Summary
Background
Suicide prevention requires a shift from relying on an at-risk individual to engage with the healthcare system. Understanding patterns of healthcare engagement by people who have died by suicide may provide alternative directions for suicide prevention.
Methods
This is a population-based case-series study of all suicide decedents (n = 3895) in New South Wales (NSW), Australia (2013–2019), with linked coronial, health services and medicine dispensing data. Healthcare trajectories were identified using a k-means longitudinal 3d analysis, based on the number and type of healthcare contacts in the year before death. Characteristics of each trajectory were described.
Findings
Five trajectories of healthcare utilisation were identified: (A) none or low (n = 2598, 66.7%), (B) moderate, predominantly for physical health (n = 601, 15.4%), (C) moderate, with high mental health medicine use (n = 397, 10.2%), (D) high, predominantly for physical health (n = 206, 5.3%) and E) high, predominantly for mental health (n = 93, 2.4%). Given that most decedents belonged to Trajectory A this suggests a great need for suicide preventive interventions delivered in the community, workplace, schools or online. Trajectories B and D might benefit from opioid dispensing limits and access to psychological pain management. Trajectory C had high mental health medicine use, indicating that the time that medicines are prescribed or dispensed are important touchpoints. Trajectory E had high mental health service predominantly delivered by psychiatrists and community mental health, but limited psychologist use.
Interpretation
Although most suicide decedents made at least one healthcare contact in the year before death, contact frequency was overall very low. Given the characteristics of this group, useful access points for such intervention could be delivered through schools and workplaces, with a focus on alcohol and drug intervention alongide suicide awareness.
Funding
Australia’s National Health and Medical Research Council.
Keywords: Retrospective, Suicides, Medicines, Administrative data, Data linkage, Mental health, Health service utilisation, Epidemiology, k-means longitudinal
Research in context.
Evidence before this study
To identify or reinforce multisectoral suicide prevention strategies, a nuanced understanding of the heterogeneity in level and type of engagement with the healthcare system before death by suicide is necessary. Before this study, we conducted an Ovid Medline search of three concepts of: suicide (“suicid∗”), health service use (“health servic∗.mp. or ∗Health Services/or mental health services.mp. or Mental Health Services/or health-care.mp or healthcare.mp. or “Delivery of Health Care”/) and the particular methodology used in the present study (latent class.mp. or cluster analys∗.mp. or Cluster Analysis/) for articles published from database inception to May 4th 2023. After title and abstract review, there were four studies relevant to our planned analysis who grouped people who died from suicide into clusters and looked at differences in healthcare utilisation, including one that grouped clusters based on healthcare trajectories. The latter found that the most common healthcare behaviour was limited contact in the last year of life. Authors concluded that very little is known about the patterns of healthcare utilisation that people who die from suicide access in the year before death.
Added value of this study
The current study adds to knowledge about healthcare utilisation gained previously, by examining healthcare use trajectories in a population-based case series of suicide decedents considering type and frequency of healthcare contacts per month in the year before death. Five health service use trajectories were determined (A) none or low (n = 2598, 66.7%), (B) moderate predominantly for physical health (n = 601, 15.4%), (C) moderate with high mental health medicine use (n = 397, 10.2%), (D) high predominantly for physical health (n = 206, 5.3% of decedents) and (E) high predominantly for mental health (n = 93, 2.4%). Key similarities between the groups were observed in terms of prior hospitalised self-harm and contact with general practitioners and pharmacists. Other potential avenues of suicide prevention highlighted through this study include pharmacist-delivered suicide prevention, monitoring of medicines especially opioids, following up patients with poor mental health who have missed appointments either via a follow-up phone call or in-person welfare checks, aftercare for people hospitalised for suicidal behaviour and providing psychological alternatives to pain management for people with chronic/worsening pain.
Implications of all the available evidence
This study highlights that, although most suicide decedents made at least one healthcare contact in the year before death, contact frequency was overall very low. Given the characteristics of this group, which were further elucidated in the current study, useful access points for such intervention could be delivered through schools and workplaces, with a focus not only on suicide awareness but on alcohol and drug intervention.
Introduction
Suicide prevention is a worldwide public health priority. In high-income countries some of the most effective suicide prevention initiatives are delivered through the healthcare system.1 Numerous studies have estimated the proportion of suicide decedents who contacted health services before death; although estimates are highly variable depending on the methodology adopted, the country and healthcare system studied and the decedent characteristics.2,3 A common finding across studies is that most decedents made at least one general healthcare visit in the year prior to death but only a minority made a mental healthcare contact. Hence, there is a general academic consensus, which is also reflected in the WHO LIVE LIFE suicide prevention implementation guide,4 that suicide prevention requires a shift away from being exclusively delivered within the healthcare system with a multisectorial approach necessary.
Previous studies have reported the frequency in which people who have died from suicide accessed mental and general health services before death, stratified according to demographic characteristics.3,5,6 A systematic review which aimed to identify the characteristics of people who died by suicide and did not have contact with a mental health professional in the year before death identified male sex, younger or older age, and rural location were consistently associated with lack of access.5 To further identify targeted suicide prevention strategies a more nuanced understanding of the heterogeneity in level and type of engagement with the healthcare system before death by suicide is necessary; using decedent characteristics, the type and frequency of healthcare contacts and the changes in pattern of engagement prior to death.
Trajectory-based modelling can identify different patterns of health service use7; which may shed light on potential suicide prevention initiatives, delivered through the health system or in alternative settings. Using whole population linked healthcare utilisation, medicine dispensing and coronial data our study aimed to determine health service use trajectories in the 12 months preceding death from suicide and to describe the key demographic, coronial and healthcare characteristics associated with each trajectory.
Methods
Ethics
This study was approved by the following ethics committees: Department of Justice and Community Safety Justice Human Research Ethics Committee (CF/17/23,250), Western Australian Coronial Ethics Committee (EC 14/18); Australian Institute of Health and Welfare (AIHW; EO2017/4/366), and the New South Wales (NSW) Population & Health Services Research Ethics Committee (2017/HRE1204).
Setting
This study was conducted using population-level data from the most populous state in Australia, NSW. NSW is a geographically diverse state which was home to approximately 6.7 million inhabitants aged 10 years or older in 20168 (population in 2016 reported as it this is the mid-point of the data collection of this case series). Of all jurisdictions in Australia, NSW records the highest number of suicides but the second-lowest age-standardised suicide rate of the eight jurisdictions.9 NSW can be divided into five classes of Remoteness Areas based on relative access to services; major city, inner regional, regional, remote and very remote.9 As reported in the 2016 census, in NSW around 65% of inhabitants resided in the major cities, 65% of inhabitants were Australian-born, 24% of households were lone person households and 55% of people were employed, 34% were not in the labour force and 3.7% were unemployed.10
Study design
We used a case series design with data linkage to state and national administrative claims databases. A protocol paper available online11 describes this study, the Australian Suicide Prevention using Health-Linked data (ASHLi) population-based case series study. In brief, closed coronial cases for deaths in people aged 10 or older which were deemed to be “intentional self-harm” after 1 July 2013 until the date that case identifiers were sent to the relevant data linkage facilities (10th October 2019), were identified by the National Coronial Information System (NCIS). Identifiers were provided by the NCIS to AIHW, who probabilistically linked12 each to their federally funded administrative records, including health service data from the Medicare Benefits Scheme (MBS) and medicine dispensing data from the Pharmaceutical Benefits Scheme (PBS). Case identifiers for NSW residents were also provided to the Centre for Health Record Linkage (CHeReL), enabling probabilistic linkage of each decedent to state-funded administrative records, including the Emergency Department Data Collection (EDDC), the Admitted Patient Data Collection (APDC) and Ambulatory Mental Health dataset (MH-AMB). For each decedent the data records for the 12 months prior to death were obtained and were accessed by the investigators in a de-identified format. The reporting of this study conforms to the RECORD (REporting of studies Conducted using Observation Routinely-collected Data) statement13 (see Supplementary Material 1), an extension to the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) guidelines.
Datasets
National Coronial Information System (NCIS)
Any death in Australia and New Zealand that is suspected to be a suicide is investigated by a coroner and information pertaining to any coronial inquiry is routinely captured in the NCIS. The NCIS carries detailed information on each decedent, including demographics, details surrounding death (including method of death) and relevant autopsy information, including all drugs detected at autopsy and their concentrations (if quantifiable).
Medicare Benefits Scheme (MBS) and Pharmaceutical Benefits Scheme (PBS)
In Australia, a wide range of health services and medicines are subsidised through the MBS and PBS, respectively. Under the schemes all Australian citizens and residents receive subsidised healthcare for out-of-hospital medical services and 75% of prescribed medicine use.14
State-based health datasets
Hospital administrative data is collected by the various states in the form of separation records for public, private and multi-purpose day hospitals (APDC) and Emergency Department (EDDC) records for all separations from public hospitals; and community-based mental health contacts (MH-AMB), for counselling, skills training, or day program activities.
Data definitions
Decedent characteristics
We described decedents according to age at death, sex, level of residential remoteness (major city, inner regional, regional, remote/very remote) and whether Australian-born (Y/N).
Coronial characteristics
Using the cause of death fields recorded for each decedent the method of death was categorised as hanging, poisoning, falls, firearm, drowning, sharp object, moving object or other. Poisoning with medicines was defined where one or more medicine(s) were determined by the coroner to contribute to the death, even if not the primary cause. Post-mortem alcohol detection was classified by a blood alcohol concentration of 0.03 g/100 mL (lower levels may be formed during post-mortem decomposition).15 Post-mortem detection of “illicit” substances included detection of non-prescription amphetamines, cannabis, cocaine, novel psychoactive substances, or their metabolites; and post-mortem opioid detection included detection of any opioid or metabolite.
Healthcare contact categorisation
Every healthcare contact for each decedent across the four healthcare datasets (MBS, APDC, EDDC and MH-AMB) was exclusively assigned as: a mental health contact, a physical health contact or an investigation (e.g., diagnostic procedures, diagnostic imaging, and pathology). Definitions for the assignment differed depending on the data source (see below).
MBS
We characterised MBS healthcare contacts by MBS item numbers, sourced from the Medicare Schedule Book.16 Using the description of the MBS item, each line of MBS data was classified as a mental health contact (consultation with a psychiatrist or psychologist, or a consultation for mental health provided by a GP or other allied health professional), a physical health contact (consultation for general health by a GP or any other consultation by a non-GP specialist, non-psychiatrist) or an investigation. The item numbers and codes comprising each category can be found in Supplementary Material 2. To ascertain unique healthcare contacts, we considered only one billing code per provider per day per individual.
EDDC/APDC
Characterisation of EDDC and APDC contacts was conducted using the primary diagnosis code for the presentation/admission, respectively. The primary diagnosis for the EDDC, dependent on the practice of the hospital, was coded using either International Classification of Diseases (ICD)-10 or Systematized Nomenclature of Medicine (SNOMED). The primary diagnosis for the APDC is coded using ICD-9 or 10. Using the primary diagnosis code, each presentation/admission was classified as a mental health contact or a physical health contact. If one hospital presentation/admission resulted in several transfers, it was considered one contact and classified according to the original presentation/admission. Hospital contacts were additionally flagged as definite or potential suicidal behaviour. The hospitalised suicidal behaviour flag was not used as a variable in the trajectory analysis, but its incidence was reported. Definite suicidal behaviour was flagged if the primary diagnosis was directly attributed to intentional self-harm, suicide attempt or suicidal thoughts; potential suicidal behaviour was flagged if the primary diagnosis was any injury, poisoning or acute intoxication of a substance without indication of intent. Supplementary Material 3 details all the primary diagnoses recorded and how they were categorised for the purposes of data analysis.
MH-AMB
Any community mental health contact that involved counselling, education, psychotherapies, skills training, or day programs was considered a mental health contact. Only one MH-AMB contact per day per individual was counted.
Medicines characterisation
Our study includes all medicines listed on the PBS which were dispensed in the community, private hospitals, and on discharge from public hospitals in most states.14 The PBS does not subsidise medicines sold over-the-counter, complementary and alternative medicines or medicines dispensed within public hospitals to inpatients. Private prescriptions (when individuals pay the entire cost of the medicine) also do not appear in PBS data. Each medicine dispensed was classified as a mental health medicine or a physical health medicine. The Anatomical Therapeutic Classification (ATC) codes used to define mental health medicines were those that are predominantly used to treat mental health conditions: N05A (antipsychotics), N05B (anxiolytics), N05C (hypnotics and sedatives), N06A (antidepressants), N06B (psychostimulants), N06C (psycholeptics and psychoanaleptics) and N07B (drugs used in addictive disorders). All other medicines were broadly classified as physical health medicines. Medicines that can be used for mental health conditions but not primarily indicated as such were included in a sensitivity analysis and listed in Supplementary Material 4.
Data analysis
For each contact point type (mental health contact, physical health contact, investigation, mental health medicine dispensed, physical health medicine dispensed) the number of contacts per 30-day period for the twelve months prior to death for each decedent was calculated. The k-means longitudinal 3d (KML3d) method works similarly to the traditional k-means algorithm, by interactively grouping individuals with similar trajectories.17 As a non-parametric approach, it does not make assumptions on data distribution or trajectory “shapes” and avoids problems with model selection.17 An additional advantage of KML3d is that it builds clusters based on a combination of different variables (in the current study, types of contact with health services) at the same time.17 The Calinski-Harabasz criterion18 was used to assess the quality of the clusters. This is essentially the ratio between the between and within-cluster variability.18 The choice for the final number of clusters was a combination of the Calinski-Harabasz criterion and the face validity of the health service use trajectories created. Three trajectory solutions presented acceptable Calinski-Harabasz values: a 3-cluster (Calinski-Harabasz criterion = 602.9), 4-cluster (Calinski-Harabasz criterion = 491.9) and 5-cluster solution (Calinski-Harabasz criterion = 425.8); for all solutions the between-cluster variation was much higher than the within-cluster variance, which is indicative of good separation. The authors chose the 5-cluster solution as it enabled the greatest differentiation between the clusters. The 3-cluster and the 4-cluster solution are included in Supplementary Material 5. Analyses were performed in R19 version 4.2.1, using package “kml3d”.17 All outcomes and analysis reported in this study were prespecified, no post-hoc analysis was performed.
Role of the funding source
The funding body had no role in study design, collection, analysis or interpretation of the data, nor in the decision to submit the paper for publication.
Results
Decedent characteristics
There were 3895 decedents included. Year of death was: 314 in 2013, 708 in 2014, 741 in 2015, 662 in 2016, 803 in 2017, 546 in 2018 and 121 in 2019 (note incidence varies each year due to the proportion of decedents with closed coronial investigations at time of data linkage, protocol paper for more information11). Overall, 76.1% (n = 2965) were male and the median age was 45 years (IQR = 27). Most decedents resided in major cities (n = 2511, 64.5%), followed by inner regional (n = 975, 25.0%), outer regional (n = 260, 6.7%), remote areas (n = 41, 1.1%), and unknown for 108 (2.8%) individuals.
Health service use trajectories
The five trajectories were named according to their health service use: (A) None or low (n = 2598, 66.7%); (B) Moderate, predominantly physical health (n = 601, 15.4%); (C) Moderate, with high mental health medicine use (n = 397, 10.2%); (D) High, predominantly physical health (n = 206, 5.3%); and (E) High, predominantly mental health (n = 93, 2.4%).
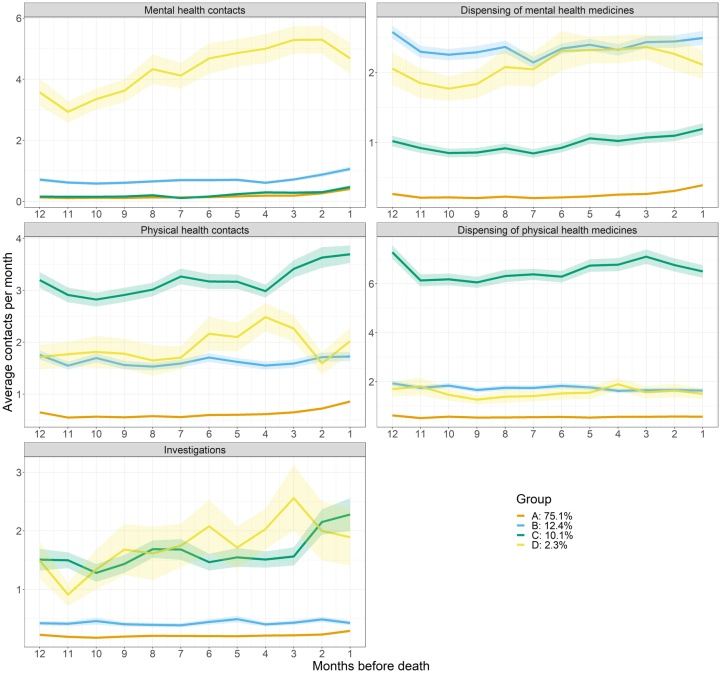
Table 1, Table 2 show demographic and coronial characteristics (respectively) for each trajectory and Fig. 1 shows the trajectories by average contact points per month for the final year of life, stratified by health contact classification. Supplementary Material 6 shows the total number of healthcare contacts for each healthcare contact category per trajectory. Fig. 2 shows box plots depicting the number of points of contact for out-of-hospital health services per trajectory (GP, psychiatrist, other medical practitioner, psychologist and community mental health). Table 3 shows the ten most common medicines dispensed in the 30 days before death for each group. The information from these results is summarised below.
Table 1.
Demographic characteristics of the case-series, and per healthcare trajectory.
| All n = 3895 | Healthcare trajectories |
|||||
|---|---|---|---|---|---|---|
| A no or low n = 2598 | B moderate, predominantly PH n = 601 | C moderate, high MH medicines n = 397 | D high, predominantly PH n = 206 | E high, predominantly MH n = 93 | ||
| Age and sex | ||||||
| Median age (IQR) | 45.0 (27) | 41.0 (25) | 64.0 (27) | 46.0 (20) | 72.0 (22) | 45.0 (22) |
| Up to 24 years of age, n (%) | 497 (13) | 464 (18) | npg | 14 (3.5) | npg | npg |
| 25–44 years of age, n (%) | 1371 (35) | 1060 (41) | 90 (15) | 167 (42) | 18 (8.7) | 36 (39) |
| 45–64 years of age, n (%) | 1324 (34) | 855 (33) | 207 (34) | 169 (43) | 56 (27) | 37 (40) |
| 65 years of age or older, n (%) | 703 (18) | 219 (8.4) | 292 (49) | 47 (12) | 131 (64) | 14 (15) |
| Male, n (%) | 2965 (76) | 2059 (79) | 460 (77) | 261 (66) | 139 (68) | 46 (50) |
| Female, n (%) | 930 (24) | 539 (21) | 141 (23) | 136 (34) | 67 (33) | 47 (50) |
| Australian-born, n (%)a | 2761 (71) | 1873 (72) | 385 (64) | 299 (75) | 133 (65) | 71 (76) |
| Geographical locationb | ||||||
| Major cities, n (%) | 2511 (65) | 1631 (63) | 397 (66) | 267 (67) | 137 (67) | 79 (85) |
| Inner regional, n (%) | 975 (25) | 660 (25) | 149 (25) | 100 (25) | 56 (27) | 10 (11) |
| Outer regional/remote, n (%) | 301 (7.7) | 227 (8.7) | 43 (7.2) | 17 (4.3) | npg | npg |
| Employment statusc | ||||||
| Employed, n (%) | 1439 (37) | 1161 (45) | 132 (22) | 107 (27) | 20 (9.7) | 19 (20) |
| Unemployed, n (%) | 895 (23) | 602 (23) | 98 (16) | 135 (34) | 28 (14) | 32 (34) |
| Retired/pensioner, n (%) | 829 (21) | 283 (11) | 303 (50) | 87 (22) | 135 (66) | 21 (23) |
| Otherd, n (%) | 236 (6.1) | 205 (7.9) | npg | 17 (4.3) | npg | npg |
| Marital statuse | ||||||
| Never married, n (%) | 1254 (32) | 946 (36) | 108 (18) | 146 (37) | 22 (11) | 32 (34) |
| Married/de facto, n (%) | 1385 (36) | 882 (34) | 269 (45) | 113 (29) | 83 (40) | 38 (41) |
| Separated/divorced, n (%) | 714 (18) | 477 (18) | 105 (18) | 82 (21) | 38 (18) | 12 (13) |
| Widowed, n (%) | 196 (5) | 57 (2.2) | 77 (13) | npg | 48 (23) | npg |
| Living circumstancesf | ||||||
| Lives alone, n (%) | 2164 (56) | 1480 (57) | 290 (48) | 240 (61) | 108 (52) | 46 (50) |
| Lives with partner/family, n (%) | 1385 (36) | 882 (34) | 269 (45) | 113 (29) | 83 (40) | 38 (41) |
IQR, interquartile range, MH: mental health; PH: physical health.
Highest proportion across the 5 healthcare trajectory per characteristic are highlighted in bold and lowest values in italic. Percentages are expressed as percentage of decedents per trajectory displaying that characteristic, apart from the total column where the percentage is expressed as percentage of the total case series.
Unknown for n = 602.
Unknown for n = 108.
Unknown for n = 506.
Includes students, prisoners, home duties and other.
Unknown for n = 346.
Unknown for n = 346.
Not provided due to suppression rules/sparse data/cell being under 6.
Table 2.
Coronial characteristics of the case-series, and per healthcare trajectory.
| All N = 3895 | Healthcare trajectory |
|||||
|---|---|---|---|---|---|---|
| A no or low n = 2598 | B moderate, predominantly PH n = 601 | C moderate, high MH medicines n = 397 | D high, predominantly PH n = 206 | E high, predominantly MH n = 93 | ||
| Method of deatha | ||||||
| Hanging | 2027 (52.0) | 1557 (59.9) | 224 (37.3) | 158 (40.0) | 49 (23.8) | 39 (41.9) |
| Any poisoning | 948 (24.3) | 501 (19.3) | 192 (31.9) | 146 (37.0) | 82 (39.8) | 27 (29.0) |
| Poisoning with medicines | 347 (8.9) | 141 (5.4) | 84 (14.0) | 68 (17.1) | 39 (18.9) | 15 (16.1) |
| Falls | 328 (8.4) | 217 (8.4) | 41 (6.8) | 37 (9.3) | 20 (9.7) | 13 (14.0) |
| Firearm | 235 (6.0) | 134 (5.2) | 55 (9.2) | npd | 34 (16.5) | npd |
| Sharp object | 113 (2.9) | 64 (2.5) | 24 (4.0) | 14 (3.5) | npd | npd |
| Moving object | 175 (4.5) | 127 (4.9) | 18 (3.0) | 22 (5.5) | npd | suppressed |
| Other | 311 (8.0) | 178 (6.9) | 73 (12.1) | 33 (8.3) | 19 (9.2) | 8 (8.6) |
| Toxicology | ||||||
| BAC ≥0.03 g/100 mL detected post-mortemb n, (%) | 902 (24.5) | 780 (31.8) | 107 (19.0) | 92 (24.3) | 27 (13.8) | 16 (18.0) |
| Mean BAC detected g/100 mLc (SD) | 0.15 (0.10) | 0.15 (0.09) | 0.15 (0.13) | 0.13 (0.09) | 0.14 (0.07) | 0.16 (0.13) |
| Opioids detected post-mortemb, n (%) | 702 (19.1) | 274 (11.2) | 180 (32.0) | 125 (33.1) | 103 (52.8) | 20 (22.5) |
| Illicit substances detected post-mortema n, (%) | 722 (19.6) | 584 (23.8) | 45 (8.0) | 72 (19.0) | 13 (6.7) | 8 (8.6) |
BAC, blood alcohol concentration; SD: standard deviation.
Highest proportion across the 5 healthcare trajectory per characteristic are highlighted in bold and lowest values in italic. Percentages are expressed as decedents per cluster displaying that characteristic, apart from the total column where the percentage is expressed as decedents out of total case series. Some data is suppressed due to low counts.
Method of death is not mutually exclusive, some individuals used a combination of the included methods.
Denominator is the number of decedents per trajectory whose forensic toxicology information was available in their coronial record; 94.5% of decedents from Group A, 93/5% Group B, 95.2% Group C, 94.7% Group D and 95.7% Group E.
Only those with a BAC of ≥0.03 g/100 mL were included in the calculation.
Not provided due to suppression rules/sparse data/cell being under 6.
Fig. 1.
Healthcare trajectories for a population-based case-series of suicide decedents in New South Wales, Australia, between 2013 and 2019. Trajectories are shown in terms of average services attended or medicines dispensed per month for each trajectory in the twelve months prior to death, with standard error shaded. Each colour represents a different trajectory as follows: Orange–Trajectory A: None or low (n = 2598, 66.7%); Light blue–Trajectory B: Moderate, predominantly physical health (n = 601, 15.4%); Green–Trajectory C: Moderate, with high mental health medicine use (n = 397, 10.2%); Yellow–Trajectory D: High, predominantly for physical health (n = 206, 5.3%); Dark blue–Trajectory E: High, predominantly for mental health (n = 93, 2.4%).
Fig. 2.
Boxplots showing the frequencies of out-of-hospital healthcare contacts in the year before death for each trajectory. Y-axis is the number of contacts with a particular health professional in the year prior to death and the x-axis is the healthcare trajectory. Each colour represents a different trajectory as follows: Orange–Trajectory A: None or low (n = 2598, 66.7%); Light blue–Trajectory B: Moderate, predominantly physical health (n = 601, 15.4%); Green–Trajectory C: Moderate, with high mental health medicine use (n = 397, 10.2%); Yellow–Trajectory D: High, predominantly physical health (n = 206, 5.3%); Dark blue–Trajectory E: High, predominantly mental health (n = 93, 2.4%). GP: general practitioner; MH: mental health.
Table 3.
The ten most common medicines dispensed in the 30 days before death for each healthcare trajectory, and the proportion of each group dispensed each medicine.
ACE: Angiotensin-converting enzyme; ARBs: Angiotensin II receptor blockers; GORD: Gastro-oesophageal reflux disease.
1Excluding insulins.
Trajectory summaries
A: none or low health service use (n = 2598, 66.7%)
Trajectory A were predominately young, male, and often employed (Table 1). A substantial proportion died by hanging and had alcohol or illicit drug exposure proximal to death (Table 2). Most cases (n = 1678, 64.6%) had no medicines dispensed in the 30 days before death, whilst antidepressants were dispensed to a minority (n = 421, 16.2%) (Table 3). Non-mental health consultations with GPs and consultations with psychiatrists were the most common out-of-hospital health contact (Fig. 2) and 26.9% (n = 700) had attended hospital for suicidal behaviour. Slight increases in mental health contacts, physical health contacts and mental health medicine dispensed in the 3 months prior to death were observed (Fig. 1). 199 decedents (7.7%) of the group had no service use at all in the year prior to death.
B: moderate health service use, predominantly physical health (n = 601, 15.4%)
Trajectory B was predominately male, aged over 65 years and often married/de facto (Table 1). One third had an antidepressant dispensed within 30 days of death (n = 204, 33.9%), and a fifth were dispensed medicines for peptic ulcer and gastro-oesophageal disease (GORD; n = 119, 19.8%) (Table 3). A non-mental health related consultation with a GP was the most common health contact (Fig. 2) and 208 (34.6%) had attended hospital for suicidal behaviour. Prominent increases in physical health contacts and investigations were observed in the 3 months prior to death, with slight increases in mental health contacts and mental health medicines dispensed (Fig. 1).
C: moderate health service use, with high mental health medicine use (n = 397, 10.2%)
Trajectory C was predominately male and aged 25–64 years with less than a third married/defacto (Table 1). Substantial proportions were dispensed psychotropic medicines in the 30 days before death, predominantly antidepressants (n = 245, 61.7%), antipsychotics (n = 156, 39.3%) and/or anxiolytics (n = 125, 31.5%) (Table 3). A non-mental health related consultation with a GP was the most common health contact (Fig. 2) and 164 (41.3%) had hospital treatment for suicidal behaviour. There were no discernible increases in health contacts in the 3 months before death (Fig. 1).
D: high health service use, predominantly for physical health (n = 206, 5.3%)
Trajectory D was predominately male, aged over 65 years and retired/pensioners (Table 1). Self-poisoning was the most frequent method of suicide (Table 2). Substantial proportions had opioids detected post-mortem; and very low proportions had alcohol or illicit substances detected post-mortem (Table 2). Opioids (n = 110, 53.4%), antidepressants (n = 99, 48.1%) and medicines for peptic ulcer and GORD (n = 96, 46.6%) were commonly dispensed in the 30 days before death (Table 3). Non-mental health GP consultations and consultations with other medical practitioners in the year prior to death were the most common out-of-hospital health contact (Fig. 2) and over half (64.9%, n = 113) had hospital treatment for suicidal behaviour. There was a negligible or minor rise in mental health and physical health contacts in the 3–5 months before death (Fig. 1).
E: high health service use, predominantly for mental health (n = 93, 2.4%)
Trajectory E was small, predominantly female and unemployed or retired/pensioners (Table 1). Antidepressants (n = 52, 55.9%), antipsychotics (n = 29, 31.2%) and anxiolytics (n = 21, 22.6%) were the most commonly dispensed medicines in the 30 days before death (Table 3). Mental health consultations with GP, psychiatrist and community mental health services were common (Fig. 2). Two thirds (66.7%, n = 62) had hospital treatment for suicidal behaviour. Utilisation of mental health, physical health and mental health medicines increased and reached a peak at around 3–4 months prior to death at which point use decreased again (Fig. 1).
Supplementary analysis
A broader inclusion of mental health medicines resulted in negligible differences to the identified groups and their trajectories.
Discussion
This study has identified five trajectories of health service use for suicide decedents in NSW in the 12-months prior to death. The key features of these trajectories may be useful to inform potential suicide prevention interventions.
Two thirds of decedents had none or low health service use, which demonstrates the necessity for a shift of potential suicide prevention interventions, away from relying heavily on an individual at risk engaging with the healthcare system.4 Some key characteristics of this trajectory are consistent with other studies of none or low service use in suicide decedents5 and that of the general Australian population,20, 21, 22 namely, that males, young people and people living remotely are less likely to make frequent contact with the healthcare system. Almost half of trajectory A were employed, with high rates of post-mortem detection of alcohol and illicit substances, who predominantly died by hanging. Given these characteristics, potential intervention settings could be in the community, online, schools, and workplaces, with a focus on suicide awareness and alcohol and drug education.
Nearly a quarter of suicide decedents were included in Trajectories B and C; steady contact with GPs, psychologists and pharmacists may provide potential opportunities for recognition and response to the modifiable proximal risk factors for suicide prevention. Trajectory B had a clear increase in use of physical health services and investigations in the 3 months before death, which may indicate worsening of chronic health or new acute conditions. A recent census-based study in Northern Ireland found that the risk of suicide increased proportionally to the number of physical health conditions and the severity of limitation to daily activity imposed by physical health conditions.23 Monitoring the mental health of individuals with worsening physical health conditions might be important. In contrast, Trajectory C showed negligible change in frequency of health contacts preceding death. Trajectory C did have moderate contact with health services, and many of these contacts may have been to renew medicine prescriptions, which might be an opportunity for suicide prevention via routine mental health check-in by prescribers or by dispensing limitations (e.g., number of tablets supplied) for potentially toxic medicines.
A minority of decedents were classified into the two high health service use groups (Trajectories D and E, 7.7%). The high and increasing frequency of service use suggests chronic severe physical and/or mental health conditions that deteriorated in the year before death. Over half of Trajectory D were dispensed an opioid in the 30 days before death, highlighting that acute onset or relapsing pain was a significant health problem. Unsurprisingly, Trajectory D also had high proportions of post-mortem detection of opioids and medicinal poisoning involved in death. Means restriction of highly toxic drugs, such as opioids, has been shown to reduce population-level rates of suicide by poisoning,24 however excessively restricting the availability of opioids for chronic pain can increase distress and suicidality.25 Instead, limited dispensing amounts, monitoring medicine use and deteriorating health might contribute to suicide prevention. Psychological alternatives to pain management (acute, relapsing, or chronic) can be effective,26 but psychologist service use in this group was low. This highlights a potential avenue for suicide prevention in the form of promotion of psychologist-delivered pain management alternatives to medicine in those with chronic pain.
Increasing use of mental health services between 12 and 3 months, then a decrease for the final 3 months before death was observed for Trajectory E. These individuals are likely recognised to be severely mentally ill, psychologically distressed, and possibly suicidal; hence a key component of decreasing their risk of suicide may be recognising a decrease in service frequency, which may be due to treatment fatigue or withdrawal of perceived ineffective treatment. Predicting patterns in medicine and health service utilisation and recognising important shifts in engagement (i.e. not attending an appointment or collecting a medicine) is an area which could provide opportunities for suicide prevention through active outreach to patients.27
Importantly there were service use characteristics observed in all trajectories. Hospital-treated suicidal behaviour occurred in 32% of the decedents, with a proportion of all individuals in each trajectory in the year before death. This reiterates the utmost importance of self-harm aftercare and active outreach in terms of its role in suicide prevention27 for which effective interventions are available such as brief contact interventions28 and safety planning-type interventions.29 Consultation with GPs were amongst the most common healthcare contact point for members of each group, a well-established finding.3 While a recent meta-analysis was unable to show significant effectiveness of suicide prevention interventions delivered by GPs,30 these finding still highlight the potential importance of providing support for GPs to effectively recognise and refer people who are suicidal. A large proportion of individuals from each group were dispensed at least one medicine in the 30 days before death, antidepressants most commonly. The role of pharmacists, as those who dispense medicines, is not well-recognised,31 despite most pharmacists reporting they have encountered a suicidal individual32 and being primely positioned to intervene.33 In all trajectories contact with psychologists was relatively low compared to other health professionals. Long waitlists and unaffordable out-of-pocket costs34 are the most likely drivers of this finding and overcoming these barriers on a national level has potential for suicide prevention. Lastly, the lack of abrupt change in service use in most types of healthcare immediately prior to suicide is notable and may suggest that crises that precipitate suicide for most people do not manifest in additional health service access.
There are limitations to this study that should be borne in mind when reflecting on the results. This study uses medio-legal and administrative data which is not designed for research purposes. As such, there is a necessity to impose definitions on the data to create variables and categories suitable for analysis. Comprehensive demographic and toxicological information for each decedent is not always available in the NCIS (although we have age and sex for all decedents) and defining suicidal behaviour using NSW hospital data is particularly challenging as the intent behind the injury or overdose is not always detailed.
Importantly, we have only examined healthcare use prior to suicide deaths that occurred in one Australian state so the generalisability of these results to the rest of the country is uncertain. However, NSW has representable demographics to the whole country,35 healthcare provision from state to state in Australia is subject to similiar issues and barriers in terms of access, and medicines and out-of-hopsital services are subsidised federally (as opposed to hospital and mental health services which are state-based). Though, given the marked differences between the Australian healthcare system and other countries, generalisability outside of Australia is likely to be low.
The healthcare behaviour of a population is highly variable with each individual lying somewhere within a continuum, the KML3d method was employed in the present study to identify distinct healthcare trajectories in order to better understand the population from a clinical perspective. Using a different approach may identify slightly different trajectories and hence it is important to treat these findings as preliminary and in need of replication. However, this is the largest suicide linkage of its kind using Australian data, and larger studies will not be possible without significant research investment in terms of both time and cost.
There is a lag-time between the death and the finalisation of the coronial enquiry and data linkage procedures, so 2019 only includes 20% of the suicides that occurred that year.11 Due to these circumstances in which coronial data are collected, linkage to other datasets, as per the current study, is necessary to increase the quality of the data. That data presented here predates the COVID-19 pandemic, which had a nuanced impact on suicide worldwide. Additionally, this study is not designed to provide evidence of risk factors for suicide as we do not have data on individuals that did not die from suicide.
Lastly, the purpose of the present study was to identify potential opportunities for boosting suicide prevention in people at risk of suicide, given particular patterns of health service utilisation. The opportunities for prevention mentioned here require appropropriate evaluation in the form of high-quality trials and should demonstrate cost-effectiveness if they are rolled out on at a population-level.
The five trajectories of health service use of suicide decedents identified in this study highlight potential areas for bosting suicide prevention including community-based suicide prevention interventions via workplaces, schools and universities, a focus on individuals in the health system who have worsening physical health conditions, particularly those prescribed opioids, and a focus on individuals that have serious mental illness and have missed or reduced frequency of appointments with their mental health professionals. Implementation of evidence-based effective aftercare interventions is an essential universal suicide prevention approach, as prior hospital-treated suicidal behaviour was observed for a proportion of individuals in all trajectories.
Contributors
KMC: Conceptualisation, Methodology, Project administration, Funding acquisition, Data curation, Writing–original draft; SS: Methodology, Formal analysis; GLC: Conceptualisation, Methodology, Writing–Review & Editing; ZA: Formal analysis, Visualisation; JER: Methodology, Writing–Review & Editing; ALS: Methodology, Writing–Review & Editing; AP: Methodology, Writing–Review & Editing; NAB: Conceptualisation, Methodology, Writing–Review & Editing; Supervision. KMC, ZA and SS accessed and verified the underlying data.
Data sharing statement
Only approved personnel may access the data. Researchers interested in collaborations or further information are invited to contact NAB at nicholas.buckley@sydney.edu.au.
Declaration of interests
GLC reports honoraia, educational and travel support from Servier, AstraZeneca, Otsuka Australia, Teva Pharma Australia, Lundbeck and Janssen-Cilag in the past 5 years. GLC also reports participation in boards for Quitlink and AFFINITY and a Chairperson role of RANZCP Clinical Practice Guidelines for Deliberate Self-harm. All other authors declare no competing interests.
Acknowledgements
This study is funded by a grant from the Australian National Health and Medical Research Council (NHMRC, REF: 1157757) and the Translational Australian Clinical Toxicology Research Group (TACT). An NHMRC Early Career Fellowship funds KC (Grant number: 1122362). The funding organizations played no part in the design of the study; nor in the preparation, review, or approval of the manuscript. We would like to thank the National Coronial Information System (NCIS) and the Victorian Department of Justice and Community Safety as the source organisation of NCIS data, the Department of Health, the Centre for Health Record Linkage (CHeReL) and the NSW Ministry of Health.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2023.102165.
Appendix A. Supplementary data
Supplementary Material 4 - 4 clusters.
Supplementary Material 4 - 3 clusters.
References
- 1.Krysinska K., Batterham P.J., Tye M., et al. Best strategies for reducing the suicide rate in Australia. Aust N Z J Psychiatry. 2016;50:115–118. doi: 10.1177/0004867415620024. [DOI] [PubMed] [Google Scholar]
- 2.Walby F.A., Myhre M., Kildahl A.T. Contact with mental health services prior to suicide: a systematic review and meta-analysis. Psychiatr Serv. 2018;69:751–775. doi: 10.1176/appi.ps.201700475. [DOI] [PubMed] [Google Scholar]
- 3.Stene-Larsen K., Reneflot A. Contact with primary and mental health care prior to suicide: a systematic review of the literature from 2000 to 2017. Scand J Public Health. 2019;47:9–17. doi: 10.1177/1403494817746274. [DOI] [PubMed] [Google Scholar]
- 4.WHO . World Health Organization; Geneva: 2021. Live life: an implementation guide for suicide prevention in countries. [Google Scholar]
- 5.Tang S., Reily N.M., Arena A.F., et al. People who die by suicide without receiving mental health services: a systematic review. Front Public Health. 2021;9:736948. doi: 10.3389/fpubh.2021.736948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tang S., Reily N.M., Arena A.F., et al. Predictors of not receiving mental health services among people at risk of suicide: a systematic review. J Affect Disord. 2022;301:172–188. doi: 10.1016/j.jad.2022.01.054. [DOI] [PubMed] [Google Scholar]
- 7.Nguena Nguefack H.L., Pagé M.G., Katz J., et al. Trajectory modelling techniques useful to epidemiological research: a comparative narrative review of approaches. Clin Epidemiol. 2020;12:1205–1222. doi: 10.2147/clep.S265287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Australian Bureau of Statistics (ABS) Australian Bureau of Statistics (ABS); Canberra: 2016. 3101.0 - Australian demographic statistics. [Google Scholar]
- 9.Australian Bureau of Statistics (ABS) 2022. Causes of Death, Australia: statistics on the number of deaths, by sex, selected age groups, and cause of death classified to the International Classification of Diseases (ICD) Canberra. [Google Scholar]
- 10.Australian Bureau of Statistics (ABS) 2017. 2071.0 - census of population and housing: reflecting Australia - stories from the census, 2016. Canberra. [Google Scholar]
- 11.Chitty K.M., Schumann J.L., Schaffer A., et al. Australian suicide prevention using health-linked Data (ASHLi): protocol for a population-based case series study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-038181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tromp M., Ravelli A.C., Bonsel G.J., et al. Results from simulated data sets: probabilistic record linkage outperforms deterministic record linkage. J Clin Epidemiol. 2011;64:565–572. doi: 10.1016/j.jclinepi.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 13.Benchimol E.I., Smeeth L., Guttmann A., et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12 doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mellish L., Karanges E.A., Litchfield M.J., et al. The Australian pharmaceutical benefits scheme data collection: a practical guide for researchers. BMC Res Notes. 2015;8:634. doi: 10.1186/s13104-015-1616-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kugelberg F.C., Jones A.W. Interpreting results of ethanol analysis in postmortem specimens: a review of the literature. Forensic Sci Int. 2007;165:10–29. doi: 10.1016/j.forsciint.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 16.Australian Government Department of Health . Department of Health; Canberra: 2020. The Medicare benefits Schedule book: operating from 1 january 2020. [Google Scholar]
- 17.Genolini C., Alacoque X., Sentenac M., et al. Kml and kml3d: R packages to cluster longitudinal data. J Stat Software. 2015;65:1–34. doi: 10.18637/jss.v065.i04. [DOI] [Google Scholar]
- 18.Caliński T., Harabasz J. A dendrite method for cluster analysis. Commun Stat. 1974;3:1–27. doi: 10.1080/03610927408827101. [DOI] [Google Scholar]
- 19.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2022. R: A language and environment for statistical computing. [Google Scholar]
- 20.Australian Institute of Health and Welfare (AIHW) Australian Government, Australian Institute of Health and Welfare; Canberra: 2019. Rural & remote health. Cat. No: PHE 255. [Google Scholar]
- 21.Australian Institute of Health and Welfare (AIHW) AIHW; Canberra: 2019. The health of Australia's males. [Google Scholar]
- 22.Walker R., Reibel T. Telethon Institute for Child Health Research, University of Western Australia and Commissioner of Children and Young People; Perth, Western Australia: 2013. Young people's experiences with health services - a literature review. [Google Scholar]
- 23.Onyeka I.N., Maguire A., Ross E., et al. Does physical ill-health increase the risk of suicide? A census-based follow-up study of over 1 million people. Epidemiol Psychiatr Sci. 2020;29:e140. doi: 10.1017/s2045796020000529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lim J.S., Buckley N.A., Chitty K.M., et al. Association between means restriction of poison and method-specific suicide rates: a systematic review. JAMA Health Forum. 2021;2:e213042. doi: 10.1001/jamahealthforum.2021.3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agnoli A., Xing G., Tancredi D.J., et al. Association of dose tapering with overdose or mental health crisis among patients prescribed long-term opioids. JAMA. 2021;326:411–419. doi: 10.1001/jama.2021.11013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Driscoll M.A., Edwards R.R., Becker W.C., et al. Psychological interventions for the treatment of chronic pain in adults. Psychol Sci Public Interest. 2021;22:52–95. doi: 10.1177/15291006211008157. [DOI] [PubMed] [Google Scholar]
- 27.Mann J.J., Michel C.A., Auerbach R.P. Improving suicide prevention through evidence-based strategies: a systematic review. Am J Psychiatry. 2021;178:611–624. doi: 10.1176/appi.ajp.2020.20060864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tay J.L., Li Z. Brief contact interventions to reduce suicide among discharged patients with mental health disorders-A meta-analysis of RCTs. Suicide Life Threat Behav. 2022;52:1074–1095. doi: 10.1111/sltb.12903. [DOI] [PubMed] [Google Scholar]
- 29.Nuij C., van Ballegooijen W., de Beurs D., et al. Safety planning-type interventions for suicide prevention: meta-analysis. Br J Psychiatry. 2021;219:419–426. doi: 10.1192/bjp.2021.50. [DOI] [PubMed] [Google Scholar]
- 30.Milner A., Witt K., Pirkis J., et al. The effectiveness of suicide prevention delivered by GPs: a systematic review and meta-analysis. J Affect Disord. 2017;210:294–302. doi: 10.1016/j.jad.2016.12.035. [DOI] [PubMed] [Google Scholar]
- 31.Murphy A.L., Gardner D.M., Chen T.F., et al. Community pharmacists and the assessment and management of suicide risk. Can Pharm J (Ott) 2015;148:171–175. doi: 10.1177/1715163515587554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carpenter D.M., Lavigne J.E., Colmenares E.W., et al. Community pharmacy staff interactions with patients who have risk factors or warning signs of suicide. Res Social Adm Pharm. 2020;16:349–359. doi: 10.1016/j.sapharm.2019.05.024. [DOI] [PubMed] [Google Scholar]
- 33.Kassir H., Eaton H., Ferguson M., et al. Role of the pharmacist in suicide prevention: primely positioned to intervene. J Pharm Pract Res. 2019;49:567–569. doi: 10.1002/jppr.1552. [DOI] [Google Scholar]
- 34.Australian Psychological Society . Australian Psychological Society Limited; Melbourne: 2022. Prevent, Respond, Adapt: Improving the mental health and wellbeing of all Australians. Pre-budget submission 2022- 23. [Google Scholar]
- 35.New South Wales . Australian Bureau of Statistics; Canberra: 2021. 2021 census all persons QuicStats. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.