Abstract
Background:
Asbestosis is a prevalent worldwide problem, but scarce data sourced from developing countries are available. We describe the sociodemographic characteristics and patterns in the occurrence of care provided for asbestosis in Colombia during the periods 2010–2014 and 2015–2019 to establish the behavior, trends, and variables associated with concentrations among people attended by asbestosis.
Methods:
A retrospective descriptive study was carried out with data from the Integrated Social Protection Information System (SISPRO) for two 5-year periods. People attended by asbestosis (ICD-10: J61) were identified; the frequency of patient visits, sociodemographic characteristics, case distribution patterns, and trends in both five-year periods were described, as was the crude frequency (cFr, 95% CI) of asbestosis (1,000,000 people/year) in both five-year periods (cFr ratio, 95% CI).
Results:
During the period 2010–2019, 765 people attended by asbestosis were identified; there were 308 people attended by asbestosis between 2010–2014 (cFr: 2.20, 1.96–2.47), and ther were 457 people attended by asbestos between 2015–2019 (cFr: 3.14, 2.92–3.50). In both periods, the estimated cFr in men was nine times the estimated cFr in women. The cFr increased in the 2015–2019 period (cFr_ratio: 1.23, 1.06–1.43). Compared with the 2010–2014 period, the cFr of asbestosis increased in women (cFr_ratio: 1.44, 1.03–2.01), in the Andean (cFr_ratio: 1.61, 1.35–1.95) and Caribbean regions (cFr_ratio: 1. 66, 1.21–2.30), in the urban area (cFr_ratio: 1.24, 1.05–1.48), and in the age groups 45–59 years (cFr_ratio: 1.34, 1.001–1.79) and ≥60 years (cFr_ratio: 1.43, 1.13–1.83).
Discussion:
During two five-year periods, the cFr of asbestosis was higher in men; between the first and second five-year periods, it increased significantly, especially in urbanized geographic areas and in populations aged ≥45 years. The estimates possibly reflect the effect of disease latency or the expected impact of public health policies to monitor asbestos exposure and complications.
Keywords: Asbestosis, Colombia, Demographics, visits distribution, people attended by asbestosis
Introduction
Asbestosis is a public health problem with potentially catastrophic effects in terms of morbidity and quality of life, and the impact is long-term and has been documented in developed and industrially developing countries [1]. Due to the latent nature and the clinical presentation often in late stages of the disease, the characterization and identification of patterns of occurrence is essential to design preventive strategies and reduce the impact for health systems [2,3]. Persons with asbestosis have had sufficient exposure to significantly raise their risk of asbestos-related cancers.
Between 1990 and 2017, the worldwide occurrence of asbestosis increased by about 115%, the same as the incidence and prevalence, mainly in high-income countries (HIC) [4]. Heterogeneity in the estimation of incidence is high and is possibly due to the lack of epidemiological or public health studies in some countries, information biases (misclassification), underreporting, surveillance and monitoring problems in health data records, or lack of uniformity in the denominators (population or highly exposed subgroups) applied to make estimates [2,4,5,6,7].
The individual and community impact of complications associated with asbestosis was noted by the World Health Organization and the International Labor Organization, and research on exposure emerged simultaneously, revealing the latent risk in homes and industry, especially in low- and medium-income countries (LIC, MIC) that, to date, maintain unhealthy patterns of production, consumption, and final disposal of asbestos [8,9].
In Colombia, during the last decade, investigations emerged that documented the magnitude of exposure to asbestos and the effects on the health of workers, giving rise to legislative changes at the national level and prohibiting the exploitation, production, commercialization, import, and export of any asbestos variety [10,11,12,13]. However, there is still no documentation that describes the national epidemiological situation regarding asbestosis or other asbestos-related diseases in Colombia, which is the main source for making public health decisions and developing the commitments established in legislative matters.
High-income countries, not including the United States where asbestos is still a legal product, have used countrywide data to report on diseases caused by asbestos [4,8]. With the new ban in Colombia, we wish to have such data as well. Despite the chance of a misclassification bias in cases of asbestosis, the coding of the Disease Classification System (ICD-9, ICD-10) has made it possible to establish surveillance and monitoring systems to design policies aimed at controlling exposure, improving diagnostic methods, and to some extent preventing some long-term complications of asbestosis through smoking cessation, as well as flu and pneumonia vaccinations as secondary measures for patients [3,8,14]. There is really no effective treatment for asbestosis, only such secondary measures.
This research compares the epidemiological findings of asbestosis during two continuous five-year periods in Colombia (2010–2014, 2015–2019) and determines the frequency at the population level using the information contained in the database of the Integrated Social Protection Information System (SISPRO) [15].
Methods
Design, place of collection, and patients
A retrospective descriptive design was carried out using the ReCORD methodological standard [1]. In the database of SISPRO, records with code J61 (ICD-10, International Classification of Diseases) were identified, and information was collected on the occurrence of asbestosis in Colombia during two five-year periods, 2010–2014 and 2015–2019 [16]. The information in the SISPRO database is public and does not include data that individualizes patients with asbestosis; therefore, this research is classified as risk-free and did not require authorization by an ethics committee for research.
Database and variables
Annual data of sociodemographic variables contained in the morbidity SISPRO platform (these modules have no restrictions on data access) were collected, including the year of occurrence, age (grouped by age cohorts), sex, health insurance (contributory, subsidiary [charity], prepaid, and others), geographic location, clinical setting, and health service provided. For each variable, people’s frequency of being attended by asbestosis, the number of annual visits (medical care provided by physicians), and the intensity of care (visits per person) was obtained [34].
Analysis of data
The data were expressed in raw counts, proportions (percentage the number of people attended by asbestosis), and frequency (Crude rates [cFr]), estimated with the number of people attended by asbestosis (ICD-10: J61) in a specific period of time, divided by the number of visits to the whole health system in the same period of time and multiplied by 1,000,000 people (1,000,000 people year). The proportion of visits during the first period (2010–2014) was 42.8% to 60.5%, and during the second period (2015–2019), it was was 53.6% to 74% (OpenEpi, Version 3.01, released April 4 and revised April 6, 2013).
A Sankey plot (SankeyMATIC (BETA)) was used to identify case patterns between geopolitical regions and time periods. Subsequently, the risk of an asbestosis diagnosis was determined according to sociodemographic variables in the period 2015–2019, using as a reference the cFr estimated in the period 2010–2014. In addition, the risk of an asbestosis diagnosis in men was estimated semiannually in the years studied (OpenEpi, Version 3.01, released April 4 and revised April 6, 2013).
To identify patterns or clusters among people attended by asbestosis and the cFr of asbestosis between departments and years of study (2010–2019), a two-way cluster analysis was used. In addition, cFr of asbestosis were expressed in annual and five-year choropleth maps. Finally, to identify department groupings, an interactive cluster analysis was carried out between the cFr observed in the 2010–2014 period (x-axis) and the cFr observed in the 2015–2019 period (y-axis) (Orange Data Mining & Fruitful, Version 3.30.1).
Results
Frequency of asbestosis
During the period 2010–2019, 765 people attended by asbestosis were identified in the SISPRO database, with 308 in the period 2010–2014 (40.3%) and 457 in the period 2015–2019 (59.1%) (Tables 1 and 2).
Table 1.
General characteristics among patients with asbestosis, 2010–2014.
|
| ||||||
|---|---|---|---|---|---|---|
| VARIABLES | 2010 | 2011 | 2012 | 2013 | 2014 | PERIOD |
|
| ||||||
| Frequency rate | 2.28 | 2.76 | 1.92 | 2.04 | 3.71 | 2.20 |
|
| ||||||
| 95%, CI | 1.67–3.04 | 2.12–3.53 | 1.41–2.56 | 1.51–2.70 | 3.05–4.48 | 1.96–2.47 |
|
| ||||||
| People attended | 47 | 60 | 59 | 47 | 125 | 308 |
|
| ||||||
| Visits | 121 | 123 | 106 | 89 | 223 | 662 |
|
| ||||||
| Intensity † | 2.57 | 2.05 | 1.79 | 1.89 | 1.78 | 2.14 |
|
| ||||||
| Life stages, years | ||||||
|
| ||||||
| <1 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
|
| ||||||
| 1–5 | 2 (4.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (0.66) |
|
| ||||||
| 6–9 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
|
| ||||||
| 10–14 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (1.9) | 2 (0.66) |
|
| ||||||
| 15–18 | 1 (2.3) | 1 (1.7) | 0 (0.0) | 0 (0.0) | 7 (6.8) | 8 (2.7) |
|
| ||||||
| 19–26 | 1 (2.3) | 4 (6.8) | 0 (0.0) | 1 (2.2) | 10 (9.7) | 16 (5.4) |
|
| ||||||
| 27–44 | 13 (30.2) | 12 (20.2) | 9 (20.4) | 11 (23.9) | 26 (25.2) | 62 (21.0) |
|
| ||||||
| 45–59 | 15 (34.9) | 17 (28.8) | 14 (31.8) | 16 (34.8) | 35 (34.0) | 71 (24.1) |
|
| ||||||
| 60+ | 11 (25.6) | 25 (42.4) | 21 (47.7) | 18 (39.1) | 24 (23.3) | 99 (33.6) |
|
| ||||||
| Sex | ||||||
|
| ||||||
| Male | 39 (83.0) | 52 (86.7) | 44 (89.8) | 39 (83.0) | 80 (76.2) | 254 (82.5) |
|
| ||||||
| Female | 8 (17.0) | 8 (13.3) | 5 (10.2) | 8 (17.0) | 25 (23.8) | 54 (17.5) |
|
| ||||||
| Health insurance | ||||||
|
| ||||||
| Subsidiary | 6 (13.9) | 10 (16.9) | 6 (13.6) | 6 (13.0) | 48 (46.6) | 76 (25.8) |
|
| ||||||
| Contributory | 29 (67.4) | 43 (72.9) | 37 (84.1) | 40 (86.9) | 51 (49.5) | 200 (67.8) |
|
| ||||||
| Prepaid | 5 (11.6) | 1 (1.7) | 0 (0.0) | 0 (0.0) | 1 (0.9) | 7 (2.4) |
|
| ||||||
| Others | 3 (7.0) | 6 (10.1) | 3 (6.8) | 0 (0.0) | 4 (3.9) | 16 (5.4) |
|
| ||||||
| Geographic location | ||||||
|
| ||||||
| Urban | 29 (67.4) | 44 (74.6) | 34 (77.3) | 36 (78.3) | 64 (62.1) | 207 (70.2) |
|
| ||||||
| Rural | 3 (7.0) | 2 (3.4) | 1 (2.3) | 1 (2.2) | 18 (17.5) | 25 (8.5) |
|
| ||||||
| Clinical setting | ||||||
|
| ||||||
| Private clinics | 33 (76.7) | 43 (72.9) | 32 (72.7) | 35 (76.1) | 55 (53.4) | 198 (67.1) |
|
| ||||||
| Public hospitals | 10 (23.2) | 16 (27.1) | 9 (20.4) | 7 (15.2) | 47 (45.6) | 89 (30.2) |
|
| ||||||
| Health service provided | ||||||
|
| ||||||
| Ambulatory | 36 (83.7) | 49 (83.0) | 39 (88.6) | 40 (86.9) | 95 (92.2) | 259 (87.8) |
|
| ||||||
| Procedure | 9 (20.9) | 13 (22.0) | 7 (15.9) | 6 (13.0) | 16 (15.5) | 51 (17.3) |
|
| ||||||
| Emergencies | 1 (2.3) | 6 (10.1) | 2 (4.6) | 3 (6.5) | 2 (1.9) | 14 (4.7) |
|
| ||||||
| In-hospital | 2 (4.6) | 5 (8.5) | 1 (2.3) | 1 (2.3) | 3 (2.9) | 12 (4.1) |
|
| ||||||
Note: Frequency rate is per million people (cFr). Intensity: visits/patients assisted ratio.
Table 2.
General characteristics among people attended by asbestosis, 2015–2019.
|
| ||||||
|---|---|---|---|---|---|---|
| VARIABLES | 2015 | 2016 | 2017 | 2018 | 2019 | PERIOD |
|
| ||||||
| Frequency rate | 2.50 | 2.44 | 3.14 | 2.61 | 4.70 | 3.14 |
|
| ||||||
| 95%, CI | 1.93–3.18 | 1.86–3.15 | 2.53–3.87 | 2.09–3.22 | 4.04–5.45 | 2.92–3.50 |
|
| ||||||
| Patients assisted | 62 | 55 | 85 | 83 | 172 | 457 |
|
| ||||||
| Visits | 187 | 148 | 160 | 189 | 237 | 921 |
|
| ||||||
| Intensity † | 3.02 | 2.69 | 1.88 | 2.28 | 1.38 | 2.02 |
|
| ||||||
| Life cycle, years | ||||||
|
| ||||||
| <1 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
|
| ||||||
| 1–5 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
|
| ||||||
| 6–9 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
|
| ||||||
| 10–14 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
|
| ||||||
| 15–18 | 1 (1.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (1.7) | 4 (0.9) |
|
| ||||||
| 19–26 | 4 (6.5) | 1 (1.8) | 2 (2.4) | 5 (6.0) | 10 (5.8) | 22 (4.8) |
|
| ||||||
| 27–44 | 19 (30.6) | 11 (20.0) | 12 (14.1) | 17 (20.5) | 39 (22.7) | 98 (21.4) |
|
| ||||||
| 45–59 | 14 (22.6) | 18 (32.7) | 33 (38.8) | 21 (25.3) | 40 (23.3) | 126 (27.6) |
|
| ||||||
| 60+ | 24 (38.7) | 25 (45.5) | 38 (44.7) | 41 (49.4) | 81 (47.1) | 209 (45.7) |
|
| ||||||
| Sex | ||||||
|
| ||||||
| Male | 51 (82.3) | 51 (92.7) | 79 (92.9) | 69 (83.1) | 107 (62.2) | 357 (78.1) |
|
| ||||||
| Female | 11 (17.7) | 4 (7.3) | 6 (7.1) | 14 (16.9) | 65 (37.8) | 100 (21.9) |
|
| ||||||
| Health insurance | ||||||
|
| ||||||
| Subsidiary | 1 (1.6) | 11 (20.0) | 9 (10.6) | 19 (22.9) | 95 (55.2) | 135 (29.5) |
|
| ||||||
| Contributory | 43 (69.4) | 41 (74.5) | 73 (85.9) | 64 (77.1) | 75 (43.6) | 296 (64.8) |
|
| ||||||
| Pre-paid | 1 (1.6) | 1 (1.8) | 2 (2.4) | 0 (0.0) | 1 (0.6) | 5 (1.1) |
|
| ||||||
| Others | 17 (27.4) | 3 (5.5) | 1 (1.2) | 0 (0.0) | 2 (1.2) | 23 (5.0) |
|
| ||||||
| Geographic place | ||||||
|
| ||||||
| Urban | 46 (74.2) | 36 (65.5) | 65 (76.5) | 65 (78.3) | 149 (86.6) | 361 (79.0) |
|
| ||||||
| Rural | 5 (8.1) | 5 (9.1) | 5 (5.9) | 9 (10.8) | 13 (7.6) | 37 (8.1) |
|
| ||||||
| Clinical settings | ||||||
|
| ||||||
| Private clinics | 44 (71.0) | 42 (76.4) | 70 (82.4) | 67 (80.7) | 95 (55.2) | 318 (69.6) |
|
| ||||||
| Public hospitals | 18 (29.0) | 9 (16.4) | 13 (15.3) | 17 (20.5) | 55 (32.0) | 105 (23.0) |
|
| ||||||
| Health service provided | ||||||
|
| ||||||
| Ambulatory | 55 (88.7) | 52 (94.5) | 78 (91.8) | 71 (85.5) | 90 (52.3) | 346 (75.7) |
|
| ||||||
| Procedure | 14 (22.6) | 15 (27.3) | 19 (22.4) | 25 (30.1) | 95 (55.2) | 168 (36.8) |
|
| ||||||
| Emergencies | 1 (1.6) | 3 (5.5) | 2 (2.4) | 1 (1.2) | 0 (0.0) | 7 (1.5) |
|
| ||||||
| In-Hospital | 2 (3.2) | 1 (1.8) | 0 (0.0) | 0 (0.0) | 1 (0.6) | 4 (0.9) |
|
| ||||||
Note: Frequency is rate per million people. Intensity: visits/patients assisted ratio.
As would be expected with frequency, the people attended by asbestosis increased progressively from the beginning to the end of each period and the highest occurrence was identified in the years 2014 and 2019. However, the annual occurrence was grouped into the frequencies observed in the years 2010, 2011, 2012, 2013 and 2015; Another group was made up of the frequencies of the 2016–2018 triennium, and finally, with the occurrences of the years 2014 and 2019 (Figure 1, left half). Additionally, a progressive decrease was observed in the intensity of care/visits per person per year provided in each period studied (Tables 1 and 2).
Figure 1.
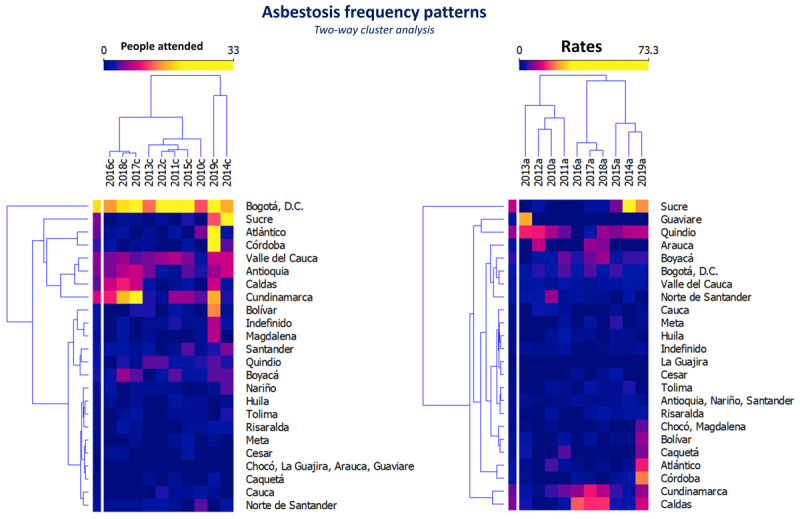
Asbestosis frequency grouped by year and department.
Two dendrograms in two-way cluster analysis are presented (years of study, departments of Colombia). On the left, they are grouped by occurrence among people attended by asbestosis, and on the right, they are grouped by cFr rate (per million people).
In the 2010–2014 period, about half of the people attended by asbestosis occurred in patients aged 27–59 years, about a third occurred in older people, and the remaining fraction was distributed in patients aged 15–26 years or in people attended by asbestosis where the age of the patients was unknown. However, as the population aged, half of people attended by asbestosis were now found in older people, in contrast to a third during the previous time period. In both periods, four out of every five people attended by asbestosis were men, two-thirds belonged to the contributory regime of insurance, at least one in four belonged to the subsidiary regime, and most were seen on an outpatient basis in urban areas or in private clinics (see Tables 1 and 2).
The majority of people attended by asbestosis were grouped in both study periods in the Andean region, followed by the Caribbean and Pacific regions. It was also observed that the occurrence among people attended by asbestosis in Bogotá was higher than that observed in other Colombian departments.
In addition, clusters of people attended by asbestosis were identified in Sucre, Atlántico, and Córdoba; Valle del Cauca, Antioquia, Caldas, and Cundinamarca; and Bolívar, Magdalena, Santander, Quindío, and Boyacá. In the remaining departments, the occurrence in the period 2010–2019 was similar (Figure 1, left half; Figure 2).
Figure 2.
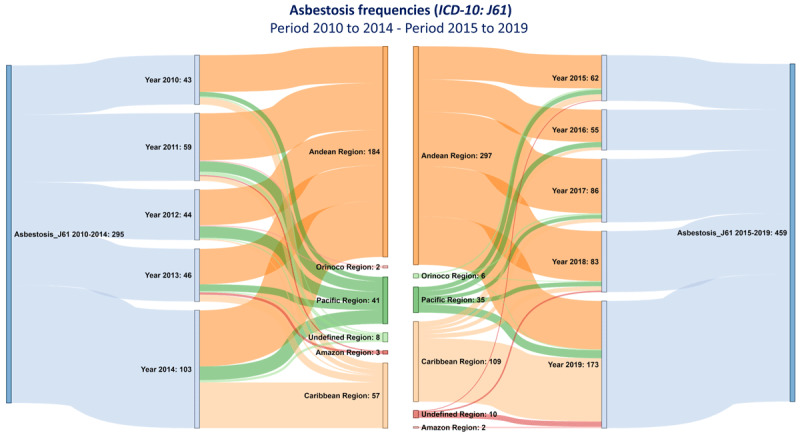
Annual and five-year occurrence of asbestosis in Colombian geopolitical regions.
The occurrence among people attended by asbestosis is presented by the study periods 2010–2014 (left) and 2015–2019 (right) and by geopolitical regions.
Asbestosis frequency estimated
The cFr among people attended by asbestosis per 1,000,000 people attended was higher in the period 2015–2019, and the frequency ratio showed an increase of 23% among people attended by asbestosis compared with that estimated for the period 2010–2014 (Figure 3, Figure S1). This 23% increase was greater than the five-year total population size increase.
Figure 3.
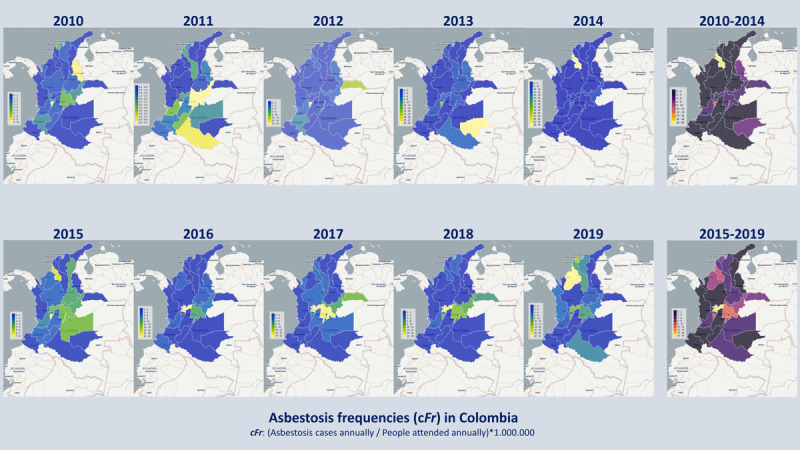
Annual and five-year dynamics of the frequency of asbestosis by departments of Colombia.
Choropleth maps of the estimated frequency of asbestosis are presented in each period studied, in the upper half for the period 2010–2014 and in the lower half for the period 2015–2019.
Clusters of disease were identified in the departments of Guaviare and Quindío during the period 2010–2013. This differs from the estimated cFr among people attended by asbestosis, as well as in the frequencies estimated in the departments of Quindío, Arauca, and Boyacá during the 2014–2019 period. In contrast, the estimated frequencies by departments of Chocó, Magdalena, Bolívar, Atlántico, Córdoba, Cundinamarca, and Caldas were grouped in 2019, and another group of frequencies was identified in the departments of Cundinamarca and Caldas during the period 2016–2018 (Figure 1).
During the 2010–2014 period, the cFr per 1,000,000 person-years ranged between 1.92 and 3.71, and in the entire period, it was estimated between 1.96 and 2.47 (95% CI). During the 2015–2019 period, the cFr per 1,000,000 person-years ranged between 2.44 and 4.70, and in the entire period, it was estimated between 2.92 and 3.50 (95% CI).
The estimated annual cFr among people attended by asbestosis by departments during the 2010–2014 period showed a highly variable behavior, contrary to what was observed in the 2015–2019 period, where high- or medium-frequency levels in chloroplethic maps (frequency intervals) were identified in distributed departments in the Andean region, the Caribbean, and specifically the Valle del Cauca (Pacific region) (Figure 3).
Increase in the frequency among people attended by asbestosis in the period 2015–2019
In both periods, the frequency of men treated for asbestosis was at least three times that of women. This ratio of asbestosis occurrence between men and women, with an effect directed at the former, was also evidenced when estimating the radius of cFr semiannually.
In Figure 4 and Table S1, it is evident that the estimated cFr in men was higher than in women in all the half-year periods. However, when estimating the cFr ratio of men and women in each period studied, only in women was a significant effect evidenced, with a 44% average risk excess among people attended by asbestosis during the period 2015–2019 (Table 3).
Figure 4.
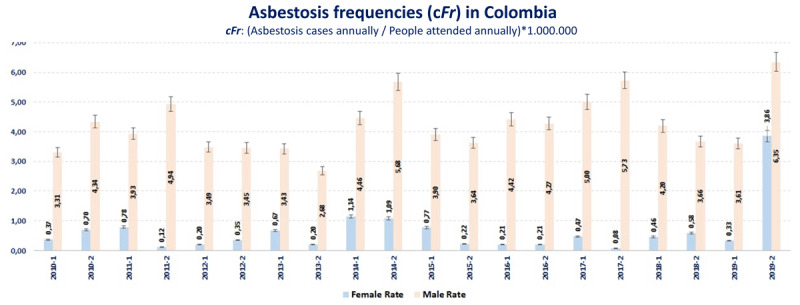
Semiannually estimated cFr of asbestosis by sex.
The crude cFr among people attended by asbestosis (y-axis) is compared between men and women on a six-monthly basis (x-axis). A cyclical behavior is observed in both men and women, and in all semesters the crude cFr among people attended by asbestosis was higher in men.
Table 3.
Sociodemographic characteristics and risk of asbestosis in the period 2015–2019.
|
| ||||
|---|---|---|---|---|
| PERIOD | PEOPLE ATTENDED BY ASBESTOSIS | PEOPLE ATTENDED | cFr (95%, CI) | cFr RATIO (95%, CI) |
|
| ||||
| 2010–2014 | ||||
|
| ||||
| Sex | ||||
|
| ||||
| Male | 254 | 63.192.758 | 4.02 (3.59–4.54) | Ref. |
|
| ||||
| Female | 54 | 92.580.322 | 0.58 (0.44–0.75) | Ref. |
|
| ||||
| Region | ||||
|
| ||||
| Andean | 184 | 64.383.129 | 2.85 (2.47–3.29) | Ref. |
|
| ||||
| Caribbean | 57 | 21.852.007 | 2.60 (1.99–3.35) | Ref. |
|
| ||||
| Pacific | 41 | 18.096.041 | 2.27 (1.65–3.04) | Ref. |
|
| ||||
| Orinoco | 2 | 2.698.003 | 0.74 (0.12–2.44) | Ref. |
|
| ||||
| Amazon | 3 | 1.109.908 | 2.70 (0.68–7.36) | Ref. |
|
| ||||
| Geographic place | ||||
|
| ||||
| Urban | 207 | 75.541.454 | 2.74 (2.38–3.13) | Ref. |
|
| ||||
| Rural | 25 | 13.154.729 | 1.90 (1.25–2.76) | Ref. |
|
| ||||
| Life cycle, years | ||||
|
| ||||
| 0–9 | 2 | 23.160.474 | 0.09 (0.01–0.28) | Ref. |
|
| ||||
| 10–18 | 10 | 17.396.011 | 0.57 (0.29–1.02) | Ref. |
|
| ||||
| 19–44 | 78 | 41.798.537 | 1.87 (1.48–232) | Ref. |
|
| ||||
| 45–59 | 71 | 17.884.745 | 3.97 (3.12–4.98) | Ref. |
|
| ||||
| 60+ | 99 | 14.440.953 | 6.85 (5.60–8.31) | Ref. |
|
| ||||
| 2015–2019 | ||||
|
| ||||
| Sex | ||||
|
| ||||
| Male | 384 | 84.889.904 | 4.52 (4.09–4.99) | 1.12 (0.96–1.32) |
|
| ||||
| Female | 101 | 120.576.485 | 0.84 (0.69–1.01) | 1.44 (1.03–2.01) |
|
| ||||
| Region | ||||
|
| ||||
| Andean | 297 | 64.234.231 | 4.62 (4.12–5.17) | 1.61 (1.35–1.95) |
|
| ||||
| Caribbean | 109 | 25.188.798 | 4.33 (3.57–5.20) | 1.66 (1.21–2.30) |
|
| ||||
| Pacific | 35 | 16.593.009 | 2.11 (1.49–2.90) | 0.93 (0.59–1.46) |
|
| ||||
| Orinoco | 6 | 2.265.331 | 2.65 (1.07–5.50) | 3.57 (0.76–25.7) |
|
| ||||
| Amazon | 2 | 965.220 | 2.07 (0.35–6.85) | 0.77 (0.09–5.15) |
|
| ||||
| Geographic place | ||||
|
| ||||
| Urban | 361 | 106.004.217 | 3.40 (3.06–3.77) | 1.24 (1.05–1.48) |
|
| ||||
| Rural | 37 | 19.009.660 | 1.94 (1.39–2.65) | 1.02 (0.61–1.72) |
|
| ||||
| Life cycle, years | ||||
|
| ||||
| 0–9 | 0 | 27.611.772 | – | – |
|
| ||||
| 10–18 | 4 | 20.798.824 | 0.19 (0.06–0.46) | 0.33 (0.09–1.04) |
|
| ||||
| 19–44 | 120 | 52.352.834 | 2.29 (1.91–2.73) | 1.23 (0.92–1.64) |
|
| ||||
| 45–59 | 126 | 23.746.715 | 5.31 (4.44–6.30) | 1.34 (1.001–1.79) |
|
| ||||
| 60+ | 209 | 21.279.942 | 9.82 (8.56–11.2) | 1.43 (1.13–1.83) |
|
| ||||
Note: The estimated cFr in the 2010–2014 period were used as a reference (Ref.) to estimate the cFr ratio.
Other sociodemographic characteristics in which an excess in the risk of an asbestosis diagnosis was estimated during the 2015–2019 period compared with what occurred during the 2010–2014 period were the occurrence in the Andean and Caribbean regions and in people in the ages ranges 45–59 and 60 and older.
Discussion
This research allowed us to describe the epidemiological situation among people attended by asbestosis in Colombia during the last two five-year periods, as well as trends and patterns grouped by social and demographic characteristics.
The epidemiology of asbestosis represents what has happened in various parts of Colombia; although there is no geographically specific available data, some parts of the population have more or less active or passive exposure [2,17].
The population with passive or active exposure is essential to describe the epidemiological situation of asbestosis, because they will be the denominators used to calculate occurrences (counts, proportions) or estimate frequencies (incidence, prevalence). However, the present investigation was developed using the number of people treated in the whole health system as denominators, proposing an assumption of active and passive exposure to asbestos in periods of time prior to the period of measurement of the occurrence [7,18,19]. In addition, it is worth mentioning that the use of administrative databases as an information resource to describe the epidemiological situation of asbestosis limits the chance of expressing the results in terms of incidences, because it is unknown whether the people attended by asbestosis reported per year are new patients or old patients seen for clinical follow-up.
In Colombia between the decades of the 1940s and 1970s, the growth of industrial production and routine use of materials, equipment, automotive parts, and other products derived from asbestos began [20]. The sources of production were oriented to growth in two domains, the asbestos cement and automotive industries, responding to a demand from migratory trends, urbanization, and the extension of road networks, which was accompanied by great transformations in social and economic matters, especially in departments located in the Andean and Caribbean region [20,21,22].
Research carried out in highly urbanized cities showed high concentrations of asbestos in the air, well above the permissible limits for breathing (0.0000–0.0043 fiber/cm3), especially in densely built-up areas where materials derived from asbestos cement were used [23]. In urban areas and in the Colombian Andean and Caribbean regions, the highest frequency among people attended by asbestosis were estimated in the two five-year periods and analyzed. Likewise, in these geopolitical regions are the cities with the highest demographic and industrial growth—factors that stimulated internal migration to main cities and influenced the level of urbanization [24,25].
During the post–World War II period, European countries and others that made up the “British Commonwealth of Nations” were left in a catastrophic situation in terms of housing and urban planning (the decade of the 1950s). As new housing was constructed and these countries reindustrialized, considerable use was made of asbestos cement and other asbestos materials [26]. In the long term, cohort studies demonstrated the risk of mesothelioma and other diseases related to active exposure to asbestos in a young, healthy adult population that migrated from Italy to Australia during the postwar period and that was looking for work and assigned to crocidolite exploitation and extraction [26,27].
This suggests that the occurrence of asbestosis and associated complications are strongly linked to processes of social and economic transformation that occurred at least three decades previously and mainly affect the actively exposed population. As noted above, since the 1950s, Colombia experienced gradual industrial and urban growth similar to what was described in the postwar period in Europe, which could lead to the increased risk of asbestosis, as well as the development of patterns and periodic and geographic clusters such as those described in the four-year period from 2010 to 2013 and the three-year periods from 2016 to 2018, and 2014, 2015, 2019, as well as observed in Sucre, Quindío, Cundinamarca, and Caldas. Some parts of Colombia are more likely to have disease due to mining or manufacturing activities. For example, in Cundinamarca is the town of Sibaté, with a well-studied asbestos situation [28].
Among the relevant results, an increase in the frequency by people attended by asbestosis was determined from one five-year period to another, with an increased risk in women, people aged 45 or over, and in populations located in the Andean and Caribbean regions. The increase in frequency between periods may be due to the accumulation of risk between five-year periods, the implementation or improvements in diagnostic processes and epidemiological surveillance, or cohort effects such as described in the Japanese population [29,30].
Among the departments of the Andean region, Bogotá stood out with the highest occurrence of people attended by asbestosis; however, this finding may be secondary to the effects of administrative directions given the availability of highly complex health institutions where patients with asbestos-related diseases are referred because they may require multidisciplinary management and work teams highly specialized in health issues, such as lung fibrosis or mesothelioma.
Although the estimated frequency among people attended by asbestosis in men was approximately nine times that estimated in women in each five-year period, the significant risk increase in women from one period to another is striking, contrary to what was observed in men. It is possible that occupational and nonoccupational exposure to asbestos, respectively, explain the frequency among people attended by asbestosis in men and the increased risk in women [4,5,6,7,9,30,31]. Work activities generally carried out by men, such as mining and construction, have been associated with asbestosis and diseases associated with asbestos exposure. In contrast, the risk of mesothelioma and death from mesothelioma is increased among women who lived near asbestos exploitation areas (i.e., mining), and that contamination of the surroundings areas could be the mechanism; it also could occur due to “familial” or “household” exposure [27,30,31].
Distribution patterns of disease could be influenced by availability of health care and the experience of practitioners [7,18]. Another limitation that frequently occurs in research on asbestosis and associated complications is the latency period for the disease. In this case, it affects the chance of identifying events that explain the estimated frequency, but it could also influence the estimated frequency in people aged 45 years or older [2,27,28,29,32,33]. Finally, it is possible that the international guidelines, adopted in Colombia and aimed at improving the diagnosis and monitoring of asbestosis, influenced the identification of cases and estimated frequency in specific geographic locations, as observed in the department of Sucre or during the five-year period 2015–2019.
We can conclude that between the five-year periods 2010–2014 and 2015–2019, the frequency among people attended by asbestosis in Colombia increased significantly from 2.2 to 3.14 cases per million people treated in the health system. The frequency was higher in men, in people aged 45 or older, and in highly urbanized geographic areas.
We consider that the occurrence of this disease should be actively monitored. Therefore, we are working on a project that contemplates the design of a clinical guideline for nonmalignant disease due to asbestos exposure, to contribute to the process of surveillance and monitoring of this public health problem. It would be also useful in the future to monitor the effects of asbestos use by establishing appropriate oversight such as a mesothelioma registry for all of Colombia.
Data Accessibility Statement
The research data can be found at the following link: https://doi.org/10.7910/DVN/LHFT4W [34].
Additional File
The additional file for this article can be found as follows:
Figure S1 and Table S1.
Funding Statement
This article is considered as a product within the framework of the project “Formulation of an integral strategy to reduce the impact on public and environmental health due to the presence of asbestos in the territory of the Department of Bolivar,” funded by the General System of Royalties of Colombia and identified with the code BPIN 2020000100366. The project is executed by the University of Cartagena, Colombia, and the Colombia Asbestos Free Foundation.
Funding Information
This article is considered as a product within the framework of the project “Formulation of an integral strategy to reduce the impact on public and environmental health due to the presence of asbestos in the territory of the Department of Bolivar,” funded by the General System of Royalties of Colombia and identified with the code BPIN 2020000100366. The project is executed by the University of Cartagena, Colombia, and the Colombia Asbestos Free Foundation.
Competing Interests
Most authors declare that they have no conflicts of interest. Arthur Leonard Frank regularly testifies in medical-legal cases primarily for plaintiffs.
Author Contributions
GAC, AAT, GV, MS, ALF, and BC designed the study and wrote the manuscript. GAC, AAT, GV, LMP, and GMA collected and analyzed the data. GAC, AAT, GV, ALF, MS, LMP, and BC wrote the article. All authors approved the final version of the manuscript.
References
- 1.Ramada Rodilla JM, Calvo Cerrada B, Serra Pujadas C, Delclos GL, Benavides FG. Fiber burden and asbestos-related diseases: an umbrella review. Gac Sanit. 2021: S0213–9111(21)00082-0. DOI: 10.1016/j.gaceta.2021.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhandari J, Thada PK, Sedhai YR. Asbestosis. [Updated September 24, 2021]. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555985/. [Google Scholar]
- 3.Marsili D, Terracini B, Santana VS, Ramos-Bonilla JP, Pasetto R, Mazzeo A, et al. Prevention of asbestos-related disease in countries currently using asbestos. Int J Environ Res Public Health. 2016; 13(5): 494. DOI: 10.3390/ijerph13050494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang M, Wang D, Gan S, Fan L, Cheng M, Yu L, et al. Increasing incidence of asbestosis worldwide, 1990–2017: Results from the Global Burden of Disease study 2017. Thorax. 2020; 75(9): 798–800. DOI: 10.1136/thoraxjnl-2020-214822 [DOI] [PubMed] [Google Scholar]
- 5.Emmett EA. Asbestos in high-risk communities: Public health implications. Int J Environ Res Public Health. 2021; 18(4): 1579. DOI: 10.3390/ijerph18041579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.West GH, Sokas RK, Welch LS. Change in prevalence of asbestos-related disease among sheet metal workers 1986 to 2016. Am J Ind Med. 2019; 62(7): 609–615. DOI: 10.1002/ajim.22998 [DOI] [PubMed] [Google Scholar]
- 7.Amodio E, Zarcone M, Casuccio A, Vitale F. Trends in epidemiology: The role of denominator fluctuation in population-based estimates. AIMS Public Health. 2021; 8(3): 500–506. DOI: 10.3934/publichealth.2021040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Furuya S, Chimed-Ochir O, Takahashi K, David A, Takala J. Global asbestos disaster. Int J Environ Res Public Health. 2018; 15(5): 1000. DOI: 10.3390/ijerph15051000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sen D. Working with asbestos and the possible health risks. Occup Med (Lond). 2015; 65(1): 6–14. DOI: 10.1093/occmed/kqu175 [DOI] [PubMed] [Google Scholar]
- 10.Lysaniuk B, Cely-García MF, Mazzeo A, Marsili D, Pasetto R, Comba P, et al. Where are the landfilled zones? Use of historical geographic information and local spatial knowledge to determine the location of underground asbestos contamination in Sibaté (Colombia). Environ Res. 2020; 191: 110182. DOI: 10.1016/j.envres.2020.110182 [DOI] [PubMed] [Google Scholar]
- 11.Colombia. Congreso de la República. Ley 1968 de 2019 (julio 11): Por el cual se prohibe el uso de asbesto en el territorio nacional y se establecen garantías de protección a la salud de los colombianos. Bogotá, DC: Diario Oficial 51011; julio 11 de 2019. [cited November 2, 2021]. Available from: https://bit.ly/2ZjBSLe. [Google Scholar]
- 12.Villamizar Guillermo, Navarro-Vargas José Ricardo. Asbestos ban. What comes after the adoption of Act 1968 of 2019? Rev. Fac. Med. 2019; 67(4): 569–569. Available from: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-00112019000400569&lng=en. DOI: 10.15446/revfacmed.v67n4.77744 [DOI] [Google Scholar]
- 13.Frank AL, Villamizar G, Bustillo Pereira JG. Radiographic changes in Colombian asbestos factory workers. Ann Glob Health. 2020; 86(1): 3. DOI: 10.5334/aogh.2634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edwards JK, Cole SR, Chu H, Olshan AF, Richardson DB. Accounting for outcome misclassification in estimates of the effect of occupational asbestos exposure on lung cancer death. Am J Epidemiol. 2014; 179(5): 641–647. DOI: 10.1093/aje/kwt309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sistema Integrado de Información de la Protección Social [Base de datos en internet]. Bogotá-Colombia: SISPRO; [actualizada en abril 2021; acceso 1 de abril de 2021]. Available at: https://www.sispro.gov.co/Pages/Home.aspx. [Google Scholar]
- 16.Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. RECORD Working Committee. The Reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. 2015; 12(10): e1001885. DOI: 10.1371/journal.pmed.1001885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noonan CW. Environmental asbestos exposure and risk of mesothelioma. Ann Transl Med. 2017; 5(11): 234. DOI: 10.21037/atm.2017.03.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cocoros NM, Ochoa A, Eberhardt K, Zambarano B, Klompas M. Denominators matter: Understanding medical encounter frequency and its impact on surveillance estimates using EHR data. EGEMS. 2019; 7(1): 31. DOI: 10.5334/egems.292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morrison CN, Rundle AG, Branas CC, Chihuri S, Mehranbod C, Li G. The unknown denominator problem in population studies of disease frequency. Spat Spatiotemporal Epidemiol. 2020; 35: 100361. DOI: 10.1016/j.sste.2020.100361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Idrovo AJ. La vergüenza y deuda pendiente de los efectos en salud relacionados con asbesto en Colombia. Rev. Univ. Ind. Santander. Salud. 2017; 49(1): 7–8. Available from: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0121-08072017000100007&lng=en. [Google Scholar]
- 21.Villamizar G. Asbesto en Colombia: Una verdad inocultable. En: Villamizar G, Camero G (coordinadores). Asbesto en Colombia, Fundamentos para el debate. Colombia: Bogotá; 2019: 131–44. [Google Scholar]
- 22.Udall A. Urbanization and rural labor supply: A historical study of Bogota, Colombia since 1920. Stud Comp Int Dev. 1980; 15(3): 70–83. DOI: 10.1007/BF02686467 [DOI] [PubMed] [Google Scholar]
- 23.Krakowiak E, Górny RL, Cembrzyńska J, Sakol G, Boissier-Draghi M, Anczyk E. Environmental exposure to airborne asbestos fibres in a highly urbanized city. Ann Agric Environ Med. 2009; 16(1): 121–128. [PubMed] [Google Scholar]
- 24.Bayram M, Bakan ND. Environmental exposure to asbestos: from geology to mesothelioma. Curr Opin Pulm Med. 2014; 20(3): 301–307. DOI: 10.1097/MCP.0000000000000053 [DOI] [PubMed] [Google Scholar]
- 25.Restrepo A. Aproximación a la planeación urbana en Colombia. Apuntes para su comprensión histórica. Estud. Demogr. Urbanos. 2019; 34(3): 665–690. Available at: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0186-72102019000300665&lng=es&nrm=iso. DOI: 10.24201/edu.v34i3.1879 [DOI] [Google Scholar]
- 26.Houston D, Ruming K. Suburban toxicity: A political ecology of asbestos in Australian cities. Geogr. Res. 2014; 52(4): 400–410. DOI: 10.1111/1745-5871.12075 [DOI] [Google Scholar]
- 27.Reid A, Merler E, Peters S, Jayasinghe N, Bressan V, Franklin P, et al. Migration and work in postwar Australia: Mortality profile comparisons between Australian and Italian workers exposed to blue asbestos at Wittenoom. Occup Environ Med. 2018; 75(1): 29–36. DOI: 10.1136/oemed-2017-104322 [DOI] [PubMed] [Google Scholar]
- 28.Ramos-Bonilla JP, Cely-García MF, Giraldo M, Comba P, Terracini B, Pasetto R, Marsili D, Ascoli V, Lysaniuk B, Rodríguez MC, Mazzeo A., Panqueva RDPL, Baldión M, Cañón D, García-Herreros LG, Pinzón B, Hernández LJ, Silva YA. An asbestos contaminated town in the vicinity of an asbestos-cement facility: The case study of Sibaté, Colombia. Environmental Research. 2019; 176: 108464. DOI: 10.1016/j.envres.2019.04.031 [DOI] [PubMed] [Google Scholar]
- 29.Chellini E, Battisti F, Pellegri M, Baldacci M, Sallese D, Cristaudo A, et al. Il percorso di sorveglianza sanitaria degli ex-esposti ad amianto in Toscana [Health surveillance program for workers with past asbestos exposure in Tuscany Region (Central Italy)]. Epidemiol Prev. 2018; 42(2): 171–177. DOI: 10.19191/EP18.2.P171.047. [DOI] [PubMed] [Google Scholar]
- 30.Zha L, Kitamura Y, Kitamura T, Liu R, Shima M, Kurumatani N, et al. Population-based cohort study on health effects of asbestos exposure in Japan. Cancer Sci. 2019; 110(3): 1076–1084. DOI: 10.1111/cas.13930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reid A, Heyworth J, de Klerk N, Musk AW. The mortality of women exposed environmentally and domestically to blue asbestos at Wittenoom, Western Australia. Occup Environ Med. 2008; 65(11): 743–749. DOI: 10.1136/oem.2007.035782 [DOI] [PubMed] [Google Scholar]
- 32.Panou V, Vyberg M, Meristoudis C, Hansen J, Bøgsted M, Omland Ø, et al. Non-occupational exposure to asbestos is the main cause of malignant mesothelioma in women in North Jutland, Denmark. Scand J Work Environ Health. 2019; 45(1): 82–89. DOI: 10.5271/sjweh.3756 [DOI] [PubMed] [Google Scholar]
- 33.Frost G. The latency period of mesothelioma among a cohort of British asbestos workers (1978–2005). Br J Cancer. 2013; 109(7): 1965–1973. DOI: 10.1038/bjc.2013.514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teherán AA. Replication data for: Epidemiology of asbestosis between 2010–2014 and 2015–2019 periods in Colombia: Descriptive Study. Harvard Dataverse, 2022; 1. DOI: 10.7910/DVN/LHFT4W [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 and Table S1.
Data Availability Statement
The research data can be found at the following link: https://doi.org/10.7910/DVN/LHFT4W [34].


