Abstract
Extracellular vesicles (EVs) are emerging mediators of intracellular and inter-organ communications in cardiovascular diseases (CVDs), especially in the pathogenesis of heart failure through the transference of EV-containing bioactive substances. microRNAs (miRNAs) are contained in EV cargo and are involved in the progression of heart failure. Over the past several years, a growing body of evidence has suggested that the biogenesis of miRNAs and EVs is tightly regulated, and the sorting of miRNAs into EVs is highly selective and tightly controlled. Extracellular miRNAs, particularly circulating EV-miRNAs, have shown promising potential as prognostic and diagnostic biomarkers for heart failure and as therapeutic targets. In this review, we summarize the latest progress concerning the role of EV-miRNAs in HF and their application in a therapeutic strategy development for heart failure.
Keywords: extracellular vesicles, microRNAs, sorting mechanism, biomarkers, heart failure
1. Introduction
Cardiovascular disease, including chronic heart failure (HF), is the number one cause of mortality and morbidity in the United States. The 2021 statistical update from the American Heart Association estimated more than 6 million Americans are living with HF. This equates to approximately 1.8% of the total US population, and this number will rise by 46% over the next several years to reach approximately 8 million by 2030 [1]. Accumulating evidence suggests that HF is a vicious cycle and neurohormonal dysregulation, including sympathetic nervous system excitation, the renin-angiotensin system activation, and others, contribute to the pathogenesis of HF [2,3,4,5,6,7,8].
It has also been well documented that clinically relevant signaling pathways (e.g., those activating angiotensin and adrenergic pathways) are well-coordinated during the development and progression of HF through a signature pattern of miRNA expression highly associated with cardiac hypertrophy and fibrosis in both mouse and human HF [9,10]. Importantly, these studies suggest that individual cardiac stress-inducible miRNAs, such as miR-208 and miR-195, are sufficient to provoke HF.
miRNAs are a class of noncoding RNAs and are well-known as fundamental regulators of gene expression by binding the 3′ UTR of targeting mRNAs or other regions, including the 5′ UTR of mRNA, coding sequence, and gene promoters to induce mRNA degradation or translational repression [11,12,13,14]. Despite the involvement of miRNAs in the pathophysiology of maladaptive remodeling in HF [15,16,17,18], extracellular miRNAs, especially those carried in extracellular vesicles (EVs), are promising biomarkers and paracrine mediators of intra and inter-organ communication as well as potential therapeutic targets. This review will focus on the roles of EV miRNAs in intercellular and inter-organ communication in the progression of HF and summarize the current progress in miRNA selectively packaged into EVs. We also focus on utilizing and targeting extracellular miRNAs as diagnostic biomarkers and therapy in HF.
2. miRNA Biogenesis and Extracellular Vesicle Selection
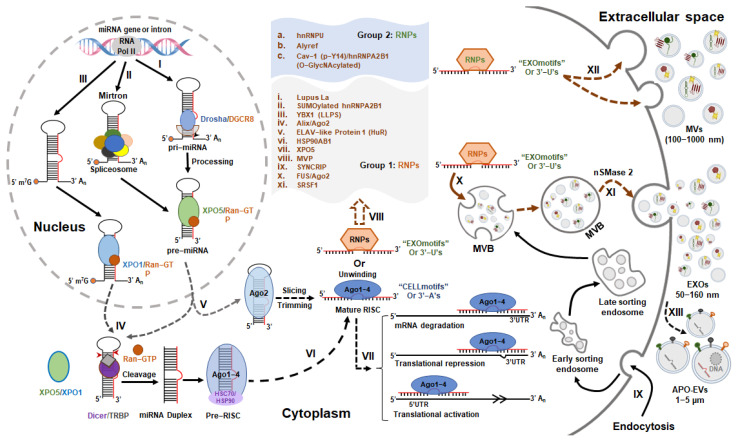
miRNAs, as a dominating class of small ncRNAs, are approximately 22 nucleotides in length and are produced by Drosha and Dicer, two RNase III proteins (see Figure 1).
Figure 1.
The biogenesis and potential sorting mechanisms of EV-miRNAs. The biogenesis of miRNAs is regulated by canonical (I) and non-canonical pathways (II and III), respectively. The latter is composed of Drosha/DGCR8-independent (II and III), Dicer-dependent (IV) and Dicer−independent pathways (V); The sorting sequences or 3′ modifications of miRNAs determine their incorporation in EVs (EXOmotifs or 3′−Uridylation) or cellular retention (CELLmotifs or 3′−Adenylation) [19,20]. The miRNAs with CELLmotifs or 3′−A’s are combined with AGO proteins to form the mature RISC (VI), and then mediate either the mRNA degradation or translational repression by binding to 3′ UTR, and also regulate the translational activation by binding to 5′ UTR (VII); The miRNAs with EXOmotifs or 3′−U’s are specifically recognized by RNA binding proteins (RNPs) (VIII), and are then sorted into microvesicles (MVs) by binding with group 2 RNPs (XII), or into Exosomes (EXOs) by binding with group 1 RNPs (X). In addition, the secretion of miRNAs is also controlled by neutral sphingomyelinase 2 (nSMase2) (XI) [21]. IX indicates the endocytosis process; XIII indicates the formation of apoptotic extracellular vesicles (APO-EVs); ALG-2-interacting protein X (Alix); Caveolin-1 (Cav-1); DiGeorge syndrome critical region 8 (DGCR8); ELAV-like protein 1 (or HuR, human antigen R); exosomes (EXOs); exportin 1 (XPO1); exportin 5 (XPO5); heat shock protein HSP 90-beta (HSP90AB1); heterogeneous nuclear ribonucleoprotein A2B1 (hnRNPA2B1); heterogeneous nuclear ribonucleoprotein U (hnRNPU); HIV-1 transactivating response (TAR) RNA-binding protein (TRBP); liquid-liquid phase separation (LLPS); major vault protein (MVP); microvesicles (MVs); multivesicular bodies (MVBs); Ras-related nuclear protein (RAN); RNA binding proteins (RNPs); RNA-induced silencing complex (RISC); RNA polymerase II (Pol II); serine/arginine-rich splicing factor 1 (SRSF1); synaptotagmin-binding cytoplasmic RNA-interacting protein (SYNCRIP); Y-box protein 1 (YBX1).
miRNAs mediate RNA silencing by targeting most protein-coding transcripts to modulate pathological processes associated with HF. Extracellular vesicles are natural membrane-bound nanoparticles released by all cells, have a wide range of diameters, and are produced by different intracellular pathways. A growing body of literature shows that EVs are important mediators of intercellular and intra-organ communication in the pathogenesis of HF by transferring bioactive materials, including miRNAs. To better understand the various roles of EV miRNAs in the progression of HF, it will be necessary to understand the biogenesis of miRNAs and EVs and the selection mechanisms of extracellular miRNAs.
2.1. miRNAs and Extracellular Vesicle Biogenesis
miRNA biogenesis is tightly controlled at all levels, including transcription, processing, modification, and Argonaute (AGO) protein loading as well as RNA decay [22]. Increasing evidence supports the view that dysregulation of miRNA biogenesis is associated with human HF [23,24,25,26]. miRNA biogenesis can be regulated either by the canonical pathway (Figure 1-I) or non-canonical pathways (Figure 1-II, III, V). The canonical pathway comprises a series of steps: First, miRNA transcription is carried out by RNA polymerase II (Pol II) and Pol II-associated transcription factors and epigenetic regulators to pri-miRNAs [27,28,29,30], followed by nuclear processing of pri-miRNAs by Drosha and DGCR8 (microprocessor complex) to pre-miRNAs [31,32]. Second, following nuclear events, nuclear export of pre-miRNAs is mediated by a transport complex comprising exportin 5 (XPO5) and GTP-binding RAN (Ras-related nuclear protein) in the cytoplasm [33], where pre-miRNAs are processed by Dicer, one RNase III-type enzyme, and TRBP (HIV-1 transactivating response (TAR) RNA-binding protein) to miRNA-duplex [34,35]. Third, selective miRNA-duplexes are loaded onto AGO proteins to form an RNA-induced silencing complex (RISC), unwinding the miRNA-duplexes. Theoretically, if one miRNA strand is selectively loaded onto an AGO protein to form the mature RISC, which further cleaves target mRNA or represses mRNA translation by binding to the 3′-UTR of mRNA [36,37], the other strand will be ejected from the RISC and subjected to degradation. However, increasing evidence not only suggests that miRNAs can bind to other regions of targets in addition to 3′-UTR including 5′-UTR, coding area, and promoter regions to activate translation or regulate transcription [38,39,40] but also both miRNA strands were found to functionally co-exist and participate in the pathogenesis of HF [41,42].
In addition to the canonical pathway, there are several non-canonical pathways involved in miRNA biogenesis. These non-canonical pathways are generally divided into two groups: Drosha/DGCR8-independent (Figure 1-II, III) and Dicer-independent pathways (Figure 1-V). Mirtron is one type of pre-miRNA produced from introns of mRNAs by splicing [43]. The 7-methylguanosine (m7G)-capped pre-miRNAs are also produced by Drosha/DGCR8-independent pathway [44]. Both pre-miRNAs are still dependent on Dicer-mediated cytoplasmic maturation, but they differ in nuclear export. Mirtron is exported by XPO5, whereas m7G-capped pre-miRNA is exported by XPO1 [22,44]. In addition, some miRNAs are made through Dicer-independent pathways (e.g., miR-451). The product of pri-miRNA-451 cleavage by Drosha is too short to be processed by Dicer, and pre-miRNA-451 will be directly loaded onto AGO2 and then sliced into an AGO-cleaved pre-miRNA-451 (ac-pre-miR-451), which will be further matured by poly (A)-specific ribonuclease PARN-mediated trimming [45].
Extracellular vesicles (EVs), as one type of membrane-enclosed nanoparticle, are attractive mediators of intercellular and inter-organ communication in various diseases, including HF [46,47,48,49]. Currently, EVs are divided into three types of vesicles in terms of their origin and mechanisms of biogenesis [50] (see Figure 1): (1) Exosomes (EXOs) (50–160 nm); (2) microvesicles (MVs) (100 nm–1000 nm) and (3) apoptotic bodies (APO-EVs) (1–5 μm). EXOs are a type of EV with an endosomal origin made by sequential invagination of the cell membrane resulting in the formation of multivesicular bodies (MVBs). The MVBs will ultimately generate exosomes by fusing with the plasma membrane and undergoing exocytosis [51,52]. Increasing evidence suggests that the biogenesis of EXOs is tightly regulated not only by the endosomal sorting complex required for transport (ESCRT) machinery, syndecan-syntenin-ALIX (Apoptosis-linked gene 2-interacting protein X), tetraspanins and ceramides during the formation of MVBs, but also by cytoskeletal elements, molecular motors and Ras-associated binding GTPases (RABs) during the transport/docking of MVBs from the cytoplasm to cell membrane. In addition, the final fusion of MVBs with the plasma membrane and the secretion of EXOs are driven by the soluble N-ethylmaleimide-sensitive factor attachment protein receptors (SNAREs), sGTPases, and calcium [50,52].
MVs are membrane-bound vesicles with a size range of 100 nm to 1000 nm, produced by direct budding and pinching of the plasma membrane. Although the biogenesis mechanisms are not as well understood, increasing evidence suggests that the formation of MVs is highly related to the regulation of cytoskeletal elements by small GTPases, such as Rho (RAS homolog) family and ADP-ribosylation factors (ARFs). They are also associated with the recruitment of the tumor susceptibility gene 101 (TSG101) by arrestin domain-containing protein 1 (ARRDC1) to the plasma membrane, facilitating the shedding and release of MVs [53,54].
Other than EXOs and MVs, apoptotic bodies are also EVs generated by dying cells during apoptosis and are generally recognized and engulfed by phagocytes [55]. However, recent studies have suggested that apoptotic bodies are generated by budding from the plasma membrane. The formation of apoptotic bodies is regulated by apoptotic cell disassembly via several molecular regulators, including ROCK, Pannexin-1, and Plexin-B2 (well-summarized in [56]). In addition, another novel beads-on-a-string membrane structure is also involved in the formation of apoptotic bodies [57]. Increasing evidence suggests that apoptotic bodies not only facilitate the clearance and degradation of apoptotic materials but also contain other biomolecular cargos (e.g., miRNAs, DNA, protein, and lipids) to mediate intercellular communication [58,59].
Although these membrane-bound vesicles differ in size distribution and mechanism of biogenesis, they are secreted by cells under various pathophysiological conditions into the extracellular space, where they mediate intercellular and inter-organ communication via EV bioactive substances, including proteins, RNAs, DNAs, and lipids. Accumulating evidence suggests that the packaging of cargos into EVs is highly selective and tightly regulated. In this review, we will also focus on the selective packaging of miRNAs into EVs.
2.2. Mechanisms of miRNA Selection into EVs
Extracellular miRNAs (Ex-miRs) have been found to be stably transported by ribonucleoproteins (RNPs), lipoproteins, and neutrophil extracellular traps [60,61,62]. However, it has become attractive to view EV function as intercellular and inter-organ mediators conveying their cargos, including noncoding RNAs, in particular, miRNAs. Interestingly, the existence of EV-miRs in the circulation of patients with cardiovascular diseases (CVDs), including HF, has raised the possibility that EV-miRs serve as prognostic and diagnostic markers and potential therapeutic targets [63,64,65]. However, the underlying mechanisms by which miRNAs are selectively secreted remain unclear.
In 2010, a study by Kosaka et al. [21] revealed that secretory miRNAs are regulated by the neutral sphingomyelinase 2 (nSMase 2), which regulates the biogenesis of ceramide and triggers exosome secretion, rather than by the ESCRT system, while the members of ESCRT regulate the biogenesis of EXOs. Increasing studies further suggest that the sorting of miRNA into EVs and their secretion are controlled by specific sequence motifs present in miRNAs that are recognized by RNA-binding Proteins (Figure 1-VIII), including heterogeneous nuclear ribonucleoprotein A2B1 (hnRNPA2B1) [66] and hnRNPU [67], Y-box protein 1 (YBX1) [68,69], synaptotagmin-binding cytoplasmic RNA-interacting protein (SYNCRIP) [70,71], ELAV-like protein 1 (or HuR, human antigen R) [72,73], HSP90AB1, XPO5 and major vault protein (MVP) [72,74], and serine/arginine splicing factor 1 (SRSF1) [75]. Recently, another RNA-binding protein, Lupus La, has been identified to mediate the selective sorting of miRNAs into EVs, and in particular, it selectively sorts miRNA-122 through the specific motifs located at the 3′ end of miRNA-122 [76]. Further studies by analyzing either the EV-enriched (EXOmotifs) or cell-enriched miRNA sequence (CELLmotifs) and structure revealed that the sorting sequences (EXOmotifs) present in miRNAs determine their secretion by EVs. Two novel RNA-binding proteins, Alyref and Fus, have also been identified to function as at least two RNA-binding proteins responsible for EXOmotif recognition and miRNA export into EVs [19].
Additionally, the post-translational modifications of some RNA-binding proteins, such as SUMOylation [66], oligomerization and ubiquitination [73], liquid-liquid phase separation (LLPS) [77], and O-GlcNAcylation [78], also control the sorting of miRNAs into EVs. Interestingly, cell activation-dependent alterations of miRNA targets promote the sorting of miRNAs into EVs [79], and modifications of miRNAs also determine the distribution of miRNA in EVs, such as 3′-end uridylation rather than adenylation [20]. In addition, the ALG-2-interacting protein X (Alix), an accessory protein of ESCRT, is also involved in the miRNA sorting to EVs by interacting with Ago2 and miRNAs during the EV biogenesis [80]. Caveolin-1 (Cav-1) was identified as the first membrane protein to be involved in the selective sorting of miRNAs to EVs by directly interacting with hnRNPA2B1, and the phosphorylation of Cav-1 at Y14 not only promotes the O-GlcNAcylation of hnRNPA2B1 but also enhances the interaction between Cav-1 and O-GlcNAcylated hnRNPA2B1, subsequently facilitating the trafficking of the Cav-1/hnRNPA2B1/miRNAs complex into MVs [78]. The studies and mechanisms cited above strongly support the conclusion that the sorting of miRNAs into EVs is highly selective and that EV secretion is tightly controlled, which may contribute to pathophysiological alterations in human diseases, including HF. For example, these EV sorting mechanisms of miRNAs have been potentially involved in the biogenesis of EV-miRNAs in heart failure (See Table 1).
Table 1.
The potential EV-sorting mechanisms of some HF-associated miRNAs.
| miRNAs | Sorting Mechanism | Functions in HF | Ref. |
|---|---|---|---|
| miR-122 | The binding of Lupus La protein, hnRNPU and/or HuR to miR122 controls extracellular export | Promote apoptosis, inflammation, fibrosis, pathological hypertrophy and remodeling | [73,76,81,82] |
| miR-223 | Selective sorting of miR-223 into EXOs by phase-separated YBX1 condensates | Promote cardiac fibrosis and hypertrophy | [69,77,83,84] |
| miR-34c-5p | The binding of Alyref and/or Fus to the CGGGAG motif at the 3′ end of miR-34c | Cardiac hypertrophy | [19,85] |
| miR-26a | The binding of Alyref and/or Fus to the CGGGAG motif at the 3′ end of miR-34c; alternatively, 3′-end uridylation of miR-26a | Protects the heart against hypertension-induced myocardial fibrosis | [19,20,86] |
| miR-30c-5p | The binding of hnRNPU to the AAMRUGCU motif of miR-30c-5p | Protects against myocardial ischemia/reperfusion injury | [67,87] |
| miR-17/92 | The binding of cav-1/hnRNPA2B1 complex to miR-17/92 regulates its MV sorting | Hypertrophic and arrhythmogenic cardiomyopathy | [78,88] |
| miR-1246 | The binding of SRSF1 to miR-1246 regulates its exosomal enrichment | Upregulated in diastolic dysfunction | [75,89] |
| miR-1231 | The binding hnRNPA2B1 to the GGAG EXOmotif at the 3′ end of miR-1231 | Induction of arrhythmias in ischemic hearts | [70,90] |
3. EV miRNAs in the Pathogenesis of Heart Failure
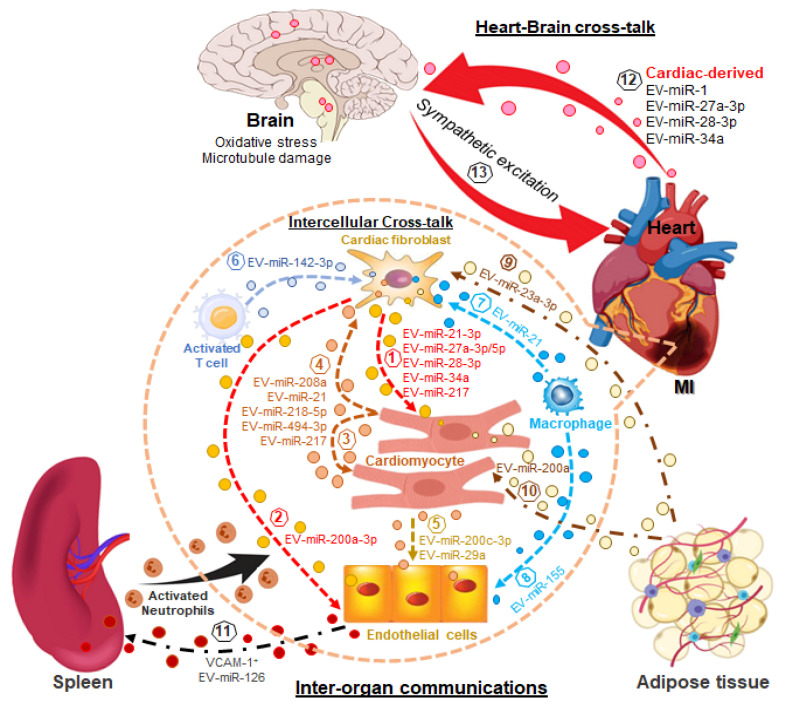
To better understand the role of EV-miRNAs in cardiac homeostasis and pathology, recent large-scale single-cell sequencing data revealed that the cellular composition of the adult human heart is heterogeneous and shows transcriptional and cellular diversity [91,92]. The human heart is composed of nine major cell types, including cardiomyocytes, cardiac fibroblasts, endothelial cells, macrophages, etc., and 20 sub-clusters of cell types within the heart [91]. Cardiac homeostasis is normally maintained by dynamic cell-cell and cell–extracellular matrix interactions [93]. When this cardiac homeostasis is disrupted, such as in response to cardiac disease or cardiac damage, the heart will undergo remodeling, which includes fibrosis and hypertrophy—both hallmarks of the HF state [94,95]. Extracellular vesicles are involved in both intercellular and inter-organ crosstalk via the effective transfer of bioactive substances into recipient cells, in particular miRNAs, which are key players in the pathogenesis of HF [96,97,98] (See Table 2, and as illustrated in Figure 2).
Table 2.
The EV-miRNAs in the pathogenesis of HF.
| Pathological Phenotype | miRNA | Cell Source | Target Cell | Potential Functional Mechanism | Ref. |
|---|---|---|---|---|---|
| Cardiac hypertrophy | miRNA-21-3p | CF | CM | Translational inhibition of both SORBS2 and PDLIM5 | [41] |
| miRNA-27a-5p | CF | CM | Translational inhibition of PDLIM5 | [42] | |
| miRNA-27a-3p, miRNA-28-3p miRNA-34a | CF | CM | Dysregulation of Nrf2/ARE signaling and oxidative stress | [99] | |
| miR-200a | Adipocyte | CM | Selective activation of PPARγ signaling and decreased TSC1 and subsequent mTOR activation | [100] | |
| miRNA-208a | CM | CM | Repression of Thrap1 and myostatin expression | [101,102] | |
| miRNA-217 | CF | CM | Targeting PTEN | [103] | |
| Cardiac fibrosis | miRNA-208a | CM | CF | Targeting Dyrk2 to promote NFAT dephosphorylation and nuclear translocation | [104] |
| miRNA-217 | CM | CF | Targeting PTEN | [103] | |
| miRNA-494-3p | CM | CF | Targeting PETN to enhance the phosphorylation of AKT, ERK, and SMAD2/3 | [105] | |
| miRNA-218-5p | CM | CF | Targeting TNFAIP3 to activate TGF-β signaling | [106] | |
| miRNA-23a-3p | Adipocyte | CF | Targeting RAP1 | [107] | |
| miR-142-3p | Activated CD4+ T cell | CF | Targeting APC to activate the WNT signaling pathway | [108] | |
| miRNA-21 | MP and/or CM | CF | Targeting Spry1 to augment ERK-MAP kinase activity | [109,110,111,112,113] | |
| Angiogenesis | miRNA-200c-3p | CM | EC | Impaired endothelial migration and tube formation, as well as a lower proliferation capacity | [114] |
| miRNA-29a | CM | EC | Inhibiting the proliferation, migration, and angiogenic ability of cardiac microvascular ECs | [115] | |
| miRNA-200a-3p | Activated CF | EC | Targeting ETS1/VEGF-A signaling axis | [116] | |
| miRNA-155 | Activated MP | EC | Targeting Sirt1/AMPKα2 and RAC1–PAK2 signaling pathways | [117] | |
| Inter-organ communications | miRNA-1 | CM | Neuron | Targeting TPPP/p25 to disturb the stability of neuronal microtubules | [102,118] |
| miRNA-27a-3p, miRNA-28-3p and miRNA-34a | CM and/or CF | Neuron | Targeting Nrf2/ARE signaling to induce oxidative stress and subsequently elicit sympathetic excitation | [49] | |
| miRNA-126 | EC | NEUT | Transcriptional activation of NEUTs and contribution to cardiac inflammation and chemokine production | [48,119,120] |
Abbreviations: adenomatous polyposis coli (APC), cardiac fibroblast (CF), cardiac myocyte (CM), dual-specificity tyrosine phosphorylation-regulated kinase 2 (Dyrk2), endothelial cell (EC), ETS Proto-Oncogene 1 (ETS1), macrophages (MP), neutrophils (NEUTs), nuclear factor of activated T cells (NFAT), Ras-related protein 1 (RAP1), Sprouty homolog 1 (Spry1), thyroid hormone-associated protein 1 (Thrap1), tuberous sclerosis complex (TSC1), tubulin polymerization promoting protein (TPPP/p25).
Figure 2.
EV miRNAs in the pathogenesis of heart failure via intercellular and inter-organ communication. miRNA-enriched EVs mediate intercellular communications: EVs from cardiac fibroblasts contribute to cardiac hypertrophy (1) and the impairment of angiogenic capacity (2); EVs derived from cardiomyocytes contribute to cardiac hypertrophy (3), fibrosis (4), and the impairment of endothelial proliferation, migration, and tube formation (5); EVs secreted by activated cardiac T cells (6) and macrophages (7) mediate cardiac fibrosis, and the inhibition of angiogenesis (8); miRNA-enriched EVs mediate inter-organ communications between adipose tissue (adipocytes) and cardiomyocytes and fibroblasts leading to fibrosis (9) and hypertrophy (10); heart (cardiac endothelial cells) and spleen (neutrophils) recruiting activated neutrophils to the ischemic region following MI increasing inflammation and promoting myocardial injury (11); cardiac derived cells communicate with neurons in the brain increasing oxidative stress and/or microtubule damage (12) eliciting sympathetic excitation which negatively regulates cardiac function in the setting of heart failure (13).
3.1. EV-miRNA in the Cardiac Hypertrophy
Under cardiac stress, the heart undergoes left ventricular hypertrophy, which is an initial compensatory mechanism. Although cardiac fibroblast-derived EVs play a critical role in inducing cardiac hypertrophy by activating the renin-angiotensin system in cardiomyocytes [121], the EV-enriched miRNAs secreted by cardiac fibroblasts in response to cardiac stress, such as miRNA-21-3p [41] and miRNA-27a-5p [42], can also be taken up by cardiomyocytes, resulting in the cardiac hypertrophy via translational inhibition of both SORBS2 and PDLIM5 [41] or PDLIM5 [42]. In addition, studies from our group also suggest that in response to cardiac stress, cardiac fibroblasts secrete EVs abundant with three miRNAs, including miRNA-27a, miRNA-28-3p, and miRNA-34a. They are taken up by cardiomyocytes, where they mediate the oxidative stress response by targeting Nrf2/ARE signaling, leading to cardiac hypertrophy [99]. In addition to cardiac fibroblasts, adipocytes increase miR-200a expression and secretion by EVs in response to selective activation of PPARγ signaling, and the uptake of EV-miR-200a by cardiomyocytes results in decreased tuberous sclerosis complex (TSC1) and subsequent mTOR activation, leading to cardiomyocyte hypertrophy [100].
3.2. EV-miRNA in the Cardiac Fibrosis
Cardiac fibrosis is another hallmark of chronic HF, characterized by extracellular matrix degradation and collagen accumulation. As one of the cardiac-specific miRNAs, miRNA-208a can also be secreted via EVs to mediate the intercellular communication between cardiomyocytes and cardiac fibroblasts and further facilitate cardiac fibroblast proliferation and differentiation into myofibroblasts [104], being transcribed by an intron of alpha-myosin heavy chain (Myh6) in cardiomyocytes, and contributes to cardiac hypertrophy and conduction defects in the heart [101,102]. This molecular mechanism further revealed that EV-miRNA-208a promotes cardiac fibrosis by targeting Dyrk2 (dual-specificity tyrosine phosphorylation-regulated kinase 2) to promote NFAT (nuclear factor of activated T cells) dephosphorylation and nuclear translocation, which triggers fibrosis. In addition, miRNA-217 was found to be elevated in the hearts of patients with chronic HF, and exogenous overexpression of miRNA-217 in cardiomyocytes in the thoracic aortic constriction (TAC)-induced HF model demonstrated enhanced pressure overload-induced cardiac dysfunction and cardiac remodeling (cardiac fibrosis and hypertrophy). Interestingly, miRNA-217 not only directly regulates cardiac hypertrophy but also indirectly contributes to cardiac fibrosis via cardiomyocyte-derived EVs by targeting PTEN in both cells [103]. Moreover, under cardiac stress, such as mechanical stretch and pressure overload, cardiomyocyte-specific Peli1 (Pellino E3 Ubiquitin Protein Ligase 1) has been involved in the enhanced transcription of miRNA-494-3p in cardiomyocytes via regulating NF-ĸB/AP-1 activation, and promotes the secretion of EV-enriched miRNA-494-3p into cardiac fibroblasts to activate cardiac fibroblasts by targeting PETN to enhance the phosphorylation of AKT, ERK, and SMAD2/3 [105]. Furthermore, HF patients with familial dilated cardiomyopathy also demonstrate late-stage cardiac fibrosis. A recent study using human iPSCs-derived cardiomyocytes as a disease model suggested that EVs derived from Ang II-stimulated DCM highly exhibit increased cardiac fibrosis and impaired cardiac function in vitro and in vivo compared to control cardiomyocytes via EV-enriched miRNA-218-5p targeting TNFAIP3 to activate TGF-β signaling [106]. Other than cardiomyocytes, Ang II-stimulated adipocytes can also secrete EV-enriched miRNA-23a-3p, which transforms cardiac fibroblasts into myofibroblasts and promotes collagen accumulation by targeting RAP1 (Ras-related protein 1) [107]. In addition, cardiac infiltration of CD4+ T cells is implicated in the healing process post-myocardial infarction (MI), contributing to cardiac fibrosis and dysfunction [122]. A mechanistic study further revealed that cardiac-activated CD4+ T cells can transport excessive miR-142-3p via EVs into cardiac fibroblasts in which miR-143-3p activates the WNT signaling pathway by targeting APC (adenomatous polyposis coli) to transform cardiac fibroblasts into activated myofibroblasts boosting post-ischemic ventricular remodeling in the progression of HF [108]. It has been well-documented that miRNA-21 is a central regulator of cardiac fibrosis in HF and shows therapeutic potential as a target for HF treatment [109,110,111,112]. Recently, using the TAC-induced HF model combined with single-cell sequencing, bioinformatics analyses revealed that EV-enriched miR-21 also determines macrophage-fibroblast crosstalk and promotes the transition from cardiac fibroblasts to activated myofibroblasts, leading to cardiac fibrosis [113].
3.3. EV-miRNA in Cardiac Angiogenesis during Heart Failure
In response to cardiac injury, intercellular communication is fundamental for maintaining homeostasis and integrity. The aforementioned studies have demonstrated that EV-enriched miRNAs derived from other types of cardiac cells, including macrophages, T cells, and adipocytes, contribute to cardiac fibrosis and/or hypertrophy in HF. EVs secreted from cardiomyocytes also play an important role in anti-angiogenesis through miRNA transfer in HF. Recently, miRNA-200c-3p has been found to be one of the most enriched miRNAs in hypertrophic cardiomyocyte-derived EVs under pressure overload and was transported into endothelial cells (ECs) in which it functions as a detrimental anti-angiogenic factor to impair endothelial function including proliferation, migration, and tube formation [114]. It has also been shown that hypertrophic cardiomyocytes induced by Ang II also release miRNA-29a via EVs to inhibit the proliferation, migration, and angiogenic ability of cardiac microvascular ECs [115]. Other than hypertrophic cardiomyocytes, activated cardiac fibroblasts can also secrete EVs abundant with miRNA-200a-3p, which mediates the cross-talk between cardiac endothelial cells and induces endothelial dysfunction by targeting the ETS1/VEGF-A signaling axis [116]. A recent study also suggested that M1 macrophages secrete pro-inflammatory EVs post-MI, which exert anti-angiogenic effects by transferring EV-enriched miR-155 into cardiac ECs to inhibit the angiogenesis and further accelerate MI injury by targeting the Sirt1/AMPKα2-endothelial nitric oxide synthase and RAC1-PAK2 signaling pathways [117].
As discussed above, cardiac EV-enriched miRNA-mediated intercellular communications play an important role in the pathogenesis of HF. However, recent studies [49,118] highlight the possibility that cardiac-derived EVs contribute to inter-organ communication during the progression of HF.
3.4. Cardiac EV miRNA-Mediated Inter-Organ Communication in Heart Failure
Increasing evidence suggests that heart-brain communication at the miRNA level contributes to neuronal dysfunction in the brain mediated by EVs in the HF state [49,118]. miRNA-1 is a cardiac miRNA abundantly expressed in the myocardium [102]. Circulating miRNA-1 was significantly increased in patients with acute myocardial infarction (AMI) [102,123]. Interestingly, cardiac-derived miRNA-1 can be transported from the infarcted heart into the hippocampus via EVs, where cardiac miRNA-1 causes neuronal microtubular damage. This is independent of brain hypoperfusion induced by MI [118], suggesting a novel mechanism by which the damaged heart contributes to brain dysfunction. A study from our group also demonstrated that cardiac-derived miRNAs can be sorted into EVs and circulate into the rostral ventrolateral medulla (RVLM) of the brain stem, where these miRNAs evoke sympathetic excitation by targeting Nrf2/ARE signaling to induce oxidative stress [49]. Moreover, it is well-documented that neutrophils promote the progression of acute MI by releasing ROS, granular components, and extracellular traps to aggravate inflammation [124,125]. Clinical evidence also shows that the numbers of peripheral blood neutrophils and plasma EVs correlate closely with the extent of acute MI, including infarct size, mortality, and HF development [48,126,127]. Interestingly, miRNA analysis of human plasma EVs from patients with AMI demonstrated twelve significantly enriched miRNAs, and two out of twelve, including miRNA-126-3p and -5p, were highly regulated and secreted by ECs post- acute MI and are responsible for cell adhesion and chemotaxis [119]. Importantly, recent studies from the same group revealed that cardiac ECs in response to cardiac injury rapidly release VCAM-1+ EVs containing miRNA-126, which preferentially mediate heart-spleen communication. These VCAM-1+ EVs rapidly and selectively recruit splenic neutrophils to peripheral blood following myocardial injury. Mechanistic studies further suggest that VCAM-1+ EVs-enriched miRNA-126 induces the transcriptional activation of neutrophils in the spleen before they arrive at the ischemic myocardium, contributing to local inflammation and chemokine production [48,120]. In addition, genetic deletion of VCAM-1 from EVs by the CRISPR-Cas9 system or silencing miRNA-126 in vivo by antagomir significantly blocked the mobilization of splenic neutrophils to the ischemic myocardium and reduced myocardial infarct size in a LAD ligation mouse model. This suggests that specific surface proteins such as VCAM-1 in EVs will determine their organotropism and functionalities of EVs.
4. Extracellular Vesicle miRNA-Based Prognosis, Diagnosis and Therapeutics of Heart Failure
Although natriuretic peptides and cardiac troponins are currently the most widely employed biomarkers for the prognosis and diagnosis of HF, next-generation biomarkers, including soluble source of tumorigenicity 2 (sST2), proenkephalin, growth differentiation factor-15 (GDF-15), and galectin-3 (Gal-3) have also been well-established as promising biomarkers for HF diagnosis and prognosis [128,129]. The discovery of altered levels of circulating miRNAs in patients with HF provides the possibility to utilize circulating miRNAs, in particular, EV-enriched miRNAs, as biomarkers for HF [63,64,130] (See Table 3).
Table 3.
The significance of EV-miRNAs as diagnostic and prognostic biomarkers in heart failure.
| miRNA | Biomarker Type | Regulation in HF | Source of miRNAs | Cohort Size | Analysis Method | Ref. |
|---|---|---|---|---|---|---|
| miR-92-5p | Diagnostic | Up | Serum (H) | n = 28 | qRT-PCR | [131] |
| miR-146a | Up | Plasma (H) | n = 192 | qRT-PCR | [132,133] | |
| miR-181c | Up | Serum (H) | n = 57 | qRT-PCR | [134] | |
| miR-495 | Up | Plasma (D) | n = 11 | qRT-PCR | [135] | |
| miR-192 | Prognostic | Up | Plasma (H) | n = 91 | qRT-PCR | [136] |
| miR-34a | Up | Plasma (H) | n = 359 | qRT-PCR | [137] | |
| miR-194 | Up | Serum (H) | n = 21 | qRT-PCR | [138] | |
| miR-425 | Down | Serum (H) | n = 31 | qRT-PCR | [139] | |
| miR-744 | Down | Serum (H) | n = 31 | qRT-PCR | [139] | |
| miR-30d | Prognostic for CRT response | Down | Plasma (H) | n = 92 | qRT-PCR | [140] |
Abbreviations: cardiac resynchronization therapy (CRT); human (H); dog (D).
Recently, circulating EV-miRNAs have been emerging as non-invasive prognostic and diagnostic biomarkers for HF, and their potential clinical applications have been well-summarized [141]. For example, some circulating EV-miRNAs, including miR-92-5p, miR-146a, miR-181c, and miR-495, showed diagnostic potential for HF, and other EV-enriched miRNAs, such as miR-192, miR-34a, miR-425, and miR-744, represent promising prognostic biomarkers for HF. Moreover, two circulating EV-enriched miRNAs associated with HF, including miR-30d-5p and miR-126a-5p, have shown promising potential as biomarkers for HFpEF (heart failure with preserved ejection fraction) in diabetes mellitus because their down-regulations in circulating EVs and the left ventricle remain consistently correlated with decreased cardiac output [142]. In addition, circulating miR-30d, especially EV-miR-30d, has shown high potential as a biomarker to evaluate left ventricular remodeling and clinical outcomes for patients with HF [140,143].
Other than serving as prognostic and diagnostic biomarkers, EV-miRNAs have been used as therapeutic targets for HF (See Table 4). Some miRNAs such as miR-126, miR-146a, miR-125a-5p, miR-125b-5p, miR-29b, miR-98-5p, miR-30e, and miR-30d have shown protective effects on cardiac function. Extracellular vesicle-based delivery of these miRNAs shows promising clinical applications in HF therapy [144,145,146,147,148,149,150]. A recent study showed the beneficial effects of adipose tissue-derived mesenchymal stem cell (ADSC)-derived EVs on acute MI-induced cardiac injury by EV-enriched miR-205, suggesting a promising therapeutic potential [151]. Moreover, increasing evidence suggests that EVs secreted by other stem cells, including human cardiac progenitors (hCPCs), mesenchymal stem cells (MSCs), and induced pluripotent stem cells (iPSCs), demonstrate angiogenic and cardioprotective properties in MI rodent models by significantly increasing the proliferation, migration, and tube formation of endothelial cells [152,153,154]. EV miRNA profiling further revealed that some angiogenic and cardioprotective miRNAs, such as miR-210 [152,153,154], miR-126, and miR-17-92 [154], are highly enriched in these stem cell-derived EVs. For example, silencing the miR-210 of MSC-EVs significantly impaired the pro-angiogenic effects in vitro and in a mouse MI model [153]. Recently, human umbilical cord mesenchymal stem cell-derived EVs pre-loaded with miR-29b mimics also demonstrated effective antifibrotic activity to prevent excessive cardiac fibrosis post-MI [146]. These studies suggest that endogenous miRNAs enriched in stem cell-derived EVs or exogenous miRNA mimics pre-loaded into stem cell-EVs exhibit a potential for MI therapy. Although stem cell-derived EV-miRNAs have shown promising therapeutic potential for HF management, it remains questionable if the beneficial contributions of other EV components, such as proteins, lipids, and various metabolites, affect cardiac function in the treatment of HF. Moreover, an interesting new therapeutic direction relates to the effects of stem cell-derived EVs in HF by engineering EVs with cardiac homing peptides and using genetic therapeutics for the delivery of miRNA-21 to effectively restore cardiac function after MI [155]. For example, hypoxia-conditioned BM-MSCs (bone marrow mesenchymal stem cells) secreted EVs abundant with miRNA-125b-5p. A cardioprotective miRNA demonstrated high specificity to the ischemic myocardium in a mouse model of acute MI when miR-125-enriched EVs were conjugated with an ischemic myocardium-targeted peptide and then administered by intravenous injection [144]. Alternatively, targeting injured cardiac-secreted EVs by exogenously pre-loading miRNA inhibitors (i.e., antagomirs) into EVs, such as miR-27a, miR-28, and miR-34a [49], as well as miR-126 [48], may represent another therapeutic strategy.
Table 4.
The potential therapeutic applications of stem cell-derived EV miRNAs in heart failure.
| miRNA | Sources | Animal Model | Function | Ref. |
|---|---|---|---|---|
| miR-125b-5p | MSC-derived hypo-EVs |
MI | Suppress the expression of the pro-apoptotic genes p53 and BAK1 in cardiomyocytes | [144] |
| miR-98-5p | hypoxic BMMSCs | I/R | Targeting TLR4 and the PI3K/Akt signaling pathway | [145] |
| miR-29b | Exogenously loaded | MI | Antifibrotic activity to prevent excessive cardiac fibrosis | [146] |
| miR-129-5p | MSCs | MI | Targeting TRAF3 and the following NF-κB signaling | [147] |
| miR-126 | ADSC | AMI | Protecting cardiac cells from apoptosis, inflammation, fibrosis, and increased angiogenesis. | [156] |
| miR-146a | ADSCs | AMI | Targeting EGR1 to attenuate AMI-induced myocardial damage | [157] |
| miR-125a-5p | MSCs | I/R | Increase M2 macrophage polarization, promote angiogenesis, and attenuate fibroblast proliferation and activation | [150] |
| miR-205 | ADSC | MI | Promote the proliferation and migration of ECs, facilitate angiogenesis, and inhibit cardiomyocyte apoptosis | [151] |
| miRNA-21 | Exogenously loaded | MI | Reduce the PDCD4 expression and attenuate cell apoptosis | [155] |
| miR-30e | MSCs | MI | Inhibit LOX1 expression and impair the NF-κB p65/Cas-9 signaling | [147] |
| miR-210 | MSCs | MI | Targeting Efna3 to improve angiogenesis | [153] |
| miR-17-92 | CPCs | I/R | Inhibit fibrosis | [158] |
Abbreviations: adipose tissue-derived mesenchymal stem cell (ADSC); acute myocardial infarction (AMI); bone marrow mesenchymal stem cells (BMMSCs); cardiac progenitor cells (CPCs); Early growth response factor 1 (EGR1); ephrin A3 (Efna3); lectin-like oxidized low-density lipoprotein receptor 1 (LOX1); ischemia-reperfusion (I/R); mesenchymal stem cells (MSCs); myocardial infarction (MI); programmed cell death 4 (PDCD4).
5. Perspectives and Future Directions
Extracellular vesicle miRNAs are attractive candidates as diagnostic and prognostic biomarkers as well as therapeutic targets. However, using EV-miRNAs for these purposes still faces great challenges in becoming well-accepted biomarkers for prognosis and diagnosis of HF. First, rigorous standards for performing EV research are imperative and are time-consuming processes, including EV categorization, purification, and separation technology development and characterization. Uniform standard guidelines are urgently needed in the field. Second, the pathogenesis of HF is complicated, and cardiac function is also influenced by systemic communication with other organs. Selective criteria are needed to evaluate the potential of EV-miRNAs for use as diagnostic and prognostic biomarkers for HF. In addition, the cell origins and categories of circulating EVs are heterogeneous, and the exploration of cell origin and sorting mechanisms of circulating EV-miRNAs will be of interest to better understand the pathophysiological functions of circulating EV-miRNAs in HF. Third, the sample size used for evaluating circulating EV-miRNAs as biomarkers for HF is still relatively small, which is insufficient to support their use as sensitive biomarkers at this time.
Although EVs have exhibited excellent properties and functions, including regulatory ability, physical stability, and immunogenicity, which render EVs a potential novel platform for drug delivery and precision therapy, the targeting specificity and delivery efficiency remain challenges. A cardiac homing peptide-guided delivery system has been used for the treatment of MI [159,160]. Given that cardiac-derived EVs also contribute to neuronal dysfunction in the brain in HF [49,118], engineered EVs derived from dendritic cells expressing Lamp2b (an exosomal membrane protein), fused to the neuron-specific RVG peptide [161], may be therapeutically used for HF management. In addition, the next generation of “Hybrid EVs” [162] produced by stem cell-derived EVs fused with modified liposomes may represent an innovative therapeutic strategy for HF treatment. The resulting hybrid EVs will not only possess the intrinsic immunomodulatory effects and blood barrier penetrating ability of original stem cell-derived EVs but also highly enrich some cardioprotective miRNAs by pre-loading them into parental liposomes. Importantly, the parental partners can be modified by either engineering them with organotropic peptides or integrating multimodal imaging capability for clinical tracking, guiding, and optimizing. Taken together, miRNAs are differentially regulated in response to heart injury and selectively sorted into EVs, contributing to the pathogenesis of HF via intercellular and/or inter-organ communications, which makes it possible to become a promising type of prognostic and diagnostic biomarker and therapeutic target for HF.
Author Contributions
C.T. and I.H.Z. conceived of the subject matter of this review. C.T. summarized the published results and drafted the manuscript. C.T., J.N.Z. and I.H.Z. revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by the National Institution of Health Grant R01HL153176 to IHZ/CT; American Heart Association (AHA) Career Development Award (19CDA34520004) to C.T.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Roger V.L. Epidemiology of Heart Failure: A Contemporary Perspective. Circ. Res. 2021;128:1421–1434. doi: 10.1161/CIRCRESAHA.121.318172. [DOI] [PubMed] [Google Scholar]
- 2.Wollert K.C., Drexler H. The renin–angiotensin system and experimental heart failure. Cardiovasc. Res. 1999;43:838–849. doi: 10.1016/S0008-6363(99)00145-5. [DOI] [PubMed] [Google Scholar]
- 3.Verbrugge F.H., Tang W.H.W., Mullens W. Renin-Angiotensin-Aldosterone System Activation During Decongestion in Acute Heart Failure. JACC Heart Fail. 2015;3:108–111. doi: 10.1016/j.jchf.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Jia G., Aroor A.R., Hill M.A., Sowers J.R. Role of Renin-Angiotensin-Aldosterone System Activation in Promoting Cardiovascular Fibrosis and Stiffness. Hypertension. 2018;72:537–548. doi: 10.1161/HYPERTENSIONAHA.118.11065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Florea V.G., Cohn J.N. The autonomic nervous system and heart failure. Circ. Res. 2014;114:1815–1826. doi: 10.1161/CIRCRESAHA.114.302589. [DOI] [PubMed] [Google Scholar]
- 6.Kishi T. Heart failure as an autonomic nervous system dysfunction. J. Cardiol. 2012;59:117–122. doi: 10.1016/j.jjcc.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Zhang D.Y., Anderson A.S. The sympathetic nervous system and heart failure. Cardiol. Clin. 2014;32:33–45. doi: 10.1016/j.ccl.2013.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Booth L.C., May C.N., Yao S.T. The role of the renal afferent and efferent nerve fibers in heart failure. Front. Physiol. 2015;6:270. doi: 10.3389/fphys.2015.00270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Rooij E., Sutherland L.B., Liu N., Williams A.H., McAnally J., Gerard R.D., Richardson J.A., Olson E.N. A signature pattern of stress-responsive microRNAs that can evoke cardiac hypertrophy and heart failure. Proc. Natl. Acad. Sci. USA. 2006;103:18255–18260. doi: 10.1073/pnas.0608791103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Rooij E., Sutherland L.B., Qi X., Richardson J.A., Hill J., Olson E.N. Control of stress-dependent cardiac growth and gene expression by a microRNA. Science. 2007;316:575–579. doi: 10.1126/science.1139089. [DOI] [PubMed] [Google Scholar]
- 11.Younger S.T., Corey D.R. Transcriptional gene silencing in mammalian cells by miRNA mimics that target gene promoters. Nucleic Acids Res. 2011;39:5682–5691. doi: 10.1093/nar/gkr155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lytle J.R., Yario T.A., Steitz J.A. Target mRNAs are repressed as efficiently by microRNA-binding sites in the 5′ UTR as in the 3′ UTR. Proc. Natl. Acad. Sci. USA. 2007;104:9667–9672. doi: 10.1073/pnas.0703820104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tay Y., Zhang J., Thomson A.M., Lim B., Rigoutsos I. MicroRNAs to Nanog, Oct4 and Sox2 coding regions modulate embryonic stem cell differentiation. Nature. 2008;455:1124–1128. doi: 10.1038/nature07299. [DOI] [PubMed] [Google Scholar]
- 14.Gu W., Xu Y., Xie X., Wang T., Ko J.H., Zhou T. The role of RNA structure at 5′ untranslated region in microRNA-mediated gene regulation. RNA. 2014;20:1369–1375. doi: 10.1261/rna.044792.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumarswamy R., Thum T. Non-coding RNAs in cardiac remodeling and heart failure. Circ. Res. 2013;113:676–689. doi: 10.1161/CIRCRESAHA.113.300226. [DOI] [PubMed] [Google Scholar]
- 16.Melman Y.F., Shah R., Das S. MicroRNAs in heart failure: Is the picture becoming less miRky? Circ. Heart Fail. 2014;7:203–214. doi: 10.1161/CIRCHEARTFAILURE.113.000266. [DOI] [PubMed] [Google Scholar]
- 17.Gholaminejad A., Zare N., Dana N., Shafie D., Mani A., Javanmard S.H. A meta-analysis of microRNA expression profiling studies in heart failure. Heart Fail. Rev. 2021;26:997–1021. doi: 10.1007/s10741-020-10071-9. [DOI] [PubMed] [Google Scholar]
- 18.Shen N.N., Wang J.L., Fu Y.P. The microRNA Expression Profiling in Heart Failure: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 2022;9:856358. doi: 10.3389/fcvm.2022.856358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garcia-Martin R., Wang G., Brandão B.B., Zanotto T.M., Shah S., Kumar Patel S., Schilling B., Kahn C.R. MicroRNA sequence codes for small extracellular vesicle release and cellular retention. Nature. 2022;601:446–451. doi: 10.1038/s41586-021-04234-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koppers-Lalic D., Hackenberg M., Bijnsdorp I.V., van Eijndhoven M.A.J., Sadek P., Sie D., Zini N., Middeldorp J.M., Ylstra B., de Menezes R.X., et al. Nontemplated nucleotide additions distinguish the small RNA composition in cells from exosomes. Cell Rep. 2014;8:1649–1658. doi: 10.1016/j.celrep.2014.08.027. [DOI] [PubMed] [Google Scholar]
- 21.Kosaka N., Iguchi H., Yoshioka Y., Takeshita F., Matsuki Y., Ochiya T. Secretory mechanisms and intercellular transfer of microRNAs in living cells. J. Biol. Chem. 2010;285:17442–17452. doi: 10.1074/jbc.M110.107821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ha M., Kim V.N. Regulation of microRNA biogenesis. Nat. Rev. Mol. Cell Biol. 2014;15:509–524. doi: 10.1038/nrm3838. [DOI] [PubMed] [Google Scholar]
- 23.Takagi M., Ono S., Kumaki T., Nishimura N., Murakami H., Enomoto Y., Naruto T., Ueda H., Kurosawa K. Complex congenital cardiovascular anomaly in a patient with AGO1-associated disorder. Am. J. Med. Genet. A. 2023;191:882–892. doi: 10.1002/ajmg.a.63089. [DOI] [PubMed] [Google Scholar]
- 24.Kumari R., Ranjan P., Suleiman Z.G., Goswami S.K., Li J., Prasad R., Verma S.K. mRNA modifications in cardiovascular biology and disease: With a focus on m6A modification. Cardiovasc. Res. 2022;118:1680–1692. doi: 10.1093/cvr/cvab160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhu M., Gao J., Lin X.J., Gong Y.Y., Qi Y.C., Ma Y.L., Song Y.X., Tan W., Li F.Y., Ye M., et al. Novel roles of an intragenic G-quadruplex in controlling microRNA expression and cardiac function. Nucleic Acids Res. 2021;49:2522–2536. doi: 10.1093/nar/gkab055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Da Costa Martins P.A., Bourajjaj M., Gladka M., Kortland M., van Oort R.J., Pinto Y.M., Molkentin J.D., De Windt L.J. Conditional dicer gene deletion in the postnatal myocardium provokes spontaneous cardiac remodeling. Circulation. 2008;118:1567–1576. doi: 10.1161/CIRCULATIONAHA.108.769984. [DOI] [PubMed] [Google Scholar]
- 27.Varela M.A., Roberts T.C., Wood M.J. Epigenetics and ncRNAs in brain function and disease: Mechanisms and prospects for therapy. Neurotherapeutics. 2013;10:621–631. doi: 10.1007/s13311-013-0212-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee Y., Kim M., Han J., Yeom K.H., Lee S., Baek S.H., Kim V.N. MicroRNA genes are transcribed by RNA polymerase II. EMBO J. 2004;23:4051–4060. doi: 10.1038/sj.emboj.7600385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krol J., Loedige I., Filipowicz W. The widespread regulation of microRNA biogenesis, function and decay. Nat. Rev. Genet. 2010;11:597–610. doi: 10.1038/nrg2843. [DOI] [PubMed] [Google Scholar]
- 30.Davis-Dusenbery B.N., Hata A. Mechanisms of control of microRNA biogenesis. J. Biochem. 2010;148:381–392. doi: 10.1093/jb/mvq096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee Y., Jeon K., Lee J.T., Kim S., Kim V.N. MicroRNA maturation: Stepwise processing and subcellular localization. EMBO J. 2002;21:4663–4670. doi: 10.1093/emboj/cdf476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gregory R.I., Yan K.P., Amuthan G., Chendrimada T., Doratotaj B., Cooch N., Shiekhattar R. The Microprocessor complex mediates the genesis of microRNAs. Nature. 2004;432:235–240. doi: 10.1038/nature03120. [DOI] [PubMed] [Google Scholar]
- 33.Lund E., Güttinger S., Calado A., Dahlberg J.E., Kutay U. Nuclear export of microRNA precursors. Science. 2004;303:95–98. doi: 10.1126/science.1090599. [DOI] [PubMed] [Google Scholar]
- 34.Park J.E., Heo I., Tian Y., Simanshu D.K., Chang H., Jee D., Patel D.J., Kim V.N. Dicer recognizes the 5′ end of RNA for efficient and accurate processing. Nature. 2011;475:201–205. doi: 10.1038/nature10198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Benoit M.P., Imbert L., Palencia A., Pérard J., Ebel C., Boisbouvier J., Plevin M.J. The RNA-binding region of human TRBP interacts with microRNA precursors through two independent domains. Nucleic Acids Res. 2013;41:4241–4252. doi: 10.1093/nar/gkt086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mourelatos Z., Dostie J., Paushkin S., Sharma A., Charroux B., Abel L., Rappsilber J., Mann M., Dreyfuss G. miRNPs: A novel class of ribonucleoproteins containing numerous microRNAs. Genes Dev. 2002;16:720–728. doi: 10.1101/gad.974702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kawamata T., Tomari Y. Making RISC. Trends Biochem. Sci. 2010;35:368–376. doi: 10.1016/j.tibs.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 38.Ni W.J., Leng X.M. miRNA-Dependent Activation of mRNA Translation. Microrna. 2016;5:83–86. doi: 10.2174/2211536605666160825151201. [DOI] [PubMed] [Google Scholar]
- 39.O’Brien J., Hayder H., Zayed Y., Peng C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018;9:402. doi: 10.3389/fendo.2018.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee S., Vasudevan S. Post-transcriptional stimulation of gene expression by microRNAs. Adv. Exp. Med. Biol. 2013;768:97–126. doi: 10.1007/978-1-4614-5107-5_7. [DOI] [PubMed] [Google Scholar]
- 41.Bang C., Batkai S., Dangwal S., Gupta S.K., Foinquinos A., Holzmann A., Just A., Remke J., Zimmer K., Zeug A., et al. Cardiac fibroblast-derived microRNA passenger strand-enriched exosomes mediate cardiomyocyte hypertrophy. J. Clin. Investig. 2014;124:2136–2146. doi: 10.1172/JCI70577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tian C., Hu G., Gao L., Hackfort B.T., Zucker I.H. Extracellular vesicular MicroRNA-27a* contributes to cardiac hypertrophy in chronic heart failure. J. Mol. Cell. Cardiol. 2020;143:120–131. doi: 10.1016/j.yjmcc.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ruby J.G., Jan C.H., Bartel D.P. Intronic microRNA precursors that bypass Drosha processing. Nature. 2007;448:83–86. doi: 10.1038/nature05983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xie M., Li M., Vilborg A., Lee N., Shu M.D., Yartseva V., Šestan N., Steitz J.A. Mammalian 5′-capped microRNA precursors that generate a single microRNA. Cell. 2013;155:1568–1580. doi: 10.1016/j.cell.2013.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cheloufi S., Dos Santos C.O., Chong M.M., Hannon G.J. A dicer-independent miRNA biogenesis pathway that requires Ago catalysis. Nature. 2010;465:584–589. doi: 10.1038/nature09092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Michel L.Y.M. Extracellular Vesicles in Adipose Tissue Communication with the Healthy and Pathological Heart. Int. J. Mol. Sci. 2023;24:7745. doi: 10.3390/ijms24097745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yuan Y., Mei Z., Qu Z., Li G., Yu S., Liu Y., Liu K., Shen Z., Pu J., Wang Y., et al. Exosomes secreted from cardiomyocytes suppress the sensitivity of tumor ferroptosis in ischemic heart failure. Signal Transduct. Target. Ther. 2023;8:121. doi: 10.1038/s41392-023-01336-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akbar N., Braithwaite A.T., Corr E.M., Koelwyn G.J., van Solingen C., Cochain C., Saliba A.E., Corbin A., Pezzolla D., Møller Jørgensen M., et al. Rapid neutrophil mobilization by VCAM-1+ endothelial cell-derived extracellular vesicles. Cardiovasc. Res. 2023;119:236–251. doi: 10.1093/cvr/cvac012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tian C., Gao L., Rudebush T.L., Yu L., Zucker I.H. Extracellular Vesicles Regulate Sympatho-Excitation by Nrf2 in Heart Failure. Circ. Res. 2022;131:687–700. doi: 10.1161/CIRCRESAHA.122.320916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rädler J., Gupta D., Zickler A., Andaloussi S.E. Exploiting the biogenesis of extracellular vesicles for bioengineering and therapeutic cargo loading. Mol. Ther. 2023;31:1231–1250. doi: 10.1016/j.ymthe.2023.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Van Niel G., D’Angelo G., Raposo G. Shedding light on the cell biology of extracellular vesicles. Nat. Rev. Mol. Cell Biol. 2018;19:213–228. doi: 10.1038/nrm.2017.125. [DOI] [PubMed] [Google Scholar]
- 52.Kalluri R., LeBleu V.S. The biology, function, and biomedical applications of exosomes. Science. 2020;367:eaau6977. doi: 10.1126/science.aau6977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nabhan J.F., Hu R., Oh R.S., Cohen S.N., Lu Q. Formation and release of arrestin domain-containing protein 1-mediated microvesicles (ARMMs) at plasma membrane by recruitment of TSG101 protein. Proc. Natl. Acad. Sci. USA. 2012;109:4146–4151. doi: 10.1073/pnas.1200448109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Clancy J.W., Schmidtmann M., D’Souza-Schorey C. The ins and outs of microvesicles. FASEB BioAdv. 2021;3:399–406. doi: 10.1096/fba.2020-00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Segawa K., Nagata S. An Apoptotic ‘Eat Me’ Signal: Phosphatidylserine Exposure. Trends Cell Biol. 2015;25:639–650. doi: 10.1016/j.tcb.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 56.Ozkocak D.C., Phan T.K., Poon I.K.H. Translating extracellular vesicle packaging into therapeutic applications. Front. Immunol. 2022;13:946422. doi: 10.3389/fimmu.2022.946422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Atkin-Smith G.K., Tixeira R., Paone S., Mathivanan S., Collins C., Liem M., Goodall K.J., Ravichandran K.S., Hulett M.D., Poon I.K. A novel mechanism of generating extracellular vesicles during apoptosis via a beads-on-a-string membrane structure. Nat. Commun. 2015;6:7439. doi: 10.1038/ncomms8439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Holmgren L., Szeles A., Rajnavölgyi E., Folkman J., Klein G., Ernberg I., Falk K.I. Horizontal transfer of DNA by the uptake of apoptotic bodies. Blood. 1999;93:3956–3963. doi: 10.1182/blood.V93.11.3956. [DOI] [PubMed] [Google Scholar]
- 59.Bergsmedh A., Szeles A., Henriksson M., Bratt A., Folkman M.J., Spetz A.L., Holmgren L. Horizontal transfer of oncogenes by uptake of apoptotic bodies. Proc. Natl. Acad. Sci. USA. 2001;98:6407–6411. doi: 10.1073/pnas.101129998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vickers K.C., Palmisano B.T., Shoucri B.M., Shamburek R.D., Remaley A.T. MicroRNAs are transported in plasma and delivered to recipient cells by high-density lipoproteins. Nat. Cell Biol. 2011;13:423–433. doi: 10.1038/ncb2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Linhares-Lacerda L., Temerozo J.R., Ribeiro-Alves M., Azevedo E.P., Mojoli A., Nascimento M.T.C., Silva-Oliveira G., Savino W., Foguel D., Bou-Habib D.C., et al. Neutrophil extracellular trap-enriched supernatants carry microRNAs able to modulate TNF-α production by macrophages. Sci. Rep. 2020;10:2715. doi: 10.1038/s41598-020-59486-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Das S., Ansel K.M., Bitzer M., Breakefield X.O., Charest A., Galas D.J., Gerstein M.B., Gupta M., Milosavljevic A., McManus M.T., et al. The Extracellular RNA Communication Consortium: Establishing Foundational Knowledge and Technologies for Extracellular RNA Research. Cell. 2019;177:231–242. doi: 10.1016/j.cell.2019.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tijsen A.J., Creemers E.E., Moerland P.D., de Windt L.J., Van der Wal A.C., Kok W.E., Pinto Y.M. MiR423-5p as a circulating biomarker for heart failure. Circ. Res. 2010;106:1035–1039. doi: 10.1161/CIRCRESAHA.110.218297. [DOI] [PubMed] [Google Scholar]
- 64.Jansen F., Yang X., Proebsting S., Hoelscher M., Przybilla D., Baumann K., Schmitz T., Dolf A., Endl E., Franklin B.S., et al. MicroRNA expression in circulating microvesicles predicts cardiovascular events in patients with coronary artery disease. J. Am. Heart Assoc. 2014;3:e001249. doi: 10.1161/JAHA.114.001249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chang Y.J., Wang K.C. Therapeutic perspectives of extracellular vesicles and extracellular microRNAs in atherosclerosis. Curr. Top. Membr. 2021;87:255–277. doi: 10.1016/bs.ctm.2021.08.005. [DOI] [PubMed] [Google Scholar]
- 66.Villarroya-Beltri C., Gutiérrez-Vázquez C., Sánchez-Cabo F., Pérez-Hernández D., Vázquez J., Martin-Cofreces N., Martinez-Herrera D.J., Pascual-Montano A., Mittelbrunn M., Sánchez-Madrid F. Sumoylated hnRNPA2B1 controls the sorting of miRNAs into exosomes through binding to specific motifs. Nat. Commun. 2013;4:2980. doi: 10.1038/ncomms3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zietzer A., Hosen M.R., Wang H., Goody P.R., Sylvester M., Latz E., Nickenig G., Werner N., Jansen F. The RNA-binding protein hnRNPU regulates the sorting of microRNA-30c-5p into large extracellular vesicles. J. Extracell. Vesicles. 2020;9:1786967. doi: 10.1080/20013078.2020.1786967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shurtleff M.J., Yao J., Qin Y., Nottingham R.M., Temoche-Diaz M.M., Schekman R., Lambowitz A.M. Broad role for YBX1 in defining the small noncoding RNA composition of exosomes. Proc. Natl. Acad. Sci. USA. 2017;114:E8987–E8995. doi: 10.1073/pnas.1712108114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shurtleff M.J., Temoche-Diaz M.M., Karfilis K.V., Ri S., Schekman R. Y-box protein 1 is required to sort microRNAs into exosomes in cells and in a cell-free reaction. elife. 2016;5:e19276. doi: 10.7554/eLife.19276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Santangelo L., Giurato G., Cicchini C., Montaldo C., Mancone C., Tarallo R., Battistelli C., Alonzi T., Weisz A., Tripodi M. The RNA-Binding Protein SYNCRIP Is a Component of the Hepatocyte Exosomal Machinery Controlling MicroRNA Sorting. Cell Rep. 2016;17:799–808. doi: 10.1016/j.celrep.2016.09.031. [DOI] [PubMed] [Google Scholar]
- 71.Hobor F., Dallmann A., Ball N.J., Cicchini C., Battistelli C., Ogrodowicz R.W., Christodoulou E., Martin S.R., Castello A., Tripodi M., et al. A cryptic RNA-binding domain mediates Syncrip recognition and exosomal partitioning of miRNA targets. Nat. Commun. 2018;9:831. doi: 10.1038/s41467-018-03182-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Statello L., Maugeri M., Garre E., Nawaz M., Wahlgren J., Papadimitriou A., Lundqvist C., Lindfors L., Collén A., Sunnerhagen P., et al. Identification of RNA-binding proteins in exosomes capable of interacting with different types of RNA: RBP-facilitated transport of RNAs into exosomes. PLoS ONE. 2018;13:e0195969. doi: 10.1371/journal.pone.0195969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mukherjee K., Ghoshal B., Ghosh S., Chakrabarty Y., Shwetha S., Das S., Bhattacharyya S.N. Reversible HuR-microRNA binding controls extracellular export of miR-122 and augments stress response. EMBO Rep. 2016;17:1184–1203. doi: 10.15252/embr.201541930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Teng Y., Ren Y., Hu X., Mu J., Samykutty A., Zhuang X., Deng Z., Kumar A., Zhang L., Merchant M.L., et al. MVP-mediated exosomal sorting of miR-193a promotes colon cancer progression. Nat. Commun. 2017;8:14448. doi: 10.1038/ncomms14448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Xu Y.F., Xu X., Gin A., Nshimiyimana J.D., Mooers B.H.M., Caputi M., Hannafon B.N., Ding W.Q. SRSF1 regulates exosome microRNA enrichment in human cancer cells. Cell Commun. Signal. 2020;18:130. doi: 10.1186/s12964-020-00615-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Temoche-Diaz M.M., Shurtleff M.J., Nottingham R.M., Yao J., Fadadu R.P., Lambowitz A.M., Schekman R. Distinct mechanisms of microRNA sorting into cancer cell-derived extracellular vesicle subtypes. elife. 2019;8:e47544. doi: 10.7554/eLife.47544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu X.M., Ma L., Schekman R. Selective sorting of microRNAs into exosomes by phase-separated YBX1 condensates. elife. 2021;10:e71982. doi: 10.7554/eLife.71982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lee H., Li C., Zhang Y., Zhang D., Otterbein L.E., Jin Y. Caveolin-1 selectively regulates microRNA sorting into microvesicles after noxious stimuli. J. Exp. Med. 2019;216:2202–2220. doi: 10.1084/jem.20182313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Squadrito M.L., Baer C., Burdet F., Maderna C., Gilfillan G.D., Lyle R., Ibberson M., De Palma M. Endogenous RNAs modulate microRNA sorting to exosomes and transfer to acceptor cells. Cell Rep. 2014;8:1432–1446. doi: 10.1016/j.celrep.2014.07.035. [DOI] [PubMed] [Google Scholar]
- 80.Iavello A., Frech V.S., Gai C., Deregibus M.C., Quesenberry P.J., Camussi G. Role of Alix in miRNA packaging during extracellular vesicle biogenesis. Int. J. Mol. Med. 2016;37:958–966. doi: 10.3892/ijmm.2016.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liu Y., Song J.W., Lin J.Y., Miao R., Zhong J.C. Roles of MicroRNA-122 in Cardiovascular Fibrosis and Related Diseases. Cardiovasc. Toxicol. 2020;20:463–473. doi: 10.1007/s12012-020-09603-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hosen M.R., Goody P.R., Zietzer A., Xiang X., Niepmann S.T., Sedaghat A., Tiyerili V., Chennupati R., Moore J.B.t., Boon R.A., et al. Circulating MicroRNA-122-5p Is Associated with a Lack of Improvement in Left Ventricular Function After Transcatheter Aortic Valve Replacement and Regulates Viability of Cardiomyocytes Through Extracellular Vesicles. Circulation. 2022;146:1836–1854. doi: 10.1161/CIRCULATIONAHA.122.060258. [DOI] [PubMed] [Google Scholar]
- 83.Liu X., Xu Y., Deng Y., Li H. MicroRNA-223 Regulates Cardiac Fibrosis After Myocardial Infarction by Targeting RASA1. Cell Physiol. Biochem. 2018;46:1439–1454. doi: 10.1159/000489185. [DOI] [PubMed] [Google Scholar]
- 84.Wang K., Long B., Liu F., Wang J.X., Liu C.Y., Zhao B., Zhou L.Y., Sun T., Wang M., Yu T., et al. A circular RNA protects the heart from pathological hypertrophy and heart failure by targeting miR-223. Eur. Heart J. 2016;37:2602–2611. doi: 10.1093/eurheartj/ehv713. [DOI] [PubMed] [Google Scholar]
- 85.Zhang Y., Ding Y., Li M., Yuan J., Yu Y., Bi X., Hong H., Ye J., Liu P. MicroRNA-34c-5p provokes isoprenaline-induced cardiac hypertrophy by modulating autophagy via targeting ATG4B. Acta Pharm. Sin. B. 2022;12:2374–2390. doi: 10.1016/j.apsb.2021.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhang W., Wang Q., Feng Y., Chen X., Yang L., Xu M., Wang X., Li W., Niu X., Gao D. MicroRNA-26a Protects the Heart Against Hypertension-Induced Myocardial Fibrosis. J. Am. Heart Assoc. 2020;9:e017970. doi: 10.1161/JAHA.120.017970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sun M., Guo M., Ma G., Zhang N., Pan F., Fan X., Wang R. MicroRNA-30c-5p protects against myocardial ischemia/reperfusion injury via regulation of Bach1/Nrf2. Toxicol. Appl. Pharmacol. 2021;426:115637. doi: 10.1016/j.taap.2021.115637. [DOI] [PubMed] [Google Scholar]
- 88.Danielson L.S., Park D.S., Rotllan N., Chamorro-Jorganes A., Guijarro M.V., Fernandez-Hernando C., Fishman G.I., Phoon C.K., Hernando E. Cardiovascular dysregulation of miR-17-92 causes a lethal hypertrophic cardiomyopathy and arrhythmogenesis. FASEB J. 2013;27:1460–1467. doi: 10.1096/fj.12-221994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nair N., Kumar S., Gongora E., Gupta S. Circulating miRNA as novel markers for diastolic dysfunction. Mol. Cell Biochem. 2013;376:33–40. doi: 10.1007/s11010-012-1546-x. [DOI] [PubMed] [Google Scholar]
- 90.Zhang J., Wu L., Li Z., Fu G. miR-1231 exacerbates arrhythmia by targeting calciumchannel gene CACNA2D2 in myocardial infarction. Am. J. Transl. Res. 2017;9:1822–1833. [PMC free article] [PubMed] [Google Scholar]
- 91.Tucker N.R., Chaffin M., Fleming S.J., Hall A.W., Parsons V.A., Bedi K.C., Jr., Akkad A.D., Herndon C.N., Arduini A., Papangeli I., et al. Transcriptional and Cellular Diversity of the Human Heart. Circulation. 2020;142:466–482. doi: 10.1161/CIRCULATIONAHA.119.045401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Litviňuková M., Talavera-López C., Maatz H., Reichart D., Worth C.L., Lindberg E.L., Kanda M., Polanski K., Heinig M., Lee M., et al. Cells of the adult human heart. Nature. 2020;588:466–472. doi: 10.1038/s41586-020-2797-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Howard C.M., Baudino T.A. Dynamic cell-cell and cell-ECM interactions in the heart. J. Mol. Cell Cardiol. 2014;70:19–26. doi: 10.1016/j.yjmcc.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 94.Wu M.P., Zhang Y.S., Xu X., Zhou Q., Li J.D., Yan C. Vinpocetine Attenuates Pathological Cardiac Remodeling by Inhibiting Cardiac Hypertrophy and Fibrosis. Cardiovasc. Drugs Ther. 2017;31:157–166. doi: 10.1007/s10557-017-6719-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Travers J.G., Kamal F.A., Robbins J., Yutzey K.E., Blaxall B.C. Cardiac Fibrosis: The Fibroblast Awakens. Circ. Res. 2016;118:1021–1040. doi: 10.1161/CIRCRESAHA.115.306565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Oh J.G., Lee P., Gordon R.E., Sahoo S., Kho C., Jeong D. Analysis of extracellular vesicle miRNA profiles in heart failure. J. Cell Mol. Med. 2020;24:7214–7227. doi: 10.1111/jcmm.15251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sun P., Wang C., Mang G., Xu X., Fu S., Chen J., Wang X., Wang W., Li H., Zhao P., et al. Extracellular vesicle-packaged mitochondrial disturbing miRNA exacerbates cardiac injury during acute myocardial infarction. Clin. Transl. Med. 2022;12:e779. doi: 10.1002/ctm2.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Das S., Halushka M.K. Extracellular vesicle microRNA transfer in cardiovascular disease. Cardiovasc. Pathol. 2015;24:199–206. doi: 10.1016/j.carpath.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 99.Tian C., Gao L., Zimmerman M.C., Zucker I.H. Myocardial infarction-induced microRNA-enriched exosomes contribute to cardiac Nrf2 dysregulation in chronic heart failure. Am. J. Physiol. Heart Circ. Physiol. 2018;314:H928–H939. doi: 10.1152/ajpheart.00602.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fang X., Stroud M.J., Ouyang K., Fang L., Zhang J., Dalton N.D., Gu Y., Wu T., Peterson K.L., Huang H.D., et al. Adipocyte-specific loss of PPARγ attenuates cardiac hypertrophy. JCI Insight. 2016;1:e89908. doi: 10.1172/jci.insight.89908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Callis T.E., Pandya K., Seok H.Y., Tang R.H., Tatsuguchi M., Huang Z.P., Chen J.F., Deng Z., Gunn B., Shumate J., et al. MicroRNA-208a is a regulator of cardiac hypertrophy and conduction in mice. J. Clin. Investig. 2009;119:2772–2786. doi: 10.1172/JCI36154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Chistiakov D.A., Orekhov A.N., Bobryshev Y.V. Cardiac-specific miRNA in cardiogenesis, heart function, and cardiac pathology (with focus on myocardial infarction) J. Mol. Cell Cardiol. 2016;94:107–121. doi: 10.1016/j.yjmcc.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 103.Nie X., Fan J., Li H., Yin Z., Zhao Y., Dai B., Dong N., Chen C., Wang D.W. miR-217 Promotes Cardiac Hypertrophy and Dysfunction by Targeting PTEN. Mol. Ther. Nucleic Acids. 2018;12:254–266. doi: 10.1016/j.omtn.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yang J., Yu X., Xue F., Li Y., Liu W., Zhang S. Exosomes derived from cardiomyocytes promote cardiac fibrosis via myocyte-fibroblast cross-talk. Am. J. Transl. Res. 2018;10:4350–4366. [PMC free article] [PubMed] [Google Scholar]
- 105.Tang C., Hou Y.X., Shi P.X., Zhu C.H., Lu X., Wang X.L., Que L.L., Zhu G.Q., Liu L., Chen Q., et al. Cardiomyocyte-specific Peli1 contributes to the pressure overload-induced cardiac fibrosis through miR-494-3p-dependent exosomal communication. FASEB J. 2023;37:e22699. doi: 10.1096/fj.202200597R. [DOI] [PubMed] [Google Scholar]
- 106.Fu X., Mishra R., Chen L., Arfat M.Y., Sharma S., Kingsbury T., Gunasekaran M., Saha P., Hong C., Yang P., et al. Exosomes mediated fibrogenesis in dilated cardiomyopathy through a MicroRNA pathway. iScience. 2023;26:105963. doi: 10.1016/j.isci.2023.105963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Su M., Li W., Yuan Y.U.E., Liu S., Liang C., Liu H.E., Zhang R., Liu Y., Sun L.I., Wei Y., et al. Epididymal white adipose tissue promotes angiotensin II-induced cardiac fibrosis in an exosome-dependent manner. Transl. Res. 2022;248:51–67. doi: 10.1016/j.trsl.2022.05.004. [DOI] [PubMed] [Google Scholar]
- 108.Cai L., Chao G., Li W., Zhu J., Li F., Qi B., Wei Y., Chen S., Zhou G., Lu X., et al. Activated CD4+ T cells-derived exosomal miR-142-3p boosts post-ischemic ventricular remodeling by activating myofibroblast. Aging. 2020;12:7380–7396. doi: 10.18632/aging.103084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hinkel R., Ramanujam D., Kaczmarek V., Howe A., Klett K., Beck C., Dueck A., Thum T., Laugwitz K.L., Maegdefessel L., et al. AntimiR-21 Prevents Myocardial Dysfunction in a Pig Model of Ischemia/Reperfusion Injury. J. Am. Coll. Cardiol. 2020;75:1788–1800. doi: 10.1016/j.jacc.2020.02.041. [DOI] [PubMed] [Google Scholar]
- 110.Ramanujam D., Sassi Y., Laggerbauer B., Engelhardt S. Viral Vector-Based Targeting of miR-21 in Cardiac Nonmyocyte Cells Reduces Pathologic Remodeling of the Heart. Mol. Ther. 2016;24:1939–1948. doi: 10.1038/mt.2016.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Thum T., Chau N., Bhat B., Gupta S.K., Linsley P.S., Bauersachs J., Engelhardt S. Comparison of different miR-21 inhibitor chemistries in a cardiac disease model. J. Clin. Investig. 2011;121:461–462. doi: 10.1172/JCI45938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Thum T., Gross C., Fiedler J., Fischer T., Kissler S., Bussen M., Galuppo P., Just S., Rottbauer W., Frantz S., et al. MicroRNA-21 contributes to myocardial disease by stimulating MAP kinase signalling in fibroblasts. Nature. 2008;456:980–984. doi: 10.1038/nature07511. [DOI] [PubMed] [Google Scholar]
- 113.Ramanujam D., Schön A.P., Beck C., Vaccarello P., Felician G., Dueck A., Esfandyari D., Meister G., Meitinger T., Schulz C., et al. MicroRNA-21-Dependent Macrophage-to-Fibroblast Signaling Determines the Cardiac Response to Pressure Overload. Circulation. 2021;143:1513–1525. doi: 10.1161/CIRCULATIONAHA.120.050682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ottaviani L., Juni R.P., de Abreu R.C., Sansonetti M., Sampaio-Pinto V., Halkein J., Hegenbarth J.C., Ring N., Knoops K., Kocken J.M.M., et al. Intercellular transfer of miR-200c-3p impairs the angiogenic capacity of cardiac endothelial cells. Mol. Ther. 2022;30:2257–2273. doi: 10.1016/j.ymthe.2022.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Li G., Qiu Z., Li C., Zhao R., Zhang Y., Shen C., Liu W., Long X., Zhuang S., Wang Y., et al. Exosomal MiR-29a in Cardiomyocytes Induced by Angiotensin II Regulates Cardiac Microvascular Endothelial Cell Proliferation, Migration and Angiogenesis by Targeting VEGFA. Curr. Gene Ther. 2022;22:331–341. doi: 10.2174/1566523222666220303102951. [DOI] [PubMed] [Google Scholar]
- 116.Ranjan P., Kumari R., Goswami S.K., Li J., Pal H., Suleiman Z., Cheng Z., Krishnamurthy P., Kishore R., Verma S.K. Myofibroblast-Derived Exosome Induce Cardiac Endothelial Cell Dysfunction. Front. Cardiovasc. Med. 2021;8:676267. doi: 10.3389/fcvm.2021.676267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Liu S., Chen J., Shi J., Zhou W., Wang L., Fang W., Zhong Y., Chen X., Chen Y., Sabri A., et al. M1-like macrophage-derived exosomes suppress angiogenesis and exacerbate cardiac dysfunction in a myocardial infarction microenvironment. Basic Res. Cardiol. 2020;115:22. doi: 10.1007/s00395-020-0781-7. [DOI] [PubMed] [Google Scholar]
- 118.Sun L.L., Duan M.J., Ma J.C., Xu L., Mao M., Biddyut D., Wang Q., Yang C., Zhang S., Xu Y., et al. Myocardial infarction-induced hippocampal microtubule damage by cardiac originating microRNA-1 in mice. J. Mol. Cell Cardiol. 2018;120:12–27. doi: 10.1016/j.yjmcc.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 119.Akbar N., Digby J.E., Cahill T.J., Tavare A.N., Corbin A.L., Saluja S., Dawkins S., Edgar L., Rawlings N., Ziberna K., et al. Endothelium-derived extracellular vesicles promote splenic monocyte mobilization in myocardial infarction. JCI Insight. 2017;2 doi: 10.1172/jci.insight.93344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Panda R., Kubes P. Extracellular vesicles selectively mobilize splenic neutrophils. Cardiovasc. Res. 2023;119:1–2. doi: 10.1093/cvr/cvad015. [DOI] [PubMed] [Google Scholar]
- 121.Lyu L., Wang H., Li B., Qin Q., Qi L., Nagarkatti M., Nagarkatti P., Janicki J.S., Wang X.L., Cui T. A critical role of cardiac fibroblast-derived exosomes in activating renin angiotensin system in cardiomyocytes. J. Mol. Cell Cardiol. 2015;89:268–279. doi: 10.1016/j.yjmcc.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Savvatis K., Pappritz K., Becher P.M., Lindner D., Zietsch C., Volk H.D., Westermann D., Schultheiss H.P., Tschöpe C. Interleukin-23 deficiency leads to impaired wound healing and adverse prognosis after myocardial infarction. Circ. Heart Fail. 2014;7:161–171. doi: 10.1161/CIRCHEARTFAILURE.113.000604. [DOI] [PubMed] [Google Scholar]
- 123.Kuwabara Y., Ono K., Horie T., Nishi H., Nagao K., Kinoshita M., Watanabe S., Baba O., Kojima Y., Shizuta S., et al. Increased microRNA-1 and microRNA-133a levels in serum of patients with cardiovascular disease indicate myocardial damage. Circ. Cardiovasc. Genet. 2011;4:446–454. doi: 10.1161/CIRCGENETICS.110.958975. [DOI] [PubMed] [Google Scholar]
- 124.Carbone F., Nencioni A., Mach F., Vuilleumier N., Montecucco F. Pathophysiological role of neutrophils in acute myocardial infarction. Thromb. Haemost. 2013;110:501–514. doi: 10.1160/TH13-03-0211. [DOI] [PubMed] [Google Scholar]
- 125.Helseth R., Shetelig C., Andersen G., Langseth M.S., Limalanathan S., Opstad T.B., Arnesen H., Hoffmann P., Eritsland J., Seljeflot I. Neutrophil Extracellular Trap Components Associate with Infarct Size, Ventricular Function, and Clinical Outcome in STEMI. Mediat. Inflamm. 2019;2019:7816491. doi: 10.1155/2019/7816491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Arruda-Olson A.M., Reeder G.S., Bell M.R., Weston S.A., Roger V.L. Neutrophilia predicts death and heart failure after myocardial infarction: A community-based study. Circ. Cardiovasc. Qual. Outcomes. 2009;2:656–662. doi: 10.1161/CIRCOUTCOMES.108.831024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Dogan I., Karaman K., Sonmez B., Celik S., Turker O. Relationship between serum neutrophil count and infarct size in patients with acute myocardial infarction. Nucl. Med. Commun. 2009;30:797–801. doi: 10.1097/MNM.0b013e32832e3a16. [DOI] [PubMed] [Google Scholar]
- 128.Magnussen C., Blankenberg S. Biomarkers for heart failure: Small molecules with high clinical relevance. J. Intern. Med. 2018;283:530–543. doi: 10.1111/joim.12756. [DOI] [PubMed] [Google Scholar]
- 129.Siranart N., Laohasurayotin K., Phanthong T., Sowalertrat W., Ariyachaipanich A., Chokesuwattanaskul R. Proenkephalin as a Novel Prognostic Marker in Heart Failure Patients: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2023;24:4887. doi: 10.3390/ijms24054887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Creemers E.E., Tijsen A.J., Pinto Y.M. Circulating microRNAs: Novel biomarkers and extracellular communicators in cardiovascular disease? Circ. Res. 2012;110:483–495. doi: 10.1161/CIRCRESAHA.111.247452. [DOI] [PubMed] [Google Scholar]
- 131.Wu T., Chen Y., Du Y., Tao J., Li W., Zhou Z., Yang Z. Circulating exosomal miR-92b-5p is a promising diagnostic biomarker of heart failure with reduced ejection fraction patients hospitalized for acute heart failure. J. Thorac. Dis. 2018;10:6211–6220. doi: 10.21037/jtd.2018.10.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Quan X., Ji Y., Zhang C., Guo X., Zhang Y., Jia S., Ma W., Fan Y., Wang C. Circulating MiR-146a May be a Potential Biomarker of Coronary Heart Disease in Patients with Subclinical Hypothyroidism. Cell Physiol. Biochem. 2018;45:226–236. doi: 10.1159/000486769. [DOI] [PubMed] [Google Scholar]
- 133.Halkein J., Tabruyn S.P., Ricke-Hoch M., Haghikia A., Nguyen N.Q., Scherr M., Castermans K., Malvaux L., Lambert V., Thiry M., et al. MicroRNA-146a is a therapeutic target and biomarker for peripartum cardiomyopathy. J. Clin. Investig. 2013;123:2143–2154. doi: 10.1172/JCI64365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sucharov C.C., Neltner B., Pietra A.E., Karimpour-Fard A., Patel J., Ho C.Y., Miyamoto S.D. Circulating MicroRNAs Identify Early Phenotypic Changes in Sarcomeric Hypertrophic Cardiomyopathy. Circ. Heart Fail. 2023;16:e010291. doi: 10.1161/CIRCHEARTFAILURE.122.010291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Yang V.K., Loughran K.A., Meola D.M., Juhr C.M., Thane K.E., Davis A.M., Hoffman A.M. Circulating exosome microRNA associated with heart failure secondary to myxomatous mitral valve disease in a naturally occurring canine model. J. Extracell. Vesicles. 2017;6:1350088. doi: 10.1080/20013078.2017.1350088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Klenke S., Eul S., Peters J., Neumann T., Adamzik M., Frey U.H. Circulating miR-192 is a prognostic marker in patients with ischemic cardiomyopathy. Future Cardiol. 2018;14:283–289. doi: 10.2217/fca-2017-0108. [DOI] [PubMed] [Google Scholar]
- 137.Lv P., Zhou M., He J., Meng W., Ma X., Dong S., Meng X., Zhao X., Wang X., He F. Circulating miR-208b and miR-34a Are Associated with Left Ventricular Remodeling after Acute Myocardial Infarction. Int. J. Mol. Sci. 2014;15:5774–5788. doi: 10.3390/ijms15045774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Matsumoto S., Sakata Y., Suna S., Nakatani D., Usami M., Hara M., Kitamura T., Hamasaki T., Nanto S., Kawahara Y., et al. Circulating p53-responsive microRNAs are predictive indicators of heart failure after acute myocardial infarction. Circ. Res. 2013;113:322–326. doi: 10.1161/CIRCRESAHA.113.301209. [DOI] [PubMed] [Google Scholar]
- 139.Wang L., Liu J., Xu B., Liu Y.L., Liu Z. Reduced exosome miR-425 and miR-744 in the plasma represents the progression of fibrosis and heart failure. Kaohsiung J. Med. Sci. 2018;34:626–633. doi: 10.1016/j.kjms.2018.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Melman Y.F., Shah R., Danielson K., Xiao J., Simonson B., Barth A., Chakir K., Lewis G.D., Lavender Z., Truong Q.A., et al. Circulating MicroRNA-30d Is Associated with Response to Cardiac Resynchronization Therapy in Heart Failure and Regulates Cardiomyocyte Apoptosis: A Translational Pilot Study. Circulation. 2015;131:2202–2216. doi: 10.1161/CIRCULATIONAHA.114.013220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zhou R., Wang L., Zhao G., Chen D., Song X., Momtazi-Borojeni A.A., Yuan H. Circulating exosomal microRNAs as emerging non-invasive clinical biomarkers in heart failure: Mega bio-roles of a nano bio-particle. IUBMB Life. 2020;72:2546–2562. doi: 10.1002/iub.2396. [DOI] [PubMed] [Google Scholar]
- 142.Huang J.P., Chang C.C., Kuo C.Y., Huang K.J., Sokal E.M., Chen K.H., Hung L.M. Exosomal microRNAs miR-30d-5p and miR-126a-5p Are Associated with Heart Failure with Preserved Ejection Fraction in STZ-Induced Type 1 Diabetic Rats. Int. J. Mol. Sci. 2022;23:7514. doi: 10.3390/ijms23147514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Li J., Salvador A.M., Li G., Valkov N., Ziegler O., Yeri A., Yang Xiao C., Meechoovet B., Alsop E., Rodosthenous R.S., et al. Mir-30d Regulates Cardiac Remodeling by Intracellular and Paracrine Signaling. Circ. Res. 2021;128:e1–e23. doi: 10.1161/CIRCRESAHA.120.317244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Zhu L.P., Tian T., Wang J.Y., He J.N., Chen T., Pan M., Xu L., Zhang H.X., Qiu X.T., Li C.C., et al. Hypoxia-elicited mesenchymal stem cell-derived exosomes facilitates cardiac repair through miR-125b-mediated prevention of cell death in myocardial infarction. Theranostics. 2018;8:6163–6177. doi: 10.7150/thno.28021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Zhang L., Wei Q., Liu X., Zhang T., Wang S., Zhou L., Zou L., Fan F., Chi H., Sun J., et al. Exosomal microRNA-98-5p from hypoxic bone marrow mesenchymal stem cells inhibits myocardial ischemia-reperfusion injury by reducing TLR4 and activating the PI3K/Akt signaling pathway. Int. Immunopharmacol. 2021;101:107592. doi: 10.1016/j.intimp.2021.107592. [DOI] [PubMed] [Google Scholar]
- 146.Yuan J., Yang H., Liu C., Shao L., Zhang H., Lu K., Wang J., Wang Y., Yu Q., Zhang Y., et al. Microneedle Patch Loaded with Exosomes Containing MicroRNA-29b Prevents Cardiac Fibrosis after Myocardial Infarction. Adv. Healthc. Mater. 2023;12:e2202959. doi: 10.1002/adhm.202202959. [DOI] [PubMed] [Google Scholar]
- 147.Pu L., Kong X., Li H., He X. Exosomes released from mesenchymal stem cells overexpressing microRNA-30e ameliorate heart failure in rats with myocardial infarction. Am. J. Transl. Res. 2021;13:4007–4025. [PMC free article] [PubMed] [Google Scholar]
- 148.Yan F., Cui W., Chen Z. Mesenchymal Stem Cell-Derived Exosome-Loaded microRNA-129-5p Inhibits TRAF3 Expression to Alleviate Apoptosis and Oxidative Stress in Heart Failure. Cardiovasc. Toxicol. 2022;22:631–645. doi: 10.1007/s12012-022-09743-9. [DOI] [PubMed] [Google Scholar]
- 149.Shafei S., Khanmohammadi M., Ghanbari H., Nooshabadi V.T., Tafti S.H.A., Rabbani S., Kasaiyan M., Basiri M., Tavoosidana G. Effectiveness of exosome mediated miR-126 and miR-146a delivery on cardiac tissue regeneration. Cell Tissue Res. 2022;390:71–92. doi: 10.1007/s00441-022-03663-4. [DOI] [PubMed] [Google Scholar]
- 150.Gao L., Qiu F., Cao H., Li H., Dai G., Ma T., Gong Y., Luo W., Zhu D., Qiu Z., et al. Therapeutic delivery of microRNA-125a-5p oligonucleotides improves recovery from myocardial ischemia/reperfusion injury in mice and swine. Theranostics. 2023;13:685–703. doi: 10.7150/thno.73568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Wang T., Li T., Niu X., Hu L., Cheng J., Guo D., Ren H., Zhao R., Ji Z., Liu P., et al. ADSC-derived exosomes attenuate myocardial infarction injury by promoting miR-205-mediated cardiac angiogenesis. Biol. Direct. 2023;18:6. doi: 10.1186/s13062-023-00361-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Barile L., Lionetti V., Cervio E., Matteucci M., Gherghiceanu M., Popescu L.M., Torre T., Siclari F., Moccetti T., Vassalli G. Extracellular vesicles from human cardiac progenitor cells inhibit cardiomyocyte apoptosis and improve cardiac function after myocardial infarction. Cardiovasc. Res. 2014;103:530–541. doi: 10.1093/cvr/cvu167. [DOI] [PubMed] [Google Scholar]
- 153.Wang N., Chen C., Yang D., Liao Q., Luo H., Wang X., Zhou F., Yang X., Yang J., Zeng C., et al. Mesenchymal stem cells-derived extracellular vesicles, via miR-210, improve infarcted cardiac function by promotion of angiogenesis. Biochim. Biophys. Acta Mol. Basis Dis. 2017;1863:2085–2092. doi: 10.1016/j.bbadis.2017.02.023. [DOI] [PubMed] [Google Scholar]
- 154.Adamiak M., Cheng G., Bobis-Wozowicz S., Zhao L., Kedracka-Krok S., Samanta A., Karnas E., Xuan Y.T., Skupien-Rabian B., Chen X., et al. Induced Pluripotent Stem Cell (iPSC)-Derived Extracellular Vesicles Are Safer and More Effective for Cardiac Repair Than iPSCs. Circ. Res. 2018;122:296–309. doi: 10.1161/CIRCRESAHA.117.311769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Song Y., Zhang C., Zhang J., Jiao Z., Dong N., Wang G., Wang Z., Wang L. Localized injection of miRNA-21-enriched extracellular vesicles effectively restores cardiac function after myocardial infarction. Theranostics. 2019;9:2346–2360. doi: 10.7150/thno.29945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Luo Q., Guo D., Liu G., Chen G., Hang M., Jin M. Exosomes from MiR-126-Overexpressing Adscs Are Therapeutic in Relieving Acute Myocardial Ischaemic Injury. Cell Physiol. Biochem. 2017;44:2105–2116. doi: 10.1159/000485949. [DOI] [PubMed] [Google Scholar]
- 157.Pan J., Alimujiang M., Chen Q., Shi H., Luo X. Exosomes derived from miR-146a-modified adipose-derived stem cells attenuate acute myocardial infarction-induced myocardial damage via downregulation of early growth response factor 1. J. Cell Biochem. 2019;120:4433–4443. doi: 10.1002/jcb.27731. [DOI] [PubMed] [Google Scholar]
- 158.Gray W.D., French K.M., Ghosh-Choudhary S., Maxwell J.T., Brown M.E., Platt M.O., Searles C.D., Davis M.E. Identification of therapeutic covariant microRNA clusters in hypoxia-treated cardiac progenitor cell exosomes using systems biology. Circ. Res. 2015;116:255–263. doi: 10.1161/CIRCRESAHA.116.304360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Vandergriff A., Huang K., Shen D., Hu S., Hensley M.T., Caranasos T.G., Qian L., Cheng K. Targeting regenerative exosomes to myocardial infarction using cardiac homing peptide. Theranostics. 2018;8:1869–1878. doi: 10.7150/thno.20524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Won Y.W., McGinn A.N., Lee M., Bull D.A., Kim S.W. Targeted gene delivery to ischemic myocardium by homing peptide-guided polymeric carrier. Mol. Pharm. 2013;10:378–385. doi: 10.1021/mp300500y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Alvarez-Erviti L., Seow Y., Yin H., Betts C., Lakhal S., Wood M.J. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat. Biotechnol. 2011;29:341–345. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- 162.Moholkar D.N., Kandimalla R., Gupta R.C., Aqil F. Advances in lipid-based carriers for cancer therapeutics: Liposomes, exosomes and hybrid exosomes. Cancer Lett. 2023;565:216220. doi: 10.1016/j.canlet.2023.216220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.