Did not evaluate sexual function |
| Veldhuis 2011a | Did not evaluate sexual function |
| Veldhuis 2011b | Did not evaluate sexual function |
| Vestergaard 2003 | Did not evaluate sexual function |
| Voipio 2002 | Did not evaluate sexual function |
| Warton 2014 | No response to author contact |
| Wolff 1982 | Did not evaluate sexual function |
| Woo 2003 | Did not evaluate sexual function |
| Yeo 2020 | Did not use HT |
| Zervoudis 2009 | Did not evaluate sexual function |
| Zhou 2011 | Did not evaluate sexual function |
| Zullo 2005 | Did not evaluate sexual function |
HT: hormone therapy
Characteristics of studies awaiting classification [ordered by study ID]
Hirschberg 2020.
| Methods | Randomized, double‐blind, placebo‐controlled, international, multicenter study |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Intervention: 0.005% estriol vaginal gel Control: placebo (moisturizing gel) |
| Outcomes | FSFI score |
| Notes | The study authors do not report how study was funded |
NCT01845649.
| Methods | RCT, multicentre in 57 locations, USA |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Estradiol vaginal cream applied daily for 14 days followed by dosing 3 times per week for 10 weeks |
| Outcomes | Self‐assessment of the symptoms of VVA, other than dyspareunia and vaginal bleeding associated with sexual activity |
| Notes | Last ipdate posted date: 9 May 2022 |
NCT02460302.
| Methods | RCT, single centre, Mount Sinai Hospital, Toronto, Canada |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Micronized vaginal progesterone 100 mg inserted vaginally, or placebo suppository inserted vaginally |
| Outcomes | Improvement in patient‐identified most bothersome symptom (vaginal dryness, itching, soreness, pain with sexual activity) |
| Notes | Study in progress |
NCT02834312.
| Methods | RCT, single centre, Belgium |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | 2.5 mg, or 5 mg, 10 mg, or 15 mg of oral estetrol |
| Outcomes | Change in the genitourinary symptoms (GSM) of menopause (time frame: from baseline to week 12): vaginal pain associated with sexual activity (none, mild, moderate or severe); vaginal bleeding associated with sexual activity (presence vs absence) |
| Notes | Study in progress |
NCT03363997.
| Methods | RCT, single centre, Campinas, SP, Brazil |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Estriol (100 mg (Test 1), 300 mg (Test 2) or 600 mg (Test 3) with continuous delivery (0.125, 0.250 or 0.500 mg/day) for 21 days. And also, characterized its safety and tolerability |
| Outcomes | Number of adverse events, in each treatment group, including clinically relevant alterations of vital signs and laboratory tests results |
| Notes | Study in progress |
Pinkerton 2017.
| Methods | RCT, multicentre, USA and Canada |
| Participants | Inclusion criteria
|
| Interventions | Intervention: conjugated estrogen (CE)/bazedoxifene (BZA) (CE 0.45 or 0.625 mg with BZA 10, 20, or 40 mg), raloxifene 60 mg Control: placebo |
| Outcomes | Sexual activity and health‐related QoL |
| Notes | Pending other possible secondary results derived from the study |
Tanmahasamut 2020.
| Methods | Double‐blind RCT |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Intervention group
Control group
|
| Outcomes | FSFI score |
| Notes | This study was registered with the Thai Clinical Trials Registry (registration number 20170322001). All study authors declare no financial support from the companies that produce and/or distribute the drugs, devices or materials described in this report. |
BMI: body mass index; BP: blood pressure; CNS: central nervous system; CVD: cardiovascular disease; ECG: electrocardiogram; FSFI: Female Sexual Function Index; FSH: follicle stimulating hormone; HT: hormone therapy; LDL: low‐density lipoprotein; QoL: quality of life; RCT: randomized controlled trial; VVA: vulvovaginal atrophy
Characteristics of ongoing studies [ordered by study ID]
NCT02668796.
| Study name | To study generic estradiol 10 mcg vaginal tablets in the treatment of vulvar and vaginal atrophy in post menopausal women |
| Methods | RCT |
| Participants | Postmenopausal women aged > 30 to < 75 years |
| Interventions | Experimental: estradiol vaginal tablets 10 mcg (Glenmark) apply using the given applicator Active comparator: Vagifem® (estradiol vaginal tablets) 10 mcg (Novo Nordisk) apply using the given applicator |
| Outcomes | Primary: the proportion of participants with at least 25% reduction from baseline in the sum of % basal/parabasal + % intermediate cells on vaginal cytology and vaginal pH < 5.0 with a change from baseline vaginal pH of at least 0.5 (time frame: day 15) Secondary: the proportion of participants with treatment success at the end of study where treatment success is defined as a women who achieves a score of 0 (none) or 1 (mild) at visit 3/end of study for the MBS (time frame: day 15] |
| Starting date | January 2016 |
| Contact information | |
| Notes | NCT02668796 |
NCT02670785.
| Study name | A safety and efficacy study of estradiol vaginal capsule in postmenopausal women with vulvovaginal atrophy |
| Methods | RCT |
| Participants | Clinical diagnosis of vulvovaginal atrophy due to post menopause; age ≥ 40 years or if bilateral oophorectomy ≥ 35 years; moderate‐severe vaginal dryness; normal breast exam; if > 40 years; vaginal pH > 5.0 < 5% superficial cells on vaginal wall cytology smear |
| Interventions | Estradiol vaginal: capsule 0.003 mg, capsule 0.01 mg, and capsule 0.02 mg |
| Outcomes | Primary: change in the percentage of vaginal superficial cells Secondary:
|
| Starting date | 15 February 2016 |
| Contact information | |
| Notes | NCT02670785 |
NCT02859285.
| Study name | The impact of hormone therapy on lower urinary tract symptoms, sexual function and psychosomatic disorder |
| Methods | RCT |
| Participants | Women aged 40‐70 years, with intact uterus seeking medical treatment for menopausal syndrome |
| Interventions | Tibolone (2.5 mg/d) for 12 consecutive weeks |
| Outcomes | Primary: menopausal symptoms Secondary: sexual function, sexual function, psychosomatic symptoms. |
| Starting date | 16 November 2012 |
| Contact information | |
| Notes | NCT01822288 |
NCT03116022.
| Study name | Use of estriol at distal third of vagina improving coital pain in post‐menopause women |
| Methods | RCT |
| Participants | Sexually active postmenopausal women of any age with complaint of vulvar and/or vaginal atrophy who also complain of bothersome decreased libido, and/or arousal, and/or orgasmic dysfunction |
| Interventions | Experimental: distal estriol group (DEG). This arm is composed of women using estriol 1 mg/1g in the distal third of the vagina every other night. Active comparator: proximal estriol group (PEG). This arm is composed of women using estriol 1 mg/1g in the proximal third of vagina every other night. |
| Outcomes | Primary: number of women with lower score of pain assessed by the McGill Pain Questionnaire.
Secondary:
|
| Starting date | 1 June 2017 |
| Contact information | |
| Notes | NCT03116022 |
BMI: body mass index; FSH: follicle stimulating hormone; MBS: most bothersome symptoms; RCT: randomized controlled trial
Differences between protocol and review
The previous review version included several changes from the planned protocol.
Primary outcome: we kept the composite score as the primary outcome to assess the global effect on sexual function. As secondary outcomes, we evaluated the individual domains of sexual function.
Secondary outcomes: we previously planned to evaluate the genitourinary system, quality of life, depression, and body mass index. However, evidence for the planned secondary outcomes would just be a subset of the overall body of evidence because the present review only includes studies that reported sexual function. In this way, we evaluate the domains of sexual function (desire, arousal, lubrication, orgasm, satisfaction, and pain).
Structure of data synthesis: we did not plan stratification of data, however, the results were confusing and we therefore stratified by participant characteristics.
We performed sensitivity analysis only by excluding studies with a high risk of bias. We were not able to perform sensitivity analysis using alternative imputation strategies as initially planned.
We have added two summary of findings tables to present the results.
There were not enough studies to perform all planned subgroup analyses by the type of menopause and sexual symptom status at baseline.
At the 2022 update we made the following changes:
In the previous version, all definitions of female sexual function were established based on Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM‐IV), and we used the North American Menopause Society (NAMS)‐2012 guideline to support hormone therapy definitions. We have updated the current review according to DSM‐V and International Classification of Disease (ICD)‐11 criteria for female sexual dysfunction diagnosis. From the six domains of sexual function (desire; arousal, lubrication, orgasm, satisfaction, and pain) we made the following adjustments. Following the latest recommendations of DSM‐V and ICD‐11, we evaluated the frequency of sexual activity, libido, desire, or interest in sex in the domain of 'desire'; we evaluated arousal and fantasy in the domain of 'arousal'; we evaluated orgasm and the number of orgasms in the domain of 'orgasm'; we evaluated pleasure or enjoyment in sex and satisfaction in the 'satisfaction' domain; we evaluated dyspareunia in the 'pain' domain, and we incorporated an assessment of the lubrication domain.
We stratified analyses by time points in effect measurements and clinically reasonable time points on effect measurements from available studies (between 12 and 16 weeks; between 22 and 26 weeks).
Contributions of authors
Drafting the protocol: Lucia AS Lara, Denisse Cartagena‐Ramos, Wellington P Martins, Jaqueline BP Figueiredo, Ana Carolina JS Rosa‐e‐Silva, Rui A Ferriani helped, and Miguel Fuentealba‐Torres
Development of search strategy: Lucia AS Lara, Denisse Cartagena‐Ramos, Wellington P Martins and Miguel Fuenteallba‐Tores
Search for trials: Lucia AS Lara, Denisse Cartagena‐Ramos, Jaqueline BP Figueiredo, Wellington P Martins and Miguel Fuenteallba‐Tores
Obtaining copies of trials: Lucia AS Lara, Denisse Cartagena‐Ramos, Jaqueline BP Figueiredo, Wellington P Martins, and Miguel Fuenteallba‐Tores
Contact authors from trials: Lucia AS Lara, Denisse Cartagena‐Ramos, and Miguel Fuenteallba‐Tores
Selection of which trials to include: Lucia AS Lara, Denisse Cartagena‐Ramos, Jaqueline BP Figueiredo, Jaqueline BP Figueiredo, Lucia AS Lara and Miguel Fuenteallba‐Tores
Extraction of data from trials: Lucia AS Lara, Denisse Cartagena and Miguel Fuenteallba‐Tores
Assessment of risk of bias in included studies: Lucia AS Lara, Denisse Cartagena‐Ramos, Wellington P Martins and Miguel Fuenteallba‐Tores
Entry of data into Review Manager: Lucia AS Lara, Wellington P Martins and Miguel Fuenteallba‐Tores
Drafting the review: Lucia AS Lara, Denisse Cartagena‐Ramos, Wellington P Martins, Ana Carolina JS Rosa‐e‐Silva, Jaqueline BP Figueiredo, Rui A Ferriani helped and Miguel Fuenteallba‐Tores
Sources of support
Internal sources
-
Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP‐USP), Brazil
Authors' salary
-
Facultad de Enfermería y Obtetricia, Universidad de los Andes, Chile, Chile
Authors' salary
External sources
-
Fundação de Apoio ao Ensino, Pesquisa e Assistência do Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FAEPA), Brazil
Funded the purchase of articles
Declarations of interest
Miguel Fuenteallba‐Tores declares no relationships or activities that could have influenced the submitted work.
Lucia A Lara declares no relationships or activities that could have influenced the submitted work.
Denisse Cartagena‐Ramos declares no relationships or activities that could have influenced the submitted work.
Jaqueline BP Figueiredo declares no relationships or activities that could have influenced the submitted work.
Ana Carolina JS Rosa‐e‐Silva declares no relationships or activities that could have influenced the submitted work.
Rui A Ferriani declares no relationships or activities that could have influenced the submitted work.
Wellington P Martins declares no relationships or activities that could have influenced the submitted work.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Archer 2019 {published data only}
- Archer DF, Goldstein SR, Simon JA, Waldbaum AS, Sussman SA, Altomare C, et al. Efficacy and safety of ospemifene in postmenopausal women with moderate-to-severe vaginal dryness: a phase 3, randomized, double-blind, placebo-controlled, multicenter trial. Menopause 2019;26(6):611-21. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bumphenkiatikul 2020 {published data only}
- Bumphenkiatikul T, Panyakhamlerd K, Chatsuwan T, Ariyasriwatana C, Suwan A, Taweepolcharoen C, et al. Effects of vaginal administration of conjugated estrogens tablet on sexual function in postmenopausal women with sexual dysfunction: a double-blind,randomized, placebo-controlled trial. BMC Womens Health 2020;12:173. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- TCTR: 20180219001. Effects of vaginal administration of conjugated estrogens tablet on sexual function in postmenopausal women with sexual dysfunction: a double-blind, randomized, placebo-controlled trial [Effects of vaginal administration of conjugated estrogens tablet on sexual function in postmenopausal women with sexual dysfunction: a double-blind, randomized, placebo-controlled trial]. https://trialsearch.who.int/Trial2.aspx?TrialID=TCTR20180219001 (registered 19 February 2018).
Bushmakin 2014 {published data only}
- Bushmakin AG, Abraham L, Pinkerton JV, Cappelleri JC, Mirkin S. Evaluation of the measurement model and clinically important differences for menopause-specific quality of life associated with bazedoxifene/conjugated estrogens. Menopause (New York, N.Y.) 2014;21:815-22. [PMID: ] [DOI] [PubMed] [Google Scholar]
Caruso 2020 {published data only}
- Caruso S, Cianci A, Sarpietro G, Matarazzo MG, Panella M, Cianci S. Ultralow 0.03 mg vaginal estriol in postmenopausal women who underwent surgical treatment for stress urinary incontinence: effects on quality of life and sexual function. Menopause 2020;27(2):162-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Constantine 2015 {published data only}
- Constantine G, Graham S, Portman DJ, Rosen RC, Kingsberg SA. Female sexual function improved with ospemifene in postmenopausal women with vulvar and vaginal atrophy: results of a randomized, placebo-controlled trial. Climacteric 2015;18:226-32. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Czarnecka 2000 {published data only}
- Czarnecka D, Klocek M, Betkowska-Korpała B, Jankowski P, Olszanecka A, Kawecka-Jaszcz K. Influence of hormone replacement therapy on the quality of life in postmenopausal women with hypertension [Wptyw hormonalnej terapii zastepczej na jakosé zycia kobiet z pierwotnym nadcisnieniem tetniczym w okresie pomenopauzalnym]. Przegl Lek 2000;57(7-8):397-401. [PMID: ] [PubMed] [Google Scholar]
Dayal 2005 {published data only}
- Dayal M, Sammel MD, Zhao J, Hummel AC, Vandenbourne K, Barnhart KT. Supplementation with DHEA: effect on muscle size, strength, quality of life, and lipids. Journal of Women's Health 2005;14(5):391-400. [PMID: ] [DOI] [PubMed] [Google Scholar]
Diem 2018 {published data only}
- Diem SJ, Guthrie KA, Mitchell CM, Reed SD, Larson JC, Ensrud KE, et al. Effects of vaginal estradiol tablets and moisturizer on menopause-specific quality of life and mood in healthy postmenopausal women with vaginal symptoms: a randomized clinical trial. Menopause 2018;07:07. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fonseca 2007 {published data only}
- Fonseca AM, Bagnoli VR, Penteado SR, Paixão JS, Cavalcanti AL, Pinotti JA. Monophasic estrogen-progestogen therapy and sexuality in postmenopausal women. Clinical Drug Investigation 2007;27(2):131-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Fonseca AM, Cavalcanti AL, Bagnoli VR, Paixão JS, Penteado SRL, Cardoso EB, et al. Effects of estradiol valerate associated with cyproterone acetate on some clinical and sexuality-related aspects in postmenopausal women [Efeitos do valerato de estradiol associado ao acetato de ciproterona em alguns parâmetros clínicos e da sexualidade em mulheres na pós-menopausa]. Einstein (Sao Paulo) 2008;6(2):170-4. [Google Scholar]
Gambacciani 2011 {published data only}
- Gambacciani M, Rosano G, Cappagli B, Pepe A, Vitale C, Genazzani AR. Clinical and metabolic effects of drospirenone-estradiol in menopausal women: a prospective study. Climacteric 2011;14(1):18-24. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gast 2009 {published data only}
- Gast MJ, Freedman MA, Vieweg AJ, De Melo NR, Girão MJ, Zinaman MJ. A randomized study of low-dose conjugated estrogens on sexual function and quality of life in postmenopausal women. Menopause 2009;16(2):247-56. [PMID: ] [DOI] [PubMed] [Google Scholar]
Haines 2009 {published data only}
- Haines C, Yu SL, Hiemeyer F, Schaefers M. Micro-dose transdermal estradiol for relief of hot flushes in postmenopausal Asian women: a randomized controlled trial. Climacteric 2009;12(5):419-26. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hemminki 2009 {published data only}
- Hemminki E, Veerus P, Pisarev H, Hovi SL, Topo P, Karro H. The effects of postmenopausal hormone therapy on social activity, partner relationship, and sexual life - experience from the EPHT trial. BMC Women's Health 2009;9:16. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Huang 2008 {published data only}
- Huang A, Yaffe K, Vittinghoff E, Kuppermann M, Addis I, Hanes V, et al. The effect of ultralow-dose transdermal estradiol on sexual function in postmenopausal women. American Journal of Obstetrics and Gynecology 2008;198(3):265e1-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hudita 2003 {published data only}
- Hudita D, Posea C, Ceausu I, Rusu M. Efficacy and safety of oral tibolone 1.25 or 2.5 mg/day vs. placebo in postmenopausal women. European Review for Medical and Pharmacological Sciences 2003;7(5):117-25. [PMID: ] [PubMed] [Google Scholar]
Laan 2001 {published data only}
- Laan E, Van Lunsen RH, Everaerd W. The effects of tibolone on vaginal blood flow, sexual desire and arousability in postmenopausal women. Climacteric 2001;4(1):28-41. [PMID: ] [PubMed] [Google Scholar]
Liberate 2011 {published data only}
- Kenemans P, Bundred NJ, Foidart JM, Kubista E, Schoultz B, Sismondi P, et al. Safety and efficacy of tibolone in breast-cancer patients with vasomotor symptoms: a double-blind, randomised, non-inferiority trial. Lancet Oncology 2009;10(2):135-46. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Merck Sharp & Dohme Corp. Livial Intervention Following Breast Cancer; Efficacy, Recurrence and Tolerability Endpoints (LIBERATE). clinicaltrials.gov 2015 July; NCT00408863. [WEB: https://clinicaltrials.gov/ct2/show/NCT00408863]
- Sismondi P, Kimmig R, Kubista E, Biglia N, Egberts J, Mulder R, et al. Effects of tibolone on climacteric symptoms and quality of life in breast cancer patients-- data from LIBERATE trial. Maturitas 2011;70(4):365-72. [PMID: ] [DOI] [PubMed] [Google Scholar]
Maki 2007 {published data only}
- Maki PM, Gast MJ, Vieweg AJ, Burriss SW, Yaffe K. Hormone therapy in menopausal women with cognitive complaints: a randomized, double-blind trial. Neurology 2007;69(13):1322-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
Mameri Filho 2005 {published data only}
- Mameri Filho J, Haidar MA, Soares Junior JM, Baracat EC. Effects of the association of estrogen and androgen in postmenopausal women [Efeitos da associação estro-androgênica em mulheres na pós-menopausa]. Revista Brasileira de Ginecologia e Obstetrícia 2005;27(3):118-24. [Google Scholar]
Mitchell 2018 {published data only}
- Mitchell CM, Reed SD, Diem S, Larson JC, Newton KM, Ensrud KE, et al. Efficacy of vaginal estradiol or vaginal moisturizer vs placebo for treating postmenopausal vulvovaginal symptoms a randomized clinical trial. JAMA Internal Medicine 2018;178(5):681-90. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Modugno 2003 {published data only}
- Modugno F, Ness RB, Ewing S, Cauley JA. Effect of raloxifene on sexual function in older postmenopausal women with osteoporosis. Obstetrics and Gynecology 2003;101(2):353-61. [PMID: ] [DOI] [PubMed] [Google Scholar]
Morais‐Socorro 2012 {published data only}
- Morais-Socorro M, Cavalcanti MA, Martins R, Neto Francisco P, Rezende A, Azevedo G, et al. Safety and efficacy of tibolone and menopausal transition: a randomized, double-blind placebo-controlled trial. Gynecological Endocrinology 2012;28(6):483-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nathorst‐Böös 1993 {published data only}
- Nathorst-Böös J, Wiklund I, Mattsson LA, Sandin K, Schoultz B. Is sexual life influenced by transdermal estrogen therapy? A double blind placebo controlled study in postmenopausal women. Acta Obstetricia et Gynecologica Scandinavica 1993;72(8):656-60. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nielsen 2006 {published data only}
- Nielsen TF, Ravn P, Pitkin J, Christiansen C. Pulsed estrogen therapy improves postmenopausal quality of life: a 2-year placebo-controlled study. Maturitas 2006;53(2):184-90. [DOI: 10.1016/j.maturitas.2005.04.003] [DOI] [PubMed] [Google Scholar]
Osmanagaoglu 2006 {published data only}
- Osmanağaoğlu MA, Atasaral T, Baltaci D, Bozkaya H. Effect of different preparations of hormone therapy on sexual dysfunction in naturally postmenopausal women. Climateric 2006;9(6):464-72. [DOI: 10.1080/13697130600997775] [DOI] [PubMed] [Google Scholar]
Seyyedi 2016 {published data only}
- Seyyedi F, Kopaei MR, Miraj S. Comparison between vaginal royal jelly and vaginal estrogen effects on quality of life and vaginal atrophy in postmenopausal women: a clinical trial study. Electronic Physician 2016;8:3184-92. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Simon 2007 {published data only}
- Simon JA, Bouchard C, Waldbaum A, Utian W, Zborowski J, Snabes MC. Low dose of transdermal estradiol gel for treatment of symptomatic postmenopausal women: a randomized controlled trial. Obstetrics and Gynecology 2007;109(3):588-96. [DOI: 10.1097/01.AOG.0000254160.62588.41] [DOI] [PubMed] [Google Scholar]
SMART‐3 {published data only}
- Bachmann G, Bobula J, Mirkin S. Effects of bazedoxifene/conjugated estrogens on quality of life in postmenopausal women with symptoms of vulvar/vaginal atrophy. Climacteric 2010;13(2):132-40. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Kagan R, Williams RS, Pan K, Mirkin S, Pickar JH. A randomized, placebo- and active-controlled trial of bazedoxifene/conjugated estrogens for treatment of moderate to severe vulvar/vaginal atrophy in postmenopausal women. Menopause 2010;17(2):281-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Speroff 2003 {published data only}
- Speroff L. Efficacy and tolerability of a novel estradiol vaginal ring for relief of menopausal symptoms. Obstetrics and Gynecology 2003;102(4):823-34. [PMID: ] [DOI] [PubMed] [Google Scholar]
Strickler 2000 {published data only}
- Strickler R, Stovall DW, Merritt D, Shen W, Wong M, Silfen SL. Raloxifene and estrogen effects on quality of life in healthy postmenopausal women: a placebo-controlled randomized trial. Obstetrics and Gynecology 2000;96(3):359-65. [PMID: ] [DOI] [PubMed] [Google Scholar]
Taylor 2017 {published data only}
- Miller VM, Naftolin F, Asthana S, Black D, Brinton E, Bufoff M, et al. The Kronos Early Estrogen Prevention Study (KEEPS): what have we learned? Menopause 2019;26(9):1071. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santoro N, Naftolin F, Black DM, Brinton EA, Budoff MJ, Cedars MI, et al. Change over time in menopausal symptoms in women randomized to oral conjugated estrogen or transdermal estradiol plus micronized progesterone versus placebo: the Kronos Early Estrogen Prevention Study (KEEPS). Menopause 2012;19:1403-4. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Tal A, Pal L, Li F, Black DM, Brinton EA, et al. Effects of oral vs transdermal estrogen therapy on sexual function in early postmenopause: ancillary study of the Kronos Early Estrogen Prevention Study (KEEPS). JAMA Internal Medicine 2017;177(10):1471-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Veerus 2006 {published and unpublished data}
- Veerus P, Hovi SL, Fischer K, Rahu M, Hakama M, Hemminki E. Results from the Estonian postmenopausal hormone therapy trial. Maturitas 2006;55(2):162-73. [PMID: ] [DOI] [PubMed] [Google Scholar]
WHI 1999 {published data only}
- Brunner RL, Gass M, Aragaki A, Hays J, Granek I, Woods N, et al. Effects of conjugated equine estrogen on health-related quality of life in postmenopausal women with hysterectomy: results from the Women's Health Initiative Randomized Clinical Trial. Archives of Internal Medicine 2005;165(17):1976-86. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gass ML, Cochrane BB, Larson JC, Manson JE, Barnabei VM, Brzyski RG, et al. Patterns and predictors of sexual activity among women in the Hormone Therapy trials of the Women's Health Initiative. Menopause 2011;18(11):1160-71. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Hays J, Ockene JK, Brunner RL, Kotchen JM, Manson JE, Patterson RE, et al. Effects of estrogen plus progestin on health-related quality of life. New England Journal of Medicine 2003;348(19):1839-54. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Shumaker SA, Legault C, Rapp SR, Thal L, Wallace RB, Ockene JK, et al. Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women: the Women's Health Initiative Memory Study: a randomized controlled trial. JAMA 2003;289(20):2651-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wiklund 1993 {published data only}
- Wiklund I, Karlberg J, Mattsson LA. Quality of life of postmenopausal women on a regimen of transdermal estradiol therapy: a double-blind placebo-controlled study. American Journal of Obstetrics and Gynecology 1993;168:824-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
WISDOM 2008 {published data only}63718836
- Vickers MR, Martin J, Meade TW, WISDOM study team. The Women's international study of long-duration oestrogen after menopause (WISDOM): a randomised controlled trial. BMC Women's Health 2007;26(7):2. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welton AJ, Vickers MR, Kim J, Ford D, Lawton BA, MacLennan AH, et al. Health related quality of life after combined hormone replacement therapy: randomised controlled trial. BMJ 2008;337(a1190):1-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yang 2004 {published data only}
- Yang TS, Wang HL, Chen YJ, Chang SP, Yuan CC. Effect of continuous administration of conjugated estrogen plus medroxyprogesterone acetate (Premelle) in postmenopausal women in Taiwan. Journal of the Chinese Medical Association 2004;67(7):336-43. [PMID: ] [PubMed] [Google Scholar]
References to studies excluded from this review
2010‐024603‐26 {unpublished data only}
- 2010-024603-26. A phase II study of low-dose vaginal estrogens in pre and postmenopausal breast cancer patients with urogenital atrophy. https://www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number%3A2010-024603-26 (first entered 1 March 2012). [EUCTR: 2010-024603-26-IT]
2014‐000179‐18 {unpublished data only}
- 2014-000179-18. Local oestrogen treatment in postmenopausal women undergoing pelvic organ prolapse surgery (LOTUS) [Local oestrogen treatment in postmenopausal women undergoing pelvic organ prolapse surgery (LOTUS) - feasibility study]. https://www.clinicaltrialsregister.eu/ctr-search/trial/2014-000179-18/GB (first entered 10 March 2015). [EUCTR: 2014-000179-18-GB]
Abedi 2018 {published data only}
- Abedi P, Najafian M, Yaralizadeh M, Namjoyan F. Effect of fennel vaginal cream on sexual function in postmenopausal women: a double blind randomized controlled trial. Journal of Medicine and Life 2018;11(1):24-8. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Abedi 2020 {published data only}
- Abedi P, Zohrabi I, Ansari S, Maraghi E, Maram NS, Houshmand G. The impact of oxytocin vaginal gel on sexual function in postmenopausal women: a randomized controlled trial. Journal of Sex & Marital Therapy 2020;46(4):337-84. [PMID: ] [DOI] [PubMed] [Google Scholar]
Abraham 2014 {published data only}
- Abraham L, Messig M, Pinkerton JV, Mirkin S, Ryan K. Menopause-specific quality of life across varying menopausal populations with conjugated estrogens/bazedoxifene. Menopause (New York, N.Y.) 2014;78(3):212-18. [PMID: ] [DOI] [PubMed] [Google Scholar]
Adler 2005 {published data only}
- Adler G, Young D, Galant R, Quinn L, Witchger MS, Maki KC. A multicenter, open-label study to evaluate satisfaction and menopausal quality of life in women using transdermal estradiol/norethindrone acetate therapy for the management of menopausal signs and symptoms. Gynecologic and Obstetric Investigation 2005;59(4):212-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Almeida 2006 {published data only}
- Almeida OP, Lautenschlager NT, Vasikaran S, Leedman P, Gelavis A, Flicker L. A 20-week randomized controlled trial of estradiol replacement therapy for women aged 70 years and older: effect on mood, cognition and quality of life. Neurobiology of Aging 2006;27(1):141-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Aptecar 2021 {published data only}
- Aptecar L, Fiteni F, Jarlier M, Delaine S, Guillerme V, Jacot W, et al. Prospective evaluation of sexual health in breast cancer women during the first year of adjuvant hormonal treatment using a cancer patient's dedicated questionnaire: a glaring gap of communication between health professionals and patients. Breast Cancer Research and Treatment 2021;18(3):705-13. [DOI: 10.1007/s10549-020-06062-x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Archer 2011 {published data only}
- Archer DF, Pickar JH, MacAllister DC, Warren M. Transdermal estradiol gel for the treatment of symptomatic postmenopausal women. Menopause 2011;18(12):1324-55. [PMID: ] [DOI] [PubMed] [Google Scholar]
Arêas 2019 {published data only}
- Arêas F, Valadares AL, Conde DM, Costa-Paiva L. The effect of vaginal erbium laser treatment on sexual function and vaginal health in women with a history of breast cancer and symptoms of the genitourinary syndrome of menopause: a prospective study. Menopause 2019;26(9):1052-8. [DOI] [PubMed] [Google Scholar]
Argyroudis 1997 {published data only}
- Argyroudis EM, Iatrakis G, Kourkoubas A, Georgoulias N, Kourounis G, Tsionis C, et al. Tibolone in the treatment of psychosomatic symptoms in menopause. Clinical and Experimental Obstetrics & Gynecology 1997;24(3):167-8. [PMID: ] [PubMed] [Google Scholar]
Bachmann 2008 {published data only}
- Bachmann G, Lobo RA, Gut R, Nachtigall L, Notelovitz M. Efficacy of low-dose estradiol vaginal tablets in the treatment of atrophic vaginitis: a randomized controlled trial. Obstetrics and Gynecology 2008;111(1):67-76. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bachmann 2009 {published data only}
- Bachmann GA, Schaefers M, Uddin A, Utian WH. Microdose transdermal estrogen therapy for relief of vulvovaginal symptoms in postmenopausal women. Menopause 2009;16(5):877-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bachmann 2010 {published data only}
- Bachmann GA, Komi JO, Ospemifene Study Group. Ospemifene effectively treats vulvovaginal atrophy in postmenopausal women: results from a pivotal phase 3 study. Menopause 2010;17(3):480-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bachmann 2011 {published data only}
- Bachmann G, Crosby U, Feldman RA, Ronkin S, Constantine GD. Effects of bazedoxifene in nonflushing postmenopausal women: a randomized phase 2 trial. Menopause 2011;18(5):508-14. [PMID: ] [DOI] [PubMed] [Google Scholar]
Barnabei 2002 {published data only}
- Barnabei VM, Grady D, Stovall DW, Cauley JA, Lin F, Stuenkel CA, et al. Menopausal symptoms in older women and the effects of treatment with hormone therapy. Obstetrics and Gynecology 2002;100(6):1209-18. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bennink 2016 {published data only}
- Bennink HC, Verhoven C, Zimmerman Y, Visser M, Foidart J-M, Gemzell-Danielsson K. Clinical effects of the fetal estrogen estetrol in a multiple-rising-dose study in postmenopausal women. Maturitas 2016;91:93-100. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bianchi‐Ferraro 2022 {published data only}
- Bianchi-Ferraro AM, Dia Oliveira C, Speck N, Campos M, Nogueira MC, Marair Gracio Ferreira S, et al. Analysis of clinical response, sexuality and vaginal health in women with genitourinary syndrome of menopause treated with topical estrogen, microablative fractional CO 2 laser and microablative fractional radiofrequency: randomized controlled trial. International Urogynecology Journal 2022;33 Suppl 2:173–519. [DOI: 10.1007/s00192-022-05295-2] [DOI] [Google Scholar]
Binder 2001 {published data only}
- Binder EF, Schechtman KB, Birge SJ, Williams DB, Kohrt WM. Effects of hormone replacement therapy on cognitive performance in elderly women. Maturitas 2001;38(2):137-46. [PMID: ] [DOI] [PubMed] [Google Scholar]
Blumel 2008 {published data only}
- Blümel JE, Del Pino M, Aprikian D, Vallejo S, Sarrá S, Castelo-Branco C. Effect of androgens combined with hormone therapy on quality of life in post-menopausal women with sexual dysfunction. Gynecological Endocrinology 2008;24(12):691-5. [PUBMED: 19172538] [DOI] [PubMed] [Google Scholar]
Bosak 2022 {published data only}
- Bosak Z, Iravani M, Moghimipour E, Haghighizadeh MH, Jelodarian P. Effect of chamomile vaginal gel on the sexual function in postmenopausal women: a double-blind randomized controlled trial. Journal of Sexual Medicine 2022;19(6):983-94. [DOI: ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bride 2014 {published data only}
- Bride M, Shuster L, Rhodes D, Grossardt B, Warndahl R, Debra B. Low dose vaginal estrogens for the treatment of vulvovaginal atrophy: a randomized, placebo-controlled trial evaluating effect of estriol, estradiol or placebo on vulvovaginal atrophy symptoms. Journal of Sexual Medicine 2014;11:220-1. [Google Scholar]
Bruno 2012 {published data only}
- Bruno RV. Treatment of urogenital atrophy with the local administration of oestrogens: a randomized, controlled study in climateric and postmenopausal women [Tratamento da atrofia urogenital com a administração local de estrogênios: um estudo randomizado, controlado em mulheres no climatério e na pós-menopausa]. Revista Brasileira de Medicina 2012;69(8-9):230-5. [Google Scholar]
Cano 2012 {published data only}
- Cano A, Estévez J, Usandizaga R, Gallo JL, Guinot M, Delgado JL, et al. The therapeutic effect of a new ultra low concentration estriol gel formulation (0.005% estriol vaginal gel) on symptoms and signs of postmenopausal vaginal atrophy: results from a pivotal phase III study. Menopause 2012;19(10):1130-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cardozo 2001 {published data only}
- Cardozo LD, Wise BG, Benness CJ. Vaginal oestradiol for the treatment of lower urinary tract symptoms in postmenopausal women--a double-blind placebo-controlled study. Journal of Obstetrics and Gynaecology 2001;21(4):383-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Casper 1999 {published data only}
- Casper F, Petri E. Local treatment of urogenital atrophy with an estradiol-releasing vaginal ring: a comparative and a placebo-controlled multicenter study. Vaginal Ring Study Group. International Urogynecology Journal and Pelvic Floor Dysfunction 1999;10(3):171-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Castelo‐Branco 2000 {published data only}
- Castelo-Branco C, Vicente JJ, Figueras F, Sanjuan A, Martinez de Osaba MJ, Casals E, et al. Comparative effects of estrogens plus androgens and tibolone on bone, lipid pattern and sexuality in postmenopausal women. Maturitas 2000;34(2):161-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cayan 2008 {published data only}
- Cayan F, Dilek U, Pata O, Dilek S. Comparison of the effects of hormone therapy regimens, oral and vaginal estradiol, estradiol + drosperinone and tibolone on sexual function in healthy postmenopausal women. Journal of Sexual Medicine 2008;5(1):132-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ceausu 2011 {published data only}
- Ceausu I, Posea C, Hudit D. Tibolone treatment - different doses and regimens. Climacteric 2011;14:117. [Google Scholar]
Concepcion 2011 {published data only}
- Concepcion N, Cano A, Estevez J, Usandizaga R, Gallo JL, Guinot M, et al. 0.005% estriol vaginal gel, a new formulation delivering an ultra-low dose of estriol per application (50 mg), is a novel treatment for postmenopausal vaginal atrophy. Climacteric 2011;14:86. [Google Scholar]
- Nieto C, Ferrer J, Castellanos E, Casanova A, De La Calle M, Delgado JL, et al. Efficacy of an ultra low dose estriol vaginal gel in treating postmenopausal women with vaginal dryness as their most bothersome symptom. Climacteric 2011;14:156. [Google Scholar]
Cruz 2018 {published data only}
- Cruz VL, Steiner ML, Pompei LM, Strufaldi R, Fonseca FLA, Santiago LH, et al. Randomized, double-blind, placebo-controlled clinical trial for evaluating the efficacy of fractional CO2 laser compared with topical estriol in the treatment of vaginal atrophy in postmenopausal women. Menopause 2018;25(1):21-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Dalil 2020 {published data only}
- Dalil H, KaboudMehri R, Mojab F, Sahranavard S, Nasiri M, Ozgoli G. Effect of Vitex agnus-castus plant on sexual function in women of reproductive age. Iranian Journal of Obstetrics, Gynecology and Infertility 2020;23(4):62-74. [Google Scholar]
Daneshmand 2015 {published data only}
- Daneshmand F, Hosseinzadeh P, Ghahiri A, Ghasemi M. A comparative study of vaginal estrogen cream and sustained released estradiol vaginal tablet (Vagifem) in the treatment of atrophic vaginitis among postmenopausal women. Journal of Research in Medical Sciences 2015;20(12):1160-5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dennerstein 1980 {published data only}
- Dennerstein L, Burrows GD, Hyman GJ, Sharpe K. Some clinical effects of oestrogen-progestogen therapy in surgically castrated women. Maturitas 1980;2(1):19-28. [PMID: ] [DOI] [PubMed] [Google Scholar]
Dessole 2004 {published data only}
- Dessole S, Rubattu G, Ambrosini G, Gallo O, Capobianco G, Cherchi PL, et al. Efficacy of low-dose intravaginal estriol on urogenital aging in postmenopausal women. Menopause 2004;11(1):49-56. [PMID: ] [DOI] [PubMed] [Google Scholar]
Diem 2006 {published data only}
- Diem S, Grady D, Quan J, Vittinghoff E, Wallace R, Hanes V, et al. Effects of ultralow-dose transdermal estradiol on postmenopausal symptoms in women aged 60 to 80 years. Menopause 2006;13(1):130-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ditkoff 1991 {published data only}
- Ditkoff EC, Crary WG, Cristo M, Lobo RA. Estrogen improves psychological function in asymptomatic postmenopausal women. Obstetrics and Gynecology 1991;78(6):991-5. [PMID: ] [PubMed] [Google Scholar]
DRKS00006888 {published data only}
- DRKS00006888. Post market clinical follow-up study of the use of the vaginal cream Remifemin® FeuchtCreme (RFC) [Post market clinical follow-up study of the use of the vaginal cream Remifemin® FeuchtCreme (RFC)]. https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00006888 (registered 20 October 2014). [DRKS-ID DER STUDIE: DRKS00006888]
Duka 2000 {published data only}
- Duka T, Tasker R, McGowan JF. The effects of 3-week estrogen hormone replacement on cognition in elderly healthy females. Psychopharmacology 2000;149(2):129-39. [PMID: ] [DOI] [PubMed] [Google Scholar]
Eftekhar 2009 {published data only}
- Eftekhar T, Akhoondzadeh S, Ghanbari Z, Iranshahr R, Haghollahi F. Effect of vaginal estrogen on post menopausal mood & sleep disturbance/ and sexual satisfaction [Investigating the effect of vaginal estrogen on mood and sleep disorders and sexual satisfaction in postmenopausal women]. Tehran University Medical Journal 2009;67(2):118-24. [Google Scholar]
Eftekhar 2020 {published data only}
- Eftekhar T, Forooghifar T, Khalili T, Shariat M, Haghollahi F. The effect of the CO 2 fractional laser or Premarin vaginal cream on improving sexual function in menopausal women: a randomized controlled trial. Journal of Lasers in Medical Sciences 2020;11(3):292-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eriksen 1992 {published data only}
- Eriksen PS, Rasmussen H. Low-dose 17 beta-estradiol vaginal tablets in the treatment of atrophic vaginitis: a double-blind placebo controlled study. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1992;44(2):137-44. [PMID: ] [DOI] [PubMed] [Google Scholar]
Eriksen 1999 {published data only}
- Eriksen B. A randomized, open, parallel-group study on the preventive effect of an estradiol-releasing vaginal ring (Estring) on recurrent urinary tract infections in postmenopausal women. American Journal of Obstetrics and Gynecology 1999;180(5):1072-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Fabian 2019 {published data only}
- Fabian C, Nye L, Powers K, Nydegger J, Kreutzjans A, Phillips T, et al. Effect of bazedoxifene and conjugated estrogen (Duavee) on breast cancer risk biomarkers in high-risk women: a pilot study. Cancer Prevention Research (Philadelphia, Pa.) 2019;12(10):711-20. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fernandes 2014 {published data only}
- Fernandes T, Costa-Paiva LH, Pedro AO, Baccaro LF, Pinto-Neto AM. Efficacy of vaginally applied estrogen, testosterone, or polyacrylic acid on vaginal atrophy: a randomized controlled trial. Menopause 2016;23(7):792-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Freedman 2009 {published data only}
- Freedman M, Kaunitz AM, Reape KZ, Hait H, Shu H. Twice-weekly synthetic conjugated estrogens vaginal cream for the treatment of vaginal atrophy. Menopause 2009;16(4):735-41. [PMID: ] [DOI] [PubMed] [Google Scholar]
Galesanu 2010 {published data only}
- Galesanu C, Lisnic N, Moisii L, Galesanu RG, Onofriescu M. Effect of hormone replacement therapy on sexual dysfunction in postmenopausal women. Gineco.ro Romania Pulsmedia Network 2010;6(3):186-91. [Google Scholar]
Galhardo 2006 {published data only}
- Galhardo CL, Soares JM Jr, Simões RS, Haidar MA, Rodrigues de Lima G, Baracat EC. Estrogen effects on the vaginal pH, flora and cytology in late postmenopause after a long period without hormone therapy. Clinical and Experimental Obstetrics & Gynecology 2006;33(2):85-9. [PMID: ] [PubMed] [Google Scholar]
Garcia de Arriba 2022 {published data only}
- Garcia de Arriba S, Gruntkemeier L, Hauser M, May TW, Masur C, Stute P. Vaginal hormone-free moisturising cream is not inferior to an estriol cream for treating symptoms of vulvovaginal atrophy: prospective, randomised study. Menopause 2021;28(7):748-55. [DOI: 10.1097/GME.0000000000001766] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gaspard 2021 {published data only}
- Gaspard U, Taziaux M, Jost M, Lobo R, Foidart JM. Effects of estetrol on vaginal cytology, genitourinary syndrome of menopause and health-related quality of life: results from the E4Relief Phase 2b Study. In: Maturitas. Conference: 13th Virtual Congress of the European Menopause, EMAS 2021. Vol. 152. 2021:71. [DOI: 10.1016/j.maturitas.2021.08.019] [DOI]
Gonenne 2006 {published data only}
- Gonenne J, Esfandyari T, Camilleri M, Burton DD, Stephens DA, Baxter KL, et al. Effect of female sex hormone supplementation and withdrawal on gastrointestinal and colonic transit in postmenopausal women. Neurogastroenterology and Motility 2006;18(10):911-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gorenstein 2011 {published data only}
- Gorenstein C, Rennó J Jr, Vieira Filho AH, Gianfaldoni A, Gonçalves MA, Halbe HW, et al. Estrogen replacement therapy and cognitive functions in healthy postmenopausal women: a randomized trial. Archives of Women's Mental Health 2011;14(5):367-73. [PMID: ] [DOI] [PubMed] [Google Scholar]
Griesser 2012 {published data only}
- Griesser H, Skonietzki S, Fischer T, Fielder K, Suesskind M. Low dose estriol pessaries for the treatment of vaginal atrophy: a double-blind placebo-controlled trial investigating the efficacy of pessaries containing 0.2 mg and 0.03 mg estriol. Maturitas 2012;71(4):360-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Guan 2010 {published data only}
- Guan YT, Cai LL, Ding HX, Chen GD, Hu Y. Clinical study on combination of multiple regimens in treatment of osteoporosis in perimenopause and postmenopausal women. Zhonghua Fu Chan Ke Za Zhi 2010;45(8):571-4. [PMID: ] [PubMed] [Google Scholar]
Hachul 2008 {published data only}
- Hachul H, Bittencourt LR, Andersen ML, Haidar MA, Baracat EC, Tufik S. Effects of hormone therapy with estrogen and/or progesterone on sleep pattern in postmenopausal women. International Journal of Gynaecology and Obstetrics 2008;103(3):207-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Harman 2014 {published data only}
- Harman S, Black D, Naftolin F, Brinton E, Budoff M, Cedars M, et al. Arterial imaging outcomes and cardiovascular risk factors in recently menopausal women: a randomized trial. Annals of Internal Medicine 2014;161:249-60. [DOI] [PubMed] [Google Scholar]
Hedrick 2009 {published data only}
- Hedrick RE, Ackerman RT, Koltun WD, Halvorsen MB, Lambrecht LJ. Transdermal estradiol gel 0.1% for the treatment of vasomotor symptoms in postmenopausal women. Menopause 2009;16(1):132-40. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hendrix 2005 {published data only}
- Hendrix SL, Cochrane BB, Nygaard IE, Handa VL, Barnabei VM, Iglesia C, et al. Effects of estrogen with and without progestin on urinary incontinence. JAMA 2005;293(8):935-48. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hodis 2001 {published data only}
- Hodis HN, Mack WJ, Lobo RA, Shoupe D, Sevanian A, Mahrer PR, et al. Estrogen in the prevention of atherosclerosis. A randomized, double-blind, placebo-controlled trial. Annals of Internal Medicine 2001;135(11):939-53. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hofling 2005 {published data only}
- Hofling M, Carlstrom K, Svane G, Azavedo E, Kloosterboer H, Von Schoultz B. Different effects of tibolone and continuous combined estrogen plus progestogen hormone therapy on sex hormone binding globulin and free testosterone levels--an association with mammographic density. Gynecological Endocrinology 2005;20(2):110-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
IRCT138809032766N1 {published data only}
- IRCT138809032766N1. Comparative effects of 2 types of hormone replacement therapy on climacteric symptoms [Comparative effects of conventional hormone replacement therapy and tibolone on climacteric symptoms and sexual dysfunction in postmenopausal women]. https://www.irct.ir/trial/2605 (registered 26 April 2010). [IRCT: 138809032766N1] [DOI] [PubMed]
IRCT2017050433817N1 {published data only}
- IRCT2017050433817N1. Laser vs vaginal conjugated estrogen in postmenopausal women [Evaluation of efficacy and safety of fractional CO2 vs vaginal conjugated estrogen in postmenopausal women diagnosed as having vulvovaginal atrophy]. https://www.irct.ir/trial/25991 (registered 8 June 2017). [IRCT: 2017050433817N1]
Islam 2021 {published data only}
- Islam RM, Davis SR, Bell RJ, Tejada-Berges T, Wrede CD, Domchek SM, et al. A prospective controlled study of sexual function and sexually related personal distress up to 12 months after premenopausal risk-reducing bilateral salpingo-oophorectom. Menopause 2021;28(7):748-55. [DOI: 10.1097/GME.0000000000001766] [PMID: ] [DOI] [PubMed] [Google Scholar]
ISRCTN46661996 {published data only}
- ISRCTN46661996. Local oestrogen treatment in postmenopausal women undergoing pelvic organ prolapse surgery [Local oestrogen treatment in postmenopausal women undergoing pelvic organ prolapse surgery (LOTUS) feasibility study]. https://doi.org/10.1186/ISRCTN46661996 (registered 28 May 2015). [ISRCTN: 46661996]
Jensen 1983 {published data only}
- Jensen J, Christiansen C. Dose-response and withdrawal effects on climacteric symptoms after hormonal replacement therapy. A placebo-controlled therapeutic trial. Maturitas 1983;5(2):125-33. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ju 2021 {published data only}
- Ju R, Ruan X, Xu X, Yang Y, Cheng J, Zhang L, et al. Sexual dysfunction in Chinese women at different reproductive stages and the positive effect of hormone replacement therapy in the early postmenopause. European Journal of Contraception & Reproductive Health Care 2021;26(3):246-54. [DOI: 10.1080/13625187.2020.1867843https://dx.doi.org/10.1080/13625187.2020.1867843] [DOI] [PubMed] [Google Scholar]
Kagan 2014 {published data only}
- Kagan R, Portman D, Archer D, Graham S, Constantine G. Responder analysis of ospemifene treatment for vulvar and vaginal atrophy in postmenopausal women in phase 3 randomized, placebo-controlled trials. Menopause (New York, N.Y.) 2014;21:1332. [Google Scholar]
Kenny 2005 {published data only}
- Kenny AM, Kleppinger A, Wang Y, Prestwood KM. Effects of ultra-low-dose estrogen therapy on muscle and physical function in older women. Journal of the American Geriatrics Society 2005;53(11):1973-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kessel 2003 {published data only}
- Kessel B, Nachtigall L, Plouffe L, Siddhanti S, Rosen A, Parsons A. Effect of raloxifene on sexual function in postmenopausal women. Climacteric 2003;6(3):248-56. [PMID: ] [PubMed] [Google Scholar]
Kimura 1995 {published data only}
- Kimura D. Estrogen replacement therapy may protect against intellectual decline in postmenopausal women. Hormones and Behavior 1995;29(3):312-21. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kingsberg 2017 {published data only}
- Kingsberg S, Kroll R, Goldstein I, Constantine G, Bernick B, Graham S, et al. Product acceptability and women's satisfaction with a low-dose solubilized vaginal estradiol softgel capsule, TX-004H. Journal of Sexual Medicine 2017;14(6 Suppl 5):e355. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kocoska‐Maras 2011 {published data only}
- Kocoska-Maras L, Zethraeus N, Rådestad AF, Ellingsen T, Schoultz B, Johannesson M, et al. A randomized trial of the effect of testosterone and estrogen on verbal fluency, verbal memory, and spatial ability in healthy postmenopausal women. Fertility and Sterility 2011;95(1):152-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kornafel 1992 {published data only}
- Kornafel KL, March CM. Estradiol gel in the treatment of menopausal symptoms: a placebo-controlled double-blind case study of efficacy and safety. Southern Medical Journal 1992;85(3):270-3. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kroll 2018 {published data only}
- Kroll R. A randomized, multicenter, double-blind study to evaluate the safety and efficacy of estradiol vaginal cream 0.003% in postmenopausal women with dyspareunia as the most bothersome symptom. Menopause 2018;25(2):133-8. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Krychman 2016 {published data only}
- Krychman M, Symons J, Portman D. Correlation of physiologic markers of vulvovaginal atrophy and symptom severity in postmenopausal women with genitourinary syndrome of menopause. Journal of Sexual Medicine 2016;13:S248. [Google Scholar]
Kumru 2008 {published data only}
- Kumru S, Yildiz FM, Godekmerdan A, Kutlu S, Yilmaz B, Gurates B. Effects of raloxifene and hormone replacement therapy on serum Th2 and Th3 type cytokine concentrations in healthy postmenopausal women: a randomised controlled trial. Archives of Gynecology and Obstetrics 2008;277(6):489-93. [PMID: ] [DOI] [PubMed] [Google Scholar]
L'Hermite 2022 {published data only}
- Ermitaño M. BIJUVA®, the only bioidentical HRT, combining estradiol and progesterone in a single pill: finally available in Belgium, after the USA (approval in 2018 by the Food and Drug Administration) ! [BIJUVA®, le seul THS bioidentique, combinant estradiol et progestérone dans une seule pilule: enfin disponible en Belgique, après les EU (approbation en 2018 par la Food and Drug Administration)]. Association des Médecins anciens étudiants de l’Université libre de Bruxelles (A.M.U.B.) 2022 2022;43(3):244-7. [DOI: 10.30637/2022.22-042] [DOI] [Google Scholar]
Lin 2011 {published data only}
- Lin SQ, Sun LZ, Lin JF, Yang X, Zhang LJ, Qiao J, et al. Estradiol 1 mg and drospirenone 2 mg as hormone replacement therapy in postmenopausal Chinese women. Climacteric 2011;14(4):472-81. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lindsay 2002 {published data only}
- Lindsay R, Gallagher JC, Kleerekoper M, Pickar JH. Effect of lower doses of conjugated equine estrogens with and without medroxyprogesterone acetate on bone in early postmenopausal women. JAMA 2002;287(20):2668-76. [PMID: ] [DOI] [PubMed] [Google Scholar]
Liu 2012 {published data only}
- Liu JH, Reape KZ, Hait HI. Synthetic conjugated estrogens-B and postmenopausal nocturnal vasomotor symptoms: a randomized controlled trial. Obstetrics and Gynecology 2012;119(1):78-84. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lobo 2009 {published data only}
- Lobo RA, Pinkerton JV, Gass ML, Dorin MH, Ronkin S, Pickar JH, et al. Evaluation of bazedoxifene/conjugated estrogens for the treatment of menopausal symptoms and effects on metabolic parameters and overall safety profile. Fertility and Sterility 2009;92(3):1025-38. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lobo 2017 {published data only}
- Lobo RA, Archer DF, Kagan R, Kaunitz AM, Constantine GD, Pickar JH, et al. A 17β-Estradiol–Progesterone Oral Capsule for Vasomotor Symptoms in Postmenopausal WomenA Randomized Controlled Trial. Obstetrics & Gynecology 2018;132(1):161-70. [DOI: 10.1097/AOG.0000000000002645] [DOI] [PubMed] [Google Scholar]
MacDonald 1994 {published data only}
- MacDonald AG, Murphy EA, Capell HA, Bankowska UZ, Ralston SH. Effects of hormone replacement therapy in rheumatoid arthritis: a double blind placebo-controlled study. Annals of the Rheumatic Diseases 1994;53(1):54-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marschalek 2022 {published data only}
- Marschalek ML, Bodner K, Kimberger O, Morgenbesser R, Dietrich W, Obruca C, et al. Sexual function in postmenopausal women with symptomatic pelvic organ prolapse treated either with locally applied estrogen or placebo: results of a double-masked, placebo-controlled, multicenter trial. Journal of Sexual Medicine 2022;19(7):1124-30. [DOI: 10.1016/j.jsxm.2022.04.007] [DOI] [PubMed] [Google Scholar]
Marsden 2000 {published data only}
- Marsden J, Whitehead M, A'Hern R, Baum M, Sacks N. Are randomized trials of hormone replacement therapy in symptomatic women with breast cancer feasible? Fertility and Sterility 2000;73(2):292-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Marx 2004 {published data only}
- Marx P, Schade G, Wilbourn S, Blank S, Moyer DL, Nett R. Low-dose (0.3 mg) synthetic conjugated estrogens A is effective for managing atrophic vaginitis. Maturitas 2004;47(1):47-54. [DOI] [PubMed] [Google Scholar]
Miller 2019 {published data only}
- Miller VM, Naftolin F, Asthana S, Black D, Brinton E, Bufoff M, et al. The Kronos Early Estrogen Prevention Study (KEEPS): what have we learned? Menopause 2019;26(9):1071. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mittal 2020 {published data only}
- Mittal M, Panay N, Supramaniam PR, Savvas M, Cardozo L, Hamoda H. Direct comparison of women's perceptions and acceptability of micronised progesterone and medroxyprogesterone acetate in combination with transdermal oestradiol in the management of young postmenopausal women, under 45 years of age. Post Reproductive Health 2020 ;26(4):210-19. [PMID: ] [DOI] [PubMed] [Google Scholar]
Mizunuma 2011 {published data only}
- Mizunuma H. Clinical usefulness of a low-dose maintenance therapy with transdermal estradiol gel in Japanese women with estrogen deficiency symptoms. Climacteric 2011;14(5):581-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Naessen 2001 {published data only}
- Naessen T, Rodriguez-Macias K, Lithell H. Serum lipid profile improved by ultra-low doses of 17 beta-estradiol in elderly women. Journal of Clinical Endocrinology and Metabolism 2001;86(6):2757-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
NCT01543399 {published data only}
- NCT01543399. Vascular effect of tibolone in the brachial artery (TDILA) [Vascular effect of tibolone versus placebo evaluated by flow-mediated dilatation of brachial artery]. https://clinicaltrials.gov/ct2/show/NCT01543399 (first posted 12 March 2012). [NCT: 01543399] [NCT01543399]
NCT01585558 {published data only}NCT01585558
- NCT01585558. Long-term safety of 30 mg and 60 mg oral daily dose of ospemifene in the treatment of vulvar and vaginal atrophy (VVA) in postmenopausal women with intact uterus [Long-term safety of 30 mg and 60 mg oral daily dose of ospemifene in the treatment of vulvar and vaginal atrophy (VVA) in postmenopausal women with intact uterus: a 40 week randomized, double blind, placebo controlled, follow-up to protocol 15-50310.]. https://clinicaltrials.gov/ct2/show/NCT01585558 (first posted 26 April 2012). [CTG: ]
NCT01779947 {published data only}
- NCT01779947. Study to evaluate the safety and bioequivalence of estradiol vaginal inserts, 10 mcg and Vagifem® 10 mcg and compare to placebo [An investigator-blind, randomized, parallel-group, placebo-controlled, multicenter study to evaluate the safety and bioequivalence of estradiol vaginal inserts, USP 10 mcg and Vagifem® (estradiol vaginal tablets) 10 mcg and compare both active treatments to a placebo control in female subjects with moderate to severe symptoms of vulvar and vaginal atrophy associated with menopause]. https://clinicaltrials.gov/ct2/show/NCT01779947 (first posted 30 January 2013). [NCT: 01779947]
NCT01822288 {published data only}20180219001
- NCT01822288. The impact of hormone therapy on lower urinary tract symptoms, sexual function and psychosomatic disorder [The impact of different hormone therapy regimens on lower urinary tract symptoms, sexual function and psychosomatic disorder]. clinicaltrials.gov/ct2/show/NCT01822288 (first received 2 April 2013). [NCT01822288]
NCT02253173 {published data only}
- NCT02253173. Estradiol vaginal softgel capsules in treating symptoms of vulvar and vaginal atrophy in postmenopausal women (REJOICE) [A phase 3, randomized, double-blind, placebo-controlled, multi-center trial to evaluate the safety and efficacy of TX-004HR in postmenopausal women with moderate to severe symptoms of vulvar and vaginal atrophy]. https://clinicaltrials.gov/ct2/show/NCT02253173 (first posted 1 October 2014). [CTG: ]
NCT02638337 {published data only}
- NCT02638337. Study to evaluate ospemifene in patients with moderate to severe vaginal dryness due to menopause [A phase 3, randomized, double-blind, placebo-controlled multicenter study to evaluate the efficacy and safety of ospemifene in patients with moderate to severe vaginal dryness, a symptom of vulvo-vaginal atrophy (VVA) due to menopause]. https://clinicaltrials.gov/ct2/show/NCT02638337 (first posted 23 December 2015). [CTG: ]
NCT03018106 {published data only}
- NCT03018106. Ospemifene vs. conjugated estrogens in the treatment of postmenopausal sexual dysfunction [Ospemifene versus conjugated estrogens in the treatment of postmenopausal sexual dysfunction]. https://clinicaltrials.gov/ct2/show/NCT03018106 (first posted 11 January 2017). [CTG: ]
Nevinny‐Stickel 1983 {published data only}
- Nevinny-Stickel J. Double-blind cross-over study with Org OD 14 and placebo in postmenopausal patients. Archives of Gynecology 1983;234(1):27-31. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nieto 2011 {published data only}
- Nieto C, Ferrer J, Castellanos E, Casanova A, De La Calle M, Delgado JL, et al. Efficacy of an ultra low dose estriol vaginal gel in treating postmenopausal women with vaginal dryness as their most bothersome symptom. Climacteric 2011;14:166. [Google Scholar]
Noguchi 2018 {published data only}
- Noguchi S, Ellis M J, Robertson JF, Thirlwell J, Fazal M, Shao Z. Progression-free survival results in postmenopausal Asian women: subgroup analysis from a phase III randomized trial of fulvestrant 500 mg vs anastrozole 1 mg for hormone receptor-positive advanced breast cancer (FALCON). Breast Cancer 2018;25:356-64. [DOI] [PubMed] [Google Scholar]
Notelovitz 2000 {published data only}
- Notelovitz M, Mattox JH. Suppression of vasomotor and vulvovaginal symptoms with continuous oral 17beta-estradiol. Menopause 2000;7(5):310-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Obel 1993 {published data only}
- Obel EB, Munk-Jensen N, Svenstrup B, Bennett P, Micic S, Henrik-Nielsen R, et al. A two-year double-blind controlled study of the clinical effect of combined and sequential postmenopausal replacement therapy and steroid metabolism during treatment. Maturitas 1993;16(1):13-21. [PMID: ] [DOI] [PubMed] [Google Scholar]
Palacios 1995 {published data only}
- Palacios S, Menendez C, Jurado AR, Castaño R, Vargas JC. Changes in sex behaviour after menopause: effects of tibolone. Maturitas 1995;22(2):155-61. [PMID: ] [DOI] [PubMed] [Google Scholar]
Palacios 2005 {published data only}
- Palacios S, Castelo-Branco C, Cancelo M J, Vazquez F. Low-dose, vaginally administered estrogens may enhance local benefits of systemic therapy in the treatment of urogenital atrophy in postmenopausal women on hormone therapy. Maturitas 2005;50(2):98-104. [PMID: ] [DOI] [PubMed] [Google Scholar]
Paraiso 2020 {published data only}
- Paraiso M, Ferrando C, Sokol E, Rardin C, Matthews C, Karram M, et al. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: the VeLVET Trial. Menopause 2020;27(1):50-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pinkerton 2014 {published data only}
- Pinkerton JV, Bushmakin A, Abraham L, Cappelleri J, Komm B. Most bothersome symptom in women with vulvar-vaginal atrophy as a moderator of treatment effects. Menopause (New York, N.Y.) 2014;21:1331. [DOI] [PubMed] [Google Scholar]
Poetry 2011 {published data only}
- Parkinson Study Group Poetry Investigators. A randomized pilot trial of estrogen replacement therapy in post-menopausal women with Parkinson's disease. Parkinsonism & Related Disorders 2011;17(10):757-60. [PMID: ] [DOI] [PubMed] [Google Scholar]
Polo‐Kantola 1998 {published data only}
- Polo-Kantola P, Portin R, Polo O, Helenius H, Irjala K, Erkkola R. The effect of short-term estrogen replacement therapy on cognition: a randomized, double-blind, cross-over trial in postmenopausal women. Obstetrics and Gynecology 1998;91(3):459-66. [PMID: ] [DOI] [PubMed] [Google Scholar]
Portman 2013 {published data only}
- Portman D, Bachmann G, Graham S. Efficacy of oral ospemifene 60mg: comparison in subpopulations. Menopause (New York, N.Y.) 2013;20:1349. [Google Scholar]
Portman 2014a {published data only}
- Portman D, Palacios S, Nappi RE, Mueck AO. Ospemifene, a non-oestrogen selective oestrogen receptor modulator for the treatment of vaginal dryness associated with postmenopausal vulvar and vaginal atrophy: a randomised, placebo-controlled, phase III trial. Maturitas 2014;78:91-8. [DOI] [PubMed] [Google Scholar]
Pradeep 2016 {published data only}
- Pradeep Y, Negi N, Srivastava A, Gupta A. The diagnosis of atrophic vaginitis by vaginal pH in postmenopausal women and evaluation of treatment response of vaginal estrogen vs. isoflavones. Climacteric 2016;19:35. [Google Scholar]
Prestwood 2003 {published data only}
- Prestwood KM, Kenny AM, Kleppinger A, Kulldorff M. Ultralow-dose micronized 17beta-estradiol and bone density and bone metabolism in older women: a randomized controlled trial. JAMA 2003;290(8):1042-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Raz 2014 {published data only}
- Raz L, Hunter LW, Jayachandran M, Heit JA, Miller VM. Differential effects of oral and transdermal menopausal hormone therapy on prostacyclin and thromboxane in platelets. Physiological Reports 2014;2(3):e00275. [DOI] [PMC free article] [PubMed] [Google Scholar]
RBR‐94dx93/1 {published data only}
- RBR-94dx93/1. Evaluation of the sexual function and vaginal environment of menopausal women before and after treatment [Evaluation of the sexual function and vaginal microbiota fractionated microablative radiofrequency for the treatment of genitourinary menopause syndrome]. https://ensaiosclinicos.gov.br/rg/RBR-94dx93/1 (registered 7 February 2018). [REBEC: RBR-94dx93]
Rebar 2000 {published data only}
- Rebar RW, Trabal J, Mortola J. Low-dose esterified estrogens (0.3 mg/day): long-term and short-term effects on menopausal symptoms and quality of life in postmenopausal women. Climacteric 2000;3(3):176-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
Reindollar 2002 {published data only}
- Reindollar R, Koltun W, Parsons A, Rosen A, Siddhanti S, Plouffe L Jr, et al. Effects of oral raloxifene on serum estradiol levels and other markers of estrogenicity. Fertility and Sterility 2002;78(3):469-72. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ribom 2011 {published data only}
- Ribom EL, Svensson P, Van Os S, Larsson M, Naessen T. Low-dose tibolone (1.25 mg/d) does not affect muscle strength in older women. Menopause 2011;18(2):194-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rigano 2001 {published data only}
- Rigano A, Rigano M, Cancellieri F, Pullè C. Sexually and well-being in early menopause. Effect of transdermal estradiol therapy. Panminerva Medica 2001;43(2):115-8. [PMID: ] [PubMed] [Google Scholar]
Russu 2011 {published data only}
- Russu MC, Mubarak N, Marin JA, Hudit D. Quality of life improvement after vaginal treatment of urogenital atrophy symptoms in postmenopause. Climateric 2011;14:181. [Google Scholar]
Saeideh 2010 {published data only}
- Saeideh Z, Raziyeh M, Soghrat F. Comparing the effects of continuous hormone replacement therapy and tibolone on the genital tract of menopausal women; a randomized controlled trial. Journal of Reproduction & Infertility 2010;11(3):183-7. [PMC free article] [PubMed] [Google Scholar]
Saletu 2002 {published data only}
- Saletu B, Anderer P, Gruber D, Metka M, Huber J, Saletu-Zyhlarz GM. Hormone replacement therapy and vigilance: double-blind, placebo-controlled EEG-mapping studies with an estrogen-progestogen combination (Climodien, Lafamme) versus estrogen alone in menopausal syndrome patients. Maturitas 2002;43(3):165-81. [PMID: ] [DOI] [PubMed] [Google Scholar]
Samaras 1999 {published data only}
- Samaras K, Hayward CS, Sullivan D, Kelly RP, Campbell LV. Effects of postmenopausal hormone replacement therapy on central abdominal fat, glycemic control, lipid metabolism, and vascular factors in type 2 diabetes. Diabetes Care 1999;22(9):1401-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Santofimia 2022 {published data only}
- Pingarron Santofimia C, Lafuente Gonzalez P, Guitierrez Velez M, Calvente Aguilar V, Poyo Torcal S, Terol Sanchez P, et al. Long-term use of ospemifene in clinical practice for vulvo-vaginal atrophy: end results at 12 months of follow-up. Gynecological Endocrinology 2022;38(7):577-82. [DOI: 10.1080/09513590.2022.2083103] [PMID: ] [DOI] [PubMed] [Google Scholar]
Santoro 2012 {published data only}
- Santoro N, Naftolin F, Black DM, Brinton EA, Budoff MJ, Cedars MI, et al. Change over time in menopausal symptoms in women randomized to oral conjugated estrogen or transdermal estradiol plus micronized progesterone versus placebo: the kronos early estrogen prevention study (KEEPS). Menopause 2012;19:1403-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Serebani 2020 {published data only}
- Sarebani Z, Alimoradi Z, Aali E, Mirzadeh M, Chegini V, Abbaspour M, et al. Investigating the effect of vitamin D vaginal suppository on sexual function among postmenopausal women: study protocol for a randomized controlled trial. BMC Womens Health 2020;20(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shah 2006 {published data only}
- Shah S, Bell RJ, Savage G, Goldstat R, Papalia MA, Kulkarni J, et al. Testosterone aromatization and cognition in women: a randomized, placebo-controlled trial. Menopause 2006;13(4):600-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sherman 2003 {published data only}
- Sherman AM, Shumaker SA, Kancler C, Zheng B, Reboussin DM, Legault C, et al. Baseline health-related quality of life in postmenopausal women with coronary heart disease: the Estrogen Replacement and Atherosclerosis (ERA) trial. Journal of Women's Health 2003;12(4):351-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
Shulman 2002 {published data only}
- Shulman LP, Yankov V, Uhl K. Safety and efficacy of a continuous once-a-week 17beta-estradiol/levonorgestrel transdermal system and its effects on vasomotor symptoms and endometrial safety in postmenopausal women: the results of two multicenter, double-blind, randomized, controlled trials. Menopause 2002;9(3):195-207. [PMID: ] [DOI] [PubMed] [Google Scholar]
Silverman 2012 {published data only}
- Silverman SL, Chines AA, Kendler DL, Kung AW, Teglbjærg CS, Felsenberg D, et al. Sustained efficacy and safety of bazedoxifene in preventing fractures in postmenopausal women with osteoporosis: results of a 5-year, randomized, placebo-controlled study. Osteoporosis International 2012;23(1):351-63. [PMID: ] [DOI] [PubMed] [Google Scholar]
Simon 1999 {published data only}
- Simon J, Klaiber E, Wiita B, Bowen A, Yang HM. Differential effects of estrogen-androgen and estrogen-only therapy on vasomotor symptoms, gonadotropin secretion, and endogenous androgen bioavailability in postmenopausal women. Menopause 1999;6(2):138-46. [PMID: ] [PubMed] [Google Scholar]
Simon 2008a {published data only}
- Simon J, Nachtigall L, Gut R, Lang E, Archer DF, Utian W. Effective treatment of vaginal atrophy with an ultra-low-dose estradiol vaginal tablet. Obstetrics and Gynecology 2008;112(5):1053-60. [PMID: ] [DOI] [PubMed] [Google Scholar]
Simon 2008b {published data only}
- Simon JA, Reape KZ, Wininger S, Hait H. Randomized, multicenter, double-blind, placebo-controlled trial to evaluate the efficacy and safety of synthetic conjugated estrogens B for the treatment of vulvovaginal atrophy in healthy postmenopausal women. Fertility and Sterility 2008;90(4):1132-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Simon 2012 {published data only}
- Simon JA, Lin VH, Radovich C, Bachmann GA, The Ospemifene Study Group. One-year long-term safety extension study of ospemifene for the treatment of vulvar and vaginal atrophy in postmenopausal women with a uterus. Menopause 2012;20(4):418-27. [PMID: ] [DOI] [PubMed] [Google Scholar]
Simunic 2003 {published data only}
- Simunic V, Banovic I, Ciglar S, Jeren L, Pavicic Baldani D, Sprem M. Local estrogen treatment in patients with urogenital symptoms. International Federation of Gynaecology and Obstetrics 2003;82(2):187-97. [PMID: ] [DOI] [PubMed] [Google Scholar]
SMART‐5 {published data only}
- Archer DF, Lobo RA, Pan K, Chines AA, Mirkin S. Safety and tolerability of bazedoxifene/conjugated estrogens in postmenopausal women: findings from a 1-year, randomized, placebo-and active-controlled, phase 3 trial. Menopause 2011;18:1355-6. [Google Scholar]
- Harvey JA, Pinkerton JV, Pan K, Thompson JR, Mirkin S, Chines AA. The effects of bazedoxifene/conjugated estrogens on breast density in postmenopausal women. Menopause 2011;18:1342. [Google Scholar]
- Mirkin S, Archer DF, Lobo RA, Pan K, Chines AA. Safety and tolerability of bazedoxifene/conjugated estrogens in postmenopausal women: findings from a 1-year, randomized, placebo, and active-controlled, phase 3 TRIAL. Maturitas 2012;71:S43-4. [Google Scholar]
- Pinkerton JV, Pan K, Abraham L, Racketa J, Chines AA, Mirkin S. Effects of bazedoxifene/conjugated estrogens on sleep parameters and health-related quality of life in postmenopausal women. Menopause 2011;18:1346. [DOI] [PubMed] [Google Scholar]
- Racketa J, Pinkerton JV, Pan K, Abraham L, Chines AA, Mirkin S. Effects of bazedoxifene/conjugated estrogens on sleep parameters and health-related quality of life in postmenopausal women. Maturitas 2012;71:S59-S60. [Google Scholar]
Sorensen 2001 {published data only}
- Sorensen MB, Rosenfalck AM, Hojgaard L, Ottesen B. Obesity and sarcopenia after menopause are reversed by sex hormone replacement therapy. Obesity Research 2001;9(10):622-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Speroff 2006 {published data only}
- Speroff L, Haney AF, Gilbert RD, Ellman H, Estradiol Acetate Investigator Group. Efficacy of a new, oral estradiol acetate formulation for relief of menopause symptoms. Menopause 2006;13(3):442-50. [PMID: ] [DOI] [PubMed] [Google Scholar]
Stening 2011 {published data only}
- Stening KD, Eriksson O, Henriksson KG, Brynhildsen J, Lindh-Åstrand L, Berg G, et al. Hormonal replacement therapy does not affect self-estimated pain or experimental pain responses in post-menopausal women suffering from fibromyalgia: a double-blind, randomized, placebo-controlled trial. Rheumatology 2011;50(3):544-51. [PMID: ] [DOI] [PubMed] [Google Scholar]
Stevenson 2010 {published data only}
- Stevenson JC, Durand G, Kahler E, Pertynski T. Oral ultra-low dose continuous combined hormone replacement therapy with 0.5 mg 17beta-oestradiol and 2.5 mg dydrogesterone for the treatment of vasomotor symptoms: results from a double-blind, controlled study. Maturitas 2010;67(3):227-32. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sun 2016 {published data only}
- Sun Z, Zhu L, Xu T, Shi X, Lang J. Effects of preoperative vaginal estrogen therapy for the incidence of mesh complication after pelvic organ prolapse surgery in postmenopausal women: is it helpful or a myth? A 1-year randomized controlled trial. Menopause 2016;23(7):740–8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Swanson 2006 {published data only}
- Swanson SG, Drosman S, Helmond FA, Stathopoulos VM. Tibolone for the treatment of moderate to severe vasomotor symptoms and genital atrophy in postmenopausal women: a multicenter, randomized, double-blind, placebo-controlled study. Menopause 2006;13(6):917-25. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tansupswatdikul 2012 {published data only}
- Tansupswatdikul P, Chaikiltisilpa S, Jaimchariyatam N, Desudchit T, Panyakhamlerd K, Jaisamrarn U, et al. Effect of estrogen therapy on objective sleep quality in postmenopausal women. Menopause (New York, N.Y.) 2012;19:1384-5. [Google Scholar]
Tinelli 2002 {published data only}
- Tinelli FG, Tinelli A, Sena T. Clinical effects of hormone replacement therapy with estradiol valerate and cyproterone acetate in perimenopausal women [Effetti di un trattamento ormonale sostitutivocon estradiolo valerato e ciproterone acetatoin donne in perimenopausa]. Minerva Ginecologica 2002;54(1):67-73. [PMID: ] [PubMed] [Google Scholar]
Tungmunsakulchai 2015 {published data only}
- Tungmunsakulchai R, Chaikittisilpa S, Snabboon T, Panyakhamlerd K, Jaisamrarn U, Taechakraichana N. Effectiveness of a low dose testosterone undecanoate to improve sexual function in postmenopausal women. BMC Women's Health 2015;2(15):113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tuomikoski 2010 {published data only}
- Tuomikoski P, Mikkola TS, Tikkanen MJ, Ylikorkala O. Hot flushes and biochemical markers for cardiovascular disease: a randomized trial on hormone therapy. Climacteric 2010;13(5):457-66. [PMID: ] [DOI] [PubMed] [Google Scholar]
Usall 2011 {published data only}
- Usall J, Huerta-Ramos E, Iniesta R, Cobo J, Araya S, Roca M, et al. Raloxifene as an adjunctive treatment for postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. Journal of Clinical Psychiatry 2011;72(11):1552-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Utian 2001 {published data only}
- Utian WH, Shoupe D, Bachmann G, Pinkerton JV, Pickar JH. Relief of vasomotor symptoms and vaginal atrophy with lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertililty and Sterility 2001;75(6):1065-79. [PMID: ] [DOI] [PubMed] [Google Scholar]
Utian 2004 {published data only}
- Utian WH, Gass ML, Pickar JH. Body mass index does not influence response to treatment, nor does body weight change with lower doses of conjugated estrogens and medroxyprogesterone acetate in early postmenopausal women. Menopause 2004;11(3):306-14. [PMID: ] [DOI] [PubMed] [Google Scholar]
Vardy 2003 {published data only}
- Vardy MD, Lindsay R, Scotti RJ, Mikhail M, Richart RM, Nieves J, et al. Short-term urogenital effects of raloxifene, tamoxifen, and estrogen. American Journal of Obstetrics and Gynecology 2003;189(1):81-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Veldhuis 2011a {published data only}
- Veldhuis JD, Erickson D, Miles JM, Bowers CY. Complex regulation of GH autofeedback under dual-peptide drive: studies under a pharmacological GH and sex steroid clamp. American Journal of Physiology Endocrinology and Metabolism 2011;300(6):E1158-65. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Veldhuis 2011b {published data only}
- Veldhuis JD, Erickson D, Wigham J, Weist S, Miles JM, Bowers CY. Gender, sex-steroid, and secretagogue-selective recovery from growth hormone-induced feedback in older women and men. Journal of Clinical Endocrinology and Metabolism 2011;96(8):2540-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vestergaard 2003 {published data only}
- Vestergaard P, Hermann AP, Stilgren L, Tofteng CL, Sørensen OH, Eiken P, et al. Effects of 5 years of hormonal replacement therapy on menopausal symptoms and blood pressure - a randomised controlled study. Maturitas 2003;46(2):123-32. [PMID: ] [DOI] [PubMed] [Google Scholar]
Voipio 2002 {published data only}
- Voipio SK, Komi J, Kangas L, Halonen K, DeGregorio MW, Erkkola RU. Effects of ospemifene (FC-1271a) on uterine endometrium, vaginal maturation index, and hormonal status in healthy postmenopausal women. Maturitas 2002;43(3):207-14. [PMID: ] [DOI] [PubMed] [Google Scholar]
Warton 2014 {published data only}
- Wharton W, Gleason C, Dowling N, Carlsson C, Brinton E, Santoro M, et al. The KEEPS-cognitive and affective study: Baseline associations between vascular risk factors and cognition. Journal of Alzheimer's Disease 2014;40(2):331–41. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wolff 1982 {published data only}
- Wolff JP, Cachelou R, Gueritee N. Absence of systemic hormonal effects in an oestradiol diether topically active on the vaginal mucosa. Maturitas 1982;4(4):239-46. [PMID: ] [DOI] [PubMed] [Google Scholar]
Woo 2003 {published data only}
- Woo J, Lau E, Ho SC, Cheng F, Chan C, Chan AS, et al. Comparison of Pueraria lobata with hormone replacement therapy in treating the adverse health consequences of menopause. Menopause 2003;10(4):352-61. [PMID: ] [DOI] [PubMed] [Google Scholar]
Yeo 2020 {published data only}
- Yeo W, Pang E, Liem GS, Suen JJ, Ng RY, Yip CC, et al. Menopausal symptoms in relationship to breast cancer-specific quality of life after adjuvant cytotoxic treatment in young breast cancer survivors. Health and Quality of Life Outcomes 2020;18(24):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zervoudis 2009 {published data only}
- Zervoudis S, Iatrakis G, Peitsidis P, Tsikouras P, Galazios G, Liberis V, et al. Tibolone vaginal versus per os administration in the management of post-menopausal symptoms. Revista Medico-Chirurgicala a Societatii de Medici si Naturalisti din Iasi 2009;113(2):471-7. [PMID: ] [PubMed] [Google Scholar]
Zhou 2011 {published data only}
- Zhou YZ, Sun LZ, Lin JF, Yang X, Zhang LJ, Qiao J, et al. Evaluation the efficacy and safety of estradiol and drospirenone tablets in the treatment of menopausal symptoms among postmenopausal Chinese healthy women: a randomized, multi-center, double-blind, placebo-controlled clinical study. Zhonghua Fu Chan Ke Za Zhi 2011;46(5):345-9. [PMID: ] [PubMed] [Google Scholar]
Zullo 2005 {published data only}
- Zullo MA, Plotti F, Calcagno M, Palaia I, Muzii L, Manci N, et al. Vaginal estrogen therapy and overactive bladder symptoms in postmenopausal patients after a tension-free vaginal tape procedure: a randomized clinical trial. Menopause 2005;12(4):421-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Hirschberg 2020 {published data only}
- Hirschberg AL, Sánchez-Rovira P, Presa-Lorite J, Campos-Delgado M, Gil-Gil M, Lidbrink E, et al. Efficacy and safety of ultra-low dose 0.005% estriol vaginal gel for the treatment of vulvovaginal atrophy in postmenopausal women with early breast cancer treated with nonsteroidal aromatase inhibitors: a phase II, randomized, double-blind, placebo-contr. Menopause 2020;27(5):526-34. [DOI: 10.1097/GME.0000000000001497] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT01845649 {published data only}
- NCT01845649. Study to evaluate safety & efficacy of WC3011 in postmenopausal women with dyspareunia [A randomized, multicenter, double-blind, vehicle-controlled study to evaluate the safety and efficacy of WC3011 in postmenopausal women with dyspareunia]. https://www.clinicaltrials.gov/ct2/show/NCT01845649 (first posted 3 May 2013). [NCT: 01845649]
NCT02460302 {published data only}
- NCT02460302. Vaginal progesterone versus placebo for the treatment of vaginal atrophy [Vaginal progesterone versus placebo for the treatment of vaginal atrophy - a double blind randomized control trial]. https://clinicaltrials.gov/ct2/show/NCT02460302 (first posted 2 June 2015). [CTG: ]
NCT02834312 {published data only}
- NCT02834312. E4Relief (response to estetrol in life Improvement for menopausal-associated hot flushes) [A multicentre dose-finding, randomised, double-blind, placebo-controlled study to select the daily oral dose of estetrol (E4) for the treatment of vasomotor symptoms in post-menopausal women]. https://clinicaltrials.gov/ct2/show/NCT02834312 (first posted 15 July 2016). [NCT: 02834312]
NCT03363997 {published data only}
- NCT03363997. Pharmacokinetics and pharmacodynamics of 3 dosages of estriol after continuous vaginal administration for 21 days [A randomized, open-label trial to evaluate the pharmacokinetics and pharmacodynamics of 3 dosages of estriol after continuous vaginal administration for 21 days in healthy, post-menopausal women]. https://clinicaltrials.gov/ct2/show/NCT03363997 (first posted 6 December 2017). [CTG: ]
Pinkerton 2017 {published data only}
- Pinkerton JV, Bushmakin AG, Bobula J, Lavenberg J, Komm BS, Abraham L. Time to first occurrence of breast pain and vaginal bleeding in phase 3 trials of CE/BZA. Menopause 2017;24:1372-7. [DOI] [PubMed] [Google Scholar]
Tanmahasamut 2020 {published data only}
- Tanmahasamut P, Jirasawas T, Laiwejpithaya S, Areeswate C, Dangrat C, Silprasit K. Effect of estradiol vaginal gel on vaginal atrophy in postmenopausal women: a randomized double-blind controlled trial. Journal of Obstetrics and Gynaecology Research 2020;46(8):1425-35. [DOI: 10.1111/jog.14336] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT02668796 {published data only}
- NCT02668796. To study generic estradiol 10 mcg vaginal tablets in the treatment of vulvar and vaginal atrophy in post menopausal women. clinicaltrials.gov/ct2/show/NCT02668796 (first received 29 January 2016). [NCT02668796]
NCT02670785 {published data only}
- NCT02670785. A safety and efficacy study of estradiol vaginal capsule in postmenopausal women with vulvovaginal atrophy. clinicaltrials.gov/ct2/show/NCT02670785 (first received 2 February 2016). [NCT02670785]
NCT02859285 {published data only}
- NCT01822288. The impact of hormone therapy on lower urinary tract symptoms, sexual function and psychosomatic disorderA Study Evaluating the Effects of Topical Clitoral Estradiol Cream in Post Menopausal Women. clinicaltrials.gov/ct2/show/NCT01822288 (first received 2 April 2013). [NCT01822288]
NCT03116022 {published and unpublished data}
- NCT03116022. Use of estriol at distal third of vagina improving coital pain in post-menopause women. clinicaltrials.gov/ct2/show/NCT03116022 (first received 14 April 2017). [NCT03116022.]
Additional references
Alexander 2004
- Alexander JL, Kotz K, Dennerstein L, Kutner SJ, Wallen K, Notelovitz M. The effects of postmenopausal hormone therapies on female sexual functioning: a review of double-blind, randomized controlled trials. Menopause 2004;11(6 Pt 2):749-65. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ali 2020
- Ali M, Ahmed H, Smail L. Psychological climacteric symptoms and attitudes toward menopause among Emirati women. International Journal of Environmental Research and Public Health 2020;13(14):5028. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Avis 2015
- Avis NE, Crawford SL, Greendale G, Bromberger JT, Everson-Rose SA, Gold EB, et al. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Internal Medicine 2015;175(4):531-9. [DOI: 10.1001/jamainternmed.2014.8063] [DOI] [PMC free article] [PubMed] [Google Scholar]
Avis 2017
- Avis NE, Colvin A, Karlamangla AS, Crawford S, Hess R, Waetjen LE, et al. Change in sexual functioning over the menopausal transition: results from the Study of Women's Health Across the Nation. Menopause 2017;24(4):3379-90. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Basson 2000
- Basson R, Berman J, Burnett A, Derogatis L, Ferguson D, Foucroy J, et al. Report of the international consensus development conference on female sexual dysfunction: definitions and classifications. Journal of Urology 2000;163(3):888-93. [PMID: ] [PubMed]
Biehl 2019
Cain 2003
- Cain VS, Johannes CB, Avis NE, Mohr B, Schocken M, Skurnick J, et al. Sexual functioning and practices in a multi-ethnic study of midlife women: baseline results from SWAN. Journal of Sex Research 2003;40:266-76. [PMID: ] [DOI] [PubMed] [Google Scholar]
Clayton 2010
- Clayton AH. The pathophysiology of hypoactive sexual desire disorder in women. International Journal of Gynaecology and Obstetrics 2010;110(1):7-11. [DOI: 10.1016/j.ijgo.2010.02.014] [DOI] [PubMed] [Google Scholar]
da Silva Lara 2009a
- da Silva Lara LA, Useche B, Rosa E Silva JC, Ferriani RA, Reis RM, Sá MF, et al. Sexuality during the climacteric period. Maturitas 2009;62(2):127-33. [PMID: ] [DOI] [PubMed] [Google Scholar]
da Silva Lara 2009b
- da Silva Lara LA, da Silva AR, Rosa ES, Chaud F, Silva-de-Sa MF, Meireles ES, Sa Rosa ES. Menopause leading to increased vaginal wall thickness in women with genital prolapse: impact on sexual response. Journal of Sexual Medicine 2009;6(11):3097-110. [DOI: 10.1111/j.1743-6109.2009.01407.x] [DOI] [PubMed] [Google Scholar]
Davis 2009
- Davis SR. Understanding female sexual function. Menopause 2009;16(3):425-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Deeks 2022
- Deeks JJ, Higgins JP, Altman DG editor(s). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Dennerstein 2003
- Dennerstein L, Alexander JL, Kotz K. The menopause and sexual functioning: a review of the population-based studies. Annual Review of Sex Research 2003;14:64-82. [PMID: ] [PubMed] [Google Scholar]
Dimenäs 1990
- Dimenäs E. The SSA-profile, an instrument for assessment of subjective symptoms among hypertensives. Scandinavian Journal of Primary Health Care. Supplement 1990;1:27-30. [PMID: ] [PubMed] [Google Scholar]
Few 1997
Flores 2021
- Flores VA, Pal L, Manson JE. Hormone therapy in menopause: concepts, controversies, and approach to treatment. Endocrine Reviews 2021;42(6):720-52. [DOI: 10.1210/endrev/bnab011] [DOI] [PubMed] [Google Scholar]
Formoso 2012
- Formoso G, Perrone E, Maltoni S, Balduzzi S, D'Amico R, Bassi C, et al. Short and long term effects of tibolone in postmenopausal women. Cochrane Database of Systematic Reviews 2012, Issue 2. Art. No: CD008536. [DOI: 10.1002/14651858.CD008536.pub2] [DOI] [PubMed] [Google Scholar]
Gass 2019
- Gass M, Larson J, Cochrane B, Manson JE, Lane B, Barnabei V, et al. Sexual activity and vaginal symptoms in the postintervention phase of the Women's Health Initiative Hormone Therapy Trials. Menopause 2019;25(3):252-64. [DOI: 10.1097/GME.0000000000000994] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gold 2000
- Gold EB, Sternfeld B, Kelsey JL, Brown C, Mouton C, Reame N, et al. Relation of demographic and lifestyle factors to symptoms in a multi-racial/ethnic population of women 40-55 years of age. American Journal of Epidemiology 2000;52(5):463-73. [PMID: ] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed September 2021. Hamilton (ON): McMaster University y Evidence Prime. Available at gradepro.org.
Greene 2008
- Greene JG. Constructing a standard climacteric scale. Maturitas 2008;61(1-2):78-84. [DOI: 10.1016/j.maturitas.2008.09.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG, Sterne JA editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from https://training.cochrane.org/handbook/archive/v5.1/.
Higgins 2022
- Higgins JP, Li T, Deeks JJ editor(s). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from https://training.cochrane.org/handbook/current/chapter-06.
Hilditch 1996
- Hilditch JR, Lewis J, Peter A, Maris B, Ross A, Franssen E, Guyatt GH, Norton PG, Dunn E. A menopause-specific quality of life questionnaire: development and psychometric properties. Maturitas 1996;24(3):161-75. [DOI: 10.1016/s0378-5122(96)82006-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hull 1999
Hunter 2000
- Hunter, M. The Women's Health Questionnaire (WHQ): the development, standardization and application of a measure of mid-aged women's emotional and physical health. Quality of Life Research 2000;9 Suppl 1:733–8. [DOI: 10.1023/A:1008973822876] [DOI] [Google Scholar]
Jacobs 2011
- Jacobs E, D'Esposito M. Estrogen shapes dopamine-dependent cognitive processes: implications for women's health. Journal of Neuroscience 2011;31(14):5286-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kenemans 2005
- Kenemans P, Speroff L, International Tibolone Consensus Group. Tibolone: clinical recommendations and practical guidelines. A report of the International Tibolone Consensus Group. Maturitas 2005;51(1):21-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kim 2015
- Kim H-K, Kang S-Y, Chung Y-J, Kim J-H, Kim M-R. The recent review of the genitourinary syndrome of menopause. Journal of Menopausal Medicine 2014;21(2):65-71. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lara 2009
- Lara LA, Useche B, Ferriani RA, Reis RM, Sá MF, Freitas MM, et al. The effects of hypoestrogenism on the vaginal wall: interference with the normal sexual response. Journal of Sexual Medicine 2009;6(1):10-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lefebvre 2022
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated September 2022). Cochrane, 2022. Available from https://training.cochrane.org/handbook/current/chapter-04.
Lethaby 2016
- Lethaby A, Reuben O, Helen R. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database of Systematic Reviews 2016, Issue 8. Art. No: CD001500. [DOI: 10.1002/14651858.CD001500.pub3] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lonnèe‐Hoffmann 2014
- Lonnèe-Hoffmann R. Sexual function in the late postmenopause: a decade of follow-up in a population-based cohort of Australian women. Journal of Menopausal Medicine 2014;11(8):2029-38. [PMID: ] [DOI] [PubMed] [Google Scholar]
MacLennan 2004
- MacLennan AH, Broadbent JL, Lester S, Moore V. Oral oestrogen and combined oestrogen/progestogen therapy versus placebo for hot flushes. Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No: CD002978. [DOI: 10.1002/14651858.CD002978.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
McCabe 2016a
- McCabe MP, Sharlip ID, Lewis R, Atalla E, Balon R, Fisher AD, et al. Incidence and prevalence of sexual dysfunction in women and men: a consensus statement from the Fourth International Consultation on Sexual Medicine 2015. Journal of Sexual Medicine 2016;13(2):144-52. [DOI: 10.1016/j.jsxm.2015.12.034] [DOI] [PubMed]
McCabe 2016b
- McCabe MP, Sharlip ID, Atalla E, Balon R, Fischer AD, Laumann E, et al. Definitions of sexual dysfunctions in women and men: a consensus statement from the fourth International Consultation on Sexual Medicine 2015. Journal of Sexual Medicine 2016;13(2):135–43. [DOI] [PubMed] [Google Scholar]
McCoy 1985
- McCoy NL, Davidson JM. A longitudinal study of the effects of menopause on sexuality. Maturitas 1985;7(3):203-10. [DOI: 10.1016/0378-5122] [PMID: ] [DOI] [PubMed] [Google Scholar]
McCoy 2000
- McCoy, N. McCoy female sexuality questionnaire. Quality of Life Research 2000;9:739–45. [DOI: 10.1023/A:1008925906947] [DOI] [Google Scholar]
McGahuey 2000
- McGahuey CA, Gelenberg AJ, Laukes CA, Moreno FA, Delgado PL, McKnight KM, et al. The Arizona Sexual Experience Scale (ASEX): reliability and validity. Journal of Sex and Marital Therapy 2000;26(1):25-40. [DOI: 10.1080/009262300278623] [PMID: ] [DOI] [PubMed] [Google Scholar]
McHorney 1994
- McHorney CA, Ware JE Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care 1994;32(1):40-66. [DOI: 10.1097/00005650-199401000-00004] [PMID: ] [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, for the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Monteleone 2018
NAMS 2012
- North American Menopause Society. The 2012 hormone therapy position statement of: The North American Menopause Society. Menopause 2012;19(3):257-71. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
NAMS 2017
- North American Menopause Society. The 2017 hormone therapy position statement of The North American Menopause Society. Menopause (New York, N.Y.) 2017;24(7):728-53. [DOI: 10.1097/gme.0000000000000921] [DOI] [PubMed] [Google Scholar]
Nappi 2009a
- Nappi RE, Lachowsky M. Menopause and sexuality: prevalence of symptoms and impact on quality of life. Maturitas 2009;63(2):138-41. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nappi 2009b
- Nappi RE, Polatti F. The use of estrogen therapy in women's sexual functioning (CME). Journal of Sexual Medicine 2009;6(3):618-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nicolosi 2004
- Nicolosi A, Laumann EO, Glasser DB. Sexual behavior and sexual dysfunctions after age 40: the global study of sexual attitudes and behaviors. Urology 2004;64(5):991-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Norman 2003
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Medical Care 2003;41:582-92. [PMID: ] [DOI] [PubMed] [Google Scholar]
Portman 2014b
- Portman DJ, Gass ML, Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women's Sexual Health and the North American Menopause Society. Menopause 2014;21(10):1063-8. [PMID: ] [DOI] [PubMed]
Review Manager 2020 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.4. Copenhagen: The Cochrane Collaboration, 2020.
Roney 2013
- Roney JR, Simmons ZL. Hormonal predictors of sexual motivation in natural menstrual cycles. Hormones and Behavior 2013;63(4):636-45. [PMID: 10.1016/j.yhbeh.2013.02.013] [PMID: PMID: 23601091] [DOI] [PubMed] [Google Scholar]
Rosen 2000
- Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D'Agostino R Jr. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. Journal of Sex and Marital Therapy 2000;26(2):191-208. [DOI: 10.1080/009262300278597] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rosen 2012
- Rosen RC, Maserejian NN, Connor MK, Krychman ML, Brown CS, Goldstein I. Characteristics of premenopausal and postmenopausal women with acquired, generalized hypoactive sexual desire disorder: the Hypoactive Sexual Desire Disorder Registry for women. Menopause 2013;19(4):396-405. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rust 1986
- Rust J, Golombok S. The GRISS: a psychometric instrument for the assessment of sexual dysfunction. Archives of Sexual Behavior 1986;15(2):157-65. [DOI: 10.1007/BF01542223] [PMID: ] [DOI] [PubMed] [Google Scholar]
Santen 2010
- Santen RJ, Allred DC, Ardoin SP, Archer DF, Boyd N, Braunstein GD, et al, Endocrine Society. Postmenopausal hormone therapy: an Endocrine Society scientific statement. Journal of Clinical Endocrinology and Metabolism 2010;95(7 Suppl 1):1-66. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Santoro 2016
- Santoro N, Worsley R, Miller KK, Parish SJ, Davis SR. Role of estrogens and estrogen-like compounds in female sexual function and dysfunction. Journal of Sexual Medicine 2016;13(3):305-16. [PMID: ] [DOI] [PubMed] [Google Scholar]
Schünemann 2021a
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook/archive/v6.2/chapter-14.
Schünemann 2021b
- Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from https://training.cochrane.org/handbook/archive/v6.2/chapter-15. [AVAILABLE FROM: www.training.cochrane.org/handbook]
Simon 2011
- Simon JA. Identifying and treating sexual dysfunction in postmenopausal women: the role of estrogen. Journal of Women's Health 2011;20(10):1453-65. [PMID: ] [DOI] [PubMed] [Google Scholar]
Simon 2018
- Simon JA, Davis SR, Althof SE, Chedraui P, Clayton AH, Kingsberg SA, et al. Sexual well-being after menopause: an International Menopause Society White Paper. Climacteric 2018;21(5):415-27. [DOI: 10.1080/13697137.2018.1482647] [PMID: PMID: 29987939] [DOI] [PubMed] [Google Scholar]
Somboonporn 2005
- Somboonporn W, Bell RJ, Davis SR. Testosterone for peri and postmenopausal women. Cochrane Database of Systematic Reviews 2005, Issue 4. Art. No: CD004509. [DOI: 10.1002/14651858.CD004509.pub2] [DOI] [PubMed] [Google Scholar]
STRAW 2008
- Stages of Reproductive Aging Workshop (STRAW) Practice committee of the American Society for Reproductive Medicine. The menopausal transition. Fertility and Sterility 2008;90 Suppl 3:S61-5. [DOI: 10.1016/j.fertnstert.2008.08.095] [DOI] [Google Scholar]
Suissa 1991
- Suissa S. Binary methods for continuous outcomes: a parametric alternative. Journal of Clinical Epidemiology 1991;44:241-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tabatabaeichehr 2018
- Tabatabaeichehr M, Mortazavi H, Abadi MH, Moayed L. Sexual desire and related factors in middle-aged and elderly married women: a cross-sectional study in Iran. Open Access Macedonian Journal Medical Sciences 2018;6(10):1906-11. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 1994
- Taylor JF, Rosen RC, Leiblum SR. Self-report assessment of female sexual function: psychometric evaluation of the Brief Index of Sexual Functioning for Women. Archives of Sexual Behavior 1994;23(6):627-43. [DOI: 10.1007/BF01541816] [PMID: ] [DOI] [PubMed] [Google Scholar]
Teng 1987
- Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. Journal of Clinical Psychiatry 1987 ;48(8):314-8. [PMID: ] [PubMed] [Google Scholar]
Walter 2001
- Walter SD. Number needed to treat (NNT): estimation of a measure of clinical benefit. Statistics in Medicine 2001;20:3947-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
Whiteley 2013
- Whiteley J, Wagner JS, Bushmakin A, Kopenhafer L, Dibonaventura M, Racketa J. Impact of the severity of vasomotor symptoms on health status, resource use, and productivity [I]. Menopause (New York, N.Y.) 2013;20(5):518-24. [DOI: 10.1097/GME.0b013e31827d38a5] [DOI] [PubMed] [Google Scholar]
Wierman 2010
- Wierman ME, Nappi RE, Avis N, Davis SR, Labrie F, Rosner W, et al. Endocrine aspects of women's sexual function. Journal of Sexual Medicine 2010;7:561-85. [PMID: ] [DOI] [PubMed] [Google Scholar]
Worsley 2017
- Worsley R, Bell RJ, Gartoulla P, Davis SR. Prevalence and predictors of low sexual desire, sexually related personal distress, and hypoactive sexual desire dysfunction in a community-based sample of midlife women. Journal of Sexual Medicine 2017;14(5):675-86. [DOI: 10.1016/j.jsxm.2017.03.254] [DOI] [PubMed]
Yazdanpanahi 2018
- Yazdanpanahi Z, Nikkholgh M, Akbarzadeh M, Pourahmad S. Stress, anxiety, depression, and sexual dysfunction among postmenopausal women in Shiraz, Iran. Journal of Family and Community Medicine 2018;25(2):82-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Nastri 2013
- Nastri CO, Lara LA, Ferriani RA, Rosa ES, Figueiredo JB, Martins WP. Hormone therapy for sexual function in perimenopausal and postmenopausal women. Cochrane Database of Systematic Reviews 2013, Issue 6. Art. No: CD009672. [DOI: 10.1002/14651858.CD009672.pub2] [DOI] [PubMed] [Google Scholar]


