Abstract
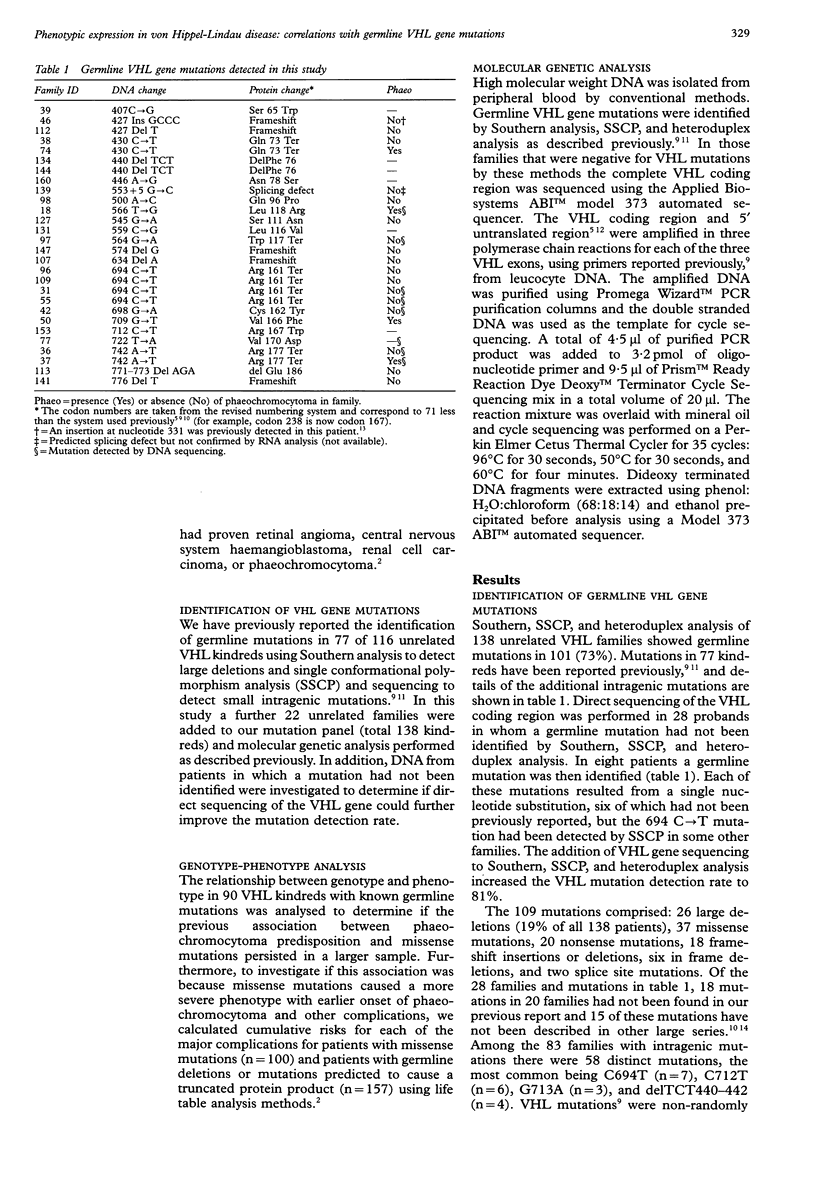
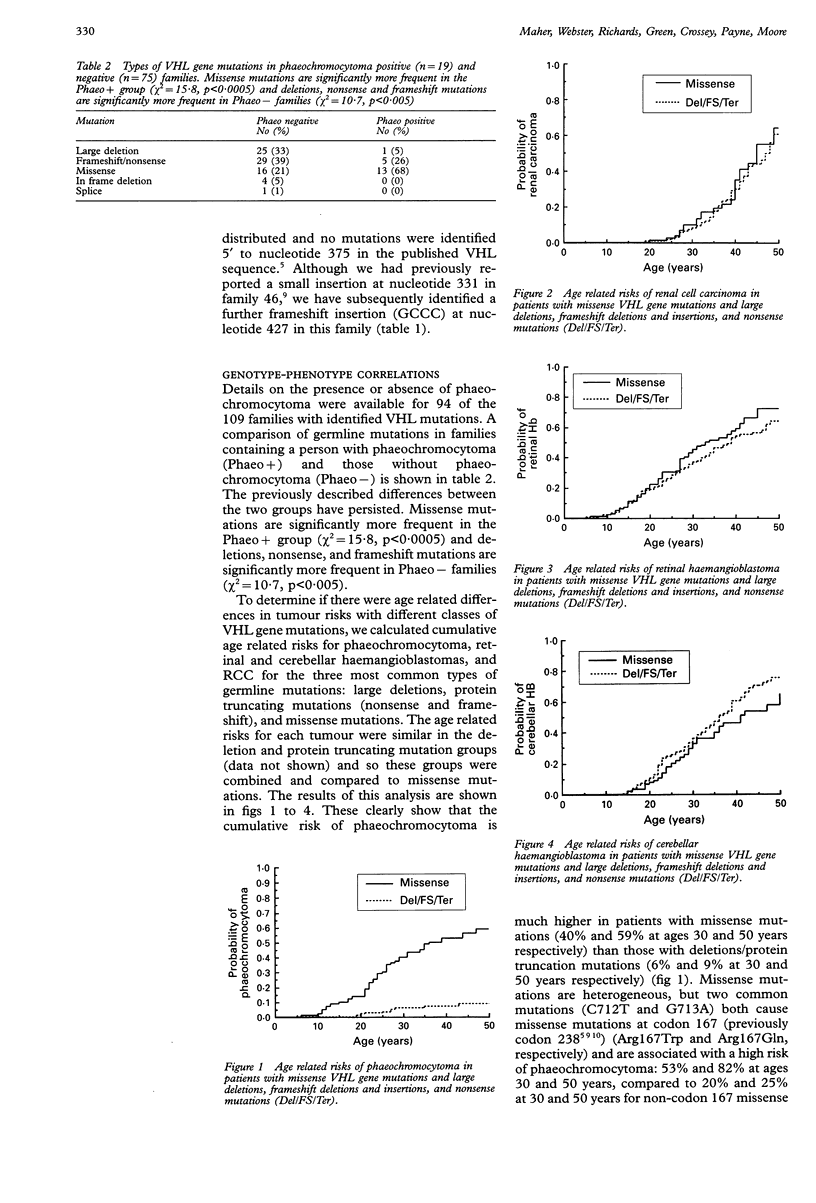
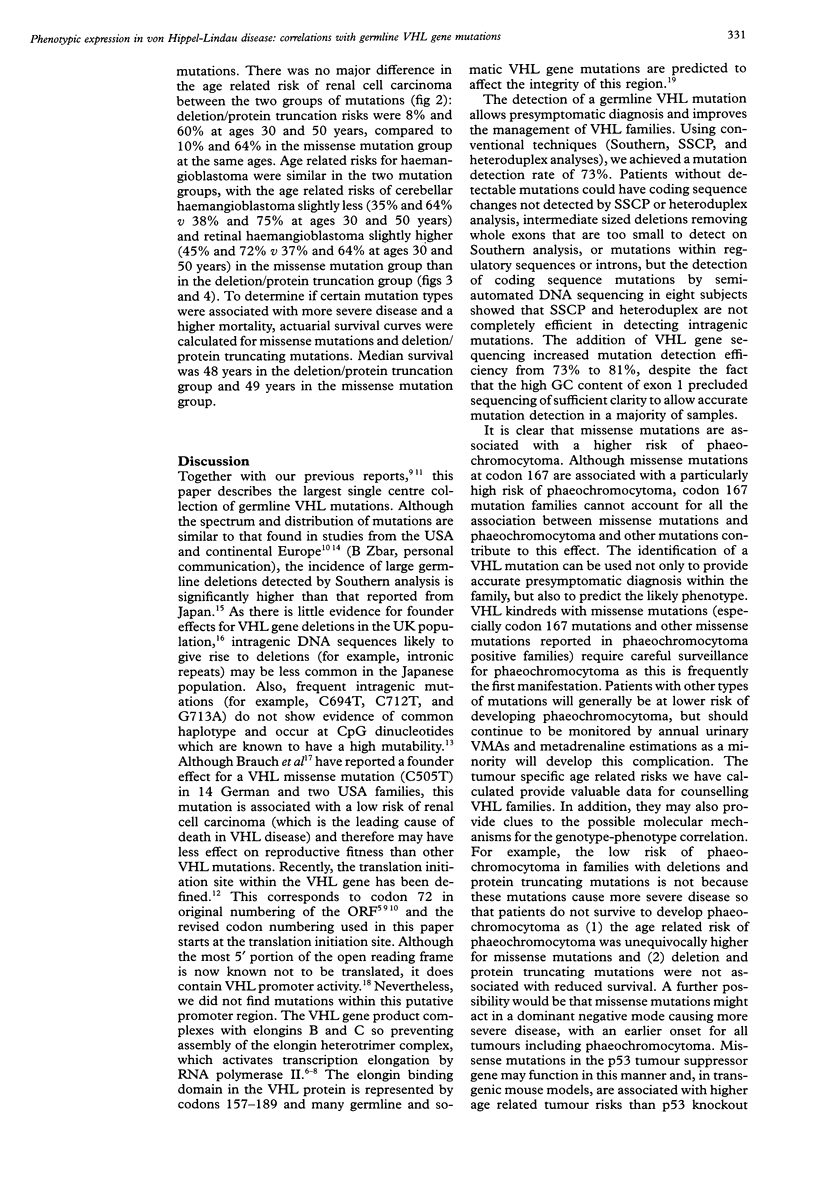
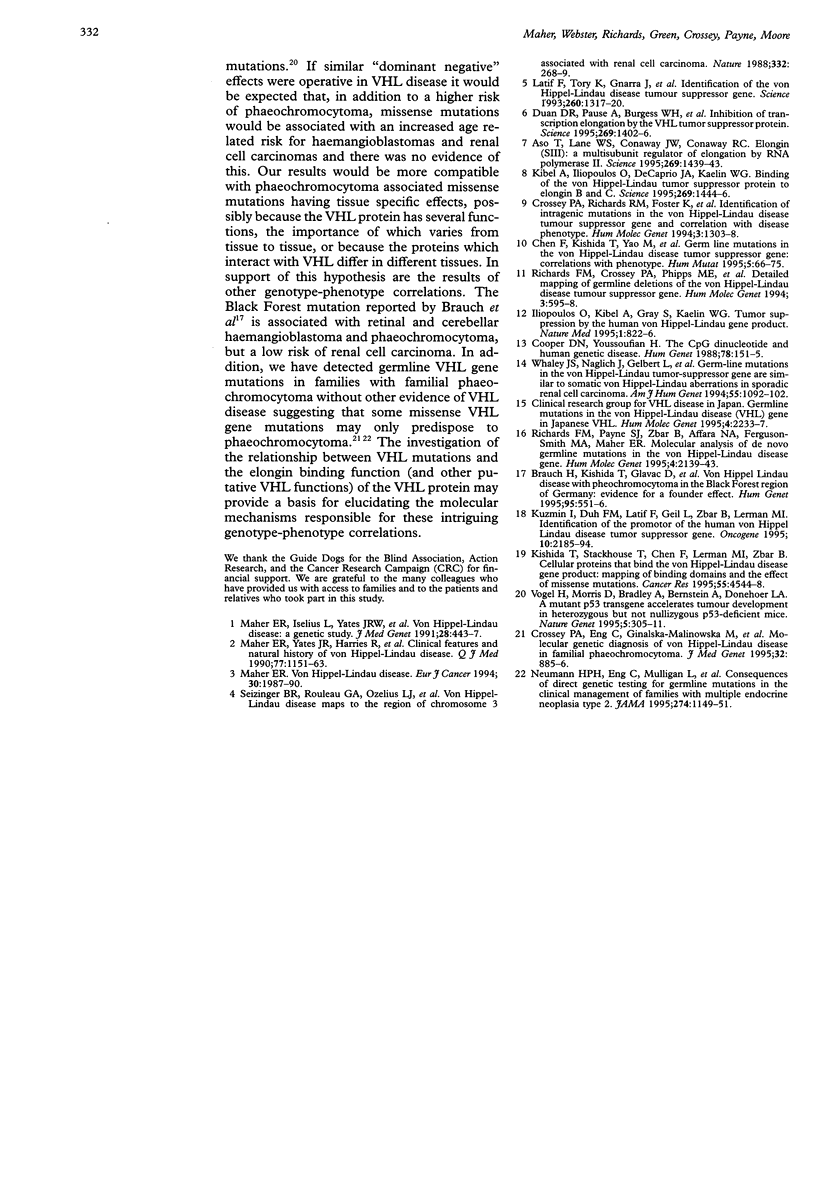
Von Hippel-Lindau disease is an autosomal dominantly inherited familial cancer syndrome predisposing to retinal and central nervous system haemangioblastomas, renal cell carcinoma, and phaeochromocytoma. VHL disease shows variable expression and interfamilial differences in predisposition to phaeochromocytoma. In a previous study of 65 VHL kindreds with defined VHL mutations we detected significant differences between VHL families with and without phaeochromocytoma such that missense mutations were more common and large deletions or protein truncating mutations less frequent in phaeochromocytoma positive families. To investigate the significance and cause of this association further, we studied 138 VHL kindreds for germline mutations and calculated the age related tumour risks for different classes of VHL gene mutations. Using SSCP, heteroduplex and Southern analysis we identified a germline VHL gene mutation in 101 families (73%). Direct sequencing of the VHL coding region further increased the mutation detection rate to 81%. In addition to precise presymptomatic diagnosis, identification of a VHL gene mutation can provide an indication of the likely phenotype. We found that large deletions and mutations predicted to cause a truncated protein were associated with a lower risk of phaeochromocytoma (6% and 9% at 30 and 50 years, respectively) than missense mutations (40% and 59%, respectively) and that missense mutations at codon 167 were associated with a high risk of phaeochromocytoma (53% and 82% at ages 30 and 50 years). Cumulative probabilities of renal cell carcinoma did not differ between the two groups (deletion/ truncation mutations: 8% and 60%, and missense mutations: 10% and 64% at ages 30 and 50 years, respectively). Age related risks for haemangioblastoma were similar in the two mutation groups, with the age related risks of cerebellar haemangioblastoma slightly less (35% and 64% v 38% and 75% at ages 30 and 50 years) and retinal haemangioblastoma slightly higher (45% and 72% v 37% and 64% at ages 30 and 50 years) in the missense mutation group than in the deletion/protein truncation group. These results provide valuable data for counselling VHL families and indicate that specific VHL mutations may be associated with different tumour susceptibility risks. There was no evidence of a generalised increase in age related tumour risks for missense mutations, suggesting that missense mutations predisposing to phaeochromocytoma have tissue specific effects, possibly because the VHL protein has several functions, the importance of which varies from tissue to tissue, or because the proteins which interact with VHL differ between different tissues.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aso T., Lane W. S., Conaway J. W., Conaway R. C. Elongin (SIII): a multisubunit regulator of elongation by RNA polymerase II. Science. 1995 Sep 8;269(5229):1439–1443. doi: 10.1126/science.7660129. [DOI] [PubMed] [Google Scholar]
- Brauch H., Kishida T., Glavac D., Chen F., Pausch F., Höfler H., Latif F., Lerman M. I., Zbar B., Neumann H. P. Von Hippel-Lindau (VHL) disease with pheochromocytoma in the Black Forest region of Germany: evidence for a founder effect. Hum Genet. 1995 May;95(5):551–556. doi: 10.1007/BF00223868. [DOI] [PubMed] [Google Scholar]
- Chen F., Kishida T., Yao M., Hustad T., Glavac D., Dean M., Gnarra J. R., Orcutt M. L., Duh F. M., Glenn G. Germline mutations in the von Hippel-Lindau disease tumor suppressor gene: correlations with phenotype. Hum Mutat. 1995;5(1):66–75. doi: 10.1002/humu.1380050109. [DOI] [PubMed] [Google Scholar]
- Cooper D. N., Youssoufian H. The CpG dinucleotide and human genetic disease. Hum Genet. 1988 Feb;78(2):151–155. doi: 10.1007/BF00278187. [DOI] [PubMed] [Google Scholar]
- Crossey P. A., Eng C., Ginalska-Malinowska M., Lennard T. W., Wheeler D. C., Ponder B. A., Maher E. R. Molecular genetic diagnosis of von Hippel-Lindau disease in familial phaeochromocytoma. J Med Genet. 1995 Nov;32(11):885–886. doi: 10.1136/jmg.32.11.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crossey P. A., Richards F. M., Foster K., Green J. S., Prowse A., Latif F., Lerman M. I., Zbar B., Affara N. A., Ferguson-Smith M. A. Identification of intragenic mutations in the von Hippel-Lindau disease tumour suppressor gene and correlation with disease phenotype. Hum Mol Genet. 1994 Aug;3(8):1303–1308. doi: 10.1093/hmg/3.8.1303. [DOI] [PubMed] [Google Scholar]
- Duan D. R., Pause A., Burgess W. H., Aso T., Chen D. Y., Garrett K. P., Conaway R. C., Conaway J. W., Linehan W. M., Klausner R. D. Inhibition of transcription elongation by the VHL tumor suppressor protein. Science. 1995 Sep 8;269(5229):1402–1406. doi: 10.1126/science.7660122. [DOI] [PubMed] [Google Scholar]
- Harvey M., Vogel H., Morris D., Bradley A., Bernstein A., Donehower L. A. A mutant p53 transgene accelerates tumour development in heterozygous but not nullizygous p53-deficient mice. Nat Genet. 1995 Mar;9(3):305–311. doi: 10.1038/ng0395-305. [DOI] [PubMed] [Google Scholar]
- Iliopoulos O., Kibel A., Gray S., Kaelin W. G., Jr Tumour suppression by the human von Hippel-Lindau gene product. Nat Med. 1995 Aug;1(8):822–826. doi: 10.1038/nm0895-822. [DOI] [PubMed] [Google Scholar]
- Kibel A., Iliopoulos O., DeCaprio J. A., Kaelin W. G., Jr Binding of the von Hippel-Lindau tumor suppressor protein to Elongin B and C. Science. 1995 Sep 8;269(5229):1444–1446. doi: 10.1126/science.7660130. [DOI] [PubMed] [Google Scholar]
- Kishida T., Stackhouse T. M., Chen F., Lerman M. I., Zbar B. Cellular proteins that bind the von Hippel-Lindau disease gene product: mapping of binding domains and the effect of missense mutations. Cancer Res. 1995 Oct 15;55(20):4544–4548. [PubMed] [Google Scholar]
- Kuzmin I., Duh F. M., Latif F., Geil L., Zbar B., Lerman M. I. Identification of the promoter of the human von Hippel-Lindau disease tumor suppressor gene. Oncogene. 1995 Jun 1;10(11):2185–2194. [PubMed] [Google Scholar]
- Maher E. R., Yates J. R., Harries R., Benjamin C., Harris R., Moore A. T., Ferguson-Smith M. A. Clinical features and natural history of von Hippel-Lindau disease. Q J Med. 1990 Nov;77(283):1151–1163. doi: 10.1093/qjmed/77.2.1151. [DOI] [PubMed] [Google Scholar]
- Neumann H. P., Eng C., Mulligan L. M., Glavac D., Zäuner I., Ponder B. A., Crossey P. A., Maher E. R., Brauch H. Consequences of direct genetic testing for germline mutations in the clinical management of families with multiple endocrine neoplasia, type II. JAMA. 1995 Oct 11;274(14):1149–1151. [PubMed] [Google Scholar]
- Richards F. M., Crossey P. A., Phipps M. E., Foster K., Latif F., Evans G., Sampson J., Lerman M. I., Zbar B., Affara N. A. Detailed mapping of germline deletions of the von Hippel-Lindau disease tumour suppressor gene. Hum Mol Genet. 1994 Apr;3(4):595–598. doi: 10.1093/hmg/3.4.595. [DOI] [PubMed] [Google Scholar]
- Richards F. M., Payne S. J., Zbar B., Affara N. A., Ferguson-Smith M. A., Maher E. R. Molecular analysis of de novo germline mutations in the von Hippel-Lindau disease gene. Hum Mol Genet. 1995 Nov;4(11):2139–2143. doi: 10.1093/hmg/4.11.2139. [DOI] [PubMed] [Google Scholar]
- Seizinger B. R., Rouleau G. A., Ozelius L. J., Lane A. H., Farmer G. E., Lamiell J. M., Haines J., Yuen J. W., Collins D., Majoor-Krakauer D. Von Hippel-Lindau disease maps to the region of chromosome 3 associated with renal cell carcinoma. Nature. 1988 Mar 17;332(6161):268–269. doi: 10.1038/332268a0. [DOI] [PubMed] [Google Scholar]
- Whaley J. M., Naglich J., Gelbert L., Hsia Y. E., Lamiell J. M., Green J. S., Collins D., Neumann H. P., Laidlaw J., Li F. P. Germ-line mutations in the von Hippel-Lindau tumor-suppressor gene are similar to somatic von Hippel-Lindau aberrations in sporadic renal cell carcinoma. Am J Hum Genet. 1994 Dec;55(6):1092–1102. [PMC free article] [PubMed] [Google Scholar]


