Abstract
Lifelong respiratory health is rooted in the structural and functional development of the respiratory system in early life. Exposures and interventions antenatally through childhood can influence lung development into young adulthood, the life stage with the highest achievable lung function. Because early respiratory health sets the stage for adult lung function trajectories and risk of developing chronic obstructive pulmonary disease, understanding how to promote lung health in children will have far reaching personal and population benefits. To achieve this, it is critical to have accurate and precise measures of structural and functional lung development that track throughout life stages. From this foundation, evaluation of environmental, genetic, metabolic, and immune mechanisms involved in healthy lung development can be investigated. These goals require the involvement of general pediatricians, pediatric subspecialists, patients, and researchers to design and implement studies that are broadly generalizable and applicable to otherwise healthy and chronic disease populations. This National Institutes of Health workshop report details the key gaps and opportunities regarding lung function and structure.
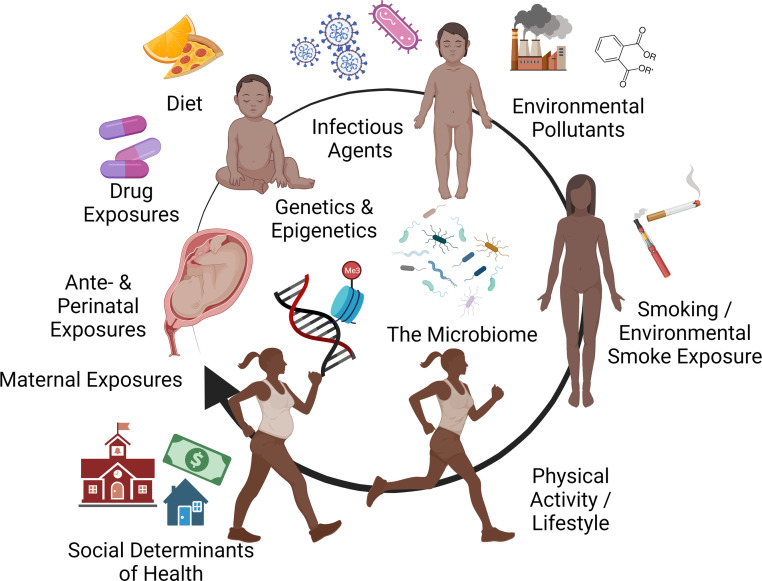
Defining and promoting pediatric pulmonary health depends on accurate measurement of lung structure and function to assess healthy lung growth and optimization of the physiologic capacity of the respiratory system. Lifelong lung function trajectories are firmly rooted in early life and are forged by the interplay of genetic predisposition and exposures to environmental pollutants, infections, and other respiratory insults (Fig 1).1 Because adult lung function is a strong predictor of mortality, achieving optimal lung health throughout childhood and adolescence has far-reaching societal benefits. Critical to this endeavor is the development of tools and techniques to effectively measure lung function and structure in a standardized way from infancy (or even in utero) through childhood.
FIGURE 1.
Factors affecting lifelong lung health. Schematic representing the interplay of genetic predisposition, host characteristics, and exposures to environmental pollutants, infections, diet, and other factors in the development of lung function and structure. Created with BioRender.com
To date, most research has focused on disease-specific respiratory outcomes. However, studying respiratory health through this lens risks missing the opportunity to define and promote factors that lead to healthy lung growth and function for the general population. Partnership between general pediatric providers, subspecialists, patients, and researchers is necessary to access large, longitudinal cohorts of research participants to answer questions that are generalizable to the health of the whole population. Broad efforts are needed to evaluate and address social disparities known to affect lung health in children and adults.
On March 29 and 30, 2021, the Division of Lung Diseases, National Heart, Lung, Blood Institute, National Institutes of Health (NIH), sponsored a multidisciplinary workshop entitled “Defining and Promoting Pediatric Pulmonary Health (DAP3H).” This report details the key gaps and opportunities regarding lung function and structure (Table 1).
TABLE 1.
Critical Gaps in Pediatric Lung Structure/Function
| Critical Gaps |
|---|
| • What are the environmental, genetic, metabolic, and immune (EGMI) mechanisms that establish lung function and structure throughout life? |
| • If evaluation of EGMI mechanisms takes 4–6 decades, how do we develop and maintain large cohorts frequently enough to understand new exposures and new lung phenotypes? |
| • How do we incorporate sophisticated personal exposure data and frequent outcome assessments into longitudinal cohort studies? |
| • Aside from tobacco cessation efforts, which strategies are practical for clinical practice in pediatrics? |
| • How do we consistently improve accuracy of spirometry in primary care? |
| • Should we incorporate lung function assessments that require less cooperation, time, and technician training, such as oscillometry, into more subspecialty clinics and into primary care? And if yes, how? |
| • How do we improve asthma control with home monitoring tools like remote spirometry? |
| • Which populations need lung structure screening, what type of screen is optimal, and how do we change treatment based on imaging findings? |
| • Which public health measures will improve lung structure at birth, promote healthy lung growth, and limit lung damage in the general population? |
| • What strategies can support equitable representation in research for minoritized and rural populations? |
| • Once identified, how to implement screening procedures into already busy pediatric health care delivery models and clinics? |
Summary of Meeting
Lifelong Pulmonary Health Starts in Childhood
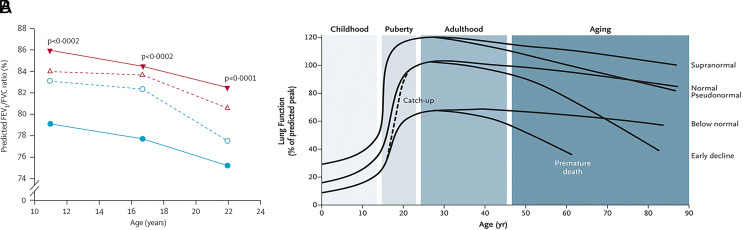
Birth cohort studies have materially added to our understanding of the development of lung function and the factors associated with both lung dysfunction and the progression to clinical disease, predominantly asthma. Low lung function at birth with an obstructive pattern precedes and predicts an increased risk of wheezing illness and asthma from childhood through the fourth decade of life.2,3 Furthermore, lung function tracks from childhood through adulthood with about 10% of individuals demonstrating lower trajectories, putting them at increased risk for chronic obstructive pulmonary disease (COPD) in later life (Fig 2).1,4–6 Persistent or recurrent wheezing in association with viral infection is associated with a loss of lung function by early school age, establishing a deficit that persists to adulthood.7 Recent evidence suggests poor growth in utero may lead to a restrictive pattern of lung function development characterized by spirometry as low forced vital capacity with a normal ratio of forced expiratory volume in 1 second/forced vital capacity, termed preserved ratio, impaired spirometry (PRISm).8 The PRISm pattern is also associated with later nonrespiratory comorbidities, including cardiovascular diseases, diabetes, metabolic syndrome, and all-cause mortality in adult life. Premature birth is associated with longstanding lung function deficits, which are more severe in those with bronchopulmonary dysplasia9 and likely increase risk for COPD in adulthood.10
FIGURE 2.
Lung function trajectories are established in childhood. (A) Lung function at birth is highly influential to airways obstruction later in life. (Image from Stern DA, Morgan WJ, Wright AL, Guerra S, Martinez FD. Lancet. 2007;370:758–764). (B) Discrete lung function trajectories from early childhood through adult life. (Image from Agustí A, Hogg JC. N Engl J Med. 2019;381:1248–1256).
Because neonatal lung function predicts lung function in the adult, we need to better understand the mechanisms determining lung function and structure at birth and if deleterious mechanisms are modifiable throughout life. In other words, what are the environmental, genetic, metabolic, and immune (EGMI) mechanisms that establish the trajectory that the lungs will follow through life? Although 40% of the lung function deficit seen in children with asthma is present at birth, 60% develops from birth to school age,11 compelling us to understand the biology underlying the loss of lung function and whether this can be ameliorated. Although recurrent exacerbations are associated with loss of lung function, inhaled steroids, the mainstay of asthma care, has no impact on long-term outcomes, either clinically12 or physiologically.13,14 It is important to elucidate the underlying EGMI mechanisms associated with the restricted growth phenotype (poor growth and PRISm) and why this phenotype is associated with the nonrespiratory comorbidities seen in this population. With the increase in nicotine use because of vaping, mitigation strategies such as vitamin C, which may attenuate the effect of nicotine, need to be evaluated, as do effective strategies for reducing vaping in adolescents15,16 and second-hand smoke in children living with smokers. Although improved prenatal care and a reduction in premature birth would be the most effective way of optimizing lung development broadly, there is still a need to understand the EGMI mechanisms influencing lung development in premature infants.17
Although there are several ongoing birth cohort studies, the risk factors influencing progressive lung development (ie, novel infections and new exposures) and our ability to noninvasively evaluate EGMI mechanisms remains a research priority. As a result, a strategy to develop new, large birth cohorts is needed. It can take 4 to 6 decades to fully understand lung disease phenotypes and the associated EGMI risk factors. A wise strategy would be to “plant” a new cohort every decade or so to “harvest” the relevant information a half a century later. There is an urgent need for a large (n = 5000), multicenter long-term birth cohort with infant lung function evaluation that characterizes antenatal and postnatal factors with biomarkers and molecular correlates to elucidate EGMI mechanisms. Evaluations should include EGMI studies with pre- and postnatal environmental evaluations, maternal risk factors, studies of the gut and respiratory microbiome, and transcriptome (ie, RNA transcripts) from the respiratory tract and peripheral immune cells as well as endocrine and metabolomics profiling. Characterization of viral and bacterial respiratory infection and immune responses should be evaluated in relation to respiratory morbidity outcomes. A similar cohort evaluating the impact of not only prematurity but also birth history should be developed as should studies evaluating COPD risk in bronchopulmonary dysplasia (BPD) survivors.
Impact of the Environment on Child Lung Health
It is widely recognized that environmental exposures to indoor and outdoor air pollutants can contribute to poor lung function and growth in children (Table 2). In low-income countries, biomass fuels used for household activities are the primary pollutant source and have been linked to childhood respiratory infection and COPD in adults.18–20 In both low- and high-income countries, ambient and household air pollutants are also prominently associated with poor lung function in childhood.21–24 Because children spend the majority of their time in an indoor home and school environment, indoor pollutant exposures, many of which are entrained from the outdoor air, are of particular concern. The effect of specific pollutants on lung function growth throughout childhood (prenatal through young adulthood) have primarily identified particulate matter, gaseous air pollutants, and personal exposure to tobacco smoke as major contributors.25 Emerging research suggests that additional indoor exposures to endocrine disrupting compounds (EDCs) such as those present in personal care products and other consumer goods, including phthalates and bisphenol A, may play a role in pediatric lung health.26 EDCs may serve as potential modulators of immune system homeostasis and allergic response27 and exert sex-specific health effects.28 Clinical trials involving multifaceted interventions in the home have consistently demonstrated improvements in symptom and health care utilization outcomes,29–35 but few report lung function improvement. These trials have been limited in the range of air pollutants addressed and the scope of intervention.36,37 The NIH-funded Environmental Influences on Child Health Outcomes project has created a large multi-institutional pediatric cohort focused on environmental exposures and their effect on pre-, peri-, and postnatal outcomes, but lacks a focus on lung growth and lung growth trajectories and is relatively limited in measurements of personal environment exposures.
TABLE 2.
Examples of Environmental Contaminants Associated with Respiratory Healtha
| Environmental Contaminant | Sources | Key Recognized or Possible Respiratory Health Effect |
|---|---|---|
| Particulate matter (PM) | • PM is a mixture of solid and/or liquid suspended air particles • Human sources include traffic, road dust, industrial sources (combustion of fossil fuels, metallurgy, ceramics, and others), domestic fuel combustion, and other human activities74 • Natural sources include wildfires, soil dust, and sea salt |
• Associated with all-cause and respiratory-related mortality75; lowered life expectancy76 • Asthma symptoms and exacerbation77 • Coughing, wheezing, and breathlessness41,78 • Impaired lung development in children23,25 • Impaired lung function in adults79 |
| Ozone (O3) | • Formed as a product of chemical reactions between sunlight, nitrogen oxides (NOx), and volatile organic compounds (VOCs) • May be emitted from various sources, including traffic, power plants, refineries, chemical plants, and other sources80 |
• Decreased lung function and lung function growth81 • Asthma symptoms and exacerbation82 • Allergic responses with coexposure to allergens37 |
| Nitrogen dioxide (NO2) | • Formed in high-temperature combustion processes such as power plants, traffic, and off-road vehicles83 | • Decreased lung function21,84–86 • Asthma exacerbations82 |
| Sulfur dioxide (SO2) | • May arise from combustion of sulfur-containing fuels (such as coal) in power plants and other industrial processes, metal extraction, and heavy vehicles87 • May also arise from natural sources such as volcanic eruptions |
• Eye and upper airway irritation • Alterations to lung function88 • Asthma exacerbations82 |
| Traffic-related air pollution (TRAP) | • Combustion of diesel and gasoline in motor vehicles • Roadways, especially those with high traffic density can be significant sources of TRAP |
• Decreased lung function21,25,84 • Asthma symptoms and exacerbations • Respiratory infections89 |
| Environmental tobacco smoke | • Smoking (cigarettes and other tobacco related products) • Second-hand smoke • Vaping/electronic cigarettes |
• Lower respiratory illnesses in infants and children, including asthma, respiratory infections90 • Decreased lung growth in children91 • Impaired lung function91 • Asthma, asthma exacerbations, severity92,93 |
| Plasticizers (eg, phthalates)b | • Present in many consumer products (eg, building materials such as polyvinyl chloride flooring, food packaging, personal care products such as hair and skin care products, toys, medications, medical tubing) • Ingestion of contaminated foods/beverages is thought to be the primary route of exposure, but inhalation and dermal absorption also plausible • Found in air, dust, food |
• Asthma/allergic symptoms and exacerbations, asthma severity46,94 • Rhinoconjunctivitis, atopic dermatitis95,96 • Airway inflammation95 |
| Formaldehyde | • Smoke from cigarettes and other tobacco products, gas stoves, and open fireplaces • Select manufactured wood products such as cabinets, furniture, plywood, particleboard, and laminate flooring • Permanent press fabrics such as those used for curtains/drapes or on furniture • Household products such as glues, paints, caulks, pesticides, cosmetics/personal care products, and detergents |
• Irritation of the nose, eyes, and throat97 • Headache, runny nose, nausea, and difficulty breathing/wheezing • Asthma exacerbations and other respiratory symptoms98,99 |
| Radon (Rn)b | • Product of the natural radioactive decay of uranium that has further decayed to radium found in soil and rocks100,101 | • Lung cancer risk102 • Possible association with chronic obstructive pulmonary disease (COPD)103 and COPD mortality104 • Emerging evidence of possible risk of airway inflammation in childhood asthma |
This list is not meant to be exhaustive and includes contaminants for which there is sufficient or suggestive/emerging evidence of adverse effects on lung health from human and animal studies.
Although findings from human studies are not conclusive at this time, some studies suggest that select exposures could impact pediatric respiratory health.
Our ability to assess the totality of environmental exposures among individuals through exposure modeling and novel methods is rapidly evolving.38–40 Some allergen coexposure studies have found amplified respiratory outcomes with exposure mixtures, but mechanistic data to examine other adjuvants, microbiome, and tissue-level pathobiology41 induced by exposures remain poorly characterized.42,43 Moreover, noninhaled routes of exposure, such as ingested or transdermal exposure to EDCs,44 may also play a role in lung health. Personal characteristics, such as obesity, genetic predisposition, or chronic conditions and comorbidities, may identify high-risk populations of children. Further data on susceptibility factors and the spatiotemporal relationships between threshold, duration, and route of exposure, host characteristics, including developmental stage during exposure, and respiratory outcomes require further study. Furthermore, lack of long-term intervention studies on pollutant mitigation impairs our understanding of potential long-term health benefits on lung growth and function. Aside from tobacco cessation efforts, few practical reduction strategies have entered clinical pediatric practice.
Social disadvantage that places historically underrepresented and understudied populations and impoverished families at high risk for poor respiratory health45 is inseparable from social determinants of health, including environmental risks. Poor and urban communities have higher levels of inhalable pollutants because of industry and traffic congestion and greater risk of dietary insufficiency and exposures to chemicals in consumer products, such as phthalates, because of “food deserts,” areas that lack affordable or good-quality fresh food but plenty of packaged and processed food items.46 Rural populations, particularly those of American indigenous populations, have high rates of indoor pollutants from wood smoke and coal combustion for home heat, which contribute to higher rates of respiratory disease, yet they remain highly understudied in public health research.47 Psychosocial distress in parents and children, which may be related to neighborhood safety, are significant risk factors for the development of wheeze, asthma, and poor lung function.48–51 Alterations in the neurohumoral development, hypothalamic pituitary axis pathways, and glucocorticoid sensitivity through epigenetic programming may lead to these clinically proven adverse outcomes in children of distressed parents or those who suffer early childhood stress.52 It is crucial to ensure that studies assess social determinants of health and include representation from historically underrepresented and understudied populations, especially considering that many environmental exposure and health disparities result from longstanding societal and structural racism.
Measuring Respiratory Function in Children
Asthma is the most common chronic respiratory condition managed in the pediatric primary care setting, impacting more than 6 million U.S. children.53 There are 3 ways to assess asthma severity and control in this setting: symptom frequency, exacerbation history, and pulmonary function as measured by spirometry. Several studies of children with asthma have shown that the severity classification level increases in up to 1 of every 3 children when lung function is considered in addition to symptom frequency.54 Children with a history of minimal symptoms but impaired lung function would likely be untreated with a controller medication without the benefit of spirometry testing.
Primary care providers manage the majority of children with asthma. Without proper training and feedback, less than half of spirometry tests performed in the primary care setting are clinically useful,55 creating a risk for misdiagnosis or unnecessary specialty referral. The quality of primary care spirometry testing can be improved with proper training and feedback, whether in-person or virtual,56 but requires financial resources and dedicated personnel to effectively implement in clinical practice. COVID-19 has created an additional barrier to conducting spirometry in the primary care setting because of reluctance to perform an aerosol-generating procedure. Home spirometry is proving to be feasible and acceptable by patients, investigators, and clinicians. The decrease in price of these devices, which use a Bluetooth connection to a smart phone, creates the potential for home spirometry testing among children with chronic respiratory illnesses such as asthma and cystic fibrosis. Its immediate availability also presents an opportunity for ongoing monitoring and more refined management, as well as the potential for exacerbation tracking. Lung function testing among preschool-aged children presents further challenges.
There are a number of gaps that need to be addressed before considering large-scale implementation of home spirometry. For example, we need feasibility and validation studies to assess the accuracy and reproducibility of home spirometry relative to office spirometry. Training and feedback procedures to optimize measurement quality need to be established and validated, as well as strategies to maintain engagement and adherence to monitoring over time. Qualitative research is needed to understand patient experience and barriers to use across wide ranges of patients (age, geography, socioeconomic status, race/ethnicity, language). We need to address the pragmatic question of whether home spirometry improves access to lung function testing, being mindful that the need for a smart phone may contribute to inequitable care, and whether it improves health outcomes in asthma and other chronic diseases. For practical implementation, how is such work financially sustained and integrated into the electronic health records and payment systems?
Although home spirometry has been shown to be a small-scale solution for home measurement among study cohorts, it has not yet diffused into primary care (or specialty offices) for management of chronic lung disease. Tests requiring less cooperation, time, and technician training, such as oscillometry, are limited to specialty settings and research and will require the same assessments of feasibility, implementation, cost-effectiveness, and broad access as spirometry to be considered more broadly.
Assessing Lung Structure in Children
Lung structure is an important component of pulmonary health but is not routinely assessed, defined, or treated. Evaluation of the structure of the respiratory system includes the lung, airway, vasculature, and chest wall. In some children, structural lung and airway damage can be extensive before symptoms are obvious,57,58 though, in many diseases, the extent of injured lung correlates with symptoms, lung function, and mortality.59–61 Children born preterm have less complicated lung architecture,62 and chest radiograph alone can predict mortality in infants born prematurely.63 Additionally, sex, race, and certain cooccurring diagnoses contribute to a further heightened risk of structural lung damage.64–66 The most common ways to assess lung structure are chest radiograph, chest computed tomography, and physical examination; however, these may miss early subtle disease. Deep learning methods can improve our ability to assess early disease using chest radiograph or chest computed tomography images.67,68 Other modalities to assess lung and airway structure, including lung magnetic resonance imaging and lung ultrasound, have proven to be sensitive outcomes in clinical research, and functional magnetic resonance imaging can simultaneously link structural imaging with lung function.69,70
To optimize respiratory health, we must consider lung structure at the time of birth, healthy lung growth during childhood, and limiting lung damage. Understanding whom to screen, when to screen, and how to screen for structural lung disease is important to change long-term outcomes. Increasing rates of premature birth lead not only to heterogeneous lung parenchymal disease seen in BPD, but can also be associated with cerebral palsy, neuromuscular scoliosis, and less effective airway clearance. Even after identifying heterogeneous lung disease in BPD, there is a gap in our knowledge of how to change treatment based on imaging findings. Furthermore, we need to identify effective and feasible public measures to improve lung structure at birth, promote healthy lung growth, and limit lung damage in the general population. To meet this goal, we need to identify in which populations lung structure screening will be most useful, and when lung damage is found, when to refer to specialists and for which treatments. Imaging techniques need to continue to evolve to improve consistency, limit noise, improve sensitivity of assessments, and identify novel methods effective for clinical use.
Initiatives to improve lung structure need to focus broadly on the population, including decreasing in utero exposures for all and especially vulnerable children including those from minoritized populations. To reach the population, care cannot only occur for those children referred to pulmonary subspecialty offices, but also to those seen in general pediatric offices, schools, and community centers. Critical steps include identifying standardized outcomes that assess and quantify lung structure, from existing sources such as chest radiographs, or from other novel techniques. Future goals include developing and implementing screening methods that can be deployed in schools or community centers, and effective treatment plans for pediatricians when lung structure abnormalities are identified.
Discussion
Lifelong respiratory health is rooted in the structural and functional development of the respiratory system in childhood. Exposures and interventions antenatally through childhood can influence lung development into young adulthood, the life stage with the highest achievable lung function. Early respiratory health sets the stage for adult lung function trajectories, risk of developing COPD, and potentially influencing other organ system health and all-cause mortality. To understand how to promote lung health in children, it is critical to have accurate and precise measures of structural and functional lung development that track throughout life stages. From this foundation, evaluation of environmental, genetic, metabolic, and immune mechanisms involved in healthy lung development can be investigated. These goals require the involvement of general pediatricians, pediatric subspecialists, and researchers to design and implement studies that are broadly generalizable and applicable to otherwise healthy and chronic disease populations.
Build Longitudinal Cohorts
Longitudinal cohorts enrolled at birth or early childhood have shed important light into the risk factors for developing chronic lung diseases such as asthma, cystic fibrosis, bronchopulmonary dysplasia, and postprematurity respiratory disease. However, individual cohort studies are limited in the depth and breadth of investigation by focusing on specific at-risk populations, lack of geographic, racial, and sociodemographic diversity, and lack of resources to collect extensive biologic samples and personalized exposure assessments with repeated sampling. While collaborations among multiple longitudinal studies71 have been successful in broadening the scientific achievements of individual studies, gaps in data harmonization and assessment standardization remain. Lung structure assessment, by imaging, biopsy, or any other means, is largely absent because of, in part, to radiation exposure and cost or complexity but also lack of standardization of techniques and interpretation.
Evaluation of respiratory outcomes, maximal lung growth and lung function throughout childhood by harnessing both observational and interventional trials with adaptive study designs may optimize power by bridging the gap between observational and intervention trials, with new interventions added as science progresses. Large cohort studies could contain high-risk populations with focused interventional trials nested within a larger general population cohort, allowing specific questions to be tailored to stratified groups while collecting comparable information among all participants. Assessments should include radiologic studies, a variety of complementary lung function tests, biobanking of specimens, and environmental exposure data, each of which is repeated frequently from birth to young adulthood to develop a detailed understanding of normal and aberrant trajectories of lung development and the inflection points at which precise interventions may be targeted.
Foster exploratory and innovative research
A fundamental challenge in pediatric respiratory research is the ability to reliably assess lung structure and lung function from infancy through adulthood with tests that are sensitive to incremental changes. Several pulmonary function tests have been used in studies of infants and preschool-aged children, including infant pulmonary function testing, specific airways resistance, the interrupter resistance technique, forced oscillometry, and multiple breath washout.72 In older children and adults, spirometry remains the gold standard, but may not be the most sensitive to changes in small-airway function. Further research to identify optimal means of assessing pulmonary function in early childhood and longitudinal studies to track lung function across all stages of development is greatly needed, as is the functional translation of lung function test results to patient-centered outcomes, such as physical function or exercise tolerance. Lung function tests for large studies or clinical practice must be simple to use, nonthreatening to children, brief to perform, have established normative data, and be easily accessible for patients, providers, and researchers. Developing screening tests for healthy and chronic disease populations to track lung development is an unmet need.
Structural assessment of lung development and disease is similarly challenging. The risk of radiation exposure or the need for sedation in young age groups are limitations. Lack of standardized techniques, unbiased methods of interpretation, and data capture harmonization across devices and sites impairs broad-based research applications. Developing repositories that can store images will improve access to shared data among broad networks of investigators and clinicians.
To move beyond the paradigm of disease-state research to one of optimizing lung health in all children, innovative research to characterize lung development and functional traits in representative groups rather than confined to clinical diagnoses will require novel techniques. Creative solutions that incorporate objective measures of lung structure and function, patient-reported outcomes, the electronic health record, remote health monitoring data, personal environmental sampling, and sophisticated analytical techniques, such as machine learning and network analysis, will be necessary.
Build Cross-Disciplinary Collaboration and Training
Integrating primary and specialty care providers, research faculty, patients and families, and community stakeholders into cross-disciplinary teams is vital to achieving research objectives in lung structure and function. Each member contributes a unique perspective in identifying the important questions, valued outcomes, and impact of the research. Building these cross-disciplinary collaborations in the early stages of project development will instill trust and ensure that the aims, methods, and outcomes of investigations are calibrated to the communities for which the research aims to serve. Moreover, it challenges the research community to answer the most impactful questions and may facilitate dissemination of knowledge and implementation of key interventions. Establishment of community-specialty clinical partnerships may also enhance early diagnosis of abnormal lung development by engaging primary care providers to be aware of early phenotypic information that would warrant further testing.
Implementing Change in Pediatric Practice
An immense challenge beyond scientific discovery is how to implement evidence-based techniques for assessing lung structure and function into clinical pediatric practice. Achieving broad range research at a population level that involves collaboration between specialists and primary care providers, reaches diverse populations with varying access to care, and produces unbiased generalizable knowledge is an ambitious undertaking. Pediatricians and specialists will need to establish cost-effective ways for early detection of lung disease that take into consideration the broader priorities of pediatric health care delivery and competing interests of the pediatric providers and the population they serve. Answering questions about which patients to screen for lung disease, where screening is performed (home, pediatrician’s office, school, or community setting), what to do with that information, including systems of collection, interpretation, timely referral to subspecialists, and reimbursement, will require engaging key stakeholders through cross-disciplinary collaboration at the outset. Input from pediatricians, the health care industry, and public policymakers is valuable to conduct research that can be used in clinical practice, readily translated to policy and cost-effective for insurers. Considering how the anticipated knowledge generated from research can be successfully implemented from the start will promote efficient translation of research to clinical care.
Address Diversity and Equity
Building clinical and research programs to meet the diverse needs of all children to ensure equity in research and clinical care is fundamentally important. Research should be informed by the needs and priorities of the communities for which it is intended to serve, and these may vary by the population. Along with clinical care, research should strive for inclusivity and equity among participants, staff, and faculty to ensure that research products are impactful to all children. Failing to study health and disease in cohorts reflective of the population widens health disparities. In addition to community engagement in research, investigations of lung function and structural development in children may begin to address these issues by considering race and ethnicity as social constructs rather than biologic variables. High-risk, minority, and rural populations present unique challenges for enrollment and retention in clinical research studies.73 The widespread adoption of remote consenting to clinical research, availability of remote monitoring, sample collection, and spirometry, along with virtual research and health care visits provides the opportunity to overcome geographic and transportation barriers to research participation for rural and poor populations. Further work to validate remote assessment methodology is still needed, but early studies suggest that remote lung function testing provides accurate data for research purposes.
Conclusions
Lifelong lung function, which is highly associated with morbidity and mortality, is rooted in childhood lung development and influenced by prenatal and early childhood exposures and the commensurate biologic response. A detailed understanding of lung function and structure among healthy populations and those with chronic respiratory diseases is essential to identifying the optimal timing and interventions to promote healthy lung development. Recent advances in lung function and structure assessment, along with novel and sophisticated techniques for sampling environmental exposures, have enabled exciting discoveries, but significant knowledge gaps and challenges remain. Breaking through the silos of academic research to promote scientific discovery in diverse populations through teams of primary care providers, specialists, community stakeholders, families, and patients will provide the optimal environment for impactful scientific discovery.
Glossary
- BPD
bronchopulmonary dysplasia
- COPD
chronic obstructive pulmonary disease
- EDC
endocrine disrupting compounds
- EGMI
environmental, genetic, metabolic, and immune
- NIH
National Institutes of Health
- PRISm
preserved ratio, impaired spirometry pattern
Footnotes
Dr DeBoer organized the structure/function component of the National Institutes of Health (NIH) meeting and reviewed and revised the manuscript; Dr Morgan organized the structure/function component of the NIH meeting and reviewed and revised the manuscript; Drs Quiros-Alcala, Rosenfeld, and Stout participated in the NIH meeting and reviewed and revised the manuscript; Dr Davis organized the Defining and Promoting Pediatric Pulmonary Health (DAP3H) meeting and reviewed and revised the manuscript; Dr Gaffin participated in the NIH meeting and drafted the initial manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: The virtual workshop upon which this report is based was funded by the US National Heart, Lung, and Blood Institute (NHLBI). The NHLBI approved the workshop concept and provided administrative support for the workshop. The views expressed in this article are those of the authors and do not necessarily represent those of the National Institutes of Health or the U.S. Department of Health and Human Services.
CONFLICT OF INTEREST DISCLOSURES: Dr DeBoer is a founder and consultant of EvoEndoscopy and has intellectual property related to endoscopy. Dr Stout is a consultant for Regeneron and Public Health Seattle-King County. Dr Gaffin receives research support from the National Institutes of Health (NIH), Boston Children’s Hospital, and Vertex pharmaceuticals, and consulting fees from Syneos health and AiCME. Dr Davis reports research funding from the NIH, Cystic Fibrosis Foundation, and ReCode therapeutics, and consulting fees from a Vertex Pharmaceuticals advisory board. Dr Davis also serves on the PCD Foundation Scientific Advisory Board. Drs Morgan and Rosenfeld have indicated they have no potential conflicts of to disclose.
References
- 1. Martinez FD. Early-life origins of chronic obstructive pulmonary disease. N Engl J Med. 2016;375(9):871–878 [DOI] [PubMed] [Google Scholar]
- 2. Lange P, Celli B, Agustí A, et al. Lung-function trajectories leading to chronic obstructive pulmonary disease. N Engl J Med. 2015;373(2):111–122 [DOI] [PubMed] [Google Scholar]
- 3. Morgan WJ, Stern DA, Sherrill DL, et al. Outcome of asthma and wheezing in the first 6 years of life: follow-up through adolescence. Am J Respir Crit Care Med. 2005;172(10):1253–1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Berry CE, Billheimer D, Jenkins IC, et al. A distinct low lung function trajectory from childhood to the fourth decade of life. Am J Respir Crit Care Med. 2016;194(5):607–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Agustí A, Hogg JC. Update on the pathogenesis of chronic obstructive pulmonary disease. N Engl J Med. 2019;381(13):1248–1256 [DOI] [PubMed] [Google Scholar]
- 6. Bui DS, Lodge CJ, Perret JL, et al. Trajectories of asthma and allergies from 7 years to 53 years and associations with lung function and extrapulmonary comorbidity profiles: a prospective cohort study. Lancet Respir Med. 2021;9(4):387–396 [DOI] [PubMed] [Google Scholar]
- 7. Guilbert TW, Singh AM, Danov Z, et al. Decreased lung function after preschool wheezing rhinovirus illnesses in children at risk to develop asthma. J Allergy Clin Immunol. 2023;151(1):138–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Voraphani N, Stern DA, Zhai J, et al. The role of growth and nutrition in the early origins of spirometric restriction in adult life: a longitudinal, multicohort, population-based study. Lancet Respir Med. 2022;10(1):59–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Simpson SJ, Logie KM, O’Dea CA, et al. Altered lung structure and function in mid-childhood survivors of very preterm birth. Thorax. 2017;72(8):702–711 [DOI] [PubMed] [Google Scholar]
- 10. Islam JY, Keller RL, Aschner JL, Hartert TV, Moore PE. Understanding the short- and long-term respiratory outcomes of prematurity and bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2015;192(2):134–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bisgaard H, Jensen SM, Bønnelykke K. Interaction between asthma and lung function growth in early life. Am J Respir Crit Care Med. 2012;185(11):1183–1189 [DOI] [PubMed] [Google Scholar]
- 12. Guilbert TW, Morgan WJ, Zeiger RS, et al. Long-term inhaled corticosteroids in preschool children at high risk for asthma. N Engl J Med. 2006;354(19):1985–1997 [DOI] [PubMed] [Google Scholar]
- 13. McGeachie MJ, Yates KP, Zhou X, et al. Patterns of growth and decline in lung function in persistent childhood asthma. N Engl J Med. 2016;374(19):1842–1852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gaffin JM, Petty CR, Sorkness CA, et al. Determinants of lung function across childhood in the Severe Asthma Research Program (SARP) 3. J Allergy Clin Immunol. 2023;151(1):138–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McEvoy CT, Shorey-Kendrick LE, Milner K, et al. Oral vitamin C (500 mg/d) to pregnant smokers improves infant airway function at 3 months (VCSIP). A randomized trial. Am J Respir Crit Care Med. 2019;199(9):1139–1147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McEvoy CT, Schilling D, Clay N, et al. Vitamin C supplementation for pregnant smoking women and pulmonary function in their newborn infants: a randomized clinical trial. JAMA. 2014;311(20):2074–2082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McEvoy CT, Jain L, Schmidt B, Abman S, Bancalari E, Aschner JL. Bronchopulmonary dysplasia: NHLBI Workshop on the Primary Prevention of Chronic Lung Diseases. Ann Am Thorac Soc. 2014;11(suppl 3):S146–S153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lim S, Bassey E, Bos B, et al. Comparing human exposure to fine particulate matter in low and high-income countries: a systematic review of studies measuring personal PM2.5 exposure. Sci Total Environ. 2022;833:155207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Po JY, FitzGerald JM, Carlsten C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax. 2011;66(3):232–239 [DOI] [PubMed] [Google Scholar]
- 20. Balmes JR. Household air pollution from domestic combustion of solid fuels and health. J Allergy Clin Immunol. 2019;143(6):1979–1987 [DOI] [PubMed] [Google Scholar]
- 21. Schultz ES, Hallberg J, Bellander T, et al. Early-life exposure to traffic-related air pollution and lung function in adolescence. Am J Respir Crit Care Med. 2016;193(2):171–177 [DOI] [PubMed] [Google Scholar]
- 22. Gauderman WJ, Gilliland GF, Vora H, et al. Association between air pollution and lung function growth in southern California children: results from a second cohort. Am J Respir Crit Care Med. 2002;166(1):76–84 [DOI] [PubMed] [Google Scholar]
- 23. Gauderman WJ, Avol E, Gilliland F, et al. The effect of air pollution on lung development from 10 to 18 years of age. N Engl J Med. 2004;351(11):1057–1067 [DOI] [PubMed] [Google Scholar]
- 24. Adamkiewicz G, Liddie J, Gaffin JM. The respiratory risks of ambient/outdoor air pollution. Clin Chest Med. 2020;41(4):809–824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rice MB, Rifas-Shiman SL, Litonjua AA, et al. Lifetime exposure to ambient pollution and lung function in children. Am J Respir Crit Care Med. 2016;193(8):881–888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Quirós-Alcalá L, Hansel NN, McCormack M, et al. Exposure to bisphenols and asthma morbidity among low-income urban children with asthma. J Allergy Clin Immunol. 2021;147(2):577–586.e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chalubinski M, Kowalski ML. Endocrine disrupters--potential modulators of the immune system and allergic response. Allergy. 2006;61(11):1326–1335 [DOI] [PubMed] [Google Scholar]
- 28. Corsini E, Ruffo F, Racchi M. Steroid hormones, endocrine disrupting compounds and immunotoxicology. Curr Opin Toxicol. 2018;10:69–73 [Google Scholar]
- 29. Morgan WJ, Crain EF, Gruchalla RS, et al. ; Inner-City Asthma Study Group . Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351(11):1068–1080 [DOI] [PubMed] [Google Scholar]
- 30. Krieger JK, Takaro TK, Allen C, et al. The Seattle-King County healthy homes project: implementation of a comprehensive approach to improving indoor environmental quality for low-income children with asthma. Environ Health Perspect. 2002;110(suppl 2):311–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Krieger J, Takaro TK, Song L, Beaudet N, Edwards K. A randomized controlled trial of asthma self-management support comparing clinic-based nurses and in-home community health workers: the Seattle-King County Healthy Homes II Project. Arch Pediatr Adolesc Med. 2009;163(2):141–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Takaro TK, Krieger J, Song L, Sharify D, Beaudet N. The Breathe-Easy Home: the impact of asthma-friendly home construction on clinical outcomes and trigger exposure. Am J Public Health. 2011;101(1):55–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Campbell JD, Brooks M, Hosokawa P, Robinson J, Song L, Krieger J. Community health worker home visits for Medicaid-enrolled children with asthma: effects on asthma outcomes and costs. Am J Public Health. 2015;105(11):2366–2372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shapiro GG, Stout JW. Childhood asthma in the United States: urban issues. Pediatr Pulmonol. 2002;33(1):47–55 [DOI] [PubMed] [Google Scholar]
- 35. Shreeve K, Woods ER, Sommer SJ, et al. Community health workers in home visits and asthma outcomes. Pediatrics. 2021;147(4):e2020011817. [DOI] [PubMed] [Google Scholar]
- 36. Phipatanakul W, Koutrakis P, Coull BA, et al. ; School Inner-City Asthma Intervention study team . Effect of school integrated pest management or classroom air filter purifiers on asthma symptoms in students with active asthma: a randomized clinical trial. JAMA. 2021;326(9):839–850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Pilotto LS, Nitschke M, Smith BJ, et al. Randomized controlled trial of unflued gas heater replacement on respiratory health of asthmatic schoolchildren. Int J Epidemiol. 2004;33(1):208–214 [DOI] [PubMed] [Google Scholar]
- 38. Agache I, Miller R, Gern JE, et al. Emerging concepts and challenges in implementing the exposome paradigm in allergic diseases and asthma: a Practall document. Allergy. 2019;74(3):449–463 [DOI] [PubMed] [Google Scholar]
- 39. O’Connell SG, Kincl LD, Anderson KA. Silicone wristbands as personal passive samplers. Environ Sci Technol. 2014;48(6):3327–3335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nyhan MM, Kloog I, Britter R, Ratti C, Koutrakis P. Quantifying population exposure to air pollution using individual mobility patterns inferred from mobile phone data. J Expo Sci Environ Epidemiol. 2019;29(2):238–247 [DOI] [PubMed] [Google Scholar]
- 41. Robinson RK, Birrell MA, Adcock JJ, et al. Mechanistic link between diesel exhaust particles and respiratory reflexes. J Allergy Clin Immunol. 2018;141(3):1074–1084.e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wu W, Jin Y, Carlsten C. Inflammatory health effects of indoor and outdoor particulate matter. J Allergy Clin Immunol. 2018;141(3):833–844 [DOI] [PubMed] [Google Scholar]
- 43. Rouadi PW, Idriss SA, Naclerio RM, et al. Immunopathological features of air pollution and its impact on inflammatory airway diseases (IAD). World Allergy Organ J. 2020;13(10):100467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bølling AK, Sripada K, Becher R, Bekö G. Phthalate exposure and allergic diseases: Review of epidemiological and experimental evidence. Environ Int. 2020;139:105706. [DOI] [PubMed] [Google Scholar]
- 45. Kopel LS, Phipatanakul W, Gaffin JM. Social disadvantage and asthma control in children. Paediatr Respir Rev. 2014;15(3):256–262, quiz 262–263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Fandiño-Del-Rio M, Matsui EC, Peng RD, Meeker JD, Quirós-Alcalá L. Phthalate biomarkers and associations with respiratory symptoms and healthcare utilization among low-income urban children with asthma. Environ Res. 2022;212(Pt B):113239. [DOI] [PubMed] [Google Scholar]
- 47. Lowe AA, Bender B, Liu AH, et al. Environmental concerns for children with asthma on the Navajo Nation. Ann Am Thorac Soc. 2018;15(6):745–753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Rosa MJ, Lee AG, Wright RJ. Evidence establishing a link between prenatal and early-life stress and asthma development. Curr Opin Allergy Clin Immunol. 2018;18(2):148–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. van Meel ER, Saharan G, Jaddoe VW, et al. Parental psychological distress during pregnancy and the risk of childhood lower lung function and asthma: a population-based prospective cohort study. Thorax. 2020;75(12):1074–1081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bandoli G, Ghosh JK, von Ehrenstein O, Ritz B. Psychosocial stressors and lung function in youth ages 10–17: an examination by stressor, age and gender. J Public Health (Oxf). 2017;39(2):297–303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lee AG, Chiu YM, Rosa MJ, et al. Association of prenatal and early childhood stress with reduced lung function in 7-year-olds. Ann Allergy Asthma Immunol. 2017;119(2):153–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wright RJ. Perinatal stress and early life programming of lung structure and function. Biol Psychol. 2010;84(1):46–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Centers for Disease Control and Prevention . Asthma in children. Available at: https://www.cdc.gov/vitalsigns/childhood-asthma/index.html. Accessed January 31, 2023
- 54. Nair SJ, Daigle KL, DeCuir P, Lapin CD, Schramm CM. The influence of pulmonary function testing on the management of asthma in children. J Pediatr. 2005;147(6):797–801 [DOI] [PubMed] [Google Scholar]
- 55. Mangione-Smith R, Zhou C, Corwin MJ, Taylor JA, Rice F, Stout JW. Effectiveness of the Spirometry 360 Quality Improvement Program for improving asthma care: a cluster randomized trial. Acad Pediatr. 2017;17(8):855–862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Stout JW, Smith K, Zhou C, et al. Learning from a distance: effectiveness of online spirometry training in improving asthma care. Acad Pediatr. 2012;12(2):88–95 [DOI] [PubMed] [Google Scholar]
- 57. Ranganathan SC, Hall GL, Sly PD, Stick SM, Douglas TA; Australian Respiratory Early Surveillance Team for Cystic Fibrosis (AREST-CF) . Early lung disease in infants and preschool children with cystic fibrosis. What have we learned and what should we do about it? Am J Respir Crit Care Med. 2017;195(12):1567–1575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Broström EB, Thunqvist P, Adenfelt G, Borling E, Katz-Salamon M. Obstructive lung disease in children with mild to severe BPD. Respir Med. 2010;104(3):362–370 [DOI] [PubMed] [Google Scholar]
- 59. Moore OA, Goh N, Corte T, et al. Extent of disease on high-resolution computed tomography lung is a predictor of decline and mortality in systemic sclerosis-related interstitial lung disease. Rheumatology (Oxford). 2013;52(1):155–160 [DOI] [PubMed] [Google Scholar]
- 60. Humphries SM, Swigris JJ, Brown KK, et al. Quantitative high-resolution computed tomography fibrosis score: performance characteristics in idiopathic pulmonary fibrosis. Eur Respir J. 2018;52(3):1801384. [DOI] [PubMed] [Google Scholar]
- 61. Sanders DB, Li Z, Brody AS, Farrell PM. Chest computed tomography scores of severity are associated with future lung disease progression in children with cystic fibrosis. Am J Respir Crit Care Med. 2011;184(7):816–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Chang DV, Assaf SJ, Tiller CJ, Kisling JA, Tepper RS. Membrane and capillary components of lung diffusion in infants with bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2016;193(7):767–771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kim HR, Kim JY, Yun B, Lee B, Choi CW, Kim BI. Interstitial pneumonia pattern on day 7 chest radiograph predicts bronchopulmonary dysplasia in preterm infants. BMC Pediatr. 2017;17(1):125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bush D, Abman SH, Galambos C. Prominent intrapulmonary bronchopulmonary anastomoses and abnormal lung development in infants and children with Down syndrome. J Pediatr. 2017;180:156–162 [DOI] [PubMed] [Google Scholar]
- 65. Bhatt SP, Bodduluri S, Nakhmani A, et al. Sex differences in airways at chest CT: results from the COPDGene cohort. Radiology. 2022;305(3):699–708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Liu GY, Khan SS, Colangelo LA, et al. Comparing racial differences in emphysema prevalence among adults with normal spirometry: a secondary data analysis of the CARDIA Lung Study. Ann Intern Med. 2022;175(8):1118–1125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Mansoor A, Perez G, Nino G, Linguraru MG. Automatic tissue characterization of air trapping in chest radiographs using deep neural networks. Annu Int Conf IEEE Eng Med Biol Soc. 2016;2016:97–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Zucker EJ, Barnes ZA, Lungren MP, et al. Deep learning to automate Brasfield chest radiographic scoring for cystic fibrosis. J Cyst Fibros. 2020;19(1):131–138 [DOI] [PubMed] [Google Scholar]
- 69. Polverino F, Hysinger EB, Gupta N, et al. Lung MRI as a potential complementary diagnostic tool for early COPD. Am J Med. 2020;133(6):757–760 [DOI] [PubMed] [Google Scholar]
- 70. Loi B, Vigo G, Baraldi E, et al. Lung ultrasound to monitor extremely preterm infants and predict bronchopulmonary dysplasia. A multicenter longitudinal cohort study. Am J Respir Crit Care Med. 2021;203(11):1398–1409 [DOI] [PubMed] [Google Scholar]
- 71. Gern JE, Jackson DJ, Lemanske RF Jr, et al. The Children’s Respiratory and Environmental Workgroup (CREW) birth cohort consortium: design, methods, and study population. Respir Res. 2019;20(1):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Rosenfeld M, Allen J, Arets BH, et al. ; American Thoracic Society Assembly on Pediatrics Working Group on Infant and Preschool Lung Function Testing . An official American Thoracic Society workshop report: optimal lung function tests for monitoring cystic fibrosis, bronchopulmonary dysplasia, and recurrent wheezing in children less than 6 years of age. Ann Am Thorac Soc. 2013;10(2):S1–S11 [DOI] [PubMed] [Google Scholar]
- 73. Kramer CB, LeRoy L, Donahue S, et al. Enrolling African-American and Latino patients with asthma in comparative effectiveness research: Lessons learned from 8 patient-centered studies. J Allergy Clin Immunol. 2016;138(6):1600–1607 [DOI] [PubMed] [Google Scholar]
- 74. Karagulian F, Belis CA, Dora CFC, et al. Contributions to cities’ ambient particulate matter (PM): a systematic review of local source contributions at global level. Atmos Environ. 2015;120:475–483 [Google Scholar]
- 75. Liu C, Chen R, Sera F, et al. Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med. 2019;381(8):705–715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Bennett JE, Tamura-Wicks H, Parks RM, et al. Particulate matter air pollution and national and county life expectancy loss in the USA: a spatiotemporal analysis. PLoS Med. 2019;16(7):e1002856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lee J-Y, Leem J-H, Kim H-C, et al. Effects of traffic-related air pollution on susceptibility to infantile bronchiolitis and childhood asthma: a cohort study in Korea. J Asthma. 2018;55(3):223–230. [DOI] [PubMed] [Google Scholar]
- 78. Patel MM, Hoepner L, Garfinkel R, et al. Ambient metals, elemental carbon, and wheeze and cough in New York City children through 24 months of age. Am J Respir Crit Care Med. 2009;180(11):1107–1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Rice MB, Ljungman PL, Wilker EH, et al. Long-term exposure to traffic emissions and fine particulate matter and lung function decline in the Framingham heart study. Am J Respir Crit Care Med. 2015;191(6):656–664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. U.S. Environmental Protection Agency . Ground-level ozone basics. Available at: https://www.epa.gov/ground-level-ozone-pollution/ground-level-ozone-basics. Accessed June 28, 2023
- 81. Holm SM, Balmes JR. Systematic review of ozone effects on human lung function, 2013 through 2020. Chest. 2022;161(1):190–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Zheng XY, Orellano P, Lin HL, Jiang M, Guan WJ. Short-term exposure to ozone, nitrogen dioxide, and sulphur dioxide and emergency department visits and hospital admissions due to asthma: a systematic review and meta-analysis. Environ Int. 2021;150:106435. [DOI] [PubMed] [Google Scholar]
- 83. U.S. Environmental Protection Agency . Basic information about NO2. Available at: https://www.epa.gov/no2-pollution/basic-information-about-no2. Accessed June 28, 2023
- 84. Schultz ES, Gruzieva O, Bellander T, et al. Traffic-related air pollution and lung function in children at 8 years of age: a birth cohort study. Am J Respir Crit Care Med. 2012;186(12):1286–1291 [DOI] [PubMed] [Google Scholar]
- 85. Gaffin JM, Hauptman M, Petty CR, et al. Nitrogen dioxide exposure in school classrooms of inner-city children with asthma. J Allergy Clin Immunol. 2018;141(6):2249–2255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Gauderman WJ, Urman R, Avol E, et al. Association of improved air quality with lung development in children. N Engl J Med. 2015;372(10):905–913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. U.S. Environmental Protection Agency . Sulfur dioxide basics. Available at: https://www.epa.gov/so2-pollution/sulfur-dioxide-basics. Accessed June 28, 2023 [PubMed]
- 88. Rosser F, Forno E, Kurland KS, et al. Annual SO2 exposure, asthma, atopy, and lung function in Puerto Rican children. Pediatr Pulmonol. 2020;55(2):330–337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Rice MB, Rifas-Shiman SL, Oken E, et al. Exposure to traffic and early life respiratory infection: A cohort study. Pediatr Pulmonol. 2015;50(3):252–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Centers for Disease Control and Prevention . The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General, 1986. Available at: https://stacks.cdc.gov/view/cdc/20799. Accessed June 28, 2023 [PubMed]
- 91. Wang L, Pinkerton KE. Detrimental effects of tobacco smoke exposure during development on postnatal lung function and asthma. Birth Defects Res C Embryo Today. 2008;84(1):54–60 [DOI] [PubMed] [Google Scholar]
- 92. Ducharme FM, Zemek R, Chauhan BF, et al. ; DOORWAY research group of the Pediatric Emergency Research in Canada (PERC) network . Factors associated with failure of emergency department management in children with acute moderate or severe asthma: a prospective, multicentre, cohort study. Lancet Respir Med. 2016;4(12):990–998 [DOI] [PubMed] [Google Scholar]
- 93. Merianos AL, Dixon CA, Mahabee-Gittens EM. Secondhand smoke exposure, illness severity, and resource utilization in pediatric emergency department patients with respiratory illnesses. J Asthma. 2017;54(8):798–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Lee JY, Lee J, Huh DA, Moon KW. Association between environmental exposure to phthalates and allergic disorders in Korean children: Korean National Environmental Health Survey (KoNEHS) 2015-2017. Int J Hyg Environ Health. 2021;238:113857. [DOI] [PubMed] [Google Scholar]
- 95. Chang W-H, Herianto S, Lee C-C, Hung H, Chen H-L. The effects of phthalate ester exposure on human health: a review. Sci Total Environ. 2021;786:147371. [DOI] [PubMed] [Google Scholar]
- 96. Bornehag CG, Sundell J, Weschler CJ, et al. The association between asthma and allergic symptoms in children and phthalates in house dust: a nested case-control study. Environ Health Perspect. 2004;112(14):1393–1397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Agency for Toxic Substances and Disease Registry . ToxFAQs for formaldehyde. Available at: https://wwwn.cdc.gov/TSP/ToxFAQs/ToxFAQsDetails.aspx?faqid=219&toxid=39. Accessed August 16, 2022
- 98. McGwin G, Lienert J, Kennedy JI. Formaldehyde exposure and asthma in children: a systematic review. Environ Health Perspect. 2010;118(3):313–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Kanchongkittiphon W, Mendell MJ, Gaffin JM, Wang G, Phipatanakul W. Indoor environmental exposures and exacerbation of asthma: an update to the 2000 review by the Institute of Medicine. Environ Health Perspect. 2015;123(1):6–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Brill AB, Becker DV, Donahoe K, et al. ; SNM Committee on Radiobiological Effects of Ionizing Radiation . Radon update: facts concerning environmental radon: levels, mitigation strategies, dosimetry, effects and guidelines. J Nucl Med. 1994;35(2):368–385 [PubMed] [Google Scholar]
- 101. Nazaroff WW, Teichman K. Indoor radon. Environ Sci Technol. 2016;24(6):774–782 [Google Scholar]
- 102. Melloni BB. Lung cancer in never-smokers: radon exposure and environmental tobacco smoke. Eur Respir J. 2014;44(4):850–852 [DOI] [PubMed] [Google Scholar]
- 103. Conde-Sampayo A, Lorenzo-González M, Fernández-Villar A, Barros-Dios JM, Ruano-Ravina A. Exposure to residential radon and COPD: a systematic review. Int J Chron Obstruct Pulmon Dis. 2020;15:939–948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Turner MC, Krewski D, Chen Y, Pope CA III, Gapstur SM, Thun MJ. Radon and COPD mortality in the American Cancer Society Cohort. Eur Respir J. 2012;39(5):1113–1119 [DOI] [PMC free article] [PubMed] [Google Scholar]