Abstract
Objective
The COVID-19 pandemic led to an increase in mortality in most countries in 2020, deviating from prior decreasing trends. In Japan, however, mortality was suggested to decrease in 2020. This study investigated long-term mortality trends and cause-specific contributions, focusing on the period of the COVID-19 pandemic in Japan.
Design
We analysed Japanese age-standardised mortality rates (ASMRs) from 1995 to 2021 using vital statistics.
Main outcome measures
The cause-specific annual ASMR changes were calculated in comparison with the previous year over the abovementioned period.
Results
There was a general downward trend in overall ASMR for both sexes until 2020 followed by a small increase in 2021. In men, the all-cause ASMR (per 100 000 persons) decreased from 1352.3 to 1328.8 in 2020 (−1.74% from 2019), and increased to 1356.3 in 2021 in men (+2.07% from 2020). In women, the all-cause ASMR decreased from 746.0 to 722.1 in 2020 (−3.20% from 2019), and increased to 737.9 (+2.19% from 2020) in 2021. ASMRs from malignant neoplasms, pneumonia, accidents and suicide (men only) continued to decrease during the COVID-19 pandemic while the trend of cardiovascular mortality increased in 2021. Analysis of ASMR changes revealed that COVID-19, senility, cardiovascular disease and ‘other causes not classified as major causes’ contributed to the all-cause mortality increase in 2021.
Conclusions
In Japan, the decreasing trend in overall mortality continued in 2020 despite the COVID-19 pandemic. However, approximately 2% mortality increase was observed in 2021, which was attributable to COVID-19, senility, cardiovascular disease and ‘other causes’. The year 2021 was a turning point of mortality trends in Japan, although continued monitoring is warranted.
Keywords: COVID-19, Epidemiology, Public health, Demography
STRENGTHS AND LIMITATIONS OF THIS STUDY.
We comprehensively analysed mortality in Japan from the Ministry of Health, Labour, and Welfare published the 2021 complete mortality data for the Japanese population.
To analyse the contribution of the cause of death to annual all-cause age-standardised mortality rates (ASMRs) changes, the cause-specific ASMR changes in comparison with those of the previous year were calculated.
This study is a descriptive analysis, and therefore, further analysis is needed to clarify the quantitative impact such as ‘excess deaths’.
In addition, long-term monitoring is necessary from 2022 onwards, especially for deaths from chronic diseases that may have long-term effects by changes in lifestyle and medical care.
Introduction
Approximately 3 years into the pandemic, the impact of COVID-19 on Japan continues to increase. Although the Japanese government did not introduce strict COVID-19 restrictions such as lockdown, people’s daily lives were affected, as were the lives of healthcare workers since the first declaration of a state of emergency in April 2020. To date, however, no nationwide mortality data that discuss the impact of the COVID-19 pandemic on mortality trends have been reported in Japan. Careful assessment of the impact of the pandemic on population health would aid in the evaluation of efforts during the pandemic and identify lessons, not only for Japan but also globally.
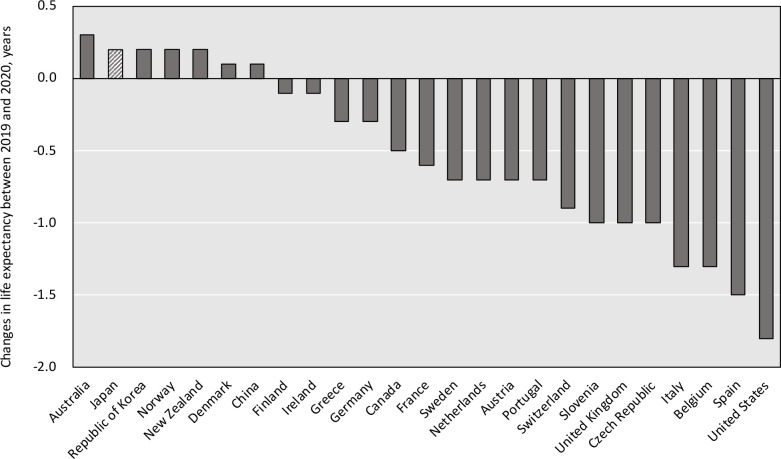
In most high-income countries, life expectancy in 2020 was shorter than that before, attributable to both the direct and indirect effects of COVID-19.1 For example, reductions in life expectancy in 2020 were observed in Russia, the USA, Spain, England/Wales, Netherlands, Sweden and France.2 However, in Japan, life expectancy was not shortened in 2020 according to the Japanese Ministry of Health, Labour and Welfare (MHLW),1 3 a deviation from the decreasing trend in most countries.1
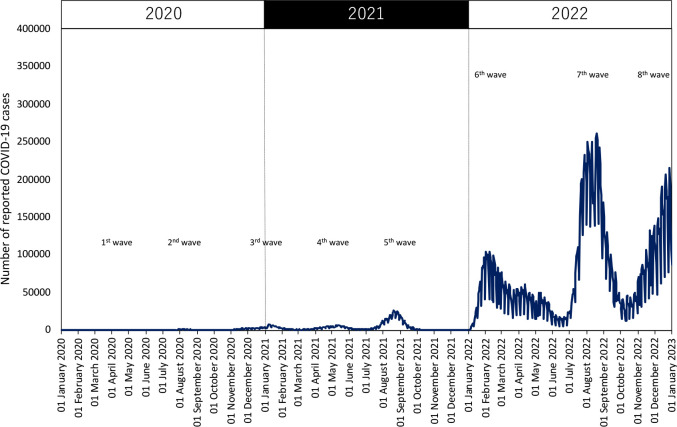
Reasons for the prolonged life expectancy in 2020 despite the pandemic are unclear. One reason could be that Japan did not experience as large a number of COVID-19 cases that year as other countries. However, Japan experienced a sixfold increase in the number of reported cases from 2020 to 2021: 234 109 cases in 2020 and 1 492 874 cases in 2021.4 Thus, annual mortality rate in 2021 in Japan may differ from the stable downward trend seen before 2020. This study aimed to explore the long-term mortality trends and cause-specific contributions during the COVID-19 pandemic in Japan, focusing on the years 2020 and 2021.
Methods
We illustrated changes in life expectancy between 2019 and 2020 for selected countries, including Japan, using data extracted from the World Development Indicators managed by the World Bank.1 To evaluate the trends in the number of COVID-19 cases in Japan, we extracted data on the daily number of reported COVID-19 cases from 16 January 2020 (the first case confirmed) to 1 January 2023 from Japanese government records.4 The numbers of deaths (5 year age intervals) between 1995 and 2021 were extracted from the vital statistics (complete deaths record) in Japan managed by MHLW.3 The 2021 complete mortality data were published in September 2022.3 The vital statistics cover all Japanese deaths that occurred in Japan. The relevant population data were also collected from the vital statistics and population census.
We calculated age-standardised mortality rates (ASMRs) for all causes of death combined and cause-specific deaths for major causes from 1995 to 2021 to assess trends in mortality rates. ASMRs were calculated using the 2015 Japan Standard Population.5 We further calculated the annual percent changes in ASMRs before and during the early part of the COVID-19 pandemic (2020 and 2021). Causes of death (the International Classification of Diseases 10th revision: ICD-10) included: certain infectious and parasitic diseases (A00-B99), malignant neoplasms (C00-C96), heart diseases (I01-I02.0, I05-I09, I20-I25, I27, I30-I52), cerebrovascular diseases (I60-I69), pneumonia (J12-J18), liver disease (K70-K76), senility (R54), accidents (V01-X59), suicide (X60-X84) and COVID-19 (U07). These classifications were based on the leading causes of death reported by the official mortality statistics from MHLW.3 MHLW follows the algorithm for classifying the causes of death based on ICD-10.
To analyse the contribution of the cause of death to annual all-cause ASMR changes, the cause-specific ASMR changes in comparison with those of the previous year were calculated for six periods from 2015–2016 to 2020–2021.
Patient and public involvement
Actual patients were not involved in this study of data.
Results
Figure 1 shows Japan was one of the countries where life expectancy was prolonged in 2020 despite having shortened in many high-income countries such as the USA and France. Figure 2 shows trends in the daily number of reported COVID-19 cases in Japan since 16 January 2020. The peak of reported COVID-19 cases was observed in August 2022 (seventh COVID-19 wave). While the absolute number of COVID-19 cases was very small in 2020, the annual number of reported COVID-19 cases increased rapidly in 2021 and 2022.
Figure 1.
Changes in life expectancy between 2019 and 2020 for selected countries for both sexes.
Figure 2.
Trends in the daily number of reported COVID-19 cases in Japan since 16 January 2020.
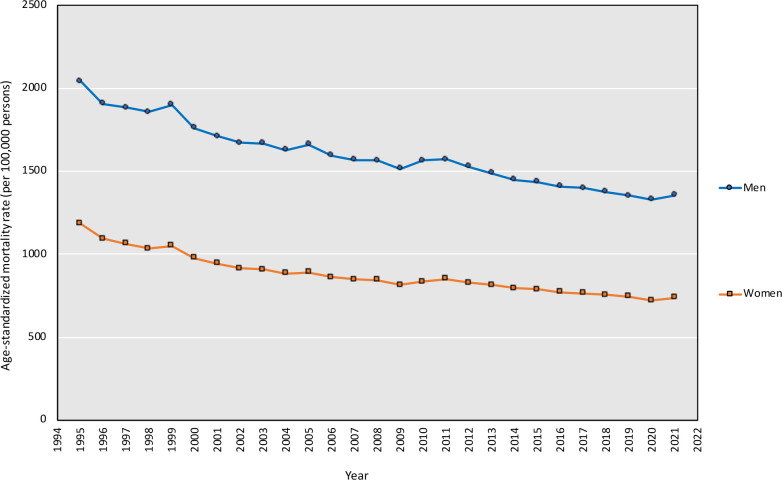
Figure 3 shows the trends in all-cause ASMRs (per 100 000 persons) between 1995 and 2021. Online supplemental table 1 shows the trends in number of deaths in Japan between 1995 and 2021. After the Great East Japan Earthquake occurred in 2011, ASMRs continued decreasing until 2020, then increased in 2021 in both sexes. For men, all-cause ASMRs (per 100 000 persons) were 1352.3 in 2019 (−1.69% from 2018), 1328.8 in 2020 (−1.74% from 2019) and 1356.3 in 2021 (+2.07% from 2020). For women, all-cause ASMRs were 746.0 in 2019 (−1.39% from 2018), 722.1 in 2020 (−3.20% from 2019) and 737.9 in 2021 (+2.19% from 2020). Age-specific analyses also showed stable to slightly increased mortality trends during the period of COVID-19 pandemic (online supplemental figure 1). Online supplemental figure 2 shows the trends in cause-specific ASMRs between 1995 and 2021. For men, COVID-19 ASMRs (per 100 000 persons) were 3.8 in 2020 and 17.5 in 2021. For women, COVID-19 ASMRs (per 100 000 persons) were 1.5 in 2020 and 7.7 in 2021. ASMRs from malignant neoplasms, pneumonia, accidents and suicide (men only) decreased during the COVID-19 pandemic in Japan while the trend of cardiovascular disease (heart disease and cerebrovascular disease combined) increased in 2021. In addition, the trend of suicide in women increased in 2020. Online supplemental figure 3 shows trends in malignant neoplasms ASMRs by cancer site. Trends in most malignant neoplasms were decreased or stable, which was not altered compared with the trends before 2020.
Figure 3.
Trends in all-cause age-standardised mortality rates between 1995 and 2021.
bmjopen-2023-071785supp001.pdf (1.5MB, pdf)
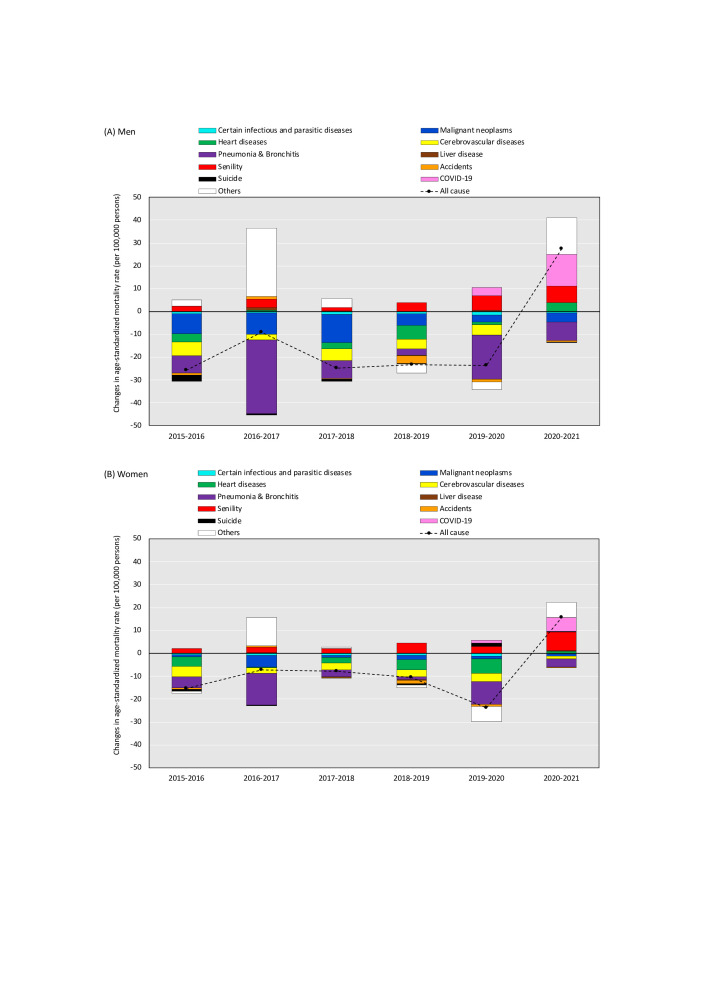
Figure 4 shows the cause-specific contribution to annual changes in all-cause ASMR. The analysis of annual ASMR changes revealed that decreases in malignant neoplasms, pneumonia, heart disease and cerebrovascular diseases continuously contributed to substantial annual mortality reductions for both sexes during 2015–2019; however, the contributions to reduction disappeared for cardiovascular disease from 2020 to 2021. COVID-19 (+13.7 per 100 000 persons for men and +6.2 per 100 000 persons for women in comparisons with the previous year) and senility (+7.4 per 100 000 persons for men and +8.1 per 100 000 persons for women in comparisons with the previous year) largely contributed to the mortality increases from 2020 to 2021. Also, ‘other causes not classified major causes’ contributed to all-cause mortality increase as well from 2020 to 2021.
Figure 4.
Cause-specific contribution to changes in all-cause age-standardised mortality rates (annual comparisons with previous year): differences in changes in ASMR between 2020 and 2021 were calculated as (ASMR2021− ASMR2020) for each cause-specific death, where ASMR=age standardised mortality rate per 100 000 persons.
Discussion
This is the first study to comprehensively report on mortality analysis in Japan since MHLW published the 2021 complete mortality data for the Japanese population. We found that the numbers of deaths from COVID-19 were 9732 (1.32% of all deaths) for men and 7034 (1.00% of all deaths) for women in 2021, a substantial increase from the year 2020 (2094 deaths for men and 1372 deaths for women). The number of deaths in the population due to diagnosed COVID-19 was relatively low compared with many other high-income countries.6 In both men and women, all-cause ASMR decreased gradually every year from 2011 to 2020 and increased from 2020 to 2021, with a slightly greater decrease in women than in men between 2019 and 2020. In Japan, declining trends in all-cause mortality reversed in 2021 for the first time since the Great East Japan Earthquake occurred in 2011.
The mortality trend varied by cause of death. The patterns of mortality change during the COVID-19 pandemic could be classified into the following three categories: (1) stable mortality decline (eg, certain infectious and parasitic diseases, malignant neoplasms and pneumonia), (2) stable mortality increase (eg, senility) and (3) reversal of decreasing mortality trend (heart diseases, cerebrovascular diseases, suicide for women). Considering these changes, a substantial mortality increase from COVID-19 and senility resulted in an all-cause mortality increase in 2021 while malignant neoplasms and pneumonia contributed to mortality declines.
Recorded mortality from malignant neoplasms declined during the COVID-19 pandemic, despite that patients diagnosed with a cancer regardless of COVID-19 status were required to postpone non-urgent surgeries, suspend outpatient visits and change treatment methods. Indeed, the numbers of cancer diagnoses, the cancer screening, outpatient visits and surgical procedures in 2020 have been reported to be lower than those before 2019.7–10 Those reports have raised deep concern about potential consequences, such as delays in diagnosis and care, decreased patient survival and increased population mortality; however, our findings revealed a decrease in 2020 and no obvious change in cancer mortality, at least in 2021. Nevertheless, further monitoring is necessary because the delays in diagnosis and treatment can exert a belated effect on mortality.
We found that the ASMR from cardiovascular disease increased in 2021. The loss of reduction trends of cardiovascular disease partially resulted in increasing all-cause mortality in 2021 for both sexes. This is supported by another study reporting excess deaths from cardiovascular disease from April to May 2021.11 As a direct pathway, the COVID-19 pandemic may have caused an increase in the prevalence of severe heart disease for the Japanese population because COVID-19 is suggested to be a risk factor for acute myocardial infarction and ischaemic stroke.12 In addition, the pandemic might have induced a delay in emergency transport and delay in arrival at hospital, resulting in the loss of timely treatment. This may be an indirect pathway through which mortality reductions of cardiovascular disease stagnated in Japan.
A substantial increase in mortality due to senility has been occurring since the mid-2000s, independent of the pandemic. This can be interpreted as a result of the rapid ageing of the Japanese population. Although we applied age-standardisation for mortality analysis, the increase in the absolute number of deaths from senility, especially for the oldest old (85 years and over), resulted in an increase in ASMR. During the pandemic, however, changes in patterns or places of medical care may have resulted in more physicians reporting senility as the cause of death, especially deaths at home. Indeed, excess deaths from senility at home have been observed since May 2020.11 As such, for the elderly, both direct and indirect death by COVID-19 may be miscoded to senility, which contributed to excess deaths in 2021. The sharp increase in deaths by ‘other causes not classified as major causes’ in 2021 (figure 3) may have occurred by a similar mechanism. Therefore, our findings suggest that senility and ‘other causes not classified as major causes’ may largely represent the excess deaths in Japan during the pandemic. This may also include underdiagnosis and potential misclassification of causes of death.
We found clear declines in mortality from infectious diseases (excluding COVID-19) and infectious pneumonia since the pandemic began in Japan. This is likely because the countermeasures for COVID-19 such as wearing a mask, hand hygiene and social distancing prevented these diseases. In addition, clear mortality declines due to accidents were observed probably because fatal traffic accidents decreased due to stay-at-home measures. These are positive outcomes of the COVID-19 measures; however, we identified an increase in suicide rate among women in 2020 and 2021. The increase did not largely impact on all-cause mortality changes for women but this is obviously a negative effect of the COVID-19 measures such as restrictions of economic activity (eg, cancellation of events and shorter business hours for restaurants).13 14
This study is a descriptive analysis of national mortality data and should accordingly be interpreted with caution. Our findings suggest that the mortality increase in 2021 may be associated with the increase in COVID-19 cases; however, further analysis is needed to clarify the quantitative impact such as ‘excess deaths’. Also, long-term monitoring is necessary from 2022 onwards, especially for deaths from chronic diseases that may have long-term effects by changes in lifestyle and medical care.
In conclusion, a sign of increasing mortality was observed in 2021 in the annual mortality rate in Japan, although the impact of the COVID-19 pandemic on mortality in Japan still seems to be limited. The observed increase in mortality was attributable to COVID-19, senility, cardiovascular disease, and ‘other causes not classified as major cause’. Taking the rapidly increasing rate of COVID-19 cases in 2022 into consideration, further monitoring is warranted for the year 2022, which may reveal a larger impact of the pandemic on mortality compared with that for 2020 and 2021.
Supplementary Material
Acknowledgments
We thank Libby Cone, MD, MA, from Dmed (http://www.dmed.co.jp) for editing English drafts of this manuscript
Footnotes
Contributors: All authors had full access to all the study data. HT is the guarantor of this work and was responsible for the integrity of the data, the accuracy of the data analysis and the drafting of the manuscript. All authors contributed to the concept and design of the study. All authors critically reviewed the manuscript. KK supervised the study and provided administrative, technical and material support.
Funding: Grants-in-Aid for Cancer Control Policy from the Ministry of Health, Labour, and Welfare, Japan (20EA1017); Japan Agency for Medical Research and Development (AMED: 22ck0106778h0001).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. This study used the vital statistics data from a portal site for Japanese Government Statistics (e-Stat: https://www.e-stat.go.jp/), and data at an individual level were not used.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1. The World Bank . Life expectancy at birth, total (years). Available: https://data.worldbank.org/indicator/SP.DYN.LE00.IN [Accessed 12 Dec 2022].
- 2. Islam N, Jdanov DA, Shkolnikov VM, et al. Effects of COVID-19 pandemic on life expectancy and premature mortality in 2020: time series analysis in 37 countries. BMJ 2021;375:e066768. 10.1136/bmj-2021-066768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ministry of Health, Labour and Welfare . Vital Statistics. Available: https://www.mhlw.go.jp/english/database/db-hw/vs01.html [Accessed 12 Dec 2022].
- 4. Ministry of Health, Labour and Welfare . Visualizing the data: information on COVID-19 infections. Available: https://covid19.mhlw.go.jp/en/ [Accessed 12 Dec 2022].
- 5. Tanaka H, Tanaka S, Togawa K, et al. Practical implications of the update to the 2015 Japan standard population: mortality archive from 1950 to 2020 in Japan. J Epidemiol 2023;33:372–80. 10.2188/jea.JE20220302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization . WHO Coronavirus (COVID-19) dashboard. Available: https://covid19.who.int [Accessed 12 Dec 2022].
- 7. Ikeda N, Yamamoto H, Taketomi A, et al. The impact of COVID-19 on surgical procedures in Japan: analysis of data from the National Clinical Database. Surg Today 2022;52:22–35. 10.1007/s00595-021-02406-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sato Y, Fujiwara Y, Fukuda N, et al. Changes in treatment behavior during the COVID-19 pandemic among patients at a cancer hospital. Cancer Cell 2021;39:130–1. 10.1016/j.ccell.2021.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Toyoda Y, Katanoda K, Ishii K, et al. Negative impact of the COVID-19 state of emergency on breast cancer screening participation in Japan. Breast Cancer 2021;28:1340–5. 10.1007/s12282-021-01272-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Okuyama A, Watabe M, Makoshi R, et al. Impact of the COVID-19 pandemic on the diagnosis of cancer in Japan: analysis of hospital-based cancer registries. Jpn J Clin Oncol 2022;52:1215–24. 10.1093/jjco/hyac129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nomura S, Eguchi A, Ghaznavi C, et al. Excess deaths from non-COVID-19-related causes in Japan and 47 prefectures from January 2020 through may 2021 by place of death. SSM Popul Health 2022;19:101196. 10.1016/j.ssmph.2022.101196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Katsoularis I, Fonseca-Rodríguez O, Farrington P, et al. Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: a self-controlled case series and matched cohort study. Lancet 2021;398:599–607. 10.1016/S0140-6736(21)00896-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sakamoto H, Ishikane M, Ghaznavi C, et al. Assessment of suicide in Japan during the COVID-19 pandemic vs previous years. JAMA Netw Open 2021;4:e2037378. 10.1001/jamanetworkopen.2020.37378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kikuchi K, Anzai T, Takahashi K. The unusual increase in suicides among women in Japan during the COVID-19 pandemic: A time-series analysis until October 2021. J Epidemiol 2023;33:45–51. 10.2188/jea.JE20220186 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-071785supp001.pdf (1.5MB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. This study used the vital statistics data from a portal site for Japanese Government Statistics (e-Stat: https://www.e-stat.go.jp/), and data at an individual level were not used.