Abstract
The experience of pain spans biological, psychological and sociocultural realms, both basic and complex, it is by turns necessary and devastating. Despite an extensive knowledge of the constituents of pain, the ability to translate this into effective intervention remains limited. It is suggested that current, multiscale, medical approaches, largely informed by the biopsychosocial (BPS) model, attempt to integrate knowledge but are undermined by an epistemological obligation, one that necessitates a prior isolation of the constituent parts. To overcome this impasse, we propose that an anthropological stance needs to be taken, underpinned by a Bayesian apparatus situated in computational psychiatry. Here, pain is presented within the context of lifeworlds, where attention is shifted away from the constituents of experience (e.g. nociception, reward processing and fear-avoidance), towards the dynamic affiliation that occurs between these processes over time. We argue that one can derive a principled method of investigation and intervention for pain from modelling approaches in computational psychiatry. We suggest that these modelling methods provide the necessary apparatus to navigate multiscale ontology and epistemology of pain. Finally, a unified approach to the experience of pain is presented, where the relational, inter-subjective phenomenology of pain is brought into contact with a principled method of translation; in so doing, revealing the conditions and possibilities of lifeworlds in pain.
Keywords: theories and models, psyciatry, embodiment, pain, anthropology, bayesian inference
Introduction
On the surface, the experience of pain appears paradoxical (Bradley 2021). It is ubiquitous, yet idiosyncratic, both basic and complex; by turns necessary and devastating. Pain is poised tantalisingly across body and mind, determined by context, yet defined by the individual. The consequences of this can be observed from the metaphorical to the practical: pain resists definition, classification and, crucially, effective treatment when it persists (Williams et al. 2020). Our understanding of pain, from a scientific perspective, has broadened considerably in the last 10 years (Moayedi and Davis 2013; Williams 2016; Karos et al. 2018; Seymour 2019; Stilwell and Harman 2019; Tabor and Burr 2019; Kiverstein et al. 2022). No longer constrained to the detection of damage, the experience of pain spans biological, psychological and sociocultural realms (Raja et al. 2020). With increasing precision, the parameters that influence our experience of pain have been identified across multiple disciplines (Wiech 2016; Buchbinder et al. 2018; Johnston et al. 2019). Yet, even with the scope that different expertise has afforded, the effective integration of these parameters remains elusive (Flor and Turk 2015).
The biopsychosocial (BPS) model (Engel 1977) stands as the principal frame in which diffuse disciplinary knowledge is drawn together in the domain of health; a pervasive philosophy that continues to influence the way researchers and clinicians alike investigate and intervene (Borrell-Carrió et al. 2004). With its roots in systems theory, the premise of the BPS was to reject biomedical reductionism in favour of a multidimensional, integrative approach to health and illness. It is argued, however, that the BPS has failed to realise these conceptual underpinnings (Benning 2015), in both theory (Pilgrim 2002; Ghaemi 2009) and practice (Cohen 1993; Suls and Rothman 2004; Kecmanovic and Hadzi-Pavlovic 2010). Pertinently, a neglect is observed in the way in which the BPS is able to accommodate the influence of large sociocultural units on the one hand, and the subjective reality of patients on the other (Benning 2015). Its inability to function across multiple scales and between multiple levels of influence—a characteristic demanded by complex conditions—is a fundamental limitation of the model. For Engel,
‘[e]ach system as well implies qualities and relationships distinctive for that level of organization and requires unique criteria for study and explanation. In no way can the methods and rules appropriate for the study and understanding of the cell as cell be applied to the study of the person as person or the family as family. Similarly, the methods needed to identify and characterize the components of the cell have to be different from those required to establish what makes for the wholeness of the cell’ (Engel 1981, 106).
The BPS model imposes that prior to an integrated consideration of the whole system, there must be isolation. And although such systems ought to be understood as nested across their scales of organisation, according to this approach they cannot be explained with a single integrative strategy. Put another way, under the BPS model, only the ontology of a disorder cuts across levels, not its epistemology; ontology being concerned with ‘what things are’, and epistemology being concerned with ‘how we come to know’ that which is (Bateson 1971, 442). Moreover, in pain research, although intended as a philosophy of care, the translation of the BPS model in theory and practice plays out under the shadow of pain’s paradoxes (Stilwell and Harman 2019). That is, where integration is sought, compartmentalised targets are found; without a truly integrative model to guide action (Borrell-Carrió et al. 2004), bio-psycho-social elements are pursued with ‘eclectic freedom’ (Ghaemi 2009), reduced to disembodied risk factors to be separated, investigated and treated (Moseley and Flor 2012; van Hecke et al. 2013; Johnston et al. 2019; Apkarian 2011). The consequence of an inadequate integrative multiscale and multilevel approach to healthcare generally and pain specifically is that despite great advances in our knowledge of pain, effective treatment remains lost in translation. We are faced with therapies that are not efficacious (Williams et al. 2020; O’Connell et al. 2023), a global opioid crisis (Marshall et al. 2019), and an increasing prevalence of persistent pain conditions that constitutes an epidemic (Gatchel 2015; Domenichiello and Ramsden 2019).
In response, we first invite a return to an anthropological perspective on the experience of pain (Good et al. 1994): centred on individual experience but inseparable from the broader socio-cultural frame. Second, we provide a structural model that guides multiscale action: a computational approach grounded in Bayesian inference. Accordingly, the goal of this paper is to outline a principled method of investigation and intervention for the experience of pain, embedded and embodied in a lifeworld.
This paper proceeds by centring on the phenomenological character of pain, while acknowledging that the experience can be described across multiple scales of organisation (i.e. it is a multiscale phenomenon). And for this reason, requires explanations that can be pitched across several levels (i.e. multilevel explanations). In the following section of this paper, we set out the necessary grounding developed through an anthropological stance to pain, understood as a relational experience. We propose that the experience of pain emerges through on-going ‘correspondence’ within a particular lifeworld (Ingold 2017). This allows us to describe the microcosm of pain experience—the local lifeworld of the individual, in relation to the macrocosm of the sociocultural niche, not isolated but subsumed within one another. Next, we present a framework borrowed from computational psychiatry to offer an apparatus that captures the multiscale nature of afflictions configured at the level of subjective experience (i.e. mental disorders (Kirmayer and Young 1999)) and an explanatory framework for a multilevel reading of such afflictions. We then propose ‘A unified approach’: detailing an integrated translation, directed towards investigation and intervention within the field of persistent pain; its proposed efficacy illustrated with a case study, drawn from anthropological inquiry, and translated through a computational psychiatry approach. It is suggested that existential anthropology and computational psychiatry together promote an embodied and embedded approach for a unified conceptualisation of pain; the two approaches underpinned by a commitment to investigate the conditions and possibilities of systems in the world.
An anthropological stance
The experience of pain is well suited to anthropological inquiry, with detailed ethnographies providing valuable insight into the human condition (Good et al. 1994; Kleinman 1997; Honkasalo 2001). Such accounts reveal the sociocultural shaping of pain, an ecosocial phenomenon, i.e. fundamentally relational in its makeup (Kirmayer 2008; Karos et al. 2018). Yet, these contributions have been largely neglected in contemporary pain inquiry, which has favoured objective accounts, informed by cognitive-behavioural (Eccleston and Crombez 1999; Vlaeyen et al. 2016), neuroscientific (Wager et al. 2013; Davis 2019) and epidemiological pursuits (Johnston et al. 2019), increasingly in the service of precision medicine (Nijs et al. 2021). In taking an anthropological turn, we assert that the success of such approaches will be determined by the attention paid to the embedded individual (Ziegelstein 2017).
As such, we define an anthropological stance in terms of an active endeavour, a mode of inquiry that approaches the experience of pain as part of an individual’s local lifeworld. In keeping with 4E approaches to cognition (Varela et al. 2017; Colombetti 2017; Gallagher 2023), the experience of pain is investigated as embodied, enacted, embedded and extended in a dynamic sociocultural niche (Kleinman 1992; Csordas 2002; Jackson 2012; Tabor et al. 2017). Additionally, this position draws on a rich history of existential approaches to suffering (Kleinman 1997; Jackson 2019) and brings them into contact with a detailed phenomenological approach to experience (Merleau-Ponty 1945; Dreyfus 1990; Jackson 2005). Under this gaze, pain cannot be separated from the individual nor a dynamism of being-in-the-world (Merleau-Ponty 1945; Dreyfus 1990).
A crucial extension gained by adopting an anthropological stance, beyond phenomenological and embodied approaches, is the conceptual reach; capturing the way in which pain and suffering has changed over time, across generations, cultures and social networks, as well as across a single lifespan. It provides the means to situate the individual in the present, informed by the past, and oriented towards an uncertain future. We now explore these means, through the conceptual metaphors of ‘lifeworlds’, ‘lines’ and ‘correspondence’.
Lifeworlds and lines
Our starting point is one of phenomenological grounding (Husserl 1970), from which our experiences are brought forth through an ongoing engagement with the world (Merleau-Ponty 1945). In following the existential anthropology of Jackson (2005), we extend this phenomenological base to incorporate a detailed reckoning of a dynamic ecosocial world; in short, a lifeworld (Jackson 2012). Our lifeworlds are not settled, but comprise a landscape through which we are able to continually negotiate a sense of ourselves, always in relation to others (Jackson 2005, 2012). A lifeworld presents an embodied history in transition, situated in the present but oriented towards the possibilities of the future; it is ‘a field charged with vitality and animated by struggle’ (Jackson 2012, 7). A lifeworld can be considered an evolving entanglement of lines, which reach out, beyond single systems, forming a meshwork. In evoking the meshwork, as Ingold does (Ingold 2015), we depart from the dominant metaphor of network (Latour 2005). Where the network makes distinct the components of a system and its lines of connection, a meshwork transfigures a system into ‘lines of becoming’ (Deleuze and Félix 1987), not curtailed by set points of beginning or end, the lines themselves become the focus, differentially corresponding with each other as they ‘bod(y) forth’ (Lefebvre 1974; Ingold 2011; 2016, 2017). These lines are indicative of system processes, from the microscopic to the macroscopic (e.g. immune dynamics, psychological states, family responsibilities and workplace identity).
In other words, the lifeworld sets the bounds on what is afforded, ‘for good and for ill’, to a particular system at a given time (Gibson 1979), and the particular entanglement of lines determines the shape of that lifeworld. It is in this formulation of lifeworlds that allows the negotiation of new possibilities within the ‘subjective in-between’ (Arendt 1958), i.e. entanglements of lines that are brought under tension or loosened through an ongoing process of correspondence.
Correspondence
Correspondence, as described by Ingold (Ingold 2015) refers to the affiliations between the lines of a lifeworld. Correspondence extends to incorporate the relation between lifeworlds, reaching out across a meshwork (Ingold 2017); affiliations that wax and wane as living systems intertwine with each other and their environment over time. It demands a focus of attention on what it is to ‘be-in-the-world’ (Heidegger 1962): in tension with other organisms. In this way, correspondence denotes the way in which the processes of a lifeworld influence each other.
Correspondence and lifeworlds
Correspondence determines the texture of our lifeworlds. An illustrative example can be observed during jazz improvisation. When a saxophonist plays, there is, necessarily, an interaction between the musician and their instrument, yet this point of connection is not correspondence. Rather, the melody that emerges from this coming together is what is meant by correspondence (Ingold 2011). Furthermore, as the bassist, trumpeter, trombonist and clarinettist join in, each with their own melody in response to the saxophonist’s ‘question’, a polyphonic experience results. Polyphony, emerging through improvised jazz can be thought of as a particular lifeworld composed of multiple lines in correspondence. As the dynamic between different musicians changes over time, with melodies rising to prominence and then receding, the correspondence is altered; an evolving process that shapes and reshapes the shared musical lifeworld. Here, each melody is a line in a polyphonic lifeworld, and it is through the correspondence of these lines that the lifeworld derives its texture. It necessitates agile attending, deployed in sympathy with one another; negligence risks discordance, incoherence, and in a musical context, noise.
Lifeworlds and correspondence in pain
In applying this conceptualisation to pain, the lifeworld must capture the multiscale aspects of the individual (micro, meso and macro), while extending beyond the individual to encompass the broader sociocultural milieu (past, present and future). Here, the lifeworld of an individual in pain, whether acute or chronic, is considered an entanglement of lines that reach beyond bodily bounds, affiliated in a way that reflects dynamic correspondence. Manifesting in a particular phenomenology for the individual, the lines of the lifeworld reach across evolutionary and life histories, biological traces, psychological repertoires, social interactions, cultural expectations, political agendas and global constraints. These lines are not separate but interwoven to form a meshwork reflective of a supersystem, in which the lifeworld for the individual in pain, is embroidered.
In most cases, the experience of pain is short-lasting, a lifeworld reshaped through the changing correspondence of its lines. Yet, for a significant number of people, the experience of pain persists (Fayaz et al. 2016). In the present context, and in keeping with recent embodied (Tabor et al. 2017; Stilwell and Harman 2019) and predictive accounts of pain (Büchel et al. 2014; Tabor and Burr 2019; Kiverstein et al. 2022), this apparent ‘stickiness’ of aversive experience (Borsook et al. 2018) is related to a continued anticipation of threat to the self. The persistent anticipation of threat involved in pain has been attributed to various mechanisms, from maladaptive learning and aberrant precision allocation in reward processing (Seymour 2019), to an altered landscape of affordances (Stilwell and Harman 2019). In common, these accounts describe the complex componentry of anticipatory protective action, from neural networks to environmental contingencies. In taking an anthropological stance, however, our attention is trained on the ways in which these processes, or lines of a lifeworld, correspond for the individual in pain over time. The greater the affiliation between lines (e.g. a physiological stress response, historical trauma, completing assignments and fulfilling socio-cultural expectations), the greater influence this entanglement of lines has on the shape of the lifeworld. It pulls tight, narrowing the lifeworld in a certain direction—a tangled skein. As a consequence, the landscape is altered, what is afforded to the individual is narrowed to reflect ‘what is at stake’ for them at that time (Miller et al. 2020). At risk for the individual in pain when correspondence constricts, is incoherence: a discordance between their local lifeworld (narrowed to reflect a need to protect), and the wider niche, soliciting engagement.
In taking this perspective, the traditional boundaries between adaptive and maladaptive pain become less distinct. Here, the experience of pain always reflects multiscale processes in correspondence at any given time, within a particular lifeworld. These processes span proximal (developmental, e.g. endocrine function) and ultimate (evolutionary, e.g. threat anticipation) timescales (Constant et al. 2022), influencing the current experience of pain. In this sense, detailing the processes of a lifeworld should determine investigation and intervention, irrespective of the duration of pain. However, the ability to contextualise the lifeworld, which considers proximal and ultimate forces in correspondence, is fraught with difficulty. Previous attempts at navigating this translation have thus far proved either overwhelmingly complex (Fabrega and Tyma 1976) or limited by simplicity (e.g. as with the BPS). A further step is required to overcome the translation gap. We have proposed that an anthropological stance provides an impetus for action, yet an apparatus is needed to enable action to be taken. To address this, we turn, in the next section, to the domain of computational psychiatry, where advances in the application of predictive modelling (Kirmayer 2019; Gómez-Carrillo and Kirmayer 2023) provide one such apparatus.
Multiscale ontology and multilevel epistemology in computational psychiatry
In the introduction, we suggested that instrumental approaches to health, specifically the BPS model, do not provide an integrative account of pain. Instead, it is implemented in a way that isolates constituent parts, across scales of influence, in an attempt to understand the whole. This is a problem for the view advocated in this paper, which seeks to provide a principled approach to pain understood as a unified phenomenon. We have suggested that an anthropological stance provides a systems approach that does not reduce pain to its componentry but describes the processes through which it may emerge and evolve. To complement this prospective approach, we now provide the apparatus for translation, appealing to the underlying epistemology and ontology of computational psychiatry.
Computational psychiatry (Corlett and Fletcher 2014; Friston et al. 2014) is a multidisciplinary domain of research in theoretical neuroscience that analyses clinical and behavioural data to design computer models of the environmental, social and neurobiological causal networks underpinning mental disorders (Huys et al. 2016; Gauld et al. 2021). Models in computational psychiatry are used to analyse, simulate and forecast the way behavioural and psychological symptoms are generated, thereby providing promising methods for phenotyping and nosology (Schwartenbeck and Friston 2016) as well as to appraise prognosis (Constant et al. 2021). As a research program, computational psychiatry contains three subdomains (Gauld et al. 2021): (i) digital psychiatry—the creation of digital interfaces to gather more ecologically valid types of data, such as ecological momentary assessment data (Shiffman et al. 2008); (ii) big data psychiatry—the use of machine learning and artificial intelligence to treat large clinical data sets; and (iii) modelling psychiatry—the use of reinforcement learning, dynamical system theory and Bayesian methods to provide biobehaviorally plausible models of symptoms of mental disorders. Empirically, Bayesian modelling methods of computational psychiatry have been used for biophysical modelling of neuronal processes (Isomura 2022; Kagan et al. 2022), behavioural and social interactional modelling of decision making under uncertainty—to find computational markers of mental disorders (Cullen et al. 2018; Smith et al. 2020a, 2020b, 2020c, 2021c; Constant et al. 2021), and for psychosocial (i.e. social, psychological and cultural) modelling—the modelling of linguistically held beliefs and expectations—to predict treatment adherence and appraisal (Smith et al. 2021a).
Biophysical, Behavioural and Psychosocial models reflect the multi-scale ontology of Bayesian modelling psychiatry; psychiatric phenomena such as mental disorders being configured at the sociocultural level, the psychological or phenomenological level, and at the biophysical level (Table 1). Bayesian modelling psychiatry also provides an epistemology—a theory of ‘how we come to know’ psychiatric phenomena, which is in turn multilevel. One way to present the epistemology of Bayesian modelling psychiatry is by appealing to David Marr’s levels of analysis (Marr 2010; Corlett and Fletcher 2014).
Table 1.
Epistemology and ontology of psychiatric phenomena
| Multi-scale ontology | ||||
|---|---|---|---|---|
| Biophysical scale model | Behavioural and social interactional scale model | Psychosocial scale model | ||
| Multi-level epistemology | Computational level | Inference problem | ||
| Algorithmic level | Bayesian inference | |||
| Implementation level | E.g. (neuro)physiology | E.g. behavioural patterns/posture | E.g. language/healthcare systems | |
Psychiatric phenomena, from the computational point of view, ought to be studied as a failure to solve the fundamental problem that systems like us must solve—that of inferring the causes of sensations, with Bayesian inference being the computational specification of the problem of inferring the causes of sensations. At the algorithmic level—the level at which one decides how to solve the computational problem, this problem is solved with Bayesian inference. And at the implementation level, Bayesian inference would be realised by the dynamics of the system of interest (e.g. the (neuro)physiology of a system configured at the biophysical level). Importantly, Bayesian inference at the algorithmic level can be used to interpret the working of many different mechanisms whose dynamics at the implementation level would conform to Bayesian inference. Under the present framework, for the sake of simplicity, only the Bayesian algorithm is reflected at the algorithmic level. However, a complete approach based on computational psychiatry could consider a variety of algorithms (e.g. machine learning, natural language processing, dynamical systems, etc.).
Through a unified ‘Bayesian’ ontology and epistemology, computational psychiatry can, in principle, provide the apparatus (e.g. hierarchical models) (Friston et al. 2017a; Ramstead et al. 2018; Badcock et al. 2019), that can facilitate the coherent translation of the dynamic correspondence between system processes for investigation and intervention. That is, a weighted appraisal of correspondence across scales and levels that guides relevant action. Note that Marr’s levels of analysis function as a general guide to the inquiry on the computational functioning of an entity configured at any ontological scale. For instance, when considering the hierarchical approach of the BPS model, one could apply Marr’s strategy for each of the levels (e.g. analyse the person out of the biosphere as an entity that can be described with multiple levels of analysis). Marr’s way of approaching levels of analysis is thus consistent with the BPS way of isolating components of the hierarchy to treat them as incommensurable. As such, we do not claim that using Marr’s levels of analysis overcomes that limitation of the BPS. Instead, by evoking the BPS model through a Marrian analysis, we are able to appeal to Bayesian modelling methods that transcend hierarchical levels. These methods allow for the comparison of activity—optimal and suboptimal—at each level by modelling them as a set of parameters (e.g. likelihood, prior, and prior preferences in the case of some models (Friston et al. 2017b) whose posterior probability can be assessed with scale independent measures (e.g. model evidence). In other words, one can apply a Marrian epistemological analysis ‘within’ each level, and each ontological level can be modelled using a Bayesian modelling approach. This step makes each level commensurable, thereby revealing a unified structure through which processes correspond for targeted investigation and intervention.
It is important to note that in recent years, computational approaches in the field of pain science have gained traction. Applied to both brain-based mechanisms and behavioural data, these accounts have identified the predictive nature of pain perception (Mancini et al. 2022; Mulders et al. 2023), revealing a diffuse neural architecture associated with anticipatory, threat-based, precision-weighting (Eckert et al. 2022; Chen and Wang 2023). Yet, in their current form, these Bayesian models remain largely confined to stimulus-response paradigms, reflecting single-scale experimental contingencies. Crucial to the adequate translation of Bayesian accounts of the multiscale phenomenon of pain is the extension in scope of the Bayesian approach to other levels of ontology (e.g. behavioural and psychological). Theory-driven computational models in pain research have explored these realms (Tabor and Burr 2019; Kiverstein et al. 2022), yet the realisation of such multiscale models in practical terms—incorporating subsystem functioning (e.g. immune, endocrine and neural systems) as well as supersystem dynamics (e.g. social networks and goal motivation)—requires adequate framing. Our proposed framework may function as such a framing that could help researchers and clinicians to identify the scale at which their inquiry is located and track the scales at which their intervention acts.
A unified approach
We submit that taken together, anthropological inquiry alongside the multiscale ontology and the multilevel epistemology of Bayesian computational psychiatry provides a unified approach to the investigation and intervention in pain. This method combines the anthropological stance described above, with the computational framework outlined in the previous section. Here, we focus our application on a clinical case described in the ethnographic work of Kleinman (Good et al. 1994) (Box 1). Under the lance of the proposed method, we indicate how such phenomenological observations may be translated into both multiscale and multilevel investigation and intervention for persistent pain. We do this by showing how, in taking the anthropological stance, one can leverage the ontological and epistemology of computational psychiatry to guide one’s action.
Box 1. Phenomenological excerpts of a clinical case: Case 1 (Kleinman 1994: 175–182).
‘At the hospital they diagnosed a concussion and I had broken a few small bones in my foot…Otherwise, there was nothing else injured. But right away I could feel the pain…And that started the whole process. Four years of pain, surgeries, casts, more pain, more tests, more drugs, more surgeries, bad surgical effects, and now this constant pain…And me, us-our lives ruined. All for what?
‘Pain patients like me are a sign of the failure of the medical care system, of something terribly wrong at the core’.
‘My generation of researchers has moved on…I have to prove that I can put in a full research day, complete projects, that I am like everyone else’.
‘It’s distressing to be viewed as a risk. I used to be seen as a rising star…There is a constant stress of producing, no matter how I feel, to be productive, act successful, present myself as healthy. But I am not healthy…Have to pretend’.
‘Now, they [her family] get pretty angry at me. They simply don’t understand what is going on. My sickness has really affected them’.
(Kleinman 1994) is meticulous in his existential accounts of individual experiences of pain, articulating the microcosmic constituents of a local world in pain (Box 1), while setting these lifeworlds in a sociocultural frame. Yet, as noted by Kleinman himself, the potential limitation of traversing between the microcosm and the macrocosm in this way, is a ‘transmogrification’ of the experience. At risk, is a sacrifice of the nuance of correspondence, the texture of pain, in pursuit of an explanation that extends and dehumanises the sufferer. Our task then, is to preserve the rich texture of local lifeworlds in translation, to affirm the humanity to which experience belongs.
The case study (Box 1) provides excerpts from the experiences of a 31-year-old Ph.D. biochemistry researcher who has suffered severe pain for 4 years following a car accident. In applying an anthropological stance, underwritten by the principles of computational psychiatry, the aim is not to recreate an abstract, computational model of the lifeworld. It is to provide an apparatus with which to take coherent action.
An apparatus for translation
Identifying the processes that make up an individual’s lifeworld, from which pain emerges becomes the primary focus of inquiry: attending to the lines and the nature of their correspondence. Promoting person-centred investigation and intervention, this principled method should be oriented around the scales of influence and the levels of explanation (Fig. 1, right panel). Specifically, the computational framework outlined provides an adumbrate for (i) the ways in which lines of the lifeworld cross scales of influence, and the strength of their correspondence (scale) and (ii) what kind of explanation one ought to adopt to make sense of the particular lifeworld and to guide decision-making (level). Here, we observe the lifeworlds of anthropology as organised around the ontology and epistemology of computational psychiatry (Fig. 1).
Figure 1.
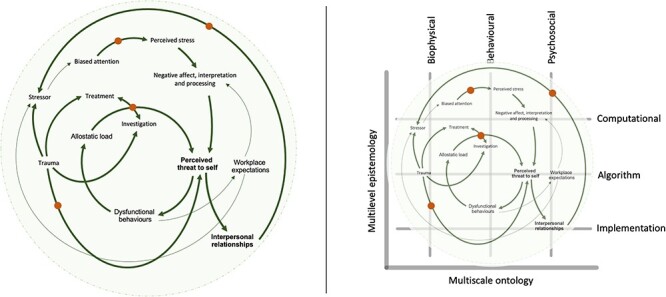
A principled method for investigation and intervention in pain based on an anthropological stance and the ontology and epistemology of computational psychiatry. Left panel. A lifeworld in pain: a schematic representation of ‘how’ the lines of a lifeworld may become entangled, unveiling relevant points of correspondence (bold), which facilitate directed inquiry (orange dots) into ‘why’ the experience of pain occurs in this way, appealing to levels of explanation. Right panel. A computational framing of a lifeworld: the X axis represents the three ontological levels of organisation that are modelled in Bayesian modelling psychiatry. The Y axis represents Marr’s three epistemological levels of explanation that Bayesian modelling psychiatry refers to explain their modelling rationales. Pain, understood as part of an inter-subjective lifeworld, incorporates processes that are located across the scales of ontology (X) and levels of epistemology (Y).
In the case study outlined (Box 1), the phenomenological references relay a tangle of lines that provide partial insight into the individual’s lifeworld. Evolving over time, the lines, denoting the processes through which pain emerges, permeate ontological scales, unbounded (Fig. 1, left panel). Attending to the lines and the way they change their affiliation resembles an ongoing education (Ingold 2018). As researchers or clinicians, we aim to learn the contingencies of experience, establishing ‘what is at stake’ for the individual.
For the 31-year-old woman in Case 1, the experience of pain does not begin with broken bones in the foot, but rather reaches out to an embodied history (past trauma, psychological traits, genetic and phenotypic dispositions) and an anticipated future (professional aspirations, interpersonal commitments and personal identity). The impact of the acute trauma (broken bones) is to draw specific lines into correspondence, informing the perception of threat to the self in the present. Over time, moment-to-moment shifts in correspondence reflect changing affiliations between processes as the individual navigates a dynamic landscape, embodied and embedded within it. This may involve a persistent stress response triggered by on-going somatosensory information, workplace expectations (‘It’s distressing to be viewed as a risk. I used to be seen as a rising star…’) and interpersonal relations (‘Now, they [her family] get pretty angry at me. They simply don’t understand what is going on’). It may also involve dysfunctional behaviours (‘There is a constant stress of producing, no matter how I feel, to be productive, act successful’), which in turn has a bearing on the perception of threat. Similarly, when investigations and interventions remain repetitive and seemingly stagnant (e.g. ‘…pain, surgeries, casts, more pain, more tests, more drugs, more surgeries, bad surgical effects, and now this constant pain…’), the correspondence between lines constricts, reflecting a narrowing of attention, precisely attuned to an ongoing perception of threat to the self. At risk, within these constricted affiliations, is a loss of coherence between the local lifeworld of the individual and her wider environment (e.g. ‘[I] present myself as healthy. But I am not healthy…I [h]ave to pretend’).
Given this complex system of correspondence, a dynamic approach to investigation is required; untethered to scales of influence (Fig. 1, right panel). Importantly, this does not necessitate radical new approaches to intervention. Instead, it demands agile attention trained on the lines of a lifeworld that evokes an iterative approach to multifaceted intervention. Much like the melodies of a jazz ensemble, interventions are seen as processes that become part of a lifeworld, attempting to reconfigure the affiliations of lines, and in so doing altering the experience of pain. Here, irrespective of the precipitating event, whether traumatic or idiopathic, the individual experiencing pain is considered at the level of the lifeworld, in which tissue integrity and anti-inflammatory medication present just one possible affiliation between processes that never occur in isolation. Expanding the scope of attention to consider multiscalar affiliations between the potential lines of influence (e.g. historic trauma, interpersonal relationships and stressor exposure) promotes interventions (psychological and behavioural therapies, medication, pain-relevant education, child support and workplace adaptations) that are deployed in an integrated, specific, and timely manner; constantly attuning to the shape of an individual’s lifeworld.
Conclusion
We have proposed that a coherent approach to the investigation and intervention of the experience of pain, whether acute or chronic, requires an anthropological stance, supported by the Bayesian apparatus of computational psychiatry. In outlining lifeworlds in pain, focussing on the dynamic correspondence that defines the shape of pain over time, and appealing to ontological and epistemological frames of reference, we are able, as patients, clinicians and researchers, to attune to the experience of pain. In so doing, we establish the principles for effective knowledge translation (a multi-scale ‘going along-with’), recognising that, as Kleinman (1997) puts it, ‘[e]xperience is emergent, not pre-formed. It changes. It goes on and on…’ and we must go along with it.
Acknowledgements
The authors would like to thank Dr Ana Gómez-Carillo (McGill University), for her generous conversations, far-reaching knowledge and clinical astuteness, which helped to guide the translation of this work.
Contributor Information
Abby Tabor, Faculty of Health and Applied Sciences, University of the West of England, Frenchay Campus, Coldharbour Ln, Stoke Gifford, Bristol BS16 1QY, UK; Centre for Pain Research, University of Bath, Claverton Down, Bath BA2 7AY, UK.
Axel Constant, Department of Engineering and Informatics, The University of Sussex, Chichester 1 Room 002, Falmer, Brighton BN1 9QJ, UK.
Data availability
No new data were generated or analysed in support of this research.
Conflict of interest
None declared.
References
- Apkarian AV. The brain in chronic pain: clinical implications. Pain Manag 2011;1:577–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arendt H. The Human Condition. Chicago: The University of Chicago Press, 1958. [Google Scholar]
- Badcock PB, Friston KJ, Ramstead MJD. The hierarchically mechanistic mind: a free-energy formulation of the human psyche. Phys Life Rev 2019;31:104–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateson G. The cybernetics of ‘self’: a theory of alcoholism. Psychiatry 1971;34:1–18. [DOI] [PubMed] [Google Scholar]
- Benning TB. Limitations of the biopsychosocial model in psychiatry. Adv Med Educ Pract 2015;6:347–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell-Carrió F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Ann Fam Med 2004;2:576–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsook D, Youssef AM, Simons L. et al. When pain gets stuck: the evolution of pain chronification and treatment resistance. Pain 2018;159:2421–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley A. The paradox of pain. Philos Q 2021;71:qaa084. [Google Scholar]
- Buchbinder R, van Tulder M, Öberg B. et al. Low back pain: a call for action. Lancet 2018;391:2384–8. [DOI] [PubMed] [Google Scholar]
- Büchel C, Geuter S, Sprenger C. et al. Placebo analgesia: a predictive coding perspective. Neuron 2014;81:1223–39. [DOI] [PubMed] [Google Scholar]
- Chen ZS, Wang J. Pain, from perception to action: a computational perspective. iScience 2023;26:105707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen CI. The biomedicalization of psychiatry: a critical overview. Community Ment Health J 1993;29:509–21. [DOI] [PubMed] [Google Scholar]
- Colombetti G. The Feeling Body: Affective Science Meets the Enactive Mind. Cambridge, MA: MIT Press, 2017. [Google Scholar]
- Constant A, Badcock P, Friston K. et al. Integrating evolutionary, cultural, and computational psychiatry: a multilevel systemic approach. Ront Psychiatry 2022;13:763380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constant A, Hesp C, Davey CG. et al. Why depressed mood is adaptive: a numerical proof of principle for an evolutionary systems theory of depression. Comput Psychiatry (Cambridge, Mass ) 2021;5:60–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corlett PR, Fletcher PC. Computational psychiatry: a Rosetta stone linking the brain to mental illness. Lancet Psychiatry 2014;1:399–402. [DOI] [PubMed] [Google Scholar]
- Csordas TJ. Embodiment as a paradigm for anthropology. In: Csordas TJ (ed.), Body/Meaning/Healing. New York: Palgrave Macmillan US, 2002, 58–87. [Google Scholar]
- Cullen M, Davey B, Friston KJ. et al. Active inference in OpenAI Gym: a paradigm for computational investigations into psychiatric illness. Biol Psychiatry Cogn Neurosci Neuroimaging 2018;3:809–18. [DOI] [PubMed] [Google Scholar]
- Davis KD. Introduction to a special issue on innovations and controversies in brain imaging of pain: methods and interpretations. Pain Rep 2019;4:e771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deleuze G, Félix G. A Thousand Plateaus: Capitalism and Schizophrenia. In: Massumi B (ed.), London: University of Minnesota Press, 1987. [Google Scholar]
- Domenichiello AF, Ramsden CE. The silent epidemic of chronic pain in older adults. Prog Neuropsychopharmacol Biol Psychiatry 2019;93:284–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreyfus HL. Being-in-the-World: A Commentary on Heidegger’s Being in Time, Division I. Cambridge, MA: MIT Press, 1990. [Google Scholar]
- Eccleston C, Crombez G. Pain demands attention: a cognitive-affective model of the interruptive function of pain. Psychol Bull 1999;125:356–66. [DOI] [PubMed] [Google Scholar]
- Eckert A-L, Pabst K, and Endres DM. A Bayesian model for chronic pain. Front Pain Res 2022;3:966034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel GL. The need for a new medical model: a challenge for biomedicine. Science 1977;196:129–36. [DOI] [PubMed] [Google Scholar]
- Engel GL. The clinical application of the biopsychosocial model. J Med Philos 1981;6:101–24. [DOI] [PubMed] [Google Scholar]
- Fabrega H Jr, Tyma S. Culture, language and the shaping of illness: an illustration based on pain. J Psychosom Res 1976;20:323–37. [DOI] [PubMed] [Google Scholar]
- Fayaz A, Croft P, Langford RM. et al. Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open 2016;6:e010364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flor H, and Turk DC. Chronic Pain: An Integrated Biobehavioral Approach. Philadelphia: Lippincott Williams & Wilkins, 2015. [Google Scholar]
- Friston KJ, Enno Stephan K, Montague R. et al. Computational psychiatry: the brain as a phantastic organ. Lancet Psychiatry 2014;1:148–58. [DOI] [PubMed] [Google Scholar]
- Friston K, FitzGerald T, Rigoli F. et al. Active inference: a process theory. Neural Comput 2017a;29:1–49. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Rosch R, Parr T. et al. Deep temporal models and active inference. Neurosci Biobehav Rev 2017b;77:388–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher S. Embodied and Enactive Approaches to Cognition. Online: Cambridge University Press, 2023. [Google Scholar]
- Gatchel RJ. The continuing and growing epidemic of chronic low back pain. Healthcare 2015;3:838–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gauld C, Dumas G, Fakra É. et al. Les trois cultures de la psychiatrie computationnelle. Ann Med Psychol Revue Psychiatrique 2021;179:63–71. [Google Scholar]
- Ghaemi SN. The rise and fall of the biopsychosocial model. Br J Psychiatry 2009;195:3–4. [DOI] [PubMed] [Google Scholar]
- Gibson JJ. The Ecological Approach to Visual Perception. Boston: Houghton Mifflin, 1979. [Google Scholar]
- Gómez-Carrillo A, Kirmayer LJ. A cultural-ecosocial systems view for psychiatry. Front Psychiatry 2023;14:1031390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Good M-JD, Brodwin P, Good B. et al. Pain as Human Experience: An Anthropological Perspective . Berkeley, California: University of California Press, 1994. [Google Scholar]
- Hecke OV, Torrance N, Smith BH. Chronic pain epidemiology and its clinical relevance. Br J Anaesth 2013;111:13–8. [DOI] [PubMed] [Google Scholar]
- Heidegger M. Being and Time. Transl. J. Macquarrie, & E. Robinson. Oxford, UK: Blackwell, 1962. [Google Scholar]
- Honkasalo ML. Vicissitudes of pain and suffering: chronic pain and liminality. Med Anthropol 2001;19:319–53. [DOI] [PubMed] [Google Scholar]
- Husserl E. The Crisis of European Sciences and Transcendental Phenomenology: An Introduction to Phenomenological Philosophy. Evanston, IL: Northwestern University Press, 1970. [Google Scholar]
- Huys QJM, Maia TV, Frank MJ. Computational psychiatry as a bridge from neuroscience to clinical applications. Nat Neurosci 2016;19:404–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingold T. Being Alive. London: Routledge, 2011. [Google Scholar]
- Ingold T. The Life of Lines. London: Routledge, 2015. [Google Scholar]
- Ingold T. Lines: A Brief History. London: Routledge, 2016. [Google Scholar]
- Ingold T. On human correspondence. J R Anthropol Inst 2017;23:9–27. [Google Scholar]
- Ingold T. Anthropology And/as Education. London: Routledge, 2018. [Google Scholar]
- Isomura T. Active inference leads to Bayesian neurophysiology. Neurosci Res 2022;175:38–45. [DOI] [PubMed] [Google Scholar]
- Jackson M. Existential Anthropology: Events, Exigencies, and Effects. Oxford: Berghahn Books, 2005. [Google Scholar]
- Jackson M. Lifeworlds: Essays in Existential Anthropology. London: University of Chicago Press, 2012. [Google Scholar]
- Jackson M. The Politics of Storytelling. Variations on a Theme by Hanah Arendt . 2nd edn. Copenhagen: Museum Tusculanum Press, 2019. [Google Scholar]
- Johnston KJA, Adams MJ, Nicholl BI. et al. Genome-wide association study of multisite chronic pain in UK Biobank. PLoS Genet 2019;15:e1008164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagan BJ, Kitchen AC, Tran NT. et al. In vitro neurons learn and exhibit sentience when embodied in a simulated game-world. Neuron 2022;110:3952–69.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karos K, Williams ACDC, Meulders A. et al. Pain as a threat to the social self: a motivational account. Pain 2018;159:1690–5. [DOI] [PubMed] [Google Scholar]
- Kecmanovic D, Hadzi-Pavlovic D. Psychiatric journals as the mirror of the dominant psychiatric model. Psychiatrist 2010;34:172–6. [Google Scholar]
- Kirmayer LJ. Culture and the metaphoric mediation of pain. Transcult Psychiatry 2008;45:318–38. [DOI] [PubMed] [Google Scholar]
- Kirmayer L. Toward an ecosocial psychiatry. World Soc Psychiatry 2019;1:30. [Google Scholar]
- Kirmayer LJ, Young A. Culture and context in the evolutionary concept of mental disorder. J Abnorm Psychol 1999;108:446–52. [DOI] [PubMed] [Google Scholar]
- Kiverstein J, Kirchhoff MD, Thacker M. An embodied predictive processing theory of pain experience. Rev Philos Psychol 2022;13:973–98. [Google Scholar]
- Kleinman A. Local worlds of suffering: an interpersonal focus for ethnographies of illness experience. Qual Health Res 1992;2:127–34. [Google Scholar]
- Kleinman A. Pain and Resistance: The Delegitimation and Relegitimation of Local Worlds. In: Good Mary-Jo DelVecchio, Brodwin Paul E, Good Byron J, Kleinman Arthur (eds.), Pain as Human Experience: An Anthropological Perspective. Berkeley, California: University of California Press, 1994; 169–97. [Google Scholar]
- Kleinman A. Social Suffering. In: Das V, Lock MM (eds), 1st edn. Berkeley, California: University of California Press, 1997. [Google Scholar]
- Latour B . Reassembling the Social: An Introduction to Actor-Network-Theory. Oxford: Oxford University Press, 2005. [Google Scholar]
- Lefebvre H. The Production of Space, Trans. Nicholson-Smith D, 1991. Oxford: Blackwell, 1974. [Google Scholar]
- Mancini F, Zhang S, Seymour B. Computational and neural mechanisms of statistical pain learning. Nat Commun 2022;13:6613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marr D. Vision: A Computational Investigation into the Human Representation and Processing of Visual Information. Cambridge, MA: MIT Press, 2010. [Google Scholar]
- Marshall B, Bland MK, Hulla R. et al. Considerations in addressing the opioid epidemic and chronic pain within the USA. Pain Manag 2019;9:131–8. [DOI] [PubMed] [Google Scholar]
- Merleau-Ponty M. (1962). Phenomenology of Perception. Smith C Trans. London: Routledge & Kegan Paul, 1945. [Google Scholar]
- Miller M, Kiverstein J, Rietveld E. Embodying addiction: a predictive processing account. Brain Cogn 2020;138:105495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moayedi M, Davis KD. Theories of pain: from specificity to gate control. J Neurophysiol 2013;109:5–12. [DOI] [PubMed] [Google Scholar]
- Moseley GL, Flor H. Targeting cortical representations in the treatment of chronic pain: a review. Neurorehabil Neural Repair 2012;26:646–52. [DOI] [PubMed] [Google Scholar]
- Mulders D, Seymour B, Mouraux A. et al. Confidence of probabilistic predictions modulates the cortical response to pain. Proc Natl Acad Sci USA 2023;120:e2212252120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijs J, George SZ, Clauw DJ. et al. Central sensitisation in chronic pain conditions: latest discoveries and their potential for precision medicine. Lancet Rheumatol 2021;3:e383–92. [DOI] [PubMed] [Google Scholar]
- O’Connell NE, Moore RA, Stewart G. et al. Trials we cannot trust: investigating their impact on systematic reviews and clinical guidelines in Spinal Pain. J Pain 2023;eprint. [DOI] [PubMed] [Google Scholar]
- Pilgrim D. The biopsychosocial model in Anglo-American Psychiatry: past, present and future? J Ment Health 2002;11:585–94. [Google Scholar]
- Raja SN, Carr DB, Cohen M. et al. The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain 2020;161:1976–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramstead MJD, Benjamin Badcock P, John Friston K. Answering Schrödinger’s question: a free-energy formulation. Phys Life Rev 2018;24:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartenbeck P, Friston K. Computational phenotyping in psychiatry: a worked example. eNeuro 2016;3: 27517087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seymour B. Pain: a precision signal for reinforcement learning and control. Neuron 2019;101:1029–41. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol 2008;4:1–32. [DOI] [PubMed] [Google Scholar]
- Smith R, Khalsa SS, Paulus MP. An active inference approach to dissecting reasons for nonadherence to antidepressants. Biol Psychiatry Cogn Neurosci Neuroimaging 2021a;6:919–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R, Kirlic N, Stewart J. et al. Long-term stability of computational parameters during approach-avoidance conflict in a transdiagnostic psychiatric patient sample. Sci Rep 2021b;11:11783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R, Kirlic N, Stewart JL. et al. Greater decision uncertainty characterizes a transdiagnostic patient sample during approach-avoidance conflict: a computational modelling approach. J Psychiatry Neurosci 2021c;46:E74–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R, Kuplicki R, Feinstein Jet al. Tulsa 1000 investigators . A Bayesian computational model reveals a failure to adapt interoceptive precision estimates across depression, anxiety, eating, and substance use disorders. PLoS Comput Biol 2020a;16:e1008484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R, Kuplicki R, Teed A. et al. Confirmatory evidence that healthy individuals can adaptively adjust prior expectations and interoceptive precision estimates. bioRxiv 2020b;1326:156–64. [Google Scholar]
- Smith R, Schwartenbeck P, Stewart JL. et al. Imprecise action selection in substance use disorder: evidence for active learning impairments when solving the explore-exploit dilemma. Drug Alcohol Depend 2020c;215:108208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stilwell P, Harman K. An enactive approach to pain: beyond the biopsychosocial model. Phenomenol Cogn Sci 2019;18:637–65. [Google Scholar]
- Suls J, Rothman A. Evolution of the biopsychosocial model: prospects and challenges for health psychology. Health Psychol 2004;23:119–25. [DOI] [PubMed] [Google Scholar]
- Tabor A, Burr C. Bayesian learning models of pain: a call to action. Curr Opin Behav Sci 2019;26:54–61. [Google Scholar]
- Tabor A, Keogh E, Eccleston C. Embodied pain-negotiating the boundaries of possible action. Pain 2017;158:1007–11. [DOI] [PubMed] [Google Scholar]
- Varela FJ, Thompson E, Rosch E. The Embodied Mind, Revised Edition: Cognitive Science and Human Experience. Cambridge, MA: MIT Press, 2017. [Google Scholar]
- Vlaeyen JWS, Crombez G, Linton SJ. The fear-avoidance model of pain. Pain 2016;157:1588–9. [DOI] [PubMed] [Google Scholar]
- Wager TD, Atlas LY, Lindquist MA. et al. An fMRI-based neurologic signature of physical pain. N Engl J Med 2013;368:1388–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiech K. Deconstructing the sensation of pain: the influence of cognitive processes on pain perception. Science 2016;354:584–7. [DOI] [PubMed] [Google Scholar]
- Williams AC. What can evolutionary theory tell us about chronic pain? Pain 2016;157:788–90. [DOI] [PubMed] [Google Scholar]
- Williams ACC, Fisher E, Hearn L, Eccleston C. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev 2020;8:CD007407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegelstein RC. Personomics: the missing link in the evolution from precision medicine to personalized medicine. J Pers Med 2017;7:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analysed in support of this research.


