Abstract
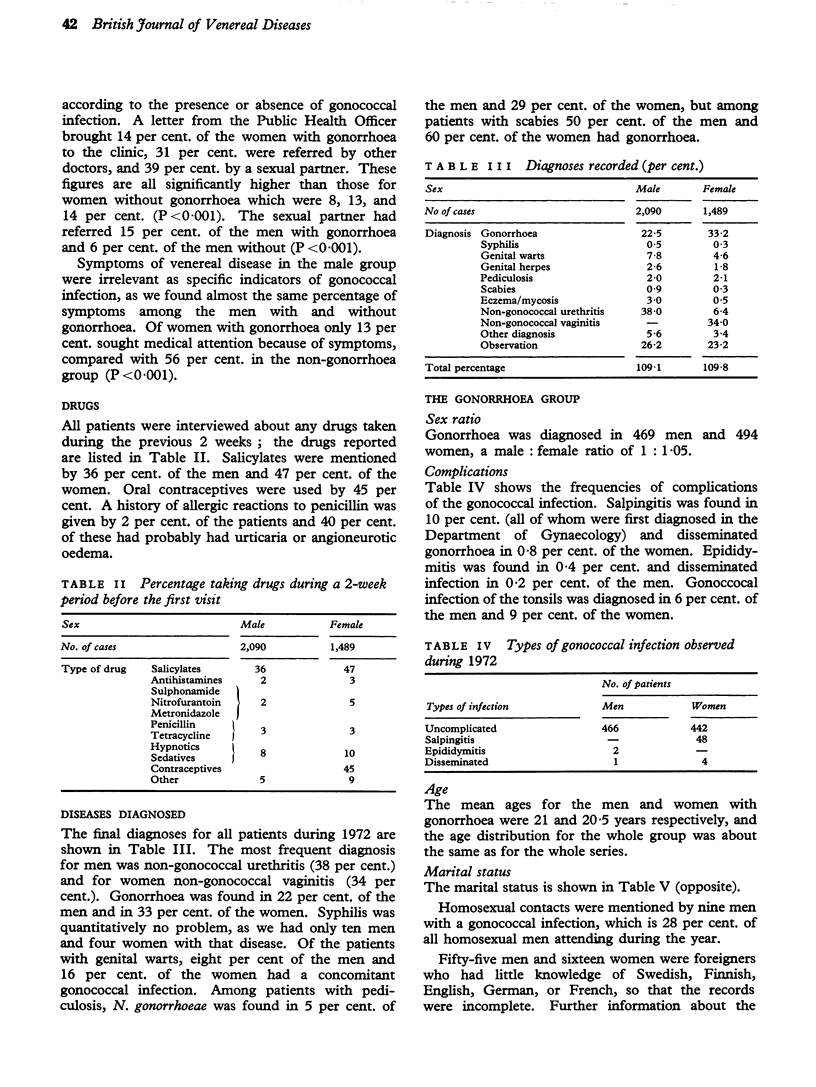
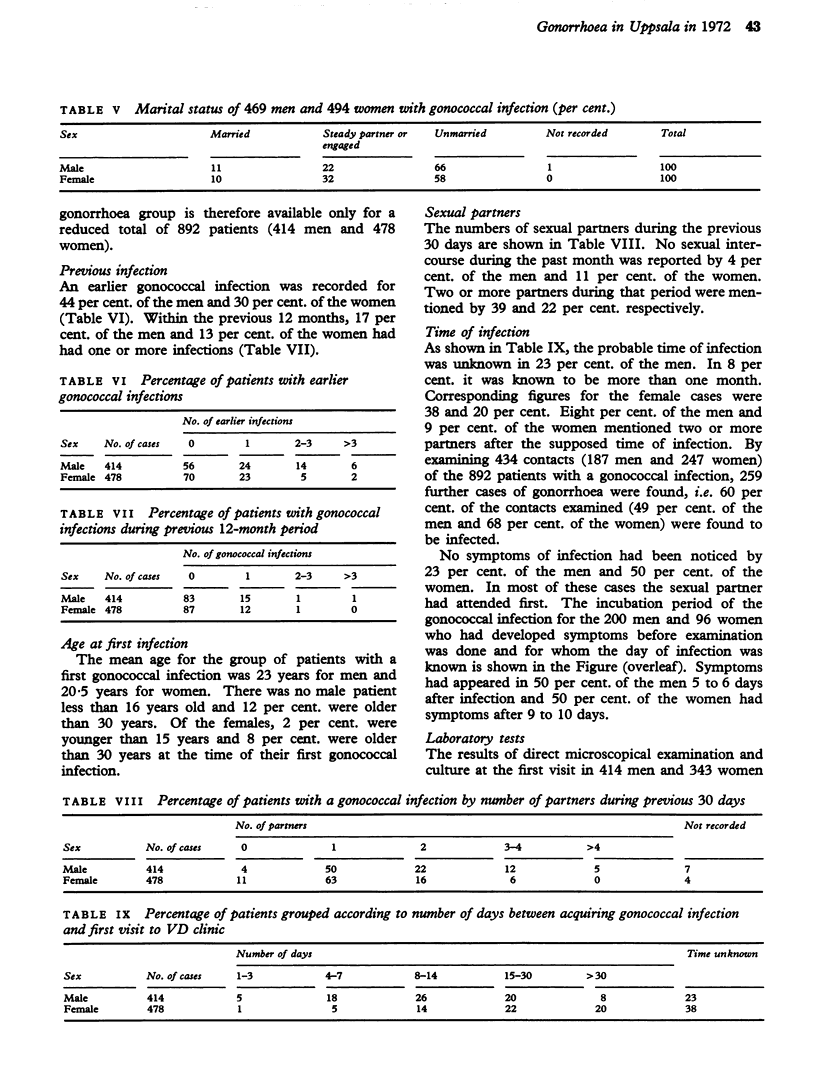
During 1972 a total of 2,090 men and 1,489 women were seen in the VD clinic in Uppsala, Sweden. The most frequent diagnosis among the men was non-gonococcal urethritis (38 per cent.) and among the women non-gonococcal vaginitis (34 per cent.), N. gonorrhoeae was found in 22 per cent. of the men and in 33 per cent. of the women, 68 per cent. of the men with gonorrhoea attended because of symptoms, but 67 per cent. of the men without gonococcal infections came for the same reason. 39 per cent. of the women with gonorrhoea attended after being told by their sexual partner; it was found that women coming because of symptoms were most likely to have non-gonococcal infection. Gonorrhoea without subjective symptoms was found in 23 per cent. of the men and 50 per cent. of the women. Gonorrhoea was found in association with scabies in 9 out of 18 men and in 3 out of 5 women. A rising incidence of pharyngeal gonococcal infections has been noticed at the clinic and the figures for 1972 were 6 per cent. of the men and 9 per cnet. of the women with gonorrhoea. The route of infection was usually oro-genital contact, but in some cases other routes had to be considered. It was not possible to define a promiscuous group of patients suitable for a planned study of prophylactic treatment, as only 2 per cent. of the men and 1 per cent. of the women had had nore than one gonococcal infection during the preceding year. The standard treatment for genital gonorrhoea (ampicillin 2 times 1 g. orally with a 5-hour interval) was very satisfactory and gave a 98 per cent. cure rate. This was possible because there were few gonococcal strains with decreased panicillin sensitivity. There were considerable problems in treating the pharyngeal infections, the standard treatment failing in 61 per cent.
Full text
PDF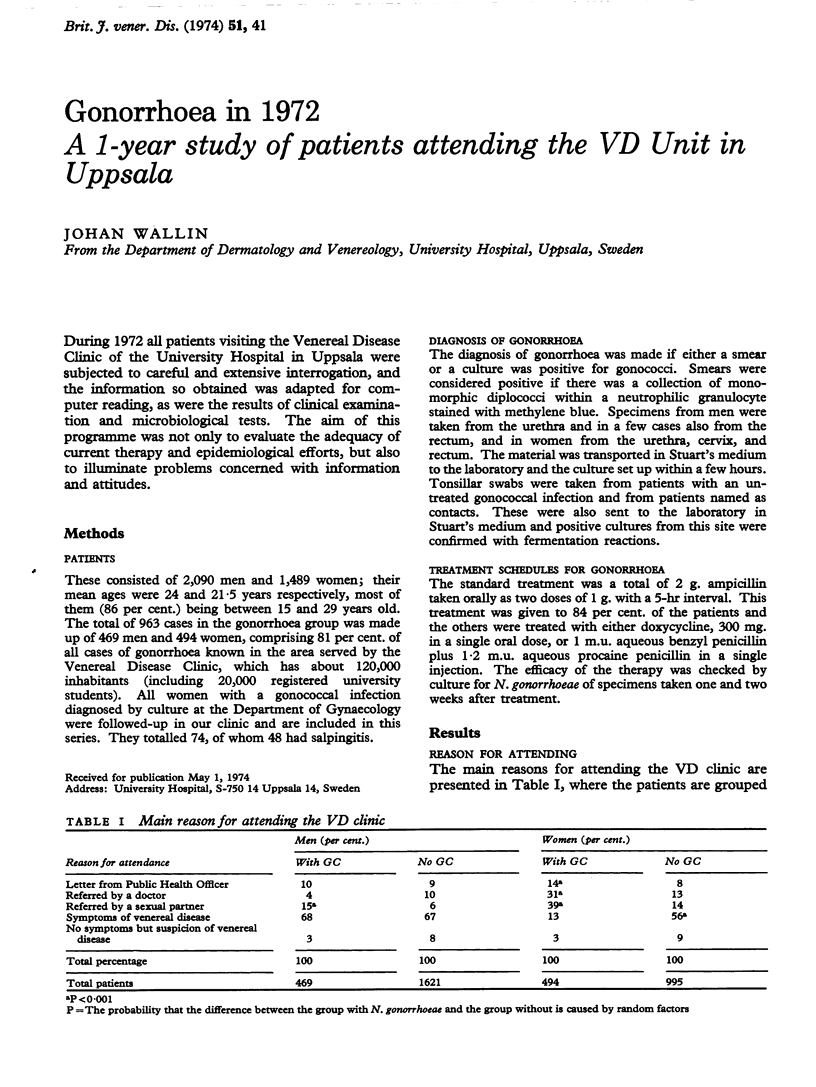
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barr J., Danielsson D. Septic gonococcal dermatitis. Br Med J. 1971 Feb 27;1(5747):482–485. doi: 10.1136/bmj.1.5747.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bro-Jorgensen A., Jensen T. Gonococcal pharyngeal infections. Report of 110 cases. Br J Vener Dis. 1973 Dec;49(6):491–499. doi: 10.1136/sti.49.6.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher I., Morton R. S. Phthirus pubis infestation. Br J Vener Dis. 1970 Aug;46(4):326–329. doi: 10.1136/sti.46.4.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammar H., Ljungberg L. Factors affecting contact tracing of gonorrhoea. Acta Derm Venereol. 1972;52(3):233–240. [PubMed] [Google Scholar]
- Molin L. Gonorrhoea in 1968. Acta Derm Venereol. 1970;50(2):157–160. [PubMed] [Google Scholar]
- Rudolph A. H., Price E. V. Penicillin reactions among patients in venereal disease clinics. A national survey. JAMA. 1973 Jan 29;223(5):499–501. [PubMed] [Google Scholar]
- Stolz E., Schuller J. Gonococcal oro- and nasopharyngeal infection. Br J Vener Dis. 1974 Apr;50(2):104–108. doi: 10.1136/sti.50.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VANARSDEL P. P., Jr ALLERGIC REACTIONS TO PENICILLIN. JAMA. 1965 Jan 18;191:238–239. doi: 10.1001/jama.1965.03080030082012. [DOI] [PubMed] [Google Scholar]
- Wiesner P. J., Tronca E., Bonin P., Pedersen A. H., Holmes K. K. Clinical spectrum of pharyngeal gonococcal infection. N Engl J Med. 1973 Jan 25;288(4):181–185. doi: 10.1056/NEJM197301252880404. [DOI] [PubMed] [Google Scholar]