Abstract
U.S. men experience substantial sexual and reproductive health needs across the life span. A significant barrier for providers in serving men in family planning, primary care, and sexually transmitted disease clinics has been the lack of standards for men’s sexual and reproductive health care. The goal of this synthesis paper is to describe the development of clinical recommendations for the delivery of family planning services for men that were developed and published by CDC and the U.S. Office of Population Affairs. This paper is intended to describe the process used from 2011 to 2014 to develop the recommendations for the delivery of comprehensive reproductive healthcare services to men, and the rationale underpinning them.
Introduction
U.S. men experience substantial sexual and reproductive health needs across the life span.1 For example, nearly four of ten men report that the last live birth they fathered was unintended.2 Men also experience high rates of sexually transmitted diseases (STDs). Chlamydia rates for men aged 15–19 years increased 6.1% from 757.0 cases per 100,000 men in 2010 to 803.0 per 100,000 in 2011; men aged 20–24 years had the highest rate (1,343.3 cases per 100,000 men), and rates increased 12.4% during 2010–2011.3
A significant barrier for providers serving men in family planning, primary care, and STD clinics is the lack of standards for men’s sexual and reproductive health care. Providing quality men’s preventive sexual and reproductive health care is one important way to reduce adverse outcomes experienced by men and their partners. Although numerous professional organizations promote delivery of clinical preventive services inclusive of sexual health,4–6 minimal guidance exists to inform the full scope of men’s clinical preventive sexual and reproductive health care. In 2011, IOM defined essential preventive health services for women, which were subsequently incorporated into law via the Patient Protection and Affordable Care Act (ACA).7 Although IOM noted the need for a similar list of essential preventive services for men, currently this is lacking.7
From 2011 to 2014, the USDHHS Office of Population Affairs (OPA) and CDC collaborated to develop clinical recommendations for providing quality family planning services, including recommendations for men and women. Although focused on family planning service providers, this effort provided an opportunity to consider a comprehensive set of sexual and reproductive health services for men and women. The collaboration drew on the strengths of both agencies: CDC has extensive expertise in developing clinical recommendations, and OPA has decades of experience in direct delivery of family planning services through its oversight of the Title X program. Established in 1970, a key purpose of the Title X program is “to assist in making comprehensive voluntary family planning services readily available to all persons desiring such services.” Men represent a small but increasing percentage of all clients served; the percentage of male clients was 3% in 1999 and 8% in 2011.8
Entitled “Providing Quality Family Planning Services: Recommendations of CDC and the U.S. Office of Population Affairs” (QFP),9 these recommendations are intended to serve as the standard of preventive care for all family planning service providers. IOM’s definition of quality of care was used as an organizing framework for the recommendations, which posits that improving the quality of services will lead to improved health outcomes.10 This definition describes six dimensions needed to achieve high-quality health care: that care must be safe, effective and reliable, patient-centered, timely, efficient, and equitable. In accordance with IOM recommendations,11,12 every effort was made to draw on existing evidence and use a transparent development process.
Thus, the goal of this synthesis paper is to describe the process of developing the clinical recommendations for men included in QFP. IOM recommends that the rationale underpinning clinical recommendations be made fully transparent.12 The rationales for other aspects of the recommendations (e.g., clinical recommendations for women, contraceptive counseling and education) are described elsewhere.13
Methods
From mid-2010 to mid-2011, several activities were conducted in an effort to develop the recommendations. Staff from the Male Training Center (MTC), a program of the Family Planning Council and a collaboration with the Johns Hopkins School of Medicine, Center for Sexually Transmitted Disease and Reproductive Health Research, Prevention, and Training that was established in 2009 through a cooperative agreement with OPA, served as the primary technical consultant throughout the process of developing the recommendations for men. A parallel approach was used in the development of methods and recommendations for clinical services for men as was used for clinical services for women.14
Framework for Men’s Sexual and Reproductive Health Care
The 1994 Cairo UN International Conference on Population and Development (ICPD) and WHO definitions of sexual and reproductive health were used to outline the full range of relevant services to be considered during the review process.15,16 The ICPD and WHO define sexual and reproductive health as being “a state of physical, mental, and social well-being and not merely the absence of disease, dysfunction, or infirmity, in all matters relating to the reproductive system, its functions, and its processes.” The definition also notes that sexual health requires a positive, respectful approach to sexuality and sexual relationships that are free of coercion, discrimination, or violence. Further, the definition states that all people, including men, should have the right to be informed of and have access to safe, effective, affordable, and acceptable family planning methods of their choice, and receive appropriate health care. From this framework, MTC staff identified specific sexual and reproductive healthcare goals related to delivering clinical preventive services to men, including promoting sexual health and development; healthy relationships; preventing unintended pregnancy, STDs/HIV, and reproductive health–related cancers; addressing issues related to infertility and sexual function; planning for the timing and spacing of children; and achieving healthy pregnancy.1
Compiling Existing Recommendations Associated with Clinical Services for Men
MTC and CDC staff developed an initial comprehensive list of federal agencies and professional medical organizations and searched for clinical recommendation statements from each of these organizations on their websites as well as the National Guideline Clearinghouse website (www.guideline.gov). Existing clinical recommendations were compiled in a two-step process. First, organizations were identified to include in the synthesis by applying the following criteria: (1) the entity is a federal agency or major professional medical organization representing established medical disciplines; (2) the entity’s recommendations are based on independent review of evidence or expert review and considered primary sources; and (3) the entity’s recommendations were developed in and for the U.S.
Existing recommendations for services related to sexual and reproductive health were then summarized (Appendix A). Specific screening components were identified for each service that related to the medical history, physical examination, and laboratory tests. A focus was placed on preventive screening rather than clinical management, as professional standards for clinical management already exist (e.g., CDC’s STD Treatment Guidelines17; the American Urological Association’s [AUA’s]18 and the American Society for Reproductive Medicine’s [ASRM’s] recommendations on infertility care19). Summaries of recommendations for counseling services are described as part of the referral/treatment process, because the need for counseling is typically dependent on the initial screening component. After summaries were compiled by topic, CDC topic experts also reviewed and made comments on the completeness and accuracy of the compilation.
Next, recommendations for each service were synthesized across organizations and those that were consistent or inconsistent across organizations were identified (e.g., they differed in the substance of the recommendation, target population, periodicity of screening). This included identifying services where no recommendation was made because of lack of evidence, where there was no evidence, or no mention was made at all.
Nineteen professional organizations and federal agencies were identified that make recommendations for a variety of preventive sexual and reproductive healthcare services for male patients across the life span, including the American Academy of Pediatrics (AAP); AUA; Society for Adolescent Health and Medicine (SAHM); American Cancer Society; ASRM; CDC; and the U.S. Preventive Services Task Force (USPSTF) (Appendix B contains a complete list of all included organizations). A document summarizing these recommendations was compiled, which outlined for each service the recommendation as originally stated by each major organization/agency, references for each source, tables synthesizing recommendations within each service across organizations/agencies, the rationale for the recommendation, and whether conflicting recommendations between organizations/agencies existed in general or for target populations. A description of the methods used by each organization/agency to generate recommendations was also included in the summary document. In total, this document summarized recommendations for 16 medical history components, 11 physical examination components, 13 laboratory tests, and four counseling components.
Choosing Clinical Screening Services through a Technical Panel Review
In July 2011, a technical panel was convened of ten clinical experts in men’s health, including practicing providers representing pediatrics, family medicine, adolescent medicine, and urology as well as representatives of various government and non-government organizations (Appendix C provides a list of technical panel members).
The framework of men’s sexual and reproductive healthcare services and the summary of existing recommendations were provided to panelists for review in advance of the meeting. Panelists were asked to consider the following questions that were based on the overarching goals of the guidelines development process and developed by CDC, OPA, and expert consultants:
Were any healthcare goals or services missing? Should any be omitted?
Were there any organizations or key reports missing? Should any be omitted?
Of all the sexual and reproductive health goals for men that were defined by ICDP and WHO, which are appropriate to deliver to men in a family planning setting?
What screening components of clinical care should be provided for each male service?
What screening components should be avoided?
The panel also provided feedback regarding clinical preventive services for men’s sexual and reproductive healthcare where recommendations or evidence were lacking. Feedback from technical panel members was provided to CDC and OPA on an individual basis (i.e., no group consensus was sought or reached).
Drafting the Clinical Recommendations for Men
After the technical panel meeting was completed, CDC and OPA used the panel’s feedback to develop a first draft of the clinical recommendations for delivering quality family planning services for men. This draft integrated recommendations on clinical services for both women and men and included an overall schema for the provision of selected services and specific screening components within each type of service. The draft recommendations were then presented to an expert work group panel in September 2011 (Appendix D provides a list of expert work group members). Members consisted of 17 experts in women’s and men’s health, including practicing providers representing obstetrics/gynecology, family medicine, adolescent medicine, and women’s health advanced practice and representatives from various government and non-government organizations. Some of the members participating in the expert work group also participated on the technical panel for men’s clinical services.
During this meeting, expert work group members were asked to consider whether the definition of family planning services was appropriate, the recommendations were feasible to implement, the schema increased or decreased barriers to care, the recommendations were appropriate for each type of family planning service, and the level of detail needed. As with the aforementioned technical panel, feedback from expert work group members was provided to CDC and OPA on an individual basis, without group consensus sought or reached. CDC and OPA then used the discussed range of perspectives to further inform a second draft of the recommendations.
The expert work group met again in February 2012 to review the revised recommendations. At the second meeting, they used the following criteria to consider the recommendations: (1) quality of the evidence; (2) positive and negative consequences of implementing the recommendations on health outcomes, costs or cost savings, and implementation challenges; and (3) relative importance of these consequences (e.g., the recommendations’ ability to have a large impact on health outcomes may be weighed more than logistical challenges of implementing it).20 As before, individual feedback (rather than group consensus) was provided to CDC and OPA, which used that feedback to make further revisions to the draft recommendations from 2012 through 2014.
Decision Process
Based on feedback from individual members of the technical panel and expert work group, CDC, and OPA made seven key decisions that greatly influenced the substance of QFP. This section describes these decisions and the rationale underpinning each.
A first decision was to use the ICPD and WHO definitions of sexual and reproductive health as a starting point for considering which men’s services should be included. This resulted in a comprehensive list of sexual and reproductive healthcare goals and related services that were further refined by subsequent decisions described below (Table 1). It also led to the acknowledgement of the need to meet the needs of diverse populations, including lesbian, gay, bisexual, or transgender (LGBT) individuals, people with disabilities, adolescents, and people with limited English proficiency.
Table 1.
Rationale for Including Preconception Health Services for Men
| Service | Rationale |
|---|---|
|
| |
| Reproductive life plan | Although not evidence-based in terms of its impact on reproductive and sexual risk behaviors among men, developing a reproductive life plan is a core recommendation in CDC’s preconception health recommendations.22 Asking about a client’s reproductive life plan is a necessary first step in assessing the need for other family planning services. |
| Medical history | Although not evidence-based in terms of its impact on reproductive and sexual risk behaviors among men, obtaining information from a medical history (e.g., about environmental hazards and toxins, medications, genetic conditions and family history, infectious diseases and vaccinations, mental health concerns) has been recommended by CDC and experts in men’s health.21,38 Obtaining a medical history is a necessary first step in assessing the need for other screening and treatment services. |
| Sexual health assessment | Although not evidence-based in terms of their direct impact on reduced sexual risk behaviors or STD incidence among men, conducting a sexual health assessment is a recommendation in the STD Treatment Guidelines,17 and a recommended first step in assessing the need for STD screening. |
| Alcohol and other drug use | Research has shown that heavy drinking (>2 drinks a day) is associated with lower levels of testosterone, semen volume, sperm count, and the number of sperm with normal morphology and motility.39 Other drugs have also been associated with male infertility, including marijuana and cocaine,40,41 and anabolic steroids.42,43 Both CDC and experts in men’s health included screening for alcohol and other drug use as a preconception health service.21,38 |
| Tobacco use | Tobacco use has been associated with decreased sperm count, abnormal sperm morphology, motility, and fertilizing capacity; it may also induce oxidative damage to sperm DNA.44 Both CDC and experts in men’s health included screening for tobacco use as a preconception health service.21,38 |
| Immunizations | There is some evidence of an association between mumps and male infertility.45,46 In addition, several vaccine-preventable diseases (flu, measles, etc.) if passed from a man to a pregnant woman could have an adverse impact on the woman and/or the infant.47,48 In addition, both CDC and experts in men’s health recommend reviewing men’s immunization status as a preconception health service.21,38 |
| Depression | Depression of the father during the postnatal development of his child has been significantly associated with poor childhood emotional and behavioral outcomes.49 Further, depressed fathers can be associated with negative mother-child interactions.50 Conversely, fathers with good mental health have been shown to reduce the impact of a mother’s depression on the child.51 In addition, both CDC and experts in men’s health included depression screening as a preconception health service.21,38 |
| Height, weight, and BMI | Obesity has been associated with lowered testosterone level, poorer semen quality, and reduced fertility.52,53 In addition, both CDC and experts in men’s health included BMI screening as a preconception health service.21,38 |
| Chlamydia Gonorrhea Syphilis | STDs are considered a men’s preconception health issue because they can lead to infertility in the female partner and severe morbidity in the child (e.g., perinatal HIV, congenital syphilis). |
| HIV/AIDS | Both CDC and experts in men’s health included STD screening and treatment as a preconception health service.21,38 |
| Diabetes | In men with diabetes mellitus type 1, semen volume, motility, and morphology are all significantly lowered compared to controls; diabetic men with unsatisfactory glycemic control had lower sperm count, motility, velocity, and viability than men with satisfactory glycemic control.54 Both CDC and experts in men’s health included screening for and managing diabetes as a preconception health service.21,38 |
STD, sexually transmitted disease.
Next, a decision was made about which clinical services for men should be considered within the context of a family planning visit. Decisions were made to promote comprehensive services while acknowledging the importance of minimizing barriers to family planning services and that the delivery of all relevant services may not be feasible during a single visit. Family planning services were considered a compilation of services embedded within a broader framework of preventive health services divided into three main categories: family planning services, related preventive health services, and other preventive health services (Figure 1). The definition of family planning services was determined to include contraception, pregnancy testing and counseling, achieving pregnancy, basic infertility, preconception health, and STD services. The rationale for including these services is that they are central to a couple’s ability to realize their reproductive goals (i.e., achieve their desired number and spacing of children).
Figure 1.
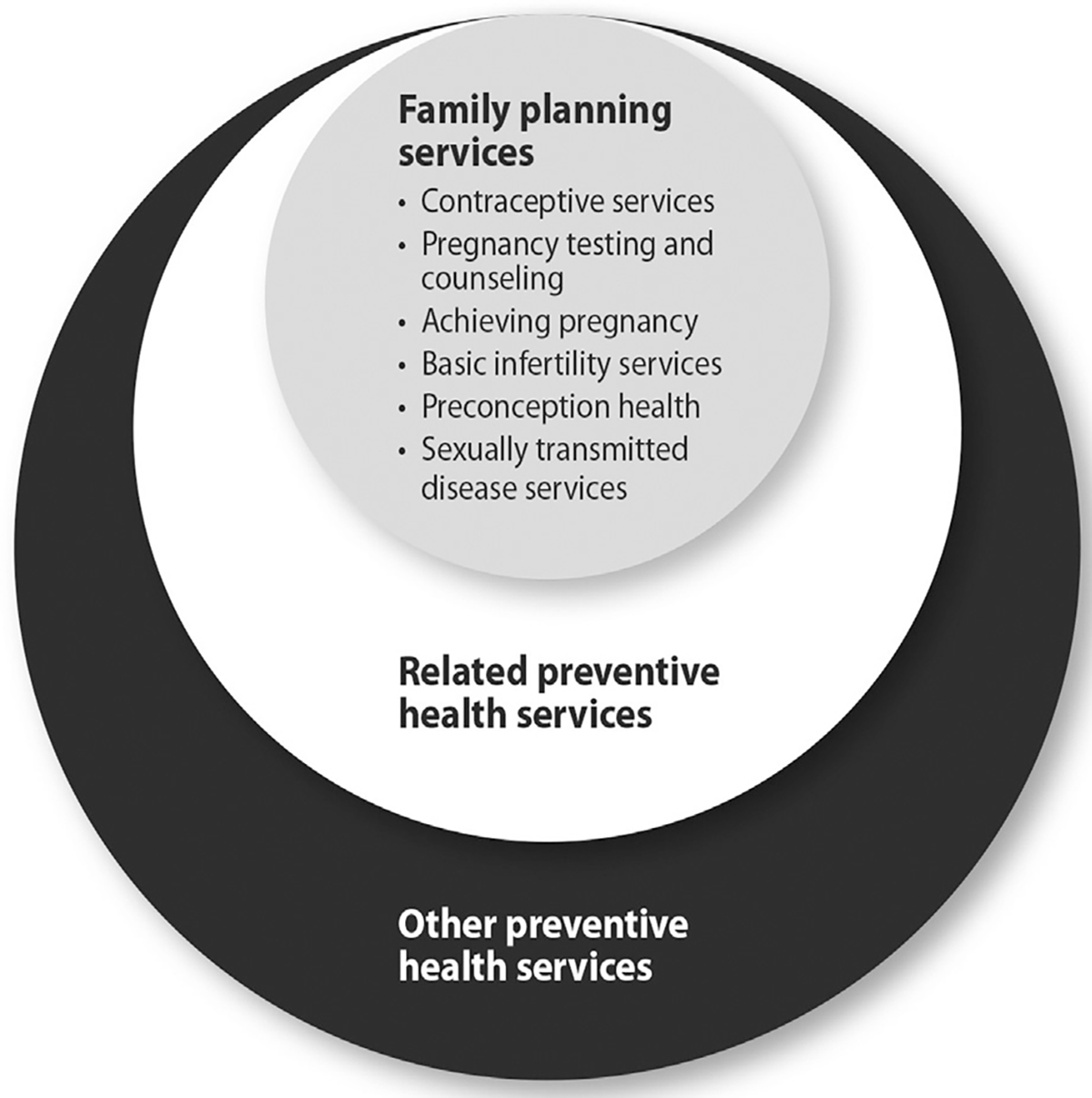
QFP’s framework of men’s preventive health services: Family planning, related and other preventive health services.
QFP, Providing Quality Family Planning Services: Recommendations of CDC and the U.S. Office of Population Affairs.
The decision to include preconception health and STD services for men was made because of their role in men’s fertility potential, in achieving a healthy pregnancy and infant, and their importance to men’s health and wellness even if they choose not to have children.21,22 The evidence base for men’s preconception health is less well established than that for women in terms of the existence of interventions to improve infant health outcomes; however, preconception health services for men were included if they had been recommended by leaders in men’s preconception health21 and there was a biologically plausible direct (e.g., STD transmission) or indirect (e.g., health condition reducing the man’s ability to impregnate a woman) link to infant health. Table 1 describes the rationale for including each preconception health service for men.
Third, the cornerstone for determining relevant services was based on assessing the client’s reproductive life plan and conducting a comprehensive sexual history. These assessments were deemed critical to offer to all men to assist in the determination of appropriate services, even if the initial reason for the visit was unrelated to family planning (e.g., if they came in for an acute care visit, STD diagnosis or treatment, or annual physical) because men may not otherwise receive those services.
How to provide each family planning service (e.g., the periodicity, which risk populations should be included) was another decision. Given inconsistencies among recommendations, decisions were made using a hierarchical approach: the technical panel adopted recommendations from CDC if they existed (e.g., HIV screening); if no CDC guideline existed, then an A or B recommendation from USPSTF was adopted. This hierarchy was chosen because CDC recommendations generally focus on populations at higher risk for disease and family planning clients were considered higher-risk populations for the considered services. CDC and USPSTF recommendations were ranked higher than those of professional medical associations because of the greater emphasis placed on evidence and use of systematic reviews of the evidence when developing recommendations. If no CDC or USPSTF recommendation existed, selected recommendations from professional medical associations were referenced. The AAP Bright Futures guidelines were referenced for adolescents because they are well recognized as the national standard of pediatric and adolescent health care.23 For some screening components, no recommendation from federal or professional organizations was identified; however, feedback based on expert opinion was that the component was integral to core family planning services and thus necessary to include in the recommendations (e.g., conducting a sexual health assessment as part of contraception services).
Table 2 summarizes the specific screening components for each service recommended in the QFP. Ultimately, for men the final guidance summarizes affirmative recommendations for eight medical history components, four physical examination components, and six laboratory tests, with three recommendations for counseling incorporated into its related screening component based on identification of risk.
Table 2.
Checklist of Family Planning and Related Preventive Health Services for Men
| Screening components and source of recommendation | Family planning services (provide services in accordance with the appropriate clinical recommendation) |
Related preventive health services | |||
|---|---|---|---|---|---|
| Contraceptive servicesa | Basic infertility services | Preconception health servicesb | STD servicesc | ||
|
| |||||
| History | |||||
| Reproductive life pland | Screen | Screen | Screen | Screen | |
| Medical historyd,e | Screen | Screen | Screen | Screen | |
| Sexual health assessmentd,e | Screen | Screen | Screen | Screen | |
| Alcohol and other drug used,e,f | Screen | ||||
| Tobacco used,f | Screen | ||||
| Immunizationsd | Screen | Screen for HPV and HBVg | |||
| Depressiond,f | Screen | ||||
| Physical exam | |||||
| Height, weight, and BMId,f | Screen | ||||
| Blood pressured,e | Screeng | ||||
| Genital exame | Screen (if clinically indicated) | Screen (if clinically indicated) | Screeng | ||
| Lab testing | |||||
| Chlamydiad | Screeng | ||||
| Gonorrhead | Screeng | ||||
| Syphilisd,f | Screeng | ||||
| HIV/AIDSd,f | Screeng | ||||
| Hepatitis Cd,f | Screeng | ||||
| Diabetesd,f | Screeng | ||||
HBV, hepatitis B virus; HPV, human papillomavirus; QFP, Providing Quality Family Planning Services: Recommendations of CDC and the U.S. Office of Population Affairs; STD, sexually transmitted disease.
No special evaluation needs to be done prior to making condoms available to males. However, when a male client requests advice on pregnancy prevention, he should be provided contraceptive services as described in the section “Provide Contraceptive Services” in the QFP.
The services listed here represent a subset of recommended preconception health services for men that were recommended and for which there was a direct link to fertility or infant health outcomes (Source: Frey K, Navarro S, Kotelchuck M, Lu M. The clinical content of preconception care: preconception care for men. Am J Obstet Gynecol. 2008;199(6)(suppl):S389-S395).
STD services also promote preconception health but are listed separately here to highlight their importance in the context of all types of family planning visits. The services listed in this column are for men without symptoms suggestive of an STD.
CDC recommendation.
U.S. Preventive Services Task Force recommendation.
Professional medical association recommendation.
Indicates that screening is suggested only for those persons at highest risk or for a specific subpopulation with high prevalence of infection or other condition.
A fifth decision concerned how to address other related preventive health services for men. Related preventive health services are services considered to be beneficial to reproductive health, closely linked to family planning services, and appropriate to deliver in the context of a family planning visit but do not contribute directly to achieving or preventing pregnancy (i.e., genital exam for male adolescents). The rationale for including these services is that many men have infrequent contact with the healthcare system, if at all,24 so there is a need to not miss opportunities to provide other preventive health services. The service included in this category is a physical exam of male adolescents to assess the progress of healthy sexual development of the genitals, based on SAHM recommendations.25
A sixth decision was to recommend against providing services shown to be ineffective or for which the potential harm outweighs the benefit (e.g., screening for testicular cancer). The rationale for this was based on recognition that clinical services are sometimes unnecessary or potentially harmful, and that explicit efforts should be made to alert providers to this fact. Accordingly, all relevant USPSTF D recommendations were noted as services not to provide. Decisions were also made to defer making any recommendation for services for which there is no USPSTF recommendation or an evidence base has not been established (e.g., anal Pap smear screening for men).
A final decision was to integrate recommendations for men’s health throughout QFP rather than having a separate section focused just on men, or treating them as a “special population.” The rationale for this approach is that it recognizes the role of men as critical partners in family planning and deserving of preventive health services in their own right.
Comment
In accordance with the IOM recommendation that guideline development processes be fully transparent, this paper describes the process of developing recommendations for delivering sexual and reproductive health care to men in a family planning setting that were included in QFP.9 These recommendations are noteworthy for several reasons. First, they represent one of the few efforts to address the delivery of a comprehensive set of clinical services for reproductive-aged men, and can serve as the foundation for national standards to deliver such services to U.S men. It is expected that these recommendations may be used in the many settings where primary care is provided (e.g., community-based health, school-based health, justice, and STD settings) and not only settings that are dedicated to the provision of family planning services.
Second, the recommendations are specific to men and address important gaps in the delivery of healthcare services to this population. Specifically, they address in part a recommendation by IOM’s Clinical Preventive Services for Women: Closing the Gaps7 that “a parallel approach could be equally useful for determining covered preventive services for men, …, and male adolescents” (Recommendation 6.3). Further, the recommendations are made at an important time in the history of improvements in the access to care for U.S. populations. Historically, many U.S. women have gained access to reproductive healthcare services through Medicaid waivers and publicly supported health plans for low-income women or women with children, whereas men were often excluded. More recently, both men and women obtained increased access and coverage for preventive sexual and reproductive health–related services through the ACA.7 Finally, an important strength of the recommendations in the QFP is that they are grounded in evidence-based clinical recommendations from federal and professional organizations wherever possible.9
The development of these recommendations also highlight new gaps and research priorities related to the delivery of sexual and reproductive healthcare services to men. Some individuals on the technical panel on men’s clinical services emphasized the importance of clinicians engaging with women and men as part of a couple, in a manner consistent with an emerging evidence base about the important role of partners in behavioral decision making.26–28 Future updates to the recommendations should consider best methods to more fully engage clients as couples, given the underlying partnered nature of these behaviors.
Also, there is a dearth of research in the domain of men’s sexual and reproductive health to inform an evidence base from which to conduct evidence-based reviews and, ultimately, inform guidance on clinical services to deliver to this population. Recommendations based on expert opinion, although on the lower end of the evidence ladder,29 have merit and can be useful in the context when high-quality evidence in the published literature is lacking and procedures are explicit and transparent.30–32 For example, recommendations outlined in this paper, especially those focused on male adolescents or the impact of men’s preconception health on infant health, are consistent with services that clinicians focused on men’s health perceived to be important to deliver.21,33 Future research is needed, as these recommendations were based primarily on expert opinion.
The recommendations also highlight services that are no longer recommended. For example, routine screening urinalysis for men (e.g., for STDs using leukocyte esterase or kidney function) is no longer recommended. Also, conducting a screening exam for testicular cancer among asymptomatic men is no longer recommended, although this USPSTF recommendation has been recently debated. Overall, the development of lists of no-longer-recommended services based on current evidence-based recommendations is consistent with the initiative of the American Board of Internal Medicine Foundation called “Choosing Wisely.”34 This initiative promotes providers and patients having discussions about these types of services to help make wise decisions about the most appropriate care based on a patient’s individual situation. QFP will be updated on a regular basis to reflect any changes in future USPSTF recommendations, or recommendations from other national professional organizations informing QFP, based on the most recent evidence-based reviews on related topics.
Finally, during the recommendation development process, several services recommended by the individual members of the technical panel to include as part of sexual and reproductive healthcare to deliver to men were not included in the final set of recommendations. Some of these services were excluded because an evidence base has not yet been established (i.e. screening for puberty and sexuality, relationships and dating, intimate personal violence, and specific male-focused counseling approaches [e.g., condom demonstration/practice]) or the current evidence base is insufficient to recommend for or against the service. Future work is needed to assist in building the evidence to determine whether such services are effective with male patients. For example, sexual minority men are found at greater risk of experiencing relationship-related violence compared with heterosexual men.35 Research and, ultimately, evidence reviews are needed to determine whether screening such at-risk male populations for intimate partner violence is warranted. Another service that was recommended by the individual members of the technical panel but not included because it fell beyond the definition of family planning for the clinical recommendations and no current federal or national professional organization recommendations exist was screening men for problems with sexual function. Identifying men with sexual function problems may help uncover those with early signs of systemic cardiovascular disease and represent opportunities for prevention, particularly among high-risk and underserved minority populations.36,37 Finally, future work should consider efforts to advance men’s sexual and reproductive health (e.g., fathering, healthy relationships) in community settings in addition to clinical services and to address the needs of men from diverse populations (e.g., rural versus urban, LGBT, Native Americans).
Conclusions
Meeting men’s sexual and reproductive health needs is important for several reasons.21 First, it is important for men’s general health in their own right. Second, it can result in improved health outcomes for men’s partners, including direct (e.g., decreased infection transmission or improved contraception use between partners) and indirect benefits (e.g., promotion of joint positive health practices). Third, men are critical partners in family planning; thus, engaging this population is essential to ensure all pregnancies are planned and wanted. Fourth, it may result in men’s improved capacity for fathering and parenting and, ultimately, improved outcomes for their children. Finally, it can be used as an opportunity to address men’s other health needs. These recommendations can assist healthcare providers and programs to provide the most-effective and -efficient services while also improving men’s access to sexual and reproductive health care. It is hoped that QFP recommendations for men will facilitate the integration of men’s healthcare into reproductive health programs in the U.S. and provide the foundation for other programs and guidance to build upon.
Supplementary Material
Acknowledgments
Publication of this article was supported by the U.S. Centers for Disease Control and Prevention (CDC) and the Office of Population Affairs (OPA).
The authors acknowledge Emily Godfrey, Naomi Tepper, and Kate Curtis from CDC for providing comments on a prior version of the manuscript, as well as members of the technical panel on clinical services for men (Appendix) and the members of the expert work group (Appendix).
This work and Drs. Marcell, McKenna, and Rompalo were supported under the Male Training Center’s cooperative agreement with the Office of Family Planning, Office of Population Affairs, DHHS (Cooperative Agreement FPTPA006011). The views expressed in this manuscript are those of the authors and do not necessarily represent the official position of CDC, the Office of Population Affairs, or DHHS.
No financial disclosures were reported by the authors of this paper.
Footnotes
Appendix
Supplementary data
Supplementary data associated with this article can be found at http://dx.doi.org/10.1016/j.amepre.2015.03.006.
References
- 1.Lindberg LD, Sonfield A, Gemmill A. Reassessing adolescent male sexual and reproductive health in the United States: research and recommendations. Am J Men’s Health. 2008;2(1):40–56. 10.1177/1557988307309460. [DOI] [PubMed] [Google Scholar]
- 2.Lindberg LD, Kost K. Exploring U.S. men’s birth intentions. Matern Child Health J. 2014;18(3):625–633. 10.1007/s10995-013-1286-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC. Sexually Transmitted Disease Surveillance, 2011. Atlanta, GA: DHHS, 2012. [Google Scholar]
- 4.Elster A, Kuzsets N. American Medical Association Guidelines for Adolescent Preventive Services (GAPS). Baltimore, MD: Williams & Wilkins, 1993. [Google Scholar]
- 5.Promoting healthy sexual development and sexuality (Bright Future Theme 8). In: Hagan JF Jr, Shaw JS, Duncan P, eds. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents —Third Edition. Elk Grove Village, IL: American Academy of Pediatrics, 2008. [Google Scholar]
- 6.American Academy of Family Physicians. Adolescent Health Care, Sexuality and Contraception 2006. American Academy of Family Physicians Policy Manual; 2008. www.aafp.org/online/en/home/policy/policies.html. [Google Scholar]
- 7.IOM. Clinical Preventive Services for Women: Closing the Gaps. Report Brief. Washington, DC: National Academies Press, 2011. [Google Scholar]
- 8.Fowler CI, Lloyd S, Gable J, Wang J, McClure E. Family Planning Annual Report: 2011 National Summary. Research Triangle Park, NC: RTI International, 2010. [Google Scholar]
- 9.CDC, Office of Population Affairs. Guidance for Providing Quality Family Planning Services: Recommendations by the CDC and the U.S. Office of Population Affairs. MMWR. 2014;63(4):1–54. [PubMed] [Google Scholar]
- 10.IOM. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press, 2001. [PubMed] [Google Scholar]
- 11.IOM. A Review of the HHS Family Planning Program: Mission, Management, and Measurement of Results. Washington, DC: National Academies Press, 2009. [PubMed] [Google Scholar]
- 12.IOM. Clinical Practice Guidelines We Can Trust. Washington, DC: National Academies Press, 2011. [PubMed] [Google Scholar]
- 13.Gavin LE, Moskosky SB, Barfield WD. Introduction to the supplement: development of federal recommedations for Family Planning Services. Am J Prev Med. 2015;49(2S1):S1–S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Godfrey EM, Tepper NK, Curtis KM, et al. Developing federal clinical care recommendations for women. Am J Prev Med. 2015;49(2S1): S6–S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.ICPD Programme of Action Summary. International Conference on Population and Development Cairo, Egypt: UN Department of Public Information; DPI/1618/POP—March 1995; 1994. www.unfpa.org/public/cache/offonce/home/sitemap/icpd/International-Conference-on-Population-and-Development/ICPD-Summary. [Google Scholar]
- 16.WHO. Defining sexual health: report of a technical consultation on sexual health, 28–31 January 2002, Geneva. Geneva, Switzerland: WHO Press; 2006. www.who.int/reproductivehealth/publications/sexual_health/defining_sh/en/. [Google Scholar]
- 17.Workowski KA, Berman S. Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR–12):1–110. [PubMed] [Google Scholar]
- 18.American Urological Association Education and Research Inc. The Optimal Evaluation of the Infertile Male: AUA Best Practice Statement. Linthicum Heights, MD: American Urological Association, 2010. [Google Scholar]
- 19.Male Infertility Best Practice Policy Committee of the American Urological Association; Practice Committee of the American Society for Reproductive Medicine. Report on optimal evaluation of the infertile male. Fertil Steril. 2006;86(5 suppl 1):S202–S209. 10.1016/j.fertnstert.2006.08.029. [DOI] [PubMed] [Google Scholar]
- 20.Guyatt GH, Oxman AD, Kunz R, et al. Going from evidence to recommendations. BMJ. 2008;336(7652):1049–1051. 10.1136/bmj.39493.646875.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frey KA, Navarro SM, Kotelchuck M, Lu MC. The clinical content of preconception care: preconception care for men. Am J Obstet Gynecol. 2008;199(6 suppl 2):S389–S395. 10.1016/j.ajog.2008.10.024. [DOI] [PubMed] [Google Scholar]
- 22.Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care—United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep. 2006;55(RR–6):1–23. [PubMed] [Google Scholar]
- 23.Hagan JF Jr, Shaw JS, Duncan P, eds. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents—Third Edition. Elk Grove Village, IL: American Academy of Pediatrics, 2008. [Google Scholar]
- 24.U.S. Census Bureau. Statistical Abstract of the United States: 2012 (131st Edition) Washington, DC: 2011. www.census.gov/compendia/statab/. [Google Scholar]
- 25.Marcell A, Bell D, Joffe A. The male genital examination: a position paper of the Society for Adolescent Health and Medicine. J Adolesc Health. 2012;50(4):424–425. 10.1016/j.jadohealth.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Forste R, Morgan J. How relationships of U.S. men affect contraceptive use and efforts to prevent sexually transmitted diseases. Fam Plann Perspect. 1998;30(2):56–62. 10.2307/2991660. [DOI] [PubMed] [Google Scholar]
- 27.Frost JJ, Darroch JE. Factors associated with contraceptive choice and inconsistent method use, United States, 2004. Perspect Sex Reprod Health. 2008;40(2):94–104. 10.1363/4009408. [DOI] [PubMed] [Google Scholar]
- 28.Severy LJ, Silver SE. Two reasonable people: joint decision-making in contraceptive choice and use. In: Severy LJ, ed., Advances in Population: Psychosocial Perspectives. London: Jessica Kingsley Publishers, 1994:207–227. [DOI] [PubMed] [Google Scholar]
- 29.Atkins D, Eccles M, Flottorp S, et al. Systems for grading the quality of evidence and the strength of recommendations, I: critical appraisal of existing approaches. The GRADE Working Group. BMC. Health Serv Res. 2004;4(1):38. 10.1186/1472-6963-4-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grol R Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001;39(8 suppl 2): II46–II54. [DOI] [PubMed] [Google Scholar]
- 31.Cheung AH, Zuckerbrot RA, Jensen PS, Stein RE, Laraque D. Expert survey for the management of adolescent depression in primary care. Pediatrics. 2008;121(1):e101–e107. 10.1542/peds.2006-3560. [DOI] [PubMed] [Google Scholar]
- 32.Bridevaux IP, Silaghi AM, Vader JP, Froehlich F, Gonvers JJ, Burnand B. Appropriateness of colorectal cancer screening: appraisal of evidence by experts. Int J Qual Health Care. 2006;18(3):177–182. 10.1093/intqhc/mzl005. [DOI] [PubMed] [Google Scholar]
- 33.Marcell AV, Ellen JM. Core sexual/reproductive health care to deliver to male adolescents: perceptions of clinicians focused on male health. J Adolesc Health. 2012;51(1):38–44. 10.1016/j.jadohealth.2011.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17): 1801–1802. 10.1001/jama.2012.476. [DOI] [PubMed] [Google Scholar]
- 35.Black MC, Basile KC, Breiding MJ, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, CDC, 2011. [Google Scholar]
- 36.Billups KL, Bank AJ, Padma-Nathan H, Katz S, Williams R. Erectile dysfunction is a marker for cardiovascular disease: results of the minority health institute expert advisory panel. J Sex Med. 2005;2(1): 40–50; discussion 50–52. 10.1111/j.1743-6109.2005.20104_1.x. [DOI] [PubMed] [Google Scholar]
- 37.Kostis JB, Jackson G, Rosen R, et al. Sexual dysfunction and cardiac risk (the Second Princeton Consensus Conference). Am J Cardiol. 2005;96 (2):313–321. 10.1016/j.amjcard.2005.03.065. [DOI] [PubMed] [Google Scholar]
- 38.CDC. Preconception care for men. www.cdc.gov/preconception/careformen/promotion.html.
- 39.Muthusami KR, Chinnaswamy P. Effect of chronic alcoholism on male fertility hormones and semen quality. Fertil Steril. 2005;84(4): 919–924. 10.1016/j.fertnstert.2005.04.025. [DOI] [PubMed] [Google Scholar]
- 40.Hampton T Researchers discover a range of factors undermine sperm quality, male fertility. JAMA. 2005;294(22):2829–2831. 10.1001/jama.294.22.2829. [DOI] [PubMed] [Google Scholar]
- 41.Fronczak C, Kim E, Barqawi A. The insults of illicit drug use on male fertility. J Androl. 2012;33(4):515–528. 10.2164/jandrol.110.011874. [DOI] [PubMed] [Google Scholar]
- 42.Torres-Calleja J, Gonzalez-Unzaga M, DeCelis-Carrillo R, Calzada-Sanchez L, Pedron N. Effect of androgenic anabolic steroids on sperm quality and serum hormone levels in adult male bodybuilders. Life Sci. 2001;68(15):1769–1774. 10.1016/S0024-3205(01)00972-9. [DOI] [PubMed] [Google Scholar]
- 43.Karila T, Hovatta O, Seppala T. Concomitant abuse of anabolic androgenic steroids and human chorionic gonadotrophin impairs spermatogenesis in power athletes. Int J Sports Med. 2004;25(4): 257–263. 10.1055/s-2004-819936. [DOI] [PubMed] [Google Scholar]
- 44.Soares SR, Melo MA. Cigarette smoking and reproductive function. Curr Opin Obstet Gynecol. 2008;20(3):281–291. 10.1097/GCO.0b013e3282fc9c1e. [DOI] [PubMed] [Google Scholar]
- 45.Davis NF, McGuire BB, Mahon JA, Smyth AE, O’Malley KJ, Fitzpatrick JM. The increasing incidence of mumps orchitis: a comprehensive review. BJU Int. 2010;105(8):1060–1065. 10.1111/j.1464-410X.2009.09148.x. [DOI] [PubMed] [Google Scholar]
- 46.Wang XX, Ying P, Diao F, et al. Altered protein prenylation in Sertoli cells is associated with adult infertility resulting from childhood mumps infection. J Exp Med. 2013;210(8):1559–1574. 10.1084/jem.20121806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rasmussen SA, Jamieson DJ, Uyeki TM. Effects of influenza on pregnant women and infants. Am J Obstet Gynecol. 2012;207(3 suppl): S3–S8. 10.1016/j.ajog.2012.06.068. [DOI] [PubMed] [Google Scholar]
- 48.White SJ, Boldt KL, Holditch SJ, Poland GA, Jacobson RM. Measles, mumps, and rubella. Clin Obstet Gynecol. 2012;55(2):550–559 10.1097/GRF.0b013e31824df256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ramchandani P, Stein A, Evans J, O’Connor TG, ALSPAC study team. Paternal depression in the postnatal period and child development: a prospective population study. Lancet. 2005;365(9478):2201–2205 10.1016/S0140-6736(05)66778-5. [DOI] [PubMed] [Google Scholar]
- 50.Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006;118(2):659–668. 10.1542/peds.2005-2948. [DOI] [PubMed] [Google Scholar]
- 51.Kahn RS, Brandt D, Whitaker RC. Combined effect of mothers’ and fathers’ mental health symptoms on children’s behavioral and emotional well-being. Arch Pediatr Adolesc Med. 2004;158(8):721–729 10.1001/archpedi.158.8.721. [DOI] [PubMed] [Google Scholar]
- 52.Sermondade N, Faure C, Fezeu L, et al. BMI in relation to sperm count: an updated systematic review and collaborative meta-analysis. Hum Reprod Update. 2013;19(3):221–231. 10.1093/humupd/dms050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stephens SM, Polotsky AJ. Big enough for an aromatase inhibitor? How adiposity affects male fertility. Semin Reprod Med. 2013;31(4): 251–257. 10.1055/s-0033-1345272. [DOI] [PubMed] [Google Scholar]
- 54.La Vignera S, Condorelli R, Vicari E, D’Agata R, Calogero AE. Diabetes mellitus and sperm parameters. J Androl. 2012;33(2):145–153 10.2164/jandrol.111.013193. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


