Abstract
Background:
Ethiopia ranked fourth in the world in terms of neonatal mortality rates, with birth asphyxia accounting for the majority of neonatal deaths.
Objective:
This study aimed to determine the prevalence of birth asphyxia and associated factors among newborns delivered in government hospitals of the Eastern Amhara region, Northeastern Ethiopia, 2022.
Methods:
A hospital-based cross-sectional study was conducted in 4 government hospitals between March 10, 2022, and May 8, 2022. The subjects in the study were selected using a systematic random sampling technique. Face-to-face interviews and chart reviews were used to collect the data. The association was discovered through multivariate logistic regression analysis.
Result:
In this study, the prevalence of birth asphyxia was 13.1% (48) of the total 367 newborns. Mothers who could not read and write (AOR = 9.717; 95% CI = 3.06, 10.857); infants born with low birth weight (AOR = 2.360; 95% CI = 1.004, 5.547); primipara mothers (AOR = 5.138; 95% CI = 1.060, 26.412); mothers with less than 37 weeks of gestation (AOR = 4.261; 95% CI = 1.232, 14.746); and caesarian section delivery (AOR = 2.444; 95% CI = 1.099, 5.432) were predictors of birth asphyxia.
Conclusion:
The magnitude of birth asphyxia has managed to remain a health concern in the study setting. As a result, special attention should be paid to uneducated and primi-mothers during antenatal care visits, and prematurity and caesarian section delivery complication reduction efforts should be bolstered to prevent birth asphyxia and its complications.
Keywords: Birth asphyxia, Eastern Amhara, adverse birth outcome, birth complications, Ethiopia
Introduction
Neonatal death is becoming an alarming problem globally. As an example, there were 2.4 million newborn deaths per year and 6700 deaths per day in 2020 worldwide. The Sub-Saharan Africa region has the world’s largest neonatal death rate and accounts for 43% of global newborn deaths. 1 Ethiopia has some of the highest neonatal mortality rates in the world, next to Sierra Leone, the Central African Republic, and Somalia, with 99 000 neonatal deaths reported in 2020, making it the fourth-highest neonatal death rate globally. 2
Birth asphyxia is characterized by an inability to initiate or maintain respiration at the baby's birth in a resource-limited setting, and that is 1 of the top reasons for neonatal mortality. 3 Accordingly, birth asphyxia, which is thought to be caused by intrapartum-related hypoxia-ischemia, accounts for 30 to 35% of neonatal deaths and 11% of under-5 child mortality worldwide.3 -5 Furthermore, it is responsible for approximately 280 000 neonatal deaths in Sub-Saharan Africa every year, with Ethiopia accounting for 34% of all neonatal deaths.6,7 Therefore, the incidence of birth asphyxia in low-resource countries (2 per 1000 live births) is ten times higher than in developed countries (26 per 1000 live births). 8 Furthermore, it is estimated that 20% of asphyxiated neonates will die within 1 month of birth, leaving 25% of survivors with permanent neurological deficits. 8 It is also responsible for 12.5% of all morbidities, including hypoxic-ischemic organ damage, severe life-long illness, developmental delays, epilepsy, and life-long functional psychotic syndromes. 9
Substantial evidence suggests that perinatal asphyxia is associated with socio-demographic factors, poor maternal health service utilization, inaccessible health facilities, and lack of skilled personnel, as well as antepartum and intrapartum-related factors.10 -13 It is estimated that three-quarters of all cases of perinatal asphyxia can be prevented, and providing neonatal resuscitation alone can prevent approximately 30% of intrapartum-related deaths.14,15 Nonetheless, the prevalence of neonatal death due to birth asphyxia is highly prevalent in sub-Saharan Africa, including Ethiopia.6,7 Ethiopia has agreed to meet the Sustainable Development Goals (SDGs) and has put in place major neonatal mortality strategies such as IMNCI, KMC, and improving NCIU service at the hospital level, qualified care provider training, essential newborn care, and neonatal resuscitation. 16 Despite these efforts to reduce perinatal asphyxia, neonatal death due to birth asphyxia remains a priority public health issue in Ethiopia. 16 .
Although many studies on perinatal asphyxia have been published in Ethiopia, particularly in the Amhara region,17 -20 there have been no studies undertaken in the eastern Amhara area, which includes public hospitals in the South Wollo, North Wollo, and Oromo special zones, concerning birth asphyxia. Thus, the goal of this study was to fill a knowledge gap about the magnitude and predictors of perinatal asphyxia in neonates delivered in government hospitals in the eastern Amhara region, Northeastern Ethiopia. As a result, health managers and professionals can identify gaps in preventive care and clinical standards for perinatal asphyxia at the hospital level.
Methods
Study design, area, and period
A hospital-based cross-sectional study was conducted in 4 government hospitals in the Eastern Amhara region from March 10, 2022, to May 8, 2022. The hospitals that took part in the study were Dessie Comprehensive and Specialized Hospital, Woldia Comprehensive and Specialized Hospital, Akesta Referral Hospital, and Kemisse General Hospital. These 4 government hospitals are estimated to serve over 10 million residents.
Study population
The study population consisted of mothers and newborn couples delivered in 4 randomly selected government hospitals in the Eastern Amhara Region during the survey period.
Eligibility criteria
This study included mothers who delivered with a gestational age greater than or equal to 28 weeks, volunteered to participate, and had a complete medical history. This study, on the other hand, excluded newborns with major congenital anomalies or syndromes, twins births, or incomplete medical records.
Sampling size determination
The sample size was calculated using a single population proportion formula with the following assumptions: a 95% confidence level, a 5% margin of error, a 32.50% prevalence from previous findings at Dessie Comprehensive Hospital, 21 and a 10% non-response rate. Finally, 367 mother-newborn pairs were included in the study.
Sampling technique
Of the total 10 public hospitals in the eastern Amhara region, 4 were selected using simple random technique through the lottery method. The average number of mothers due to give birth per month in each of the selected hospitals was calculated based on the number of mothers who gave birth in each of the selected hospitals in the quarter preceding the date of collection. Based on this, the total average number of deliveries per month was 1860 (600 in Dessie Hospital, 450 in Woldiya Hospital, 390 in Akesta Hospital, and 420 in Kemisse Hospital). Then, in the selected hospitals, a commensurate allotment based on size was made. As a result, 118 mother-newborn pairs were involved at Dessie Comprehensive Specialized Hospital, 89 at Woldiya Comprehensive Specialized Hospital, 77 at Akesta General Hospital, and 83 at Kemisse General Hospital. Ultimately, a systematic random sampling technique was used to obtain the mother-newborn pair for every 5th delivery.
Data collection tool and Techniques
The data collection instrument was adapted from the Ethiopian Demographic and Health Survey (EDHS) document.22 -24 The adapted tool was then modified and contextualized to fit the objectives of the study and translated into the local Amharic language. The tool was divided into 4 sections. The first section discusses sociodemographic factors gathered through face-to-face interviews, such as mothers’ educational status, occupational status, income, age, marital status, family size, and place of residence. The second section includes obstetrics and antepartum-related questions. Obstetric factors such as gravidity, parity, and a history of adverse birth outcomes were involved. Furthermore, antepartum-related factors included ANC visits, ANC initiation time and frequency, ANC visit interventions (TT vaccines, iron tablets), and whether or not a pregnancy-related medical illness occurred. Because the study was prospective, the missing variables in the maternal medical record related to obstetrics and antepartum were addressed through a face-to-face interview. The third section deals with intrapartum-related factors like labor process, hospital arrival, mode of delivery, labor durations, fetal presentations, the onset of rapture of membrane, amniotic fluid status, and whether labor was obstructed or not. These data were collected through chart review. The last section involved newborn characteristics such as newborn sex, gestational age, APGAR score, birth weight, and health problems experienced immediately after birth like asphyxia. The third section dealt with intrapartum-related factors such as labor process, hospital arrival, mode of delivery, labor durations, fetal presentations, the onset of membrane rupture, amniotic fluid status, and whether or not labor was obstructed. This information was gathered through chart review. The final section covered newborn characteristics such as newborn sex, gestational age, APGAR score, birth weight, and immediate postpartum newborn health problems such as asphyxia. The information was gathered by reviewing the newborn file. All deliveries took place at the study’s participating hospitals (Dessie, Woldiya, Akesta, and Kemisse), and newborns with health issues, including birth asphyxia, were transferred from the delivery unit to the NICU of each hospital. The instrument’s reliability was tested using Cronbach’s alpha among the 5% study population, which was 0.821, indicating that the instrument was reliable. Following the pretest, intrapartum variables such as fetal brady or tachy, as well as fetal movements, were removed from the instrument due to inconsistency in the review chart.
Statistical analysis
Training was provided to 4 BSc midwives hired as data collectors, and a pre-test was performed on 5% of the sample size at Haik General Hospital. The dataset was cleaned, encoded, and entered into Epi Info version 7.1.0 before being exported to the statistical package SPSS version 26 for analysis Descriptive statistics, binary and multivariate logistic regression analyses were used to analyze the data. During the binary logistic regression analysis, variables that had a P-value of less than .2 were included in the multivariate logistic regression analysis. Finally, in the multivariate logistic regression analysis, the strength of the association was determined using an odds ratio with a 95% confidence interval, and a P-value of .05 was used as a critical point to determine the association's significance.
Operational definitions
The APGAR score is a rating that is used in the early evaluation of a newborn. 3
Activity (score 0-2): if the baby was flaccid (score 0), some flexion (score 1), and well flexion (score 2). 25
Pulse (score 0-2): if the baby’s pulse was absent (score 0), less than 100 per minute (score 1), or greater than 100 per minute (score 2). 25
Grimace (score 0-2): If the baby did not respond (score 0), he or she will grimace (score 1) and cough or sneeze (score 2). 25
Appearance (score 0-2): If the baby was pale/blue (score 0), had blue extremities (score 1), or was completely pink (score 2). 25
Respiration (score 0-2): if the baby had absent breathing (score 0), weak breathing (score 1), and a good cry (score 2). 25
Level of APGAR score: an APGAR score of 0 to 3 was considered low, a score of 4 to 6 was considered moderate, and a score of 7 to 10 was considered normal. 25
Perinatal asphyxia (PNA) is diagnosed whenever the newborn baby does not cry and requires resuscitation, or if the APGAR score at the 5th minute is less than 7. 3
Stage I PNA was diagnosed when the level of consciousness was hyper-alert, muscle tone and posture were normal, myoclonus was present, the Moro reflex was strong, the pupils were in mydriasis, there were no seizures, the duration was less than 24 hours, and the outcome was good. 25
Stage II PNA was diagnosed when the level of consciousness was lethargic, muscle tone was hypotonic, posture was flexion, tendon reflexes or clonus were hyperactive, myoclonus was present, the Moro reflex was weak, the pupils were in miosis, seizures were common, the duration was between 24 hours to 14 days, and the outcome was variable. 25
Stage III PNA was diagnosed when the level of consciousness was stuporous, muscle tone was flaccid, posture was decerebrate, tendon reflexes or clonus were absent, myoclonus was absent, the Moro reflex was absent, the pupils were in unequal or poor light reflex, seizures were decerebrated, the duration was days to weeks, and the outcome was death or severe deficits. 25
Result
Respondents’ socio-demographic profile
The study enrolled 367 mother-to-newborn pairs, yielding a response rate of 100%. The mother’s mean age was 27.8 years (SD ± 4.6 years), and the preponderance of these women, 68.7% (252), were between the ages of 21 and 34. Moreover, about 58.6% (215) of respondents were urban residents. Of the total respondents, 90.2% (331), were married, 75.5% (277) had a family size of <4, 54% (198) were housewives by occupation, and 25.1% (92) had secondary education status (Table 1).
Table1.
Socio-demographic characteristics of mothers who gave birth in government hospitals of Eastern Amhara Region, Northeastern Ethiopia, 2022 (n = 367).
| Variables | Frequency (n = 367) | Percent |
|---|---|---|
| Age of mothers | ||
| 19-20 y | 53 | 14.4 |
| 21-34 y | 252 | 68.7 |
| 35-49 y | 62 | 16.9 |
| Residence | ||
| Rural | 152 | 41.4 |
| Urban | 215 | 58.6 |
| Religion | ||
| Orthodox | 107 | 29.2 |
| Protestant | 11 | 3 |
| Muslim | 249 | 67.8 |
| Number of family size | ||
| <4 | 277 | 75.5 |
| ≥4 | 90 | 24.5 |
| Marital status | ||
| Married | 331 | 90.2 |
| Single | 18 | 4.9 |
| Divorced | 16 | 4.4 |
| Windowed | 2 | .5 |
| Occupational status | ||
| Housewife | 198 | 54 |
| Civil servant | 35 | 9.5 |
| Farmer | 74 | 20.2 |
| Merchant | 48 | 13.1 |
| Others | 12 | 3.3 |
| Educational status | ||
| Unable to read and write | 90 | 24.5 |
| Only able to read and write | 45 | 12.3 |
| Primary education (1-8 grade level) | 87 | 23.7 |
| Secondary education (9-12 grade level) | 92 | 25.1 |
| Tertiary education (college or university graduate) | 53 | 14.4 |
Obstetrics and antepartum related factors
Regarding obstetric characteristics, 56.7% (208) and 50.1% (184) mothers were multigravida and multipara, respectively. Forty-five (12.3%) of mothers had previous adverse birth results. Although nearly all 96.2% (353) mothers had ANC follow-up during their current pregnancy, only 65.4% (240) of participants had 4 or more ANC visits, and just 51.5% (189) of mothers had early ANC visits. Moreover, 92.4% (339) mothers received TT vaccines, 78.5% (288) were given iron supplements, and 40.6% (149) had complications during their current pregnancy. Eclampsia, Antepartum Hemorrhage (APH), and infection were the leading causes of these complications in 19.9% (73), 11.7% (43), and 4.63% (17) of mothers, respectively (Table 2).
Table 2.
Obstetrics and antepartum-related characteristics of mothers who gave birth in government hospitals in Amhara Eastern Region, in 2022 (n = 367).
| Obstetrics and antepartum related factors | Frequency | Percent |
|---|---|---|
| Gravidity | ||
| Primigravida | 159 | 43.3 |
| Multigravida | 208 | 56.7 |
| Parity | ||
| Primipara | 183 | 49.9 |
| Multipara | 184 | 50.1 |
| Had a history of adverse birth results | ||
| Yes | 45 | 12.3 |
| No | 322 | 87.7 |
| ANC follow up | ||
| Yes | 353 | 96.2 |
| No | 14 | 3.8 |
| ANC time initiation | ||
| ≤12 wk | 189 | 51.5 |
| >13 wk | 164 | 44.7 |
| ANC follow-up frequency | ||
| <4 | 113 | 30.8 |
| ≥4 times | 240 | 65.4 |
| TT vaccine | ||
| Yes | 339 | 92.4 |
| No | 28 | 7.6 |
| Frequency of TT vaccine | ||
| Once | 48 | 13.1 |
| ≥2 times | 291 | 79.3 |
| History of iron intake | ||
| Yes | 288 | 78.5 |
| No | 79 | 21.5 |
| Medical illness during pregnancy | ||
| Yes | 149 | 40.6 |
| No | 218 | 59.4 |
| Type of medical illness during pregnancy | ||
| Eclampsia | 73 | 19.9 |
| APH | 43 | 11.7 |
| Infection | 17 | 4.63 |
| Gestational DM | 10 | 2.72 |
| Others | 6 | 1.63 |
Intrapartum related factors
The majority of the mothers, 83.1% (305), had a history of 37 or above weeks of gestational age. Of the total study participants, 79% (290) arrived at the hospital in the case of referral, 37.9% (139) of mothers had spontaneous labor onset, 77.4% (284) had less than 12 hours of labor duration, and 45% (165) of mothers were delivered through normal spontaneous vaginal delivery. The majority of study participants, 78.2% (287), underwent intrapartum rupture of the fetal membranes, while 80 (21.8%) underwent premature rupture. Meconium-stained amniotic fluid was observed in 15.5% (57) of the mothers after the membrane rupture. Furthermore, the majority 92.9% (341) of the fetuses had a cephalic presentation (Table 3).
Table 3.
Obstetrics and intrapartum attributes of mothers who delivered in government hospitals in northeast Ethiopia in the East Amhara region in 2022 (n = 367).
| Obstetric and intrapartum factors | Frequency (n = 367) | Percent |
|---|---|---|
| Labor process | ||
| Spontaneous | 139 | 37.9 |
| Induced | 228 | 62.1 |
| Hospital arrival | ||
| Referral | 290 | 79 |
| Emergency | 14 | 3.8 |
| Self-initiated | 63 | 17.2 |
| Mode of delivery | ||
| SVD | 165 | 45 |
| Instrumental delivery | 57 | 15.5 |
| CS | 145 | 39.5 |
| Gestational age | ||
| <37 wk | 62 | 16.9 |
| ≥37 wk | 305 | 83.1 |
| Labor duration | ||
| ≤12 h | 284 | 77.4 |
| >12 h | 83 | 22.6 |
| Presentation of the fetus at birth | ||
| Cephalic | 341 | 92.9 |
| Non-cephalic | 26 | 7.1 |
| Premature rupture of membrane | ||
| Yes | 80 | 21.8 |
| No | 287 | 78.2 |
| Status of amniotic fluid | ||
| Clear | 310 | 84.5 |
| Meconium stained | 57 | 15.5 |
| Obstructed labor | ||
| Yes | 246 | 67 |
| No | 121 | 33 |
| Delivery time | ||
| Day | 123 | 33.5 |
| Night | 244 | 66.5 |
Obstructed labor occurs when the baby is physically blocked from exiting the pelvis during childbirth despite the uterus contracting normally.
Newborn characteristics
Two hundred and sixteen (58.9%) of newborns were males. The majority of newborns, 83.1% (305), were born-to-term, 76.3% (280) weighed 2500g or more at birth, and 80.1% (294) and 86.92% (319) of newborns scored 7 to 10 APGAR at 1and 5 minutes, respectively. Besides, 25% (92) newborns had a health problem at birth. Of the total of 78 delivery complications experienced, perinatal asphyxia was responsible for approximately 61.54% (48) of cases, followed by chorioamnionitis 17.95% (14) and macrosomia 15.38% (12) (Table 4).
Table 4.
Characteristics of neonates delivered to government hospitals in eastern Amhara, north-eastern Ethiopia, 2022 (n = 367).
| Newborn characteristics | Frequency (n = 367) | Percent |
|---|---|---|
| Infant sex | ||
| Male | 216 | 58.9 |
| Female | 151 | 41.1 |
| Cry and had breathing at birth | ||
| Yes | 319 | 89.9 |
| No | 48 | 13.1 |
| APGAR score at 1 min | ||
| 7-10 | 319 | 86.9 |
| 4-6 | 40 | 10.9 |
| ≤3 | 8 | 2.2 |
| APGAR score at 5 min | ||
| 7-10 | 319 | 86.9 |
| 4-6 | 36 | 9.8 |
| ≤3 | 12 | 3.3 |
| Gestational age | ||
| Term (≥37 wk gestational age) | 305 | 83.1 |
| Pre-term (<37 wk gestational age) | 62 | 16.9 |
| Birth weight | ||
| ≥2500 g | 280 | 76.3 |
| <2500 g | 87 | 23.7 |
| Complications of deliveries | ||
| Yes | 92 | 25 |
| No | 275 | 75 |
| Types of complications of deliveries (N = 78) | ||
| Birth asphyxia | 48 | 61.54 |
| Chorioamnionitis | 14 | 17.95 |
| Macrosomia | 12 | 15.38 |
| Birth injury | 4 | 5.13 |
Hospital inventory on birth asphyxia
Each government hospital has a neonatal resuscitation corner and resuscitation materials such as Ambu bags, masks (0 and 1 size), suction material, and a stethoscope in the delivery room. After a successful resuscitation attempt in the delivery room, all babies were transferred to the Neonatal Intensive Care Unit for further treatment and evaluation. For stages II and III of perinatal asphyxia, all Neonatal Intensive Care Units had oxygen, fluid, and essential drugs. Only 57.8% (46) of the 81 midwifery professionals received neonatal resuscitation training. However, all neonatal nurses and comprehensive nurses in the Neonatal Intensive Care Unit received current neonatal resuscitation training. In the Neonatal Intensive Care Unit, there are only 4 pediatricians available in 2 hospitals (Dessie and Woldiya comprehensive hospitals). Furthermore, both the delivery room and the Neonatal Intensive Care Unit had the resuscitation flow chart and current guidelines. There were no special rooms in hospitals for the treatment of birth asphyxia, which increased the risk of hospital-acquired infection.
The extent of birth asphyxia
The prevalence of perinatal asphyxia was 13.1% (48) (Figure 1). Three-quarters (36) of the asphyxiated neonates were admitted with stage II PNA, and a quarter (12) were admitted with stage III PNA.
Figure 1.
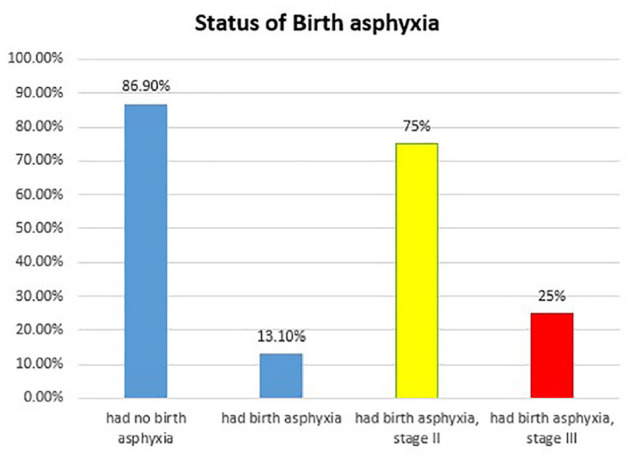
The prevalence of perinatal asphyxia in neonates delivered in government hospitals in the Eastern Amhara Region of North Eastern Ethiopia in 2022 (n = 367).
Birth asphyxia and associated factors
Upon making a bivariate logistic regression analysis, mothers who were unable to read or write, civil servants and others by occupation, and primipara mothers with less than 37 weeks of gestational age and CS were associated with perinatal asphyxia. Besides, those variables that had a P-value less than .2 during the bivariate analysis are transferred and analyzed in backward logistic regression.
The following variables were found to be predictors of birth asphyxia after performing a multivariable logistic regression analysis: mothers who were unable to read and write; low birth weight infants; primipara mothers who were less than 37 weeks of gestational age; and CS delivery. Moreover, the odds of birth asphyxia among mothers who are unable to read and write were almost 10 times higher (AOR = 9.717; 95% CI = 3.06, 10.857) compared to mothers with higher educational status. Similarly, those mothers who were only able to read and write were almost 3 times more likely (AOR = 3.163; 95% CI = 1.21, 8.334) to have birth asphyxia than mothers who had tertiary education status. Low-birth-weight infants and primipara mothers had roughly 2 times (AOR = 2.360; 95% CI = 1.004, 5.547) and 5 times (AOR = 5.138; 95% CI = 1.060, 26.412) higher odds of birth asphyxia than their counterparts. Besides, those mothers who had less than 37 weeks of gestational age were nearly 4 times more likely (AOR = 4.261; 95% CI = 1.232, 14.746) to have birth asphyxia than their counterparts. When CS participants were compared to those who had spontaneous vaginal delivery, the odds of birth asphyxia were nearly twice as high (AOR = 2.444; 95% CI = 1.099, 5.432). Finally, being a civil servant and other occupations were thought to have a protective effect against birth asphyxia (Table 5).
Table5.
Factors associated with perinatal asphyxia among newborns delivered in government hospitals of Eastern Amhara Region, North Eastern Ethiopia, 2022 (n = 367).
| Variables | Perinatal asphyxia | COR (CI; 95%) | AOR (CI; 95%) | P-value | |
|---|---|---|---|---|---|
| Yes (n) (%) | No (n) (%) | ||||
| Participant’s occupation | |||||
| Housewife | 20 (41.7%) | 178 (55.8%) | Reference | Reference | Reference |
| Civil servant | 11 (22.9%) | 24 (7.5%) | 0.245 (0.105, 0.574)* | 0.167 (0.066, 0.426)* | .003 |
| Farmer | 7 (14.6%) | 67 (21%) | 1.075 (0.435, 2.660) | 0.866 (0.333, 2.253) | .768 |
| Merchant | 6 (12.5%) | 42 (13.2%) | 0.787 (0.297, 2.080) | 0.720 (0.259, 2.000) | .529 |
| Others | 4 (8.3%) | 8 (2.5%) | 0.225 (0.062, 0.813)* | 0.379 (0.096, 1.495) | .166 |
| Educational status | |||||
| Unable to read and write | 6 (12.5%) | 84 (26.3%) | 4.658 (1.651, 13.147)* | 9.717 (3.06, 10.857)** | .000 |
| Only able to read and write | 9 (18.8%) | 36 (11.3%) | 1.695 (0.726, 3.956) | 3.163 (1.201, 8.334)** | .002 |
| Primary education | 14 (29.2%) | 73 (22.9%) | 1.3 (0.497, 3.401) | 1.736 (0.600, 5.028) | .309 |
| Secondary education | 6 (12.5%) | 86 (27%) | 4.55 (1.611, 12.848) | 5.940 (1.971, 17.905) | .407 |
| Tertiary education | 13 (27.1%) | 40 (12.5%) | Reference | Reference | Reference |
| Newborn birth weight | |||||
| Normal birth weight (>2500 g) | 41 (85.4%) | 239 (74.9%) | Reference | Reference | Reference |
| Low birth weight (<2500 g) | 7 (14.1%) | 80 (25.1%) | 1.961 (0.846, 4.544) | 2.360 (1.004, 5.547)** | .000 |
| Parity | |||||
| Primipara | 29 (60.4%) | 144 (45.1%) | 4.5 (1.059, 19.116)* | 5.138 (1.060, 26.412)** | .014 |
| Multipara | 16 (33.3%) | 168 (52.7%) | 2.128 (0.519, 8.717) | 1.954 (0.393, 9.721) | .457 |
| Nullipara | 3 (6.3%) | 7 (2.2%) | Reference | Reference | Reference |
| Gestational age | |||||
| < 7 wks | 3 (6.3%) | 59 (18.5%) | 3.404 (1.023, 11.328)* | 4.261 (1.232, 14.746)** | .020 |
| ≥37 wks | 45 (93.8%) | 260 (81.5%) | Reference | Reference | reference |
| Mode of delivery | |||||
| SVD | 25 (52.1%) | 140 (43.9%) | Reference | Reference | Reference |
| Instrumental delivery | 12 (25.0%) | 45 (14.1%) | 0.670 (0.311, 1.440) | 0.731 (0.320, 1.670) | .50 |
| CS | 11 (22.9%) | 134 (42.0%) | 2.175 (1.030, 4.594)* | 2.444 (1.099, 5.432)** | .028 |
In bivariate and multivariable analysis, * and ** denote statistically significant associations at P.05, respectively.
Discussion
The magnitude of perinatal asphyxia in this study was significant, and it remains a public health issue in the study area. Birth asphyxia has been linked to an uneducated mother, a low-birth-weight infant, a primiparous mother, a gestational age of less than 37 weeks, and a CS delivery. Based on this study's findings, the prevalence of perinatal asphyxia was 13.1% (48), which is consistent with research findings from Gondar Teaching Hospital, northwest Ethiopia (12.5%), Nigist Elene Hospital, southern Ethiopia (15.1%), and Jimma Zone, southwest Ethiopia (12.5%).9,26,27 Furthermore, it is comparable to the studies conducted in Eastern Africa (15.9%) and Nigeria (11.1%).10,28 However, the findings of this survey are markedly below the national average value for Ethiopia (22.8%), 14 the Tigray region, northern Ethiopia (22.1%), 29 Ayder Hospital, northern Ethiopia (48%), 11 Bahirdar City, northwest Ethiopia (21.7%), 30 and the North-Eastern Amhara (22.6%). 31 The disparity could be attributed to sampling size, the number of institutions, and population characteristics. However, this finding outperformed those of the Deredewa Hospital study by 2.5%, 32 which could be explained by discrepancies in the sample size, trends in health service accessibility during ANC and institutional delivery, and population characteristics such as Deredewa Hospital serving primarily urban residents.
According to this study's findings, newborns born to mothers who are unable to read or write are nearly ten times more likely to suffer from birth asphyxia than newborns born to mothers with a higher educational status. This is in line with studies conducted nationally 14 and at Diredewa Hospital. 32 This implies that preventive activities at the community and facility levels for adverse birth outcomes, such as birth asphyxia, should be strengthened. Furthermore, with a focus on illiterate mothers, early detection of abnormalities during pregnancy and labor, as well as the quality of delivery care, should be improved.
According to the findings of this study, babies born to primipara mothers were nearly 5 times more likely than their counterparts to suffer from birth asphyxia. This is similar to studies in Ethiopia, 14 including Nigist Elene Memorial Hospital, 26 North Eastern Amhara, 31 and Jimma Medical Center. 33 One possible explanation is that being a primipara mother increases the risk of complications during pregnancy and the intrapartum period due to the mother’s young age. 25 Indeed, primipara mothers are susceptible to mal-presentation and obstructed labor, including suffering from a lack of advancement in their labor process. 25 As a result, the risk of birth asphyxia is increased by all of the preceding factors. Furthermore, primipara mothers may be ignorant, have late initiation of and poor adherence to ANC, and fail to anticipate that their baby will have medical complications during pregnancy and delivery, resulting in a negative fetal outcome, including birth asphyxia.
Mothers who were less than 37 weeks of gestational age had twice the odds of birth asphyxia as their counterparts. This is in line with studies from Ethiopia, 14 including Nigist Elene Memorial Hospital, 26 Bahirdar City, 30 and Addis Ababa, 34 as well as Northern Tanzania, 35 Karachi, 36 and Indonesia. 37 This may be due to the cluelessness of body organs, particularly respiratory components, in newborn babies prior to 34 weeks after conception, who lack emulsifiers and may try to maintain respiration and tissue oxygenation upon birth. As a result, birth asphyxia can be severe at times, resulting in neurological damage such as cerebral palsy and necrotizing enterocolitis. 38 Premature infants are often more likely to develop co-morbidities, which will interfere with their normal postpartum functioning. 25 This implies that early detection and management of adverse birth outcomes during ANC visits, as well as having a well-organized neonatal intensive care unit service, must be improved at the health facility and hospital level to prevent major neonatal deaths due to birth asphyxia.
According to the study, a baby born via CS had nearly twice the risk of developing birth asphyxia as a baby born via spontaneous vaginal delivery. This is consistent with studies in Ethiopian regions such as Tigray, Addis Ababa, and the Jimma zone.27,29,34 This is also similar to the findings in Thailand, Nigeria, and Iran.39 -41 This could be because, apart from a vaginal birth, CS birth does not induce genital tract contraction yet can induce breathing exercise, which aids in fluid expulsion from the lungs and is more likely to cause respiratory distress. 42 Another possible explanation is that most indications of the CS jeopardize adequate oxygen delivery to the fetus. The clinical implication appears to be that CS delivery complications should be reduced and need more effort to improve. As a result, adverse birth outcomes such as birth asphyxia will be reduced.
Low birth weight neonates were nearly twice as likely as normal birth weight neonates to develop birth asphyxia. Similar study findings were observed in Ethiopia, 43 Pakistan, 36 and East Java. 44 This could be explained by the fact that because a large proportion of small babies are pre-term, they may not have enough surfactant, resulting in difficulty breathing, difficulty in cardiopulmonary transition, and subsequent birth asphyxia. 25
Conclusion
The extent of perinatal asphyxia in this study was significant but less than the national figure, and it managed to remain a health issue in the study area. Perinatal asphyxia was strongly associated with a mother’s inability to write and read, an infant born with low birth weight and a primiparous mother, having a gestational age of less than 37 weeks, and having a CS delivery. This implies that birth asphyxia prevention measures, such as paying special attention to uneducated and primi-mothers during antenatal care visits and prematurity reduction efforts, should be strengthened. To meet the national and Sustainable Development Goals, reducing caesarian section delivery complications will require significant effort.
Strengths and limitations
We used the Switchboard, a peer-reviewed and validated survey tool, and worked with more than 3 public hospitals. However, due to the nature of the study design, we were unable to establish a causal relationship. In addition, reviewing a medical chart might not always provide true information. As a result, an observational follow-up study with qualitative triangulation is required for further study.
Acknowledgments
The authors are grateful to the medical directors and professionals at Dessie Comprehensive and Specialized Hospital, Woldia Comprehensive and Specialized Hospital, Akesta Referral Hospital, and Kemisse General Hospital for their kind cooperation. We are also grateful to the data collectors and respondents to the study.
Abbreviations: APH: Antepartum Hemorrhage
APGAR: Appearance Pulse Activity and Respiratory rate
AOR: Adjusted Odds Ratio
ANC: Ante-Natal Care
COR: Crude Odds Ratio
CS: Caesarian Section
IMNCI: Integrated Management of Neonatal and Child Illness
KMC: Kangaroo Mother Care
PNA: Perinatal Asphyxia
SD: Standard Deviation
SDGs: Sustainable Development Goals
SVD: Spontaneous Vaginal Delivery
TT: Tetanus Toxoid
WHO: World Health Organization
ORCID iD: Muluken Amare Wudu  https://orcid.org/0000-0003-0292-6029
https://orcid.org/0000-0003-0292-6029
Declarations
Ethics Approval and Consent to Participate: The review committee of the College of Medicine and Health Science, Wollo University, Dessie, Ethiopia, vetted and approved the study procedures (WU/CMHS/425/2022) on March 2, 2022, and granted ethical approval. Dessie, Woldiya, Akesta, and Kemisse hospitals in the Amhara region also provided explicit consent letters. Having fully understood the purpose of the study, each respondent provided written consent prior to the interview. In addition, the study was carried out in accordance with the Declaration of Helsinki. Recalcitrant study participants were excluded from the survey. Anonymized data was collected, and participant information was kept confidential.
Consent for Publication: Not applicable.
Author Contributions: MAW contributed to conceptualization; data curation; formal analysis; investigation; methodology; project administration, software, writing – original draft. TAB contributed to conceptualization; data curation; formal analysis; methodology; project administration; writing – review and editing.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of Data and Materials: Any data produced or reviewed as part of this study are included in the manuscript and are also readily accessible to the corresponding author.
References
- 1. WHO. Newsroom/Fact sheets/Detail/Newborn Mortality; 28 January 2022. [Google Scholar]
- 2. United Nations Inter-agency Group for Child Mortality Estimation (UN IGME). Levels & trends in child mortality: Report 2021, estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation. United Nations Children’s Fund, New York; 2021. [Google Scholar]
- 3. Lawn JE, Kinney M, Blencowe H. Every newborn. An executive summary for The Lancet’s Series. Lancet. 2014;384:1-8.24998002 [Google Scholar]
- 4. United Nations Inter-Agency Group for Child Mortality Estimation. Levels & trends in child mortality: Report 2019, estimates developed by the United Nations Inter-Agency Group for Child Mortality Estimation. United Nations Children’s Fund; 2019. [Google Scholar]
- 5. Wang H, Liddell CA, Coates MM, et al. Global, regional, and national levels of neonatal, infant, and under-5 mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:957-979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization. Global health observatory data repository world health organization, 2015. World Health Organization; 2019. [Google Scholar]
- 7. UNICEF. World Bank; United Nations. Levels & trends in child mortality: Report 2014, Estimates developed by the UN Inter-Agency Group for Child Mortality Estimation, United Nations Children’s Fund; 2015. [Google Scholar]
- 8. Odd D, Heep A, Luyt K, Draycott T. Hypoxic-ischemic brain injury: Planned delivery before intrapartum events. J Neonatal Perinatal Med. 2017;10:347-533. [DOI] [PubMed] [Google Scholar]
- 9. Demisse AG, Alemu F, Gizaw MA, Tigabu Z. Patterns of admission and factors associated with neonatal mortality among neonates admitted to the neonatal intensive care unit of University of Gondar Hospital, Northwest Ethiopia. Pediatric Health Medi Ther. 2017;8:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Workineh Y, Semachew A, Ayalew E, Animaw W, Tirfie M, Birhanu M. Prevalence of perinatal asphyxia in East and Central Africa: systematic review and meta-analysis. Heliyon. 2020;6:e03793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gebregziabher GT, Hadgu FB, Abebe HT. Prevalence and associated factors of perinatal asphyxia in neonates admitted to ayder comprehensive specialized hospital, Northern Ethiopia: a cross-sectional study. Int J Pediatr. 2020;2020:4367248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bayih WA, Yitbarek GY, Aynalem YA, et al. Prevalence and associated factors of birth asphyxia among live births at Debre Tabor General Hospital, North Central Ethiopia. BMC Pregnancy Childbirth. 2020;20:1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Meshesha AD, Azage M, Worku E, Bogale GG. Determinants of birth asphyxia among newborns in referral hospitals of Amhara national regional state, Ethiopia. Pediatric Health Medi Ther. 2020;11:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Desalew A, Semahgn A, Tesfaye G. Determinants of birth asphyxia among newborns in Ethiopia: A systematic review and meta-analysis. Int J Health Sci. 2020;14:35. [PMC free article] [PubMed] [Google Scholar]
- 15. Manu A, Arifeen S, Williams J, et al. Assessment of facility readiness for implementing the WHO/UNICEF standards for improving quality of maternal and newborn care in health facilities–experiences from UNICEF’s implementation in three countries of South Asia and sub-Saharan Africa. BMC Health Serv Res. 2018;18:1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Federal Democratic Republic of Ethiopia Ministry of Health. National Strategy for Newborn and Child Survival in Ethiopia, 2015/16–2019/20. Maternal and Child Health Directorate Federal Ministry of Health. AddisAbaba. 2015. [Google Scholar]
- 17. Ajibo BD, Wolka E, Aseffa A, et al. Determinants of low fifth minute Apgar score among newborns delivered by cesarean section at Wolaita Sodo University Comprehensive Specialized Hospital, Southern Ethiopia: an unmatched case control study. BMC Pregnancy Childbirth. 2022;22:665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bayih WA, Tezera TG, Alemu AY, Belay DM, Hailemeskel HS, Ayalew MY. Prevalence and determinants of asphyxia neonatorum among live births at Debre Tabor General Hospital, North Central Ethiopia: a cross-sectional study. Afr Health Sci. 2021;21:385-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tibebu NS, Emiru TD, Tiruneh CM, et al. Magnitude of birth asphyxia and its associated factors among live birth in north Central Ethiopia 2021: an institutional-based cross-sectional study. BMC Pediatr. 2022;22:425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yitayew YA, Yalew ZM. Survival status and predictors of mortality among asphyxiated neonates admitted to the NICU of Dessie comprehensive specialized hospital, Amhara region, Northeast Ethiopia. PLoS ONE. 2022;17:e0279451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cherie N, Mebratu A. Adverse birth out comes and associated factors among delivered mothers in Dessie referral Hospital, North-East Ethiopia. Sci Rep. 2022;12:22514.36581660 [Google Scholar]
- 22. Demographic E. Health Survey: Addis Ababa, Ethiopia, and Calverton. Central Statistical Agency and ORC Macro; 2006. [Google Scholar]
- 23. Macro: CSAaO. Ethiopia Demographic and Health Survey 2011. Central Statistical Agency and ORC Macro; 2011. [Google Scholar]
- 24. Macro: CSAaO. Ethiopia Demographic and Health Survey 2016.Central Statistical Agency and ORC Macro; 2016. [Google Scholar]
- 25. Ethiopia Federal Ministry of Health. Neonatal Intensive Care Unit (NICU) Management Protocol. Federal Ministry of Health; 2021. [Google Scholar]
- 26. Abdo RA, Halil HM, Kebede BA, Anshebo AA, Gejo NG. Prevalence and contributing factors of birth asphyxia among the neonates delivered at Nigist Eleni Mohammed memorial teaching hospital, Southern Ethiopia: a cross-sectional study. BMC Pregnancy Childbirth. 2019;19:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Belachew T, Joseph J. Birth asphyxia and associated factors among newborns delivered in Jimma zone public hospitals, Southwest Ethiopia: a cross-sectional study. J Midwifery Reproductive Health. 2018;6):1289-1295. [Google Scholar]
- 28. Ochoga MO, Ejeliogu EU, Michael A, et al. Prevalence, risk factors and outcomes of perinatal asphyxia in newborns at Benue state university teaching hospital Makurdi. J Res Basic Clin Sci. 2021;2:17-24. [Google Scholar]
- 29. Gebreheat G, Tsegay T, Kiros D, et al. Prevalence and associated factors of perinatal asphyxia among neonates in general hospitals of Tigray, Ethiopia, 2018. BioMed Res Int. 2018;1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dabalo ML, Animen Bante S, Belay Gela G, et al. Perinatal Asphyxia and Its Associated Factors among Live Births in the Public Health Facilities of Bahir Dar City, Northwest Ethiopia, 2021. Int J Pediatr. 2021; 1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Woday A, Muluneh A, St Denis C. Birth asphyxia and its associated factors among newborns in public hospital, northeast Amhara, Ethiopia. PLoS ONE. 2019;14:e0226891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ibrahim NA, Muhye A, Abdulie S. Prevalence of birth asphyxia and associated factors among neonates delivered in Dilchora Referral Hospital. Dire Dawa, Eastern Ethiopia. Clin Mother Child Health. 2017;14:2. [Google Scholar]
- 33. Kebede EB, Akuma AO, Tarfa YB. Perinatal asphyxia among neonates admitted to Jimma Medical Center, Jimma, Ethiopia. Glob Pediatr Health. 2020; 7:1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mulugeta T, Sebsibe G, Fenta FA, Sibhat M. Risk factors of perinatal asphyxia among newborns delivered at public hospitals in Addis Ababa, Ethiopia: a case-control study. Pediatric Health Med Ther. 2020;11:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mitao M, Philemon R, Obure J, Mmbaga BT, Msuya S, Mahande MJ. Risk factors and adverse perinatal outcome associated with low birth weight in Northern Tanzania: a registry-based retrospective cohort study. Asian Pac J Reprod. 2016;5:75-79. [Google Scholar]
- 36. Aslam HM, Saleem S, Afzal R, et al. Risk factors of birth asphyxia. Ital J Pediatr. 2014;40:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Opitasari C, Andayasari L. Maternal Education, Prematurity and the Risk of Birth Asphyxia in Selected Hospitals in Jakarta. National Institute of Health Research and Development, Indonesian Ministry of Health; 2015. [Google Scholar]
- 38. Dashe JS, Bloom SL, Spong CY, Hoffman BL. Williams Obstetrics. McGraw Hill Professional; 2018. [Google Scholar]
- 39. Sattayaruk S, Luengratsameerung S, Wiriyasirivaj B, Phaloprakarn C. Antepartum and intrapartum risk factors associated with low one-minute Apgar score: a case-control study. Thai J Obstet Gynecol. 2014;22:118. [Google Scholar]
- 40. Ige OO. Risk factors and mortality rate of severely asphyxiated neonates in a tertiary center in north-central Nigeria. Jos J Med. 2013;7:10-14. [Google Scholar]
- 41. Zamzami TY, Al-Saedi SA, Marzouki AM, Nasrat HA. Prediction of perinatal hypoxic encephalopathy: proximal risk factors and short-term complications. J Clin Gynecol Obstet. 2014;3:97-104. [Google Scholar]
- 42. Interprofessional Education and Research Committee of the Champlain Maternal Newborn Regional Program (CMNRP). Newborn Adaptation to Extrauterine Life and Newborn Assessment: A Self-Learning Module. 2013;7–11. Available: http://www.cmnrp.ca/uploads/documents/
- 43. Sendeku FW, Azeze GG, Fenta SL. Perinatal asphyxia and its associated factors in Ethiopia: a systematic review and meta-analysis. BMC Pediatr. 2020;20:1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Purwaningsih Y, Dewi YL, Indarto D, Murti B. Factors associated with newborn asphyxia at Dr. Harjono Hospital, Ponorogo, East Java. J Mater Child Health. 2018;3:287-293. [Google Scholar]


