Abstract
Objectives
Method-dependent comparison of antimicrobial agents’ efficacy against oral pathogens.
Materials and methods
Several sodium hypochlorite solutions (NaOCl)—Perisolv®, Carisolv® and Dakin’s solution—were equated with chlorhexidine (CHX) and hydrogen peroxide (H2O2) against ten oral micro-organisms related to caries and periodontitis using different minimum inhibitory concentration (MIC) and the minimum bactericidal concentration (MBC) techniques. Agents were adjusted to the final 70 mmol/L concentration of active chlorine molecule.
Results
Apart from H2O2 and the amino acids of Perisolv®, all the agents revealed an antimicrobial effect. Agar diffusion test ranked CHX (p < 0.05) as the most effective against all ten specimens, followed by the NaOCl of Perisolv® and Dakin’s solution. Correspondingly, in broth microdilution on agar, CHX was the most effective in eradicating micro-organisms at 0.03 mmol/L compared with 2.2 mmol/L of Dakin’s solution. In contrast, the bactericidal concentration of Dakin’s solution was the most effective at 0.2 mmol/L, (p < 0.001), followed by Perisolv® (2.14 mmol/L), CHX (2.38 mmol/L) and Carisolv® (3.33 mmol/L) after 5 and 10 min in broth dilution test. In live/dead analysis, 60-min exposure to a 2-fold concentration of agents resulted in two-log Aggregatibacter actinomycetemcomitans inhibition by CHX (35 mmol/L) whilst Streptococcus mutans was more susceptible, in 0.8 and 8.8 mmol/L, after 10 min to CHX and Dakin’s respectively.
Conclusion
Replacement of CHX with tested hypochlorite agents showed evident potential and promoted rapid antimicrobial effect.
Clinical relevance
Effective antimicrobial agents are crucial in controlling pathogen-induced oral infections increasing clinical possibilities to combat oral biofilms. Additionally, CHX substitution with hypochlorite agents could eliminate CHX’s adverse effects.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00784-023-05190-0.
Keywords: Chlorhexidine, Chlorine compounds, Dakin’s, Dental caries, Oral disease, Periodontitis
Introduction
Oral biofilms, associated with oral diseases including dental caries and periodontitis, comprise a large number of oral micro-organisms [1–3]. A vast community of bacteria is closely related to the occurrence and function of the complex dental plaque that further can lead to the tissue destruction at patient level and outlines oral infections [3–8].
In dental caries, many of the acid-producing bacteria are gram-positive in nature, including Streptococcus mutans, Streptococcus mitis and Actinomyces naeslundii [5, 9], whereas periodontally related species, such as Staphylococcus aureus, Prevotella intermedia, Prevotella nigrescens and Fusobacterium nucleatum, are more frequently facultative anaerobes and belong to the phylum of gram-negative bacteria [10, 11]. Collectively, the microbiome is a direct precursor of the induced diseases [2, 6]; however, Streptococcus mutans is still the main contributor to the adhesion and dwelling of the dental biofilm as a result of its amyloid formation capacity [5, 12].
Over time, different preventive strategies have been used to reduce the number of micro-organisms and, thereby, the risk of disease [13–15]. Interest has focused on mechanical plaque removal, but a variety of antimicrobial agents have also been introduced [16].
Chlorhexidine is a compound that has been shown to possess bactericidal properties and it works by damaging the outer cell layers of bacterial cells, leading to passive diffusion through the inner layer and the subsequent collapse of the membrane potential and lysis of the cells. Studies have reported that gram-positive cocci bacteria are particularly sensitive to chlorhexidine [17]. However, the rate of this reaction is dependent on the pH of the environment in which it occurs [18]. Against periodontal diseases, chlorhexidine (CHX) is the golden standard amongst oral antiseptics and is therefore frequently used [19, 20]. However, the effect of CHX on dental caries is more uncertain [21]. Additionally, local side-effects are reported, particularly from the use of CHX, including discoloration of the teeth and tongue, as well as taste disturbances [21–23].
Agents such as peroxides, Taurolidine, Triclosan, essential oils and Povidone-iodine have been recommended as substitutes for CHX solutions due to their capacity to penetrate the biofilm mass, resulting in either a bacteriostatic or a bactericidal effect [24–28]. Oxidising agents, such as hydrogen peroxide (H2O2), are commonly used in clinical settings due to their broad-spectrum antimicrobial activity. H2O2 is effective against gram-negative bacteria and is considered environmentally and tissue friendly, as it rapidly decomposes into water and oxygen [18]. The main constituent of Dakin’s dental solution is sodium hypochlorite (NaOCl), which has well-known antimicrobial properties due to its action as an oxidising agent [7]. The exact mechanism of action is not fully understood, but it is believed that these agents transfer electrons from the substrate, resulting in substrate’s oxidation and simultaneous reduction of the agent, a process that disrupts and/or cleaves the chemical bonds in proteins, carbohydrates [29] and lipids [17]. At alkaline pH, the dominant form of chlorine is hypochlorite (OCl-), which is known to have a more rapid reaction and greater efficacy against bacterial spores compared with other forms [17]. It is therefore routinely used during endodontic work [30]. In addition to NaOCl’s broad antimicrobial features, it does not stain the tissue and is easy to use [31, 32].
Sodium-hypochlorite-based products with added amino acids, launched at the end of the 20th century, are used in chemo-mechanical caries removal (Carisolv®) [33, 34] and in cleansing the periodontal pocket (Perisolv®) [35]. These products possess an antimicrobial capacity with a grade [36] comparable to Dakin’s solution [7] or stabilised hypochlorous acid [37]. Apart from other halogens—fluoride (F-), bromide (Br-) and iodide (I-)—in aqueous solutions known to be antibacterial, chloride (Cl-) is more compatible with biological enzymatic reactions and therefore has least side effects [38]. On the contrary to the relatively unreactive hydrogen peroxide representing slow reaction kinetics with the biomolecules [18, 39, 40], the oxidative chlorine solutions (NaOCl) are both short-lived and easily turned into tissue friendly salt products [40, 41].
This study aimed to compare the efficacy of currently available chlorine solutions, especially chloramine-containing solutions, with other well-known antimicrobial substances on different oral pathogens. The null hypothesis states that chloramines do not have the potential to act as an antimicrobial agent against bacteria related to caries and periodontitis.
Materials and methods
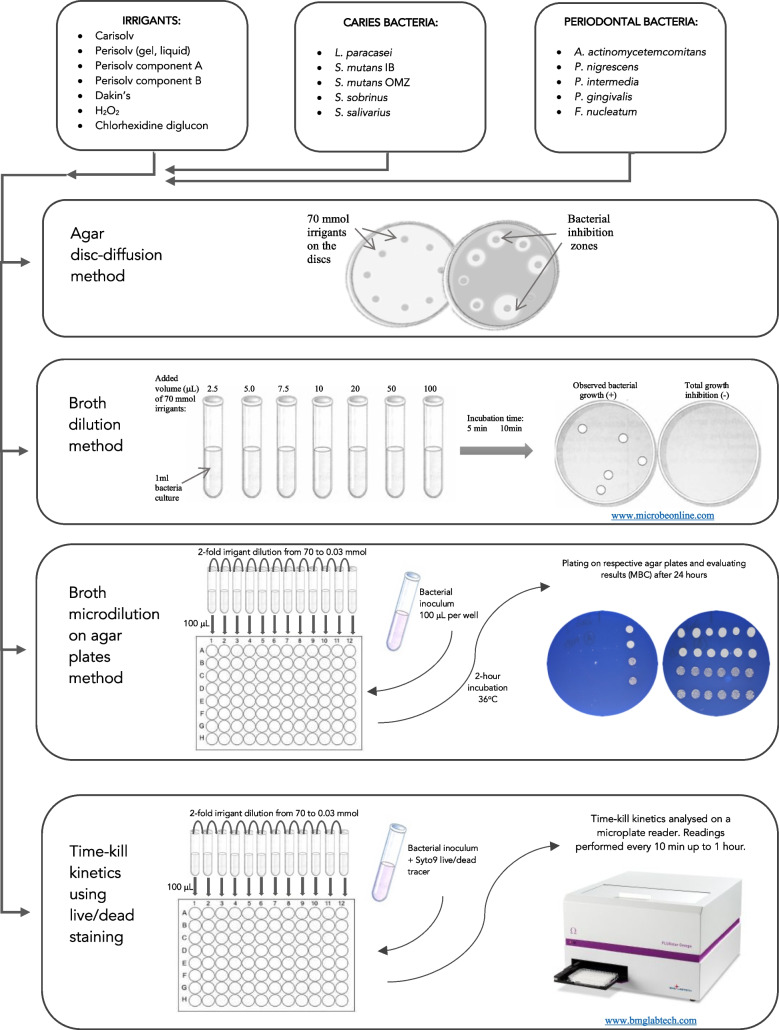
Selected irrigants (Table 1) were tested to verify their antimicrobial potency against ten different bacterial strains related to dental caries and periodontitis (Table 2). The efficacy of irrigants was compared using several methods to determine both the minimal inhibitory concentration (MIC) and the minimum bactericidal concentration (MBC) values. A flowchart of methods included in this study is presented in Fig. 1.
Table 1.
List of irrigants used in the study. The final concentration of chemicals was adjusted regarding the active chlorine at 70 mmol/L (~0.5% of active chlorine) before use
| Irrigant | Active part | pH | Abbreviation | Manufacturer |
|---|---|---|---|---|
| Carisolv® (gel) | -NH2Cl | 11.0 | CAR | RLS Global AB, Gothenburg, Sweden |
| Perisolv® (gel) | -NH2Cl | 11.0 | PER | RLS Global AB, Gothenburg, Sweden |
| Perisolv® (liquid) | -NH2Cl | 11.0 | NOG | RLS Global AB, Gothenburg, Sweden |
| Perisolv, component A (liquid)* | -OCl | 11.0 | OCL | RLS Global AB, Gothenburg, Sweden |
| Amino acids of Perisolv, component B (gel)** | -NH2 | 11.0 | AAP | RLS Global AB, Gothenburg, Sweden |
| Dakin’s solution | -(H)OCl | 9.0 | DAK | APL, Sweden |
| Hydrogen peroxide solution | -O2 | 4.0 | H2O2 | 16 911, MERCK KGaA, Darmstadt, Germany |
| Chlorhexidine diglucon | -HN(C(NH)NH2)2 | 7.0 | CHX | C9394, MERCK KGaA, Darmstadt, Germany |
*Component A, 135 ± 25 mmol l-1; **component B, 53 mmol l-1
Table 2.
Bacterial specimens used in the study
| Bacterial strains | Group | Gram | Abbreviation | Selective agar |
|---|---|---|---|---|
| Lactobacillus paracasei CCUG 32212 | Caries | Positive | LBC | RogosaA |
| Streptococcus mutans IB | Caries | Positive | SM-IB | MSBB |
| Streptococcus mutans OMZ65 | Caries | Positive | SM-65 | MSBB |
| Streptococcus sobrinus B13 | Caries | Positive | SS-B13 | MSBB |
| Streptococcus salivarius ATCC8618 | Caries | Positive | SS-8618 | MSC |
| Porphyromonas gingivalis OMGS1740 | Periodontal | Negative | PG | BrucellaD |
| Prevotella nigrescens ATCC33563 | Periodontal | Negative | PN | BrucellaD |
| Prevotella intermedia ATCC25611 | Periodontal | Negative | PI | BrucellaD |
|
Aggregatibacter actinomycetemcomitans ATCC29522 serotype b, smooth phenotype |
Periodontal | Negative | AA | TSBE |
| Fusobacterium nucleatum ATCC10953 | Periodontal | Negative | FN | BrucellaD |
ADifcoTM Rogosa SL Agar (Becton and Dickinson, Le Pont de Claix, France)
BDifcoTM Mitis Salivarius Agar (Becton and Dickinson, Le Pont de Claix, France, supplemented with bacitracin and saccharose)
CDifcoTM Mitis Salivarius Agar (Becton and Dickinson, Le Pont de Claix, France)
DBrucella Agar (Neogen, Lab Acumedic, Heywood, UK)
ETryptic Soy Agar (TSB) ( Sigma-Aldrich, Darmstadt, Germany)
Fig. 1.
Study design and methods flow chart
Preparation of the irrigants
Active chlorine was determined, if applicable, spectrophotometrically (Spectroquant®, chlorine test, 1.00599.0001, Merck, Darmstadt, Germany) at 557 nm. The utilised standard curve gave a molar absorptivity, ε: value at 23,000 (mol/L)-1*cm-1, further used to calculate the total of free and combined chlorine (only active chlorine) in agents using the Beer-Lambert law. The chloramine-based products hold an excess of free chlorine ≈ 80 mmol/L after subtracting the stoichiometric component A (140 ± 7 mmol/L) and component B (53 ± 1 mmol/L amino acids) respectively before mixing. Irrigants containing active chlorine were adjusted with water to the same concentration (70 mmol/L of free or combined chlorine, representing 0.5% w/v of the active substance in DAK, PER and CAR); detailed information is presented in Table 1. Sodium hypochlorite, chlorhexidine and hydrogen peroxide were handled according to EU legalisation from a safety and biocompatibility perspective (the MDR directive in ISO 10993). Furthermore, preparation and handling followed the laboratory’s local restrictions, the material safety data sheet (MSDS) and instructions for use (IFU) when using commercial products.
Preparation of micro-organisms
The bacterial strains obtained from ATCC (LGC standards, SE) were kept in −80°C at the Department of Cariology, University of Gothenburg, Sweden, before use. Isolated colonies from overnight growth on agar were transferred to phosphate buffer and washed twice. The optical density of each suspension was as assessed at 500 nm and adjusted to 0.5. These standardized suspensions were used for subsequent experiments. Viable bacterial counts (CFU; colony forming units) were obtained after 10-fold dilutions were plated on to respective agar and incubated for 2 days at 37°C under anaerobic conditions. Detailed information about bacterial strains is presented in Table 2.
Agar disc diffusion method
Agar plates were inoculated with the test specimen by swabbing the surface with 3–4 mL of the bacterial suspension. The excess suspension was removed with sterile cotton and plates were dried at 37°C for 30 min to ensure the agar surface was dry. Filter paper discs (Ø, 6 mm) were impregnated with 10 μL of irrigants (70 mmol/L), placed on the agar surface and incubated at 37°C for 24 h in anaerobic conditions (85% N2, 10% CO2, 5% H2). The size of the diameters of the inhibition zones was measured after incubation; all the series were performed in triplicate.
Broth dilution method
Single volumes (2.5, 5.0, 7.5, 10.0, 20.0, 50.0 and 100.0 μL) of the commercial agents (70 mmol/L) were added to test tubes containing 1 mL of bacterial suspension using a Hamilton syringe (0-50 μL). A droplet of the agent was placed on the neck of the tube until all seven volumes had been added. At an exact time, all the tubes were vortexed for 5 s. After five and 10 min of reaction, bacteria were sampled (25 μL in duplicates) and inoculated on blood agar plates. The plates were incubated anaerobically at 37°C for one to three days. The results were confirmed under the microscope and registered as (-) 100% lethality, total inhibition and (+) where one or more colonies were detected. The reported values represented the minimum volume required to obtain the complete lethality of bacterial cells (see Table 3).
Table 3.
MBC values for each agent on each bacterial strain
| 2.3 Agar disc diffusion (inhibition zone, MV ± SD, mm) | 2.4 Broth dilution (μL of agent, 70 mmol/L, that eradicated bacteria after 5/10 min) | 2.5 Broth microdilution on agar plates (MBC, mmol/L) | 2.6 Efficacy of active chlorine ** | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CAR | PER | NOG | OCL | AAP | DAK | H2O2 | CHX | CAR | PER | DAK | CHX | H2O2 | CAR | PER | DAK | CHX | H2O2 | CAR 5 min |
CAR 10 min |
PER 5 min |
PER 10min |
|
| Lactobacillus paracasei CCUG 32212 | 7.0 ± 0.7 | 6.7 ± 0.2 | 6.5 ± 0.0 | 9.3 ± 0.9 | 6.0 ± 0.0 | 10.3 ± 0.3 | 6.0 ± 0.0 | 14.0 ± 1.0 | 100/50 | 50/50 | 2.5/2.5 | 20/20 | >100/>100 | 8.8 | 2.2 | 2.2 | 0.14 | 35 | 12.49 | 12.19 | 12.19 | 12.19 |
| Streptococcus mutans IB | 9.8 ± 0.3 | 7.4 ± 0.8 | 7.0 ± 0.0 | 8.5 ± 0.4 | 6.0 ± 0.0 | 9.3 ± 0.8 | 6.0 ± 0.0 | 15.5 ± 0.4 | 50/20 | 50/20 | 2.5/2.5 | 50/50 | >100/>100 | > 70 | 17.5 | 4.4 | 0.14 | 70 | 11.96 | 11.56 | 11.96 | 11.56 |
| Streptococcus mutans OMZ65 | 7.7± 0.8 | 7.0 ± 0.7 | 6.5 ± 0.0 | 9.8 ± 1.3 | 6.0 ± 0.0 | 11.0 ± 0.0 | 6.0 ± 0.0 | 15.8 ± 0.3 | 100/50 | 20/7.5 | 2.5/2.5 | 50/20 | >100/>100 | > 70 | 17.5 | 4.4 | 0.07 | > 70 | 12.49 | 12.19 | 11.79 | 11.36 |
| Streptococcus sobrinus B13 | 6.7 ± 0.3 | 6.7 ± 0.2 | 6.5 ± 0.0 | 9.0 ± 0.5 | 6.0 ± 0.0 | 9.5 ± 0.0 | 6.0 ± 0.0 | 16.3 ± 0.3 | 100/100 | 10/10 | 2.5/2.5 | 50/50 | >100/>100 | > 70 | n/a | 4.4 | 0.14 | 70 | 12.49 | 12.49 | 11.49 | 11.49 |
| Streptococcus salivarius ATCC8618 | 6.8 ± 0.3 | 6.8 ± 0.2 | 6.5 ± 0.0 | 8.8 ± 0.6 | 6.0 ± 0.0 | 9.3 ± 0.2 | 6.0 ± 0.0 | 12.8 ± 0.6 | 50/20 | 20/20 | 2.5/2.5 | 50/50 | >100/>100 | > 70 | n/a | 4.4 | 0.03 | 17.5 | 13.26 | 12.86 | 12.86 | 12.86 |
| Caries group sum of means* | 38.0d | 34.6e | 33.0f | 45.4c | 30.0g | 49.4b | 30.0g | 74.4a | 400/240 | 150/107.5 | 12.5/12.5 | 220/190 | >500 | |||||||||
| Porphyromonas gingivalis OMGS1740 | 10.5 ± 1.5 | 7.6 ± 1.3 | 6.5 ± 0.0 | 9.3 ± 0.9 | 6.0 ± 0.0 | 9.2 ± 0.6 | 6.0 ± 0.0 | 18.8 ± 0.8 | 10/7.5 | 20/7.5 | 2.5/7.5 | 50/50 | >100/>100 | n/a | n/a | n/a | n/a | n/a | 11.88 | 11.75 | 11.88 | 11.76 |
| Prevotella nigrescens ATCC33563 | 7.5 ± 1.5 | 7.5 ± 1.5 | 9.0 ± 0.0 | 13.5 ± 0.5 | 6.0 ± 0.0 | 9.5 ± 0.0 | 6.0 ± 0.0 | 20.7 ± 0.5 | 20/20 | 100/20 | 5/5 | 50/20 | >100/>100 | n/a | n/a | n/a | n/a | n/a | 11.95 | 11.95 | 12.65 | 11.95 |
| Prevotella intermedia ATCC25611 | 9.3 ± 0.3 | 7.5 ± 1.0 | 9.0 ± 2.5 | 10.3 ± 0.8 | 6.0 ± 0.0 | 9.8 ± 0.3 | 6.0 ± 0.0 | 19.7 ± 0.5 | 20/20 | 20/20 | 5/2.5 | 50/50 | >100/>100 | n/a | n/a | n/a | n/a | n/a | 12.20 | 12.20 | 12.20 | 12.20 |
| Agregatibacter actinomycetemcomitans ATCC29522 | 6.8± 0.8 | 7.1 ± 1.4 | 6.5 ± 0.0 | 7.5 ± 0.0 | 6.0 ± 0.0 | 7.8 ± 0.6 | 6.0 ± 0.0 | 16.4 ± 0.4 | 5/5 | 10/2.5 | 2.5/2.5 | 20/20 | >100/>100 | 70 | > 70 | 8.8 | 0.07 | > 70 | 11.45 | 11.45 | 12.06 | 12.06 |
| Fusobacterium nucleatum ATCC10953 | 6.5± 0.0 | 7.2 ± 0.8 | 6.5 ± 0.0 | 13.5 ± 0.5 | 6.0 ± 0.0 | 9.0 ± 0.5 | 6.0 ± 0.0 | 18.3 ± 1.3 | 20/50 | 5/5 | 2.5/2.5 | 50/20 | >100/>100 | 4.4 | 70 | 4.4 | 0.03 | 70 | 12.46 | 12.86 | 11.86 | 11.86 |
| Periodontal group sum of means * | 30.1e | 36.9d | 37.5d | 54.1b | 30.0e | 45.3c | 30.0e | 94.0a | 75/102.5 | 155/55 | 17.5/20 | 220/160 | >500 | |||||||||
| RANKING based on sum of means | 4 | 5 | 6 | 2 | 7 | 3 | 7 | 1 | 4 | 2 | 1 | 3 | 5 | |||||||||
*Denote letters, in agar disc diffusion test, indicate significant difference (one-way ANOVA with Tukey-Kramer post hoc test; p<0.05) amongst agents for sum of means for caries and periodontal group, same letter indicates no difference
**Active Cl+: bacterial cell (log10 mol/CFU)
n/a, results unavailable due to technical difficulties
Broth microdilution on agar plates
The ten tested micro-organism cultures, suspended in Mueller Hinton Broth, supplemented with 20.25 mg Ca2+ and 11.5 mg Mg2+ per litre, adjusted to 0.5 at OD550, were distributed (100 μL) into 96-well microtiter plates (ThermoFisher Scientific, UK). The 2-fold dilutions (from 70 to 0.03 mmol/L) of the commercial agents (CAR, PER, DAK, CHX, H2O2) were prepared and then added to the 96-well microtiter plate in aliquots of 100 μL. After mixing with bacterial suspension, the final concentration ranged from 0.02 to 35 mmol/L. Positive (100 μL Triton, X-100, Sigma-Aldrich) and negative controls (no agent) were included. The plates were then sealed with an adhesive plastic film and incubated for 2 h at 36 ± 1°C. After incubation, 10 μL of each sample was plated on corresponding agar plates (Table 2). The plates were incubated anaerobically for 24 h at 37°C and the results were evaluated. The tests were run in duplicate.
Calculation of the efficacy of the active chlorine on different bacterial species
For CAR and PER, the reactivity of active chlorine in relation to the number of bacterial cells was calculated. The active chlorine (Cl+) was calculated from the molecular concentration (mol/L) in set volumes (L) using Avogadro’s constant, numbers of particles in reciprocal mole (NA=6.022×1023/mol). These numbers were compared with the total number of bacterial cells from the established (CFU) resulting in the ratio (Cl+/bacterial cell), see Table 3.
Time-kill kinetics method using live/dead staining
Live/dead staining was used to detect the antimicrobial efficacy of the commercial agents in damaging or killing the bacterial cells in a concentration- and time-dependent manner, a method known as time-kill kinetics. Standardized bacterial suspensions were prepared in the manner mentioned above. The live/dead tracer, Syto 9 and propidium iodide were prepared following the protocol for Invitrogen (Filmtracer live/dead biofilm viability kit L 10316, Invitrogen) and 160 μL of the film tracer mixture was added to 16 mL of each bacterial suspension. Mixed bacterial suspensions were next added to the 96-well microtiter plate in aliquots of 100 μL. The antimicrobial agents were also prepared in the same manner as 2-fold dilutions (70 mmol/L), with the final concentration range from 0.02 to 35 mmol/L in aliquots of 100 μL. Before the test, standard curves for each tested specimen stained with Syto 9 were created. Positive (100 μL Triton, X-100, Sigma-Aldrich) and negative controls (no agent) were included. Kinetics were measured in a microplate reader (CLARIOstar, BMG Labtech, GmbH, Germany, equipped with the CLARIOstar software, 2013) using the Syto 9 dye with an excitation/emission maximum at 480/500 nm for intact cells (green) and 490/635 nm for lysed cells (red) respectively. Readings started directly after adding agents and data were collected every 10 min up to 1 h, at 37°C with rate 2 shaking in between measurements. Tests were performed in triplicate.
Statistical analyses
The mean values ± SD of each test replicate were calculated. A two-factor ANOVA Tukey’s multiple comparison test was used to compare the difference between the MIC values for the agents for different micro-organisms. p < 0.05 was considered statistically significant. Secondly, a two-way ANOVA, Sidak’s multiple comparison test, was used to compare caries and periodontal bacteria when treated with PER and CHX.
Results
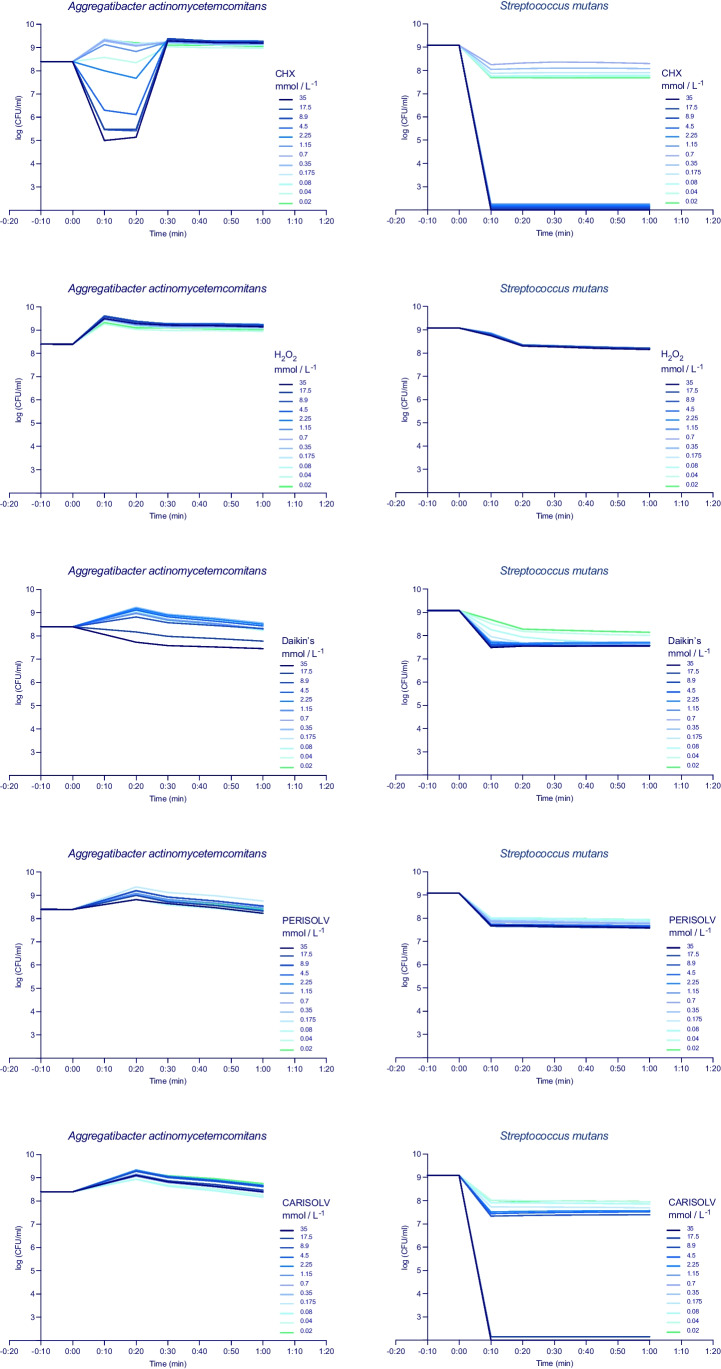
The summarised results are presented in Table 3. CHX was the most efficient antibacterial agent in the disc diffusion test, the microdilution on agar plates and the time-to-kill analysis. In contrast, sodium hypochlorite was more potent in the direct broth dilution method. Chloramines (PER) and (CAR) showed great efficacy in the time-to-kill analysis for S. mutans (Fig. 5).
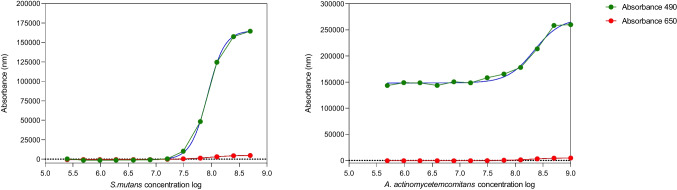
Fig. 5.
Time-kill curves for all the tested irrigants and one bacterium from each group; AA (periodontal) SM-IB (cariogenic). Twelve 2-fold dilutions are plotted, and the antimicrobial was added at start timepoint and monitored up to 1 h
Agar disc diffusion method
The irrigants displayed distinct antimicrobial characteristics, apart from H2O2 and AAP (both ranking 7), where no growth inhibition was observed (Table 3). The results were analysed for differences between the agents and between the two groups of bacteria: cariogenic and periodontal. The strongest, statistically significant effect on all bacteria was observed for CHX (ranking 1), followed by OCl and Dakin’s solution. The weakest inhibitory effect was observed for NOG (ranking 6). Overall, CAR exhibited a more substantial inhibitory effect than PER. Moreover, OCL (ranking 2) and PER (ranking 5) were more effective against periodontal, gram-negative bacteria, whilst DAK (ranking 3) and CAR (ranking 4) inhibited cariogenic, gram-positive bacteria more efficiently. In all, CHX was the preferred antimicrobial agent to use between both groups of bacteria, with a significant difference in comparison to all the other agents, p < 0.05.
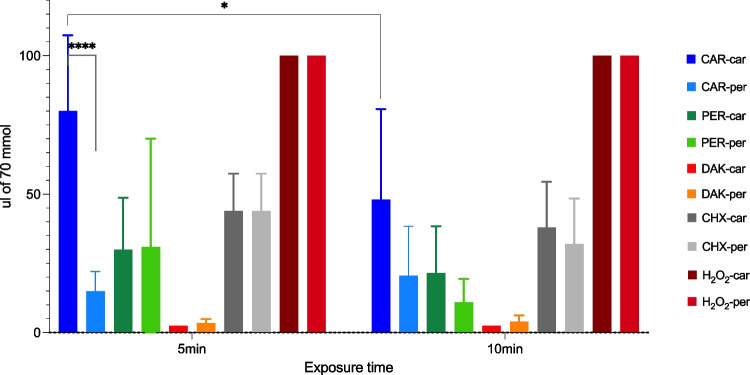
Broth dilution method
The broth dilution method revealed that the lowest instant killing volume, after 5-min exposure, for DAK was 2.5 μL (all bacterial strains except PN and PG), followed by PER (for FN) and CAR (for AA) 5 μL and for CHX (for LBC and AA) 20 μL (Table 3). Hydrogen peroxide did not inhibit the growth of any tested bacteria. The lowest instant killing effect was more pronounced after 10 min; however, the lethality pattern was similar, regardless of the exposure time. Bacterial groups, caries and periodontal, only differed significantly in response to CAR treatment (two-way ANOVA with Sidak’s multiple comparisons test, p<0.0001). Additionally, a significant difference in CAR treatment was observed in cariogenic bacteria between five and 10 min (p<0.05), Fig. 2. Significant differences between agents were observed; Table 4 presents details in supplementary material.
Fig. 2.
Volume (μL, MV, SD) of 70 mmol agents needed to eradicate five bacterial strains in each group of bacteria (caries and periodontal)
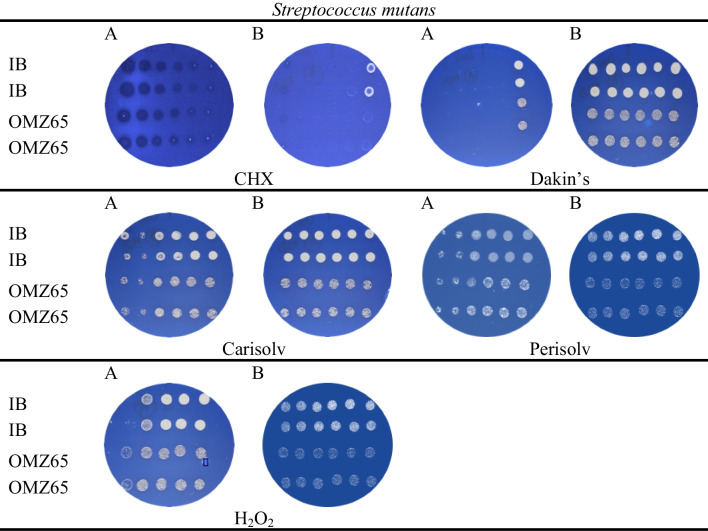
Broth microdilution on agar plates
All the agents inoculated in microbial suspensions showed an antimicrobial effect observed on agar plates. Figure 3 presents the representative results obtained for two strains of Streptococcus mutans. The MBC values for each agent on each bacterial strain are shown in Table 3. Generally, the lowest MBC value was recorded for CHX (0.03 mmol/L), followed by Dakin’s (2.2 mmol/L) and chloramines (PER, CAR) (2.2–8.8 mmol/L), with H2O2 being least effective. As expected, due to bacterial structure, the gram-negative bacteria within the periodontal group were more susceptible than the gram-positive, cariogenic bacteria.
Fig. 3.
Broth microdilution on agar plates in duplicate. Growth inhibition of Streptococcus mutans IB (top two rows) and Streptococcus mutans OMZ65 (bottom two rows) on Mitis Salivarius Bacitracin agar by test agents at different concentrations from the left: Plate A: 70, 35, 17.5, 8.8, 4.4, 2.2 mmol L-1; Plate B: 1.1, 0.5, 0.3, 0.14, 0.07, 0.03 mmol L-1. Drops without colonies (or empty agar surface) equal the MBC value, indicating that the test solution has reduced ≥ 99% of the bacteria. Positive and negative controls worked as expected, not shown
Calculation of the efficacy of the active chlorine on different bacterial species
To calculate the number of single chlorine molecules contributing to the MBC effect of an agent, the stoichiometric ratio of chlorine vs the bacterial cells (1:1) per specimen was calculated. The impact of chloramines (CAR and PER) was similar on SM-IB (11.96), PI (12.20) and PN (11.95), whilst a variation was observed for the remaining bacterial specimens (Table 3). PER emerged as more efficacious, with a lower chlorine/bacteria ratio (≤ 12) than CAR for most tested bacterial species.
Time-kill kinetics method using live/dead staining
A standard curve of bacterial growth was produced for each tested bacterial species for the live/dead analysis with Syto 9 (490:650 nm), with the absorbance of the living cells at 490 nm that increased over time and the absorbance at 650 nm for lysed cells (Fig. 4).
Fig. 4.
Standard curve of S. mutans and A. actinomycetemcomitans by Syto 9, live/dead (green 490; red 650nm; blue nonlinear fit curve)
The time-kill curves for five agents (CHX, H2O2, DAK, PER, CAR) using A. actinomycetemcomitans and S. mutans IB are shown in Fig. 5. CHX induced a bacteriostatic effect in all analysed bacteria; the activity depended on the concentration of the agent and differed between bacterial strains. Bactericidal activity, greater than a three log10-fold decrease, was obtained with 8.9 mmol/L for AA and 1.15 mmol/L for SM-IB as early as the tenth minute of the test. A similar kinetic pattern was obtained for DAK and PER, with the inhibition of bacterial growth up to 1.5 log10. CAR inhibited the growth of Streptococcus mutans after 10 min in 17.5 mmol/L. H2O2 induced minimal growth inhibition in SM-IB and did not affect the growth of AA.
Discussion
Different antimicrobial agents are regularly applied for dental clinical use, where a reduction in the microbiota leads to a positive outcome in caries and periodontitis treatment. This study compared different commercial chlorine agents with chlorhexidine and hydrogen peroxide using four different MIC methods. The net MIC result favoured chlorhexidine and Dakin’s solution. Furthermore, chloramines were found to have an antimicrobial effect; as a result, the null hypothesis is rejected.
Agar disc diffusion method
The disc diffusion test established that CHX was the most effective agent, with the diameter of inhibition zones significantly larger than that of other tested agents. These results also agree with other studies showing the more significant impact of CHX on inhibition zones in lower concentrations than NaOCl [42]. On the other hand, CHX and hypochlorite irrigants are reported to produce a similar reduction in bacterial levels during root canal therapy [30], but in vitro testing is highly dependent on its concentration [43, 44]. However, the reaction with CHX is much slower than with the oxidative sodium hypochlorite, which reacts readily in forming short-lived intermediaries [17, 40]. This means that sodium hypochlorite compound is consumed at a higher rate and may explain the better result obtained by CHX in the disc diffusion method that does not deteriorate at the same rate and would therefore be more beneficial under long-term exposure. Moreover, it is vital to consider the molecular weight of an active substance when validating its antibacterial activity. This was found by Müller et al. in 2008 comparing the cytotoxicity and antibacterial activity of commercial agents, where the ranking order was considerably different based on molar concentration (mol/L), apart from mass concentration (w/v) [43]. This was especially evident for reagents with a relatively high molecular weight, such as PHMB and CHX. This was also the basis of this study and the reason why all the concentrations were equaled. Furthermore, CHX was slightly more efficacious on periodontitis bacteria than caries bacteria, which is consistent with the agent being used more frequently in the periodontitis context [24]. However, apart from discolouration and taste disturbances, there are a few cases reporting adverse side effects from CHX. It should be noted that CHX is considered a hidden allergen and might be involved in more cases than recognised [45].
The efficacy of component A in PER, OCL and DAK surpass CHX. These oxidative forms of chlorine act as oxidative agents and gain electrons in the reaction with bacterial proteins, carbohydrates and lipids, thereby disturbing the bacterial cell membrane, most often into lysis [17, 46]. This is a process that resembles the MPO (myeloperoxidase) reaction from the radical oxygen system (ROS) of the immune system, turning HOCl into potent chloramines for the killing of bacterial pathogens in an alkaline milieu [40, 47]. These reactions are considered rapid or short lived [46], as they involve both redox and radical systems [17, 46]. However, rapid agent decomposition may facilitate cell survival during analysis in an agar disc diffusion test, making it less suitable. On the other hand, according to the collision theory in thermodynamics and as stated in the Arrhenius Equation, the rate of a chemical reaction is proportional to the number of collisions between reactant molecules [48]. Moreover, it will increase in a volume (increased surface size) compared with a solid state (disc), as both molecular movement and contact are increased in a solution [48], which is why rapid reaction mechanisms might be more favoured in methods that involve solvents or suspensions.
Regarding the bacterial groups, DAK was more effective in the caries group, whilst OCL (comp A) was more effective in the periodontal group, where there is no marked difference other than the pH value. Comparable results for chloramines, PER and CAR, were observed, with CAR being more effective, especially on caries bacteria, and thus in line with the intent of use. Chloramines have slightly lower oxidative power (oxidation state +½ of chlorine) than both OCL (component A of Perisolv) (+I, Cl+) and Dakin’s solution (+I, Cl+) and this could explain the lowered inhibitory effect of CAR and PER in comparison with the other aforementioned irrigants. In addition, chloramines are reported to be very unstable and are turned into radicals from the homolysis of N-Cl, thus being consumed rapidly and not effective for a long exposure time [40, 46].
Hydrogen peroxide and AAP (component B of Perisolv) were not effective. AAP (amino acids, pH 10.5) is not a potent antimicrobial agent and, as a result, no growth inhibition was observed. Hydrogen peroxide (oxidation state -I of oxygen, pH 4) is readily decomposed into water if not handled properly and, if so, when it has perhaps evaporated [49], it will have little inhibitory effect. Furthermore, lower concentrations of H2O2, through bacterial enzymes such as peroxidases, may induce tolerance to lower concentrations of H2O2 [17]. Even though the concentrations were equalled, the pH of the irrigants was different; OCL (pH 11) and DAK (pH 9), which may influence the results.
It is worth noting that commercially available dental solutions containing CHX and H2O2 exhibit significantly lower and higher concentrations, respectively, when compared to 70 mmol/L concentrations used in this study. Specifically, CHX solution typically range from 1 to 2 mmol/L (1–2 mg/ml), whilst H2O2 have concentrations as high as 800 mmol/L (3%). These findings suggest that CHX demonstrates a strong antibacterial efficacy, even at very low concentrations with regard to the commercially available products. On the other hand, and in line with the commercial concentrations, H2O2 requires relatively high concentrations to achieve a similar effect. This indicates the importance of understanding the mechanism behind the active ingredients, when evaluating the efficacy of dental products which can only be compared if concentrations are equaled.
Broth dilution
DAK, with its significantly smallest bactericidal volume at both 5 and 10 min of treatment, was followed by PER, CHX and CAR, with H2O2 the least effective (p<0.001). The low reactivity of H2O2 could be attributed to its decomposition into water [49]. The molecular size and redox reactions of the microbicidal agents may play a role in their effectiveness. Smaller molecules like DAK and PER, which are less sterically hindered than CHX, may disperse more easily in a closed container, leading to a more potent antimicrobial effect. The capacity of chlorine atoms to ‘jump’ between reactants before reaching equilibrium [40] in a hypochlorite solution may also contribute to the longer antimicrobial effect. Taken as a whole, this will favour the oxidative power of hypochlorite solution, for example, compared with CHX. On the other hand, CHX overcame the efficacy of the oxidative H2O2, which was suspected of being a potent antimicrobial agent after reaction with amines and sulphur components from bacterial cells [17, 47, 50], but this was not observed. Again, the unwanted decomposition of H2O2 or an effect of the slightly acidic pH of the H2O2 solution could have hindered these outcomes. Chlorine is perhaps a more potent oxidising agent in bacterial suspensions [51]. Even though CAR was the only agent showing a significant difference in sensitivity between caries and periodontal bacteria and time, significantly smaller volumes of DAK, PER and CHX are needed to obtain lethality.
Broth microdilution on agar plates
Like previous methods, CHX emerged as most effective, with MBC values below 0.15 mmol/L, followed by Dakin’s solution (2–4 mmol/L) and chloramines (8–17 mmol/L). Hydrogen peroxide was again ineffective. Perisolv had a slightly stronger bactericidal effect than Carisolv, possibly due to added titanium dioxide [51]. Dakin’s solution, which is a buffered solution (NaHCO3, pH 9) without amine functions, has a higher oxidative number of the chlorine than the chloramines and this perhaps contributes to the improved effect. In another study, sodium hypochlorite was tested with well-known antibiotics with both a lower antimicrobial effect (MBC; 20mmol/L) and less effect on gram-negative bacteria [52]. In addition, Carisolv and Perisolv are formulated in cellulose gels, which might also be seen as a physical diffusion barrier. Due to their inability to maintain stable anaerobic conditions during preparation and treatment, we did not obtain results for three periodontal bacteria: PG, PI and PN. The remaining AA and FN followed earlier trends of treatment, with CHX and DAK being the most effective.
Time-kill kinetics method using live/dead staining
Previous studies have investigated the kinetics of CHX on skin infection bacteria using live/dead staining. The results demonstrated that CHX inhibited bacterial count by two logarithmic units at low concentrations (0.125 mmol/L) over the course of several days [53].
As a result, our study monitored bacterial growth exposed to agents over time using Syto 9 dye. We found that the bacteriostatic effect or inhibition using a similar technique with the Syto 9 dye was dependent on their concentration and varied between the tested bacteria. A three-log inhibition change in AA growth was observed during CHX treatment (35-8.9 mmol/L) after 10 min; however, after 30 min, a total recovery was observed. The bactericidal effect of CHX on SM was obtained after 10 min with concentrations of ≥1.15 mmol, whilst lower concentrations resulted in a 1.5-log inhibition change. The periodontal group of bacteria was less sensitive than the caries group and in line with our calculation of single chlorine atoms needed to kill a single bacterial cell at a ratio of 1:1.
Exposure to DAK and PER resulted in a maximum 1.5-log inhibition of S. mutans, with no recovery phase. A. actinomycetemcomitans responded with a one-log inhibition to the highest DAK concentration and was not affected by PER treatment. Once again, the periodontal group was more resistant to treatments than the caries group. Thus, one conclusion is that chlorine and not chloramines have the same effect on bacteria. A bactericidal effect was observed using Carisolv (chloramine without titanium, ≥17.5 mmol/L) in S. mutans after just 10 min. Carisolv appeared to affect the caries bacteria in the same way as CHX. A. actinomycetemcomitans growth was not influenced by any CAR concentration.
Hydrogen peroxide treatment resulted in less than a one-log inhibition of S. mutans and no inhibitory changes in AA growth pattern. These results may again depend on the decomposition of the molecule into H2O [17, 49]. The reactivity of hydrogen peroxide is highly restricted by pH, where alkalinity increases its oxidative effect [46]. In this study, the hydrogen peroxide had an acidic pH.
The initial aim of this study was to evaluate the efficacy of different agents and their performance by diverse antimicrobial methodologies. For this purpose, individual bacterial strains were used. These may not reflect the true situation of a complex oral biofilm as a dysbiotic biofilm would involve many more parameters. It is in future projects a plan to analyse the response of dysbiotic biofilms to examined irrigants using most suitable method.
Conclusions
Chloramines demonstrated antimicrobial effect in all methods, with convincing results in the kinetic study (CAR) and broth dilution (PER); the null hypothesis is therefore rejected. CHX, on the other hand, is a resilient compound that resists long exposure time, no matter which methodology is used. From the broth dilution methodology in direct contact with a bacterial suspension in the short term, DAK was superior. For this reason, the chosen method must take the mechanism of the substance into account when determining the MIC values for different antimicrobial agents and gram-positive and gram-negative bacteria differed widely depending on both the method and the agent used.
Supplementary information
(DOCX 18 kb)
Author contributions
All the authors whose names appear on the submission are responsible for the content presented in this paper and every author was involved in at least one of the following, conception, design, acquisition and interpretation of the data, as well as drafting, revising and reviewing the manuscript. The authors alone are responsible for the accuracy and integrity of any part of the work. Before submission, all the authors (Dr. Ulrica Scherdin-Almhöjd, MSc. Anna Lerhkinder, Dr. Ann-Marie Roos-Jansåker and Dr. Peter Lingström) approved the final version.
Funding
Open access funding provided by University of Gothenburg. This work has been supported by Stiftelserna Wilhelm and Martina Lundgrens Ref no. (2019-3134).
Data Availability
The data that support the findings of this study are available from the corresponding author in response to a reasonability request.
Declarations
Ethical approval and consent to participate.
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Marsh PD. Microbiology of dental plaque biofilms and their role in oral health and caries. Dent Clin N Am. 2010;54(3):441–454. doi: 10.1016/j.cden.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Diaz PI, Chalmers NI, Rickard AH, Kong C, Milburn CL, Palmer RJ, Jr, et al. Molecular characterization of subject-specific oral microflora during initial colonization of enamel. Appl Environ Microbiol. 2006;72(4):2837–2848. doi: 10.1128/AEM.72.4.2837-2848.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vieira Colombo AP, Magalhães CB, Hartenbach FA, Martins do Souto R, Maciel da Silva-Boghossian C. Periodontal-disease-associated biofilm: a reservoir for pathogens of medical importance. Microb Pathog. 2016;94:27–34. doi: 10.1016/j.micpath.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Valm AM. The structure of dental plaque microbial communities in the transition from health to dental caries and periodontal disease. J Mol Biol. 2019;431(16):2957–2969. doi: 10.1016/j.jmb.2019.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lamont RJ, Koo H, Hajishengallis G. The oral microbiota: dynamic communities and host interactions. Nat Rev Microbiol. 2018;16(12):745–759. doi: 10.1038/s41579-018-0089-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Durand R, Roufegarinejad A, Chandad F, Rompré PH, Voyer R, Michalowicz BS, et al. Dental caries are positively associated with periodontal disease severity. Clin Oral Investig. 2019;23(10):3811–3819. doi: 10.1007/s00784-019-02810-6. [DOI] [PubMed] [Google Scholar]
- 7.Ueno CM, Mullens CL, Luh JH, Wooden WA. Historical review of Dakin’s solution applications. J Plast Reconstr Aesthet Surg. 2018;71(9):e49–e55. doi: 10.1016/j.bjps.2018.05.023. [DOI] [PubMed] [Google Scholar]
- 8.Bowden GH. Does assessment of microbial composition of plaque/saliva allow for diagnosis of disease activity of individuals? Community Dent Oral Epidemiol. 1997;25(1):76–81. doi: 10.1111/j.1600-0528.1997.tb00902.x. [DOI] [PubMed] [Google Scholar]
- 9.Lemos JA, Quivey RG, Koo H, Abranches J. Streptococcus mutans: a new Gram-positive paradigm? Microbiology (Reading) 2013;159(Pt 3):436–445. doi: 10.1099/mic.0.066134-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stokowa-Sołtys K, Wojtkowiak K, Jagiełło K. Fusobacterium nucleatum - friend or foe? J Inorg Biochem. 2021;224:111586. doi: 10.1016/j.jinorgbio.2021.111586. [DOI] [PubMed] [Google Scholar]
- 11.Popova C, Dosseva-Panova V, Panov V. Microbiology of periodontal diseases. A review Biotechnology & Biotechnological Equipment. 2013;27:3754–3759. doi: 10.5504/BBEQ.2013.0027. [DOI] [Google Scholar]
- 12.Besingi RN, Wenderska IB, Senadheera DB, Cvitkovitch DG, Long JR, Wen ZT, et al. Functional amyloids in Streptococcus mutans, their use as targets of biofilm inhibition and initial characterization of SMU_63c. Microbiology (Reading) 2017;163(4):488–501. doi: 10.1099/mic.0.000443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roos-Jansåker AM, Renvert S, Egelberg J. Treatment of peri-implant infections: a literature review. J Clin Periodontol. 2003;30(6):467–485. doi: 10.1034/j.1600-051X.2003.00296.x. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez S, Cohen CL, Galván M, Alonaizan FA, Rich SK, Slots J. Gingival bleeding on probing: relationship to change in periodontal pocket depth and effect of sodium hypochlorite oral rinse. J Periodontal Res. 2015;50(3):397–402. doi: 10.1111/jre.12219. [DOI] [PubMed] [Google Scholar]
- 15.Fischer RG, Lira Junior R, Retamal-Valdes B, Figueiredo LC, Malheiros Z, Stewart B, et al. Periodontal disease and its impact on general health in Latin America. Section V: Treatment of periodontitis. Braz Oral Res. 2020;34(supp1 1):e026. doi: 10.1590/1807-3107bor-2020.vol34.0026. [DOI] [PubMed] [Google Scholar]
- 16.Milgrom P, Horst JA, Ludwig S, Rothen M, Chaffee BW, Lyalina S, et al. Topical silver diamine fluoride for dental caries arrest in preschool children: a randomized controlled trial and microbiological analysis of caries associated microbes and resistance gene expression. J Dent. 2018;68:72–78. doi: 10.1016/j.jdent.2017.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDonnell G, Russell AD. Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev. 1999;12(1):147–179. doi: 10.1128/CMR.12.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McDonnell G. 7.4.2 Oxidizing agents. Antiseptics and disinfectants: activity, action, and resistance. American Society for Microbiology (ASM); 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cosyn J, Sabzevar MM. Subgingival chlorhexidine varnish administration as an adjunct to same-day full-mouth root planing. II Microbiological observations J Periodontol. 2007;78(3):438–445. doi: 10.1902/jop.2007.060222. [DOI] [PubMed] [Google Scholar]
- 20.Varoni E, Tarce M, Lodi G, Carrassi A. Chlorhexidine (CHX) in dentistry: state of the art. Minerva Stomatol. 2012;61(9):399–419. [PubMed] [Google Scholar]
- 21.Autio-Gold J. The role of chlorhexidine in caries prevention. Oper Dent. 2008;33(6):710–716. doi: 10.2341/08-3. [DOI] [PubMed] [Google Scholar]
- 22.Gürgan CA, Zaim E, Bakirsoy I, Soykan E. Short-term side effects of 0.2% alcohol-free chlorhexidine mouthrinse used as an adjunct to non-surgical periodontal treatment: a double-blind clinical study. J Periodontol. 2006;77(3):370–384. doi: 10.1902/jop.2006.050141. [DOI] [PubMed] [Google Scholar]
- 23.Chiewchalermsri C, Sompornrattanaphan M, Wongsa C, Thongngarm T. Chlorhexidine allergy: current challenges and future prospects. J Asthma Allergy. 2020;13:127–133. doi: 10.2147/JAA.S207980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Slots J. Selection of antimicrobial agents in periodontal therapy. J Periodontal Res. 2002;37(5):389–398. doi: 10.1034/j.1600-0765.2002.00004.x. [DOI] [PubMed] [Google Scholar]
- 25.Rosas-Ledesma P, Mariscal A, Carnero M, Muñoz-Bravo C, Gomez-Aracena J, Aguilar L, et al. Antimicrobial efficacy in vivo of a new formulation of 2-butanone peroxide in n-propanol: comparison with commercial products in a cross-over trial. J Hosp Infect. 2009;71(3):223–227. doi: 10.1016/j.jhin.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 26.Teles RP, Teles FR. Antimicrobial agents used in the control of periodontal biofilms: effective adjuncts to mechanical plaque control? Braz Oral Res. 2009;23(Suppl 1):39–48. doi: 10.1590/S1806-83242009000500007. [DOI] [PubMed] [Google Scholar]
- 27.Bürgers R, Witecy C, Hahnel S, Gosau M. The effect of various topical peri-implantitis antiseptics on Staphylococcus epidermidis, Candida albicans, and Streptococcus sanguinis. Arch Oral Biol. 2012;57(7):940–947. doi: 10.1016/j.archoralbio.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 28.Eick S, Radakovic S, Pfister W, Nietzsche S, Sculean A. Efficacy of taurolidine against periodontopathic species--an in vitro study. Clin Oral Investig. 2012;16(3):735–744. doi: 10.1007/s00784-011-0567-2. [DOI] [PubMed] [Google Scholar]
- 29.Tawakoli PN, Ragnarsson KT, Rechenberg DK, Mohn D, Zehnder M. Effect of endodontic irrigants on biofilm matrix polysaccharides. Int Endod J. 2017;50(2):153–160. doi: 10.1111/iej.12604. [DOI] [PubMed] [Google Scholar]
- 30.Gonçalves LS, Rodrigues RC, Andrade Junior CV, Soares RG, Vettore MV. The effect of sodium hypochlorite and chlorhexidine as irrigant solutions for root canal disinfection: a systematic review of clinical trials. J Endod. 2016;42(4):527–532. doi: 10.1016/j.joen.2015.12.021. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez S. Review of the literature on sodium hypochlorite as a treatment modality in periodontal disease. J West Soc Periodontol Periodontal Abstr. 2013;61(1):5–9. [PubMed] [Google Scholar]
- 32.Galván M, Gonzalez S, Cohen CL, Alonaizan FA, Chen CT, Rich SK, et al. Periodontal effects of 0.25% sodium hypochlorite twice-weekly oral rinse. A pilot study. J Periodontal Res. 2014;49(6):696–702. doi: 10.1111/jre.12151. [DOI] [PubMed] [Google Scholar]
- 33.Asal MA, Abdellatif AM, Hammouda HE. Clinical and microbiological assessment of carisolv and polymer bur for selective caries removal in primary molars. Int J Clin Pediatr Dent. 2021;14(3):357–363. doi: 10.5005/jp-journals-10005-1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fure S, Lingström P. Evaluation of different fluoride treatments of initial root carious lesions in vivo. Oral Health Prev Dent. 2009;7(2):147–154. [PubMed] [Google Scholar]
- 35.Kubasiewicz-Ross P, Hadzik J, Gedrange T, Dominiak M, Jurczyszyn K, Pitułaj A, et al. Antimicrobial efficacy of different decontamination methods as tested on dental implants with various types of surfaces. Med Sci Monit. 2020;26:e920513. doi: 10.12659/MSM.920513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lager A, Thornqvist E, Ericson D. Cultivatable bacteria in dentine after caries excavation using rose-bur or carisolv. Caries Res. 2003;37(3):206–211. doi: 10.1159/000070446. [DOI] [PubMed] [Google Scholar]
- 37.Aherne O, Ortiz R, Fazli MM, Davies JR. Effects of stabilized hypochlorous acid on oral biofilm bacteria. BMC Oral Health. 2022;22(1):415. doi: 10.1186/s12903-022-02453-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simchowitz L. Interactions of bromide, iodide, and fluoride with the pathways of chloride transport and diffusion in human neutrophils. J Gen Physiol. 1988;91(6):835–860. doi: 10.1085/jgp.91.6.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Andrés CMC, Pérez de la Lastra JM, Juan CA, Plou FJ, Pérez-Lebeña E. Chemistry of hydrogen peroxide formation and elimination in mammalian cells, and its role in various pathologies. Stresses. 2022;2(3):256–274. doi: 10.3390/stresses2030019. [DOI] [Google Scholar]
- 40.Hawkins CL, Pattison DI, Davies MJ. Hypochlorite-induced oxidation of amino acids, peptides and proteins. Amino Acids. 2003;25(3-4):259–274. doi: 10.1007/s00726-003-0016-x. [DOI] [PubMed] [Google Scholar]
- 41.Abdel-Fattah AKSH. Action of sodium hypochlorite on a-amino acids. Chem Zvesti. 1971;25:222–230. [Google Scholar]
- 42.Luddin N, Ahmed HM. The antibacterial activity of sodium hypochlorite and chlorhexidine against Enterococcus faecalis: a review on agar diffusion and direct contact methods. J Conserv Dent. 2013;16(1):9–16. doi: 10.4103/0972-0707.105291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Müller G, Kramer A. Biocompatibility index of antiseptic agents by parallel assessment of antimicrobial activity and cellular cytotoxicity. J Antimicrob Chemother. 2008;61(6):1281–1287. doi: 10.1093/jac/dkn125. [DOI] [PubMed] [Google Scholar]
- 44.Ferraz CC, Gomes BP, Zaia AA, Teixeira FB, Souza-Filho FJ. Comparative study of the antimicrobial efficacy of chlorhexidine gel, chlorhexidine solution and sodium hypochlorite as endodontic irrigants. Braz Dent J. 2007;18(4):294–298. doi: 10.1590/S0103-64402007000400004. [DOI] [PubMed] [Google Scholar]
- 45.Doolan BT, Crilly HM. Chlorhexidine wipes: time to stop and think about allergy. Anaesth Intensive Care. 2019;47(1):90–95. doi: 10.1177/0310057X18811974. [DOI] [PubMed] [Google Scholar]
- 46.Fukuzaki S. Mechanisms of actions of sodium hypochlorite in cleaning and disinfection processes. Biocontrol Sci. 2006;11(4):147–157. doi: 10.4265/bio.11.147. [DOI] [PubMed] [Google Scholar]
- 47.Akong-Moore K, Chow OA, von Köckritz-Blickwede M, Nizet V. Influences of chloride and hypochlorite on neutrophil extracellular trap formation. PLoS One. 2012;7(8):e42984. doi: 10.1371/journal.pone.0042984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zumdahl SS. Chemistry. 8. Houghton Mifflin Harcourt; 2010. [Google Scholar]
- 49.Williams M. The Merck Index: An Encyclopedia of Chemicals, Drugs, and Biologicals, 15th M.J. O'Neil , Royal Society of Chemistry, Cambridge,UK ISBN 9781849736701; 2708 pages. April 2013, $150 with 1-year free access to The Merck Index Online. Drug Development Research. 2013;74(5):339-.
- 50.Marcinkiewicz J, Kontny E. Taurine and inflammatory diseases. Amino Acids. 2014;46(1):7–20. doi: 10.1007/s00726-012-1361-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clapp PA, Davies MJ, French MS, Gilbert BC. The bactericidal action of peroxides; an E.P.R. spin-trapping study. Free Radic Res. 1994;21(3):147–167. doi: 10.3109/10715769409056566. [DOI] [PubMed] [Google Scholar]
- 52.Rodríguez-Melcón C, Alonso-Calleja C, García-Fernández C, Carballo J, Capita R (2021) Minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) for twelve antimicrobials (biocides and antibiotics) in eight strains of Listeria monocytogenes. Biology (Basel) 11(1) [DOI] [PMC free article] [PubMed]
- 53.Brun P, Bernabè G, Marchiori C, Scarpa M, Zuin M, Cavazzana R, et al. Antibacterial efficacy and mechanisms of action of low power atmospheric pressure cold plasma: membrane permeability, biofilm penetration and antimicrobial sensitization. J Appl Microbiol. 2018;125(2):398–408. doi: 10.1111/jam.13780. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 18 kb)
Data Availability Statement
The data that support the findings of this study are available from the corresponding author in response to a reasonability request.