Abstract
Background:
More intense cyclones are expected in the future as a result of climate change. A comprehensive review is urgently needed to summarize and update the evidence on the health effects of cyclones.
Objectives:
We aimed to provide a systematic review with meta-analysis of current evidence on the risks of all reported health outcomes related to cyclones and to identify research gaps and make recommendations for further research.
Methods:
We systematically searched five electronic databases (MEDLINE, Embase, PubMed, Scopus, and Web of Science) for relevant studies in English published before 21 December 2022. Following the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines, we developed inclusion criteria, screened the literature, and included epidemiological studies with a quantitative risk assessment of any mortality or morbidity-related outcomes associated with cyclone exposures. We extracted key data and assessed study quality for these studies and applied meta-analyses to quantify the overall effect estimate and the heterogeneity of comparable studies.
Results:
In total, 71 studies from eight countries (the United States, China, India, Japan, the Philippines, South Korea, Australia, Brazil), mostly the United States, were included in the review. These studies investigated the all-cause and cause-specific mortality, as well as morbidity related to injury, cardiovascular diseases (CVDs), respiratory diseases, infectious diseases, mental disorders, adverse birth outcomes, cancer, diabetes, and other outcomes (e.g., suicide rates, gender-based violence). Studies mostly included only one high-amplitude cyclone (cyclones with a Saffir–Simpson category of 4 or 5, i.e., Hurricanes Katrina or Sandy) and focused on mental disorders morbidity and all-cause mortality and hospitalizations. Consistently elevated risks of overall mental health morbidity, post-traumatic stress disorder (PTSD), as well as all-cause mortality or hospitalizations, were found to be associated with cyclones. However, the results for other outcomes were generally mixed or limited. A statistically significant overall relative risk of 1.09 [95% confidence interval (CI): 1.04, 1.13], 1.18 (95% CI: 1.12, 1.25), 1.15 (95% CI: 1.13, 1.18), 1.26 (95% CI: 1.05, 1.50) was observed for all-cause mortality, all-cause hospitalizations, respiratory disease, and chronic obstructive pulmonary disease hospitalizations, respectively, after cyclone exposures, whereas no statistically significant risks were identified for diabetes mortality, heart disease mortality, and preterm birth. High between-study heterogeneity was observed.
Conclusions:
There is generally consistent evidence supporting the notion that high-amplitude cyclones could significantly increase risks of mental disorders, especially for PTSD, as well as mortality and hospitalizations, but the evidence for other health outcomes, such as chronic diseases (e.g., CVDs, cancer, diabetes), and adverse birth outcomes remains limited or inconsistent. More studies with rigorous exposure assessment, of larger spatial and temporal scales, and using advanced modeling strategy are warranted in the future, especially for those small cyclone-prone countries or regions with low and middle incomes. https://doi.org/10.1289/EHP12158
Introduction
Cyclones, including hurricanes and tropical storms, are among the most destructive weather phenomena globally and may cause devastating impact on society. For example, Hurricane Sandy made landfall in eight countries from the Caribbean to Canada and inflicted nearly in damage.1 Recent cyclone seasons have produced stronger and longer-lasting cyclones than previously recorded.2,3 Under a warming climate, future cyclones are expected to be more intense (i.e., greater maximum windspeeds and larger amount of rainfall) and more destructive,4,5 which suggests that cyclones will remain an important public health concern.
Traditionally, the official reported losses (e.g., mortality) associated with cyclones are estimated based on the direct exposures to cyclone hazards that occurred within a brief window (i.e., first hours and days) after a cyclone.6 These may not adequately capture the health impacts that are indirectly attributable to the event. Population-based epidemiological studies that involve statistical analysis by comparison of the health outcomes of higher exposure level with those of lower exposure level or without exposure could provide more accurate estimates of the magnitude and pattern of the health effects.
Accumulating epidemiological evidence has indicated that cyclones were associated with a series of health outcomes, including mortality,7–11 noncommunicable disease,12–15 adverse birth outcomes,16–18 infectious diseases,19–21 and mental disorders.22–25 Except for the direct physical impacts (e.g., drowning, injury, carbon monoxide poisoning),26 cyclones could also have indirect, persisting or delayed adverse effects on human health possibly related to interrupted health care services, contaminated floodwater, and infection outbreaks.14,27,28 However, the results were mixed and, to our knowledge, no systematic review with meta-analysis has been conducted to comprehensively summarize the findings. Previous reviews were generally descriptive and did not perform a systematical search of databases29,30 or only focused on specific outcomes among certain subpopulations (e.g., hurricane-related asthma among children).31 Furthermore, several recent important studies on the associations of cyclones with health were published after these reviews.7,13–15,17,22,32
We aimed to conduct an up-to-date systematic review and comprehensive meta-analyses of epidemiological studies on the health risks related to cyclone exposures. This review will inform health care professionals and policymakers on the characteristics and likely magnitude of the health effects of cyclones and propose future directions for research in this field.
Methods
Search Strategy
The systematic review and meta-analysis were performed in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines and checklist.33 We registered a systematic review protocol at PROSPERO (https://www.crd.york.ac.uk/prospero) with the identification number CRD42022320523.
Five electronic databases (MEDLINE, Embase, PubMed, Scopus, and Web of Science) were systematically searched to find relevant studies in English published up to 7 April 2022. An updated search was conducted on 21 December 2022. The search strategies for each database are detailed in Table S1. Briefly, a combination of medical subject heading terms and free-text words in titles, abstracts, and key words concerning cyclones (e.g., cyclonic storms, hurricanes, typhoons) and human health outcomes (e.g., health, disease, mortality, morbidity, pregnant, and mental outcomes) were used for the literature search. The results were then restricted to studies of humans. In addition, the reference lists of all included articles and pertinent reviews were also screened manually to identify more studies.
Inclusion and Exclusion Criteria
The studies included had to meet the following inclusion criteria grouped according to the population–exposure–comparator–outcome (PECO) framework34,35:
Population—population-based studies with no restriction on sex, age, or region
Exposures—studies of short-term () or long-term () exposures to any landfall cyclones, including tropical storms, hurricanes, and typhoons (Table S1)
Comparators—observational and analytical studies reporting original effect estimates [e.g., excess events, odds ratio (OR), relative risk (RR), hazard risk (HR), percentage change] by comparing risk between individuals or populations exposed to different cyclone levels or different exposures within individuals or populations at different time points
Outcomes—studies reporting any adverse human health outcomes, such as morbidity or mortality (Table S1)
Studies published in a peer-reviewed journal with full text available.
Studies with the following descriptions were excluded:
Population—nonhuman studies (e.g., animal studies)
Exposures—studies focused only on the health effects of the subsequent events caused by cyclones, such as power outage, flood, injury, stress or trauma; studies investigating the moderation or mediation effects of personal or community characteristics on the health effects of cyclones
Comparators—studies without comparative risk effect estimates between higher and lower levels of cyclone exposure
Outcomes—studies without an assessment of human health outcome (e.g., studies that evaluated the health care service disruptions, health-related economic costs of cyclones).
For multiple studies of repeated data (e.g., overlapping population), the one with more observations or more thorough reporting was included.
Study Selection
All studies included in the final review or synthesis were identified in several stages, beginning with downloading all searched articles into a reference manager software (EndNote X20; Clarivate Analytics). An initial deletion of duplicates was conducted using the function incorporated in the software. Then, (W.H. and Y.Gao) independently reviewed the titles and abstracts of the remaining studies to remove obviously irrelevant articles. Finally, the remaining studies were screened for full texts for eligibility. Any uncertainty and disagreement were solved by discussion with a third coauthor (R.X.).
Data Extraction
For each eligible study, the following information was extracted: first authors and publication year, study period, setting, design and population, sample size, exposure assessment method, exposure window (i.e., the hypothetical post-cyclone period during which the cyclone effects persist), comparison (i.e., the pre-cyclone period or individuals selected as the comparison group to derive the effect estimates), outcome, study cyclone(s), statistical method, and effect estimates (i.e., the effect estimates of adverse health outcomes related to cyclone exposures). Two authors (W.H. and Y.Gao) independently performed the procedure and any conflict was adjudicated by a third author (R.X.).
Study Quality Assessment
We assessed study quality using the risk of bias (ROB), defined as the systematic errors that could be introduced into the effect estimations by the study characteristics,36 for each included study. As previously described,37 we used the National Institutes of Environmental Health Sciences’ National Toxicology Program Office of Health Assessment and Translation (OHAT) tool to assess the ROB.38 Eight criteria, including key (exposure assessment, outcome assessment, and confounding bias) and other criteria (selection bias, attrition/exclusion bias, selective reporting bias, conflict of interest, and other sources of bias), were evaluated for each study. Each criterion was categorized as “low,” “probably low,” “probably high,” or “high” risk based on the adapted criteria of ROB assessment tailored for the systematic review (Table S2). Based on the OHAT tool guidelines, studies with at least one key criterion and at least three of the five other criteria considered “high” or “probably high” were excluded from the review.
Statistical Analysis
We performed meta-analyses when three or more comparable effect estimates were identified.35,39–42 Specifically, effect estimates were regarded as comparable if a) they focused on the same specific health outcome; b) they were based on the same data type [e.g., mortality, emergency department (ED) visits, hospitalization, incidence]; and c) they were derived from a model with a same definition for cyclone exposure variable (e.g., exposed vs. unexposed). Owing to the great difference in the definitions for the exposure variable among studies with a continuous cyclone exposure variable in the model (typically studies on mental health; e.g., self-reported scores for a level of being affected), we selected the point effect estimates with their corresponding 95% confidence intervals (CIs) derived from the models with a binary cyclone exposure variable (i.e., exposed vs. unexposed) for meta-analysis. In addition, given the very limited number of comparable estimates from studies on continuous outcomes, we performed meta-analysis only on the effect estimates from studies on dichotomous outcomes (i.e., excess events, OR, RR, HR, percentage change). OR was deemed as comparable to the RR for a rare health outcome (event rates ; e.g., mortality, preterm birth).43,44
The overall effect estimates for each pair of exposure–health outcome were quantified using the random-effects meta-analysis model. Sensitivity analysis by excluding each individual effect estimate in turn was conducted to check the robustness of the overall effect estimate for each pair of exposure–health outcome. The summary measure for each meta-analysis was the RR of a specific health outcome between the cyclone-exposed and non–cyclone-exposed groups. Both statistics and Q-test were used to evaluate the consistency and between-study heterogeneity.45 Forest plots and contour-enhanced funnel plots were employed to visually inspect the significance and size of the study-specific and the meta-effect estimates and to differentiate publication bias from other forms of asymmetry.46 To further quantitatively assess the funnel plot asymmetry, Egger’s test of the intercept was performed47 and trim and fill analysis was conducted by imputing hypothetically missing studies once statistically significant asymmetry was detected.48
All analyses were carried out using R (version 4.0.5; R Development Core Team) based on the meta and metafor packages. A two-tailed was considered statistically significant.
Results
Studies Characteristics
A total of 19,330 papers were initially identified in the systematic literature search (Figure S1). After excluding duplicates and topic relevance assessment by title and abstract screens, 293 papers were sought for retrieval and a full-text review, among which 8 records were identified through the review of the references. Eight studies assessed the excess mortality in Puerto Rico after Hurricane Maria.8,49–55 We included only the paper by Cruz-Cano and Mead8 because it included the longest study period and largest amount of data and reported cause-specific excess mortality instead of focusing only on all-cause excess mortality or subpopulation (e.g., Hispanic origin, patients with kidney failure) compared with the other studies. Finally, 71 eligible papers were included in the review, and 32 estimates from 18 of the included studies underwent a further meta-analysis.
The basic characteristics of the 71 studies are summarized in Table S3. Studies from eight different countries were included, mostly from the United States (58/71), followed by China (6/71). Time-series or case-crossover design based on counts data were the most commonly used study designs (33/71), followed by a cohort design (18/71). Approximately 70% (49/71) of the included studies focused on only one cyclone (mostly Hurricanes Katrina or Sandy). Most of the included studies focused on the general population (27/71) and assessed cyclone exposures based on cyclone hit time and track or official disaster declaration (e.g., disaster declaration by Federal Emergency Management Agency; 42/71), followed by self-administered questionnaire (13/71). Five most recent studies used a wind field model to quantify the spatial intensity of cyclones and assessed the cyclone exposures at the county level.7,13–15,17 In addition, the hypothetical exposure window of cyclones ranged greatly, from 1 d to following cyclone exposures, across included studies, with the majority concentrated at d (Figure 1A). The included studies generally assessed the cyclone-related health risks by comparing participants with cyclone exposures to those with lower level or without exposures or by comparing the counts of adverse health outcomes during the hypothetical cyclone exposure window to those during the defined comparison period without cyclone exposures. The selection of the comparison period varied considerably among the included studies, with the majority using a time period ranging from 1 wk to 9 y prior to cyclone exposure (32/71) or nonexposure days before and after the exposure window (12/71; e.g., same months in other nonexposure years) as the comparison period. After organizing the studies by outcomes (some studies reported effect estimates for more than one type of health outcome), 15.3% of the included studies were on mental health, followed by all-cause mortality or hospitalization (11.9%) and CVDs (11.9%; Figure 1B).
Figure 1.
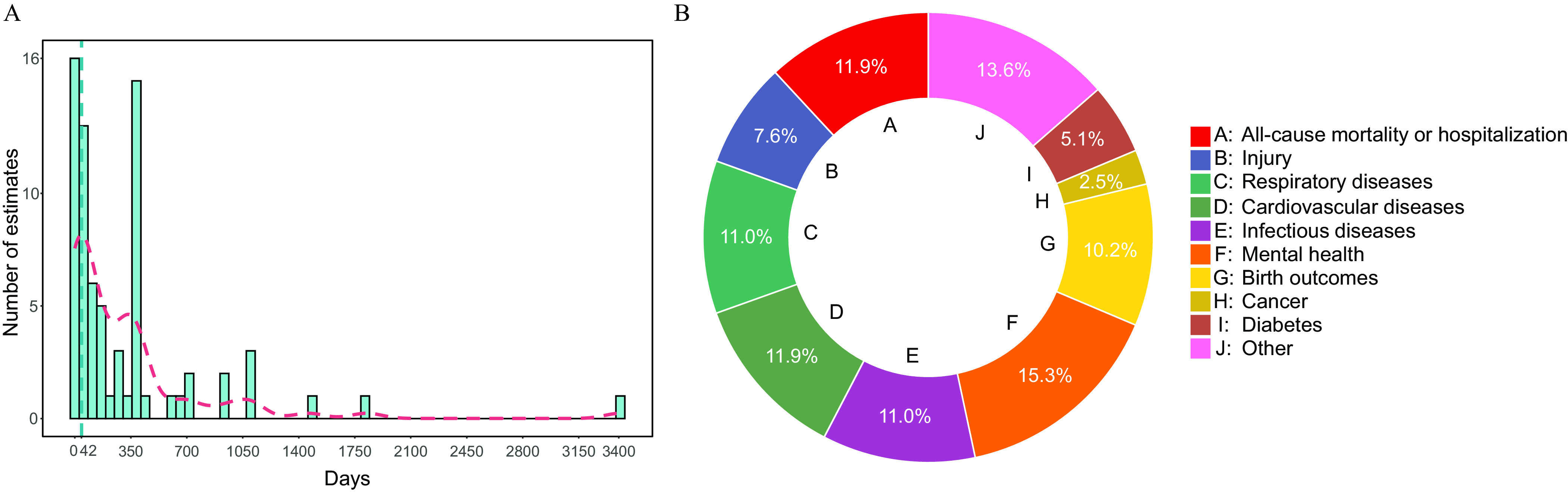
Distribution of (A) exposure windows and (B) outcomes among all included studies (Table S3).
The ROB assessment of the included studies and the details of assessment are shown in Table S4 and Table S5, respectively. None of the included studies was excluded owing to high ROB. However, a major concern about the study quality was exposure assessment bias because most included studies did not involve models supplemented by continuous measurements of cyclone exposures (e.g., cyclone-related peak sustained windspeed, cumulative rainfall) to quantify the time–space varying spatial intensity.
Cause-Specific Mortality Associated with Cyclones
All-cause mortality.
The cyclone-related risk for all-cause mortality was assessed by 9 studies from the United States,8,9,11,13,54,56–59 1 study from South Korea,60 and 1 study with a setting of 16 small, low-income countries in the Caribbean and Central America.10 Eight of them (8/11, 72%), mostly on a high-amplitude hurricane (cyclones with a Saffir–Simpson category of 4 or 5), observed statistically significant elevated mortality during a post-cyclone period of 7 d to 1 y.8–11,54,56,59,60 For example, a retrospective cohort study on 340,656 individuals ( years of age) with diabetes from the United States found the individuals affected by Hurricanes Katrina and Rita had a 40% higher all-cause mortality risk in the first month after the cyclone, and that difference fell to 10% in y.59 However, the remaining 3 studies (3/11) on 53 tropical cyclones13 and Hurricane Katrina,57,58 with exposure windows of from 11 d to 1 y, did not observe a statistically significant increase in all-cause mortality in the U.S. general population. Among the 11 studies on all-cause mortality, 6 could be included in the meta-analysis with a meta- (95% CI: 1.04, 1.13) for all-cause mortality (Figure 2). The meta-RR was robust to the sensitivity analysis by excluding each effect estimate in turn (Table S6). High between-study heterogeneity was observed (, ). The funnel plot (Figure S2a) and Egger’s regression test () indicated statistically insignificant asymmetry. The remaining 5 studies could not be included in the meta-analysis because of the difference in estimate types compared with other studies. For example, 1 ecological study reported country-level excess deaths per 100,000 population ranging from 1.5 to 259.3 among countries with different gross domestic product (GDP) level and cyclones with different amplitude.10
Figure 2.
![Figure 2 is a forest plot, plotting study, including cyclones (top to bottom), ranging as All-cause mortality: Quast and others (2019), including Hurricane Katrina and Rita; Kutner and others (2009), including Hurricane Katrina; Dosa and others (2020), including Hurricane Irma; Kim and others (2017), including Hurricane Sandy; Cruz-Cano and Mead (2019), including Hurricane Maria; Kim and others (2013), including Three T Cs; Overall: Heterogeneity: uppercase italic i squared equals 78 percent, lowercase italic p less than 0.01; Heart disease mortality: Cruz-Cano and Mead (2019), including Hurricane Maria; Quast and others (2019), including Hurricane Katrina and Rita; Hendrickson and Vogt (1996), including Hurricane Iniki; Overall: Heterogeneity: uppercase italic i squared equals 63 percent, lowercase italic p equals 0.07; Diabetes mortality: Cruz-Cano and Mead (2019), including Hurricane Maria; Quast and others (2019), including Hurricane Katrina and Rita; Hendrickson and Vogt (1996), including Hurricane Iniki; Overall: Heterogeneity: uppercase italic i squared equals 91 percent, lowercase italic p less than 0.01 (y-axis) across Estimate, ranging from 0.75 to 1 in increments of 0.25, 1 to 1.5 in increments of 0.5, and 1.5 to 2.5 in increments of 1 (x-axis) for relative risks [95 percent confidence intervals] and Weight (percentage).](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/2006/10461789/1dbc124cc625/ehp12158_f2.jpg)
Random-effect meta-analysis of risk of mortality from all causes, heart diseases, and diabetes associated with cyclone exposures (study details, including , can be found in Table S3). Weights represent the percentages of contribution of each study effect estimate to the overall meta-estimate. Note: CI, confidence interval; RR, relative risk; TC, tropical cyclone.
CVD-related mortality.
The CVD-related mortality associated with cyclones were estimated by six studies from the United States.7,8,11,59,61,62 Among them, five studies reported statistically significant elevated mortality risk from CVDs associated with high-amplitude hurricanes8,11,59,61,62 or tropical cyclones (cyclones with a maximum sustained windspeed of knots).7 The statistically significant adverse effects were observed from 1 month for tropical cyclones7 to 1 y for high-amplitude hurricanes (i.e., Hurricanes Katrina and Rita)8,11,59,62 after the cyclone exposure. For example, a case-crossover study on all tropical cyclones that hit the United States from 1988 to 2018 found that each additional cyclone day per month was associated with 1.2% [95% credible interval (CrI): 0.6%, 1.7%] increases in monthly county-level death rates for CVDs in the month following a tropical cyclone.7 Another cohort study on Medicare participants with diabetes ( years of age) affected by Hurricanes Katrina and Rita found a 15% (95% CI: 11%, 19%) increase in mortality risk from heart diseases in 1 y after hurricane exposure.59 However, the mortality risks could be heterogeneous by different types of CVD. Two studies, on Hurricanes Sandy62 and Iniki,61 respectively, reported no statistically significant association between cyclone exposures and stroke, whereas higher mortality risk from myocardial infarction was observed after the hurricane.62
Three studies on cyclone-related heart disease mortality could be included in the meta-analysis and a statistically insignificant overall association with a meta- (95% CI: 0.99, 1.30) was observed (Figure 2).8,59,61 The effect estimate from the study on Hurricane Iniki61 had a strong impact on the magnitude of the meta-RR (Table S6). High heterogeneity (, ) and statistically insignificant asymmetry were also found among the studies (Figure S2b; for Egger’s regression ). The remaining CVD-related mortality outcomes (i.e., all-cause CVDs,7,11 myocardial infarction,62 and stroke61,62) could not be included in the meta-analysis owing to the limited number of comparable effect estimates. For example, only two studies reported the RRs of mortality from stroke associated with cyclone exposures.61,62
Respiratory diseases-related mortality.
Only three studies from the United States estimated the respiratory diseases-related excess mortality associated with cyclones.7,11,61 Two of them detected statistically significant elevated mortality risk from respiratory diseases associated with cyclone exposures.7,11 Specifically, one time-series study on the population years of age affected by Hurricane Sandy found an elevated risk of respiratory disease mortality with an (95% CI: 1.15, 1.33) during a 3-month post-hurricane period,11 and another case-crossover study on all tropical cyclones that hit the United States from 1988 to 2018 found a 1.3% (95% CrI: 0.2%, 2.4%) increase in monthly county-level death rates for respiratory diseases in the month following a tropical cyclone for each increase in monthly cyclone exposure day.7 The remaining one time-series study did not observe a statistically significant change in respiratory disease mortality in the 12-month period following Hurricane Iniki for the general population.61 These three studies could not be included in the meta-analysis owing to the limited number of comparable effect estimates given that one of them reported absolute change in death rate in respiratory mortality for each additional cyclone day per month7 while the other two studies reported RR of respiratory mortality associated with cyclone exposures.11,61
Diabetes mortality.
The excess mortality from diabetes associated with cyclones was estimated by three studies from the United States. Among them, two time-series studies, on Hurricanes Maria and Iniki, observed an elevated mortality risk from diabetes (RRs ranged from 1.41 to 2.61) in the general population during a post-cyclone exposure period of 40 d8 and 1 y,61 respectively, whereas the remaining one retrospective study, on 340,656 Medicare participants with diabetes years of age, reported a decreased change in the 1-y period following Hurricanes Katrina and Rita.59 Overall, a statistically insignificant association of cyclone exposures and diabetes mortality [ (95% CI: 0.80, 2.47)] with high heterogeneity (, ) was observed for these three studies8,59,61 (Figure 2). The effect estimate from the study on Hurricane Iniki61 was an influential observation for the meta-RR (Table S6). Statistically insignificant asymmetry was found by funnel plot (Figure S2c) and Egger’s regression test ().
Cancer, injury, infectious disease-related, and other mortality.
Two studies from the United States estimated the excess mortality from cancer associated with cyclones in the general population.7,61 Both of them suggested no association of cancer mortality with exposures to tropical cyclones7 or Hurricane Iniki.61 Injury-related excess mortality associated with cyclones was quantified by three studies from the United States. The increases in injury-related mortality in the general population were observed during a 2-month post-cyclone period [monthly county-level death rates for each additional tropical cyclone day, 3.7% (95% CrI: 2.5%, 4.9%)]7 and during a 90-d post-cyclone period [RR for Hurricane (95% CI: 1.05, 1.44)],11 respectively, but not in the 12-month period following Hurricane Iniki.61 Infectious disease-related mortality associated with cyclones for the general population was estimated by two studies, and both of them indicated a statistically significant elevation during a 3-month post-cyclone period [monthly county-level death rates for each additional tropical cyclone day, 1.8% (95% CrI: 0.1%, 3.6%)7 and RR for Hurricane (95% CI: 1.12, 1.29)].11 For other cyclone-related mortality, statistically significant increases in mortality from neuropsychiatric conditions,7 Alzheimer’s disease,8 septicemia,8 and nephritis59 after a tropical cyclone have also been suggested by three studies from the United States. These studies could not be included in the meta-analysis because less than three comparable effect estimates were observed for each specific outcome. For example, of the three injury-related mortality studies, one reported absolute changes in cyclone-related mortality,7 and the other two reported relative changes in it.11,61
Cause-Specific Morbidity Associated with Cyclones
All-cause hospitalization.
The excess risk for all-cause hospitalization associated with cyclone exposures was estimated by five studies from the United States.9,56,63–65 Four of these studies observed an increased risk of all-cause hospitalization for up to 3 months after a high-amplitude hurricane (e.g., Hurricanes Katrina, Sandy, or Wilma).9,56,63,65 A case-crossover study on eight large-scale hurricanes reported an elevated risk ranging from 15% to 37% for all-cause hospitalization among the population years of age in the 1-month period following cyclone exposures.63 However, another time-series study on Hurricane Sandy showed no change in inpatient use inside the storm zone but did show a statistically significant reduction outside the storm zone over the 1-y post-cyclone period.64 The meta-analysis of 10 estimates from three studies suggest a meta- (95% CI: 1.12, 1.25) for being hospitalized after cyclone exposures (Figure 3).63–65 The meta-RR was generally robust to the sensitivity analysis by excluding each estimate in turn (Table S6). High between-study heterogeneity (, ), as well as statistically insignificant asymmetry (Figure S3a; for Egger’s regression ), were observed. The remaining two studies were not included in the meta-analysis because one study9 focused on absolute change in hospitalization rate and the other study56 reported OR rather than RR for all-cause hospitalization associated with cyclones.
Figure 3.
![Figure 3 is a forest plot, plotting study, including cyclones (top to bottom), ranging as All-cause hospitalization: Bell and others (2021), including Hurricane Frances; Bell and others (2021), including Hurricane Ivan, Bell and others (2021), including Hurricane Katrina, Bell and others (2021), including Hurricane Wilma, Bell and others (2021), including Hurricane Rita, Bell and others (2021), including Hurricane Ike, Bell and others (2021), including Hurricane Irene, Bell and others (2021), including Hurricane Sandy, Sharp and others (2016), including Hurricane Sandy, Howard and others, including Hurricane Katrina; Overall: Heterogeneity: uppercase italic i squared equals 98 percent, lowercase italic p less than 0.01; Respiratory diseases hospitalization: van Loenhout and others, including Typhoon Haiyan; Parks and others (2021), including all T Cs hit U S between 1999 and 2014; Yan and others (2021), including 74 Atlantic-basin T Cs; Overall: Heterogeneity: uppercase italic i squared equals 35 percent, lowercase italic p equals 0.21; C O P D hospitalization: Bell and others (2021), including eight large-scale hurricanes; Parks and others (2021), including all T Cs hit U S between 1999 and 2014; Yan and others (2021), including 74 Atlantic-basin T Cs; Overall: Heterogeneity: uppercase italic i squared equals 98 percent, lowercase italic p less than 0.01; Preterm birth: Meir and others (2021), Hurricanes Katrina, Antipova and Curtis (2015), including Hurricane Andrew; Sun and others (2020), including 58 T Cs; Harville and others (2022), including Hurricane Michael; and Overall: Heterogeneity: uppercase italic i squared equals 90 percent, lowercase italic p less than 0.01 (y-axis) across Estimate, ranging from 0.8 to 1 in increments of 0.2, 1 to 1.25 in increments of 0.25, and 1.25 to 2 in increments of 0.75 (x-axis) for relative risks [95 percent confidence intervals] and Weight (percentage).](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/2006/10461789/51180f2607b5/ehp12158_f3.jpg)
Random-effect meta-analysis of risk of all-cause hospitalization, respiratory diseases hospitalization, COPD hospitalization and preterm birth associated with cyclone exposures (study details, including , can be found in Table S3). Weights represent the percentages of contribution of each study effect estimate to the overall meta-estimate (Table S3). Note: CI, confidence interval; COPD: chronic obstructive pulmonary disease; RR, relative risk; TC, tropical cyclone.
CVD-related morbidity.
Nine studies in the United States reported CVD-related excess morbidity associated with cyclones.12–15,62,66–69 Among them, six studies focused on hospitalization,13–15 ED visits,12 physician visits,67 or total visits and admissions69 due to all-cause CVD. Three of these six studies observed increased hospitalizations [ (95% CI: 1.02, 1.05)]15 within 7 d, total visits and admissions within 1 y [ (95% CI: 2.00, 2.01)]69 among the population years of age, and increased physician visits within 2 wk among the general population [ (95% CI: 1.51, 4.49)]67 following cyclone exposures. However, two studies that included tropical cyclones reported no change in CVD hospitalization 1 wk after the cyclones among the population years of age14 and a reduced hospitalization rate during an 11-d period after the cyclone for the general population,13 respectively. Another time-series study on Hurricane Sandy observed an increased risk of ED visits for CVDs in the population years of age in the week following the cyclone but a decreased rate among those 0–17 years of age for up to 3 wk.12
Specific CVD morbidity risks associated with cyclone exposures were estimated in four studies.15,62,66,68 In the month following a large-scale hurricane (e.g., Hurricane Sandy), increased hospitalization risks were found for myocardial infarction [ (95% CI: 1.16, 1.28)] and stroke [ (95% CI: 1.03, 1.11)] for the general population62 and for congestive heart failure for the people years of age [ (95% CI: 1.17, 1.21)].66 One cohort study on 909 individuals years of age reported no statistically significant higher risk of new-onset heart diseases for the participants who lived in high-impacted areas (census blocks with a storm surge of foot, of houses damaged or reported greater than the average number of housing assistance registrations) compared with those who did not in the 4 y after Hurricane Sandy.68 Another case-crossover study on 74 tropical cyclones across 175 U.S. counties observed increased risks for being hospitalized owing to heart failure [ (95% CI: 1.04, 1.11)] but not for myocardial infarction, ischemic heart disease, cerebrovascular disease, heart rhythm disturbance, or peripheral vascular disease among the population years of age over the 10-d post-cyclone period.15 These studies of CVD-related excess morbidity were not included in the meta-analysis because there were fewer than three comparable effect estimates for each specific outcome. As shown above, for the most studied all-cause CVD morbidity,12–15,67,69 three studies were on hospitalization (one reported absolute change13 and the other two reported absolute change14,15 associated with cyclones), two studies were on physician visits67 and ED visits,12 respectively, and the remaining one was on all department visits (including hospitalization and ED and outpatient visits).69 For the other cause-specific CVD morbidity outcomes,15,62,66,68 the studies identified were very limited and therefore insufficient for a meta-analysis.
Respiratory diseases-related morbidity.
Respiratory diseases-related excess morbidity associated with cyclones was estimated in the United States (9 studies)12–15,66–70 and the Philippines (1 study).71 Among them, six studies focused on hospitalization,13–15,71 ED visits,12 and total visits and admissions69 due to all-cause respiratory diseases, and they consistently observed a statistically significant increased risk among the general population. The elevated risks could be seen up to 11 d after a tropical cyclone13 or 1 y after a high-amplitude hurricane, such as Sandy.69 However, a statistically insignificant change or decreasing rate in ED visits for respiratory diseases was found in younger adults (18–64 years of age) in the week after Hurricane Sandy.12 Of the six studies on all-cause respiratory diseases-related morbidity,12–15,69,71 three of them, on hospitalizations for respiratory diseases, were included in the meta-analysis.14,15,71 The other three studies were not included because two of them were on ED visits12 and total admission and visits,69 respectively, and the remaining one reported absolute changes in the rate.13 A meta-RR of 1.15 (95% CI: 1.13, 1.18) showed an overall increased risk for being hospitalized for respiratory diseases after exposure to cyclones (Figure 3). The effect estimate from the study on 74 Atlantic-basin tropical cyclones15 had a strong impact on the magnitude of the meta-RR (Table S6). Funnel plot (Figure S3b) and Egger’s regression test () indicated a statistically insignificant asymmetry.
Specifically, for chronic obstructive pulmonary disease (COPD), studies reported a consistently increased hospitalization rate [4.6% per 100,000 population (95% CI: 2.1%, 6.8%)] among the general population13 and higher hospitalization risks (RR ranged from 1.06 to 1.44) among the population years of age14,15,66 associated with cyclone exposures. The elevated risks were observed at a post-cyclone period of up to 11 d for a tropical cyclone14,15 or 30 d for a large-scale hurricane.66,67 Of the four studies on COPD hospitalizations,13–15,66 three14,15,66 were included in the meta-analysis and one13 was not included owing to its different effect estimate type (hospitalization rate per 100,000 population). An overall increased risk for COPD hospitalizations [meta- (95% CI: 1.05, 1.50)], but with high heterogeneity (, ), was observed after cyclone exposures (Figure 3). Funnel plot (Figure S3c) and Egger’s regression test () indicated statistically insignificant asymmetry. Contrary findings were observed by three studies that estimated the cyclone-related asthma morbidity.15,67,70 Two of them found elevated hospitalizations and physician visits for asthma in populations y old15 or for all ages,67 respectively, for up to 2 wk after the hurricane, whereas another time-series study suggested no change in asthma-related ED visits for the general population in the 1-month period following Hurricane Irene.70 Another two studies on Hurricane Sandy68 and 74 tropical cyclones15 also suggested a null association of incidence of COPD or asthma and hospitalizations for upper respiratory infections with cyclone exposures, respectively.
Mental health-related morbidity.
The excess risk for mental health-related morbidity associated with cyclones was estimated by 17 U.S. studies, including 15 studies on a single cyclone (mostly Hurricane Sandy or Hurricane Katrina)22–25,64,72–81 and two studies on multiple cyclones.82,83 These studies generally assessed cyclone exposure as a continuous score to quantify the impact level based on the self-reported cyclone experience derived from questionnaires, as opposed to the cyclone time and track of impact or official declaration used in studies of other health outcomes. For overall mental health-related morbidity, consistently adverse associations with cyclone exposures were observed. Seven studies on large-scale hurricanes reported increased mental health service visits22,64,80,82 or hospitalization,22 poor mental health days,74,78 and higher mental illness prevalence25 for up to 3 y after cyclone exposures. For example, a time-series study on Hurricane Sandy found that changes in service use were most pronounced over the 1-y period after the cyclone, with a 10% (95% CI: 7%, 13%) increase in ED services for mental illness in the storm zone.64 Another cross-sectional study on 1,869 adults observed a doubled prevalence of mental illness in the month after Hurricane Katrina [ (95% CI: 1.80, 3.20)].25
For morbidity related to mental subtypes, eight studies reported a consistently higher risk of PTSD either among the general population,24,72,75,77 pregnant women,76 or certain occupational groups (e.g., high school students, public health workers)23,73,83 associated with a higher level of cyclone exposures. For example, a cohort study on 292 pregnant women found an RR of 3.68 (95% CI: 1.80, 7.52) for having PTSD among those with two or more severe experiences of hurricanes.76 Another cross-sectional study on 747 adults surveyed 1 y after Hurricane Katrina reported a 69% (95% CI: 22%, 133%) higher risk for having PTSD among the participants who stayed in the hardest-hit area (New Orleans) during the cyclone compared with those who did not.77 A more prolonged higher risk of PTSD was found among the participants who were directly affected by Hurricane Sandy compared with their counterparts in a cohort study of 130 adults followed up more than 2 y after the hurricane [ (95% CI: 1.10, 2.20)].75
However, less consistent associations were found for morbidity related to anxiety and depression. Two studies surveyed after Hurricane Sandy detected a null association of cyclone exposure levels with anxiety among adults.24,75 Another case-crossover study found an increased hospitalization risk for anxiety 2 y following Hurricane Sandy among the population years of age, but not for anxiety department visits.22 Similarly, higher risks of depression were found to be associated with higher cyclone exposure level in two studies on pregnant women and World Trade Center workers who experienced Hurricane Katrina and Hurricane Sandy, respectively, but not in the other three studies on general adults exposed to Hurricanes Sandy or Maria. Increased risks of ED visit or hospitalization for mood disorders, adjustment disorders, psychosis, alcohol and substance abuse, suicide, and intentional harm among the people years of age over a 3-y period following Hurricane Sandy22 and increased risks of behavioral disorder among the public-school students over 1 y following Hurricane Katrina79 were also suggested by two studies. These studies of mental health-related morbidity could not be included in the meta-analysis because there were fewer than three comparable effect estimates for each specific outcome. For the most studied outcomes of PTSD23,24,72,73,75–77,83 and depression,24,73,75,76,81 an incomparable definition of cyclone exposure level based on the self-reported cyclone experience from self-administered questionnaire was used across studies (i.e., the effect estimates were not derived from a uniform cyclone exposure variable of exposed vs. unexposed). For the other mental health morbidity outcomes, as shown above, the studies identified were very limited and therefore insufficient for a meta-analysis.
Adverse birth outcomes.
The excess risks for adverse birth outcomes associated with cyclones were estimated by nine studies from the United States,16–18,84–89 three studies from Australia,90 Brazil,91 and the Philippines,71 respectively. Cyclone-related preterm birth risks were reported in seven studies,16–18,87–90 and two of them observed statistically significant higher risks among the women who experienced a hurricane during pregnancy.18,89 However, a null association was found in the other four studies on a high-amplitude hurricane16,87,88 or 58 tropical cyclones.17 One cross-sectional study with 647,634 births in Queensland, Australia, examined the association of trimester-specific cyclone exposure with preterm birth and found that only tropical cyclone exposure in early pregnancy was associated with higher odds of preterm births.90 Four17,18,87,88 of these seven studies on preterm birth that reported relative change in the risk of preterm birth associated with cyclones (i.e., exposed vs. unexposed) were included in the meta-analysis, whereas the other three studies16,89,90 were not included because one of them reported only the trimester-specific effect estimate,90 one reported absolute change in the incidence rate,89 and the remaining one used a continuous cyclone exposure level based on self-reported cyclone experience.16 An overall statistically insignificant association [meta- (95% CI: 0.91, 1.29); Figure 3] with high heterogeneity (, ) and statistically insignificant asymmetry (Figure S4; Egger’s regression test, ) were found between cyclone exposures and preterm births. The meta-RR was consistently statistically insignificant in sensitivity analysis performed by excluding each estimate in turn (Table S6).
Birth weight-related outcomes were examined in six studies.16,18,85,88,89,91 Four of them reported an association of cyclone exposures with lower birth weight,89,91 increased risk of low birth weight88,89 after a high-amplitude hurricane and higher risk of low birth weight among newborn babies who had perinatal exposure to high hurricane exposure (having three or more severe experiences due to hurricane) compared with those without high hurricane exposure.16 However, no statistically significant changes in the risk of low birth weight after the hurricane were found in the remaining two studies.18,85 These six studies on birth weight were not included in the meta-analysis because three of them reported an incomparable absolute change in the risk of low birth weight (i.e., change in probability,91 county-level rate,85 or incidence89) associated with cyclones, and another one used cyclone exposure levels defined based on self-reported cyclone experience.16 For other birth outcomes, infant temperament,84 birth rate85 and fetal death85 were found to be not associated with cyclone exposures, whereas increased fetal distress86 and shortened gestation lengths89 were observed after a high-amplitude hurricane.
Infectious disease-related morbidity.
The excess risks for infectious disease-related morbidity related to cyclones were reported in Southeast China (5 studies),19,20,32,92,93 the Philippines (1 study),71 South Korea (1 study),60 the United States (3 studies),14,21,94 and India (1 study).95 Among them, two studies focused on overall infectious disease-related morbidity and both of those suggested an increased hospitalization risks for any infectious and parasitic diseases among the general population in eastern Visayas, the Philippines, over the 3-wk period after Typhoon Haiyan [ (95% CI: 1.20, 3.50)]71 and in the population years of age in the East Coast of the United States in the week after a tropical cyclone [ (95% CI: 1.01, 1.08)],14 respectively.
Mixed findings were observed for the associations of cyclone exposures with morbidity of cause-specific infectious diseases.19–21,32,60,92–94 For example, a time-series study on 65 tropical cyclones in Southeast China between 2005 and 2011 found that tropical cyclones were more likely to immediately increase the risk of intestinal and contact-transmitted infectious diseases while decreasing the risk of respiratory infectious diseases among the general population.92 Increased risks of leptospirosis,21 dengue,32,92,93 and infectious diarrhea19,20,60,95 were observed among the general population over a post-cyclone period for up to 4 wk, whereas an immediate reduction in risks of measles, mumps, varicella, and vivax malaria after tropical cyclones92 and a prolonged decline in human immunodeficiency virus testing rate for up to 17 wk after the Hurricane Sandy94 were also suggested. These studies of infectious disease-related morbidity were not included in the meta-analysis owing to the very limited comparable effect estimates caused by the highly heterogeneous outcome definition. For example, for the most studied outcome of diarrhea (4/11 studies),19,20,60,95 two focused on infectious diarrhea,19,60 one on dysentery-related diarrhea,20 and the remaining one on all-cause diarrhea.95
Injury, diabetes, cancer, and other morbidities.
Six U.S. studies investigated injury morbidity associated with cyclones.12,14,67,69,96,97 Consistently elevated risks of morbidity related to injury (hospitalizations,14 ED visits,12 total visits and admissions69) were observed among the population years of age after cyclone exposures. A time-series study on Hurricane Sandy reported more than twice the risk of total visits and admissions due to injury in the 1 y after the hurricane [ (95% CI: 2.43, 2.44)] than in the pre-hurricane periods for the people aged years of age.69 However, less consistent associations were found in the general67,97 or younger population.12,96 For example, an ecological study on Hurricane Floyd suggested an elevated risk of inflicted and noninflicted traumatic brain injury (RR ranged from 5.1 to 10.7) in the 6 months following the hurricane among the children ( months of age).96 On the other hand, another time-series study, on Hurricane Sandy, observed a decreased rate of ED visit due to injury for up to 3 wk among adults (18–64 years of age) or children and adolescents (0–17 years of age).12
For cyclone-related morbidity of diabetes reported by three U.S. studies, only one on eight large-scale hurricanes suggested an increased risk of diabetes hospitalizations among the population years of age [ (95% CI: 1.03, 1.10)] in the month after the hurricane,66 whereas the other two, on Hurricanes Sandy and Maria, reported no associations of diabetes incidence with high hurricane exposure (defined as living in a higher impacted area with a stronger storm surge or a higher number of damaged homes reported) among the people years of age68 and a decreased rates of diabetes among the adults after the hurricane,81 respectively. With respect to cancer morbidity, one study, which included all tropical cyclones that made landfall in the United States between 1999 and 2014, found an average of 4% (95% CI: 3%, 6%) decrease in cancer hospitalization among the population years of age during the week following the cyclone event.14
For other morbidities, increased risks of ED visits for all causes,12,98 renal disease,12 skin and soft tissue infections,12 opioid abuse,99 acute gastrointestinal illness,100 and diabetes exacerbation (i.e., increased glycemic control, blood pressure, and low-density lipoprotein after the cyclone),101 as well as higher risks of overall morbidity,58 gender-based violence,102 physical symptoms (i.e., headaches or migraines, digestive problems),103 and takotsubo syndrome hospitalization,104 were also found to be associated with cyclone exposures. These studies were not included in the meta-analysis because less than three comparable effect estimates were detected for each specific outcome. For the most studied outcome of injury-related morbidity in six studies,12,14,67,69,96,97 four of them were on physician visits,67 hospitalizations,14 ED visits,12 and total admissions and visits69 for all-cause injury, respectively, and one study was on the incidence of inflicted traumatic brain injury.96 For the other outcomes, as indicated above, the studies identified for each specific outcome were very limited and therefore insufficient for a meta-analysis.
Discussion
Key Findings
In the present study, we have comprehensively summarized and quantitatively synthesized the evidence on the health effects of cyclone exposures. A total of 71 eligible studies from eight countries (the United States, China, India, Japan, the Philippines, South Korea, Australia, Brazil) were included, the majority of which were from the United States. These studies investigated the all-cause and cause-specific mortality, as well as morbidity related to injury, CVDs, respiratory diseases, infectious diseases, mental disorders, adverse birth outcomes, cancer, diabetes, and other outcomes (e.g., suicide rates, gender-based violence). Studies mostly included only one cyclone (mostly Hurricane Katrina or Hurricane Sandy) and focused on mental disorders morbidity, as well as all-cause mortality and hospitalizations within 1.5 y after cyclone exposure. Consistently elevated risks of overall mental health-related morbidity and PTSD, as well as all-cause mortality or hospitalizations, were found to be associated with cyclone exposures. Evidence for other outcomes was generally mixed or limited. Further meta-analysis showed modest-to-strong associations between cyclone exposures and all-cause mortality, hospitalizations for all causes, respiratory diseases, and COPD, whereas no associations were found between cyclone exposures and heart disease mortality, diabetes mortality, and preterm birth. High between-study heterogeneity was found for the magnitude of the estimates.
Comparison with Prior Reviews and Interpretations
Four reviews summarized the health impacts of cyclone exposures recently.30,105–107 In 2019, Wang et al. conducted a meta-analysis on the PTSD prevalence among survivors after a tropical cyclone from 39 studies and found the combined prevalence of PTSD after a cyclone was considerably high (17.81%).105 By comparison, among the eight studies23,24,72,73,75–77,83 that evaluated PTSD risk associated with cyclones, we observed consistent findings of substantially higher PTSD risk among the general population,24,72,75,77 pregnant women,76 and certain occupational groups (e.g., high school students, public health workers)23,73,83 who were affected by cyclones for up to 2 y after cyclones exposures. In 2020, Rashida et al. qualitatively reviewed 15 studies on the health effects of cyclones among dialysis patients and found that cyclone exposures were generally associated with increased hospitalizations and ED visits.106 This is consistent with our findings of a robust positive association of cyclone exposures with all-cause hospitalization. In 2021, a more comprehensive scoping review included 24 studies on the health effects of cyclones found that cyclones were associated with the occurrence and exacerbation of multiple diseases.30 One more recent review with meta-analysis synthesized 37 studies on natural disasters and child development and health but included only one study on cyclones.107 In comparison with these two reviews, the results of the present study are different in some respects, which could be attributed to the differences in the number and characteristics of the studies included. The present review systematically and comprehensively reviewed 71 studies on cyclones and health to date and conducted a meta-analysis to quantify the overall magnitude and heterogeneity of the cyclone effects across studies.
Potential Pathways and Vulnerable Population
We found cyclones were consistently associated with elevated risks of PTSD, as well as all-cause mortality and hospitalizations. Cyclones can contribute to the elevated risks of adverse health outcomes through both direct and indirect pathways. Direct impacts, such as physical trauma (e.g., injury, drowning) during exposure, could more immediately increase the risks of hospitalizations and mortality compared with the indirect impacts. Despite the great variation in exposure window among previous studies, elevated all-cause hospitalizations and mortality were mostly observed within 90 d following cyclone exposures. Indirect impacts such as sociopsycho environmental stress, poor or undernutrition associated with cyclones (e.g., loss of property and resources, evacuation, interruption of medical and social support) could manifest at a longer term to increase the risks of occurrence and deterioration of chronic diseases (e.g., mental disorders, CVDs). The elevated PTSD risks among previous studies were mostly observed at months following cyclone exposures. Some studies observed an increased risk of PTSD even after cyclone exposures.72,75
Although limited, evidence also consistently suggested increased morbidity of all respiratory diseases or infectious and parasitic diseases associated with cyclones. The elevated risks in respiratory diseases morbidity following cyclone exposures may be partially attributed to the increased needs for medical equipment to breathe as result of the power outages commonly resulting from cyclone winds.108,109 Increased allergens, especially mold in water-damaged buildings, and air pollutants during debris cleaning may also increase the severity of respiratory diseases and be responsible for the elevated respiratory diseases morbidity.30,110 The elevated rates in morbidity of all infectious and parasitic diseases after cyclones could be attributed to the increased chances of transmission and breeding grounds for microorganisms associated with cyclones (e.g., more contaminated water or bioaerosols).111 However, the indirect pathways through which the cyclones affect most health outcomes remain largely unclear and may vary depending on the cyclones’ physical characteristics (e.g., wind force, precipitation, duration), population background, and geography.
Stratified analyses by potential effect modifiers (e.g., age, gender, race, socioeconomic status) were performed by previous studies to explore vulnerable populations. Children and older adults were generally found to be more susceptible to direct outcomes, such as injury and infection, or indirect outcomes, such as the psychological stress of cyclones.7,20,22,97,112 Children years of age experiencing one or more cyclones were found to have higher risks of mental health disorders in adulthood.113 The adverse effects of cyclones could be more profound and longer-lasting among children and the older adults. Although most studies reported similar direct outcomes (i.e., injury) of cyclones for females and males,7,32,97 women appear to be more likely to suffer psychological distress (e.g., anxiety, PTSD, gender-based violence) than men following cyclone exposures.75,102,114–117 However, the specific reasons for the disproportionate outcomes across sex and age groups remain unclear and may vary by health outcome. The differences in activity pattern (e.g., mobility level),12,118 physiology (e.g., physical strength, health condition),119 awareness (e.g., disaster preparedness),30 and social support120 could be the potential contributing factors. Public and personal services and assistance may need to be extended beyond the immediate aftermath of the cyclone, particularly to the disadvantaged population. Higher risks of adverse outcomes of cyclones were also observed for the lower socioeconomic brackets10,22 or people with preexisting health conditions.59,66 For example, the fatality rate for people living in countries with the lowest tertile of GDP per capita was times greater than those in the highest tertile of GDP per capita after experiencing high-amplitude cyclones.10 The limited resources in a low-income setting hinder efforts for effective disaster responses and management, which have enormous potential to mitigate the adverse effects of cyclones.121,122 Owing to the great heterogeneity across previous studies (e.g., exposure assessment, modeling strategy, subgroup classification) and the lack of evidence for each comparable exposure–outcome pair within subgroups, we could not provide a quantitative and comprehensive assessment for the vulnerable subpopulations associated with cyclones. Despite many claimed disparities in cyclones’ effects across certain subgroups, these differences must be interpreted cautiously owing to the limited generalizability.
Research Gaps and Future Perspectives
First, we found that most studies available on the health effects of cyclone exposures were based in the United States, whereas evidence from other cyclone-prone countries, especially those relatively small and developing countries or regions (e.g., Vietnam, Cuba, the Philippines, Taiwan) is relatively scarce.123 Studies from these countries or regions are highly warranted to characterize the geographical pattern of cyclone health effects and to assess the potential contributing factors (e.g., socioeconomic and demographic factors, government effectiveness) to the heterogeneity of effects.
Second, the elevated risks of overall mental health-related morbidity, PTSD, as well as all-cause mortality or hospitalization associated with cyclone exposures, have been well documented (Table S2), whereas the evidence on cyclones and other health outcomes, such as chronic diseases (e.g., CVDs, cancer, diabetes), and adverse birth outcomes (e.g., preterm birth, low birth weight), remains limited or inconsistent. Although it is currently not well established, the risk and burden of these diseases indirectly triggered by cyclones could considerably outweigh those associated directly with the cyclones themselves.124 More work needs to be done to consistently quantify the excess risk and burden, as well as to identify and formalize the pathways through which cyclones affect these understudied health outcomes.
Third, previous studies have generally investigated the health outcomes associated with one cyclone within a limited geographic region and time span. Further, the considerable heterogeneity in previous studies in terms of exposure assessment, modeling strategy, and exposure window hindered the synthesis and generalizability of the findings. There is an overall research gap in consistently quantifying the health risks and burdens associated with cyclones over long time spans. Future studies with a long-term follow-up for multiple cyclones are needed to explore the time trend of the global, regional, and national health risks and burden of cyclones under the context of a changing climate.
Fourth, the ROB assessment indicated a major concern about exposure assessment bias among previous studies. The exposure assessments of cyclones in previous studies were generally based on questionnaires, the time of landfall, or the cyclone track, which is a static point-in-time estimate. These data do not account for the time-varying spatial structure of cyclones (i.e., the intensity and extent of the winds) and lead to potentially higher risks of exposure classification (e.g., the inaccurate estimate of the duration of cyclone for participants) and fail to account for the time-varying and cumulative effects of cyclone exposures. Advanced models with high spatiotemporal resolution (e.g., wind field model) are highly warranted in future studies to assess the cyclone exposure with different continuous metrics (e.g., cyclone-related full wind field, cumulative precipitation) in an attempt to characterize the exposure–lag–response (ELR) relationship of cyclones and health outcomes. The evidence on the ELR relationship between cyclone exposure metrics (e.g., maximum windspeed, cumulative rainfall, distance) and public health is scarce, which could have important implications for disaster planning and policy making. More effort should be made to estimate the ELR relationship considering cyclone-specific health risks based on an advanced model with consistent and rigorous quantitative assessment of cyclone exposures.13
Finally, most prior studies derived the excess mortalities or morbidities related to cyclones using prepost comparisons or unexposed neighboring areas as controls. This may lead to residual confounding by either temporal trends or spatial gradients in the health risks.17 Analytical strategy with a self-matched design for exposed days with unexposed days in both pre- and post-cyclone periods is recommended for future studies based on time-series surveillance data of health.7,14,15,17
Limitations
Several limitations should be noted in our study. First, the high between-study heterogeneity that we detected reduced the credibility of the pooled estimates. Second, given the limited number of comparable studies to be included in the meta-analysis, the limitations of visual assessment of funnel plots for publication bias and the low power of statistical tests for small-sample effects, such as Egger’s test, should also be acknowledged in this study. We also could not conduct meta-regression to examine the source of heterogeneity because there were not enough comparable studies (a minimum of 10 studies is required for a meta-regression model).125,126 Third, as a systematic review that aimed to quantify the health outcomes related to cyclone exposures, studies on the health effects of subsequent events after cyclones (e.g., secondary losses from cyclones) or studies that used mediation analysis to assess the pathways between cyclone exposures and health outcomes were excluded.127–135 Further work may be needed to include these studies and systematically synthesize the pathways for specific health outcomes and the effects for a specific cyclone-related event (e.g., flood, disaster-related stress). Fourth, although there were a few studies from developing countries, such as China and the Philippines, most of the included studies came from the United States. The between-country difference in factors, such as the rate of urbanization and population background in coastal cities, may reduce the generalizability of current evidence to populations in other countries. Fifth, our findings were also affected by the risk of residual and unmeasured confounding of the included studies. As indicated in the ROB assessment, the confounding bias could vary markedly across studies. For example, a low risk from confounding bias was observed in well-controlled studies like Sun et al., which adjusted for long-time trend, seasonality, day of week, daily expected number of health outcomes and county random intercept in the model,17 whereas high risks were found in another nine studies that did not account for any confounding factor when assessing the elevated health risks associated with cyclone exposures9,18,20,25,60,61,67,92,102 (e.g., crude RRs derived by comparing outcome counts for exposed and nonexposed periods136; Table S5). The expected variation in health outcomes as a result of factors, such as natural variations of time trend and population background, is an important potential confounder, particularly for time-series and case-crossover studies of long-term health impacts of cyclones. Sixth, although some included studies explored effect modifications by several factors (e.g., age, sex) in subgroup analyses, we could not perform a quantitative and conclusive summary of these findings owing to the limited comparable evidence. Thus, our results may be less relevant for vulnerable population subgroups. Finally, we included only studies published in peer-reviewed journals, so some eligible gray literature may have been omitted in the present study.
Conclusions
Although there is considerable heterogeneity in the magnitude of the effect estimates, the evidence generally supported elevated risks of overall mental health morbidity, PTSD, and all-cause mortality or hospitalization following a large-scale cyclone. Evidence on the risks and burdens of other health outcomes, such as chronic diseases (e.g., CVDs, cancer, diabetes) and adverse birth outcomes associated with cyclones, was limited or inconsistent. Several research gaps, including the lack of a rigorous quantitative and continuous assessment of cyclone exposures, the great inconsistency in modeling approaches, study designs, analytical strategies and exposure window, and the potential issues in the comparability and generalizability of results, should be noted among most previous studies. To enhance our understanding of the spatiotemporal health impacts of cyclones under a changing climate, more work over larger scales of space and time with multiple cyclones and advanced modeling strategy is highly warranted.
Supplementary Material
Acknowledgments
Contributions of the authors were as follows: draft writing, methodology, and formal analysis: W.H.; review and editing: R.X., Z.Y., P.Y., T.Y., E.A.R., S.L., and Y.Guo; resources, conceptualization, supervision, and project administration funding acquisition: Y.Guo and S.L.
W.H., Y.Gao, R.X., P.Y., and T.Y. are supported by the China Scholarship Council (W.H.: 202006380055; Y.Gao: 202008110182; R.X.: 201806010405; P.Y.: 201906210065; and T.Y.: 201906320051). Z.Y. is supported by a Monash Graduate Scholarship and Monash International Tuition Scholarship. Y.Guo is supported by a Career Development Fellowship (GNT1163693) and a Leader Fellowship (GNT2008813) of the Australian National Health and Medical Research Council. S.L. is supported by an Emerging Leader Fellowship (GNT2009866) of the Australian National Health and Medical Research Council.
This study was supported by the Australian Research Council (DP210102076) and the Australian National Health and Medical Research Council (GNT2000581).
All data used in our study are available online.
References
- 1.Diakakis M, Deligiannakis G, Katsetsiadou K, Lekkas E. 2015. Hurricane Sandy mortality in the Caribbean and continental North America. Disaster Prev Manag 24(1):132–148, 10.1108/DPM-05-2014-0082. [DOI] [Google Scholar]
- 2.Wang S, Toumi R. 2021. Recent migration of tropical cyclones toward coasts. Science 371(6528):514–517, PMID: , 10.1126/science.abb9038. [DOI] [PubMed] [Google Scholar]
- 3.Li L, Chakraborty P. 2020. Slower decay of landfalling hurricanes in a warming world. Nature 587(7833):230–234, PMID: , 10.1038/s41586-020-2867-7. [DOI] [PubMed] [Google Scholar]
- 4.Bhatia K, Vecchi G, Murakami H, Underwood S, Kossin J. 2018. Projected response of tropical cyclone intensity and intensification in a global climate model. J Climate 31(20):8281–8303, 10.1175/JCLI-D-17-0898.1. [DOI] [Google Scholar]
- 5.Bhatia KT, Vecchi GA, Knutson TR, Murakami H, Kossin J, Dixon KW, et al. 2019. Recent increases in tropical cyclone intensification rates. Nat Commun 10(1):3942, PMID: , 10.1038/s41467-019-11922-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shultz JM, Peek L, Galea S. 2022. Advances in estimating mortality associated with tropical cyclones in the US. JAMA 327(10):929–931, PMID: , 10.1001/jama.2022.0069. [DOI] [PubMed] [Google Scholar]
- 7.Parks RM, Benavides J, Anderson GB, Nethery RC, Navas-Acien A, Dominici F, et al. 2022. Association of tropical cyclones with county-level mortality in the US. JAMA 327(10):946–955, PMID: , 10.1001/jama.2022.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cruz-Cano R, Mead EL. 2019. Causes of excess deaths in Puerto Rico after Hurricane Maria: a time-series estimation. Am J Public Health 109(7):1050–1052, PMID: , 10.2105/AJPH.2019.305015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dosa D, Feng Z, Hyer K, Brown LM, Thomas K, Mor V. 2010. Effects of Hurricane Katrina on nursing facility resident mortality, hospitalization, and functional decline. Disaster Med Public Health Prep 4(suppl 1):S28–S32, PMID: , 10.1001/dmp.2010.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dresser C, Allison J, Broach J, Smith ME, Milsten A. 2016. High-amplitude Atlantic hurricanes produce disparate mortality in small, low-income countries. Disaster Med Public Health Prep 10(6):832–837, PMID: , 10.1017/dmp.2016.62. [DOI] [PubMed] [Google Scholar]
- 11.Kim S, Kulkarni PA, Rajan M, Thomas P, Tsai S, Tan C, et al. 2017. Hurricane Sandy (New Jersey): mortality rates in the following month and quarter. Am J Public Health 107(8):1304–1307, PMID: , 10.2105/AJPH.2017.303826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weinberger KR, Kulick ER, Boehme AK, Sun S, Dominici F, Wellenius GA. 2021. Association between Hurricane Sandy and emergency department visits in New York City by age and cause. Am J Epidemiol 190(10):2138–2147, PMID: , 10.1093/aje/kwab127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nethery RC, Katz-Christy N, Kioumourtzoglou MA, Parks RM, Schumacher A, Anderson GB. 2023. Integrated causal–predictive machine learning models for tropical cyclone epidemiology. Biostatistics 24(2):449–464, PMID: , 10.1093/biostatistics/kxab047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parks RM, Anderson GB, Nethery RC, Navas-Acien A, Dominici F, Kioumourtzoglou MA. 2021. Tropical cyclone exposure is associated with increased hospitalization rates in older adults. Nat Commun 12(1):1545, PMID: , 10.1038/s41467-021-21777-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yan M, Wilson A, Dominici F, Wang Y, Al-Hamdan M, Crosson W, et al. 2021. Tropical cyclone exposures and risks of emergency Medicare hospital admission for cardiorespiratory diseases in 175 urban United States counties, 1999–2010. Epidemiology 32(3):315–326, PMID: , 10.1097/EDE.0000000000001337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xiong X, Harville EW, Mattison DR, Elkind-Hirsch K, Pridjian G, Buekens P. 2008. Exposure to Hurricane Katrina, post-traumatic stress disorder and birth outcomes. Am J Med Sci 336(2):111–115, PMID: , 10.1097/MAJ.0b013e318180f21c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sun S, Weinberger KR, Yan M, Anderson GB, Wellenius GA. 2020. Tropical cyclones and risk of preterm birth: a retrospective analysis of 20 million births across 378 US counties. Environ Int 140:105825, PMID: , 10.1016/j.envint.2020.105825. [DOI] [PubMed] [Google Scholar]
- 18.Antipova A, Curtis A. 2015. The post-disaster negative health legacy: pregnancy outcomes in Louisiana after Hurricane Andrew. Disasters 39(4):665–686, PMID: , 10.1111/disa.12125. [DOI] [PubMed] [Google Scholar]
- 19.Deng Z, Xun H, Zhou M, Jiang B, Wang S, Guo Q, et al. 2015. Impacts of tropical cyclones and accompanying precipitation on infectious diarrhea in cyclone landing areas of Zhejiang Province, China. Int J Environ Res Public Health 12(2):1054–1068, PMID: , 10.3390/ijerph120201054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang W, Xun HM, Zhou MG, Jiang BF, Wang SW, Guo Q, et al. 2015. Impacts of Typhoon ‘Koppu’ on infectious diarrhea in Guangdong Province, China. Biomed Environ Sci 28(12):920–923, PMID: , 10.3967/bes2015.127. [DOI] [PubMed] [Google Scholar]
- 21.Sanders EJ, Rigau-Pérez JG, Smits HL, Deseda CC, Vorndam VA, Aye T, et al. 1999. Increase of leptospirosis in dengue-negative patients after a hurricane in Puerto Rico in 1996 [correction of 1966]. Am J Trop Med Hyg 61(3):399–404, PMID: , 10.4269/ajtmh.1999.61.399. [DOI] [PubMed] [Google Scholar]
- 22.Begum TF, Lin Z, Primeau M, Lin S. 2022. Assessing short-term and long-term mental health effects among older adults after Hurricane Sandy. Sci Total Environ 825:153753, PMID: , 10.1016/j.scitotenv.2022.153753. [DOI] [PubMed] [Google Scholar]
- 23.Garrison CZ, Weinrich MW, Hardin SB, Weinrich S, Wang L. 1993. Post-traumatic stress disorder in adolescents after a hurricane. Am J Epidemiol 138(7):522–530, PMID: , 10.1093/oxfordjournals.aje.a116886. [DOI] [PubMed] [Google Scholar]
- 24.Schwartz RM, Rothenberg P, Kerath SM, Liu B, Taioli E. 2016. The lasting mental health effects of Hurricane Sandy on residents of the Rockaways. J Emerg Manag 14(4):269–279, PMID: , 10.5055/jem.2016.0292. [DOI] [PubMed] [Google Scholar]
- 25.Kessler RC, Galea S, Jones RT, Parker HA, Hurricane Katrina Community Advisory Group. 2006. Mental illness and suicidality after Hurricane Katrina. Bull World Health Organ 84(12):930–939, PMID: , 10.2471/blt.06.033019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Konkel L. 2020. Tropical cyclone exposures and health: a new data set to assess associations over time. Environ Health Perspect 128(12):124001, PMID: , 10.1289/EHP8653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jiao Z, Kakoulides SV, Moscona J, Whittier J, Srivastav S, Delafontaine P, et al. 2012. Effect of Hurricane Katrina on incidence of acute myocardial infarction in New Orleans three years after the storm. Am J Cardiol 109(4):502–505, PMID: , 10.1016/j.amjcard.2011.09.045. [DOI] [PubMed] [Google Scholar]
- 28.Furukawa K, Ootsuki M, Kodama M, Arai H. 2012. Exacerbation of dementia after the earthquake and tsunami in Japan. J Neurol 259(6):1243, PMID: , 10.1007/s00415-011-6329-x. [DOI] [PubMed] [Google Scholar]
- 29.Mitchell RD, Aitken P, Franklin RC. 2014. The physical health impacts of tropical cyclones. Ann ACTM 15(1):2–8, 10.3316/informit.174837299731422. [DOI] [Google Scholar]
- 30.Waddell SL, Jayaweera DT, Mirsaeidi M, Beier JC, Kumar N. 2021. Perspectives on the health effects of hurricanes: a review and challenges. Int J Environ Res Public Health 18(5):2756, PMID: , 10.3390/ijerph18052756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cowan KN, Pennington AF, Gregory T, Hsu J. 2022. Impact of hurricanes on children with asthma: a systematic literature review. Disaster Med Public Health Prep 16(2):777–782, PMID: , 10.1017/dmp.2020.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li C, Zhao Q, Zhao Z, Liu Q, Ma W. 2021. The association between tropical cyclones and dengue fever in the Pearl River Delta, China during 2013–2018: a time-stratified case-crossover study. PLoS Negl Trop Dis 15(9):e0009776, PMID: , 10.1371/journal.pntd.0009776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. 2010. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341, PMID: , 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 34.Morgan RL, Whaley P, Thayer KA, Schünemann HJ. 2018. Identifying the PECO: a framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ Int 121(pt 1):1027–1031, PMID: , 10.1016/j.envint.2018.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Braithwaite I, Zhang S, Kirkbride JB, Osborn DPJ, Hayes JF. 2019. Air pollution (particulate matter) exposure and associations with depression, anxiety, bipolar, psychosis and suicide risk: a systematic review and meta-analysis. Environ Health Perspect 127(12):126002, PMID: , 10.1289/EHP4595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Woodruff TJ, Sutton P. 2014. The Navigation Guide systematic review methodology: a rigorous and transparent method for translating environmental health science into better health outcomes. Environ Health Perspect 122(10):1007–1014, PMID: , 10.1289/ehp.1307175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huang WZ, Yang BY, Zeeshan M, Dong GH. 2021. Chapter 10 – Associations between ambient particulate matter and lung cancer: a systematic review and meta-analyses up to 2020. In: Air Pollution, Climate, and Health. Gao M, Wang Z, Carmichael G, eds. Amsterdam, the Netherlands: Elsevier, 207–228. [Google Scholar]
- 38.NTP (National Toxicology Program). 2023. Risk of bias tool. https://ntp.niehs.nih.gov/whatwestudy/assessments/noncancer/riskbias [accessed 2 July 2023].
- 39.Boogaard H, Patton AP, Atkinson RW, Brook JR, Chang HH, Crouse DL, et al. 2022. Long-term exposure to traffic-related air pollution and selected health outcomes: a systematic review and meta-analysis. Environ Int 164:107262, PMID: , 10.1016/j.envint.2022.107262. [DOI] [PubMed] [Google Scholar]
- 40.Hashizume M, Kim Y, Ng CFS, Chung Y, Madaniyazi L, Bell ML, et al. 2020. Health effects of Asian dust: a systematic review and meta-analysis. Environ Health Perspect 128(6):066001, PMID: , 10.1289/EHP5312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Luo YN, Huang WZ, Liu XX, Markevych I, Bloom MS, Zhao T, et al. 2020. Greenspace with overweight and obesity: a systematic review and meta-analysis of epidemiological studies up to 2020. Obes Rev 21(11):e13078, PMID: , 10.1111/obr.13078. [DOI] [PubMed] [Google Scholar]
- 42.Quansah R, Armah FA, Essumang DK, Luginaah I, Clarke E, Marfoh K, et al. 2015. Association of arsenic with adverse pregnancy outcomes/infant mortality: a systematic review and meta-analysis. Environ Health Perspect 123(5):412–421, PMID: , 10.1289/ehp.1307894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grimes DA, Schulz KF. 2008. Making sense of odds and odds ratios. Obstet Gynecol 111(2 pt 1):423–426, PMID: , 10.1097/01.AOG.0000297304.32187.5d. [DOI] [PubMed] [Google Scholar]
- 44.Sedgwick P. 2014. Relative risks versus odds ratios. BMJ 348:g1407, 10.1136/bmj.g1407. [DOI] [Google Scholar]
- 45.Higgins JPT, Thompson SG. 2002. Quantifying heterogeneity in a meta‐analysis. Stat Med 21(11):1539–1558, PMID: , 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 46.Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. 2008. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol 61(10):991–996, PMID: , 10.1016/j.jclinepi.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 47.Egger M, Smith GD, Schneider M, Minder C. 1997. Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634, PMID: , 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Duval S, Tweedie R. 2000. Trim and fill: a simple funnel‐plot–based method of testing and adjusting for publication bias in meta‐analysis. Biometrics 56(2):455–463, PMID: , 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 49.Santos-Burgoa C, Sandberg J, Suárez E, Goldman-Hawes A, Zeger S, Garcia-Meza A, et al. 2018. Differential and persistent risk of excess mortality from Hurricane Maria in Puerto Rico: a time-series analysis. Lancet Planet Health 2(11):e478–e488, PMID: , 10.1016/S2542-5196(18)30209-2. [DOI] [PubMed] [Google Scholar]
- 50.Santos-Lozada AR, Howard JT. 2018. Use of death counts from vital statistics to calculate excess deaths in Puerto Rico following Hurricane Maria. JAMA 320(14):1491–1493, PMID: , 10.1001/jama.2018.10929. [DOI] [PubMed] [Google Scholar]
- 51.Rivera R, Rolke W. 2018. Estimating the death toll of Hurricane Maria. Significance 14(1):8–9, 10.1111/j.1740-9713.2018.01102.x. [DOI] [Google Scholar]
- 52.Kishore N, Marqués D, Mahmud A, Kiang MV, Rodriguez I, Fuller A, et al. 2018. Mortality in Puerto Rico after Hurricane Maria. N Engl J Med 379(2):162–170, PMID: , 10.1056/NEJMsa1803972. [DOI] [PubMed] [Google Scholar]
- 53.Marazzi M, Miloucheva B, Bobonis GJ. 2022. Mortality of Puerto Ricans in the USA post Hurricane Maria: an interrupted time series analysis. BMJ Open 12(8):e058315, PMID: , 10.1136/bmjopen-2021-058315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Acosta RJ, Irizarry RA. 2022. A flexible statistical framework for estimating excess mortality. Epidemiology 33(3):346–353, PMID: , 10.1097/EDE.0000000000001445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rivera-Hernandez M, Kim D, Nguyen KH, Thorsness R, Lee Y, Swaminathan S, et al. 2022. Changes in migration and mortality among patients with kidney failure in Puerto Rico after Hurricane Maria. JAMA Health Forum 3(8):e222534, PMID: , 10.1001/jamahealthforum.2022.2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dosa DM, Skarha J, Peterson LJ, Jester DJ, Sakib N, Ogarek J, et al. 2020. Association between exposure to Hurricane Irma and mortality and hospitalization in Florida nursing home residents. JAMA Netw Open 3(10):e2019460, PMID: , 10.1001/jamanetworkopen.2020.19460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kutner NG, Muntner P, Huang Y, Zhang R, Cohen AJ, Anderson AH, et al. 2009. Effect of Hurricane Katrina on the mortality of dialysis patients. Kidney Int 76(7):760–766, PMID: , 10.1038/ki.2009.268. [DOI] [PubMed] [Google Scholar]
- 58.Burton LC, Skinner EA, Uscher-Pines L, Lieberman R, Leff B, Clark R, et al. 2009. Health of Medicare Advantage plan enrollees at 1 year after Hurricane Katrina. Am J Manag Care 15(1):13–22, PMID: , https://europepmc.org/article/med/19146360. [PubMed] [Google Scholar]
- 59.Quast T, Andel R, Sadhu AR. 2019. Long-term effects of disasters on seniors with diabetes: evidence from Hurricanes Katrina and Rita. Diabetes Care 42(11):2090–2097, PMID: , 10.2337/dc19-0567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim S, Shin Y, Kim H, Pak H, Ha J. 2013. Impacts of typhoon and heavy rain disasters on mortality and infectious diarrhea hospitalization in South Korea. Int J Environ Health Res 23(5):365–376, PMID: , 10.1080/09603123.2012.733940. [DOI] [PubMed] [Google Scholar]
- 61.Hendrickson LA, Vogt RL. 1996. Mortality of Kauai residents in the 12-month period following Hurricane Iniki. Am J Epidemiol 144(2):188–191, PMID: , 10.1093/oxfordjournals.aje.a008907. [DOI] [PubMed] [Google Scholar]
- 62.Swerdel JN, Janevic TM, Cosgrove NM, Kostis JB, Myocardial Infarction Data Acquisition System (MIDAS 24) Study Group. 2014. The effect of Hurricane Sandy on cardiovascular events in New Jersey. J Am Heart Assoc 3(6):e001354, PMID: , 10.1161/JAHA.114.001354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bell SA, Iwashyna TJ, Zhang X, Chen B, Davis MA. 2021. All-cause hospitalizations after large-scale hurricanes among older adults: a self-controlled case series study. Prehosp Disaster Med 36(1):25–31, PMID: , 10.1017/S1049023X20001387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sharp MJ, Sun M, Ledneva T, Lauper U, Pantea C, Lin S. 2016. Effect of Hurricane Sandy on health care services utilization under Medicaid. Disaster Med Public Health Prep 10(3):472–484, PMID: , 10.1017/dmp.2016.75. [DOI] [PubMed] [Google Scholar]
- 65.Howard D, Zhang R, Huang Y, Kutner N. 2012. Hospitalization rates among dialysis patients during Hurricane Katrina. Prehosp Disaster Med 27(4):325–329, PMID: , 10.1017/S1049023X12000945. [DOI] [PubMed] [Google Scholar]
- 66.Bell SA, Donnelly JP, Li W, Davis MA. 2022. Hospitalizations for chronic conditions following hurricanes among older adults: a self-controlled case series analysis. J Am Geriatr Soc 70(6):1695–1703, PMID: , 10.1111/jgs.17702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hendrickson LA, Vogt RL, Goebert D, Pon E. 1997. Morbidity on Kauai before and after Hurricane Iniki. Prev Med 26(5 pt 1):711–716, PMID: , 10.1006/pmed.1997.0196. [DOI] [PubMed] [Google Scholar]
- 68.Sands LP, Do Q, Du P, Pruchno R. 2022. Peritraumatic stress from a disaster increases risk for onset of chronic diseases among older adults. Innov Aging 6(1):igab052, PMID: , 10.1093/geroni/igab052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lawrence WR, Lin Z, Lipton EA, Birkhead G, Primeau M, Dong GH, et al. 2019. After the storm: short-term and long-term health effects following Superstorm Sandy among the elderly. Disaster Med Public Health Prep 13(1):28–32, PMID: , 10.1017/dmp.2018.152. [DOI] [PubMed] [Google Scholar]
- 70.Cowan KN, Pennington AF, Sircar K, Flanders WD. 2021. Asthma-related emergency department visits in North Carolina following Hurricane Irene. Disaster Med Public Health Prep 17:e16, PMID: , 10.1017/dmp.2021.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.van Loenhout JAF, Cuesta JG, Abello JE, Isiderio JM, de Lara-Banquesio ML, Guha-Sapir D. 2018. The impact of Typhoon Haiyan on admissions in two hospitals in Eastern Visayas, Philippines. PLoS One 13(1):e0191516, PMID: , 10.1371/journal.pone.0191516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schwartz RM, Rasul R, Gargano LM, Lieberman-Cribbin W, Brackbill RM, Taioli E. 2019. Examining associations between Hurricane Sandy exposure and posttraumatic stress disorder by community of residence. J Trauma Stress 32(5):677–687, PMID: , 10.1002/jts.22445. [DOI] [PubMed] [Google Scholar]
- 73.Bromet EJ, Clouston S, Gonzalez A, Kotov R, Guerrera KM, Luft BJ. 2017. Hurricane Sandy exposure and the mental health of World Trade Center responders. J Trauma Stress 30(2):107–114, PMID: , 10.1002/jts.22178. [DOI] [PubMed] [Google Scholar]
- 74.An R, Qiu Y, Xiang X, Ji M, Guan C. 2019. Impact of Hurricane Katrina on mental health among US adults. Am J Health Behav 43(6):1186–1199, PMID: , 10.5993/AJHB.43.6.15. [DOI] [PubMed] [Google Scholar]
- 75.Schwartz RM, Gillezeau CN, Liu B, Lieberman-Cribbin W, Taioli E. 2017. Longitudinal impact of Hurricane Sandy exposure on mental health symptoms. Int J Environ Res Public Health 14(9):957, PMID: , 10.3390/ijerph14090957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Harville EW, Xiong X, Pridjian G, Elkind-Hirsch K, Buekens P. 2009. Postpartum mental health after Hurricane Katrina: a cohort study. BMC Pregnancy Childbirth 9:21, PMID: , 10.1186/1471-2393-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mills LD, Mills TJ, Macht M, Levitan R, De Wulf A, Afonso NS. 2012. Post-traumatic stress disorder in an emergency department population one year after Hurricane Katrina. J Emerg Med 43(1):76–82, PMID: , 10.1016/j.jemermed.2011.06.124. [DOI] [PubMed] [Google Scholar]
- 78.Bozick R. 2021. The effects of Hurricane Harvey on the physical and mental health of adults in Houston. Health Place 72:102697, PMID: , 10.1016/j.healthplace.2021.102697. [DOI] [PubMed] [Google Scholar]
- 79.Tian XL, Guan X. 2015. The impact of Hurricane Katrina on students’ behavioral disorder: a difference-in-difference analysis. Int J Environ Res Public Health 12(5):5540–5560, PMID: , 10.3390/ijerph120505540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fried BJ, Domino ME, Shadle J. 2005. Use of mental health services after Hurricane Floyd in North Carolina. Psychiatr Serv 56(11):1367–1373, PMID: , 10.1176/appi.ps.56.11.1367. [DOI] [PubMed] [Google Scholar]
- 81.Cortes YI, Lassalle PP, Perreira KM. 2023. Health care access and health indicators in Puerto Rico pre- and post- Hurricane Maria: behavioral risk factor surveillance system (2015–2019). J Immigr Minor Health 25(2):247–254, PMID: , 10.1007/s10903-022-01391-z. [DOI] [PubMed] [Google Scholar]
- 82.Frahm KA, Barnett SD, Brown LM, Hickling EJ, Olney R, Campbell RR, et al. 2013. Posttraumatic stress disorder and use of psychiatric and alcohol related services: the effect of the 2004–2005 Florida hurricane seasons on veterans. Community Ment Health J 49(6):636–642, PMID: , 10.1007/s10597-012-9558-2. [DOI] [PubMed] [Google Scholar]
- 83.Fullerton CS, McKibben JBA, Reissman DB, Scharf T, Kowalski-Trakofler KM, Shultz JM, et al. 2013. Posttraumatic stress disorder, depression, and alcohol and tobacco use in public health workers after the 2004 Florida hurricanes. Disaster Med Public Health Prep 7(1):89–95, PMID: , 10.1017/dmp.2013.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tees MT, Harville EW, Xiong X, Buekens P, Pridjian G, Elkind-Hirsch K. 2010. Hurricane Katrina-related maternal stress, maternal mental health, and early infant temperament. Matern Child Health J 14(4):511–518, PMID: , 10.1007/s10995-009-0486-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Grabich SC, Robinson WR, Konrad CE, Horney JA. 2017. Impact of hurricane exposure on reproductive health outcomes, Florida, 2004. Disaster Med Public Health Prep 11(4):407–411, PMID: , 10.1017/dmp.2016.158. [DOI] [PubMed] [Google Scholar]
- 86.Zahran S, Snodgrass JG, Peek L, Weiler S. 2010. Maternal hurricane exposure and fetal distress risk. Risk Anal 30(10):1590–1601, PMID: , 10.1111/j.1539-6924.2010.01453.x. [DOI] [PubMed] [Google Scholar]
- 87.Meir O, Satu K, Xie X, Abdissa N, Lubna P, Sangita J. 2021. The impact of Hurricane Katrina, a major natural disaster, on assisted reproductive outcomes through an analysis of 451,848 ART cycles. Sci Rep 11(1):17864, PMID: , 10.1038/s41598-021-97402-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Harville EW, Pan K, Beitsch L, Sherchan SP, Gonsoroski E, Uejio C, et al. 2023. Hurricane Michael and adverse birth outcomes in the Florida panhandle: analysis of vital statistics data. Disaster Med Public Health Prep 17:e94, PMID: , 10.1017/dmp.2021.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hochard J, Li Y, Abashidze N. 2022. Associations of hurricane exposure and forecasting with impaired birth outcomes. Nat Commun 13(1):6746, PMID: , 10.1038/s41467-022-33865-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Parayiwa C, Harley D, Clark R, Behie A, Lal A. 2022. Association between severe cyclone events and birth outcomes in Queensland, Australia, 2008–2018: a population based retrospective cohort study. Aust N Z J Public Health 46(6):835–841, PMID: , 10.1111/1753-6405.13273. [DOI] [PubMed] [Google Scholar]
- 91.de Oliveira VH, Lee I, Quintana-Domeque C. 2023. Natural disasters and early human development: Hurricane Catarina and infant health in Brazil. J Hum Resour 58(3):819–851, 10.3368/jhr.59.1.0816-8144R1. [DOI] [Google Scholar]
- 92.Zheng J, Han W, Jiang B, Ma W, Zhang Y. 2017. Infectious diseases and tropical cyclones in southeast China. Int J Environ Res Public Health 14(5):494, PMID: , 10.3390/ijerph14050494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li C, Zhao Z, Yan Y, Liu Q, Zhao Q, Ma W. 2022. Short-term effects of tropical cyclones on the incidence of dengue: a time-series study in Guangzhou, China. Parasit Vectors 15(1):358, PMID: , 10.1186/s13071-022-05486-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ekperi LI, Thomas E, LeBlanc TT, Adams EE, Wilt GE, Molinari NA, et al. 2018. The impact of Hurricane Sandy on HIV testing rates: an interrupted time series analysis, January 1, 2011–December 31, 2013. PLoS Curr 10:ecurrents.dis.ea09f9573dc292951b7eb0cf9f395003, PMID: , 10.1371/currents.dis.ea09f9573dc292951b7eb0cf9f395003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Panda S, Pati KK, Bhattacharya MK, Koley H, Pahari S, Nair GB. 2011. Rapid situation & response assessment of diarrhoea outbreak in a coastal district following tropical cyclone AILA in India. Indian J Med Res 133(4):395–400, PMID: . [PMC free article] [PubMed] [Google Scholar]
- 96.Keenan HT, Marshall SW, Nocera MA, Runyan DK. 2004. Increased incidence of inflicted traumatic brain injury in children after a natural disaster. Am J Prev Med 26(3):189–193, PMID: , 10.1016/j.amepre.2003.10.023. [DOI] [PubMed] [Google Scholar]
- 97.Marshall EG, Lu SE, Shi Z, Swerdel J, Borjan M, Lumia ME. 2016. Work-related unintentional injuries associated with Hurricane Sandy in New Jersey. Disaster Med Public Health Prep 10(3):394–404, PMID: , 10.1017/dmp.2016.47. [DOI] [PubMed] [Google Scholar]
- 98.Lin CH, Hou SK, Shih FFY, Su S. 2013. The effect of tropical cyclones (typhoons) on emergency department visits. J Emerg Med 45(3):372–379, PMID: , 10.1016/j.jemermed.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 99.McCann-Pineo M, Taioli E, Schwartz RM. 2021. Exposure to Hurricane Sandy and risk of opioid abuse. Subst Use Misuse 56(8):1241–1245, PMID: , 10.1080/10826084.2021.1912098. [DOI] [PubMed] [Google Scholar]
- 100.Quist AJL, Fliss MD, Wade TJ, Delamater PL, Richardson DB, Engel LS. 2022. Hurricane flooding and acute gastrointestinal illness in North Carolina. Sci Total Environ 809:151108, PMID: , 10.1016/j.scitotenv.2021.151108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fonseca VA, Smith H, Kuhadiya N, Leger SM, Yau CL, Reynolds K, et al. 2009. Impact of a natural disaster on diabetes: exacerbation of disparities and long-term consequences. Diabetes Care 32(9):1632–1638, PMID: , 10.2337/dc09-0670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Anastario M, Shehab N, Lawry L. 2009. Increased gender-based violence among women internally displaced in Mississippi 2 years post-Hurricane Katrina. Disaster Med Public Health Prep 3(1):18–26, PMID: , 10.1097/DMP.0b013e3181979c32. [DOI] [PubMed] [Google Scholar]
- 103.Zacher M, Raker EJ, Arcaya MC, Lowe SR, Rhodes J, Waters MC. 2021. Physical health symptoms and Hurricane Katrina: individual trajectories of development and recovery more than a decade after the storm. Am J Public Health 111(1):127–135, PMID: , 10.2105/AJPH.2020.305955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kanaoka K, Okayama S, Terasaki S, Nakano T, Ishii M, Nakai M, et al. 2020. Role of climatic factors in the incidence of Takotsubo syndrome: a nationwide study from 2012 to 2016. ESC Heart Fail 7(5):2629–2636, PMID: , 10.1002/ehf2.12843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wang Z, Wu X, Dai W, Kaminga AC, Wu X, Pan X, et al. 2019. The prevalence of posttraumatic stress disorder among survivors after a typhoon or hurricane: a systematic review and meta-analysis. Disaster Med Public Health Prep 13(5–6):1065–1073, PMID: , 10.1017/dmp.2019.26. [DOI] [PubMed] [Google Scholar]
- 106.Smith RS, Zucker RJ, Frasso R. 2020. Natural disasters in the Americas, dialysis patients, and implications for emergency planning: a systematic review. Prev Chronic Dis 17:E42, PMID: , 10.5888/pcd17.190430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lafortune S, Laplante DP, Elgbeili G, Li X, Lebel S, Dagenais C, et al. 2021. Effect of natural disaster-related prenatal maternal stress on child development and health: a meta-analytic review. Int J Environ Res Public Health 18(16):8332, PMID: , 10.3390/ijerph18168332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lane K, Charles-Guzman K, Wheeler K, Abid Z, Graber N, Matte T. 2013. Health effects of coastal storms and flooding in urban areas: a review and vulnerability assessment. J Environ Public Health 2013:913064, PMID: , 10.1155/2013/913064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Liu H, Davidson RA, Rosowsky DV, Stedinger JR. 2005. Negative binomial regression of electric power outages in hurricanes. J Infrastruct Syst 11(4):258–267, 10.1061/(ASCE)1076-0342(2005)11:4(258). [DOI] [Google Scholar]
- 110.Bourgeois B, Owens JW. 2014. The influence of Hurricanes Katrina and Rita on the inflammatory cytokine response and protein expression in A549 cells exposed to PM2.5 collected in the Baton Rouge–Port Allen industrial corridor of southeastern Louisiana in 2005. Toxicol Mech Methods 24(3):220–242, PMID: , 10.3109/15376516.2014.881945. [DOI] [PubMed] [Google Scholar]
- 111.Shultz JM, Russell J, Espinel Z. 2005. Epidemiology of tropical cyclones: the dynamics of disaster, disease, and development. Epidemiol Rev 27:21–35, PMID: , 10.1093/epirev/mxi011. [DOI] [PubMed] [Google Scholar]
- 112.Lonigan CJ, Shannon MP, Taylor CM, Finch AJ Jr, Sallee FR. 1994. Children exposed to disaster: II. Risk factors for the development of post-traumatic symptomatology. J Am Acad Child Adolesc Psychiatry 33(1):94–105, PMID: , 10.1097/00004583-199401000-00013. [DOI] [PubMed] [Google Scholar]
- 113.Maclean JC, Popovici I, French MT. 2016. Are natural disasters in early childhood associated with mental health and substance use disorders as an adult? Soc Sci Med 151:78–91, PMID: , 10.1016/j.socscimed.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 114.Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Belesova K, Boykoff M, et al. 2019. The 2019 report of the Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet 394(10211):1836–1878, PMID: , 10.1016/S0140-6736(19)32596-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mills MA, Edmondson D, Park CL. 2007. Trauma and stress response among Hurricane Katrina evacuees. Am J Public Health 97(suppl 1):S116–S123, PMID: , 10.2105/AJPH.2006.086678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kim H, Han SB, Kim JH, Kim JS, Hong E. 2010. Post-Nargis medical care: experience of a Korean disaster relief team in Myanmar after the cyclone. Eur J Emerg Med 17(1):37–41, PMID: , 10.1097/MEJ.0b013e32832d3bc6. [DOI] [PubMed] [Google Scholar]
- 117.McDermott B, Cobham V, Berry H, Kim B. 2014. Correlates of persisting posttraumatic symptoms in children and adolescents 18 months after a cyclone disaster. Aust N Z J Psychiatry 48(1):80–86, PMID: , 10.1177/0004867413500349. [DOI] [PubMed] [Google Scholar]
- 118.Kabir R, Khan HTA, Ball E, Caldwell K. 2016. Climate change impact: the experience of the coastal areas of Bangladesh affected by Cyclones Sidr and Aila. J Environ Public Health 2016:9654753, PMID: , 10.1155/2016/9654753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Doocy S, Dick A, Daniels A, Kirsch TD. 2013. The human impact of tropical cyclones: a historical review of events 1980–2009 and systematic literature review. PLoS Curr 5:ecurrents.dis.2664354a5571512063ed29d25ffbce74, PMID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zalta AK, Tirone V, Orlowska D, Blais RK, Lofgreen A, Klassen B, et al. 2021. Examining moderators of the relationship between social support and self-reported PTSD symptoms: a meta-analysis. Psychol Bull 147(1):33–54, PMID: , 10.1037/bul0000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Thomalla F, Schmuck H. 2004. “We all knew that a cyclone was coming”: disaster preparedness and the cyclone of 1999 in Orissa, India. Disasters 28(4):373–387, PMID: , 10.1111/j.0361-3666.2004.00264.x. [DOI] [PubMed] [Google Scholar]
- 122.Uddin J, Mazur RE. 2015. Socioeconomic factors differentiating healthcare utilization of cyclone survivors in rural Bangladesh: a case study of Cyclone Sidr. Health Policy Plan 30(6):782–790, PMID: , 10.1093/heapol/czu057. [DOI] [PubMed] [Google Scholar]
- 123.Murakami H, Delworth TL, Cooke WF, Zhao M, Xiang B, Hsu PC. 2020. Detected climatic change in global distribution of tropical cyclones. Proc Natl Acad Sci USA 117(20):10706–10714, PMID: , 10.1073/pnas.1922500117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.McKinney N, Houser C, Meyer-Arendt K. 2011. Direct and indirect mortality in Florida during the 2004 hurricane season. Int J Biometeorol 55(4):533–546, PMID: , 10.1007/s00484-010-0370-9. [DOI] [PubMed] [Google Scholar]
- 125.Yang BY, Fan S, Thiering E, Seissler J, Nowak D, Dong GH, et al. 2020. Ambient air pollution and diabetes: a systematic review and meta-analysis. Environ Res 180:108817, PMID: , 10.1016/j.envres.2019.108817. [DOI] [PubMed] [Google Scholar]
- 126.Fan SJ, Heinrich J, Bloom MS, Zhao TY, Shi TX, Feng WR, et al. 2020. Ambient air pollution and depression: a systematic review with meta-analysis up to 2019. Sci Total Environ 701:134721, PMID: , 10.1016/j.scitotenv.2019.134721. [DOI] [PubMed] [Google Scholar]
- 127.Abramson DM, Park YS, Stehling-Ariza T, Redlener I. 2010. Children as bellwethers of recovery: dysfunctional systems and the effects of parents, households, and neighborhoods on serious emotional disturbance in children after Hurricane Katrina. Disaster Med Public Health Prep 4(suppl 1):S17–S27, PMID: , 10.1001/dmp.2010.7. [DOI] [PubMed] [Google Scholar]
- 128.Lowe SR, Tracy M, Cerdá M, Norris FH, Galea S. 2013. Immediate and longer-term stressors and the mental health of Hurricane Ike survivors. J Trauma Stress 26(6):753–761, PMID: , 10.1002/jts.21872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Fussell E, Lowe SR. 2014. The impact of housing displacement on the mental health of low-income parents after Hurricane Katrina. Soc Sci Med 113:137–144, PMID: , 10.1016/j.socscimed.2014.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lowe SR, Raker EJ, Arcaya MC, Zacher ML, Waters MC, Rhodes JE. 2020. A life-course model of trauma exposure and mental health among low-income survivors of Hurricane Katrina. J Trauma Stress 33(6):950–961, PMID: , 10.1002/jts.22581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Arcaya MC, Subramanian SV, Rhodes JE, Waters MC. 2014. Role of health in predicting moves to poor neighborhoods among Hurricane Katrina survivors. Proc Natl Acad Sci USA 111(46):16246–16253, PMID: , 10.1073/pnas.1416950111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lai BS, La Greca AM, Colgan CA, Herge W, Chan S, Medzhitova J, et al. 2020. Sleep problems and posttraumatic stress: children exposed to a natural disaster. J Pediatr Psychol 45(9):1016–1026, PMID: , 10.1093/jpepsy/jsaa061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Osofsky JD, Osofsky HJ, Weems CF, King LS, Hansel TC. 2015. Trajectories of post-traumatic stress disorder symptoms among youth exposed to both natural and technological disasters. J Child Psychol Psychiatry 56(12):1347–1355, PMID: , 10.1111/jcpp.12420. [DOI] [PubMed] [Google Scholar]
- 134.Lai BS, La Greca AM, Brincks A, Colgan CA, D’Amico MP, Lowe S, et al. 2021. Trajectories of posttraumatic stress in youths after natural disasters. JAMA Netw Open 4(2):e2036682, PMID: , 10.1001/jamanetworkopen.2020.36682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Raker EJ, Lowe SR, Arcaya MC, Johnson ST, Rhodes J, Waters MC. 2019. Twelve years later: the long-term mental health consequences of Hurricane Katrina. Soc Sci Med 242:112610, PMID: , 10.1016/j.socscimed.2019.112610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Rothman KJ, Greenland S, Lash TL. 2008. Modern Epidemiology, vol 3. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


