Abstract
Background and objective
There is currently no FDA-approved medical therapy for delayed graft function (DGF). Dexmedetomidine (DEX) has multiple reno-protective effects preventing ischemic reperfusion injury, DGF, and acute kidney injury. Therefore, we aimed to evaluate the reno-protective effects of perioperative DEX during renal transplantation.
Methods
A systematic review and meta-analysis synthesizing randomized controlled trials (RCTs) from WOS, SCOPUS, EMBASE, PubMed, and CENTRAL until June 8th, 2022. We used the risk ratio (RR) for dichotomous outcomes and the mean difference for continuous outcomes; both presented with the corresponding 95% confidence interval (CI). We registered our protocol in PROSPERO with ID: CRD42022338898.
Results
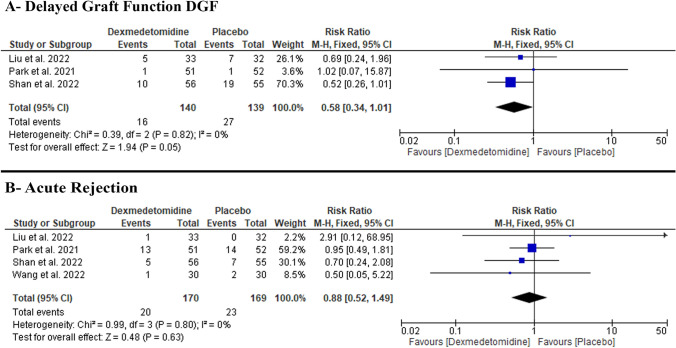
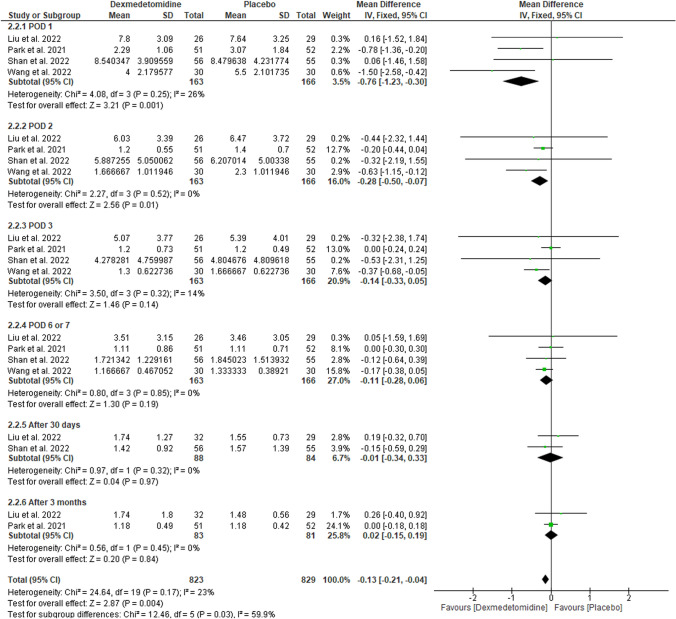
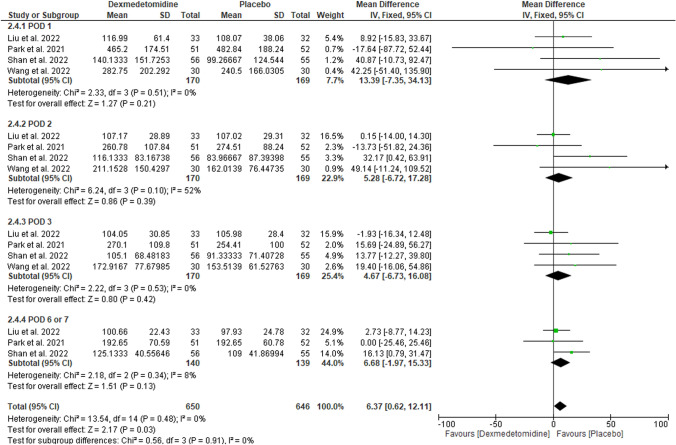
We included four RCTs with 339 patients. Pooled risk ratio found no difference between DEX and placebo in reducing DGF (RR: 0.58 with 95% CI [0.34, 1.01], p = 0.05) and acute rejection (RR: 0.88 with 95% CI [0.52, 1.49], p = 0.63). However, DEX improved short-term creatinine on day 1 (MD: − 0.76 with 95% CI [− 1.23, − 0.3], p = 0.001) and day 2 (MD: − 0.28 with 95% CI [− 0.5, − 0.07], p = 0.01); and blood urea nitrogen on day 2 (MD: − 10.16 with 95% CI [− 17.21, − 3.10], p = 0.005) and day 3 (MD: − 6.72 with 95% CI [− 12.85, − 0.58], p = 0.03).
Conclusion
Although there is no difference between DEX and placebo regarding reducing DGF and acute rejection after kidney transplantation, there may be some evidence that it has reno-protective benefits because we found statistically significant improvement in the short-term serum creatinine and blood urea nitrogen levels. More trials are required to investigate the long-term reno-protective effects of DEX.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11255-023-03568-3.
Keywords: DEX, Dexmedetomidine, Kidney transplantation, Systematic review, Meta-analysis
Introduction
End-Stage Renal Disease (ESRD) is a global health burden. In the 2021 annual report, the United States Renal Data System (USRDS) reported a continuous increase in the ESRD prevalence over the years, with 2302 cases per million in 2019 compared to 1582 cases per million in 2000 [1]. Dialysis and kidney transplantation are the only treatment options for ESRD. Transplantation is superior to dialysis in every aspect. With the increase in ESRD cases, the Kidney transplantation rate increased from 15,220 in 2000 to 24,502 in 2019 [2]. Patients receiving kidney transplants are at a greater risk for graft ischemia–reperfusion injury (IRI), which decreases the rates of transplantation success [3, 4].
The transplanted kidney suffers from ischemia and a lack of nutrients during renal transplantation. Ischemia starts with sympathetic overactivity from the surgical stress causing vasoconstriction of the renal arteries [5]. Moreover, transplanting kidneys from deceased donors, clamping the renal arteries, and prolonging the time interval between extraction, transport, and implantation can further make the kidney more vulnerable to ischemic effects [5]. On restoring the blood flow after transplantation, the graft becomes at risk of oxidative injury and inflammation, damaging the tubular and endothelial cells, and eventually leading to IRI [4]. IRI can lead to delayed graft function (DGF), reduced graft survival, and acute kidney rejection [6–8].
Dexmedetomidine (DEX) is an alpha-2-adrenoreceptor agonist [9] that has procedural sedative, analgesic, sedative, anxiolytic, and sympatholytic effects [10, 11]. DEX downregulated the inflammatory reactions in rats [12]. Furthermore, in the meta-analysis conducted by Wang et al. [13] over 60–70 studies in surgical patients, they found that DEX attenuated perioperative stress, inflammation, and immune reactions compared to the control group [13]. Yang et al. [14] and Li et al. [15] reported that DEX reduced the activation of NLRP3 inflammasome. Regarding renal effects, on one hand, DEX was also reported to have a reno-protective effect against IRI and Acute Kidney Injury (AKI) [16–21] as well as DGF [22]. On the other hand, DEX might cause dose-dependent bradycardia and hypotension [23], which might adversely affect renal microcirculation [23, 24].
Despite the growing evidence about the reno-protective effects of DEX, its perioperative use in kidney transplantation is still inconclusive, with multiple recent trials investigating it [25–28]. Therefore, we performed this systematic review and meta-analysis to synthesize evidence from the published randomized controlled trials (RCTs) on the reno-protective efficacy of perioperative DEX in patients undergoing kidney transplantation.
Methodology
Protocol registration
Our review procedure was registered and published in PROSPERO with ID: CRD42022338898. We conducted a systematic review and meta-analysis sincerely guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [29] and the Cochrane Handbook of Systematic reviews and meta-analysis [30]. The PRISMA 2020 checklist is illustrated in Table S1.
Data sources and search strategy
Web of Science, SCOPUS, EMBASE, PubMed (MEDLINE), and Cochrane Central Register of Controlled Trials (CENTRAL) were systematically searched by two reviewers (B.A. and M.T.) from inception until June 8th, 2022. No search filters were used. The detailed search approach and results are outlined in Table S2.
Eligibility criteria
We included RCTs with the following PICO criteria: population (P): patients receiving either living or deceased-donor kidney transplant; intervention (I): perioperative DEX regardless of dosage and duration of administration; control (C): saline placebo; outcomes (O): primary outcomes: incidence of DGF defined as required dialysis within one week following transplantation [31, 32] and incidence of acute graft rejection. Our secondary outcomes are the post-transplant kidney function tests irrespective of the postoperative day (POD) of assessment (creatinine, cystatin, blood urea nitrogen (BUN), urine output, and glomerular filtration rate (GFR).
Animal studies, pilot studies, observational studies (cohort, case–control, cross-sectional, case series, and case reports), single-arm clinical trials, in vitro studies (tissue and culture studies), book chapters, editorials, press articles, and conference abstracts were all excluded from our analysis.
Study selection
After duplicates were removed using Covidence online software, two investigators (A.H. and A.M.) independently evaluated the titles and abstracts of the retrieved records. (5) Then, they checked the full texts of the relevant records for the previously mentioned eligibility criteria. To resolve any disagreements, a third reviewer (B.K.) was invited.
Data extraction
Using a pilot-tested extraction form, four reviewers (A.H., A.M., B.K., and M.A.A.) independently extracted the following data from the included articles: study characteristics (first author name, year of publication, country, study design, total participants, DEX’s dose and duration of administration, donor status, and follow-up duration); baseline information (age, sex, body mass index, hypertension, diabetes, dialysis history, ABO incompatibility, serum creatinine, and heart rate); efficacy outcomes data (incidence of DGF, acute rejection, and post-transplantation kidney function tests). Disagreements were resolved through discussion.
Risk of bias and quality assessment
Using The Cochrane Collaboration's technique for assessing the risk of bias in randomized trials, four reviewers (A.H., A.M., B.K., and M.A.A.) independently assessed the included studies for risk of bias (ROB) [33], based on the following domains: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other potential sources of bias. Disagreements were resolved by discussion. For the quality of evidence assessment, two reviewers (M.T. and B.A.) adopted the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) working group guidelines [34, 35]. Inconsistency, imprecision, indirectness, publication bias, and bias risk were considered. Our findings on the quality of evidence were justified, documented, and included in each outcome's reporting. Any disagreements were handled through consensus.
Statistical analysis
The statistical analysis was carried out with RevMan v5.3 software [36]. We pooled dichotomous outcomes using risk ratio (RR) presented with the corresponding 95% confidence interval (CI) and continuous outcomes using mean difference (MD) with 95% CI. We used the I-square and Chi-square tests to examine heterogeneity; the Chi-square test determines if there is substantial heterogeneity, while the I-square determines the magnitude of heterogeneity. A substantial heterogeneity (for the Chi-square test) is defined as an alpha level below 0.1, according to the Cochrane Handbook (chapter nine) [30], while the I-square test is interpreted as follows: (0–40%: not significant; 30–60%: moderate heterogeneity; 50–90%: substantial heterogeneity; and 75–100%: considerable heterogeneity). We utilized the fixed-effects model. We also conducted a subgroup analysis depending on the time of assessment. Because we only included less than ten studies in each outcome, we did not conduct funnel plots to reveal publication bias, as advised by Egger et al. [37].
Results
Search results and study selection
We identified 1334 records after databases searching, then 430 duplicates were excluded. Title and abstract screening excluded 889 irrelevant records. We proceeded to full-text screening with 15 articles, 11 articles were excluded, and finally, only four articles met our inclusion criteria. The PRISMA flow chart of the detailed selection process is demonstrated in Figure S1.
Characteristics of included studies
We included four trials [25–28] with a total of 339 participants who were randomized to either perioperative DEX (n = 170) or saline infusion (n = 169). Further included trials’ characteristics are presented in Table 1. DEX was administered after induction of anesthesia till the end of the operation in two trials [26, 27], with one trial administrating DEX for 15 min before the induction of anesthesia and until 30 min after it [25] and another until two hours after the end of surgery [28]. The mean age of the DEX group and the control group are (43.67 ± 22.57) and (43.33 ± 14.79), respectively. Female participants were a total of 142 (39.9%) divided between the DEX group and the control group, 70 (39.8%) and 72 (41.1%) participants, respectively. Further baseline characteristics of the participants are presented in Table 2.
Table 1.
Summary characteristics of the included trials
| Study ID | Study design | Country | Graft source | Total participants | DEX dose | Primary outcome | DGF definition | Rejection confirmation method |
|---|---|---|---|---|---|---|---|---|
| Liu et al. 2022 [25] | Single-center, double-blinded RCT | China | Deceased donors | 65 | Initial loading dose of (0.6 μg/kg IV) over 15 min before anesthesia, then infusion of (0.4 μg/kg/h) until 30 min after reperfusion of transplanted kidney | Concentrations of KIM-1, Cr, blood urea, β2-MG, CysC, eGFR), and urine output | Need for dialysis during the first week after transplantation | N/A |
| Park et al. 2021 [26] | Single-center, double-blinded RCT | South Korea | Living donors | 103 | Infusion of (0.4 μg/kg/h) starting immediately after anesthesia induction and until the end of surgery | Cr concentration on POD7 | Need for dialysis during the first week after transplantation | Biopsy |
| Shan et al. 2022 [27] | Single-center, double-blinded RCT | China | Deceased donors | 111 | Infusion of (0.4 μg/kg/h) starting immediately after anesthesia induction and until the end of surgery | DGF | Need for dialysis during the first week after transplantation | Biopsy |
| Wang et al. 2022 [28] | Single-center, single-blinded RCT | Taiwan | Living donorsa | 60 | Infusion of (0.1–0.7 μg/kg/h) according to the patient response, starting immediately after anesthesia induction and until two hours after the end of surgery | Cr concentration on POD2 | N/A | N/A |
RCT randomized controlled trials, DEX dexmedetomidine, IV intravenous, DGF delayed graft function, KIM-1 urinary kidney injury molecule-1, Cr serum Creatinine, β2-MG β2 microglobulin, CysC Cystatin C, eGFR estimated glomerular filtration rate, POD postoperative day, N/A not available
aWith 2 participants receiving kidney grafts from deceased donors
Table 2.
Baseline characteristics of the participants
| Study ID | No. of patients | Age (years) Mean (SD) |
Gender (female) No. (%) |
Comorbidity N. (%) |
BMI Mean (SD) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HTN | DM | |||||||||||
| DEX | Control | DEX | Control | DEX | Control | DEX | Control | DEX | Control | DEX | Control | |
| Liu et al. 2022 [25] | 33 | 32 | 40.76 (8.78) | 42.59 (9.49) | 10 (30.30) | 6 (18.75) | N/A | N/A | N/A | N/A | 24.15 (3.87) | 23.20 (3.07) |
| Park et al. 2021 [26] | 51 | 52 | 50 (8.39) | 48.33 (12.96) | 28 (55) | 29 (56) | 45 (88) | 45 (87) | 18 (35) | 14 (30) | N/A | N/A |
| Shan et al.2022 [27] | 56 | 55 | 43.5 (10.7) | 43.3 (10.9) | 20 (35.7) | 27 (49.1) | 56 (100) | 55 (100) | 3 (5.4) | 3 (5.5) | 21.8 (3.2) | 21.1 (3.2) |
| Wang et al. 2022 [28] | 30 | 30 | 43.67 (22.57) | 43.33 (14.79) | 12 (40) | 10 (33) | 25 (83) | 16 (53) | 4 (13) | 6 (20) | N/A | N/A |
| Study ID | Dialysis history | ABO incompatibility N. (%) |
Creatinine Mg/dl Mean (SD) |
Hear rate, bpm Mean (SD) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Duration Mean (SD) |
Hemodialysis N. (%) |
Peritoneal dialysis N. (%) |
||||||||||
| DEX | Control | DEX | Control | DEX | Control | DEX | Control | DEX | Control | DEX | Control | |
| Liu et al. 2022 [25] | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 11.24 (3.74) | 10.64 (3.22) | 79.97 (14) | 77.94 (13.7) |
| Park et al. 2021 [26] | 2.33 (3.81) | 2.33 (3.81) | 41 (80) | 40 (77) | 6 (12) | 6 (12) | 24 (47) | 19 (37) | 5.9 (1.98) | 6.13 (1.83) | 62 (7.63) | 66 (13.72) |
| Shan et al.2022 [27] | 23.2 (20.16) | 31 (34.26) | 34 (61) | 38 (69) | 22 (39) | 17 (31) | N/A | N/A | 10.52 (3.00) | 10.28 (3.41) | 82.3 (13.1) | 80.5 (12.9) |
| Wang et al. 2022 [28] | N/A | N/A | 19 (63) | 17 (57) | 11 (37) | 13 (43) | 8 (27) | 9 (30) | 11.3 (4.1) | 11.5 (4.5) | 86 (14.79) | 87 (20.24) |
DEX dexmedetomidine, N/A not available, N number, SD standard deviation, bpm beat per minute
Risk of bias and quality of evidence
We assessed the quality of the included studies according to the Cochrane risk of bias tool, as shown in Figure S2. All of the included trials had a low risk of selection bias except Liu et al. [25], with a high risk of selection bias. Moreover, all included trials had a low risk of performance and detection biases except Wang et al. [28], with a high risk of performance and detection biases. Also, all of the included trials had a low risk of attrition bias except Liu et al. [25], with a high risk of attrition bias. Furthermore, all included trials had a low risk of reporting bias except Liu et al. [25], with an unclear risk of reporting bias. Finally, all of the included trials had a low risk of other biases. Author judgments are furtherly clarified in Table S3.
Using the GRADE system, all the included primary outcomes yielded low-quality evidence. Details and explanations are clarified in Table S4.
Primary outcomes
DGF
We found no difference between DEX and placebo regarding the incidence of DGF (RR: 0.58 with 95% CI [0.34, 1.01], p = 0.05) (low-quality evidence) (Fig. 1A, Table S4). The pooled studies were homogenous (p = 0.81, I-square = 0%).
Fig. 1.
Forest plot of the primary outcomes [A: delayed graft function (DGF), B: acute rejection]. I2 I-squared, CI confidence interval
Acute rejection
We found no difference between DEX and placebo regarding the incidence of acute rejection (RR: 0.88 with 95% CI [0.52, 1.49], p = 0.63) (low-quality evidence) (Fig. 1B, Table S4). The pooled studies were homogenous (p = 0.8, I-square = 0%).
Secondary outcomes
Creatinine (mg/dl)
The pooled mean difference favored DEX over placebo on POD 1 (MD: − 0.76 with 95% CI [− 1.23, − 0.3], p = 0.001), POD 2 (MD: − 0.28 with 95% CI [− 0.5, − 0.07], p = 0.01); however, we found no difference between DEX and placebo on POD 3 (MD: − 0.14 with 95% CI [− 0.33, 0.05], p = 0.14), POD 6/7 (MD: − 0.11 with 95% CI [− 0.28, 0.06], p = 0.19), after 30 days (MD: − 0.01 with 95% CI [− 0.34, 0.33], p = 0.97), and after three months (MD: 0.02 with 95% CI [− 0.15, 0.19], p = 0.84) (Fig. 2). Our results were homogenous with (p > 0.1, I-square > 50%).
Fig. 2.
Forest plot of creatinine (mg/dl). I2 I-squared, CI confidence interval
Urine output (mL/h)
We found no difference between DEX and placebo on POD 1 (MD: 13.39 with 95% CI [− 7.35, 34.13], p = 0.21), POD 2 (MD: 5.28 with 95% CI [− 6.72, 17.28], p = 0.39), POD 3 (MD: 4.67 with 95% CI [− 6.73, 16.08], p = 0.42), and POD 6/7 (MD: 6.68 with 95% CI [− 1.97, 15.33], p = 0.13) (Fig. 3). Our results were homogenous with (p > 0.1, I-square > 50%).
Fig. 3.
Forest plot of urine output (mL/h). I2 I-squared, CI confidence interval
Cystatin C (mg/L)
We found no difference between DEX and placebo on POD 1 (MD: − 0.15 with 95% CI [− 0.34, 0.05], p = 0.15), POD 2 (MD: − 0.02 with 95% CI [− 0.19, 0.16], p = 0.86), and after 30 days (MD: − 0.09 with 95% CI [− 0.29, 0.11], p = 0.38) (Figure S3). Our results were homogenous with (p > 0.1, I-square = 0%).
BUN (mg/dl)
The pooled mean difference favored DEX over placebo on POD 2 (MD: − 10.16 with 95% CI [− 17.21, − 3.10], p = 0.005), POD 3 (MD: − 6.72 with 95% CI [− 12.85, − 0.58], p = 0.03); however, we found no difference between DEX and placebo on POD 1 (MD: − 8.40 with 95% CI [− 17.98, 1.18], p = 0.09), POD 6/7 (MD: − 1.09 with 95% CI [− 6.80, 4.63], p = 0.71) (Figure S4). Our results were homogenous with (p > 0.1, I-square > 50%).
eGFR (mL/min/1.73 m2)
We found no difference between DEX and placebo on POD 6/7 (MD: − 4.09 with 95% CI [− 12.41, 4.24], p = 0.34), after 30 days (MD: − 0.14 with 95% CI [− 7.27, 7.00], p = 0.97), and after three months (MD: 0.30 with 95% CI [− 5.47, 6.06, p = 0.92) (Figure S5). Our results were homogenous with (p > 0.1, I-square = 0%).
Discussion
DEX has been reported to have reno-protective effects in different literature [16–22]. After analyzing the pooled data from the included RCTs [25–28], we found that perioperative infusion of DEX in patients undergoing renal transplantation decreased serum creatinine levels in POD1 and POD2 and serum BUN levels in POD2 and POD3, compared to placebo. However, we found no superiority of DEX compared to placebo in decreasing the incidences of DGF and acute graft rejection. Furthermore, postoperative levels of eGFR; cystatin c; urine output; BUN in POD 1 and POD 6/7; and creatinine in POD3, POD 6/7, POD 30, and POD 90 were similar in both DEX and placebo groups.
The reno-protective effects of DEX have been extensively investigated with multiple proposed mechanisms. First, DEX can prevent adrenergic vasoconstriction responses in the kidney and promote nitric oxide-dependent vasodilatation, sustaining glomerular filtration and renal blood flow [25, 38, 39]. Second, DEX inhibits ERK1/2 and NF-κB and modulates inflammatory cytokines decreasing TNF and IL-6, hence attenuating the systematic inflammatory response [25, 40–42]. Third, Liu et al. [25] detected decreased levels of kidney injury molecule 1 (KIM-1) with DEX compared to placebo. To clarify, KIM-1 is considered an ideal biomarker of kidney injury [25]. Moreover, KIM-1 has been reported to be a reliable predictor of inflammatory kidney injury and hence long-term graft survival [43, 44]. Finally, DEX can promote autophagy by reducing NLRP3 inflammasome activation; therefore, DEX ameliorates kidney IRI after transplantation [14].
Despite the previous reno-protective effects of DEX, our pooled analysis found no difference in DGF incidence. We can attribute this difference to the fact that most clinical trials evaluating the reno-protective effects of DEX excluded patients with deteriorated renal functions [20, 45, 46]. In this regard, assessing the reno-protective impact of DEX during kidney transplantation surgery in patients with renal impairment experiencing cold kidney ischemia may show different findings [25]. However, in a retrospective cohort, Chen et al. [29] reported decreased incidence of post-operative DGF with perioperative DEX injection. DGF in renal transplantation results from IRI and activation of the immune system. DGF is associated with biopsy-proven acute graft rejection [8], increased graft immunogenicity, decreased graft survival, and chronic graft failure [47]. Accordingly, preventing DGF in the early phase after renal transplantation is very critical in determining the long-term prognosis. To date, there is no FDA-approved treatment for DGF prevention, up to our knowledge. However, given our understanding of the DGF pathophysiology, measures decreasing the IRI, including vasodilators, antioxidants, anti-inflammatory, and immunosuppressive therapies, might help decrease its incidence.
Besides DGF, acute rejection is another complication that occurs because of IRI [7, 8]. Recipients with DGF are at a higher risk of developing acute graft rejection, with a 49% incidence of acute rejection in patients with DGF compared to 35% in those without DGF [48]. In line with our DGF findings, DEX was not different from the placebo in preventing acute graft rejection; however, Chen et al. [22] reported that perioperative DEX decreased the incidence of acute rejection in the early port transplantation phase. The rationale behind this difference is unclear, but our pooled analysis included few patients compared to Chen et al. [22]; hence, our analysis can be underpowered to detect this effect. Another reasonable rationale is that the ischemic injury of the graft starts directly after kidney organ recovery [49]. Accordingly, pre-treatment with DEX in the recipient alone is probably inadequate to prevent IRI, which is a pervasive limitation in the clinical research of organ transplantation [26].
Creatinine (Cr) level is also associated with the allograft function [50, 51]. It is suggested that a 0.3 mg/dl (25 μmol/l) increase in the serum Cr from baseline is an indicator of acute kidney injury and is associated with increased mortality risk and other adverse outcomes [52, 53]. Similarly, Pascual et al. [54] reported that early change in the serum Cr after transplantation was strongly correlated with long-term graft survival (> 10 years). To detect the early changes in the graft’s function, Park et al. [26] also targeted a 0.3 mg/dl (25 μmol/l) change in serum Cr levels. Compared to the placebo, DEX was superior in the short-term in the first 48 h after transplantation; however, DEX did not show superior effects in the post-transplantation serum Cr in POD7, after three months, and after six months.
Moreover, higher urine output early post-transplantation is associated with favorable graft outcomes [55]. It is difficult to determine the baseline urine output early after transplantation; however, it tends to stable by the first month [55]. Given the alpha-2-adrenoreceptor agonist activity of DEX, it can inhibit renin secretion and increase urine output. The use of DEX was associated with increased urine output in the first 24 h after coronary artery bypass graft surgery [55]. However, in our analysis, we did not find a significant increase in urine output in the DEX group compared to the placebo after transplantation. Of the included studies, only Shan et al. [27] reported an increase in urine output in the DEX group in POD2 and POD7.
Cystatin c inhibits lysosomal cysteine proteinases, and multiple studies have suggested its superiority in calculating GFR to determine renal function [56]. In a study conducted by White et al., GFR measurements derived from cystatin C were demonstrated to be more accurate than creatinine-based GFR measurements in kidney transplant patients when compared to the measured GFR [57]. Similarly, current eGFR equations which rely on creatinine measurements have been shown to lack accuracy in kidney transplant patients [32]. However, in our study, no difference in Cystatin C was observed between DEX treatment and placebo groups in POD 1, POD 2, or after 30 days. In the same line, a meta-analysis conducted by Shlikpak et al. involving 11 general-population studies and five studies of chronic kidney disease cohorts showed that utilizing cystatin c independently or in addition to creatinine when calculating eGFR ameliorates the usage of eGFR to assess the risk of ESRD as well as death [58]. Hence, we believe that further studying the utilization of cystatin c to evaluate kidney function in transplant patients may lead to a more accurate assessment of kidney graft function and improvements in patient outcomes.
BUN is a marker that is associated with urea excretion the excretory functions of the kidney [58]. Notably, Seki et al. conducted a study on patients with chronic kidney disease and found that increased BUN levels were associated with negative kidney outcomes irrespective of eGFR values [59]. Their findings suggested that BUN levels may play a greater role in evaluating renal functions in patients with chronic kidney disease than previously considered [59]. In our study, we found that the pooled mean difference of BUN favored the DEX as compared to the placebo on POD 2 and 3. However, no significant difference was exhibited between the DEX and placebo groups on POD 1. Although independent BUN levels cannot necessarily be indicative of renal function, the benefits observed on POD 2 and 3 with DEX treatment may be suggestive of improved excretory kidney function post-graft transplantation. Combined with the evidence from Seki et al. [59], we believe that BUN levels may be accurately considered in the kidney transplantation patient population and aid in the accurate assessment of renal function.
GFR is conventionally used to assess renal function as well as identify kidney disease stages. Many different equations have been determined to calculate GFR, which largely rely on creatinine levels, which can be influenced by several factors such as hydration, metabolic function, and drug interactions [60]. Estimated GFR or eGFR calculated using both creatinine and cystatin c levels have demonstrated greater accuracy as opposed to using one or the other [58, 60]. Moreover, creatinine-based eGFR is less accurate in patients with lower GFR or chronic kidney disease, and thus utilizing both cystatin c, and creatinine has been strongly suggested to accurately determine renal function in these patients [58, 60]. In our study, the results demonstrated no difference in eGFR between DEX or placebo groups in any of the time intervals, including POD 6, POD 7, after 30 days, or after three months. Based solely on these results, DEX treatment did not seem to influence renal function. As referenced earlier, eGFR loses its accuracy in patients with chronic kidney disease and determined renal function, so our results regarding eGFR values may not be indicative of true renal function, especially as subjects are post-graft transplantation.
In comparison with other procedures, perioperative infusion of DEX showed different results. Some studies reported a decrease in the incidence of acute kidney injury [20, 45, 46], while others reported no renal benefits of its use [55, 61, 62]. Perioperative DEX in liver transplantation decreased the IRI and improved graft outcomes through its sedative and immunosuppressive effects [63].
Despite the protective effects of DEX on IRI, DEX perioperative use is usually associated with the incidence of clinically significant bradycardia and hypotension [23, 24], and low cardiac output or low blood pressure can impair microcirculation [64]. Shan et al. [27] is the only included RCT that reported the incidence of bradycardia (16.1% vs. 9.1%) and hypotension (14.3% vs. 10.9%) in DEX and placebo groups, respectively, without statistically significant association [27]. Moreover, Wang et al. found that DEX has not affected the patency of sublingual microcirculation, implying the safety of DEX during kidney transplantation [28]. However, Liu et al. reported that DEX was associated with bradycardia without reporting clear data, and all cases were successfully treated with atropine [25].
Strengths
Our meta-analysis is the first to address the reno-protective effects of perioperative DEX in renal transplantation, according to our best knowledge. We also adhered to PRISMA guidelines while conducting this review [29]. Furthermore, we conducted a quality of evidence assessment using the most recent GRADE guidelines [34, 35].
Limitations
Our study has a few limitations: first, we only included four single-center RCTs with a relatively small number of participants. Second, several factors might alter the effect of DEX on kidney transplantation outcomes, including drug interactions, living versus deceased donors, post-transplantation complications, and management [63]. Third, DEX dosage and duration of perioperative infusion varied across the included RCTs, which may confound our findings. Fourth, we could not add the outcomes of bradycardia and hypotension in our meta-analysis as only one RCT [27] reported them. Finally, DGF assessment is dependent on physicians’ subjective experience, which may affect their decision on whether to dialyze graft recipients or not [26].
Conclusion
Evidence of DEX’s reno-protective effects in kidney transplantation is uncertain, with no difference compared to placebo in preventing DGF and acute rejection. However, we found statistically significant improvement in the short-term serum creatinine and blood urea nitrogen which warrants more multi-center, large-scale clinical trials to furtherly investigate the reno-protective effects of DEX, especially in the long-term.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
MT conceived the idea. BA and MT designed the research workflow. BA and MT searched the databases. AM, and AH screened the retrieved records, and BK resolved the conflicts. AM, AH, MAA, and BK extracted relevant data, assessed the quality of evidence, and MT resolved the conflicts. MT and BA performed the analysis. MT, AG, and AJ wrote the final manuscript. All authors have read and agreed to the final version of the manuscript.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). We received no funding for this study.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Annual Data Report|USRDS. https://adr.usrds.org/2021/end-stage-renal-disease/1-incidence-prevalence-patient-characteristics-and-treatment-modalities
- 2.(2021) Annual Data Report|USRDS. https://adr.usrds.org/2021/end-stage-renal-disease/7-transplantation. Accessed 20 Aug 2022
- 3.Smith SF, Hosgood SA, Nicholson ML. Ischemia-reperfusion injury in renal transplantation: 3 key signaling pathways in tubular epithelial cells. Kidney Int. 2019;95:50–56. doi: 10.1016/j.kint.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 4.Ponticelli C. Ischaemia-reperfusion injury: a major protagonist in kidney transplantation. Nephrol Dial Transpl. 2014;29:1134–1140. doi: 10.1093/ndt/gft488. [DOI] [PubMed] [Google Scholar]
- 5.Rosner MH, Portilla D, Okusa MD. Analytic reviews: cardiac surgery as a cause of acute kidney injury: pathogenesis and potential therapies. J Intensive Care Med. 2008;23:3–18. doi: 10.1177/0885066607309998. [DOI] [PubMed] [Google Scholar]
- 6.Chen R, Wang H, Song L, et al. Predictors and one-year outcomes of patients with delayed graft function after deceased donor kidney transplantation. BMC Nephrol. 2020;21:526. doi: 10.1186/s12882-020-02181-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perico N, Cattaneo D, Sayegh MH, Remuzzi G. Delayed graft function in kidney transplantation. Lancet. 2004;364:1814–1827. doi: 10.1016/S0140-6736(04)17406-0. [DOI] [PubMed] [Google Scholar]
- 8.Wu WK, Famure O, Li Y, Kim SJ. Delayed graft function and the risk of acute rejection in the modern era of kidney transplantation. Kidney Int. 2015;88:851–858. doi: 10.1038/ki.2015.190. [DOI] [PubMed] [Google Scholar]
- 9.Zhao Y, He J, Yu N, et al. Mechanisms of dexmedetomidine in neuropathic pain. Front Neurosci. 2020 doi: 10.3389/fnins.2020.00330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gerlach AT, Murphy CV, Dasta JF. An updated focused review of dexmedetomidine in adults. Ann Pharmacother. 2009;43:2064–2074. doi: 10.1345/aph.1M310. [DOI] [PubMed] [Google Scholar]
- 11.Abdelazeem B, Malik B, Mohamed MMG, et al. Meta-analysis comparing dexmedetomidine versus standard of care for sedation in patients with sepsis. Proc (Bayl Univ Med Cent) 2021;35:184–189. doi: 10.1080/08998280.2021.1997063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tan F, Chen Y, Yuan D, et al. Dexmedetomidine protects against acute kidney injury through downregulating inflammatory reactions in endotoxemia rats. Biomed Rep. 2015;3:365–370. doi: 10.3892/br.2015.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang K, Wu M, Xu J, et al. Effects of dexmedetomidine on perioperative stress, inflammation, and immune function: systematic review and meta-analysis. Br J Anaesth. 2019;123:777–794. doi: 10.1016/j.bja.2019.07.027. [DOI] [PubMed] [Google Scholar]
- 14.Yang T, Feng X, Zhao Y, et al. Dexmedetomidine enhances autophagy via α2-AR/AMPK/mTOR pathway to inhibit the activation of NLRP3 inflammasome and subsequently alleviates lipopolysaccharide-induced acute kidney injury. Front Pharmacol. 2020 doi: 10.3389/fphar.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Y, Pan Y, Gao L, et al. Dexmedetomidine attenuates pancreatic injury and inflammatory response in mice with pancreatitis by possible reduction of NLRP3 activation and up-regulation of NET expression. Biochem Biophys Res Commun. 2018;495:2439–2447. doi: 10.1016/j.bbrc.2017.12.090. [DOI] [PubMed] [Google Scholar]
- 16.Cai Y, Xu H, Yan J, et al. Molecular targets and mechanism of action of dexmedetomidine in treatment of ischemia/reperfusion injury. Mol Med Rep. 2014;9:1542–1550. doi: 10.3892/mmr.2014.2034. [DOI] [PubMed] [Google Scholar]
- 17.Gu J, Sun P, Zhao H, et al. Dexmedetomidine provides renoprotection against ischemia-reperfusion injury in mice. Crit Care. 2011;15:R153. doi: 10.1186/cc10283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ma J, Chen Q, Li J, et al. Dexmedetomidine-mediated prevention of renal ischemia-reperfusion injury depends in part on cholinergic anti-inflammatory mechanisms. Anesth Analg. 2020;130:1054. doi: 10.1213/ANE.0000000000003820. [DOI] [PubMed] [Google Scholar]
- 19.Tang C, Hu Y, Gao J, et al. Dexmedetomidine pretreatment attenuates myocardial ischemia reperfusion induced acute kidney injury and endoplasmic reticulum stress in human and rat. Life Sci. 2020;257:118004. doi: 10.1016/j.lfs.2020.118004. [DOI] [PubMed] [Google Scholar]
- 20.Soh S, Shim J-K, Song J-W, et al. Effect of dexmedetomidine on acute kidney injury after aortic surgery: a single-centre, placebo-controlled, randomised controlled trial. Br J Anaesth. 2020;124:386–394. doi: 10.1016/j.bja.2019.12.036. [DOI] [PubMed] [Google Scholar]
- 21.Kwiatkowski DM, Axelrod DM, Sutherland SM, et al. Dexmedetomidine is associated with lower incidence of acute kidney injury after congenital heart surgery. Pediatr Crit Care Med. 2016;17:128–134. doi: 10.1097/PCC.0000000000000611. [DOI] [PubMed] [Google Scholar]
- 22.Chen J, Perez R, de Mattos AM, et al. Perioperative dexmedetomidine improves outcomes of kidney transplant. Clin Transl Sci. 2020;13:1279–1287. doi: 10.1111/cts.12826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee S. Dexmedetomidine: present and future directions. Korean J Anesthesiol. 2019;72:323–330. doi: 10.4097/kja.19259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tripodaki ES, Tasoulis A, Koliopoulou A, et al. Microcirculation and macrocirculation in cardiac surgical patients. Crit Care Res Pract. 2012;2012:654381. doi: 10.1155/2012/654381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu Z, Jin Y, Feng C, et al. Renoprotective effect of intraoperative dexmedetomidine in renal transplantation. Comput Math Methods Med. 2022 doi: 10.1155/2022/9275406. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 26.Park JH, Koo BN, Kim MS, et al. Effects of intraoperative dexmedetomidine infusion on renal function in elective living donor kidney transplantation: a randomized controlled trial. Can J Anesth. 2022;69:448–459. doi: 10.1007/s12630-021-02173-1. [DOI] [PubMed] [Google Scholar]
- 27.Shan X, Hu L, Wang Y, et al. Effect of perioperative dexmedetomidine on delayed graft function following a donation-after-cardiac-death kidney transplant. JAMA Netw Open. 2022;5:e2215217. doi: 10.1001/jamanetworkopen.2022.15217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang YC, Wang MJ, Lee CY, et al. Effects of perioperative dexmedetomidine infusion on renal function and microcirculation in kidney transplant recipients: a randomised controlled trial. Ann Med. 2022;54:1233–1243. doi: 10.1080/07853890.2022.2067351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 doi: 10.1136/BMJ.N71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. Cochrane Handb Syst Rev Interv. 2019 doi: 10.1002/9781119536604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ann Lim M, Bloom RD. Medical therapies to reduce delayed graft function and improve long-term graft survival are we making progress? Clin J Am Soc Nephrol. 2020;15:13–15. doi: 10.2215/CJN.13961119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kasiske BL, Zeier MG, Craig JC, Ekberg H, Garvey CA, Green MD, Jha V, Josephson MA, Kiberd BA, Kreis HA, McDonald RA, Newmann JM, Obrador GT, Chapman JR, Flavio GVSA. KDIGO—Kidney Disease Improving Global Outcomes: Transplant Work Group. Clinical Practice guideline for the care of Kidney transplant recipients. Am J Transpl. 2009;9:S1–155. doi: 10.1111/j.1600-6143.2009.02834.x. [DOI] [PubMed] [Google Scholar]
- 33.Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011 doi: 10.1136/BMJ.D5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guyatt GH, Oxman AD, Kunz R, et al. Rating quality of evidence and strength of recommendations: what is “quality of evidence” and why is it important to clinicians? BMJ Br Med J. 2008;336:995. doi: 10.1136/BMJ.39490.551019.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guyatt GH, Oxman AD, Vist GE, et al. Rating quality of evidence and strength of recommendations: GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ Br Med J. 2008;336:924. doi: 10.1136/BMJ.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.RevMan|Cochrane Training. https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revman. Accessed 3 Aug 2021
- 37.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/BMJ.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee JE, Jung H, Cho JD, et al. The role of dexmedetomidine in hepatic ischemia-reperfusion injury via a nitric oxide-dependent mechanism in rats. Transpl Proc. 2021;53:2060–2069. doi: 10.1016/j.transproceed.2021.05.008. [DOI] [PubMed] [Google Scholar]
- 39.Fukuda M, Vazquez AL, Zong X, Kim SG. Effects of the α2-adrenergic receptor agonist dexmedetomidine on neural, vascular and BOLD fMRI responses in the somatosensory cortex. Eur J Neurosci. 2013;37:80–95. doi: 10.1111/ejn.12024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lempiäinen J, Finckenberg P, Mervaala EE, et al. Dexmedetomidine preconditioning ameliorates kidney ischemia-reperfusion injury. Pharmacol Res Perspect. 2014;2:3. doi: 10.1002/prp2.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Si Y, Bao H, Han L, et al. Dexmedetomidine attenuation of renal ischaemia-reperfusion injury requires sirtuin 3 activation. Br J Anaesth. 2018;121:1260–1271. doi: 10.1016/j.bja.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 42.Ji F, Li Z, Ypoung JN, et al. Post-bypass dexmedetomidine use and postoperative acute kidney injury in patients undergoing cardiac surgery with cardiopulmonary bypass. PLoS ONE. 2013;8:10. doi: 10.1371/journal.pone.0077446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xu PC, Zhang JJ, Chen M, et al. Urinary kidney injury molecule-1 in patients with IgA nephropathy is closely associated with disease severity. Nephrol Dial Transpl. 2011;26:3229–3236. doi: 10.1093/ndt/gfr023. [DOI] [PubMed] [Google Scholar]
- 44.Van Timmeren MM, Vaidya VS, Van Ree RM, et al. High urinary excretion of kidney injury molecule-1 is an independent predictor of graft loss in renal transplant recipients. Transplantation. 2007;84:1625–1630. doi: 10.1097/01.tp.0000295982.78039.ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Balkanay OO, Goksedef D, Omeroglu SN, Ipek G. The dose-related effects of dexmedetomidine on renal functions and serum neutrophil gelatinase-associated lipocalin values after coronary artery bypass grafting: a randomized, triple-blind, placebo-controlled study. Interact Cardiovasc Thorac Surg. 2015;20:209–214. doi: 10.1093/ICVTS/IVU367. [DOI] [PubMed] [Google Scholar]
- 46.Cho JS, Shim JK, Soh S, et al. Perioperative dexmedetomidine reduces the incidence and severity of acute kidney injury following valvular heart surgery. Kidney Int. 2016;89:693–700. doi: 10.1038/ki.2015.306. [DOI] [PubMed] [Google Scholar]
- 47.Siedlecki A, Irish W, Brennan DC. Delayed graft function in the kidney transplant. Am J Transpl. 2011;11:2279–2296. doi: 10.1111/j.1600-6143.2011.03754.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yarlagadda SG, Coca SG, Formica RN, et al. Association between delayed graft function and allograft and patient survival: a systematic review and meta-analysis. Nephrol Dial Transpl. 2009;24:1039–1047. doi: 10.1093/ndt/gfn667. [DOI] [PubMed] [Google Scholar]
- 49.Kosieradzki M, Rowiński W. Ischemia/reperfusion injury in kidney transplantation: mechanisms and prevention. Transpl Proc. 2008;40:3279–3288. doi: 10.1016/j.transproceed.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 50.Lezaic V, Dajak M, Radivojevic D, et al. Cystatin C and serum creatinine as predictors of kidney graft outcome. Int Urol Nephrol. 2014;46:1447–1454. doi: 10.1007/s11255-013-0624-7. [DOI] [PubMed] [Google Scholar]
- 51.Goldberg RJ, Weng FL, Kandula P. Acute and chronic allograft dysfunction in kidney transplant recipients. Med Clin North Am. 2016;100:487–503. doi: 10.1016/j.mcna.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 52.Nanda R, Zanotti-Cavazzoni SL. Early changes in organ function predict eventual survival in severe sepsis. Yearb Crit Care Med. 2007;2007:207–209. doi: 10.1016/s0734-3299(08)70353-8. [DOI] [PubMed] [Google Scholar]
- 53.Lassnigg A, Schmidlin D, Mouhieddine M, et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol. 2004;15:1597–1605. doi: 10.1097/01.ASN.0000130340.93930.DD. [DOI] [PubMed] [Google Scholar]
- 54.Pascual J, Marcén R, Zamora J, ét al. Very early serum creatinine as a surrogate marker for graft survival beyond 10 years. J Nephrol. 2009;22(1):90–98. [PubMed] [Google Scholar]
- 55.Khosroshahi HT, Oskui R, Shoja MM, et al. Time-dependent variations in urine output after renal transplantation. Transpl Proc. 2007;39:932–933. doi: 10.1016/j.transproceed.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 56.Santos J. Estimating glomerular filtration rate in kidney transplantation: still searching for the best marker. World J Nephrol. 2015;4:345. doi: 10.5527/wjn.v4.i3.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.White C, Akbari A, Hussain N, et al. Estimating glomerular filtration rate in kidney transplantation: a comparison between serum creatinine and cystatin C-based methods. J Am Soc Nephrol. 2005;16:3763–3770. doi: 10.1681/ASN.2005050512. [DOI] [PubMed] [Google Scholar]
- 58.Shlipak MG, Matsushita K, Ärnlöv J, et al. Cystatin C versus creatinine in determining risk based on kidney function. N Engl J Med. 2013;369:932–943. doi: 10.1056/nejmoa1214234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Seki M, Nakayama M, Sakoh T, et al. Blood urea nitrogen is independently associated with renal outcomes in Japanese patients with stage 3–5 chronic kidney disease: a prospective observational study. BMC Nephrol. 2019 doi: 10.1186/s12882-019-1306-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Musso CG, Álvarez-Gregori J, Jauregui J, Macías-Núñez JF. Glomerular filtration rate equations: a comprehensive review. Int Urol Nephrol. 2016;48:1105–1110. doi: 10.1007/s11255-016-1276-1. [DOI] [PubMed] [Google Scholar]
- 61.Moon T, Tsai JY, Vachhani S, et al. The use of intraoperative dexmedetomidine is not associated with a reduction in acute kidney injury after lung cancer surgery. J Cardiothorac Vasc Anesth. 2016;30:51–55. doi: 10.1053/j.jvca.2015.03.025. [DOI] [PubMed] [Google Scholar]
- 62.Bayram A, Esmaoglu A, Akin A, et al. The effects of intraoperative infusion of dexmedetomidine on early renal function after percutaneous nephrolithotomy. Acta Anaesthesiol Scand. 2011;55:539–544. doi: 10.1111/j.1399-6576.2011.02427.x. [DOI] [PubMed] [Google Scholar]
- 63.Lee CF, Cheng CH, Hung HC, et al. Sedative and immunosuppressive effects of dexmedetomidine in transplantation. Pharmaceuticals. 2021 doi: 10.3390/ph14080825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xu JY, Ma SQ, Pan C, et al. A high mean arterial pressure target is associated with improved microcirculation in septic shock patients with previous hypertension: a prospective open label study. Crit Care. 2015 doi: 10.1186/s13054-015-0866-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.