Abstract
Background
Various rehabilitation treatments may be offered following carpal tunnel syndrome (CTS) surgery. The effectiveness of these interventions remains unclear. This is the first update of a review first published in 2013.
Objectives
To review the effectiveness and safety of rehabilitation interventions following CTS surgery compared with no treatment, placebo, or another intervention.
Search methods
On 29 September 2015, we searched the Cochrane Neuromuscular Specialised Register, the Cochrane Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, CINAHL Plus, AMED, LILACS, and PsycINFO. We also searched PEDro (3 December 2015) and clinical trials registers (3 December 2015).
Selection criteria
Randomised or quasi‐randomised clinical trials that compared any postoperative rehabilitation intervention with either no intervention, placebo, or another postoperative rehabilitation intervention in individuals who had undergone CTS surgery.
Data collection and analysis
Two review authors independently selected trials for inclusion, extracted data, assessed risk of bias, and assessed the quality of the body of evidence for primary outcomes using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach according to standard Cochrane methodology.
Main results
In this review we included 22 trials with a total of 1521 participants. Two of the trials were newly identified at this update. We studied different rehabilitation treatments including immobilisation using a wrist orthosis, dressings, exercise, controlled cold therapy, ice therapy, multi‐modal hand rehabilitation, laser therapy, electrical modalities, scar desensitisation, and arnica. Three trials compared a rehabilitation treatment to a placebo, four compared rehabilitation to a no treatment control, three compared rehabilitation to standard care, and 15 compared various rehabilitation treatments to one another.
Overall, the included studies were very low in quality. Thirteen trials explicitly reported random sequence generation; of these, five adequately concealed the allocation sequence. Four trials achieved blinding of both participants and outcome assessors. Five were at high risk of bias from incompleteness of outcome data at one or more time intervals, and eight had high risk of selective reporting bias.
These trials were heterogeneous in terms of treatments provided, duration of interventions, the nature and timing of outcomes measured, and setting. Therefore, we were not able to pool results across trials.
Four trials reported our primary outcome, change in self reported functional ability at three months or more. Of these, three trials provided sufficient outcome data for inclusion in this review. One small high‐quality trial studied a desensitisation programme compared with standard treatment and revealed no statistically significant functional benefit based on the Boston Carpal Tunnel Questionnaire (BCTQ) (mean difference (MD) ‐0.03, 95% confidence interval (CI) ‐0.39 to 0.33). One low‐quality trial assessed participants six months post surgery using the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire and found no significant difference between a no formal therapy group and a group given a two‐week course of multi‐modal therapy commenced at five to seven days post surgery (MD 1.00, 95% CI ‐4.44 to 6.44). One very low‐quality quasi‐randomised trial found no statistically significant difference in function on the BCTQ at three months post surgery with early immobilisation (plaster wrist orthosis worn until suture removal) compared with a splint and late mobilisation (MD 0.39, 95% CI ‐0.45 to 1.23).
Differences between treatments for secondary outcome measures (change in self reported functional ability measured at less than three months; change in CTS symptoms; change in CTS‐related impairment measures; presence of iatrogenic symptoms from surgery; return to work or occupation; and change in neurophysiological parameters) were generally small and not statistically significant. Few studies reported adverse events.
Authors' conclusions
There is limited and, in general, low quality evidence for the benefit of the reviewed interventions. People who have undergone CTS surgery should be informed about the limited evidence of effectiveness of postoperative rehabilitation interventions. Until researchers provide results of more high‐quality trials that assess the effectiveness and safety of various rehabilitation treatments, the decision to provide rehabilitation following CTS surgery should be based on the clinician's expertise, the patient's preferences and the context of the rehabilitation environment. It is important for researchers to identify patients who respond to a particular treatment and those who do not, and to undertake high‐quality studies that evaluate the severity of iatrogenic symptoms from surgery, measure function and return‐to‐work rates, and control for confounding variables.
Keywords: Female; Humans; Male; Carpal Tunnel Syndrome; Carpal Tunnel Syndrome/rehabilitation; Carpal Tunnel Syndrome/surgery; Outcome Assessment, Health Care; Postoperative Care; Postoperative Care/methods; Randomized Controlled Trials as Topic; Rehabilitation; Rehabilitation/methods
Plain language summary
Rehabilitation following carpal tunnel release
Review question
Are rehabilitation interventions after surgery for carpal tunnel syndrome effective and safe?
Background
Carpal tunnel syndrome (CTS) is a condition in which a nerve that runs through a bony and fibrous tunnel in the wrist is compressed. This leads to pain, numbness and tingling in the hand, sometimes extending into the forearm. At advanced stages, some people with CTS have weakness and muscle wasting in the hand. CTS is more common in women and individuals with certain risk factors, such as diabetes, obesity, arthritis, older age, working in certain occupations, and previous wrist fracture. Many people undergo surgery to reduce pressure on the nerve, to lessen pain, and improve sensation and hand function. Sometimes individuals receive rehabilitation following CTS surgery. Rehabilitation treatments are believed to speed up recovery and manage pain or symptoms from the surgery itself. This is the first update of a review first published in 2013.
Study characteristics
On 29 September 2015, we searched for all relevant clinical trials in which a rehabilitation treatment was compared with another rehabilitation treatment, no treatment or placebo (sham treatment). We found 22 trials with a total of 1521 participants that assessed the benefits and harms of different rehabilitation treatments following CTS surgery. Two of the trials were newly identified at this update.
Key results and quality of the evidence
Based on these studies, we found limited and low quality evidence for the benefit of the reviewed treatments, including immobilisation with a wrist orthosis (splint), use of dressings post surgery, exercise, cold and ice therapy, different types of hand rehabilitation provided in combination, laser therapy, electrical treatments, scar desensitisation, and arnica. Few studies reported on the safety of these treatments.
More research is needed to investigate the effectiveness and safety of the various types of rehabilitation treatment available for people following CTS surgery.
The evidence is up to date to September 2015.
Summary of findings
Summary of findings for the main comparison. Multi‐modal hand therapy versus normal activities and advice for people who have had carpal tunnel release surgery.
| Multi‐modal hand therapy versus normal activities and advice for people who have had carpal tunnel release surgery | ||||||
|
Patient or population: people who have had carpal tunnel release surgery Intervention: multi‐modal hand therapy Comparison: normal activities and advice | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Normal activities and advice | Multi‐modal hand therapy | |||||
| Long‐term improvement in functional ability (DASH) ‐ DASH at 6 months post surgery | The mean long‐term improvement in functional ability (DASH) ‐ DASH at 6 months post surgery in the control group was 18 | The mean long‐term improvement in functional ability (DASH) ‐ DASH at 6 months post surgery in the intervention group was 1 higher (4.44 lower to 6.44 higher) | ‐ | 150 (1 RCT) | ⊕⊕⊕⊝ Low1,2 | No significant difference |
| Change in impairment measure (grip strength) ‐ 6 months post surgery | The mean change in impairment measure (grip strength) ‐ 6 months post surgery in the control group was 26.6 | The mean change in impairment measure (grip strength) ‐ 6 months post surgery in the intervention group was 0.4 lower (3.59 lower to 2.79 higher) | ‐ | 150 (1 RCT) | ⊕⊕⊕⊝ Low1,2 | No significant difference |
| Change in impairment measure (lateral pinch strength) ‐ 6 months post surgery | The mean change in impairment measure (lateral pinch strength) ‐ 6 months post surgery in the control group was 7.8 | The mean change in impairment measure (lateral pinch strength) ‐ 6 months post surgery in the intervention group was 0.2 lower (0.94 lower to 0.54 higher) | ‐ | 150 (1 RCT) | ⊕⊕⊕⊝ Low1,2 | No significant difference |
| Return to normal occupations ‐ at the end of treatment (2 weeks post surgery) | Study population | RR 0.96 (0.78 to 1.18) | 150 (1 RCT) | ⊕⊕⊕⊝ Low1,2 | ‐ | |
| 727 per 1000 | 698 per 1000 (567 to 858) | |||||
| Return to normal occupations ‐ 4 weeks after completion of treatment (6 weeks post surgery) | Study population | RR 1.02 (0.89 to 1.17) | 150 (1 RCT) | ⊕⊕⊕⊝ Low1,2 | ‐ | |
| 831 per 1000 | 848 per 1000 (740 to 972) | |||||
| Return to normal occupations ‐ 6 weeks after completion of treatment (8 weeks post surgery) | Study population | RR 1.04 (0.97 to 1.12) | 150 (1 RCT) | ⊕⊕⊕⊝ Low1,2 | ‐ | |
| 935 per 1000 | 972 per 1000 (907 to 1000) | |||||
| Adverse effects | Study population | RR 0.53 (0.05 to 5.69) | 150 (1 RCT) | ⊕⊕⊕⊝ Moderate1,2 | ‐ | |
| 26 per 1000 | 14 per 1000 (1 to 148) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Downgraded (‐1) for risk of bias. Participants were not blinded and outcomes reported in the Methods were not reported in the Results.
2Downgraded (‐1) for imprecision. Wide confidence intervals were provided for the reported outcome.
Background
Description of the condition
Carpal tunnel syndrome (CTS) is a neurological condition caused by compression of the median nerve at the wrist due to increased pressure within the carpal tunnel (AAOS 2007; Phalen 1966). Patients with CTS usually present with sensory or motor symptoms, or both, in the hand and wrist. Patients often experience pain, paraesthesia or numbness in the distal distribution of the thumb, index and middle fingers, and in the radial half of the ring finger (Phalen 1966; Rempel 1998). Extramedian spread of sensory and pain symptoms has been reported in 37.5% of patients (Zanette 2010). At advanced stages, wasting of the thenar muscles and hand weakness are observed (Ibrahim 2012).
CTS is one of the most common disorders of the upper extremity (AAOS 2007). The prevalence of CTS in the general population is 3.8% when diagnosed clinically and 2.7% when diagnosed neurophysiologically (Atroshi 1999). CTS is more prevalent among women than among men (Gelfman 2009). Whilst some authors have indicated that occupational risk factors, such as vibration, force and repetition (Barcenilla 2012; Burt 2011; Herbert 2000), and certain occupations contribute to CTS (Armstrong 2008; Kim 2004; Wyatt 2012), controversy continues regarding its work‐relatedness (Stapleton 2006). Other risk factors for CTS, such as obesity, diabetes, previous wrist fracture, and arthritis, have been suggested (Geoghegan 2004; Lam 1998; Palmer 2007; Van Rijn 2009).
CTS can be treated both non‐surgically (conservatively) and surgically. Conservative treatment options are usually offered to individuals who experience mild or intermittent symptoms, are pregnant, or cannot or choose not to have surgery (Page 2012a). Non‐surgical interventions that may be offered include therapeutic ultrasound, splinting, exercise prescription, mobilisation techniques, ergonomic modification, oral medication, corticosteroid injections, vitamins and complementary therapies (Marshall 2007; O'Connor 2012; Page 2012a; Page 2012b; Page 2012c). Few have any proven therapeutic benefit.
CTS surgery ‐ most commonly referred to as carpal tunnel release (CTR) ‐ may be indicated for individuals with persistent symptoms that have not responded to conservative management, those presenting with more severe symptoms (such as frequent numbness or thenar muscle wasting) or those with electrophysiologically severe disease (Scholten 2007; Verdugo 2008). Surgery involves division of the transverse carpal ligament to increase the volume of the carpal tunnel, thereby reducing pressure on the median nerve (Aroori 2008). In the United States of America, approximately 40% of patients with CTS are treated operatively (Wilson 2003), and in the United Kingdom, 31% of persons with CTS undergo surgery (Latinovic 2006). CTR has a reported long‐term success rate of 75% to 90% (Louie 2012).
Two surgical approaches are commonly used to release the transverse carpal ligament: open CTR and endoscopic CTR. In open CTR, the carpal tunnel ligament is divided by a palmar incision. In recent years, minimal‐incision‐open (or mini‐open) techniques have become more common in an attempt to minimise surgical trauma, iatrogenic symptoms from the surgery and recovery time (Bromley 1994). Over time, several variations of these techniques have been developed to reduce postoperative pain, improve function and shorten recovery time. A number of secondary procedures may be performed concurrently. These include techniques such as epineurotomy, internal neurolysis, synovectomy and reconstruction of the transverse carpal ligament (Huisstede 2010). Endoscopic CTR (ECTR) involves division of the transverse carpal ligament whilst leaving overlying structures intact. This is believed to reduce postoperative pain and scarring while hastening early return to function and work (Sanati 2011). Two techniques are commonly used for ECTR: the single‐portal technique (Agee 1992) and the two‐portal technique (Chow 1989).
Complications following CTR may include nerve injury, neuroma formation, palmar arch injury, hematomas, complex regional pain syndrome, tendon adhesions, bowstringing of the flexor tendons, pillar pain, scar pain and other iatrogenic complications resulting from surgery (Braun 2002). Furthermore, symptoms of CTS may recur or persist following surgical release (Gerritsen 2001; Hunter 1991; Idler 1996). Reasons for persistence of symptoms following surgical release include incorrect diagnosis, inadequate decompression of the median nerve, iatrogenic compression or nerve injury, double crush syndrome, and end‐stage disease (Idler 1996; Louie 2012). The prognosis following CTS has been associated with several factors, such as age, psychological factors, workers' compensation, duration of CTS symptoms, presence of thenar atrophy and absence of sensory and motor nerve conduction (Amick 2004; Bland 2001; Cowan 2012; Finestone 1996). The presence of other disorders, such as rheumatoid arthritis and diabetes, may also affect the prognosis (DeStefano 1997).
Description of the intervention
Various rehabilitation treatments may be recommended following CTR. These interventions are believed to expedite recovery by improving mobility, strengthening the hand and promoting earlier return to function and work (Pomerance 2007; Provinciali 2000). Interventions that may be prescribed to manage iatrogenic symptoms of surgery include control of postoperative swelling, scar desensitisation, management of pillar pain and wound healing (Janssen 2009; Powell 2003; Ritting 2012). Therefore, postoperative rehabilitation might include interventions such as advice, exercise prescription, mobilisation techniques, splinting of the wrist with an orthosis, wound and scar management, oedema management, electrotherapy, cryotherapy, desensitisation, ergonomic modification, strengthening and work modification (Groves 1989; Nathan 1993). These interventions may be provided as stand‐alone interventions or as part of a programme of rehabilitation treatments.
How the intervention might work
The goal of postoperative rehabilitation is to speed up and enhance symptom resolution and functional recovery following surgery. Various arguments in support of individual rehabilitative techniques have been reported. For instance, immobilisation of the wrist with an orthosis has been recommended to minimise postoperative pain, wound dehiscence, and nerve entrapment, and to prevent bowstringing of the flexor tendons (Bury 1995; Jessurun 1988). Laser therapy and modalities that use electrical stimulation have been advocated to stimulate wound healing and neuronal regeneration and to control pain postoperatively (Alves 2011; Gordon 2010). Lighter postoperative dressings are advocated to allow easier and earlier mobilisation of the hand and wrist (Ritting 2012). Advocates of early mobilisation following surgery propose that motion of the wrist and digits promotes longitudinal gliding of the median nerve through the surgical bed and prevents adhesion formation between the nerve and the flexor tendons (Nathan 1993; Skirven 1994). Oedema management techniques are used to minimise effects of the inflammatory response on digital range of motion (Hayes 2002). Scar management techniques, such as massage, pressure, and application of silicon‐based products, are advocated to loosen adhesions between skin and underlying tissues, to aid in desensitisation of the incisional scar and to promote scar remodelling (Hayes 2002; Powell 2003). Strengthening exercises and progressive functional activities are incorporated into the rehabilitative programme to maximise occupational performance following surgery (Hayes 2002; Nathan 1993). Some authors advocate the use of comprehensive multi‐component therapy programmes (consisting of various rehabilitation treatments, such as advice, mobilisation and management of iatrogenic symptoms from surgery by physiotherapists or occupational therapists who specialise in hand therapy) to promote early return to function and work (Nathan 1993). Nathan 1993 also found that compliance with hand therapy was the strongest prognostic factor for early return to function and work.
Why it is important to do this review
The evidence base for rehabilitation following CTR has grown. Three reviews have focused on specific treatments following CTR (Huisstede 2010; Isaac 2010; Keilani 2002). Cochrane systematic reviews have explored various non‐surgical interventions (Marshall 2007; O'Connor 2012; Page 2012a; Page 2012b; Page 2012c) and surgical treatment options (Scholten 2007; Vasiliadis 2013; Verdugo 2008) for CTS. However, no Cochrane systematic review has examined rehabilitation treatments following surgical management of CTS. There are many rehabilitation treatments that may be offered to patients who have had CTR. As evidence and guidelines for the use of any of these interventions are limited, a Cochrane systematic review is warranted.
This is the first update of a review first published in 2013.
Objectives
To assess the effectiveness and safety of rehabilitation interventions after CTS surgery compared with no treatment, placebo, or another treatment.
Methods
Criteria for considering studies for this review
Types of studies
All published and unpublished studies using or attempting to use a randomised methodology to compare postoperative rehabilitation treatment with no treatment (or a placebo) or another rehabilitation treatment.
We excluded studies that compared surgery with rehabilitation interventions or any interventions provided before surgery, and interventions that were not considered to be rehabilitation treatment, for example, postoperative analgesia. We imposed no restrictions by year of publication or by language.
Types of participants
All participants with a diagnosis of CTS (as defined by the authors of each study) who underwent CTR, endoscopically or via any open technique.
Types of interventions
All postoperative rehabilitation treatments, including advice, exercise, use of a hand or wrist orthosis, scar management, oedema management, electrotherapy, desensitisation, ergonomic modification, work modification, exercise prescription and return‐to‐work interventions.
We excluded any intervention that occurred before surgery or at the time of surgery, for example, type of anaesthetic or suture type. We also excluded postoperative analgesia.
Types of outcome measures
We modified outcomes from the original protocol for this review (O'Connor 2003). We detailed changes in the section Differences between protocol and review.
Primary outcomes
Long‐term change in self reported functional ability as measured on a continuous scale (e.g. Functional Scale from the Boston Carpal Tunnel Questionnaire (BCTQ); Disabilities of the Arm, Shoulder and Hand questionnaire (DASH)). Long‐term benefit was defined as lasting three months or more.
Secondary outcomes
Short‐term change in self reported functional ability as measured on a continuous scale (e.g. Functional Scale from BCTQ or DASH). Short‐term change was defined as less than three months.
Short‐term (at less than three months) and long‐term (three months or more) change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
Short‐term (at less than three months) and long‐term (three months or more) change in CTS‐related impairment measures (e.g. grip and pinch strength).
Presence of iatrogenic symptoms secondary to CTR (e.g. swelling, scar pain, excessive scarring, and pillar pain) at short‐term (less than three months) and long‐term (three months or more) follow‐up.
Return to work or occupation (measured as 'yes' or 'no') at three months.
Short‐term (less than three months) and long‐term (three months or more) change in neurophysiological parameters (via nerve conduction studies).
Presence of adverse events resulting from rehabilitation at short‐term (less than three months) and long‐term (three months or more) follow‐up.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Neuromuscular Specialised Register (CNMD) (29 September 2015), the Cochrane Central Register of Controlled Trials (CENTRAL) (2015, Issue 8), MEDLINE (January 1966 to September 2015), EMBASE (January 1980 to September 2015), CINAHL Plus (January 1937 to September 2015), AMED (January 1985 to September 2015), LILACS (January 1982 to September 2015), PsycINFO (January 1806 to September 2015), PEDro (January 1999 to December 2015), the World Health Organization (WHO) International Clinicial Trials Registry Platform (ICTRP) (3 December 2015), the UK Clinical Research Network Study Portfolio (3 December 2015) and ClinicalTrials.gov (3 December 2015).
The search strategies are detailed in the following appendices: Cochrane Neuromuscular Specialised Register (Appendix 1), CENTRAL (Appendix 2), MEDLINE (Appendix 3), EMBASE (Appendix 4), CINAHL Plus (Appendix 5), AMED (Appendix 6), LILACS (Appendix 7), PsycINFO (Appendix 8), PEDro (Appendix 9), and clinical trials registers (Appendix 10).
Searching other resources
We searched bibliographies of relevant trials identified by this strategy. When possible, we contacted authors of identified papers to determine whether they knew of other published or unpublished trials.
Data collection and analysis
Review authors followed recommended strategies for data collection and analysis documented in Chapters 7 and 9 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Selection of studies
Two review authors independently selected trials for possible inclusion against a predetermined checklist of inclusion criteria (see Criteria for considering studies for this review). Each review author independently examined the titles and abstracts of trials for possible inclusion identified from the search and categorised studies into the following groups.
Possibly relevant: studies that met the inclusion criteria and studies from which it was not possible to determine whether they met the criteria by review of title or abstract.
Excluded: studies that did not meet the inclusion criteria.
Two review authors then independently reviewed the full text of all studies to determine possible relevance. Each of these review authors compiled a list of trials that met the inclusion criteria. Review authors compared the lists and a third review author resolved any discrepancies that could not be resolved through discussion.
Data extraction and management
Two review authors independently extracted data using a data extraction form specifically developed for this review. Review authors resolved any discrepancies through discussion until they reached consensus. We piloted and accordingly modified the data extraction form before use. In addition to collecting relevant data to perform the risk of bias assessment along with study results, we collected the following information for each study:
Details of the participant sample (age, sex, diagnostic criteria used to confirm CTS, severity of symptoms, duration of symptoms, details of surgical intervention, recruitment method, inclusion and exclusion criteria, number of participants or wrists randomised);
Types of interventions used and comparison groups (description of interventions, method of delivery, duration).
Outcome measures (description and timing).
Two review authors compiled all comparisons and entered outcome data into Cochrane statistical software (Review Manager 5 (RevMan 2012)) for meta‐analysis. Another review author cross‐checked entered data for accuracy. One review author obtained missing data from trial authors when possible. When these efforts were unsuccessful, we included the study in the review and described it fully but did not include it in the meta‐analysis. We entered a description of this process in the notes section of the Characteristics of included studies table.
Assessment of risk of bias in included studies
Two review authors independently assessed included trials using the 'Risk of bias' tool described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We assessed the following items:
random sequence generation;
allocation concealment;
blinding of participants and study personnel;
blinding of outcome assessment;
incomplete outcome data (defined separately for data measured at less than three months, and three months or more);
selective reporting;
other sources of bias.
We rated each item as at low, unclear, or high risk of bias. When criteria were unclear, one review author attempted to obtain further information from the authors of the trial. The review authors resolved any discrepancies by discussion.
Measures of treatment effect
We expressed results as risk ratios (RRs) with 95% confidence intervals (CIs) for dichotomous outcomes, and as mean differences (MDs) with 95% CIs for continuous outcomes, if the same measurement tool was used across separate studies. Alternatively, we used standardised mean differences (SMDs) when studies measured the same outcome with different measurement tools.
Unit of analysis issues
As CTS can affect one or both hands, a unit of analysis error can occur if an appropriate statistical analysis is not used (Stanek 1996). Hence, we sought information about the unit of randomisation (participants or wrists). In studies that randomised wrists, we sought information about whether, in participants with bilateral CTS, each wrist was allocated to a different treatment, or whether no such constraint was present. Given that results are unlikely to be independent for wrists from the same participant, we assessed how investigators accounted for this in their analyses (e.g. paired or matched analyses, generalised estimating equations). If reports did not include this information, we contacted trialists for clarification. We requested individual wrist outcome data from trialists for re‐analysis of the data.
Dealing with missing data
We contacted authors of included studies by mail or by email to request missing information about study design, outcome data, or attrition rates such as dropouts, losses to follow‐up and withdrawn study participants. In relevant sections of this review, we indicated where unpublished data had been obtained from the trial authors.
Assessment of heterogeneity
Review authors assessed clinical heterogeneity by determining whether characteristics of participants, interventions, outcome measures, and timing of outcome measurements were similar across studies. We assessed statistical heterogeneity using the Chi2 statistic and the I2 test (Higgins 2011).
We interpreted the I2 statistic using the following boundaries as an approximate guide:
0% to 40%: might not show important heterogeneity;
30% to 60% may represent moderate heterogeneity;
50% to 90% may represent substantial heterogeneity;
75% to 100% may represent considerable heterogeneity (Deeks 2011).
Assessment of reporting biases
To assess small‐study effects, we intended to generate funnel plots if meta‐analyses included at least 10 studies examining the same treatment comparison (Sterne 2011). To assess outcome reporting bias, we searched protocols of trials on the clinical trials register maintained by the US National Institutes of Health (http://clinicaltrials.gov); we looked at trials published after 1 July 2005 using the Clinical Trial Register, ICTRP (http://apps.who.int/trialssearch), and compared these with the corresponding published randomised controlled trials (Dwan 2008; Dwan 2011).
Data synthesis
We performed statistical analysis using RevMan 5.3. We planned to pool results of studies with similar characteristics (participants, interventions, outcome measures and timing of outcome measurements) to obtain estimates of the efficacy of specific interventions following CTR. We planned to pool results in a meta‐analysis using either a fixed‐effect or a random‐effects model (depending on the level of clinical and methodological heterogeneity). When data could not be combined, we presented the results as a narrative synthesis. We set statistical significance at P < 0.05 for primary and secondary outcome measures.
Subgroup analysis and investigation of heterogeneity
We planned the following prespecified subgroup analyses to assess effects of symptom severity and type of surgical intervention.
-
Severity of CTS symptoms (Szabo 1994):
early CTS, defined as intermittent symptoms, no motor impairment and normal electrophysiological tests;
intermediate CTS, defined as constant symptoms with abnormal electrophysiological tests, with or without motor impairment;
advanced CTS, defined as severe loss of sensory and motor function, the presence of thenar muscle atrophy and weakness, and abnormal electrophysiological and sensory tests.
-
Type of surgical intervention:
endoscopic (single portal or double portal);
open;
minimal‐incision open;
another carpal tunnel surgery (including secondary procedures, such as epineurotomy, internal neurolysis, synovectomy or reconstruction of the transverse carpal ligament).
Sensitivity analysis
We used predetermined sensitivity analyses to assess the effect of excluding studies when (1) allocation concealment was rated as inadequate, not used or unclear (and attempts to clarify with study authors failed); (2) blinding of outcome assessment was not done or was rated as unclear (and attempts to clarify with study authors failed); and (3) intention‐to‐treat analysis was not performed or was unclear (and attempts to clarify with study authors failed). These quality criteria have been shown to influence estimates of treatment effects (Jüni 2001).
`Summary of findings' table
We presented results of the most important comparison of the review in a `Summary of findings' table, which summarise the quality of the evidence, the magnitude of effect of the interventions studied and the sum of available data on outcomes (Schünemann 2011a). The `Summary of findings' table includes an overall grading of the evidence related to each of the primary outcomes, according to the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) Working Group approach (Schunemann 2011b).
For dichotomous outcomes (including presence of iatrogenic symptoms, return to work, and adverse event reporting), we calculated the absolute risk difference using RevMan and expressed the result as a percentage; percentage change was calculated as the risk ratio, and was expressed as a percentage.
For continuous outcomes (including long‐term and short‐term changes in self reported functional ability, changes in CTS clinical symptoms, changes in CTS‐related impairment measures, and changes in neurophysiological parameters), the absolute risk difference was calculated as improvement in the intervention group minus improvement in the control group, expressed in the original units (i.e. mean difference from RevMan divided by units in the original scale), and was expressed as a percentage. Relative percentage change was calculated as the absolute change (or mean difference) divided by the baseline mean of the control group, expressed as a percentage.
We included the following outcomes.
Long‐term improvement in functional ability (DASH) ‐ DASH at six months post surgery.
Change in impairment measure (grip strength) at six months post surgery.
Change in impairment measure (lateral pinch strength) at six months post surgery.
Return to normal occupation ‐ at completion of treatment (two weeks post surgery).
Return to normal occupation ‐ four weeks after completion of treatment (six weeks post surgery).
Return to normal occupation ‐ six weeks after completion of treatment (eight weeks post surgery).
Adverse effects.
Results
Description of studies
Results of the search
Initial searches, which were conducted in April 2012 for the first version of this review, identified a total of 1091 records across databases, clinical trials registers and other sources. Searches were rerun in September 2014, when electronic searches provided by Cochrane Neuromuscular identified a further 140 records; again in September 2015, an updated search found a further 43 new references. Review authors searched PEDro (145 records) and clinical trials registries (332 records). The number of hits from all database and clinical trials registry searches for this update totalled 1503 (Table 1).
We retrieved no articles from the reference lists of potentially eligible studies identified through any of the searches. In total, we selected 35 full‐text papers for review plus two registry records, from which we excluded 10.
At the time the first review was conducted, three studies were awaiting classification (Gordon 2007; NCT00845325; NCT00435149). Since then, we have reclassified one as an ongoing study, as recruitment is still under way (NCT00845325). We have added two studies from the 2014 and 2015 searches to those awaiting classification (Dehghani 2014; Fibir 2014).
Among all searches, 22 studies met the inclusion criteria. These included 20 studies from the 2012 search (Alves 2011; Bhatia 2000; Bury 1995; Cebesoy 2007; Cook 1995; Fagan 2004; Finsen 1999; Gordon 2010; Hochberg 2001; Huemer 2007; Janssen 2009; Jeffrey 2002; Li 2008; Martins 2006; Pomerance 2007; Powell 2003; Provinciali 2000; Ritting 2012; Stevinson 2003; Williams 2008). The updated search in 2014 yielded two additional studies eligible for inclusion in the review (Jerosch‐Herold 2012; Sawan 2013).
Table 1 reports the number of records retrieved by each search strategy. A flow diagram of the study selection process is presented in Figure 1.
1.

Diagram showing the flow of studies through the study selection process.
Table 1
| Number of records retrieved by each search strategy | |||
| Database | Period searched | Date searched | Number of hits |
| Cochrane Neuromuscular Specialised Register | 29 September 2015 | 29 September 2015 | 166 |
| CENTRAL | 2014, Issue 8 | 29 September 2015 | 236 |
| MEDLINE | January 1966 to September 2015 | 29 September 2015 | 285 |
| EMBASE | January 1980 to September 2015 | 29 September 2015 | 203 |
| CINAHL PLUS | January 1937 to September 2015 | 29 September 2015 | 106 |
| AMED | January 1985 to September 2015 | 29 September 2015 | 23 |
| LILACS | January 1982 to September 2015 | 29 September 2015 | 4 |
| PsycINFO | January 1806 to September 2015 | 29 September 2015 | 3 |
| PEDro | January 1999 to December 2015 | 03 December 2015 | 145 |
| ClinicalTrials.gov (www.clinicaltrials.gov) | 03 December 2015 | 03 December 2015 | 123 |
| Current Controlled Trials Register (UK Trials) (www.controlled‐trials.com) | 03 December 2015 | 03 December 2015 | 29 |
| WHO ICTRP (http://www.who.int/ictrp/en/) | 03 December 2015 | 03 December 2015 | 180 |
Included studies
Twenty‐two trials met the inclusion criteria and are described in full in the Characteristics of included studies. The included studies involved a total of 1521 participants, of whom 296 were male and 744 female (with demographic data missing for 481 participants). The trials presented findings across 11 treatments: immobilisation using a wrist orthosis, dressings, exercise, controlled cold therapy, ice therapy, multi‐modal hand rehabilitation, laser therapy, electrical modalities, scar desensitisation, sensory relearning and arnica. Rehabilitation interventions varied in type, intensity, duration and treatment setting. In 15 studies, participants contributed only one CTS‐affected wrist to the study (Alves 2011; Cebesoy 2007; Cook 1995; Fagan 2004; Gordon 2010; Hochberg 2001; Huemer 2007; Janssen 2009; Jerosch‐Herold 2012; Pomerance 2007; Powell 2003; Ritting 2012; Sawan 2013; Stevinson 2003; Williams 2008). In five studies, some participants had bilateral CTR and contributed both wrists to the analysis (Bury 1995; Finsen 1999; Jeffrey 2002; Martins 2006; Provinciali 2000). Of these, two randomised each wrist to different interventions (Finsen 1999; Martins 2006); one randomised both wrists to the same intervention (Jeffrey 2002); and two were unclear regarding the wrist allocation method used (Bury 1995; Provinciali 2000). A unit of analysis error occurred in three of these studies, as no attempt was made to control the correlation between wrists (Finsen 1999; Martins 2006; Provinciali 2000). Jeffrey 2002 avoided a unit of analysis error. However, it was unclear whether a unit of analysis error occurred in Bury 1995. In two studies, it was unclear whether any participants had bilateral CTS (Bhatia 2000; Li 2008), so a unit of analysis error may have occurred.
Four of the 22 included studies reported the primary outcome for this review at three months or more (Cebesoy 2007; Gordon 2010; Pomerance 2007; Powell 2003). However, only three studies reported data in a meaningful format that allowed entry into RevMan (Cebesoy 2007; Pomerance 2007; Powell 2003).
Secondary outcomes were reported as follows: short‐term change in self reported functional ability at less than three months in five studies (Cebesoy 2007; Cook 1995; Jerosch‐Herold 2012; Powell 2003; Williams 2008); change in CTS clinical symptoms ‐ the most common outcome ‐ in 16 studies (Alves 2011, Bhatia 2000; Bury 1995; Cebesoy 2007; Cook 1995; Finsen 1999; Gordon 2010; Hochberg 2001; Huemer 2007; Jeffrey 2002; Jerosch‐Herold 2012; Martins 2006; Pomerance 2007; Powell 2003; Stevinson 2003; Williams 2008); change in CTS impairment measures (grip or pinch strength) in 10 studies (Bury 1995; Cook 1995; Finsen 1999; Gordon 2010; Huemer 2007; Janssen 2009; Jeffrey 2002; Pomerance 2007; Ritting 2012; Sawan 2013); presence of iatrogenic symptoms related to CTR in 10 studies (Alves 2011; Cook 1995; Fagan 2004; Finsen 1999; Hochberg 2001; Huemer 2007; Jeffrey 2002; Martins 2006; Powell 2003; Stevinson 2003); return to work or occupation in six studies, although the time interval was not always adequately defined (Alves 2011; Bury 1995; Cook 1995; Finsen 1999; Pomerance 2007; Provinciali 2000); change in neurophysiological parameters (nerve conduction studies) in three studies (Gordon 2010; Huemer 2007; Sawan 2013); and adverse events related to the rehabilitation intervention in 10 studies (Alves 2011; Bury 1995; Cebesoy 2007; Huemer 2007; Jeffrey 2002; Pomerance 2007; Powell 2003; Ritting 2012; Stevinson 2003; Williams 2008). In some studies, adverse events were reported as iatrogenic symptoms of the surgery, not as adverse events of the rehabilitation intervention.
One of the studies was unpublished, and review authors obtained data entirely from unpublished sources (thesis and communication with trial authors) (Powell 2003). We obtained additional data not reported in study publications from trialists of the following studies: Alves 2011; Finsen 1999; Janssen 2009; Jerosch‐Herold 2012; Martins 2006; Provinciali 2000; Stevinson 2003; Williams 2008. A number of attempts to contact authors of other trials for clarification of information were unsuccessful (Bhatia 2000; Bury 1995; Cook 1995; Fagan 2004; Gordon 2010; Hochberg 2001; Huemer 2007; Li 2008; Pomerance 2007; Ritting 2012; Sawan 2013).
Suitability of trials for meta‐analysis
We were not able to statistically pool data from the included trials because they were too clinically heterogeneous with respect to type and duration of interventions and outcome measures reported. Twelve types of postoperative rehabilitation treatment were identified in the included trials (immobilisation with wrist splint, soft bulky dressings, exercise, specific nerve and tendon gliding exercises, controlled cold therapy, ice therapy, multi‐modal hand rehabilitation, laser therapy, continuous ultrasound, scar desensitisation, sensory relearning and arnica). The duration of treatment ranged from 48 hours (in Bhatia 2000) to six weeks (in Sawan 2013). In 12 trials (Bhatia 2000; Bury 1995; Cebesoy 2007; Cook 1995; Finsen 1999; Gordon 2010; Huemer 2007; Jeffrey 2002; Li 2008; Pomerance 2007; Provinciali 2000; Stevinson 2003), the reported data could not be included in the statistical analysis for several reasons: omission of measures of variability in reports of continuous outcomes (Bury 1995; Cook 1995; Huemer 2007; Jeffrey 2002; Pomerance 2007; Provinciali 2000), no report of the number of participants assessed for an outcome measure (Provinciali 2000), outcome data presented in graphical or other format (Gordon 2010), conclusions stated without support for point estimates, measures of variability or frequency counts of outcomes (Cook 1995; Bhatia 2000; Bury 1995), or CTS‐specific data not provided when participants with other diagnoses were included in the study (Li 2008). Two studies reported median values and CIs indicating skewed data (Finsen 1999; Stevinson 2003); data were not appropriate for inclusion in a standard meta‐analysis.
Summary details of trials are provided in the Characteristics of included studies.
Excluded studies
We excluded 10 studies after review of the full‐text publication. Reasons for exclusion of studies, which are provided in Characteristics of excluded studies,included non‐randomised study design and lack of investigation of post‐CTR interventions.
Risk of bias in included studies
Full details of the 'Risk of bias' assessments are available in the 'Risk of bias' tables; a summary is presented in Figure 2 and Figure 3. For studies in which we rated the risk of bias as unclear, we attempted to contact trial authors to request clarification or additional data.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study. Key: red = high risk of bias; yellow = unclear risk of bias; green = low risk of bias; blank = not applicable.
3.
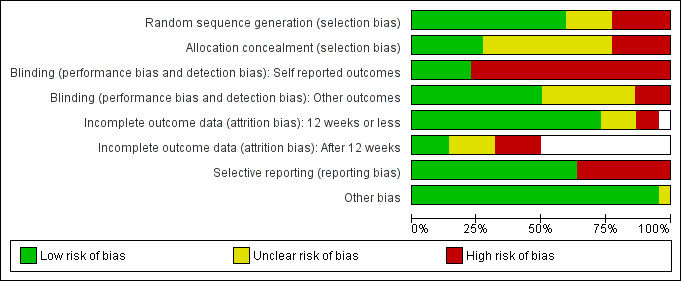
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies (22 studies).
Allocation
We rated generation of the randomisation sequence as at low risk of bias in 13 included trials (Bhatia 2000; Bury 1995; Fagan 2004; Gordon 2010; Hochberg 2001; Janssen 2009; Jerosch‐Herold 2012; Pomerance 2007; Powell 2003; Ritting 2012; Sawan 2013; Stevinson 2003; Williams 2008). Six trials used random number tables to determine allocation sequence (Bhatia 2000; Bury 1995; Gordon 2010; Hochberg 2001; Ritting 2012; Stevinson 2003), and two trials used random envelope draw (Fagan 2004; Williams 2008). One trial used a technique of randomly drawing coloured cubes from a bag (Janssen 2009), and three trials drew allocation from a box or a bowl (Pomerance 2007; Powell 2003; Sawan 2013). One trial used a blocked randomisation sequence (Jerosch‐Herold 2012). Five included trials used some form of alternation (i.e. a non‐random sequence) (Alves 2011; Cebesoy 2007; Finsen 1999; Huemer 2007; Martins 2006). Four studies did not clearly report the randomisation process used (Cook 1995; Jeffrey 2002; Li 2008; Provinciali 2000), and attempts to obtain this information from trial authors were unsuccessful.
Allocation concealment was rated at low risk of bias in six of the included trials (Jeffrey 2002; Jerosch‐Herold 2012; Pomerance 2007; Powell 2003; Sawan 2013; Stevinson 2003). In Gupta 2011, concealment was achieved by use of sequentially numbered, sealed envelopes. Jeffrey 2002 and Stevinson 2003 used an external entity to conceal allocation. Pomerance 2007, Powell 2003 and Sawan 2013 drew allocations out of a box or a bag. Allocation concealment was rated as at high risk of bias in five trials (Alves 2011; Cebesoy 2007; Finsen 1999; Huemer 2007; Williams 2008). Alves 2011 and Huemer 2007 used an alternate method for assigning allocation with odd and even numbers. Finsen 1999 used participants' social security numbers to allocate them to groups. In an unpublished communication received from Jerosch‐Herold 2012, a clinical trials data manager external to the study generated and maintained the randomisation sequence, which was accessed electronically at the time of randomisation. Williams 2008 used the same pieces of paper drawn alternately from an envelope. The remaining 11 studies were rated as having unclear risk of bias, as they did not report any method of concealing the allocation sequence or they reported only some components (Bhatia 2000; Bury 1995; Cook 1995; Fagan 2004; Gordon 2010; Hochberg 2001; Janssen 2009; Li 2008; Martins 2006; Provinciali 2000; Ritting 2012). Attempts to clarify this with trial authors were unsuccessful.
Blinding
Five included studies achieved blinding of participants and study personnel for self reported outcomes and were rated as having low risk of bias (Alves 2011; Janssen 2009; Jeffrey 2002; Powell 2003; Stevinson 2003). This blinding was achieved by delivering a 'sham' or placebo intervention, most commonly with identical looking tablets or ointments (Alves 2011; Jeffrey 2002; Stevinson 2003), or by not informing participants of treatments offered to other group(s) (Powell 2003). Seventeen included studies were not able to achieve participant blinding and were rated as having a high risk of bias (Bhatia 2000; Bury 1995; Cebesoy 2007; Cook 1995; Fagan 2004; Finsen 1999; Gordon 2010; Hochberg 2001; Huemer 2007; Jerosch‐Herold 2012; Li 2008; Martins 2006; Pomerance 2007; Provinciali 2000; Ritting 2012; Sawan 2013; Williams 2008). However, the nature of these interventions (e.g. wrist orthosis versus no orthosis) precluded blinding.
Blinding of independent outcome assessors was achieved in 11 included studies (Janssen 2009; Jeffrey 2002; Jerosch‐Herold 2012; Martins 2006; Pomerance 2007; Powell 2003; Provinciali 2000; Ritting 2012; Sawan 2013; Stevinson 2003; Williams 2008). Blinding of participants completing self reported outcome measures was not achieved in several studies, most probably due to the nature of the interventions. Blinding of outcome assessors was unclear in eight studies (Bhatia 2000; Bury 1995; Cook 1995; Fagan 2004; Finsen 1999; Gordon 2010; Huemer 2007; Li 2008). In these instances, an explicit statement regarding assessor blinding was not included in the trial description, and attempts to clarify this issue with trial authors were unsuccessful. Blinding of outcome assessors was not adequate in three studies, which were rated as having high risk of bias (Alves 2011; Cebesoy 2007; Hochberg 2001).
Incomplete outcome data
We rated 16 studies as having a low risk of bias for completeness of outcome data at less than three months (Alves 2011; Cebesoy 2007; Fagan 2004; Gordon 2010; Hochberg 2001; Huemer 2007; Janssen 2009; Jeffrey 2002; Jerosch‐Herold 2012; Li 2008; Martins 2006; Pomerance 2007; Powell 2003; Sawan 2013; Stevinson 2003; Williams 2008). Of these trials, the percentage lost to follow‐up ranged up to 33% of randomised participants (Hochberg 2001). We rated three studies as unclear in this domain (Bhatia 2000; Cook 1995; Provinciali 2000) and two studies as at high risk of bias (Finsen 1999; Ritting 2012). One trial did not evaluate outcome measures at less than three months (Bury 1995). Six included trials achieved complete follow‐up of the data set (Alves 2011; Cook 1995; Finsen 1999; Huemer 2007; Provinciali 2000; Sawan 2013).
We rated three studies as having a low risk of bias for completeness of outcome data at three months or more (Alves 2011; Gordon 2010; Pomerance 2007), two studies as unclear in this domain (Bury 1995; Cook 1995), and four as having a high risk of bias at one or both time points (Bhatia 2000; Finsen 1999; Li 2008; Stevinson 2003). Thirteen studies did not evaluate outcome measures at three months or more (Cebesoy 2007; Fagan 2004; Hochberg 2001; Huemer 2007; Janssen 2009; Jeffrey 2002; Jerosch‐Herold 2012; Martins 2006; Powell 2003; Provinciali 2000; Ritting 2012; Sawan 2013; Williams 2008).
Selective reporting
We rated 14 studies as having a low risk of bias for selective reporting (Alves 2011; Bhatia 2000; Cebesoy 2007; Hochberg 2001; Janssen 2009; Jeffrey 2002; Jerosch‐Herold 2012; Li 2008; Martins 2006; Powell 2003; Ritting 2012; Sawan 2013; Stevinson 2003; Williams 2008). We assessed eight as having a high risk of bias for selective outcome reporting, as they did not specify results for some of the outcomes listed in the Methods section, only partially reported the results, or provided them in a format that was not suitable for meta‐analysis (Bury 1995; Cook 1995; Fagan 2004; Finsen 1999; Gordon 2010; Huemer 2007; Pomerance 2007; Provinciali 2000).
Other potential sources of bias
We judged all studies as having a low risk of bias for this domain, except Stevinson 2003, which we judged as unclear in this domain, as it was not clearly reported whether protocol violations significantly influenced the data obtained. Attempts to clarify the data received from trial authors were unsuccessful.
Effects of interventions
See: Table 1
Low‐level laser therapy (single intervention) versus 'sham' therapy (placebo)
One trial examined the benefit of low‐level laser therapy following CTR compared with a placebo intervention in 58 participants (Alves 2011). Low‐level laser therapy was applied with an aluminium gallium Ibramed laser pen with 830 nm wavelength and 30 mW power. Treatments were delivered in five daily consecutive sessions, with a rest (no treatment) interval of two days, followed by another five consecutive days of treatment. Laser was delivered at a total of 3 Joules at three points in the carpal tunnel (pisiform, middle of the carpal tunnel and distal limit of the carpal tunnel). Outcomes were assessed at two weeks and at one, two, three and six months or until discharge (mean 3.6 months both groups). Outcomes included iatrogenic pain following surgery (pillar pain or palmar pain); iatrogenic scar discomfort; paraesthesia or numbness; other clinical signs of CTS (numbness, nocturnal pain, paraesthesia, pain or positive Tinel's sign); and time to return to activities of daily living (ADL) and work.
Primary outcomes
The primary outcome measures were:
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Alves 2011 did not assess function on a continuous scale; hence no data could be entered into RevMan. However, trialists reported that all participants in both groups returned to normal ADL.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Not reported in Alves 2011.
-
Change in CTS symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
Symptoms including pain, paraesthesia, numbness and clinical signs (Durkan's test, Tinel's sign, Phalen's test) of CTS were reported as dichotomous outcomes at one, two, three and six months (or on discharge). Average time to discharge for both groups was 3.6 months (intervention group range: one to six months; placebo group range: one to eight months). Results were reported as dichotomous outcomes and were analysed in RevMan as RRs (Analysis 1.1; Analysis 1.2; Analysis 1.3; Analysis 1.4; Analysis 1.5).
No statistically significant differences were noted between participants who received low‐level laser therapy and the placebo group in numbness or palmar pain at one, two and three months post surgery. Clinical signs in low‐level laser and placebo groups at one and two months post surgery were statistically similar (no clinical signs in either group at three months); no nighttime pain was reported in either group at one, two or three months (Analysis 1.2; Analysis 1.3; Analysis 1.4; Analysis 1.5).
Results indicated no statistically significant difference in numbness and paraesthesia at six months post surgery among participants who received low‐level laser therapy versus placebo (Analysis 1.3; Analysis 1.4). None of the participants in either group displayed clinical signs (Durkan's test, Tinel's sign, Phalen's sign) or nighttime pain at six months post operation (Analysis 1.5).
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
Not reported.
-
Presence of iatrogenic symptoms secondary to CTR (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Scar pain and pillar pain were reported as dichotomous outcomes (present versus not present) at one, two, three and six months, or until participants were discharged. Results indicated no statistically significant difference between the low‐level laser therapy group and the placebo group in scar pain and pillar pain at one, two, three and six months post surgery (Analysis 1.6; Analysis 1.7).
-
Return to work or occupation (measured as `yes' or `no') at three months.
All participants (n = 58) in both groups returned to normal occupations at less than three months (Analysis 1.8).
-
Change in neurophysiological parameters (on nerve conduction studies).
Nerve conduction studies were not performed in this study.
-
Presence of adverse events resulting from rehabilitation.
No participants required re‐operation as a result of treatment (Analysis 1.9).
1.1. Analysis.

Comparison 1 Low‐level laser versus placebo, Outcome 1 Change in CTS symptoms (night‐time pain).
1.2. Analysis.

Comparison 1 Low‐level laser versus placebo, Outcome 2 Change in CTS symptoms (palmar pain).
1.3. Analysis.

Comparison 1 Low‐level laser versus placebo, Outcome 3 Change in CTS symptoms (numbness).
1.4. Analysis.

Comparison 1 Low‐level laser versus placebo, Outcome 4 Change in CTS symptoms (paraesthesia).
1.5. Analysis.

Comparison 1 Low‐level laser versus placebo, Outcome 5 Number with CTS clinical signs (Durkan's, Tinel's, Phalen's tests, numbness, paraesthesia, nighttime pain).
1.6. Analysis.

Comparison 1 Low‐level laser versus placebo, Outcome 6 Iatrogenic symptoms (scar pain).
1.7. Analysis.

Comparison 1 Low‐level laser versus placebo, Outcome 7 Iatrogenic symptoms (pillar pain).
1.8. Analysis.

Comparison 1 Low‐level laser versus placebo, Outcome 8 Return to ADL or work (6 months).
1.9. Analysis.

Comparison 1 Low‐level laser versus placebo, Outcome 9 Adverse events (surgery).
Immobilisation (single intervention) versus bulky dressing (single intervention)
We identified two randomised trials (Bhatia 2000; Bury 1995). These trials evaluated effects of immobilisation using a wrist orthosis compared with bulky dressings allowing limited wrist mobility. However, treatment duration and outcomes measured were too clinically heterogeneous for pooling of results.
Bhatia 2000 allocated 130 participants to plaster of Paris splint compared with a bulky dressing applied immediately and worn for 48 hours post surgery. Outcomes assessed included number of pain relief tablets (co‐proxamol) taken and pain intensity measured twice per day for 72 hours post surgery. Trial authors did not report whether participants had bilateral CTR; hence the exact number of wrists included is unknown.
Bury 1995 investigated whether a bulky dressing plus wrist orthosis or a bulky wool and crepe dressing alone worn for two weeks post surgery had better outcomes at final follow‐up (range 3.8 to 7.8 months). Outcomes assessed were patient‐reported outcomes, patient‐reported satisfaction, frequency of residual or recurrent symptoms and complications, digital and wrist range of motion, grip and pinch strength, and thenar muscle function. Results for some outcomes were not reported in the publication, and attempts to obtain these data from trial authors were unsuccessful. Forty‐seven participants were randomised and 40 participants (43 wrists) were included for analysis.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Not reported.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Not reported.
-
Change in CTS symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
Pain was measured in Bhatia 2000 on a visual analogue scale (VAS) twice daily for 72 hours after surgery. No numerical data suitable for entry into RevMan 5 were provided. Using the Mann‐Whitney U test, study authors reported no statistically significant difference in VAS pain scores between participants wearing a wrist orthosis and those wearing a bulky dressing at two weeks of follow‐up.
Bury 1995 reported the number of participants who were 'symptom‐free' and the number 'improved' or 'cured' versus worse or unchanged. Results were dichotomous and were analysed in RevMan as RRs (Analysis 2.1; Analysis 2.2). Bury 1995 found no statistically significant benefit from two weeks of immobilisation with a wrist orthosis over a bulky dressing in terms of being symptom free, or 'improved' or 'cured' rather than 'unchanged' or 'worse' at final follow‐up (mean of six months postoperatively) (Analysis 2.1; Analysis 2.2).
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
Reported in Bury 1995 but not measured in Bhatia 2000.
Bury 1995 measured grip strength (kg) and lateral pinch strength (kg) at a mean of six months of follow‐up but reported only mean values with no measure of variability; investigators reported no statistically significant difference between groups on either measure.
-
Presence of iatrogenic symptoms secondary to CTR (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Not reported.
-
Return to work or occupation (measured as `yes' or `no') at three months.
Reported in Bury 1995 but not measured in Bhatia 2000.
In Bury 1995, seven (27%) participants in the splinted group and two (12%) in the bulky dressing group did not return to work at final follow‐up (average 5.7 months); the difference was not statistically significant (Analysis 2.3).
-
Change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation.
Reported in Bury 1995 but not measured in Bhatia 2000.
In Bury 1995, the wrist orthosis group reported no adverse effects, whereas one participant in the bulky dressing group had persistent symptoms and underwent revision surgery; this difference between groups was not statistically significant (Analysis 2.4).
2.1. Analysis.

Comparison 2 Immobilisation (wrist splint) versus mobilisation (bulky dressing), Outcome 1 Change in CTS symptoms (participant report of being symptom free).
2.2. Analysis.
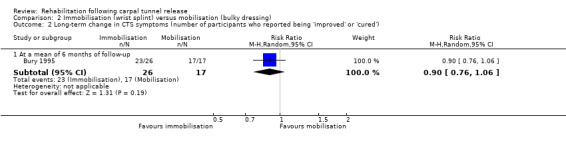
Comparison 2 Immobilisation (wrist splint) versus mobilisation (bulky dressing), Outcome 2 Long‐term change in CTS symptoms (number of participants who reported being 'improved' or 'cured').
2.3. Analysis.

Comparison 2 Immobilisation (wrist splint) versus mobilisation (bulky dressing), Outcome 3 Return to normal occupations.
2.4. Analysis.

Comparison 2 Immobilisation (wrist splint) versus mobilisation (bulky dressing), Outcome 4 Adverse effects.
Immobilisation (single intervention) versus mobilisation (multiple interventions)
Four trials investigated immobilisation versus mobilisation (Cebesoy 2007; Cook 1995; Finsen 1999; Martins 2006). One quasi‐randomised trial investigated immobilisation (plaster wrist orthosis worn until suture removal) and late mobilisation (bulky dressing worn for a three‐week period and immediate early mobilisation exercises) (Cebesoy 2007). Cook 1995 randomly allocated participants to immobilisation with a volar wrist orthosis worn for two weeks or to a bulky dressing and advice to move the hand and wrist with no restrictions. One quasi‐randomised trial compared use of a plaster wrist orthosis for two weeks versus a light dressing and active mobilisation within comfort from 48 hours post surgery (Finsen 1999). Martins 2006 investigated the efficacy of immobilisation with a neutral wrist orthosis worn for two weeks post surgery versus no orthosis and unrestricted movement of the wrist and fingers.
Cebesoy 2007, Cook 1995, Finsen 1999, and Martins 2006 compared effects of immobilisation using a wrist orthosis versus mobilisation with active movement of the affected limb when commenced immediately postoperatively (Cebesoy 2007), on the first postoperative day (Cook 1995), or the second postoperative day (Finsen 1999; Martins 2006). Duration of orthotic use varied between trials: Cebesoy 2007 immobilised the wrists for 10 days, Cook 1995 and Martins 2006 immobilised affected wrists for two weeks, whilst Finsen 1999 immobilised affected wrists for four weeks. However, in Finsen 1999 trialists reported six deviations from protocol in which people were splinted for a shorter or longer time.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Reported in Cebesoy 2007.
Function was assessed using the Functional Severity Scale on the BCTQ preoperatively and three months post surgery in Cebesoy 2007. No statistically significant differences in function were noted between participants receiving bulky dressing and early mobilisation compared with those receiving splint and late mobilisation at three months post surgery (Analysis 3.1).
3.1. Analysis.

Comparison 3 Immobilisation (plaster of Paris splint) versus bulky dressing and mobilisation, Outcome 1 Long‐term improvement in functional ability (BCTQ Functional Status Score).
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Reported in Cebesoy 2007 and Cook 1995.
At one month post surgery in Cebesoy 2007, investigators noted no statistically significant difference in improvement in function (using the BCTQ Functional Severity Scale) between participants receiving bulky dressing and early mobilisation and those receiving orthosis and late mobilisation (Analysis 3.2).
Cook 1995 included the time that participants reported return to normal functional activities of daily living on a continuous scale (from date of surgery to date of activity resumption). No measures of variability were reported, so data could not be entered into RevMan for analysis. However, using a two sample t‐test, the trialists reported a more rapid return to activities in the dressing plus early mobilisation group (mean six days in the non‐splinted group versus 12 days in the splinted group; P = 0.0004).
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
Reported in Cebesoy 2007, Cook 1995, Finsen 1999 and Martins 2006.
-
CTS symptom severity
In Cebesoy 2007, researchers assessed symptoms of CTS using the BCTQ Symptom Severity Scale preoperatively and at one month and three months post surgery. They observed no statistically significant difference in symptom scores between splint and late mobilisation groups at one month or three months (Analysis 3.3).
In Martins 2006, change on the BCTQ Symptom Severity Scale and in Symptom Intensity Score were measured at the end of two weeks' treatment, and were reported as end point mean ± standard deviation (SD) scores and as index mean ± SD scores (calculated as preoperative value ‐ postoperative value/preoperative value). At the end of two weeks of treatment, trialists found no statistically significant differences on the BCTQ Symptom Severity Scale or in Symptom Intensity Score. They observed no statistically significant difference at two weeks in change from preoperative Symptom Severity Score or Symptom Intensity Score (Analysis 3.3, Analysis 3.4;Analysis 3.5).
-
CTS pain severity using a VAS
Cook 1995 assessed pain severity using a VAS (1 to 10) at the end of two weeks of treatment and at two and 10 weeks after cessation of treatment. However, trial authors reported no measures of variability, which precluded entry of data into RevMan. According to study authors, who used an independent samples t‐test, "Average subjective pain rating on a ten point scale was significantly better for the unsplinted patients 14 days after surgery (0.9 for unsplinted versus 2.4 for splinted, P = 0.001) and 1 month after surgery (0.5 for unsplinted versus 1.5 for splinted, P = 0.01). Subjective rating and pain rating did not differ between the two groups 3 and 6 months after surgery."
CTS pain severity (0 to 100 scale) was also assessed in Finsen 1999 at two weeks, six weeks, and six months post surgery. However, study authors reported median values and CIs that were reflective of skewed data (hence not appropriate for inclusion in a standard meta‐analysis). According to study authors, based on results from non‐parametric statistical tests, VAS pain values were not significantly different between immobilised and mobilised groups at any time point post surgery.
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
Reported in Cook 1995 and Finsen 1999.
Grip strength and key pinch strength were measured in Cook 1995 at the end of two weeks of treatment, and at two weeks and 10 weeks after treatment ceased. Measures of variability (e.g. SDs) were not reported by trial authors, and attempts to obtain them were unsuccessful. According to study authors, based on an independent samples t‐test, "Grip strength was slightly greater in unsplinted patients at 14 days after surgery (15 kg in unsplinted versus 10 kg in splinted, P = 0.003) and at 1 month (18 kg in unsplinted versus 14 kg in splinted, P = 0.02). By 3 months grip strength was equivalent in the two groups. Similarly, key pinch strength recovered more rapidly in the unsplinted hands at 14 days (6 kg versus 4 kg, P = 0.01) and 1 month (7 kg versus 5 kg, P = 0.01), but did not differ by 3 months".
Finsen 1999 assessed impairment using measures of grip strength, key pinch strength, and pinch strength between the thumb and fourth and fifth fingers (4/5‐pinch). However, median values and 95% CIs were reported, and attempts to obtain data suitable for inclusion in RevMan 5 were unsuccessful. Based on non‐parametric tests, study authors reported that "There was a considerable loss of strength in the operated hand, compared to preoperative values at 6 weeks for all three parameters. The reductions in grip and key pinch strength were almost identical in the two treatment groups" and "4/5 pinch strength was also significantly reduced in both groups at 6 weeks".
Impairment was assessed using grip strength and key pinch strength in Cook 1995 at six months after treatment cessation. Study authors reported no numerical data, and attempts to obtain these data were unsuccessful. The study authors reported only that they applied a two‐sample t test and "...by 6 months grip strength in both groups slightly exceeded preoperative grip strength....".
Grip strength, key pinch strength, and pinch strength between the thumb and fourth and fifth fingers (4/5‐pinch) were also measured in Finsen 1999 at six months post surgery, but data were reported in a format that was not suitable for entry into RevMan 5. According to the study authors, "At 6 months, the grip strength had returned to preoperative values in both groups and the key pinch strength had improved considerably. Again, the values in the two groups were almost the same...It [4/5 pinch strength] had improved after 6 months, but was still around 20% lower than preoperatively. Patients in the immobilised group were slightly weaker than the others, but the difference was not statistically significant".
Two‐point discrimination and touch sensation determined by Semmes‐Weinstein monofilaments were measured in Cook 1995 at the end of two weeks of treatment, and at two weeks and 10 weeks after treatment ceased. Measures of variability were not reported by trial authors, and attempts to obtain data were unsuccessful. According to the study authors, an independent sample t‐test revealed that "improvement in two‐point discrimination and sensibility measured using Semmes‐Weinstein monofilaments was similar in the two groups of patients". At the end of two weeks of treatment, touch sensation was measured using two‐point discrimination in Martins 2006. Investigators noted a significant difference between end point scores of immobilisation and mobilisation groups. However, the difference between change scores at two weeks post operation was not statistically significant (Analysis 3.6;Analysis 3.7).
-
Presence of iatrogenic symptoms secondary to CTR (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Reported in Cook 1995, Finsen 1999 and Martins 2006.
Finsen 1999, Cook 1995 and Martins 2006 reported the presence of iatrogenic complications resulting from CTR surgery. Cook 1995 reported that no wound complications nor bowstringing of tendons was observed in either group. Further, they reported no statistically significant difference between orthosis and mobilisation (using range‐of‐motion exercises) groups in the incidence of scar tenderness or pillar pain at one month. No statistically significant difference was found in Finsen 1999 between wrist immobilisation and mobilisation groups in frequency of scar discomfort pain, hypothenar pain or thenar pain at six weeks and at six months. Martins 2006 reported that no median nerve lesion, wound dehiscence or tendon injuries were experienced in either group. For all analyses, see Analysis 3.8.
-
Return to work or occupation (measured as `yes' or `no') at three months.
Reported in Cook 1995 and Finsen 1999.
Cook 1995 reported the mean number of days until return to activities of daily living, to light duty work, and to full duty work. However, they reported no measures of variability. Using an independent samples t‐test, study authors reported: "Unsplinted patients had a more rapid return to activities of daily living (average six days in unsplinted, 12 days in splinted, P = 0.0004); more rapid return to light duty work (15 days in unsplinted, 24 days in splinted, P = 0.01); and more rapid return to full duty work (17 days in unsplinted, 27 days in splinted, P = 0.005)".
Finsen 1999 reported the number of weeks sicklisted by participants in each group who had been gainfully employed before CTR. Study authors reported median values and CIs that were reflective of skewed data (not appropriate for inclusion in a standard meta‐analysis). Gainfully employed participants in both the mobilisation group and the immobilised group were sicklisted for a median of six weeks postoperatively (95% CI 5 to 6 weeks and 4 to 7 weeks, respectively).
-
Change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation.
In Cebesoy 2007, 16 of 20 participants (80%) in the splinted group reported a heavy feeling and discomfort caused by the intervention, whereas none of the participants in the bulky dressing group reported this problem (Analysis 3.9). No flexor bowstringing was reported in either group.
Cook 1995, Finsen 1999 and Martins 2006 reported complications (iatrogenic symptoms) resulting from carpal tunnel surgery rather than complications resulting from the rehabilitation intervention.
3.2. Analysis.

Comparison 3 Immobilisation (plaster of Paris splint) versus bulky dressing and mobilisation, Outcome 2 Short‐term improvement in functional ability (BCTQ Functional Status Score).
3.3. Analysis.

Comparison 3 Immobilisation (plaster of Paris splint) versus bulky dressing and mobilisation, Outcome 3 Change in CTS symptoms (BCTQ Symptom Severity Score).
3.4. Analysis.

Comparison 3 Immobilisation (plaster of Paris splint) versus bulky dressing and mobilisation, Outcome 4 Change in CTS symptoms (Symptom Intensity Score).
3.5. Analysis.

Comparison 3 Immobilisation (plaster of Paris splint) versus bulky dressing and mobilisation, Outcome 5 Change score between baseline and 2 weeks (Symptom Intensity Score).
3.6. Analysis.

Comparison 3 Immobilisation (plaster of Paris splint) versus bulky dressing and mobilisation, Outcome 6 Change in impairment (sensibility measured using static two‐point discrimination).
3.7. Analysis.

Comparison 3 Immobilisation (plaster of Paris splint) versus bulky dressing and mobilisation, Outcome 7 Change score between baseline and 2 weeks (Discrimination Index).
3.8. Analysis.

Comparison 3 Immobilisation (plaster of Paris splint) versus bulky dressing and mobilisation, Outcome 8 Iatrogenic symptoms.
3.9. Analysis.

Comparison 3 Immobilisation (plaster of Paris splint) versus bulky dressing and mobilisation, Outcome 9 Adverse event.
Elevation (single intervention) versus standard care (control)
Fagan 2004 compared the benefit of elevation using a home elevation device with a Bradford sling suspended vertically at night and a crepe sling when ambulant for five days post surgery versus control (standard care), in 43 participants. Outcomes included hand volume using a volume displacement apparatus (assessed preoperatively and at five days post surgery), pain (assessed once a day for five days post surgery) and daily analgesic usage (for five days).
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Not reported.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Pain was assessed on a VAS (0 to 10 scale) at five days post surgery. No statistically significant difference in this outcome was noted between participants using a home elevation device and a Bradford sling and those receiving standard care (Analysis 4.1).
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
Not reported.
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
Not reported.
-
Presence of iatrogenic symptoms secondary to CTR (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Swelling (volume) was assessed preoperatively and at five days post surgery with a volume displacement apparatus. Investigators found no statistically significant difference in swelling between the home elevation device and standard care (Analysis 4.2).
-
Return to work or occupation (measured as `yes' or `no') at three months.
Not reported.
-
Short‐term (less than three months) and long‐term (three months or more) change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation at short‐term (less than three months) and long‐term (three months or more) follow‐up.
Not reported.
4.1. Analysis.

Comparison 4 Specialised home elevation device versus standard sling, Outcome 1 Short‐term improvement in CTS symptoms (VAS pain 0 to 10) (3 months or less).
4.2. Analysis.

Comparison 4 Specialised home elevation device versus standard sling, Outcome 2 Iatrogenic symptoms (swelling).
Electrical stimulation (single intervention) versus no treatment (control)
Gordon 2010 compared use of electrical stimulation of the median nerve 30 minutes after CTR for one hour versus no treatment. Twenty‐five participants (25 wrists) were allocated to the intervention group or the control group. Outcomes included results of nerve conduction studies, BCTQ (Symptom Severity Score and Functional Status Scores) and hand touch sensation with Semmes‐Weinstein monofilaments. Outcomes were assessed twice preoperatively, and at three, six to eight and 12 months post surgery.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
In Gordon 2010, BCTQ Functional Status Score was used to measure functional ability at three, six to eight and 12 months post surgery. Statistics were reported graphically, and attempts to obtain numerical data from trial authors were unsuccessful.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Not reported.
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
BCTQ (Symptom Severity Score) was used to measure functional ability at three, six to eight and 12 months post surgery. Statistics were reported graphically, and attempts to obtain numerical data from trial authors were unsuccessful.
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
Impairment in touch sensation was measured with Semmes‐Weinstein monofilaments at three, six to eight and 12 months post surgery. Statistics were reported graphically, and attempts to obtain numerical data from trial authors were unsuccessful.
-
Presence of iatrogenic symptoms secondary to CTR (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Not reported.
-
Return to work or occupation (measured as `yes' or `no') at three months.
Not reported.
-
Change in neurophysiological parameters (on nerve conduction studies).
Nerve conduction (using motor terminal latency and sensory terminal latency) was measured at baseline (preoperatively) and at three months post surgery. Study authors stated that "the latency did not change significantly in the control group in the postoperative period, while in contrast, significant acceleration in the motor latency occurred early in the stimulation group at 3 months. Motor latencies from 3 months onwards were the same as that for the healthy subjects. Similarly, early recovery of conduction velocity of the sensory nerve fibres was found in the stimulation group at 3 months when amplitude of the SNAP had not yet changed significantly from preoperative values. In contrast recovery was delayed in the control patient group".
-
Presence of adverse events resulting from rehabilitation.
Not reported.
Controlled cold therapy and narcotic use (multiple interventions) versus ice therapy plus narcotic use (multiple interventions)
One randomised trial (Hochberg 2001) compared controlled cold therapy (plus narcotic use) with ice therapy (plus narcotic use). Controlled cold therapy was applied with a thermostatically controlled cooling blanket maintained at 7.2°C continuously for 12 hours per day for three days post surgery. Ice therapy was applied with a commercially available ice pack applied immediately after surgery, and on return home use of an ice bag (ice cubes in a plastic bag) for 12 hours per day for three days post surgery. Participants in both groups were provided with 28 combined hydrocodone and paracetamol pain relief tablets. Seventy‐two participants (72 wrists) were randomly allocated to either of the intervention groups. Outcomes, which were measured preoperatively, immediately post surgery and three days post surgery, included swelling measured at the wrist by circumference and pain intensity.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Not reported.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Not reported.
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
Intensity of pain severity (measured on a 0 to 10 VAS) was measured before CTR and at the end of three days of treatment. Endpoint and change scores were reported on the basis of a per‐protocol analysis and an intention‐to‐treat analysis. At the end of three days of treatment, participants receiving controlled cold therapy were found to have statistically significantly less pain than those receiving ice therapy on the basis of a per‐protocol analysis (MD ‐2.80, 95% CI ‐4.50 to ‐1.10) and an intention‐to‐treat analysis (MD ‐1.90, 95% CI ‐3.51 to ‐0.29). However, although the controlled cold therapy group had a statistically significantly greater reduction in pain from baseline to day three on the basis of a per‐protocol analysis (MD ‐2.80, 95% CI ‐4.88 to ‐0.72), no statistically significant change in pain between groups was found when an intention‐to‐treat analysis was performed (MD ‐1.40, 95% CI ‐3.24 to 0.44) (Analysis 5.1).
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
Not reported.
-
Presence of iatrogenic symptoms secondary to CTR surgery (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Swelling was recorded by taking wrist circumference measurements immediately postoperatively and at three days post surgery. Both end point and change scores were reported on the basis of a per‐protocol analysis and an intention‐to‐treat analysis. At the end of three days of treatment, investigators reported no statistically significant difference in the amount of swelling (end point score) between controlled cold therapy and ice therapy groups on the basis of a per‐protocol analysis or an intention‐to‐treat analysis. However, when change scores were measured, the controlled cold therapy group had a statistically significantly greater reduction from baseline to day three compared with the ice therapy group on the basis of a per‐protocol analysis (MD ‐1.00, 95% CI ‐1.26 to ‐0.74) and intention‐to‐treat analyses (MD ‐1.10, 95% CI ‐1.33 to ‐0.87) (Analysis 5.2).
We have assumed that the mean change from baseline to day three in oedema (wrist circumference) in the "ice therapy group" was incorrectly reported by trial authors. In both cases, the value reported was ‐0.7, but end point scores suggest that these values should be +0.7, as wrist circumference increased in the ice therapy group. Further, study authors report the following: "At 3 days, of the 24 CCT [controlled cold therapy] patients, 19 showed reduction in mean wrist circumference from baseline, three showed no change and two showed an increase. In contrast, all patients in the ice therapy group showed an increase in mean wrist circumference at 3 days. When all patients for whom edema scores were available were included in an intention‐to‐treat analysis, the CCT group again showed a statistically significant greater reduction in wrist circumference from baseline and significantly greater mean percentage reduction in wrist circumference than the ice‐therapy group." Attempts to contact study authors to confirm this have been unsuccessful.
-
Return to work or occupation (measured as `yes' or `no') at three months.
Not reported.
-
Change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation.
Not reported.
5.1. Analysis.

Comparison 5 Controlled cold therapy versus ice therapy, Outcome 1 Short‐term improvement in CTS symptoms (VAS pain 0 to 10) (3 months or less).
5.2. Analysis.

Comparison 5 Controlled cold therapy versus ice therapy, Outcome 2 Iatrogenic symptoms (swelling).
Bulky dressing and splint (single intervention) versus light dressing (single intervention)
One trial by Huemer 2007 allocated 50 participants (50 wrists) to either a bulky dressing with a volar wrist orthosis in a neutral position for 48 hours post surgery or to a light bandage dressing worn for 48 hours post surgery. Outcomes were measured preoperatively and at three months post surgery and included pain intensity, two‐point discrimination, grip strength, results of nerve conduction studies and scar tenderness.
Primary outcome
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Not reported.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Not reported.
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness and paraesthesia).
Pain (VAS 0 to 10) was assessed in Huemer 2007 at the end of two days of treatment; however, no measure of variability was reported, so data could not be entered into RevMan. No statistically significant difference between participants wearing a wrist splint and those wearing a light dressing for 48 hours post CTR was reported.
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
In Huemer 2007, CTS‐related impairment was assessed using measures of grip strength (kg) at three months post surgery. Only mean values were reported (no measures of variability were available). Study authors reported no statistically significant differences.
Two‐point discrimination was used to measure hand numbness. However, no measurement of variability was reported, so data could not be entered into RevMan.
-
Presence of iatrogenic symptoms secondary to CTR (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Participants in Huemer 2007 were asked to report whether they had no perceptible scar pain, scar pain with pressure or scar pain at rest at three months of follow‐up. Investigators reported no statistically significant difference between immobilisation and light dressing groups in the number of participants who reported having no perceptible scar pain at three months (Analysis 6.1).
-
Return to work or occupation (measured as `yes' or `no') at three months.
Not reported.
-
Change in neurophysiological parameters (on nerve conduction studies).
Distal motor latency (ms) was reported in Huemer 2007 as mean improvement from baseline to three months of follow‐up. However, only mean values were given, so no data could be entered into RevMan 5.1. Study authors reported no statistically significant difference between splint and light dressing groups.
-
Presence of adverse events resulting from rehabilitation.
Huemer 2007 reported no median nerve, digital nerve, vascular, or tendon complications in either group, and no delayed wound healing.
6.1. Analysis.

Comparison 6 Bulky dressing plus splint versus light dressing, Outcome 1 Iatrogenic symptom (scar pain).
Contrast baths plus exercise (multiple interventions) versus contrast baths (single intervention) versus exercise (single intervention)
One randomised trial (Janssen 2009) allocated 58 participants to contrast baths alone or to contrast baths plus exercise, or to exercise only for treatment of postoperative oedema in the period immediately after CTR. Outcomes, which were measured immediately after treatment delivered 10 to 14 days post surgery, included hand volume assessed by the water displacement method.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Not reported.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Not reported.
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness and paraesthesia).
Not reported.
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
Not reported.
-
Presence of iatrogenic symptoms secondary to CTR (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Oedema (measured as change in hand volume in mL) was measured before and after the intervention at 10 to 14 days post surgery. Janssen 2009 found no statistically significant difference in swelling between participants receiving contrast baths plus exercises and those receiving contrast baths alone. Swelling was greater with contrast baths plus exercises than with exercises alone (MD 23.20, 95% CI 3.60 to 42.80), and swelling was greater with contrast baths alone than with exercises alone (MD 32.00, 95% CI 12.61 to 51.39) (Analysis 7.1; Analysis 8.1; Analysis 9.1).
-
Return to work or occupation (measured as `yes' or `no') at three months.
Not reported.
-
Change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation.
Not reported.
7.1. Analysis.
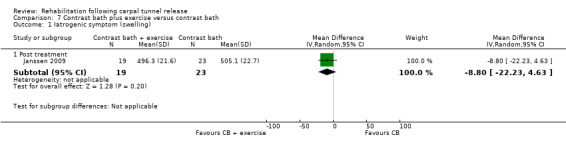
Comparison 7 Contrast bath plus exercise versus contrast bath, Outcome 1 Iatrogenic symptom (swelling).
8.1. Analysis.
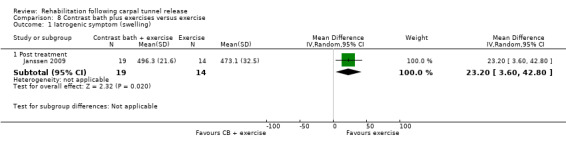
Comparison 8 Contrast bath plus exercises versus exercise, Outcome 1 Iatrogenic symptom (swelling).
9.1. Analysis.

Comparison 9 Contrast bath versus exercise, Outcome 1 Iatrogenic symptom (swelling).
Arnica (single intervention) versus `sham' therapy (placebo)
One randomised trial (Jeffrey 2002) examined the efficacy of arnica D6 tablets and ointment used postoperatively for swelling and bruising. Forty participants (80 wrists) were allocated to the intervention group or the placebo group. They were advised to take the tablets three times daily for two weeks and to commence massage of the ointments around the wound at 72 hours post surgery until two weeks post surgery. Outcomes were measured preoperatively and at one week and two weeks post surgery. Outcomes included grip strength, wrist circumference, pain intensity, and adverse events such as allergy or infection.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Not reported.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than 3 months
Not reported.
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness and paraesthesia).
Pain intensity during the postoperative period was measured on a VAS (which was converted to a 0 to 10 scale) at the end of one and two weeks of treatment. However, only mean values were reported numerically (SDs were presented graphically, but could not be extracted using Microsoft Paint). Using Student's t‐test or the Mann‐Whitney U test, the authors reported that "At 1 week, the Arnica group had a mean hand‐discomfort score of 2.6 compared with 3.5 for the placebo group; this was not significantly different. At 2 weeks, the Arnica group had a mean hand‐discomfort score of 1.3 compared with 2.5 for the placebo group, which was statistically significant (P < 0.03)."
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
Grip strength (kg) was measured in Jeffrey 2002. No statistically significant difference in percentage change from preoperative values was found between participants receiving arnica D6 tablets and ointment and those receiving placebo at the end of one and two weeks of treatment (Analysis 10.1).
-
Presence of iatrogenic symptoms secondary to CTR (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Jeffrey 2002 found no statistically significant difference between arnica D6 tablets and ointment versus placebo in terms of percentage change from preoperative value in hand swelling (wrist circumference) at the end of one week and two weeks' treatment (Analysis 10.2).
-
Return to work or occupation (measured as `yes' or `no') at three months.
Not reported.
-
Change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation.
In Jeffrey 2002, no adverse effects (such as allergy or infection) were reported in the arnica or placebo group.
10.1. Analysis.

Comparison 10 Arnica versus placebo, Outcome 1 Change in impairment measure (grip strength).
10.2. Analysis.

Comparison 10 Arnica versus placebo, Outcome 2 Iatrogenic symptom (swelling; % wrist circumference change difference).
High‐dose arnica (single intervention) versus low‐dose arnica (single intervention) versus `sham' therapy (placebo)
Stevinson 2003 randomly allocated 64 participants to high‐dose (30C) arnica tablets or to low‐dose (6C) arnica tablets or to placebo. Arnica was taken three times per day for seven days preoperatively and for 14 days postoperatively. The placebo tablets were identical in appearance to the arnica tablets. Outcomes included pain assessed by the short‐form McGill Pain Questionnaire (MPQ), bruising measured by colour analysis from a photograph of participants' hands, clinician‐rated bruising, swelling measured by wrist circumference, use of analgesic medication, and adverse events.
Primary outcomes
-
Change in self reported functional ability as measured on a continuous scale at three months or more.
Not reported.
Secondary outcomes
-
Change in self reported functional ability as measured on a continuous scale at less than three months.
Not reported.
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
Pain was assessed using the MPQ (0 to 100 VAS) and by asking participants to rate whether they experience different pain descriptor words such as 'stabbing, 'gnawing' and 'shooting'. However, data for these continuous measures could not be entered into RevMan 5, as only median (range) values were reported. Using Chi2 tests, study authors reported only that: "Postoperative pain did not differ between the groups at day 4 according to VAS scores..." They also reported: "The only group difference that approached statistical significance was the MPQ descriptors' total score (Chi2 = 6.72, d.f. = 2, P = 0.04) where the placebo group had lower scores than the arnica 30C group at day nine (U = 122.0, P = 0.01, Mann–Whitney U test)."
-
Short‐term (less than three months) and long‐term (three months or more) change in CTS‐related impairment measures (e.g. grip and pinch strength).
Not reported.
-
Presence of iatrogenic symptoms secondary to CTR surgery (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Stevinson 2003 reported the number of participants rated by a clinician as having no, mild to moderate, or severe bruising after 4, 9 and 14 days of treatment. We dichotomised participants into those rated as having 'no bruising' and those rated as having mild to moderate or severe bruising. Investigators found no statistically significant difference in the number of participants rated as having no bruising between arnica 30C and placebo, between arnica 6C and placebo or between the two doses of arnica, at any of the three time points (Analysis 11.1; Analysis 12.1;Analysis 13.1). Stevinson 2003 also assessed the extent of bruising (by taking a photograph of participants' wrists and analysing blue and red channel brightness). Similarly, bruising did not differ between groups at day four in terms of blue or red channel brightness.
-
Return to work or occupation (measured as `yes' or `no') at three months.
Not reported.
-
Change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation.
In Stevinson 2003, eight participants reported adverse effects: three in the placebo group (heartburn; sore throat and flu‐like symptoms; faintness and headache), three in the arnica 30C group (dry mouth; headache; feeling ‘throbby’ in head/neck) and two in the arnica 6C group (drowsiness; sore tongue). Differences between groups (arnica 30C versus placebo, arnica 6C versus placebo and arnica 30C versus arnica 6C) were not statistically significant (Analysis 11.2; Analysis 12.2; Analysis 13.2).
11.1. Analysis.

Comparison 11 High‐dose arnica oral tablets versus placebo, Outcome 1 Iatrogenic symptoms (number of participants with no clinician‐rated bruising).
12.1. Analysis.

Comparison 12 Low‐dose arnica tablets versus placebo, Outcome 1 Iatrogenic symptoms (number of participants with no clinician‐rated bruising).
13.1. Analysis.

Comparison 13 High‐dose versus low‐dose oral arnica tablets, Outcome 1 Iatrogenic symptoms (number of participants with no clinician‐rated bruising).
11.2. Analysis.

Comparison 11 High‐dose arnica oral tablets versus placebo, Outcome 2 Adverse effects.
12.2. Analysis.

Comparison 12 Low‐dose arnica tablets versus placebo, Outcome 2 Adverse events.
13.2. Analysis.

Comparison 13 High‐dose versus low‐dose oral arnica tablets, Outcome 2 Adverse events.
Electrical stimulation versus decimer wave therapy versus combined therapy versus control
Li 2008 enrolled three different treatment groups and a no treatment control group to examine the benefit of decimeter wave therapy and electrical stimulation for recovery of nerve function following peripheral nerve entrapment surgery. Each treatment group was treated for 20 days and then had a 10‐day break, for three months. The first intervention group was given once‐daily electrical stimulation, six minutes per session, and the second group, daily decimeter wave therapy with a mild‐hot therapeutic instrument applied at early stages at 10 to 15 W for 10 minutes per session, increased to 10 to 30 W in the middle‐late phase of treatment for 20 minutes per session. The third group received compound physical factor treatment (electrical stimulation and decimeter wave therapy combined). A total of 124 participants with peripheral nerve entrapment were allocated to the four groups; 75 of them had CTS. Trial authors did not report CTS‐specific data, and attempts to obtain this information were unsuccessful. Therefore, we were not able to analyse outcome data in this review.
Multi‐modal hand therapy (multiple interventions) versus no formal therapy (control)
Pomerance 2007 examined the effects of a formal programme of multi‐modal hand therapy (consisting of six 30‐minute sessions of nerve gliding, range of motion and strengthening and additional treatments, e.g. massage, fluidotherapy with a qualified hand therapist). Treatments were provided over a two‐week period starting at five to seven days post surgery. The control group received advice regarding tendon gliding exercises and scar massage before surgery but no formal therapy after surgery. A total of 150 participants were randomised. Outcomes included time to return to work, pain intensity, lateral pinch strength, grip strength, function using the DASH questionnaire, persistence of symptoms, wound dehiscence and an economic evaluation of the intervention.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
DASH was measured at five and a half months post treatment (six months post surgery). Investigators reported no statistically significant difference between treatments (Analysis 14.1).
14.1. Analysis.

Comparison 14 Multi‐modal hand therapy versus normal activities/exercise, Outcome 1 Long‐term improvement in functional ability (DASH).
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Not reported.
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
Change in CTS clinical symptoms was measured in Pomerance 2007 on a VAS (0 to 10) to assess CTS pain at the end of two weeks of treatment, at 2, 4, and 10 weeks and five and a half months after completion of treatment (2, 4, 6, and 12 weeks and six months post surgery). However, no numerical data were reported for this outcome, and study authors reported only that when applying Student's t‐test, they found no statistically significant difference in pain complaints at any time point post surgery between multi‐modal hand therapy and no therapy groups.
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
Grip strength (kg) and lateral pinch strength (kg) were measured in Pomerance 2007. Change in grip strength was not statistically significantly different in the multi‐modal hand therapy group compared with the control group at any time point (Analysis 14.2). Nor was multi‐modal hand therapy found to improve lateral pinch strength compared with controls (Analysis 14.3).
-
Presence of iatrogenic symptoms secondary to CTR (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Not reported.
-
Return to work or occupation (measured as `yes' or `no') at three months.
The number of participants in each group who returned to regular duty work at certain time points was recorded by Pomerance 2007. Data were reported separately for cases with Medicare insurance, commercial insurance, and workers' compensation insurance, but these data were combined for entry into RevMan. Investigators found no statistically significant difference between multi‐modal hand therapy and no formal therapy in terms of the number of participants in each group who had returned to work by two weeks post surgery, but at six weeks post surgery (RR 1.02, 95% CI 0.89 to 1.17) and at eight weeks post surgery (RR 1.04, 95% CI 0.97 to 1.12), results favoured the therapy group. It was reported that all participants in this trial had returned to regular duty work by 12 weeks following CTR (Analysis 14.4).
-
Change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation.
Pomerance 2007 reported that three adverse effects occurred throughout the study period: one in the multi‐modal hand therapy group and two in the no therapy control group, with no statistically significant difference between groups. These participants experienced wound dehiscence when sutures were removed five days postoperatively (Analysis 14.5).
14.2. Analysis.

Comparison 14 Multi‐modal hand therapy versus normal activities/exercise, Outcome 2 Change in impairment measure (grip strength).
14.3. Analysis.
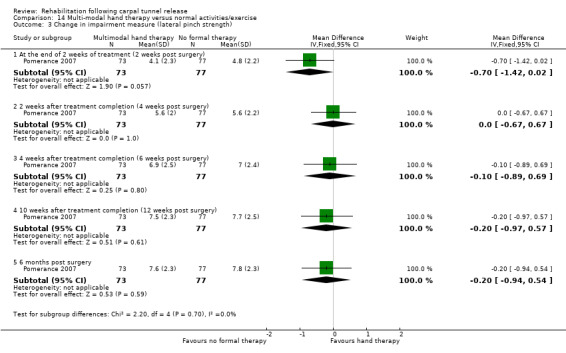
Comparison 14 Multi‐modal hand therapy versus normal activities/exercise, Outcome 3 Change in impairment measure (lateral pinch strength).
14.4. Analysis.

Comparison 14 Multi‐modal hand therapy versus normal activities/exercise, Outcome 4 Return to normal occupations.
14.5. Analysis.

Comparison 14 Multi‐modal hand therapy versus normal activities/exercise, Outcome 5 Adverse effects.
Desensitisation therapy (as part of multiple interventions) versus standard treatment (control)
The Powell 2003 unpublished study randomly allocated 29 participants to a graduated desensitisation programme for three months or to a standard treatment control group. Outcomes were measured at three weeks, six weeks, and three months post operation. Outcomes included scar sensitivity assessed by a dolorimeter (pressure gauge), patient‐reported scar sensitivity, functional status using the BCTQ Functional Status Scale, and grip strength.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
BCTQ Functional Status Scale was used to record functional ability at three months. Investigators reported no statistically significant benefit of graded desensitisation over standard treatment (Analysis 15.1).
15.1. Analysis.

Comparison 15 Desensitisation therapy (as part of multiple interventions) versus no treatment, Outcome 1 Long‐term improvement in functional ability (BCTQ Functional Status Score).
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
BCTQ Functional Status Scale was used to measure self reported functional ability at three weeks and six weeks. No statistically significant difference was found between intervention and control groups at three or six weeks postoperatively (Analysis 15.2).
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness and paraesthesia).
Discomfort was measured on a 0 to 100 VAS. Investigators found no statistically significant differences between intervention and control groups at three, six and 12 weeks postoperatively (Analysis 15.3).
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
Impairment was assessed by measuring grip strength. Trial authors found no statistically significant differences between groups at three, six and 12 weeks postoperatively (Analysis 15.4).
-
Presence of iatrogenic symptoms secondary to CTR (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Iatrogenic symptoms including scar sensitivity were assessed by an objective dolorimeter pressure gauge. Investigators found no statistically significant differences between groups at three, six and 12 weeks postoperatively (Analysis 15.5).
-
Return to work or occupation (measured as `yes' or `no') at three months.
Not reported.
-
Change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation.
No adverse events were recorded in the intervention or control group with respect to wound dehiscence.
15.2. Analysis.

Comparison 15 Desensitisation therapy (as part of multiple interventions) versus no treatment, Outcome 2 Short‐term improvement in functional ability (BCTQ Functional Status Score).
15.3. Analysis.

Comparison 15 Desensitisation therapy (as part of multiple interventions) versus no treatment, Outcome 3 Change in CTS symptoms (pain or discomfort).
15.4. Analysis.

Comparison 15 Desensitisation therapy (as part of multiple interventions) versus no treatment, Outcome 4 Change in impairment measure (grip strength).
15.5. Analysis.

Comparison 15 Desensitisation therapy (as part of multiple interventions) versus no treatment, Outcome 5 Iatrogenic symptoms (scar sensitivity assessed by dolorimetry).
Multi‐modal therapy (multiple interventions) versus progressive patient‐directed home exercise programme (single intervention)
Provinciali 2000 examined the benefits of a multi‐modal formal therapy programme (10 one‐hour sessions of physiotherapy including soft tissue mobilisation, exercises, scar massage, nerve gliding, grip and pinch exercises, motor dexterity exercises, sensory stimulation and sensory re‐education by the same physiotherapist), compared with a progressive patient‐directed home exercise programme. Outcomes included hand dexterity on the nine‐hole peg test, hand function assessed by the Jebsen‐Taylor test, BCTQ Symptom Severity Scale outcomes and time to return to work for workers' compensation participants. One hundred participants were allocated to each group; some participants were reported to have had bilateral surgeries.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Not reported.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Not reported.
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
Symptom severity was assessed in Provinciali 2000 using the Italian version of the BCTQ at the end of two weeks of treatment (one month post surgery) and two months later. Study authors reported only summed scores across participants for items 1 to 10 (with no measures of variability). Therefore, these data could not be entered into RevMan 5 for statistical analysis. Using a Chi2 test and applying the Bonferroni correction, which resulted in the criterion for statistical significance being set at P < 0.001, study authors reported no significant difference in occurrence of CTS symptoms between the multi‐modal hand therapy group and the home exercises group at either time point.
-
Change in CTS‐related impairment measures (e.g. grip and pinch strength).
Not reported.
-
Presence of iatrogenic symptoms secondary to CTR surgery (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Not reported.
-
Return to work or occupation (measured as `yes' or `no') at three months.
Provinciali 2000 measured the mean number of days until participants returned to work. However, workers' compensation cases were excluded, and the report does not state the number excluded from this outcome analysis or the proportion of participants returning to work in each group. Therefore, these data could not be entered into RevMan for analysis.
-
Change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation.
Not reported.
Short duration postoperative dressing (single intervention) versus extended duration postoperative dressing (single intervention)
Two trials (Ritting 2012; Williams 2008) investigated the effects of short versus extended duration postoperative dressing. In Ritting 2012, 94 participants were allocated to a postoperative bulky dressing worn for 48 to 72 hours or for nine to 14 days. Outcomes were measured at two weeks and six to 12 weeks post surgery and included BCTQ, grip strength, tip pinch strength, three‐point pinch strength, lateral pinch strength and wound healing. Williams 2008, in a study that included 100 participants, compared outcomes from a bulky dressing applied for 24 hours versus one applied for two weeks post surgery. Outcomes were assessed preoperatively and at the end of the intervention (two weeks) and included BCTQ and change in iatrogenic symptoms.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Measured in Ritting 2012 but not in Williams 2008.
Ritting 2012 measured overall results of the BCTQ (Symptom Severity Score and Functional Status Score reported as a combined score) at six to 12 weeks. As the functional status score was not reported separately, no data could be entered into Revman for this outcome.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Measured in Williams 2008 but not in Ritting 2012.
Williams 2008 analysed BCTQ Functional Status Scores and found no statistically significant difference in end point scores at two weeks, but the change from baseline score favoured the extended duration dressing (MD 0.40, 95% CI 0.05 to 0.75) (Analysis 16.1).
Ritting 2012 reported overall BCTQ and Functional Status Scores, but results were not available for analysis.
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
Measured in Williams 2008 but not measured in Ritting 2012.
Williams 2008 analysed Symptom Severity Scores from the BCTQ and found no statistically significant differences between groups at end point (two weeks). However, trial authors found a statistically significant difference in change scores (baseline to two weeks) (MD 0.30, 95% CI 0.01 to 0.59) (Analysis 16.2), favouring the extended duration dressing.
Ritting 2012 reported an overall BCTQ, and results of the Symptom Severity Score subscale were not available for further analysis.
-
Change in CTS‐related impairment measures (based on grip and pinch strength).
Measured in Ritting 2012 but not in Williams 2008.
Ritting 2012 examined differences in grip strength and pinch strength (tip pinch, three‐point pinch and lateral pinch) between groups at two weeks and at six to 12 weeks post surgery. Grip strength was statistically significantly better in the group in which the postoperative dressing had been removed earlier (MD ‐16.00, 95% CI ‐21.57 to ‐10.43; Analysis 16.3). Investigators found no statistically significant differences in three‐point pinch or lateral pinch but reported a small statistically significant difference favouring the short dressing group for tip pinch (MD ‐1.20, 95% CI ‐2.35 to ‐0.05) (Analysis 16.4).
-
Presence of iatrogenic symptoms secondary to CTR surgery (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Measured in both Ritting 2012 and Williams 2008.
Wound healing based on a qualitative assessment describing the status of the wound (pristine, erythema, dehiscence or drainage) as reported in Ritting 2012. Study authors reported no complications in either group at the final postoperative evaluation in Ritting 2012. One participant in the longer duration dressing group had slight wound dehiscence at the two‐week visit, which resolved later with wound care. No complications (including infection and wound status) during the two weeks after surgery were reported in either group in Williams 2008.
-
Return to work or occupation (measured as `yes' or `no') at three months.
Not reported.
-
Change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation.
Not reported in Ritting 2012 nor in Williams 2008. Complications were reported as iatrogenic symptoms resulting from surgery rather than from the interventions.
16.1. Analysis.

Comparison 16 Short duration dressing versus extended duration dressing, Outcome 1 Short‐term improvement in functional ability (BCTQ Functional Status Score).
16.2. Analysis.

Comparison 16 Short duration dressing versus extended duration dressing, Outcome 2 Change in CTS symptoms (BCTQ Symptom Severity Score).
16.3. Analysis.

Comparison 16 Short duration dressing versus extended duration dressing, Outcome 3 Change in impairment measure (grip strength).
16.4. Analysis.

Comparison 16 Short duration dressing versus extended duration dressing, Outcome 4 Change in impairment measure (pinch strength).
Sensory relearning home programme (single intervention) versus no treatment (control)
One trial randomising 31 participants to examine the effects of a four‐week sensory relearning programme compared with no treatment (Jerosch‐Herold 2012). The sensory relearning programme was developed specifically for the trial and included techniques for retraining discriminative functional sensibility. Participants were provided with a standard set of materials and instructions, which could be tailored according to their level of sensory impairment, and were instructed to practice the programme for five to 10 minutes, three times daily. Outcomes were measured at four and eight weeks post randomisation and included sensory impairment (Weinstein Enhanced Sensory Test (WEST), static two‐point discrimination and Shape Texture Identification (STI) test), dexterity (Moberg pick‐up test) and DASH questionnaire results.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Not reported.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Short‐term change in functional ability was measured in Jerosch‐Herold 2012 on the DASH questionnaire. Investigators reported no significant differences between groups; adjusted mean difference (given baseline scores and age) was 3.96 (95% CI ‐5.38 to 13.3) at four weeks and 1.17 (95% CI ‐10.19 to 12.53) at eight weeks.
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
-
Jerosch‐Herold 2012 used various outcome measures to examine CTS clinical symptoms.
Weinstein Enhanced Sensory Test (WEST).
Static two‐point discrimination according to Moberg.
Shape Texture Indentification (STI) test.
Results indicated that the mean unadjusted difference at four weeks was 0.3 (95% CI ‐1.41 to 0.75) for the WEST; ‐0.50 (95% CI ‐1.59 to 0.58) for the Moberg two‐point discrimination test; and 0.89 (95% CI ‐0.36 to 2.14) for the STI test. At eight weeks, the mean unadjusted difference was 0.10 (95% CI ‐0.38 to 0.59) for the WEST; 0.16 (95% CI ‐1.76 to 2.07) for the Moberg; and 1.37 (95% CI 0.18 to 2.57) for the STI test.
-
-
Change in CTS‐related impairment measures (based on grip and pinch strength).
Not reported.
-
Presence of iatrogenic symptoms secondary to CTR surgery (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Not reported.
-
Return to work or occupation (measured as `yes' or `no') at three months.
Not reported.
-
Change in neurophysiological parameters (on nerve conduction studies).
Not reported.
-
Presence of adverse events resulting from rehabilitation.
Not reported.
Continuous ultrasound plus nerve and tendon gliding exercises (multiple interventions) versus laser therapy plus nerve and tendon gliding exercises (multiple interventions) versus nerve and tendon gliding exercises (multiple interventions)
One trial investigated the effectiveness of continuous ultrasound plus nerve and tendon gliding exercises versus laser therapy plus nerve and tendon gliding exercises versus nerve and tendon gliding exercises alone (Sawan 2013). A total of 45 participants were randomised to one of the six‐week programmes. Outcomes were assessed at 10 weeks following randomisation (i.e. four weeks after cessation of the interventions). Outcome measures included pain, pinch strength and motor and sensory distal latency of the median nerve assessed on an electromyography (EMG) machine.
Primary outcomes
-
Long‐term change in self reported functional ability as measured on a continuous scale at three months or more.
Not reported.
Secondary outcomes
-
Short‐term change in self reported functional ability as measured on a continuous scale at less than three months.
Not reported.
-
Change in CTS clinical symptoms as measured on a continuous scale (e.g. pain, numbness, and paraesthesia).
Pain was measured on a visual analogue scale. Investigators found a significant improvement in pain in all three groups between baseline and evaluation at 10 weeks. Additionally they found a significant difference in favour of the ultrasound group compared with the exercise groups (MD 1.8, P < 0.01) and in favour of the laser group over the exercise groups (MD 1.2, P < 0.05). However, study authors described no significant difference between ultrasound and laser groups (MD 0.6, P > 0.05).
-
Change in CTS‐related impairment measures (based on grip and pinch strength).
Pinch strength was measured in Sawan 2013. Investigators reported significant improvement in all three groups between baseline and evaluation at 10 weeks and no significant differences between ultrasound and laser groups post treatment. A significant difference favoured the ultrasound group over the laser group at 19 weeks (MD 4, P < 0.01). However, trial authors described no significant differences between laser and exercise groups.
-
Presence of iatrogenic symptoms secondary to CTR surgery (e.g. swelling, scar pain, excessive scarring, and pillar pain).
Not reported.
-
Return to work or occupation (measured as `yes' or `no') at three months.
Not reported.
-
Change in neurophysiological parameters (on nerve conduction studies).
Motor and sensory distal latency of the median nerve was measured in Sawan 2013. Study authors described significant improvement in all groups when baseline scores were compared with scores obtained at 10 weeks. Investigators reported no significant differences at 10 weeks between ultrasound and laser groups but significant differences in favour of the ultrasound group over the exercise group at 10 weeks (MD 0.94, P < 0.01) and in favour of the laser group over the exercise group (MD 0.84, P < 0.05).
-
Presence of adverse events resulting from rehabilitation.
Not reported.
Subgroup and sensitivity analyses
We could not perform subgroup analyses in this review. Clinical heterogeneity of interventions and outcomes or paucity of specified subgroups distinguished by trialists meant that these analyses were not possible. Furthermore, sensitivity analyses were not performed, as no meta‐analyses were conducted.
Discussion
Summary of main results
The objective of this systematic review was to determine the effectiveness and safety of various rehabilitation treatments to optimise outcomes following carpal tunnel release (CTR) compared with no treatment, placebo, or another non‐surgical intervention. We included 22 studies investigating a total of 1521 participants. Included studies showed that currently limited and low to very‐low quality evidence is available to support the use of a variety of rehabilitation treatments after CTR. These studies were heterogeneous in types of rehabilitation treatment provided; intensity, dosage and duration of treatment; timing of treatment; outcome assessment; and treatment setting. Therefore, we could not pool data across studies.
Among the quality issues of these studies, unit of analysis errors are important. Jeffrey 2002 avoided a unit of analysis error; Finsen 1999, Martins 2006 and Provinciali 2000 committed such errors; and whether such errors occurred was unclear in Bury 1995, Bhatia 2000 and Li 2008. Therefore, clinicians and researchers must interpret the results of these studies with caution.
One study compared multiple treatments to a control (Li 2008); six studies compared one rehabilitation treatment to no treatment (Fagan 2004; Gordon 2010; Jerosch‐Herold 2012; Li 2008; Pomerance 2007; Powell 2003); three studies compared one rehabilitation treatment to placebo (Alves 2011; Jeffrey 2002; Stevinson 2003); and 15 studies compared one rehabilitation treatment to other rehabilitation treatments (Bhatia 2000; Bury 1995; Cebesoy 2007; Cook 1995; Finsen 1999; Hochberg 2001; Huemer 2007; Janssen 2009; Li 2008; Martins 2006; Provinciali 2000; Ritting 2012; Sawan 2013; Stevinson 2003; Williams 2008).
Only four studies reported the primary outcome of interest, that is, long‐term self reported functional ability at three months or more (Cebesoy 2007; Gordon 2010; Pomerance 2007; Powell 2003). Only three of these trials reported outcome data suitable for inclusion in this review (Cebesoy 2007; Pomerance 2007; Powell 2003). One high‐quality trial with a small sample size found no statistically significant effect on the Boston Carpal Tunnel Questionnaire (BCTQ) of a desensitisation programme over standard treatment (Powell 2003). One low‐quality trial assessed 150 participants at six months post surgery using the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire and found no statistically significant difference in scores between the no therapy group (instructed preoperatively on tendon gliding exercises, scar massage and return to activity) and a group given a two‐week course of multi‐modal therapy commenced at five to seven days post surgery (Pomerance 2007). However, this study included only employed persons, which limits the generalisability of findings to non‐employed or retired people. One very low‐quality quasi‐randomised trial found that participants who received a bulky dressing and commenced early mobilisation showed no statistically significant difference in function on BCTQ at three months post surgery when compared with participants who received a postoperative wrist orthosis at three months post surgery (Cebesoy 2007).
Two low‐quality trials compared immobilisation using a wrist orthosis to a bulky dressing and mobilisation (Bhatia 2000; Bury 1995). Both reported incomplete data and limited data on measures of variability. Bury 1995 found that improvement in carpal tunnel syndrome (CTS) symptoms among participants who wore a wrist orthosis for two weeks was not statistically significantly different from improvement among those who wore a bulky dressing. Lack of participant blinding in this study means that outcomes should be interpreted with caution, as reporting of participant symptoms may have been influenced by knowledge of the intervention group.
Four trials compared immobilisation of the wrist using an orthosis with a programme of early mobilisation (Cebesoy 2007; Cook 1995; Finsen 1999; Martins 2006). Studies by Cook 1995 and Finsen 1999 provided incomplete data, which limited analysis and reporting of study results. Measures of variability were missing for several outcome measures in each trial, and some outcomes were reported as median values, indicating that data may have been skewed (Finsen 1999). Martins 2006 found no significant differences between the two interventions, which suggests that one intervention is not superior to the other in terms of change in CTS symptom severity and sensibility measured using two‐point discrimination. No significant differences in iatrogenic symptoms secondary to CTR were found between groups in studies by Cook 1995 and Finsen 1999. Only one study reported adverse events related to the intervention (Cebesoy 2007). Cebesoy 2007 reported that 80% of participants in the splinted group experienced discomfort compared to none in the mobilisation group, which was a statistically significant difference. However, results from these studies should be interpreted with caution as they lacked appropriate randomisation (Cebesoy 2007; Finsen 1999; Martins 2006).
Two randomised controlled trials (RCTs) investigated the use of arnica as an intervention compared with placebo (Jeffrey 2002; Stevinson 2003). Results of Jeffrey 2002 suggested no significant differences in grip strength or swelling after seven days of arnica compared with placebo. Stevinson 2003 found no difference between participants who received high or low doses of oral arnica when compared with those given placebo with respect to bruising of the hand post surgery.
Two trials compared multi‐modal hand therapy or physiotherapy to a non‐graduated home exercise programme (preoperative education regarding tendon gliding exercises, scar management and advice on return to activity) (Pomerance 2007) or a progressive patient‐directed home exercise programme (Provinciali 2000). Provinciali 2000 did not report outcome data in a manner that allowed further analysis. Pomerance 2007 found no significant differences between groups during the short‐term postoperative period or at three months of follow‐up for changes in self reported functional ability and impairment measures based on grip or pinch strength.
We identified two trials that compared short duration postoperative dressing versus extended duration dressing (Ritting 2012; Williams 2008). Williams 2008 found no significant differences between short and longer duration dressings in terms of improved functional status and symptom severity on the BCTQ, and Ritting 2012 found that participants who had their dressing removed early had better grip and pinch strength. However, neither study provided participant blinding. These results should be interpreted with caution as participant assessments of effectiveness may have been influenced by their awareness of the intervention.
One RCT compared continuous ultrasound in conjunction with nerve and tendon gliding exercises versus laser therapy plus nerve and tendon gliding exercises versus nerve and tendon gliding exercises alone (Sawan 2013). This study found significant improvement after treatment in all groups but no significant difference between continuous ultrasound with nerve and tendon gliding exercises, laser therapy with exercises and exercise alone. Investigators found significant differences between the ultrasound and exercise groups and between the laser therapy and exercise groups. However, trialists did not compare these interventions for any of the outcomes included in this review. No participant blinding was provided in this study; therefore, participants' assessment of effectiveness of pain may have been influenced by their knowledge of the intervention to which they were allocated.
We identified one trial that examined a sensory relearning home programme versus no treatment control (Jerosch‐Herold 2012). Trialists found weak evidence supporting use of a sensory relearning programme in a pilot study design. In general, trialists had controlled risks of bias for selection, attrition and reporting. However, participants were not blinded for the duration of the study. Therefore, study results must be considered in the light of the high risk of performance bias.
One moderate‐quality randomised trial found no statistically significant differences in the amount of swelling among participants receiving contrast baths plus exercises compared with those receiving contrast baths alone, although investigators reported statistically significantly more swelling than with exercise alone (Janssen 2009). Further, those receiving contrast baths alone had statistically significantly more swelling than those receiving exercises alone.
We identified one randomised trial that compared effects of controlled cold therapy versus ice therapy commenced immediately post surgery and continued for three days (Hochberg 2001). Results from this trial support the use of controlled cold therapy over ice therapy for both pain and swelling reduction in the short term. However, participants and outcome assessors in this study were not blinded, and this may have influenced their expectations of the effects of interventions.
We identified one quasi‐randomised trial that compared low‐level laser therapy with placebo laser treatment (Alves 2011). Trialists found no statistically significant differences in CTS symptoms with low‐level laser therapy versus placebo and no differences between groups in the return to work outcome at three months post surgery. Results of this trial should be interpreted cautiously as participants were allocated to groups according to a quasi‐random sequence.
Fagan 2004 examined elevation using a home elevation device and a Bradford sling versus standard care. Trialists found no statistically significant differences between groups in terms of pain or swelling.
Trials conducted by Gordon 2010 (electrical stimulation versus control), Huemer 2007 (bulky dressing and splint versus light dressing), and Li 2008 (electrical stimulation versus decimeter wave therapy versus no treatment control) did not report outcome data in a format that was meaningful, or provided incomplete data that could not be analysed.
Overall completeness and applicability of evidence
Evidence in this review is limited in its completeness and applicability. Authors of included studies did not provide important details about the conduct of studies and did not report complete data. Inclusion of a wide variety of rehabilitation treatments in this review made it difficult for review authors to draw conclusions about the overall efficacy of rehabilitation interventions after CTR. In addition, we were not able to include in this review a number of treatments used in rehabilitation (such as ultrasound, scar massage, mobilisation techniques, strengthening, return to work interventions and work modification) because no RCTs had evaluated their efficacy. Moreover, two studies investigated the benefits of a programme of multi‐modal hand therapy, making it difficult to isolate interventions within the multi‐component treatment that could be effective (Pomerance 2007; Provinciali 2000). Several studies did not report demographic data such as gender and age distribution, setting, details of the type of CTS and eligibility criteria; this limits the potential to generalise findings of these studies to a particular population or treatment setting. Only three studies clearly reported results of interventions at three months or longer (Alves 2011; Gordon 2010; Pomerance 2007).
Quality of the evidence
Methodological quality varied greatly across studies. All studies were small, ranging from 21 participants (in Gordon 2010) to a maximum of 150 participants (in Pomerance 2007). Four studies included 100 or more participants who underwent CTR and were randomised (Bhatia 2000; Pomerance 2007; Provinciali 2000; Williams 2008). According to the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach (Schunemann 2011b), the overall quality of evidence was moderate when multi‐modal hand therapy was compared with a control of advice and normal activity and when the primary outcome was reviewed.
Only 13 trials explicitly reported that the sequence was generated in a randomised fashion (Bhatia 2000; Bury 1995; Fagan 2004; Gordon 2010; Hochberg 2001; Janssen 2009; Jerosch‐Herold 2012; Pomerance 2007; Powell 2003; Ritting 2012; Sawan 2013; Stevinson 2003; Williams 2008). Four trials adequately concealed the allocation sequence (Pomerance 2007; Powell 2003; Sawan 2013; Stevinson 2003). This is important as inadequate allocation concealment can lead to distortion of treatment effects (Odgaard‐Jensen 2011).
Few trials were rated as having low risk of performance bias and detection bias for self reported outcomes because of lack of participant and personnel blinding. Only four studies achieved blinding of both participants and outcome assessors (Janssen 2009; Jeffrey 2002; Powell 2003; Stevinson 2003). Lack of blinding of participants is often unavoidable in situations for which the interventions are obvious (e.g. type of dressing or intervention versus lack thereof). Therefore, minimising performance and detection bias is almost impossible. However, this can be problematic as participants in trials with unblinded assessment of subjective outcomes, such as pain and function, are estimated to exaggerate the treatment benefit (Wood 2008). Therefore, these studies need to be interpreted with some caution. In comparison, blinding of outcome assessors is nearly always possible but was not clearly reported in 11 of the 20 studies (Alves 2011; Bhatia 2000; Bury 1995; Cebesoy 2007; Cook 1995; Fagan 2004; Finsen 1999; Gordon 2010; Hochberg 2001; Huemer 2007; Li 2008).
Risk of bias from incomplete outcome data was unclear or high for both short‐term and long‐term data in five studies (Bhatia 2000; Bury 1995; Cook 1995; Finsen 1999; Provinciali 2000), and eight studies had high risk of bias from selective reporting (Bury 1995; Cook 1995; Fagan 2004; Finsen 1999; Gordon 2010; Huemer 2007; Pomerance 2007; Provinciali 2000). Studies with high risk of selective reporting bias are problematic as they can bias results and conclusions of a systematic review (Kirkham 2010).
In general, further research is very likely to have an important impact on our confidence in the estimate of the treatment effect, but this needs to consist of efficacious therapies provided in studies of adequate power, with valid outcomes assessed at appropriate periods of time.
Potential biases in the review process
Although review authors attempted to minimise bias in selection of studies for this review, collection of published data and analysis, our searches were limited to electronic databases and clinical trial registries. We included one unpublished study identified through a clinical trials database (Powell 2003), but we may have missed results of some unpublished studies. Furthermore, it was difficult to obtain all relevant data required for a systematic review from the authors of the included studies, often because of the length of time that had passed since some of the studies were completed. It was also difficult to assess selective outcome reporting for studies for which study protocols or trial registry data were not available or accessible, and for which study authors did not adequately report the methods used.
Agreements and disagreements with other studies or reviews
To our knowledge, only three other systematic reviews have been published in this domain (Huisstede 2010; Isaac 2010; Keilani 2002). Keilani 2002 published a review in German, which reviewed the effects of mobilisation and splinting interventions on symptoms after CTR by reviewing both randomised and non‐randomised studies. This review is awaiting translation. Isaac 2010 reviewed RCTs that compared wrist immobilisation to another intervention or control in studies that included more than 30 participants who had undergone open CTR and were published in English. Isaac 2010 identified articles by Bury 1995, Cebesoy 2007, Cook 1995, Finsen 1999, and Martins 2006. Huisstede 2010 briefly reviewed rehabilitation interventions after CTR as part of a larger review on the effectiveness of CTR, and identified articles by Bury 1995, Cebesoy 2007, Chaise 1994, Cook 1995, Finsen 1999, Hochberg 2001, Huemer 2007, Jeffrey 2002, Martins 2006, Pomerance 2007, Provinciali 2000, and Stevinson 2003. Huisstede 2010 listed the trial by Cook 1995 as providing a preoperative rather than a postoperative intervention and did not make clear why it was classified this way.
Findings of our review are generally consistent with those of Isaac 2010 and Huisstede 2010 in concluding that evidence is limited and insufficient to determine whether immobilisation post CTS surgery has a beneficial effect. However, we believe that this review is the most comprehensive yet, as the review by Isaac 2010 did not include the study by Bhatia 2000, and Huisstede 2010 did not include Fagan 2004, Li 2008 or Williams 2008. It is unclear why the search strategies did not identify these trials.
In addition, since the time these reviews were published, additional trials have been completed (Alves 2011; Alves 2011; Gordon 2010; Jerosch‐Herold 2012; Ritting 2012; Sawan 2013).
Authors' conclusions
Implications for practice.
Limited and very low‐quality evidence is available for rehabilitation treatments following carpal tunnel release (CTR). People who have undergone CTR require sufficient information to make an informed decision about recommended rehabilitation treatments. They need to be informed of the limited evidence of effectiveness and safety of any interventions recommended by the treatment provider. Factors to be considered before treatment providers and those who refer patients for treatment recommend a rehabilitation following surgery for carpal tunnel syndrome (CTS) are the environmental context, the nature of the intervention, and the patient's preference. Benefits of rehabilitation treatments in the short term compared with the long term have not been adequately evaluated.
Implications for research.
Carpal tunnel release surgery is generally successful in reducing symptoms of CTS with few reported adverse events (Vasiliadis 2013; Verdugo 2008). Therefore, studies with large samples and the power to detect statistically significant differences between groups are needed to determine the effects of interventions in improving postoperative outcomes, including function and return to work. The high success rate of surgery may contribute to the lack of high‐quality studies. Second, a wide variety of poor outcomes are possible after surgery, and it can be difficult to design a study to examine multiple outcomes while controlling for various confounding variables. Poor outcomes can result from failure to relieve preexisting symptoms or iatrogenic complications from the surgery itself (e.g. scar pain, hypersensitivity, and reduced grip strength). However, for patients who have persistent symptoms or iatrogenic effects resulting from CTR, research into effects of various rehabilitation modalities remains relevant and necessary.
Therefore, additional high‐quality randomised controlled trials are needed to assess the effectiveness and safety of rehabilitation treatments delivered after CTR. Researchers must consider various issues when designing a study (Peters 2014). Trials should attempt to blind participants and outcome assessors when possible. Trial authors should clearly report demographic details and rehabilitation setting information, so that results can be interpreted and applied to similar populations and settings. In addition, data on adverse effects of the rehabilitation intervention rather than iatrogenic effects of the surgery should be recorded. If participants with bilateral CTS are included in the study, trialists should use appropriate methods and should clearly report how bilateral cases were handled in their statistical analysis to prevent a unit of analysis error. Study authors should place trial information on appropriate clinical trials registers to ensure transparent reporting of methods planned for their study. Moreover, trialists should be careful to include in the study report means and appropriate measures of variability for all outcomes prespecified in their methods, thereby avoiding selective reporting bias. The nature of these interventions and the results reported by trials included in this review show that benefit may be observed for early return to function and return to work that is not observed at three months or later. However, longer‐term effectiveness should not be ignored. Assessment of longer‐term benefit after cessation of the intervention should be incorporated in future research. Researchers should focus on postoperative care regimens that have been designed to reduce the symptoms of CTS. They need to measure the severity and type of CTS symptoms preoperatively and should stratify the patient population accordingly. Additionally, consistent reporting of outcomes (common instruments and timing of outcome assessments) will allow for meta‐analysis of similar outcomes in future reviews. The only consistent effects of treatment involved CTS symptom scores; therefore, these outcomes might be useful to include in future studies. Finally, many commonly used rehabilitation treatments have not yet been evaluated for their effectiveness or safety, and these therapies should be included in future trials.
What's new
| Date | Event | Description |
|---|---|---|
| 29 September 2015 | New search has been performed | Updated version of the review completed |
| 29 September 2015 | New citation required but conclusions have not changed | Searches updated. Two new studies included |
Acknowledgements
We would like to acknowledge Denise O'Connor and Cathy Dabourn, who produced the initial protocol for this review in 2003. We would like to thank Angela Gunn and Ruth Brassington from the Cochrane Neuromuscular Group for assistance in devising the search strategy, performing searches and providing editorial support. We also would like to thank the trialists who provided additional information on the included studies.
We would like to thank the following institutions for support provided during the review.
Brisbane Hand and Upper Limb Research Institute, Brisbane, Australia.
School of Health and Rehabilitation Sciences, The University of Queensland, Brisbane, Australia.
This project was supported by the National Institute for Health Research via Cochrane Infrastructure funding to the Cochrane Neuromuscular Disease Group. The views and opinions expressed herein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health. The Cochrane Neuromuscular Disease Group is also supported by the MRC Centre for Neuromuscular Diseases.
Appendices
Appendix 1. Cochrane Neuromuscular Specialised Register (CRS) search strategy
#1 MeSH DESCRIPTOR Carpal Tunnel Syndrome [REFERENCE] [STANDARD] #2 "carpal tunnel" [REFERENCE] [STANDARD] #3 ("nerve entrapment" or "nerve compression" or "entrapment neuropathy" or "entrapment neuropathies") and carpal [REFERENCE] [STANDARD] #4 #1 or #2 or #3 [REFERENCE] [STANDARD] #5 MeSH DESCRIPTOR Rehabilitation Explode All [REFERENCE] [STANDARD] #6 "postoperative care" [REFERENCE] [STANDARD] #7 MeSH DESCRIPTOR Musculoskeletal Manipulations Explode All [REFERENCE] [STANDARD] #8 MeSH DESCRIPTOR Exercise Movement Techniques Explode All [REFERENCE] [STANDARD] #9 MeSH DESCRIPTOR Physical Therapy Modalities Explode All [REFERENCE] [STANDARD] #10 "Casts, Surgical" [REFERENCE] [STANDARD] #11 ultrasound or scar or rehabilitation or work or "cold therapy" or" ice therapy" or splint* or exercis* or mobili* or educat$ or "activity modification" or ergonomic* [REFERENCE] [STANDARD] #12 immobili* or "hand elevation" or sling or strength* or oedema* or edema* or compress* or massage or gliding or thermotherapy or "physical therapy" or "manual therapy" or "occupational therapy" or osteopath* or chiropract* or postoperative [REFERENCE] [STANDARD] #13 physiotherapy:ab [REFERENCE] [STANDARD] #14 #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 [REFERENCE] [STANDARD] #15 "decompression, surgical" [REFERENCE] [STANDARD] #16 "decompression, surgery" [REFERENCE] [STANDARD] #17 surgical or epineurotomy or reconstruct* or release or decompress* or endoscop* [REFERENCE] [STANDARD] #18 "hand surgery" [REFERENCE] [STANDARD] #19 #15 or #16 or #17 or #18 [REFERENCE] [STANDARD] #20 #4 and #14 and #19 [REFERENCE] [STANDARD] #21 (#4 and #14 and #19) AND (INREGISTER) [REFERENCE] [STANDARD]
Appendix 2. CENTRAL search strategy
#1 "Carpal Tunnel Syndrome" #2 ("nerve entrapment" or "nerve compression" or "entrapment neuropath*") #3 "median nerve entrapment" #4 #1 or #2 or #3 #5 MeSH descriptor: [Rehabilitation] explode all trees #6 MeSH descriptor: [Musculoskeletal Manipulations] explode all trees #7 MeSH descriptor: [Physical Therapy Modalities] explode all trees #8 MeSH descriptor: [Exercise Movement Techniques] explode all trees #9 "postoperative care" or splint or ultrasound or scar or rehabilit* or "cold therapy" or "ice therapy" or exercise or mobili* educat* or "activity modification" or ergonomic* #10 immobili* or "hand elevation" or sling or strength* or oedema or edema or compress* or massage or gliding or thermotherapy or "physical therapy" or physiotherapy or "manual therapy" or "occupational therapy" or osteopath* or chiropract* or postoperative #11 surgical near/2 cast or surgical near/2 casts #12 #5 or #6 or #7 or #8 or #9 or #10 or #11 #13 #4 and #12 #14 "hand surgery" or surgical or epineurotomy or decompress* or reconstruct* or release or endoscop* or octr or ectr #15 #13 and #14
Appendix 3. MEDLINE (OvidSP) search strategy
Database: Ovid MEDLINE(R) <1946 to September Week 3 2015> Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 randomized controlled trial.pt. (410772) 2 controlled clinical trial.pt. (91620) 3 randomized.ab. (303022) 4 placebo.ab. (157349) 5 drug therapy.fs. (1835560) 6 randomly.ab. (214614) 7 trial.ab. (315133) 8 groups.ab. (1353637) 9 or/1‐8 (3461345) 10 exp animals/ not humans.sh. (4115201) 11 9 not 10 (2950677) 12 Carpal Tunnel Syndrome/ (7447) 13 carpal tunnel.mp. (9066) 14 or/12‐13 (9066) 15 exp REHABILITATION/ (160661) 16 rh.fs. (175287) 17 Postoperative Care/ (54102) 18 exp Musculoskeletal Manipulations/ (13154) 19 exp Exercise Movement Techniques/ (5937) 20 exp Physical Therapy Techniques/ (133929) 21 SPLINTS/ (7721) 22 Casts, Surgical/ (7982) 23 (ultrasound or scar$ or rehabilit$ or work or cold therap$ or ice therapy or splint$ or exercis$ or mobili$ or educat$ or activity modification or ergonomic$).mp. (1938764) 24 (immobili$ or hand elevation or sling or strength$ or oedema$ or edema$ or compress$ or massage or gliding or thermotherapy or physical therap$ or physiotherap$ or manual therap$ or occupational therap$ or osteopath$ or chiropract$).mp. (656762) 25 pain, postoperative/ (29532) 26 postoperative.tw. (314517) 27 or/15‐25 (2724506) 28 11 and 14 and 27 (697) 29 Decompression, Surgical/ (11169) 30 microvascular decompression surgery/ (220) 31 (surgical or epineurotomy or reconstruct$ or release or decompress$ or endoscop$).tw. (1370143) 32 hand surgery.mp. (2235) 33 or/29‐32 (1373892) 34 11 and 14 and 27 and 33 (310) 35 remove duplicates from 34 (285)
Appendix 4. EMBASE (OvidSP) search strategy
Database: Embase <1980 to 2015 Week 39> Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 crossover‐procedure.sh. (44496) 2 double‐blind procedure.sh. (123594) 3 single‐blind procedure.sh. (21014) 4 randomized controlled trial.sh. (384091) 5 (random$ or crossover$ or cross over$ or placebo$ or (doubl$ adj blind$) or allocat$).tw,ot. (1186103) 6 trial.ti. (185705) 7 or/1‐6 (1330070) 8 (animal/ or nonhuman/ or animal experiment/) and human/ (1410904) 9 animal/ or nonanimal/ or animal experiment/ (3451083) 10 9 not 8 (2866684) 11 7 not 10 (1222395) 12 limit 11 to embase (1004187) 13 carpal tunnel syndrome/ (11608) 14 carpal tunnel syndrome.mp. (12463) 15 ((nerve entrapment or nerve compression or entrapment neuropath$) and carpal).mp. (2003) 16 or/13‐15 (12593) 17 rehabilitation/ (55900) 18 postoperative care/ (70474) 19 manipulative medicine/ (9011) 20 physiotherapy/ (59859) 21 splint/ (7493) 22 plaster cast/ (7668) 23 postoperative pain/ (45949) 24 (ultrasound or scar$ or rehabilit$ or work or cold therap$ or ice therapy or splint$ or exercis$ or mobili$ or educat$ or activity modification or ergonomic$).mp. (2919974) 25 (immobili$ or hand elevation or sling or strength$ or oedema$ or edema$ or compress$ or massage or gliding or thermotherapy or physical therap$ or physiotherap$ or manual therap$ or occupational therap$ or osteopath$ or chiropract$).mp. (991834) 26 postoperative.tw. (420970) 27 exp "bandages and dressings"/ (37329) 28 or/17‐27 (4117547) 29 12 and 16 and 28 (513) 30 (hand surgery or surgical or epineurotomy or reconstruct$ or release or endoscop$ or octr or ectr).mp. (2294944) 31 exp decompression surgery/ (37019) 32 30 or 31 (2314414) 33 12 and 16 and 28 and 32 (204) 34 remove duplicates from 33 (203)
Appendix 5. CINAHL Plus (EBSCOhost) search strategy
Tuesday, September 29, 2015 11:30:25 AM S32 S30 AND S31 4 S31 EM 20140807‐ 376,609 S30 S18 and S24 and S28 and S29 106 S29 hand surgery or surgical or epineurotomy or reconstruct* or release or endoscop* or octr or ectr 169,119 S28 S25 or S26 or S27 1,074,337 S27 bandage* or dressing* or immobili or hand elevation or sling or strength* or oedema* or edema* or compress* or massage or gliding or thermotherapy or physical therap* or physiotherap* or manual therap* or occupational therap* or osteopath* or chiropract* or postoperative 295,788 S26 ultrasound or scar* or rehabilit* or work or cold therap or ice therapy or splint* or exercis* or mobili* or educat* or activity modification or ergonomic* 868,104 S25 (MH "Manual Therapy+") OR (MH "Massage") OR (MH "Manipulation, Osteopathic") OR (MH "Rehabilitation") OR (MH "Hand Therapy") OR (MH "Physical Therapy") OR (MH "Cryotherapy") 71,670 S24 s19 or s20 or s21 or s22 or s23 2,473 S23 entrapment neuropath* and carpal 56 S22 nerve compression and carpal 183 S21 nerve entrapment and carpal 66 S20 carpal tunnel syndrome 2,459 S19 (MH "Carpal Tunnel Syndrome") 2,181 S18 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 773,607 S17 ABAB design* 94 S16 TI random* or AB random* 155,409 S15 ( TI (cross?over or placebo* or control* or factorial or sham? or dummy) ) or ( AB (cross?over or placebo* or control* or factorial or sham? or dummy) ) 309,105 S14 ( TI (clin* or intervention* or compar* or experiment* or preventive or therapeutic) or AB (clin* or intervention* or compar* or experiment* or preventive or therapeutic) ) and ( TI (trial*) or AB (trial*) ) 109,150 S13 ( TI (meta?analys* or systematic review*) ) or ( AB (meta?analys* or systematic review*) ) 39,963 S12 ( TI (single* or doubl* or tripl* or trebl*) or AB (single* or doubl* or tripl* or trebl*) ) and ( TI (blind* or mask*) or AB (blind* or mask*) ) 24,004 S11 PT ("clinical trial" or "systematic review") 130,582 S10 (MH "Factorial Design") 948 S9 (MH "Concurrent Prospective Studies") or (MH "Prospective Studies") 273,601 S8 (MH "Meta Analysis") 23,244 S7 (MH "Solomon Four‐Group Design") or (MH "Static Group Comparison") 48 S6 (MH "Quasi‐Experimental Studies") 7,527 S5 (MH "Placebos") 9,427 S4 (MH "Double‐Blind Studies") or (MH "Triple‐Blind Studies") 32,595 S3 (MH "Clinical Trials+") 192,364 S2 (MH "Crossover Design") 13,341 S1 (MH "Random Assignment") or (MH "Random Sample") or (MH "Simple Random Sample") or (MH "Stratified Random Sample") or (MH "Systematic Random Sample") 70,494
Appendix 6. AMED (OvidSP) search strategy
Database: AMED (Allied and Complementary Medicine) <1985 to September 2015> Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 Randomized controlled trials/ (1734) 2 Random allocation/ (313) 3 Double blind method/ (555) 4 Single‐Blind Method/ (66) 5 exp Clinical Trials/ (3476) 6 (clin$ adj25 trial$).tw. (6210) 7 ((singl$ or doubl$ or treb$ or trip$) adj25 (blind$ or mask$ or dummy)).tw. (2562) 8 placebos/ (563) 9 placebo$.tw. (2781) 10 random$.tw. (15267) 11 research design/ (1822) 12 Prospective Studies/ (841) 13 meta analysis/ (152) 14 (meta?analys$ or systematic review$).tw. (2646) 15 control$.tw. (31739) 16 (multicenter or multicentre).tw. (881) 17 ((study or studies or design$) adj25 (factorial or prospective or intervention or crossover or cross‐over or quasi‐experiment$)).tw. (11422) 18 or/1‐17 (49153) 19 carpal tunnel syndrome/ or carpal tunnel syndrome.tw. (499) 20 ((nerve entrapment or nerve compression or entrapment neuropath$) and carpal).mp. (55) 21 or/19‐20 (500) 22 rehabilitation/ (47964) 23 postoperative care/ (1401) 24 exp musculoskeletal manipulations/ (5000) 25 physical therapy modalities/ or exp exercise movement techniques/ (4417) 26 exp physical therapy modalities/ (22261) 27 splints/ (122) 28 (ultrasound or scar$ or rehabilit$ or work or cold therap$ or ice therapy or splint$ or exercis$ or mobili$ or educat$ or activity modification or ergonomic$).mp. (97072) 29 (immobili$ or hand elevation or sling or strength$ or oedema$ or edema$ or compress$ or massage or gliding or thermotherapy or physical therap$ or physiotherap$ or manual therap$ or occupational therap$ or osteopath$ or chiropract$).mp. (55957) 30 pain postoperative/ (229) 31 postoperative.tw. (4500) 32 or/22‐31 (133296) 33 (hand surgery or surgical or epineurotomy or reconstruct$ or release or decompress$ or endoscop$ or octr or ectr).mp. (8947) 34 18 and 21 and 32 and 33 (23) 35 remove duplicates from 34 (23)
Appendix 7. LILACS search strategy
(("carpal tunnel syndrome" OR "sindrome del Tunel Carpiano" or "Sindrome do Tunel Carpal" or "Nerve Compression" or "Compresion Nerviosa" or "Compressao Nervosa" or "nerve entrapment" or "entrapment neuropathy") and carpal) and (E02.831$ or Rehabilitation or Rehabilitacion or Reabilitacao or "Postoperative Care" or "Cuidados Postoperatorios" or "Cuidados Pos‐Operatorios" or E02.190.599$ or "Musculoskeletal Manipulations" or "Manipulaciones Musculoesqueleticas" or "Manipulacoes Musculoesqueleticas" or E02.779$ or "Physical Therapy Modalities" or "Modalidades de Fisioterapia" or Splint$ or Ferula$ or Contencoe$ or "Casts, Surgical" or "Moldes Quirurgicos" or "Moldes Cirurgicos" or ultrasound or scar$ or rehabilit$ or work or "cold therapy" or "ice therapy" or Cryotherapy or Crioterapia or Crioterapia or exercis$ or mobili$ or educat$ or "activity modification" or ergonomic$ or immobili$ or "hand elevation" or sling or strength$ or oedema$ or edema$ or compress$ or massage or gliding or thermotherapy or" physical therapy" or physiotherap$ or "manual therapy" or "occupational therapy" or "Terapia Ocupacional" or osteopath$ or chiropract$ or Postoperative or Postoperatorio or Pos‐Operatória) and ("Decompression, Surgical" or "Descompresion Quirurgica" or "Descompressao Cirurgica" or surgical or epineurotomy or reconstruct$ or release or decompress$ or endoscop$ or "hand surgery") and ((PT:"Randomized Controlled Trial" or "Randomized Controlled trial" or "Ensayo Clínico Controlado Aleatorio" or "Ensaio Clínico Controlado Aleatório" or PT:"Controlled Clinical Trial" or "Ensayo Clínico Controlado" or "Ensaio Clínico Controlado" or "Random allocation" or "Distribución Aleatoria" or "Distribuição Aleatória" or randon$ or Randomized or randomly or "double blind" or "duplo‐cego" or "duplo‐cego" or "single blind" or "simples‐cego" or "simples cego" or placebo$ or trial or groups) AND NOT (B01.050$ AND NOT (humans or humanos or humanos)))
Appendix 8. PsycINFO (OvidSP) search strategy
Database: PsycINFO <1806 to September Week 4 2015> Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 (random$ or rct or cct or factorial$ or crossover$ or cross over$ or cross‐over$ or placebo$ or (doubl$ adj blind$) or (singl$ adj blind$) or assign$ or allocat$ or volunteer$).tw. (271953) 2 carpal tunnel syndrome.mp. (317) 3 (ultrasound or scar$ or rehabilit$ or work or cold therap$ or ice therapy or splint$ or exercis$ or mobili$ or educat$ or activity modification or ergonomic$).mp. (946110) 4 (immobili$ or hand elevation or sling or strength$ or oedema$ or edema$ or compress$ or massage or gliding or thermotherapy or physical therap$ or physiotherap$ or manual therap$ or occupational therap$ or osteopath$ or chiropract$).mp. (124593) 5 (postoperative care or manipulation or splint$1).mp. (21704) 6 or/3‐5 (1048351) 7 (decompression or surgical or epineurotomy or reconstruct$ or release or decompress$ or endoscop$ or octr or ectr).mp. (63635) 8 1 and 2 and 6 and 7 (3)
Appendix 9. PEDRO search strategy
#1 "Carpal Tunnel"
Appendix 10. Clinical trials registers searches
#1 "Carpal Tunnel"
Appendix 11. Glossary
Bowstringing of the tendons ‐ tendon takes the shortest route across the wrist joint
Cryotherapy ‐ therapeutic intervention using ice
Double crush syndrome ‐ compression of a nerve at more than one site (e.g. at the neck and the wrist)
Epineurotonomy ‐ division of a thickened nerve sheath or epineurium
Iatrogenic symptoms ‐ inadvertent adverse complications resulting from medical treatment
Internal neurolysis ‐ removal of scar tissue from the nerve
Palmar arch injury ‐ injury to an artery in the hand
Paraesthesia ‐ sensation of tingling or burning
Pillar pain ‐ tenderness at the base of the palm superficial to the carpal tunnel
Synovectomy ‐ surgical removal of a part of the synovial membrane (lining) of a joint
Data and analyses
Comparison 1. Low‐level laser versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in CTS symptoms (night‐time pain) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 At 1 month post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 At 2 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 At 3 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.4 At 6 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Change in CTS symptoms (palmar pain) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 At 1 month post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.34, 1.54] |
| 2.2 At 2 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.02, 1.30] |
| 2.3 At 3 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.86] |
| 2.4 At 6 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 15.24] |
| 3 Change in CTS symptoms (numbness) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 At 1 month post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.11, 1.27] |
| 3.2 At 2 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.08 [0.00, 1.31] |
| 3.3 At 3 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.65] |
| 3.4 At 6 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.2 [0.01, 3.99] |
| 4 Change in CTS symptoms (paraesthesia) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 At 1 month post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.11, 1.27] |
| 4.2 At 2 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.08 [0.00, 1.31] |
| 4.3 At 3 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.65] |
| 4.4 At 6 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.2 [0.01, 3.99] |
| 5 Number with CTS clinical signs (Durkan's, Tinel's, Phalen's tests, numbness, paraesthesia, nighttime pain) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 At 1 month post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [0.33, 27.18] |
| 5.2 At 2 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.65] |
| 5.3 At 3 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.4 At 6 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Iatrogenic symptoms (scar pain) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 At 1 month post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.30, 1.06] |
| 6.2 At 2 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.14, 1.81] |
| 6.3 At 3 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 3.02] |
| 6.4 At 6 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.86] |
| 7 Iatrogenic symptoms (pillar pain) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 At 1 month post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [0.53, 3.36] |
| 7.2 At 2 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.19, 1.74] |
| 7.3 At 3 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.21, 2.12] |
| 7.4 At 6 months post surgery | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.86] |
| 8 Return to ADL or work (6 months) | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.94, 1.07] |
| 9 Adverse events (surgery) | 1 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Immobilisation (wrist splint) versus mobilisation (bulky dressing).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in CTS symptoms (participant report of being symptom free) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 At a mean of 6 months of follow‐up | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.52, 1.70] |
| 2 Long‐term change in CTS symptoms (number of participants who reported being 'improved' or 'cured') | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 At a mean of 6 months of follow‐up | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.76, 1.06] |
| 3 Return to normal occupations | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.62, 1.11] |
| 3.1 At a mean of 5.7 months of follow‐up | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.62, 1.11] |
| 4 Adverse effects | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.01, 5.16] |
Comparison 3. Immobilisation (plaster of Paris splint) versus bulky dressing and mobilisation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Long‐term improvement in functional ability (BCTQ Functional Status Score) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 At 3 months | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.39 [‐0.45, 1.23] |
| 2 Short‐term improvement in functional ability (BCTQ Functional Status Score) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 At 1 month | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐0.95, 2.15] |
| 3 Change in CTS symptoms (BCTQ Symptom Severity Score) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 At 2 weeks post surgery | 1 | 52 | Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐3.49, 1.59] |
| 3.2 Change score between baseline and 2 weeks | 1 | 52 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.04, 0.10] |
| 3.3 At 1 month post surgery | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐1.53, 0.85] |
| 3.4 At 3 months post surgery | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 1.60 [‐0.12, 3.32] |
| 4 Change in CTS symptoms (Symptom Intensity Score) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 At 2 weeks post surgery | 1 | 52 | Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐1.68, 0.14] |
| 5 Change score between baseline and 2 weeks (Symptom Intensity Score) | 1 | 52 | Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.01, 0.23] |
| 6 Change in impairment (sensibility measured using static two‐point discrimination) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 At 2 weeks post surgery | 1 | 52 | Mean Difference (IV, Random, 95% CI) | ‐1.43 [‐2.50, ‐0.36] |
| 7 Change score between baseline and 2 weeks (Discrimination Index) | 1 | 52 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.17, 0.13] |
| 8 Iatrogenic symptoms | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Scar tenderness at 1 month post surgery | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.90, 3.42] |
| 8.2 Pillar pain at 1 month post surgery | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 2.4 [0.99, 5.81] |
| 8.3 Scar discomfort/pain at 6 weeks | 1 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.59, 1.54] |
| 8.4 Hypothenar pain at 6 weeks | 1 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.39, 3.99] |
| 8.5 Thenar pain at 6 weeks | 1 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 2.5 [0.24, 26.48] |
| 8.6 Scar discomfort/pain at 6 months | 1 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.42, 3.38] |
| 8.7 Hypothenar pain at 6 months | 1 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 3.57 [0.39, 32.87] |
| 8.8 Thenar pain at 6 months | 1 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.08, 18.36] |
| 9 Adverse event | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1 Discomfort or heavy feeling caused by intervention | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 33.0 [2.11, 515.02] |
| 9.2 Bowstringing of flexor tendons | 2 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 Wound dehiscence | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 4. Specialised home elevation device versus standard sling.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term improvement in CTS symptoms (VAS pain 0 to 10) (3 months or less) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 At the end of 5 days of treatment | 1 | 41 | Mean Difference (IV, Random, 95% CI) | ‐0.5 [‐1.36, 0.36] |
| 2 Iatrogenic symptoms (swelling) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 At the end of 5 days of treatment | 1 | 41 | Mean Difference (IV, Random, 95% CI) | 4.0 [‐40.27, 48.27] |
Comparison 5. Controlled cold therapy versus ice therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term improvement in CTS symptoms (VAS pain 0 to 10) (3 months or less) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 At the end of 3 days of treatment (per protocol analysis) | 1 | 44 | Mean Difference (IV, Random, 95% CI) | ‐2.8 [‐4.50, ‐1.10] |
| 1.2 At the end of 3 days of treatment (intention‐to‐treat analysis) | 1 | 65 | Mean Difference (IV, Random, 95% CI) | ‐1.90 [‐3.51, ‐0.29] |
| 1.3 Change from baseline to day 3 (per protocol analysis) | 1 | 42 | Mean Difference (IV, Random, 95% CI) | ‐2.8 [‐4.88, ‐0.72] |
| 1.4 Change from baseline to day 3 (intention‐to‐treat analysis) | 1 | 63 | Mean Difference (IV, Random, 95% CI) | ‐1.40 [‐3.24, 0.44] |
| 2 Iatrogenic symptoms (swelling) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 At the end of 3 days of treatment (per protocol analysis) | 1 | 48 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐1.02, 1.02] |
| 2.2 At the end of 3 days of treatment (intention‐to‐treat analysis) | 1 | 72 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐1.21, 0.41] |
| 2.3 Change from baseline to day 3 (per protocol analysis) | 1 | 47 | Mean Difference (IV, Random, 95% CI) | ‐1.0 [‐1.26, ‐0.74] |
| 2.4 Change from baseline to day 3 (intention‐to‐treat analysis) | 1 | 71 | Mean Difference (IV, Random, 95% CI) | ‐1.1 [‐1.33, ‐0.87] |
Comparison 6. Bulky dressing plus splint versus light dressing.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Iatrogenic symptom (scar pain) | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 5.0 [0.25, 99.16] |
| 2 Adverse event (median nerve, digital nerve, vascular, tendon complications, delayed wound healing) | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
6.2. Analysis.

Comparison 6 Bulky dressing plus splint versus light dressing, Outcome 2 Adverse event (median nerve, digital nerve, vascular, tendon complications, delayed wound healing).
Comparison 7. Contrast bath plus exercise versus contrast bath.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Iatrogenic symptom (swelling) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Post treatment | 1 | 42 | Mean Difference (IV, Random, 95% CI) | ‐8.80 [‐22.23, 4.63] |
Comparison 8. Contrast bath plus exercises versus exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Iatrogenic symptom (swelling) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Post treatment | 1 | 33 | Mean Difference (IV, Random, 95% CI) | 23.20 [3.60, 42.80] |
Comparison 9. Contrast bath versus exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Iatrogenic symptom (swelling) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Post treatment | 1 | 37 | Mean Difference (IV, Random, 95% CI) | 32.0 [12.61, 51.39] |
Comparison 10. Arnica versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in impairment measure (grip strength) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 At 1 week post surgery | 1 | 74 | Mean Difference (IV, Random, 95% CI) | 11.40 [‐3.78, 26.58] |
| 1.2 At 2 weeks post surgery | 1 | 74 | Mean Difference (IV, Random, 95% CI) | 5.40 [‐18.63, 29.43] |
| 2 Iatrogenic symptom (swelling; % wrist circumference change difference) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 At 1 week post surgery | 1 | 74 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.53, 0.93] |
| 2.2 At 2 weeks post surgery | 1 | 74 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.34, 0.74] |
Comparison 11. High‐dose arnica oral tablets versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Iatrogenic symptoms (number of participants with no clinician‐rated bruising) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 At 4 days | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.83 [0.50, 6.71] |
| 1.2 At 9 days | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.43, 4.42] |
| 1.3 At 14 days | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.1 [0.42, 2.86] |
| 2 Adverse effects | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Arnica 30C | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.23, 4.37] |
Comparison 12. Low‐dose arnica tablets versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Iatrogenic symptoms (number of participants with no clinician‐rated bruising) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 At 4 days | 1 | 42 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [0.50, 6.71] |
| 1.2 At 9 days | 1 | 42 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.21, 3.24] |
| 1.3 At 14 days | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.22, 2.01] |
| 2 Adverse events | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.12, 3.57] |
Comparison 13. High‐dose versus low‐dose oral arnica tablets.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Iatrogenic symptoms (number of participants with no clinician‐rated bruising) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 At 4 days | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.34, 2.93] |
| 1.2 At 9 days | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [0.46, 6.06] |
| 1.3 At 14 days | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.5 [0.50, 4.52] |
| 2 Adverse events | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.28, 8.04] |
Comparison 14. Multi‐modal hand therapy versus normal activities/exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Long‐term improvement in functional ability (DASH) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 DASH at 6 months post surgery | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐4.44, 6.44] |
| 2 Change in impairment measure (grip strength) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 At the end of 2 weeks of treatment (2 weeks post surgery) | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐4.00, 2.60] |
| 2.2 2 weeks after treatment completion (4 weeks post surgery) | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐2.83, 3.23] |
| 2.3 4 weeks after treatment completion (6 weeks post surgery) | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐2.81, 3.01] |
| 2.4 10 weeks after treatment completion (12 weeks post surgery) | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐3.43, 2.23] |
| 2.5 6 months post surgery | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐3.59, 2.79] |
| 3 Change in impairment measure (lateral pinch strength) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 At the end of 2 weeks of treatment (2 weeks post surgery) | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐1.42, 0.02] |
| 3.2 2 weeks after treatment completion (4 weeks post surgery) | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.67, 0.67] |
| 3.3 4 weeks after treatment completion (6 weeks post surgery) | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.89, 0.69] |
| 3.4 10 weeks after treatment completion (12 weeks post surgery) | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.97, 0.57] |
| 3.5 6 months post surgery | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.94, 0.54] |
| 4 Return to normal occupations | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 At treatment completion (2 weeks post surgery) | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.78, 1.18] |
| 4.2 4 weeks after treatment completion (6 weeks post surgery) | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.89, 1.17] |
| 4.3 6 weeks after treatment completion (8 weeks post surgery) | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.97, 1.12] |
| 5 Adverse effects | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.05, 5.69] |
Comparison 15. Desensitisation therapy (as part of multiple interventions) versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Long‐term improvement in functional ability (BCTQ Functional Status Score) | 1 | 27 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.39, 0.33] |
| 1.1 At 12 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.39, 0.33] |
| 2 Short‐term improvement in functional ability (BCTQ Functional Status Score) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 At 3 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.76, 0.16] |
| 2.2 At 6 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.35, 0.39] |
| 3 Change in CTS symptoms (pain or discomfort) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 At 3 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | ‐13.30 [‐27.29, 0.69] |
| 3.2 At 6 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | ‐9.40 [‐23.87, 5.07] |
| 3.3 At 12 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | 4.9 [‐14.69, 24.49] |
| 4 Change in impairment measure (grip strength) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 At 3 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | 0.41 [‐3.95, 4.77] |
| 4.2 At 6 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | 1.80 [‐4.01, 7.61] |
| 4.3 At 12 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐7.38, 5.78] |
| 5 Iatrogenic symptoms (scar sensitivity assessed by dolorimetry) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 At 3 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | 0.26 [‐0.30, 0.82] |
| 5.2 At 6 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.49, 0.81] |
| 5.3 At 12 weeks post surgery | 1 | 27 | Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.46, 0.12] |
| 6 Adverse events (wound dehiscence) | 1 | 27 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
15.6. Analysis.

Comparison 15 Desensitisation therapy (as part of multiple interventions) versus no treatment, Outcome 6 Adverse events (wound dehiscence).
Comparison 16. Short duration dressing versus extended duration dressing.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term improvement in functional ability (BCTQ Functional Status Score) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 At 2 weeks post surgery | 1 | 100 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.25, 0.45] |
| 1.2 Change in Functional Status Score baseline to 2 weeks | 1 | 100 | Mean Difference (IV, Random, 95% CI) | 0.40 [0.05, 0.75] |
| 2 Change in CTS symptoms (BCTQ Symptom Severity Score) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 At 2 weeks | 1 | 100 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.26, 0.26] |
| 2.2 Change in Symptom Severity Score baseline to 2 weeks | 1 | 100 | Mean Difference (IV, Random, 95% CI) | 0.30 [0.01, 0.59] |
| 3 Change in impairment measure (grip strength) | 1 | 66 | Mean Difference (IV, Random, 95% CI) | ‐16.0 [‐21.57, ‐10.43] |
| 3.1 At 6 to 12 weeks | 1 | 66 | Mean Difference (IV, Random, 95% CI) | ‐16.0 [‐21.57, ‐10.43] |
| 4 Change in impairment measure (pinch strength) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Tip pinch 6 to 12 weeks | 1 | 66 | Mean Difference (IV, Random, 95% CI) | ‐1.20 [‐2.35, ‐0.05] |
| 4.2 3‐point pinch at 6 to 12 weeks | 1 | 66 | Mean Difference (IV, Random, 95% CI) | ‐1.10 [‐2.28, 0.08] |
| 4.3 Lateral pinch at 6 to 12 weeks | 1 | 66 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐1.88, 0.48] |
| 5 Adverse event | 2 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
16.5. Analysis.

Comparison 16 Short duration dressing versus extended duration dressing, Outcome 5 Adverse event.
Comparison 17. Sensory retraining programme versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in CTS symptoms (WEST) | 1 | 52 | Mean Difference (IV, Random, 95% CI) | 0.47 [0.13, 0.80] |
| 1.1 At 4 weeks | 1 | 26 | Mean Difference (IV, Random, 95% CI) | 0.54 [0.09, 0.99] |
| 1.2 At 8 weeks | 1 | 26 | Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.14, 0.88] |
| 2 Change in CTS symptoms (2‐point discrimination) | 1 | 52 | Mean Difference (IV, Random, 95% CI) | ‐2.31 [‐3.73, ‐0.90] |
| 2.1 At 4 weeks | 1 | 26 | Mean Difference (IV, Random, 95% CI) | ‐2.39 [‐4.13, ‐0.65] |
| 2.2 At 8 weeks | 1 | 26 | Mean Difference (IV, Random, 95% CI) | ‐2.17 [‐4.59, 0.25] |
| 3 Change in CTS symptoms (STI) | 1 | 52 | Mean Difference (IV, Random, 95% CI) | 1.78 [0.88, 2.68] |
| 3.1 At 4 weeks | 1 | 26 | Mean Difference (IV, Random, 95% CI) | 1.61 [0.32, 2.90] |
| 3.2 At 8 weeks | 1 | 26 | Mean Difference (IV, Random, 95% CI) | 1.94 [0.68, 3.20] |
| 4 Change in CTS symptoms (locognosia) | 1 | 52 | Mean Difference (IV, Random, 95% CI) | 6.04 [2.19, 9.89] |
| 4.1 At 4 weeks | 1 | 26 | Mean Difference (IV, Random, 95% CI) | 5.70 [‐0.07, 11.47] |
| 4.2 At 8 weeks | 1 | 26 | Mean Difference (IV, Random, 95% CI) | 6.31 [1.14, 11.48] |
| 5 Short‐term improvement in functional ability (DASH) | 1 | 52 | Mean Difference (IV, Random, 95% CI) | ‐9.96 [‐22.07, 2.16] |
| 5.1 At 4 weeks | 1 | 26 | Mean Difference (IV, Random, 95% CI) | ‐7.58 [‐23.92, 8.76] |
| 5.2 At 8 weeks | 1 | 26 | Mean Difference (IV, Random, 95% CI) | ‐12.86 [‐30.91, 5.19] |
17.1. Analysis.

Comparison 17 Sensory retraining programme versus control, Outcome 1 Change in CTS symptoms (WEST).
17.2. Analysis.

Comparison 17 Sensory retraining programme versus control, Outcome 2 Change in CTS symptoms (2‐point discrimination).
17.3. Analysis.

Comparison 17 Sensory retraining programme versus control, Outcome 3 Change in CTS symptoms (STI).
17.4. Analysis.

Comparison 17 Sensory retraining programme versus control, Outcome 4 Change in CTS symptoms (locognosia).
17.5. Analysis.

Comparison 17 Sensory retraining programme versus control, Outcome 5 Short‐term improvement in functional ability (DASH).
Comparison 18. Continuous ultrasound plus exercises versus laser therapy plus exercises.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in impairment (pinch strength) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | 1.40 [0.23, 2.57] |
| 2 Change in CTS symptoms (pain VAS) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.05, ‐0.15] |
| 3 Change in neurophysiological parameters (motor distal latency) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.43, 0.23] |
| 4 Change in neurophysiological parameters (sensory distal latency) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.31, 0.51] |
18.1. Analysis.

Comparison 18 Continuous ultrasound plus exercises versus laser therapy plus exercises, Outcome 1 Change in impairment (pinch strength).
18.2. Analysis.

Comparison 18 Continuous ultrasound plus exercises versus laser therapy plus exercises, Outcome 2 Change in CTS symptoms (pain VAS).
18.3. Analysis.

Comparison 18 Continuous ultrasound plus exercises versus laser therapy plus exercises, Outcome 3 Change in neurophysiological parameters (motor distal latency).
18.4. Analysis.

Comparison 18 Continuous ultrasound plus exercises versus laser therapy plus exercises, Outcome 4 Change in neurophysiological parameters (sensory distal latency).
Comparison 19. Continuous ultrasound plus exercises versus exercises alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in impairment (pinch strength) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | 4.0 [3.14, 4.86] |
| 2 Change in CTS symptoms (pain VAS) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐1.80 [‐2.30, ‐1.30] |
| 3 Change in neurophysiological parameters (motor distal latency) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.42, ‐0.46] |
| 4 Change in neurophysiological parameters (sensory distal latency) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.85, 0.13] |
19.1. Analysis.

Comparison 19 Continuous ultrasound plus exercises versus exercises alone, Outcome 1 Change in impairment (pinch strength).
19.2. Analysis.
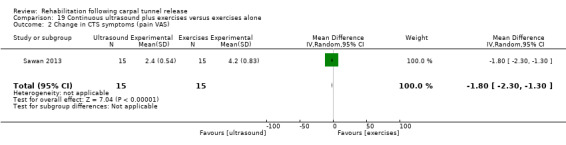
Comparison 19 Continuous ultrasound plus exercises versus exercises alone, Outcome 2 Change in CTS symptoms (pain VAS).
19.3. Analysis.

Comparison 19 Continuous ultrasound plus exercises versus exercises alone, Outcome 3 Change in neurophysiological parameters (motor distal latency).
19.4. Analysis.

Comparison 19 Continuous ultrasound plus exercises versus exercises alone, Outcome 4 Change in neurophysiological parameters (sensory distal latency).
Comparison 20. Laser therapy plus exercises versus exercises alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in impairment (pinch strength) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | 2.60 [1.49, 3.71] |
| 2 Change in CTS symptoms (pain VAS) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐1.20 [‐1.75, ‐0.65] |
| 3 Change in neurophysiological parameters (motor distal latency) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐0.84 [‐1.36, ‐0.32] |
| 4 Change in neurophysiological parameters (sensory distal latency) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.86, ‐0.06] |
20.1. Analysis.

Comparison 20 Laser therapy plus exercises versus exercises alone, Outcome 1 Change in impairment (pinch strength).
20.2. Analysis.

Comparison 20 Laser therapy plus exercises versus exercises alone, Outcome 2 Change in CTS symptoms (pain VAS).
20.3. Analysis.

Comparison 20 Laser therapy plus exercises versus exercises alone, Outcome 3 Change in neurophysiological parameters (motor distal latency).
20.4. Analysis.

Comparison 20 Laser therapy plus exercises versus exercises alone, Outcome 4 Change in neurophysiological parameters (sensory distal latency).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alves 2011.
| Methods | Single‐blind RCT Participant blinding |
|
| Participants |
Details of sampling framea,b Total n eligible = not reported Total n excluded pre‐randomisation = not reported Total n randomised = 58 participants (58 wrists) Total n available for follow‐up = 58 participants (58 wrists) Total n analysed = 58 participants (58 wrists) Intervention group n = 29 participants (29 wrists) Placebo group n = 29 participants (29 wrists) Gender distribution Intervention group: 8 males; 21 females Placebo group: 4 males; 25 females Mean ± SD (range) agea Intervention group: 44.3 ± 11.53 years (25 to 80 years) Placebo group: 51.9 ± 17.69 years (24 to 89 years) Mean ± SD (range) duration of CTS symptomsa Intervention group: 1.97 years ± 2.04 months (6 months to 10 years) Placebo group: 2.17 years ± 2.40 months (6 months to 10 years) Inclusion criteria
Exclusion criteria
Details of surgical intervention Open carpal tunnel release (CTR) CTS diagnostic criteria (case definition) CTS diagnosis based on both a clinical and an electroneuromyographic diagnosis of CTS Symptom severity Moderate to severe CTS symptoms according to Gelberman et al classification (Gelberman 1998)a |
|
| Interventions |
Intervention group 1: low‐level laser therapy Low‐level laser therapy (with aluminium gallium Ibramed laser pen, wavelength 830 nm, power 30 mW) performed in 10 daily, consecutive sessions at an interval of 2 days using a total of 3 J, at 3 points of the carpal tunnel (CT) (pisiform, middle of CT, distal limit of CT) Placebo group 2: sham therapy Placebo laser therapy performed in 10 daily, consecutive sessions at an interval of 2 days using a total of 3 J, at 3 points of the CT (pisiform, middle of CT, distal limit of CT) |
|
| Outcomes | Outcomesc were assessed at 2 weeks and at 1, 2, 3 and 6 months after surgery, or until participant was asymptomatic and was discharged from treatmentd
|
|
| Notes |
aStudy authors were contacted to clarify data and provided clarification as indicated bPersonal communication with trialist confirmed that no participants had bilateral CTS Quote (unpublished data): "Only one wrist per participant *was contributed*". Comment: Data are reported to be based on the number of participants, which is equal to the number of included wrists. Hence a unit of analysis error is unlikely to have occurred cThe method used to measure outcomes was not reported in the publication dMean time to discharge was reported by trial authors: "Thus in both groups the mean time to discharge was 3.6 months, whereas in group 1 it ranged from one to six months to discharge, and in group 2 from one to eight months” (pg. 699) eThis outcome was not specified in our review, so data were not entered for statistical analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Patients were randomly and sequentially divided into two groups" Quote (unpublished data): "Patients were sequentially divided into two groups (the even numbers were for laser, the odd numbers were for placebo)" Comment: Random sequence was not adequately generated |
| Allocation concealment (selection bias) | High risk | Quote: "Patients were randomly and sequentially divided into two groups" Quote (unpublished data): "Patients were sequentially divided into two groups (the even numbers were for laser, the odd numbers were for placebo)" Comment: Allocation apparently was not adequately concealed |
| Blinding (performance bias and detection bias) Self reported outcomes | Low risk | Quote: "Neither groups of patients knew the identity of the members of the placebo group or treatment group" Comment: Participants were blind to the intervention |
| Blinding (performance bias and detection bias) Other outcomes | High risk | Quote: "We did not achieve the necessary structure to exclude the surgeon's awareness of the group to which the patients belonged" Quote: "Both groups were assessed regularly by the surgeon after the procedure, in visits two weeks after the surgery, and in the first, second, third and sixth postoperative months or until patients were asymptomatic and capable of returning to work or their civilities of daily living. During the visits, they were evaluated in terms of symptoms of palmar pain, pillar pain, paraesthesia, nighttime pain, pain or discomfort at the site of the scar and Tinel's test, as well as time taken to return to activities of daily living or to work" Quote: "The electroneuromyographs were executed by examiners who did not come into contact with the study data" Comment: Treaters were not blind to the intervention nor were most outcome assessments blinded. Outcome assessors for the electromyographs were most probably blind to the intervention |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "No patients abandoned the study" Comment: Reported data are likely to be based on a complete sample |
| Incomplete outcome data (attrition bias) After 12 weeks | Low risk | Quote: "No patients abandoned the study" Comment: Reported data are likely to be based on a complete sample |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes specified in the Methods section of the publication were reported in the prespecified way, except electroneuromyographic evaluations. It is unclear from the publication how the percentage of abnormal findings at baseline (preoperation) and on discharge or at 6 months was calculated and recorded. This was later clarified by trial authors, and results were entered into RevMan accordingly |
| Other bias | Low risk | No other sources of bias were identified |
Bhatia 2000.
| Methods | RCT No blinding |
|
| Participants |
Details of sampling framea Total n eligible = not reported Total n excluded prerandomisation = not reported Total n randomised = 130 participants Total n available for follow‐up = 102 participants Total n analysed = 102 participants Intervention group 1: n = 45 completed trial Intervention group 2: n = 57 completed trial Gender distribution Not reported Mean ± SD (range) age Not reported Mean ± SD (range) duration of CTS symptoms Not reported Inclusion criteria
No exclusion criteria specified Details of surgical intervention Type of surgical release (open, mini‐open or endoscopic) not reported. Operation performed under local anaesthetic with tourniquet control CTS diagnostic criteria (case definition) Not reported Symptom severity Not reported |
|
| Interventions |
Group 1: splint for 48 hours post operation Immobilisation (volar plaster of Paris splint) for the first 48 hours after surgery Group 2: bulky dressing for 48 hours post operation Bulky wool and crepe bandage dressing for the first 48 hours after surgery Participants advised to remove the splint or dressing 48 hours postoperatively. Discharged home with a supply of co‐proxamol tablets for pain relief for 72 hours |
|
| Outcomes | Participants assessed their outcomes twice daily for 72 hours after surgery. Outcome data were returned to the researchers 2 weeks postoperatively
|
|
| Notes |
aThe number of CTS‐affected wrists in this trial was not reported, so a unit of analysis variance may have occurred bThis outcome was not specified in our review, so data were not entered for statistical analysis cMean and SD values for this outcome measure were not reported Attempts to contact trial authors for incomplete or unclear data were unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were randomised using random number tables to receive either a palmar plaster splint or a bulky wool and crepe bandage postoperatively" Comment: The allocation sequence probably was adequately generated |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The patients were randomised using random number tables to receive either a palmar plaster splint or a bulky wool and crepe bandage postoperatively" Comment: Not enough information was available to reveal whether allocation concealment was adequate |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Quote: "A prospective randomised single blind trial was performed of 102 patients undergoing carpal tunnel release" Comment: Trial authors do not specify whether participants were blinded, but the nature of the interventions makes it unlikely |
| Blinding (performance bias and detection bias) Other outcomes | Unclear risk | Quote: "A prospective randomised single blind trial was performed of 102 patients undergoing carpal tunnel release" Comment: Trial authors do not specify whether outcome assessors were blind |
| Incomplete outcome data (attrition bias) 12 weeks or less | Unclear risk | Quote: "Of the 130 patients entered into the study, 102 completed the protocol" Comment: Reasons for attrition/exclusions were not reported |
| Incomplete outcome data (attrition bias) After 12 weeks | High risk | Comment: The final follow‐up was at 72 hours post surgery or 24 hours after the intervention ceased |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes specified in the Methods section of the publication were reported in the prespecified way |
| Other bias | Low risk | No other sources of bias were identified |
Bury 1995.
| Methods | RCT No blinding reported |
|
| Participants |
Details of sampling framea,b Total n eligible = not reported Total n excluded prerandomisation = not reported Total n randomised = 47 participants Total n available for follow‐up = 40 participants (43 wrists) Total n analysed = 40 participants (43 wrists) Intervention group 1: n = 26 Intervention group 2: n = 17 Gender distribution Group 1: 2 males; 24 females Group 2: 2 males; 15 females Mean ± SD (range) agec Intervention group 1: 43 years (range 19 to 79 years) Intervention group 2: 39 years (range 21 to 74 years) Mean ± SD (range) duration of CTS symptomsc Duration of CTS symptoms for both groups 13 months (range 5 to 36 months). No group‐specific data provided Inclusion criteria Patients with diagnosis of CTS scheduled for surgery after failed conservative management by wrist splinting Exclusion criteria Patients who had undergone prior carpal tunnel surgery Details of surgical intervention
CTS diagnostic criteria (case definition)
Symptom severity Not reported |
|
| Interventions |
Group 1: bulky dressing plus splint for 2 weeks post operation Immobilisation (bulky dressing and neutral wrist splint) for 2 weeks after surgery Group 2: bulky dressing for 2 weeks post operation Bulky dressing consisting of a bandage for 2 weeks after surgery |
|
| Outcomes | Outcomesc were assessed at mean follow‐up period of 6 months postoperatively (range 3.8 to 7.8 months)
|
|
| Notes |
aQuote: "32 of 40 patients had bilateral symptoms and 3 patients underwent staged bilateral surgery during the trial period" Quote: "The ratios of...bilateral symptoms...were not statistically significantly different between the two treatment groups (p>0.05)" Although the distribution of bilateral cases between groups was not statistically significant, a unit of analysis error may have occurred, although this is not clearly reported in the publication bData reported only for participants completing treatment. Note also, 3 participants underwent bilateral procedures cMeasures of variability (SDs) for these outcome measures were not reported. An attempt to obtain the required data from trial authors was unsuccessful dData on these outcomes were not reported in published trial. An attempt to obtain data from trial authors was unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After the decision was made to intervene surgically, informed consent was obtained and each patient was randomised by a random number generator into two groups" Comment: The allocation sequence probably was generated adequately |
| Allocation concealment (selection bias) | Unclear risk | Quote: "After the decision was made to intervene surgically, informed consent was obtained and each patient was randomised by a random number generator into two groups" Comment: Not enough information was available to reveal whether allocation concealment was adequate |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: This was not reported, but because of the nature of the interventions (splint or bulky dressing), it is unlikely that blinding occurred |
| Blinding (performance bias and detection bias) Other outcomes | Unclear risk | Comment: Not enough information was available to reveal whether outcome assessors were blinded |
| Incomplete outcome data (attrition bias) After 12 weeks | Unclear risk | Quote: "Seven patients with eight carpal tunnel releases were lost to follow up, leaving 40 cases with 43 procedures available for review. Twenty‐six had a postoperative splint for 2 weeks and 17 had only a bulky dressing placed" Comment: Trial authors did not report how many participants were randomised to each group at inception, so it is unclear how many were lost to follow‐up from each group. In addition, the timing of outcome assessment for each participant is unclear as outcomes were assessed at follow‐up (range 3.8 to 7.8 months) |
| Selective reporting (reporting bias) | High risk | Comment: Most outcomes prespecified in the Methods were reported in the Results section, but only in terms of mean scores and of "statistically or non‐statistically significant" (with no P values provided ‐ only an indication that P < 0.05 or P > 0.05). No SD or SE values were reported for any outcomes. Results for the outcome "thenar muscle function" were not reported |
| Other bias | Low risk | No other sources of bias were identified |
Cebesoy 2007.
| Methods | Quasi‐RCT No blinding reported |
|
| Participants |
Details of sampling frame Total n eligible = not reported Total n excluded prerandomisation = not reported Total n randomised = 46 participants (46 wrists)a Total n available for follow‐up = 40 participants (40 wrists)a Total n analysed = 40 participants (40 wrists)a Intervention group 1: n = 20 participants (20 wrists)a Intervention group 2: n = 20 participants (20 wrists)a Gender distribution Group 1: 7 males; 13 females Group 2: 5 males; 15 females Mean ± SD (range) ageb Group 1: 36 years (32 to 44 years) Group 2: 37 years (33 to 43 years) Mean ± SD (range) duration of CTS symptoms Group 1: not reported Group 2: not reported Inclusion criteria Patients with idiopathic CTS who were unresponsive to conservative treatment and were booked for carpal tunnel surgery Exclusion criteria
Surgical details Open CTR CTS diagnostic criteria (case definition) Pain (especially night pain), numbness and tingling in the median innervated fingers, positive Tinel’s sign, positive Phalen’s sign Symptom severity Preoperative symptom severity reported as an outcome on the BCTQ |
|
| Interventions |
Intervention group 1: splint with plaster of Paris cast Plaster of Paris splint applied after wound closure and worn until sutures were removed (approximately 10 days post operation) plus standard physical exercises after splint was removed at 10 days. Wrist immobilised by splint to the metacarpophalangeal (MCP) joint heads Intervention group 2: bulky dressing and physical exercises Bulky dressing applied after wound closure and worn until sutures were removed (approximately 10 days post operation) plus standard physical exercises immediately after surgery. Dressing allowed wrist and finger mobility Both groups discharged on the day of surgery and given paracetamol for 2 days of pain relief |
|
| Outcomes | Outcomes were assessed preoperatively and at 1 and 3 months postoperatively and included
|
|
| Notes |
aQuote: "Patients were excluded from this study if they had:...(2) a diagnosis of bilateral CTS..." Comment: A unit of analysis error could not have occurred bSDs not reported in the publication cThis outcome was not specified in our review, so data were not entered into RevMan Attempts to contact trial authors for missing or unclear information were unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "After inclusion and exclusion criteria had been applied, patients were randomly divided into 2 groups. Patient chart numbers given by the secretary were used for randomisation. If the chart number was even, the patient was assigned to the splint group. If the number was odd, the patient was given a bulky bandage postoperatively" Comment: A non‐random process was used to generate the allocation sequence |
| Allocation concealment (selection bias) | High risk | "After inclusion and exclusion criteria had been applied, patients were randomly divided into 2 groups. Patient chart numbers given by the secretary were used for randomisation. If the chart number was even, the patient was assigned to the splint group. If the number was odd, the patient was given a bulky bandage postoperatively" Comment: Allocation was potentially foreseeable by investigators enrolling participants; this represents a risk of selection bias |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: This was not reported, but because of the nature of the intervention (splint versus bulky bandage), it is unlikely that blinding occurred |
| Blinding (performance bias and detection bias) Other outcomes | High risk | Comment: Blinding of participants and personnel was not reported, and all outcomes were subjective. Given the nature of the interventions, it is unlikely that blinding occurred |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "Three patients in each group did not receive proper follow‐up and were excluded from the study during the final evaluation. They reported no problems during the phone interview. In all, 40 patients remained at the time of the final evaluation" Comment: It is clear from the publication that all data are based on 40 participants with CTS, and it is clear from which groups participants were excluded |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes specified in the Methods were fully reported in the Results section of the publication |
| Other bias | Low risk | No other sources of bias were identified |
Cook 1995.
| Methods | RCT No blinding |
|
| Participants |
Details of sampling framea Total n eligible = not reported Total n excluded prerandomisation = not reported Total n randomised = 50 participants (50 wrists) Total n available for follow‐up = not reported Total n analysed = not reported Intervention group 1: n = 25 participants (25 wrists) Intervention group 2: n = 25 participants (25 wrists) Gender distribution Not reported Mean ± SD (range) age Not reported Mean ± SD (range) duration of CTS symptoms Not reported Inclusion criteria Patients with isolated, uncomplicated idiopathic CTS scheduled for carpal tunnel surgery Exclusion criteria
CTS diagnostic criteria (case definition)
Details of surgical intervention
Symptom severity Not reported |
|
| Interventions |
Intervention group 1: immobilisation with a splint for 2 weeks post operation Volar wrist splint with wrist in neutral, allowing full finger motion for 2 weeks after surgery. Mean wear time 13.2 days Intervention group 2: mobilisation at 1 day post operation The soft bulky bandage applied at surgery was removed on the first postoperative day. A sticking plaster was applied to the wound, and participants were allowed unrestricted active mobilisation from day 1 |
|
| Outcomes | Outcomesb were assessed at 2 weeks and at 1, 3 and 6 months postoperatively and included
|
|
| Notes |
aQuote: "Patients with isolated, uncomplicated carpal tunnel syndrome scheduled for treatment by surgical release of the flexor retinaculum were included in this study" It is clear that all participants contributed only 1 wrist to the analysis bSome outcomes were not reported numerically or graphically in the publication cMeasures of variability (SDs) for these outcome measures were not reported Attempts to obtain missing or unclear data from trial authors were unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomised to two groups for postoperative management" Comment: Information was insufficient to reveal the adequacy of the sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "50 consecutive patients meeting the entrance criteria gave informed consent, enrolled in the study and were randomly divided into two groups of 25 patients each" Comment: Information was insufficient to reveal the adequacy of allocation concealment |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: This was not reported, but because of the nature of the interventions, it is unlikely that blinding occurred |
| Blinding (performance bias and detection bias) Other outcomes | Unclear risk | Comment: Information was insufficient to reveal whether outcome assessors were blinded |
| Incomplete outcome data (attrition bias) 12 weeks or less | Unclear risk | Comment: Withdrawals or losses to follow‐up were not reported by trial authors, but this does not mean that none occurred |
| Incomplete outcome data (attrition bias) After 12 weeks | Unclear risk | Comment: Withdrawals or losses to follow‐up were not reported by trial authors, but this does not mean that none occurred |
| Selective reporting (reporting bias) | High risk | Comment: Outcome reporting for most outcomes was incomplete (e.g. reported only as 'significantly different', with no numerical data). Hence data could not be entered into RevMan. Most outcomes were not reported at prespecified time points. Results for pain intensity were not reported at all |
| Other bias | Low risk | No other sources of bias were identified |
Fagan 2004.
| Methods | RCT No blinding reported |
|
| Participants |
Details of sampling framea Total n eligible = not reported Total n excluded prerandomisation = not reported Total n randomised = 43 participants (43 wrists) Total n available for follow‐up = 41 participants (41 wrists) (1 participant from each group was withdrawn) Total n analysed = 41 participants (41 wrists) (1 participant from each group was withdrawn) Intervention group 1: n = 21 wrists randomised; 20 wrists completed Standard care group 2: n = 22 wrists randomised; 21 wrists completed Gender distribution 16 males; 27 females Mean ± SD (range) age Intervention group 1: 44 years (SD and range not reported) Standard care group 2: 47 years (SD and range not reported) Mean ± SD (range) duration of CTS symptoms Not reported Inclusion criteria Patients booked to undergo day‐case, primary carpal tunnel decompression Exclusion criteria
CTS diagnostic criteria (case definition) Not reported Details of surgical intervention
Symptom severity Not reported |
|
| Interventions |
Intervention group: elevation Home elevation device and Bradford sling (a foam, dog‐leg‐shaped support that wraps around the elbow and lower arm) were used for 5 days after CTR. The sling was suspended, allowing vertical elevation of the hand with the elbow at approximately 90°. The home elevation device allowed participants to suspend the Bradford sling at home. Participants were instructed to use the sling device during sleep as much as practicable. When ambulant, they were instructed to use a high crepe arm sling with the elbow flexed approximately 45° and the hand above the heart Standard care group: no elevation A standard crepe sling that held the elbow at approximately 90° was worn for 5 days after CTR. Participants were instructed to use the sling as much as was required for comfort, and to sleep as normal |
|
| Outcomes | • Hand volume measured with a volume displacement apparatus. The hand is inserted into a tank of water to a reproducible level on each occasion, and the observer measures the displaced water (mL) in a measuring cylinder that is equal to the volume of the hand. This is repeated 3 times and a mean is calculated. This outcome was assessed before surgery and at the end of treatment (5 days post surgery) • Pain on a visual analogue scale once a day for 5 days after surgeryb • Analgesic use recorded by participants on a chart to indicate the number of analgesics used each day for 5 daysc |
|
| Notes |
aIt was clear that all participants had only 1 CTS‐affected hand because volumetric measurements were taken of the "operated hand" and the "non‐operated hand". A unit of analysis error could not have occurred bMeasurement units were not stated, but we assume from the results in Table 1 (pg. 460) that a 0 to 10 VAS scale was used cThis outcome was not specified in our review, so data were not entered for statistical analysis Attempts to contact trial authors for incomplete or unclear data were unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "On admission to the day‐case unit the patients were consented and randomised to the treatment or control group by envelope draw" Comment: The random sequence probably was adequately generated |
| Allocation concealment (selection bias) | Unclear risk | Quote: "On admission to the day‐case unit the patients were consented and randomised to the treatment or control group by envelope draw" Comment: It is not clearly reported whether the envelopes were sequentially numbered, opaque, and sealed |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: This was not reported, but because of the nature of the interventions, it is unlikely that participants could have been blind to which treatment they received |
| Blinding (performance bias and detection bias) Other outcomes | Unclear risk | Quote: "To reduce observer error, our hand physiotherapist measured both pre‐ and postoperative volumes for each patient" Comment: Information was insufficient to determine whether the outcome assessor was blind to treatment allocation |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "One patient in each group was withdrawn because of failure to attend research follow‐up, although they were seen for routine follow‐up" Comment: Withdrawals were clearly reported and were unlikely to have biased estimates of treatment effect sizes |
| Selective reporting (reporting bias) | High risk | Comment: VAS pain was recorded daily for 5 days, but only 1 mean value was reported by trial authors. Also, analgesic use was reported only in terms of no significant difference between groups (with no numerical data or P values reported) |
| Other bias | Low risk | No other sources of bias were identified |
Finsen 1999.
| Methods | Quasi‐RCT No blinding reported |
|
| Participants |
Details of sampling framea Total n eligible = not reporteda Total n excluded prerandomisation = not reported Total n randomised = 74 participants (82 wrists) Total n available for follow‐up = not reported Total n analysed = not reported Intervention group 1: n = 37 hands Intervention group 2: n = 45 hands Gender distribution Group 1: 11 males; 26 females Group 2: 11 males; 34 females Mean ± SD (range) age Intervention group 1: 51 years (range 21 to 86 years) (measures of variability not reported) Intervention group 2: 48 years (range 26 to 80 years) (measures of variability not reported) Mean ± SD (range) duration of symptoms Not reported Inclusion criteria Patients with diagnosis of CTS scheduled for open surgery with trial author Exclusion criteria No disease or recent injuries that would interfere with grip strength measurements CTS diagnosis (case definition)b CTS diagnosis made clinically by surgeon Details of surgical intervention
Eight participants underwent bilateral operations Symptom severityb Moderate to severe CTS as determined by surgeon |
|
| Interventions | A bulky compression dressing was applied to all participants’ operated hands after the operation. This was removed 2 days postoperatively, and participants received treatments as outlined below Intervention group 1: immobilisation for 4 weeks post operation A plaster wrist splint positioned in slight dorsiflexion was applied to the operated hand(s) of participants for 2 weeks after surgery. After 2 weeks, sutures were removed and the plaster splint was replaced with a simple rigid orthosis for an additional 2 weeks. Both splints allowed full finger motion. Total time wearing splint was 4 weeks. Note: Study authors stated that additional physiotherapy was not usually prescribed but did not specify its frequency Intervention group 2: early mobilisation post operation The bulky compression dressing applied at surgery was removed on the second postoperative day and was replaced with light dressings. Participants were allowed to actively mobilise the wrist and fingers of their operated hand(s) within the limits of comfort but were asked to avoid heavy lifting for the first 6 postoperative weeks |
|
| Outcomes | Outcomesc assessed preoperatively and at 6 weeks and 6 months postoperatively
|
|
| Notes |
aEight bilateral cases were included. Hands of bilateral procedures were assigned to alternate treatment groups and were analysed as separate observations. Unit of analysis error was likely bData were obtained via communication with trial authors cResults for these outcomes were reported as median values and 95% CIs and were analysed by non‐parametric statistical analysis (suggesting skewed data). Therefore, these data were not entered into RevMan for analysis. Trial authors were not able to provide raw data or statistical analysis suitable for inclusion in RevMan |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Randomization was performed by adding up the 11 digits in the patient's social security number. When the sum was an odd number, he was allocated to one study group, when it was even, he was allocated to the other" Comment: A quasi‐random process was used to generate the allocation sequence |
| Allocation concealment (selection bias) | High risk | Quote: "Randomization was performed by adding up the 11 digits in the patient's social security number. When the sum was an odd number, he was allocated to one study group, when it was even, he was allocated to the other" Comment: Risk of bias was high as investigators could possibly foresee assignments |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: This was not reported, but because of the nature of the interventions (immobilisation versus no immobilisation), it is unlikely that participants were blind to treatment allocation |
| Blinding (performance bias and detection bias) Other outcomes | Unclear risk | Quote: "To reduce bias, the investigator who had seen the patient preoperatively, and in many cases done the operation, did not perform the postoperative follow‐ups" Comment: Information was insufficient to determine whether assessors were blind to treatment allocation for all outcomes |
| Incomplete outcome data (attrition bias) 12 weeks or less | High risk | Comment: Study authors reported on 7 participants classified as 'protocol deviants' and indicated that these were "retained in their allotted groups". No withdrawals or losses to follow‐up were reported, but the data in Table 2 are based on less than the complete sample at 6 weeks of follow‐up, and no explanation is given as to why |
| Incomplete outcome data (attrition bias) After 12 weeks | High risk | Comment: Study authors report on 7 participants classified as 'protocol deviants' and indicate that these were "retained in their allotted groups". No withdrawals or losses to follow‐up were reported, but the data in Table 2 are based on less than the complete sample at 6 months of follow‐up, and no explanation is given as to why |
| Selective reporting (reporting bias) | High risk | Comment: Trial authors reported results for the outcomes of scar discomfort or pain, hypothenar pain, thenar pain, and number of days to return to work; however, none of these were prespecified in the Methods section of the publication. All other outcomes prespecified in the Methods section were reported |
| Other bias | Low risk | No other sources of bias were identified |
Gordon 2010.
| Methods | RCT No blinding reported |
|
| Participants |
Details of sampling framea Total n eligible = 25 participants (25 wrists) Total n excluded prerandomisation = 0 participants Total n randomised = 25 participants (25 wrists) Total n available for follow‐up = 21 participants (21 wrists) Total n analysed = 21 participants (21 wrists) Intervention group 1: n = 13 participants randomised; 11 completed Intervention group 2: n = 12 participants randomised; 10 completed Gender distribution Group 1: 5 males; 6 females Group 2: 3 males; 7 females Mean ± SD (range) age Group 1: 53 years (SE = 18) (range not reported) Group 2: 61 years (SE = 16) (range not reported) Mean ± SD (range) duration of CTS symptoms Group 1: not reported Group 2: not reported Inclusion criteria
Exclusion criteria
CTS diagnostic criteria (case definition)
Surgical details
Symptom severity Moderate to severe CTS or progressive symptoms ≥ 2 years |
|
| Interventions |
Group 1: electrical stimulation of the median nerve for 1 hour commenced 30 minutes post surgery With the participant in the lying position, the operated hand was stabilised in an elevated position. Stimulating electrodes were connected to a Grass (SD9) stimulator: The proximal wire electrode was connected to the cathode, and the distal one to the anode. Surface electrodes on the thenar eminence were connected to an electromyography machine (NeuroSoft Inc., Sterling, Virginia). Trial investigators gradually increased stimulation intensity to the maximal tolerance limit (4 to 6 V, 0.1 to 0.8 ms duration) as a continuous 20 Hz train for 1 hour. These intensities were sufficient to induce a fused tetanic contraction but not to induce excessive discomfort Group 2: no treatment control |
|
| Outcomes | Outcomes were assessed twice preoperation and at 3, 6 to 8, and 12 months post operation and included
|
|
| Notes |
aAll participants had bilateral CTS but provided only 1 wrist for treatment. Therefore, a unit of analysis error could not have occurred bStatistics were represented graphically and not numerically, so they could not be entered into RevMan for analysis Attempts to obtain missing or unclear data from trial authors were unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were randomised to the control or the stimulation group by using the random number generation function in a commercially available software program (Excel, Microsoft Inc.)" Comment: Random sequence appears to have been adequately generated |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Subjects were randomised to the control or the stimulation group by using the random number generation function in a commercially available software program (Excel, Microsoft Inc.)" Comment: Method used to conceal allocation sequence was not reported |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: Blinding of participants and personnel was not reported, but given the nature of the interventions, it is unlikely that blinding occurred |
| Blinding (performance bias and detection bias) Other outcomes | Unclear risk | Comment: Blinding of assessors of objective outcomes was not reported. Although this could have occurred, it cannot be assumed |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "Twenty five eligible CTS subjects participated in the study, all of whom had surgical decompression of the carpal tunnel under local anaesthesia (1% lidocaine). However, 4 subjects (2 males and 2 females) withdrew from the study because of development of other medical conditions or occupational commitments which prevented them to return for follow up. Two of these patients belonged to the control and 2 to the stimulation group. Therefore, the results are from 21 subjects: 8 males and 13 females" Quote: "Ten patients were assigned to the control group (no electrical stimulation, ES) and 11 patients to the stimulation group (1 h 20 Hz ES). All subjects attended the first postoperative follow‐up, whereas 19 of them were available for the second and third postoperative evaluations. Two of the subjects who missed appointments belonged to the control and one to the stimulation group" Comment: Numbers and reasons for incomplete outcome data were reported and are unlikely to have impacted the results |
| Incomplete outcome data (attrition bias) After 12 weeks | Low risk | Quote: "Twenty five eligible CTS subjects participated in the study, all of whom had surgical decompression of the carpal tunnel under local anaesthesia (1% lidocaine). However, 4 subjects (2 males and 2 females) withdrew from the study because of development of other medical conditions or occupational commitments which prevented them to return for follow up. Two of these patients belonged to the control and 2 to the stimulation group. Therefore, the results are from 21 subjects: 8 males and 13 females" Quote: "Ten patients were assigned to the control group (no electrical stimulation, ES) and 11 patients to the stimulation group (1 h 20 Hz ES). All subjects attended the first postoperative follow‐up, whereas 19 of them were available for the second and third postoperative evaluations. Two of the subjects who missed appointments belonged to the control and one to the stimulation group" Comment: Numbers and reasons for incomplete outcome data were reported and are unlikely to have impacted the results |
| Selective reporting (reporting bias) | High risk | Comment: All outcome data were reported in figure format (as mean or median ± SD) for all outcomes. No numerical data were reported in the publication and none could be obtained |
| Other bias | Low risk | No other sources of bias were identified |
Hochberg 2001.
| Methods | RCT No blinding |
|
| Participants |
Details of sampling framea Total n eligible = not reported Total n excluded prerandomisation = not reported Total n randomised = 72 participants (72 wrists) Total n available for follow‐up = 72 participants available for follow‐up (including 24 protocol violators) Total n analysed = 48 participants (48 wrists) (12 participants excluded from each group) Intervention group 1: n = 36 participants; 24 participants analysed Intervention group 2: n = 36 participants; 24 participants analysed Gender distribution 46 males; 26 females Mean ± SD (range) age 69% of participants younger than 45 years (no descriptive statistics reported) Mean ± SD (range) duration of symptoms Not reported Inclusion criteria Patients diagnosed with CTS and scheduled to undergo single open CTR after failed conservative management Exclusion criteria
CTS diagnostic criteria (case definition)
Details of surgical intervention
Symptom severity Not reported |
|
| Interventions |
Intervention group 1: controlled cold therapy (and narcotic use) Participants applied controlled cold therapy (CCT) to their affected hand or wrist continuously for 12 hours per day, immediately post surgery, until 3 days postoperatively. Expected daily exposure to treatment was 720 minutes. A thermostatically controlled cooling blanket (maintained at 7.2°C) was used to deliver cold therapy directly over the volar surface of the surgical dressings with a Temptek T‐1000 device Intervention group 2: ice therapy (and narcotic use) Participants applied a commercially available ice pack over the volar surface of their surgical dressings immediately after surgery. On return home, participants used a conventional ice bag (plastic bag with ice cubes) to deliver ice therapy to their affected hand or wrist when the cold pack lost its effectiveness. Ice therapy was applied in 12‐hour periods, beginning immediately after surgery, until 3 days postoperatively. Expected daily exposure to treatment was 360 minutes. Participants were asked to alternate ice applications with no ice at 20‐minute intervals, for a total of 12 hours per day Participants in both groups were provided with external immobilisation and a surgical dressing less than 3 mm thick. The CCT device or ice was placed directly over the dressing on the dorsal aspect of the hand. Participants in both groups were given 28 hydrocodone + acetaminophen tablets on the day of surgery to take as required for pain relief |
|
| Outcomes | Outcomes assessed preoperatively, immediately postoperatively and 3 days after operation
|
|
| Notes |
aQuote: "All patients presenting with carpal tunnel syndrome who were to undergo single open surgical procedures were eligible for participation in the study" Comment: This suggests that treatment was administered to only 1 hand per participant, so a unit of analysis error is unlikely bThis outcome was not specified in our review, so data were not entered for statistical analysis Attempts to contact trial authors to ask for missing or unclear data were unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Treatment assignment was based on a computer‐generated randomisation list ensuring equal, unbiased distribution of patients into each group" Comment: The sequence generation probably was adequate |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Treatment assignment was based on a computer‐generated randomisation list ensuring equal, unbiased distribution of patients into each group" Comment: Information was insufficient to determine whether allocation concealment was adequate |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: This was not reported, but because of the nature of the interventions, it is unlikely that participants were blinded to the intervention they received |
| Blinding (performance bias and detection bias) Other outcomes | High risk | Quote: "All measures were recorded by an unblinded observer" Comment: Outcome assessor was not blind to treatment allocation |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "Prior to the performance of any analysis, 24 patients were excluded, 12 in each group. Reasons for exclusions are presented in Table 1" Comment: Exclusions were clearly reported, and an identical number of exclusions were described per group; these are unlikely to have biased the estimate of effect size. The number of participants included in the analysis of each outcome was clearly reported in the tables of results. Intention‐to‐treat analyses were performed on and reported for pain and swelling (wrist circumference) outcomes |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes specified in the Methods section of the publication were reported in the Results section in a prespecified way |
| Other bias | Low risk | No other sources of bias were identified |
Huemer 2007.
| Methods | Quasi‐RCT | |
| Participants |
Details of sampling framea Total n eligible = not reporteda Total n excluded prerandomisation = not reported Total n randomised = 50 participants (50 wrists) Total n available for follow‐up = 50 participants (50 wrists) Total n analysed = 50 participants (50 wrists) Intervention group 1: n = 25 Intervention group 2: n = 25 Gender distribution Not reported Mean ± SD (range) age Not reported Mean ± SD (range) duration of symptoms Not reported Inclusion criteria Diagnosis of isolated, idiopathic CTS No exclusion criteria specified CTS diagnostic criteria (case definition) Diagnosis of isolated, idiopathic CTS was based on a history of sensory disturbances along the distribution of the median nerve with dysaesthesia and pain and an abnormal electrodiagnostic study according to published practice parameters for electrodiagnosis of CTS, including distal motor latencies (conduction distance 6.5 cm; abnormal value > 4.5 ms) and median sensory conduction velocity (between wrist and index finger; abnormal value < 46 m/s) Details of surgical intervention
Symptom severity Not reported |
|
| Interventions |
Group 1: bulky dressing with a volar splint left in place for 48 hours with the wrist in neutral position Group 2: light bandage worn for 48 hours |
|
| Outcomes | Outcomes were assessed preoperatively and at 3 months of follow‐up and included
|
|
| Notes |
aQuote: "All patients who presented to our department with isolated, idiopathic CTS between January and May 2006 were included in this study" Comment: This indicates that each participant contributed only 1 wrist to the study and thus a unit of analysis error has not occurred bMeasures of variability (SDs) for outcome measures were not reported cTrial authors did not report which instrument was used to measure this outcome, nor did they provide an accompanying citation Attempts to contact trial authors to ask for incomplete or unclear data were unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "The randomisation was accomplished by applying a volar splint to every even numbered patient in the consecutive list of 50 patients in this study" Comment: A non‐random process was used to generate the allocation sequence |
| Allocation concealment (selection bias) | High risk | Quote: "The randomisation was accomplished by applying a volar splint to every even numbered patient in the consecutive list of 50 patients in this study" Comment: An alternating sequence generation was used, so investigators enrolling participants could possibly foresee interventions, introducing the potential for selection bias |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: This was not reported, but because of the nature of the interventions (light bandage versus splint), participant blinding was unlikely |
| Blinding (performance bias and detection bias) Other outcomes | Unclear risk | Comment: Insufficient information was provided |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "All recruited patients completed the study with no dropouts in either group" Comment: Reported data are likely to be based on a complete sample |
| Selective reporting (reporting bias) | High risk | Quote: "After carpal tunnel release, all patients reported almost complete resolution of their symptoms, which consisted of numbness, especially at night, as well as pain and tingling" Comment: Trial authors do not report how these symptoms were measured. Only mean scores (no SDs or 95% CIs) were reported for all outcomes, and outcomes were reported in terms of "significantly different" between time points or between groups, but no P values were reported |
| Other bias | Low risk | No other sources of bias were identified |
Janssen 2009.
| Methods | Double‐blind RCT Blinded participants and outcome assessors |
|
| Participants |
Details of sampling framea Total n eligible = 58 participants (58 wrists) Total n excluded prerandomisation = 0 participants Total n randomised = 58 participants (58 wrists) Total n available for follow‐up = 56 participants (56 wrists) Total n analysed = 56 participants (56 wrists) Intervention group 1: n = 19 participants completed Intervention group 2: n = 23 participants completed Intervention group 3: n = 14 participants completed Gender distributionb Group‐specific gender distribution not reported Total randomised: 22 males; 36 femalesa Mean ± SD (range) ageb Group‐specific data not reported Total randomised: 51.5 (SD and range not reported) Mean ± SD (range) duration of CTS symptomsb Not reported Inclusion criteria
Exclusion criteria
CTS diagnostic criteria (case definition) Clinical examination and electromyographic testing Details of surgical intervention Open CTR Symptom severityb Not reported |
|
| Interventions |
Group 1: contrast baths plus exercise Involved hand was placed in hot water up to the proximal wrist crease, and the participant immediately began by doing 10 gentle, pain‐free, deliberate composite fists; one every 6 s. Exercises were then immediately replicated in cold water, and participants continued this process of shifting the hand back and forth between hot and cold baths for a total of 11 min Group 2: contrast baths without exercise Involved hand was placed in hot water up to the proximal wrist crease for 1 min, followed by immersion in cold water in the same position for 1 min. The hand was shifted back and forth between hot and cold baths for a total of 11 min. Group 3: exercise only The participant performed 10 gentle, pain‐free, deliberate composite fists ‐ one every 6 s. The participant paused for 4 s after each 10 repetitions and continued this process for a total 11 min |
|
| Outcomes | Outcome assessed immediately after treatment before open CTR and after treatment delivered 10 to 14 days post CTR
|
|
| Notes |
aOnly 1 affected hand per participant was evaluated in this study, so a unit of analysis error resulting from the correlation between 2 wrists in bilateral CTS participants could not have occurred bStudy authors were contacted for clarification of unclear or unreported items. Unpublished data were received via personal communication with trial authors Participants received interventions before and after open carpal tunnel surgery; data included in this review pertain only to evaluation after surgery |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The subjects were assigned to the different treatment groups by random assignment with replacement—each subject picked one of three different coloured cubes from a cloth bag. The cubes were then returned to the bag so that subsequent participants had an equal chance of picking from all three coloured cubes" Comment: The random allocation sequence probably was adequately generated |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The subjects were assigned to the different treatment groups by random assignment with replacement—each subject picked one of three different coloured cubes from a cloth bag. The cubes were then returned to the bag so that subsequent participants had an equal chance of picking from all three coloured cubes" Quote (unpublished data): "Randomisation into the groups was concealed from the evaluator by a separate team member"a Comment: Information was insufficient to determine whether the allocation sequence was adequately concealed |
| Blinding (performance bias and detection bias) Self reported outcomes | Low risk | Quote: "The subjects were blinded to group assignment and knew only that they were receiving a treatment" Comment: Participants were probably blind to treatment allocation |
| Blinding (performance bias and detection bias) Other outcomes | Low risk | Quote: "All evaluations were conducted by two certified hand therapists (RGJ, DAS). The evaluating therapist was blinded to the specific treatment group for each subject" Comment: Outcome assessors probably were blind to treatment allocation |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "The pre‐surgery subjects were divided as follows—Treatment Group 1: Contrast Baths with Exercise had 18 participants, Treatment Group 2: Contrast Baths without Exercise had 22 participants, and Treatment Group 3: Exercise Alone had 18 participants. Eight subjects studied preoperatively were unavailable for postoperative data collection and dropped out of the study. Reasons cited by subjects for dropping out of the study included the amount of time it took for the evaluation and treatment, and/or rescheduling of follow‐up surgeon visits without rescheduling of therapy follow‐up visits. Fifty subjects continued with the study after their surgery. Six additional subjects were recruited for data collection after CTR surgery, although they did not participate before surgery. A total of 56 subjects were thus treated and evaluated for the study post‐surgery. The post surgery subjects were divided as follows—Treatment Group 1: Contrast Baths with Exercise had 19 participants, Treatment Group 2: Contrast Baths without Exercise had 23 participants, and Treatment Group 3: Exercise Alone had 14 participants" Comment: Numbers of dropouts and reasons for withdrawals were reported and were unlikely to have an impact on the results |
| Selective reporting (reporting bias) | Low risk | Comment: Outcomes for this study were fully reported in the Results section of the publication |
| Other bias | Low risk | No other sources of bias were identified |
Jeffrey 2002.
| Methods | Randomised, double‐blind, placebo‐controlled trial Blinded participants and assessors |
|
| Participants |
Details of sampling frame Total n eligible = not reported* Total n excluded prerandomisation = not reporteda Total n randomised = 40 participants (80 wrists)b Total n available for follow‐up = not reporteda Total n analysed = 37 participants (74 wrists)b Intervention group 1: n = 20 participants (40 hands)b Intervention group 2: n = 17 participants (34 hands)b Gender distribution Intervention group: 12 males; 8 females Placebo group: 6 males; 11 females Mean ± SD (range) age Intervention group 1: 51 ± 14 yearsb Intervention group 2: 55 ± 19 yearsb Mean ± SD (range) duration of symptomsa Not reported Inclusion criteria
Exclusion criteria
CTS diagnostic criteria (case definition)a Not reported Surgical details
Symptom severitya Not reported |
|
| Interventions |
Group 1: arnica Three arnica D6 tablets 3 times daily (total 9 tablets/day) from the day of surgery for 2 weeks, plus application and gentle massage with arnica ointment 3 times daily around (but not in) the wound and on the front of the wrist after removal of the dressing 72 hours post surgery, for 2 weeks Group 2: placebo Placebo (not specified by trial authors, so it is assumed that 3 placebo tablets were taken 3 times daily and placebo ointment was applied 3 times daily for 2 weeks) After surgery, participants in both groups received a bulky dressing, with free fingers and thumb to allow mobility. No splint was used. Participants were given an exercise sheet. Dressing was removed at 3 days and sutures after 1 week. Participants were routinely discharged after 2 weeks |
|
| Outcomes | Outcomes were assessed preoperatively and 1 and 2 weeks after surgery
|
|
| Notes |
aAttempts to contact trial authors for clarification of unclear or incomplete data were unsuccessful bData reported only for participants completing treatment (n = 37) cOnly mean was reported numerically (SD was presented graphically) Quote: "All patients who received bilateral endoscopic carpal tunnel releases (ECTRs) performed by the senior author between June 1998 and January 2000 were considered for this study" Quote: "The results are presented as the mean of both sides at each time interval" Comment: This suggests that data are based on the number of participants, not on the number of independent wrists, so a unit of analysis error is unlikely |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The Arnica and placebo preparations were formulated by Weleda Ltd, a licensed UK manufacturer, which also performed the randomisation" Comment: Insufficient information was provided |
| Allocation concealment (selection bias) | Low risk | Quote: "The Arnica and placebo preparations were formulated by Weleda Ltd, a licensed UK manufacturer, which also performed the randomisation" Comment: The allocation sequence probably was adequately concealed until interventions were assigned |
| Blinding (performance bias and detection bias) Self reported outcomes | Low risk | Quote: "Double‐blind, randomised comparison of Arnica administrations versus placebo" Quote: "The placebo and active preparations looked exactly the same?" Comment: Participants probably were blind to treatment allocation |
| Blinding (performance bias and detection bias) Other outcomes | Low risk | Quote: "After gathering the data, the authors were provided with the allocations of patients into two groups so we could perform the data analysis. Only after the data analysis was complete were we informed which group received placebo and which received Arnica" Comment: Outcome assessors probably were blind to treatment allocation |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "Forty patients were entered into the trial. Three patients were excluded because of conversion to an open release on one or both sides. Twenty patients were in the arnica group and 17 were in the placebo group" Comment: Trial authors did not specify how many participants were randomly allocated to each group, but the exclusion of three participants is probably unlikely to have resulted in significant bias in the outcomes reported |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes specified in the Methods section of the publications were reported in the prespecified way |
| Other bias | Low risk | No other sources of bias were identified |
Jerosch‐Herold 2012.
| Methods | Parallel‐group, single‐blind, pilot RCT Blinded outcome assessor |
|
| Participants |
Setting Outpatient orthopaedic surgical department of a large UK teaching hospital Details of sampling frame Total n eligible = 34 Total n excluded prerandomisation = 3 Total n randomised = 31 (1 withdrew after randomisation) Total n available for follow‐up = 26 (4 weeks); 24 (8 weeks) Total n analysed = 26 (4 weeks); 24 (8 weeks) Intervention group 1: n = 16 baseline; 13 (4 weeks); 11 (8 weeks) Control group 2: n = 15 baseline; 13 (4 weeks); 13 (8 weeks) Gender distribution Group 1: 8 males; 8 females Group 2: 9 males; 6 females Mean ± SD (range) age Group 1: 65.8 ± 13.4 years Group 2: 71.9 ± 13.6 years Mean ± SD (range) duration of CTS symptoms (since surgery)a Group 1: 18.2 ± 7.6 months Group 2: 16.9 ± 6.6 months Duration of symptoms before surgery was not collected Inclusion criteria
Exclusion criteria
CTS diagnostic criteria (case definition)a Those responding with mild or worse numbness (score ≥ 2) in a previously operated hand and mild or worse difficulty with grasping and using small objects (score ≥ 2) were invited to attend a clinical assessment of hand sensibility. Clinical assessment involved standardised tests: (1) touch threshold using WEST (Connecticut Bioinstruments, Riverdal, Connecticut, USA); (2) statistical 2‐point discrimination according to Moberg; (3) a locognosia test; and (4) STI test. Those with diminished sensibility as detected by ≥ 2 of the 4 tests were considered eligible Surgical details Open carpal tunnel releaseb Symptom severity Symptom severity was measured as part of the baseline screening |
|
| Interventions |
Intervention group 1: sensory retraining intervention Sensory retraining intervention was developed specifically for the trial. It included techniques for retraining discriminative functional sensibility suitable for patients after CTR. Participants were given a standardised set of materials and instructions but were told that they may alter the materials used to suit their level of sensory impairment, such as by replacing training objects with smaller or more complex and intricate ones. Standard materials consisted of 9 textures made from different textile materials, an opaque cloth bag containing 14 small objects (various sizes of metal nuts, bolts, coins, wooden knobs, balls and buttons) and a booklet of standardised instructions. Participants were asked to practice their exercises in short sessions of 5 to 10 minutes at least 3 times per day for 4 weeks, and to record daily the type and frequency of their exercises Control group 2: no treatment |
|
| Outcomes | Outcomes were assessed at baseline (preintervention/randomisation), at cessation of the intervention (4 weeks) and at 4 weeks after cessation of the intervention (i.e. 8 weeks from baseline assessment) • Functional sensibility based on 4 assessments ∘ Touch threshold using the Weinstein Enhanced Sensory Test (WEST) ∘ Static 2‐point discrimination according to Moberg (mm) ∘ Locognosia test (0 to 56, > 49 = normal) ∘ Shape‐Texture Identification test (STI) rated on a 5‐point scale (4 = normal) • Moberg pick‐up test (log of seconds)c • DASH questionnaire (0 to 100; higher score indicates higher disability) • Adherence was assessed with a diaryd |
|
| Notes |
aStudy authors reported duration of symptoms since surgery bUnpublished data were provided by trialists c"The Moberg test, although continuous, was very positively skewed, and it was therefore logarithmically transformed before analysis" dOutcome was not included in this review Quote: "In patients with bilateral CTD only the hand with worse numbness was assessed" Comment: It is unlikely that a unit of analysis error would have occurred, as it appears that only 1 hand from each participant was entered into the trial This was a pilot trial and no sample size calculations were performed, so the study may have been underpowered to reveal differences between groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A simple blocked (random permuted block length of 2 and 4) randomisation sequence was generated independently" From the acknowledgements, it appears that trial authors used a randomisation service Comment: It is most likely that the random sequence was adequately generated |
| Allocation concealment (selection bias) | Low risk | Quote (unpublished data): "The randomisation sequence was generated and held separately by the Norwich clinical trials data manager. No one in the trial team had access to this randomisation sequence. The data manager set up a simple web‐based randomisation programme on a secure web‐based system to which only the PI had log‐in access. Once the participant was assessed and screening for eligibility and had given fully informed consent, the PI would log into the web‐based randomisation system, enter the patient unique ID and the system would provide a group allocation which was then communicated to the patient" Comment: The randomisation allocation was likely adequately concealed up until the interventions were assigned |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Quote: "The lack of blinding of patients is a potential source of bias, and the possibility of a Hawthorne effect cannot be ruled out" Comment: Participants were not blinded, possibly because of the nature of the interventions. It is assumed that the nature of the intervention precluded blinding of treaters |
| Blinding (performance bias and detection bias) Other outcomes | Low risk | Quote/s: "Group allocation remained concealed from the independent assessor, who undertook all follow‐up assessments until the completion of the trial", and "Blinding was successfully maintained until the end of the final assessment at 8 weeks for all except 1 patient" Comment: Outcome assessors appear to have been blinded for the duration of the trial, except for 1 participant at the 8‐week follow‐up review |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "Thirty‐one patients attended for an assessment and were randomised, and 24 completed follow‐up at 8 weeks" Comment: Trial authors also included a CONSORT diagram flow chart |
| Incomplete outcome data (attrition bias) After 12 weeks | Unclear risk | This was not reported |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the Methods section of the publication were reported in the Results section of the publication. In the trials register, notification (ISRCTN30848329) reported 'sensory tests' but the types of tests were not detailed; trialists have provided unpublished data to support that these were prespecified before commencement of the trial |
| Other bias | Low risk | No other sources of bias were identified |
Li 2008.
| Methods | RCT No blinding |
|
| Participants |
Details of sampling frame Total n eligible = not reported Total n excluded prerandomisation = not reported Total n randomised = 124 participants (75 CTS participants) Total n available for follow‐up = 124 participants (75 CTS participants) Total n analysed = 124 participants (75 CTS participants) Intervention group 1: n = 31 participants randomised (18 of whom had median nerve entrapment syndrome) Intervention group 2: n = 31 randomised (21 of whom had median nerve entrapment syndrome) Intervention group 3: n = 31 randomised (17 of whom had median nerve entrapment syndrome) Control group 4: n = 31 randomised (19 of whom had median nerve entrapment syndrome) Gender distribution (All participants: gender of CTS participants not reported separately) Group 1: 13 males; 18 females Group 2: 11 males; 20 females Group 3: 9 males; 22 females Group 4: 8 males; 23 females Mean ± SD (range) age (All participants: age of CTS participants not reported separately. Mean and SD not reported) Group 1: range 23 to 61 years Group 2: range 25 to 59 years Group 3: range 26 to 57 years Group 4: range 28 to 56 years Mean ± SD (range) duration of CTS symptoms Not reported Inclusion criteria All participants met the diagnostic standard of peripheral nerve entrapment syndrome as defined by Doctor Chen in 1995 (Li 2008). Diagnostic criteria: (1) paraesthesia in the region dominated by the entrapped nerve, such as pain numbness and malaise, alternation between mild and severe levels, gradual aggravation and pain and aggravation at night; (2) sensitisation or degeneration of sensory functions, or even sensory deprivation in regions dominated by the injured nerve; (3) tender points, strand‐like tender masses or Tinel's syndrome at entrapped sites to irritate the most sensitive regions; (4) amyotrophy, weakness or reduced muscle force and disturbed motor co‐ordination in nerve‐dominated regions Exclusion criteria Not reported CTS diagnostic criteria (case definition) See inclusion criteria Details of surgery Not reported |
|
| Interventions |
Intervention group 1: electrical stimulation Multi‐form wave therapeutic equipment used to treat patients in the electrical stimulation group after neurolysis. Wave form, stimulus width, interval time and stimulus intensity were regulated on the basis of grade of nerve injury. Details were as follows: mild nerve injury: 50 to 100 ms stimulus width and 1500 to 2000 ms intervals; moderate nerve injury: 100 to 200 ms stimulus width and 3000 to 4000 ms intervals; severe nerve injury: 200 to 300 ms stimulus width and 3000 to 6000 ms intervals. Current dosage was 20 to 40 mA. Electrical stimulation was given for 6 min per session, once a day, and 20 days was regarded as 1 treatment cycle. Intercycle intervals were 10 days, and treatment was performed for 3 successive months Intervention group 2: decimeter wave therapy A TMA‐A double‐frequent mild‐hot therapeutic instrument was used on participants in the decimeter wave group after neurolysis. The therapeutic programme was adapted to the early and middle‐late phase. In the early phase, the decimeter wave was 10 to 15 W, 10 min per session once a day; in the middle‐late phase, the decimeter wave was 10 to 30 W, 20 min per session once a day. Twenty days was regarded as 1 treatment cycle. Intercycle intervals were 10 days, and treatment was performed for 3 successive months Intervention group 3: compound physical factor treatment (electrical stimulation and decimeter wave therapy combined) Participants in the compound physical factor group after neurolysis were treated the same as the decimeter wave group and the electrical stimulation group, respectively. Treatment was performed once a day, and 20 days was regarded as 1 course. Intercycle intervals were 10 days, and treatment was performed for 3 successive months Control group 4: no physical treatment |
|
| Outcomes | Outcomes assessed at 1, 2 and 3 months post surgery (3 months post surgery, equal to end of 3 months of treatment)
(Excellent efficacy: M5, M4, S4, S3, generally normal electromyogram; good efficacy: M3, S3, mostly recovered electromyogram; passable efficacy: M2, S2, slightly recovered electromyogram; poor efficacy: M1, M0, S1, S0, no recovery in the electromyogram. Grades set by the Subassociation of Hand Surgery, Chinese Medical Associationb) |
|
| Notes |
aThis outcome was not included in our review; thus, data were not included in our statistical analysis bAs this publication reports results of rehabilitation after a mixture of nerve entrapment surgeries, and it is not clear whether participants offered more than 1 hand, a unit of analysis error may have occurred. Attempts to contact trial authors to obtain this information and CTS‐specific data including incomplete or unclear data were unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "All patients were randomly divided into four groups: electrical stimulation group, decimeter wave group, compound physical factor group, and control group, with 31 subjects in each group" Comment: No information on allocation sequence generation was reported |
| Allocation concealment (selection bias) | Unclear risk | Quote: "All patients were randomly divided into four groups: electrical stimulation group, decimeter wave group, compound physical factor group, and control group, with 31 subjects in each group" Comment: No information on allocation sequence concealment was reported |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: Blinding of participants and personnel was not reported, but given the nature of the intervention, it is unlikely that participant blinding occurred |
| Blinding (performance bias and detection bias) Other outcomes | Unclear risk | Comment: Blinding of outcome assessors was not reported; however, this may have occurred |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "All initially recruited 124 patients with peripheral nerve entrapment syndrome were included in the final analysis" Comment: All participants randomised were analysed; no attrition/exclusions were reported |
| Incomplete outcome data (attrition bias) After 12 weeks | High risk | Comment: Last outcome assessment was performed at the completion of the intervention period, at 3 months post operation |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the Methods section were reported in the Results section of the publication |
| Other bias | Low risk | No other sources of bias were identified |
Martins 2006.
| Methods | Single‐blind quasi‐RCT Blinded assessors |
|
| Participants |
Details of sampling framea,b Total n eligible = 52 participants Total n excluded prerandomisation = 1 participant Total n randomised = 51 participants (53 wrists) Total n available for follow‐up = 50 participants (52 wrists) (1 participant excluded after randomisation) Total n analysed = 50 participants (52 wrists) Of the 7 participants who had bilateral involvement and underwent surgical procedures at separate times for each wrist, only 2 were included in the study for analysis (and 5 were not included in the analysis)a Intervention group 1: n = 25 participants (26 wrists) commenced study; 25 participants (26 wrists) completed study Intervention group 2: n = 26 participants (27 wrists) commenced study; 25 participants (26 wrists) completed study Gender distributiona Group 1: 3 male; 23 female (data include excluded participants) Group 2: 3 male; 23 female (data include excluded participants) Total sample distribution: 6 males; 46 females Mean age ± SD (range)a Group 1: 47.8 ± 11.5 years (26 to 74 years) Group 2: 51.7 ± 6.8 years (39 to 64 years) Total sample: 49.8 years (26 to 74 years) Mean ± SD (range) duration of CTS symptomsa Group 1: 29.5 ± 27.5 months (6 to 96 months) Group 2: 29.2 ± 23.1 months (8 to 72 months) Total sample: 29.31 (6 to 72) months Inclusion criteria
Exclusion criteria
CTS diagnostic criteria (case definition) Based on symptoms and findings on physical examination. Clinical examination included the presence of typical sensory symptoms, Tinel's sign, Phalen’s and Durkan’s tests, sensory testing by 2‐point discrimination, muscle testing and examination of thenar atrophy. All participants had electrophysiological confirmation of CTS Details of surgical intervention
Seven participants had bilateral involvement and underwent surgical procedures at separate intervals for each hand Symptom severity Not reported |
|
| Interventions |
Group 1: wrist immobilisation using a splint in the neutral position for 2 weeks post surgery Group 2: no splint worn and participants encouraged to move their hands and fingers freely No other treatment, including anti‐inflammatory drugs, was used in either group All participants received the same immediate postoperative care. Each wrist was immobilised in a soft dressing and a light compressive bandage for 48 hours; after that, 2 groups were formed according to the treatment adopted |
|
| Outcomes | Outcome assessments were performed preoperatively and at 14 days postoperatively
|
|
| Notes |
aData obtained from personal communication with trial authors bQuote: "Seven patients had bilateral involvement and underwent surgical procedures on separate time for each hand" Quote: "Randomisation of the wrists was used in this study" Quote: "Each wrist was considered as an independent variable" Comment: Outcomes reported are based on the number of wrists; thus a unit of analysis error is likely to have occurred cResults were expressed as the mean total score for answered questions, and as a symptom severity/intensity index, calculated as "preoperative value ‐ postoperative value/preoperative value" dResults were expressed as mean score in mm, and as discrimination index, calculated as "preoperative value ‐ postoperative value/preoperative value" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Fifty two patients with idiopathic carpal tunnel syndrome were randomly selected in two groups after open carpal tunnel release" Quote (unpublished data): "a simple randomisation was used. After surgery each patient was alternatively allocated within the treatment groups" Comment: The random sequence was not adequately generated |
| Allocation concealment (selection bias) | Unclear risk | Quote: "All patients received the same immediate postoperative care. Each wrist was immobilized in a soft dressing and light compressive bandage for 48 hours and, after that, two groups with 26 patients were formed according to the treatment adopted" Comment: Insufficient information was provided |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: As a result of the nature of the interventions (splint versus no splint), blinding of participants or personnel is unlikely |
| Blinding (performance bias and detection bias) Other outcomes | Low risk | Quote: "The evaluations were performed pre‐operatively and repeated fourteen days after the surgery in a blind fashion" Quote (unpublished data): "Result[s] were noted in protocol without information about the treatment method. The examiner had access to the protocol that did not report the method of treatment. All postoperative follow‐up physical examinations were completed by one examiner who did not participate in the surgery and who had no knowledge of group assignments. However he could obtain information about treatment by questioning patients" Comment: Outcome assessors were probably blind to treatment allocation |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "Fifty‐two patients fulfilled the inclusion criteria during the study period. We had two exclusions in this study, one patient with classical symptoms who presented with a persistent median artery with large diameter at surgery and a patient who presented postoperative wound infection" Quote (unpublished data): "From the patients who had bilateral carpal tunnel syndrome, only two of the wrists were included in this study" and "One was excluded before randomisation, and had an anatomical variation observed during surgery (a large median artery), and the other was excluded after randomisation when a wound infection was detected" Comment: Incomplete outcome data appear to have been adequately addressed |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes specified in the Methods section of the publication were reported in the prespecified way |
| Other bias | Low risk | No other sources of bias were identified |
Pomerance 2007.
| Methods | Single‐blind RCT Blinded assessors |
|
| Participants |
Details of sampling framea Total n eligible = not reported Total n excluded prerandomisation = not reported Total n randomised = 150 participants (150 wrists) Total n available for follow‐up = 150 participants (150 wrists) Total n analysed = 150 participants (150 wrists) Intervention group 1: n = 73 Intervention group 2: n = 77 Gender distribution Gender distribution not clearly reported Mean ± SD (range) age Intervention group 1: 47 years (no measures of variability reported) Control group 2: 45 years (no measures of variability reported) Inclusion criteria
Exclusion criteria
CTS diagnostic criteria (case definition)
Details of surgical intervention
Symptom severity Advanced carpal tunnel (as identified and described in study inclusion and exclusion criteria) |
|
| Interventions |
Intervention group 1: formal therapy programme for 2 weeks post operation Two‐week formal therapy exercise programme of 6 sessions (nerve gliding exercises, range of motion, and strengthening). Each therapy session consisted of approximately 30 min with a certified hand therapist along with any additional treatments (massage, fluidotherapy etc.) used at each session. Participants were encouraged to use the hands for activities of daily living, and were encouraged to increase hand use Control group 2: no formal therapy programme No formal therapy programme was provided by a hand therapist, but participants were advised to avoid direct pressure over the incision and were encouraged to use the hands for activities of daily living, and to increase hand use Both groups were instructed preoperatively that no restrictions would be applied to motion of the operated hand and wrist, and no splints would be used after surgery; they were instructed in differential tendon gliding exercises and scar massage. Return to their desired activity or work was discussed with all participants preoperatively, and timing was based on job duties. All were allowed to be off work until the first postoperative visit (5 to 7 days). At that visit, return to work was allowed for all participants; job modifications, if any, were based on upper extremity requirements. Participants were allowed to return to modified activity while avoiding any forceful gripping or direct pressure over the incision site. They were advanced to full activities or work during subsequent visits unless complications resulted from surgery. Participants who did not have the option of modified duty because of the policy of the employer were off work until their symptoms and clinical evaluation allowed unrestricted work After surgery, participants in both groups were instructed that they could remove the dressing the following day if desired and shower, replacing the postoperative dressing with a standard adhesive strip. They were advised to avoid direct pressure over the incision and to keep the incision clean. Sutures were removed at the first postoperative visit (5 to 7 days), and participants were encouraged to use their hand for activities of daily living, and to increase hand use |
|
| Outcomes | • Return to work dates were recorded for both modified and regular duty. Results were reported as the number of participants returning to work at certain dates, categorised by insurance status (Medicare, commercial, or workers’ compensation). Assessed at 2, 4 and 6 weeks and at 3 and 6 months post surgery • Pain on an analogue 10‐point pain scale ranging from 0 = no pain to 10 = severe pain. Assessed preoperatively and postoperativelyb • Lateral pinch strength (kg) on a Preston pinch gauge (JA Preston Corporation, Clifton, New Jersey, USA). Assessed preoperatively and at 2, 4 and 6 weeks and 3 and 6 months post surgery • Grip strength (kg) determined by a dynamometer at position II as described by Mathiowietz et al (Asimov Engineering Corporation, Los Angeles, California, USA). Assessed preoperatively and at 2, 4 and 6 weeks and 3 and 6 months post surgery • Disability assessed by the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire. This outcome was measured only at the final postoperative visit (6 months post surgery) • Persistence of symptoms (participants were questioned for persistence of nocturnal symptoms, paraesthesias and incision difficulties) • Complications (wound dehiscence) • Economic evaluation (cost of care comparison between groups)c |
|
| Notes |
aQuote: "No bilateral surgeries were performed" Comment: It can be assumed that each participant contributed 1 wrist to the analysis, so a unit of analysis error is unlikely bTrial authors did not report how these data were recorded or at what time points they were measured cThis outcome was not specified in this review; hence, data were not entered into RevMan for analysis Attempts to contact trial authors for clarification of incomplete or unclear data were unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Once patients met the entry criteria, they were then randomised into 1 of 2 groups by having a staff member not involved in the study blindly draw a paper from a box. The box had equal numbers of marked and unmarked papers. Those with a mark were randomised to a 2‐week course of therapy...The patients with unmarked papers were randomised to a group without formal therapy" Comment: The allocation sequence probably was adequately generated |
| Allocation concealment (selection bias) | Low risk | Quote: "Once patients met the entry criteria, they were then randomised into 1 of 2 groups by having a staff member not involved in the study blindly draw a paper from a box. The box had equal numbers of marked and unmarked papers. Those with a mark were randomised to a 2‐week course of therapy...The patients with unmarked papers were randomised to a group without formal therapy" Comment: The allocation sequence probably was adequately concealed until interventions were assigned |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: This was not reported, but because of the nature of the interventions (therapist‐guided exercise programme versus instructions for home exercise only), it is unlikely that participants would have been blind to treatment allocation |
| Blinding (performance bias and detection bias) Other outcomes | Low risk | Quote: "At each office visit, clinical evaluation was completed by staff blinded to whether or not the patient was in formal therapy" Comment: Outcome assessors probably were blind to treatment allocation |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "No patients were lost to follow‐up, and none crossed over between groups" Comment: The data set probably was complete as no withdrawals were reported throughout the study period |
| Incomplete outcome data (attrition bias) After 12 weeks | Low risk | Quote: "No patients were lost to follow‐up, and none crossed over between groups" Comment: The data set probably was complete as no withdrawals were reported throughout the study period |
| Selective reporting (reporting bias) | High risk | Comment: Most of the outcomes specified in the Methods section were reported in the prespecified way (grip strength, pinch strength, disability based on the DASH questionnaire). However, preoperative pain and postoperative pain were not reported separately per group (only the mean score for the combined sample at these time points was reported). Recurrence of symptoms was not reported at all |
| Other bias | Low risk | No other sources of bias were identified |
Powell 2003.
| Methods | Double‐blind RCT Blinded assessors and participants |
|
| Participants |
Details of sampling framea Total n eligible = 40 participants (40 wrists) Total n excluded prerandomisation = 11 participants (11 wrists) Total n randomised = 29 participants (29 wrists) Total n available for follow‐up = 27 participants (27 wrists) Total n analysed = 27 participants (27 wrists) Intervention group 1: n = 13 Control group 2: n = 14 Gender distribution No group‐specific data reported Total sample: 5 males; 22 females Mean ± SD (range) age 53 years (33 to 83 years) Group 1: 48.5 years (33 to 83 years) Group 2: 54.5 years (34 to 80 years) Median duration of CTS symptoms No group‐specific data reported Total sample: 2 years (1 to 10 years) Inclusion criteria
Exclusion criteria None, although it was planned that patients who developed complications would be withdrawn for initiation of appropriate therapy CTS diagnostic criteria (case definition) Diagnosed by clinical examination by consultant surgeon Details of surgical intervention
No bilateral operations were performed Symptom severity Not reported |
|
| Interventions | All participants received a postoperative bulky dressing, which was reduced to a smaller dressing by the participant at 48 hours to enable gentle active mobilisation of the hand. All participants were given standard postoperative instructions, which included advice on elevation to minimise oedema, gentle active mobilisation of the hand and avoidance of heavy activities Sutures were removed at 14 days by a wound nurse to standardise suture removal and wound management. A light dressing was applied to the wound site, and participants were asked to keep the scar covered until their next review. The nature of CTS and the CTR were discussed with each participant, and general advice was given regarding their likely return to function based on recent research evidence and clinical experience. Interventions were assigned to each group at a hand therapy assessment 1 week later Intervention group 1: desensitisation Intervention group received a general hand exercise regimen and a desensitisation programme, which was demonstrated and advised by the occupational therapist. Participants were instructed to massage their scar tissue with a continuous, circular massage for 2 min, 5 times daily. They were then instructed to repeat the exercise with a rough towel, which was rubbed gently over the scar. All participants in the treatment group received a desensitisation programme advice sheet with specific instructions. This programme was upgraded at 6 weeks and at 3 months Control group 2: standard treatment control Control group received a general hand exercise regimen, and individuals were advised to carry out 5 of each of the wrist and hand exercises 5 times daily. An advice sheet was given detailing exercises, along with their intensity and regularity. Participants were advised to avoid heavy activities, such as ironing, carrying groceries and participating in contact sports |
|
| Outcomes | Outcomes were assessed at baseline (3 weeks post operation) and at 6 weeks and 3 months post operation
|
|
| Notes | All data were reported from unpublished sources (unpublished Master's thesis and personal communication) aQuote: "Twenty three subjects had bilateral carpal tunnel symptoms, and seven of these had undergone a previous CTR on the opposite hand" Comment: Trial authors reported that no bilateral surgeries were performed. Hence, a unit of analysis error would not have occurred |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Simple random sampling using even and odd numbered raffle tickets was chosen to give an equal and random chance of selection to the treatment and control groups. At the start of the session, subjects were asked to randomly pick a raffle ticket from a bowl, and were allocated a group. Subjects with even numbered tickets were placed in the treatment group, odd numbers in the control group" Comment: The random sequence was adequately generated |
| Allocation concealment (selection bias) | Low risk | Quote: "Simple random sampling using even and odd numbered raffle tickets was chosen to give an equal and random chance of selection to the treatment and control groups. At the start of the session, subjects were asked to randomly pick a raffle ticket from a bowl, and were allocated a group. Subjects with even numbered tickets were placed in the treatment group, odd numbers in the control group" Comment: The intervention allocation was adequately concealed |
| Blinding (performance bias and detection bias) Self reported outcomes | Low risk | Quote: "Subjects who underwent operations on the same day were allocated review appointments at different times/days to minimise communication between control and treatment group subjects" Quote: "Patients were not advised which group they were in to maintain blinding" Comment: Participants probably were blinded to whether they were in the intervention or the control group |
| Blinding (performance bias and detection bias) Other outcomes | Low risk | Quote: "At this stage, each subject was asked to attend a separate assessment booth set up by the OTT, for the subjective and objective assessments. The OTT was blinded to which group each subject belonged to avoid bias during assessments" Comment: The outcome assessor most probably was blinded to intervention allocation of participants. However, because of the nature of the intervention (desensitisation versus no desensitisation techniques), it would be unlikely that those administering treatment were blinded to the intervention group |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "Two male patients withdrew from the study at the six week stage. Their data [were] too small to be significant, therefore we removed [them] for purposes of the analysis" Comment: Withdrawals and how they were dealt with are clearly reported in the thesis |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes specified in the Methods section of the publication were reported on in the prespecified way |
| Other bias | Low risk | No other sources of bias were identified |
Provinciali 2000.
| Methods | Single‐blind quasi‐RCT Blinded assessor |
|
| Participants |
Details of sampling framea Total n eligible = not reported Total n excluded prerandomisation = not reported Total n randomised = 100 participants Total n available for follow‐up = not reported Total n analysed = not reported Intervention group 1: n = 50 Intervention group 2: n = 50 Gender distribution No group‐specific gender distributions reported Total sample: 18 males; 82 females Mean ± SD (range) age 54.7 ± 12.4 years (range 24 to 86 years) Group 1: 57.4 years (range 24 to 86 years) Group 2: 55.5 years (range 29 to 79 years) Mean ± SD (range) duration of symptoms Not reported Inclusion criteria
No exclusion criteria specified CTS diagnostic criteria (case definition)
Surgical details
Symptom severityb Mild (early): n = 0 Moderate (intermediate): n = 25 Severe (advanced): n = 75 Group 1: 11 moderate; 39 severe Group 2: 14 moderate; 36 severe |
|
| Interventions |
Intervention group 1: multi‐modal rehabilitation from 12 days postoperatively Participants received 10 sessions of physiotherapy (of 1 hour duration) for 2 weeks starting at day 12 postoperatively. Treatment consisted of progressive stretching of the palmar fascia for soft tissue mobilisation, progressive straightening exercises of abductor pollicis brevis and opponens pollicis, massage for softening the surgical scar, nerve gliding, grip and pinch exercises, motor dexterity exercises, sensory stimulation of the affected area of the hand and discriminative sensory re‐education exercises. Participants were treated by the same physiotherapist Intervention group 2: progressive home exercise programme Participants were instructed in a progressive home exercise programme designed to gradually increase strength and endurance. No splinting was used in these participants |
|
| Outcomes | Outcome assessed on the day of surgery, at day 12 postoperatively (before rehabilitation and at suture removal) and at 1 month and 2 months after surgery
|
|
| Notes |
aSome participants underwent bilateral surgery. It is unclear how many wrists in total were included in the study and therefore in the analysis. Quote (unpublished data): "We enrolled 100 wrists, some of them [were] operated at both wrists in different time. We considered the two data independently" Comment: A unit of analysis error was likely as bilateral wrists were analysed independently bSeverity of CTS symptoms was classified according to Stevens 1997. Mild = prolonged distal latency (relative or absolute) of sensory or mixed nerve action potentials (NAPs) with or without sensory nerve action potential (SNAP) amplitude below the lower limit of normal. Moderate = abnormal median sensory latencies as above, and (relative or absolute) prolongation of median motor distal latency. Severe = prolonged median motor and sensory distal latencies, with an absent SNAP or a mixed NAP, or low‐amplitude or absent thenar compound muscle action potentials. Needle examination often reveals fibrillation potentials, reduced recruitment and motor unit potential changes cMean and SD for this outcome were not reported in sufficient detail to be entered into RevMan for statistical analysis (data presented only in graphical form). No appropriate data could be obtained from trial authors dNo SDs were reported for this outcome; therefore it could not be entered into RevMan for statistical analysis eThis trial did not report on the number of workers' compensation participants excluded from this outcome analysis. Therefore, these data could not be entered into RevMan for analysis Giattini 1999 appears to be a precursor to this trial. Attempts to obtain this information from trial authors were unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomised into two groups using sequentially numbered, sealed envelopes" Quote (unpublished data): "The orthopedic unit communicated to the neuro‐rehabilitation clinic the list of patients reserved for surgery and one person, not engaged in the study with the patients formulated the two random lists with sequentially numbered sealed envelopes" Comment: The sequence was not randomly generated |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were randomised into two groups using sequentially numbered, sealed envelopes" Comment: Although the allocation sequence probably was adequately concealed, it is not clear whether the sequentially numbered, sealed envelopes were opaque |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Quote (unpublished data): "Participants were not blind to the intervention" Comment: Participants were not blinded to the intervention |
| Blinding (performance bias and detection bias) Other outcomes | Low risk | Quote: "In the present study, the examiner measured the time to complete each task using a chronometer, and was blind to the postsurgical treatment of each patient" Quote: "The evaluation[s] were made by a single examiner unaware of the postsurgical treatment" Comment: The outcome assessor probably was blind to treatment allocation |
| Incomplete outcome data (attrition bias) 12 weeks or less | Unclear risk | Comment: No exclusions/withdrawals were reported, but this does not mean that none occurred. Thus, it is unclear whether reported outcomes are based on a complete data set |
| Selective reporting (reporting bias) | High risk | Comment: All outcomes were reported numerically or graphically, but only mean scores were provided (no SDs or 95% CIs) and no P values were reported (when applicable, outcomes were reported as significantly or non‐significantly different between time points or groups) |
| Other bias | Low risk | No other sources of bias were identified |
Ritting 2012.
| Methods | RCT Blinded outcome assessor |
|
| Participants |
Details of sampling framea Total n eligible = 96 participants (96 wrists) Total n excluded prerandomisation = 2 participants (2 participants declined randomisation) Total n randomised = 94 participants (94 wrists) Total n available for follow‐up = 94 at first follow‐up (9 to 14 days) and 66 at final follow‐up (6 to 12 weeks) Total n analysed = 94 at first follow‐up (9 to 14 days) and 66 at final follow‐up (6 to 12 weeks) Intervention group 1: n = 45 participants; 30 participants completed study (15 participants lost to follow‐up) Intervention group 2: n = 49 participants; 36 participants completed study (13 participants lost to follow‐up) Gender distribution Intervention group 1: 14 males; 31 females Intervention group 2: 7 males; 42 females Mean age ± SD (range) Intervention group 1: 46.3 ± 14.8 years Intervention group 2: 44.8 ± 12.3 years Inclusion criteria
Exclusion criteria
CTS diagnostic criteria (case definition) Not reported Details of surgical intervention Mini‐open CTR performed by a single surgeon Symptom severity Not recorded |
|
| Interventions |
Intervention group 1: short postoperative dressing Participants were instructed to remove the bulky postoperative dressing at 48 to 72 hours and were provided with normal adhesive dressings. Participants were instructed to keep their wound dry until first postoperative visit at 9 to 14 days Intervention group 2: extended postoperative dressing Participants were instructed to keep the bulky postoperative dressing in situ until the first postoperative visit at 9 to 14 days No participants in either group were splinted, and all were instructed to commence finger mobilisation immediately after surgery. Sutures in both groups were removed at the first postoperative visit at 9 to 14 days |
|
| Outcomes | Outcomes assessed at 2 and 6 to 12 weeks postoperativelyb
|
|
| Notes |
aData reportedly were based on the number of participants who underwent unilateral surgery. This suggests that treatment was administered for only 1 wrist per participant, and thus outcomes were based on 1 wrist per participant. Hence a unit of analysis error is unlikely to have occurred bMean and SD for postoperative intervals for study outcomes were not reported and therefore could not be entered into RevMan for statistical analysis. Attempts to obtain this information from trial authors have been unsuccessful cThis outcome was not specified in our review, so data were not entered for statistical analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A randomised number table for 2 treatment groups was computer generated and subjects were consecutively randomised" Comment: The randomisation sequence probably was generated adequately |
| Allocation concealment (selection bias) | Unclear risk | Quote: "A randomised number table for 2 treatment groups was computer generated and subjects were consecutively randomised" Comment: Information was insufficient to reveal whether the allocation sequence was adequately concealed until interventions were assigned |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Comment: Participants were aware to which group they had been allocated |
| Blinding (performance bias and detection bias) Other outcomes | Low risk | Quote: "We took measurements using a goniometer, a hand dynamometer and a pinch meter under the care of 1 of 2 occupational therapists who were blinded to the protocol" Comment: The outcome assessor appears to have been blinded to the intervention |
| Incomplete outcome data (attrition bias) 12 weeks or less | High risk | Quote: "All 94 patients were available for analysis at 9 to 14 days, and 66 patients returned again between 6 and 12 weeks postoperatively" Quote: "This study has several weaknesses. Although initial follow‐up was 100%, follow‐up at 6 to 12 weeks was 70%. Both groups had an equal number of patient[s] lost to follow‐up which we speculate resulted from clinical improvement" Comment: Reported data for the final postoperative visit (6 to 12 weeks) are not based on a complete sample (15 participants in group 1 and 13 participants in group 2 were lost to follow‐up). Data reported for the 9 to 14 day visit constituted a complete sample |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes specified in the Methods section of the publication were reported in the prespecified way |
| Other bias | Low risk | Quote: "All patients completed objective preoperative testing including wrist range of motion and grip, tip and three‐point pinch and lateral pinch strength. Subjective evaluation included the Levine‐Katz questionnaire which is a previously validated outcomes scale for CTS" AND (Wound) "...the therapists could have used a graded system rather than a qualitative assessment of wound healing..." Comment: Most of the outcome measures used probably were appropriate and standardised instruments |
Sawan 2013.
| Methods | Parallel‐group, single‐blinded (outcome assessor) RCT | |
| Participants |
Setting Health insurance hospital outpatient clinic in Cairo, Egypt Details of sampling frame Total n eligible = 75 Total n excluded prerandomisation = 30 Total n randomised = 45 Total n available for follow‐up = 45 Total n analysed = 45 Intervention group 1: n = 15 Intervention group 2: n = 15 Intervention group 3: n = 15 Gender distribution Intervention group 1: 0 males; 15 females Intervention group 2: 0 males; 15 females Intervention group 3: 0 males; 15 females Mean age ± SD (range) Intervention group 1: 40.4 ± 4.5 years Intervention group 2: 39.8 ± 4.82 years Intervention group 3: 40.4 ± 3.21 years Mean duration of symptoms ± SD (range) Not reported Inclusion criteria
Exclusion criteria
CTS diagnostic criteria (case definition) Diagnosis was performed by neurosurgeon and orthopaedic surgeons and was confirmed by abnormal electrophysiological results (prolonged distal latency > 4.2 ms and sensory distal latency > 3.6 ms), positive Phalen's test and Tinel's test Details of surgical intervention No specific details reported (i.e. open, endoscopic or minimal incision) Symptom severity Refer to CTS diagnostic criteria |
|
| Interventions | Treatment duration was 6 weeks Continuous ultrasound group Using a BIOREM s.r.1 CE 0434.Electro medical Model BRTL 4 A Received the same exercises and continuous ultrasound (scanner type) with 1 MHz frequency; 1.5 w/cm2 intensity of continuous mode for 5 minutes applied over the carpal tunnel area and expanded from wrist crease to palmar region of the wrist joint Laser therapy group Using an Elettronica Pagani, model HPL 1.6 class 1, type B Received the same exercises and low‐level laser therapy with wavelength of 830 nm‐energy 9 Joule over the course of the median nerve of the wrist for 15 minutes. Laser therapy (scanner type) was applied at an 8 cm segment of the skin on the palmar surface of the hand, starting about 3 cm from the proximal border of the flexor retinaculum, then passed distally 5 cm across the retinaculum with width 5 cm over the thenar eminence Nerve and tendon gliding exercise group Received nerve and tendon gliding exercises for the affected hand. Before exercise, affected hand was placed in warm water (40° to 45°) for 4 minutes and in cold water (20° to 25°) for 1 minute. Median nerve gliding exercises were performed at 6 positions: (1) wrist in neutral position, thumb and fingers flexed; (2) wrist in neural position, fingers and thumb extended; (3) wrist and fingers extended, thumb in neutral position; (4) wrist, fingers and thumb extended; (5) forearm in supination; and (6) opposite hand applying a gentle stretch to the thumb. Tendon gliding exercises were performed in 5 positions: (1) starting with the fingers straight; (2) hook fist followed by return to straight hand; (3) making a fist then returning to straight hand; (4) making a table‐top; and (5) making a straight fist then returning to straight hand. Each exercise was performed 3 to 5 times a day. Every position was maintained for several seconds and was repeated 5 times at each session for a total of 3 to 5 sessions per day |
|
| Outcomes |
Time points Outcomes were assessed 4 weeks after completion of 6 weeks of treatment (i.e. 10 weeks after randomisation) Description of outcomes • Pain intensity on a visual analogue scale (VAS). Participants were asked to rate their pain on a 0 to 10 scale (0 = no pain; 10 = worst possible pain) • Thenar muscle pinch strength assessed by a Jamar pinch dynamometer IL 60440‐4989 model. Participants were asked to apply firm pressure with the thumb and index finger of the affected hand 3 times, and the average was taken • Motor and sensory distal latency of the median nerve assessed by an EMG machine of TOENNIES Neuroscreen Plus system Motor distal latency: In a seated position, active surface electrodes were placed over the motor point of the abductor pollicis brevis muscle, while a reference electrode was placed over the proximal phalanx of the thumb 3 to 4 cm distal to the active electrode. Group electrode was placed over the dorsum of the hand between stimulating and recording electrodes. Stimulating electrodes were placed between flexor digitorum superficialis and flexor carpi radialis tendons as first stimulation, and were placed at the elbow (cubital fossa) as second stimulation Sensory distal latency: Ring electrode of the index finger was used, and electrophysiological examination was performed at baseline before and after treatment by standard techniques |
|
| Notes | Participants had transverse carpal ligament release only of the dominant hand. Therefore a unit of analysis error could not have occurred | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly classified into three equal groups of 15, random allocation was conducted by folding 45 papers and placing them in a bag ‐ three series of 15 papers were written with either US Gr, LASER Gr, or Ex Gr, each patient had to pull one folded paper from the bag" Comment: It appears that the random sequence was adequately generated (i.e. drawing of lots) |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomly classified into three equal groups of 15, random allocation was conducted by folding 45 papers and placing them in a bag – three series of 15 papers were written either US Gr, LASER Gr or Ex Gr, each patient had to pull one folded paper from the bag" Comment: An adequate method was used to conceal the sequence |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Quote: "The study was double blinded, as both patient and physical therapist did not know which group the patients were allocated to (one independent blinded assessor from the admission office of the outpatient clinic of health insurance hospital performed the pre & post assessment without knowing in which group the patients were allocated to or knowing what the patients had received. Treatment was performed by another independent outpatient physical therapist" Comment: Given the nature of the intervention, it is unclear how participants could have been blinded to the intervention they received. The physical therapist was not blinded |
| Blinding (performance bias and detection bias) Other outcomes | Low risk | Quote: "The study was double blinded, as both patient and physical therapist did not know in which group the patients were allocated to (one independent blinded assessor from the admission office of the outpatient clinic of health insurance hospital performed the pre & post assessment without knowing in which group the patients were allocated to or knowing what the patients had received. Treatment was performed by another independent physical therapist" Comment: It appears that outcome assessors were blinded |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Comment: No attrition was reported, and outcome data reported were based on the number of participants reportedly randomly assigned |
| Incomplete outcome data (attrition bias) After 12 weeks | Unclear risk | This was not reported |
| Selective reporting (reporting bias) | Low risk | All outcomes specified in the Methods section of the publication were reported in the Results in the prespecified way |
| Other bias | Low risk | Participants had only their dominant had operated on, so no unit of analysis errors occurred |
Stevinson 2003.
| Methods | Randomised, triple‐blind, placebo‐controlled trial Blinded participants, treaters and assessors |
|
| Participants |
Details of sampling framea Total n eligible = 90 participants Total n excluded prerandomisation = 26 participants (7 declined participation; 19 excluded) Total n randomised = 64 participants (64 wrists) Total n available for follow‐up = 62 participants (62 wrists)b Total n analysed = 62 participants (62 wrists)b Intervention group 1: n = 21 participants randomised; 20 completed trial Intervention group 2: n = 21 participants randomised; 20 completed trial Placebo group 3: n = 22 participants randomised; 22 completed trial Gender distributionb Intervention group 1: 3 males; 17 females Intervention group 2: 8 males; 12 females Placebo group 3: 2 males; 20 females Mean ± SD (range) ageb Group 1: 47.5 years (range 30 to 68 years) Group 2: 51 years (range 30 to 68 years) Group 3: 51 years (range 33 to 57 years) Inclusion criteria
Exclusion criteria
CTS Diagnosis (case definition) Not reported Details of surgical intervention
Symptom severity Not reported |
|
| Interventions |
Intervention group 1: high (30C) homeopathic arnica tablets to be taken 3 times daily for 7 days preoperatively and 14 days postoperatively Intervention group 2: low (6C) homeopathic arnica tablets to be taken 3 times daily for 7 days preoperatively and 14 days postoperatively Placebo group 3: placebo tablets (indistinguishable from arnica tablets) to be taken 3 times daily for 7 days preoperatively and 14 days postoperatively Participants were advised to refrain from handling the tablets and from eating, drinking, smoking or brushing teeth within 20 minutes of taking the tablets, and were asked to suck the tablets rather than simply swallow them. Homeopathic and placebo tablets were supplied by A Nelson & Co Ltd (London, UK). For all participants after surgery, a palmar plaster splint was applied to maintain the wrist in slight dorsiflexion, allowing the fingers to be gently mobilised within the dressing, and the hand was elevated in a high sling. Oral analgesic medication (paracetamol or diclofenac) was routinely prescribed on discharge. All participants were seen by the physiotherapist at 4, 9, and 14 days post surgery. At day 4, the splint was removed, and digits and wrists were mobilised. A Futura aluminium wrist splint was given to participants to wear for an additional week. Sutures were removed at day 14 |
|
| Outcomes | • Pain assessed by the short‐form McGill Pain Questionnaire, which includes a 0 to 100 visual analogue scale (VAS) to indicate the intensity of pain and a list of 15 descriptive words (e.g. stabbing, gnawing, shooting), each rated on a 4‐point scale (0 = none, 1 = mild, 2 = moderate, 3 = severe), yielding a total score ranging from 0 to 45. Measured presurgery and at 4, 9 and 14 days post surgeryb • Objectively measured bruising: a photograph of the participant's wrist at the distal crease taken under standard lighting conditions. For each participant, frames representative of normal skin (thenar zone) and of bruised areas (operative site) were selected. The distribution of red and blue pixels within each frame was calculated. This information, displayed as a histogram of the number of pixels (y‐axis) against an increasing scale of colour brightness from 0 to 255 (x‐axis), enabled a comparison of the colour of the bruised area against the colour of the normal skin. Measured at 4, 9 and 14 days post surgeryb • Clinician‐rated bruising, assessed independently by 2 plastic surgeons on a 3‐point scale (0 = none, 1 = mild‐moderate, 2 = severe). Measured at 4, 9, and 14 days post surgeryb • Swelling: measured as wrist circumference (mm) at the distal wrist crease. Three readings were taken of each measurement. Measured presurgery and at 4, 9, and 14 days post‐surgeryb • Use of analgesic medication measured daily in the first 4 days post surgery by ticking boxes in the study diary to indicate the number of tablets taken each dayc • Adverse events with the medication |
|
| Notes |
aIt is assumed that all participants had only 1 CTS‐affected wrist, as 1 of the exclusion criteria was "subsequently undergoing surgery on the other hand", and in Table 1 (pg. 62), the numbers of right and left hands receiving surgery per group were reported, and the sum total was 64 hands. A unit of analysis error is unlikely to have occurred bData were reported only for participants completing treatment (n = 62). Endpoint and change score data were reported only as median values (range), which are not appropriate for entry into RevMan 5 for statistical analysis. cThis outcome was not specified in our review, so data were not entered for statistical analysis Attempts to contact trial authors for incomplete or unclear data were unsuccessful |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Medication bottles were labelled with study numbers derived from a computer‐generated randomisation list in blocks of three by an individual not involved with running the trial" Comment: The randomisation sequence probably was generated adequately |
| Allocation concealment (selection bias) | Low risk | Quote: "Medication bottles were labelled with study numbers derived from a computer‐generated randomisation list in blocks of three by an individual not involved with running the trial. The randomisation list was kept in a sealed envelope in a locked drawer until the end of the trial" Comment: The allocation sequence probably was adequately concealed until interventions were assigned |
| Blinding (performance bias and detection bias) Self reported outcomes | Low risk | Quote: "All patients and investigators, including the surgeon, physiotherapists and data analysts, remained blind to treatment allocation until after data analysis" Quote: "Patient blinding seemed to remain intact throughout the study. 7/20 patients in the arnica 6C group, 3/22 in the placebo group and 7/20 in the arnica 30C group correctly identified their treatment allocation at the end of the trial" Comment: Participants probably were blind to treatment allocation |
| Blinding (performance bias and detection bias) Other outcomes | Low risk | Quote: "All patients and investigators, including the surgeon, physiotherapists and data analysts, remained blind to treatment allocation until after data analysis" Comment: Outcome assessors probably were blind to treatment allocation |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote: "Of the 64 patients recruited to the trial, 62 were included in the analysis. One patient in the arnica 6C group did not undergo the scheduled surgery so was no longer eligible for the trial and one patient from the arnica 30C group withdrew from the study before undergoing surgery because she believed that the tablets were causing her to feel 'unhappy or low'" Quote: "In total there were data missing at one or more time points on at least one outcome for 10 patients ‐ 3 of these were from the arnica 6C group, 5 from the placebo group and 2 from the arnica 30C group" Quote: "Intention‐to‐treat analyses were conducted on all randomised patients remaining in the trial at the time of surgery. Missing data were replaced with the median value of the total sample" Comment: Incomplete outcome data were clearly addressed |
| Incomplete outcome data (attrition bias) After 12 weeks | High risk | Comment: This was not applicable, as the latest follow‐up was done at the end of treatment (14 days post surgery) |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes specified in the Methods section of the publication were reported in the prespecified way |
| Other bias | Unclear risk | Quote: "Adherence was incomplete in all three groups. As judged by tablet counts at the end of the trial, the number of patients who had taken less than 90% of their tablets was 9/20 for the arnica 6C group, 7/22 for the placebo group and 6/20 for the arnica 30C group" Comment: It is not clear whether these protocol violators significantly influenced the data obtained |
Williams 2008.
| Methods | Single‐blind RCT Blinded outcome assessors |
|
| Participants |
Details of sampling framea Total n eligible = not reported Total n excluded prerandomisation = not reported Total n randomised = 100 participants (100 wrists) Total n available for follow‐up = 100 participants (100 wrists) Total n analysed = 100 participants (100 wrists) Intervention group 1: n = 49 participants Intervention group 2: n = 51 participants Gender distribution Group 1: 9 males; 40 females Group 2: 13 males; 38 females Mean ± SD (range) age Group 1: 57 ± 13.4 years Group 2: 55 ± 14.5 years Mean ± SD (range) duration of CTS symptoms Not reported Inclusion criteria
Exclusion criteria Not reported CTS diagnostic criteria (case definition)b Diagnosis was made from patient history and clinical examination. If any doubt arose, nerve conduction studies were performed Details of surgical interventionb Open CTR was performed under local anaesthetic with a tourniquet Symptom severity Not reported |
|
| Interventions |
Group 1: bulky dressing for 24 hours In Group 1, the hand was shown to the participant, and it was explained that the Mepore dressing should stay in place for the full 2‐week period. A bulky dressing of gauze, wool and crepe was placed over the top of the Mepore dressing. Participants were advised to remove the bulky gauze, wool and crepe after 24 hours Group 2: bulky dressing for 2 weeks Participants in Group 2 were advised to leave the bulky gauze, wool and crepe dressing in situ for 2 weeks, when they would be seen for a postoperative visit Participants in both groups were told to leave the Mepore dressing in place and to contact the department should they have any problems during the 2‐week interval |
|
| Outcomes | Outcomes assessed preoperatively and at the end of the 2‐week treatment period
|
|
| Notes |
aQuote (unpublished data): "No bilateral cases were performed as this was departmental procedure at the time. No patients who had treatment for both wrists at different times were included in the study as the time elapsed between treatments was longer than the study period and therefore patients could not be included twice" Comment: No unit of analysis error occurred bStudy authors were contacted to clarify unclear or unreported data. Unpublished data were obtained directly from study authors through personal communication |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Within a single list, performed by the same consultant or registrar plastic surgeon, patients could be randomly allocated to either of the two groups" Quote: "Patients were randomised preoperatively, at the time of consent, to a 24 h or 2 week group" Comment: Information was insufficient to reveal the adequacy of the random sequence generation Quote (unpublished data): "Pieces of paper were drawn from an envelope for each patient to dictate [to] which arm the patient was allocated"a Comment: The sequence was adequately generated |
| Allocation concealment (selection bias) | High risk | Quote: "Within a single list, performed by the same consultant or registrar plastic surgeon, patients could be randomly allocated to either of the two groups" Quote: "Patients were randomised preoperatively, at the time of consent, to a 24 h or 2 week group" Comment: Information was insufficient to reveal whether the allocation was concealed Quote (unpublished data): "All the numbers were drawn out of the same envelope and the numbers were then replaced so as to maintain the likelihood of drawing each arm for each patient"a Comment: The allocation does not appear to have been adequately concealed |
| Blinding (performance bias and detection bias) Self reported outcomes | High risk | Quote (unpublished data): "This [participant blinding] was not possible as if they were in the group who had the dressing for the shorter period, they had the dressing removed earlier"a Comment: Participants and personnel were not blind to treatment allocation |
| Blinding (performance bias and detection bias) Other outcomes | Low risk | Quote (unpublished data): "Post‐operatively all patients had the same scars and no dressings. Patients did not tell, [nor] assessors ask, how long the dressing had been applied and therefore all patients appeared the same to the assessors, independently of the study arm to which they had been allocated. The scores could them be matched to the intervention"a Comment: Outcome assessors were adequately blinded |
| Incomplete outcome data (attrition bias) 12 weeks or less | Low risk | Quote (unpublished data): "All patients returned for post‐operative visits and were assessed"a Quote: "No patients in the longer dressing wearers removed their dressing early. They were all still on at 2 weeks and no patients who were supposed to leave the dressing on briefly left it on for 2 weeks" Comment: Results were based on a complete data set. No protocol violators were identified |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the Methods were reported in the Results section of the publication. All outcomes were reported numerically with appropriate statistical analysis |
| Other bias | Low risk | No other sources of bias were identified |
ADL: activities of daily living
BCTQ: Boston Carpal Tunnel Questionnaire
CCT: controlled cold therapy
CI: confidence interval
CT: carpal tunnel
CTR: carpal tunnel release
CTS: carpal tunnel syndrome
EMG: electromyography
MPQ: McGill Pain Questionnaire
NAP: nerve action potential
RCT: randomised controlled trial
SD: standard deviation
SE: standard error
SNAP: sensory nerve action potential
STI: Shape‐Texture Identification test
TCL: transverse carpal ligament
VAS: visual analogue score or scale
WEST: Weinstein Enhanced Sensory Test
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Atherton 1999 | Not a study investigating a rehabilitation treatment following carpal tunnel surgery |
| Chaise 1994 | Not a study investigating a rehabilitation treatment following carpal tunnel surgery |
| Chmielewska 2013 | Not an RCT |
| Cornesse 2010 | Not a study investigating a rehabilitation treatment following carpal tunnel surgery |
| Gupta 2011 | Not a study investigating a rehabilitation treatment following carpal tunnel surgery |
| Heuser 2007 | Not a RCT |
| Husby 2001 | Not a study investigating a rehabilitation treatment following carpal tunnel surgery |
| Karamanis 2011 | Not a study investigating a rehabilitation treatment following carpal tunnel surgery. |
| Ozer 2005 | Not a study investigating a rehabilitation treatment following carpal tunnel surgery |
| Romeo 2011 | Not a RCT |
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Dehghani 2014.
| Methods | RCT |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Only the abstract has been retrieved. We are awaiting the full text for review |
Fibir 2014.
| Methods | RCT |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | This study is awaiting translation from Czechoslavakian |
Gordon 2007.
| Methods | RCT |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | It is unknown whether this data set is a separate data set for Gordon 2010; hence further clarification has been sought from trial authors. No response from trial authors has yet been received |
NCT00435149.
| Methods | RCT (single‐blinded outcome assessor)a |
| Participants |
Details of sampling frame Estimated enrolment: 100 participants Setting: Vanderbilt Orthopaedic Institute & Vanderbilt University Inclusion criteria
Patient selection factors include
Exclusion criteria
Surgical details
|
| Interventions |
Intervention group 1: immobilisation for 1 week post surgery CTR followed by splinting Intervention group 2: no immobilisation post surgery CTR followed by a bandage over the incision site after surgery |
| Outcomes | Participants will be followed up for 6 months
|
| Notes | aTrial investigators have indicated through private correspondence that this study has been completed as a pilot but was not published. They have not provided further data to enable risk of bias evaluation nor data for meta‐analysis |
CTR: carpal tunnel release
CTS: carpal tunnel syndrome
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
NCT00845325.
| Trial name or title | RCT (single‐blinded outcome assessor)a |
| Methods |
Details of sampling frame Estimated enrolment: 100 participants Setting: Vanderbilt Orthopaedic Institute & Vanderbilt University Inclusion criteria
Patient selection factors include
Exclusion criteria
Surgical details Open CTR |
| Participants |
Intervention group 1: immobilisation for 1 week post surgery CTR followed by splinting Intervention group 2: no immobilisation post surgery CTR followed by a bandage over the incision site after surgery |
| Interventions | Participants will be followed up for 6 months
|
| Outcomes | aTrial investigators have indicated through private correspondence that this study has been completed as a pilot but was not published. They have provided no additional data to enable risk of bias evaluation nor data for meta‐analysis |
| Starting date | December 2008 |
| Contact information | Stephen Colbert, University of Missouri‐Columbia |
| Notes |
CTR: carpal tunnel release
CTS: carpal tunnel syndrome
RCT: randomised controlled trial
Differences between protocol and review
We updated 'Risk of bias' methods and added outcomes for inclusion in a 'Summary of findings' table. We updated background information to reflect changes in the literature since the protocol was published in 2003. We updated references to previous versions of RevMan software. We expanded 'types of interventions' included in this review to include rehabilitation interventions, and we excluded interventions related to postoperative analgesia. We modified outcomes from the original protocol (O'Connor 2003) for the review for consistency with other Cochrane reviews on CTS (Marshall 2007; Page 2012a; Page 2012b; Page 2012c; O'Connor 2012; Scholten 2007; Vasiliadis 2013; Verdugo 2008). In addition, we included secondary outcomes regarding return to work. We amended subgroup analyses to reflect current surgical interventions. We removed from the review 'timing of rehabilitation' and 'other concomitant conditions' subgroup analyses. We amended the sections on 'assessment of heterogeneity' and 'sensitivity analysis' since the protocol was formulated. We added sections on 'unit of analysis' and 'assessment of reporting biases'.
We included in the most recently published version of this review an overall grading of the evidence based on the GRADE approach, in keeping with Cochrane recommendations since the time the previous version of this review was published.
Denise O'Connor and Cathy Dabourn withdrew from authorship after publication of the protocol, and a new team of review authors amended the existing protocol as indicated in this review in accordance with guidelines provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Contributions of authors
SUSAN PETERS (SP) was involved in the following aspects of the review: updating the most recent version of the review, design of the review (in collaboration with previous protocol authors); undertaking the search of studies (along with Angela Gunn of the Cochrane Neuromuscular Diseases Group); screening search results (independently of, but in addition to, MP); organising retrieval of papers; screening retrieved papers against inclusion/exclusion criteria (independently of, but in addition to, MP); appraising the risk of bias of papers (independently of, but in addition to, MP); extracting data from included studies (independently of, but in addition to, MP); writing to study investigators to ask for additional information; summarising the risk of bias of included studies; compiling the summary of comparisons and tables of included, excluded, awaiting and ongoing studies; entering data into RevMan; analysing data; interpreting study findings; writing the review; and providing final approval of the version to be published.
MATTHEW PAGE (MP) was involved in the following aspects of the review: updating the most recent version of the review, design of the review (in collaboration with previous protocol authors); screening the search results (independently of, but in addition to, SP); screening retrieved papers against inclusion/exclusion criteria (independently of, but in addition to, SP); appraising the risk of bias of papers (independently of, but in addition to, SP); extracting data from included studies (independently of, but in addition to, SP); entering data into RevMan; performing analysis of data; interpreting study findings; writing the review; and providing final approval of the version to be published.
VENERINA JOHNSTON (VJ) was involved in the following aspects of the review: designing the review (in collaboration with previous protocol authors); designating the third assessor for disputes; interpreting study findings; writing the review; and providing final approval of the version to be published.
MICHEL COPPIETERS (MC) was involved in the following aspects of the review: designing the review (in collaboration with previous protocol authors); interpreting study findings; writing the review; and providing final approval of the version to be published.
MARK ROSS (MR) was involved in the following aspects of the review: interpreting study findings; writing the review; and providing final approval of the version to be published.
Sources of support
Internal sources
Brisbane Hand and Upper Limb Rehabilitation Institute, Brisbane, Australia.
Division of Physiotherapy, School of Health and Rehabilitation Sciences, The University of Queensland, Australia.
External sources
No external sources of support were provided for this review, Other.
Declarations of interest
S Peters: none known.
MJ Page: none known.
MW Coppieters: none known.
M Ross: none known.
V Johnston: none known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Alves 2011 {published data only}
- Alves MPT, Araujo GCS. Low‐level laser therapy after carpal tunnel release. Revista Brasileira de Ortopedia 2011;46(6):697‐701. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bhatia 2000 {published data only}
- Bhatia R, Field J, Grote J, Huma H. Does splintage help pain after carpal tunnel release?. Journal of Hand Surgery (British and European Volume) 2000;25(2):150. [DOI: 10.1054/jhsb.1999.0365; PUBMED: 11062571] [DOI] [PubMed] [Google Scholar]
Bury 1995 {published data only}
- Bury TF, Akelman E, Weiss APC. Prospective, randomized trial of splinting after carpal tunnel release. Annals of Plastic Surgery 1995;35(1):19‐22. [PUBMED: 7574280] [DOI] [PubMed] [Google Scholar]
Cebesoy 2007 {published data only}
- Cebesoy O, Kose KC, Kuru I, Altinel L, Gul R, Demirtas M. Use of a splint following open carpal tunnel release: a comparative study. Advances in Therapy 2007;24(3):478‐84. [PUBMED: 17660155] [DOI] [PubMed] [Google Scholar]
Cook 1995 {published data only}
- Cook AC, Szabo RM, Birkholz SW, King EF. Early mobilization following carpal tunnel release. A prospective randomised study. Journal of Hand Surgery (British and European Volume) 1995;20(2):228‐30. [PUBMED: 7797977] [DOI] [PubMed] [Google Scholar]
Fagan 2004 {published data only}
- Fagan DJ, Evans A, Ghandour A, Prabhkaran P, Clay NRC. A controlled clinical trial of postoperative hand elevation at home following day‐case surgery. Journal of Hand Surgery (British and European Volume) 2004;29(5):458‐60. [PUBMED: 15336749] [DOI] [PubMed] [Google Scholar]
Finsen 1999 {published and unpublished data}
- Finsen V, Andersen K, Russwurm H. No advantage from splinting the wrist after open carpal tunnel release. A randomised study of 82 wrists. Acta Orthopaedica Scandinavica 1999;70(3):288‐92. [PUBMED: 10429608] [DOI] [PubMed] [Google Scholar]
Gordon 2010 {published data only}
- Gordon T, Amirjani N, Edwards DC, Chan KM. Brief post‐surgical electrical stimulation accelerates axon regeneration and muscle reinnervation without affecting the functional measures in carpal tunnel syndrome patients. Experimental Neurology 2010;223(1):192‐202. [PUBMED: 19800329] [DOI] [PubMed] [Google Scholar]
Hochberg 2001 {published data only}
- Hochberg J. A randomised prospective study to assess the efficacy of two cold‐therapy treatments following carpal tunnel release. Journal of Hand Therapy 2001;14(3):208‐15. [PUBMED: 11511016] [DOI] [PubMed] [Google Scholar]
Huemer 2007 {published data only (unpublished sought but not used)}
- Huemer GM, Koller M, Pachinger T, Dunst KM, Schwarz B, Hintringer T. Postoperative splinting after open carpal tunnel release does not improve functional and neurological outcome. Muscle and Nerve 2007;36(4):528‐31. [PUBMED: 17617802] [DOI] [PubMed] [Google Scholar]
Janssen 2009 {published data only (unpublished sought but not used)}
- Janssen RG, Schwartz DA, Velleman PF. A randomized controlled study of contrast baths on patients with carpal tunnel syndrome. Journal of Hand Therapy 2009;22(3):200‐7. [PUBMED: 19375278] [DOI] [PubMed] [Google Scholar]
Jeffrey 2002 {published data only (unpublished sought but not used)}
- Jeffrey SLA, Belcher HJCR. Use of Arnica to relieve pain after carpal‐tunnel release surgery. Alternative Therapies in Health and Medicine 2002;8(2):66‐8. [PUBMED: 11892685] [PubMed] [Google Scholar]
Jerosch‐Herold 2012 {published and unpublished data}
- Jerosch‐Herold C, Shepstone L, Miller L. Sensory relearning after surgical treatment for carpal tunnel syndrome: a pilot clinical trial. Muscle Nerve 2012;46:885‐90. [DOI] [PubMed] [Google Scholar]
Li 2008 {published data only (unpublished sought but not used)}
- Li G, Tian D, Yu J, Li W, Meng J. Synergistic effects of compound physical factor treatment on neurological outcome after peripheral nerve entrapment surgery. Neural Regeneration Research 2008;3(1):97‐100. [EMBASE: 2008144777] [Google Scholar]
Martins 2006 {published and unpublished data}
- Martins RS, Siqueira MG, Simplício H. Wrist immobilization after carpal tunnel release: a prospective study. Arquivos de Neuro‐Psiquiatria 2006;64(3A):596‐9. [PUBMED: 17119800] [DOI] [PubMed] [Google Scholar]
Pomerance 2007 {published data only (unpublished sought but not used)}
- Pomerance J, Fine I. Outcomes of carpal tunnel surgery with and without supervised postoperative therapy. Journal of Hand Surgery. American Volume 2007;32(8):1159‐63. [PUBMED: 17923296] [DOI] [PubMed] [Google Scholar]
Powell 2003 {unpublished data only}
- Powell F. Desensitisation techniques: do they reduce scar sensitivity following carpal tunnel release? (A pilot study). Unpublished Masters Thesis 2003.
Provinciali 2000 {published and unpublished data}
- Giattini A, Logullo F, Morici D, Castellani G, Provinciali L. Physiotherapy reduced the recovery time after carpal tunnel syndrome. Neurorehabilitation and Neural Repair 1999;13(1):51. [Google Scholar]
- Provinciali L, Giattini A, Splendiani G, Logullo F. Usefulness of hand rehabilitation after carpal tunnel surgery. Muscle and Nerve 2000;23(2):211‐6. [PUBMED: 10639613] [DOI] [PubMed] [Google Scholar]
Ritting 2012 {published data only (unpublished sought but not used)}
- NCT01310218. Length of post operative dressing after carpal tunnel release. www.clinicaltrials.gov/show/NCT01310218 (accessed 15 November 2012). [ClinicalTrials.gov Identifier: NCT01310218]
- Ritting AW, Leger R, O'Malley MP, Mogielnicki H, Tucker R, Rodner CM. Duration of postoperative dressing after mini‐open carpal tunnel release: a prospective, randomized trial. Journal of Hand Surgery. American Volume 2012;37(1):3‐8. [PUBMED: 22133704] [DOI] [PubMed] [Google Scholar]
Sawan 2013 {published data only}
- Sawan SA, Sayed Mahmoud HM, Hussien MM. Effect of different physical therapy modalities on post‐operative recovery following transverse carpal ligament release: a randomized controlled trial. Physiotherapy Practice and Research 2013;34(2):75‐82. [DOI: 10.3233/PPR-130024] [DOI] [Google Scholar]
Stevinson 2003 {published data only (unpublished sought but not used)}
- Stevinson C, Devaraj VS, Fountain‐Barber A, Hawkins S, Ernst E. Homeopathic arnica for prevention of pain and bruising: randomized placebo‐controlled trial in hand surgery. Journal of the Royal Society of Medicine 2003;96(2):60‐5. [PUBMED: 12562974] [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2008 {published and unpublished data}
- Williams AM, Baker PA, Platt AJ. The impact of dressings on recovery from carpal tunnel decompression. Journal of Plastic, Reconstructive and Aesthetic Surgery 2008;61(12):1493‐5. [PUBMED: 17983881] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Atherton 1999 {published data only}
- Atherton WG, Faraj AA, Riddick AC, Davis TR. Follow‐up after carpal tunnel decompression ‐ general practitioner surgery or hand clinic? A randomised prospective study. Journal of Hand Surgery. British Volume 1999;24(3):296‐7. [DOI] [PubMed] [Google Scholar]
Chaise 1994 {published data only}
- Chaise F, Guest M, Bellemère P, Friol JP, Gaisne E, Lehert P. The efficacy of naftidrofuryl on unexpected autonomic symptoms following carpal tunnel surgery. Annales de Chirurgie de la Main et du Membre Supérieur 1994;13(3):214‐21. [DOI] [PubMed] [Google Scholar]
Chmielewska 2013 {published data only}
- Chmielewska D, Skeczek‐Urbaniak A, Kubacki J, Blaszczak E, Kwasna K. Effectiveness of carpal tunnel syndrome rehabilitation after endoscopic versus open surgical release. Ortopedia Traumatologia Rehabilitacja 2013;5(6):417‐27. [DOI] [PubMed] [Google Scholar]
Cornesse 2010 {published data only}
- Cornesse D, Senard M, Hans GA, Kirsch M, Hick C, Hallet C, et al. Comparison between two intraoperative intravenous loading doses on pain after minor hand surgery: two grams versus one gram. Acta Chirurgica Belgica 2010;110(5):529‐32. [PubMed] [Google Scholar]
Gupta 2011 {published data only}
- Gupta A, Rawal N, Magnuson A, Alnehill H, Pettersson K. Patient controlled regional analgesia after carpal tunnel release: a double‐blind study using distal perineural catheters. Journal of Hand Surgery. European Volume 2011;36(3):219‐25. [DOI: 10.1177/1753193410390130] [DOI] [PubMed] [Google Scholar]
Heuser 2007 {published data only}
- Heuser A, Kourtev H, Winter S, Fensterheim D, Burdea G, Hentz V, et al. Telerehabilitation using the Rutgers Master II glove following carpal tunnel release surgery: proof‐of‐concept. IEEE Transactions of Neural Systems and Rehabilitation Engineering 2007;15(1):43‐9. [DOI] [PubMed] [Google Scholar]
Husby 2001 {published data only}
- Husby T, Haugstvedt JR, Fyllingen G, Skoglund LA. Acute postoperative swelling after hand surgery: an exploratory, double blind, randomised study with paracetamol, naproxen and placebo. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery 2001;35(1):91‐8. [DOI] [PubMed] [Google Scholar]
Karamanis 2011 {published data only}
- Karamanis N, Papanagiotoi M, Varitimidis S, Basdekis G, Stamatiou G, Dailiana Z, et al. The effect of local anaesthetics in rehabilitation after open carpal tunnel release. Journal of Bone and Joint Surgery. British Volume 2011;93‐B(Suppl II):219. [Google Scholar]
Ozer 2005 {published data only}
- Ozer H, Solak S, Oguz T, Ocguder A, Colakoglu T, Babacan A. Alkalinisation of local anaesthetics prescribed for pain relief after surgical decompression of carpal tunnel syndrome. Journal of Orthopaedic Surgery 2005;13(3):285‐9. [DOI] [PubMed] [Google Scholar]
Romeo 2011 {published data only}
- Romeo P, D'Agostino C, Lazzerini A, Sansone VC. Extracorporeal shock wave therapy in pillar pain after carpal tunnel release: a preliminary study. Ultrasound in Medicine and Biology 2011;37(10):1603‐8. [DOI: 10.1016/j.ultrasmedbio.2011.07.002] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Dehghani 2014 {published data only}
- Dehghani M, Alerasoul S, Saadatpoor L, Alerasoul M. Comparing the positive results of carpal tunnel syndrome surgery in two groups of patients with and without splint. Journal of Isfahan Medical School 2014;31(267):2155‐61. [Google Scholar]
Fibir 2014 {published data only}
- Fibir A, Cap R, Vanek J. Effectiveness of the temporary splinting after carpal tunnel release. Ceska a Slovenska Neurologie a Neurochirurgie 2014;77(6):691‐7. [Google Scholar]
Gordon 2007 {published data only (unpublished sought but not used)}
- Gordon T, Brushart TM, Amirjani N, Chan KM. The potential of electrical stimulation to promote functional recovery after peripheral nerve injury ‐ comparisons between rats and humans. Acta Neurochirurgica Supplement 2007;100:3‐11. [DOI] [PubMed] [Google Scholar]
NCT00435149 {published data only}
- NCT00435149. Post‐operative mobilisation of carpal tunnel syndrome. http://clinicaltrials.gov/ct2/show/NCT00435149 (accessed 3 December 2015).
References to ongoing studies
NCT00845325 {published data only}
- NCT00845325. Early motion following carpal tunnel release. http://clinicaltrials.gov/ct2/show/NCT00845325 (accessed 24 August 2015).
Additional references
AAOS 2007
- American Academy of Orthopedic Surgeons. Clinical practice guideline on the diagnosis of carpal tunnel syndrome. www.aaos.org/research/guidelines/CTS_guideline.pdf 2007 (accessed 16 November 2012).
Agee 1992
- Agee JM, McCarroll HR Jr, Tortosa RD, Berry DA. Szabo MR, Peimer CA. Endoscopic release of the carpal tunnel: a randomized prospective multicenter study. Journal of Hand Surgery. American Volume 1992;17(6):987‐95. [DOI] [PubMed] [Google Scholar]
Amick 2004
- Amick BC 3rd, Habeck RV, Ossmann J, Fossel AH, Keller R, Katz JN. Predictors of successful work role functioning after carpal tunnel release surgery. Journal of Occupational and Environmental Medicine 2004;46(5):490‐500. [DOI] [PubMed] [Google Scholar]
Armstrong 2008
- Armstrong T, Dale AM, Franzblau A, Evanoff BA. Risk factors for carpal tunnel syndrome and median neuropathy in a working population. Journal of Occupational and Environmental Medicine 2008;50(12):1355‐64. [DOI: 10.1097/JOM.0b013e3181845fb1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Aroori 2008
- Aroori S, Spence RA. Carpal tunnel syndrome. Ulster Medical Journal 2008;77(1):6‐17. [PMC free article] [PubMed] [Google Scholar]
Atroshi 1999
- Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosén I. Prevalence of carpal tunnel syndrome in a general population. JAMA 1999;282(2):153‐8. [DOI] [PubMed] [Google Scholar]
Barcenilla 2012
- Barcenilla A, Lmarch LM, Chen JS, Sambrook PN. Carpal tunnel syndrome and its relationship to occupation: a meta‐analysis. Rheumatology 2012;51:250‐61. [DOI: 10.1093/rheumatology/ker108] [DOI] [PubMed] [Google Scholar]
Bland 2001
- Bland JD. Do nerve conduction studies predict the outcome of carpal tunnel decompression?. Muscle and Nerve 2001;24(7):935‐40. [DOI] [PubMed] [Google Scholar]
Braun 2002
- Braun RM, Rechnic M, Fowler E. Complications related to carpal tunnel release. Hand Clinics 2002;18(2):347‐57. [DOI] [PubMed] [Google Scholar]
Bromley 1994
- Bromley GS. Minimal‐incision open carpal tunnel decompression. Journal of Hand Surgery. American Volume 1994;19(1):119‐20. [DOI: 10.1016/0363-5023(94)90234-8] [DOI] [PubMed] [Google Scholar]
Burt 2011
- Burt S, Crombie K, Wurzelbacker S, Ramsey J, Deddens J. Workplace and individual risk factors for carpal tunnel syndrome. Journal of Occupational and Environmental Medicine 2000;68:928‐33. [DOI: 10.1136/oem.2010.063677] [DOI] [PubMed] [Google Scholar]
Chow 1989
- Chow JCY. Endoscopic release of the carpal ligament: a new technique for carpal tunnel syndrome. Arthroscopy: The Journal of Arthroscopic and Related Surgery 1989;5(1):19‐24. [DOI: 10.1016/0749-8063(89)90085-6] [DOI] [PubMed] [Google Scholar]
Cowan 2012
- Cowan J, Makanji H, Mudgal C, Jupiter J, Ring D. Determinants of return to work after carpal tunnel release. Journal of Hand Surgery 2012;37(A)(1):18‐27. [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altmand DG. Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S editor(s). Cochrane Handbook of Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org, 2011. [Google Scholar]
DeStefano 1997
- DeStefano F, Nordstrom D, Vierkant RA. Long‐term symptom outcomes of carpal tunnel syndrome and its treatment. Journal of Hand Surgery. American Volume 1997;22(2):200‐10. [DOI] [PubMed] [Google Scholar]
Dwan 2008
- Dwan K, Altman DG, Arnaiz JA, Bloom J, Chan AW, Cronin E, et al. Systematic review of the empirical evidence of study publication bias and outcome reporting bias. PLoS One 2008;3(8):e3081. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dwan 2011
- Dwan K, Altman DG, Cresswell L, Blundell M, Gamble CL, Williamson PR. Comparison of protocols and registry entries to published reports for randomised controlled trials. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.MR000031.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Finestone 1996
- Finestone HM, Woodbury GM, Collavini T, Marchuk Y, Maryniak O. Severe carpal tunnel syndrome: clinical and electrodiagnostic outcome of surgical and conservative treatment. Muscle and Nerve 1996;19(2):237‐9. [DOI] [PubMed] [Google Scholar]
Gelberman 1998
- Gelberman RH, Rydevik BL, Pess GM, Szabo RM, Lundborg G. A scientific basis for clinical care. Orthopaedic Clinics of North America 1998;19(1):115‐24. [PubMed] [Google Scholar]
Gelfman 2009
- Gelfman R, Melton LJ Jr, Yawn BP, Wollan PC, Amadio PC, Stevens JC. Long‐term trends in carpal tunnel syndrome. Neurology 2009;72(1):33‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Geoghegan 2004
- Geoghegan JM, Clark DI, Bainbridge LC, Smith C, Hubbard R. Risk factors in carpal tunnel syndrome. Journal of Hand Surgery. British Volume 2004;29(4):315‐20. [DOI: 10.1016/j.jhsb.2004.02.009] [DOI] [PubMed] [Google Scholar]
Gerritsen 2001
- Gerritsen AAM, Uitdehaag BMJ, Geldere D, Scholten RJPM, Vet HCW, Bouter LM. Systematic review of randomized clinical trials of surgical treatment for carpal tunnel syndrome. British Journal of Surgery 2001;88(10):1285‐95. [DOI] [PubMed] [Google Scholar]
Giattini 1999
- Giattini A, Logullo F, Morici D, Castellani G, Provinciali L. Physiotherapy reduced the recovery time after carpal tunnel syndrome. Neurorehabilitation and Neural Repair 1999;13(1):51. [DOI: 10.1177/154596839901300188] [DOI] [Google Scholar]
Groves 1989
- Groves EJ, Rider BA. A comparison of treatment approaches used after carpal tunnel release surgery. American Journal of Occupational Therapy 1989;43(6):398‐402. [DOI] [PubMed] [Google Scholar]
Hayes 2002
- Hayes EP, Carney K, Wolf J, Smith JM, Akelman E. Carpal tunnel syndrome. In: Hunter JM, Mackin EJ, Callahan AD editor(s). Rehabilitation of the Hand and Upper Extremity. 5th Edition. St Louis: Mosby, 2002:643‐59. [Google Scholar]
Herbert 2000
- Herbert R, Gerr F, Dropkin J. Clinical evaluation and management of work‐related carpal tunnel syndrome. American Journal of Industrial Medicine 2000;37:62‐74. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Review of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. [Google Scholar]
Huisstede 2010
- Huisstede BM, Randsdorp MS, Coert JH, Glerum S, Middelkoop M, Koes BW. Carpal tunnel syndrome. Part II: effectiveness of surgical treatments ‐ a systematic review. Archives of Physical Medicine and Rehabilitation 2010;91(7):1005‐24. [DOI] [PubMed] [Google Scholar]
Hunter 1991
- Hunter JM. Recurrent carpal tunnel syndrome, epineural fibrous fixation and traction neuropathy. Hand Clinics 1991;7(3):491‐504. [PubMed] [Google Scholar]
Ibrahim 2012
- Ibrahim I, Khan WS, Goddard N, Smitham P. Carpal tunnel syndrome: a review of the recent literature. Open Orthopaedics Journal 2012;6(Suppl 1: M8):69‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Idler 1996
- Idler RS. Persistence of symptoms after surgical release of compressive neuropathies and subsequent management. Orthopedic Clinics of North America 1996;27(2):409‐16. [PubMed] [Google Scholar]
Isaac 2010
- Isaac S, Okoro T, Danial I, Wildin C. Does wrist immobilization following open carpal tunnel release improve functional outcome? A literature review. Current Reviews in Musculoskeletal Medicine 2010;3(1):11‐7. [DOI: 10.1007/s12178-010-9060-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jessurun 1988
- Jessurun W, Hillen B, Huffstadt AJC. Carpal tunnel syndrome: postoperative care. Handchirurgie, Mikrochirurgie, Plastiche Chirurgie 1988;20(1):39‐40. [PubMed] [Google Scholar]
Jüni 2001
- Jüni P, Altman DG, Egger M. Systematic reviews in health care: assessing the quality of controlled clinical trials. British Medical Journal 2001;323(7303):42‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Keilani 2002
- Keilani MY, Crevenna R, Fialka‐Moser V. Postoperative rehabilitation of patients with carpal tunnel syndrome. Wiener Medizinische Wochenschrift 2002;152(17‐18):479‐80. [DOI] [PubMed] [Google Scholar]
Kim 2004
- Kim JY, Kim J, Son JE, Yun SK. Prevalence of carpal tunnel syndrome in meat and fish processing plants. Journal of Occupational Health 2004;46(3):230‐4. [PUBMED: 5215667] [DOI] [PubMed] [Google Scholar]
Kirkham 2010
- Kirkham JJ, Dwan KM, Altman DG, Gamble C, Dodd S, Smyth R, et al. The impact of outcome reporting bias in randomised controlled trials on a cohort of systematic reviews. BMJ 2010;340:c365. [PUBMED: 20156912] [DOI] [PubMed] [Google Scholar]
Lam 1998
- Lam N, Thurston A. Association of obesity, gender, age and occupation with carpal tunnel syndrome. Australian and New Zealand Journal of Surgery 1998;68(3):190‐3. [DOI] [PubMed] [Google Scholar]
Latinovic 2006
- Latinovic R, Gulliford MC, Hughes RAC. Incidence of common compressive neuropathies in primary care. Journal of Neurology, Neurosurgery and Psychiatry 2006;77(2):263‐5. [DOI: 10.1136/jnnp.2005.066696] [DOI] [PMC free article] [PubMed] [Google Scholar]
Louie 2012
- Louie D, Earp B, Blazar P. Long‐term outcomes of carpal tunnel release: a critical review of the literature. Hand 2012 June 22;Online:1‐5. [DOI: 10.1007/s11552-012-9429-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marshall 2007
- Marshall SC, Tardif G, Ashworth NL. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD001554.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nathan 1993
- Nathan PA, Meadows KD, Keniston RC. Rehabilitation of carpal tunnel surgery patients using a short surgical incision and an early program of physical therapy. Journal of Hand Surgery. American Volume 1993;18(6):1044‐50. [DOI] [PubMed] [Google Scholar]
O'Connor 2003
- O'Connor D, Daborn C. Rehabilitation treatments following carpal tunnel surgery. Cochrane Database of Systematic Reviews 2003, Issue 2. [DOI: 10.1002/14651858.CD004158] [DOI] [Google Scholar]
O'Connor 2012
- O'Connor D, Page MJ, Massy‐Westropp N. Ergonomic positioning or equipment for treating carpal tunnel syndrome. Cochrane Database of Systematic Reviews 2012, Issue 1. [DOI: 10.1002/14651858.CD009600] [DOI] [PMC free article] [PubMed] [Google Scholar]
Odgaard‐Jensen 2011
- Odgaard‐Jensen J, Vist GE, Timmer A, Kunz R, Akl EA, Schünemann H, et al. Randomisation to protect against selection bias in healthcare trials. Cochrane Database of Systematic Reviews 2011, Issue 4. [DOI: 10.1002/14651858.MR000012.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Page 2012a
- Page MJ, O'Connor D, Pitt V, Massy‐Westropp N. Therapeutic ultrasound for carpal tunnel syndrome. Cochrane Database of Systematic Reviews 2012, Issue 1. [DOI: 10.1002/14651858.CD009601] [DOI] [PubMed] [Google Scholar]
Page 2012b
- Page MJ, O’Connor D, Pitt V, Massy‐Westropp N. Exercise and mobilisation interventions for carpal tunnel syndrome. Cochrane Database of Systematic Reviews 2012, Issue 6. [DOI: 10.1002/14651858.CD009899] [DOI] [PMC free article] [PubMed] [Google Scholar]
Page 2012c
- Page MJ, Massy‐Westropp N, O'Connor D, Pitt V. Splinting for carpal tunnel syndrome. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD010003] [DOI] [PMC free article] [PubMed] [Google Scholar]
Palmer 2007
- Palmer KT, Harris CE, Coggon D. Carpal tunnel syndrome and its relation to occupation: a systematic literature review. Occupational Medicine 2007;57(1):57‐66. [DOI] [PubMed] [Google Scholar]
Peters 2014
- Peters S, Coppieters M, Johnston V. Interpreting systematic reviews: looking beyond the all too familiar conclusion. Journal of Hand Therapy 2014;27(1):1‐3. [DOI] [PubMed] [Google Scholar]
Phalen 1966
- Phalen GS. The carpal tunnel syndrome. Seventeen years' experience in diagnosis and treatment of six hundred and fifty‐four hands. Journal of Bone and Joint Surgery 1966;48(2):211‐28. [PubMed] [Google Scholar]
Rempel 1998
- Rempel D, Evanoff B, Amadio PC, Krom M, Franklin G, Franzblau A, et al. Consensus criteria for the classification of carpal tunnel syndrome in epidemiologic studies. American Journal of Public Health 1998;88(10):1447‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2012 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
Sanati 2011
- Sanati KA, Mansouri M, Macdonald D, Ghafghazi S, Macdonald E, Yadegarfar G. Surgical techniques and return to work following carpal tunnel release: a systematic review and meta‐analysis. Journal of Occupational Rehabilitation 2011;21(4):474‐81. [DOI] [PubMed] [Google Scholar]
Scholten 2007
- Scholten RJPM, Mink van der Molen A, Uitdehaag BMJ, Bouter LM, Vet HCW. Surgical treatment options for carpal tunnel syndrome. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD003905.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schunemann 2011b
- Schunemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting and drawing conclusions. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. www.cochrane‐handbook.org. The Cochrane Collaboration, 2011. [Google Scholar]
Schünemann 2011a
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and 'Summary of findings' tables. In: Higgins JPT, Green S editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. www.cochrane‐handbook.org, 2011. [Google Scholar]
Skirven 1994
- Skirven T, Trope J. Complications of immobilization. Hand Clinics 1994;10(1):53‐61. [PubMed] [Google Scholar]
Stanek 1996
- Stanek EJ 3rd, Pransky G. Unilateral vs. bilateral carpal tunnel: challenges and approaches. American Journal of Industrial Medicine 1996;29(6):669‐78. [DOI] [PubMed] [Google Scholar]
Stapleton 2006
- Stapleton MJ. Occupation and carpal tunnel syndrome. ANZ Journal of Surgery 2006;76(6):494‐6. [DOI: 10.1111/j.1445-2197.2006.03770.x] [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D. Addressing reporting biases. In: Higgins JPT, Green S, editor(s). Cochrane Handbook of Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Stevens 1997
- Stevens JC. AAEM minimonograph #26: the electrodiagnosis of carpal tunnel syndrome. American Association of Electrodiagnostic Medicine. Muscle and Nerve 1997;20(12):1477‐86. [DOI] [PubMed] [Google Scholar]
Szabo 1994
- Szabo RM, Steinberg DR. Nerve entrapment syndromes in the wrist. Journal of the American Academy of Orthopedic Surgeons 1994;2(2):115‐23. [DOI] [PubMed] [Google Scholar]
Van Rijn 2009
- Rijn RM, Huisstede BMA, Koes BW, Burdorf A. Associations between work‐related factors and the carpal tunnel syndrome ‐ a systematic review. Scandinavian Journal of Work, Environment and Health 2009;35(1):19‐36. [DOI] [PubMed] [Google Scholar]
Vasiliadis 2013
- Vasiliadis HS, Georgoulas P, Shrier I, Salanti G, Scholten RJ. Endoscopic release for carpal tunnel syndrome. Cochrane Database of Systematic Reviews 2014, Issue 1. [DOI: 10.1002/14651858.CD008265.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Verdugo 2008
- Verdugo RJ, Salinas RS, Castillo J, Cea JG. Surgical versus non‐surgical treatment for carpal tunnel syndrome. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD001552.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2003
- Wilson JK, Sevier TL. A review of treatment for carpal tunnel syndrome. Disability and Rehabilitation 2003;25(3):113‐9. [DOI: 10.1080/0963828021000007978] [DOI] [PubMed] [Google Scholar]
Wood 2008
- Wood l, Egger M, Gluud LL, Schulz KF, Jüni P, Altman DG, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta‐epidemiological study. BMJ 2008;336(7644):601‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wyatt 2012
- Wyatt MC, Gwynne‐Jones DP, Veale GA. Lamb boning ‐ an occupational cause of carpal tunnel syndrome?. Journal of Hand Surgery. European Volume 2012;38(1):61‐6. [DOI: 10.1097/JOM.0b013e3181845fb1] [DOI] [PubMed] [Google Scholar]
Zanette 2010
- Zanette G, Cacciatori C, Tamburin S. Central sensitization in carpal tunnel syndrome with extraterritorial spread of sensory symptoms. Pain 2010;148(2):227‐36. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Peters 2013
- Peters S, Page MJ, Coppieters MW, Ross M, Johnston V. Rehabilitation following carpal tunnel release. Cochrane Database of Systematic Reviews 2013, Issue 6. [DOI: 10.1002/14651858.CD004158.pub2] [DOI] [PubMed] [Google Scholar]


