Abstract
Background
Attention-Deficit / Hyperactivity Disorder (ADHD) is prevalent at a higher rate in correctional settings than in the general population. Treatment of ADHD in this environment is challenging as stimulants, the most common treatment for ADHD, require cautious prescribing in the context of frequent substance use disorders (SUD) and diversion in the institutional setting. In addition, both pharmacological and non-pharmacological treatment approaches require significant staff resources. The aim of this scoping review is to map and summarize all literature addressing treatment of ADHD specifically in correctional settings, synthesize the evidence supporting various approaches, and highlight areas for future research. Due to the limited number of primary research studies addressing this question directly, we chose a scoping review methodology that would allow us to explore what kinds of studies and literature exist and include all types of articles directly related to our question.
Results
Five-hundred sixty-five relevant articles were screened. Thirty-two articles were included in the final review. Eleven of the articles reported primary research. Five of these articles were based on three randomized controlled trials. Among randomized controlled trials on the effect of stimulants, inclusion criteria, outcome measures and effectiveness varied widely. Non-male and non-white populations were under-represented. Among review articles and recommendations opinion was inconsistent, with some recommending stimulants as first-line treatment and others recommending they be avoided altogether. The effect of non-stimulant medications was examined in 2 small studies. The only non-pharmacological treatment examined was dialectical behavior therapy, and only feasibility was reported. Four articles provided practice recommendations from consensus or expert opinion. Two of these recommended stimulants as first-line treatment, and two recommended stimulants as treatment of last resort.
Conclusions
We found a diverse but shallow literature addressing our research question. Primary research in the corrections setting is limited and varies in inclusion criteria, outcomes studied, and effectiveness. Recommendations on treatment are inconsistent. Future research should address methods of diagnosis, the role of non-stimulants, non-pharmacological interventions, non-male and non-white people who are incarcerated (PWAI), and effects of treatment method on patients, staff and other PWAI. Better research and guidance on treating ADHD has potential to improve health of PWAI, the institutional environment, and resource utilization.
Keywords: Attention-deficit/hyperactivity disorder (ADHD), Treatment, Intervention, Stimulants, Inmates (people who are incarcerated (PWAI)), Correctional setting, Prison, Review
Background
Definition of attention-deficit/hyperactivity disorder
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental condition characterized by inattention, hyperactivity, or impulsivity that interferes with daily functioning, interpersonal activity, and academic achievement. Although most commonly diagnosed in childhood, ADHD can continue into adulthood. Diagnosis of ADHD is extremely challenging and subjective. As of 2013, the major method used by practitioners to diagnose ADHD is based on DSM-5 criteria. For adults 17 years and older, diagnosis requires at least 5 symptoms of either inattention or hyperactivity lasting at least 6 months. In addition, the symptoms must have been present since before age 12, present in at least two different settings, not caused by other disorders, and interfere with the individual’s quality of life (American Psychiatric Association, 2013). Examples of inattention symptoms include trouble maintaining attention, forgetfulness, and failure to pay close attention to details. Examples of hyperactivity symptoms include fidgeting, excessive talking, and an inability to stay seated for long periods of time. Other methods for diagnosing ADHD include various ADHD self- or clinician-rated screening tools. Each tool is subjective and unique, which creates inconsistencies with ADHD diagnosis. Overall, diagnosing ADHD is difficult due to the lack of objective criteria, symptomatic behaviours being on a spectrum with normal behaviour, and the possibility of other comorbid mental health conditions causing similar symptoms (Katzman et al., 2017).
ADHD prevalence in correctional facilities
The Canadian Community Health Survey estimated the prevalence of clinician-diagnosed adult ADHD within the general population to be 2.7% (Connolly et al., 2019). The prevalence of ADHD has consistently been found to be higher in correctional settings than in the general population. Diverse studies estimate the prevalence of ADHD in correctional facilities in the range from 9.1 to 45% (Beaudry et al., 2021; Billstedt et al., 2017; Blocher et al., 2001; Cahill et al., 2012; Curran & Fitzgerald, 1999; Eyestone & Howell, 1994; Ginsberg et al., 2010; Hamzeloo et al., 2016; Konstenius et al., 2015; Lindgren et al., 2002; Moore et al., 2016; Rösler et al., 2004). A systematic review of 102 studies and 69,997 participants from detention settings, 27.5% of which were adults, reported an adult ADHD prevalence of 26.2% (Baggio et al., 2018). The review found no significant difference between prevalence rates identified using screening tools or clinical interviews. Specifically in Canada, one study found the prevalence of adult ADHD in 497 Canadian males experiencing incarceration to be 16.5% based on the Adult ADHD Self-Reporting Scale (ASRS) (Usher et al., 2013).
Behaviours concurrent with ADHD such as increased defiant and antisocial behaviour, and substance use disorders (SUD), are likely to play a role in the observed higher prevalence in correctional facilities (Ginsberg et al., 2010). A study by Velez-Pastrana et al. (2020), found individuals experiencing incarceration with ADHD had a significantly higher risk for lifetime SUD (OR = 2.17) and current SUD (OR = 2.08).
ADHD treatment in adults
Much of the clinical guidance for treating adults in the general population who suffer from ADHD recommends simulants as the first line pharmaceutical approach. However, there remains significant uncertainty about the value of, and best approach to, treatment of ADHD in adults (Huang et al., 2020; Castells et al., 2018; Cândido et al., 2021; NICE, 2018; CADDRA, 2020). This uncertainty arises from challenges with diagnosis (especially in the context of co-morbidity with other mental illness and addiction), heterogeneity and low quality of scientific methods, inconsistency in the clinical outcomes that show improvement, and a short duration of follow-up for most studies. In addition, treatment with stimulants is difficult as they may be abused and lead to negative health outcomes. Stimulants can also cause safety concerns in correctional facilities due to diversion. Although non-stimulants can be used with less risk of abuse, they do not have the same short-term effectiveness as stimulants (Cortese et al., 2018). And finally, a recent Cochrane review of immediate-release methylphenidate for adult ADHD in general populations concluded there was no certain evidence that it could reduce ADHD symptoms more than lithium or placebo treatment (Cândido et al., 2021).
Due to constraints of time and resources, and the movement of individuals between institutions, nonpharmacologic treatments may be challenging to provide in correctional settings (Young & Cocallis, 2019). Furthermore, screening for ADHD within these settings is often inadequate, preventing individuals from being identified for treatment. These diagnostic and treatment challenges combined with ADHD’s high prevalence in correctional facilities pose a complex challenge.
Study purpose
There is currently no widely agreed upon treatment method for individuals with ADHD in correctional facilities. While there is an abundance of literature relating ADHD to criminality or addressing treatments outside of correctional settings, this review will focus solely on treatments within institutions, for which the body of literature is much smaller. A scoping review was chosen for our inquiry due to the diversity of literature currently available. Our study goals are to map the types of articles and research studies, describe the range of research methods and outcomes, identify areas of consensus and controversy, identify research gaps, and ultimately inform treatment recommendations and guidelines.
Methods
The methodology for our scoping review follows the 5-step approach outlined by Arksey and O’Malley (2005): (1) identifying the research question, (2) identifying relevant studies, (3) study selection, (4) charting the data, and (5) collating, summarizing and reporting the results. In keeping with scoping review methodology, our research question evolved somewhat as study questions and methods included in the literature became evident. A search strategy was developed in consultation with a university librarian. The initial literature search was conducted in October 2021 and updated in December 2022. It included the search terms identified in Table 1. The final research question was: what treatments have been studied, showing what effectiveness, among people in correctional facilities?
Table 1.
Key terms used in the literature search
| Attention Deficit Disorder with Hyperactivity AND | Correctional Facilities AND | Therapeutics |
|---|---|---|
| Attention deficit hyperactivity disorder OR attention deficit disorder with hyperactivity OR attention deficit disorder* OR attention deficit hyperactivity disorder* OR attention deficit-hyperactivity disorder* OR ADHD OR ADDH | Prison* OR jail* OR correction* facilit* OR detention centre* OR detention center* OR incarcerated OR detainee* OR remand OR confinement | Pharmac* OR drug* OR intervention* OR health care OR therapeutic* OR therapies OR therapy OR treatment* |
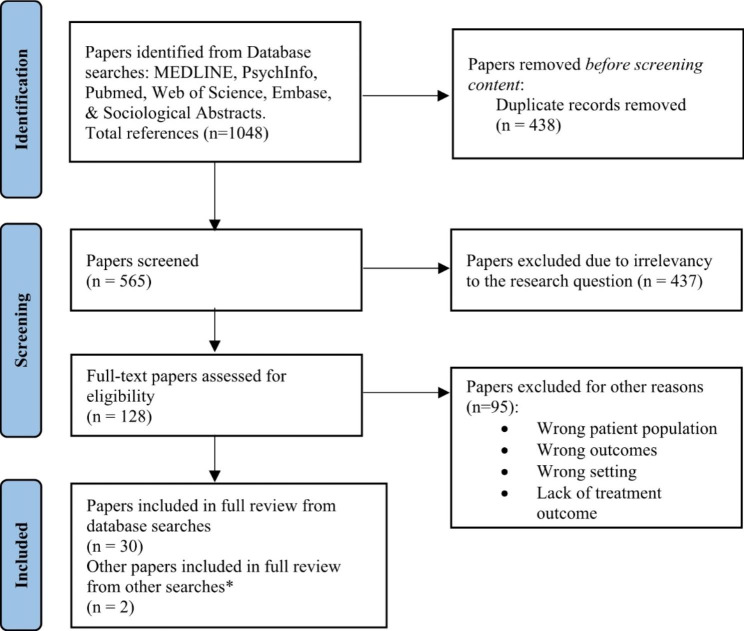
The search was conducted in the following databases: Ovid MEDLINE Epub ahead of print (1946–2021), APA PsychInfo, Pubmed, Web of Science, Embase, and Sociological Abstracts. We did not conduct a search of the grey literature. Relevant studies were identified as those that involved the following: (a) adult populations in correctional settings and (b) the treatment of (c) ADHD. All types of research papers from any year were included. Articles were reviewed using the Covidence web platform. Both researchers screened the titles and abstracts of the 565 articles resulting from the initial search to determine inclusion for full review. Inclusion criteria for this step were kept broad to identify as many relevant articles as possible. Of these articles, 128 were selected and underwent a full-text review by one researcher (CB) to further determine relevance to the research question. Thirty of these articles fit the scope of our research goals and an additional 2 relevant articles that were published after the date of the initial search were included in the final report. Figure 1 shows a PRISMA diagram of the complete process.
Fig. 1.
PRISMA diagram of selection process for articles (Page et al., 2021)
* Both articles were published after the date of the database search and were found by authors when reading literature relating to the scoping review
Results
Mapping the characteristics of articles reviewed
The outcome of our final review is summarized in Tables 2, 3 and 4. Articles are mapped as types of studies by country of origin in Table 2. Methods and results of each primary research study are summarized in Table 3, and all other studies in Table 4.
Table 2.
Types of articles by country of origin
| Article Type | Sweden (n = 6) | USA (n = 11) | UK (n = 8) | Spain (n = 1) | Switzerland (n = 1) | Germany (n = 1) | Canada (n = 2) | Multi-national (n = 2) |
|---|---|---|---|---|---|---|---|---|
| Primary Research (n = 11) | 5 | 4 | 2 | 0 | 0 | 0 | 0 | 0 |
|
RCT* Quasi-experimental Case series Chart review Evaluation/QI** |
4 1 0 0 0 |
0 1 1 1 1 |
1 0 0 0 1 |
n/a | n/a | n/a | n/a | n/a |
| All Other Articles (n = 21) | ||||||||
| Non-systematic review, consensus statement, expert opinion, recommendation | 1 | 7 | 6 | 1 | 1 | 1 | 2 | 2 |
Notes:
*Two separate randomized controlled trials (RCTs) were completed. One RCT had one article published and the other had three separate papers published, thus totaling four RCT articles
**Evaluation of implementation of program or approach, or strategy to improve quality (QI)
Table 3.
Summary of primary research articles
| Author/Year | Study Type | Country | Intervention | Population | Screening/Diagnosis | n | Follow-up (Weeks) | Results | COI* |
|---|---|---|---|---|---|---|---|---|---|
| Asherson 2022 | RCT | UK | OROS-MPH | Male 16–25 | Barkley/clinical interview | 200 | 8 | No difference in ADHD symptoms or secondary outcomes self and observer rated. | Y |
| Ginsberg, 2012 | RCT | Sweden | OROS-MPH | Male 21–61 | WURS-25/ASRS/clinical interview | 30 | 5 + 47 open label ext. | Treatment improved self- and observer-rated ADHD symptoms. Treatment and placebo both improved during open-label extension. No drug misuse detected. | Y |
| Ginsberg, 2012 | RCT | Sweden | OROS-MPH | Male 21–61 | WURS-25/ASRS/clinical interview | 30 | 5 + 47 open label ext. | Treatment improved verbal working memory, visuospatial working memory, verbal abstract reasoning, motor activity, and some aspects of quality of life. | Y |
| Ginsberg 2015 | RCT | Sweden | OROS-MPH | Male 21–61 | WURS-25/ASRS/clinical interview | 24 (year 1), 20 (year 3) |
5 + 47 open label ext. Follow up at 1 & 3 year |
ADHD symptom improvement maintained at 1- and 3- year follow up. Participants continuing medication had less ADHD symptoms, alcohol/drug misuse, and functional impairment. | Y |
| Konstenius 2014 | RCT double blind | Sweden | OROS-MPH | Male 18–65 w/ amphetamine dependence; final 2 weeks before release | WURS/ASRS/CCPT/clinical interview | 54 | 24 | Compared to placebo, treatment group improved self- and clinician-rated severity, sig more drug-negative urines, longer median retention to treatment, longer time till relapse, and decreased cravings compared to placebo. | N |
| Jillani 2016 | Case series | USA | Atomoxetine | Male 16–20 | Clinical interview | 5 | 10 | Investigator-rated ADHD symptoms improved and reduction in anxiety symptoms. | Y |
| Bastiaens 2019 | Chart review | USA | Non-stimulants | PWAI with ADHD | Clinical interview | 108 | n/a | ADHD symptoms improved on average. Patients with no history of stimulant use had better treatment response. | N |
| Muld 2016 | Quasi-experimental | Sweden | DBT | Males in compulsory care | WURS / ASRS / Clinical interview | 40 | 6 | Improved Self rated ADHD symptoms and general well-being, but no change in staff ratings. | N |
| Chaplin, 2021 | QI | UK | Improvements to ADHD pathway | Males | brief-BAARS / DIVA-5 | n/a | n/a | Structured screening, staff training, and other improvements lead to more ADHD diagnosis and treatment. | NS |
| Martin, 2006 | Quasi-experimental | USA | EEG biofeedback | Male 14–17 | ADHD diagnosis or psychologist screen | 7 | 7–10 | ADHD symptoms improved, worsened, or didn’t change for different participants. Some improvements in secondary measures. | NS |
| Appelbaum, 2011 | Evaluation | USA | Treatment program pathway | Male | n/a | 16,795 | n/a | Over 2 years, 116 received stimulant treatment out of 16,795 candidates. 11 had treatment withdrawn due to misuse. | N |
Notes: *COI (Conflict of Interest): Y = present, N = not present, NS = not specified
Table 4.
Summary of review, recommendation and opinion articles
| Author/Year | Article Type | Country | Main Points | COI |
|---|---|---|---|---|
| Young 2018 | Consensus | UK | Screen all PWAI for ADHD. Stimulants first line, non-stimulants when ineffective/SUD. Include psychoeducation, psychological, and psychosocial components. Treat severe comorbidity before ADHD. Promote significant PWAI engagement in treatment. | Y |
| Appelbaum, 2009 | Protocol | USA |
Diagnosis: Consensus by 2 psychiatrists, diagnosis of ADHD before age 12, psych testing by doctoral psychologist, and clinically significant behaviour impairment. Treatment: Non-pharm first line, non-stimulants second line, stimulants if others not effective. Continuation of treatment requires objective improvement and compliance |
NS |
| Scott 2016 | Expert opinion | Canada | Modification of Appelbaum, 2009. Suggests addition of improved screening and behavioural interventions. First line treatment should depend on facility. | Y |
| Young, 2011 | Consensus | UK | Suggests improved screening, staff training, and resource availability to PWAI. Methylphenidate first-line, atomoxetine/dexamphetamine when abuse potential. Treat comorbidities. Benefits of stimulants outweigh risks. | Y |
| Mattes, 2016 | Review | USA | Stimulant risks may outweigh benefits. Mixed research on current medications. Alpha-2 agonists potential medication. | N |
| Knecht 2015 | Systematic review | Spain | Self-report tools debatable, Coolidge Correctional Inventory specifically made for PWAI. Medication first-line when less severe symptoms. Tailored interventions needed if comorbidities. | Y |
| Young, 2019 | Review | UK | Some concerns of stimulants may be unsubstantiated. Non-stimulants can be used when comorbid SUD. Focus on psychological, behavioural, and educational needs. | Y |
| Sebastian 2019 | Review | Germany | Focus on substance use interventions and reduce violence/offending. Completion/adherence to rehabilitation plans is likely challenge. Early intervention programs required. | Y |
| Tully, 2022 | Review | UK | Proper diagnosis/treatment of ADHD time-consuming, takes away from treating other conditions. Current research on medications is limited & questionable. Be cautious when prescribing. | N |
| Retz 2021 | Review | Multi-national | Early recognition and intervention essential. Concerns of stimulants may be outweighed by benefits. Atomoxetine good alternative when comorbid SUD. Address psychological, behavioral, and educational needs. | NS |
| Sutton, 2016 | Text & opi-nion | Canada | Non-stimulants may not be ideal in prison. Continuous performance tests may reduce malingering. Calls for practice guidelines, currently lack of consistency. | N |
| Appelbaum, 2008 | Review | USA | PWAI staging behaviour can overburden psychiatrists. Guidelines/ consistency may mitigate issues. Misuse/diversion should prompt discontinuation of stimulants. Education/group therapy may benefit PWAI. | N |
| Burns, 2009 | Text & opi-nion | USA | Discourages use of stimulants due to prevalence of SUD, misuse potential, and burden/safety concerns. | NS |
| Young, 2011 | Review | Multi-national | Treatment requires complex plan that considers rehabilitation/comorbidity consideration. Early intervention crucial. | N |
| Ginsberg 2013 | Text & opi-nion | Sweden | Medication can be beneficial but should be used carefully. Pros outweigh cons if treatment controlled and individualized. | Y |
| Hall, 2016 | Commentary | USA | Diagnosis made difficult by high rates of trauma, SUD, and comorbidity. Treatment should include behavioral component. | N |
| UKAAN, 2013 | Chapter in book | UK | Comprehensive, individualized treatment programs needed. | NS |
| Barry, 2008 | Review | USA | Consider biological/genetic components in treatment. | NS |
| Young, 2015 | Conference abstract | UK | Multimodal treatments may have a greater effect. R&R2ADHD developed for corrections. | Y |
| Fructuoso, 2019 | Letter to editor | Switzerland | Stimulants are effective treatment, but major risk of misuse/diversion/safety for PWAI and staff. Suggests consideration of alternative approaches, such as non-addictive drugs or non-pharm interventions. | NS |
| Boutwell 2020 | Review | USA | Stimulants are effective but concerned about safety/cost/side effects. | NS |
Summary of themes arising
Diagnosis and screening
Success of treatment will inevitably depend on the reliability of the diagnostic method. We found diverse approaches to diagnosis in the primary research studies reported. Among these studies, 6 used a clinical interview, 4 used the ASRS, 3 used WURS, 1 used CCPT, 1 used the brief-BAARS, 1 used the self-rated Barkley ADHD scale, and 3 were unclear/unspecified regarding what diagnosis or screening method was used. The UK expert consensus statement suggests the specific use of CHAT in youth followed by SNAP-IV / Conners’ CBRS, and the brief-BAARS in adults followed by an interview with CAADID, DIVA-2, or ACE+ (Young et al., 2018).
Authors discussed this inconsistency as one of the largest barriers to treating ADHD in corrections, along with the common presence of co-morbid mental health, addiction and personality disorders. Some suggest the creation of a standardized approach to screening and diagnosis of ADHD (Young et al., 2011, 2018; Scott et al., 2016; Knecht et al., 2015; Sutton & Kolla, 2016). Such guidelines could also be used to reduce burden on correctional clinicians (Sutton & Kolla, 2016). In addition to this, some articles suggest systematic ADHD screening for PWAI, either upon entry to any institution or on a regular basis (Young et al., 2011, 2018).
Pharmaceutical treatment
Most primary studies that we identified tested the effects of stimulants. Among the RCTs looking at methylphenidate, one found significantly improved observer-rated and self-rated ADHD symptoms, including clinician-rated severity and global functioning, cognitive measures, motor activity, and quality of life, compared to placebo (Ginsberg & Lindefors, 2012; Ginsberg et al., 2012). Observer and self-reported ADHD symptoms remained improved in 1- and 3-year follow up (Ginsberg et al., 2015). Another RCT found methylphenidate significantly improved self-reported ADHD symptoms and clinician-rated severity, but not clinician-rated improvement, compared to placebo (Konstenius et al., 2014). This RCT also found the treatment group had significantly less drug-positive urine tests. The most recent and largest RCT of methylphenidate found no significant differences in any measured outcome between treatment and placebo groups (Asherson et al., 2022). Additionally, more adverse events occurred in treatment groups than in placebo groups for all 3 RCTs.
Primary studies of non-stimulant treatment of ADHD in correctional settings were limited. One case series of 5 individuals on atomoxetine found it was able to reduce investigator-rated ADHD symptomatology and anxiety (Jillani et al., 2016). A retrospective chart review of atomoxetine and alpha-2 agonists showed that both improved clinician-rated severity (Bastiaens et al., 2019). In addition to primary research studies, one review was focused on the potential of alpha-2 agonists and suggested them as a potential treatment for patients in corrections facilities with ADHD (Mattes, 2016). The majority of review and opinion articles were in support of the use of medication for ADHD treatment. Most authors view stimulant medication as a component of multimodal treatment that would reduce symptomology to allow patients to gain optimal benefit from non-medical treatments (Ginsberg et al., 2013).
Non-pharmacological interventions
Non-pharmacological interventions are a component of multimodal treatment. Although we found only limited research evidence, there is significant expert support for non-medical interventions as effective treatments. These interventions are challenging to implement in correctional facilities due to considerations such as restricted resources. PWAI also have unpredictable time in institutions due to transfers or releases (Young & Cocallis, 2019), making shorter programs preferrable (Young et al., 2018). Only 2 primary studies utilizing non-pharmaceutical treatment were found. EEG biofeedback had mixed results on ADHD symptoms and cognitive measures, which were only completed on a small sample of patients (Martin & Johnson, 2006). DBT was found to be a feasible treatment option that significantly reduced self-rated ADHD symptoms (Muld et al., 2016). Overall, authors generally suggested key components of treatment should include education about ADHD, psychotherapy, behavioural control, and mentorship (Young et al., 2018; Scott et al., 2016; Appelbaum, 2008; Fructuoso, 2019). The R&R2-ADHD treatment program is a brief group cognitive skills program that has been widely promoted in publications by its creator, Susan Young. This program received support in 11 articles, 6 of those co-authored by the program creator. Primary studies of this treatment among people experiencing incarceration were not published by the time we conducted our review (Young & Ross, 2021). Finally, several articles recommended frameworks that should be adopted when treating ADHD in corrections. The Risk-Needs-Responsivity model was mentioned in 3 articles and ensures PWAI are given an appropriate service that matches their risk of recidivism (Young et al., 2011; Sebastian et al., 2019; Sutton & Kolla, 2016).
Impacts on the institutional environment
There were no measures of impact on the institutional environment of the corrections facilities, other PWAI, clinicians, or other correctional staff. However, review articles have speculated that treatment is likely to reduce problematic behaviours, aggression, and potentially comorbidities (Mattes, 2016; Muld et al., 2016). Improved screening may also be validating for PWAI (Tully, 2022). One author speculated that if PWAI believe they can easily acquire prescriptions for stimulants, it may overburden psychiatrists and have effects on the correctional environment (Appelbaum, 2008).
Controversy surrounding the use of stimulants
Stimulants are, on one hand, the most studied treatment for ADHD both in the general population and, as we have observed in our study, in people within correctional settings. On the other hand, their potential to cause physical dependency and harmful side effects is reported as being considerable. As described above, primary studies focusing on the effectiveness of stimulants in correctional settings have shown conflicting results. It is not surprising then that we identified review, opinion and consensus articles offering conflicting advice about ADHD treatment and policy.
Several concerns are raised. Due to the high comorbidity with substance use disorders the potential for misuse and diversion is raised frequently (Scott et al., 2016; Young et al., 2011; Mattes, 2016; Young & Cocallis, 2019; Sebastian et al., 2019; Knecht et al., 2015; Appelbaum, 2008; Burns, 2009; Ginsberg et al., 2013; Fructuoso, 2019). In addition, some authors raise concern regarding risk of burden on limited staff resources with the increased workload in storing and monitoring administration of stimulants, as well as risk to the security of both PWAI and staff (Young & Cocallis, 2019; Appelbaum, 2008; Burns, 2009). We did not identify empirical evidence to support these concerns. Additionally, there are concerns about the potential side effects of stimulants (Boutwell et al., 2020). We found empirical evidence for side effects among the primary studies that utilized stimulants, most of which were reported as mild to moderate (Ginsberg & Lindefors, 2012; Konstenius et al., 2014). Following from all of these concerns, some authors conclude that risk may outweigh benefit in the prescribing of stimulants in correctional settings (Mattes, 2016; Burns, 2009; Boutwell et al., 2020), while others support the use of stimulants as first line treatment especially when extended release and water soluble formulations are used, decreasing risk of diversion (Young et al., 2018; Scott et al., 2016; Young & Cocallis, 2019; Knecht et al., 2015; Retz et al., 2021; Sutton & Kolla, 2016). Protocols used to manage other kinds of controlled medications (Young et al., 2011, 2018; Scott et al., 2016; Young & Cocallis, 2019), and use of continuous performance tests to monitor for diversion (Sutton & Kolla, 2016) are examples of approaches suggested for decreasing misuse and diversion. Still, we did not identify empirical evidence concerning the benefit of these procedures from articles in our scoping review.
Some authors suggest the abuse potential of stimulants is overstated as a link between stimulant use and subsequent abuse has not been established (Scott et al., 2016). Some cite that research has found stimulant use in general populations can prevent SUDs if treatment predates the SUD and is well supervised (Young & Cocallis, 2019; Hall et al., 2016). It has been suggested that it is unethical to withhold stimulants from PWAI, since they are an accepted standard of treatment in the general population (Young & Cocallis, 2019). It has also been suggested that it is unethical to provide stimulant treatment to PWAI with the current evidence available (Tully, 2022). Some authors support stimulants as first-line treatments, but recommend using non-stimulants when SUDs are present (Young et al., 2011, 2018; Young & Cocallis, 2019), while others argue that the high prevalence of SUDs in PWAI is reason enough to avoid the use of stimulants altogether (Burns, 2009).
Gaps in research knowledge
There are significant gaps in what we found in primary, empirical research regarding treatment of people with ADHD in correctional facilities. First, there is little demographic diversity, with only one primary study including women. Only three primary articles mentioned racial demographics. All three studies were conducted on predominately white identifying individuals (62.5%, 90%, 82%), highlighting a lack of racial diversity in the current literature (Asherson et al., 2022; Bastiaens et al., 2019; Chaplin et al., 2021). There were only 2 studies of non-stimulant medications, both with no control group and with small samples. Studies of non-pharmacological treatment were few, small and also not controlled. There is a gap in consensus-based, consistent screening and diagnosis, and outcome measures. There is no research on the impact of treatment on the working and living environment of correctional facilities. And finally, we found no primary research addressing the impact of ADHD treatment in correctional facilities on relevant outcomes in the community following release such as reduced SUD, recidivism, and improved quality of life.
Discussion
We found that the scientific knowledge base related to ADHD treatment in correctional settings has only a small number of primary studies. These studies are made up of small samples that are overwhelmingly white males, primarily focused on stimulants as treatment, diverse in methodology and outcomes, short in follow-up and inconsistent in results. We identified articles offering narrative review, expert opinion, and recommendations. These vary widely in their guidance. This presents a challenging foundation on which to base policy and clinical practice guidance for clinicians caring for people in correctional facilities.
Although not the subject of this scoping review, there is a substantial knowledge base that draws on primary research on ADHD treatment outside of the correctional facility context. This evidence is relevant to the treatment of ADHD in PWAI, but the degree to which it can be extrapolated is uncertain. People in correctional facilities have higher rates of comorbidity with SUD and mental illness than people with ADHD in the general population. In addition, patterns of socialization, interaction with facility staff and policies, prevalence of violence, and drug market dynamics within institutions will all play a role in both the need for, and the effectiveness of, ADHD treatment.
The unique and complex factors surrounding ADHD diagnosis and treatment in correctional facilities require specific and relevant treatment research to inform policy and clinical practice. We suggest that the current knowledge base is not adequate for this purpose. Our study sheds light on the critical need for research conducted among PWAI, as well as clinicians and institution staff. This research needs to be guided by stakeholder input including people who have experience living with ADHD in situations of incarceration, clinicians who have experience making treatment decisions with these patients, and facility staff who have experience with the socialization and security of PWAI within institutions. A research agenda should include consensus-based treatments; use consistent diagnostic criteria, treatment protocols and outcome measures; and include demographically representative populations of PWAI.
Our study has not captured grey literature. It has not provided quantitative synthesis of data, nor has it provided systematic assessment of reliability of the literature. However, the number of studies and participants, and the methodological diversity among these, renders more systematic synthesis inappropriate. Our scoping review approach to this question was well suited to mapping the characteristics of the knowledge base, and for qualitatively exploring the range of methods and findings.
Conclusions
The current literature on ADHD treatments in correctional settings is diverse and contentious. Additional high quality research is needed to improve health outcomes for individuals with ADHD experiencing incarceration.
Acknowledgements
The authors thank Ann Kelly for assistance in developing the search strategy.
Authors’ contributions
DG was responsible for the conception of the study design. CB collected and summarized the data, CB and DG reviewed papers, CB drafted the manuscript, CB and DG revised the manuscript.
Funding
Self-funded.
Data Availability
All articles resulting from each step in the search and screening process have been retained by the authors and are available on request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 10.1176/appi.books.9780890425596
- Appelbaum KL. Assessment and treatment of correctional inmates with ADHD. The American Journal of Psychiatry. 2008;165(12):1520–1524. doi: 10.1176/appi.ajp.2008.08060849. [DOI] [PubMed] [Google Scholar]
- Appelbaum KL. Attention deficit hyperactivity disorder in prison: A treatment protocol. The Journal of the American Academy of Psychiatry and the Law. 2009;37(1):45–49. [PubMed] [Google Scholar]
- Appelbaum KL. Stimulant use under a prison treatment protocol for attention-deficit/hyperactivity disorder. Journal of Correctional Health Care: The Official Journal of the National Commission on Correctional Health Care. 2011;17(3):218–225. doi: 10.1177/1078345811401356. [DOI] [PubMed] [Google Scholar]
- Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Asherson P, Johansson L, Holland R, Bedding M, Forrester A, Giannulli L, Ginsberg Y, Howitt S, Kretzschmar I, Lawrie S, Marsh C, Kelly C, Mansfield M, McCafferty C, Khan K, Müller-Sedgwick U, Strang J, Williamson G, Wilson L, Thomson L. OROS-methylphenidate to reduce ADHD symptoms in male prisoners aged 16–25 years: A RCT. Efficacy and Mechanism Evaluation. 2022;9(6):1–114. doi: 10.3310/THEI8200. [DOI] [PubMed] [Google Scholar]
- Baggio S, Fructuoso A, Guimaraes M, Fois E, Golay D, Heller P, Perroud N, Aubry C, Young S, Delessert D, Gétaz L, Tran NT, Wolff H. Prevalence of attention deficit hyperactivity disorder in detention settings: A systematic review and meta-analysis. Frontiers in Psychiatry. 2018;9:331. doi: 10.3389/fpsyt.2018.00331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry LM, Gaines T. Attention deficit hyperactivity disorder: Intervention as crime prevention. The Journal of Behavior Analysis of Offender and Victim Treatment and Prevention. 2008;1(2):154–170. doi: 10.1037/h0100441. [DOI] [Google Scholar]
- Bastiaens L, Scott O, Galus J. Treatment of adult ADHD without stimulants: Effectiveness in a dually diagnosed correctional population. The Psychiatric Quarterly. 2019;90(1):41–46. doi: 10.1007/s11126-018-9602-7. [DOI] [PubMed] [Google Scholar]
- Beaudry G, Yu R, Långström N, Fazel S. An updated systematic review and meta-regression analysis: Mental disorders among adolescents in juvenile detention and correctional facilities. Journal of the American Academy of Child and Adolescent Psychiatry. 2021;60(1):46–60. doi: 10.1016/j.jaac.2020.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billstedt E, Anckarsäter H, Wallinius M, Hofvander B. Neurodevelopmental disorders in young violent offenders: Overlap and background characteristics. Psychiatry Research. 2017;252:234–241. doi: 10.1016/j.psychres.2017.03.004. [DOI] [PubMed] [Google Scholar]
- Blocher D, Henkel K, Retz W, Retz-Junginger P, Thome J, Rösler M. [Symptoms from the spectrum of Attention-Deficit/Hyperactivity disorder (ADHD) in sexual delinquents] Fortschritte Der Neurologie · Psychiatrie. 2001;69(10):453–459. doi: 10.1055/s-2001-17562. [DOI] [PubMed] [Google Scholar]
- Boutwell BB, Kavish N, Narvey C. The efficacy, ethics, & pitfalls of stimulants for justice system involved individuals. Neuroscience and Biobehavioral Reviews. 2020;116(oa7, 7806090):120–129. doi: 10.1016/j.neubiorev.2020.06.003. [DOI] [PubMed] [Google Scholar]
- Burns KA. The top ten reasons to limit prescription of controlled substances in prisons. The Journal of the American Academy of Psychiatry and the Law. 2009;37(1):50–52. [PubMed] [Google Scholar]
- CADDRA (2020). Canadian ADHD Practice Guidelines (4.1). https://www.caddra.ca/wp-content/uploads/Canadian-ADHD-Practice-Guidelines-4.1-January-6-2021.pdf
- Cahill BS, Coolidge FL, Segal DL, Klebe KJ, Marle PD, Overmann KA. Prevalence of ADHD and its subtypes in male and female adult prison inmates: Prevalence of ADHD. Behavioral Sciences & the Law. 2012;30(2):154–166. doi: 10.1002/bsl.2004. [DOI] [PubMed] [Google Scholar]
- Cândido, R. C. F., de Padua, M., Golder, C. A., S., & Junqueira, D. R. (2021). Immediate-release methylphenidate for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database of Systematic Reviews, 2021(1), 10.1002/14651858.CD013011.pub2 [DOI] [PMC free article] [PubMed]
- Castells X, Blanco-Silvente L, Cunill R. Amphetamines for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Systematic Review. 2018;8:Cd007813. doi: 10.1002/14651858.CD007813.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaplin, E., Rawat, A., Perera, B., McCarthy, J., Courtenay, K., Forrester, A., Young, S., Hayward, H., Sabet, J., Underwood, L., Mills, R., Asherson, P., & Murphy, D. (2021). Prisoners with attention deficit hyperactivity Disorder: Co-morbidities and service pathways. International Journal of Prisoner Health. 10.1108/IJPH-03-2021-0020 [DOI] [PubMed]
- Connolly RD, Speed D, Hesson J. Probabilities of ADD/ADHD and related substance use among canadian adults. Journal of Attention Disorders. 2019;23(12):1454–1463. doi: 10.1177/1087054716647474. [DOI] [PubMed] [Google Scholar]
- Cortese S, Adamo N, Giovane CD, Mohr-Jensen C, Hayes AJ, Carucci S, Atkinson LZ, Tessari L, Banaschewski T, Coghill D, Hollis C, Simonoff E, Zuddas A, Barbui C, Purgato M, Steinhausen HC, Shokraneh F, Xia J, Cipriani A. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: A systematic review and network meta-analysis. The Lancet Psychiatry. 2018;5(9):727–738. doi: 10.1016/S2215-0366(18)30269-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran S, Fitzgerald M. Attention deficit hyperactivity disorder in the prison population. American Journal of Psychiatry. 1999;156(10):1664–a. doi: 10.1176/ajp.156.10.1664-a. [DOI] [PubMed] [Google Scholar]
- Eyestone LL, Howell RJ. An epidemiological study of attention-deficit hyperactivity disorder and major depression in a male prison population. The Bulletin of the American Academy of Psychiatry and the Law. 1994;22(2):181–193. [PubMed] [Google Scholar]
- Fructuoso A. Management of attention deficit/hyperactivity disorder and the use of stimulants in prison. Evaluation of the risks and benefits. Revista Espanola de Sanidad Penitenciaria. 2019;21(2):113–114. doi: 10.4321/S1575-06202019000200008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsberg Y, Lindefors N. Methylphenidate treatment of adult male prison inmates with attention-deficit hyperactivity disorder: Randomised double-blind placebo-controlled trial with open-label extension. The British Journal of Psychiatry: The Journal of Mental Science. 2012;200(1):68–73. doi: 10.1192/bjp.bp.111.092940. [DOI] [PubMed] [Google Scholar]
- Ginsberg Y, Hirvikoski T, Lindefors N. Attention deficit hyperactivity disorder (ADHD) among longer-term prison inmates is a prevalent, persistent and disabling disorder. Bmc Psychiatry. 2010;10:112. doi: 10.1186/1471-244X-10-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsberg Y, Hirvikoski T, Grann M, Lindefors N. Long-term functional outcome in adult prison inmates with ADHD receiving OROS-methylphenidate. European Archives of Psychiatry and Clinical Neuroscience. 2012;262(8):705–724. doi: 10.1007/s00406-012-0317-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsberg Y, Langstrom N, Larsson H, Lichtenstein P. ADHD and criminality: Could treatment benefit prisoners with ADHD who are at higher risk of reoffending? Expert Review of Neurotherapeutics. 2013;13(4):345–348. doi: 10.1586/ern.13.22. [DOI] [PubMed] [Google Scholar]
- Ginsberg Y, Langstrom N, Larsson H, Lindefors N. Long-term treatment outcome in adult male prisoners with Attention-Deficit/Hyperactivity disorder: Three-year naturalistic follow-up of a 52-week methylphenidate trial. Journal of Clinical Psychopharmacology. 2015;35(5):535–543. doi: 10.1097/JCP.0000000000000395. [DOI] [PubMed] [Google Scholar]
- Hall RCW, Myers WC. Challenges and limitations to treating ADHD in incarcerated populations. Journal of the American Academy of Psychiatry and the Law Online. 2016;44(2):164–170. [PubMed] [Google Scholar]
- Hamzeloo M, Mashhadi A, Salehi Fadardi J. The prevalence of ADHD and comorbid disorders in iranian adult male prison inmates. Journal of Attention Disorders. 2016;20(7):590–598. doi: 10.1177/1087054712457991. [DOI] [PubMed] [Google Scholar]
- Huang H, Huang H, Spottswood M, Ghaemi N. Approach to evaluating and managing adult attention-deficit/hyperactivity disorder in primary care. Harvard Review of Psychiatry. 2020;28(2):100. doi: 10.1097/HRP.0000000000000248. [DOI] [PubMed] [Google Scholar]
- Jillani S, Patel P, Trestman R, Kamath J. Atomoxetine for the treatment of ADHD in incarcerated adolescents. The Journal of the American Academy of Psychiatry and the Law. 2016;44(2):158–163. [PubMed] [Google Scholar]
- Katzman MA, Bilkey TS, Chokka PR, Fallu A, Klassen LJ. Adult ADHD and comorbid disorders: Clinical implications of a dimensional approach. Bmc Psychiatry. 2017;17(1):302. doi: 10.1186/s12888-017-1463-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knecht C, De Alvaro R, Martinez-Raga J, Balanza-Martinez V. Attention-deficit hyperactivity disorder (ADHD), substance use disorders, and criminality: A difficult problem with complex solutions. International Journal of Adolescent Medicine and Health. 2015;27(2):163–175. doi: 10.1515/ijamh-2015-5007. [DOI] [PubMed] [Google Scholar]
- Konstenius M, Jayaram-Lindstrom N, Guterstam J, Beck O, Philips B, Franck J. Methylphenidate for attention deficit hyperactivity disorder and drug relapse in criminal offenders with substance dependence: A 24-week randomized placebo-controlled trial. Addiction (Abingdon England) 2014;109(3):440–449. doi: 10.1111/add.12369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konstenius M, Larsson H, Lundholm L, Philips B, van de Glind G, Jayaram-Lindström N, Franck J. An epidemiological study of ADHD, substance use, and comorbid problems in incarcerated women in sweden. Journal of Attention Disorders. 2015;19(1):44–52. doi: 10.1177/1087054712451126. [DOI] [PubMed] [Google Scholar]
- Lindgren M, Jensen J, Dalteg A, Meurling AW, Ingvar DH, Levander S. Dyslexia and AD/HD among swedish prison inmates. Journal of Scandinavian Studies in Criminology and Crime Prevention. 2002;3(1):84–95. doi: 10.1080/140438502762467227. [DOI] [Google Scholar]
- Martin G, Johnson CL. The boys totem town neurofeedback project: A pilot study of EEG biofeedback with incarcerated juvenile felons. Journal of Neurotherapy. 2006;9(3):71–86. doi: 10.1300/J184v09n03_05. [DOI] [Google Scholar]
- Mattes JA. Treating ADHD in prison: Focus on Alpha-2 agonists (clonidine and guanfacine) The Journal of the American Academy of Psychiatry and the Law. 2016;44(2):151–157. [PubMed] [Google Scholar]
- Moore E, Sunjic S, Kaye S, Archer V, Indig D. Adult ADHD among NSW prisoners: Prevalence and psychiatric comorbidity. Journal of Attention Disorders. 2016;20(11):958–967. doi: 10.1177/1087054713506263. [DOI] [PubMed] [Google Scholar]
- Muld B, Jokinen J, Bolte S, Hirvikoski T. Skills training groups for men with ADHD in compulsory care due to substance use disorder: A feasibility study. ADHD-Attention Deficit and Hyperactivity Disorders. 2016;8(3):159–172. doi: 10.1007/s12402-016-0195-4. [DOI] [PubMed] [Google Scholar]
- NICE (2018). Attention deficit hyperactivity disorder: Diagnosis and management. NICE Guideline. https://www.nice.org.uk/guidance/ng87 [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, Moher D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Bmj. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Retz W, Ginsberg Y, Turner D, Barra S, Retz-Junginger P, Larsson H, Asherson P. Attention-Deficit/Hyperactivity disorder (ADHD), antisociality and delinquent behavior over the lifespan. Neuroscience And Biobehavioral Reviews. 2021;120:236–248. doi: 10.1016/j.neubiorev.2020.11.025. [DOI] [PubMed] [Google Scholar]
- Rösler M, Retz W, Retz-Junginger P, Hengesch G, Schneider M, Supprian T, Schwitzgebel P, Pinhard K, Dovi-Akue N, Wender P, Thome J. Prevalence of attention deficit-/hyperactivity disorder (ADHD) and comorbid disorders in young male prison inmates. European Archives of Psychiatry and Clinical Neuroscience. 2004;254(6):365–371. doi: 10.1007/s00406-004-0516-z. [DOI] [PubMed] [Google Scholar]
- Scott DA, Gignac M, Kronfli RN, Ocana A, Lorberg GW. Expert opinion and recommendations for the management of attention-deficit/hyperactivity disorder in correctional facilities. Journal of Correctional Health Care: The Official Journal of the National Commission on Correctional Health Care. 2016;22(1):46–61. doi: 10.1177/1078345815618392. [DOI] [PubMed] [Google Scholar]
- Sebastian, A., Retz, W., Tuscher, O., & Turner, D. (2019). Violent offending in borderline personality disorder and attention deficit/hyperactivity disorder. Neuropharmacology, 156(nzb, 0236217), 107565. 10.1016/j.neuropharm.2019.03.008 [DOI] [PubMed]
- Sutton W, Kolla NJ. A hard pill to swallow: Prescribing stimulants within the prison setting. Journal of the American Academy of Psychiatry and the Law. 2016;44(3):297–299. [PubMed] [Google Scholar]
- Tully J. Management of ADHD in prisoners—evidence gaps and reasons for caution. Frontiers in Psychiatry. 2022;13:771525. doi: 10.3389/fpsyt.2022.771525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UKAAN (2013). Attention deficit hyperactivity disorder and the criminal justice system. In Kings College London (Ed.), Handbook for Attention Deficit Hyperactivity Disorder in Adults (pp. 145–151). Springer Healthcare Ltd. 10.1007/978-1-908517-79-1_10
- Usher AM, Stewart LA, Wilton G. Attention deficit hyperactivity disorder in a canadian prison population. International Journal of Law and Psychiatry. 2013;36(3):311–315. doi: 10.1016/j.ijlp.2013.04.005. [DOI] [PubMed] [Google Scholar]
- Vélez-Pastrana MC, González RA, Ramos-Fernández A, Padilla RRR, Levin FR, García CA. Attention deficit hyperactivity disorder in prisoners: Increased substance use disorder severity and psychiatric comorbidity. European Addiction Research. 2020;26(4–5):179–190. doi: 10.1159/000508829. [DOI] [PubMed] [Google Scholar]
- Young S. Psychosocial treatment of offenders with ADHD. ADHD Attention Deficit and Hyperactivity Disorders. 2015;7(SUPPL. 1):S4. doi: 10.1007/s12402-015-0169-y. [DOI] [Google Scholar]
- Young S, Cocallis KM. Attention deficit hyperactivity disorder (ADHD) in the Prison System. Current Psychiatry Reports. 2019;21(6):41. doi: 10.1007/s11920-019-1022-3. [DOI] [PubMed] [Google Scholar]
- Young, S., & Ross, R. (2021). R&R2 for youths and adults with ADHD. https://www.researchgate.net/publication/348607351_RR2_for_Youths_Adults_with_ADHD
- Young S, Thome J. ADHD and offenders. The World Journal of Biological Psychiatry: The Official Journal of the World Federation of Societies of Biological Psychiatry. 2011;12(101120023):124–128. doi: 10.3109/15622975.2011.600319. [DOI] [PubMed] [Google Scholar]
- Young SJ, Adamou M, Bolea B, Gudjonsson G, Muller U, Pitts M, Thome J, Asherson P. The identification and management of ADHD offenders within the criminal justice system: A consensus statement from the UK adult ADHD network and criminal justice agencies. Bmc Psychiatry. 2011;11(100968559):32. doi: 10.1186/1471-244X-11-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S, Gudjonsson G, Chitsabesan P, Colley B, Farrag E, Forrester A, Hollingdale J, Kim K, Lewis A, Maginn S, Mason P, Ryan S, Smith J, Woodhouse E, Asherson P. Identification and treatment of offenders with attention-deficit/hyperactivity disorder in the prison population: A practical approach based upon expert consensus. Bmc Psychiatry. 2018;18(1):281. doi: 10.1186/s12888-018-1858-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All articles resulting from each step in the search and screening process have been retained by the authors and are available on request.