Triple-negative breast cancer (TNBC) has aggressive characteristics as exemplified by the high risk of recurrence, metastasis, and patient mortality.1 Cytotoxic chemotherapy may reduce tumor burden initially, but leave behind chemo-resistant breast cancer stem cells (BCSCs) that lead to tumor recurrence and metastasis.2 Chemotherapy induces BCSC enrichment through the activation of glutathione biosynthesis pathways, which increases intracellular glutathione levels and specifies the BCSC phenotype through complicated downstream signaling pathways.3 Glutathione S-transferases (GSTs), a superfamily (which contains seven cytosolic classes: Alpha, Kappa, Mu, Omega, Pi, Theta, and Zeta, and one microsomal class MGSTs) of phase II enzymes that catalyze the conjugation of glutathione with electrophilic compounds, play a critical role in detoxification and chemotherapy resistance of cancer cells. However, the role of GSTs in the regulation of BCSCs is largely elusive. In the present study, we first investigated the expression of all GST family members in response to chemotherapeutic drug carboplatin treatment at the dose of IC50 in multiple TNBC cell lines, and found four members of the GST Mu family (GSTM1, GSTM2, GSTM3, and GSTM4) were markedly repressed in all four cell lines (Fig. 1A). GSTM1/2/3/4 mRNA and protein were also repressed by other FDA-approved chemotherapy drugs paclitaxel and gemcitabine at the dose of IC50 in TNBC cell lines (Fig. 1B; Fig. S1A–D). Carboplatin also repressed GSTM1/2/3/4 expression in vivo, as shown in SCID (severe combined immunodeficiency) mice transplanted with MDA-MB-231 cells (Fig. 1C) and in MMTV-PyMT transgenic mice (a genetically engineered autochthonous breast cancer model) (Fig. 1D) that were treated by carboplatin.
Figure 1.
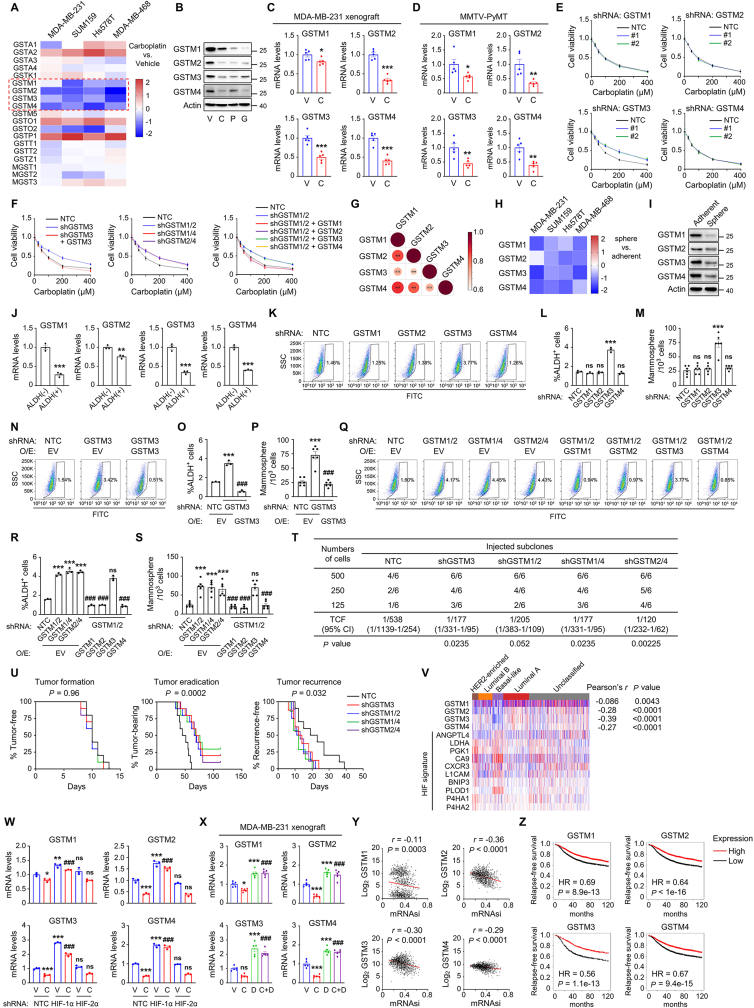
Chemotherapy induces breast cancer stem cell enrichment through repression of GSTM1/2/3/4. (A) TNBC cell lines were treated with carboplatin at the dose of IC50 for 72 h and RT-qPCR was performed for expression of glutathione S-transferases. (B) MDA-MB-231 cells were treated with vehicle (V), 100 μM carboplatin (C), 10 nM paclitaxel (P), or 10 nM gemcitabine (G) for 72 h and immunoblot assays were performed to analyze GSTM protein expression. (C) MDA-MB-231 cells were implanted into the mammary fat pad of female SCID mice and mice were treated with vehicle or carboplatin (20 mg/kg on days 0, 5, 10). Tumors were harvested on day 13 for RT-qPCR (mean ± SEM; n = 5); ∗P < 0.05, ∗∗∗P < 0.001 vs. V. (D) MMTV-PyMT transgenic mice were treated with vehicle or carboplatin (20 mg/kg on days 0, 5, 10) and tumors were harvested on day 13 for RT-qPCR (mean ± SEM; n = 5); ∗P < 0.05, ∗∗P < 0.01 vs. V. (E, F) MDA-MB-231 subclones were treated with carboplatin at indicated doses for 72 h and cell counting kit-8 (CCK-8) assay was performed (mean ± SEM; n = 3). (G) The correlation of protein sequences was analyzed. (H) TNBC cell lines were cultured on standard polystyrene tissue culture plates (adherent) or ultra-low adherence plates (sphere) for 7 days and RT-qPCR was performed. (I) MDA-MB-231 cells were cultured on standard polystyrene tissue culture plates or ultra-low adherence plates for 7 days and immunoblot assays were performed. (J) MDA-MB-231 cells were sorted into ALDH-negative (−) and ALDH-positive (+) populations by flow cytometry and RT-qPCR was performed (mean ± SEM; n = 3); ∗∗P < 0.01, ∗∗∗P < 0.001 vs. ALDH (−). (K–S) The percentage of ALDH+ cells (L, O, R; mean ± SEM; n = 3) and the number of mammospheres per 1000 cells seeded (M, P, S; mean ± SEM; n = 6) were determined in MDA-MB-231 subclones. The representative results of the Aldefluor assay were shown (K, N, Q). ∗∗∗P < 0.001 vs. NTC; ###P < 0.001 vs. shGSTM3 in (L, M), ###P < 0.001 vs. shGSTM1/2 in (R, S); ns, not significant. (T) SCID mice were injected with indicated numbers of MDA-MB-231 subclone cells and tumor-initiating cell frequency (TCF) with 95% confidence intervals (CI) was calculated. (U) 2 × 106 MDA-MB-231 subclone cells were implanted into SCID mice. When tumors became palpable, mice were treated with 20 mg/kg carboplatin every 5 days until tumors were no longer palpable. Kaplan–Meier survival curves of tumor-free (left), tumor-bearing (center), and recurrence-free (right) were plotted and P values of log-rank tests are shown (n = 10). (V) Expression of GSTM1/2/3/4 and ten mRNAs encoded by HIF target genes are shown for primary breast cancers accessed from the TCGA database. (W) MDA-MB-231 subclones were treated with vehicle or 100 μM carboplatin for 72 h and RT-qPCR was performed (mean ± SEM; n = 3); ∗P < 0.05, ∗∗P < 0.01, ∗∗∗P < 0.001 vs. NTC V; ###P < 0.001 vs. NTC C; ns, not significant. (X) MDA-MB-231 cells were implanted into the mammary fat pad of female SCID mice and mice were treated with vehicle, carboplatin (20 mg/kg on days 0, 5, 10), digoxin (2 mg/kg on days 1–13), or carboplatin and digoxin. Tumors were harvested on day 13 for RT-qPCR (mean ± SEM; n = 5); ∗P < 0.05, ∗∗∗P < 0.001 vs. V; ###P < 0.001 vs. C; ns, not significant. (Y) Pearson's test was performed to analyze the correlation of GSTM1/2/3/4 mRNA expression with mRNAsi in TCGA samples. (Z) Kaplan–Meier analyses of relapse-free survival were performed based on clinical and molecular data from 4,929 breast cancer patients. The patients were stratified by GSTM1/2/3/4 mRNA levels in the primary tumor, which were greater (red) or less (black) than the median level. The hazard ratio (HR) and P value (log-rank test) are shown.
To investigate the role of GSTM1/2/3/4 in response to chemotherapy, we generated short hairpin RNA (shRNA)-mediated GSTM1/2/3/4 knockdown subclones in MDA-MB-231 and SUM159 cells (Fig. S2A) and found that knockdown of GSTM1/2/3/4 did not affect cell proliferation rate (Fig. S2B). GSTM3 knockdown made MDA-MB-231 and SUM159 cells more resistant to carboplatin treatment (Fig. 1E; Fig. S2C), which was rescued by transfection with an shRNA-resistant GSTM3 expression vector (Fig. 1F left; Fig. S2D). Interestingly, although knockdown of GSTM1, GSTM2, or GSTM4 did not affect sensitivity to carboplatin (Fig. 1E; Fig. S2C), the combination of double knockdown of these three made MDA-MB-231 and SUM159 cells more resistant to carboplatin treatment (Fig. 1F middle; Fig. S2E), suggesting a redundant role of these three proteins. The effect of GSTM1/2 double knockdown was rescued by overexpression of shRNA-resistant GSTM4, as well as GSTM1 or GSTM2, but not GSTM3 (Fig. 1F right; Fig. S2F), which further confirmed the redundancy of GSTM1/2/4, but not GSTM3. These results were consistent with the correlation analysis of GSTMs based on protein sequences (Fig. 1G).
Next, we investigated the role of GSTMs in the regulation of the BCSC phenotype. GSTM1/2/3/4 mRNA and protein levels were all significantly decreased in BCSC-enriched nonadherent mammosphere cultures (Fig. 1H, I) and aldehyde dehydrogenase positive (ALDH+) population (Fig. 1J; Fig. S3A), suggesting a negative correlation of GSTM1/2/3/4 expression with the BCSC phenotype. Knockdown of GSTM3, but not GSTM1/2/4, increased the percentage of ALDH+ cells (Fig. 1K, L; Fig. S3B) and the number of mammosphere-forming cells (Fig. 1M; Fig. S3C) in MDA-MB-231 and SUM159 cells, which was rescued by overexpression of shRNA-resistant GSTM3 (Fig. 1N–P; Fig. S3D, E). The combination of GSTM1/2/4 double knockdown also increased the percentage of ALDH+ cells (Fig. 1Q, R; Fig. S3F) and the number of mammosphere-forming cells (Fig. 1S; Fig. S3G) in MDA-MB-231 and SUM159 cells. Overexpression of shRNA-resistant GSTM1, GSTM2, or GSTM4, but not GSTM3, abrogated the induction of BCSC population mediated by GSTM1/2 double knockdown (Fig. 1Q–S; Fig. S3F, G), confirming the redundant role of GSTM1/2/4 in the regulation of the BCSC phenotype.
To investigate the role of GSTMs in regulating the BCSC phenotype in vivo, we performed tumorigenicity assays by injecting 500, 250, and 125 cells of the MDA-MB-231 NTC (nontargeting control), GSTM3-, GSTM1/2-, GSTM1/4-, and GSTM2/4-knockdown subclone into the mammary fat pad (MFP) of SCID mice. Knockdown of GSTM3, or double knockdown of GSTM1/2, GSTM1/4, or GSTM2/4 significantly increased tumor-initiating capacity (Fig. 1T). To determine the role of GSTMs in response to chemotherapy in vivo, we injected 2 × 106 cells of the MDA-MB-231 NTC, GSTM3-, GSTM1/2-, GSTM1/4-, and GSTM2/4-knockdown subclone into the MFP of SCID mice. When tumors became palpable, we started to treat the mice with 20 mg/kg carboplatin every 5 days. Treatment was terminated when tumors were no longer palpable, and the mice were monitored for tumor recurrence. Knockdown of GSTM3, or double knockdown of GSTM1/2, GSTM1/4, or GSTM2/4, did not affect time to tumor formation (Fig. 1U, left), but significantly increased time to tumor remission (Fig. 1U, middle), which is consistent with the in vitro results that GSTMs knockdown did not affect cell growth but made cells resistant to carboplatin treatment. Most importantly, the knockdown of GSTM3, or double knockdown of GSTM1/2, GSTM1/4, or GSTM2/4, significantly decreased the time to tumor recurrence (Fig. 1U, right), demonstrating that GSTMs inhibit the BCSC phenotype after carboplatin treatment in vivo.
Next, we investigated the regulatory mechanism of GSTMs repression in response to chemotherapy. The transcription factor hypoxia-inducible factors (HIFs) have been reported to play a critical role in chemotherapy-mediated BCSC maintenance and specification.4 Therefore, we examined whether chemotherapy-mediated GSTM repression is HIF-dependent. We analyzed gene expression data from 1097 breast cancer patients in the Cancer Genome Atlas (TCGA) database and found that the expression of GSTM1/2/3/4 was all negatively correlated with a HIF-metagene signature (Fig. 1V), suggesting that their expression is repressed by HIFs in primary human breast cancer samples. We generated shRNA-mediated HIF-1α or HIF-2α knockdown subclones in MDA-MB-231 and SUM159 cells and found that HIF-1α knockdown, but not HIF-2α knockdown, increased GSTM1/2/3/4 expression, and abrogated carboplatin-mediated GSTM1/2/3/4 repression in MDA-MB-231 (Fig. 1W) and SUM159 (Fig. S4A) cells. Pharmacological inhibition of HIF-1α by digoxin also increased GSTM1/2/3/4 expression and abrogated carboplatin-mediated GSTM1/2/3/4 repression (Fig. S4B). We also treated SCID mice injected with MDA-MB-231 cells with carboplatin (20 mg/kg every 5 days) in combination with digoxin (2 mg/kg daily) and found that digoxin abrogated carboplatin-mediated repression of GSTM1/2/3/4 expression in tumor samples (Fig. 1X). Taken together, these data indicate that chemotherapy regulates GSTM1/2/3/4 expression in a HIF-1-dependent manner in vitro and in vivo.
To determine the clinical implication of GSTM expression in breast cancer, we interrogate data from TCGA and revealed a negative correlation of GSTM1/2/3/4 expression with mRNA expression-based stemness index (mRNAsi), a machine learning-based parameter that evaluates cancer cell stemness in primary patients' samples (Fig. 1Y).5 We also analyzed expression data and clinical information from 4929 breast cancer patients and stratified patients according to GSTM1/2/3/4 expression. Kaplan–Meier plots revealed that GSTM1/2/3/4 mRNA levels greater than the median were associated with increased relapse-free survival (Fig. 1Z). These data indicate that GSTM1/2/3/4 expression is associated with the inhibition of BCSC phenotype and better clinical outcomes in breast cancer patients.
In summary, we demonstrate that chemotherapy-repressed GSTM expression plays a critical role in the regulation of the BCSC phenotype. Among GSTM family members, GSTM1, GSTM2, and GSTM4 are closely correlated in function and have a redundant role in the regulation of chemotherapy responses and the BCSC phenotype, although the different regulatory role of GSTM3 and GSTM1/2/4 is not fully delineated. The molecular mechanisms through which GSTMs regulate chemotherapy-induced BCSC enrichment, especially whether the glutathione s-transferase enzymatic activity of GSTMs is required in this process, need to be further elucidated. Mechanistically, GSTM expression is repressed by chemotherapy treatment in a HIF-1-dependent manner. This study brings new insights into the molecular mechanism of chemotherapy-induced BCSC enrichment, and provides a different role of HIF-1 in the regulation of the BCSC phenotype, through transcriptional repression of downstream genes.
Ethics declaration
Animal protocols were approved by the Institutional Animal Care and Use Committee of Shandong University.
Author contributions
J.H., G.J., and H.L. designed the research study. J.H., Y.Y., Y.H., and J.H. performed experiments and acquired data. Y.Y. and Y.H. performed database analyses. J.H., Y.Y., and Y.H. performed statistical analyses. J.H., G.J., and H.L. analyzed the data and wrote the manuscript. G.J. and H.L. supervised the study. All authors reviewed and commented on the manuscript.
Conflict of interests
The authors declare no competing interests.
Funding
This work was supported by the Natural Science Foundation of Shandong Province, China (No. ZR2021YQ50, Excellent Young Scholars Program). H.L. is the Taishan Scholar Young Talent Professor of Shandong Province, China, and the Cheeloo Young Talent Professor at Shandong University.
Footnotes
Peer review under responsibility of Chongqing Medical University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.gendis.2023.04.005.
Contributor Information
Guangyu Ji, Email: jigy2022@sdu.edu.cn.
Haiquan Lu, Email: lvhaiquan@sdu.edu.cn.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Dent R., Trudeau M., Pritchard K.I., et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;13(15 Pt 1):4429–4434. doi: 10.1158/1078-0432.CCR-06-3045. [DOI] [PubMed] [Google Scholar]
- 2.Pece S., Tosoni D., Confalonieri S., et al. Biological and molecular heterogeneity of breast cancers correlates with their cancer stem cell content. Cell. 2010;140(1):62–73. doi: 10.1016/j.cell.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 3.Lu H., Samanta D., Xiang L., et al. Chemotherapy triggers HIF-1-dependent glutathione synthesis and copper chelation that induces the breast cancer stem cell phenotype. Proc Natl Acad Sci U S A. 2015;112(33):E4600–E4609. doi: 10.1073/pnas.1513433112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu H., Xie Y., Tran L., et al. Chemotherapy-induced S100A10 recruits KDM6A to facilitate OCT4-mediated breast cancer stemness. J Clin Invest. 2020;130(9):4607–4623. doi: 10.1172/JCI138577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malta T.M., Sokolov A., Gentles A.J., et al. Machine learning identifies stemness features associated with oncogenic dedifferentiation. Cell. 2018;173(2):338–354. doi: 10.1016/j.cell.2018.03.034. e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.