ABSTRACT
Purpose
This study aimed to compare the impact of hot-humid environmental conditions on performance outcomes, thermoregulatory responses, and thermal perception during exercise between elite para- and able-bodied (AB) athletes.
Methods
Twenty elite para-athletes (para-cycling and wheelchair tennis) and 20 elite AB athletes (road cycling, mountain biking, beach volleyball) performed an incremental exercise test in a temperate environment (mean ± SD, 15.2°C ± 1.2°C; relative humidity, 54% ± 7%) and a hot-humid environment (31.9°C ± 1.6°C, 72% ± 5%). Exercise tests started with a 20-min warm-up at 70% of maximal heart rate, after which power output increased by 5% every 3 min until volitional exhaustion.
Results
Time to exhaustion was shorter in hot-humid versus temperate conditions, with equal performance loss for para- and AB athletes (median (interquartile range), 26% (20%–31%) vs 27% (19%–32%); P = 0.80). AB athletes demonstrated larger exercise-induced increases in gastrointestinal temperature (Tgi) in hot-humid versus temperate conditions (2.2 ± 0.7 vs 1.7 ± 0.5, P < 0.001), whereas Tgi responses in para-athletes were similar between conditions (1.3 ± 0.6 vs 1.3 ± 0.4, P = 0.74). Para- and AB athletes showed similar elevations in peak skin temperature (P = 0.94), heart rate (P = 0.67), and thermal sensation score (P = 0.64) in hot-humid versus temperate conditions.
Conclusions
Elite para-athletes and AB athletes demonstrated similar performance decrements during exercise in hot-humid versus temperate conditions, whereas Tgi elevations were markedly lower in para-athletes. We observed large interindividual variation within both groups, suggesting that in both para- and AB athletes, personalized heat mitigation plans should be developed based on individual thermal testing.
Key Words: PARALYMPIC, OLYMPIC, TOKYO 2020, HYPERTHERMIA, HEAT STRESS, ADAPTED SPORTS
Sports events for elite athletes are increasingly being held in hot and/or humid summer conditions, and exercise under extreme temperatures is expected to be more common in the future because of climate change (1). During exercise in hot-humid conditions, heat dissipation through convection, radiation, and evaporation is restricted and may be insufficient to compensate the body’s metabolic heat production. The resultant heat strain induces cardiovascular challenges, as well as changes in central nervous system function and muscle metabolism, which may all contribute to a substantial reduction in aerobic exercise performance (2,3).
Performance decrements in the heat have been investigated extensively in able-bodied (AB) athletes (4–7). However, to our knowledge, heat-related performance losses have not been quantified in para-athletes. Many para-athletes may demonstrate amplified performance losses compared with AB athletes, because impairments such as a spinal cord injury, limb deficiency, or cerebral palsy can affect thermoregulatory abilities (8–10). On the other hand, many para-athletes perform either upper-body exercise or lower-body exercise at a lower intensity and may therefore produce less metabolic heat than AB athletes, potentially reducing overall heat strain and the associated performance loss. Notwithstanding, the para-athlete population is highly heterogeneous, which may cause large interindividual variability in the response to exercise under heat stress.
The aim of this study was to compare the impact of hot-humid environmental conditions on performance outcomes, thermoregulatory responses, and thermal perception during exercise between elite para- and AB athletes. We hypothesized that para-athletes may demonstrate less heat-related performance loss than AB athletes, as exercise may be associated with a lower heat production and therefore lower heat strain in para- versus AB athletes.
METHODS
Participants
In this study, we included 20 elite para-athletes and 20 elite AB athletes. Eleven para-athletes and 12 AB athletes were endurance trained, whereas 9 para-athletes and 8 AB athletes were mixed trained (11) (Table 1). All athletes were Dutch, recruited via TeamNL (the Olympic division of all Dutch sports federations) infrastructures, and competing at an international level. None of the participating athletes were heat acclimatized. Twelve of the 21 female participants used contraception, whereas 4 did not, and 5 did not report. The study was carried out in accordance with the Declaration of Helsinki and was approved by the Medical Ethical Committee of the Radboud University Medical Centre (no. 2018-4640). All participants gave their written informed consent before the testing procedures. The data that support the findings of this study are available from the corresponding author upon reasonable request.
TABLE 1.
Characteristics of PARA and AB athletes.
| PARA (n = 20) | AB (n = 20) | P | |
|---|---|---|---|
| Age (yr) | 29 ± 10 (16–50) | 27 ± 4 (21–36) | 0.34 |
| Sex (male/female) | 11/9 (55% male) | 8/12 (40% male) | — |
| Height (cm) | 175 ± 11 (160–194) | 181 ± 14 (162–211) | 0.18 |
| Body mass (kg) | 67 ± 11 (47–87) | 71 ± 15 (52–106) | 0.30 |
| Sports disciplines | Para-cycling, n = 11 Wheelchair tennis, n = 9 |
Road cycling, n = 7 Mountain biking, n = 5 Beach volleyball; n = 8 |
— |
| Impairment types | Lower limb deficiency, n = 9 (unilateral n = 5, bilateral n = 4) Spinal cord injury (paraplegia), n = 4 Visual impairment, n = 2 Other physical impairmentsa, n = 5 |
— | — |
Data are presented as mean ± SD (range).
aPeripheral neuropathy (n = 2), connective tissue disorder (n = 1), limb malformation (n = 1), spastic hypertonia (n = 1).
PARA. para-athletes.
Study design
The current study is part of the ThermoTokyo research project, of which the rationale and design have been described previously (7,12). Participants performed two personalized incremental exercise tests in a climate chamber. All AB athletes and 4 para-athletes performed lower-body exercise, whereas 16 para-athletes performed upper-body exercise. The first exercise test was conducted in temperate conditions (ambient temperature, 15.2°C ± 1.2°C; relative humidity, 54% ± 7%; wet-bulb globe temperature, 11.9°C ± 0.8°C), which was then repeated in the second test under hot-humid conditions, as expected during the Tokyo 2020 Olympic and Paralympic Games (ambient temperature, 31.9°C ± 1.6°C; relative humidity, 72% ± 5%; wet-bulb globe temperature, 28.8°C ± 0.9°C). Visits took place at the same time of day, separated by 7 (6–7) d (median (interquartile range)). Participants were instructed to, preceding both tests, refrain from strenuous exercise (24 h) and consumption of alcohol or caffeine (12 h), replicate their diet from awakening onwards, consume their last meal ≥3 h before, and consume ~500 mL of water in the 2 h before. During both tests, they wore the same sports clothing and were not allowed to drink. All tests were performed outside of the summer months (October–April).
Personalized incremental exercise test
Exercise tests were performed on a cycling ergometer (Lode ergometer, Lode B.V., Groningen, the Netherlands (lower-body exercise) or TechnoGym Top Excite+700i, TechnoGym, Cesena, Italy (upper body exercise)) or on the participant’s personal (hand) bike installed in a stationary device (Tacx Neo Smart T2800 or Tacx Booster T2500, Tacx B.V., Wassenaar, the Netherlands) or Cyclus 2 (RBM elektronik-automation, Leipzig, Germany). After the participants entered the climate chamber, cycling ergometer settings were adjusted to fit the participant. Then, participants rested for 5 min in seated position (i.e., baseline), after which the 20-min warm-up phase started. All AB athletes started the warm-up at 100 W, whereas para-athletes started at variable power outputs (30–100 W) based on the estimated individual exercise capacity. After 3 min, power output was gradually adjusted to reach 70% of the participant’s maximal heart rate, obtained from training data or a previous graded exercise test. Further power output adjustments were made each minute until a stable target heart rate was reached. Power output was then kept constant for the remaining minutes of the warm-up phase. After the 20-min warm-up phase, the incremental phase started, in which power output was increased every 3 min by 5% of the power output corresponding to 70% of the maximal heart rate. Exercise was continued until volitional exhaustion. This personalized exercise protocol (i.e., the workloads during the warm-up and incremental stage) was determined in the temperate condition and repeated in the hot-humid condition. Participants were instructed to maintain a cadence of 80–100 rpm throughout the protocol. Ambient temperature, relative humidity, and wet-bulb globe temperature were measured using a portable climate-monitoring device (Davis Instruments Inc., Hayward, CA).
Measurements
Gastrointestinal temperature (Tgi) was continuously measured using a validated telemetric temperature capsule system (myTemp, Nijmegen, the Netherlands) (13,14). Participants ingested the capsule 3.2 (3–3.5) h before both study visits. Skin temperature of the posterior side of the neck (Tsk,neck) was continuously measured using a wireless temperature sensor (iButton DS1922L; Dallas Semiconductor Corp, Dallas, TX), attached to the skin using Tegaderm Film (Tegaderm, Neuss, Germany). Heart rate was continuously measured using a Polar system (Polar V800; Polar Electro Oy, Kempele, Finland). Body mass (in shorts and underwear, towel-dried) was measured to the nearest 100 g using an electronic weighing scale (Seca robusta 813 scale, Hamburg, Germany) before and directly after the exercise protocol to estimate whole-body sweat rate (WBSR). Perceptual scores were obtained at baseline, every 5 min during the warm-up phase, every 3 min during the incremental phase, and at exercise cessation. Thermal sensation, thermal comfort, and rating of perceived exertion were rated on a 7-point, 4-point, and 15-point scale, respectively (15,16). Thermal sensation ranged from −3 (cold) to +3 (hot), thermal comfort ranged from 1 (comfortable) to 4 (very uncomfortable), and rating of perceived exertion ranged from 6 (very, very light) to 20 (maximal exertion).
Calculations
Time to exhaustion (TTE) was measured from the start of the warm-up until volitional exhaustion. Peak power output (PPO) was calculated as follows: PPO (W) = workload in last complete step (W) + ((time in last incomplete step (min) ÷ step duration (min)) × step size (W)).
Relative TTE and PPO performance losses in hot-humid relative to temperate conditions were calculated as follows: performance loss (%) = (value hot-humid − value temperate) ÷ value temperate ×100. We also calculated the absolute changes in performance, physiological, and perceptual outcomes in hot-humid relative to temperate conditions (ΔHOT–TEMP).
Total work done was estimated by the following: Total work (kJ·kg−1) = (mean power output (W) × exercise time (s) ÷ 1000) ÷ body mass (kg).
Physiological data were averaged over 1 min, from which baseline resting values (last minute before start exercise), and peak values (highest minute) were taken. The difference between Tgi and Tsk,neck during exercise was calculated as a measure of the core-to-skin temperature gradient.
Statistical analysis
All data were formatted using MATLAB (R2012b; The MathWorks Inc., Natick, MA). Further (statistical) analyses were performed using R software (version 4.1.1; R Foundation for Statistical Computing, Vienna, Austria) in the Rstudio environment (version 2021.09.0 + 351; Rstudio, Inc., Boston, MA). The level of statistical significance was set at P < 0.050. Data were reported as mean ± SD (in case of normal distribution) or median (interquartile range; in case of nonnormal distribution, categorical variables, or <10 data points).
In this study, we used a mixed design, with two between-participant levels (para-athletes, AB athletes) and 2 within-participant levels (hot-humid conditions, temperate conditions). To investigate changes in performance, and physiological and perceptual variables on the within-participant level, we performed a paired samples t-test or a nonparametric Wilcoxon signed rank test. To investigate changes in these variables on the between-participant level, we performed a Welch’s t-test or a nonparametric Wilcoxon rank sum test. Normality of the data was tested per variable, for each cell of the design. When one or more cells of the design did not follow a normal distribution (Shapiro–Wilk test, P < 0.05), Wilcoxon tests were used for all pairwise comparisons of that variable, and data were reported as median (interquartile range). Wilcoxon tests were also used to analyze all categorical variables.
RESULTS
Personalized incremental exercise test
Power output during the warm-up phase was 65 (55–85) W for para-athletes and 145 (121–165) W for AB athletes (P < 0.001). During the incremental phase, power output was increased every 3 min by 5 (3.2–5) W for para-athletes and 9 (6–10) W for AB athletes (P < 0.001). Total work was lower for para-athletes compared with AB athletes in both temperate and hot-humid conditions (Table 2).
TABLE 2.
Exercise performance and physiological responses in PARA and AB athletes in HOT and TEMP conditions, including within- and between-group pairwise comparisons.
| PARA | AB | PARA vs AB | |
|---|---|---|---|
| Mean ± SD or Median (IQR) | Mean ± SD or Median (IQR) | P | |
| TTE (min) | n = 20 | n = 20 | |
| TEMP | 54 (41 to 62) | 58 (45 to 71) | 0.29 |
| HOT | 40 (30 to 47) | 40 (35 to 51) | 0.29 |
| ΔHOT–TEMP | −14 (−19 to −8)*** | −13 (−24 to −11)*** | 0.49 |
| PPO (W) | n = 20 | n = 20 | |
| TEMP | 131 (102 to 175) | 261 (228 to 321) | <0.001 |
| HOT | 102 (86 to 143) | 225 (182 to 264) | <0.001 |
| ΔHOT–TEMP | −20 (−35 to −15)*** | −39 (−53 to −29)*** | 0.007 |
| Total work (kJ·kg−1) | n = 20 | n = 20 | |
| TEMP | 5 (3.4 to 6.4) | 10.2 (6.4 to 12.7) | <0.001 |
| HOT | 2.9 (2 to 4.8) | 7.2 (5 to 7.6) | <0.001 |
| ΔHOT–TEMP | −1.6 (−2.3 to −0.9)*** | −2.6 (−5.6 to −2.1)*** | 0.003 |
| Tgi, baseline (°C) | n = 15 | n = 19 | |
| TEMP | 37.2 ± 0.5 | 36.9 ± 0.4 | 0.08 |
| HOT | 37.2 ± 0.3 | 36.9 ± 0.4 | 0.043 |
| ΔHOT–TEMP | 0 ± 0.5 | 0.1 ± 0.3 | 0.79 |
| Tgi, rise (°C) | n = 15 | n = 19 | |
| TEMP | 1.3 ± 0.4 | 1.7 ± 0.5 | 0.01 |
| HOT | 1.3 ± 0.6 | 2.2 ± 0.7 | <0.001 |
| ΔHOT–TEMP | 0 ± 0.5 | 0.5 ± 0.5*** | 0.007 |
| Tgi, peak (°C) | n = 19 | n = 19 | |
| TEMP | 38.5 (38.2 to 38.8) | 38.6 (38.2 to 38.9) | 0.43 |
| HOT | 38.5 (38.1 to 39) | 39.3 (38.8 to 39.4) | 0.004 |
| ΔHOT–TEMP | 0.2 (−0.3 to 0.4) | 0.6 (0.2 to 0.9)*** | 0.006 |
| Tsk,neck, baseline (°C) | n = 18 | n = 19 | |
| TEMP | 31.9 (31 to 32.7) | 31.9 (31.2 to 32.4) | 0.82 |
| HOT | 34.8 (34.5 to 35.2) | 34.8 (34.4 to 35.2) | 1.00 |
| ΔHOT–TEMP | 3 (2.1 to 3.8)*** | 3.1 (2.2 to 3.8)*** | 1.00 |
| Tsk,neck, peak (°C) | n = 18 | n = 19 | |
| TEMP | 33.2 (32.2 to 33.8) | 34.2 (33.1 to 34.7) | 0.07 |
| HOT | 36.6 (36.2 to 36.9) | 37.8 (37.1 to 38.1) | 0.006 |
| ΔHOT–TEMP | 3.6 (2.9 to 4.4)*** | 3.7 (2.6 to 4.6)*** | 0.94 |
| Tgi-Tsk,neck gradient, mean (°C) | n = 14 | n = 18 | |
| TEMP | 5.5 (5.1 to 7.8) | 5.4 (4.6 to 5.8) | 0.14 |
| HOT | 1.6 (1.5 to 2.5) | 1.4 (1 to 1.8) | 0.07 |
| ΔHOT–TEMP | −4.1 (−5.8 to −3.6)** | −3.6 (−4.8 to −3.1)*** | 0.17 |
| HR, baseline (bpm) | n = 19 | n = 20 | |
| TEMP | 75 (67 to 86) | 65 (61 to 80) | 0.08 |
| HOT | 87 (75 to 98) | 71 (67 to 81) | 0.007 |
| ΔHOT–TEMP | 8 (6 to 16)*** | 10 (1 to 16) | 0.64 |
| HR, mean (bpm) | n = 20 | n = 20 | |
| TEMP | 151 ± 12 | 143 ± 11 | 0.046 |
| HOT | 157 ± 13 | 149 ± 10 | 0.03 |
| ΔHOT–TEMP | 6 ± 7** | 5 ± 8** | 0.70 |
| HR, peak (bpm) | n = 20 | n = 20 | |
| TEMP | 181 ± 11 | 175 ± 11 | 0.13 |
| HOT | 184 ± 13 | 180 ± 11 | 0.28 |
| ΔHOT–TEMP | 4 ± 8 (P = 0.057) | 5 ± 9* | 0.67 |
| WBSR (L·h−1) | n = 18 | n = 20 | |
| TEMP | 0.6 ± 0.3 | 0.9 ± 0.3 | 0.002 |
| HOT | 0.9 ± 0.5 | 1.5 ± 0.6 | 0.003 |
| ΔHOT–TEMP | 0.3 ± 0.4** | 0.6 ± 0.3*** | 0.049 |
For the within-participant comparisons between hot-humid and temperate conditions, asterisks denote P values <0.04. Exact P values are given when P = 0.06–0.04. P values <0.05 are displayed in bold.
*P = 0.04–0.01.
**P = 0.01–0.001.
***P < 0.001.
HOT, HOT-humid; HR, heart rate TEMP, temperate; PARA, para-athletes.
Exercise performance
TTE did not differ between para- and AB athletes in both conditions, and was shorter in hot-humid versus temperate conditions for both groups (Fig. 1; Table 2). TTE performance loss was 26% (20%–31%) for para-athletes and 27% (19%–32%) for AB athletes, and did not differ between groups (P = 0.80). Absolute PPO was lower for para-athletes than for AB athletes in both conditions, and lower in hot-humid versus temperate conditions for both groups (Fig. 1; Table 2). PPO performance loss was 14% (12%–21%) for para-athletes and 14% (11%–20%) for AB athletes (P = 0.84). Figure 2 shows performance losses across subgroups of para- and AB athletes.
FIGURE 1.
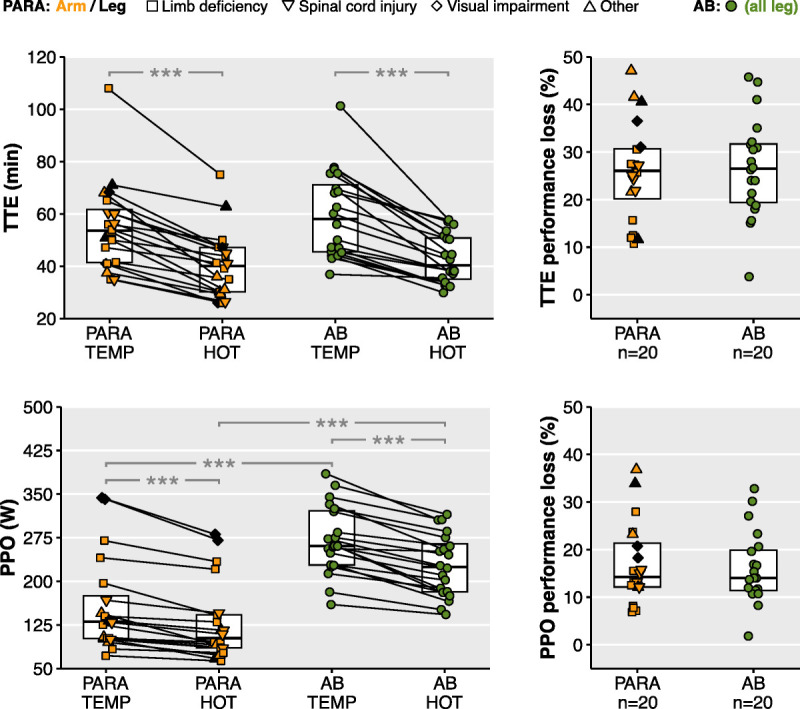
The left panels show TTE and PPO in temperate (TEMP) and hot-humid (HOT) conditions, for both para-athletes (PARA) and AB athletes. The right panels show the TTE and PPO performance loss in hot-humid vs temperate conditions. For para-athletes, fill and shape indicate exercise mode and impairment type, respectively. Average data are presented as median (IQR). Asterisks denote P values <0.04, with * for 0.04–0.01, ** for 0.01–0.001, and *** for <0.001, whereas exact P values are presented when P = 0.06–0.04.
FIGURE 2.
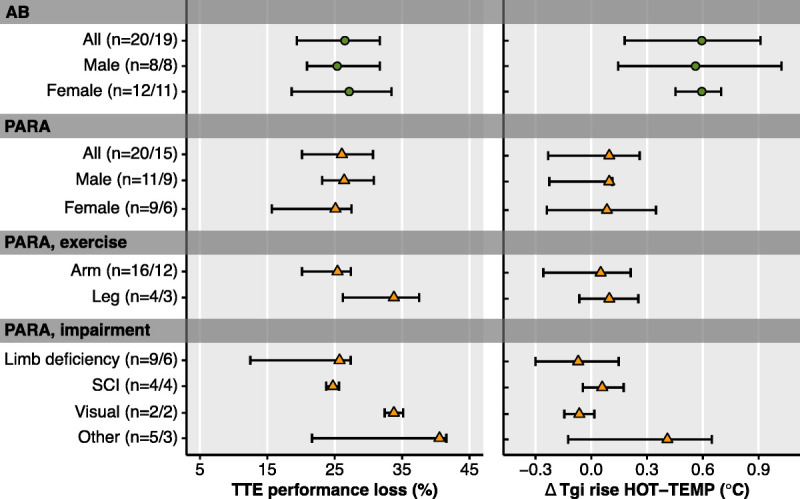
TTE performance loss and the exercise-induced Tgi rise in hot-humid (HOT) relative to temperate conditions (TEMP) for subgroups of AB athletes and para-athletes (PARA). Data are presented as median (IQR). Number of datapoints (n) are presented as (n performance/n Tgi rise).
Thermophysiological responses
Because of technical issues, Tgi data were unavailable for one para-athlete and one AB athlete, and only partial Tgi data were available for four para-athletes. Tsk,neck data were unavailable for two para-athletes and one AB athlete.
The exercise-induced rise in Tgi was lower for para-athletes than for AB athletes, in both hot-humid (para 1.3°C ± 0.6°C vs AB 2.2°C ± 0.7°C, P < 0.001) and temperate (para 1.3°C ± 0.4°C vs AB 1.7°C ± 0.5°C, P = 0.01) conditions (Fig. 3; Table 2). The Tgi rise for para-athletes was similar in hot-humid and temperate conditions, whereas the Tgi rise for AB athletes was greater in hot-humid versus temperate conditions (Fig. 4). Figure 2 shows the impact of hot-humid conditions on the exercise-induced Tgi rise across para- and AB subgroups. Peak Tsk,neck was lower for para-athletes than for AB athletes in hot-humid (para 36.6°C (36.2°C–36.9°C) vs AB 37.8°C (37.1°C–38.1°C), P = 0.006), but not temperate (para 33.2°C (32.2°C–33.8°C) vs AB 34.2°C (33.1°C–34.7°C), P = 0.07) conditions. Para- and AB athletes showed similar peak Tsk,neck elevations in hot-humid versus temperate conditions (Fig. 4; Table 2). In the para-athletes, average Tsk,neck decreased near the end of exercise in temperate conditions (Fig. 4), with the individual responses being highly heterogeneous (see Supplemental Figs. 1 and 2, Supplemental Digital Content, http://links.lww.com/MSS/C873). The athletes showing a clear decrease in Tsk,neck during exercise (n = 7) had a lower mean power output than the athletes demonstrating a clear increase in Tsk,neck (n = 8).
FIGURE 3.
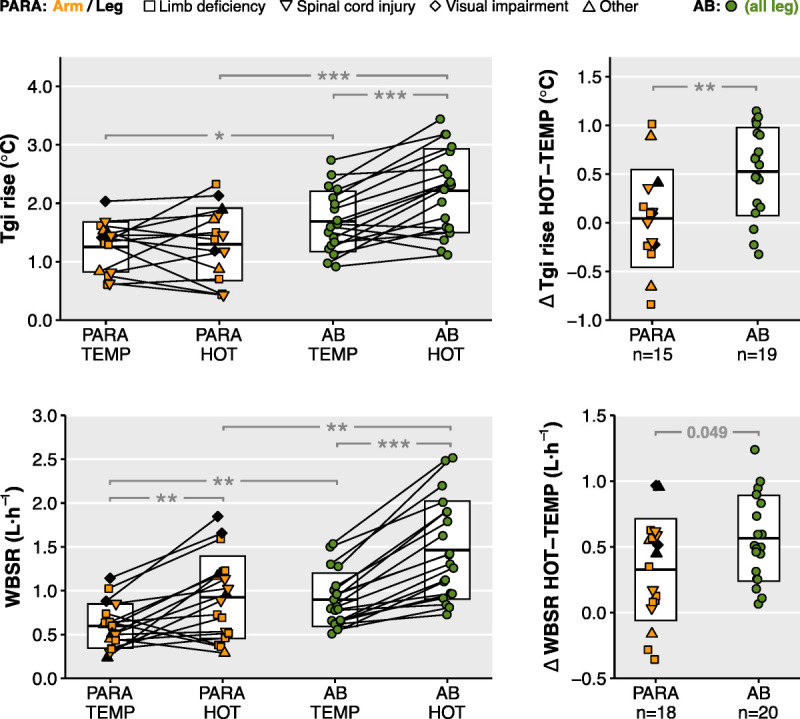
The left panels show the exercise-induced Tgi rise and WBSR in temperate (TEMP) and hot-humid (HOT) conditions, for both para-athletes (PARA) and AB athletes. The right panels show the absolute change in Tgi rise and WBSR in hot-humid vs temperate conditions. For para-athletes, fill and shape indicate exercise mode and impairment type, respectively. Average data are presented as mean ± SD. Asterisks denote P values <0.04, with * for 0.04–0.01, ** for 0.01–0.001, and *** for <0.001, whereas exact P values are presented when P = 0.06–0.04.
FIGURE 4.
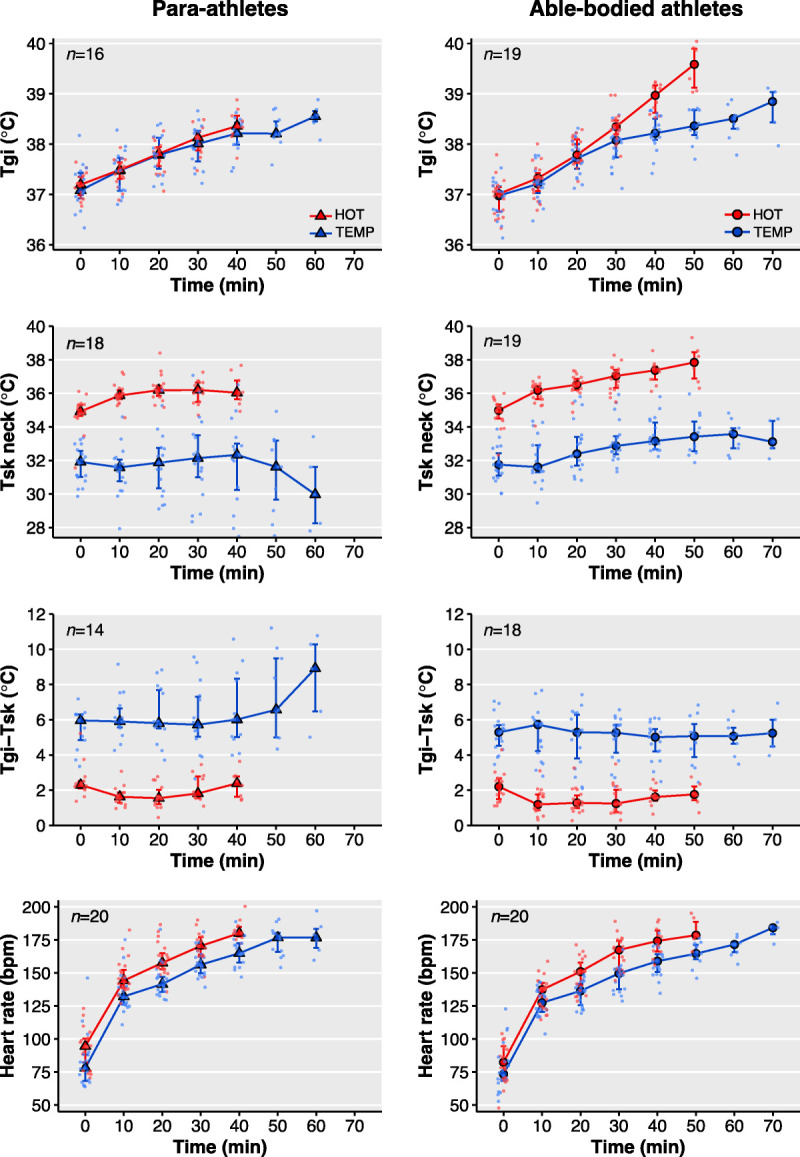
Tgi, Tsk,neck, core-to-skin temperature gradient (Tgi-Tsk), and heart rate over time in temperate (TEMP) and hot-humid (HOT) conditions, for both para-athletes (left) and AB athletes (right). Data are presented as median (IQR) for all time points with sample size ≥3.
Mean exercise heart rate was higher for para-athletes than for AB athletes, in both hot-humid (para 157 ± 13 bpm vs AB 149 ± 10 bpm, P = 0.03) and temperate (para 151 ± 12 vs AB 143 ± 11 bpm, P = 0.046) conditions. For both groups, mean heart rate was elevated in hot-humid versus temperate conditions (Table 2). Peak heart rate was similar between para- and AB athletes in both hot-humid (para 184 ± 13 bpm vs AB 180 ± 11 bpm, P = 0.28) and temperate (para 181 ± 11 bpm vs AB 175 ± 11 bpm, P = 0.13) conditions (Fig. 4; Table 2).
WBSR was lower for para-athletes than for AB athletes, in both hot-humid (para 0.9 ± 0.5 L·h−1 vs AB 1.5 ± 0.6 L·h−1, P = 0.003) and temperate (para 0.6 ± 0.3 L·h−1 vs AB 0.9 ± 0.3 L·h−1, P = 0.002) conditions. The WBSR elevation in hot-humid versus temperate conditions was larger in AB athletes than in para-athletes (Fig. 3; Table 2).
Perceptual responses
Para- and AB athletes showed similar baseline and maximal thermal sensation scores (Fig. 5; ΔHOT–TEMP para vs AB, P = 0.22 (baseline), P = 0.64 (max)). In hot-humid conditions, para-athletes felt less thermally comfortable than AB athletes during baseline rest (ΔHOT–TEMP para vs AB, P = 0.041), but this difference disappeared during exercise (ΔHOT–TEMP para vs AB, P = 0.89). Maximal ratings of perceived exertion were similar among conditions and athlete groups (para: temperate vs hot-humid, 20 (19–20) vs 20 (20–20), P = 0.40; AB: temperate vs hot-humid, 20 (19–20) vs 20 (20–20), P = 0.67; ΔHOT–TEMP para vs AB: P = 0.73).
FIGURE 5.
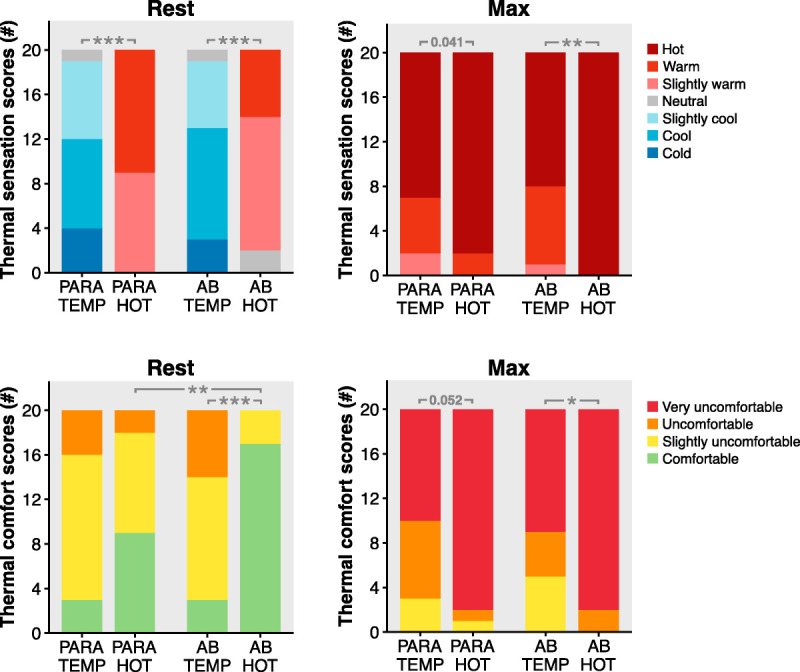
Count (#) of resting and maximal thermal sensation and thermal comfort scores, in temperate (TEMP) and hot-humid (HOT) conditions, for both para-athletes (PARA) and AB athletes. Asterisks denote P values <0.04, with * for 0.04–0.01, ** for 0.01–0.001, and *** for <0.001, whereas exact P values are presented when P = 0.06–0.04.
DISCUSSION
We compared the impact of hot-humid environmental conditions on performance outcomes, thermoregulatory responses, and thermal perception during exercise between elite para- and AB athletes. Elite para-athletes and AB athletes demonstrated similar heat-induced performance decrements, whereas Tgi elevations were markedly lower in para-athletes. Para- and AB athletes showed similar elevations in exercise Tsk, heart rate, and thermal sensation score in hot-humid versus temperate conditions. Large interindividual variability was observed within both para- and AB athlete groups, with heat-related performance losses ranging from 5% to 50% and exercise-induced Tgi rises ranging from −1°C to +1°C in hot-humid versus temperate conditions.
Exercise performance
Our findings indicate that a hot-humid environment induces considerable performance losses in both para- and AB athletes, resembling previous AB studies (4–7). We are the first to quantify the magnitude of heat-induced performance losses in elite para-athletes. Interestingly, performance was considerably impaired in para-athletes, despite similar Tgi in hot-humid and temperate conditions. These findings support the notion that performance impairments in the heat are not only caused by elevations in core temperature but also follow from complex interactions between physiological and perceptual factors (2,3). Indeed, previous AB research also showed that heat-induced performance decrements can occur in the absence of an exacerbated rectal temperature response (4). During incremental exercise to exhaustion in the heat, cardiovascular limitations likely play a major role in the development of fatigue and reduction of maximal aerobic capacity (2,3). We therefore propose that the performance losses in the present study may be attributed to a skin temperature-mediated increase in cardiovascular strain in hot-humid versus temperate conditions (2–4). A high skin temperature narrows the core-to-skin temperature gradient, which increases skin blood flow demands and consequently lowers stroke volume. During submaximal exercise, heart rate increases to maintain cardiac output, but at maximal exercise, cardiac output is likely compromised, accelerating exhaustion (2,3). Indeed, in our study, para- and AB athletes demonstrated similar elevations in neck skin temperature, core-to-skin temperature gradient, and mean heart rate in hot-humid versus temperate conditions. Hence, the skin temperature-mediated increase in cardiovascular strain in hot-humid relative to temperate conditions may have been the primary factor compromising maximal exercise performance in both groups.
Another explanation for the comparable performance losses between para- and AB athletes may relate to the thermal perception during exercise. Previous studies, involving various exercise protocols (self-paced, constant workload, incremental), demonstrated that thermal perception can influence exercise performance independent of core temperature (17–19). During exercise in the heat, skin temperature elevation may aggravate thermal perception and cardiovascular strain, leading to an increased perceived exertion at a given work rate, and thereby a reduction in voluntary exercise capacity (20). In our study, para- and AB athletes demonstrated similar heat-induced elevations in neck skin temperature and heart rate, as well as comparable aggravation of maximal thermal sensation and comfort scores. This was indeed accompanied by a heat-induced increase in perceived exertion for both groups; in hot-humid conditions, maximal perceived exertion scores were similar to that in temperate conditions, even though power output was considerably lower. Thus, the hot-humid environment elicited comparable perceptual responses in para- and AB athletes, which may have impaired exercise performance to a similar extent.
Heat strain
The hot-humid environment exacerbated the hyperthermic response during exercise in AB athletes but not para-athletes. This may be unexpected because it has been suggested that para-athletes have a reduced thermoregulatory ability due to their impairment, exposing them to a greater risk for hyperthermia and exertional heat illness than AB athletes (9,21,22). However, one should take into account that during training and competition, para-athletes will likely exercise at a lower work rate and with a smaller muscle mass than AB athletes, especially those who are wheelchair-bound, resulting in a lower metabolic heat production. To simulate such a realistic scenario, we implemented a personalized exercise protocol, which allowed all athletes to exercise at a similar relative exercise intensity and to reach their individual maximum. Using this approach, we observed that work rate and thus metabolic heat production were considerably lower in para-athletes compared with AB athletes, presumably explaining their lower peak Tgi and WBSR values. The lower WBSR in para-athletes likely resulted from the lower requirement for evaporation, but might also relate to a reduced body surface area for sweating in the para-athletes with an amputation or spinal cord injury (n = 13) (23,24). The lower heat strain in para-athletes compared with AB athletes raises doubt whether, in a real-world sport scenario, the risk for excessive hyperthermia and exertional heat illness is actually higher in para-athletes. This question is further justified by our recent study in which we observed that the incidence of exertional heat illness in Paralympic athletes may be lower than expected (25). Nevertheless, it must be recognized that para-athletes may exhibit severe hyperthermia during competition in the heat, especially those performing lower-body exercise at high intensity or those with a high-level spinal cord injury (8–10). Future experimental studies are required to identify which para-athlete subgroups are at highest risk for severe hyperthermia, considering exercise mode, impairment type, and competition demands. Most importantly, we observed large interindividual differences in the heat-induced Tgi responses, especially within the para-athlete group, emphasizing the need for individual thermal testing of elite athletes in preparation for competition in the heat.
Strengths and limitations
Our study was, to our knowledge, the first to investigate heat-related performance losses in para-athletes. This was done within a well-controlled laboratory setting, and in a unique group of elite athletes. Notwithstanding these strengths, some limitations should be considered. First, we included a heterogeneous group of para-athletes. We explored differences in heat-induced performance decrements or Tgi responses across para-athlete subgroups, but given the low sample size of these subgroups, we need to interpret this with caution. Athletes with severe thermoregulatory impairments, such as a high-level spinal cord injury, may not be able to adequately dissipate the heat produced during exercise, potentially resulting in severe hyperthermia (8). Future studies should investigate heat-induced performance decrements in this specific para-athlete subgroup. Second, the personalized exercise protocol in the present study differs from real-world sports situations with respect to intensity requirements, behavioral responses (e.g., pacing and tactical decisions), and environmental factors (e.g., solar radiation and wind). This may limit the translation to field settings. However, an observational field study may hinder the direct comparison of performance loss between para- and AB athletes, because of uncontrolled factors such as variations in ambient conditions, or influence of tactical elements. Furthermore, we preferred the personalized incremental exercise test to exhaustion over a time trial approach, to allow comparisons across athletes from various sports disciplines. A time-trial approach may not be appropriate for athletes inexperienced with time trials (e.g., tennis players, beach volleyball players), as there may be a learning effect resulting in pacing adjustments from the first to the second test (26). Altogether, this novel and well-controlled assessment of heat-related performance losses in para-athletes provides a solid basis for future research (in the field).
Practical implications
This study provides a unique insight into heat-related performance decrements in elite para-athletes and demonstrates how this relates to performance impairments in elite AB athletes. The comparison to AB athletes is valuable, as practical guidelines and recommendations are predominantly based on AB research (27–30). Our findings suggest that para-athletes, like AB athletes, should use heat mitigation strategies to attenuate performance losses in the heat. However, the optimal type of cooling may depend on the thermoregulatory responses accompanying the performance loss. For para-athletes exercising at a low work rate, a high core temperature may rarely be the main factor limiting exercise performance. These athletes might therefore predominantly benefit from cooling techniques that reduce the exercise-induced rise in skin temperature and improve thermal perception (e.g., cooling vest, cold packs), rather than methods that primarily aim to attenuate the rise in core temperature (e.g., ice slurry). However, we observed large interindividual differences within both para- and AB athlete groups, suggesting that individual testing of elite athletes is necessary to develop personalized heat mitigation plans.
CONCLUSIONS
Hot-humid conditions severely impaired exercise performance in both elite para-athletes and elite AB athletes, as evidenced by reductions in TTE of 26% (20%–31%) and 27% (19%–32%), respectively. AB athletes demonstrated considerable Tgi elevations in hot-humid versus temperate conditions, whereas no Tgi differences were apparent in para-athletes. Nevertheless, para- and AB groups showed similar elevations in exercise Tsk, heart rate, and thermal sensation score in hot-humid versus temperate conditions. These findings suggest that both para- and AB athletes should utilize heat mitigation strategies to attenuate performance loss during competition in the heat. Extensive thermal testing in both para- and AB settings is recommended to determine the optimal heat mitigation strategy for each individual athlete.
Acknowledgments
The authors would like to thank the participating athletes (including their coaches and staff) for their participation in and dedication to the study. The authors would also like to thank NOC*NSF and Sport Science and Innovation Centre Papendal for their valuable assistance with recruitment and data collection, and for the use of their climate chamber. We recognize the excellent assistance of Sam Ballak, Lars Bouten, Dominique ten Haaf, Iris Hesen, Bregina Kersten, Joep van Kesteren, Sophie Kroesen, Meijke Linders, and Malou Nuijten in the data collection for the present study.
This study was funded by ZonMw (no. 546001003) as part of the ThermoTokyo project. P. A. was funded by the Nederlandse Organisatie voor Wetenschappelijk Onderzoek (P16-28). All authors declare that they have no conflict of interest to report relevant to the present study. The results of this study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. The results of the present study do not constitute endorsement by the American College of Sports Medicine.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.acsm-msse.org).
Contributor Information
PUCK ALKEMADE, Email: puck.alkemade@vu.nl.
JOHANNUS Q. DE KORTE, Email: yannick.dekorte@radboudumc.nl.
COEN C. W. G. BONGERS, Email: coen.bongers@han.nl.
HEIN A. M. DAANEN, Email: h.a.m.daanen@vu.nl.
MARIA T. E. HOPMAN, Email: maria.hopman@radboudumc.nl.
THOMAS W. J. JANSSEN, Email: t.w.j2.janssen@vu.nl.
REFERENCES
- 1.Smith KR Woodward A Lemke B, et al. The last Summer Olympics? Climate change, health, and work outdoors. Lancet. 2016;388(10045):642–4. [DOI] [PubMed] [Google Scholar]
- 2.Nybo L, Rasmussen P, Sawka MN. Performance in the heat—physiological factors of importance for hyperthermia-induced fatigue. Compr Physiol. 2014;4(2):657–89. [DOI] [PubMed] [Google Scholar]
- 3.Périard JD, Eijsvogels TMH, Daanen HAM. Exercise under heat stress: thermoregulation, hydration, performance implications, and mitigation strategies. Physiol Rev. 2021;101(4):1873–979. [DOI] [PubMed] [Google Scholar]
- 4.Tatterson AJ, Hahn AG, Martini DT, Febbraio MA. Effects of heat stress on physiological responses and exercise performance in elite cyclists. J Sci Med Sport. 2000;3(2):186–93. [DOI] [PubMed] [Google Scholar]
- 5.Arngrímsson SÁ, Petitt DS, Borrani F, Skinner KA, Cureton KJ. Hyperthermia and maximal oxygen uptake in men and women. Eur J Appl Physiol. 2004;92(4):524–32. [DOI] [PubMed] [Google Scholar]
- 6.Périard JD, Cramer MN, Chapman PG, Caillaud C, Thompson MW. Cardiovascular strain impairs prolonged self-paced exercise in the heat. Exp Physiol. 2011;96(2):134–44. [DOI] [PubMed] [Google Scholar]
- 7.de Korte JQ, Bongers CCWG, Hopman MTE, Eijsvogels TMH. Exercise performance and thermoregulatory responses of elite athletes exercising in the heat: outcomes of the Thermo Tokyo study. Sports Med. 2021;51(11):2423–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Price MJ, Trbovich M. Thermoregulation following spinal cord injury. In: Romanovsky A, editor. Handbook of Clinical Neurology. Thermoregulation: From Basic Neuroscience to Clinical Neurology, Part II. Amsterdam (the Netherlands): Elsevier; 2018. pp. 799–820. [DOI] [PubMed] [Google Scholar]
- 9.Griggs KE, Stephenson BT, Price MJ, Goosey-Tolfrey VL. Heat-related issues and practical applications for Paralympic athletes at Tokyo 2020. Temperature (Austin). 2020;7(1):37–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stephenson BT, Hoekstra SP, Tolfrey K, Goosey-Tolfrey VL. High thermoregulatory strain during competitive paratriathlon racing in the heat. Int J Sports Physiol Perform. 2020;15(2):231–7. [DOI] [PubMed] [Google Scholar]
- 11.Pelliccia A Sharma S Gati S, et al. 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease: the task force on sports cardiology and exercise in patients with cardiovascular disease of the European Society of Cardiology (ESC). Eur Heart J. 2021;42(1):17–96. [DOI] [PubMed] [Google Scholar]
- 12.de Korte JQ Bongers CCWG Hopman MTE, et al. Performance and thermoregulation of Dutch Olympic and Paralympic athletes exercising in the heat: rationale and design of the Thermo Tokyo study: the journal temperature toolbox. Temperature (Austin). 2021;8(3):209–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bongers CCWG, Daanen HAM, Bogerd CP, Hopman MTE, Eijsvogels TMH. Validity, reliability, and inertia of four different temperature capsule systems. Med Sci Sports Exerc. 2018;50(1):169–75. [DOI] [PubMed] [Google Scholar]
- 14.Bongers CCWG, Hopman MTE, Eijsvogels TMH. Validity and reliability of the myTemp ingestible temperature capsule. J Sci Med Sport. 2018;21(3):322–6. [DOI] [PubMed] [Google Scholar]
- 15.Gagge AP, Stolwijk JA, Hardy JD. Comfort and thermal sensations and associated physiological responses at various ambient temperatures. Environ Res. 1969;2(3):209–29. [DOI] [PubMed] [Google Scholar]
- 16.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–81. [PubMed] [Google Scholar]
- 17.Schlader ZJ, Simmons SE, Stannard SR, Mündel T. The independent roles of temperature and thermal perception in the control of human thermoregulatory behavior. Physiol Behav. 2011;103(2):217–24. [DOI] [PubMed] [Google Scholar]
- 18.Stevens CJ, Thoseby B, Sculley DV, Callister R, Taylor L, Dascombe BJ. Running performance and thermal sensation in the heat are improved with menthol mouth rinse but not ice slurry ingestion. Scand J Med Sci Sports. 2016;26(10):1209–16. [DOI] [PubMed] [Google Scholar]
- 19.Kroesen SH, de Korte JQ, Hopman MTE, Bongers CCWG, Eijsvogels TMH. Impact of thermal sensation on exercise performance in the heat: a Thermo Tokyo sub-study. Eur J Appl Physiol. 2022;122(2):437–46. [DOI] [PubMed] [Google Scholar]
- 20.Flouris AD, Schlader ZJ. Human behavioral thermoregulation during exercise in the heat. Scand J Med Sci Sports. 2015;25(Suppl 1):52–64. [DOI] [PubMed] [Google Scholar]
- 21.Grobler L, Derman W, Racinais S, Ngai ASH, van de Vliet P. Illness at a Para Athletics Track and Field World Championships under hot and humid ambient conditions. PM R. 2019;11(9):919–25. [DOI] [PubMed] [Google Scholar]
- 22.Hosokawa Y Adami PE Stephenson BT, et al. Prehospital management of exertional heat stroke at sports competitions for Paralympic athletes. Br J Sports Med. 2022;56(11):599–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gagnon D, Jay O, Kenny GP. The evaporative requirement for heat balance determines whole-body sweat rate during exercise under conditions permitting full evaporation. J Physiol. 2013;591(11):2925–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cramer MN, Jay O. Biophysical aspects of human thermoregulation during heat stress. Auton Neurosci. 2016;196:3–13. [DOI] [PubMed] [Google Scholar]
- 25.Alkemade P Daanen HAM Janssen TWJ, et al. Heat preparedness and exertional heat illness in Paralympic athletes: a Tokyo 2020 survey. Temperature (Austin). 2022;2147364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Corbett J, Barwood MJ, Parkhouse K. Effect of task familiarisation on distribution of energy during a 2000 m cycling time trial. Br J Sports Med. 2009;43(10):770–4. [DOI] [PubMed] [Google Scholar]
- 27.Casa DJ DeMartini JK Bergeron MF, et al. National Athletic Trainers’ Association position statement: exertional heat illnesses. J Athl Train. 2015;50(9):986–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Racinais S Alonso JM Coutts AJ, et al. Consensus recommendations on training and competing in the heat. Br J Sports Med. 2015;49(18):1164–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pryor JL, Johnson EC, Roberts WO, Pryor RR. Application of evidence-based recommendations for heat acclimation: individual and team sport perspectives. Temperature (Austin). 2019;6(1):37–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roberts WO, Armstrong LE, Sawka MN, Yeargin SW, Heled Y, O’Connor FG. ACSM expert consensus statement on exertional heat illness: recognition, management, and return to activity. Curr Sports Med Rep. 2021;20(9):470–84. [DOI] [PubMed] [Google Scholar]


