Microprocessor stance and swing control orthosis for patients dependent on a knee-ankle-foot-orthosis for walking: A randomized, controlled crossover trial
Andreas Kannenberg, MD (GER), PhD and Shane Wurdeman, PhD, CP, FAAOP (D)
on behalf of the International Investigator Consortium Otto Bock Healthcare LP, Austin, TX. Email: andreas.kannenberg@ottobock.com
Introduction: For patients with paresis or paralysis of the quadriceps and other knee-stabilizing muscles, locked knee-ankle-foot orthoses (KAFOs) have been the standard of care for a long time. Improvements in KAFO technology, such as posterior offset KAFOs and stance control orthoses (SCO), have improved functionality for patients with free swing but work reliably and safely on level ground only. The C-Brace is the first microprocessor stance and swing control orthosis (MP-SSCO) that makes the benefits of microprocessor-controlled prosthetic knees including stumble recovery now available to patients who are dependent on a KAFO to restore walking capability. The purpose of this study was to test the hypothesis that patients experience improved balance, fewer falls, and improved mobility and quality of life when using the C-Brace compared to standard KAFOs and SCOs.
Methods: Legacy KAFO users with Berg Balance scores <45 were enrolled in 13 clinics in four countries (Germany, Austria, Netherlands, USA) and randomized to KAFO/C-Brace or C-Brace/KAFO home use for 3 months with each orthosis in this randomized, controlled crossover trial. The primary outcome measure was the Berg Balance Scale (BBS) (1). Secondary outcome measures assessed were: Dynamic Gait Index (DGI) (1), falls, Activity-specific Balance Confidence (ABC) scale (2), fear of falling, Reintegration into Normal Living Index (RNLI) (3), Orthotic and Prosthetic Users´ Survey–Lower Extremity Functional Profile (OPUS-LEFS) (4), SF-36v2 (5), EQ-5D-5L (6).
Results: Intention-to-treat analysis (ITT, including dropouts) with 102 participants and per-protocol analysis (PP, without dropouts) with 69 participants. With the C-Brace in the PP analysis, the BBS improved by 3.6 ± 6.1 points (p < 0.00006) vs. KAFO and 7.4 ± 7.7 (p < 0.00001) vs. baseline. Significantly fewer participants presented BBS scores <40 indicative of almost 100% fall risk (12 vs. 25, p = 0.00361). Mean falls reduced from 5.0 ± 18.9 with KAFO to 1.1 ± 3.3 with C-Brace (p = 0.002). The ABC score improved by 11.3 ± 22.7 (p = 0.00011), and significantly fewer patients presented ABC scores <67 indicating increased fall risk with the C-Brace than with KAFO (31 vs. 48, p = 0.0008). Also, the fear of falling indoors (p = 0.0023) and outdoors (p = 0.0065) reduced significantly with the C-Brace. The DGI improved by 1.0±3.7 (p = 0.005), and the OPUS-LEFS by 2.0±5.2 (p = 0.00019). The SF-36 improved significantly in the domains of physical functioning (p < 0.00001), emotional well-being (p = 0.0011), general health (p = 0.0038), health change (p = 0.0045), and energy/fatigue (p = 0.022). Significant improvements were also found in the RNLI (p = 0.042) and EQ-5D-5L Utility score (p = 0.037).
Discussion: The improvements in balance, falls, fall risk, function and mobility can be attributed to the stumble recovery and controlled knee flexion during weight bearing of the C-Brace. These device features and functions have a positive impact on the quality of life of users with increased fall risk compared to the use of standard KAFOs and SCOs.
Conclusion: The C-Brace represents a viable orthotic option for KAFO and SCO users with increased fall risk and reduced mobility.
Disclosure: Andreas Kannenberg is a full-time employee of Otto Bock Healthcare LP.
References
1. Shumway-Cook A, et al. Phys Ther. 1997 Aug;77(8):812-819.
2. Lajoie Y, et al. Arch Gerontol Geriatr 2004;38(1):11-26.
3. Wood-Dauphoneé SL, et al. Arch Phys Med Rehabil 1988;69:583-590.
4. Heinemann AW, et al. Prosthet Orthot Int 2003;27:191-206.
5. Ware JE. Boston, Mass: The Health Institute New England Medical Center; 1997.
6. Brooks R. Health Policy 1996;37:53–72.
Upper extremity myoelectric interface and control methodologies: A single blinded randomized clinical trial
Matthew Wernke PhD1, Laura Katzenberger CPO2, Glenn Schrober CPO3 , Jeff Denune CP4, Brian Kaluf5, James Colvin MS1
1 Willow Wood Global LLC, 2 Handspring, 3 Optimus Prosthetics, 4 Motus Research, 5 Ability P&O
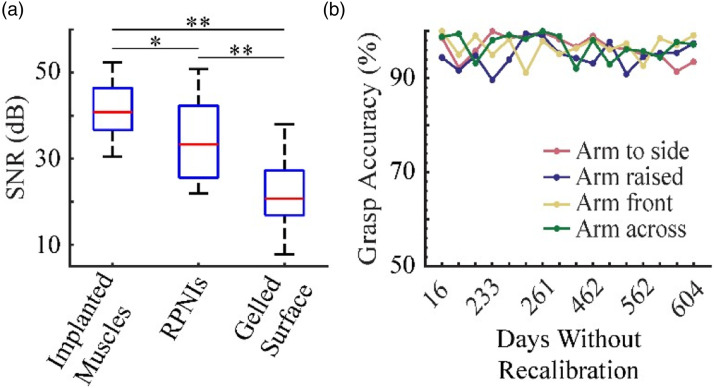
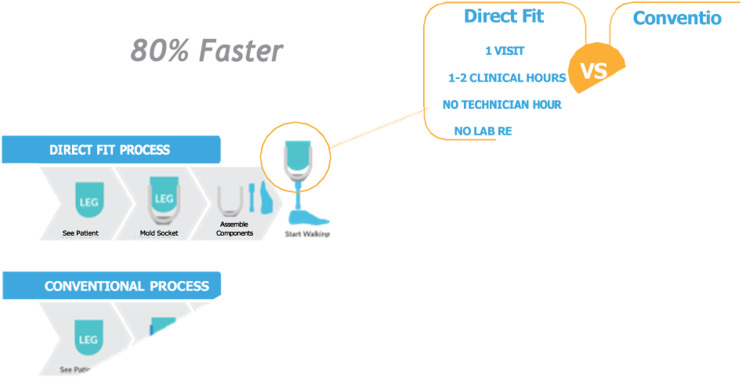
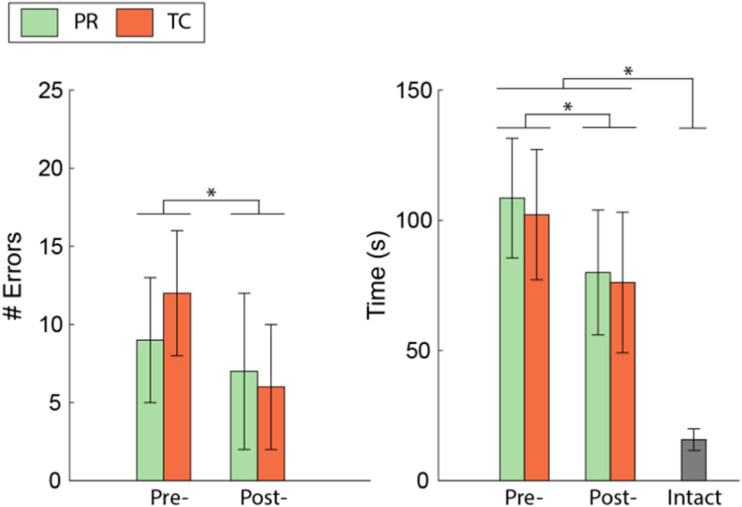
Introduction: The performance of upper extremity myoelectric prostheses and the satisfaction of their wearers is dependent on the interface and control methodologies chosen. Control of these devices has traditionally been with dual site (DS) control. Pattern recognition (PR) aims to alleviate the need for targeted electrode placement. One persistent challenge with all control methodologies is obtaining noise-free muscle signals. Several attempts have sought to embed the electrode into a liner1-3, to maintain better electrode-to-skin contact. The first commercial solution to this end is the Alpha Control Liner (ACL). The purpose here is to prospectively compare user performance and satisfaction while using these different myoelectric interfaces and control methodologies.
Methods: Subjects: Twenty-one transradial myoelectric prosthesis users were enrolled in this prospective study. Study procedures were executed by independent clinical sites. Prior to the study, a formal training workshop was completed to ensure consistent execution across all sites. All subjects completed three conditions in random order: 1) DS control with socket embedded electrodes; 2) Coapt PR with socket embedded electrodes; and 3) Coapt PR with the ACL. Study criteria required at least two myoelectrically controlled degrees of freedom.
An initial data collection was completed immediately following participant fitting and training of the condition. A final data collection occurred after 6 weeks of at-home use. At each data collection visit, the participants first completed the subjective feedback prior to the performance tests to avoid any frustration during the performance test from influencing their responses regarding at-home use. Data collected at each timepoint included Objective performance data (Activity Measures for Upper Limb Amputees (AMULA) and elbow range of motion) and subjective data (Orthotic and Prosthetic User Survey (OPUS) Upper Extremity Functional Status, Health Quality of Life, and Satisfaction with Device and Services sections; McGann Feedback Form; and the Socket Comfort Score). Subjective data on the ease of fitting, training, and delivering the study treatments were collected from the study prosthetists.
The data analyst was blinded to the study condition for all data. The same analyst scored all the AMULA videos to ensure consistent interpretation of the scoring criteria. The elbow range of motion with the prosthesis was normalized to the range of motion without a prosthesis.
Results: Full data sets were collected for sixteen of the twenty- one subjects. AMULA performance was significantly higher for the ACL+PR condition compared to DS condition (p = 0.001) and PR condition (p=0.01). Elbow range of motion was on average 11% higher for the ACL+PR condition compared to the other conditions. The subjective responses collected through the OPUS sections indicated moderate and nonsignificant differences between the conditions. Study clinicians indicated the ACL+PR condition required the fewest hours spent fitting the socket, the fewest number of check sockets, the easiest to modify the positive, and the easiest to select myosites. The DS condition was rated easiest to train, although most of the participants were existing DS users.
Conclusion: The results provide evidence that the ACL+PR had the best overall performance across the outcomes tested, likely due to better management of electrode-to-skin contact. Subjective surveys provided inconclusive results. We hypothesize that differences in subjective data between conditions may have been reduced due to ceiling effects. This may indicate the need for new surveys designed to compare these technologies.
Significance: The study represents one of the largest prospective studies of this population. The work provides new evidence to guide clinical care to those that stand to benefit from a myoelectric prosthesis. Although differences between the types of control were found, the biggest impact were due to changes in the interface. The ACL+PR may prove to overcome some of the more troublesome challenges of traditional myoelectric systems and provide an option to gain better performance without requiring the patient to undergo surgical intervention, as required in recent advancements with implantable electrodes to measure muscle contractions.
Disclosure: Some authors are employees of Willow Wood.
Acknowledgments: This work was supported through the Orthotics and Prosthetics Outcomes Research Program under Award No. W81XWH-17-1-043. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense.
References
1. Salam Y. JPO; 6(4), 119-120. 1994.
2. Daly W. JPO. 12(3), 88-91. 2000.
3. Reissman T. PLOS One. 13 (6), 2018.
A pilot study to evaluate the effects of hydraulic ankle-foot prostheses on standing and walking performance in K2-level ambulators
Steven A. Gard, PhD1,2, Paul Hammond II, MS2, Michael Cavanaugh, MSHI, CPO1 and Rebecca Stine, MS2
1 Northwestern University Prosthetics-Orthotics Center, 2 Jesse Brown VA Medical Center, Chicago, IL sgard@northwestern.edu www.nupoc.northwestern.edu
Introduction: Prosthesis users perform many basic walking activities indoors and outdoors, where traversing uneven terrain and slopes, or ascending and descending stairs, may be necessary in addition to level-ground walking. Increased prosthetic ankle range of motion (ROM) may lead to improved kinematics and kinetics on slopes and stairs in K2-level transtibial amputees. Hydraulic ankle-foot (HAF) components can adapt to uneven ground and have an increased ankle joint ROM that may be beneficial for transtibial amputees in performing daily mobility tasks (1, 2). The purpose of this pilot study was to evaluate the effects of a HAF component on the walking and standing abilities of K2-level transtibial amputees.
Methods: The following inclusion criteria were used to identify prospective participants for our pilot study: age 18-80 years, unilateral transtibial amputation, residual limb length classified as medium, prosthesis user for at least one year prior to enrolling in the study, K2-level ambulator, good sensation on their residual limb, good skin integrity upon visual inspection, does not require the use of assistive devices to walk, clinically presents with good standing balance and recovery, and not currently taking medications that are known to affect gait and balance. In a cross-over study design, subjects were randomly fitted with either the College Park Industries OdysseyK2 HAF prosthesis or Celsus prosthetic foot, and permitted two weeks to accommodate before returning for the data acquisition session of walking and standing analyses.
Quantitative gait analyses were conducted as the subjects ambulated along the level and sloped walkways and ascended/descended stairs. Standing analyses were completed as subjects stood statically on level and sloped surfaces. After the data acquisition session, subjects’ perceptions with the different prosthetic configurations were recorded using the Locomotor Capabilities Index, Hill Assessment Index, and Stair Assessment Index to document the research participants’ abilities to perform different tasks with the HAF prosthesis compared to a non- hydraulic prosthesis. We also administered a customized questionnaire that we developed to record the subjects’ perceptions of walking with the two different prosthetic feet.
Results: Three subjects meeting the inclusion criteria were enrolled and tested for this study. Contrary to expectations, the HAF component had little effect during level and upslope walking. However, the ankle motion when descending a slope demonstrated reasonably good accommodation with the HAF component, with the foot in pronounced plantarflexion throughout stance phase compared with the control foot (Figure 1).
Figure 1.
The HAF appeared to accommodate reasonably well when subjects walked down a slope.
The most compelling data that we obtained differentiating function between the HAF and control feet was during quiet standing on different sloped surfaces. The HAF component automatically adjusted to the slope of the surface, requiring less accommodation by the subject at their knee and hip joints. At the conclusion of the study, subjects 1 & 2 indicated a general preference for the control foot, while subject 3 indicated a preference for the HAF component.
Conclusion: Hydraulic ankle-foot components do not appear to offer much benefit to K2-level ambulators at this time. More research into the effects of hydraulic ankle-foot components on K2-level ambulators is encouraged, particularly as commercially available designs undergo further refinement.
Significance: The main advantage of a hydraulic foot-ankle component among unilateral, transtibial prosthesis users appears to be in reducing compensatory joint actions while standing on sloped surfaces, which is not the primary consideration when fitting these types of components.
Acknowledgements: This work was funded by an AOPA Research Award administered by the Center for Orthotic and Prosthetic Learning and Outcomes/Evidence-Based Practice (COPL).
References
1. Johnson L, et al. J Rehabil Res Dev. 2014;51(3):429-38.
2. Sedki & Moore. Prosthet Orthot Int. 2013;37(3):250-4.
Advanced wearable fitness tracker for transtibial limb loss: A feasibility study using the Oura ring
John Chomack1,2*, MS, Alexis Sidiropoulos1, PhD, Jason Maikos1, PhD
1 Department of Veterans Affairs New York Harbor Healthcare System, New York, NY, USA, 2 Narrows Institute for Biomedical Research and Education, Inc. Brooklyn, NY, USA *Corresponding Author john.chomack@va.gov
Introduction: A primary goal of prosthetic clinical practice is to help individuals with lower limb loss (LLL) regain functional independence in their everyday lives. However, current clinical practice mainly utilizes clinic-based outcomes and lacks an objective perspective of a patient’s activity in their community [1]. To provide patients with a prosthesis that meets their needs, community ambulation data is required. Commercially available wearable fitness trackers (WFT) have been mostly limited to studying step counts in the LLL populations [2]. However, these WFTs are designed for populations without gait abnormalities experienced by these populations [3]. As such, the purpose of this study was to address the feasibility of using an advanced WTF, Oura Ring (OR) (Oura Health Ltd), as an accurate, health-related activity measuring device for those with LLL. To obtain real-world functional information and facilitate more effective evidence-based clinical treatments, this study used the OR to collect measures of step count, activity levels, and heart rate (HR) to compare outcomes to validated monitoring devices. It was hypothesized that the OR would collect accurate step count and HR in this population, and no statistically significant differences between the OR and validated monitoring devices would be evident.
Methods: Twelve individuals with transtibial limb loss (age 55 ± 12.6 years, height 1.73 ± 0.09 m, weight 86.2 ± 25.1 kg) with at least 6 months of prosthesis or osseointegration experience were recruited at Veterans Affairs New York Harbor Healthcare System (VANYHHS). Study procedures were approved by the VANYHHS Institutional Review Board. After being fit and acclimated to the OR (10-14 days), participants performed 3 tasks at baseline: initial resting HR, 6 Minute Walk Test (6MWT), and post-activity, 30-minute resting HR. Participants completed the 6MWT while wearing the OR, a StepWatch4TM (Modus Health, Inc) (SW4), a Polar H10 HR sensor (Polar Electro, Inc), and a chest-mounted video camera (COOAU, Ltd) to determine feasibility and accuracy. Resting HR was recorded with both the OR and the Polar H10. Participants were then sent home with the OR and the SW4 for 1-month of home and community use. After 1 month, participants returned for the final visit and repeated the same tasks collected at baseline. Outcomes were assessed for accuracy using percent error. Non- parametric analyses (Kruskal-Wallis H test and post hoc Mann- Whitney U test) determined significant differences between outcomes from the OR and each validated measurement device.
Results: No significant differences in HR were found between the Polar H10 and OR during any task (p<0.05). The OR had significant differences in step count between the SW4 (p=0.02) and the video camera (p=0.01) (Table 1). This is represented as percent error of steps between the OR and the SW4 19.3% (16.5) and video camera 20.6% (17.1) (Table 1).
Table 1.
Outcome measures and percent error among devices.

|
Conclusion: The OR collected step count, resting HR, and 6MWT for individuals with LLL, demonstrating its feasibility for use in this population. It is currently unknown if the step count inaccuracies between OR and SW4/video camera were caused by potential abnormal gait patterns associated with transtibial limb loss or due to the 3D accelerometery step recognition used by the OR. This discrepancy could be investigated with a control population and closely monitoring excessive arm swing. Further understanding of step recognition or use of a different activity parameter with the OR will need to be explored to potentially aid traditional prosthetic clinical outcomes with accurate community ambulation data. This study will seek to further investigate the accuracy of community-based activity and potential motivational aspects of this device on patients.
Significance: WFTs have the potential to provide objective data necessary for individualized healthcare and prosthetic prescription practices to improve prosthesis satisfaction and quality of life.
Disclosure: The views and opinions expressed herein do not state or reflect those of the Department of Veterans Affairs. There is no COI.
Acknowledgements: This study was funded by the Orthotic and Prosthetic Education Research Foundation and the American Orthotic Prosthetic Association. The authors thank the Narrows Institute for Biomedical Research and Education, Inc for grant management.
References
1. Halsne, E. G., et al. (2013). J RR&D, 50 (4), 515-530.
2. Chadwell, A., et al. (2020). J NeuroEng & Rehab. 17 (93).
3. Hafner, B. J., et al. (2009). J RR&D, 46 (3), 417-434.
Algorithmic two-site selection for upper-limb myoelectric prosthetic control
Kelly, C.1, Lawrence, K.1, Rozell, B.1, Martinez Luna, C.1, Clancy, E.2, Latour, D.3, Farrell, T.1
1 Liberating Technologies, Inc., 2 Worcester Polytechnic Institute, and 3 Single-Handed Solutions, LLC. toddfarrell@liberatingtech.com
Introduction: Reliably controlling upper limb prostheses continues to be a limiting factor in clinical deployment. This unreliability can lead to fatigue causing considerable reductions in function, which is found to be a main cause of prosthesis abandonment1. Ultimately, preventing the issue of unreliable prosthesis control can lead to a substantial increase in the quality of life of people living with limb absence.
The OptiMyo system was designed to address this problem by finding the optimal 2-site electrode locations and control strategy algorithmically.
Methods: The OptiMyo system consists of 128 monopolar electromyographic (EMG) channels that were filtered and converted to differential channels representing conventional electrode spacing. An algorithm was developed to identify the optimal site locations and incorporates accidental co-contraction, natural movement, the weight of a socket, and arm position during both intended and unintended actuation of the prosthesis (Figure 1).
Figure 1.
A visualization of the output from the OptiMyo system on a subject’s extensor muscles. Darker red sections reflect a higher (better) score.
Each subject was consented to an IRB-approved protocol and had sites located by the OptiMyo system and by traditional methods using the technique taught to student prosthetists at the University of Salford. The sites were evaluated by measuring the “EMG Skill” through the use of static and dynamic tracking exercises similar to those proposed by Chadwell2.
Subjects: 4 people: 2 male, 2 female. Age: 33 ± 9 yrs
Apparatus: OT Bioelettronica EMG-USB
Results: EMG Skill testing showed better results for the OptiMyo System in 12 out of 20 static testing conditions (Figure 2). Additionally, 3 out of 4 subjects scored better with the OptiMyo system during dynamic testing.
Figure 2.
Difference in EMG skill between the two methods (error bars show 95% confidence interval). Negative values represent those tests where the OptiMyo sites had better scores.
Discussion: The EMG Skill results were similar between subjects using sites selected from the first iteration of the OptiMyo system and sites selected following traditional site finding methods.
Conclusion: The first iteration of the OptiMyo system demonstrated equivalence to the current standard of care for myoelectric site finding. There are clear and obvious improvements to be made to the algorithm, and these changes will be implanted with additional testing on limb absent subjects to be completed in the summer of 2022.
Clinical applications: With further improvements the OptiMyo system has the ability to improve the myoelectric site finding process and control strategy selection for upper-limb prosthetics. The OptiMyo system can simplify and streamline the fitting process for clinicians while also providing data on the entire arm during simulated real life-scenarios (different arm movements, weight of socket, etc.).
Future iterations of the OptiMyo system will aim to select the best control strategy, gain, and dead band level for each patient.
Acknowledgements: This project is supported by the Administration for Community Living (ACL), U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $99,971 with 100 percent funded by ACL/HHS (Award # 90BISA0046-01-00). The contents are those of the authors and do not necessary represent the official views of, nor an endorsement, by ACL/HHS, or the U.S. Government.
References
1. Biddiss E., Am J Phys Med Rehabil, 86, 977-87, 2007
2. Chadwell A., Frontiers in Neurorobotics, 10, 2016
An examination of 3-dimensional change for infants with deformational plagiocephaly
Tiffany Graham, MSPO C/LPO, FAAOP(D); Jijia Wang, PhD; Victoria Moses, MPO; Shea Briggs, MPO; Olivia Sheffer, MPO; Amy Payne MPO; Lindsay Pauline, MPO; Tristine Lam, MPO; Ashton Blasingim MPO; Cayman Holley, MPO; Tally Marlow, MPO; Rami Hallac, PhD1
1 University of Texas Southwestern Medical Center, Dallas, Texas, USA, Tiffany.Graham@utsouthwestern.edu
Introduction or purpose: Traditionally, when an infant is treated for a deformational head shape (DHS), asymmetries between the left and right cranium are quantified by taking diagonal measurements along the greater equator of the skull, and asymmetry is expressed comparison of the diagonal length asymmetries1. However, quantification via 2- dimensional measurements at a single level of the cranium might not always accurately portray a 3-dimensional change2. 3-dimen- sional changes were examined in infants treated for DHS asym- metries to compare net quadrant growth during each of these treatment methods, as well as net asymmetry change seen posttreatment (natural growth).
Methods: Two-month old infants with DHS began repositioning therapy (RT) and received physical therapy if torticollis was present. For persistent cranial deformation, caregivers were given the option to begin treatment with a cranial remolding orthosis (CRO) at 4, 5, or 6 months of age. At 6 months of age, any infant who had not switched to CRO treatment was permanently assigned to RT. In- fants received 3dMD scans at 2 months of age, at clinical resolu- tion of their head shape, and at 12 months of age. If their head shape was not resolved by 12 months of age, they received only two 3dMD scans (at 2 and 12 months of age). Clinical resolution was based on measured cranial valult asymmetry index1 and a visual assessment by the treating orthotist.
Consecutive scans were aligned based on 25 landmarks, aniso- tropically scaled, and analyzed using a MATLAB algorithm. A morphometric analysis quantified net 3-dimensional change of the head shape between two consecutive 3dMD scans. The cra- nium was then divided into quadrants. The percentage of net growth of flattened quadrants was found by dividing the differ- ence between mean net growth of the flattened quadrant and the bossed quadrants, divided by the mean net growth of the bossed quadrants. A negative percentage indicated a worsening of the head shape (bossed quadrants growing more than flattened quad- rants) and a positive percentage indicated improvement. Excel was used to plot mean changes in cranial shape and the Kruskal- Wallis test was used to compare mean net percentage change short quadrants between groups.
Results: Twenty-six infants were enrolled and followed. Figure 1 shows morphometric changes for an infant who underwent RT, transitioned to a CRO until the head shape was resolved, and was followed through natural growth to 12 months of age.
Figure 1.
Morphometric changes between consecutive 3dMD scans for a subject treated for a posterior right cranial flattening.
When comparing the net 3-dimensional changes (Figure 2), the percentage of mean net flattened quadrants' growth showed statistical differences between the CRO group and both the RT and natural-growth groups but no statistical dif- ference between the RT and Natural course groups (RT vs
Figure 2.
A comparison of the net 3-dimensional changes based on treatment group (CRO group statistically different from other groups).
CRO p=0.0022*; RT vs Natural p=0.1014; and CRO vs Nat- ural p=0.0015*). The CRO group averaged a positive change in quadrant asymmetries of 23.1%, while the RT group averaged 4.4% improvement and the post-correction group averaged a regression of 0.9%. Due to the methodol- ogy of the study, there were more infants in the RT group (n=26) than CRO group (n=13) or post-correction natural growth group (n=16).
Conclusion: A three-dimensional analysis revealed statistically signifi- cant differences between the CRO group and both the RT and natural growth post correction group, with the CRO group having more favorable reductions of asymmetries.
Significance: Many studies have shown CRO treatment to be effective3, but a few have compared CRO treatment results to RT and natural growth and none have used a 3-dimensional analysis of cranial morphemic changes to compare treatment results.
Disclosure: Authors have no conflicts of interest to disclose.
Aknowledgements: This work was supported by an AOPA Research Award administered by the Center for Orthotics and Prosthetics Learning and Outcomes/Evidence based Practice.
References
1. Holowka MA, et al. J Craniofac Surg; 28(3):717-722; 2017.
2. Abernethy LM, et al. J Craniofac Surg; 33(1):e88-e92; 2022.
3. Kilmo P, et al. Neurosurgery; 79(5), 623-624, 2016.
Assessing lower-limb prosthetic users’ activity levels: A comparison of clinical and real-world measures
Antunes, I. MBE1, Assis, A. MBE1, Castro, M. MBE1, Carvalho, V. BSPO, CPO1
1 Adapttech, biomed@adapttech.eu
Purpose: Users of lower-limb prosthetics have their functional levels assessed through in-clinic self-reported and performance-based Outcome Measures1. In this study, wearable pedometers were used to track their overall levels of activity in real-world settings. The goal of this abstract is to present a comparison between both types of assessment and to demonstrate how daily-life activity monitoring introduces reliability and completeness in mobility potential evaluation, mitigating some limitations of relying exclusively on clinical assessments.
Implementation: Four patients were initially assessed through the collection of AMPPRO questionnaires, from which in- clinic K-levels were obtained. Before leaving the clinic, they received a pedometer to wear every day for eight days. In this period, step data was collected for the derivation of metrics including Blind 2-Minute Walk Tests (B2MWT), corresponding to the number of strides taken during 2 minutes of continuous walking. The average of the B2MWTs collected throughout the evaluation period was determined, as well as the proportion of days with B2MWTs detections. The frequency of occurrence of different stepping rates (cadences) was also determined per patient. Balancing both clinician assessments and derivations from step data2, we could obtain a “Calculated K-level”. This calculation considers metrics such as energy expenditure (kcal burned), peak cadence, daily steps, and cadence variability during the acquisition days.
Results: Data regarding AMPPRO (and resulting K-level) collection, B2MWTs, and step count, for all patients, is shown in Table 1. The frequency of different cadences’ occurrence is pictured on Figure 1.
Table 1.
Patient data collected during study.
| Patient ID | AK1 | AK2 | BK1 | BK2 |
|---|---|---|---|---|
| AMPPRO | 37 | 38 | 35 | 42 |
| In-clinic K-level | 3 | 3 | 2 | 3 |
| Average B2MWT (strides) | 130 | 108 | 92 | 118 |
| % of days with ≥1 detected B2MWT | 75 | 25 | 100 | 50 |
| Average Daily steps | 5989 | 4064 | 9539 | 6071 |
| Calculated K-level 2 | 3.8 | 3.4 | 3.7 | 3.7 |
Figure 1.
Cadence histograms for the four evaluated patients.
Comparisons between the two above-knee (AK1 and AK2) and the two below-knee (BK1 and BK2) amputees were analyzed.
AK1 and AK2, both clinically evaluated as K-3, showed significant differences when remotely evaluated: AK1 performed B2MWTs in 75% of the days, while AK2 only walked for 2 continuous minutes in 25% of the observed days.
Figure 1 demonstrates that AK1 attained higher cadences for a greater percentage of time (≈70% of time at 130-140 steps/min) and registered a higher number of 2-minute gait bout occurrences.
Combining activity monitoring parameters with the initial in-clinic evaluation, AK1 achieved a “Calculated K-level” of 3.8, which is corroborated by a set of metrics that dictate a typical K-4 profile3 (5000 or more daily steps and best registered cadence above or equal to 100 steps/min). AK2 showed a lower level of activity, with a daily step count typical of K-3 profiles3 (2500 or more daily steps), and their “Calculated K-level” was of 3.4.
At the clinic, BK2 was rated as a K-3, whereas BK1 was classified as a K-2 (Table 1). BK1 walked at lower cadences than BK2 (Figure 1), but exhibited higher levels of daily activity, with around 2000 B2MWTs detected at a pace of 90–100 steps per minute. Table 1 also reveals that, although BK2 only walked continuously for 2- minute bouts in 50% of the days, BK1 performed B2MWTs every day. For both, the daily step count achieved was typical of K-4 prosthesis users2, with BK1 presenting a considerably higher value (taking, in average, 3468 more daily steps than BK2).
The “Calculated K-level” was 3.7 for both patients, which is supported by established reference cadence values2 that place both patients in high gait intensity ranks (cadence above 80 steps/min) and above the defined thresholds of typical K-4 profiles3.
Conclusion: In this study, remote monitoring proved to be effective in the evaluation of patients, complementing their clinic assessment, and supporting a more informed decision regarding K-level attribution. In conclusion, remote monitoring may provide a more thorough and accurate picture of a patient’s ability to ambulate in real-world situations.
References
1. Heinemann, Allen et al. Physical medicine and rehabilitation clinics of North America, (2014), 10.1 016/j.pmr.2013.09.002.
2.Orendurff, M. S. et al. J Rehabil Assist Technol Eng 3, (2016), 10.1177/2055668316670535
3. Godfrey, et al. JPO Journal of Prosthetic and Orthotics 30, 20-30, (2018), 10.1097/JPO.0000000000000166.
Characteristics of prosthetic and orthotic device users utilizing ADA paratransit services
Caitlin Bowman*, BS, and Clive D’Souza, PhD
University of Pittsburgh, Department of Rehabilitation Science and Technology, Prosthetics and Orthotics Program * clb276@pitt.edu
Gerald Stark, Ph.D, MSEM, CPO/L, FAAOP
Director of Clinical Affairs, Ottobock Patient Care, Signal Mountain Tennessee
Introduction: The World Health Organization (WHO) reports a 69.4% increase in years lived with a disability worldwide in the last 20 years, with 2.41 billion people needing access to rehabilitation healthcare1. Currently, the US Centers for Disease Control (CDC) reports 1 in 4 people have a disability, and 25% of all adults living with disability do not have adequate access to healthcare2. The International Society of Prosthetics and Orthotics (ISPO) identifies transportation as a key barrier to orthotic compliance3. Aligning with the WHO’s Biopsychosocial Model of Disability, as well as a known social determinant of health, access to transportation significantly impacts a person’s ability to receive orthotic and prosthetic (O&P) care. ADA paratransit services are curb-to- curb services provided by public transit agencies to supplement transportation needs of people with disabilities for work, education, and healthcare who report difficulty using conventional fixed-route transit services. However, many people with disabilities report barriers and difficulties with paratransit services, making it hard to be compliant with their healthcare appointments. This study aimed to better understand the characteristics and travel needs of paratransit users that also reported using an O&P device. No study to our knowledge has described O&P patient demographics as it relates to paratransit use.
Methods: This study was a secondary analysis of data collected by the Ann Arbor Area Transportation Authority (TheRide, Ann Arbor, MI) as part its routine process for determining applicant eligibility for ADA paratransit services. The study used de-identified secondary data and was hence determined to be IRB exempt. Of 3,000 approved ADA application forms from 2015-2018, 1,440 forms were randomly selected.
Information about demographics (sex, age), mobility aid(s), medical condition, and barriers to transit were transcribed for analysis. A section of the application form requires a licensed professional (social worker, PT, OT, MD) to verify medical diagnosis, which were subsequently converted to ICD-10 codes. The present analysis focused on a subset of ICD-10 codes common to O&P patient populations yielding a sample of 323 paratransit users.
Results: Fifty-four of the 323 (or 16.7%) users selected reported using a prosthetic (N = 17) or orthotic (N = 40) device (3 users reported using both). P&O users were significantly younger (mean ± SD: 54.5 ± 20.2 years; range 10-94 years) than non- P&O device users (62.3 ± 20.0; range 16-102 years; t = 2.58, p = 0.010), and with 54% (vs. 62%) identifying as females. Nearly 67% (N = 36) of the P&O users had multiple chronic conditions, compared to 60% of those who did not use P&O devices. Figure 1 lists the eight prevalent diagnoses among P&O users (Figure 1). Users of a P&O device also reported other mobility devices, namely, cane (46%), walker (39%), manual wheelchair (30%) and powered wheelchair (28%). Among people not using a P&O device, mobility devices used were: cane (37%), walker (35%), manual wheelchair (30%), powered wheelchair (25%), scooter (4%), portable oxygen (3%), service animal (3%), and crutches (2%).
Figure 1.
Counts for the eight most prevalent diagnoses among paratransit users (N=323) with P&O devices vs others.
Conclusion: Inadequate transportation and multiple chronic conditions could explain non-compliance with O&P care. Transit barriers to O&P care could help explain the reported lack of using or having an O&P device among users with certain conditions, such as amputation. Analysis is ongoing to investigate associations between health measures including the Charleston Comorbidity Index and environmental barriers using the International Classification of Functioning, Disability, and Health (ICF). Further research using the ICF is needed to quantify impacts of transportation barriers on patients’ ability to obtain O&P devices and maintain treatment compliance.
Significance: All patients deserve access to O&P care, and transportation to and from appointments impacts accessibility of care.
Understanding which O&P patient subpopulations experience transportation barriers allows clinicians to advocate for these patients. This knowledge will help practice administrators identify O&P patients having greater need for paratransit services, and/or requiring different scheduling considerations.
Disclosure: Neither author have potential conflicts of interest to disclose.
Aknowledgements: This study was funded by the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) via grants #90IF0094 (2015-2018; PI: Clive D’Souza), and #90RTHF0001 (2018-2023; PI: Michelle Meade). The authors are grateful to TheRide for the data provided.
References
1. Cieza A et al. 2019. Lancet. 2020;396(10267):2006-2017. doi:10.1016/S0140-6736(2032340-0)
2. Centers for Disease Control and Prevention, Disability and Health Data System (DHDS) https://dhds.cdc.gov
3. Marcotte D, et al. Prosthet Orthot Int. 2022. doi:10.1097/PXR.0000000000000145
Clinical Survey of Transtibial and Transfemoral Initial Alignment Methodologies
Gerald Stark, Ph.D, MSEM, CPO/L, FAAOP
Director of Clinical Affairs, Ottobock Patient Care, Signal Mountain Tennessee
Introduction: Clinically, transtibial and transfemoral initial alignment methodology seems to differ greatly between clinicians and locations, even though many of the parameters and guidelines have been historically established in prosthetic programs.1,3,4,5 Anecdotally the author has encountered many heuristics that vary and may be reflective of clinic type, volume of fittings, and experience level. Certain aspects of hip or knee flexion, initial foot placement in the frontal and sagittal planes, and adduction of the interface appear to have evolved or altered due to componentry limitation s and/or combine the practice of bench alignment with initial static fitting. One common practice is to have the transtibial patient stand with full load bearing while supported in a “natural” or comfortable knee flexion. Transfemoral initial alignment also varies with componentry and patient variation
Methods: Initially a qualitative phenomenology was conducted with five (5) practitioners with 2, 11, 17, 22, and 35 years of experience. The aspects that were consistent to influence methodologies were experience, office type, patient volume, alignment methodologies, frontal/sagittal foot position, knee/hip flexion, hip/knee adduction. A 9-question survey created on a third- party survey provider and the link was posted on the O-and-P List Serv and open for 24 days from 5/17/22- 6/15/22 with three reminders. The questions were divided into categorical variables of experiencee, office type, and volume demographic factors, then Likert weighting of transtibial and transfemoral alignment features, then a comment section regarding differences of initial alignment in the way it was taught vs. the clinical methods used currently.
Results: The survey resulted 114 respondents with 100% completion rate and average time of 5m:45s, which is slightly lower 90.5% degree of confidence by Slovin’s estimation. 2 As with other surveys 26 years or more was the highest percentage with 29.82% but 6-10 years second at 17.54%. Regional Multi-Center was higher with 29.82% followed by Single Private Office at 24.56%. The number of new Transtibial Patients per month was evenly distributed with 22.81% saying 4-5/month followed by 21.05% of 2-3/month.
Transfemoral was more definitive with 42.11% indicating 2-3/month. A majority, 28.95%, indicated they perform their initial bench alignment with a patient weight bearing on a stand and the alignment lines are drawn with vertical lines at the proximal bisection and 23% indicated their own “special” methods. 21.05% indicated they followed original bench alignment practice before weight bearing. highest at 3.71 weighting, then Frontal plane set at MTP Bisection at 3.43, and then Knee Flexion of Socket at 5-7° at 3.34. Lowest was Foot set posterior in sagittal plane at 2.88. For Transfemoral Alignment a clear majority still used TKA at 79.82% and the European Plum Line at 10.53%. Highest rated practice was Hip Flexion 5° more than Hip Contracture at 3.97 then Foot Outset at 3.68, and Socket Adduction at 7°-12°at 3.58. Lowest was begin with 0° hip flexion at 2.14. In terms of comments 78 of the 114 answered with 28 answered alignment is very different than in school because their experience has provided reference. 12 indicated that their “Eye Ball Method” is satisfactory. Conversely, 23 said they follow the rules from school as a starting point and make adjustments as needed and 14 indicated they follow manufacturers established guidelines.(Figure 1)
Figure 1.
Survey results of TT initial alignment practices.
Discussion: Transtibial and “Other” and “Natural” alignment was rated highly, which may indicate greater individuality of alignment heuristics. Although there were many correlations of the factors most were only slight at (r ≃ 3.5). More simple alignment methods, eliminating flexion, adduction, and foot position were significantly related to volume, but only slightly. Experience level to type of alignment method was also significantly related but also only slightly. There were no significantly predictive relationships except R2=.534 between TT per month and inset, TF per month, TT Natural alignment, and Type of office.2
References
1) NUPOC TT & TF Prosthetics Manual, (1991).
2) Field, A., Discovering Statistics, 2009
3) Radcliffe, C. Artif Limbs (1955)
4) Radcliffe & Foort, UCB Biomechanics (1961)
5) Blumentritt, S. Prosthet Orthot Int (1997)
Comparative observational pilot study – blind test hydrostatic casting vs. other residual limb impression methods
Jeffrey A. Denune, CP/L
Motus Research LLC
Introduction: To maximize socket performance and comfort without adversely affecting residual limb health, a prosthetist custom fits a socket for every patient using plaster wraps or computer aided design (CAD). Although the use of the socket is to ambulate in full weight bearing environment, currently almost all of fittings and plaster casting takes place in a seated or standing in non- weight bearing environment. Hydrostatic casting while bearing weight is an alternative to traditional casting impression methods in providing lower limb amputees. Previous research related to the new method have shown positive results in regard to the patient’s acceptance, the limited number of necessary modifications and the high amount of successfully produced sockets. For this study, the application and fit of the sockets in relation to proprioception, the mastering of a distance and the length of distance, as well as the patient’s subjective perception were examined and the results were compared to other shape capture methods.
Method: In a pilot study of three different Trans-Tibial residual limb shape capture methods for producing prosthetic sockets were compared. I) Traditional plaster hand casting (reference group-1), II) Optical scanning / CAD tracer (reference group-2), iii) Hydrostatic cast impression, the Symphonie Aqua System enables the shape capture under load (weight bearing, Test group-3) of the residual limb. A plater impression is taken of the residual limb in a standing position. Simulation of a prosthetic socket under actual loading conditions and to produce a plaster impression while bearing full weight. Due to the hydrostatic pressure, the sensitive areas, bony structures, pressure and pain points, tissue on the residual limb are recognized. The plaster impression is smoothed only with minimal modifications. The resulting socket fit to the anatomy of the residual limb. All three shape capture techniques currently require a diagnostic / test socket made of a thermoplastic material to confirm fit and patient comfort. After trying the test socket on the patient in a static and dynamic environment. It is commonly modified until an acceptable wearing comfort level is reached, and the fit is considered correct from the Prosthetist and patient’s feedback, and considerations of biomechanical points of view.
Participants: Seven Trans-Tibial amputee patients were recruited (2 females, 5 males), aged 20 to 70 years, in varying states of physical condition. Three of the study participants were amputated on the left side, four on the right side. K2 and K3 subjects were chosen dependent on level of ambulation with or without assisted devices.
Apparatus: Optical the following equipment/apparatus were used for the study: scanning / CAD tracer and Hydrostatic cast impression using the Symphonie Aqua System.
Procedures: For the Omega CAD, subjects Omega CAD files were all modified by the author, reducing the scan by -5% globally. The aqua system was performed by trained prosthetist from Romedis GmbH, who smoothed the plaster model. The hand cast was the SoC socket and they were modified in the conventional manner by each subjects provider Prosthetist.
Statistical analysis. Because of limited number of subjects in this pilot study, no statistical analysis could be performed, the results from this study will however, be critical to determine sample size for a larger controlled randomized study.
Results: The comparison of the volume demonstrated that the hydrostatically produced sockets had a larger volume than those produced by either the plaster hand cast method or the 3D optical scanning method.
TUG: the hydrostatic socket, the mean time for performing TUG was 9.12 sec (n=7), whereas hand cast socket mean time required to perform TUG was 14.06 sec and the 3D scanned socket mean time for TUG was 11.55 seconds.
2MWT: This test revealed that the subjects using the hydrostatic socket were able to walk a longer distance (91.0 meters) in two minutes than with the other sockets (Mean for hand cast = 85.5 meters) for the and 88.3 meters for the 3D scanned socket.
Conclusion: All seven patient’s shape captured under a weight bearing environment comment that the Aqua socket was more comfortable even though the socket was obviously larger than the traditional hand cast or CAD sockets. The Aqua sockets presented a very different shape than traditional sockets, with the distal end being more bulbous. All seven felt that the suspension was equal to or better than the comparator sockets. A better understanding of how this can play a roll in improved limb health and circulation is needed in future research.
Funded by Romedis GmbH
Compensatory trunk movements of transfemoral amputees when walking with different gait velocities
E Pröbsting1, M Ernst1, TM Köhler1, T Schmalz1, V Schopper1,2, Malte Bellmann1
1 Ottobock SE & Co. KGaA, Clinical Research and Services, Biomechanics, Germany, 2 German Sport University Cologne, Germany. Eva.Proebsting@ottobock.de
Introduction: After transfemoral amputation, asymmetric motion patterns of the pelvis and upper body can be observed in the frontal plane. During the prosthetic side stance phase, an increased lateral trunk lean toward the prosthetic side has been shown [1-4]. Different calculation methods are used to determine the trunk movement. In orthopedic technology, the 7th cervical vertebra (C7) is usually taken as an orientation for the trunk overhang.
Methods: Based on the experience in orthopedic technology, a marker model for motion analysis of persons with a transfemoral amputation (TF) was developed, which determines, among other things, lateral trunk lean in the frontal plane using the axis from C7 to the sacrum and the center of the pelvis for a new trunk segment (Figure 1). Level walking of 10 transfemoral amputees with 3 different velocities (slow, mid, fast) was biomechanically analysed.
Figure 1.
Definition of a new segment, the C7-Sacrum- Segment, to define compensatory trunk movements of transfemoral amputees. Lateral trunk lean is defined as the frontal angle between this segment and the global coordinate system, normalised on a static trial.
All subjects used a microprocessor knee joint (Genium, Ottobock) for gait analysis and in daily life. An optoelectronic camera system with twelve Bonita cameras (VICON, GB) was used to record the kinematics and two linked force plates (KISTLER AG, CH) recorded the kinetics. For comparison, the same analysis was performed for 30 non- amputee subjects (NA).
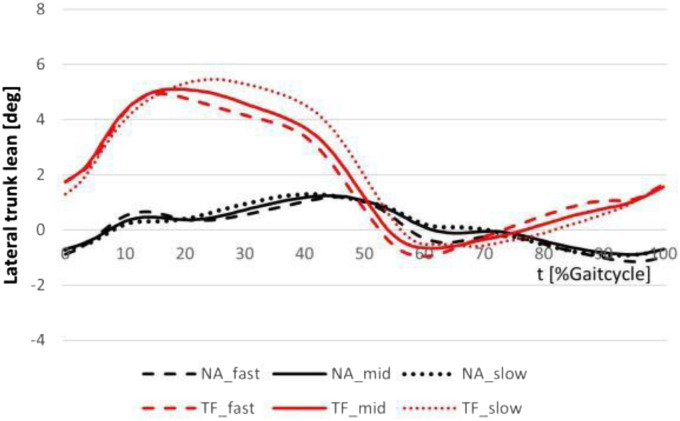
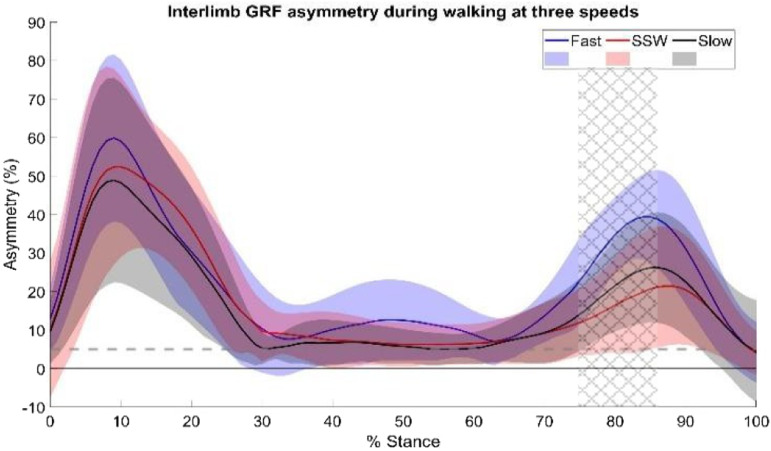
Results: The lateral trunk lean of the TF is extremely different from the result of the NA. A different motion pattern with a larger range of motion was observed (see Figure 2). During prosthetic side stance the trunk leans to the ipsilateral side and is rapidly moved to the contralateral side at the end of stance. The maximum range of motion of this segment is increased in the TFs with 6.5deg (slow), 6.2deg (mid), 6.3deg (fast) compared with 2.3deg (slow), 2.1deg (mid), 2.4deg (fast) in the NAs. No difference could be found between the different velocities in the NAs. A longer period of maximal ipsilateral trunk lean was observed in the TF group.
Figure 2.
Lateral trunk lean of TF (red) and NA (black) during level walking with three different velocities.
Conclusion: The pattern of lateral trunk lean determined with the new segment shows comparable results as described in the literature [1-4]. A clear difference of this motion between NA and TF could be shown. In both groups, the range of motion is the lowest with the mid velocity. For TF the motion pattern changed slightly with changing speed, showing greater compensatory mechanisms when walking at slow and fast self-selected speed. With a similar use of a marker on the C7 and the sacrum Köhler et al. showed that this parameter could be useful to determine a suitable socket adduction position in the frontal plane [4]. In the latter, no segment was defined. An angle calculation was used based on the projection of the markers onto the frontal plane of the global coordination system. Nevertheless, the pattern and range of motion are comparable to the results of the 3D calculation method in the current study.
Significance: The lateral trunk lean analysed with a segment using the C7, the sacrum and the center of pelvis shows a relevant compensatory mechanism of TF amputees and could be used for determining prosthetic aspects.
Disclosure: Eva Pröbsting, Michael Ernst, Thomas Maximilian Köhler, Thomas Schmalz and Malte Bellmann are full time employees of Ottobock.
References
[1] H. Goujon-Pillet et al (2008)
[2] A. Cappozzo et al (1982)
[3] C.M. Butowicz et al (2018)
[4] T.M. Köhler et al. (2021)
Design and fitting of a custom-made carbon-fiber ankle foot orthosis for sprinting
Francesca Gariboldi1, Matteo Grandi2, Fabrizio Giacchi2, Gregorio Teti2, Nicola Petrone1, Andrea Giovanni Cutti2
1 University of Padova, Italy; 2 Centro Protesi INAIL, Italy E-mail: francesca.gariboldi@phd.unipd.it
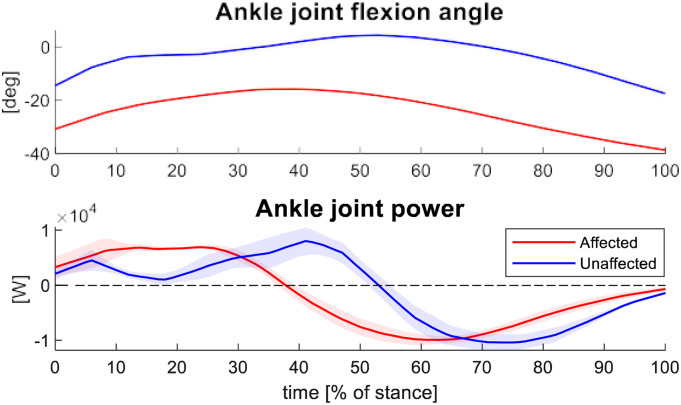
Introduction: Ankle Foot Orthoses (AFOs) are commonly prescribed to improve gait in patients with foot drop disorder1. However, their application for sport activities in subjects with spastic hemiplegia is rare. This study describes the design and fitting of a custom-made carbon-fiber composite AFO for sprinting to be used in combination with conventional spiked sprinting shoes, for a 26-year-old female paralympic athlete with an acquired right spastic hemiplegia. The athlete came to our observation after rejecting a traditional AFO with neutral ankle alignment (0° ankle flexion) which did not conform to her ankle attitude during running and lacked sufficient foot frontal plane stability, causing her foot to continuously slip out of her shoe, and eventually leading to the formation of an edema to her lateral malleolus. The custom-made AFO had to fulfill the following requirements: satisfactory energy storage and return (ESR) exploiting the non-spastic range of motion; sufficient forefoot flexion; stability of the foot on the frontal plane; avoiding knee hyperextension.
Methods: To maximize energy storage and return, the AFO was designed to allow ankle flexion well outside the subject spastic range, i.e. from 10° of ankle plantarflexion to any degree of dorsiflexion. Therefore, during casting, the AFO neutral position was set to around 40° of ankle plantarflexion, to allow the athlete to take advantage of 30° range of flexion for ESR. Moreover, to promote ESR, the AFO was designed with an anterior shell2. The carbon fiber layup was designed to create different areas of stiffness. The AFO insole heel and posterior bar (area 1) had to be stiffer to allow most ESR, while the forefoot insole plate (area 2) had to be more flexible to ensure a metatarsophalangeal flexion of over 40° without breaking, which is the value that we measured on the athlete during sprinting start. The AFO was integrated in a commercially available and certified sprinting shoe with spikes for track (Figure 1): the AFO insole plate was covered with anti-slippery material and inserted in the shoe through a cut performed in the shoe heel counter.
Figure 1.
AFO integrated in a sprinting shoe with spikes.
The behavior of the AFO was assessed through high-speed video analysis during training and competition (sprinting), and through a full indoor biomechanical assessment with force plates and an optoelectronic mock-up system during skipping, to assess a high force, high frequency condition. Results of the biomechanical assessment are reported in the results section.
Results: The AFO mold was digitally rectified and carved in polyurethane foam. The AFO was then manufactured with prepreg carbon fiber, modulating the stiffness by adjusting the layup in the 2 areas: 7 unidirectional plies (area 1); 1 unidirectional ply between 2 twill plies (area 2).
The subject gave a positive response to the custom-made AFO in terms of stability, not reporting any pain, and was able to successfully use it for the Tokyo 2020 paralympic games. No failures were reported in more than 6 months of use.
Results of the biomechanical assessment of skipping are reported in Figure 2 and refer to 3 body weight (1800N) of maximum vertical load. The ankle joint angles display a similar trend and range (20°) with an angular offset of around 20°, illustrating how the AFO is effective in mimicking the unaffected trend while keeping the affected ankle outside the spastic range. There is also a similarity in the power trend between affected and unaffected side.
Figure 2.
Ankle dorsi(+) / plantar(-) flexion and ankle power (compression(+) / extension(-)) normalized to stance time.
Conclusion: The custom-made AFO with anterior shell and two different stiffness areas proved to be effective for the athlete, allowing her to compete at national and international levels.
Significance: This study could provide a reference for the design and construction of custom-made AFO for subjects with spastic hemiplegia aiming to engage in athletics track competitions.
Disclosure: None.
Acknowledgement: The authors kindly acknowledge INAIL and the University of Padua for funding the study through the OLYMPIA project.
References
1. Pourhosseingholi E, et al. Med J Islam Repub Iran. 3, 33:50, 2019.
2. Chen C, et al. Brain Sci. 12, 454, 2022.
Effect and benefit of ankle foot orthoses for patients with weakness of the plantar and dorsiflexors: Biomechanical comparison of different orthotic concepts.
T Schmalz1, M Bellmann1, M Burkhardt2, H Drewitz1, A Kannenberg3
1 Ottobock SE & Co. KGaA, Clinical Research and Services, Biomechanics, Germany, 2 Albert-Ludwigs- University Freiburg, 3 Otto Bock Healthcare LP USA. schmalz@ottobock.de
Introduction: Patients with both plantar and dorsiflexor weakness often show abnormal knee loading in addition to instabilities of the ankle joint. This can be treated using ankle-foot orthoses (AFO) that utilize effects of the ground reaction force (GRF) [1,2]. Options are jointless carbon fibre orthoses (JLO) and articulated orthoses, which can be further differentiated into AFOs with conventional ankle joints (small ROM, rigid stops – CAJ) and those with expanded ROM and customizable resistance to both movement directions (“reactive- dynamic ankle” – RDA [3]). The aim of the present study was to compare the effectiveness of different AFO concepts for supporting movement patterns of daily living using biomechanical parameters.
Methods: Seven patients (91±15kg, 1.85±0.10m, 57±15y) with plantar and dorsiflexor weakness resulting from various neurological conditions (manual muscle test grades 1-3 [4]) were enrolled in the study. All patients currently use an RDA-AFO (4 bilaterally, 3 unilaterally) and have previous experience with either JLO or CAJ. Four orthotic configurations (RDA, CAJ, JLO, no orthosis - WO) were studied during the following movement patterns: self-paced level walking at medium speed, walking up and down an incline (10°), and standing on an incline (+10°, 0°, -10°). Kinematic data was measured with an optoelectronic system (VICON) coupled with two force plates (KISTLER) to measure GRF.
Results: Walking without orthoses, two patients showed knee hyperextension, one a distinct crouch gait, two a tendency towards crouch gait, and two normal knee joint characteristics. The unphysiological dorsi and plantarflexion WO was reduced by all AFO-types. With CAJ, excessive reductions of 6-7° dorsiflexion and 7-9° plantarflexion at push-off were measured in all tasks compared to RDA and JLO (p<0.01). This effect was accompanied by reduced horizontal propulsion forces, reduced peak ankle power at push-off and partially abrupt knee extension during stance. No significant differences were found between RDA and JLO; both AFOs stabilised the ankle and normalised knee movement and loading (Figure 1). When standing WO, slightly increased knee flexion (2-12°) and forward trunk inclination (1-5°) were found in all tasks. All AFOs show a normalising effect when standing uphill.
Figure 1.
External orthotic side sagittal knee moment walking up an incline. Group mean curve of bilaterally (left) and unilaterally (right) affected patients. Norm data of healthy control group shown as grey shaded area.
Conclusion: CAJ restrict the physiological dynamics of locomotion and lead to partially abnormal knee loading. RDA and JLO show considerably greater patient benefits. In the studied movement tasks, these two orthosis concepts show similar effects and largely normalise movement and loading patterns of the knee. For more demanding activities, e.g., steeper inclines or uneven surfaces, patients anecdotally report advantages of RDA over JLO. These activities should be investigated in future studies.
Significance: The RDA concept increases the effectiveness of AFO fittings used for patients with both plantar and dorsiflexor muscle weakness.
Disclosure: Thomas Schmalz, Malte Bellmann, Heiko Drewitz and Andreas Kannenberg are full time employees of Ottobock.
References
[1] S.F. Tyson et al. (Clin Rehabil 2013)
[2] T. Kobayashi et al.(Clin Biomech 2017)
[3] T. Schmalz et al. (JPO 2022)
[4] V. Janda (Interdruck Leipzig 1972)
Effectiveness of a 3D-printed cranial orthosis with novel closure system
Jared Howell, MS, CPO/L, FAAOP1, Russ Lundstrom, MS2, Hannelore Willenborg, Dr.3, Dorothea Daenter, Prof. Dr. med. Msc3
1 Baylor College of Medicine, Houston, TX, 2 Ottobock, Austin, TX, USA, 3 Hannover University Hospital Center, Hannover, Germany
Introduction: Cranial remodeling orthoses (CROs) are used to correct positional cranial deformities in infants: plagiocephaly, brachycephaly, or a combination of these two deformities. CROs have historically been manufactured using a thick foam inner lining covered by a thermoplastic shell. Fitting of these orthoses requires frequent adjustments and management for removal of foam lining and shaping by the orthotist. With growing popularity and availability of quality 3D printer’s new designs have emerged and been FDA cleared as alternatives to the historical approaches.
This study was designed to assess the effectiveness of a 3D- printed CRO with a novel closure mechanism (Ottobock MyCRO Band), as well as any adverse effects associated with this treatment, to educate health professionals and authorities on the benefits of CRO treatment for cranial deformities.
Methods: This is a cross-sectional study consisting of a collection of retrospective clinical data from orthotists from May 1st, 2020, through May 1st, 2021, along with a survey of parents that included the Quebec User Evaluation of Satisfaction with assistive Technology 2.0 (QUEST). The effectiveness was measured comparing the head deformation at the beginning and end of treatment. Cranial measurements, width, length, and two transcranial diagonals taken 30 degrees off midline, were taken to calculate the cephalic index (CI), the ratio of the cranial width and length, and the cranial vault asymmetry index (CVAI); the % difference between the diagonals.
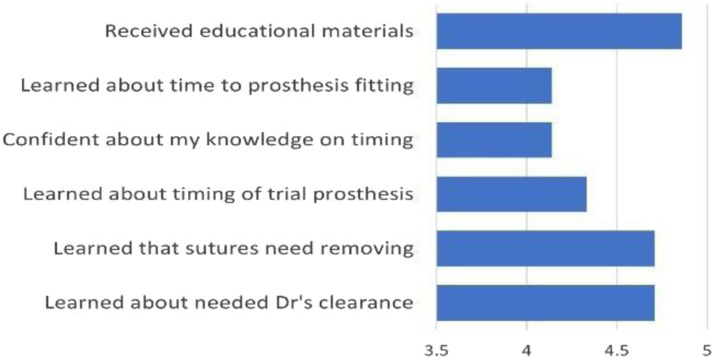
Results: 12 O&P clinics in France participated. 452 infants were eligible for study enrollment: 41 were excluded as consent of parents was not obtained, and 2 were excluded as deformation characteristics were missing. Correction of cranial deformation was analyzed on 362 infants. The mean age was 6.6 months (3.3 – 17.8), 74% male. 196 (47.9%) had plagiocephaly, 66.8%, 25.5% and 7.7% severe, moderate and mild, respectively. 91 (22.2%) had brachycephaly, 70.3% severe and 29.7% moderate, and 122 (29.8%) had asymmetrical brachycephaly, 67.7% severe and 32.8% moderate. 313 parents responded to the survey.
Mean treatment duration was 135.7 days, longer for severe deformation (144.1) than for moderate (119.5). During the first visit, the 1st scan of the head was performed. During the 2nd visit, after an average 9.2 days, the orthosis was delivered.
First, second and third visits with 3D scans were conducted an average of 6.4, 12.7 and 19.4 weeks after CRO, respectively. During the first 3 months, 95% of parents reported that the infants were wearing their CROs every day, 83%, higher than 22 hours per day, and 13%, between 15 and 21 hours per day. the infants with the CRO only part-time; they also reported that 87% of infants never remove their CROs by themselves.
For plagiocephaly, CVAI was significantly reduced by 6.1 points (p < 0.0001). For brachycephaly, CI was significantly reduced by 7.6 points (p < 0.0001). For dual diagnosis CVAI was significantly reduced by 4.8 points (p < 0.0001) and CI was significantly reduced by 6.3 points (p < 0.0001). (Figure 1)
Figure 1.
Reductions of head deformation over time.
During the CRO treatment, mean cranial perimeter increased from 440.1 to 459.4 mm. Parents reported a global satisfaction score of 4.5 / 5 from the QUEST, and 88% of parents were quite satisfied or very satisfied with the CRO treatment.
Discussion: The average changes in CI and CVAI seen in this study after CRO treatment were similar to those reported in the literature.
Conclusion: The effectiveness of early treatment with a CRO was confirmed with a significant reduction of cranial deformation reported on the analysis of infants with cranial deformation. The survey completed by the parents confirmed a general high level of satisfaction. During the CRO treatment, cranial perimeter growth was not limited by the orthosis.
Significance: The MyCRO band is an effective treatment option for positional cranial deformities in infants.
Disclosure: Russ Lundstrom is an employee of Ottobock HealthCare. Jared holds a faculty appointment in the department of PM&R at Baylor College of Medicine, and an affiliation with Ottobock Patient Care, LLC.
Effects of physical therapy and compliance with deformational head shape treatments
Victoria Mosses, MPO; Jijia Wang, PhD; Shea Briggs, MPO; Olivia Sheffer, MPO; Amy Payne MPO; Lindsay Pauline, MPO; Tristine Lam, MPO; Ashton Blasingim MPO; Cayman Holley, MPO; Tally Marlow, MPO; Tiffany Graham, MSPO, C/LPO, FAAOP(D)1
1 University of Texas Southwestern Medical Center, Dallas, Texas, USA, Tiffany.Graham@utsouthwestern.edu
Introduction or purpose: A deformational head shapes (DHS) is often treated with repo- sitioning therapy (RT) or a cranial remolding orthosis (CRO), and infants with torticollis are recommended to receive con- current physical therapy (PT)1. Adherence with CRO treat- ment protocols have been shown to affect CRO treatment outcomes2 but the affect of concurrent PT has not been thor- oughly examined. This study examines the impact of compli- ance with RT, PT, and CRO wear on DHS treatment outcomes and investigates factors which may influence compliance.
Methods: Two-month old infants with DHS began RT (and PT if torticollis was present) and were measured monthly while in treatment. For persistent cranial deformation, caregivers were given the option to begin CRO treatment at 4, 5, or 6 months of age. At 6 months of age, any infant who had not switched to CRO treatment was permanently assigned to RT. At 12 months of age, infants received final evaluations. Caregiver surveys were taken at follow up visits.
Definitions of treatment compliance:
Infants attend ≥70% of all recommended visits AND
RT: "always/often" repositioning at ≥90% of visits
CRO: "always/often" wearing 23 hours/day at ≥90% of visits Participant demographics were complied in Excel and Chi- square test used to compare gender distributions. MATLAB was used to examine changes in compliance based on survey answers. Overall compliance was reported based on treatment group. Fisher's exact test was used to compare overall rates of compliance and severity distribution by treatment group.
Results: Forty three infants were enrolled and followed. No statistical differences were found in gender distributions (p=0.4164). In- fants with concurrent PT were more compliant with head shape treatment than the infants who were not concurrently enrolled, but differences were not statistically significant (Table 1). Caregiver happiness with their child's head shape and infants attending daycare ≥3 days/week were not found to have significantly different treatment compliance. In RT, in- fants who stayed positioned for ≥10 minutes at a time were more likely to achieve cranial correction (100% vs 75% cor- rection; p=0.5147).
Table 1.
Treatment compliance by treatment group. No statistical differences between subjects with or without concurrent PT.

|
Compliant infants achieved correction more often than noncompliant subjects (Table 2) There was no statistical dif- ferences between severity-head shape subgroups, but when stratisfying by severity alone, the RT group had statistically fewer severe head shapes than the RT+CRO group (RT mod- erate n=13 and severe n=5 while RT+CRO moderate n=3 and severe n=10; p=0.0113).
Table 2.
Distribution of infants who did and did not achieve correction, based on treatment groups (no statistically significant differences).

|
Conclusion: Infants who were more compliant tended to correct their DHS more often, and concurrent enrollment with PT improved compliance. Statistical results are limited by the number of in- fants included, a larger study is needed for future analysis. In this study, more severe infants tended toward the RT+CRO group and therefore the correction rates cannot be directly compared between treatment groups, but results support a link between compliance and correction rates within the treatment groups. (Table 3)
Table 3.
Presenting severity3 distribution by treatment group.

|
Significance: Torticollis has been shown to complicate RT treatment4. Re- sults indicate infants with torticollis should be concurrently enrolled in PT to improve their chances of correcting their head shape. Factors other than compliance contribute to the success of DHS treatment, but the importance of compliance should be emphasized at clinical visits.
Disclosure: Authors have no conflicts of interest to disclose.
Aknowledgements: This work was supported by an AOPA Research Award ad- ministered by the Center for Orthotics and Prosthetics Learn- ing and Outcomes/Evidence based Practice.
References
1. Kilmo P, et al. Neurosurgery; 79(5), 623-624, 2016.
2. Corso J & Thach S. AAOP Annual Meeting, Nashville, TN, USA, 2023.
3. Holowka MA, et al. J Craniofac Surg; 28(3):717-722; 2017.
4. Steinberg JP, et al. Plast Reconstr Surg; 135, 833-842, 2015.
Feasibility of predicting successful return to duty following major lower limb injury using clinical outcomes
Riley C. Sheehan, PhD1-3, W. Lee Childers, PhD, CP2-4, John Fergason, CPO, PLO2, Megan Loftsgaarden, DO2, Joseph Alderete, MD, FAOA2
1 Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., 2 Center for the Intrepid-Brooke Army Medical Center, 3 Uniformed Services University of the Health Sciences, 4 DoD/VA Extremity Trauma and Amputation Center of Excellence riley.c.sheehan.ctr@health.mil
Introduction: Major lower extremity injury is prevalent across civilian and military sectors. These injuries often result in complex limb salvage operations or amputations which can limit functional abilities1. Military service requires a high level of function and can represent the upper end of community ambulation.
Advances in orthotic and prosthetic (O&P) care, as well as surgical and rehabilitation interventions, enable injured Service Members (SM) to regain high levels of function following their injury2. Following injury and treatment, the medical and command teams must determine whether a SM may return to duty (RTD) with or without limitations, or if the SM meets physical and medical requirements to deploy.
There are many factors that influence a SM’s ability to perform their duties. It can be difficult to evaluate and consider all of these factors in RTD decision-making. While several screening tools exist, the decisions rely heavily on provider knowledge and experience with very little precision application or widely applicable tools. Many of those experienced clinical providers have retired from active service creating a need for tools that can fill the experience gap and inform clinical decision-making. Classifier models are one method to combine multiple factors and predict appropriate classification of new samples (e.g., RTD or separation). The goal of this study was to determine the feasibility of developing a model to predict successful RTD following major lower limb injury based on clinical outcome measures.
Methods: This analysis leveraged previously collected outcome data for SMs with major lower limb injury that required the use of O&P devices3,4. Of the 11 SMs we followed up with, 6 returned to duty with no restrictions while the other 5 did not RTD or had some form of activity limitation. Physical function was evaluated using the Lower Extremity Function Scale (LEFS), two novel physical performance measures specifically designed to evaluate lower extremity function in SMs (Stand-Prone-Stand and Stand- Kneel-Stand)5, and three measures extracted from a simulated dismounted patrol assessment (distance completed, frontal and sagittal angular momentum)3. All data collections were approved by the local IRB.
A LASSO regression with a binomial distribution was used for this initial evaluation. The process selects the most relevant variables and creates an equation that predicts a probability of successful RTD between 0 and 1. In order to translate the probability into a classification (e.g., successful vs unsuccessful RTD), Receiver Operating Characteristic plot was used to determine the optimal threshold value for the classification. The model was evaluated using the sensitivity, specificity, and overall classification accuracy.
Results: The LASSO regression identified the LEFS and the Stand- Kneel-Stand time on the uninjured side as the relevant factors. Using the optimal threshold value of 0.61, 10 of the 11 participants were correctly classified. The sensitivity was 0.83, specificity was 1, and the overall classification accuracy was 0.91.
Conclusion: The LEFS and Stand-Kneel-Stand time on the uninjured side were able to correctly classify a SM’s successful RTD. This model may also work for classifying any P&O patient’s return to high function. Kneeling to standing transitions require strength, range of motion, and coordination beyond that needed for basic ambulation. In addition, both outcome measures can be collected quickly in a clinical setting and could be used to demonstrate the potential of a patient to return to high function. While this analysis was based on a small dataset, it shows the feasibility of using classification tools like LASSO regression for creating decision support tools. The use of LASSO regression can also assist with variable selection. This ensures that only the most relevant variables for prediction are assessed, reducing the time burden for clinical evaluation.
Signficance: The development of more robust models using larger datasets has the potential to bring much needed objective quantitative data to the complex, but critical decision of RTD following major lower limb injury. This approach can also be leveraged to inform other multifactorial questions in the O&P domain including return to high function for those in the civilian healthcare system.
Disclaimer: The views expressed herein are those of the author(s) and do not reflect the official policy or position of Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., Brooke Army Medical Center, the Department of Defense, or any agencies under the U.S. Government.
Acknowledgments: The original data collection was supported by the Center for Rehabilitation Sciences Research awards HU00012120074 and HU00012220038. The current project is supported by CDMRP OPORP award W81XWH2120021.
References
1. Belmont PJ, et al. J Surg Orthop Adv; 19(1), 2-7, 2010.
2. Mazzone B, et al. J Orthop Sports Phys Ther; 49(7), 529-535, 2019.
3. Rabago CA, et al. PLoS one: 14(12), 2019.
4. Sheehan RC, et al. Mil Med; 186(7-8), e777-e783, 2021.
5. Sheehan RC, et al. Mil Med; 2022.
Game-based myocontrol practice for improving pattern recognition performance
Zachary A. Wright, PhD, Andru Liu, MS, Mathew L. Elwin, PhD, Blair Lock, MsE.
Coapt, LLC, Chicago, IL, USA, www.coaptengineering.com
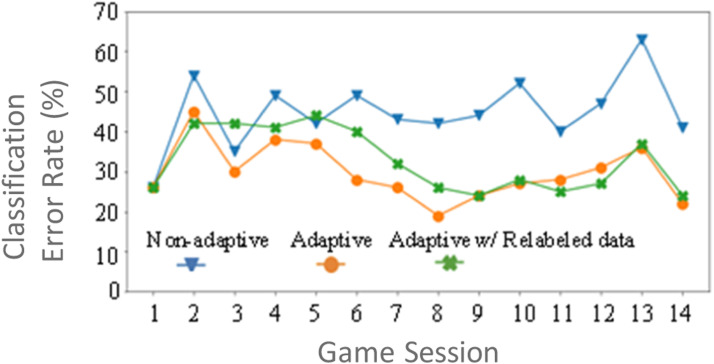
Introduction: Advanced pattern recognition algorithms for upper-limb myoelectric prosthesis control can adapt to variation in users’ muscle activity patterns [1]. Users often try to make consistent and repeatable muscle contractions when they train (i.e., calibrate) their control system. While this can help maximize classification accuracy under ideal conditions, several factors (muscle fatigue, limb position, force modulation, etc.) can change control performance under realistic conditions [2]. To encourage EMG input variation, users may benefit from training that simulates real-world prosthesis use. Here, we investigate using virtual games to adapt users’ pattern recognition controller based on their muscle activity patterns while they practice their prosthesis control.
Methods: Ten individuals with upper-limb difference (7 transradial and 3 transhumeral) who are existing myoelectric pattern recognition prosthesis wearers (mean Age ± std = 43.2 ± 10.3 yrs.; mean Prosthesis Use ± std = 38.8 ± 29.7 mos.) played a virtual game called In-The-Zone (Figure 1). The number of game sessions completed across two weeks varied among study participants. Data recorded in each game session was randomly split in half to generate training and test datasets consisting of the mean absolute value (MAVs) calculated on 8 EMG channels and the target (i.e., prompted) motion which represent the input feature set and the labeled motion classes, respectfully, for constructing an LDA classifier.
Figure 1.
In-the-Zone - Users modulate their muscle contraction intensity for a specified target motion (e.g., Hand Open) to proportionally control the size of a black ring. The objective of the game is to move and hold the black ring inside a yellow ring which represents a target intensity level.
We compared the performance of a Non-adaptive and an Adaptive LDA model in classifying user intention (assumed to be the target motion) in the test datasets across game sessions. An initial LDA classifier was built using the training dataset from each participant’s first game session. For the Non- adaptive model, the initial classifier was used to predict user intention in the test datasets in each subsequent game session. For the Adaptive model [3], the initial classifier was first adapted using the LDA classifiers built from the training datasets from each subsequent game session and then evaluated on the test datasets.
Results: Figure 2 shows the classification error rates of model predictions on the test datasets (50% of the game data) from each subsequent game session for one representative participant. Across game sessions, the error rate of the Non- adaptive model increased while the error rate of the Adaptive model decreased. These trends in model performance were consistent across seven participants. To summarize the
Figure 2.
Offline model performance for one representative participant showing the Adaptive LDA model outperforming the Non-adaptive LDA model across game sessions.
Differences in model performance across participants, we compared the change in classification error rates, defined as the difference in error rates between the last and first game sessions, between models. We found that the change in error rates for the Adaptive model (mean ± std, 6.5% ± 11.3%) were less than the Non-adaptive model (11.2% ± 13.4%); however, this result is not considered significant (p = 0.43).
Discussion: We implemented an adaptive algorithm that updates a pattern recognition classifier based on user control inputs while playing a virtual game. This adaptive algorithm attempts to learn the user’s muscle activity patterns corresponding to prosthesis motions across days of practice. Our results suggest that adjusting an LDA model to new inputs during gameplay can improve motion classification over time. We expect that implementation of the adaptive model online, i.e., updating users’ control system after each game then having them play again, would result in better performance than the offline analysis performed here. Nonetheless, our results are promising and point towards the need to further investigate the potential clinical benefits of our methods.
Significance: Virtual game training has shown to be an effective rehabilitation tool for practicing myoelectric prosthesis control. Here, we showed that virtual games can also be applied to learn the user’s control preferences under simulated use conditions. Virtual games can complement self-initiated calibration to encourage variability in muscle patterns for individual motions. The In-the-Zone game trains just one aspect of myoelectric prosthesis control – proportional control. However, other virtual games, such as posture-matching, motion sequencing or ones that are more interactive and involve residual limb movement or more functional tasks in virtual environments can also be applied.
Disclosure: Lock is co-founder and CEO and Wright is Research Principal Investigator at Coapt, LLC.
References
1. Cummins F, et al. Proc. of MyoElectric Cont Symp; 2017.
2. Kyranou I, et al. Front Neurorobot; pp. 12:58, 2018.
3. Vidovic MMC, et al. IEEE Trans on Neur Sys and Rehab Eng; pp. 961-970, 2016.
Ground clearance and compensatory strategies – influencing factors for lower limb prosthetics
Thomas Maximilian Köhler, MSc, CPO1, Malte Bellmann, PhD, CPO1
1 Ottobock SE & Co. KGaA, Clinical Research and Services, Research Biomechanics, Germany thomasmaximilian.koehler@ottobock.de
Introduction: Tripping is a safety risk for lower limb amputees and it is mainly affected by ground clearance during prosthetic side swing phase. To compensate for a lack of ground clearance, compensatory movements are necessary. However, such reduce walking efficiency. Thus, a prosthesis that provides a technical solution for ensuring adequate ground clearance during swing phase on the prosthetic side is desirable1-3.
The aim of this study was to investigate influencing factors of different prosthetic components and alignments on the resulting ground clearance and possible compensatory strategies for transfemoral amputees.
Methods: The following influencing factors were investigated: different principles of prosthetic knee joints (monocentric and polycentric) and feet (conventional energy storage and return, hydraulic ankle), swing phase control, ap-position of the prosthetic knee joint and foot, length of the prosthesis. Eight unilateral transfemoral amputees participated in this study.
Kinematic and kinetic parameters were recorded in a gait laboratory with a 12-camera optoelectronic system (Vicon, GB) and two piezoelectric force plates (Kistler, CH) embedded in a 12-m walkway. The measurements were performed during level ground walking with self- selected slow, mid, and fast velocity.
Results: Multiple systematic effects were observed. With increasing maximum knee flexion angle in swing phase minimum ground clearance (MGC) was increased (Figure 1). A more anterior shifted knee joint and more posterior shifted foot resulted in increased MGC. Main compensatory strategy for inadequate ground clearance was plantar flexion on the contralateral side during prosthetic side swing phase (vaulting).
Figure 1.
Ground clearance when walking with different maximum swing phase knee flexion angle (prosthetic side, mid velocity).
Conclusion: The results showed that the prosthetic alignment as well as the swing phase control of the prosthetic knee joint have a strong impact on the resulting ground clearance and compensatory strategies.
Significance: A more anterior aligned prosthetic knee joint and a more posterior aligned foot can enhance ground clearance. Furthermore, a swing phase control that enables adequate knee flexion independent from the walking velocity is crucial for ensuring ground clearance.
Disclosure: Mr. Thomas Maximilian Köhler and Dr. Malte Bellmann are employees of Ottobock SE & Co. KGaA
References
1. Sensinger JW, et al. IEEE Trans Neural Syst Rehabil Eng 21(1):74–80, 2013
2. Lechler K. Can Prostheht Orthot J 2(1), 2018
3. Köhler TM, et al. Can Prosthet Orthot J 3(1), 2020
Hand surgeon understanding of partial hand prostheses: Results of a national survey study
Emily M. Graham1, Christopher M. Baschuk2, Diane J. Atkins3, Lana Hutchinson4, Christopher C. Duncan5, Shaun D. Mendenhall1,6
(1) The Children’s Hospital of Philadelphia, Division of Plastic and Reconstructive Surgery, Philadelphia, PA, USA, (2) Handspring Clinical Services, Salt Lake City, UT, USA, (3) Department of Physical Medicine and Rehabilitation, Baylor College of Medicine, Houston, TX, USA, (4) Department of Occupational Hand Therapy, University of Utah, Salt Lake City, UT, USA, (5) Department of Physical Medicine and Rehabilitation, University of Utah School of Medicine, Salt Lake City, UT, USA, (6) Division of Plastic Surgery, University of Utah School of Medicine, Salt Lake City, UT. chris@pointdesignsllc.com
Introduction: Partial hand amputations are devastating injuries that often negatively impact individuals and communities. Partial hand prostheses can mitigate the burdens of living with an amputation, especially when reconstruction alone cannot restore form or function1. However, hand surgeons may be unfamiliar with these newer devices since the prosthetic field is rapidly progressing and many surgeons work independently without the support of a multidisciplinary team. Assessing surgeon awareness of the modern partial hand prosthetic devices and measuring the degree of collaboration within a multidisciplinary team may help improve amputee care and advocacy.
Methods: A nationally distributed electronic survey was distributed within the United States of America to hand surgeon members of the American Association of Hand Surgery with the intent of assessing surgeon familiarity with partial hand prosthetic devices and their clinical applications. Secondary aims explored degree of collaboration with prosthetists, therapists, and physical medicine and rehabilitation physicians. Survey items utilized Likert 5-point scales, rank order, multiple choice, and yes/no question formats. Responses were compared by training background (orthopaedic or plastic surgery) and by years of experience (10 years in practice) using independent t- tests. Demographic and clinical decision making questions were reported as proportions and/or were reassigned into a binary format for Fisher’s exact analyses.
Figure 1.
Distribution of hand surgeon participation in multidisciplinary teams.
Results: Overall, hand surgeons are unfamiliar with modern partial hand prosthetic devices. Regardless of the level of amputation, activity-specific prostheses were popular answer choices. Body-powered and passive functional devices were under- utilized responses for digital and transdigital amputations. Myoelectric devices were frequently listed as options for digital and transdigital amputations. Plastic trained hand surgeons were more likely to list toe-to-hand transfers as treatment options for multilevel digital amputations (p=0.03) and transmetacarpal amputations (p=0.02). Senior hand surgeons were more likely to suggest no treatment for partial thumb amputations (p=0.02). Hand surgeons identified cost and difficulty with insurances as significant barriers to prosthesis utilization. Perceived barriers were not influenced by years of experience (p=0.95 and p=0.83, respectively) or training background (p=0.96 and p=0.59, respectively). The majority of the cohort denied working within a multidisciplinary hand team (76.2%) or consulting with a prosthetist prior to revisional surgeries (71.4%). Plastic trained hand surgeons were more likely to highly rank the importance of having a prosthetist present during amputee rehabilitation than orthopaedic trained hand surgeons (p=0.02).
Discussion: This survey demonstrates that hand surgeons are not familiar with modern partial hand prostheses. This may reflect a need for educational initiatives on a national level. Most hand surgeons also do not work within multidisciplinary teams or understand the roles of other hand team members. Encouraging participation in such teams may mitigate these findings and improve amputee care.
Conclusion: Traumatic partial hand amputations are devastating injuries that frequently impair independence and identity. Through recent engineering advancements, partial hand prosthetic devices are increasingly available and functional, and have the potential to mitigate many of the challenges faced by those living with an amputation. However, this study shows that hand surgeons are not familiar with these newer prostheses. Expanding surgeon knowledge and encouraging multidisciplinary collaboration may enhance amputee care.
Significance: Understanding the knowledge gap that exists outside of the prosthetics profession relative to partial hand prosthetic rehabilitation should encourage prosthetists to reach out to their local referral sources to provide additional clinical education. Prosthetists can utilize the findings of this research to coordinate the organization of multidisciplinary prosthetic rehabilitation teams.
References
1. Graham, E. el al. Hand Clinics. 37(1), 167-187, 2021.
Importance of passive dorsiflexion range of motion in the ankle: A case study where dynamic contracture treatment corrects alignment in the AFO to limit knee hyperextension.
Flora Versyck, CPO, PT
Educator & Clinical Specialist, Basko Healthcare, f.versyck@basko.com
Introduction of purpose: Soleus contractures in patients with hemiplegia can have a significantly negative impact upon the passive range of motion (PROM) of the ankle towards dorsiflexion (DF). This limited ROM results in focal plantarflexion (PF) contracture due to soleus’ monoarticular role. A contracture is the inability of a joint to complete its full ROM and results in resistance to passive mobilization but can be treated using effective Low Load Prolonged Stretch (LLPS), increasing muscle elongation by remodelling the sarcomere number. During gait, a plantarflexion contracture can lead to knee hyperextension. Limited ankle DF can also result in issues with postural control, because ankle dorsiflexion PROM can influence dynamic balance and anterior lean of the torso. By addressing the soleus contracture, knee hyperextension can then be reduced with a tuned ventral shell Ankle Foot Orthosis (AFO) provided that there is sufficient DF PROM and a minimum Quadriceps strength of MRC 4/5. This case study presents the case of a 51 year-old female with sequelae, thirty-years post CVA with a profound dorsiflexor deficit and 10° PF contracture. Over a two-year period, the patient experienced knee hyperextension following years of active ambulation, walking with high heels to compensate a DF deficit but with knee hyperextension of 18 degrees measured during stance.
Methods: Manual Measurements of PROM with the knee in 90° and 0° were taken with the goniometer. To treat the soleus contracture, a custom made resting AFO with a dynamic contracture MultiMotion ankle joint was used, following a LLPS-protocol of 5 to 7 hrs a day, combined with exercises and follow-up by the physical therapist. To assess the impact of the PF contracture on postural control, photographs were taken before and after dynamic contracture management. Photographs were also taken after contracture management in a tuned, Triple Action AFO to assess the impact of the AFO on the knee hyperextension. The patient’s gait was video recorded also to evaluate the effect of the aligned and ROM adjusted anterior shell AFO.
Results: Dynamic contracture management resulted in an increased PROM of 15° towards DF and permitted the Triple Action AFO alignment to be inclined 5° towards dorsiflexion to incline the Shank to Vertical Angle (SVA). The final static alignment of the AFO combined with a 1 cm heel height of the shoe 9° of inclination. With this combined therapy and tuning of the AFO, a reduction of 27° was realized in knee hypertension towards knee flexion and a dynamic correction of knee kinematics was realized during gait to neutral. This overall outcome increased the patient’s walking speed by as much as 25.5 percent and significant increase of the step length.
Conclusion: These results demonstrate the importance of biomechanical principles that must be considered when fitting an AFO. Dynamic contracture treatment following the LLPS protocol has proven its long-term effectiveness, and demonstrated that adequate PROM of the ankle is necessary to correctly align an AFO. Without addressing the PF contracture the effectiveness of the AFO in reducing knee hypertension is attenuated.
It can be argued that increasing PROM towards dorsiflexion can help to correct genu recurvatum, given adequate quadriceps strength and a well- tuned Triple Action ankle-foot orthosis.
Significance: This case example demonstrates the importance of comprehensive orthotic care including therapeutic treatment to prevent or treat contractures and obtain PROM at the ankle which is necessary to reduce knee hyperextension by facilitating shank inclination using an independently tuned AFO. Despite this outstanding solution, applying contracture treatment followed by an individually customized orthosis is an individual pathway to be followed for each new patient. Additional considerations include proximal stability (strength and coordination) , and more specifically control of the M. Gluteus Medius.
Disclosure: Flora Versyck works for Basko Healthcare, distributor of Becker’s Triple Action joint.
References
1. Kobayashi t, et al. Clin Biomech (bristol, avon). 2016 jun;35:81-5. Doi: 10.1016/j.clinbiomech.2016.04.011. Epub 2016 apr 23.
2. Kobayashi T, Orendurff MS, Hunt G, Gao F, lecursi N, Lincoln LS,. Clin Biomech (Bristol, Avon). 2018 Nov;59:47-55.
Improved DASH outcome measure in chronic stroke after myoelectric arm orthosis use at home: A retrospective study
Sarah R. Chang, PhD1, Nicole Hofland, MS, OTR/L2, Zhengyi Chen, PhD3, Harry Kovelman, MD2, George F. Wittenberg, MD, PhD4, Jonathan Naft, CPO5
1 Orthocare Innovations, LLC, WA, 2 Myomo, Inc., MA, 3 Case Western Reserve University, OH, 4 University of Pittsburgh, PA, 5 Geauga Rehabilitation Engineering, Inc., OH, USA schang@orthocareinnovations.com
Introduction: Persistent upper limb impairment after a stroke adversely affects an individual’s quality of life, and ability to carry out self-care tasks1. The MyoPro® custom-fabricated myoelectric orthosis is designed to restore function in the upper limb by providing rigid support to the weak arm and powered movement to assist the hand and elbow. Sensors in the MyoPro measure volitionally generated electromyography signals in the upper limb muscles to control active assistance in elbow flexion/extension and opening/closing of the fingers. In a previous study with the MyoPro and individuals with brachial plexus injury, the Disabilities of the Arm, Shoulder and Hand (DASH) outcome measure was administered to evaluate the functional change in the upper extremity and reported an improvement of 11-points in mean DASH score2. The purpose of this study was to retrospectively evaluate the outcomes and clinical benefits provided by the MyoPro orthosis in individuals 65 and older with upper limb impairment secondary to a stroke.
Methods: The DASH is a patient-reported questionnaire that assesses disability in the upper extremity using Likert scales about physical function, symptom severity, and social participation. We hypothesized that the change in score on the DASH questionnaire would be improved after using the MyoPro.
Individuals 65 years of age or older with upper extremity impairment due to stroke and who received a custom fabricated MyoPro prior to participation were eligible.
Participants had to have completed the DASH outcome measure prior to receiving the brace (pre-MyoPro) and at least six months after having the brace (post-MyoPro). The study did not govern participant training, specific MyoPro use, or clinical interventions. A Generalized Estimating Equation model was applied.
Results: Nineteen individuals with chronic stroke (at least 1.6 years since stroke onset with median of 3.8 years) participated in the study. After using the MyoPro, 17 of 19 participants reported a lower score indicating an improved DASH score. The mean DASH score decreased 18.07 points [95% confidence interval: (-25.41, -10.72) with p<0.0001]. Figure 1
Figure 1.
Scatter plot of change in the DASH score for each participant (indicated by number) with respect to years between stroke onset and receiving the MyoPro (dotted line = 0-point change in DASH score, dashed line = mean change in DASH score, dash-dot line = median in years between stroke onset and receiving the MyoPro).
Discussion and conclusion: The minimal clinically important difference (MCID) for the DASH has been reported as 10.83 points2. Thirteen participants (68.42%) reported at least a 10.83-point change in their DASH score after using the MyoPro.
Significance: The reported change in the DASH score is meaningful as it may suggest that the use of the MyoPro has potentially enabled these individuals with upper limb impairment to now be more independent in their activities of daily living
Disclosure: SRC and JN’s employers received compensation for the coordination and execution of this research. ZC received compensation for performing the statistical analyses. NH and HK were employees of Myomo, Inc. GW is on the Clinical Advisory Board of Myomo and Neuro-innovators, LLC.
Acknowledgements: The study was supported by Myomo, Inc.
References
1. Olesh EV, et al. PLoS ONE. 2014;9:e104487.
2. Pulos N, et al. Prosthet Orthot Int. 2021;45:521-525.
Improvement in fast walking speed and daily step counts: Interim results from the international C-Brace® registry
Russ Lundstrom, MS1, Tyler Klenow, Arri Morris, BS1, Barbara Pobatschnig, Msc2, Andreas Kannenberg, MD, PhD1
1 Ottobock, Austin, TX, USA, 2 Ottobock, Vienna, Austria, russ.lundstrom@ottobock.com
Introduction: The C-Brace is a microprocessor-controlled Stance and Swing Controlled Orthosis (MP-SSCO®) developed to overcome the limitations of KAFOs that do not offer damped knee flexion during weight-bearing or dynamic swing control and has recently been approved for coverage in Medicare beneficiaries. Previous studies have shown that C-Brace improves gait and increases walking speed and endurance1.
While walking speed is an indicator of ambulatory capacity, greater number of daily step counts have been significantly associated with lower all-cause mortality in the US population.2 While step count is known to vary in orthotic patient populations, walking speed previously explained a significant proportion of step count variance in individuals with SCI in the literature.3 However, longitudinal evaluation of either measure in C-Brace users has yet to be disseminated.
A prospective, multicenter registry was designed to gather real-world safety and effectiveness data from patients that have been fitted with a C-Brace. The purpose of this interim analysis of registry data was to determine the effect of
C-Brace utilization on walking speed and step activity after 12-months of wear. A secondary purpose was to determine to what level results correlate in improving or declining subjects.
Methods: 46 O&P clinics in the United States and Germany have participated in the registry to date. Assessments were done at baseline with the existing orthosis and at 6 and 12 months with the C-Brace. Outcome measures included the 10-meter Walk Test for Fast Walking Speed (FWS) and daily step counts collected over 2-week periods using the Fitbit Zip attached to the orthosis. Interim results for these outcomes assessed at 12 months are presented. Data from 6-months visits were carried forward to account for missing 12-month data.
Results: 26 subjects from 19 sites had both baseline and either 6-month or 12-month data available for this analysis. All but one subject from one site with post-stroke diagnosis were excluded, as they had no step count data, primarily a therapeutic effect, and were analyzed separately4. Subjects were 9 female/17 male, mean age of 49 yrs and mean weight of 181 (86-270) lbs. 7 subjects were bilateral users. Diagnoses included incomplete spinal cord injury (9), trauma (4), polio (3), iatrogenic (2), traumatic brain injury (1), stroke (1), lumbar degeneration (1), lupus (1), muscular dystrophy (1), multiple sclerosis (1), inclusion body myositis (1), and unknown (1). While step count data was collected at baseline in all subjects, only 12 subjects had step count data collected at follow up. The mean scores for the outcomes, FWS and step counts are summarized in Table 1. The numbers of subjects showing changes for each outcome measures are shown in Table 2. Changes of +1.0 m/s were considered clinically meaningful for FWS and +500 steps for average steps per day.
Table 1.
Mean ± SD at baseline and 6 or 12-months after C-Brace fitting.
| Outcome | Baseline | 6 or 12M | Change |
|---|---|---|---|
| FWS m/s (n=25) | 0.70 ± 0.36 | 0.98 ± 0.28 | +0.28 ± 0.33 |
| Steps per day (n=12) | 1530 ±1104 | 1996±1278 | +467±1354 |
Table 2.
Subjects showing clinically meaningful changes vs. baseline.
| Outcome | Improved | No Change | Declined |
|---|---|---|---|
| FWS | 18 (72%) | 5 | 2 |
| Steps per day | 5 (42%) | 5 | 2 |
FWS was not correlated with the average steps per day at baseline. However, changes in FWS were correlated with changes in steps per day (R=0.76, p=0.007). 10 of 12 subjects with step count data increased in at least one measure.
Conclusion: Interim results from this prospective registry revealed that the majority of subjects showed clinically meaningful average improvements in walking speed 6-12 months, but these improvements didn’t always translate into increased step counts. However, all subjects that increased in step counts also showed meaningful increases in walking speed.
Significance: Increases in walking speed after fitting with a C-Brace may also translate to increases in activity as measured by a pedometer, but not in all patients.
Disclosure: All authors are employees of Ottobock.
References
1. Deems-Dluhy et al. Arch PMR. 2020; 102(2):233-44.
2. Saint -Maurice et al. JAMA. 2020;323(12):1151-60.
3. Stevens et al. Top SCI Rehabil. 2013;19(1):47-53.
4. Chang 2020. Poster presentation at 46th Academy Annual Meeting
Improving prosthetic hand control with high amplitude EMG from RPNIs and implanted electrodes
Alex K. Vaskov1, Christina Lee1, Dylan M. Wallace1, Alicia J. Davis1, Deanna H. Gates1, Paul S. Cederna1, and Cynthia A. Chestek1
1 University of Michigan, Ann Arbor, MI, USA
Introduction: Advanced prosthetic limbs have the potential to increase functionality for patients with upper limb amputations. However, this potential is often unrealized due to an inability to record strong and reliable control signals for multiple hand and wrist functions. Regenerative Peripheral Nerve Interface (RPNI) surgery is commonly performed to treat residual limb pain1, and also amplifies efferent motor action potentials to produce control signals in lieu of missing muscles2. This study examines the signal quality of implanted EMG electrodes in RPNIs and residual muscles in four patients and its implications for accurate and stable prosthetic hand control.
Methods: Surgical procedures: An RPNI consists of a free muscle graft reinnervated by a transected peripheral nerve1,2. Three participants with transradial amputations (P1, P2, P3) had intramuscular bipolar electrodes surgically implanted into previously created RPNIs on their median nerve, ulnar nerve, and residual innervated muscles. A fourth participant with a transradial amputation (P4) had RPNIs created on his median, ulnar, and radial nerves and electrodes implanted in the same operation. The percutaneous electrodes were connected to a neural signal processor (Blackrock Neurotech, Salt Lake City, UT) and real-time computer.
SNR Measurements: A virtual hand cued participants to make individual finger and wrist movements with their phantom hand. Signal-to-Noise Ratios (SNRs) were calculated by dividing the root mean square (RMS) of EMG during the strongest movement by the rest RMS. P1 completed 9 SNR sessions over 276 days, P2 has completed 37 sessions over 1541 days, P3 completed 11 sessions over 338 days, and P4 has completed 7 sessions over 195 days. P2 and P4 each completed one SNR session with surface EMG simultaneously recorded using adhesive electrodes with conductive gel.
Prosthetic Control: Movement classifiers were calibrated with the same approach: participants mimicked cued movements with their phantom hand. The procedure took less than 5 minutes and calibrations were stable across multiple sessions. All four participants controlled multiple hand and wrist functions of a virtual hand and commercial prostheses (LUKE arm or i-Limb with Ottobock wrist).
Results: No serious adverse events have occurred related to the study intervention. Across all four participants, the implanted RPNIs produced large amplitude EMG with a median SNR of 33.3dB (46.4 gain, n = 13). Figure 1(a) shows this was comparable to, but less than, the SNR from electrodes implanted in residual innervated muscles, median 40.8dB (109.6 gain, n = 25).
Figure 1.
a) Boxplots of the signal to noise ratio from implanted residual innervated muscles, implanted RPNIs, and gelled adhesive surface electrodes (* p < 0.05, ** p <0.01, Wilcoxon rank sum). b) P2 three grasp accuracy with no recalibration in four arm positions across 16 sessions.
Implanted electrodes recorded significantly stronger signals than P2 and P4’s surface EMG, which had a median SNR of 20.7dB (10.9 gain, n = 16 channels).
Animal studies have shown a RPNI reinnervation period of about three months3. P4’s RPNIs had an average SNR of 24.1dB (16.1 gain) 103 days after RPNI creation and electrode implantation. On day 188, P4’s average RPNI SNR increased to 35.2dB (57.5 gain) and has remained stable since, with an average of 35.3dB (57.9 gain) on day 298.
P2 completed a structured no recalibration assessment in which she donned her prostheses and completed a grasp matching task with a four movement classifier (fist, pinch, point, rest) in four different arm positions. Figure 1(b) shows that her performance remained stable with an average daily accuracy above 94% across 604 days without recalibration.
Conclusion: RPNIs and implanted EMG electrodes produce strong and reliable signals for prosthetic control. RPNI surgery and electrode implantation can be performed separately or at the same time. The next steps of this research are to miniaturize electronics for take home studies and commercialization.
Significance: The use of implanted electrodes provides accurate multi- function control of prosthetic devices and also reduces socket complexity by eliminating the absolute requirement for electrode to skin contact within the prosthetic socket.
Consistent and reliable control may greatly reduce the initial device learning curve, speeding up adoption and increasing the effectiveness of occupational therapy. In summary, this technology can affect multiple factors to accelerate and improve healthcare for patients with upper limb amputations.
Acknowledgments: This work was funded by DARPA 66001-16-4006 and NIH R01NS105132. Ossur provided prosthetic hands for the study.
References
1. Kubiak, et al. Plast Reconstr Surg 144, 3, 2019
2. Vu, et al. Sci Transl Med 12, 533, 2020
3. Vu, et al. IEEE TSNRE, 26, 2, 2018
Individuals with osseointegrated prostheses use an intact limb reliance strategy during locomotion
Jenna Burnett, MS1, Ross H. Miller, PhD1, and Jae Kun Shim, PhD1
1 Dept. of Kinesiology, University of Maryland, College Park, USA, jburnet@umd.edu
Introduction: Individuals with lower extremity amputation commonly struggle to meet the recommended physical activity, resulting in chronic health problems, with these problems further exacerbated by socket-related complaints2 which make it difficult for them to wear their prosthesis for long periods of time. These individuals also tend to rely on their intact limb for propulsive work during locomotion1, resulting in large interlimb asymmetries. Osseointegrated (OI) prostheses remove the socket entirely, and appear to improve functional and clinical performance3, but whether the rigid connection provided by an OI prosthesis influences the intact limb reliance is unknown. To understand how an OI prosthesis influences the intact limb reliance, the interlimb ground reaction force (GRF) asymmetry during walking at three speeds was investigated. We hypothesized that the interlimb GRF asymmetry would increase at the faster walking speed, but would be similar at the slower and preferred speeds, as the prosthesis is unable to provide the additional propulsive work required at faster walking, resulting in an intact limb reliance strategy.
Methods: Eight individuals (5 men, 52.2 years old, 85.88 kg, 1.79 m, and 3 women, 46.3 years old, 60.37 kg, 1.67 m) with transfemoral amputation who use an OI prosthesis were recruited. After the consent process, individuals were asked to walk at three speeds (slow, preferred, and fast), with each speed subjectively chosen by the individual. GRF data was collected at 1000 Hz using eight 6DoF piezoelectric force platforms (Kistler, Switzerland) arranged in a single row located within a raised platform. The GRF during stance for each limb was extracted using Visual3D (C-Motion, Germantown, MD, USA) and the interlimb asymmetry was calculated for each percentile of stance4. Three stance phases from each participant at each walking speed were analyzed using Statistical Parametric Mapping with a 1-way ANOVA of walking speed (critical p value = 0.05), followed by two-sample t-tests for statistically different main effects (critical p value = 0.02).
Results: For all walking speeds, the interlimb GRF asymmetry (Figure 1) was over the 5% threshold for the entire stance phase, indicating that the GRF magnitude is asymmetric. The largest asymmetries occurred during the initial braking period with an asymmetry of between 45 and 60%, and during the propulsive period with an asymmetry between 20 and 40%. However, the only period with statistically different interlimb GRF asymmetry (p<0.05, crosshatched region) across walking speeds occurred between 77 and 86% of stance. Post-hoc testing indicated that the asymmetry was significantly greater in the faster walking condition when compared to both the preferred ( p<0.02) and slower (p<0.02) walking speeds, but there were no differences in the preferred and slower speed asymmetries.
Figure 1.
Average interlimb GRF asymmetry and standard deviation during stance for three walking speeds (Fast, Preferred, Slow). The gray dotted line represents the asymmetry threshold such that a value greater than 5% is considered asymmetric. Statistical differences were found in the cross-hatched region.
Discussion and conclusion: Our hypothesis of statistically greater interlimb GRF asymmetry during walking at faster speeds, but not during slower or preferred speeds was supported. While the interlimb asymmetry indicates that there exists some intact limb reliance at all walking speeds, the interlimb GRF asymmetry was statistically greater during faster walking due to an offloading of the GRF to the intact limb. This offloading may be due to the prosthesis and amputated limb being unable to generate the required work, resulting in compensations by the intact limb and larger differences in interlimb GRF.
Significance: Despite the evidence for improved performance with the rigid OI prosthesis, individuals with lower limb amputation may still use an intact limb reliance strategy when walking at all speeds. This intact limb reliance may be further exacerbated by faster speeds, as the maximum capacity of the prosthesis may be exceeded by the locomotion requirements, requiring compensations by the intact limb.
Acknowledgments: This work was supported by the CDMRP under the DoD OPORP mechanism.
References
1. Pinhey SR, et al. J Biomech. 2022;134.
2. Sherman RA. J Rehabil Res Dev. 1999;36(2).
3. Van De Meent H, et al. Arch Phys Med Rehabil. 2013;94(11):2174-2178.
4. Winiarski S, et al. Gait Posture. 2021;90:9-15.
Integrating outcome measure data collection with the National Limb Loss and Preservation Registry
Sarah R. Chang, PhD, Jung Kim, David A. Boone, BSPO, MPH, PhD
Orthocare Innovations, LLC, WA, USA schang@orthocareinnovations.com
Introduction: The Clinical Outcome Measures Electronic Toolkit (COMET) mobile application (app) assists clinicians in easily selecting outcome measures to collect with their patients and efficiently administers, scores, and exports the data into a report that clinicians can include in the patient medical record and use to support clinical decisions1,2. The P&O COMET mobile app includes several relevant outcome measures such as the Prosthetic Mobility Questionnaire, Socket Comfort Score, and Numeric Pain Rating Scale. Additional efforts have been made to advance clinical care through the creation of the Limb Loss and Preservation Registry (Registry) that serves as a general database to track and analyze patient outcomes data such as age, gender, type of limb loss or preservation surgery, and prosthetic device3. To increase the database of evidence, the Registry needs additional pathways to gather data on patient outcomes. The purpose of this project was to extend the P&O COMET mobile app to facilitate outcome measure data collection with the National Limb Loss and Preservation Registry.
Methods: To share outcome measure data with the Registry, a data dictionary was needed to define the data structure and acceptable data fields. Once the data types were established, the P&O COMET mobile app underwent updates to provide the necessary security and user interface to enable export of the data files compatible with the Registry. Testing was performed to ensure data fields were in the correct format and the files could be accepted by the Registry after upload.
Results: An outcome measure entity was created within the Registry to enable sharing of the outcome measure results gathered from the P&O COMET mobile app. The data dictionary defined the naming conventions for each data type, accepted data type, data length, data format, and data validation. Based on the data dictionary, the compatible data file (JSON) was established.
The P&O COMET mobile app retained its core functionality of providing outcome measures in a digital format, automatically calculating the score, and generating a PDF report for inclusion in the patient medical record. To integrate with the Registry, the app has new features to allow patient data to be saved securely in an encrypted database and to automatically generate the Registry-compatible data files. Figure 1
Figure 1.
Diagram of P&O COMET mobile app relationship with patients, clinicians, and the Registry.
Discussion and conclusion: Clinics can continue to collect outcome measures with the P&O COMET mobile app and now have the ability to export the data to share with the Registry. Sharing outcome measure results with the Registry provides the opportunity to gather longitudinal patient outcomes data that can support evidence- based clinical practice.
Significance: The P&O COMET mobile app provides an additional pathway to gather and share patient outcomes data with the Limb Loss and Preservation Registry to advance our care for patients with limb loss and limb difference.
Disclosure: The authors are employees of Orthocare Innovations, LLC.
Acknowledgements: The work was supported by an AOPA Research Award administered by the Center for Orthotic and Prosthetic Learning. We thank the Registry team for their support.
References
1. P&O Comet [Mobile app]. Version 1.1.0. Apple App Store: Orthocare Innovations, LLC; 2021. https://apps.apple.com/us/app/p-o-comet/id1583880880.
2. P&O Comet [Mobile app]. Version 1.1.0. Google Play Store. Orthocare Innovations, LLC; 2021. https://play.google.com/store/apps/details?id=com.orthoc areinnnovations.oi_flutter_comet.
3. Limb Loss and Preservation Registry.<https://www.llpregistry.org/> Accessed March 31, 2022.
Limb health and socket pressure in response to powered ankle prostheses
Jeffrey Denune1, CPO, Surya Gnyawali1, PhD, Myia Dickens2, Sri Nikhitha Kondreddi1, Bryce Hockman1, Whitney Pratt1, MD, Patrick Wensing2, PhD, James P. Schmiedeler2, PhD, and Sashwati Roy1, PhD
1 Indiana University School of Medicine, Indianapolis, IN 46202, 2 Aerospace and Mechanical Engineering, University of Notre Dame, Notre Dame, IN 46556
Introduction: Technological advancements in active prosthetic devices for individuals with transtibial amputation offer the potential for superior function in key areas that could lead to improved quality of life. Providing controlled plantar/dorsiflexion in either swing (microprocessor-controlled prostheses) or late stance (prostheses with powered propulsion) is likely to become the gold standard in the future as technology continues to improve. Despite the future with the active prosthetics, relatively little is known about the impact of active transtibial prostheses on socket pressure, and no studies have examined their effects on direct measures of limb health. Prosthetic fit is the primary concern of most individuals with lower-limb amputation since persistent discomfort can necessitate prosthesis disuse or abandonment. Therefore, how active prostheses affect fit is a critical knowledge gap as these devices become more prevalent.
Objective. The main objective of this research is to perform a clinical study to understand and quantify the effects of powered transtibial prostheses on socket loading and direct measures of residual limb health. The following two aims are addressed in the clinical study: Specific Aim 1: Determine the effects of a powered transtibial prosthesis on the socket pressure for level-ground walking, stair ascent/descent, and ramp ascent/descent in comparison to a microprocessor-controlled prosthesis and a passive prosthesis. Specific Aim 2: Determine the relative impact on residual limb health of the use of a powered prosthesis, a microprocessor-controlled prosthesis, and a passive prosthesis for individuals with transtibial amputation
Methods: Clinical study design: Subjects with unilateral transtibial amputations were recruited from the Indiana University Health (IUH) clinics. Subjects must be non-smokers, ages 18-65, weighing less than 280 lbs, ability to ambulate at a K3 level or higher without an assistive device and the subjects should be at least 3 months post-amputation. The study is a randomized open label prospective study. devices: Device A. Empower ankle by Otto Bock, is a powered prosthesis that provides active propulsion in late stance to mimic the positive work performed by the ankle plantar flexors in push-off. Device B. PROPRIO FOOT® by Ossur, is a microprocessor-controlled prosthesis that regulates the angle of ankle dorsiflexion during the swing

PROPRIO FOOT® Ossur Empower ankle Otto Bock
phase. The clinical study includes three study visits 4 weeks apart where following consent, the baseline line data is collected with the standard of care SoC device at visit one, at this visit based on randomization the subjects will be fitted either with device A or B. Next two visits occur 4 weeks apart with data collection on use with the devices A or B. For outcomes, In-socket pressure data, gait and functional data using motion sensors, patient reported outcomes as well as limb health data is collected.
Results & conclusions: To date this study is ongoing and scheduled completion of all fifteen transtibial subjects by August 2023. Data analysis is underway and will be presented at the time of the National meeting of AOPA 2023. The primary outcomes will be first time presented at the meeting. The work will provide evidence-based data to determine if the use of powered prostheses affects residual limb health, both on short time scales typical of single-day locomotion activities and on a four-week time scale of regular use. Additionally, the study will determine how socket pressures during locomotion activities may be correlated with residual limb health when using active prostheses. In both regards, this study will be the first to quantify these important aspects that play a direct role in device fit and long-term adoption.
Acknowledgements: Funded by DoD W81XWH2110459
Measuring the metabolic energy consumption in prosthetics and orthotics: Which is an appropriate study design?
Malte Bellmann1,2, Thomas Schmalz1
1 Clinical Research and Services, Ottobock SE & Co. KGaA, Göttingen, 2 PFH Private University of Applied Sciences, Göttingen malte.bellmann@ottobock.com
Introduction: The metabolic energy consumption (MEC) of locomotion is increased when walking with prostheses and orthoses. This is mainly caused by restricted muscle group functions and compensational movements. As an example, the MEC of lower limb amputees is increased significantly the higher the amputation level is. The aim of an orthopedic intervention is restoring the impaired body function best possible in order to achieve a more natural gait including metabolically efficiency. Next to established biomechanical and clinical methods, measuring the MEC seems to be an adequate addition to evaluate the effect of prosthetic and orthotic interventions. Nevertheless, the correct methodological approach is crucial regarding the validity and relevance of the results.
Methods: An analysis of the existing literature investigating prostheses and orthoses by measuring the MEC was conducted. The aim was to identify appropriate reference numbers of repeated measurements that can be conducted by protheses and orthoses users. Additionally, a case study with a repetitive design was performed. This study design included one transtibial amputee (TTA) and one transfemoral amputee (TFA). Ascending a 5° ramp with an active foot optimally adjusted with (ON) and without (OFF) active push-off was analyzed. Each examination incorporated a spiroergometry measurement on a treadmill (0° and 5° inclination) using the Cortex MetaMax 3B. Four measurement sessions with three examinations each were completed with both subjects within 2 weeks. The order of the foot setting (ON or OFF) was randomized for the respective examinations within one session. There were 6 possible orders of foot settings: ON/OFF/ON, OFF/ON/OFF, ON/ON/OFF, OFF/OFF/ON, OFF/ON/ON, ON/OFF/ OFF. Four of these combinations have been selected randomly for each subject.
Results: Former studies measuring the MEC while using prosthetic or orthotic interventions were not designed as repetitive and randomized investigations over a period of several days. Some studies eliminate possible adaptation effects as walking on a treadmill or wearing silicon masks of a portable measurement system by randomization [1,2]. But some study designs did not consider these effects influencing the validity of the data significantly [3,4].
For this case study, the uptake of oxygen (ml O2/min per kg bodyweight) was used as the measure for the MEC. For the TTA while walking on level ground, means between 12,1 and 11,7 mlO2/min/kg (foot ON) and 13,3 and 12,5 mlO2/min/kg (foot OFF) were measured. For the TFA, the results were between 12,4 and 10,6 mlO2/min/kg (foot ON) and 12,7 and 11,3 mlO2/min/kg (foot OFF), respectively. When walking on the 5° incline, the results for the TTA were between 15,5 and 15,3 mlO2/min/kg (foot ON) and 17,1 and 15,7 mlO2/min/kg (foot OFF). For the TFA, the results for this walking condition were between 14,9 and 14,0 mlO2/min/kg (foot ON) and 15,7 and 14,0 mlO2/min/kg (foot OFF), respectively.
For both subjects, a continuous stepwise reduction of the MEC could be found over the period of all four sessions. Thus, the individual adaptation to the measurement set-up led to a subsequent lower MEC after a series of repetition.
Conclusion: To eliminate side effects like individual adaptation to new and specific measurement situations, the study design of investigating technological impacts on the MEC of prosthetic and orthotic users is crucial. Thus, a test trial for a first adaptation to the test set-up before conducting the measurements is mandatory and repetitions of the specific measurement situations seem to be essential. But the number of repeated measures should not exceed the capabilities of the individual subject. The results of this study suggest a repetition within a few days in a randomized order.
Significance: The study design of measuring the metabolic energy consumption of prosthetic and orthotic users is crucial in terms of data validity. A repetitive, randomized cross-over design (A-B-B-A or B-A-A-B) is recommended.
Disclosure: M. Bellmann, T. Schmalz are employees of Ottobock SE & Co. KGaA, M. Bellmann is associated with PFH Göttingen as well.
References
1. T. Schmalz; 2002, Gait Posture
2. M. Bellmann; 2010, Arch Phys Med Rehab
3. H. Herr; 2012, Proc Biol Sci.
4. E.R. Esposito; 2016, Prosthet Orthot Int.
Moisture mitigation for overall health and mobility of the amputee
Surya C. Gnyawali, PhD1, Jeffery Denune, CP1, Jóna Valgerður Kristjánsdóttir, MSc2, Knut Lechler, CPO2, Chandan K. Sen, PhD1 and Sashwati Roy, PhD1
1 Department of Surgery, Indiana University School of Medicine, Indianapolis, USA, 2 Össur R&D, Reykjavik, Iceland
Purpose: Following amputation, preservation of residual limb health is critical for the overall health and mobility of the amputee. Sweat and heat build-up at the skin-liner interface remains a major challenge and impairs the quality-life of amputees. Prosthetic liners are primarily made of heat insulating materials that retain heat resulting in a sweating of the residual limb-liner interface thereby resulting in the liner- socket to slide off and affecting the quality suspension of the prosthetic leg. Inappropriate suspension may cause shear forces compromising residual limb health, skin breakdown, and potential injury. Therefore, we hypothesized that an adequate management of perforated liner and socket system will result in reduction of sweat at the skin-liner interface which will in turn help improve socket fit for individuals with trans-femoral amputation. The primary objective of this study is to evaluate the efficacy of the perforated ‘AeroFit Liner’, and Socket solution (Össur) compared to seal-in silicone liner and non- perforated direct socket suspension system through measured relative humidity on residual limb skin during increased perspiration conditions.
Methods: Following the guidelines of institutional review board of the Indiana University School of Medicine, nine adult individuals with unilateral transfemoral amputation were recruited to participate in this study. Participants were using seal-in silicone liner and direct socket as their routine standard of care (SoC), able to walk on a treadmill for 20 minutes, follow the protocol, and were able to response to questionnaires. We designed a 10- week study in which subjects were either randomized to investigational or SoC sockets. The humidity in the skin-liner interface was measured baseline and during the treadmill-walk in a heated (28 ± 2°C) and humidity (42% ± 2 %) controlled room using a TMSR147WD data logger and sensor system adhered on the limb skin. During questionnaire, the subject responded for socket fit comfort score & comprehensive lower limb amputee socket survey (CLASS). Figure 1
Figure 1.
Study timeline and design.
Results: Data from all nine subjects showed that the humidity measured from the investigational liner-socket system significantly reduced (n=9, *p <0.0007) compared to the SoC liner-socket system. Likewise, the data on relative humidity reduction as measured by the area under the humidity-time curve (mean ± SD, 30 ± 12.50%, n = 9, *p <0.0001) corroborated to the direct measurement of relative humidity form limbs. The data showed significant inter-subject variability (p = 0.0042). However, there was no significant difference in the period (p = 0.582), sequence (p = 0.290), and treatment effects for stability (p = 0.582), comfort (p = 0.626), and total CLASS scores (p = 0.4869).
Thus, we evaluated the hypothesis that the amount of sweat produced as rated by the perceived sweat score (a higher score indicates a lower amount of sweat) and found that perforated solution (mean score ± SD, 8.44 ± 2.01) was significantly better (p=0.028) than the non-perforated (mean score ± SD, 7.22 ± 2.82), hence the hypothesis was tested positive. Figure 2
Figure 2.
Representative relative humidity plots. Environmental humidity when donning AeroFit (blue line) and SoC (green line). Gray vertical lines show the time events during study: baseline, liner don, socket don, walk start, walk end and resting, four square step test (FSST), walking on stairs, and doff respectively from left to right.
Conclusion: In conclusion, perforated investigational device effectively mitigates the moisture build-up at the skin-liner interface compared to conventional suspension which is anticipated to provide an improved socket fit.
Significance: A significant reduction in relative humidity on the skin liner interface was observed. No change in the temperature was noted on the interface. Significant reduction in humidity on the skin was perceived by the users when compared to using a SoC system. No significant worsening in stability, suspension or comfort was perceived by users as compared to SoC system.
Disclosure: Authors have no potential conflicts of interest in the abstract.
Acknowledgments: This work was supported by Össur to SR.
References
1. Rink, C. Gnyawali SC, et al. Elevated vacuum suspension preserves residual-limb skin health in people with lower-limb amputation: Randomized clinical trial. J Rehabil Res Dev (2016).
2. Petrofsky, J. S. et al. The interrelationship between air temperature and humidity as applied locally to the skin: the resultant response on skin temperature and blood flow with age differences. Med Sci Monit. (2012).
3. Ghoseiri, K. & Safari, M. R. Prevalence of heat and perspiration discomfort inside prostheses: literature review. J Rehabil Res Dev (2014)
Myoelectric orthosis assists functional activities in individuals with upper limb impairment after 3-months of home use
Sarah R. Chang, PhD1, Nicole Hofland, MS, OTR/L2, Zhengyi Chen, PhD3, Curtis Tatsuoka, PhD4, Lorie G. Richards, PhD, OTR/L, FAHA, FAOTA5, Margaretta Bruestle, MS2, Harry Kovelman, MD2, Jonathan Naft, CPO6
1 Orthocare Innovations, LLC, WA, 2 Myomo, Inc., MA, 3 Case Western Reserve University, OH, 4 University of Pittsburgh, PA, 5 University of Utah, UT, 6 Geauga Rehabilitation Engineering, Inc., OH, USA schang@orthocareinnovations.com
Introduction: After a stroke, as many as 80% of individuals have full or partial paralysis on one side of the body1. Upper limb hemiparesis can severely limit the ability to use the affected side to complete activities of daily living (ADLs) and instrumental activities of daily living (IADLs). The MyoPro® custom-fabricated myoelectric orthosis is designed to restore function in the upper limb by providing rigid support to the weak arm and powered movement to assist the hand and elbow. Sensors in the MyoPro measure volitionally generated electromyography signals in the upper limb muscles to control active assistance in elbow flexion/extension and opening/closing of the fingers. Prior research has shown improved motor control and user-reported function and independence when using the MyoPro2. The purpose of this study was to observe the functional gains in completing standardized functional tasks in the home with and without the MyoPro in individuals with upper limb impairment due to stroke.
Methods: Individuals post-stroke participated in four data collection sessions remotely over videoconference after being fit with the MyoPro for the first time: 2-weeks after (2-Weeks), one month after (Month-1), two months after (Month-2), and three months after (Month-3). In each session, participants completed a standardized set of functional tasks with and without the MyoPro. Tasks included: moving object to mouth (“pickle”), holding object in space (“bag”), stabilizing object (“mixing bowl”), and moving object to a new location (“towel”). Participants’ total completion time and overall successful ability to complete the tasks were analyzed. The with and without MyoPro total time difference (w/wo- TtimeDiff) was calculated by subtracting the total completion time without the MyoPro from the total completion time with the MyoPro at each time point. Longitudinal mixed models on task completion time with LASSO selected covariates and longitudinal mixed logistic regression models on the success of task completion with LASSO selected covariates were analyzed. P-values were adjusted for multiple testing (three time points) using the Holm-Bonferroni correction.
Results: Clinically meaningful improvements were observed on the functional tasks in the participants’ homes. Statistically significant changes from 2-Weeks for the w/wo-TtimeDiff were observed by Month-2 for the “pickle” task (adjusted p=0.020), by Month-1 for the “bag” task (adjusted p=0.034), by Month-1 for the “bowl” task (adjusted p<0.001), and by Month-1 for the “towel” task (adjusted p=0.023). *adjusted p < 0.05; **adjusted p < 0.01. Figure 1
Figure 1.
Trajectory of mean change from Two Weeks of w/wo MyoPro device total time difference for the ‘pickle’ task over the time points. Results of longitudinal linear mixed effects model adjusted for the first time point (2-Weeks) w/wo total time difference value and other chosen covariates. *adjusted p < 0.05; **adjusted p < 0.01.
Discussion and conclusion: Participants required a shorter time to complete the functional tasks with the MyoPro as compared to without the MyoPro within the first three months.
Significance: Use of the MyoPro can increase activity participation and decrease disability when performing ADLs and IADLs in individuals after stroke.
Disclosure: SRC and JN’s employers received compensation for the coordination and execution of this research. LGR is a member of the Myomo Advisory Board. ZC and CT received compensation for performing the statistical analyses and preparation of this manuscript. NH, MB, and HK were employees of Myomo, Inc.
Acknowledgements: The study was supported by Myomo, Inc.
References
1. “Hemiparesis”. Accessed October 27, 2022. <https://www.stroke.org>.
2. McCabe JP, et al. PLoS ONE. 2019;14:e0215311.
Narrowing the performance gap for bilateral transfemorl prosthesis users with their unilateral peers using advanced microprocessor knee technology
Tyler Klenow, MBA, MSPO, CPO, FAAOP, Arri Morris, BSE, MS, Russ Lundstrom, BSE, MS
Ottobock Healthcare LP, Austin, TX, USA tyler.klenow@ottobock.com
Introduction: Individuals with transfemoral amputation (TFA) constitute a small portion of the population with amputation in the US.1 These patients often have poor rehabilitation outcomes due to an increased energy expenditure as high as 2.5x the rate of intact individuals and 2x unilateral TFA users.2 Bilateral TFAs are also at a higher risk of stumbles and falls than other users and are completely reliant on prosthetic technology to navigate ramps and stairs.
While a significant effort exists to bring technological advancements to patients with TFA in microprocessor knees (MPKs), specific technological advancements for bilateral users have not been developed. So, a ruleset change was developed specifically for bilateral users in the Genium X3 product line (Ottobock Se & Co., Duderstadt, Germany) The purpose of this study was to evaluate the efficacy of the new ruleset for bilateral users with TFA compared to their unilateral peers while not reducing the effectiveness of the product overall.
Methods: Current Genium or X3 users with at least 6 months of use were recruited from two sites in the US. The IRB- approved clinical trial was divided into two phases to allow for iterative change to the Genium X3 product based on direct feedback from users and prosthetists. Following enrollment subjects performed a baseline data collection including the L-Test, ABC, PLUS-M, and a study-specific feedback questionnaire. These measures were repeated in addition to the ADL-Q during a final data collection after eight weeks of home-use in the commercial version of the product update.
Results: The final product update included a new ruleset and upgraded hydraulic components. Twenty-six subjects were enrolled and n=25 completed the study including 16 unilateral, nine bilateral, and one TTA/TFA, subjects. The nine bilateral subjects were age-matched to nine unilateral subjects in an ad-hoc between-groups comparison reported here. Age-matched subjects with unilateral amputation demonstrated faster times on the
L-Test than the bilateral group (p=0.027) at final assessment. Unilateral subjects also demonstrated significantly fewer stumbles and falls in the eight weeks prior to the final assessment than the bilateral group (Table1).
Table 1.
Stumbles and falls at baseline and final assessment.
| Session | Bilateral | Unilateral age-matched mean diff. | p-value |
|---|---|---|---|
| Stumbles | |||
| Baseline | 25.85 ± 60.28 | −18.5 | 0.299 |
| Final | 3.9 ± 2.39 | −2.8 | 0.003 |
| Falls | |||
| Baseline | 1.89 ± 1.51 | −21.2 | 0.055 |
| Final | 1.72 ± 2.59 | −21.5 | 0.034 |
No other statistically significant differences were shown between groups. However, several clinically meaningful differences were shown including 36% greater comparative ease and 41% greater comparative safety in the bilateral group. The categories with largest perceived difference (>0.5) between groups included Family Role, Social and Leisure Activities, and Shopping. The item with the single largest difference between groups was walking down ramps in the Mobility category. The study also noted a markedly higher proportion of bilateral subjects using the stair ascent mode compared to unilateral subjects.
Conclusion: The product update improved outcomes in several categories for both groups of users, especially for bilateral users in perceived ease and safety. The overall effectiveness did not decrease during the study period.
Significance: Improvements to advanced MPK technology tailored to the needs of bilateral users can close the performance gap between bilateral and unilateral users as evidenced by the lack of significant differences in some standardized measures. Despite the improvement, significant differences still exist highlighting the disproportionate need bilateral subjects have for advanced technology. Advanced MPK use for active bilateral TFA users should be the standard of care.
Disclosure: Tyler Klenow, Arri Morris, and Russel Lundstrom are employees of Ottobock Healthcare LP.
References
1. Ziegler-Graham et al. Arch PMR. 2008;89(3):422-9.
2. Ladlow et al. PLoS One. 2019;14(1):e0209249.
Osseointegration outcomes following amputee lengthening
Jason Hoellworth1; Kevin Tetsworth1,2, Atiya Oomatia,1,3,4, Munjed Al Muderis1,2,3,4,5
1 Osseointegration Group of Australia, Australia, 2 Macquarie University Hospital, Sydney, Australi, 3 The University of Sydney, Australia, 4 Macquarie University, Australia, 5 Notre Dame University, Australia atiya@osseointegrationaustralia.com.au
Purpose: Percutaneous EndoProsthetic Osseointegration for Limbs (PEPOL) facilitates improved quality of life (QOL) and objective mobility for most amputees discontent with their traditional socket prosthesis (TSP) experience. Some amputees desiring PEPOL have residual bone much shorter than the currently marketed press-fit implant lengths of 14-16 cm, potentially a risk for failure to integrate. We report on the techniques used, complications experienced, the management of those complications, and the overall mobility outcomes of seven patients who had femur distraction osteogenesis (DO) with a Freedom nail followed by PEPOL.
Methods: Retrospective evaluation of a prospectively maintained database identified nine patients (5 females) who had transfemoral DO in preparation for PEPOL with two years of follow-up after PEPOL. Six patients had traumatic causes of amputation, one had perinatal complications, one was performed to manage necrotizing fasciitis and one was performed as a result of osteosarcoma.
Results: The average age at which DO commenced was 39.4±15.9 years, and seven patients had their amputation more than ten years prior (average 25.5±18.8 years). The residual femurs on average started at 102.2±39.7 mm and were lengthened 58.1±20.7 mm, 98±45% of goal (99±161% of the original bone length). Five patients (56%) had a complication requiring additional surgery: four events of inadequate regenerate were managed with continued lengthening to desired goal followed by autograft placement harvested from contralateral femur reaming; one patient had the cerclage wires break which required operative replacement.
All patients had osseointegration performed, at 355±123 days after the initial lengthening nail surgery. One patient had K-level >2 before DO, at a mean of 3.4±0.6 (2.6-4.4) years following osseointegration six patients had K-level >2. The 6 Minute Walk Test remained unchanged (267±56 vs 308 ± 117 meters). Patient self-rating of prosthesis function, problems, and amputee situation did not significantly change from before DO to after osseointegration. Six patients required additional surgery following osseointegration: six to remove fixation plates placed to maintain distraction osteogenesis length at osseointegration; two required irritation and debridement for infection.
Conclusion: Extremely short residual femurs which make TSP use troublesome can be lengthening with externally controlled telescoping nails, and successfully achieve osseointegration. However, it is imperative to counsel patients that additional surgery to address inadequate regenerate or to remove painful hardware used to maintain fixation may be necessary. This may improve the amputee’s expectations before beginning on a potentially arduous process.
Significance: This article is the first to directly address the outcomes, and management of osseointegration prosthesis following a limb lengthening procedure for individuals unable to use traditional socket prosthesis due to short stump.
Disclosure: Dr. Al Muderis consults for and receives royalties from companies including: Osseointegration International Pty Ltd (Australia), Osseo-PL Inc (USA), Osseo-PL GmbH (Germany), AQ Implants GmbH (Germany) and Permedica S.P.A (Italy).
Perceived hazard exposure and accommodation while pregnant and not pregnant in orthotic & prosthetic employees
Sophia Mancini, MS, and Rebecca Spragg, CPO
Eastern Michigan University Orthotics & Prosthetics, Ypsilanti, MI, mancini13sl@gmail.com
Introduction or purpose: O&P presents several hazards to clinicians and technicians such as loudness, grinding by-products, hazardous fumes, and machinery.1 Other healthcare fields, such as nursing2, have identified occupational risks for pregnant women, however, no accumulated information on the specific risks for pregnant employees in O&P. The purpose of this research was to identify workplace exposure frequency by female clinicians and technicians, as well as adjustments made during pregnancy, and awareness of the Pregnancy Discrimination Act (PDA).
Methods: Procedures: The study received IRB approval (UHSRC-FY22-23-21). Subjects were recruited to complete a 10-15 minute survey on pregnancy history, workplace accommodations, and PDA knowledge. Participants rated their perceived exposure frequency to 9 hazards for two conditions: pregnant (P) and not-pregnant (NP).
Participants: Inclusion criteria: (1) female biological sex, (2) O&P clinician or technician, (3) was/is pregnant while working in O&P, (4) work at least 20 hours/week prior to family and medical leave associated with pregnancy, and (5) practiced at least 1 year prior to conception.
Data Analysis: Data analysis completed using SPSS. Non-parametric Wilcoxon Signed Ranks Tests to determine if significant differences (p<0.05) existed between exposure while P and NP. Mann-Whitney U tests to determine if significant differences (p<0.05) existed between hazard exposure and pregnancy accommodation, pregnancy loss, and awareness of legal rights.
Results: Analyses were performed on 75 responses. 51% of respondents have heard of the PDA, but over half were not aware of their rights outlined by it and 44% of respondents have never requested accommodations from their employer. Common reasons for not requesting accommodations included: fear of retaliation, being perceived as weak or a hindrance, lack of staff, and general unawareness of laws, options, and what to request of the 9 hazards surveyed, aerosol (p=0.033) and resin (p=0.035) exposure had a significant difference in frequency of use while P compared to NP. While there were no significant data between pregnancy loss and hazard exposure, trends indicate decreased resin exposure while P (p=0.223) or NP (p=0.284) in those who did not experience spontaneous pregnancy loss.
Conclusion: The results of this study are the first of their kind in O&P. Half of females who responded were unaware of their rights during pregnancy. This may mean that females in O&P do not generally seek accommodations, however, several responses to this survey indicate otherwise. These results suggest that employees don’t request accommodations due to fear, working conditions, or lack of knowledge. Of the hazards addressed in this research, several include teratogens, including acetones, glues/adhesives, thinners, aerosol sprays and resins.3 The results of this study suggest that individuals avoid aerosol sprays and resins during pregnancy.
All other hazards had no significant difference in usage, despite their previously identified danger. Further research is needed to determine how these exposures and different levels affect female health and pregnancy outcomes.
Significance: Currently, there are no official guidelines for pregnant women in O&P. Identifying the hazard exposure frequency as well as accommodations that can be requested, and the legal rights of individuals during pregnancy will allow employees to protect themselves.
Disclosure: Authors have no conflicts of interest to disclose.
Acknowledgments: This work was funded by The James H. Brickley Endowment for Faculty Professional Development and Innovation.
References
1. Rahmawati RF, Suzianti A. Identifying Hazards and Risk Assessment in Hazardous Process of Making Prosthesis and Orthosis. In: Proceedings of the 3rd Asia Pacific Conference on Research in Industrial and Systems Engineering 2020. APCORISE 2020. Association for Computing Machinery; 2020:164-168. doi:10.1145/3400934.3400965.
2. Rainbow JG, Dolan HR, Farland L. Nurses’ experiences of working while pregnant: A qualitative descriptive study. International Journal of Nursing Studies. 2021;124:104092. doi:10.1016/j.ijnurstu.2021.104092
3. Sampson, ES. Occupational considerations and hazards facing pregnant clinicians in orthotics and prosthetics. Poster presented at: American Academy of Orthotists & Prosthetists National Meeting; March 2, 2023. Nashville, TN.
Possible implications of pediatric chest wall surgeries on the risk of development of spinal deformities
Rachel White, CPO and Michael Ginzburg Psy.D., MA., MS., CO, LMFT
UC Davis Health, Spine Center Senior Orthotist, Sacramento, CA, USA, Rewhite@ucdavis.edu
Introduction: Scoliosis is a tri-planar deformity of the spine, that is at least 10 degrees, and is routinely seen in orthopedic and multidisciplinary settings12. Most broadly, the scoliotic curves can be described as congenital, neuromuscular, degenerative, or idiopathic; with idiopathic being the most diagnosed1. The prevalence of adolescent idiopathic scoliosis is approximately 1-3% of the adolescent US population3. The prevalence of idiopathic early childhood scoliosis is reported as being less than 1% (Yang et al., 2016). In the thoracic spine, right-sided curves are more common, while sex ratio of idiopathic curves is 10:1 female: male. Detection, monitoring, and the use of orthotic interventions are important in the management of scoliosis. Curves exceeding 40 degrees can lead to pain, cosmetic deformities and psychosocial/emotional distress11, while higher magnitude curves can lead to pulmonary disorders with surgery warranted in severe cases8. Further, curves exceeding 40 degrees at the time of skeletal maturity are statistically likely to continue to progress in adulthood6 further increasing biopsychosocial challenges of the impacted individuals. Appropriate detection and treatment of this condition can, therefore, carry significant implications throughout the lifespan of those diagnosed.
Methods: A review of PubMed digital library was conducted using the search terms “scoliosis,” “thoracotomy,”” sternotomy,” “congenital heart disease,” and “CDH.” The identified publications were reviewed, in their entirety, for confounding variables such as co-occurrence of neuromuscular or orthopedic disorders. 13 studies were identified for inclusion and reviewed in their entirety, spanning publication dates 1993-2020. The prevalence of scoliosis of the overall surgical population and within surgical subtypes was analyzed. The descriptions of the scoliotic curves within the surgical population were also scrutinized and compared to the population norms.
Data analysis: Of the studies reviewed, 9 identified a significant correlation between the surgeries performed and incidence of scoliosis. The range of prevalence of the scoliotic curves varied between the high of 66% and low of 6.6%, with mean reported scoliotic prevalence at 36.14%. One study reported outcomes in the non- operative and operative groups described by the same diagnosis as experiencing 55% and 15% incidence of scoliosis, respectfully. Conversely, 3 studies reported insignificant correlation between the surgeries performed and scoliosis risk, with a high of 2.8% and a low of 1.1%.
Conclusions: The current body of literature suggests that early pediatric thoracic surgical procedures increase the risk of developing scoliosis as compared to the non-surgical populations, and that the scoliotic curves may have clinically relevant distinctions from those described by the Idiopathic Scoliosis diagnosis. The estimation of risk is complicated by a significant discrepancy of the prevalence of scoliosis in the post-surgical groups. There appears to be a prominent gap of knowledge as to how pediatric chest wall surgeries impact the participant’s risk of developing spinal pathologies and the extent to which the post-surgical presentations are biomechanically distinct from the idiopathic scoliosis condition. Additional context as to the correlation between specific diagnoses or procedures and scoliotic curve risk, type, and progression potential can be beneficial to the detection and the improvement of the clinical outcomes for those experiencing scoliosis symptomology. Further exploration of this relationship, ideally through large sample size, multicenter studies, appears as warranted.
Clinical Significance: The relationship between early childhood thoracic surgery and onset of scoliosis is controversial. The clinical guidance regarding the treatment of scoliotic curves for patients that have undergone thoracic surgery is similarly lacking. The clinicians addressing this population can benefit from greater clinical context as to how the co- occurrence of these diagnoses can potentially impact the treatment course of the involved populations. A critical concept of scoliosis management is that early detection and non-operative treatment modalities are inseparable, in that the curvatures that are not clinically detected cannot befit from the mitigation of surgical risk by conservative strategies, with curves exceeding 50 degrees considered as surgical cases9. Simultaneously, no evidence of harm in screening of 10–18-year-old individuals for incidence of scoliosis has been detected6. Additional vigilance in screening individuals that have undergone childhood thoracic surgeries is, therefore, recommended. Further, increased individual attention is warranted when treating patients with a history of early childhood thoracic surgeries in an Orthotics & Prosthetics setting as they may experience earlier onset, higher likelihood of progression, and a gender ratio that is different from Idiopathic Scoliosis cases7.
Disclosures: The authors have no disclosures.
Potentially inappropriate medication use among adults with lower-limb loss: a Beers criteria-based study
Samantha Jeanne Stauffer, CPO, MSOP1,2 and Jaclyn Megan Sions, PT, DPT, PhD1
1 University of Delaware, Newark, DE, 2 Independence Prosthetics-Orthotics, Inc., Newark, DE; sstauffe@udel.edu
Introduction or purpose: The American Geriatrics Society Beers Criteria list identifies potentially inappropriate medications (PIMs) for older adults. These medications, whose risks outweigh their benefits or which have safer alternatives, contribute to increased risk of hospitalization and drug-induced problems (e.g., falls) among adults ≥65 years old.1,2
An alarmingly high rate (>50%) of drug interaction warnings at discharge after high-level amputation surgery,3 suggest medications may not be properly managed in this population. As more than half of adults with lower-limb loss (LLL) report ≥1 fall per year,4 violations of the Beers Criteria, which may increase fall risk, may also be cause for heightened concern in this patient population.
To date, no literature exists assessing medication use among this at-risk population through application of the Beers Criteria. Thus, the aim of this study was to examine frequency of PIM use among older adults with LLL.
Methods: Participants: Data was obtained from adults ≥65 years-old with LLL seen during outpatient multidisciplinary Limb Loss Clinics held Sept 2013 to Dec 2022 (IRB#531197).
Outcomes: Medication lists and fall history were obtained via participant interview with the medical team. Missing data was extracted from prosthetic medical records ± 1 month from the onsite Limb Loss Clinic date.
Data Analysis: Potentially inappropriate medications (PIMs) of the classification “to be avoided” and “to be used with caution” were identified using the American Geriatric Society Beers criteria relevant to the year the participant was seen in the clinic.
Results: Participants (n=82) were 72.9±6.6 years-old, 77.8% male, and 74.4% Caucasian. Of the 82, 59 (72.0%) reported a dysvascular cause of amputation, 66 (80.5%) had unilateral limb involvement, and 34 (41.5%) had ≥ 1 amputation at or above the level of the knee. Median time since amputation was 3.6 years (25th, 75th percentile: 1.1, 8.1). Falls within the past year were reported by 40 (48.8%).
The median number of prescribed medications was 6 (25th, 75th: 4, 9). Of the 82 participants, 41 (50.0%) had at least one Beers criteria violation (Figure 1). The most common PIMs “to be avoided” were benzodiazepines (n=5). The most common PIMs “to be used with caution” were aspirin (n=13) for primary prevention of cardiac events for those ≥80 (revised to ≥70 in 2019) and diuretics (n=10) for management of hypertension and cardiovascular disease. No sociodemographic characteristics arose as risk factors for PIM prescription (p>0.05).
Figure 1.
Frequency and classes of PIM prescription among adults ≥65 years-old with major LLL.
Conclusion: This study indicates PIMs prescription is common among older adults with LLL, especially benzodiazepines, aspirin, and diuretics. Per the Beers Criteria, benzodiazepines should be avoided due to heightened sensitivity among the elderly, leading to dizziness and increased risk of falls.5 Diuretics are to be used with caution due to elevated risk of hyponatremia, whose symptoms include confusion, fatigue, and dizziness.6 Benzodiazepines and diuretics may exacerbate the already high fall risk of adults with LLL.3, 7
Aspirin is recommended to be used with caution due to risk of major bleeding among those ≥ 80 years (revised to ≥ 70 years in 2019). Of the 13 who reported this PIM, 11 reported diabetes, obesity, and/or history of tobacco use, which further increases risk of major bleeding.8
High prevalence of PIM use raises concerns, as this factor may elevate preexisting risk of adverse health outcomes in this population. As no sociodemographic risk factors for PIM use arose, scrutiny of medication use may be indicated for all older adults with LLL. Further research on the implications of PIM use in this population is needed.
Significance: Use of PIMs, especially those which exacerbate fall risk, is common among older adults with LLL. Greater attention should be paid to medications post-amputation to minimize potential adverse consequences.
Disclosures/acknowledgments: Stauffer’s PhD is supported by the Independence Prosthetics-Orthotics Graduate Education Fund.
References
1. Fick DM, et al. Res Nurs Health; 7(5), 42-51, 2008.
2. Perri M, et al. Ann Pharmacother; 39(3), 405-11, 2005.
3. Bastas G, et al. Am J Phys Med Rehabil; 100(11), 1087-92, 2021.
4. Hunter SW, et al. PM&R; 9(2), 170-81, 2017.
5. Davies SJC, et al. J Psychopharmacol: 36(4): 460-69, 2022.
6. Marcum ZA, et al. J Gerontol A Biol Sci Med Sci: 70(12), 1562-8, 2015.
7. de Jong MR, et al. Ther Adv Drug Saf; 4(4), 147-54, 2013.
8. Mahady SE, et al. Gut; 70, 717-24. 2021.
Predicting scoliosis outcome
Gez Bowman, CO, MBAPO
Valley Orthopedic Technology
Introduction: There is little consensus in the medical community as to the required average daily wear time (ADW) for an effective scoliosis bracing treatment. Patients continue to be given a subjective value for the number of hours they need to wear their brace, ranging from 8 hours/day to 23.5 hours/day.
However, multiple prior studies have shown that bracing outcomes are proportional to average daily wear time (ADW). In addition, other studies have shown that outcomes are proportional to in-brace correction (IBC) and that the amount of IBC varies considerably between the braces used and between orthotists. Given these two factors and making some simple basic assumptions we can determine a more mathematical approach to brace wear time, thereby removing the subjectivity of ADW from bracing treatment protocols.
Methods: A successful outcome in bracing requires an accurate application of forces. An approximate measure of this accuracy is the IBC. By recognizing the relationship between IBC and outcome and also ADW and outcome, a mathematical formula has been developed to predict the outcome of brace treatment. A popular recent wearing protocol is to allow a patient a “weekend off per month”. As this reduces the ADW, the mathematical formula shows the effect this has on the outcome prediction.
Results: Comparing the actual results of several braced scoliosis patients with the outcome prediction numbers shows a significant correlation of the two values. The prediction formula is now routinely used in the authors clinic to present to patients the expected outcome of treatment and show how it varies depending on the number of hours worn. It has proven to act as a motivator to encourage compliance with full-time bracing wear schedules.
Conclusion: Once a patient has had their in-brace x-ray and we have determined the IBC, use of a mathematical formula using the given values for IBC and ADW could be a useful tool for the treatment team to predict outcome and/or show the need for changes to the treatment. When the formula suggests a negative outcome, it would demonstrate a need for modifications to the brace to improve IBC and/or changes to the ADW.
References
1. Agabegi, Steven. Step-Up to Medicine. LWW, 2019.
2. Barton, Cameron B., and Stuart L. Weinstein. "Adolescent Idiopathic Scoliosis: Natural History." Pathogenesis of Idiopathic Scoliosis, 2017, pp. 27-50.
3. Bleiziffer, Sabine, et al. "The influence of right anterolateral thoracotomy in prepubescent female patients on late breast development and on the incidence of scoliosis." The Journal of Thoracic and Cardiovascular Surgery, vol. 127, no. 5, 2004, pp. 1474-1480.
4. Dubousset, Jean. "Definition of Adolescent Idiopathic Scoliosis." Pathogenesis of Idiopathic Scoliosis, 2017, pp. 1-25.
5. Eby, Sarah F., et al. "Thoracogenic spinal deformity: a rare cause of early-onset scoliosis." Journal of Neurosurgery: Spine, vol. 29, no. 6, 2018, pp. 674-679.
6. Feiz, Hojjat H., et al. "Scoliosis after thoracotomy/sternotomy in children with congenital heart disease." Indian Journal of Orthopaedics, vol. 46, no. 1, 2012, pp. 77-80.
7. Glotzbecker, M. P., et al. "Scoliosis after chest wall resection." Journal of Children's Orthopaedics, vol. 7, no. 4, 2013, pp. 301-307, doi:10.1007/s11832-013-0519-2.
8. Grossman, David C., et al. "Screening for Adolescent Idiopathic Scoliosis." JAMA, vol. 319, no. 2, 2018, p. 165.
9. Herrera-Soto, Jose A., et al. "Spinal Deformity After Combined Thoracotomy and Sternotomy for Congenital Heart Disease." Journal of Pediatric Orthopaedics, vol. 26, no. 2, 2006, pp. 211- 215.Horne, J. P., Flannery, R., &Usman, S. (2014). Adolescent idiopathic scoliosis: diagnosis and management. Am Fam Physician, 89(3), 193-8.
10. Hresko, M. T., et al. "Early Detection of Scoliosis—What the USPSTF “I” Means for Us." JAMA Pediatrics, vol. 172, no. 3, 2018, p. 216.
11. Illés, Tamás S., et al. "The third dimension of scoliosis: The forgotten axial plane." Orthopaedics & Traumatology: Surgery & Research, vol. 105, no. 2, 2019, pp. 351-359.
12. Kuznia, Angela L et al. “Adolescent Idiopathic Scoliosis: Common Questions and Answers.” American family physician vol. 101,1 (2020): 19-23.
13. Lehnert-Schroth, Christa. Three-dimensional Treatment for Scoliosis: A Physiotherapeutic Method for Deformities of the Spine. 2007.
14. Mishra, Prabal R., et al. "Scoliosis after thoracotomy repair of esophageal atresia: a systematic review." Pediatric Surgery International, vol. 36, no. 7, 2020, pp. 755-761.
15. Peltonen, Jari, et al. "Surgical correction of spinal deformities after solid organ transplantation in childhood." European Spine Journal, vol. 15, no. 8, 2006, pp. 1230-1238.
16. Roclawski, Marek, et al. "Scoliosis in Patients with Aortic Coarctation and Patent Ductus Arteriosus: Does Standard Posterolateral Thoracotomy Play a Role in the Development of the Lateral Curve of the Spine?" Pediatric Cardiology, vol. 30, no. 7, 2009, pp. 941-945.
17. Scalabre, Aurélien, et al. "Prognostic Risk Factors for the Development of Scoliosis After Chest Wall Resection for Malignant Tumors in Children." Journal of Bone and Joint Surgery, vol. 96, no. 2, 2014, p. e10.
18. Soliman, Hany A., et al. "Prevalence and natural history of scoliosis and associated congenital vertebral anomalies in patients operated for esophageal atresia with or without tracheoesophageal fistula." Journal of Pediatric Surgery, vol. 54, no. 7, 2019, pp. 1308-1311.
19. Van Biezen, F. C., et al. "Scoliosis in children after thoracotomy for aortic coarctation." The Journal of Bone & Joint Surgery, vol. 75, no. 4, 1993, pp. 514-518.
Prospective fall risk measures in people who used a unilateral lower-limb prosthesis
Graci Finco, PhD, CPO1; Cody McDonald, PhD, CPO2; Sarah Moudy, PhD1
1 University of North Texas Health Science Center, Fort Worth, TX, 2 University of Washington, Seattle, WA MalakaFinco@my.unthsc.edu
Purpose: Falls are prevalent in people who use unilateral lower-limb prostheses.1 Despite higher fall prevalence, fall-related injuries, and fall-related medical costs in this population compared to non-amputees, fall risk is still not effectively screened.2 Clinical outcome measures could help screen fall risk, but few studies have examined association between clinical outcome measures and falls.2 A recent study found the Timed Up and Go (TUG), Four Square Step Test (FSST) and Amputee Mobility Predictor with Prosthesis (AMPPRO) could each significantly distinguish retrospective fallers from non-fallers.3 However, clinical outcome measures associated with prospective falls are also needed to help proactively assess potential fall risk, and mitigate issues with retrospective fall data, such as recall bias and gait changes after a fall occurs.2 Prospective fall risk measures that are easily implemented in clinic could help improve quality of life and reduce medical costs. One recent study determined no clinical outcome measures alone were effective at distinguishing 6-month prospective fallers from non-fallers.4 Rather, a combination of the TUG, FSST, and fall history were associated with the number of 6-month prospective falls.4 Gait parameters might be more effective at determining prospective fall risk than any clinical outcome measure alone, but no studies have investigated this relationship. We sought to determine if any clinical outcome measure scores or gait parameters could significantly distinguish between fallers and non-fallers using either retrospective or prospective fall reporting to define groups.
Methods: This study was approved by the North Texas Regional IRB. Participants who used unilateral transtibial or transfemoral prostheses were included, and completed several clinical outcome measures: Socket Comfort Score (SCS), Prosthetic Limb Users Survey of Mobility (PLUS-M), Activities Specific Balance Confidence Scale (ABC), Patient-Reported Outcomes Measurement Information System (PROMIS-29), TUG, FSST, and AMPPRO. Participants walked 8 meters five times while wearing inertial measurement units (IMUs; iSen, STT Systems, Spain) to obtain spatiotemporal and joint angle data, and pressure insoles (Loadsol, Novel Electronics Inc., USA) to obtain ground reaction force data. Gait parameters included walking speed, peak sagittal plane joint angles at the hip, knee, and ankle, and peak ground reaction force. Symmetry between prosthetic and intact limbs was calculated for peak parameters using a standard equation.5 Participants were asked their 12- month retrospective fall history during the study visit, and then reported their falls every 2 weeks via survey for 6 months following the study visit. A Mann-Whitney U test was used to determine if any clinical outcome measure or gait parameters could significantly distinguish fallers from non-fallers.
Results: 22 participants (age 57.6 ± 4.2 years, 15 transtibial, 7 transfemoral) completed the in-person visit, and 1 participant was lost to 6-month prospective follow-up. (Table 1)
Table 1.
Age, number of people who used a transtibial (TT) or transfemoral (TF) prosthesis, and parameters that significantly distinguished fallers and non-fallers.
| 12-month Retrospective | 6-Month Prospective | |||||
|---|---|---|---|---|---|---|
| Non- Fallers (n=12) | Fallers (n=10) | p- value | Non- Fallers (n=11) | Fallers (n=10) | p- value | |
| Age(yrs) | 57.5±15.0 | 56.8±13.8 | 0.899 | 55.0±16.4 | 60.6±11.7 | 0.376 |
| TT/TF | 8/4 | 7/3 | 0.874 | 8/3 | 6/4 | 0.562 |
| Speed (m/s) | 0.6±0.2 | 0.5±0.14 | 0.138 | 0.7±0.2 | 0.5±0.1 | 0.048 |
| TUG(s) | 9.7±1.8 | 11.1±3.0 | 0.090 | 9.6±2.0 | 11.6±2.2 | 0.035 |
| FSST(s) | 12.7±5.4 | 14.8±3.4 | 0.040 | 11.6±3.2 | 16.5±4.5 | 0.007 |
Values are depicted as mean ± standard deviation. Significance (bold text) was considered p<0.05.
Conclusion: This is the first study to find several clinical outcomes alone (walking speed, TUG, FSST) could distinguish 6-month prospective fallers from non-fallers, with fallers showing slower times than non-fallers. Overall, our results align with previous research that found the FSST and TUG seem to be most useful to distinguish fallers from non-fallers.2-3 No gait symmetry parameters or self-report clinical outcomes were significant. Future research can determine cut-off scores and assess generalizability of our findings with a larger sample size.
Significance: Slower walking speed, TUG times, and FSST times could help proactively assess fall risk in this population.
Disclosure: This study is funded by the Center for Orthotic and Prosthetic Learning and Outcomes/Evidence-Based Practice distributed by the American Orthotic and Prosthetic Association.
Acknowledgements: Thanks to Cody Longenbaugh (Baker O&P), Mark Ashford (Hanger Clinic), Cait Finnerty, Shawn Kennedy, and Tasha Buxton for help with recruitment and data collection.
References
[1] Kim et al. PM&R 2019; 11: 344–353.
[2] Finco, Sumien, Moudy. JAGS 2023; 71:3.
[3] Hakim et al. J Dev Phys Disabil 2018; 30: 677–688.
[4] Sawers & Hafner. PM&R 2021; 1-11.
[5] Finco, Moudy, Patterson. JPO 2023; 35:1.
Ratcheting prosthetic fingers significantly improve outcomes for people with partial hand amputation
Ben Pulver, MS1 (ben@pointdesignsllc.com), Jacob Segil, PhD1,2, Stephen Huddle, MS1,3, Richard Weir, PhD1,3, Jack Patte3, Levin Sliker, PhD1
1 Point Designs, 2 University of Colorado Boulder, 3 University of Colorado Denver | Anschutz
Introduction: There are more than 25,000 partial hand amputations each year in the U.S1. There are now many more devices available to treat partial hand amputations, but there is still not an adequate amount of quantitative clinical data to support the application of these devices. This presents regulatory and reimbursement challenges for both manufacturers and practitioners which ultimately limits access to partial hand prostheses. A robust interventional clinical study on partial hand prostheses was conducted to address this need.
Patient outcomes before and after being fit with ratcheting mechanical prosthetic fingers were assessed using two task-based and two patient reported outcome measures.
Methods: The Western Institutional Review Board approved this study (protocol #20182022), and informed consent was obtained from all subjects.
Participants: Eleven (11) subjects with partial hand amputation were recruited. Eight (8) participants were male, and three (3) were female; with an age range of 22 – 61 years. Inclusion criteria was loss of at least index and/or middle fingers, but an intact thumb.
Prosthesis: Each subject was fit with a partial hand prosthesis made of a HTV silicone liner, carbon fiber frame, and ratcheting mechanical prosthetic fingers. Procedures: Subjects participated in four data collection sessions: prior to prosthesis fitting (Pre), immediately after definitive prosthesis fitting (Post), 30 days after prosthesis fitting (30-day post), and 60 days after prosthesis fitting (60-day post). Outcome measures were collected each session using the EQ- 5D-5L, DASH, SHAP, and CAPPFUL.
Analysis: A linear mixed effects model was used. The model determined how significant age, gender, hand dominance, days since amputation, the number of fingers involved, and prosthesis use were in determining the total scores for all outcome measures.
Results: All post-fitting visits were coded as the “Prosthesis” condition and the pre-fitting visit was coded at the “No Prosthesis” condition. Significant differences between these two conditions were found for the DASH, EQ-5D-5L, and CAPPFUL. The SHAP did not show a significant difference. Table 1
Table 1.
Effect of partial hand prostheses on outcomes.
| Fixed Effects | Outcome Measure | Coefficient | p. Value | Low. CI | High. CI |
|---|---|---|---|---|---|
| No Prosthesis vs | DASH | −12.2 | 1.92E-05** | −17.1 | −7.4 |
| EQ-5D-5L | 4.8 | 0.002** | 2.0 | 7.7 | |
| Prosthesis | CAPPFUL | 12.7 | 0.018* | 2.5 | 22.9 |
| SHAP | 2.5 | 0.408 | −3.4 | 8.3 |
*p < 0.05, ** p < 0.01.
No significant effects were found for age, gender, hand dominance, or days since amputation. There was a significant difference in the SHAP and CAPPFUL scores with and without a prosthesis for the 4-finger presentations.
Conclusion: There was a significant improvement in both patient reported and task-based outcome measures from the no prosthesis condition to the prosthesis condition. Additionally, a larger benefit was found for patients missing 4 fingers. This demonstrates that partial hand prostheses are state-of-the-art and clinically sound treatments for partial hand amputation.
Significance: This study provides quantitative data demonstrating the benefits of partial hand prostheses. These data can be used to improve insurance authorization requests and regulatory submissions. Additionally, this study identified a possible need for a task-based outcome measure more tailored to the partial hand population.
Disclosure: Authors Pulver and Sliker are employees of Point Designs and authors Segil, Huddle, Weir, and Sliker are co-founders of Point Designs.
Acknowledgements: Research was supported, in part, by the NICHD of the NIH under Award Number R42HD097827
References
1. Conn, J. M, et. al. (2005). Annals of emergency medicine, 45(6), 630-635.
Scoping review of the evidence on powered prosthetic ankle-foot components
Andreas Kannenberg, MD (GER), PhD
Otto Bock HealthCare, Austin, TX. Email: andreas.kannenberg@ottobock.com
Introduction: Powered prosthetic ankle-foot (PwrAF) components have been available commercially for about a decade and subjected to a fair amount of biomechanical and clinical research projects. However, acceptance by healthcare payers is still scarce. For that reason, a scoping review of the existing literature on PwrAF was conducted to extract potential patient benefits and identify potential research gaps.
Methods: A literature search with terms pertaining to PwrAF for persons with transtibial amputations (TTA) was performed in 4 literature databases and archives of several journals. Identified publications were screened for pertinence by title and abstract first. Papers with unclear pertinence were reviewed as full texts. Methodological quality of pertinent publications was assessed using the criteria of the State of the Science Evidence Report Guidelines of the AAOP (1). Findings of publications with sufficient quality were extracted and are presented descriptively.
Results: The literature search yielded 628 publications. After removal of duplicates, non-pertaining and basic technical articles, predominantly biomechanical publications, and studies conducted with prototypes not available to the public, 21 publications on commercially available PwrAF remained for full-text review. Of these, 5 case series were excluded for insufficient methodological quality. Thus, 16 publications on clinical studies were included in this scoping review.
The only consistent benefit found was the reduction of sound knee pain, amputated side knee pain, and low-back pain (2,3) that is based on biomechanical unloading mechanisms confirmed by a number of biomechanical studies (4,5). The reduction in pain is accompanied by a reduction in pain-related activity restrictions and an increase in patient-reported mobility (2,3).
Early studies of the inventors of the BiOM® foot found significant and clinically meaningful improvements in self-selected walking speed and metabolic energy consumption that could not or only partially be confirm by independent groups. Thus, the state of the evidence for these outcomes as well as for performance-based and patient-reported function and mobility in general must be referred to as “conflicting”.
Some studies found that, depending on the outcome measures assessed, 30-50% of their subjects benefited individually from the PwrAF. It appears that many users struggle to effectively utilize the power delivered by the ankle for propulsion, ambulation, and function. Though the evidence suggests that the current version of the PwrAF (Empower®) has a substantially higher responder rate than the previous version (BiOM®), patient selection, device tuning, and patient training remain absolutely critical success factors.
Discussion: Persons with TTA may experience clinical benefits from PwrAF. However, research suggests that the adaptation of neuromuscular control to the increased power delivered by the PwrAF may not be intuitive for many potential users. Therefore, further research is needed to better characterize individuals who are most likely to benefit from a PwrAF and to develop a device-specific training program that helps persons with TTA adapt to and effectively utilize the ankle power delivered for mobility.
Conclusion: Persons with TTA may benefit from a PwrAF, but more research is needed to improve the responder rate.
Disclosure: The author is a full-time employee of Otto Bock Healthcare LP.
References
1. Hafner BJ. Washington (DC): American Academy of Orthotists & Prosthetists (AAOP); 2008.
2. Kannenberg A, et al., Front Rehabil Sci 2022; 2:805151.
3. Cacciola CE, et al., J Prosthet Orthot 2022; Online first publication.
4. Grabowski AM, et al., J NeuroEng Rehabil 2013;7;10:49.
5. Russell Esposito E, et al, Clin Biomech (Bristol, Avon) 2014 Dec;29(10):1186-92.
Skills transference and limb loading in augmented reality prosthesis training: A case study
Christopher L. Hunt1 and Rahul R. Kaliki1
1 Infinite Biomedical Technologies, LLC, USA
Introduction: Augmented reality (AR) has emerged as an exciting modality for prosthesis training in recent years1,2. Despite the popularity of AR, it has been difficult to show its efficacy in transferring learned motor skills to those required for real- world prosthesis operation. While recent work has shown that replicating dynamic interactions (e.g. socket forces, limb loading) improves the process of skill transference2,3, these principles have yet to be demonstrated in an individual with upper-limb loss (ULL). In this work, we present a case study wherein an individual with ULL underwent a multi-session AR prosthesis training regimen with limb loading.
Methods: This study was conducted in accordance with a protocol approved by the Johns Hopkins University School of Medicine Institutional Review Board.
A participant with ULL underwent a 7-session prosthesis training regimen2. During the first session (the pre-test), the participant’s ability to control a prosthesis was assessed using the Prosthetic Hand Assessment Measure (PHAM)4. The participant was tasked with operating a myoelectric prosthesis to complete 40 object manipulations, each separated into four phases: Reach, Grasp, Transport, and Release. During each of the following 5 sessions, the participant performed the same sequence of object manipulation in AR, controlling a virtual prosthesis to complete a virtual replica of the PHAM2. The participant donned a non-operational, physical prosthesis to simulate load bearing. In the final session, the participant repeated the assessment from session 1 (post-test).
The participant was a 54-year-old female with bilateral upper- limb and lower-limb amputations secondary to scleroderma complications. The participant was five years removed from her last upper-limb surgical revision and naïve to both pattern recognition myoelectric control and AR display modalities. The participant completed the experimental protocol using her transradial residual limb.
Results: The participant demonstrated increased performance on the PHAM post-training with limb loading. Although the participant progressed only slightly in task completion rate between the pre- and post-test assessments (+2.5%), she was able to complete more phases of object manipulation in general. In both the pre- and post-test, the participant had no issue completing the Reach phase of all manipulations (100%). However, the participant was able to complete more of all other phases of object manipulation post-training: Grasp (15% vs 55%), Transport (5% vs 37.5%), and Release (0% vs 2.5%) (Table 1). Phase Completion Percentage (%)
Table 1.
Task performance results for the pre- and post-test physical assessments. Bolded valued indicate phases where there was improved performance in the post-test.
| Reach | Grasp | Transport | Release | |
|---|---|---|---|---|
| Pre – | 100 | 15 | 5 | 0 |
| Post – | 100 | 55 | 37.5 | 2.5 |
Conclusion: Results from this preliminary case study demonstrate an increase in object manipulation competency post-training. Although the performance increase (in terms of completion percentage of the Release phase) is modest, the participant showed a clear increase in competency when grasping and transporting the object. The asymmetry in Grasp and Release performance may be due to the increased difficulty of the Release phase. During Grasp, an individual may lower the required precision by relying on surface forces to help slide the object out of its holder, an interaction which is not possible during Release. An extension of this work may explore AR interventions in motor tasks where Grasp and Release are of equal difficulty (e.g. the Gaze and Assessment Measure5). Although this study is a promising first step, future work with a larger cohort of participants is required to further explore the generalizability of these principles.
Significance: The preliminary results highlighted in this case study present evidence that socket and limb loading is crucial for effective virtual prosthesis training for an individual with ULL. They also indicate the need to include prosthetic training in the rehabilitation plan for new technologies.
Disclosure: The authors have no potential conflicts of interest.
Acknowledgements: This work was funded under the National Institutes of Health Grant No. DM190888 and under the Department of Defense Grant No. 136019.
References
1. Boschmann A, et al. J Neuroeng Rehabil; 2021
2. Hunt CL, et al. J Neuroeng Rehabil; 2023.
3. Chappell D, et al. IEEE Robot Automat; 2022.
4. Hunt CL, et al. Myoelectric Control Symp; 2017.
5. Williams HE, et al. PLoS One; 2019I.
Skin assessment on people of color in prosthetics and orthotics
Richardson G,1 Cheever S,2 Phillips D,3 Spaulding S,3 McDonald CL3
Thompson's Custom Orthotics & Prosthetics, Spokane, WA 1 , Cornerstone Prosthetics and Orthotics, Everett, WA 2 , University of Washington, Seattle, WA 3
Introduction: Darker skin tones are currently underrepresented in orthotic and prosthetic (O&P) clinical education. Teaching resources on skin problems related to the use of O&P devices primarily focus on Caucasian skin.1-2 Because evaluation of the skin is such an important aspect of how prosthetists and orthotists assess socket fit, orthosis fit, residual limbs and wound healing, the omission of darker skin tones in educational materials likely contributes to disparities in patient outcomes. If students and clinicians are not trained to identify skin problems on darker skin tones, many treatable issues may go unidentified and untreated resulting in patient pain, injury, reduced mobility, or compromised health. Materials for teaching evaluation of darker toned skin do not currently exist in O&P education or professional continuing education.
Methods: We are developing an evidence-based digital handbook that includes images and descriptions of various skin problems related to O&P as they appear on darker skin tones.
To create this handbook, we are using a step-wise approach. The first step was to finalize a prioritized list of clinical assessment areas and common skin problems seen among O&P users. This list was created by searching through current resources in O&P clinical education, a literature review of available evidence in dermatology and O&P, and clinical expertise from prosthetists, physiatrists, and dermatologists.
Next, we created a website (Figure 1) and intake survey (using REDCap) to facilitate submission of images by O&P users and/or their providers. The website and survey include guidelines on best practice for image capture and a requirement to include a color correction swatch for standardization across images. We are now ready to solicit images from the O&P community using the established website and submission portal.
Figure 1.
The O&P Skin Tone Project website.
Results: To date, we have established a website and standardized processes for the collection of images and permissions for image use. Processes have been piloted with five individuals to ensure clarity of instructions and usability of interface. Pilot funding to support payment for images has also been secured.
Next steps for the project include engagement with the O&P community to recruit individuals willing to share their images. Additionally, an advisory board of clinicians, O&P users, and related stakeholders will be established to guide project progress, development, and dissemination. Figure 2
Figure 2.
Example digital handbook page.
Conclusions: The digital handbook currently being developed will serve as a tool to advance teaching practices in O&P education and provide continuing education to increase awareness and skill of clinicians to accurately identify skin conditions on darker skin tones. The handbook will be available free of charge within O&P education and as a clinical resource.
Significance: A handbook to increase awareness and skin assessment skills related to O&P on darker skin tones is needed to improve equity in patient care and outcomes. To make this project a success, we need participation from the O&P community.
Disclosure: The authors have no conflict of interest.
Acknowledgments:
References
1. Levy SW. Prosthet Orthot Int. 1980 Apr;4(1):37-44.
2. Highsmith MJ. Amputee Coalition website.
3. The O&P Skin Tone Project, available at https://sites.google.com/view/opskintoneproject/home.
Socket Comfort Score: Comparing current transtibial socket with custom direct fit socket
Pamela K Hale, CPO
Amparo Prosthetics, pam@amparo.world
Introduction or purpose: The purpose of this case study is to define a method for collecting and evaluating Socket Comfort Score (SCS) data as more transtibial amputees are fit with custom direct fit sockets. Direct fit transtibial sockets are designed to bypass the conventional process of providing a prosthesis and improve the time to delivery. Prosthetic intervention without multiple visits to a prosthetist’s office for evaluation, casting, check socket fitting and finally delivery is beneficial for the patient and practice.
Socket comfort is paramount to fit, function and acceptance of the prosthesis. It is important to verify socket comfort when introducing a new socket material and technique for fabricating and fitting a socket. This single subject case study reports on the socket comfort of the new socket as compared to the previous socket fabricated in a traditional fashion.
Methods: A single subject was identified by convenience as a patient model by the prosthetist learning the direct fit technique. The subject completed the Socket Comfort Survey regarding their current prosthesis prior to interaction with the prosthetist. The subject was interviewed by the treating prosthetist regarding age, height, weight, gender, date of amputation, cause of amputation, K level, age of current socket, and specific areas of residual limb discomfort. The prosthetist inspected and documented the features of the current prosthetic socket, suspension, alignment and foot/ankle. The prosthetist determined the number and type of visits in order to provide the current prosthesis. The prosthetist then applied the direct fit socket after preparing the residual limb as the “positive model”. The prosthesis was statically and dynamically aligned once the socket trim lines were finished the socket was mounted to a foot and pylon. The patient then ambulated with the direct fit socket prosthesis for 30” then completed a Socket Comfort Survey regarding the direct fit socket. The subject would have been excluded from the trial if they had an open wound on their residual limb.
Results: The subject is a 55-year-old male, 6’2” and 210 pounds with a left transtibial amputation and functions at a high K3 level.
His leg was amputated in 1993 after 6 years of limb salvage attempts following a shot gun trauma to his lower leg. His current socket was delivered March 2022 and is 1 year old. It is a total surface bearing design socket constructed of rigid acrylic and carbon fiber with pin/lock suspension and a 6 mm gel liner and a K3 level foot. He currently utilizes 14 ply socks to maintain fit. From evaluation to delivery took 7 visits, with many trial periods of the socket lasting up to 2 weeks. He rated his socket comfort a 0/10.
The direct fit socket was fabricated as a total surface bearing socket and fit in one visit within 45” and he had a completed prosthesis in 1.5 hours including static and dynamic alignment. The socket was fit over a 6 mm gel liner with pin/lock suspension. After ambulating with the socket for 2 days over 10 hours in a large warehouse he added 2 ply socks. Figure 1
Figure 1.
Delivery timeline.
Conclusion: For this subject the direct fit socket was more comfortable and was delivered in a timelier manner. Providing a comfortable socket within a day is advantageous for amputees to start rehabilitation earlier and to reduce interruption to function and activities of daily living. Additionally, reduced transportation and time in prosthetist’s offices are valuable improve attendance at school, work and in life.
Significance: The case study shows that there is a viable alternative to conventional socket fabrication that meets the needs of the patient in socket fit, comfort and function. This case study highlighted the outcomes measures that can be collected to further this study with a larger subject pool. By measuring and evaluating socket comfort and time to delivery a case can be made for providing custom direct fit sockets as a new standard of care.
Disclosure: Pamela K Hale, CPO is a paid consultant for Amparo Prosthetics, a manufacturer of a direct fit socket.
Acknowledgments: Thank you to Mr. T Dunn, for his insight and enthusiasm.
References
Hanspal, R. S., Fisher, K., & Nieveen, R. (2003). Prosthetic socket fit comfort score. Disability and Rehabilitation, 25(22), 1278–1280. https://doi.org/10.1080/09638280310001603983
The Coffee Task: An assessment of multi-grip upper limb prosthetic performance
Christina Lee, Alicia Davis, Jordan Kartes, Alex Vaskov, and Deanna H. Gates*
University of Michigan, Ann Arbor, MI, USA Email: gatesd@umich.edu
Introduction: It is difficult to determine functional benefits of multi-grip prostheses due to a lack of standardized assessments that evaluates performance during grasp transitions. Existing and commonly used assessments largely focus on performance during a single grasp without consideration of the ability to successfully select appropriate grasps for the task.1-3 Here, we propose a functional assessment, the Coffee Task, which addresses this gap by specifically measuring performance as individuals use a series of grasps in sequence. To be suitable for clinical and research purposes, outcome measures must be validated, highly reliable, and be easily interpretable. To ensure the Coffee task met these criteria, we evaluated inter- rater reliability, known-group difference validity, convergent validity, and responsiveness.
Methods: The Coffee Task is a bilateral activity of daily living, during which individuals simulate brewing a cup of coffee in a pod- style coffee maker using three functional grasps (fist, pinch, point) and five grasp transitions. There are two separate versions of the task: segmented and continuous. During the segmented version, participants are given up to five attempts to complete all parts of the task, including selecting the appropriate grip for each segment. During the continuous version, individuals complete the task without breaks with the goal of completing the task as fast as possible, with a maximum of 2.5 minutes. The main outcomes of the segmented and continuous task are number of errors and completion time, respectively.
Ten healthy individuals who provided consent to participate completed the two versions of the Coffee Task and the Box and Block Test (BBT)3 before and after 30-minutes of training. They completed the task first with their intact limbs (continuous only), and then with a prosthetic emulator on their right limb using an i-Limb Quantum (Ossur, Reykjavik, Iceland) with trigger control and pattern recognition over two experiment sessions, in random order. Two independent raters assessed the Coffee Task outcomes using video recordings. We evaluated inter-rater reliability, known-group and convergent validity, and responsiveness to change.
Results: Inter-rater reliability: The intra-class correlation coefficient (ICC) of the number of errors and completion time were 0.991 and 0.997 respectively (p < 0.001).
Known-group validity: On average, completion time was 75.8- s faster when participants used their intact limb compared to the prosthetic emulator (p < 0.001; Figure 1).
Figure 1.
Number of errors and completion time for pattern recognition (PR; green) and trigger control (TC; red) with error bars (standard deviation). Average completion time with intact limb (grey; no emulator) was used to determine known-group validity. Statistically significant (p < 0.05) comparisons are noted with *.
Convergent validity: There were moderate correlations between the number of blocks moved during the BBT and the continuous (|r| = 0.74, p < 0.001) and segmented (|r| = 0.43, p = 0.010) Coffee Tasks.
Responsiveness to Change: The participants completed the Coffee Task with fewer number of errors and faster completion time post-training compared to pre-training (p < 0.003; Figure 1). There was no difference in performance between the two control approaches (p > 0.409).
Figure 1.
Boolean subtraction of the “socket interlocking element” and foot from the full box.
Conclusion: The Coffee Task had high inter-rater reliability and demonstrated known-group and convergent validity. The Coffee Task was responsive to changes due to training and may therefore be suitable to track the learning progress of a new prosthesis user or differentiate performance between new and experienced users. Future work should obtain reliability and validity measures in individuals with limb loss who use multi-articulating prostheses in daily life.
Significance: The Coffee Task is a valid and reliable method of quantifying grip-switching performance.
Acknowledgments: This work was supported by the Department of Defense award number HT9425-23-1-0097 and the Rackham predoctoral research grant at the University of Michigan. We thank Ossur for providing the prosthesis used in this study.
References
1. Light. Arch Phys Med Rehabil. 83(6): 776-83, 2002.
2. Hussaini. Prosthet. Orthot. Int. 43(5): 485-91, 2019.
3. Mathiowetz. Am J Occup Ther. 39(6): 386-91, 1985.
The effect of early COVID-19 policy on a multi-national cohort of individuals dependent on knee-ankle-foot orthoses for ambulation
Tyler Klenow, MBA, MSPO, CPO, FAAOP
Ottobock Healthcare LP, Austin, TX, USA, tyler.klenow@ottobock.com
Introduction: Early COVID-19 policy included stay-at-home orders and recommendations of various lengths and severities from local governments across the world. In addition, anxieties regarding the pandemic persist and reduce in- person community engagement. Overall, marked reductions in physical activity, mobility, and walking have been reported in the literature.1 While several reports regarding the effect of COVID-19 on orthotic and prosthetic care delivery have been published,2 no studies regarding the physical performance of corresponding patient populations have been disseminated.
A multi-national crossover study of the efficacy of the C-Brace (OttoBock Se&Co., Duderstadt, Germany), a microprocessor-controlled stance and swing orthosis compared to traditional KAFOs (Locked KAFOs and SCOs) in a dependent cohort was being conducted during this time. The purpose of this work was to describe the mobility, physical performance, and quality of life reported in this cohort before and after the onset of COVID-19. It was hypothesized that a decrease would be noted in all outcomes during this period consistent with existing literature.
Methods: A several-month pause was placed on the aforementioned crossover trial at the onset of COVID-
19. Subjects who had not completed the protocol performed a reassessment of study outcome measures to ensure they still met inclusion criteria before resuming their respective trial phase. A primary analysis of values from the most recent evaluation prior to the pause and this reassessment for the Berg Balance Scale (BBS), Activity-specific Balance Confidence Scale (ABC), EQ- 5D-5L, falls, and self-reported distance walked per day was conducted in subjects from the United States (US) and Europe (EU). Statistical analysis was calculated using repeated-measures t-tests. A secondary ad-hoc analyses between bracing conditions using appropriate two-sample t-tests were also conducted. The a-priori significance level for all tests was set at p≤0.05.
Results: Thirty-one subjects (n=31) completed a reassessment and were included in the analyses. None of the outcomes reached statistical significance in the primary repeated measures analysis. The secondary analysis revealed declines in the mean difference of each outcome in the KAFO group which reached the level of statistical significance when compared to the mean differences in C-Brace group with the BBS, EQ-5D-5L, and distance walked (p<0.05). Table 1
Table 1.
Total sample and bracing group mean difference comparison before and after COVID-19 onset.
| Mean Differences before and after COVID-19 | ||||
|---|---|---|---|---|
| OM | Total Δ | C-Brace Δ | KAFO Δ | Mean Diff. p -value |
| BBS | 1.29 | 4.57 | −2.32 | 0.011 |
| ABC | −6.91 | −5.04 | −11.31 | 0.252 |
| EQ-5D-5L | −0.007 | 0.018 | −0.062 | 0.039 |
| Falls | 5.6 | −14.3 | 18.6 | 0.059 |
| Distance Walked (mi.) | −0.26 | 0.44 | −0.70 | 0.031 |
Conclusion: The hypothesis that all outcomes would decline due to COVID-19 was not supported. A secondary analysis revealed the KAFO group did decline in each outcome as anticipated, but the C-Brace improvements in 4/5 outcomes and more modest decline in the ABC inflated the means on aggregate.
Significance: The C-Brace group showed significant improvements in mobility, distance walked per day, and quality of life as well as marked improvement in falls compared to the KAFO group despite the onset of COVID-19. The KAFO followed the expected trend of decline during the early COVID-19 period consistent with other literature.
Disclosure: Tyler Klenow is an employee of Ottobock Healthcare LP, the North American Manufacturer of the C-Brace.
Acknowledgments: The C-Brace Crossover Study was made possible through cooperation with multiple clinical partners including Hanger Clinic.
References
1. Park et al. J Glob Health. 2022; 12: 05003.
2. Eddison et al. Prosthet Orthot Int. 2021; 45(5):373-7.
The importance of implementing of a mechanical stance control orthosis in an early stage during rehabilitation in order to improve standing, walking and activities of daily living.
Flora Versyck, CPO, PT
Basko Healthcare, f.versyck@basko.com
Introduction: Choosing the correct orthosis at the right moment in a rehabilitation process for patients with severe knee instability due to quadriceps disfunction is a major issue.
The decision for a MSCO is often made too late or too conservative due to a lack of knowledge about the possibilities the MSCO can offer in the clinical rehabilitation process or because of the cost price of the orthosis not being properly considered in the overall rehabilitation process.
The MSC hinge does not impose restrictions during gait but only gives the security by locking the knee during stance phase.
The purpose of the MSCO consists to activate the full body function and not to stimulate the compensatory gait in order to improve functional activities and to get patients faster back to the most normal life as possible.
The persons in this case studies had a decrease or stagnation of the body control during rehabilitation without an MSCO, as well as during postural static position as during gait.
Method: All patients were tested with the testing device and after having the approval of the multidisciplinary team they received a custom made KAFO with the Swing Phase Lock joint as knee joint and a double action joint on the ankle with a dorsal flexion stop and dorsal flexion assistance if needed.
The use of the orthosis has been supported by physical rehabilitation following a written plan of treatment which stimulates postural and gait training. The mechanical stance control joint requires active body posture and controlled movement of the patient which stimulates the entire muscle chain (whether or not actively present). To observe the improvements with the MSCO, TUG-test, MRC-scale, 6 minute walking test, Patient Specific Functional Scale and pain Scale were used. All tests were done with and without the MSCO and were video recorded. All data were documented and differences in speed, pain and functionality were calculated with the G-walk sensor, chronometer or with approved scales.
Results: 3 active persons, 2 male and 1 female with average age of 43.66 years old were included in this case study. They all had quadriceps insufficiency less than or equal to 3 following the MRC scale. 2 persons had dorsal flexors deficit and 2 persons walked with a cane. All persons showed a Genu Recurvatum since minimum several months or even years.
The outcome measures with the MSCO were positive, up to 29,7% faster in walking speed with pain rated at 1 instead of 6 with the MSCO and without a cane. The rating on the PSFS improved from average 2 to 7 in less than 2 weeks. One person with Multiple Sclerosis improved the muscle force from 3 to 4+ in 18 months. One person was able to go back to work after he received the orthosis.
Conclusion: To use MSCO early in rehabilitation helps avoiding compensation techniques and means freedom by walking without a cane, walking faster, more active body function and a greater participation. The 3 persons all regretted not having been helped with MSCO before. Not having restrictions during gait, MSCO should be implemented earlier in rehabilitation even if recovery is expected.
Some topics of the MSCO need to be discussed such as Gait analysis and energetic tests could have been added.
The impact of an early application of the MSCO for quadriceps deficiency has been shown to have benefits not only on the activity level but also on the overall cost of rehabilitation.
Significance: The impact of rapid intervention with an MSCO for quadriceps failure or knee instability is manifold. On the one hand we see a faster evolution of the patient during rehabilitation, on the other hand a mentally better condition, and in addition there is a chance of recuperation of muscle strength through correct alignment and therefore stimulation.
Disclosure: Flora works for Basko Healtchare, manufacturer of Swing Phase Lock
References
Zissimopoulos A, Fatone S, Gard S. Biomechanical and energetic effects of a stance control orthotic knee joint. Journal of Rehabilitation Research and Development.2007, 44(4):503-514
Deckers J. Swing Phase Lock plan of treatment. 2015
Use of outcomes to achieve the impossible: Approval of MPK in K2 patients
Andreas Kannenberg, MD (GER)1, PhD; Seth O´Brien, CP, FAAOP(D)2; Pete Freigang, CPO3
1 Otto Bock Healthcare LP, Austin, TX, 2 Artificial Limb Specialists, Phoenix, AZ, 3 Wright&Filippis, Saginaw, MI Email: andreas.kannenberg@ottobock.com
Introduction: The concept of evidence-based medicine and practice combines the clinical expertise of the clinician with the consideration of the best available published scientific evidence and patient values for clinical decision-making. Using outcome measures to identify and demonstrate unmet patient needs, assess the effects of an intervention, and convince a healthcare payer to cover an intervention is part of evidence-based practice. Many CPOs believe that it is impossible to get an MPK approved by Medicare for a K2 patient. We present two case studies that have demonstrated that it is possible to achieve such approval with proper documentation of outcome measures.
Methods: We performed a retrospective chart review of two patients with transfemoral amputation and K2 mobility using non-microprocessor knees (NMPK) and having health insurance through Medicare who underwent trial fittings with the MPK Kenevo for three months. For both trials, Kenevo loaners had been made available by Ottobock.
Results: Patient #1 was a 70-year old male using a 3R62 (multiaxial knee with friction swing control) and a walker. In the 4 weeks prior to the trial fitting, he had experienced 8 stumbles. With the 3R62 knee, he performed the Timed-up-and-go test [TUG] in 26.7 s and had an ABC score of 29, both indicating an increased risk of falling. After 3 months of Kenevo use, he had not experienced any stumbles, performed the TUG in 12.2 s and had an ABC score of 70, both no longer indicating an increased risk of falling. In addition, the PLUS-M T- score had improved from 37.9 with the 3R62 to 49.8 with the Kenevo, clearly exceeding the minimal detectable change (MDC) of 4.5 points and indicating a clinically meaningful improvement in patient-reported mobility. With these documented results, Medicare issued a pre- authorization for a Kenevo and paid the claim. Patient #2 was an 81-year old male using a 3R92 (single axis friction knee with manual lock). He had adopted a very secure forward leaning gait pattern with strong reliance on the walker and extensive use of a wheelchair indoors and outdoors as well as a powered scooter outdoors. After 2 months of Kenevo use, he mostly walked with the walker indoors and considerably reduced his use of the wheelchair. His ABC score had improved from 8.5 to 38, his PLUS-M T-score from 39.0 to 42.9, and his Patient-specific functional scale [PSFS] had considerably improved for 3/5 activities of daily living important to him. With these results, Medicare issued a pre-authorization and paid for a Kenevo.
Discussion: The Medicare Local Coverage Determination (LCD) for Lower Limb Prostheses (L33787) contains the provision that “Coverage [beyond K-level restrictions listed in the respective paragraphs] is extended only if there is sufficient clinical documentation of functional need for the technologic or design feature of a given type of foot/knee. This information must be retained in the treating practitioner's or prosthetist's files.” The presented case studies demonstrate that the knowledgeable use of outcome measures and clinical observation satisfy the requirement for additional documentation.
Conclusion: Knowledgeable use of evidence-based practice and outcome measures yields a great potential to improve the quality of clinical care and business results in O&P.
Disclosure: Andreas Kannenberg is a full-time employee of Otto Bock Healthcare LP. Artificial Limb Specialists and Wright & Filippis are both part of the Ottobock Patient Care network.
References
1. Lajoie Y, Gallagher SP. Arch Gerontol Geriatr 2004;38(1):11-26.
2. Dite W, Temple VA. Arch Phys Med Rehabil 2002; 83(11):1566-1571.
3. Resnik L, Borgia M. Phys Ther 2011;91(4):555-565.
4. Hafner BJ, Morgan SJ, Askew RL, Salem R. J Rehabil Res Dev 2016;53(6):797-812.
AFO shape capture techniques and a weight bearing scanning platform for improved shape capture for high activity ankle-foot orthoses
Richard Miltenberger Jr, CPO, Gary Wall, CPO
rm@mecuris.com Ph: (971) 300-7308 gwall@hanger.com , Ph: (706) 339-9675
Introduction: Proper fit of ankle-foot orthoses (AFO’s) is crucial for the treatment and rehabilitation of patients with foot and ankle disorders. Current 3D scanning methods have limitations in capturing the limb shape, sometimes leading to ill-fitting AFOs that can compromise gait mechanics or result in discomfort.
While many scanning supports are being used in practice, many of these fail to capture an optimal position for the patient. To address this challenge, we are presenting a new weight bearing scanning platform and technique.
Methods: A practitioner may use any scanner that is compatible with our scanning platform. The patient places their foot on the platform fully standing in the correct posture, and the scanner captures the image in a matter of minutes or seconds. The resulting scan is then used to create a digital model of the AFO that can be 3D printed or manufactured using traditional techniques. Software for digital manipulation of the foot and ankle is used to fine tune alignment.
Importance: It is important when fitting high activity AFO’s that the alignment be tuned in such a way that the trajectory of the strut mechanism is appropriate for the patient being fitted. Much in the same way that a prosthetic foot is aligned and using the same principles. However, for AFO’s, this must be done in the shape capture stage, and not the fitting stage. This means that capturing proper alignment at the shape capture stage is crucial for the proper functioning of the AFO is designed for high velocity activities.
Results: Our presentation will cover our methods and discoveries in the area of AFO scanning, as well as digital manipulation, and show results from our fittings using this new method of scanning.
Significance: While the results from using this scanning platform are still incoming, we have begun to address a significant issue in AFO fabrication by providing a weight bearing shape capture and concurrent AFO alignment. Using the correct scanning platform can potentially reduce the time and cost of production while enhancing the patient's experience by providing a more comfortable and precise fit. This provides insight into another area of general concern when it comes to digital design of AFO’s.
Disclosure: Richard Miltenberger is a paid consultant with Mecuris, GmbH. The Mecuris software in some form may be shown during the presentation for illustrative purposes but is not the central concern of this presentation.
Prior work:
1. Tri-planar Scanning Platform. Comb3D https://www.combscan.com/fixture
2. Techmed https://techmed3d.com/product/maid-standard/
3. Biosculptor https://biosculptor.com/?page_id=7579
4. Thuasne https://bmiortho.com/images/3D-Scanner_External-Use.pdf
A digital process to replicate the socket and the foot alignment in below knee running specific prostheses
Andrea Giovanni Cutti1, Maria Grazia Santi2, Francesca Gariboldi2, Fabrizio Giacchi1, Nicola Petrone2, Gregorio Teti1
1 Centro Protesi INAIL, Italy, 2 University of Padova, Italy E-mail: ag.cutti@inail.it
Introduction: A well fit socket and a fine-tuned foot alignment are crucial elements in a running-specific prosthesis to allow Paralympic athletes to express their full competitive potential. For this reason, once a satisfactory socket-foot configuration is established, it would be beneficial to reproduce the same conditions when renewing the prosthesis or to further improve the set-up through small adjustments in a very controlled manner. At present, this requires elaborated bench procedures (e.g. through custom adaptations of transfer devices to accommodate sprinting specific running blades), which are prone to manual error, cumbersome in use and possibly leading to socket damages or destruction.
In this study, we propose an original digital CAD/CAM workflow that allows replicating the full alignment of transtibial and partial foot sprinting prostheses, implementing controlled quantitative adjustments to the configuration, or performing socket adaptations.
Methods: The method requires a digital scanning system, a 3D mesh editing software and a milling machine or 3D printer.
The workflow consists of six phases:
1. Scanning the inner part of the socket and the foot, correctly assembled. Due to scanner limitations, these elements might need to be digitized with different devices or in separate sessions. To allow spatial registration of the two meshes, it is essential to have a common element visible in both scans.
2. Rigid spatial registration between the two scans is performed using geometrical features detected on the common element.
3. If necessary, socket modification or alignment adjustments can be virtually completed in the 3D software taking full advantage of accurate computational geometry tools.
4. A “socket interlocking element” is generated in a 3D software and it is connected to the socket mesh through Boolean operation.
5. An “alignment box” is designed in the 3D software from a full box by Boolean subtraction of the foot and of the socket interlocking element (Figure 1).
6. Fabrication of the socket with its interlocking element and of the “alignment box” using a milling machine or additive manufacturing techniques (Figure 2).
7. The socket is laminated leaving its interlocking element unaffected; the foot connector is screwed on the foot.
8. The socket interlocking elements and the foot are physically positioned in the dedicated housings of the alignment box.
9. A physical connection between foot and socket is created by following the typical procedure of pouring expanded polyurethane (EP) between the two.
Figure 2.
Socket interlocking element (on the left) and alignment box (on the right) obtained with a milling machine.
Results: This procedure was successfully adopted to replicate the alignment of the prostheses of 5 athletes of the Italian Athletics Paralympic Team and proved to be applicable in 4 different types of running blades, namely Ossur Xtreme, Xcel, Xpand and Ottobock Sprinter.
Conclusion: The workflow addresses an unsolved issue in the construction of sprinting specific prosthesis, which can be easy to replicate in O&P services equipped with 3D scanners and a 3D printer or milling machine. The outcome proved to be a reliable method to replicate an existing socket and its alignment relative to the foot, or to perform corrections in a very controlled manner.
Significance: The study suggests an innovative method to overcome the existing difficulties associated to socket-foot alignment replication in sprinting specific below knee prosthesis.
Disclosure: None.
Acknowledgement: The authors kindly acknowledge INAIL and the University of Padova for funding the study through the OLYMPIA Project.
Aether digital platform: The role of cloud-based software to enhance data efficiency in myoelectric hands
Sarra Mullen, CP, LPa and Dhruv Agrawal
a Aether U.S., Chicago, IL, USA, b Aether Biomedical Sp. Z o.o., Poznan, Poland sarra.mullen@aetherbiomedical.com dhruv@aetherbiomedical.com
Introduction: Myoelectric prosthetic technology first became used in rehabilitation centers around the world in the 1980's1. Even though the systems have advanced they are still very uni-directional with no integration into the digital ecosystem. Information is given from patient to device but no data is being transfered back to the patient or the clinician. With the recent advancement with myoelectric hand technology - we have not seen the same level of advancement being achieved at the software level. The objective of this presentation is to demonstrate examples and the powerful role that a cloud-based digital platform incorporating machine learning, AI, and IoT software technology can can play in enhancing myoelectric hand data efficiency.
Methods: Built a cloud-based digital platform software (Aether Digital Platform) with the vision of supporting end-to-end patient journey in a data-driven manner. Components of the digital platform include web-based clinician facing software, mobile patient facing application, multi-articulating myoelectric hand (Zeus,hardware), device usage monitoring device (hardware), which all interact with each other. Sucessful integration makes the digital platform a breeding ground for innovation2
Results: The primary objective that we set out to achieve with the Aether Digital Platform was to 1) provide device usage monitoring data to clinicians and support them in delivering outcome-driven care. 2) support traceability in parameter changes associated with setting up the Zeus multi-articulating myoelectric hand. 3) reduce physical barriers between patients and clinicians and allow interactive changes in the parameters of prosthetic devices, remotely (IoT). The digital platform format promises a number of benefits by encouraging integration among devices allowing for increased continuity of care.
Conculsion: The field of upper extremity myoelectric prosthetics would benefit from adopting a cloud-based digital platform to enhance the continuum of patient care and the possibility of an alternative reoccurring revenue stream.
However, we do not have the current infrastructure for widespread adoption across all myoelectric hand hardware devices - this technology will be advancing and expansion is on the horizon.
Significance: With it's IoT features, Aether Digital Platform focuses on reducing the physical barriers that limits the relationship between clinicians, patients and the myoelectric device. Collecting real-time data associated with usage of the device, remote configuration (synchronous and asynchronous) can decrease non-billable time that a clinician spends with patients, collect data that can be used for insurance justification as well as alternative methods of recurring payment.
Disclosure: The authors disclose a relationship with Aether Biomedical/Aether U.S.
References
1. Behrend, Caleb, et al. "Update on advances in upper extremity prosthetics." The Journal of hand surgery 36.10 (2011): 1711-1717.
2. Yoo, Y., Boland, R. J., Lyytinen, K., & Majchrzak, A. "Organizing for innovation in the digitized world." Organization Science, 23(5),(2012): 1398-1408.
Benefits of a simulation model for digital manufacturing in the O&P industry
Ylli Binakaj1, Eva Hildsberg2
1 Project Lead Research project SIGMA3D and Product Owner Mecuris3D Creator at Mecuris GmbH, 2 Usability Expert and Product Owner Mecuris Solution Platform at Mecuris GmbH
Introduction: 3D printing as a new manufacturing process in the O&P business not only brings new possibilities within the design process but also new materials to which there is still little experience. This knowledge about the materials used so far, such as carbon fiber or plastics, has been built up over many decades. To compensate this lack of knowledge, it requires time, money and resources to test the aids beforehand, which is difficult to do in day-to-day business.
With the help of finite element analysis, we want to simulate in advance the behavior of a digitally designed hand orthosis before manufacturing in 3D printing processes and display the result to the user via an interface.
Methods: First, a physical test stand was set up to verify the method of testing and to generate data for the simulation regarding the material behavior as well as the acting forces and the bending on the orthosis.
These results were then used to build a simulation model. An iterative improvement of the simulation model took place based on the results of the physical test bench. We used a visual measurement technique with a GOM measurement system to accurately analyze the deformations of the orthosis during force application to improve the simulation model continuously.
Results: In step 1 a survey with 145 companies in the assistive technology industry participating confirms for the project's need:
• About 80% of custom device manufacturers are in favor of automatic creation of various components of documentation.
• Nearly every second company lacks human resources to implement the changed requirements
• One in five manufacturers lacks financial resources.
In step 2 a prototype of a simulation model for generic hand orthosis designs showing the loading condition of a digitally tested aid is being created.
In step 3 we generate an overview of the validity and utility of simulation models under current regulatories. Embedding the simulation model into the digital value chain enables a fully comprehensive processing of the scan to the orthosis.
For step 2 and 3, concrete results can only be delivered after the publication of the project (02/2023).
Conclusion: Digital manufacturing comes with certain hurdels. In this regard simulation can not only have a cost-reducing effect on testing but also helps create necessary documentation to fulfill physical tests is crucial for valid results and a high validity of the simulation model. The implementation in digital value chains and the upstream and downstream steps are decisive for how good the user experience is and whether the digital production of aids can succeed.
Speakers: Benjamin Groeschel, Head of Sales (Masters of Mechanical Engineering) bg@mecuris.com Tel +0114989200057-320 US toll free: (+1) 888 683 4886
Bianca Weber, COO at Mecuris (Bachelor of Medical Engineering. MBA & Eng. Degree Business Admin.) bw@mecuris.com
Tel +0114989200057-320
US toll free: (+1) 888 683 4886
Going digital with digits
Chris Baschuk, MPO, CPO, FAAOP(D)
Director of Clinical Services, Point Designs, LLC chris@pointdesignsllc.com
This symposium for the O&P Digital Education Program is meant to provide participants with an overview of the history of partial hand prosthetic rehabilitation including the technologies and techniques that have historically been utilized. This background will then be juxtaposed with new digital fabrication processes that are now beginning to be utilized in this space. Specifically, it will highlight how Point Designs has developed a digital pathway to partial hand cFab services. This pathway reduces waste and has transformed what historically has been a challenging fabrication process for most facilities into a streamlined, guided process. This process integrates 3D scanning, 3D modeling, 3D design reviews, and additively manufactured diagnostic and definitive sockets. A central component of this digital process is the virtual consultations with clinicians where different alignments can be reviewed digitally and approved. During these digital alignment consultations different sizes of fingers can be quickly interchanged allowing the clinician to choose the correct size digits without having to ship multiple sizes back and forth. By integrating these digital components, Point Designs has increased the accessibility of highly functional partial hand prostheses for a patient population that has historically been underserved. Jeff Soelberg, an individual with a partial hand amputation, will share his experience of being fit with a prosthesis designed through this digital process and the improved outcomes that he has experienced as a direct result of his additively manufactured prosthesis.
Outline:
- • Historical partial hand solutions
- o Robin Aids
- o Opposition posts
- o Silicone restorations
- o Handi-hook
- • Historical partial hand fabrication techniques:
- o Silicone impression
- o Plaster modifications
- o Blister form diagnostic socket
- o Bivalve duplication technique
- o Jigs for partial hand digit transfer
- o Lamination layup techniques
- • Digital transformation:
- o Shape capture techniques
- o 3D scanning
- o Model rectification
- ⁃ Software
- • Geomagic Freeform
- • nTopology
- o Digital alignment transfer
- o Socket design dFam
- • Guiding principles of partial hand socket design:
- o No more leg sockets on hands
- o Palmar platform
- o Thenar/hypothenar hooks
- o Metacarpal cap
- o Dorsal desert
- • Improved patient outcomes because of additive manufacturing
- o Lighter socket
- o More flexible
- o Lower profile
- o Increased wear time/utilization
- o Reproducible
- o Infinite customization
Multi-lingual evaluation of patient outcomes using mobile app technology
David A. Boone, BSPO, MPH, PhD, Jung Kim, Jessica Garries, MS, Sarah R. Chang, PhD
Orthocare Innovations, LLC, WA, USA dboone@orthocareinnovations.com
Introduction: The number of individuals in the U.S. that speak a language other than English continues to rise1 and, language barriers are a contributing factor in the increasing health disparities experienced by minority populations2. The language barrier can make it difficult for a patient to fully convey their health concerns to their provider and for the provider to understand the patient’s needs. Further, health care providers are increasingly using patient-reported outcome measures (PROMs) as a routine part of clinical care, but the use and collection of PROMs may be limited in patient populations that prefer to speak a language other than English.
Comprehension of the questions in the PROMs can be challenging if health literacy or reading skills are low, resulting in inaccurate responses or inability to complete the measures. The purpose of this project was to develop an outcome measures mobile app that switches between languages in real-time for administering and interpreting results, to support orthotic and prosthetic (O&P) practitioners in communicating via a patient’s preferred language.
Methods: Validated outcome measures that are typically in paper format were identified and digitally transformed for inclusion in a mobile app. Features were implemented in the app to display each question with response options for an individual outcome measure, automatically calculate the resulting score, and generate a PDF report of the results. Language switching features included in the app allow the patient to select their preferred language to complete the outcome measure. Once the patient completes the outcome measure, the results can be reviewed in the health care provider’s preferred language.
Results: The Clinical Outcome Measures Electronic Toolkit (COMET) mobile app allows users to easily select the appropriate measure for a patient to complete and administer the test (Figure 1). Patients can have increased comprehension and confidence when completing PROMs in their preferred language. The app can be used in English or Spanish. At completion of the measure, a PDF can be exported in English or Spanish that documents the patient’s responses and can be included in the electronic medical record or shared with the patient. The COMET mobile app has been released to iOS and Android App Stores for O&P clinics to download and use.
Figure 1.
Mobile app displayed in Spanish (left) for patient- reported outcome measures and PDF report in English (right).
Discussion and conclusion: COMET can be used to measure and immediately analyze patients’ outcome measure data to inform clinical decisions. The mobile app is designed to be easily extended to other languages when valid translations are available. Furthermore, the mobile app can instantly switch between patient-preferred and provider-preferred languages to reduce communication barriers and increase understanding between patients and providers.
Significance: By enabling patients to complete outcome measures in their preferred non-English language, English-speaking providers can take actionable treatment steps based on the evidence to appropriately address the specific health needs of each individual, including those in minority populations.
Disclosure: The authors are employees of Orthocare Innovations, LLC.
Acknowledgements: This work was supported by Orthocare Innovations, COPL, AOPA, and the National Institute on Minority Health and Health Disparities (Grant# R43MD018240).
References
1. U.S. Census Bureau: S1601: Language Spoken at Home. 2019 American Community Survey 1-Year Estimates (Accessed March 31, 2022).
2. Timmins CL. J Midwifery Womens Health. 2002;47:80– 96.
Improving quality of life: Getting comfortable with additive manufacturing
Kevin Yap
kevin.yap@endeavor3d.com , Office: 404 383 1170
The O&P industry revolves around mass customization, from specialized insoles tailored to the patient’s feet to AFOs which are produced in varying batches. We are not robots and unfortunately, every human being is unique and there is no one size fits all solution to enable us to get to the comfort levels we seek. Current mass manufacturing methods typically deal in large volumes to reduce cost and lead times without catering to unique requirements.
Fortunately, Additive Manufacturing is fantastic for high mix-low volume production, a perfect fit for the ever-changing needs of patients. With an ever- expanding range of materials, colors and designs, AM is able to take on the unique requirements of various individuals to produce the right support they require.
AM has grown by leaps and bounds over the last few years. Coupled with 3D scanning and new post processing technologies, we are now able to accurately scan a patient and produce the right support the first time. This greatly improves patient care and cuts down on cost and lead time from unnecessary waste.
With digital designs of patients, minor modifications can be made as the patient’s body changes over time. This is especially so in young children who outgrow their Orthotics or Prosthetics rapidly and that results in exorbitant costs to treat the children, oftentimes resulting in neglect.
Additive Manufacturing is not a shortcut or a substitute for current manufacturing methods, but a complement to existing ones to improve everyone’s quality of life, quickly.
Contact: Kevin Yap
Technical Sales Engineer Email: kevin.yap@endeavor3d.com Office: 404 383 1170 Mobile: 347 217 7143
Endeavor 3D
One Endeavor Way Douglasville, GA 30134
Measurement of Flexible Inner Socket Wall Thickness: A Comparison of Fabrication Techniques
Santini M1, Smith SD1, Geary P1, Olpin C1, Berke GM1,2,3
1. Medical Creations Inc, Denver CO, 2. Adjunct Clinical Associate Professor, Stanford University, Department of Orthopaedic Surgery, Palo Alto CA, 3. Berke Prosthetics/ Orthotics, San Mateo CA, 4. Rebound Prosthetics, Denver CO.
Introduction: Flexible inner sockets (FIS) have been used in combination with prosthetic sockets for many years. The FIS is provided to improve comfort for the patient while adding more adjustability to the socket for the practitioner. To create an FIS, blister-forming and drape-forming techniques are commonly used for trans-tibial sockets. These techniques can result in large variabilities in wall thickness during the forming process. Measuring the wall thickness is not clinically performed and wall thickness variability is not understood. Having uniform wall thickness is desirable clinically due to improved fit and durability. The purpose of this study was to develop a measurement technique for FIS wall thickness and compare the wall thickness of FIS samples produced with different forming techniques.
Methods: Blister-formed EVA, Drape-formed EVA, and the Xtremity FIS were compared. Three different limb models were selected to form each type of FIS. Three samples per group were collected. The limb model profiles are conical, standard, and narrow. An experienced technician formed all blister-forming and drape-forming EVAs. Preliminary data of two limb profiles and two samples per group are reported. The full study will be completed in 30 days.
Forming the FIS Samples: A 3/8” x 16” x 16” Duraflex EVA was used for blister- forming, a 5/32” x 16” x 16” Streifeneder EVA was used for drape-forming, and a custom Xtremity FIS preform was used for the Xtremity FIS. Each material was heated in accordance with the manufacturers’ recommendation and formed over the plaster model. Vacuum was applied. After the recommended time under vacuum, the finial trim lines were established, and each FIS was finished.
Measuring FIS Wall Thickness: The finished flexible inner sockets were sectioned down the anterior, medial, lateral, and posterior portions of the FIS. The sections were cut from predetermined marks on the positive limb model for consistency. Practitioners take their circumference measurements in 1-inch increments for modifications, so a similar technique was performed for this study. 1- inch increments were marked along the cross-section of the FIS from the distal end to the proximal trim lines. Wall thickness measurements were taken at each 1-inch increment with calibrated calipers. The wall thickness measurements were recorded for each location. The thickness range was reported for all the forming techniques. Table 1
Table 1.
Wall thickness range at each measured location.
| Average Wall Thickness Range (mm) | ||||
|---|---|---|---|---|
| FIS Type | Anterior | Medial | Lateral | Posterior |
| Blister-Formed FIS | 2.40 | 2.16 | 2.35 | 2.60 |
| Drape-Formed FIS | 1.84 | 1.92 | 1.86 | 0.66 |
| Xtremity Formed FIS | 0.60 | 0.95 | 0.48 | 0.30 |
Results: Preliminary results show the FIS systems have variability in wall thickness in the finished FIS systems. The max wall thickness variability in the blister-formed and drape-formed EVA FIS was over double the Xtremity FIS. The Xtremity FIS system has a wall thickness variation of less than 1 mm. Table 2
Table 2.
Maximum FIS wall thickness range for each forming technique.
| FIS Type | Maximum Wall Thickness Range |
|---|---|
| Blister-Formed FIS | 2.58 mm |
| Drape-Formed FIS | 2.01 mm |
| Xtremity FIS | 0.95 mm |
Discussion & conclusion: The study demonstrates that there is thickness variability across all fabrication techniques and products., and some fabrication techniques produce less variability than others. A practitioner needs to be aware of this when selecting an FIS forming process.
A more uniform wall thickness FIS translates to less bulk or thinning for the amputee wearing the FIS. The uniform wall thickness provides consistency in cushioning and comfort throughout the socket. If a practitioner or technician wants a more uniform FIS, grinding the FIS is required to remove bulk. Certain techniques do not need extra fabrication time to achieve a more uniform FIS.
Preliminary data has been reported in this abstract, and the full study will be completed in the next 30 days.
Medium-term outcomes of transfemoral osseointegration in association with total hip replacement
Jason Hoellwarth1, Atiya Oomatia,1,2,3, Munjed Al Muderis1,2,3,4,5
1 Osseointegration Group of Australia, Australia, 2 Macquarie University, Australia, 3 The University of Sydney, Australia, 4 Macquarie University Hospital, Sydney, Australia, 5 Notre Dame University, Australia atiya@osseointegrationaustralia.com.au
Purpose: Osseointegration is a novel approach for the treatment and rehabilitation of amputees that can eliminate the problems associated with socket prostheses. Transfemoral osseointegration (TFOI) for amputees has substantial literature proving superior quality of life and mobility versus a socketed prosthesis. Some amputees have hip arthritis that would be relieved by a total hip replacement (THR). No other group has reported performing a THR in association with TFOI (THR+TFOI). We report the outcomes of eight patients who had THR+TFOI, followed for an average 5.2 years.
Methods: Our osseointegration registry was retrospectively reviewed to identify all patients who had TFOI and also had THR, performed at least two years prior. Six patients had TFOI then THR, one simultaneous, one THR then TFOI. All constructs were in continuity from hip to prosthetic limb. Outcomes were: complications prompting surgical intervention, and changes in subjective hip pain, K- level, daily prosthesis wear hours, Questionnaire for Persons with a Transfemoral Amputation (QTFA), and Short Form 36 (SF36). All patients had clinical follow-up, but one patient did not have complete mobility and quality of life survey data at both time periods.
Results: Four (50%) were male, average age 52.7±14.8 years. Three patients (38%) had amputation for trauma, three for osteosarcoma, one each (13%) infected total knee and persistent infection after deformity surgery. One patient died one year after THR+TOFA from subsequently diagnosed pancreatic cancer. One patient had superficial debridement for infection with implant retention after five years. No implants were removed, no fractures occurred. All patients reported severe hip pain preoperatively versus full relief of hip pain afterwards. K-level improved from 0/8=0% K>2 (six were wheelchair-bound) to 5/8=63% (p=.026). At least 8 hours of prosthesis wear was reported by 2/7=29% before TOFA vs 5/7=71% after (p=.286). The QTFA improved in all categories, but not significantly: Global (40.0±21.6 vs 60.0±10.9, p=.136), Problem (50.2±33.2 vs 15.4±8.4, p=.079), and Mobility (35.9±26.8 vs 58.3±30.7, p=.150). The SF36 also improved minimally and not significantly: Mental (53.6±12.0 vs 54.7±4.6, p=.849) and Physical (32.5±10.9 vs 36.3±11.2, p=.634).
Conclusion: THR+TFOI is a successful reconstruction option for amputees who desire relief from severe pain related to hip joint degeneration, and also the opportunity for improved mobility and quality of life that TFOI typically confers. In our cohort, the procedure proved safe: no associated deaths, no removals, one soft tissue debridement. Mobility improved markedly. Quality of life improved, but not to significant thresholds as measured by the surveys. THR+TFOI appears safe and reasonable to offer to transfemoral amputees with painful hip joint degeneration.
Signifiance: The findings of the current study will impact clinical decision-making regarding utilization of modern intramedullary prosthesis. The current study is the first to present long term data on the potential benefits of treating patients with osseointegration combined with hip replacement.
Disclosure: Dr. Al Muderis consults for and receives royalties from companies including: Osseointegration International Pty Ltd (Australia), Osseo-PL Inc (USA), Osseo-PL GmbH (Germany), AQ Implants GmbH (Germany) and Permedica S.P.A (Italy).
Patient education for immediate post-amputation recovery
Karli Kochman, CFo1 Max Hurwitz, DO2 Goeran Fiedler, PhD1
1 University of Pittsburgh Prosthetics and Orthotics, 2 University of Pittsburgh School of Medicine, UPMC Department of Physical Medicine and Rehabilitation karlikochman@gmail.com
Introduction or purpose: An amputation is a life changing event both physically and mentally, and the rehabilitation process is complex and lengthy. Knowing the milestones and healthcare professionals involved, is vital to a person’s success after an amputation.
Patient education is an important tool that conveys essential information from the healthcare team and is demonstrated to improve patient outcomes1 but current patient education content and distribution is not standardized following an ampuation.2 We aimed to improve patient understanding of the post- amputation recovery timeline through formal education material.
Methods: A literature review was conducted to gauge current patient education for post-operative amputees and best practices for educational materials. The search demonstrated the lack of standardized patient education for people with new limb loss. It also revealed “chunked” information such as bullet points or an infographic is an ideal method to present educational intervention.3
In response, an infographic (Figure 1) was created to identify post-operative milestones, time estimates, and healthcare professionals involved in the pre- prosthetic stage. It depicts post-operative recovery as a collaborative ongoing process. The Infographics were distributed to new amputees at their first post- operative encounter with a prosthetic clinician, and surveys with Likert scale response options were used to collect participant-reported feedback.
Figure 1.
Infographic.
Survey results were analyzed by quantifying the categorical responses and determining the attitude to each prompt.
Results: Survey results: Twenty-four infographics were distributed, and seven completed surveys were collected. All participants agreed or strongly agreed they had learned about the milestones in their recovery (Figure 2). Time-based questions received few ‘unsure’ and ‘disagree’ responses. A question regarding confidence in their knowledge about their recovery received a single ‘unsure’ response.
Figure 2.
Users' agreement on statements (1-5 scale).
Prosthetic clinicians’ feedback about the infographic intervention: Feedback included that the infographic was a “great deliverable. You can make it patient specific and “write notes, names, and appointments directly on the sheet.” Several clinicians commented that the infographic was a “…good reminder. Like, you could just put it on the fridge.” Most clinicians agreed that it was a good depiction of the rehabilitation as an ongoing process. Recommended improvement included to differentiate inpatient and outpatient physical therapy.
Conclusion: The patient education infographic was positively received by new amputees and clinicians. It is a tool that can be used as a reference for people with new limb loss to keep track of their progress through recovery and the roles of their healthcare team.
Significance: Measures to improve outcomes after an amputation should include effective communication materials for the post-operative period.
Acknowledgements: University of Pittsburgh, School of Health Rehabilitation Sciences, Prosthetics and Orthotics. Elizur Corporation, University of Pittsburgh Medical Center, Physical Medicine and Rehabilitation.
References
1. Heng H, et al. BMC Geriatrics 2020; 20(1)
2. Farrokhi S, et al. Mil Med. 2019;184(11-12
3. Tetlan L, et al. Vis Lang 2016
Pre-determining pectus bracing outcome
Gez Bowman CO, MBAPO
Valley Orthopedic Technology, Los Angeles, CA gdbowman@yahoo.com
Introduction: Pectus Carinatum (PC) bracing is a relatively new concept. Because it is a pediatric bracing solution and relates to the torso, patients are often referred to orthotists who specialize in scoliosis bracing. As a result, often the same bracing wear time schedules are used as that of scoliosis bracing and these scoliosis brace wear schedules vary considerably among the orthotic community. However, PC bracing differs from scoliosis bracing in complexity, correctability, duration of need and risk of recurrence. Based upon the author’s experience with different wearing schedules, obvious differences have been noted in the outcome achieved.
Methods: As a brace with simpler biomechanical principles, the PC bracing parameters that determine outcome are more easily determined and measured. By first determining the Max Outcome Potential (MOP) and then applying the Average Daily Wear time (ADW) a formula is presented to pre-determine the final outcome of PC Bracing and the duration of time needed to achieve the MOP. Given this information, this then allows for the end user to adjust their ADW to achieve their MOP.
Results: The author’s clinical experience suggests full-time brace wear results in both improved correction and reduced treatment duration as compared to part-time bracing.
The MOP and ADW are now routinely used in the authors clinic to present to patients the expected outcome of treatment and treatment duration. It has proven to act as a motivator to encourage compliance with recommended brace wear schedules.
Conclusion: The orthotic community should consider adopting full-time brace wear schedules for PC bracing to maximize outcomes. Use of the ADW/MOP formula when evaluating patients allows the orthotist to present mathematical reasoning for the differences in eventual bracing outcome depending on the wear schedule adopted.
Racial bias in orthotics and prosthetics
McDonald CL,1 Brinkmann J,2 Mitsou L,3 Hoffman-Finitsis A,3 Bretl S4
University of Washington, Seattle, WA 1 , Northwestern University, Chicago, IL 2 , University of Hartford, West Hartford, CT 3 , Alabama State University, Montgomery, AL 4
Introduction: A growing body of evidence details racial disparities in prosthetics and orthotics access and outcomes.1-2 To reduce racial health disparities among minortized groups, we must identify and address the underlying causes of inequity. Structural, institutional, and interpersonal racism have been associated with disparate outcomes across health care.3 Interpersonal racism occurs between individuals when racial beliefs affect interactions. Racial beliefs include both implicit and explicit biases, which have been found to influence diagnosis and treatment decisions.4 Biases are well documented in many health professions but have not yet been explored in orthotics and prosthetics (O&P). To assess the current state of racial bias in O&P, we conducted a cross-sectional survey of implicit and explicit biases among O&P clinicians, educators, and students.
Methods: Sample: All current US O&P educators, students, and BOC certified clinicians were asked to participate. A random sample of ABC certified clinicians were invited.
Study design: Cross-sectional digital survey. An institutional review board reviewed and deemed all study procedures to be exempt.
Eligibility criteria: 18 years of age or older, proficient in English, and self-reported role as a O&P clinician, resident, educator, or student.
Procedures: Each participant was self-screened for eligibility. If eligible, the participant was directed to the survey for their reported role in O&P. The survey included demographic, work or education questions, and explicit racial preference questions. Participants then completed the Race Implicit Association Test.
Analysis: Participants were grouped by self-reported role. Descriptive statistics were used to characterize demographic and work or education related information and racial preferences for each group. The IAT effect was calculated as the standardized difference in mean response time on two conditions of the IAT, presented as the IAT D score.5 Effect size for implicit bias was calculated by role, race/ethnicity, and gender groups. Spearman’s rank-order correlation was used to assess correlation between implicit and explicit racial bias. Group level comparisons of IAT scores were made using independent t-tests and Analysis of Variance as appropriate.
Results: A sample of 454 individuals completed the survey (136 students, 24 educators, 294 clinicians/residents). Many participants (255) were screened out due to ineligibility or the survey being closed. Eighty-seven individuals began the survey but did not complete it.
Overall, study participants were fairly young (36% between 25-34 yrs), identified as women (52%), white (80%), and had attained a master’s degree (46%, excluding current students). Compared to the general population, the O&P sample had a similar distribution of implicit racial preference (Figure 1). No significant difference was found between role groups (clinician/residents, students, educators). However, statistically significant differences were found by gender (men vs. women), and race (Black verus non-Black and non-Hispanic White versus not non-Hispanic White). Women, Black individuals and those who did not identify as non-Hispanic White had significantly less implicit racial bias.
Figure 1.
Comparison of implicit racial bias results between the general population and the O&P sample.
Most participants reported no explicit racial preference (81% clinicians, 80% students, 71% educators). Those who did report preference, tended to report slight preference for White people (11% clinicians, 14% students, 25% educators) or slight preference for Black people (5% clincians, 2% students, 4% educators).
Conclusion: Study results suggest O&P providers, educators and students have similar implicit racial bias as the general population. However, women and minority racial and ethinic groups (Black people and those who are not non-Hispanic White) have less implicit racial bias against Black individuals. Conversely, most study participants do not report explicit racial preference. Further research should examine the complex relationship between implicit bias, explicit bias, clinician actions and O&P patient outcomes.
Significance: Implicit bias training for O&P professionals through active learning exercises and self-reflection may be considered to address unconscious bias that may influence clinical decisions. Study data also support the need for active recruitment of individuals with diverse backgrounds into O&P clinical practice and education.
Disclosure: The authors have no conflict of interest.
Acknowledgments: This work was funded by an Orthotics and Prosthetics Foundation for Education and Research grant.
References
1. Resnik L. J Rehabil Res Dev. 2015;52(6):641-52.
2. McDonald CL. Disabil Rehabil. Published online Feb. 27, 2023:1-7.
3. Paradies Y. PLoS ONE 2015;10(9):e0138511
4. FitzGerald C. BMC Medical Ethics. 2017;18:19.
5. Greenwald A. J Pers Soc Psychol. 2003;85(2):197-216.
Technology-based assessment of transtibial prosthesis user’s functionality and comparison with traditional methods – a case study
Castro, M. MBE1, Carvalho, V. BSPO, CPO1, Antunes, I. MBE1
1 Adapttech, biomed@adapttech.eu
Purpose: In this abstract, the functional level of a transtibial prosthesis user is evaluated through a technological approach. For this assessment, a pedometer was worn daily, collecting step data-derived metrics, which, together with a small set of clinical information, could derive a more objective K-level than the one obtained through standard approaches.
Not only this work aims to demonstrate the repeatability and reliability of this type of technology for functional assessment, but also to highlight the fallibility of the traditional mobility level rating methods, as they do not measure capacity of performing activities of daily life in real-life conditions.
Implementation: The patient is a 63-year-old woman and has been a right transtibial amputee for the past 40 years. She has worn a prosthesis ever since. Additionally, she has a hip prosthesis on the contralateral leg. She is clinically rated as a K-2 and her prosthetic components are suitable for her functional level. She does not require ambulation aids, even though she lives in an area with cobblestone streets and uneven terrain.
Two evaluations of her functional outcomes were performed with a six-month interval in between. Evaluations comprised the retrieval of Outcome Measures in the clinic, but also the daily use, for a 9- day-period, of an activity monitor, which counts steps during community ambulation. This step count was not only used to derive metrics about the patient’s performance, but also to identify 2-minute gait bouts, which we refer to as blind 2 Minute Walk Tests.
Results: Her first evaluation occurred in August, a month marked by her town’s popular festivities, in which she participated. Six months later, in February, no major events took place, and the patient would only follow her daily routines. These involved long walks along her town’s boardwalk. A summary of some of the metrics acquired through pedometer data during the evaluation periods is present in Table 1.
Through the step data acquired daily, we could see that her average and maximum daily step count decreased during the second assessment, in comparison to the first one. Although there are few recommendations about amputees’ optimal step count, the studies reviewed in 1 show an average number of steps per day for transtibial amputees of 5929±3047, which the patient surpasses by, on average, 45.6%.
Her cadence values, in the two evaluations, match published reference values 2, which present a mean reference value for transtibial amputees of 103.78±9.48 steps/min. In fact, her best achieved cadences are typical of K-4 patients, according to existing literature3.
Also, when performing a 2-Minute Walk Test in the clinic, the patient could cover 121.7 meters in the first evaluation and 117 meters in the second. However, when these parameters were blindly obtained during the evaluation period, the patient covered, in average, 12.9% less ground in two minutes of continuous walking. Her unawareness about the collection of this outcome measure allowed it to be unconstrained by the “white-coat effect”. It is worth noting that automated tests are unaware of short pauses, turns taken, different terrains, or presence of obstacles during their administration, which can negatively influence the patient’s average reported performance. This can explain the results presented in Table 1. In terms of gait intensity, defined thresholds4 place the patient in a high intensity rank (above 80 steps/min) during 37.1% of the time in the first evaluation, and 43.8% in the second. This reveals the patient’s capacity of reaching a high cadence and being able to vary it, which is key in the assessment of a K- level. Daily monitoring provided unique insight, as the patient's clinic visits showed little variability in gait speed and medium intensity cadence.
Table 1.
Sample of pedometer-collected data in the two evaluation periods.
| Pedometer-collected data (9 days) | First Evaluation | Second Evaluation |
|---|---|---|
| Average daily steps | 8995±3046 | 8274±2263 |
| Maximum daily steps | 14,662 | 11,858 |
| Average best cadence of day (steps/min) | 97.8±2.7 | 101.2±2.4 |
| Maximum cadence (steps/min) | 102 | 106 |
| Maximum 2MWT (meters) | 103 | 105 |
| Calculated K-level4 | 3.7 | 3.8 |
Conclusion: On the two evaluations, a K-level calculation, which weighted the clinical opinion with the pedometer-based evaluation,4 rated the patient above 3.5. These values do not agree with the K- level of 2 that had been previously attributed to her, based on in-clinic tests such as the AMPPRO and the PLUS-M™. The calculated K-level was largely influenced by the high number of steps taken per day during the patient’s daily life, which positively impacted her energy expenditure, and by her potential to vary cadence.
In conclusion, this case study supports the need for real-life monitoring of prosthetic users through automated methods.
References
1. Wong, C. K. et al. Phys Ther 101, (2021).
2. Schmid-Zalaudek, K. et al. J Clin Med 11, 2683 (2022). 3.Godfrey, et al. JPO Journal of Prosthetics and Orthotics 30, 20–30 (2018).
4.Orendurff, M. S. et al. J Rehabil Assist Technol Eng 3, 205566831663631 (2016).
Transcutaneous osseointeration for patients with a history of burn trauma
Amanullah Haidari1; Jason Hoellworth1, Atiya Oomatia,1,2, Munjed Al Muderis1,2,3,4,5
1 Osseointegration Group of Australia, Australia, 2 The University of Sydney, Australia, 3 Macquarie University Hospital, Sydney, Australia, 4 Macquarie University, Australia, 5 Notre Dame University, Australia. atiya@osseointegrationaustralia.com.au
Purpose: Patients who have had lower limb amputation due to severe burn trauma often struggle with traditional socket prosthesis (TSP) wear even more than typical amputees because the socket irritates the compromised skin. This leads to poor mobility and quality of life (QOL). Transcutaneous osseointegration has been proven to be a safe and effective alternative to TSP rehabilitation which usually provides superior mobility and QOL. However, the compatibility of osseointegration with burned skin is unknown. This study answers the following question: what are the changes in mobility, QOL, and complications experienced for burned-related amputees following osseointegration?
Methods: A retrospective review of our osseointegration registry identified five patients whose amputation was performed due to burn trauma: one unilateral transfemoral amputation (TFA), one unilateral transtibial amputation (TTA), one bilateral TFA, and two bilateral TTA. Analysis was performed of their preoperative and postoperative mobility (daily prosthesis wear hours, K-level, timed up and go (TUG), and 6 minute walk test (6MWT)) and QOL metrics (Questionnaire for Persons with a Transfemoral Amputation (QTFA) and Short Form 36 (SF36)). Complications and benefits specific to burn amputees were also noted. Means were compared using Student’s t-test and frequencies using Fisher’s Exact test with significance set as p<0.05.
Results: Patients who wore their prosthesis >12 hours daily improved from 0/2=0% vs 3/4=75% (p=0.400), and patients with a K-level of at least 2 improved from 0/3=0% vs 3/3=100% (p=0.100). Patients with a TUG of >50 improved from 0/4=0% vs 2/3=66% (p=0.143). QTFA global scores improved from 45.83±29.47 vs 54.17±30.81 (p=0.768) though QTFA mobility score worsened from 55.28±44.87 (p=0.711). QTFA problem score improved from 26.66±10 vs 19.79±13.35 (p=0.563). SF36 PCS improved from 27.09±10.39 vs 32.53±16.92 (p=0.647) and SF36 MCS improved from 47.81±13.27 vs 44.74±16.13 (p=0.800). Four patients had complications prompting operative intervention this includes debridement for infection and removal of implant. A specific benefit of osseointegration was noted for two patients who had flexion contractures of their hips and knees, respectively, while using a TSP, but which markedly improved following osseointegration.
Conclusion: All of the patients specifically reported substantial improvement of their burned skin following the elimination of a socket prosthesis. Transcutaneous osseointegration is a safe and effective rehabilitation option for amputees with a history of burn trauma. No patients have had skin breakdown or other skin issues associated with being an osseointegrated amputee. Mobility and quality of life have improved, though not significantly.
Although infection can occur, revision osseointegration can restore the mobility and QOL benefits following the eradication of infection.
Signifiance: The findings of the current study will impact clinical decision-making regarding utilization of modern intramedullary prosthesis. The current study is the first to present mid- term data on the potential benefits of treating patients with osseointegration who are unable to wear socket prosthesis due to skin breakdown and sensitivity.
Disclosure: Dr. Al Muderis consults for and receives royalties from companies including: Osseointegration International Pty Ltd (Australia), Osseo-PL Inc (USA), Osseo-PL GmbH (Germany), AQ Implants GmbH (Germany) and Permedica S.P.A (Italy).
Transcutaneous osseointegration reconstruction for wheelchair bound transfemoral amputees (K0 Level)
Kevin Tetsworth1,2, Atiya Oomatia,1,3,4, Munjed Al Muderis1,2,3,4,5
1 Osseointegration Group of Australia, Australia, 2 Macquarie University Hospital, Sydney, Australia, 3 The University of Sydney, Australia, 4 Macquarie University, Australia, 5 Notre Dame University, Australia atiya@osseointegrationaustralia.com.au
Purpose: Traditional socket prosthesis (TSP) rehabilitation for amputees is associated with substantial dissatisfaction due to poor mobility and pain from soft tissue squeezing. Osseointegration (OI), the implantation of a transcutaneous bone-anchored metal nail which attaches to a prosthetic limb, eliminates skin compression and prosthesis fit issues, providing superior mobility and quality of life (QOL) for most amputees versus TSP. The potential for OI to benefit patients with exceptionally poor mobility is understudied. To address this knowledge gap, this project investigated the mobility and QOL changes, along with postoperative complications, for wheelchair bound (Medicare K-Level 0) transfemoral amputees.
Methods: A retrospective chart review was performed to identify transfemoral amputees who presented with wheelchair-bound mobility (K0) and had at least five years of post-osseointegration follow-up. Outcome measures included changes in mobility (K- level, daily prosthesis wear hours, Timed Up and Go (TUG), 6 minute walk test (6MWT)) and QOL (Questionnaire for persons with a Transfemoral Amputation (QTFA); Short Form Health Survey 36 (SF36). Adverse events recorded included debridement for infection, implant revision surgery, fractures, and implant failures. Means were compared using Student’s t-test and frequencies were compared using Fisher’s Exact Test; significance was set at p<0.05.
Results: 9 patients (2 male 7 female) with mean age 48.2±7.7 (range 34-59) years were included. All results are compared as preoperative vs postoperative values. Statistically significant improvement occurred for all mobility metrics. The proportion of patients achieving K-level >2 improved from 0/9=0% to [9/9=100%], p<0.001. The 6MWT improved from 0±0 to 320.65±57 meters (p<0.001). The TUG improved from incapable to 10.68±2.7 seconds (p<0.001). Statistically significant QOL metrics included QTFA global score (33.33±31 vs 68.52±21, p=0.039), SF36 physical component score (30.03±6.3 vs 42.34±12, p=0.023) and the SF36 mental component score (47.89±8.8 vs 51.95±10.4, p=0.332). Six patients required operative intervention to address complications. Five developed infections: three had debridement, and 2 required implant removal and reimplantation. One patient developed aseptic loosening and periprosthetic fracture managed with removal and re-implantation. Those requiring operative intervention showed lower 6MWT (311.8±46.5 vs 338.46±70.33, p=0.657), Q-TFA global (62.50±14.23 vs 80.56±27.50, p=0.456), SF36 physical (40.92±9.98 vs 45.17±13.97, p=0.030) and mental (49.12±11.17 vs 57.62±5.41, p=0.220) scores compared to patients without complications requiring operative intervention.
Conclusion: Osseointegration does confer significant sustained mobility and quality of life improvement for wheelchair bound transfemoral amputees. All 9 K0 patients had statistically improved mobility and QOL after osseointegrated reconstruction. This supports osseointegration as an effective rapid and long term rehabilitation alternative for patients who have the neurologic and muscular capacity to walk but are unable due to issues related to their TSP.
Signifiance: The findings of the current study will impact clinical decision-making regarding utilization of modern intramedullary prosthesis. The current study is the first to present long term data on the potential benefits of treating patients with osseointegration.
Disclosure: Dr. Al Muderis consults for and receives royalties from companies including: Osseointegration International Pty Ltd (Australia), Osseo-PL Inc (USA), Osseo-PL GmbH (Germany), AQ Implants GmbH (Germany) and Permedica S.P.A (Italy).
Wearable ultrasound system for controlling upper limb prosthetics
Zahra Taghizadeh, MS, Ahmed Bashatah, MS, Samuel Acuña, PhD, Siddhartha Sikdar, PhD
Department of Bioengineering, George Mason University, Fairfax, USA ztaghiza@gmu.edu
Introduction or purpose: Sonomyography (SMG), an emerging modality that uses ultrasound to detect muscle deformation, has shown promise as a method for real-time derivation of control signals from functional activity of muscles and classifying various hand grasps of individuals with upper limb loss1. The objective of this study was to improve reliability of classifying different grasps by investigating the effect of different training paradigms.
Methods: In this study, we utilized a 4-channel ultrasound system with miniaturized electronics optimized for forearm applications2 to capture a 4-channel M-mode images of the in vivo muscle interfaces of 3 participants. the participants were asked to perform 4 grasps (including Rest, Power, Tripod, and Pronation) under two training conditions and different sets were collected for training and testing. In the static training condition, the subject performed the grasps at a specified location in the space in front of them. In the dynamic training condition, the subject held the grasp while moving their arm in the 3D space in front of them which is shown in Figure 1. We classified the grasps using linear discriminant analysis and calculated classification accuracy to quantify performance.
Figure 1.
Patterns showing training and test data collection.
Results: The average classification accuracy for each strategy is shown in Table 1, which illustrates that the use of dynamic training led to improvements in classification accuracy. In the first place, we trained the classifier just by collecting the static training data at point 1 only which is the most common arm position during daily activity. This study demonstrates the utility of different training and test patterns to increase robustness of classification. It also demonstrates that continuous dynamic training may not always lead to better performance compared to a simpler static training.
Table 1.
Classification accuracy of 3 different training approaches.
| Dynamic test | Static test | |
|---|---|---|
| Static Training Point 1 | 59.22% ±20.93 | 60.34%± 28.51 |
| Static Training all Points | 90.56%±1.67 | 88.11% ± 9.1 |
| Continuous Dynamic Training | 87.35%±9.09 | 78.84% ±17.04 |
Conclusion: The feasibility of using Sonomyography (SMG) in classification of grasps in prosthetic application has been previously demonstrated. This study evaluated the effect of arm position and dynamic arm movement during training and testing. The results indicate that static training at a single arm position is not reliable, but that static training at different arm positions can improve classification accuracy during dynamic arm movement.
Signifance: In this study, we investigated how different training patterns can affect the performance of the classification algorithm.
Acknowledgements: This work was supported by NIH grant U01EB027601.
References
1. Engdahl, S. M., Acuña, S. A., King, E. L., Bashatah, A. & Sikdar, S. First Demonstration of Functional Task Performance Using a Sonomyographic Prosthesis: A Case Study. Front. Bioeng. Biotechnol. 10, 1–20 (2022).
2. Tarbox, E. et al. Low-power ultrasound imaging systems using time delay spectrometry. IEEE Int. Ultrason. Symp. IUS (2017) doi:10.1109/ULTSYM.2017.8092322.
Who are we helping? Demographic characteristics of amputee population at a level 1 trauma, academic health care center
Whitney Pratt, MD PhD1, Regan Johnson PT DPT2, Julie Salin PT DPT 2, Peter Altenburger, PT PhD 3
1 Indiana University School of Medicine, 2 Indiana University Health, 3 Indiana University, wpratt@iuhealth.org
Introduction: The IU Health Center for Limb Loss (CLL) is based on an academic health center campus at a Level I Trauma Center serving patients fromall over the state and region. The CLL was established to provide comprehensive, multidisciplinary limb loss care and address gaps in management related to suboptimal care coordination1. We developed a detailed patient database to facilitate analysis of patient demographics to help uncover potential barriers and limitations to care for specific patient groups. We hope to identify opportunities to improve continuity of care and eliminate inequities in functional outcomes which have been demonstrated amongst underserved patient groups.2
Methods: A retrospective study examined 176 patient with limb loss treated at the IU Health CLL from 2016-2023.
Data was collected using structured chart review in the Cerner EMR and includedbasic demographic information, K-level, medical comorbidities, and surgical details. We collected self-reportedquality of life data usingthe SF-36. We administered the amputee mobility predictor with prosthesis (AMPRO), as able, on our patient population. Figure 1
Figure 1.
Reason for amputation for patients treated in the CLL..
Results: Data will be presented on the demographic characteristics of the patients treated in the CLL with correlation to functional outcome data where available. Figure 2
Figure 2.
Sex of patients treated in the CLL.
Conclusions: Analysis of the collected patient demographics demonstrates the diversity of patients served at the IU Health CLL. Both traumatic and vascular etiologies of amputation are well represented, offering further opportunity to explore differences between these patient groups. Differences in functional outcomes related to sex, age, race and other patient characteristics may represent potential inequities related to barriers specific to certain subpopulations.
Significance: Further in-depth analysis of patient demographic data and collection of additional outcome data will help uncover complexcontributors to health care disparities that impact functional outcomes within the amputee population. Efforts should be made to address identified barriers and improve access to quality limb loss for all patients
Disclosures: None.
References
1. Gailey R, et al. Physical Therapy, 100, 773-787, 2020.
2. Tse C, et al. J Clin Orthop Trauma, 10, :S100-S105, 2019.
Interprofessional community reintegration for patients with upper or lower limb loss: Life hacks for prosthetic wearers
R Van Veld, B O’Steen
SRT Prosthetics & Orthotics (affiliated with Össur Americas), Indianapolis, IN
Description: People with limb loss encounter many barriers when they begin attempting to rejoin their communities after receiving their prostheses. These barriers may superficially present as physical ones, but there can also be a psychological barrier for those who lack confidence in their ability to use their prosthetic device correctly in a consistent and safe manner.
Prosthetists do address some community reintegration topics in their patient education, but they may not think as in depth about them as therapists are trained to do. On the contrary, physical and occupational therapists specialize in functional tasks and related reintegration, but they may not feel comfortable with how a prosthetic device works to be able to guide their patients in these areas.
This program will provide interprofessional discussion on common community barriers such as driving, grocery stores, and air travel, for patients with either upper or lower limb prosthetic limbs.
Attendees will be encouraged to actively pursue interprofessional communication in the outpatient setting for best patient outcome and most efficient use of financial resources. Presenters will bring their own extensive experience working with patients experiencing amputation from the OT and PT perspective, as well as information gleaned from successful wearers of prosthetic devices.
Objectives: Upon completion of this course, you will be able to:
1. Appreciate the challenges people with limb loss encounter during community reintegration.
2. Strategize solutions for people with limb loss in specific community settings and tasks.
3. Develop patient education approaches to cover frequently asked questions from people with limb loss.
4. Improve patient outcomes through interprofessional plans of care for people using prosthetic devices.
References
1. Darter BJ, Hawley CE, Armstrong AJ, Avellone L, Wehman P. Factors Influencing Functional Outcomes and Return-to-Work After Amputation: A Review of the Literature. Journal of occupational rehabilitation. 2018 Dec 1;28(4):656-65.
2. Godlwana L, Stewart A. The impact of lower limb amputation on community reintegration of a population in Johannesburg: A qualitative perspective. South African Journal of Physiotherapy. 2013 Jan 16;69(4):48-54.
3. Resnik L, Borgia M, Silver B. Measuring community integration in persons with limb trauma and amputation: a systematic review. Archives of physical medicine and rehabilitation. 2017 Mar 1;98(3):561-80.
4. Roepke AM, Williams RM, Turner AP, Henderson AW, Norvell DC, Henson H, Hakimi KN, Czerniecki JM. A longitudinal study of social participation after dysvascular lower extremity amputation. American journal of physical medicine & rehabilitation. 2017 Oct 1;96(10):741-7.
5. Roffman CE, Buchanan J, Allison GT. Predictors of non-use of prostheses by people with lower limb amputation after discharge from rehabilitation: development and validation of clinical prediction rules. Journal of physiotherapy. 2014 Dec 1;60(4):224-31.
6. Sions JM, Manal TJ, Horne JR, Sarlo FB, Pohlig RT. Balance-confidence is associated with community participation, perceived physical mobility, and performance-based function among individuals with a unilateral amputation. Physiotherapy theory and practice. 2018 Jun 29:1-8.
Microprocessor stance and swing control orthoses (MP-SSCO): A milestone in neuro-orthotics
Chairman: Andreas Kannenberg, MD (GER), PhD
Speakers: Andreas Hahn, PhD, Arun Jayaraman, PT, PhD, Russ Lundstrom, MS, Shane Wurdeman, PhD, CPO, FAAOP
Abstract: Locked knee-ankle-foot orthoses (LKAFOs) that force patients to always walk with a stiff orthotic leg are the standard of care for individuals with knee instability due to neuromuscular or central nervous disease. Technological “advances”, made decades ago, such as posterior-offset KAFOs and stance control orthoses lock the orthotic knee during stance and unlock it for free swing. However, the benefits of these orthoses are primarily limited to level walking. Thus, orthotists and KAFO users are faced with a tremendous technology and clinical benefit gap compared to the prosthetic options for patients with amputations. A microprocessor stance and swing control orthosis (MP-SSCO – C-Brace®) that closes this gap has been available for about 10 years.
The symposium will give a comprehensive overview on the clinical research performed with the C-Brace. It will summarize all published studies and present yet unpublished clinical results of two ongoing trials. One study is investigating the potential benefits of the MP-SSCO in the post-acute rehabilitation of patients with incomplete spinal cord injuries. The second trial is an international, randomized, multi- center study with 75 current KAFO users at 14 sites in 4 countries. Preliminary results shortly after completion of the study showed statistically significant and clinically meaningful improvements in risk of falling, actual falls, performance-based and patient reported function and mobility.
First subgroup analyses revealed important differences between patients with different underlying conditions and types of conventional orthoses currently used. The complete statistical analysis will give orthotists valuable guidance for the differential orthotic treatment of their KAFO patients.
Learning objectives
1. Understand the current body of evidence for the MP-SCCO.
2. Be able to apply the evidence on differential benefits of the MP-SSCO on patient groups with different medical conditions and current KAFO types.