Abstract
Objective:
Breast cancer is a highly prevalent cancer in females worldwide, with new cases around one million every year. In Pakistan, cancer of breast is the most common carcinoma in diagnosis, with one in nine females. Due to high burden of breast cancer in Pakistan, presented work purposes to investigate knowledge and awareness of breast carcinoma, its symptoms, and risk factors among Pakistani women, which play an important part in the early diagnosis of breast cancer.
Methods:
A sample of 1000 females were approached generally from universities, hospitals, public places, local markets, rural areas and other cities for on-site data collection through face-to-face interviews and online data collection through telephonic interviews in Pakistan using the Breast Cancer Awareness Measure (BCAM). By using SPSS V. 25.0, the information provided by the individuals first changed in awareness scores and was then analyzed.
Results:
The study displayed, that mainstream participants lacked knowledge of breast carcinoma (63.2%) and the importance of its screening tools (64.7% and 83.2% lacked knowledge of mammography and BRCA tests respectively) for early detection. Almost 45% of respondents never noticed a change in their breasts. Most participants were unaware about breast cancer development is age-related and lifetime risk. Slightly more than 50% of the participants of the study were not knowledgeable regarding modifiable risk factors of breast carcinoma. A commonly known symptom was Breast lump by 53% of the respondents. Association was determined between demographic variables and breast cancer knowledge scores. Only 37.4% of respondents were found to be knowledgeable regarding breast cancer.
Conclusion:
BCAM is a productive instrument to assess awareness of breast carcinoma in females. The study indicated awareness of breast cancer is suboptimal in the population of Pakistan. Efforts should be made by public awareness campaigns and broadcasting of information about breast cancer and health education to increase awareness of risk factors.
Key Words: Breast cancer awareness measurement, symptoms, prevention, barriers
Introduction
Breast cancer is the most frequent malignant tumor of breasts in women globally (Ferlay et al., 2015). According to WHO figures, each year 1.5M women are diagnosed with breast cancer throughout the world (Zahra et al., 2013). Incidences of breast carcinoma are rapidly growing in Asia contributing to a global burden of disease. The prevalence in Pakistan is the highest in Asia demonstrating that 1 in 9 women is positive for breast cancer (Ghoncheh et al., 2015). The occurrence, mortality and morbidity level of breast cancer among women increased in low as well as in high-resource settings because of increased urbanization (Liu et al., 2014).
Knowledge of BC risk factors that includes age, weight, reproductive health, lifestyle, history, alcohol intake, smoking, age at menarche, menopause and early diagnosis can help to reduce the mortality rates and hazardous complications of breast cancer. In case of breast cancer, knowledge about signs, symptoms and techniques including mammography, molecular testing and self-examination is crucial for improving the patient’s prognosis (Saeed et al., 2014). Breast cancer survival rate fluctuates significantly around the world, up to 80%, 60% and 40% in high-, middle- and low-income countries respectively because developed countries have high awareness levels about early diagnosis and treatment of breast cancer (Qasim et al., 2020).
Breast cancer awareness means whether a woman has knowledge of breast carcinoma and has confidence to diagnose breast changes and report these changes promptly to healthcare providers. Breast Cancer Awareness Measurement (BCAM) is an authentic tool for measuring awareness of breast carcinoma in UK females and is easy to learn compared to adult literature (Linsell et al, 2010). Breast Cancer Awareness Measure properties in a diverse population have reported satisfactory reliability and validity (Liu et al., 2019).
Breast Health Global Initiative (BHGI) reports show that breast cancer could be easier to manage and earlier to diagnose, if women have proper knowledge of breast cancer (Amin et al., 2020). So far, awareness of breast carcinoma, signs & symptoms and risk factors and breast checking frequency are not measured among the women in Pakistan. Therefore, a questionnaire-based survey has been conducted to discover the real situation of current knowledge, attitude and awareness regarding the disease among women in Pakistan. Generally, inadequate knowledge, the gap in awareness, ignorance act and low education are major reasons behind late breast cancer detection.
Materials and Methods
Study design
A cross-sectional descriptive study was carried out to measure breast tumor awareness in Pakistani women. The methodological study was performed from September 2019 to February 2021 among 1147 Pakistani women. A random sampling technique was used to choose general women from various areas of Pakistan.
Questionnaire design and ethical consideration
The ethical committee (School of biological sciences), Punjab University has approved the modus operandi of the study regarding the research on humans. Consent was taken against each topic of the study before gathering the data. This is a questionnaire-based study, during designing the protocols, a careful approach was used to discuss the problems like early symptoms of breast cancer and related risk factors.
Participants
General guidelines recommend that routine breast carcinoma screening should perform on both types of females (at high or low risk). General population was taken as a sample group in other versions of BCAM in different countries (Liu et al., 2019). Therefore, this study implemented a suitable sampling method, and general public females were recruited to contribute to the survey. A total of 1,147 women with inclusion criteria of ≥14 age and able to understand/speak Urdu or English) were selected. The purpose of the study was communicated to all the respondents, and they can refuse or accept to participate as well of their own will. Almost 147 participants who did not answer questions of Breast Cancer Awareness Measures were excluded and 1,000 surveys were filled by females from schools, colleges, universities, and various public places of Pakistan.
Data collection from participants
Two methods were adopted for the collection of data: online data collection through telephonic interviews and face-to-face interviews. There were two steps followed for data gathering; first, all the questionnaire was transferred to the computer to make an electronic form of BCAM survey and secondly, the file of the questionnaire was filled one by one via telephonic interviews.
Breast Cancer Awareness Measurement (BCAM) tool
A joint work among Cancer Research UK, University College London and King’s College London was done and they established the BCAM to assess the knowledge of women about breast carcinoma. Linsell (2010) validated the consistency of the BCAM. BCAM comprises seven areas as follows: 1) Knowledge of symptoms, 2) Confidence, skills and behavior concerning detecting a breast change, 3) Delay in contacting the doctor, 4) Barriers in medical assistance, 5) Age-related and lifetime risk knowledge, 6) Knowledge of the NHS Screening Programme and 7) Risk factors information. The present study was conducted on six domains (1, 2, 3, 4, 5 and 7) based on expert advice that applied to the Pakistani population.
Statistical analysis
Data were recorded taken from study results and analyzed by SPSS V.25.0. The categorical variables were measured using frequency percentage, mean and standard deviation (SD); p<0.05 was found statistically significant. Association between demographic factors and Breast self-examination were measured using the multivariate logistic regression model and adjusted odd ratios (OR) & 95% confidence intervals (CI) were calculated. The cross-tabulation and descriptive statistics were applied. The Chi-square test was used to determine the association between socioeconomic status and knowledge of mammograms and BRCA. The scoring of responses was calculated. The correct response was considered equal to 1 which means sufficient knowledge and the wrong answer was considered as 0 score which means insufficient knowledge. A total score of each respondent was calculated by summing the correct responses of four domains 1: information of symptoms, 2: data related to age- & life-time risk, 3: Knowledge of screening tools & 4: risk factors’ knowledge), that make an aggregate of 24 questions. A total score of 0-12 was considered as insufficient knowledge while score more than 12 were categorized as sufficient knowledge. Association was assessed between mean score of knowledge and demographic factors.
Health behavior parameters
Health behavior characteristics were calculated, as defined by Shahab et al., 2018. Body Mass Index of participants were measured by height & weight and respondents were categorized into 4-BMI-based classes; 1) underweight (< 18.5 kg/m²), 2) normal/healthy weight (18.5 kg/m² - 24.9 kg/m²), 3) overweight (25.0 kg/m² - 29.9 kg/m²) and 4) obese (≥ 30 kg/m²). Respondents who were performing the physical activity for more than 30 min on at least five days per week considered that they are fulfilling guidelines. Participants were asked about their smoking status and were classified as ex-smokers, smokers, or never-smokers (Milton et al., 2011). Fruit/vegetable consumption levels were also assessed and participants that claim to consume at least five days/week were found as achieving guidelines. Cumulative behavior score was calculated – individuals that didn’t meet guidelines were given a score of 1 which means high risk, the only case of smoking, two scored for current smoking and one for past smoking. As consumption of alcohol is illegal in Pakistan and people tend to hide facts or lie in response to this question, we did not calculate the alcohol consumption levels of participants. This concluded that the high score shows a high risk for the overall health behavior range of 0-5.
Results
A total of 1,000 respondents participated in the survey out of 1147 and the response rate was found to be 87.2%.
Demographic characteristics and knowledge of screening tools, Confidence/skills/behavior concerning breast changes, anticipated delay in contacting the doctor, age-related and lifetime risk
The majority of respondents in the presented work were 18-35 years age group (82.0%). The mean age was found to be 27.4 ± 9.70 years and range of age was 15 to 80 years. The socioeconomic status of white-collar workers was 76.5% while the marital status of single was 64.5%. Approximately 50.2% of study population was currently in full-time education and only 28.5% were from non-biology field with never studied cancer-related courses (73.2%). More than half of the participants were meeting the guideline of fruit and vegetable consumption (82%) and physical activity status (67.2). However, 76.2% were those who didn’t have cancer history in their family. The findings of the knowledge of screening methods showed that the majority of the study population were lacking the knowledge. Most of them didn’t hear of mammogram (64.7%) and BRCA (83.2%). Nearly 43.7% were those who didn’t check their breasts and very few were those who checked breasts once a month (15.8%) or once a week (12%), 20.8% were those who didn’t notice change in their breasts. Only 13% were found to be more confident that they can identify the changes in their breasts. Very few participants knew who is more prone to breast tumors. Nearly half of the participants identified “women of any age” as having breast cancer risk related to age (42.2%). However, 7% of study subjects correctly identified that “70-year-old women” as a BC risk factor. Moreover, 24.1% correctly identified “one in nine women” as a lifetime breast cancer risk. The majority of the participants (30.1%) were unaware of who can face the lifetime breast cancer risk given in Table 1.
Table 1.
Descriptive Statistics
| Age (Years) | Demographics | N (%) |
|---|---|---|
| <18 | 33 (33.0) | |
| 18-35 | 820 (82.0) | |
| 36-50 | 109 (10.9) | |
| >50 | 38 (3.8) | |
| Marital-Status | Single | 645 (64.5) |
| Married | 322 (32.2) | |
| Widowed | 28 (2.8) | |
| Divorced | 5 (0.5) | |
| Socioeconomic-Status | White-collar-workers | 765 (76.5) |
| Blue-collar-workers | 235 (23.5) | |
| Ethnicity | South-Punjab | 62 (6.2) |
| Central-Punjab | 857 (85.7) | |
| North-Punjab | 15 (1.5) | |
| Other than Punjab | 66 (6.6) | |
| Years of Education | Un-Educated/Illiterate | 106 (10.6) |
| <5-years | 37 (3.7) | |
| >5-years | 48 (4.8) | |
| 10-years | 67 (6.7) | |
| 12-years | 167 (16.7) | |
| 14-years | 216 (21.6) | |
| 16-years | 219 (21.9) | |
| 18-years and more | 140 (14.0) | |
| Specialization (if 14-16) YoE | Biology | 290 (29.0) |
| Non-Biology | 285 (28.5) | |
| NA | 425 (42.5) | |
| Have you ever study Cancer-related course | Yes | 268 (26.8) |
| No | 732 (73.2) | |
| Smoking-Status | Smoker | 9 (0.9) |
| Never smoker | 981 (98.1) | |
| Ex-smoker | 10 (1.0) | |
| Fruits/Vegetable consumption (Meeting-guidelines) |
Yes | 820 (82.0) |
| No | 180 (18.0) | |
| Physical activity status (Meeting-guidelines) |
Yes | 676 (67.6) |
| No | 324 (32.4) | |
| Family history of cancer | Yes | 238 (23.8) |
| No | 762 (76.2) | |
| Demographics | N (%) | |
| Below-18.5(Underweight) | 185 (18.5) | |
| 18.5–24.9(Normal/Healthy Weight) | 553 (55.3) | |
| 25.0–29.9(Overweight) | 184 (18.4) | |
| 30.0 and Above(Obese) | 78 (7.8) | |
| Yes | 353 (35.3) | |
| No | 647 (64.7) | |
| Yes | 40 (4.0) | |
| No | 960 (96.0) | |
| Yes | 168 (16.8) | |
| No | 832 (83.2) | |
| Yes | 15 (1.5) | |
| No | 985 (98.5) | |
| At least once a week | 120 (12.0) | |
| At least once a month | 158 (15.8) | |
| At least once every 6 months | 109 (10.9) | |
| Rarely or never | 437 (43.7) | |
| Don't Know | 125 (12.5) | |
| Refused | 51 (5.1) | |
| Very-confident | 130 (13.0) | |
| Fairly-confident | 206 (20.6) | |
| Slightly-confident | 230 (23) | |
| Not at all-confident | 208 (20.8) | |
| Don't Know | 163 (16.3) | |
| Refused | 63 (6.3) | |
| A 30-year woman | 101 (10.1) | |
| A 50-year woman | 146 (14.6) | |
| A 70-year woman | 70 (7.0) | |
| A woman of any age | 422 (42.2) | |
| Don't Know | 248 (24.8) | |
| Refused | 13 (1.3) | |
| 1 in 3 women | 57 (5.7) | |
| 1 in 9 women | 241 (24.1) | |
| 1 in 100 women | 267 (26.7) | |
| 1 in 1000 women | 125 (12.5) | |
| Don't Know | 301 (30.1) | |
| Refused | 9 (9.0) |
Socioeconomic status vs knowledge of mammogram and BRCA
Significance was determined between socioeconomic status and knowledge of mammograms and BRCA. Less white-collar workers were found with lacked the knowledge of mammogram (56.2%) and BRCA (79.3%) as compared to while blue-collar workers with lacked knowledge of mammogram (90.6%) and BRCA (95.7%) and P-Value was found to be ˂0.001.
Risk factors of breast carcinoma
A total of 9 risk factors for Breast Carcinoma were studied. Nearly 32.4% & 19.8% participants answered “agree” & “strongly agree” respectively for the risk factor of “family history of Breast Carcinoma”. The majority were unaware of risk factors like late menopause (63.2%), using Hormone Replacement Therapy (58.2%), kids in the late stage of life (57.4%), menstruating at an early age (55.1%), consumption of alcohol more than one unit/day (40.3%), doing less physical activity that didn’t meet standards (45.2%) and having overweight (39.7%) given in Table 2.
Table 2.
Risk Factors of Breast Cancer
| Risk Factors |
Having a past history of breast cancer | Using HRT (Hormone Replacement Therapy) | Drinking more than 1 unit of alcohol a day | Being overweight (BMI over 25) |
Having a close relative with breast cancer | Having children later on in life or not at all | Starting your periods at an early age | Having a late menopause |
Doing less than 30 mins of moderate physical activity 5 times a week |
|---|---|---|---|---|---|---|---|---|---|
| Strongly Agree | 19.8 | 8.1 | 7.3 | 7.7 | 14.9 | 5.4 | 3.7 | 4.2 | 6.3 |
| Agree | 32.4 | 18.7 | 30.7 | 28.5 | 38.4 | 13.6 | 12.8 | 10.7 | 24.6 |
| Not Sure | 24 | 58.2 | 40.3 | 39.7 | 27.9 | 57.4 | 55.1 | 63.2 | 45.2 |
| Disagree | 19.6 | 11.3 | 13.7 | 19.5 | 13.5 | 18.2 | 24.3 | 18.8 | 21.1 |
| Strongly Disagree | 4.2 | 3.7 | 8 | 4.6 | 5.3 | 5.4 | 4.1 | 3.1 | 2.8 |
Barriers to seeking medical help
Data was analyzed to measure the proportion of participants who could face barriers to seeking medical help. Approximately 30% and 18.2% respondents answered “yes often” and “yes sometimes” respectively for being too embarrassed to see doctor for breast cancer. Almost 19.1% and 30.4% participants answered “yes often” or “yes sometimes” for being too scared to see the doctor. Nearly 57.4% didn’t feel any difficulty in talking to the doctor, making a doctor‘s appointment (60.6%), and arranging transport (63.8% shown in Table 3).
Table 3.
Distribution of Barriers to Seeking Help in Respondents
| Barriers to seeking medical help | Too embarrassed to go and see the doctor | Too scared to go and see the doctor | Worried about wasting the doctor’s time | I find my doctor difficult to talk to | Difficult to make an appointment with the doctor | Too busy to make time to go to the doctor | Too many other things to worry about | Difficult to arrange transport to the doctor’s surgery | Worrying about what the doctor might find may stop me from going to the doctor | Not feeling confident talking about my symptom with the doctor |
|---|---|---|---|---|---|---|---|---|---|---|
| Yes often | 18.2 | 19.1 | 8.8 | 12.2 | 9.9 | 15.4 | 18.5 | 8.3 | 8.7 | 12.1 |
| Yes sometimes | 30 | 30.4 | 9.4 | 19.9 | 19.4 | 23 | 20.3 | 16.8 | 25.5 | 31.3 |
| No | 45.5 | 44.3 | 73.4 | 57.4 | 60.6 | 53.4 | 49.7 | 63.8 | 52.8 | 45.3 |
| Don't Know | 5.6 | 5.5 | 9.9 | 9 | 8.8 | 7 | 9.1 | 9.8 | 10.6 | 9.3 |
| Refused | 1.1 | 0.7 | 1.5 | 1.5 | 1.3 | 1.2 | 2.4 | 1.3 | 2.4 | 2 |
Knowledge of symptoms
Data was analyzed to determine the frequency of respondents who could identify potential breast cancer symptoms. Frequencies of participants who answered ‘yes’ to symptoms of BC were as: discharge/bleeding from the breast nipple (68.7%), armpit/breast pain (66.4%), breast thickening or breast lump (61.7%), breast shape changes (55.3%), breast size changes (53.5%), and thickening/lump in armpit (53%), However, one-third of respondents didn’t know about symptoms like: breast skin dimpling (35.7%), breast skin redness (31.9%), changes in the position of breast nipple (31.9%) and rashes of breast nipple (33.9%) shown in Table 4.
Table 4.
Distribution of Knowledge of Symptoms in Respondents
| Knowledge of Symptoms | Have you ever had breast cancer | Change in the position of your nipple could be a sign of breast cancer? such as pointing up or down or in a different direction to normal | Pulling in of your nipple could be a sign of breast cancer? where the nipple no longer points outwards, but into the breast | Pain in one of your breasts or armpit could be a sign of breast cancer? | Puckering or dimpling of your breast skin could be a sign of breast cancer? like a dent or orange peel appearance | Discharge or bleeding from your nipple could be a sign of breast cancer? | Lump or thickening in your breast could be a sign of breast cancer? | Nipple rash could be a sign of breast cancer? | Redness of your breast skin could be a sign of breast cancer? | Lump or thickening under your armpit could be a sign of breast cancer? | Changes in the size of your breast or nipple could be signs of breast cancer? | Changes in the shape of your breast or nipple could be signs of breast cancer? |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | 5.7 | 45.5 | 39.1 | 66.4 | 52.5 | 68.7 | 61.7 | 40.9 | 48.2 | 53 | 53.5 | 55.3 |
| No | 91 | 22.1 | 19.1 | 12.2 | 11.2 | 8 | 7.9 | 24.1 | 19.2 | 11.4 | 13.8 | 12.8 |
| Don’t Know | 3.1 | 31.9 | 40.5 | 21.1 | 35.7 | 22.6 | 29.9 | 33.9 | 31.9 | 34.8 | 31 | 30.7 |
| Refused | 0.2 | 0.5 | 1.3 | 0.3 | 0.6 | 0.7 | 0.5 | 1.1 | 0.7 | 0.8 | 1.7 | 1.2 |
Association between demographic variables and Breast Self-Examination (BSE)
Table 5 showed a significant association of women’s socioeconomic status with BSE. (p = 0.001). Multivariable analysis showed that white-collar workers (adjusted odd ratio [aOR]: 2.178; 95% CI: 1.571-3.081 were more conscious to get BSE. Association between family history and BSE was not found statistically significant.
Table 5.
Association between Demographic Variables and BSE (N=1000)
| Variables | Breast Self-Examination | Univariate | Multivariate | |||
|---|---|---|---|---|---|---|
| Yes n (%) | No n (%) | OR (95% CI) | P-value | OR (95% CI) | P-value | |
| 387 (38.7) | 613 (61.3) | |||||
| Marital Status | ||||||
| Single | 256 (66.1) | 389 (63.5) | 1 | ˂0.001 | 1 | ˂0.386 |
| Married | 131 (34.0) | 224 (36.5) | 1.125 (0.862-1.470) | 0.889 (0.680-1.161) | ||
| Socio-economic status | ||||||
| Blue collar-worker | 60 (25.50) | 175 (74.50) | 1 | ˂0.001 | 1 | ˂0.001 |
| White collar-worker | 327 (42.70) | 438 (57.30) | 0.459 (0.331-0.636) | 2.178 (1.571-3.081) | ||
| Family history of breast cancer | ||||||
| Yes | 99 (41.6) | 139 (58.4) | 1 | ˂0.125 | 1 | ˂0.295 |
| No | 288 (37.8) | 474 (62.2) | 1.235 (0.884-1.725) | 1.172 (0.871-1.577) | ||
Association between variables & breast cancer knowledge scores
Data of association across the variables and knowledge score was obtained given in Table 6. Younger women (18-35 years) were found to have sufficient knowledge (10.08 ± 5.99) as compared (4.06 ± 4.71) to the older women (above 50 years). Knowledge score was positively associated with education level and a significant correlation was found between women’s knowledge score and socioeconomic status.
Table 6.
Association between Demographic Variables and Total Breast Cancer Knowledge Scores (n=1,000)
| Variables | Knowledge of Breast Cancer | |||
|---|---|---|---|---|
| Sufficient n=374(37.4%) | Insufficient n=626(62.6%) | Mean±SD | P-value | |
| Age | ||||
| <18-years | 2 (6.0) | 31 (94.0) | 4.06±4.71 | ˂0.001 |
| 18-35 years | 319 (38.9) | 501 (61.1) | 10.08±5.99 | |
| 36-50 years | 42 (38.5) | 67 (61.5) | 9.35±6.10 | |
| >50 years | 11 (28.9) | 27 (71.1) | 7.71±6.01 | |
| Marital Status | ||||
| Single | 437 (67.8) | 208 (32.2) | 9.27±5.92 | ˂0.001 |
| Married | 189 (53.2) | 166 (46.8) | 10.51±6.27 | |
| Socio-Economic status | ||||
| Blue-collar worker | 51 (21.7) | 184 (78.3) | 7.35±5.50 | ˂0.001 |
| White-collar worker | 323 (42.2) | 442 (57.8) | 10.43±6.06 | |
| Year of Education | ||||
| Uneducated/illiterate | 10 (9.4) | 96 (90.6) | 4.86±4.92 | ˂0.001 |
| <5-years | 6 (16.2) | 31 (83.8) | 7.14±4.85 | |
| >5-years | 12 (25.0) | 36 (75.0) | 7.87±5.63 | |
| 10-years | 17 (25.4) | 50 (74.6) | 7.54±5.58 | |
| 12-years | 54 (32.3) | 113 (67.7) | 8.53±5.54 | |
| 14-years | 69 (31.9) | 147 (68.1) | 9.74±4.81 | |
| 16-years | 113 (51.6) | 106 (48.4) | 11.35±5.94 | |
| 18-years/more | 93 (66.4) | 47 (33.6) | 14.50±5.93 | |
| Family history of breast cancer | ||||
| Yes | 102 (42.8) | 136 (57.2) | 10.50±5.90 | ˂0.046 |
| No | 272 (35.7) | 490 (64.3) | 9.46±6.11 | |
Association of health behavior characteristics and knowledge score
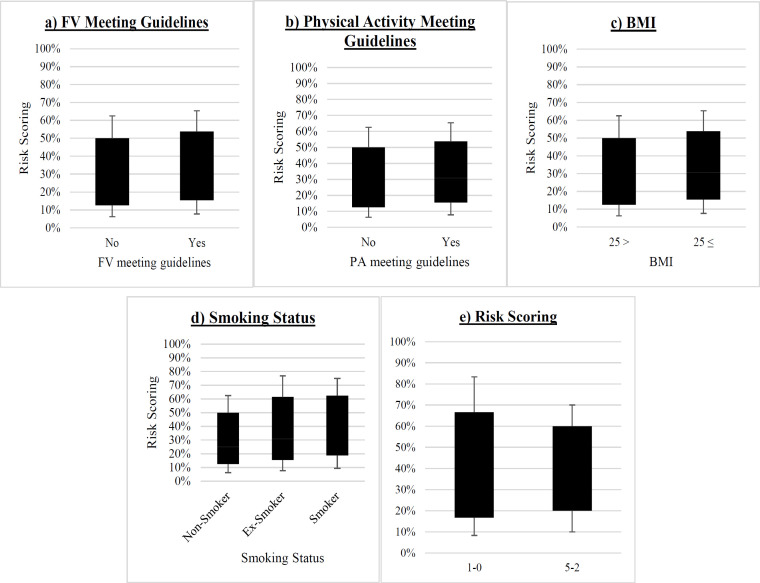
Score of attitude measurement (health risk score) was calculated by questioning the public and measuring their extent of response to a series of behavior practices on different topics, in terms as they agree or not with them (Figure 1). In the presented study, accumulative behavior risk scores were also determined (mentioned in methodology).
Figure 1.
Behavior Characteristics and Health Risk Scoring
The association was measured among health behavior parameters (BMI, smoking status, level of fruits/vegetable consumption, and physical activity) with an aggregate knowledge score. A significant association was found between all except smoking status given in Table 7.
Table 7.
Association between Behavior Characteristics and Knowledge Score
| Behavior Characteristics | Knowledge score | Univariate | ||
|---|---|---|---|---|
| Sufficient n=374 (37.4%) |
Insufficient n=626 (62.3%) |
OR (95% CI) | P-value | |
| BMI | ||||
| Less than 25 | 241 (32.7) | 497 (67.3) | 1 | ˂0.001 |
| Equal and above 25 | 133 (50.8) | 129 (49.2) | 2.126 (1.596-2.833) | |
| Fruit & Vegetable consumption meeting guidelines | ||||
| Yes | 340 (41.5) | 480 (58.5) | 1 | ˂0.001 |
| No | 34 (18..9) | 146 (81.1) | 0.329 (0.221-0.490) | |
| Physical Activity meeting guidelines | ||||
| Yes | 283 (41.9) | 393 (58.1) | 1 | ˂0.001 |
| No | 91 (28.1) | 233 (71.9) | 0.542 (0.407–0.722) | |
| Smoking status | ||||
| Never smoker | 371 (37.8) | 610 (62.2) | ˂0.125 | |
| Ex-Smoker | 1 (10) | 9 (90) | ||
| Smoker | 2 (22.2) | 7 (77.8) | ||
| Health Risk score | ||||
| Low | 315 (39.2) | 488 (60.8) | 1 | ˂0.016 |
| High | 59 (29.9) | 138 (70.1) | 0.662 (0.473 – 0.927) | |
Discussion
High awareness about risk factors, warning signs, diagnosis, and treatment are essential for limiting the development of breast tumors and early detection to improve breast cancer survival. The overall awareness of breast cancer was suboptimal in the presented study. To our knowledge, such type of study to measure breast cancer awareness among women in Pakistan had never been done before. The presented study revealed that there is a significant correlation in educational background to the level of breast cancer awareness. Gupta (2015) performed the same study that Indian women had low cancer literacy of risk factors irrespective of their educational background and socioeconomic status. This might be because the majority of respondents had the socioeconomic status of white-collar workers. And as to the level of education, 21.9% were having education of 16 years, and from the non-biology field (28.5%) with never studied cancer-related courses was 73.2%. There is also a possibility that the educational system does not provide an understanding of breast cancer awareness, especially to non-biology field students. In addition, previous studies revealed that awareness levels positively correlated with educational status (Linsell et al., 2010; Liu et al. 2014). All the differences can be due to cultural variations and geographical differences.
The majority was unaware regarding breast cancer screening tools that mammography and BRCA are effective methods for early detection. A study in China showed that only 26.8% were those who heard about Breast Cancer screening tools (Dinegde et al., 2017). We can infer that Pakistan has very few national and regional breast cancer screening awareness programs and media campaigns in the form of demonstrations and lectures in educational settings.
Almost 43.7% of Pakistani women in this study reported were those who didn’t check their breasts however very less respondents were those who knew that they had to check their breasts. likewise, in Indonesia, work reported that only 21.2% of women did BSE (Nurleli et al., 2014), whereas contrary, in a previous study, 52.3% Indonesian females were those who did every month their BSE (Solikhah et al., 2017). This might be because majority of them didn’t know when to perform BSE and what symptoms of breast cancer are. Another study revealed that increased knowledge improved the perception of women regarding breast checking benefits and in turn strengthened BSE and enhanced confidence in them so they can examine breast changes (Syed et al., 2017). Almost 45% of respondents didn’t observe changes in their breasts, so they didn’t consult a doctor ever for breast changes. Similarly, another study conducted by (Linsell et al., 2010) in the UK found low confidence to notice a variation in breasts (31%).
The results of the presented study showed that most Pakistani women do not have knowledge regarding breast cancer development in the body is a lifetime risk and can be age-related. Similar results reported previously that most study population was not aware of the age-related risk like older women are more prone to breast cancer (Nurleli et al., 2014).
Various factors affect adult females’ risk of breast cancer development. Some factors are modifiable however, most of the factors are social, economic, lifestyle, and environmental. Knowledge of these factors is essential for women early in life so that they can change their behaviors and risk perceptions to make the right lifestyle choices. A total of nine risk factors were analyzed. All those respondents who answered “agree/strongly agree” believed in knowing the risk factors of breast tumors. Almost 50% of members have the knowledge that family history can be a risk factor. It might be due to increased awareness of risk factors in the individuals who had direct experience of taking care of their relatives (1st degree) with Breast Cancer. Previously reported that the majority of participants were aware that close relatives with breast carcinoma and family history were prominent risk in disease development (Almutairi et al., 2016).
The vast number of the participants of the presented study didn’t have information that starting menopause at a later stage (63.2%), HRT (58.2%), delayed children in life (57.4%) and early periods (55.1%) were risk factors of BC. Liu, 2014 and Gupta, 2015 presented the same analysis previously and revealed risk factors of breast cancer had very less awareness. As respondents of the study were in the age group that can make reproductive decisions; therefore, they need to be knowledgeable regarding non-modifiable biological risk factors.
The majority of participants were aware of nearly 5 or all potential symptoms of developing breast cancer. Similar work was reported previously that most participants have high awareness levels regarding signs/symptoms of disease (Amin et al., 2020). In contrast, another study conducted in China reported a low level of awareness regarding warning signs of breast tumor (Liu et al., 2014). There is a possibility that healthcare providers having close relative with breast cancer could enhance awareness in terms of symptoms and confidence to detect breast changes. They can have more knowledge of how frequently one can check breasts to prevent from disease.
The possible barriers in getting medical help after noticing changes in breasts were numerous; embarrassment, being worried about other things and being busy were provided by respondents as some of the top reasons representing social stigmas that need to be addressed. These results draw attention to possible shortcomings of our health system that visiting doctor for checkup may be considered a time-consuming assignment and health might not be a priority of participants. Furthermore, the environment of examining the patients may not ensure complete privacy/satisfactorily comfortable. Moreover, majority of study population said they didn’t think that they were wasting the doctor’s time. It means embarrassment is a major barrier in seeking medical help. However, communication and hesitancy can cause an interruption in seeking help. Same findings including the unavailability of lady doctors and shyness were reported as a cause of delayed medical help in a previous study conducted by Radi (2013) and Mamdouh et al., (2014).
A significant association was found between demographic variables and knowledge score of respondents. Younger women were more knowledgeable compared to older women due to more literacy rate in them. These findings were similar to a study conducted previously in China by Liu et al., (2014). In contrast, another study represented that older women were more aware than younger women (Masood et al., 2016).
Despite the interesting findings, the presented study has several limitations. Firstly, lack of funding sources limited the study to collect data majorly from 3 to 4 cities of Punjab. Therefore, the findings of this study are not generalizable to the whole Pakistani Population. Secondly, the convenience sampling method was applied to reach out to participants because of the absence of a sampling frame, which might cause an uneven enrollment from various demographic areas. Thirdly, this study did not apply any intervention as well as nor provide information on whether especially planned programs enhance breast tumor awareness or not, so more work can be conducted to explore these questions.
We concluded that the study findings presented baseline information on women’s attitudes, knowledge, and practices related to breast tumor and their risk factors. Overall, the awareness among female respondents of the study was found very poor and inadequate. In the study area of Pakistan, due to cultural sensitivity, a female cannot openly share issues related to breasts and cannot discuss it even with their close relatives, therefore, most of the females remain undiagnosed and untreated. Further research is required to enhance women’s confidence, knowledge, and reporting of breast cancer awareness within cultural limitations by healthcare professionals, public and private sectors. Current study findings propose the need for, effective, socially acceptable, and culturally appropriate breast cancer awareness programs to enhance the awareness level of disease among women in Pakistani settings. Currently, television broadcasts and media commonly show that unhealthy food and lifestyle of women are the cause of breast tumors, but they don’t focus on actual causes like knowledge regarding lifetime-, age-related risk factors, and signs/symptoms of the disease. These findings should be utilized as an advocacy tool for planners and policymakers to introduce awareness programs and breast screening in the country.
Author Contribution Statement
ZS conceptualize and wrote the first draft. ZS and AJ collected the data. ZS analyzed the data. AJ reviewed the literature. Both authors reviewed the paper and approved the final version of the manuscript.
Acknowledgements
The authors would like to thank all the participants in this study for their voluntary participation. The authors thank the authorities and the health professionals of Pakistani institutions for their help in data collection.
If it was approved by any scientific Body/ if it is part of an approved student thesis
This manuscript is the part of my Ph.D. thesis having the title “Current state of breast cancer diagnosis, prognosis and awareness in Pakistan”.
How the ethical issue was handled (name the ethical committee that approved the research)
The ethical committee (School of biological sciences), Punjab University has approved the modus operandi of the study regarding the research on humans. Consent was taken against each topic of the study before gathering the data. This is a questionnaire-based study, during designing the protocols, a careful approach was used to discuss the problems like early symptoms of breast cancer and related risk factors.
Availability of data (if apply to your research)
The relevant data has already been attached as a supplementary data.
Statement conflict of interest
The authors have no conflict of interest to disclose.
References
- Almutairi KM, Ahmad M, Vinluan JM, Almutairi A. Random cross-sectional determination of the level of awareness among female Saudi patients about breast cancer. J Cancer Educ. 2016;31:131–5. doi: 10.1007/s13187-015-0795-2. [DOI] [PubMed] [Google Scholar]
- Amin MN, Uddin MG, Uddin MN, et al. A hospital-based survey to evaluate knowledge, awareness and perceived barriers regarding breast cancer screening among females in Bangladesh. Heliyon. 2020;6:e03753. doi: 10.1016/j.heliyon.2020.e03753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinegde NG, Xuying L. Awareness of breast cancer among female care givers in tertiary cancer hospital, China. Asian Pac J Cancer Prev. 2017;18:1977–83. doi: 10.22034/APJCP.2017.18.7.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- Linsell L, Forbes LJL, Burgess C, et al. Validation of a measurement tool to assess awareness of breast cancer. Eur J Cancer. 2010;46:1374–81. doi: 10.1016/j.ejca.2010.02.034. [DOI] [PubMed] [Google Scholar]
- Ghoncheh M, Mohammadian-Hafshejani A, Salehiniya H. Incidence and mortality of breast cancer and their relationship to development in Asia. Asian Pac J Cancer Prev. 2015;16:6081–7. doi: 10.7314/apjcp.2015.16.14.6081. [DOI] [PubMed] [Google Scholar]
- Gupta A, Shridhar K, Dhillon PK. A review of breast cancer awareness among women in India: cancer literate or awareness deficit? Eur J Cancer. 2015;51:2058–66. doi: 10.1016/j.ejca.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu LY, Wang F, Yu LX, et al. Breast cancer awareness among women in Eastern China: A cross-sectional study. BMC Public Health. 2014;14:1–8. doi: 10.1186/1471-2458-14-1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N, Wang J, Chen DD, et al. Tools for the assessment of breast cancer screening beliefs in women: a literature review. J Comp Eff Res. 2019;8:645–55. doi: 10.2217/cer-2018-0142. [DOI] [PubMed] [Google Scholar]
- Mamdouh HM, El-Mansy H, Kharboush IF. Barriers to breast cancer screening among a sample of Egyptian females. J Family Commun Med. 2014;21:119–124. doi: 10.4103/2230-8229.134771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masood I, Saleem A, Hassan A, Sadeeqa S, Akbar J. A quantitative study to assess breast cancer awareness among females in Bahawalpur, Pakistan. Cogent Med. 2016;3:1236479. [Google Scholar]
- Milton K, Bull FC, Bauman A. Reliability and validity testing of a single-item physical activity measure. Br J Sports Med. 2011;45:203–8. doi: 10.1136/bjsm.2009.068395. [DOI] [PubMed] [Google Scholar]
- Nurleli, Petpichetchian W, Maneewat K. Patient delay in consulting a medical doctor among Aceh women with breast cancer. Songklanagarind J Nurs. 2014;2014:1–11. [Google Scholar]
- Qasim S, Tayyab H, Zulqadar K, et al. Breast Cancer knowledge and perceived barriers to help seeking among pre-clinical and clinical female medical students of King Edward Medical University, Lahore: a cross-sectional study. BMC Med Educ. 2020;20:222. doi: 10.1186/s12909-020-02132-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radi SM. Breast Cancer Awareness among Saudi females in Jeddah. Asian Pac J Cancer Prev. 2013;14:4307. doi: 10.7314/apjcp.2013.14.7.4307. [DOI] [PubMed] [Google Scholar]
- Saeed RS, Bakir YY, Ali LM. Are women in Kuwait aware of breast cancer and its diagnostic procedures. Asian Pac J Cancer Prev. 2014;15:6307–13. doi: 10.7314/apjcp.2014.15.15.6307. [DOI] [PubMed] [Google Scholar]
- Shahab L, McGowan JA, Waller J, Smith SG. Prevalence of beliefs about actual and mythical causes of cancer and their association with socio-demographic and health-related characteristics: Findings from a cross-sectional survey in England. Eur J Cancer. 2018;103:308–16. doi: 10.1016/j.ejca.2018.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solikhah S, Supannee P, Nitchamon R, Cameron PH. Validation of an Indonesian version of the breast cancer awareness scale (BCAS-1) Asian Pac J Cancer Prev. 2017;18:515–22. doi: 10.22034/APJCP.2017.18.2.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed S, Nagugi A, Ochieng P, Mwenda AS, Salam R. Training health workers in clinical breast examination for early detection of breast cancer in low- and middle-income countries. Cochrane Database Syst Rev. 2017;2017:CD012515. doi: 10.1002/14651858.CD012515.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahra F, Humayoun F, Yousaf T, Khan NA. Evaluation of risk factors for carcinoma breast in Pakistani women. J Fatima Jinnah Med Assoc. 2013;1:34–8. [Google Scholar]