Abstract
Introduction: Urinary incontinence is one of the most common long term side effects after robotic prostatectomy (RALP), and significantly impacts patient quality of life. Pelvic floor muscle training (PFMT) has been a standard part of the urologist’s armamentarium for maximizing continence outcomes post-op. Recently, aerobic and resistance exercises have been described as improving functional outcomes post RALP. We performed a systematic review to determine the influence of exercise, in the form of PFMT, aerobic exercise, and resistance training, on incontinence post-RALP. Materials and Methods: This systematic review was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, with database searches performed on January 14, 2022 and again on August 10, 2022 to account for any new publications. The search identified 1675 papers. Of the 1675 papers, 1007 were found to be duplicates, leaving 668 total studies for screening. Of the 668 papers, nine met all inclusion criteria. Of the nine, four studies presented data from patients who had undergone RALP and were included in the final descriptive systematic review. Results: Sayilan et al. and Milios et al. showed postoperative PFMT and physical activity resulted in significantly improved continence outcomes at 1 and 6 months and 2, 6, and 12 weeks postoperatively, respectively. Heydenreich et al. combined PFMT with an oscillating rod therapy, which was found to significantly improve both postoperative urinary continence and health related quality of life compared to PFMT and relaxation techniques alone. On the contrary, Goode et al. examined delivery of exercise information and demonstrated no difference in continence outcomes between focused telehealth PFMT program and generic prostate cancer education. Conclusion: Pelvic floor muscle training, with or without adjunct therapies, results in improved continence outcomes post RALP. Supervised training programs may or may not accelerate this finding. There is no recent literature to support or refute the benefit of aerobic exercise or resistance training on reducing post-prostatectomy incontinence after RALP.
Keywords: Prostate cancer, robotic prostatectomy, continence, exercise, pelvic floor muscle training
Introduction
Prostate cancer (PCa) is the most common solid organ malignancy in men and the second most common cause of cancer-related deaths [1]. The standard treatments for localized and locally advanced PCa are either radical prostatectomy (RP) or radiation therapy (RT) with or without concomitant androgen deprivation therapy (ADT), although some higher risk patients may have a combination of both in a multidisciplinary approach [2]. Erectile dysfunction and urinary incontinence are the most common long term side effects post RP, and significantly impact patient quality of life [3].
The prevalence of urinary incontinence after RP ranges from 8-25% and usually arises from a combination of urethral sphincter deficiency and detrusor overactivity [4-6]. In the robotic era, only 17% of men have an immediate return of urinary continence after Foley catheter removal [7]. Although rates of urinary continence post-robotic-assisted radical prostatectomy (RALP) vary according to surgical technique, and most patients become continent by eight weeks post-op, postoperative urinary dysfunction is still the most significant predictor of health-related quality of life [8]. Despite this, studies have shown surgical teams are prone to under-counsel patients regarding the true impact of incontinence post-RALP during preoperative discussions [9].
As a result, there has been renewed interest in adjunctive therapies to reduce the prevalence of post-prostatectomy incontinence (PPI) and improve early return of urinary continence. Given its safety and cost effectiveness, pelvic floor muscle training (PFMT) has been a standard part of the urologist’s armamentarium for maximizing continence outcomes post-op. These exercises are often started preoperatively and are continued after surgery. Repeated contractions of the pelvic floor muscles, particularly the striated levator ani and coccygeus muscles, leads to increased pelvic floor strength and endurance that partially compensates for urethral sphincter insufficiency [10,11]. The role of aerobic exercise and resistance training on PPI has also been explored. The former aims to improve physiologic functional capacity, typically by incorporating activities using large muscle groups such as walking, running, and cycling [12,13]. The latter involves repeated movements against an external load or resistance, resulting in greater muscle strength and morphology [14,15].
This systematic review aims to determine the influence of exercise, in the form of PFMT, aerobic exercise, and resistance training, on incontinence post-RALP.
Methods
Literature search
This study was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [16]. A medical librarian (L.M.) conducted a comprehensive search to identify studies discussing the impact of PFMT, aerobic exercise, and resistance exercise on continence outcomes in patients post-RALP. Searches were conducted on January 14, 2022, in the following electronic databases: Ovid MEDLINE (Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R) 1946 to January 13, 2022); Ovid Embase (Embase Classic+Embase 1947 to 2022 January 13); and the Cochrane Central Register of Controlled Trials (CENTRAL). Searches were re-run in the same databases on August 10, 2022, to account for any recent publications. The search strategy included all appropriate controlled vocabulary and keywords for prostate cancer, robotic prostatectomy, pelvic floor muscle therapy, exercise, and continence. The full search strategy is available from authors by request. No date, language, or article type restrictions were included in the search strategy. Reference lists of included studies were reviewed to identify any additional studies missed by database searches. The search identified 1675 papers. Of the 1675 papers, 1007 were found to be duplicates, leaving 668 total studies for screening.
Inclusion criteria
Studies must have reported continence outcomes in adult PCa patients over 18 years of age. Patients must have undergone RALP with a subsequent clinic or home-based exercise intervention (aerobic exercise, resistance exercise, PFMT, or related intervention). Prospective studies published in English were included. The Eligibility PICOS Criteria are described in Table 1.
Table 1.
Eligibility per PICOS criteria
| Parameter | Description |
|---|---|
| P Population | Adult prostate cancer patients who underwent robotic-assisted radical prostatectomy |
| I Intervention | A clinic or home-based exercise intervention (aerobic exercise, resistance exercise, and pelvic floor muscle training or related intervention) |
| C Comparison | Standard care; group without the intervention of interest |
| O Outcomes | Continence measures as described by the study |
| S Study Design | Prospective studies |
Analysis
Electronic database search results were uploaded to Covidence v3018. The titles and abstracts were screened independently by two reviewers (K.P. and J.A.). Any disagreements were resolved by discussion, which included a separate third reviewer (S.R.). Once manuscripts passed the first review, a full-text review followed in the same manner with the same reviewers.
Of the 668 papers, 79 were evaluated for full text eligibility. Of the 79, four studies presented data from patients who had undergone RALP and met all other inclusion criteria and were included in the final descriptive systematic review. The full Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram outlining the study selection process is shown in Figure 1 [17].
Figure 1.
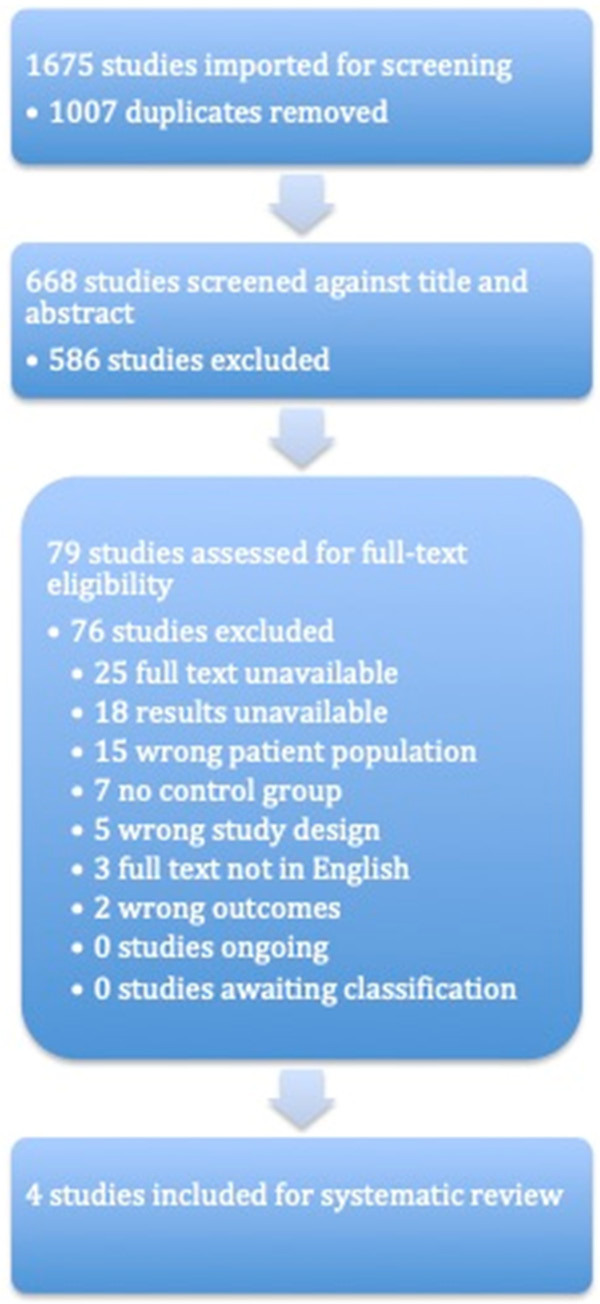
PRISMA flow diagram for study selection.
Cohen’s Kappa statistic was used to calculate the agreement level between reviewers to test the intercoder reliability of the screening process [18]. This statistic allows the comparison of inter-rater reliability between papers using relative observed agreement. The score ranges from -1 (complete disagreement) to +1 (full agreement). Both reviewers (K.P. and J.A.) agreed to include four studies after a full-text review, resulting in a Cohen’s Kappa statistic of 1.
Results
Sayilan et al. looked at the effect of PFMT on PPI at 1, 3, and 6 months post-RALP. Patients were randomized to receive standard PFMT (3 sets of 10 contractions held for 10 seconds with 10 seconds of rest between, with one set completed when supine, one while sitting, and the last while standing, for a total of 30 contractions daily) or given breathing exercises with no PFMT. Continence outcomes were measured primarily by the Incontinence Assessment Scale - International Consultation on Incontinence Questionnaire Short-Form (ICIQ-SF). Continence was also investigated by the self-reported number of pads used per week. ICIQ-SF scores were significantly lower for the PFMT group at 3- and 6-months suggesting improved continence and quality of life in the PFMT group. Significant differences in pad utilization were also seen between the two groups at one and six months post-op. At one month, over 80% of patients in the experimental group required less than one pad/day, compared to 23.3% of patients in the control group. Results were similarly different at six months, with 100% of patients in the experimental group requiring less than one pad a day compared to 53.3% of patients in the control group [19].
Milios et al. studied whether incorporating fast twitch muscle training into standard PFMT could improve continence outcomes post-RALP. The control group completed standard PFMT for a total of 30 contractions daily. The novel intervention required six sets of the standard exercises completed while standing with six additional sets of 10 contractions held for 1 second with 1 second of rest between (120 contractions daily). These outpatient interventions, standard and novel regimens, began five weeks prior to surgery and continued for 12 weeks postoperatively. Continence was measured by a 24-hour pad test at baseline, 2-, 6-, and 12 weeks postoperatively, with complete continence deemed a 24-hour pad test with 0 g weight change. After 12 weeks, 74% of the intervention group achieved continence with a 0 g difference in their 24-hour pad test, compared to only 43% in the control group. Although both groups showed improvements across the study period, ANOVA and post-hoc t-tests showed significant improvement in continence in the intervention group compared to the standard PFMT group, as seen by a decrease in 24-hour pad weight at all time points post-surgery. Most patients underwent robot-assisted procedures, but some also underwent open prostatectomy. These continence results held true even when adjusting for the surgical approach [20].
Heydenreich et al. investigated the effect of PFMT on continence outcomes after radical prostatectomy. This study compared three weeks of daily supervised PFMT (30 minutes daily) in an inpatient rehabilitation center with either oscillating rod treatment or relaxation therapy (both for an additional 30 minutes daily). Continence outcomes were measured by 1- and 24-hour pad tests. Improved continence outcomes were seen in both groups at the 1- and 24-hour pad tests between baseline and after three weeks of treatment, but the improvement was more significant for patients who underwent PFMT in combination with oscillating rod treatment. The benefit of the oscillating rod was also more significant for patients with more severe incontinence at baseline, defined as >50 g on the 1-hour pad test. These results were seen across all surgical approaches-open, laparoscopic, and robotic. Subgroup analysis was not performed to examine continence outcomes in patients only undergoing RALP [21].
Goode et al. examined the effectiveness of a telehealth-delivered perioperative PFMT program for men undergoing RP on post-prostatectomy incontinence. Men were randomized to receive a telehealth behavioral program with education, PFMT, bladder control techniques, or general prostate cancer education. These were completed for 1-4 weeks pre-procedure and eight weeks post-prostatectomy. The authors did not find significant differences in time to continence after six months. They also did not find any significant differences in secondary outcomes of incontinence severity, pad use, impact from incontinence on daily activities and quality of life, and perceived symptom improvement at 6, 9, and 12 months. Subgroup analysis between men who underwent robotic and open prostatectomy was not performed [22].
The characteristics of the four included studies are summarized in Table 2. These studies were assessed for quality using the PRISMA criteria for systematic reviews and meta-analyses and is reported in Table 3.
Table 2.
Characteristics and outcomes of included studies
| Study | Year | Study Type | Country | Treatment Intervention (Aerobic, Resistance, PFMT) | Control Regimen | Continence Definition | Cohort Size (n) | Mean Age | Assessment and Follow-Up | Key Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Milios J et al. | 2019 | Randomized Controlled Trial | Australia | PFMT | Usual Care | Collection of 24 h pad weight scores: | Total = 84 | 63 ± 7 years | Baseline | At 2 weeks post-op |
| • ‘mild’ <100 g, | Intervention = 45 | 2-week post | • Intervention = 14% dry | |||||||
| • ‘moderate’ 100-400 g, | Control = 39 | 6-week post | • Control = 4% dry | |||||||
| • ‘severe’ >400 g | 12-week post | At 6 weeks post-op | ||||||||
| • Intervention = 32% dry | ||||||||||
| • Control = 11% dry | ||||||||||
| At 12 weeks post-op | ||||||||||
| • Intervention = 74% dry | ||||||||||
| • Control = 43% dry | ||||||||||
| Sayilan A et al. | 2018 | Randomized Controlled Trial | Turkey | A standard perioperative physiotherapy program, consisting of PFMT and general physical activity | Usual care | Number of pads | Total = 60 | 63 ± 8.61 years | Month 0 | Significant difference in number of pads at 1 and 6 months |
| Intervention = 30 | Month 1 | |||||||||
| Control = 30 | Month 3 | |||||||||
| Month 6 | ||||||||||
| Heydenreich et al. | 2019 | Randomized Controlled Trial | Germany | PFMT and oscillating rod | PFMT with relaxation techniques | 1 and 24 hours pad test | Total = 184 | 64.1 ± 6.94 years | 3 weeks post | Intervention with significant reduction in urinary incontinence in 1 and 24 hour pad tests (P = 0.008, 2, P = 0.012) and improvement of HRQL (P = 0.017) |
| Quality of life | Intervention = 93 | |||||||||
| Control = 91 | ||||||||||
| Goode et al. | 2022 | Randomized Controlled Trial | United States | Telehealth behavioral program with education, PFMT, bladder control techniques | Telehealth general prostate cancer education | Time to continence following surgery measured by the ICIQ short form | Total = 175 | 61.7 | 6-month post | No significant differences in ICIQ scores |
| Intervention = 90 | 9-month post | |||||||||
| Control = 80 | 12-month post |
Table 3.
Quality assessment of included studies
| Assessment questions | Sayilan A et al. | Milios J et al. | Heydenreich et al. | Goode et al. | |
|---|---|---|---|---|---|
| 1 | Was the study described as randomized, a randomized trial, a randomized clinical trial or an RCT? | Yes | Yes | Yes | Yes |
| 2 | Was the method of randomization adequate (i.e., use of randomly generated assignment)? | Yes | Yes | Yes | Yes |
| 3 | Was the treatment allocation concealed (so that assignments could not be predicted)? | Yes | Yes | Yes | Yes |
| 4 | Were study participants and providers blinded to treatment group assignment? | No | No | No | No |
| 5 | Were the people assessing the outcomes blinded to the participants’ group assignments? | No | No | No | No |
| 6 | Were the groups similar at baseline on important characteristics that could affect outcomes (e.g., demographics. risk factors. comorbid conditions)? | Yes | Yes | Yes | Yes |
| 7 | Was the overall drop-out rate from the study at endpoint 20% or lower of the number allocated to treatment? | Yes | Yes | Yes | Yes |
| 8 | Was the differential drop-out rate (between treatment groups) at endpoint 15 percentage points or lower? | Yes | Yes | Yes | Yes |
| 9 | Was there high adherence to the intervention protocols for each treatment group? | Yes | Yes | Yes | Yes |
| 10 | Were other interventions avoided or similar in the groups (e.g., similar background treatments)? | Yes | Yes | Yes | Yes |
| 11 | Were outcomes assessed using valid and reliable measures. Implemented consistently across all study participants? | Yes | Yes | Yes | Yes |
| 12 | Did the authors report that the sample size was sufficiently large to be able to detect a difference in the main outcome between groups with at least 80% power? | Yes | No (>70% power) | Yes | Yes |
| 13 | Were all randomized participants analyzed in the group to which they were originally assigned, i.e., did they use an intention-to-treat analysis? | Yes | Yes | Yes | Yes |
| 14 | OVERALL STUDY QUALITY (POOR/FAIR/GOOD) | Fair (small sample size) | Fair (small sample size) | Good | Good |
Discussion
This review has demonstrated that there is a paucity of studies examining the effect of exercise on PPI in men undergoing RALP. Nevertheless, the trials highlighted have examined the specific role of PFMT with or without adjunctive therapies. Summarizing these four studies has provided three major takeaways for future researchers: 1) There is no current consensus on how best to measure continence outcomes, which hinders our ability to objectively compare interventions aimed at relieving PPI. 2) Although general aerobic exercise is mentioned to patients as an adjunctive therapy for improving continence post-RALP, no recent prospective trials have investigated its effectiveness. 3) Differences in duration from prostatectomy to rehabilitation, the number and duration of pelvic muscle contractions, and whether adjunctive tools are utilized may each influence continence outcomes in patients.
PPI can be measured using quantitative and qualitative tools. Quantitative scales include the 1-hour and 24-hour pad tests, as well as number of pads utilized. The timed pad tests are useful because they provide the amount of urine lost by weight difference in grams between the unused ‘dry’ pad and the used, ‘wet’ pad. The weight can be used to quantify the amount urine lost which can in turn be used to define or stage PPI. Relying on the reported number of pads utilized in a day is subject to multiple forms of bias - some patients may choose to change their pads more frequently at lesser degrees of urine leakage than others; others may drink significantly more water throughout a day, causing more frequent leakages and thus more pad changes; some individuals have access to home health aids to help them with scheduled voiding to help prevent leakages resulting in fewer pads utilized. Although this measure is easier to obtain, it is likely subject to more internal variability.
Although quantitative measures help us determine the amount of incontinence, they do not provide insight into its impact on quality of life. Qualitative measures aim to assess this by collecting patients’ self-described severity of leakage. These scales include the International Consultation on Incontinence Questionnaire - Short Form (ICIQ-SF) and the Functional Assessment of Cancer Therapy - Prostate (FACT-P) [4,23]. Three of the four studies incorporated these forms, with Goode et al. and Sayilan et al. utilizing ICIQ-SF and Heydenreich et al. using FACT-P. While quantitative descriptions of PPI are useful for clinical studies, the quality-of-life outcomes and degree of bother may prove to be better indicators for patient-centered care. Although two individuals may have similar incontinence based on quantitative measures, a patient with significantly more bother or significantly poorer quality-of-life may benefit from more aggressive interventions.
Classically, the approach to PPI has been to start physical therapy and anticholinergic medication after the procedure, with additional surgical procedures reserved for refractory incontinence. Most published studies have examined the effect of post-operative PFMT on the time to return to continence after open and laparoscopic prostatectomy. Although post-operative exercise and PFMT have demonstrated a beneficial effect on time to continence after RP, more focused research has investigated ways to improve outcomes [24,25]. PFMT regimens are now being explored as peri-operative interventions (pre- and post-operative utilization), even incorporating adjuvant tools such as biofeedback and ultrasound-guided muscle training to enhance their effectiveness [26-28]. Although the first meta-analysis examining the efficacy of pre-operative PFMT found no significant improvement in PPI 3-, 6-, or 12 months post-RP [29], a more recent meta-analysis found that pre-operative PFMT significantly reduced the incidence of short-term PPI at 1, 3, and 6 months. This difference was lost at 12 months [30].
Aside from utilizing PFMT in the pre-operative period, other studies have examined the effects of time to therapy and the incorporation of biofeedback into PFMT. A randomized controlled trial comparing two different PFMT regimens to no PFMT showed that those patients who underwent physiotherapy post-RP were more likely to be continent at one year than those without, with an odds ratio for continence recovery of 2.06 vs. 0.15 [31]. In their subgroup analysis, the authors found a higher percentage of patients undergoing physiotherapy without biofeedback were continent at one year after RP than those with biofeedback (92.3% vs. 29.1%). This is contrary to what a recent review highlighted, that biofeedback generally improves patient instruction on PFMT [26]. Baumann et al. also showed in a systematic review that supervised pelvic floor physiotherapy resulted in improved urinary continence post-RP compared to unsupervised physiotherapy, particularly in the first six months post-surgery [32]. The consensus in the literature is that early incorporation of PFMT results in an earlier return of continence post-RP, with direct supervision and biofeedback potentially augmenting this return [33].
The individual characteristics of each of the four studies included in this narrative review merit discussion. All studies except Heydenreich et al. compared PFMT alone to no PFMT. The latter included the additional use of an oscillating rod and compared this combination to PFMT alone. The definition of continence varied considerably across the studies. Sayilan et al. described continence as pad-free status, while Milios et al. used pad-free status or 0-gram net-pad weight. One and 24-hour pad tests were used by Heydenreich et al., while Goode et al. utilized the ICIQ-UI definition of continence. The length of follow-up also varied between studies. For example, while Heydenreich et al. touted the beneficial effect of PFMT with oscillating rod training on continence outcomes, their patients were only followed for three weeks, limiting the long-term applicability of their results. These patients also had inpatient, supervised, daily training to improve adherence, limiting generalizability to the outpatient setting. The authors also introduced confounders into their study design as the treatment group also experienced 30 minutes more of PFMT than the control group, making it difficult to determine whether oscillating rod adjunctive therapy contributed to the improved outcomes or the extra time of therapy.
While Milios et al. endeavored to determine whether recruitment of fast twitch muscle fibers to PFMT would improve PPI, the interventional exercises quadrupled the number of required pelvic floor contractions daily, making it impossible to determine if the incorporation of fast twitch exercises improved outcomes or if doubling the standard regimen improved outcomes. Goode et al. looked at the perioperative use of PFMT as delivered through telehealth and found that telehealth delivery of a PFMT regimen did not outperform a general PCa education program. This is notable since PFMT and Kegel exercises have become more “mainstream”. It begs the question of whether those men in the general education program came across videos or instructions online that prompted them to start pelvic floor exercises independently, thus nullifying any benefit of telehealth instruction seen in this study.
While ambitious in study design, our systematic review was limited by the dearth of prospective literature examining exercise therapy post-RALP as well as only fair quality of existing literature. PFMT and Kegel exercises have been widely described historically, and the four studies incorporated in the review solely compared various interventions incorporating PFMT. None of the included studies described aerobic or resistance exercise as therapeutic options for PPI. Additionally, while three of our included studies described the benefit of PFMT (with or without adjunct treatments) over no therapy, one appeared to question the utility of telehealth and supervised education.
Conclusion
Pelvic floor muscle training, with or without adjunct therapies, results in improved continence outcomes post RALP. Supervised training programs may or may not accelerate this finding. There is no recent literature to support or refute the benefit of aerobic exercise or resistance training on reducing post-prostatectomy incontinence after RALP.
Disclosure of conflict of interest
None.
References
- 1.American Cancer Society. Facts & Figures 2023. Atlanta, Ga: American Cancer Society; 2023. [Google Scholar]
- 2.Achard V, Panje CM, Engeler D, Zilli T, Putora PM. Localized and locally advanced prostate cancer: treatment options. Oncology. 2021;99:413–421. doi: 10.1159/000513258. [DOI] [PubMed] [Google Scholar]
- 3.Alivizatos G, Skolarikos A. Incontinence and erectile dysfunction following radical prostatectomy: a review. ScientificWorldJournal. 2005;5:747–758. doi: 10.1100/tsw.2005.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holm HV, Fosså SD, Hedlund H, Schultz A, Dahl AA. How should continence and incontinence after radical prostatectomy be evaluated? A prospective study of patient ratings and changes with time. J Urol. 2014;192:1155–1161. doi: 10.1016/j.juro.2014.03.113. [DOI] [PubMed] [Google Scholar]
- 5.Stanford JL, Feng Z, Hamilton AS, Gilliland FD, Stephenson RA, Eley JW, Albertsen PC, Harlan LC, Potosky AL. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the prostate cancer outcomes study. JAMA. 2000;283:354–360. doi: 10.1001/jama.283.3.354. [DOI] [PubMed] [Google Scholar]
- 6.Patel MI, Yao J, Hirschhorn AD, Mungovan SF. Preoperative pelvic floor physiotherapy improves continence after radical retropubic prostatectomy. Int J Urol. 2013;20:986–992. doi: 10.1111/iju.12099. [DOI] [PubMed] [Google Scholar]
- 7.Sammon JD, Sharma P, Trinh QD, Ghani KR, Sukumar S, Menon M. Predictors of immediate continence following robot-assisted radical prostatectomy. J Endourol. 2013;27:442–446. doi: 10.1089/end.2012.0312. [DOI] [PubMed] [Google Scholar]
- 8.Penson DF, Feng Z, Kuniyuki A, McClerran D, Albertsen PC, Deapen D, Gilliland F, Hoffman R, Stephenson RA, Potosky AL, Stanford JL. General quality of life 2 years following treatment for prostate cancer: what influences outcomes? Results from the prostate cancer outcomes study. J. Clin. Oncol. 2003;21:1147–1154. doi: 10.1200/JCO.2003.07.139. [DOI] [PubMed] [Google Scholar]
- 9.Trofimenko V, Myers JB, Brant WO. Post-prostatectomy incontinence: how common and bothersome is it really? Sex Med Rev. 2017;5:536–543. doi: 10.1016/j.sxmr.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 10.Anderson CA, Omar MI, Campbell SE, Hunter KF, Cody JD, Glazener CM. Conservative management for postprostatectomy urinary incontinence. Cochrane Database Syst Rev. 2015;1:CD001843. doi: 10.1002/14651858.CD001843.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang YC, Chang KV. Kegel Exercises. In: StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.; 2022. [Google Scholar]
- 12.Soriano-Maldonado A, Carrera-Ruiz Á, Díez-Fernández DM, Esteban-Simón A, Maldonado-Quesada M, Moreno-Poza N, García-Martínez MDM, Alcaraz-García C, Vázquez-Sousa R, Moreno-Martos H, Toro-de-Federico A, Hachem-Salas N, Artés-Rodríguez E, Rodríguez-Pérez MA, Casimiro-Andújar AJ. Effects of a 12-week resistance and aerobic exercise program on muscular strength and quality of life in breast cancer survivors: study protocol for the EFICAN randomized controlled trial. Medicine (Baltimore) 2019;98:e17625. doi: 10.1097/MD.0000000000017625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Idorn M, Thor Straten P. Exercise and cancer: from “healthy” to “therapeutic”? Cancer Immunol Immunother. 2017;66:667–671. doi: 10.1007/s00262-017-1985-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, Bandera EV, Hamilton KK, Grant B, McCullough M, Byers T, Gansler T. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62:243–274. doi: 10.3322/caac.21142. [DOI] [PubMed] [Google Scholar]
- 15.Borde R, Hortobágyi T, Granacher U. Dose-response relationships of resistance training in healthy old adults: a systematic review and meta-analysis. Sports Med. 2015;45:1693–1720. doi: 10.1007/s40279-015-0385-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hrobjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 2012;22:276–282. [PMC free article] [PubMed] [Google Scholar]
- 19.Aydın Sayılan A, Özbaş A. The effect of pelvic floor muscle training on incontinence problems after radical prostatectomy. Am J Mens Health. 2018;12:1007–1015. doi: 10.1177/1557988318757242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Milios JE, Ackland TR, Green DJ. Pelvic floor muscle training in radical prostatectomy: a randomized controlled trial of the impacts on pelvic floor muscle function and urinary incontinence. BMC Urol. 2019;19:116. doi: 10.1186/s12894-019-0546-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heydenreich M, Puta C, Gabriel HH, Dietze A, Wright P, Zermann DH. Does trunk muscle training with an oscillating rod improve urinary incontinence after radical prostatectomy? A prospective randomized controlled trial. Clin Rehabil. 2020;34:320–333. doi: 10.1177/0269215519893096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goode PS, Johnson TM 2nd, Newman DK, Vaughan CP, Echt KV, Markland AD, Kennedy R, Van Arsdalen KN, Rais-Bahrami S, Issa MM, Barnacastle S, Wright KC, McCabe P, Malone MP, Redden DT, Burgio KL. Perioperative mobile telehealth program for post-prostatectomy incontinence: a randomized clinical trial. J Urol. 2022;208:379–387. doi: 10.1097/JU.0000000000002697. [DOI] [PubMed] [Google Scholar]
- 23.Penson DF. Post-prostatectomy incontinence and pelvic floor muscle training: a defining problem. Eur Urol. 2013;64:773–776. doi: 10.1016/j.eururo.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 24.Filocamo MT, Li Marzi V, Del Popolo G, Cecconi F, Marzocco M, Tosto A, Nicita G. Effectiveness of early pelvic floor rehabilitation treatment for post-prostatectomy incontinence. Eur Urol. 2005;48:734–738. doi: 10.1016/j.eururo.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 25.Park SW, Kim TN, Nam JK, Ha HK, Shin DG, Lee W, Kim MS, Chung MK. Recovery of overall exercise ability, quality of life, and continence after 12-week combined exercise intervention in elderly patients who underwent radical prostatectomy: a randomized controlled study. Urology. 2012;80:299–305. doi: 10.1016/j.urology.2011.12.060. [DOI] [PubMed] [Google Scholar]
- 26.Mungovan SF, Carlsson SV, Gass GC, Graham PL, Sandhu JS, Akin O, Scardino PT, Eastham JA, Patel MI. Preoperative exercise interventions to optimize continence outcomes following radical prostatectomy. Nat Rev Urol. 2021;18:259–281. doi: 10.1038/s41585-021-00445-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nahon I, Martin M, Adams R. Pre-operative pelvic floor muscle training--a review. Urol Nurs. 2014;34:230–237. [PubMed] [Google Scholar]
- 28.Goonewardene SS, Gillatt D, Persad R. A systematic review of PFE pre-prostatectomy. J Robot Surg. 2018;12:397–400. doi: 10.1007/s11701-018-0803-8. [DOI] [PubMed] [Google Scholar]
- 29.Wang W, Huang QM, Liu FP, Mao QQ. Effectiveness of preoperative pelvic floor muscle training for urinary incontinence after radical prostatectomy: a meta-analysis. BMC Urol. 2014;14:99. doi: 10.1186/1471-2490-14-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rangganata E, Rahardjo HE. The effect of preoperative pelvic floor muscle training on incontinence problems after radical prostatectomy: a meta-analysis. Urol J. 2021;18:380–388. doi: 10.22037/uj.v18i.6481. [DOI] [PubMed] [Google Scholar]
- 31.Rajkowska-Labon E, Bakuła S, Kucharzewski M, Sliwiński Z. Efficacy of physiotherapy for urinary incontinence following prostate cancer surgery. Biomed Res Int. 2014;2014:785263. doi: 10.1155/2014/785263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baumann FT, Reimer N, Gockeln T, Reike A, Hallek M, Ricci C, Zopf EM, Schmid D, Taaffe D, Newton RU, Galvao DA, Leitzmann M. Supervised pelvic floor muscle exercise is more effective than unsupervised pelvic floor muscle exercise at improving urinary incontinence in prostate cancer patients following radical prostatectomy - a systematic review and meta-analysis. Disabil Rehabil. 2022;44:5374–5385. doi: 10.1080/09638288.2021.1937717. [DOI] [PubMed] [Google Scholar]
- 33.Wu ML, Wang CS, Xiao Q, Peng CH, Zeng TY. The therapeutic effect of pelvic floor muscle exercise on urinary incontinence after radical prostatectomy: a meta-analysis. Asian J Androl. 2019;21:170–176. doi: 10.4103/aja.aja_89_18. [DOI] [PMC free article] [PubMed] [Google Scholar]


